Contents
What are sweat glands
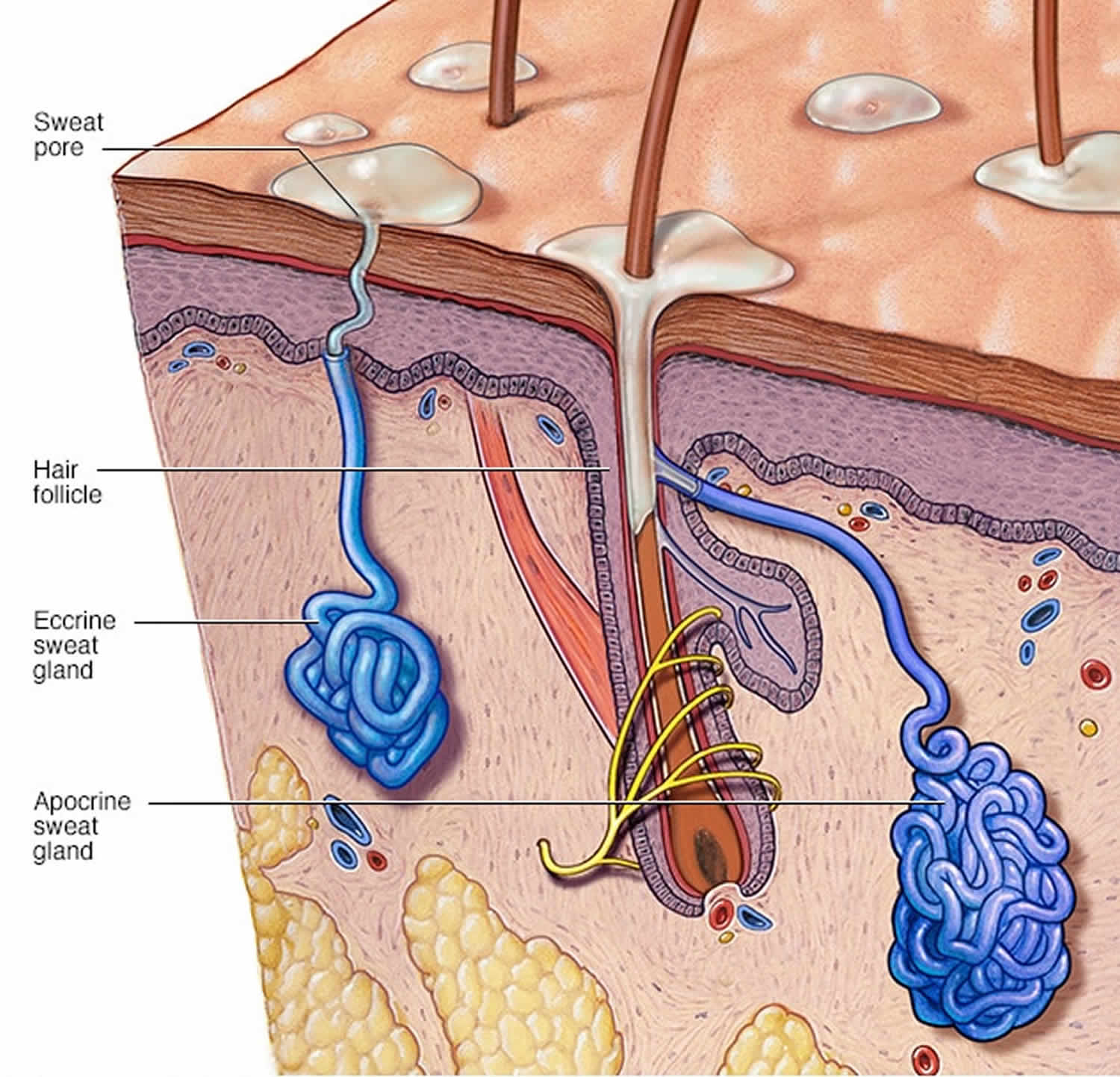
Sweat glands are appendages of the the skin. Your skin has two types of sweat glands: eccrine and apocrine sweat glands. They differ in embryology, distribution, and function. Eccrine sweat glands occur over most of your body and open directly onto the surface of your skin. Apocrine glands open into the hair follicle, leading to the surface of the skin. Apocrine sweat glands develop in areas abundant in hair follicles, such as on your scalp, armpits, groin, periumbilical region, external ear canal, on the eyelids and areola 1. Eccrine and apocrine sweat glands, hair follicles and sebaceous glands (which produce sebum) are often referred to as epidermal adnexal structures.
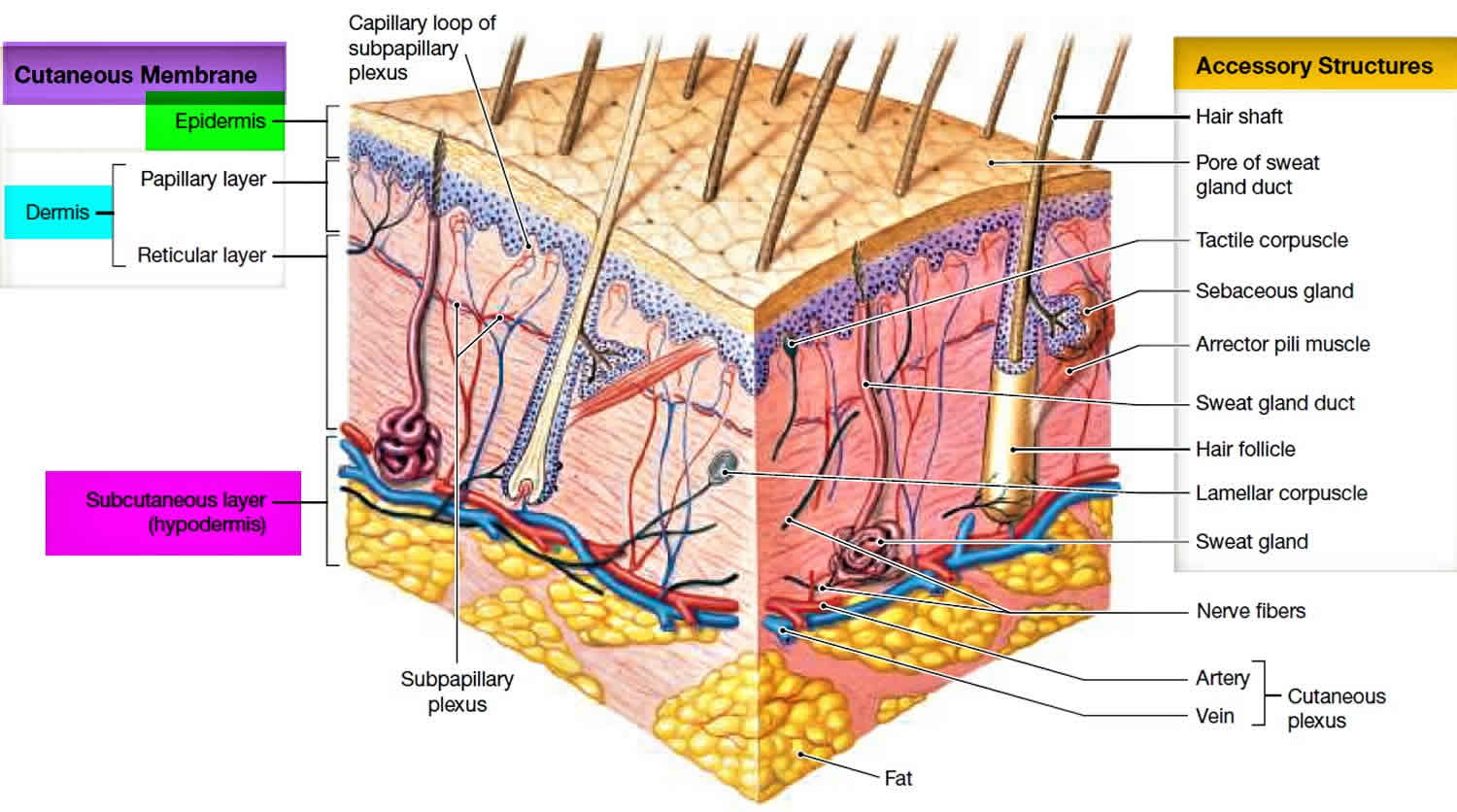
Thin skin covers most of the body and contains sweat glands, in addition to hair follicles, hair arrector muscles, and sebaceous glands. Exceptions are the vermillion border of the lips, external ear canal, nail beds, glans penis, clitoris, and labia minora, which do not contain sweat glands. Thick skin covers the palms, soles, and corresponding surfaces of the fingers and toes. Its epidermis alone is about 0.5 mm thick, due to a very thick surface layer of dead cells called the stratum corneum (see Figure 2). Thick skin has sweat glands but no hair follicles or sebaceous (oil) glands. The rest of the body is covered with thin skin, which has an epidermis about 0.1 mm thick, with a thin stratum corneum. It possesses hair follicles, sebaceous glands, and sweat glands.
Eccrine sweat glands are simple, coiled, tubular glands present throughout your body skin, but are highest in density on the palms and soles. Eccrine sweat glands secrete a salty solution (sweat), which reaches the skin pores via an eccrine duct. Eccrine sweat is a sterile electrolyte solution primarily containing sodium chloride, potassium and bicarbonate, with smaller quantities of various other components such as glucose and antimicrobial peptides. Sweat rate differs depending on site on your body, the degree of thermal or physical stress, and between individuals.
Eccrine sweat glands play an important role in the regulation of your body temperature via evaporative heat loss 2. When the internal temperature of your body rises, eccrine sweat glands release water (sweat) to the skin surface. There, it quickly evaporates, subsequently cooling the skin and blood beneath. This is the most effective means of thermoregulation in humans. Eccrine sweat glands also participate in ion and nitrogenous waste excretion. In response to emotional or thermal stimuli, eccrine sweat glands can produce at least 500 mL to 750 mL in a day 3. Under maximal stimulation, the body can produce 3 liters of eccrine sweat per hour.
In contrast, apocrine glands produce an oily fluid rich in triglycerides and fatty acids – subsequent colonization by anaerobic bacteria results in body odor.
Both eccrine and apocrine sweat glands originate from the epidermis 2. Eccrine sweat glands begin as epithelial cellular buds that grow into the underlying mesenchyme. The glandular secretory components are then formed by elongation of the gland and coiling of the ends. Primordial sweat ducts are formed by epithelial attachments of the developing gland. Finally, the central cells degenerate to form the lumen of the sweat duct. Cells on the periphery of the gland differentiate into secretory and myoepithelial cells. Myoepithelial cells are thought to be specialized smooth muscle cells that function to expel sweat from the gland. Eccrine sweat glands first appear on the palms and soles during the fourth month of gestation; they become functional soon after birth.
On the other hand, apocrine sweat glands do not function until hormonal stimulation during puberty, and their ducts do not open onto the skin surface. This is because these glands originate from the stratum germinativum of the epidermis. Therefore, down-growth does not produce a duct open to the skin surface. Instead, the ducts open into hair follicles and sweat is released through the hair opening in the skin. The canals of these apocrine sweat gland ducts enter the hair follicle superficial to the sebaceous gland, which results in a protein-rich sweat rather than the watery sweat associated with eccrine sweat glands.
Sweat gland lesions generally have variable apocrine or eccrine differentiation. Traditionally these lesions have been categorized under either the apocrine or eccrine groups, but significant overlaps do exist.
Overactive sweat glands also called hyperhydrosis is the excessive excretion of sweat above the quantity needed for thermoregulation. Overactive sweat glands (hyperhydrosis) can be idiopathic or due to another endocrine, neurologic, or infectious disorders. Treatment options include topical medications, oral medications, surgical procedures, or botulinum toxin injection. Bromhidrosis is a similar disorder that presents with excessive malodorous perspiration. It can involve either apocrine or eccrine sweat glands; apocrine bromhidrosis tends to develop after puberty, while eccrine bromhidrosis may develop at any age. It is caused by excessive perspiration that secondarily becomes malodorous by bacterial breakdown. Because poor hygiene most often aggravates bromhidrosis, an effective treatment is improving personal hygiene. Surgical approaches, antibacterial agents, and antiperspirants are treatment options as well.
The sweat glands of patients with cystic fibrosis (CF) are ineffective at reabsorbing salt which has major implications. Cystic fibrosis is an autosomal recessive congenital disease in which the cystic fibrosis transmembrane regulator (CFTR) that normally inhabits the apical membrane of epithelial cells is defective. CFTR is a transmembrane protein that functions as part of a cAMP-regulated chloride ion channel; in normal sweat glands, the ductal epithelium reabsorbs sodium and chloride ions in response to aldosterone so that sweat is hypotonic. In cystic fibrosis patients, the sweat glands fail to reabsorb chloride which affects sodium reabsorption resulting in salty sweat and an inability of sweat glands to participate in ion regulation. Disruption of the same membrane proteins in the respiratory and gastrointestinal epithelium result in accumulations of thick mucus.
Another autosomal recessive congenital disorder that affects sweat glands is lamellar ichthyosis. Infants present with persistent scaling skin and growth of hair may be curtailed. Impairment of sweat gland development often causes infants to suffer in severely hot weather as they cannot maintain thermoregulation through sweating.
Hidradenitis suppurativa is a chronic, inflammatory disease affecting the hair follicles. This ailment has classically been associated with the apocrine sweat glands as it manifests after puberty in the apocrine-gland concentrated areas of the body. However, the pathophysiology involves follicular occlusion rather than an apocrine disorder as previously thought. Patients often present with tender, suppurative subcutaneous nodules and abscesses in the axillae and groin. The lesions can form sinus tracts and extensive scarring.
Hypohydrotic ectodermal dysplasia is a disease characterized by hypotrichosis (decreased growth of scalp and body hair), hypodontia (congenital absence of teeth), and hypohidrosis. The term “hypohidrotic” indicates impairment in the ability to perspire. Patients born with hipohydrotic ectodermal dysplasia have difficulty regulating body temperature and therefore must learn to modify their environment in order to control exposure to heat.
Figure 1. Sweat glands
Figure 2. Skin anatomy
Types of sweat glands
There are two types of sweat glands: eccrine glands and apocrine sweat glands. Both eccrine and apocrine sweat glands secrete in a merocrine manner such that substances are released by exocytosis without damage or loss of the secreting cell 4.
Apocrine sweat glands
Apocrine sweat glands present at birth do not become active until puberty. Apocrine sweat glands, also referred to as odoriferous sweat glands, are known for producing malodorous perspiration. Apocrine sweat glands are large, branched glands that are associated with hair follicles mostly confined to the armpit (axillary) and groin (perineal) regions, including the perianal region, labia majora in women, and the scrotum and prepuce in men. Apocrine sweat glands are also present in the nipples and areolar tissue surrounding the nipples 1.
Apocrine sweat glands start to function at puberty under the stimulation of sex hormones, however, in humans, their function is unknown. Some hypothesize that apocrine glands are responsible for body odor or pheromone production 5. While the initial secretion of apocrine sweat glands is milky, viscous protein-rich product and odorless, bacteria on the skin surface eventually breaks down the fluid, releasing a distinctive odor. Modified apocrine sweat glands include the wax-producing ceruminous glands of the external auditory meatus, the Moll glands found at the free margins of the eyelids, and the mammary glands of the breast.
Apocrine sweat glands receive adrenergic sympathetic innervation. Because apocrine sweat glands respond to norepinephrine, they are involved in emotional sweating due to stress, fear, pain, and sexual stimulation.
Apocrine sweat glands are larger than eccrine glands, with a 10-fold greater diameter 6. Apocrine sweat glands are made up of 2 primary parts: a coiled secretory structure and an accompanying straight duct. The coiled secretory structure, which is the gland itself, is located in the lower dermis or the subcutaneous fat and is composed only of secretory cells. The gland contains multiple large granules. The accompanying straight duct enters the infundibulum. Apocrine sweat glands originate from the hair germ and therefore generally enter the pilosebaceous follicle at its infundibulum; however, occasionally the duct will open directly on the skin surface in proximity to the pilosebaceous follicle.
The gland, or coiled secretory structure, is made up of a single layer of cuboidal or columnar cells, which rest on a layer of myoepithelial cells. The ductal portion is made up of a double layer of basophilic cells, with a periluminal eosinophilic cuticle.
The distinct characteristic of apocrine glands is that they secrete their product through decapitation, which entails membrane budding of the apical cytoplasm. This process involves 3 distinct phases. First, the apical cap is formed. This is followed by formation of a dividing membrane at the base of the apical cap. Finally, tubules form parallel to the dividing membrane, which creates both a base for the secreted apical cap, as well as a roof for the remaining secretory cell.
Primary disorders of apocrine glands include apocrine bromhidrosis, which refers to excessive body odor arising from the secretions of the apocrine glands. This most commonly occurs in the axillae but may occur from secretions of the apocrine glands in the genitals or the plantar aspect of the feet. The second primary disorder of the apocrine glands, apocrine chromhidrosis, is a rare disorder in which the apocrine glands secrete colored apocrine sweat. This is generally found in the axillary and facial apocrine glands but can be seen in the areola apocrine glands. Two secondary disorders of the apocrine glands include Fox-Fordyce disease and hidradenitis suppurativa (acne inversa). In these disorders, apocrine glands are secondarily affected.
Apocrine glands in the mammary region can also transform to apocrine carcinoma, a rare form of female breast cancer with an incidence of 0.5% to 4%.
Finally, apocrine metaplasia can occur, in which non-apocrine cells transform to apocrine phenotype. This is most commonly seen in the breast as fibrocystic change and is a benign lesion of the breast, with no increased risk for breast cancer.
Eccrine sweat glands
Eccrine sweat glands are distributed over the entire body skin, but are highest in density on the palms and soles (with about 700 glands per square centimeter). Eccrine sweat glands secrete a salty solution (sweat), which reaches the skin pores via an eccrine duct. Eccrine sweat is a sterile electrolyte solution primarily containing sodium chloride, potassium and bicarbonate, with smaller quantities of various other components such as glucose and antimicrobial peptides. Sweat rate differs depending on site on the body, the degree of thermal or physical stress, and between individuals. Under maximal stimulation, the body can produce 3 liters of eccrine sweat per hour.
Eccrine sweat glands play an important role in the regulation of body temperature. Eccrine sweat glands receive sympathetic innervation via cholinergic fibers that send impulses in response to changes in core body temperature. Sympathetic innervation to the sweat glands is mediated by the thermoregulatory center of the hypothalamus. A short preganglionic cholinergic fiber is originating from the thoracolumbar region of the spinal cord synapses with the postganglionic neuron via nicotinic acetylcholine. The postganglionic fiber releases acetylcholine, which differs from all other sympathetic postganglionic fibers that release norepinephrine. Cholinergic stimulation of muscarinic receptors induces sweating.
Sweat glands function
Sweating is your body’s mechanism to cool itself. Your nervous system automatically triggers your sweat glands when your body temperature rises. Sweating also normally occurs, especially on your palms, when you’re nervous.
Sweat glands also play a regenerative role in skin damage 2. In second-degree cutaneous burns, which extend into the reticular dermis, regeneration of the epithelium occurs via skin appendages including hair follicles, sebaceous glands, and sweat glands. The epithelial cells surrounding these appendages produce more epithelial cells that progress to form a new epithelium, a process that can take 1 to 3 weeks.
Apocrine sweat glands function
Apocrine sweat glands start to function at puberty under the stimulation of sex hormones, in humans, their function is unknown 5. Some hypothesize that apocrine glands are responsible for body odor or pheromone production. While the initial secretion of apocrine glands is milky and odorless, bacteria on the skin surface eventually breaks down the fluid, releasing a distinctive odor.
Although the exact function of apocrine glands varies depending on the gland’s location, apocrine glands are believed to be an evolutionary remnant of an odorous organ of animals. For example, the scent glands of the skunk are modified apocrine-type structures 6.
Eccrine sweat glands function
Eccrine sweat glands play an important role in the regulation of body temperature. Eccrine glands are distributed over the entire body skin, but are highest in density on the palms and soles. Eccrine glands secrete sweat, which is a weak salt solution that reaches the skin pores via an eccrine duct. These are distributed over the entire body but are most numerous on the palms and soles (with about 700 glands per square centimeter).
Eccrine sweat is a sterile electrolyte solution primarily containing sodium chloride, potassium and bicarbonate, with smaller quantities of various other components such as glucose and antimicrobial peptides. Sweat rate differs depending on site on the body, the degree of thermal or physical stress, and between individuals.
Eccrine sweat glands also participate in ion and nitrogenous waste excretion. In response to emotional or thermal stimuli, eccrine sweat glands can produce at least 500 mL to 750 mL in a day 3. Under maximal stimulation, the body can produce 3 litres of eccrine sweat per hour.
Where are sweat glands located
Apocrine sweat glands, also referred to as odoriferous sweat glands, are known for producing malodorous perspiration. Apocrine sweat glands are large, branched glands that are mostly confined to the armpit (axillary) and groin (perineal) regions, including the perianal region, labia majora in women, and the scrotum and prepuce in men. Apocrine sweat glands are also present in the nipples and areolar tissue surrounding the nipples, periumbilical region, external auditory canals, and on the eyelids 1. Some apocrine glands have specific names, for example, those on the eyelids are referred to as Moll’s glands, and those on the external auditory meatus are termed ceruminous glands. While they can be found in many locations on the body, they secrete specific products at each distinct location.
Eccrine sweat glands are distributed over the entire body skin, but are highest in density on the palms and soles (with about 700 glands per square centimeter).
Overactive sweat glands
Overactive sweat glands is also called hyperhidrosis is the name given to abnormally excessive and uncontrollable sweating that’s not necessarily related to heat or exercise. With overactive sweat glands you may sweat so much that it soaks through your clothes or drips off your hands. Besides disrupting normal daily activities, this type of heavy sweating can cause social anxiety, embarrassment and interferes with many daily activities.
Overactive sweat glands (hyperhidrosis) can be localized or generalized.
- Localized hyperhidrosis affects armpits, palms, soles, face or other sites
- Generalized hyperhidrosis affects most or all of the body
Overactive sweat glands (hyperhidrosis) can be primary or secondary.
Primary hyperhidrosis:
- Starts in childhood or adolescence
- May persist lifelong or improve with age
- There may be a family history
- Tends to involve armpits, palms and or soles symmetrically
- Usually, sweating reduces at night and disappears during sleep
Secondary hyperhidrosis:
- Less common than primary hyperhidrosis
- More likely to be unilateral and asymmetrical, or generalised
- Can occur at night or during sleep.
- Due to endocrine or neurological conditions
Primary hyperhidrosis is reported to affect 1–3% of the US population and nearly always starts during childhood or adolescence. The tendency may be inherited, and it is reported to be particularly prevalent in Japanese people.
Secondary hyperhidrosis is less common and can present at any age. Sometimes an underlying cause may be found and treated.
Overactive sweat glands treatment usually helps, beginning with prescription-strength antiperspirants. If antiperspirants don’t help, you may need to try different medications and therapies. In severe cases, your doctor may suggest surgery either to remove the sweat glands or to disconnect the nerves responsible for the overproduction of sweat.
Sometimes excessive sweating is a sign of a serious condition.
Seek immediate medical attention if your heavy sweating is accompanied by lightheadedness, chest pain or nausea.
See your doctor if:
- Sweating disrupts your daily routine
- Sweating causes emotional distress or social withdrawal
- You suddenly begin to sweat more than usual
- You experience night sweats for no apparent reason
Overactive sweat glands symptoms
Most people sweat when they exercise or exert themselves, are in a hot environment, or are anxious or under stress. The excessive sweating experienced with hyperhidrosis far exceeds such normal sweating.
The type of hyperhidrosis that usually affects the hands, feet, underarms or face causes at least one episode a week, during waking hours. And the sweating usually occurs on both sides of the body.
Overactive sweat glands causes
The most common form of hyperhidrosis is called primary focal (essential) hyperhidrosis. With this type, the nerves responsible for signaling your sweat glands become overactive, even though they haven’t been triggered by physical activity or a rise in temperature. With stress or nervousness, the problem becomes even worse. This type usually affects your palms and soles and sometimes your face. There is no medical cause for this type of hyperhidrosis. It may have a hereditary component, because it sometimes runs in families.
Primary hyperhidrosis appears to be due to overactivity of the hypothalamic thermoregulatory centre in the brain and is transmitted via the sympathetic nervous system to the eccrine sweat gland.
Triggers to attacks of sweating may include:
- Hot weather
- Exercise
- Fever
- Anxiety
- Spicy food
Secondary hyperhidrosis occurs when excess sweating is due to a medical condition. It’s the less common type. It’s more likely to cause sweating all over your body. Conditions that may lead to heavy sweating include:
- Diabetes
- Menopause hot flashes
- Thyroid problems
- Low blood sugar
- Some types of cancer
- Heart attack
- Nervous system disorders
- Infections
Certain medications also can lead to heavy sweating, as can opioid withdrawal.
Causes of secondary localized hyperhidrosis include:
- Stroke
- Spinal nerve damage
- Peripheral nerve damage
- Surgical sympathectomy
- Neuropathy
- A brain tumour
- Chronic anxiety disorder
Causes of secondary generalized hyperhidrosis include:
- Obesity
- Diabetes
- Menopause
- Overactive thyroid
- Cardiovascular disorders
- Respiratory failure
- Other endocrine tumors, eg phaeochromocytoma
- Parkinson disease
- Hodgkin lymphoma
- Drugs: alcohol, caffeine, corticosteroids, cholinesterase inhibitors, tricyclic antidepressants, selective serotonin reuptake inhibitors, nicotinamide and opioids
Overactive sweat glands complications
Complications of hyperhidrosis include:
- Infections. People who sweat profusely are more prone to skin infections.
- Social and emotional effects. Having clammy or dripping hands and perspiration-soaked clothes can be embarrassing. Your condition may affect your pursuit of work and educational goals.
Overactive sweat glands diagnosis
During your appointment, your doctor will ask about your medical history and symptoms. You may also need a physical exam or tests to further evaluate the cause of your condition.
Hyperhidrosis is usually diagnosed clinically. Tests relate to the potential underlying cause of hyperhidrosis and are rarely necessary for primary hyperhidrosis.
Lab tests
Your doctor may recommend blood, urine or other lab tests to see if your sweating is caused by another medical condition, such as an overactive thyroid (hyperthyroidism) or low blood sugar (hypoglycemia).
Sweat tests
A number of tests are available to pinpoint the areas of sweating and estimate the severity of your condition, including an iodine-starch test, skin conductance and a thermoregulatory sweat test.
The precise site of localized hyperhidrosis can be revealed using the Minor test.
- Iodine (orange) is painted onto the skin and air dried.
- Starch (white) is dusted on the iodine.
- Sweating is revealed by a change to dark blue/black color.
Overactive sweat glands treatment
If an underlying medical condition is contributing to the problem, that condition will be treated first. If no clear cause can be found, treatment focuses on controlling excessive sweating. Sometimes you may need to try a combination of treatments. And even if your sweating improves after treatment, it may recur.
Medications
Drugs used to treat hyperhidrosis include:
- Prescription antiperspirant. Your doctor may prescribe an antiperspirant with aluminum chloride (Drysol, Xerac Ac). This product can cause skin and eye irritation. Antiperspirants contain 10–25% aluminium salts to reduce sweating; “clinical strength” aluminium zirconium salts are more effective than aluminium chloride. It’s usually applied to the affected skin before you go to bed. Then you wash the product off when you get up, taking care to not get any in your eyes. If your skin becomes irritated, hydrocortisone cream might help. Antiperspirants are available as a cream, aerosol spray, stick, roll-on, wipe, powder, and paint. Specific products are available for different body sites such as underarms, other skin folds, face, hands and feet.
- Topical anticholinergics. A prescription cream that contains glycopyrrolate and oxybutynin gel have been successful in reducing sweating that affects the face and head; cloths containing glycopyrronium tosylate (Qbrexza™) were approved by the FDA in July 2018 for axillary hyperhidrosis in adults and children 9 years of age and older. Dusting powder is available containing the anticholinergic drug, diphemanil 2%.
- Nerve-blocking medications. Some oral medications block the chemicals that permit certain nerves to communicate with each other. This can reduce sweating in some people. Possible side effects include dry mouth, blurred vision and bladder problems.
- Antidepressants. Some medications used for depression can also decrease sweating. In addition, they may help decrease the anxiety that worsens the hyperhidrosis.
- Botulinum toxin injections. Treatment with botulinum toxin (Botox, Myobloc, others) temporarily blocks the nerves that cause sweating. Your skin will be iced or anesthetized first. Each affected area of your body will need several injections. The effects last six to 12 months, and then the treatment needs to be repeated. This treatment can be painful, and some people experience temporary muscle weakness in the treated area.
Oral medications
Oral anticholinergic drugs
- Available drugs are propantheline 15–30 mg up to three times daily, oxybutynin 2.5–7.5 mg daily, benztropine, glycopyrrolate (unapproved).
- They can cause dry mouth, and less often, blurred vision, constipation, dizziness, palpitations and other side effects.
- People with glaucoma or urinary retention should not take them.
- Caution in elderly patients: increased risk of side effects is reported, including dementia.
- Oral anticholinergics may interact with other medications.
Beta-blockers
- Beta blockers block the physical effects of anxiety.
- They may aggravate asthma or symptoms of peripheral vascular disease.
Calcium channel blockers, alpha adrenergic agonists (clonidine) nonsteroidal anti-inflammatory drugs and anxiolytics may also be useful for some patients.
Surgical and other procedures
Surgical removal of axillary sweat glands
Overactive sweat glands in the armpits may be removed by several methods, usually under local anaesthetic.
- Tumescent liposuction (sucking them out)
- Subcutaneous curettage (scraping them out). If excessive sweating occurs just in your armpits, removing the sweat glands there may help. A minimally invasive technique called suction curettage may be an option, too, if you aren’t responding to other treatments.
- Microwave thermolysis (the MiraDry® system approved by FDA in 2011). With this therapy, a device that delivers microwave energy is used to destroy sweat glands. Treatments involve two 20- to 30-minute sessions, three months apart. Possible side effects are a change in skin sensation and some discomfort. This therapy may be expensive and not widely available.
- Subdermal Nd:YAG laser
- High-intensity micro-focused ultrasound (experimental)
- Surgery to cut out the sweat gland-bearing skin of the armpits. If a large area needs to be removed, it may be repaired using a skin graft
Other hyperhidrosis treatments include:
Nerve surgery (sympathectomy). During this procedure, the surgeon cuts, burns or clamps the spinal nerves that control sweating in your hands. In some cases, this procedure triggers excessive sweating in other areas of your body (compensatory sweating). Surgery is generally not an option for isolated head and neck sweating. A variation on this procedure interrupts the nerve signals without removing the sympathetic nerve (sympathotomy).
Division of the sympathetic spinal nerves by chemical or surgical endoscopic thoracic sympathectomy (ETS) may reduce sweating of face (T2 ganglion) or armpit and hand (T3 or T4 ganglion) but is reserved for the most severely affected individuals due to potential risks and complications.
- Hyperhidrosis may recur in up to 15% of cases.
- Sympathectomy is often accompanied by undesirable skin warmth and dryness.
- New-onset hyperhidrosis of other sites occurs in 50–90% of patients, and is severe in 2%. It is reported to be less frequent after T4 ganglion sympathectomy compared with T2 ganglion sympathectomy.
- Serious complications include Horner syndrome, pneumothorax (in up to 10%), pneumonia and persistent pain (in fewer than 2%).
Lumbar sympathectomy is not recommended for hyperhidrosis affecting the feet, as it can interfere with sexual function.
Lifestyle and home remedies
The following suggestions may help you cope with sweating and body odor:
- Use antiperspirant. Nonprescription antiperspirants contain aluminum-based compounds that temporarily block the sweat pore. This reduces the amount of sweat that reaches your skin. This type of product may help with minor hyperhidrosis.
- Apply astringents. Apply over-the-counter products containing tannic acid (Zilactin) to the affected area.
- Bathe daily. Regular bathing helps keep the number of bacteria on your skin in check. Dry yourself thoroughly, especially between the toes and under the arms.
- Choose shoes and socks made of natural materials. Shoes made of natural materials, such as leather, can help prevent sweaty feet by allowing your feet to breathe. When you’re active, moisture-wicking athletic socks are a good choice.
- Change your socks often. Change socks or hose once or twice a day, drying your feet thoroughly each time. You may want to try pantyhose with cotton soles.
- Use over-the-counter foot powders to help absorb sweat.
- Air your feet. Go barefoot when you can, or at least slip out of your shoes now and then.
- Choose clothing to suit your activity. Generally, wear natural fabrics, such as cotton, wool and silk, which allow your skin to breathe. When you exercise, you might prefer fabrics designed to wick moisture away from your skin.
- Try relaxation techniques. Consider relaxation techniques such as yoga, meditation and biofeedback. These can help you learn to control the stress that triggers sweating.
Coping and support
Hyperhidrosis can be the cause of discomfort and embarrassment. You may have trouble working or enjoying recreational activities because of wet hands or feet or wet stains on clothing. You might feel anxious about your symptoms and become withdrawn or self-conscious. You may be frustrated or upset by other people’s reactions.
Besides talking with your doctor, you may want to talk with a counselor or a medical social worker. Or you may find it helpful to talk with other people who have hyperhidrosis.
Bromhidrosis
Bromhidrosis is a condition of abnormal or offensive body odor, to a large extent determined by apocrine gland secretion, although other sources may play a role. Sudoriferous (sweat) glands are divided into two types: apocrine and eccrine. There is some cross-over.
Eccrine glands
- Found over your entire body and produce a dilute salt solution in response to increased body temperature.
- Eccrine sweat is normally odorless but can start to smell if bacteria get a chance to break down the stale sweat. It can also assume an offensive odor after ingestion of various substances, including foods (e.g. garlic, curry), alcohol, or certain medications.
Apocrine glands
- Found in limited areas, most notably the underarms, breasts and groin region and produce a thick secretion that contains pheromones (“personal scent”).
- Apocrine sweat is odorless when it first appears on the skin but within an hour bacteria that normally live on the skin break down the sweat to produce an offensive body odor.
- Body odor is worse if there are more bacteria present or the level of apocrine sweat production is high.
Apocrine bromhidrosis is the most common type of bromhidrosis and results from the bacterial breakdown of apocrine sweat, essentially all within the armpit area. Fatty acids and ammonia are the major products of bacterial breakdown and the odor has been described as pungent, rancid, musty or “sour and sweet”.
Although both types of bromhidrosis may occur in people of all races, sex and age, some differences do exist between the two types.
Who causes bromhidrosis?
Apocrine bromhidrosis
- Possibly associated with a positive family history
- Only occurs after puberty, as the apocrine glands are not active until puberty is reached
- More common in men than women, which may be a reflection of greater apocrine gland activity in men than in women
- Skin usually appears normal except when bromhidrosis is associated with concomitant skin condition such as erythrasma
- Corynebacterium species are the most common bacteria found in the armpit and have been shown to produce the offensively smelling fatty acids.
Eccrine bromhidrosis
- Occurs in all races
- May be rarely caused by metabolic disorders, e.g. amino acid disturbances (trimethylaminuria [fish odour syndrome]), sweaty feet syndrome, odour of cat syndrome
- Possibly caused by ingestion of certain foods or medications
- Bromhidrosis caused by bacterial degradation of the skin protein keratin may be associated with maceration and a thick mat of moist keratin present on the skin
- The role of excessive eccrine secretion (hyperhidrosis) in causing bromhidrosis is unclear. It may promote the spread of apocrine sweat and cause further
- bacterial overgrowth and decomposition, or it may improve the symptoms of bromhidrosis by flushing away the more smelly apocrine sweat.
Bromhidrosis diagnosis
The clinician’s perception of smell is the only tool needed to diagnose bromhidrosis. Taking a medical history may reveal diseases or conditions that contribute to the occurrence of bromhidrosis e.g. obesity, diabetes mellitus, and intertrigo.
One distinction the clinician must be aware of is the difference between the true bromhidrosis patient and the bromhidrosiphobic individual. Bromhidrosiphobic patients have a morbid dread of bodily odors and their sensory delusions can be an early warning sign of schizophrenia.
Bromhidrosis treatment
The two main factors to consider when treating bromhidrosis are to:
- Keep the number of naturally occurring skin bacteria to a minimum
- Keep skin in the area, namely the armpit in apocrine bromhidrosis, as dry as possible
Improved hygiene and topical therapy are the main treatment options for mild cases of bromhidrosis and may include the following.
- Washing the underarm at least twice daily with germicidal soap
- Regular shaving of underarm hair to prevent accumulation of bacteria and sweat on hair shafts
- Prompt removal of sweaty clothing
- Try anti-odor anti-microbial socks and other garments impregnated with silver or copper
- Use of topical deodorants
- Treatment of coexisting skin conditions such as intertrigo, erythrasma and trichomycosis axillaris
- Electrolysis to remove hair shaft and follicle
If hyperhidrosis is a contributing factor, this needs to be treated first, usually with the use of antiperspirants.
The treatments described above do not offer a cure for bromhidrosis and results can often be short lived and incomplete. A visit to a specialist physician may provide more permanent treatment options, and include:
- removal of apocrine sweat glands by superficial liposuction
- removal of apocrine sweat glands by surgical excision
If hyperhidrosis is a contributing factor, this needs to be treated first, usually with the use of antiperspirants. If this fails and the hyperhidrosis is a problem in its own right, then the following options may be considered:
- anticholinergic or beta-blocking drugs (beta blockers)
- iontophoresis
- botulinum toxin injection
- chemical or surgical sympathectomy
- microwave treatment of axillary eccrine glands
These treatments may not help the bromhidrosis, however, as this condition is often independent of hyperhidrosis and, as mentioned above, may in some cases be lessened by associated hyperhidrosis.
Inflammation of sweat glands
Hidradenitis suppurativa also known as acne inversa, is a rare, chronic, inflammatory disease affecting the hair follicles that features small, boil-like nodules and abscesses under the skin that culminate in pus-like discharge, difficult-to-heal open wounds (sinuses) and scarring. Hidradenitis suppurativa has classically been associated with the apocrine sweat glands as it manifests after puberty in the apocrine-gland concentrated areas of the body. However, the hidradenitis suppurativa pathophysiology involves follicular occlusion rather than an apocrine disorder as previously thought. Patients often present with tender, suppurative subcutaneous nodules and abscesses in the axillae and groin. The lesions can form sinus tracts and extensive scarring.
Hidradenitis suppurativa also has significant psychological impact and many patients suffer from impairment of body image, depression and anxiety.
Hidradenitis suppurativa typically develop where the skin rubs together, such as the armpits, the groin, between the buttocks and under the breasts. The lumps may break open and smell or cause tunnels under the skin.
Hidradenitis suppurativa tends to start after puberty. It can persist for many years and worsen over time, with serious effects on your daily life and emotional well-being. Early diagnosis and treatment can help manage the symptoms, keep new lumps from forming and prevent complications, such as scarring or depression.
Early detection of hidradenitis suppurativa is key to getting effective treatment. See your doctor if your condition:
- Is painful
- Doesn’t improve in a few weeks
- Returns within weeks of treatment
- Appears in several locations
- Recurs often
If you’ve already received a diagnosis of hidradenitis suppurativa, keep in mind that the warning signs of a disease flare (recurrence) are often similar to those that occurred originally. Also pay attention to any new signs or symptoms. These may indicate either a recurrence or a complication of treatment.
Inflammation of sweat glands causes
Hidradenitis suppurativa develops when hair follicles become blocked and inflamed. No one knows exactly why this blockage occurs. Factors that may play a role include hormones, metabolic syndrome, genetics, an irregular immune system response, smoking and excess weight.
Hidradenitis suppurativa is not caused by an infection and can’t be transmitted sexually. It’s not contagious and is not due to poor hygiene.
Risk factors for hidradenitis suppurativa
Factors that may increase your risk may include:
- Age. Hidradenitis suppurativa most commonly occurs in women between the ages of 20 and 29. An early age of onset may be associated with developing more widespread disease.
- Your sex. Women are more likely to develop hidradenitis suppurativa than are men.
- Family history. A tendency to develop hidradenitis suppurativa can be inherited.
- Having certain other conditions. Hidradenitis suppurativa can be associated with several other conditions, including arthritis, severe acne, obesity, inflammatory bowel disease, Crohn’s disease, metabolic syndrome and diabetes.
- Smoking. Smoking tobacco has been linked to hidradenitis suppurativa.
Inflammation of sweat glands symptoms
Hidradenitis suppurativa commonly occurs around hair follicles with many oil and sweat glands, such as in the armpits, groin and anal area. It may also occur where skin rubs together, such as the inner thighs, under the breasts and between the buttocks. Hidradenitis suppurativa can affect one spot or multiple areas of the body.
Signs and symptoms of hidradenitis suppurativa include:
- Blackheads. Small pitted areas of skin containing blackheads — often appearing in pairs or a “double-barreled” pattern — are a common feature.
- Red, tender bumps. These bumps often enlarge, break open and drain pus. The drainage may have an odor. Itching and burning may accompany the bumps. They usually appear in areas where skin rubs against skin.
- Painful, pea-sized lumps. These hard lumps, which develop under the skin, may persist for years, enlarge and become inflamed.
- Tunnels. Over time, tracts connecting the lumps may form under the skin. These wounds heal very slowly, if at all, and can leak pus.
Hidradenitis suppurativa usually starts between puberty and age 40 with a single, painful bump that persists for weeks or months. For some people, the disease progressively worsens and affects multiple areas of their body. Other people experience only mild symptoms. Excess weight, stress, hormonal changes, heat or humidity can worsen symptoms. In women, the disease severity may lessen after menopause.
Inflammation of sweat glands complications
Persistent and severe hidradenitis suppurativa often causes complications, including:
- Infection. The affected area is susceptible to infection.
- Scars and skin changes. The wounds may heal but leave rope-like scars, pitted skin or patches of skin that are darker than normal.
- Restricted movement. Sores and scar tissue may cause limited or painful movement, especially when the disease affects the armpits or thighs.
- Obstructed lymph drainage. The most common sites for hidradenitis suppurativa also contain many lymph nodes. Scar tissue can interfere with the lymph drainage system, which may result in swelling in the arms, legs or genitals.
- Social isolation. The location, drainage and odor of the sores can cause embarrassment and reluctance to go out in public, leading to sadness or depression.
- Cancer. Rarely, patients with advanced hidradenitis suppurativa can develop squamous cell carcinoma in the affected skin.
Inflammation of sweat glands diagnosis
Your doctor will ask you about your signs and symptoms, examine the affected skin and take your medical history.
No laboratory test is available to diagnose hidradenitis suppurativa. But if pus or drainage is present, your doctor might send a sample of the fluid to a laboratory for testing to rule out a boil infection or other skin disorders.
Inflammation of sweat glands treatment
There is no cure for hidradenitis suppurativa. But early and long-term treatment may help control pain, promote wound healing, keep new lumps from forming and prevent complications.
Several treatment options are available. Talk with your doctor about the risks and benefits of each and which combination of self-care, drugs or surgical procedures are right for you.
Medications
Your doctor might prescribe one or more of the following types of medications:
- Topical and oral drugs. These include antibiotics and drugs derived from vitamin A (retinoids).
- Other drugs that reduce inflammation. Injecting steroid medications directly into the tender nodule can reduce inflammation. Oral steroids, such as prednisone, can also help. But long-term use of prednisone has many side effects, including bone thinning (osteoporosis).
- Hormones. Small studies comparing oral antibiotics with hormonal therapy showed the hormonal therapy to be as effective as antibiotics in treating sores of hidradenitis suppurativa. Further study is needed. Hormonal therapy is not suitable for pregnant women due to the risk of side effects.
- Drugs that suppress the immune system. The drugs infliximab (Remicade) and adalimumab (Humira) show promise in the treatment of hidradenitis suppurativa. These “biologics” are TNF inhibitors. They work by neutralizing an immune system protein known as tumor necrosis factor (TNF). Researchers continue to assess these and similar drugs. Possible side effects include an increased risk of infection, heart failure and certain types of cancers.
- Pain medication. If over-the-counter pain relievers don’t help, your doctor may prescribe a stronger type. Examples include a fentanyl patch, codeine, morphine, gabapentin and pregabalin.
Surgery and other procedures
Hidradenitis suppurativa may be treated with various surgical approaches. The method used depends on the extent and location of the wounds, among other factors.
- Uncovering the tunnels. Known as unroofing, this procedure is gaining favor over incision and drainage. Your doctor cuts away the skin and flesh that cover any interconnected tunnels. This solution usually doesn’t have to be repeated.
- Punch debridement. This procedure is also called mini-unroofing and may be used to remove a single inflamed nodule.
Incision and drainage. Surgical drainage may be an option when the disease involves a single small area. This treatment generally provides short-term pain relief, but the sores tend to recur. - Tissue-sparing excision with electrosurgery. This may be an option for people with severe hidradenitis suppurativa. It combines skin-tissue-sparing excision with electrosurgical peeling (STEEP). The goal is to remove diseased tissue and preserve healthy tissue. You will be given general anesthesia for the STEEP procedure.
- Surgical removal. Surgical treatment of recurrent or severe symptoms involves removal of all involved skin. A skin graft may be necessary to close the wound. Even after you have surgery, sores may still occur in other areas. In men whose condition involves the area between the anus and scrotum, surgical removal of the scrotum is almost always necessary.
Lifestyle and home remedies
Mild hidradenitis suppurativa may be treated with only self-care measures. But self-care is also an important complement to any medical treatment you may be getting. The following suggestions may help relieve discomfort and speed healing of sores:
- Follow a daily skin-care routine. Gently wash your body with a nonsoap cleanser such as Cetaphil. Use only your hands, not washcloths, loofahs or other items that might irritate the skin. If odor is a concern, try an antibacterial body wash. Then apply an over-the-counter antibiotic cream. It might also help to apply extra absorbent powder or zinc oxide. Using antiperspirants may help keep the skin dry. Stop using any product that irritates your skin.
- Manage your pain. Gently applying a wet, warm washcloth, teabag or other sort of compress can help reduce swelling and ease pain. Keep it on for about 10 minutes. Ask your doctor to recommend the most appropriate pain reliever. And talk with your doctor about how to properly dress and care for your wounds at home.
- Avoid tight clothes and irritating products. Wear loose, lightweight clothes to reduce friction. Some women find that using tampons rather than sanitary pads causes less friction with the skin. Use detergents and other products that are free of perfumes, dyes and enzymes.
- Avoid injuring the skin. For example, don’t squeeze the pimples and sores. And stop shaving affected skin.
- Keep a healthy weight and stay active. Not being at a healthy weight can make symptoms worse. Try to find activities that don’t irritate your skin.
- Consider altering your diet. In an informal study, 47 people with hidradenitis suppurativa gave up dairy products and processed sugar and flour. Of those, 83 percent experienced reduced symptoms. Also, a study reported on 12 people being treated for hidradenitis suppurativa who avoided beer and other foods containing brewer’s yeast or wheat. They all saw their symptoms clear up within a year.
- Avoid all tobacco products. If you smoke, try to quit. Smoking and other tobacco use may play a role in making hidradenitis suppurativa worse.
Alternative medicine
- Zinc supplements taken daily may help reduce inflammation and prevent new outbreaks.
Coping and support
One of the greatest challenges of living with hidradenitis suppurativa may be coping with pain and embarrassment. Painful sores might affect your sleep, mobility or sex life. If the sores are draining pus, they can smell, despite good self-care. You might feel anxious and become withdrawn, self-conscious or depressed.
Try to find support among your family and friends. You may also find the concern and understanding of other people with hidradenitis suppurativa comforting. Ask your doctor for a referral to a mental health professional or contact information for a support group.
- Agarwal S, Krishnamurthy K. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jan 25, 2019. Histology, Skin.[↩][↩][↩]
- Hodge BD, Brodell RT. Anatomy, Skin Sweat Glands. [Updated 2019 Apr 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482278[↩][↩][↩]
- Grubbs H, Morrison M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Dec 6, 2018. Embryology, Hair[↩][↩]
- Jung D, Kim YB, Lee JB, Muhamed AMC, Lee JY. Sweating distribution and active sweat glands on the scalp of young males in hot-dry and hot-humid environments. Eur. J. Appl. Physiol. 2018 Dec;118(12):2655-2667[↩]
- Patel BC, Treister AD, Lio PA. Anatomy, Skin, Sudoriferous Gland. [Updated 2019 Apr 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513244[↩][↩]
- Murphrey MB, Vaidya T. Histology, Apocrine Gland. [Updated 2019 Feb 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482199[↩][↩]