Contents
What is syringomyelia
Syringomyelia is the development of a fluid-filled cyst (syrinx) within your spinal cord. Syringomyelia develops when cerebrospinal fluid (CSF), which usually flows around the outside of your brain and spinal cord, collects inside your spinal cord and forms a fluid-filled cyst (syrinx). Over time, the cyst may enlarge, damaging your spinal cord and causing pain, weakness and stiffness, among other symptoms. Syringomyelia applies to any cavity within the substance of the spinal cord that may or may not communicate with the central canal (ependyma does not line the cavity wall). In syringomyelia, there is a dissection of the ependymal lining of the central canal and cerebrospinal fluid (CSF) collection within the cord itself. Therefore, the collection does not have an ependymal lining.
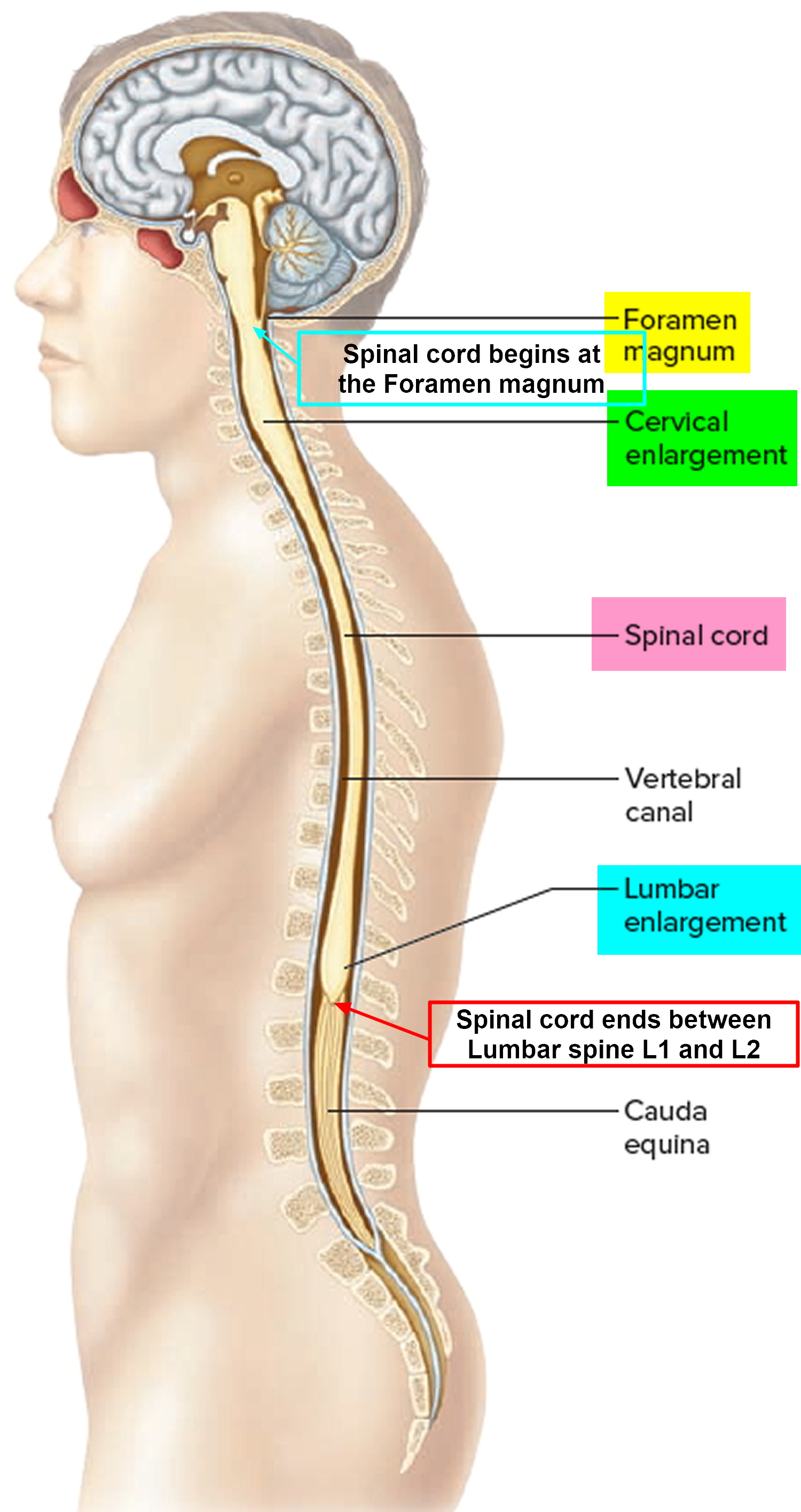
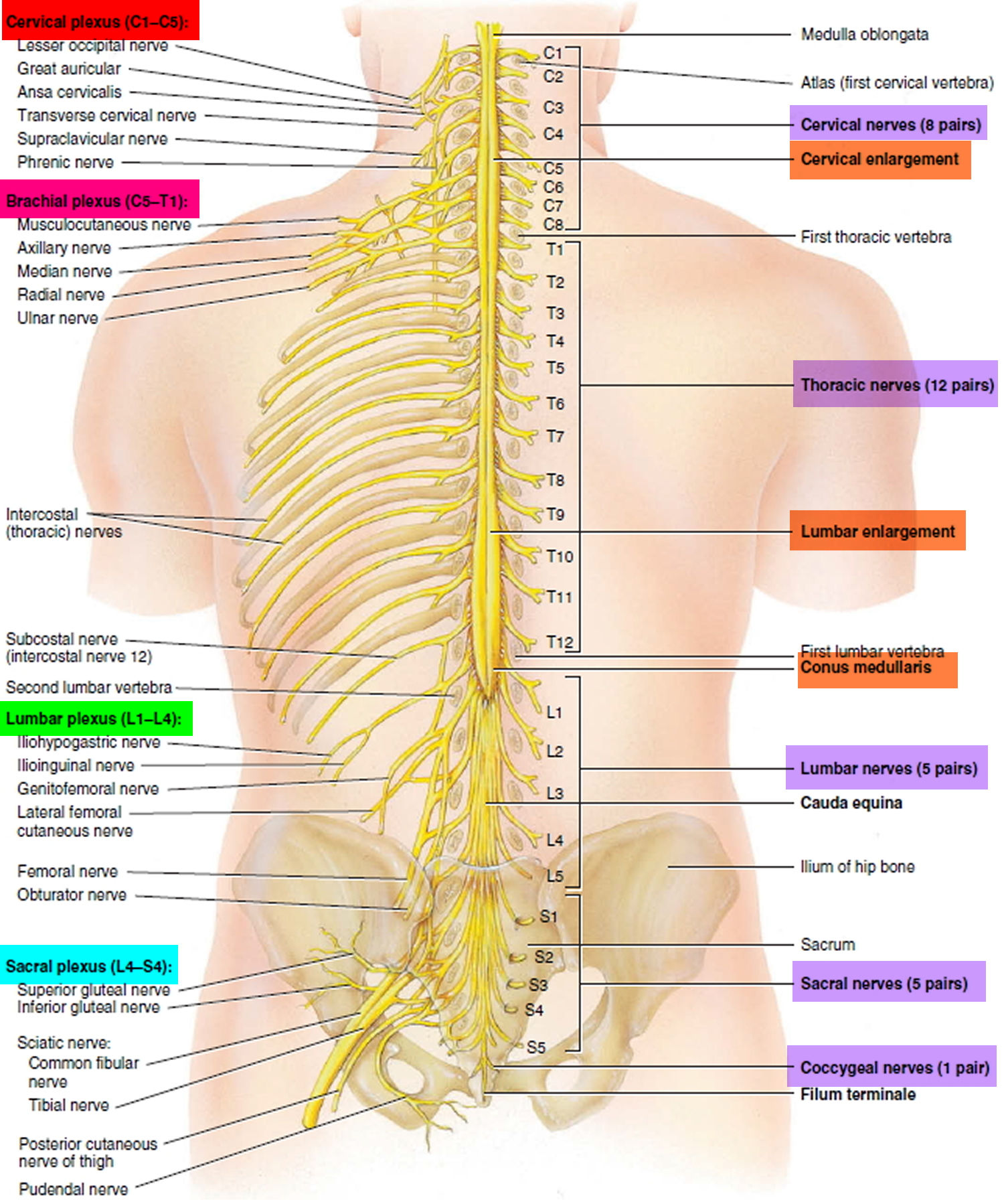
Characteristically, the syrinx is in the cervicothoracic cord, with C2 to T9 being the most common location, however the lesion may descend all the way down to the conus medullaris. There are numerous causes and associations, and these are discussed in more depth in the general article on syrinx.
Estimated prevalence of syringomyelia is about 8.4 cases per 100,000 people and occurs more frequently in men than in women. Syringomyelia usually appears in the third or fourth decade of life, with a mean age of onset of 30 years. Rarely, syringomyelia may develop in childhood or late adulthood.
Syringomyelia has several possible causes, though the majority of cases are associated with a condition in which brain tissue protrudes into your spinal canal (Chiari malformation).
Other causes of syringomyelia include spinal cord tumors, spinal cord injuries and damage caused by inflammation around your spinal cord.
The following are types of syringomyelia:
Syringomyelia with fourth ventricle communication
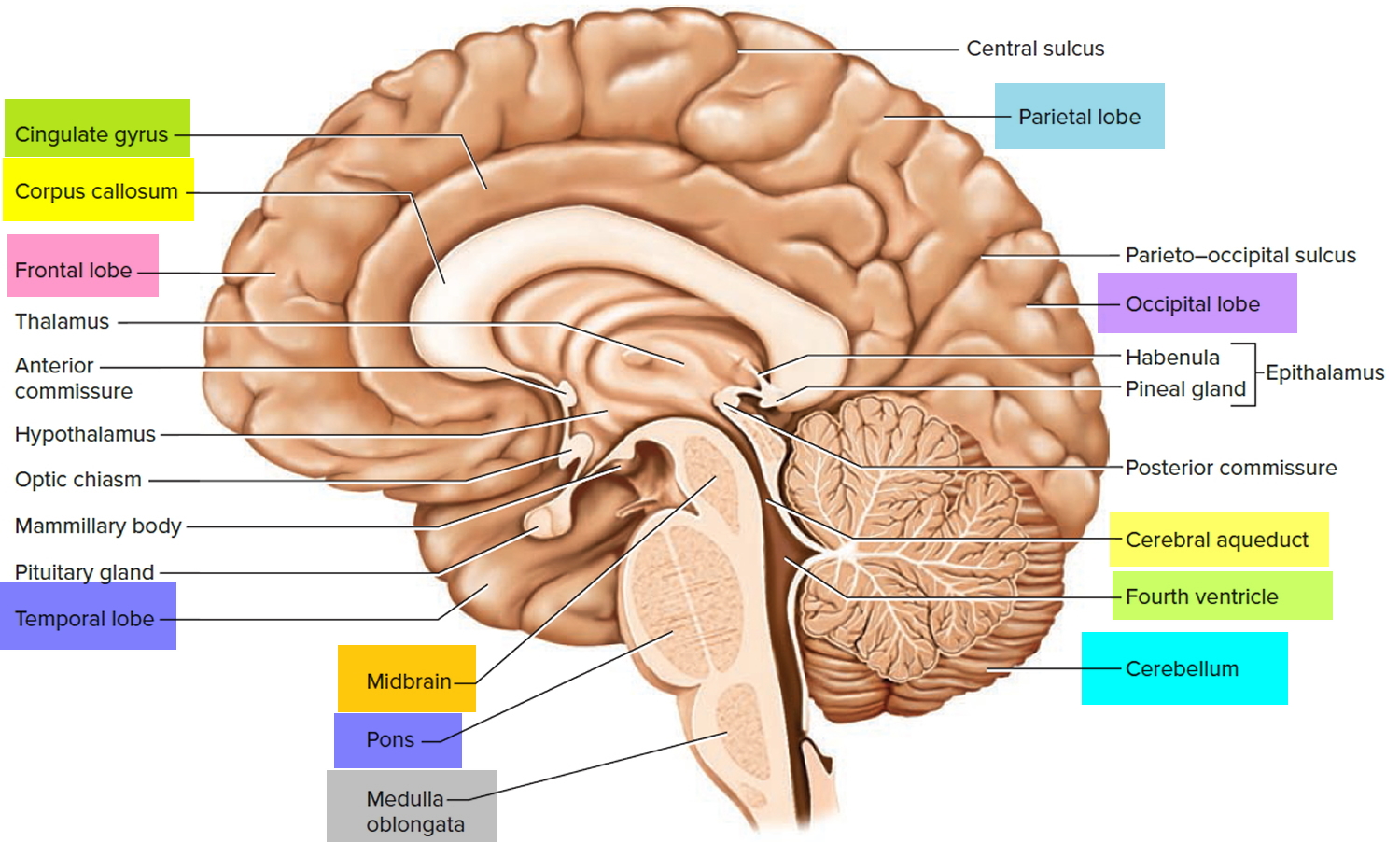
About 10% of syringomyelia cases are of this type. This communication can be observed on MRI. In some cases, a blockage of cerebrospinal fluid (CSF) circulation occurs (see Figures 4, 5 and 6). A shunt operation may be the best therapeutic option for these patients.
Syringomyelia due to blockage of CSF circulation (without fourth ventricular communication)
Representing at least 50% of all cases, this is the most common type of syringomyelia. Obstruction of cerebrospinal fluid (CSF) circulation from the basal posterior fossa to the caudal space may cause syringomyelia of this type. The most common example is Arnold-Chiari malformation, which is also associated with communicating syringomyelia. Other causes include the following:
- Basal arachnoiditis (postinfectious, inflammatory, postirradiation, blood in subarachnoid space) 1
- Basilar impression or invagination
- Meningeal carcinomatosis
- Pathological masses (arachnoid cysts, rheumatoid arthritis pannus, occipital encephalocele, tumors)
Syringomyelia due to spinal cord injury
Fewer than 10% of syringomyelia cases are of this type. Mechanisms of injury include (1) spinal trauma, (2) radiation necrosis, (3) hemorrhage from aneurysm rupture or arteriovenous malformation or in a tumor bed, (4) infection (spinal abscess, human immunodeficiency virus, transverse myelitis), and (5) cavitation following ischemic injury or degenerative disease.
Syringomyelia and spinal dysraphism
Spinal dysraphism may cause syringomyelia through a variety of mechanisms, including those mentioned under the previous three categories. Identification and treatment of associated dysraphism has the greatest impact on arresting progression of syringomyelia.
If syringomyelia isn’t causing any problems, monitoring the condition may be all that’s necessary. But if you’re bothered by symptoms, you may need surgery.
Syringomyelia due to intramedullary tumors
Fluid accumulation is usually caused by secretion from neoplastic cells or hemorrhage. The tumors most often associated with syringomyelia are ependymoma and hemangioblastoma. Extramedullary intradural and extradural tumors are considered separately under the second category because the mechanism of syrinx formation is blockage of the cerebrospinal fluid (CSF) pathway.
Idiopathic syringomyelia
Idiopathic syringomyelia has an unknown cause and cannot be classified under any of the previous categories 2. Surgical decompression can help in some patients with remarkable neurologic deficit.
Syringomyelia can cause symptoms such as:
Patients with this condition demonstrate a wide variety of neurological symptoms depending on where exactly the syrinx is located, but classically patients present with:
- Pain and weakness in the back, shoulders, arms or legs
- Headaches
- Inability to feel hot or cold
This motor and sensory impairment can eventually cause atrophy, which begins in the hands and progresses proximally, resulting in deformities such as ‘claw hands’ and Charcot’s arthropathy 3.
Symptoms vary according to the size and location of the syrinx. They often begin in early adulthood.
Figure 1. Spinal cord
Figure 2. Spinal cord segments
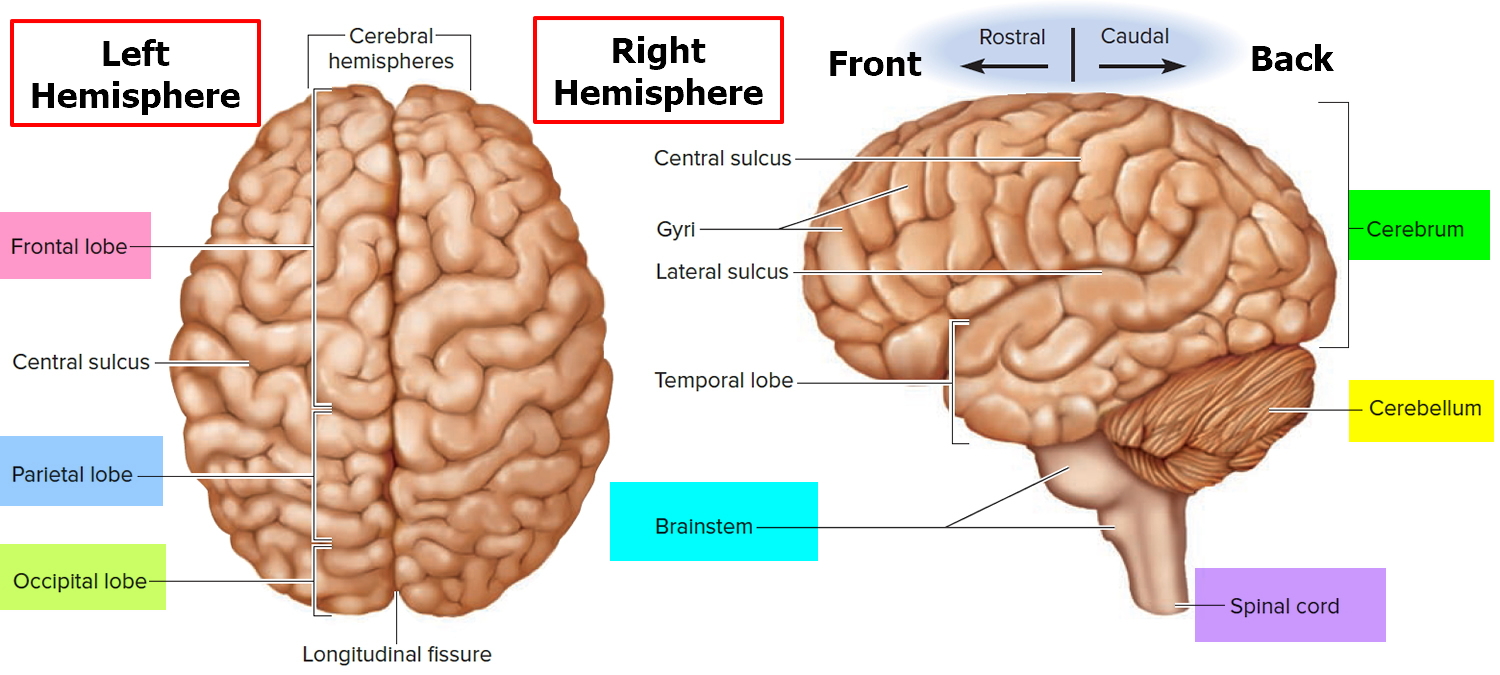
Figure 3. Human brain
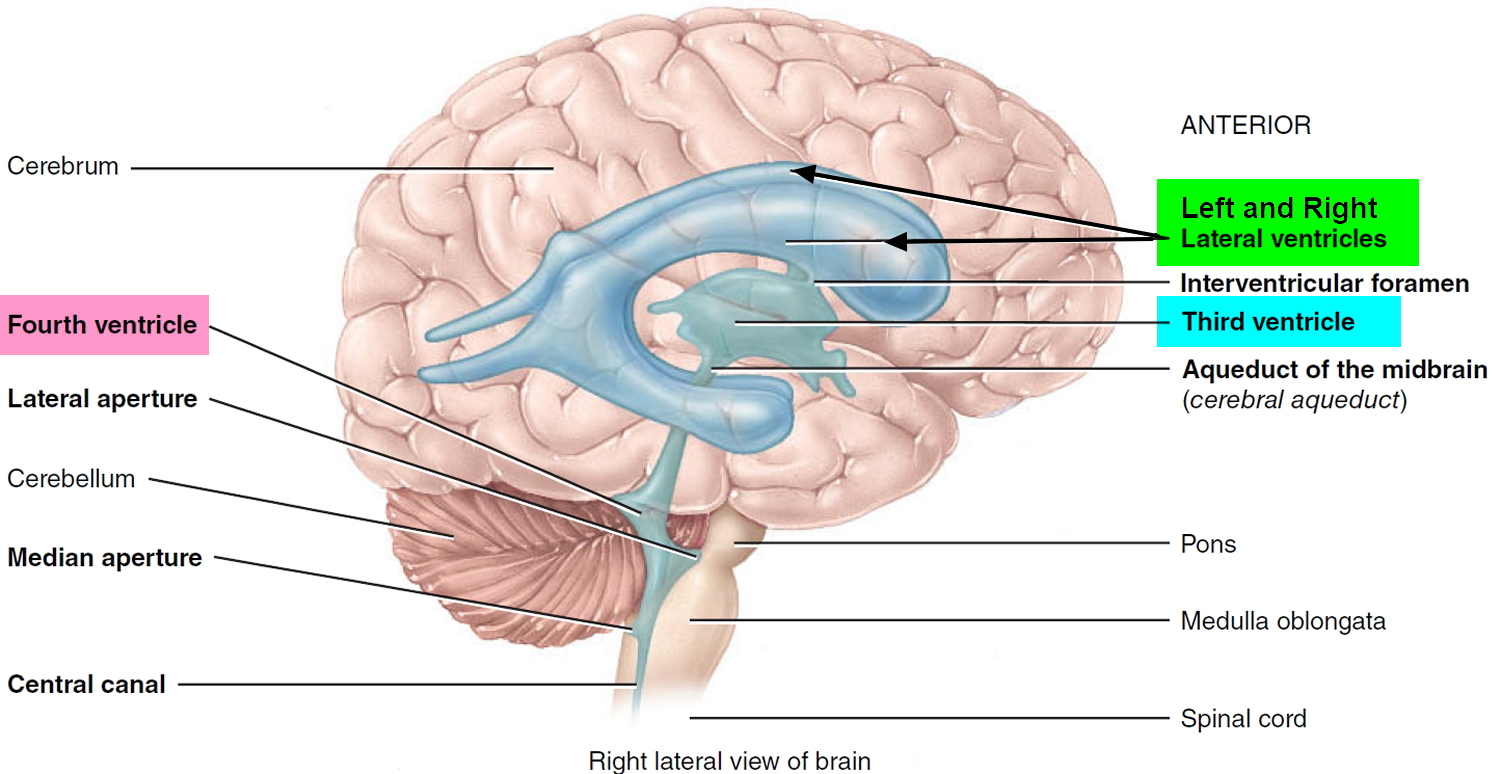
Figure 4. Medial aspect of the human brain
Figure 5. Ventricles of the brain
Figure 6. Cerebrospinal fluid formation, absorption and circulation around and within the brain
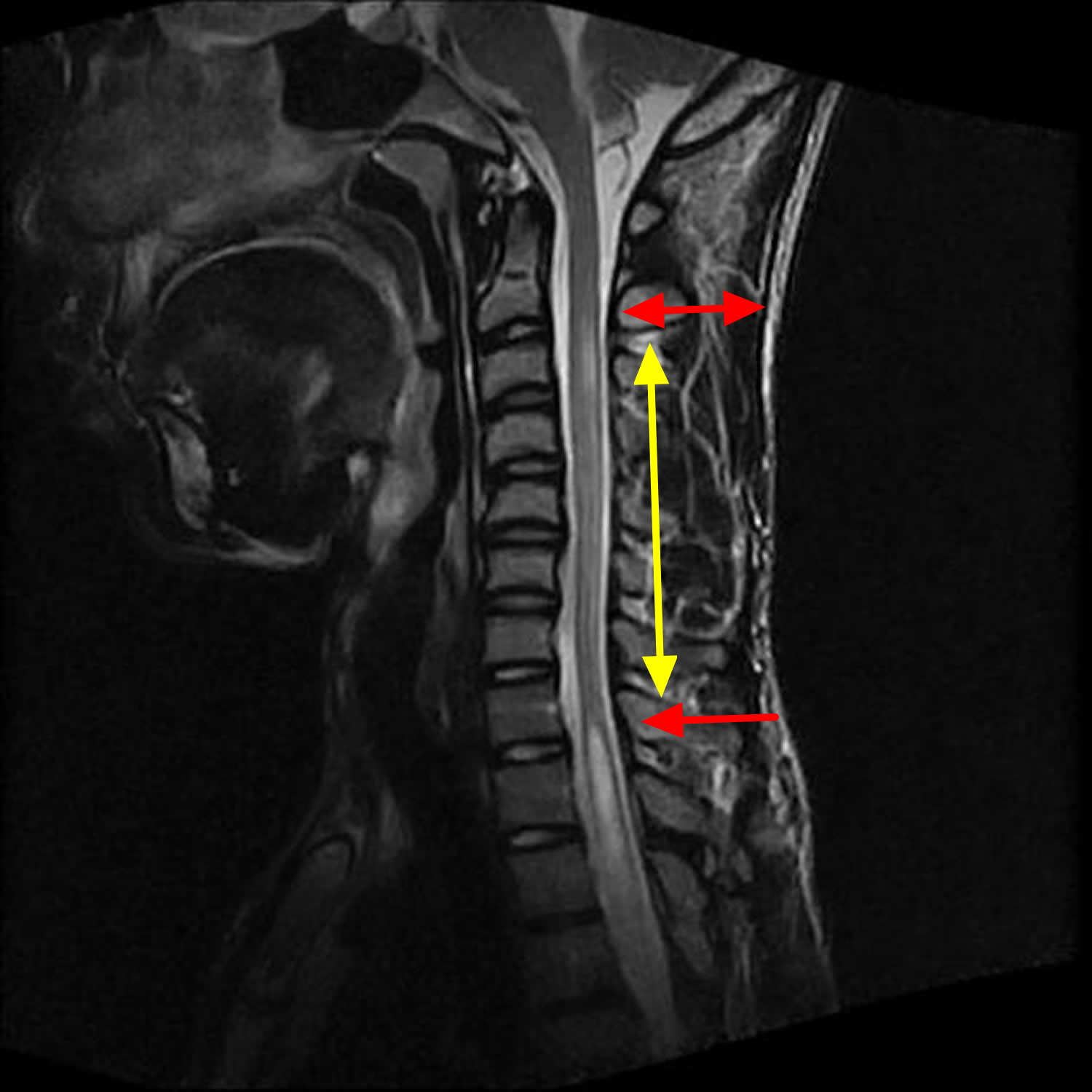
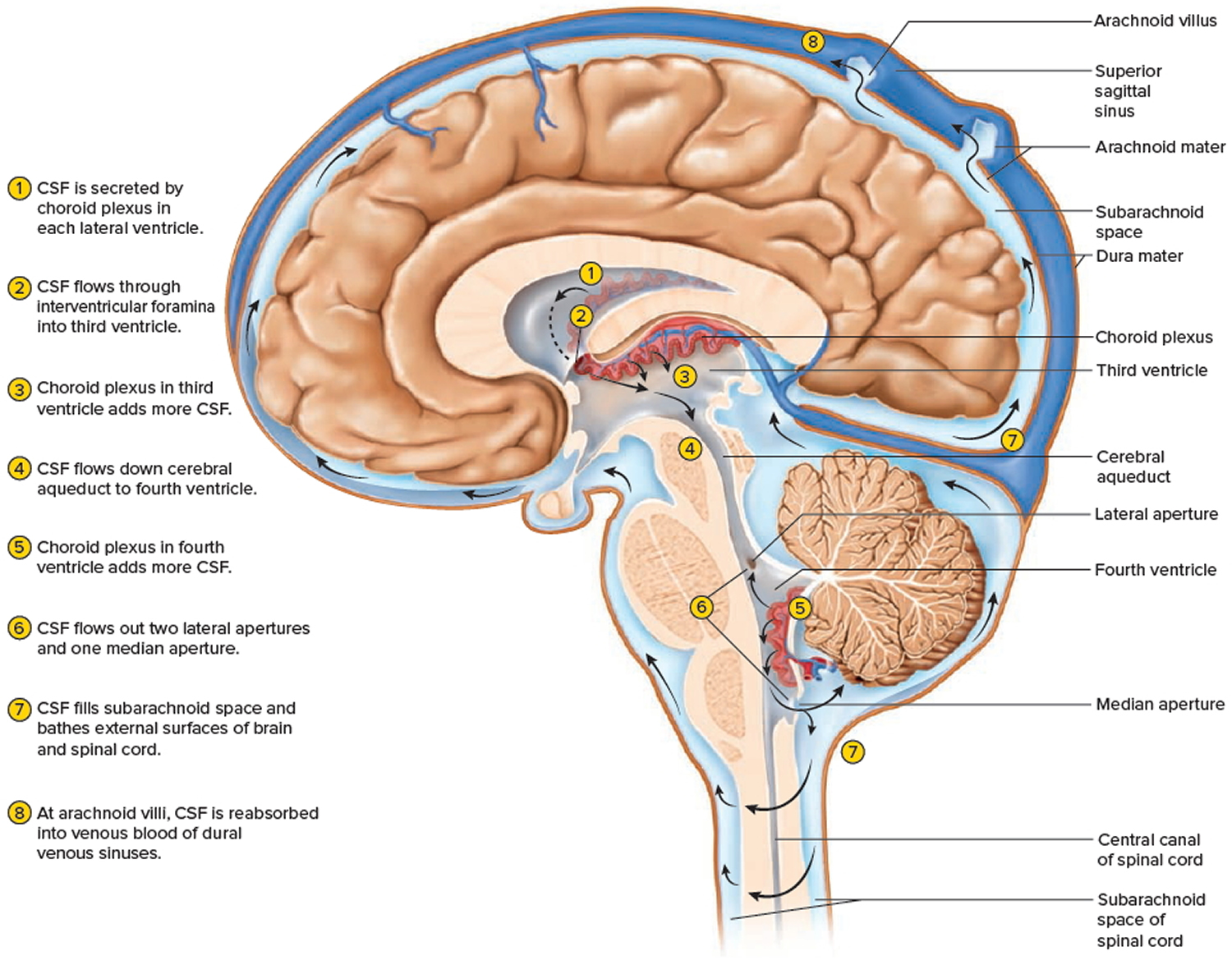 Figure 7. Syringomyelia MRI scan – there is an extensive syrinx extending from the C2/3 level all the way down to T11/12 level.
Figure 7. Syringomyelia MRI scan – there is an extensive syrinx extending from the C2/3 level all the way down to T11/12 level.Chiari malformation syringomyelia
A Chiari malformation, previously called an Arnold-Chiari malformation, is where the lower part of the brain pushes down into the spinal canal.
There are four main types, but type 1, called Chiari I, is the most common.
In someone with Chiari type I malformation, the lowest part of the back of the brain extends into the spinal canal. This can put pressure on the brainstem, spinal cord, and obstruct the flow of fluid (Figure 8).
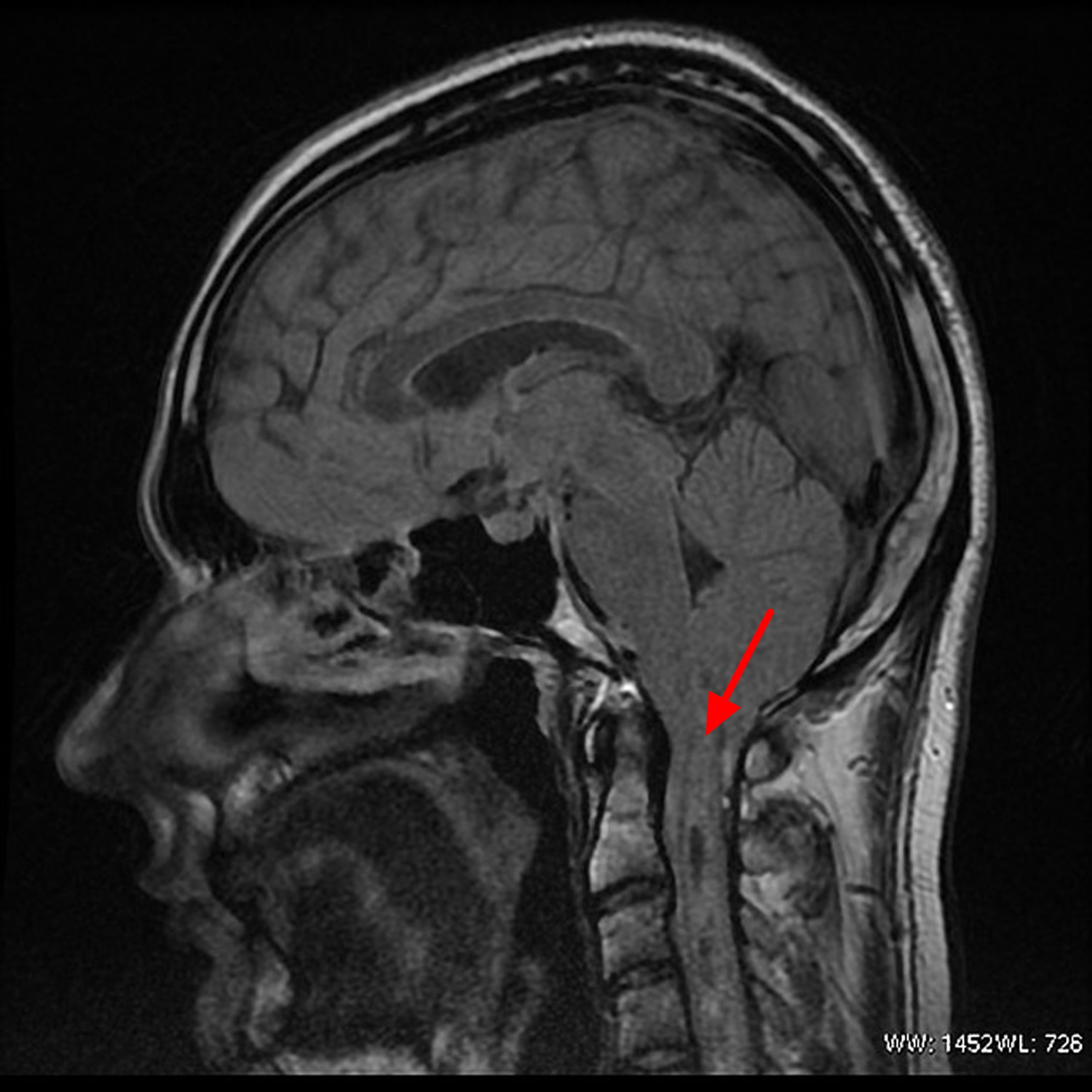
Figure 8. Chiari malformation syringomyelia
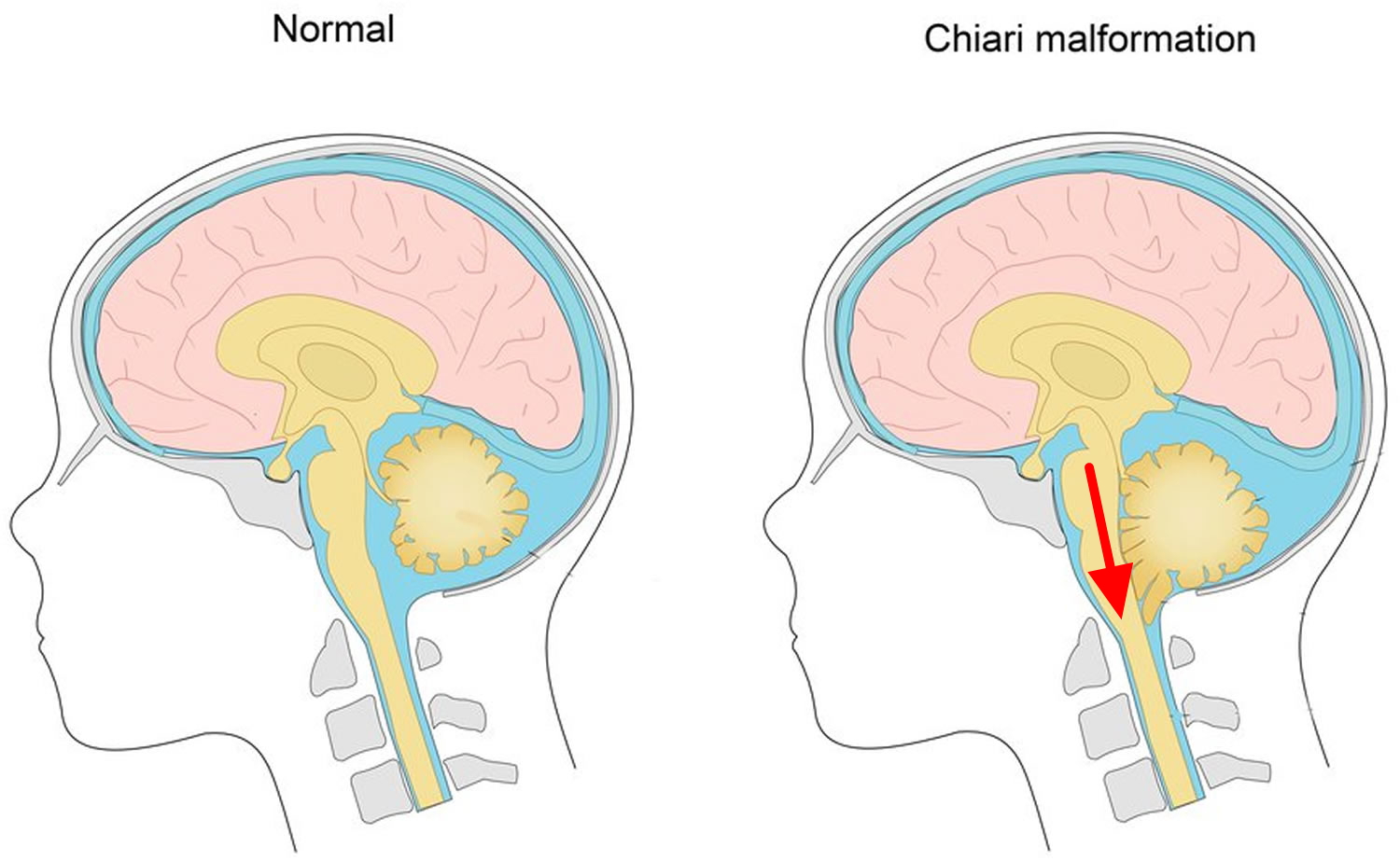 Figure 9. Chiari malformation syringomyelia MRI scan – note herniation of cerebellar tonsil is seen, with a large cervicodorsal syrinx extending from C1 to C7-C8 level.
Figure 9. Chiari malformation syringomyelia MRI scan – note herniation of cerebellar tonsil is seen, with a large cervicodorsal syrinx extending from C1 to C7-C8 level.The severity of Chiari malformations can vary from person to person, but generally:
- Chiari 1 malformations aren’t considered life-threatening
- Some people experience painful headaches, movement problems and other unpleasant symptoms (see below), but many people won’t have any symptoms
- There’s a chance of developing syringomyelia (where a fluid-filled cavity called a syrinx develops in the spinal cord), which can damage the spinal cord if not treated promptly
- Surgery can usually stop the symptoms getting worse and can sometimes improve them, although some problems may remain
Talk to your doctor about what the condition means, what the implications may be for your health and what treatment you may need.
Chiari 1 malformations causes
The exact cause of Chiari I malformations is unknown. It tends to be present from birth, but is normally only found in adulthood when symptoms develop or when an MRI scan is done.
Many cases are thought to be the result of part of the skull not being large enough for the brain.
Chiari I malformations can also develop in people with a tethered spinal cord, a build-up of fluid on the brain (hydrocephalus), and some types of brain tumour.
Chiari malformations can sometimes run in families. It’s possible that some children born with it may have inherited a faulty gene that caused problems with their skull development.
But the risk of passing a Chiari malformation on to your child is very small. And remember: even if your children do inherit it, they may not experience symptoms.
Symptoms of Chiari Type 1 malformations
Many people with a Chiari 1 malformation will not have any symptoms. Sometimes they’re only found after an (MRI) scan of the brain is carried out for another reason.
If symptoms do develop, they can include:
- headaches – these are usually felt at the back of the head and may be brought on or made worse by coughing, straining, sneezing or bending over
- neck pain
- dizziness and balance problems
- muscle weakness
- numbness or tingling in the arms or legs
- blurred vision, double vision and sensitivity to light
- swallowing problems
- hearing loss and tinnitus
- feeling and being sick
- difficulty sleeping (insomnia) and depression
If you develop syringomyelia, you may also experience problems using your hands, difficulty walking, pain, and problems with bladder or bowel control.
If you’ve been diagnosed with a Chiari malformation, you should contact your doctor for advice if you develop any new symptoms or your symptoms worsen.
Treatments for Chiari 1 malformations
Treatment for Chiari I malformation depends on whether you have any symptoms and how severe they are. You might not need any treatment if you don’t have any symptoms.
Painkillers can help relieve any headaches and neck pain.
If your headaches are severe or you have problems caused by the pressure on your spinal cord (such as movement difficulties), surgery may be recommended.
Surgery
The main operation for Chiari malformation is called decompression surgery.
Under general anesthetic a cut is made at the back of your head and the surgeon removes a small piece of bone from the base of your skull. They may also remove a small piece of bone from the top of your spine.
This will help reduce the pressure on your brain and allow the fluid in and around your brain and spinal cord to flow normally.
Other procedures that may be necessary include:
- Endoscopic third ventriculostomy – a small hole is made in the wall of one of the cavities of the brain, releasing trapped fluid. See treating hydrocephalus for more information.
- Ventriculoperitoneal shunting – a small hole is drilled into the skull and a thin tube called a catheter is passed into the brain cavity to drain trapped fluid and relieve the pressure. See treating hydrocephalus for more information.
- Untethering – some children with a type 1 Chiari malformation have a tethered spinal cord, which means it is abnormally attached within the spine. Untethering involves separating the spinal cord and releasing tension in the spine.
- Spinal fixation – some people with Chiari I will have a hypermobility syndrome, such as Ehlers-Danlos syndrome, and may require surgery to stabilize their spine.
The aim of surgery is to stop existing symptoms getting any worse. Some people also experience an improvement in their symptoms, particularly their headaches.
However, surgery sometimes results in no improvement or symptoms getting worse. There’s also a small risk of serious complications, such as paralysis or a stroke.
Talk to your surgeon about the different surgical options and what the benefits and risks of each are.
Syringomyelia and syringobulbia
Syringobulbiais very rare condition defined as slit-like fluid cavity in the brain stem 4. Syringobulbia can be accompanied by syringomyelia either communicating or non- communicating with it 5. Several conditions have been reported to be associated with syringobulbia including neoplasms 6, spinal cord traumas or lesions such as tethered cord 7, hind-brain herniation 8, infections such as meningitis 9 and in isolation 10. However an isolated syringobulbia is an extremely rare condition and a few reports are available in the literature about this pathology 11. The clinical presentation depends on the site of the cavity and the involved structures 12 which ranges from asymptomatic presentation to cranial nerve palsy 13, vocal cord paralysis 14 and facial myokymia (an involuntary, spontaneous, localised quivering of a few facial muscles) 15. Most often the onset of the sign and symptoms is insidious, with dysphagia, hiccough, or hoarseness of voice 14. Later, as the lesion becomes more extensive, the subjective symptoms may ameliorate or disappear being replaced by objective signs. It has been reported that nystagmus is the most common neurologic finding of syringobulbia, together with trigeminal sensory loss 12. Greenlee and co-workers 5 reported cranial nerve dysfunction in all of their patients; most of their patients had multiple nerves affected.
Post-traumatic syringomyelia has been wieldy described previously with an incidence of 0.3-3.2% in those suffering from spinal cord trauma 16. However, traumatic brain injury has not been reported as the mechanism and etiology of isolated syringobulbia. The current body of literature describing syringobulbia consists of case reports or small case series linked with syringomyelia.
Syringobulbia can be encountered as a late complication of syringomyelia as the cavity may extend toward brain stem. Several mechanisms have been introduced for the formation of the syringobulbia concurrent syringomyelia. One possible mechanism is the rupture of the paracentral cervical syrinx rostrally resulting in syrinx formation in the brain stem 17. The other mechanism is dilation and propagation of the spinal central canal to the medulla oblongata and brain stem leading to syringobulbia. One possible mechanism for isolated syringobulbia is the extravasation and entrance of the fluid from the perivascular spaces and cisterns into the brain stem. Encephalomalacia at the site of previous brain stem contusions could also be the origin of cavitation and syrinx formation. The interesting point is that the syrinx in syringobulbia does not have ependymal lining and usually communicates with fourth ventricle 18.
Treatment options are limited for the isolated syringobulbia although several approaches have been reported for syringobulbia concurrent syringomyelia 5. As only few case reports have addressed isolated syringobulbia, the treatment option is experimental models and evidence regarding this issue is extremely scarce in the literature. Greenlee et al. 5 showed that posterior fossa decompression is a safe and effective treatment. Other surgical optionsinclude drainage or decompression of the syrinx cavity with diversion of fluid to the subarachnoid space or peritoneal cavity 19. As the data is scarce regarding the treatment of isolated syringobulbia, the results are variable and the treatment option should be chosen based on underlying etiology, to achieve the best outcome.
Syringomyelia causes
It’s unclear exactly how and why syringomyelia happens. When it develops, cerebrospinal fluid — the fluid that surrounds, cushions and protects your brain and spinal cord — collects within the spinal cord itself, forming a fluid-filled cyst (syrinx).
Several conditions and diseases can lead to syringomyelia, including:
- Chiari malformation, a condition in which brain tissue protrudes into your spinal canal
- Meningitis, an inflammation of the membranes surrounding your brain and spinal cord
- Spinal cord tumor, which may interfere with the normal circulation of cerebrospinal fluid
- Conditions present at birth, such as a tethered spinal cord, a condition caused when tissue attached to your spinal cord limits its movement
- Spinal cord injury, which may cause symptoms months or even years after the initial injury
Cause of syringomyelia often is associated with craniovertebral junction abnormalities.
Bony abnormalities include the following:
- Small posterior fossa
- Platybasia and basilar invagination
- Assimilation of the atlas
Soft-tissue masses of abnormal nature include the following:
- Tumors (e.g., meningioma at foramen magnum)
- Inflammatory masses
Neural tissue abnormalities include the following:
- Cerebellar tonsils and vermis herniation
- Chiari malformation
Membranous abnormalities include the following:
- Arachnoid cysts 20, rhombic roof, or vascularized membranes
- Posthemorrhagic or postinflammatory membranes
Other causes not associated with craniovertebral abnormalities may include the following:
- Arachnoid scarring related to spinal trauma
- Arachnoid scarring related to meningeal inflammation
- Arachnoid scarring related to surgical trauma
- Subarachnoid space stenosis due to spinal neoplasm or vascular malformation
- Subarachnoid space stenosis, with possible scarring, related to disk and osteophytic disease
- Idiopathic
Syringomyelia prognosis
Prognosis depends on the underlying cause, the magnitude of neurological dysfunction, and the location and extension of the syrinx.
Patients presenting with moderate or severe neurological deficits fare much worse than those patients with mild deficits. Patients with central cord syndrome have poor response to treatment.
Assessing treatment results is difficult because of the rarity of syringomyelia, variability of presentation and natural history, and the relatively short follow-up in most studies. In one study, half of all patients with syringomyelia were in clinically stable condition for several years.
Although an older study had suggested that 20% of patients died at an average of 47 years, mortality rates are likely lower in today’s patients as a result of surgical interventions and better treatment of complications associated with significant paresis, such as pulmonary embolism.
Syringomyelia life expectancy
Natural history of syringomyelia still is not well understood. Although older studies had suggested that 20% of patients died at an average age of 47 years, mortality rates are likely lower in today’s patients as a result of surgical interventions and better treatment of complications associated with significant paresis, such as pulmonary embolism 21.
Syringomyelia complications
In some people, syringomyelia can become a progressive disorder and lead to serious complications. In others, there may be no associated symptoms, and no intervention is necessary.
Myelopathy is the most serious consequence of syringomyelia. The following are the seven grade classifications of disability from myelopathy according to the Modified Nurick Classification.
- Grade 0 – No root signs or symptoms
- Grade I – Root signs or symptoms; no evidence of cord involvement
- Grade II – Signs of cord involvement; normal gait
- Grade III – Mild gait abnormality; able to be employed
- Grade IV – Gait abnormality prevents employment
- Grade V – Able to ambulate only with assistance
- Grade VI – Chairbound or bedridden
Complications due to myelopathy include the following:
- Recurrent pneumonia
- Paraplegia or quadriplegia
- Decubitus ulcers
- Bowel and urinary dysfunction
Complications that may occur as a syrinx enlarges or if it damages nerves within your spinal cord include:
- Scoliosis — an abnormal curve of your spine
- Chronic pain — damage to the spinal cord can cause severe, chronic pain
- Motor difficulties — weakness and stiffness in your leg muscles can eventually affect your gait
Syringomyelia symptoms
Syringomyelia symptoms usually progresses slowly over time; the course may extend over many years. Syringomyelia may have a more acute course, especially when the brain stem is affected (i.e., syringobulbia). Syringomyelia usually involves the cervical area. Symptomatic presentation depends primarily on the location of the lesion within the neuraxis.
If your syringomyelia is caused by protrusion of brain tissue into your spinal canal (Chiari malformation), symptoms generally may begin between ages 25 and 40.
In some cases, coughing or straining may trigger symptoms of syringomyelia, although neither causes syringomyelia.
The following early signs and symptoms of syringomyelia may affect the back of your neck, shoulders, arms and hands first:
- Muscle weakness and wasting (atrophy)
- Loss of reflexes
- Loss of sensitivity to pain and temperature
Other signs and symptoms of syringomyelia may include:
- Stiffness in your back, shoulders, arms and legs
- Pain in your neck, arms and back
- Bowel and bladder function problems
- Muscle weakness and spasms in your legs
- Spinal curvature (scoliosis)
Sensory
Syrinx interrupts the decussating spinothalamic fibers that mediate pain and temperature sensibility, resulting in loss of these sensations, while light touch, vibration, and position senses are preserved (dissociated sensory loss).
When the cavity enlarges to involve the posterior columns, position and vibration senses in the feet are lost; astereognosis may be noted in the hands.
Pain and temperature sensation may be impaired in either or both arms, or in a shawllike distribution across the shoulders and upper torso anteriorly and posteriorly.
Dysesthetic pain, a common complaint in syringomyelia, usually involves the neck and shoulders, but may follow a radicular distribution in the arms or trunk. The discomfort, which is sometimes experienced early in the course of the disease, generally is deep and aching and can be severe.
Motor
Syrinx extension into the anterior horns of the spinal cord damages motor neurons (lower motor neuron) and causes diffuse muscle atrophy that begins in the hands and progresses proximally to include the forearms and shoulder girdles. Clawhand may develop.
Respiratory insufficiency, which usually is related to changes in position, may occur.
Autonomic
Impaired bowel and bladder functions usually occur as a late manifestation.
Sexual dysfunction may develop in long-standing cases.
Horner syndrome may appear, reflecting damage to the sympathetic neurons in the intermediolateral cell column.
Extension of the syrinx
A syrinx may extend into the medulla, producing a syringobulbia 22. This syndrome is characterized by dysphagia, nystagmus, pharyngeal and palatal weakness, asymmetric weakness and atrophy of the tongue, and sensory loss involving primarily pain and temperature senses in the distribution of the trigeminal nerve.
Rarely, the syrinx cavity can extend beyond the medulla in the brain stem into the centrum semiovale (syringocephalus).
Lumbar syringomyelia can occur and is characterized by atrophy of the proximal and distal leg muscles with dissociated sensory loss in the lumbar and sacral dermatomes. Lower limb reflexes are reduced or absent. Impairment of sphincter function is common.
Other manifestations
Painless ulcers of the hands are frequent. Edema and hyperhidrosis can be due to interruption of central autonomic pathways.
Neurogenic arthropathies (Charcot joints) may affect the shoulder, elbow, or wrist 23. Scoliosis is seen sometimes 24.
Acute painful enlargement of the shoulder is associated with destruction of the head of the humerus.
Syringomyelia diagnosis
To diagnose syringomyelia, your doctor will begin by asking about your medical history and doing a complete physical examination.
In some cases, syringomyelia may be discovered incidentally during a spine MRI or computerized tomography (CT) scan conducted for other reasons.
If your doctor suspects syringomyelia, you’ll likely undergo tests that may include:
- Magnetic resonance imaging (MRI). An MRI of your spine and spinal cord is the most reliable tool for diagnosing syringomyelia. An MRI uses radio waves and a strong magnetic field to produce detailed images of your spine and spinal cord. If a syrinx has developed within your spinal cord, your doctor will be able to view it on the MRI. In some cases, a specialist will inject a dye into a blood vessel in your groin, which travels through blood vessels to your spine and reveals tumors or other abnormalities. An MRI may be repeated over time to monitor the progression of syringomyelia.
- Computerized tomography (CT) scan. A CT scan uses a series of X-rays to create a detailed view of your spine and spinal cord. A CT scan may show if you have tumors or other spine conditions.
Syringomyelia treatment
Treatment for syringomyelia depends on the severity and progression of your signs and symptoms.
Monitoring
If syringomyelia is discovered on an MRI scan that’s done for an unrelated reason, and syringomyelia isn’t causing signs or symptoms, monitoring with periodic MRI and neurological exams may be all that’s needed.
Surgery
If syringomyelia is causing signs and symptoms that interfere with your daily life, or if signs and symptoms rapidly worsen, your doctor will usually recommend surgery.
The goal of surgery is to remove the pressure the syrinx places on your spinal cord and to restore the normal flow of cerebrospinal fluid. This can help improve your symptoms and nervous system (neurological) function. The type of surgery you’ll need depends on the underlying cause of syringomyelia.
Several types of surgery options are available to reduce pressure on your brain and spinal cord. Surgery types include:
- Treating Chiari malformation. If syringomyelia is caused by Chiari malformation, your doctor may recommend surgery that involves enlarging the opening at the base of your skull (suboccipital craniectomy) and expanding the covering of your brain (dura mater). This surgery can reduce pressure on your brain and spinal cord, restore the normal flow of cerebrospinal fluid, and may improve or resolve syringomyelia.
- Draining the syrinx. To drain the syrinx, your doctor will surgically insert a drainage system, called a shunt. It consists of a flexible tube that keeps fluid from the syrinx flowing in the desired direction. One end of the tubing is placed in the syrinx, and the other is placed in another area of your body such as your abdomen.
- Removing the obstruction. If something within your spinal cord, such as a tumor or a bony growth, is hindering the normal flow of cerebrospinal fluid, surgically removing the obstruction may restore the normal flow and allow fluid to drain from the syrinx.
- Correcting the abnormality. If a spinal abnormality is hindering the normal flow of cerebrospinal fluid, surgery to correct it, such as releasing a tethered spinal cord, may restore normal fluid flow and allow the syrinx to drain.
Surgery doesn’t always effectively restore the flow of cerebrospinal fluid, and the syrinx may remain, despite efforts to drain the fluid from it.
Follow-up care
Follow-up care after surgery is critical because syringomyelia may recur. You’ll need regular examinations with your doctor, including periodic MRIs, to assess the outcome of surgery.
The syrinx may grow over time, requiring additional treatment. Even after treatment, some signs and symptoms of syringomyelia may remain, as a syrinx can cause permanent spinal cord and nerve damage.
Lifestyle and home remedies
Taking the following steps may help reduce the effects of syringomyelia on your daily living.
Avoid activities that may make symptoms worse
If you’ve been diagnosed with syringomyelia, avoid any activity that involves heavy lifting, straining or putting excessive force on your spine.
Consider physical therapy
If syringomyelia causes ongoing neurological problems that decrease your mobility and activity, such as muscle weakness, pain, fatigue or stiffness, a physical therapist may be able to create an exercise program for you that can help reduce these symptoms.
Talk to your doctor about physical therapists in your area who have expertise in neurological conditions.
Manage chronic pain
Chronic pain can be a problem with syringomyelia. If you’re experiencing chronic pain, talk to your doctor about treatment options. Many medical centers have doctors who specialize in pain management.
Often, the most appropriate approach for treatment of chronic pain due to syringomyelia is to have a health care team that includes your neurosurgeon, neurologist, a rehabilitation specialist and a pain management physician who can work together to create an appropriate plan for your situation.
Coping and support
Living with syringomyelia and its complications can be challenging. You may feel as if syringomyelia affects every aspect of your life and would love to not think about it for a day, especially if you have constant reminders, such as chronic pain or nerve issues.
Having someone to talk with or lean on can be invaluable. Whether it’s a trusted friend, counselor or therapist, you may find encouragement and comfort in a good listener.
Another source of support and information may be a syringomyelia support group. Your doctor may be able to recommend a local group, or you can find groups online. Support groups provide a forum for sharing experiences and can be good sources of information, offering useful or helpful tips for people with syringomyelia.
- Nakanishi K, Uchiyama T, Nakano N, et al. Spinal syringomyelia following subarachnoid hemorrhage. J Clin Neurosci. 2012 Apr. 19(4):594-7.[↩]
- Kim J, Kim CH, Jahng TA, Chung CK. Clinical course of incidental syringomyelia without predisposing pathologies. J Clin Neurosci. 2012 Feb 29.[↩]
- Boon NA, Colledge NR, Davidson SS et-al. Davidson’s principles & practice of medicine. Churchill Livingstone. (2006) ISBN:0443100578.[↩][↩][↩]
- Taghipour M, Derakhshan N, Ghaffarpasand F. Isolated Post-Traumatic Syringobulbia; Case Report and Review of the Literature. Bulletin of Emergency & Trauma. 2014;2(4):166-169. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4771293/[↩]
- Greenlee JD, Menezes AH, Bertoglio BA, Donovan KA. Syringobulbia in a pediatric population. Neurosurgery. 2005;(6):1147–53. discussion -53. https://www.ncbi.nlm.nih.gov/pubmed/16331163[↩][↩][↩][↩]
- Muroi A, Syms NP, Oi S. Giant syringobulbia associated with cerebellopontine angle arachnoid cyst and hydrocephalus. J Neurosurg Pediatr. 2011;8(1):30–4. https://www.ncbi.nlm.nih.gov/pubmed/21721885[↩]
- Priyadarshini H, Harish A. Syringomyelia with syringobulbia. J Assoc Physicians India. 2007;55:855. https://www.ncbi.nlm.nih.gov/pubmed/18405132[↩]
- Iseri PK, Efendi H, Demirci A, Komsuoglu S. Fibrous dysplasia of the cranial bones: a case report and review of the literature. Yale J Biol Med. 2005;78(3):141–5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2259144/pdf/16464312.pdf[↩]
- Schon F, Bowler JV. Syringomyelia and syringobulbia following tuberculous meningitis. J Neurol. 1990;237(2):122–3. https://www.ncbi.nlm.nih.gov/pubmed/2192017[↩]
- Gennaro P, Miller M. Syringobulbia without syringomyelia. Arch Neurol. 1983;40(6):394. https://jamanetwork.com/journals/jamaneurology/article-abstract/581954[↩]
- Gennaro P, Miller M. Syringobulbia without syringomyelia. Arch Neurol. 1983;40(6):394. https://www.ncbi.nlm.nih.gov/pubmed/6847457[↩]
- Nogues M, Lopez L, Meli F. Neuro-ophthalmologic complications of syringobulbia. Curr Neurol Neurosci Rep. 2010;10(6):459–66. https://www.ncbi.nlm.nih.gov/pubmed/20711820[↩][↩]
- Jha S, Das A, Gupta S, Banerji D. Syringomyelia with syringobulbia presenting only with paralysis of 9th and 10th cranial nerves. Acta Neurol Scand. 2002;105(4):341–3. https://www.ncbi.nlm.nih.gov/pubmed/11939952[↩]
- Viswanatha B. Syringomyelia with syringobulbia presenting as vocal fold paralysis. Ear Nose Throat J. 2009;88(7):E20. https://www.ncbi.nlm.nih.gov/pubmed/19623519[↩][↩]
- Riaz G, Campbell WW, Carr J, Ghatak N. Facial myokymia in syringobulbia. Arch Neurol. 1990;47(4):472–4. https://www.ncbi.nlm.nih.gov/pubmed/2181981[↩]
- Carroll AM, Brackenridge P. Post-traumatic syringomyelia: a review of the cases presenting in a regional spinal injuries unit in the north east of England over a 5-year period. Spine (Phila Pa 1976) 2005;30(10):1206–10. https://www.ncbi.nlm.nih.gov/pubmed/15897837[↩]
- Sherman JL, Citrin CM, Barkovich AJ. MR imaging of syringobulbia. J Comput Assist Tomogr. 1987;11(3):407–11. https://www.ncbi.nlm.nih.gov/pubmed/3571579[↩]
- Morgan D, Williams B. Syringobulbia: a surgical appraisal. J Neurol Neurosurg Psychiatry. 1992;55(12):1132–41. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1015326/pdf/jnnpsyc00497-0030.pdf[↩]
- Robinson L, Bisnaire D. Syringomyelia and syringobulbia: pathophysiology, surgical treatment and nursing implications. J Neurosci Nurs. 1990;22(2):69–75. https://www.ncbi.nlm.nih.gov/pubmed/2139684[↩]
- Kiran NA, Kasliwal MK, Suri A, Mahapatra AK. Giant posterior fossa arachnoid cyst associated with syringomyelia. Clin Neurol Neurosurg. 2010 Feb 4.[↩]
- Sixt C, Riether F, Will BE, Tatagiba MS, Roser F. Evaluation of quality of life parameters in patients who have syringomyelia. J Clin Neurosci. 2009 Oct 7.[↩]
- Viswanatha B. Syringomyelia with syringobulbia presenting as vocal fold paralysis. Ear Nose Throat J. 2009 Jul. 88(7):E20.[↩]
- Nacir B, Arslan Cebeci S, Cetinkaya E, Karagoz A, Erdem HR. Neuropathic arthropathy progressing with multiple joint involvement in the upper extremity due to syringomyelia and type I Arnold-Chiari malformation. Rheumatol Int. 2009 Jun 23.[↩]
- Cardoso M, Keating RF. Neurosurgical management of spinal dysraphism and neurogenic scoliosis. Spine (Phila Pa 1976). 2009 Aug 1. 34(17):1775-82. [↩]