Contents
Throat cancer
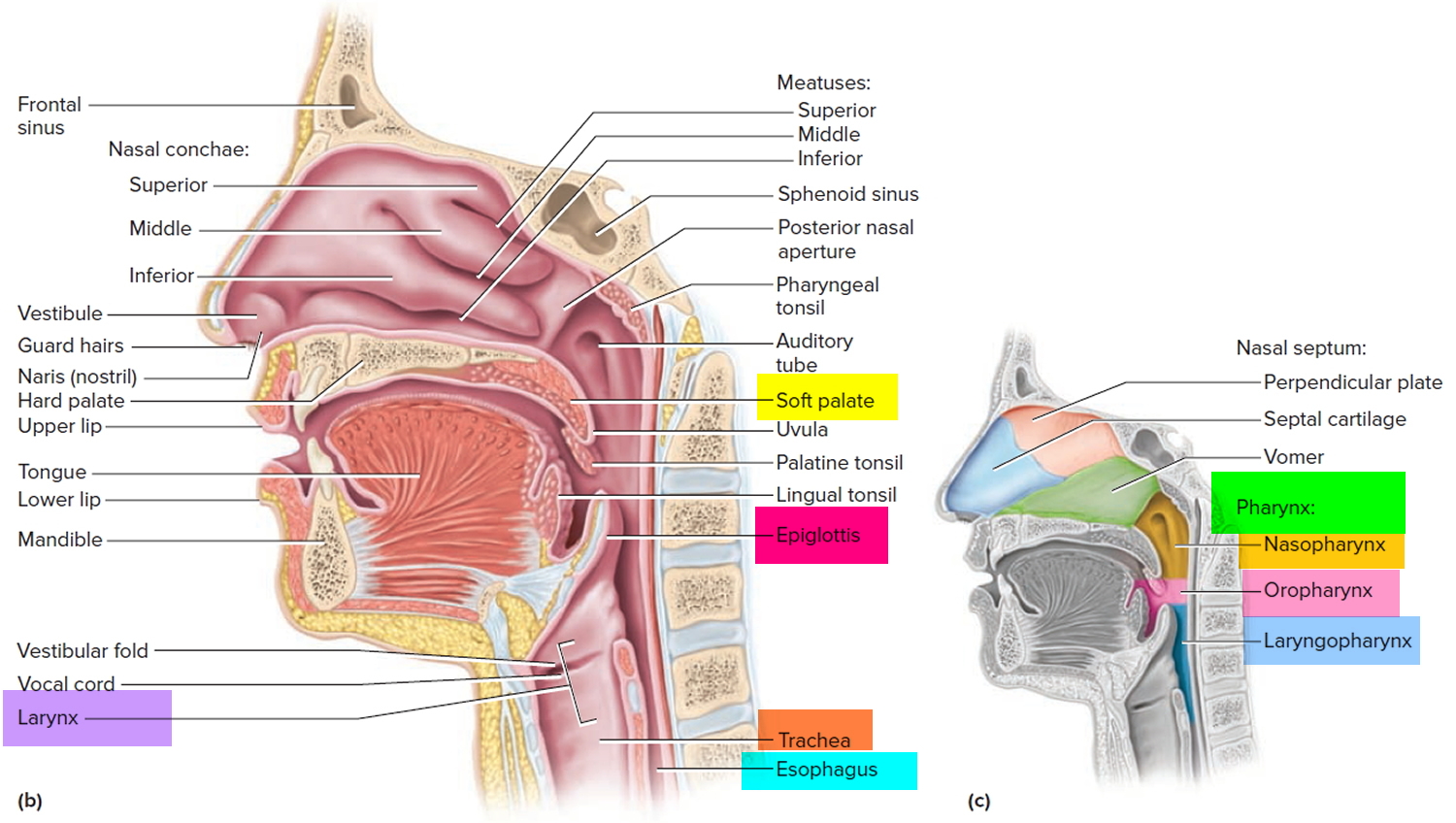
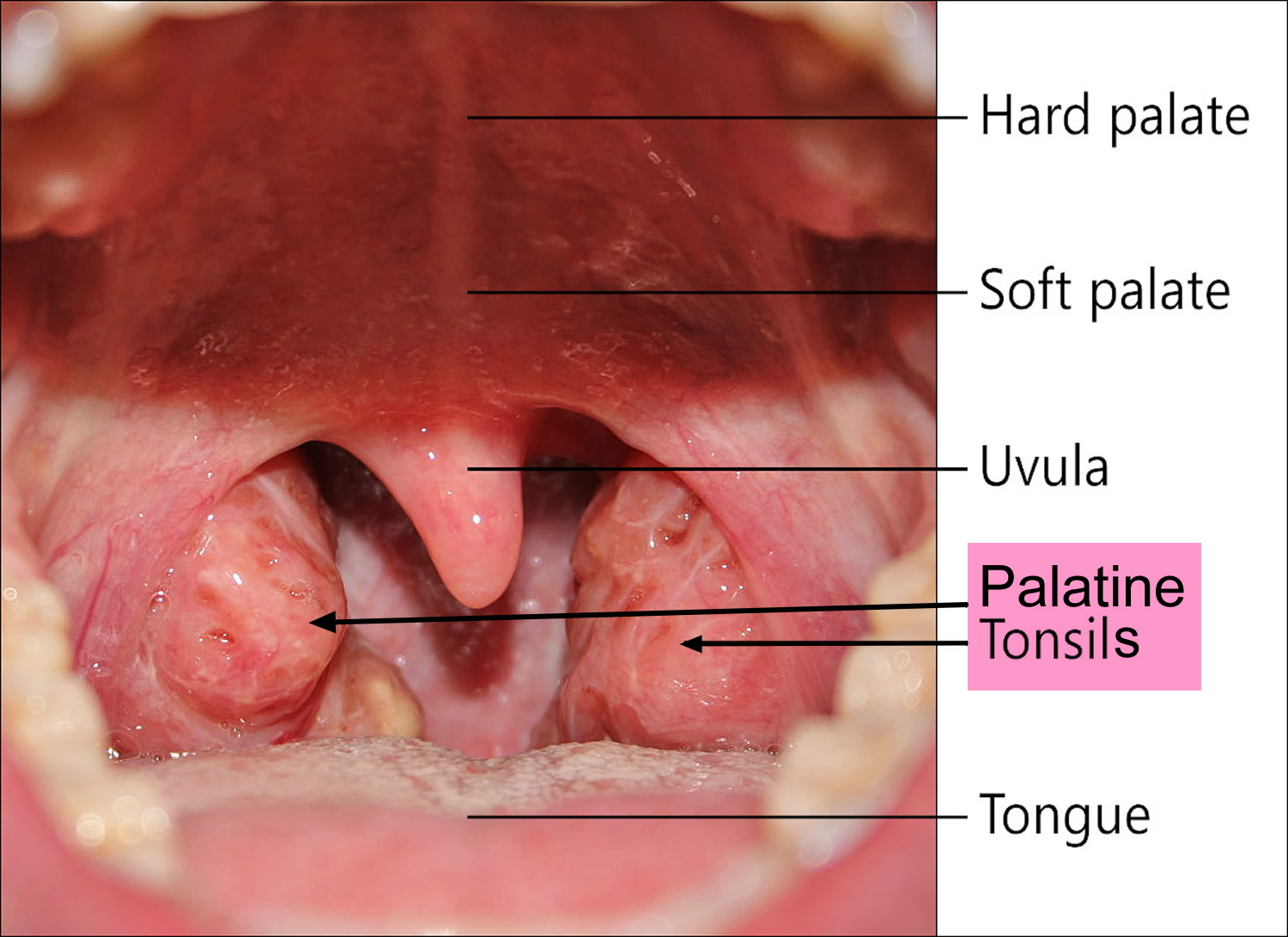
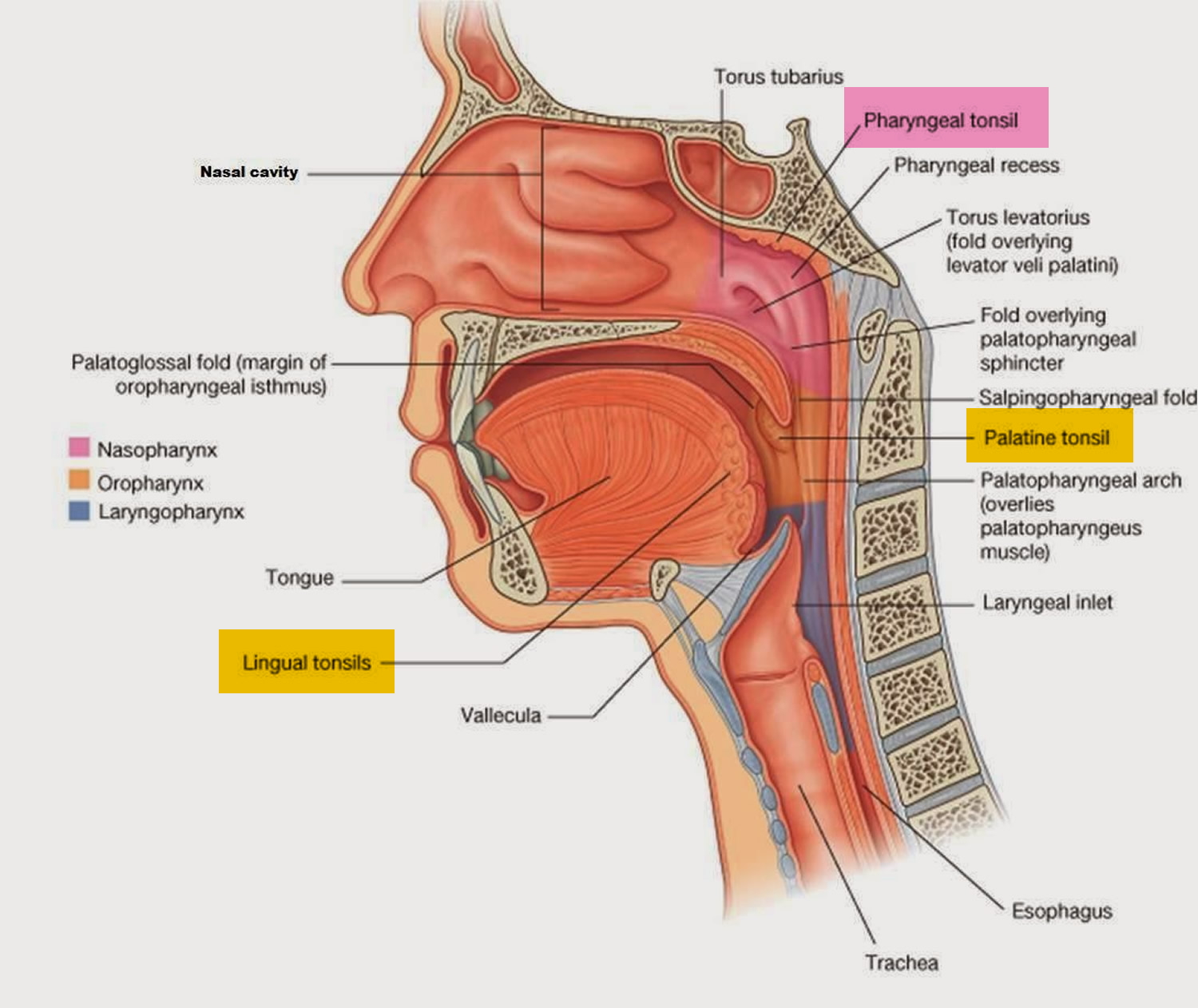
Throat cancer refers to cancer that begins in the throat (pharynx), voice box (larynx) or tonsils 1. The throat (also called pharynx) is a tube that runs from the back of the nose to your gullet (oesophagus) and the windpipe (trachea) (see Figure 1).
Your throat is a muscular tube that begins behind your nose and ends in your neck. Throat cancer has different names, depending on which part of the throat is affected. The different parts of your throat are called the oropharynx, the hypopharynx, the nasopharynx, and the larynx or voice box (see Figures 1 and 2).
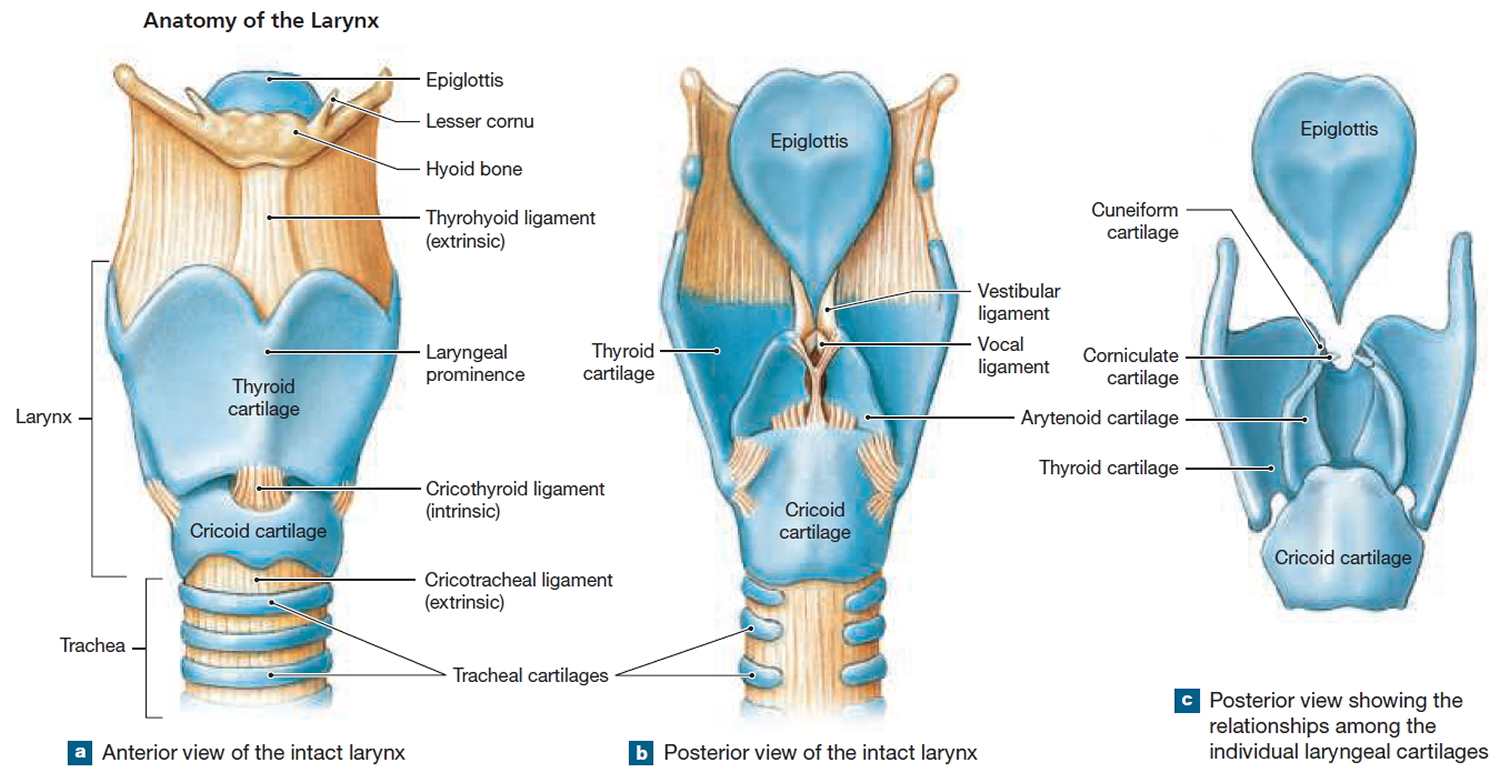
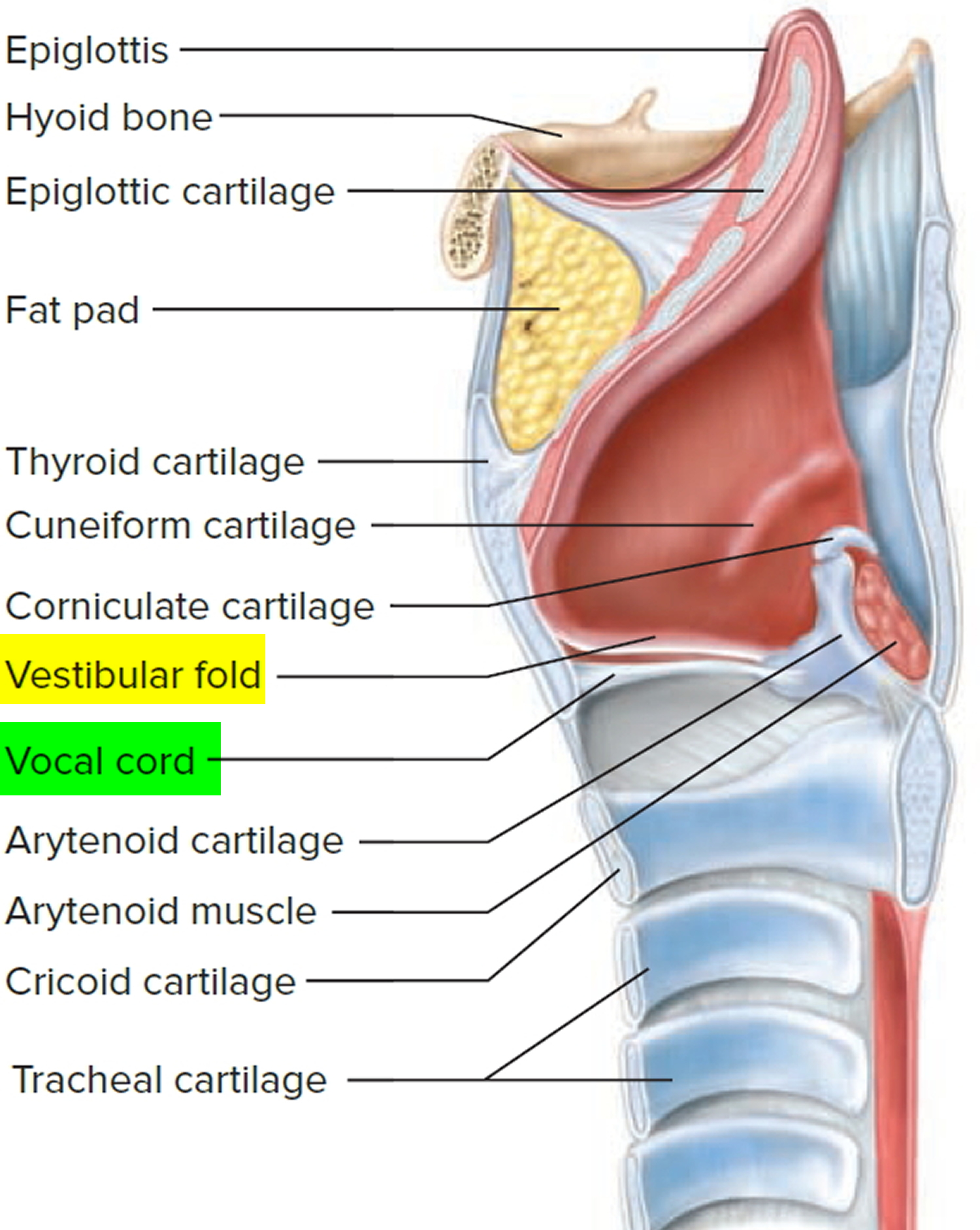
Your voice box (larynx) sits just below your throat and also is susceptible to throat cancer. The voice box (larynx) is made of cartilage and contains the vocal cords that vibrate to make sound when you talk (see Figure 2).
Throat cancer can also affect the piece of cartilage (epiglottis) that acts as a lid for your windpipe (see Figure 2). Tonsil cancer, another form of throat cancer, affects the tonsils, which are located on the back of the throat (see Figure 3 and 4).
Throat cancer is a type of head and neck cancer. Throat cancer most often begins in the flat cells that line the inside of your throat.
The main risk factors for throat cancer are using tobacco heavy drinking. Certain types of throat cancer also have other risk factors. For example, having HPV is a risk factor for oropharyngeal cancer.
Symptoms of throat cancer may include:
- A sore throat that does not go away
- A lump in the neck
- Pain or ringing in the ears
- Trouble swallowing
- Ear pain
To diagnose throat cancers, doctors may do a physical exam and history, imaging tests, and a biopsy. You may also need other tests, depending on the type of cancer. Treatments include surgery, radiation therapy, and chemotherapy. Treatment for some types of throat cancer may also include targeted therapy. Targeted therapy uses substances that attack cancer cells without harming normal cells.
Throat cancer can be successfully treated if it is diagnosed early. If you have any concerns, make an appointment to visit your doctor.
The pharynx and the larynx
The pharynx, is a common passageway shared by both the digestive and respiratory systems. The pharynx is a muscular funnel extending about 13 cm (5 in.) from the posterior nasal apertures to the larynx. The pharynx is attached above to the base of the skull and is continuous below, approximately at the level of cervical vertebrum C6, with the top of the esophagus. The walls of the pharynx are attached anteriorly to the margins of the nasal cavities, oral cavity, and larynx. Muscles of the pharynx play necessary roles in swallowing and speech.
The pharynx is subdivided into three regions (Figure 1):
- the Nasopharynx,
- the Oropharynx, and
- the Laryngopharynx.
Figure 1. Pharynx and larynx anatomy
The pharynx connects the nose, mouth, and throat. The digestive and respiratory systems share the pharynx. It extends between the posterior nasal apertures and the entrances to the trachea and esophagus. The curving superior and posterior walls are attached to the axial skeleton, but the lateral walls are flexible and muscular.
The Nasopharynx
The posterior apertures (choanae) of the nasal cavities open into the nasopharynx above the soft palate. The nasopharynx receives the auditory (eustachian) tubes from the middle ears and houses the pharyngeal tonsil. The nasopharynx passes only air and is lined by pseudostratified columnar epithelium. Inhaled air turns 90° downward as it passes through the nasopharynx. Relatively large particles (>10 μm) generally cannot make the turn because of their inertia. They collide with the wall of the nasopharynx and stick to the mucosa near the tonsil, which is well positioned to respond to airborne pathogens.
The Oropharynx
The oropharynx extends between the soft palate and the base of the tongue at the level of the hyoid bone. Like the posterior and inferior portions of the nasopharynx, the posterior portion of the oral cavity communicates directly with the oropharynx. The epithelium changes from a pseudostratified ciliated columnar epithelium to a nonkeratinized (mucosal type) stratified squamous epithelium at the boundary between the nasopharynx and oropharynx. The posterior margin of the soft palate supports the dangling uvula and two pairs of muscular pharyngeal arches, the posterior arch and the anterior arch.
The Laryngopharynx
The narrow laryngopharynx includes the region of the pharynx lying between the hyoid bone and the entrance to the esophagus. Like the oropharynx, the laryngopharynx is lined with a stratified squamous epithelium that resists abrasion, chemicals, and pathogens.
The Larynx
The larynx is the upper end of the lower airway. It is continuous with the trachea below and the pharynx posterosuperiorly.
The larynx is a cartilaginous chamber about 4 cm (1.5 in.) long. Its primary function is to keep food and drink out of the airway, but it evolved the additional role of sound production (phonation) in many animals; hence, we colloquially think of it as the “voice box.”
Figure 2. Larynx anatomy
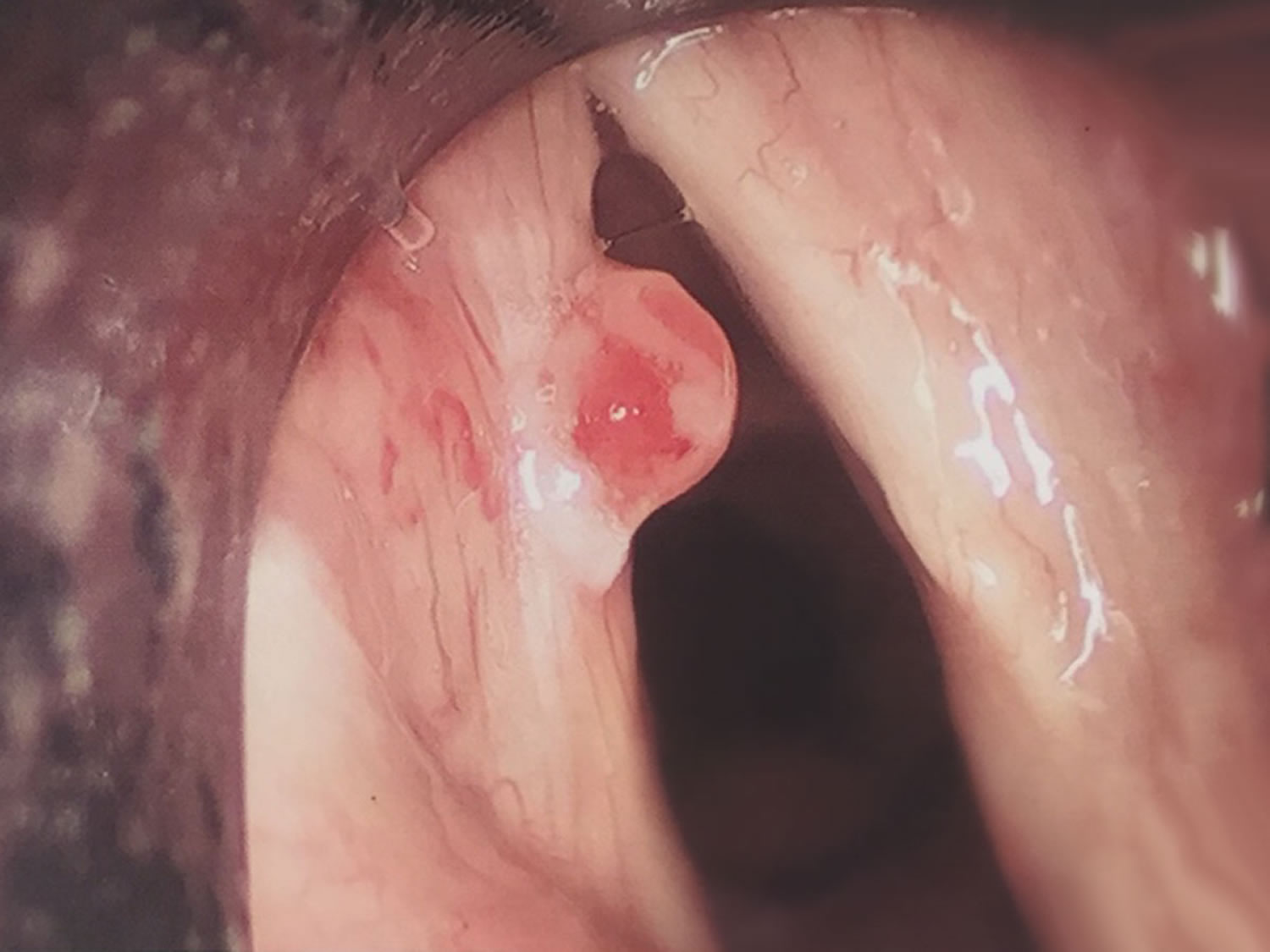
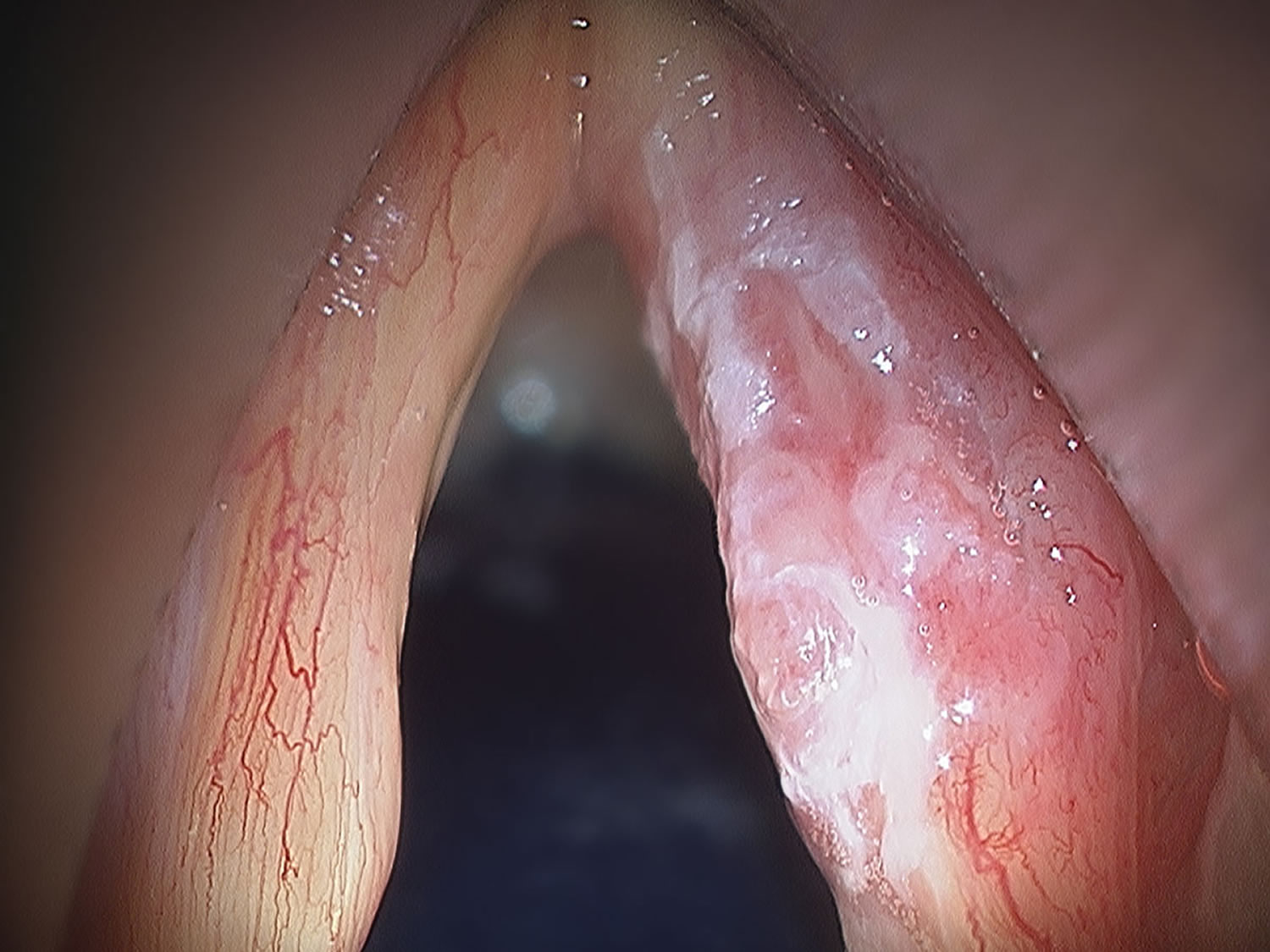
What does throat cancer look like
Figure 5. Larynx cancer
Figure 6. Glottic cancer
Types of throat cancer
Throat cancer is a general term that applies to cancer that develops in the throat (pharyngeal cancer) or in the voice box (laryngeal cancer). The throat and the voice box are closely connected, with the voice box located just below the throat.
Though most throat cancers involve the same types of cells, specific terms are used to differentiate the part of the throat where cancer originated.
- Nasopharyngeal cancer begins in the nasopharynx — the part of your throat just behind your nose.
- Oropharyngeal cancer begins in the oropharynx — the part of your throat right behind your mouth that includes your tonsils.
- Hypopharyngeal cancer (laryngopharyngeal cancer) begins in the hypopharynx (laryngopharynx) — the lower part of your throat, just above your esophagus and windpipe.
- Glottic cancer begins in the vocal cords.
- Supraglottic cancer begins in the upper portion of the larynx and includes cancer that affects the epiglottis, which is a piece of cartilage that blocks food from going into your windpipe.
- Subglottic cancer begins in the lower portion of your voice box, below your vocal cords.
Nasopharyngeal cancer
Nasopharyngeal cancer is a cancer that starts in the nasopharynx, the upper part of the throat behind the nose and near the base of skull (see Figure 1).
Several types of tumors can develop in the nasopharynx. Some of these tumors are benign (non-cancerous), but others are malignant (cancerous). It is important to discuss what type of tumor you might have with your doctor.
Nasopharyngeal cancer is fairly rare. In most parts of the world (including the United States), there is less than one case for every 100,000 people each year. In 2015, about 3,200 cases will occur in the United States.
This cancer is, however, much more common in certain parts of Asia and North Africa, particularly in southern China. It is also more common among Inuits of Alaska and Canada, and among some immigrant groups in the United States, such as recent Chinese and Hmong immigrants.
The risk of nasopharyngeal carcinoma increases slowly throughout life, but it can occur in people of any age, including children. About half of the people with nasopharyngeal carcinoma in the United States are younger than 55 years old.
Benign nasopharyngeal tumors
Benign tumors of the nasopharynx are fairly rare and tend to develop in children and young adults. These tumors do not spread to other parts of the body and are usually not life-threatening. They include tumors or malformations of the vascular (blood-carrying) system, such as angiofibromas and hemangiomas, and benign tumors of minor salivary glands within the nasopharynx.
Treatment of these benign tumors (if it is needed) is different from that for cancerous nasopharyngeal tumors and is not covered further in this document. If you have one of these tumors, you and your doctor will talk about what treatments might be appropriate for you.
Nasopharyngeal cancers
These tumors can invade surrounding tissues and spread to other parts of the body.
Nasopharyngeal carcinoma: This is by far the most common malignant tumor of the nasopharynx. A carcinoma is a cancer that starts in epithelial cells – the cells lining the internal and external surfaces of the body. Most of the rest of this document refers to nasopharyngeal carcinoma.
There are 3 types of nasopharyngeal carcinoma, based on how the cancer cells look under the microscope:
- Keratinizing squamous cell carcinoma
- Non-keratinizing differentiated carcinoma
- Undifferentiated carcinoma
Each of these types is seen more often in some areas of the world than in others. In southern China, where nasopharyngeal carcinoma is much more common, nearly all cases are the undifferentiated type. In the United States, where nasopharyngeal carcinoma is rare, about 1 out of 5 cases are the keratinizing type.
Even though these types look different when seen under a microscope, studies have shown they start from the same cell type – the epithelial cells that line the surface of the nasopharynx. The treatment is also usually the same for all types of nasopharyngeal carcinoma. The stage of the cancer – how far it has grown and spread – is often more important than its type in predicting a person’s outlook (prognosis).
Many nasopharyngeal carcinomas also contain lots of immune system cells, especially lymphocytes. The term lymphoepithelioma is sometimes used to describe an undifferentiated nasopharyngeal carcinoma with many lymphocytes among the cancer cells. The presence of these cells does not usually affect the choice of treatment options. But they may be a clue to developing new treatments since they may represent the body’s attempt to “reject” the tumor.
Other cancers in the nasopharynx: Other types of cancers can arise in the nasopharynx.
Lymphomas can sometimes start in the nasopharynx. They are cancers of immune system cells called lymphocytes, which are found throughout the body, including in the nasopharynx. These cancers are discussed in Non-Hodgkin Lymphoma.
Adenocarcinoma and adenoid cystic carcinoma are cancers that can develop in the minor salivary glands in the nasopharynx, but these cancers are more commonly found in the nose (nasal cavity) or mouth (oral cavity).
What Causes Nasopharyngeal Cancer?
The exact cause of most cases of nasopharyngeal cancer is not known. But scientists have found that the disease is linked with certain diets, infections, and inherited characteristics. Research is being done to learn more about these causes.
In recent years, scientists have studied how the Epstein-Barr virus (EBV) may cause cells in the nasopharynx to become cancerous, but much still remains to be learned. In developed countries, most people infected with EBV develop only infectious mononucleosis (mono), and their immune system is able to recognize and destroy the virus. These people recover without any long-term problems. But in some cases, pieces of viral DNA mix with the DNA of cells in the nasopharynx.
DNA is the chemical in each of your cells that makes up your genes, the instructions for how your cells function. You usually look like your parents because they are the source of your DNA. But DNA affects more than how you look. Some genes contain instructions for controlling when cells grow and divide into new cells. Viruses such as EBV also contain DNA. When a cell is infected with the virus, the viral DNA may mix with the normal human DNA. Epstein-Barr virus (EBV) DNA may instruct the cells of the nasopharynx to divide and grow in an abnormal way.
But Epstein-Barr virus (EBV) infection only rarely results in nasopharyngeal carcinoma, so other factors probably play a role in whether or not it causes cancer. Eating a diet high in salt-cured fish and meat seems to increase the ability of EBV to cause nasopharyngeal carcinoma. Studies show that foods preserved in this way may produce chemicals that can damage DNA. The damaged DNA alters a cell’s ability to control its growth and replication.
Some studies suggest that inheriting certain tissue types may contribute to a person’s risk of developing nasopharyngeal carcinoma. Because the tissue type plays a role in the function of the immune system, some scientists suspect that an abnormal immune reaction to EBV infection may be involved. The details of how certain tissue types might increase nasopharyngeal carcinoma risk are still being worked out.
Risk Factors for Nasopharyngeal Cancer
A risk factor is anything that affects a person’s chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking, can be changed. Others, like a person’s age or family history, can’t be changed.
But risk factors don’t tell us everything. Having a risk factor, or even several risk factors, does not mean that you will get the disease. And many people who get the disease may have few or no known risk factors.
Scientists have found several risk factors that make a person more likely to develop nasopharyngeal cancer. These include:
- Gender
- Ethnicity and where you live
- A certain kind of diet
- Infection with the Epstein-Barr virus
- Genetic factors
- Family history
Smoking, alcohol, and some workplace exposures may also increase the risk of this cancer.
These risk factors are discussed in more detail below
Gender
Nasopharyngeal carcinoma is found about twice as often in males as it is in females.
Race/ethnicity and where you live
Nasopharyngeal carcinoma is most common in southern China (including Hong Kong), Singapore, Vietnam, Malaysia, and the Philippines. It is also fairly common in Northwest Canada and Greenland.
People of south China have a lower risk of nasopharyngeal carcinoma if they move to another area that has lower rates of nasopharyngeal carcinoma (like the US or Japan), but their risk is still higher than for people who are native to areas with lower risk. Over time, their risk seems to go down. The risk also goes down in new generations. Although whites born in the United States have a low risk of nasopharyngeal carcinoma, whites born in China have a higher risk.
In the United States, nasopharyngeal carcinoma is most common in Asian and Pacific Islanders (particularly Chinese Americans), followed by American Indian and Alaskan natives, African Americans, whites, and Hispanics/Latinos.
Diet
People who live in parts of Asia, northern Africa, and the Arctic region where nasopharyngeal carcinoma is common, typically eat diets very high in salt-cured fish and meat. Indeed, the rate of this cancer is dropping in southeast China as people begin eating a more Westernized diet. In contrast, some studies have suggested that diets high in fruits and vegetables may lower the risk of nasopharyngeal carcinoma.
Epstein-Barr virus infection
Almost all nasopharyngeal carcinoma cells contain parts of the Epstein-Barr virus (EBV), and most people with nasopharyngeal carcinoma have evidence of infection by this virus in their blood. Infection with EBV is very common throughout the world, often occurring in childhood. In the United States, where infection with this virus tends to occur in slightly older children, it often causes infectious mononucleosis (“mono”), usually in teens.
The link between EBV infection and nasopharyngeal carcinoma is complex and not yet completely understood. EBV infection alone is not enough to cause nasopharyngeal carcinoma, since infection with this virus is very common and this cancer is rare. Other factors, such as a person’s genes, may affect how the body deals with EBV, which in turn may affect how EBV contributes to the development of nasopharyngeal carcinoma.
Genetic factors
A person’s genes may affect their risk for nasopharyngeal carcinoma. For example, just as people have different blood types, they also have different tissue types. Studies have found that people with certain inherited tissue types have an increased risk of developing nasopharyngeal carcinoma. Tissue types affect immune responses, so this may be related to how a person’s body reacts to Epstein-Barr virus (EBV) infection.
Family history
Family members of people with nasopharyngeal carcinoma are more likely to get this cancer. It is not known if this is because of inherited genes, shared environmental factors (such as the same diet or living quarters), or some combination of these.
Other possible risk factors
- Tobacco and alcohol use: Most (but not all) studies have found that smoking may contribute to the development of nasopharyngeal carcinoma, especially the keratinizing type. Some studies have linked heavy drinking to this type of cancer. More research is needed to define these links, but they seem to be much weaker than the link between tobacco and alcohol use and most other types of cancers that start in the throat.
- Workplace exposures: Some studies have suggested that workplace exposure to formaldehyde or wood dust may increase the risk of nasopharyngeal carcinoma. Still, not all studies have shown this and this link isn’t clear.
Can Nasopharyngeal Cancer Be Prevented?
Most people in the United States who develop nasopharyngeal cancer have no avoidable risk factors, so their cancers could not have been prevented. The possible links with tobacco and heavy alcohol use are not clear, so it’s not known if avoiding these can lower a person’s risk of nasopharyngeal carcinoma. However, both tobacco and alcohol use have clearly been linked to a number of other cancers, as well as other health problems, so avoiding them can have many health benefits.
Because certain dietary factors have been linked with nasopharyngeal carcinoma risk, reducing or eliminating some types of food may lower the number of cases in parts of the world where nasopharyngeal carcinoma is common, such as southern China, northern Africa, and the Arctic region. Descendants of Southeast Asians who immigrated to the United States and eat a typical American diet, for example, have a lower risk of developing nasopharyngeal carcinoma. But these dietary factors are not thought to account for all cases of nasopharyngeal carcinoma in most other parts of the world. Other factors, such as genetics, are likely to play a part as well.
Can Nasopharyngeal Cancer Be Found Early?
In the United States and other countries where nasopharyngeal cancer is fairly rare, most doctors do not recommend routine screening for this cancer (screening is testing for cancer in people without any symptoms). There are no simple, non-invasive exams or blood tests that can reliably find this cancer early.
But in some parts of the world such as China, where nasopharyngeal carcinoma is common, some people are being screened routinely for this cancer. They are first selected because their blood shows evidence of infection with the Epstein-Barr virus, although EBV infection is much more common than nasopharyngeal carcinoma. They are given regular exams of the nasopharynx and neck. This approach can also be used in families when one member has developed nasopharyngeal carcinoma. It isn’t known if this strategy lowers the death rate from this cancer.
Sometimes nasopharyngeal carcinoma can be found early if it causes symptoms that make patients seek medical attention. The symptoms may even seem unrelated to the nasopharynx (for example, a constant feeling of fullness in one ear). But in most people, nasopharyngeal carcinomas may not cause symptoms until they have reached an advanced stage.
Signs and Symptoms of Nasopharyngeal Cancer
About 3 out of 4 people with nasopharyngeal carcinoma complain of a lump or mass in the neck when they first see their doctor. There may be lumps on both sides of the neck towards the back. The lumps are usually not tender or painful. This is caused by the cancer spreading to lymph nodes in the neck, making them larger than normal. Lymph nodes are glands or organs that contain collections of immune system cells that are found throughout the body. Normally, they are smaller than the size of a pea.
Other possible symptoms of nasopharyngeal carcinoma include:
- Hearing loss, ringing in the ear, or feeling of fullness in the ear (especially on one side only)
- Ear infections that keep coming back
- Nasal blockage or stuffiness
- Nosebleeds
- Headache
- Facial pain or numbness
- Trouble opening the mouth
- Blurred or double vision
Ear infections are common in children, but are less common in adults. If you develop an infection in one ear and you have not had ear infections in the past, it is important to have a specialist examine your nasopharynx. This is especially true if you don’t have an upper respiratory tract infection (like a “cold”) along with the ear infection.
Many of the symptoms and signs of nasopharyngeal carcinoma are more often caused by other, less serious diseases. Still, if you have any of these problems, it’s important to see your doctor right away so the cause can be found and treated, if needed.
Nasopharyngeal Cancer Diagnosis
Nasopharyngeal cancer is most often diagnosed when a person goes to a doctor because of symptoms such as a lump in the neck. The doctor will take a history, do an exam, and then may refer the patient to a specialist and/or order some tests.
Medical history and physical exam
If you have any signs or symptoms that suggest you might have nasopharyngeal cancer, your doctor will want to get your complete medical history to learn about your symptoms and any possible risk factors, including your family history.
A physical exam will be done to look for signs of nasopharyngeal carcinoma or other health problems. During the exam, the doctor will pay special attention to the head and neck area, including the nose, mouth, and throat; the facial muscles, and the lymph nodes in the neck.
If your doctor suspects you may have a tumor or other problem in the nose or throat, he or she may order imaging tests (such as CT or MRI) to look at the head and neck area more closely. Your doctor may also refer you to an otolaryngologist (a doctor specializing in ear, nose, and throat problems, also sometimes called an ENT doctor), who will do a more thorough exam of the nasopharynx. The nasopharynx is a difficult area to examine. Most other kinds of doctors do not have the specialized training or equipment to do a thorough exam of this part of the body.
Exams of the nasopharynx
The nasopharynx is located deep inside the head and is not easily seen, so special techniques are needed to examine this area. There are 2 main types of exams used to look inside the nasopharynx for abnormal growths, bleeding, or other signs of disease. Both types of exams are usually done in the doctor’s office.
- For indirect nasopharyngoscopy, the doctor uses special small mirrors and lights placed at the back of your throat to look at the nasopharynx and nearby areas.
- For direct nasopharyngoscopy, the doctor uses a fiber-optic scope known as a nasopharyngoscope (a flexible, lighted, narrow tube inserted through the nose) to look directly at the lining of the nasopharynx. You will have numbing medicine sprayed into your nose before the exam to make it easier. This is the method most often used to carefully examine the nasopharynx.
If a tumor starts under the lining of the nasopharynx (in the tissue called the submucosa), it may not be possible to see it directly on physical exam, which is why imaging tests such as CT scans (see below) may be needed as well.
Biopsy
Symptoms and the results of exams can suggest that a person might have nasopharyngeal carcinoma, but the actual diagnosis is made by removing cells from an abnormal area and looking at them under a microscope. This is known as a biopsy. Different types of biopsies may be done, depending on where the abnormal area is.
Endoscopic biopsy
If a suspicious growth is found in the nasopharynx during an exam, the doctor may remove a biopsy sample with small instruments and the aid of a fiber-optic scope. Often, biopsies of the nasopharynx are done in the operating room as an outpatient procedure. The sample is then sent to a lab, where a pathologist (a doctor who specializes in diagnosing and classifying diseases in the lab) looks at it under a microscope. If the biopsy sample contains cancer cells, the pathologist sends back a report describing the type of the cancer.
Nasopharyngeal carcinoma is not always visible during an exam. If a person has symptoms suggesting nasopharyngeal carcinoma but nothing abnormal is seen on exam, the doctor may biopsy normal-looking tissue, which may be found to contain cancer cells when looked at under the microscope.
Fine needle aspiration (FNA) biopsy
An FNA biopsy may be used if you have a suspicious lump in or near your neck. For this procedure, the doctor uses a thin, hollow needle attached to a syringe to aspirate (withdraw) a few drops of fluid containing cells and tiny fragments of tissue. A local anesthetic (numbing medicine) may be used on the skin where the needle will be inserted might be numbed with a local anesthetic but sometimes this is not needed.
The doctor places the needle directly into the mass for about 10 seconds and withdraws cells and a few drops of fluid. The cells are then looked at under a microscope to see if they are cancerous.
An FNA biopsy can help determine if an enlarged lymph node in the neck area is caused by a response to an infection, the spread of cancer from somewhere else (such as the nasopharynx), or a cancer that begins in lymph nodes – called a lymphoma. If the cancer started somewhere else, the FNA biopsy alone might not be able to tell where it started. But if a patient already known to have nasopharyngeal carcinoma has enlarged neck lymph nodes, FNA can help determine if the spread of nasopharyngeal carcinoma caused the lymph node swelling.
Imaging tests
Imaging tests use x-rays, magnetic fields, sound waves, or radioactive particles to create pictures of the inside of your body. Imaging tests may be done for a number of reasons, including to help find a suspicious area that might be cancerous, to learn how far cancer may have spread, and to help determine if treatment has been effective.
Chest x-ray
If you have been diagnosed with nasopharyngeal carcinoma, a plain x-ray of your chest may be done to see if the cancer has spread to your lungs. This is very unlikely unless your cancer is far advanced. This x-ray can be done in any outpatient setting. If the results are normal, you probably don’t have cancer in your lungs.
Computed tomography (CT) scan
The CT scan is an x-ray test that produces detailed cross-sectional images of your body. Instead of taking one x-ray, a CT scanner takes many pictures as it rotates around you. A computer then combines them into images of slices of the part of your body that is being studied.
Before the pictures are taken, you may get an IV (intravenous) line through which a kind of contrast dye (IV contrast) is injected. This helps better outline structures in your body. You may also be asked to drink 1 to 2 pints of a liquid called oral contrast. This helps outline the intestine so that certain areas are not mistaken for tumors. It may not be needed for CT scans of the nasopharynx.
The injection can cause some flushing (redness and warm feeling). Some people are allergic and get hives or, rarely, more serious reactions like trouble breathing and low blood pressure. Be sure to tell the doctor if you have any allergies or have ever had a reaction to a contrast material used for x-rays.
You need to lie still on a table while the scan is being done. During the test, the table slides in and out of the scanner, a ring-shaped machine that completely surrounds the table. You might feel a bit confined by the ring you have to lie in while the pictures are being taken.
A CT scan of the head and neck can provide information about the size, shape, and position of a tumor and can help find enlarged lymph nodes that might contain cancer. CT scans or MRIs are important in looking for cancer that may have grown into the bones at the base of the skull. This is a common place for nasopharyngeal cancer to grow. CT scans can also be used to look for tumors in other parts of the body.
Magnetic resonance imaging (MRI) scan
Like CT scans, MRI scans provide detailed images of soft tissues in the body. But MRI scans use radio waves and strong magnets instead of x-rays. The energy from the radio waves is absorbed and then released in a pattern formed by the type of body tissue and by certain diseases. A computer translates the pattern into very detailed images of parts of the body. A contrast material called gadolinium is often injected into a vein before the scan to better see details.
MRI scans may be a little more uncomfortable than CT scans. They take longer – often up to an hour. You may be asked to lie on a table that slides inside a large tube, which is confining and can upset people with a fear of enclosed spaces. Special, “open” MRI machines can sometimes help with this if needed, but the drawback is that the images may not be as clear. The MRI machine makes buzzing and clicking noises that you may find disturbing. Some places will provide earplugs to help block this noise out.
Like CT scans, MRIs can be used to try to determine if the cancer has grown into structures near the nasopharynx. MRIs are a little better than CT scans at showing the soft tissues in the nose and throat, but they’re not quite as good for looking at the bones at the base of the skull, a common place for nasopharyngeal cancer to grow.
Positron emission tomography (PET) scan
For a PET scan, you receive an injection of a form of radioactive sugar (known as fluorodeoxyglucose or FDG). The amount of radioactivity used is low. Because cancer cells in the body are growing rapidly, they absorb large amounts of the sugar. After about an hour, you are moved onto a table in the PET scanner. You lie on the table for about 30 minutes while a special camera creates a picture of areas of radioactivity in the body. The picture is not finely detailed like a CT or MRI scan, but it provides helpful information about your whole body.
Your doctor may use this test to see if the cancer has spread to your lymph nodes. It can also help give the doctor a better idea of whether an abnormal area on a chest x-ray may be cancer. A PET scan can also be useful if your doctor thinks the cancer may have spread but doesn’t know where.
Some machines are able to do both a PET and CT scan at the same time (PET/CT scan). This lets the doctor compare areas of higher radioactivity on the PET with the more detailed appearance of that area on the CT.
Blood tests
Blood tests are not used to diagnose nasopharyngeal carcinoma, but they may be done for other reasons, such as to help determine whether the cancer may have spread to other parts of the body.
Routine blood counts and blood chemistry tests
Routine blood tests can help determine a patient’s overall health. These tests can help diagnose malnutrition, anemia (low red blood counts), liver disease, and kidney disease. And they may suggest the possibility of spread of the cancer to the liver or bone, which may prompt further testing.
In people getting chemotherapy, blood tests are important to see if the treatment is damaging the bone marrow (where new blood cells are made), liver, and kidneys.
Epstein-Barr virus (EBV) DNA levels
In some patients, the blood level of EBV DNA may be measured before and after treatment to help show how effective treatment is.
Nasopharyngeal Cancer Stages
After someone is diagnosed with nasopharyngeal cancer, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it. Doctors also use a cancer’s stage when talking about survival statistics.
The earliest stage of nasopharyngeal carcinoma is stage O, also known as carcinoma in situ (CIS). The other main stages range from I (1) through IV (4). Some stages are split further, using capital letters (A, B, etc.). As a rule, the lower the number, the less the cancer has spread. A higher number, such as stage IV, means cancer has spread more. And within a stage, an earlier letter means a lower stage. Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
How is the stage determined?
The staging system most often used for nasopharyngeal cancer is the American Joint Committee on Cancer (AJCC) TNM system, which is based on 3 key pieces of information:
- The extent of the main tumor (T): How far has the tumor grown into nearby structures?
- The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes in the neck? If so, how large are they?
- The spread (metastasis) to distant sites (M): Has the cancer spread to distant parts of the body? (The most common sites of spread are the lungs, liver, bones, or lymph nodes in distant parts of the body.)
These categories are determined mainly based on the results of any exams, biopsies, and imaging tests that have been done. Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced.
Once the T, N, and M categories of the cancer have been determined, this information is combined in a process called stage grouping to assign an overall stage. For more information, see Cancer Staging.
The system described below is the most recent AJCC system for nasopharyngeal carcinoma, effective January 2018.
Nasopharyngeal carcinoma staging can be complex. If you have questions about your cancer’s stage and what it might mean for you, ask your doctor to explain it to you in a way you understand.
Table 1. Stages of nasopharyngeal cancer
| AJCC stage | Stage grouping | Stage description* |
| 0 | Tis N0 M0 | The tumor is only in the top layer of cells lining the inside of the nasopharynx, and has not grown any deeper (Tis). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| I | T1 N0 M0 | The tumor is in the nasopharynx. It might also have grown into the oropharynx (the part of the throat in the back of the mouth) and/or nasal cavity but no farther (T1) The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
|
II | T1 (or T0) N1 M0 | The tumor is in the nasopharynx. It might also have grown into the oropharynx (the part of the throat behind the mouth) and/or nasal cavity but no farther (T1). OR no tumor is seen in the nasopharynx, but cancer is found in lymph nodes in the neck and is Epstein-Barr virus (EBV) positive, which makes it very likely to be NPC (T0). The cancer has spread to 1 or more lymph nodes on one side of the neck, or it has spread to lymph nodes behind the throat. In either case, no lymph node is larger than 6 cm across (N1). The cancer has not spread to distant parts of the body (M0). |
| OR | ||
| T2 N0 or N1 M0 | The tumor has grown into the tissues of the left or right sides of the upper part of the throat (but not into bone) (T2). The cancer has not spread to nearby lymph nodes (N0). OR it has spread to 1 or more lymph nodes on one side of the neck, or it has spread to lymph nodes behind the throat. In either case, no lymph node is larger than 6 cm across (N1). The cancer has not spread to distant parts of the body (M0). | |
|
III | T1 (or T0) N2 M0 | The tumor is in the nasopharynx. It might also have grown into the oropharynx (the part of the throat behind the mouth) and/or nasal cavity but no farther (T1). OR no tumor is seen in the nasopharynx, but cancer is found in lymph nodes in the neck and is Epstein-Barr virus (EBV) positive, which makes it very likely to be NPC (T0). The cancer has spread to lymph nodes on both sides of the neck, none of which is larger than 6 cm across (N2). The cancer has not spread to distant parts of the body (M0). |
| OR | ||
| T2 N2 M0 | The tumor has grown into the tissues of the left or right sides of the upper part of the throat (but not into bone) (T2). The cancer has spread to lymph nodes on both sides of the neck, none of which is larger than 6 cm across (N2). The cancer has not spread to distant parts of the body (M0). | |
| OR | ||
| T3 N0 to N2 M0 | The tumor has grown into the sinuses and/or the bones nearby (T3). The cancer might or might not have spread to nearby lymph nodes in the neck or behind the throat, but none are larger than 6 cm across (N0 to N2). The cancer has not spread to distant parts of the body (M0). | |
|
IVA | T4 N0 to N2 M0 | The tumor has grown into the skull and/or cranial nerves, the hypopharynx (lower part of the throat), the main salivary gland, or the eye or its nearby tissues (T4). The cancer might or might not have spread to nearby lymph nodes in the neck or behind the throat, but none are larger than 6 cm across (N0 to N2). The cancer has not spread to distant parts of the body (M0). |
| OR | ||
| Any T N3 M0 | The tumor might or might not have grown into structures outside the nasopharynx (any T). The cancer has spread to lymph nodes that are either larger than 6 cm across, or located in the shoulder area just above the collarbone (N3). The cancer has not spread to distant parts of the body (M0). | |
| IVB | Any T Any N M1 | The tumor might or might not have grown into structures outside the nasopharynx (any T). The cancer might or might not have spread to nearby lymph nodes (any N). The cancer has spread to distant parts of the body (M1). |
*The following additional categories are not listed in the table above:
- TX: Main tumor cannot be assessed due to lack of information.
- NX: Nearby lymph nodes cannot be assessed due to lack of information.
Survival Rates for Nasopharyngeal Cancer by Stage
Statistics on the outlook for a certain type and stage of cancer are often given as 5-year survival rates, but many people live longer – often much longer – than 5 years.
But keep in mind that survival rates are estimates – your outlook can vary based on a number of factors specific to you.
Cancer survival rates don’t tell the whole story.
Survival rates are often based on previous outcomes of large numbers of people who had the disease, but they can’t predict what will happen in any particular person’s case. There are some limitations to remember:
- The numbers below are among the most current available. But to get 5-year survival rates, doctors have to look at people who were treated at least several years ago. As treatments are improving over time, people who are now being diagnosed with nasopharyngeal cancer may have a better outlook than these statistics show.
- These statistics are based on the stage of the cancer when it was first diagnosed. They do not apply to cancers that later come back or spread, for example.
- The outlook for people with nasopharyngeal cancer varies by the stage (extent) of the cancer – in general, the survival rates are higher for people with earlier stage cancers. But many other factors can also affect a person’s outlook, such as a person’s age and overall health, where the cancer is in the body, and how well the cancer responds to treatment. The outlook for each person is specific to their circumstances.
Your doctor can tell you how these numbers may apply to you, as he or she is familiar with your particular situation.
Survival rates for nasopharyngeal cancer
The numbers below were published in 2010 in the 7th edition of the AJCC Cancer Staging Manual and are based on people diagnosed between 1998 and 1999.
| Stage | Relative 5-year survival rate |
| I | 72% |
| II | 64% |
| III | 62% |
| IV | 38% |
Remember, these survival rates are only estimates – they can’t predict what will happen to any individual. We understand that these statistics can be confusing and may lead you to have more questions. Talk with your doctor to better understand your situation.
Nasopharyngeal cancer treatment
After the cancer is found and staged, your cancer care team will discuss treatment options (choices) with you. Depending on the stage of the cancer, your overall health, and other factors, your treatment options may include:
- Surgery
- Radiation therapy
- Chemotherapy
- Targeted therapy
Depending on the stage of the cancer, some of these treatments may be combined. For most nasopharyngeal cancers, a combination of radiation therapy and chemotherapy is used.
Oral Cavity and Oropharyngeal Cancer
Oral cavity cancer, or just oral cancer, is cancer that starts in the mouth (also called the oral cavity). Oropharyngeal cancer starts in the oropharynx, which is the part of the throat just behind the mouth.
The oral cavity includes the lips, the inside lining of the lips and cheeks (buccal mucosa), the teeth, the gums, the front two-thirds of the tongue, the floor of the mouth below the tongue, and the bony roof of the mouth (hard palate). The area behind the wisdom teeth (called the retromolar trigone) can be included as a part of the oral cavity, although it is often considered part of the oropharynx.
The oropharynx is the part of the throat just behind the mouth. It begins where the oral cavity stops. It includes the base of the tongue (the back third of the tongue), the soft palate (the back part of the roof of the mouth), the tonsils, and the side and back wall of the throat.
The oral cavity and oropharynx help you breathe, talk, eat, chew, and swallow. Minor salivary glands throughout the oral cavity and oropharynx make saliva that keeps your mouth moist and helps you digest food.
The different parts of the oral cavity and oropharynx are made up of several types of cells. Different cancers can develop from each type of cell. The differences are important, because they can influence a person’s treatment options and prognosis (outlook).
Several types of cancers can start in the mouth or throat.
Squamous cell carcinomas
More than 90% of cancers of the oral cavity and oropharynx are squamous cell carcinomas, also called squamous cell cancers. These cancers begin in early forms of squamous cells, which are flat, scale-like cells that normally form the lining of the mouth and throat.
The earliest form of squamous cell cancer is called carcinoma in situ, meaning that the cancer cells are present only in the outer layer of cells called the epithelium. This is different from invasive squamous cell carcinoma, where the cancer cells have grown into deeper layers of the oral cavity or oropharynx.
Verrucous carcinoma
Verrucous carcinoma is a type of squamous cell carcinoma that makes up less than 5% of all oral cancers. It is a low-grade (slow growing) cancer that rarely spreads to other parts of the body, but it can grow deeply into surrounding tissue.
If they are not treated, areas of ordinary squamous cell cancer may develop within some verrucous carcinomas. Some verrucous carcinomas may already have areas of ordinary squamous cell cancer that are not recognized in the biopsy sample. Cells from these areas of squamous cell carcinoma may then spread to other parts of the body.
For all of these reasons, verrucous carcinomas should be removed promptly, along with a wide margin of surrounding normal tissue.
Minor salivary gland carcinomas
Minor salivary gland cancers can develop in the glands in the lining of the mouth and throat. There are several types of minor salivary gland cancers, including adenoid cystic carcinoma, mucoepidermoid carcinoma, and polymorphous low-grade adenocarcinoma.
Lymphomas
The tonsils and base of the tongue contain immune system (lymphoid) tissue, where cancers called lymphomas can start.
The American Cancer Society’s most recent estimates for oral cavity and oropharyngeal cancers in the United States are for 2018:
About 51,540 people will get oral cavity or oropharyngeal cancer.
An estimated 10,030 people will die of these cancers.
These cancers are more than twice as common in men as in women. They are about equally common in blacks and in whites.
In recent years, the overall rate of new cases of this disease has been stable in men and dropping slightly in women. However, there has been a recent rise in cases of oropharyngeal cancer linked to infection with human papillomavirus (HPV) in white men and women.
The death rate for these cancers has been decreasing over the last 30 years.
Oral cavity and oropharyngeal cancers occur most often in the following sites:
- The tongue
- The tonsils and oropharynx
- The gums, floor of the mouth, and other parts of the mouth
The rest are found in the lips, the minor salivary glands (which often occur in the roof of the mouth), and other sites.
The average age of most people diagnosed with these cancers is 62, but they can occur in young people. They are rare in children, but a little more than one-quarter occur in patients younger than 55.
The rates of these cancers vary among countries. For example, they are much more common in Hungary and France than in the United States and much less common in Mexico and Japan.
When patients newly diagnosed with oral and oropharyngeal cancers are carefully examined, a small portion will have another cancer in a nearby area such as the larynx (voice box), the esophagus (the tube that carries food from the throat to the stomach), or the lung. Some who are cured of oral or oropharyngeal cancer will develop another cancer later in the lung, mouth, throat, or other nearby areas. For this reason, people with oral and oropharyngeal cancer will need to have follow-up exams for the rest of their lives. They also need to avoid using tobacco and alcohol, which increase the risk for these second cancers.
What Causes Oral Cavity and Oropharyngeal Cancers?
Doctors and scientists can’t say for sure what causes each case of oral cavity or oropharyngeal cancer. But they do know many of the risk factors and how some of them may lead to cells becoming cancerous.
Scientists believe that some risk factors, such as tobacco or heavy alcohol use, may cause these cancers by damaging the DNA of cells that line the inside of the mouth and throat.
DNA is the chemical in each of our cells that makes up our genes — the instructions for how our cells function. We usually look like our parents because they are the source of our DNA. However, DNA affects more than how we look. Some genes called proto-oncogenes can help control when cells grow and divide. DNA changes can change these into genes that promote cell division that are called oncogenes. Some genes that slow down cell division or make cells die at the right time and are called tumor suppressor genes. DNA changes can turn off tumor suppressor genes, and lead to cells growing out of control. Cancers can be caused by DNA changes that create oncogenes or turn off tumor suppressor genes.
When tobacco and alcohol damage the cells lining the mouth and throat, the cells in this layer must grow more rapidly to repair this damage. The more often cells need to divide, the more chances there are for them to make mistakes when copying their DNA, which may increase their chances of becoming cancerous.
Many of the chemicals found in tobacco can damage DNA directly. Scientists are not sure whether alcohol directly damages DNA, but they have shown that alcohol helps many DNA-damaging chemicals get into cells more easily. This may be why the combination of tobacco and alcohol damages DNA far more than tobacco alone.
This damage can cause certain genes (for example, those in charge of starting or stopping cell growth) to malfunction. Abnormal cells can begin to build up, forming a tumor. With additional damage, the cells may begin to spread into nearby tissue and to distant organs.
In human papillomavirus (HPV) infections, the virus causes cells to make 2 proteins known as E6 and E7. When these are made, they turn off some genes that normally help keep cell growth in check. Uncontrolled cell growth may in some cases lead to cancer. When HPV DNA is found in the tumor cells, especially in non-smokers who drink little or no alcohol, HPV is thought to be the likely cause of the cancer.
Some people inherit DNA mutations (changes) from their parents that increase their risk for developing certain cancers. But inherited oncogene or tumor suppressor gene mutations are not believed to cause very many cancers of the oral cavity or oropharynx.
Some oral cavity and oropharyngeal cancers have no clear cause. Some of these cancers may be linked to other, as of yet unknown risk factors. Others may have no external cause — they may just occur because of random DNA mutations inside a cell.
Risk Factors for Oral Cavity and Oropharyngeal Cancers
Tobacco and alcohol
Tobacco and alcohol use are among the strongest risk factors for oral cavity and oropharyngeal cancers.
Tobacco use
Most people with oral cavity and oropharyngeal cancers use tobacco, and the risk of developing these cancers is related to how much and how long they smoked or chewed.
Smokers are many times more likely than non-smokers to develop these cancers. Tobacco smoke from cigarettes, cigars, or pipes can cause cancers anywhere in the mouth or throat, as well as causing cancers of the larynx (voice box), lungs, esophagus, kidneys, bladder, and several other organs.
Pipe smoking is a particularly significant risk for cancers in the area of the lips that touch the pipe stem.
It is important for smokers who have been treated for oral cavity or oropharyngeal cancer to quit smoking, even if their cancer seems to be cured. Continuing to smoke greatly increases their risk of developing a second cancer of the mouth, throat, larynx (voice box), or lung.
Oral tobacco products (snuff or chewing tobacco) are linked with cancers of the cheek, gums, and inner surface of the lips. Using oral tobacco products for a long time poses an especially high risk. These products also cause gum disease, destruction of the bone sockets around teeth, and tooth loss. It is also important for people who have been treated for oral cavity or oropharyngeal cancer to give up any oral tobacco products.
Drinking alcohol
Drinking alcohol increases the risk of developing oral cavity and oropharyngeal cancers. About 7 out of 10 patients with oral cancer are heavy drinkers.
Drinking and smoking together
The risk of these cancers is even higher in people who both smoke and drink alcohol, with the highest risk in heavy smokers and drinkers. According to some studies, the risk of these cancers in heavy drinkers and smokers may be as much as 100 times more than the risk of these cancers in people who don’t smoke or drink.
Betel quid and gutka
In Southeast Asia, South Asia, and certain other areas of the world, many people chew betel quid, which is made up of areca nut and lime wrapped in a betel leaf. Many people in these areas also chew gutka, a mixture of betel quid and tobacco. People who chew betel quid or gutka have an increased risk of cancer of the mouth.
Human papillomavirus (HPV) infection
Human papillomavirus (HPV) is a group of more than 150 types of viruses. They are called papillomaviruses because some of them cause a type of growth called a papilloma. Papillomas are not cancers, and are more commonly called warts.
Infection with certain types of HPV can also cause some forms of cancer, including cancers of the penis, cervix, vulva, vagina, anus, and throat. Other types of HPV cause warts in different parts of the body.
HPV can be passed from one person to another during skin-to-skin contact. One way HPV is spread is through sexual activity, including vaginal and anal intercourse and even oral sex.
HPV types are given numbers. The type linked to throat cancer (including cancer of the oropharynx) is HPV16.
Most people with HPV infections of the mouth and throat have no symptoms, and only a very small percentage develop oropharyngeal cancer. Oral HPV infection is more common in men than in women. In some studies, the risk of oral HPV infection was linked to certain sexual activities, such as open mouth kissing and oral-genital contact (oral sex). Smoking also increases the risk of oral HPV infection . At this time the US Food and Drug Administration has not approved a test for HPV infection of the mouth and throat.
The number of oropharyngeal cancers linked to HPV has risen dramatically over the past few decades. HPV DNA (a sign of HPV infection) is now found in about 2 out of 3 oropharyngeal cancers and in a much smaller fraction of oral cavity cancers. The reason for the rising rate of HPV-linked cancers is unclear, although some think that it could be because of changes in sexual practices in recent decades, in particular an increase in oral sex.
Oropharyngeal cancers that contain HPV DNA tend to have a better outlook than those without HPV.
Gender
Oral and oropharyngeal cancers are more common in men than in women. This might be because men have been more likely to use tobacco and alcohol in the past.
Age
Cancers of the oral cavity and oropharynx usually take many years to develop, so they are not common in young people. Most patients with these cancers are older than 55 when the cancers are first found. But this may be changing as HPV-linked cancers become more common.
Ultraviolet (UV) light
Sunlight is the main source of UV light for most people. Cancers of the lip are more common in people who have outdoor jobs where they are exposed to sunlight for long periods of time.
Poor nutrition
Several studies have found that a diet low in fruits and vegetables is linked with an increased risk of cancers of the oral cavity and oropharynx.
Weakened immune system
Oral cavity and oropharyngeal cancers are more common in people who have a weak immune system. A weak immune system can be caused by certain diseases present at birth, the acquired immunodeficiency syndrome (AIDS), and certain medicines (such as those given after organ transplants).
Graft-versus-host disease
Graft-versus-host disease (GVHD) is a condition that sometimes occurs after a stem cell transplant. During this medical procedure, blood stem cells from a donor are used to replace bone marrow that has been destroyed by disease, chemotherapy, or radiation. GVHD occurs when the donor stem cells recognize the patient’s cells as foreign and launch an attack against them. GVHD can affect many tissues of the body, including those in the mouth. This increases the risk of oral cancer, which can occur as early as 2 years after GVHD.
Genetic syndromes
People with certain syndromes caused by inherited defects (mutations) in certain genes have a very high risk of mouth and throat cancer.
Fanconi anemia is a condition that can be caused by inherited defects in several genes that contribute to repair of DNA. People with this syndrome often have blood problems at an early age, which may lead to leukemia or aplastic anemia. They also have a very high risk of cancer of the mouth and throat.
Dyskeratosis congenita is a genetic syndrome that can cause aplastic anemia, skin rashes, and abnormal fingernails and toenails. People with this syndrome also have a very high risk of developing cancer of the mouth and throat at an early age.
Lichen planus
This disease occurs mainly in middle-aged people. Most often it affects the skin (usually as an itchy rash), but it sometimes affects the lining of the mouth and throat, appearing as small white lines or spots. A severe case may slightly increase the risk of oral cancer.
Unproven or controversial risk factors
Mouthwash
Some studies have suggested that mouthwash with a high alcohol content might be linked to a higher risk of oral and oropharyngeal cancers. But recent research has questioned these results. Studying this possible link is complicated by the fact that smokers and frequent drinkers (who already have an increased risk of these cancers) are more likely to use mouthwash than people who neither smoke nor drink.
Irritation from dentures
It has been suggested that long-term irritation of the lining of the mouth caused by poorly fitting dentures is a risk factor for oral cancer. But many studies have found no increased risk in denture wearers overall.
Poorly fitting dentures can tend to trap agents that have been proven to cause oral cancer, such as alcohol and tobacco particles, so denture wearers should have them checked by a dentist regularly to ensure a good fit. All denture wearers should remove their dentures at night and clean and rinse them thoroughly every day.
Oral Cavity and Oropharyngeal Cancers Prevention
Avoid risk factors
Not all cases of oral cavity and oropharyngeal cancer can be prevented, but the risk of developing these cancers can be greatly reduced by avoiding certain risk factors.
Limit smoking and drinking
Tobacco and alcohol are among the most important risk factors for these cancers. Not starting to smoke is the best way to limit the risk of getting these cancers. Quitting tobacco also greatly lowers your risk of developing these cancers, even after many years of use. The same is true of heavy drinking. Limit how much alcohol you drink, if you drink at all.
HPV infection
The risk of infection of the mouth and throat with the human papillomavirus (HPV) is increased in those who have oral sex and multiple sex partners. But again, HPV is very common, so having sex with even one other person can put you at risk.
These infections are also more common in smokers, which may be because the smoke damages their immune system or the cells that line the oral cavity. These infections are common and rarely cause symptoms. Although HPV infection is linked to oropharyngeal cancer, most people with HPV infections of the mouth and throat do not go on to develop this cancer. In addition, many oral and oropharyngeal cancers are not related to HPV infection.
In recent years, vaccines that reduce the risk of infection with certain types of HPV have become available. These vaccines were originally meant to lower the risk of cervical cancer, but they have been shown to lower the risk of other cancers linked to HPV as well, such as cancers of the penis, anus, vulva, and vagina. HPV vaccination may also lower the risk of mouth and throat cancers, but this has not yet been proven.
Since these vaccines are only effective if given before someone is infected with HPV, they are given when a person is young, before they are likely to become sexually active.
Limit exposure to ultraviolet (UV) light
Ultraviolet radiation is an important and avoidable risk factor for cancer of the lips, as well as for skin cancer. If possible, limit the time you spend outdoors during the middle of the day, when the sun’s UV rays are strongest. If you are out in the sun, wear a wide-brimmed hat and use sunscreen and lip balm with a sun protection factor (SPF) of at least 30.
Eat a healthy diet
A poor diet has been linked to oral cavity and oropharyngeal cancers, although it’s not exactly clear what substances in healthy foods might be responsible for reducing the risk of these cancers.
In general, eating a healthy diet is much better than adding vitamin supplements to an otherwise unhealthy diet. The American Cancer Society recommends eating a healthy diet that emphasizes plant foods. This includes eating at least 2½ cups of vegetables and fruits every day. Choosing whole-grain breads, pastas, and cereals instead of refined grains, and eating fish, poultry, or beans instead of processed meat and red meat may also help lower your risk of cancer.
Wear properly fitted dentures
Avoiding sources of oral irritation (such as dentures that don’t fit properly) may also lower your risk for oral cancer.
Treat pre-cancerous growths
Areas of leukoplakia or erythroplakia in the mouth sometimes progress to cancer. Doctors often remove these areas, especially if a biopsy shows they contain areas of dysplasia (abnormal growth) when looked at under a microscope.
But removing areas of leukoplakia or erythroplakia does not always prevent someone from getting oral cavity cancer. Studies have found that even when these areas are completely removed, people with certain types of erythroplakia and leukoplakia still have a higher chance of developing a cancer in some other area of their mouth.
This may be because the whole lining of the mouth has probably been exposed to the same cancer-causing agents that led to these pre-cancers (like tobacco). This means that the entire area may already have early changes that can lead to cancer. This concept is called field cancerization.
It is important for patients who have had these areas removed to continue having checkups to look for cancer, and for new areas of leukoplakia or erythroplakia.
Chemoprevention
In recent years, doctors have been testing medicines to try to help lower the risk of these cancers. This approach, called chemoprevention, is particularly needed for people who have a higher risk of these cancers, such as those with leukoplakia or erythroplakia.
Several kinds of drugs have been studied for oropharyngeal cancer chemoprevention, but most of the research has focused on drugs related to vitamin A (retinoids). Studies so far have shown that retinoids can cause some areas of leukoplakia to shrink or even go away temporarily. But these studies have not found a long-term benefit in preventing cancer or helping patients live longer. At the same time, most of these drugs have bothersome and even serious side effects.
Signs and Symptoms of Oral Cavity and Oropharyngeal Cancer
Possible signs and symptoms of these cancers can include:
- A sore in the mouth that does not heal (most common symptom)
- Pain in the mouth that doesn’t go away (also very common)
- A lump or thickening in the cheek
- A white or red patch on the gums, tongue, tonsil, or lining of the mouth
- A sore throat or a feeling that something is caught in the throat that doesn’t go away
- Trouble chewing or swallowing
- Trouble moving the jaw or tongue
- Numbness of the tongue or other area of the mouth
- Swelling of the jaw that causes dentures to fit poorly or become uncomfortable
- Loosening of the teeth or pain around the teeth or jaw
- Voice changes
- A lump or mass in the neck
- Weight loss
- Constant bad breath
Many of these signs and symptoms can also be caused by things other than cancer, or even by other cancers. Still, it is very important to see a doctor or dentist if any of these conditions lasts more than 2 weeks so that the cause can be found and treated, if needed.
Oral Cavity and Oropharyngeal Cancers Diagnosis
A doctor or dentist may find some cancers or pre-cancers of the mouth and throat during an exam, but many of these cancers are found because of signs or symptoms a person is having. The patient should see a doctor who will examine him or her. Then, if cancer is suspected, tests will be needed.
Medical history and physical exam
Complete head and neck exam
The specialist will pay special attention to the head and neck area, being sure to look and feel for any abnormal areas. This exam will include the lymph nodes of the neck, which will be felt carefully for any signs of cancer.
Because the oropharynx is deep inside the neck and some parts are not easily seen, the doctor may use mirrors or special fiber-optic scopes to examine these areas while you are in the doctor’s office.
Indirect pharyngoscopy and laryngoscopy: For this exam, the doctor uses small mirrors placed at the back of your mouth to look at the throat, base of the tongue, and part of the larynx (voice box).
Direct (flexible) pharyngoscopy and laryngoscopy: For this exam, the doctor inserts a flexible fiber-optic scope (called an endoscope) through the mouth or nose to look at some areas that can’t easily be seen with mirrors, such as the region behind the nose (nasopharynx) and the larynx, or to see certain areas clearer.
Both types of exams can be done in the doctor’s office. For either type of exam, the doctor may spray the back of your throat with numbing medicine first to help make the exam easier.
Panendoscopy
During a panendoscopy, the doctor uses different types of endoscopes passed down the mouth or nose to perform laryngoscopy, esophagoscopy, and (at times) bronchoscopy. This lets the doctor thoroughly examine the oral cavity, oropharynx, larynx (voice box), esophagus (tube leading to the stomach), and the trachea (windpipe) and bronchi (breathing passageways in the lungs).
This exam is usually done in an operating room while you are under general anesthesia (asleep). The doctor uses a laryngoscope to look for tumors in the throat and larynx. Other parts of the mouth, nose, and throat are examined as well. If a tumor is found that is large or seems likely to spread, the doctor may also need to use an esophagoscope to look into the esophagus or a bronchoscope to look into the trachea and bronchi.
Your doctor will look at these areas through the scopes to find any tumors, see how large they are, and see how far they may have spread to surrounding areas. A small piece of tissue from any tumors or other abnormal areas may be removed (biopsied) to be looked at under a microscope to see if they contain cancer. Biopsies can be done with special instruments operated through the scopes.
Biopsy
In a biopsy, the doctor removes a sample of tissue to be looked at under a microscope. The actual diagnosis of oral and oropharyngeal cancers can only be made by a biopsy. A sample of tissue or cells is always needed to confirm that cancer is really present before treatment is started. Several types of biopsies may be used, depending on each case.
Exfoliative cytology
In this technique, the doctor scrapes a suspicious area and smears the collected tissue onto a glass slide. The sample is then stained with a dye so the cells can be seen under the microscope. If any of the cells look abnormal, the area can then be biopsied.
The advantage of this technique is that it is easy, and even only slightly abnormal-looking areas can be examined. This can make for an earlier diagnosis and a greater chance of cure if there is cancer. But this method does not detect all cancers. Sometimes it’s not possible to tell the difference between cancerous cells and abnormal but non-cancerous cells (dysplasia) with this approach, so a biopsy would still be needed.
Incisional biopsy
For this type of biopsy, the doctor cuts a small piece of tissue from an area that looks abnormal. This is the most common type of biopsy to sample areas in the mouth or throat.
The biopsy can be done either in the doctor’s office or in the operating room, depending on where the tumor is and how easy it is to get a good tissue sample. If it can be done in the doctor’s office, the area around the tumor will be numbed before the biopsy is taken. If the tumor is deep inside the mouth or throat, the biopsy might be done in the operating room with the patient under general anesthesia (in a deep sleep). The surgeon uses special instruments through an endoscope to remove small tissue samples.
Fine needle aspiration (FNA) biopsy
For this test, the doctor uses a very thin, hollow needle attached to a syringe to draw (aspirate) some cells from a tumor or lump. These cells are then looked at under a microscope to see if cancer is present.
FNA biopsy is not used to sample abnormal areas in the mouth or throat, but is sometimes used when a patient has a neck mass that can be felt or seen on a CT scan. FNA can be helpful in several different situations, such as:
Finding the cause of a new neck mass: An FNA biopsy is sometimes used as the first test for someone with a newly found neck lump.
The FNA may show that the neck mass is a benign (non-cancerous) lymph node that has grown in reaction to a nearby infection, such as a sinus or tooth infection. In this case, treatment of the infection is all that is needed. Or the FNA may find a benign, fluid-filled cyst that can be cured by surgery. But even when the FNA results are benign, if the patient has symptoms suggesting cancer, more tests (such as pharyngoscopy and panendoscopy) are needed.
If the FNA finds cancer, the doctor looking at the sample can usually tell what type of cancer it is. If the cells look like a squamous cell cancer, more exams will be done to search for the source of the cancer in the mouth and throat. If the FNA shows a different type of cancer, such as lymphoma or a cancer that has spread to a lymph node in the neck from another organ (like the thyroid, stomach, or lungs) more tests will be done to find it, and specific treatment for that type of cancer will be given.
Learning the extent of a known cancer: FNA is often done in patients who are known to have oral or oropharyngeal cancer to find out if the cancer has spread to lymph nodes in the neck. This information will help the doctor decide the best treatment for the cancer.
Seeing if cancer has come back after treatment: FNA may be used in patients whose cancer has been treated by surgery and/ or radiation therapy, to find out if a new neck mass in the treated area is scar tissue or a cancer that has come back.
Lab tests of biopsy samples
All biopsy samples are sent to a lab to be viewed under a microscope by a pathologist, a doctor who is specially trained to diagnose cancer with lab tests. The doctor can usually tell cancer cells from normal cells, as well as what type of cancer it is, by the way the cells look. In some cases, the doctor may need to coat the cells with special stains to help tell what type of cancer it is.
HPV testing: For cancers of the throat, doctors often have the biopsy samples tested to see if HPV infection is present. This information can help the doctor predict the probable course of the cancer, as people whose cancers are linked to HPV tend to do better than those whose cancers are not.
This testing is not routinely used to guide treatment at this time, but in the future it might help doctors decide which patients might be able to get less aggressive treatment.
Imaging tests
Imaging tests use x-rays, magnetic fields, or radioactive substances to create pictures of the inside of your body. Imaging tests are not used to diagnose oral cavity or oropharyngeal cancers, but they may be done for a number of reasons both before and after a cancer diagnosis, including:
- To help look for a tumor if one is suspected
- To learn how far cancer may have spread
- To help determine if treatment has been effective
- To look for possible signs of cancer recurrence after treatment
Imaging tests include:
- Chest x-ray
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
- Positron emission tomography (PET)
Barium swallow
A barium swallow can be used to examine the lining of the upper part of the digestive system, especially the esophagus (the tube connecting the throat to the stomach). In this test, you drink a chalky liquid called barium to coat the walls of your throat and esophagus. A series of x-rays of the throat and esophagus is taken as you swallow, which the barium outlines clearly.
Because patients with oral and oropharyngeal cancers are at risk for cancer of the esophagus, your doctor may order this test to check for this cancer. It is also useful to see if the cancer is causing problems with normal swallowing.
Other tests
Other tests may be done as part of a workup if a patient has been diagnosed with oral cavity or oropharyngeal cancer. These tests are not used to diagnose the cancer, but they may be done for other reasons, such as to see if a person is healthy enough for treatments such as surgery, radiation therapy, or chemotherapy.
Blood tests
No blood tests can diagnose cancer in the oral cavity or oropharynx. However, your doctor may order routine blood tests to help determine your overall health, especially before treatment such as surgery. Such tests can help diagnose malnutrition, low red blood cell counts (anemia), liver disease, and kidney disease. Blood tests may also suggest the cancer has spread to the liver or bone. When this occurs, more testing is needed.
Other tests before surgery
If surgery is planned, you might also have an electrocardiogram (EKG) to make sure your heart is functioning well. Some people having surgery also may need tests of their lung function. These are known as pulmonary function tests (PFTs).
Dental exam
When radiation therapy will be used as part of the treatment, it is likely you will be asked to see a dentist, who will help with preventive dental care and may remove teeth, if necessary, before radiation treatment is started.
If the cancer is located in your jaw or the roof of your mouth, a dentist with special training (a prosthodontist) may be asked to evaluate you. This dentist can make replacements for missing teeth or other structures of the oral cavity to help restore your appearance, comfort, and ability to chew, swallow, and speak after treatment. If part of the jaw or roof of the mouth (palate) will be removed with the tumor, the prosthodontist will work to ensure that the replacement artificial teeth and the remaining natural teeth fit together correctly. This can be done with dentures, other types of prostheses, or dental implants.
Oral Cavity and Oropharyngeal Cancer Stages
The earliest stage oral cavity or oropharyngeal cancers are called stage O (carcinoma in situ), and then range from stages I (1) through IV (4). As a rule, the lower the number, the less the cancer has spread. A higher number, such as stage IV, means cancer has spread more. And within a stage, an earlier letter means a lower stage. Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
The staging system most often used for oral cavity or oropharyngeal cancers is the American Joint Committee on Cancer (AJCC) TNM system, which is based on 3 key pieces of information:
- The extent of the tumor (T): How large is the main (primary) tumor and which, if any, tissues of the oral cavity or oropharynx it has spread to?
- The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes?
- The spread (metastasis) to distant sites (M): Has the cancer spread to distant organs such as the lungs?
Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced. Once a person’s T, N, and M categories have been determined, this information is combined in a process called stage grouping to assign an overall stage.
The staging system in the table below is based on the most recent AJCC system, effective January 2018. It uses the pathologic stage (also called the surgical stage). It is determined by examining tissue removed during an operation. Sometimes, if surgery is not possible right away or at all, the cancer will be given a clinical stage instead (which is not shown below). This is based on the results of a physical exam, endoscopy exam, biopsy, and imaging tests. The clinical stage will be used to help plan treatment. Sometimes, though, the cancer has spread further than the clinical stage estimates, and may not predict the patient’s outlook as accurately as a pathologic stage.
Oropharyngeal cancers that contain HPV DNA (called p16 positive) tend to have a better outlook than those without HPV (p16 negative). Because p16 positive cancers have a better prognosis than p16 negative oropharyngeal cancers, a separate staging system has been made. Both systems are described below.
Cancer staging can be complex, so ask your doctor to explain it to you in a way you understand.
Table 2. Lip, Oral Cavity and p16 negative Oropharynx Stages
| AJCC Stage | Stage grouping | Lip, Oral Cavity and p16 negative Oropharynx Stage Description* |
| 0 | Tis N0 M0 | The cancer is still within the epithelium (the top layer of cells lining the oral cavity and oropharynx) and has not yet grown into deeper layers. It has not spread to nearby lymph nodes (N0) or distant sites (M0). This stage is also known as carcinoma in situ (Tis). |
| I | T1 N0 M0 | The cancer is 2 cm (about ¾ inch) or smaller. It’s not growing into nearby tissues (T1). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| II | T2 N0 M0 | The cancer is larger than 2 cm but no larger than 4 cm (about 1½ inch). It’s not growing into nearby tissues (T2). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| III
| T3 N0 M0 | The cancer is larger than 4 cm (T3). For cancers of the oropharynx, T3 also includes tumors that are growing into the epiglottis (the base of the tongue). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| OR | ||
| T1, T2, T3 N1 M0 | The cancer is any size and may have grown into nearby structures if oropharynx cancer(T1-T3) AND has spread to 1 lymph node on the same side as the primary tumor. The cancer has not grown outside of the lymph node and the lymph node is no larger than 3 cm (about 1¼ inch) (N1). It has not spread to distant sites (M0). | |
| IVA | T4a N0 or N1 M0 | The cancer is any size and is growing into nearby structures such as:
This is known as moderately advanced local disease (T4a). AND either of the following:
It has not spread to distant sites (M0). |
| OR | ||
| T1, T2, T3 or T4a N2 M0 | The cancer is any size and may have grown into nearby structures (T0-T4a). It has not spread to distant organs (M0). It has spread to one of the following:
| |
| IVB | Any T N3 M0 | The cancer is any size and may have grown into nearby soft tissues or structures (Any T) AND any of the following:
It has not spread to distant organs (M0). |
| OR | ||
| T4b Any N M0 | The cancer is any size and is growing into nearby structures such as the base of the skull or other bones nearby, or it surrounds the carotid artery. This is known as very advanced local disease (T4b). It might or might not have spread to nearby lymph nodes (Any N). It has not spread to distant organs (M0). | |
| IVC | Any T Any N M1 | The cancer is any size and may have grown into nearby soft tissues or structures (Any T) AND the it might or might not have spread to nearby lymph nodes (Any N). It has spread to distant sites such as the lungs (M1). |
* The following additional categories are not described in the table above:
- TX: Main tumor cannot be assessed due to lack of information.
- T0: No evidence of a primary tumor.
- NX: Regional lymph nodes cannot be assessed due to lack of information.
Table 3. p16 positive Oropharynx Stages
| AJCC Stage | Stage grouping | p16 positive Oropharynx Stage Description* |
| I | T0, T1 or T2 N0 or N1 M0 | The cancer is no larger than 4 cm (about 1 1/2 inches) (T0 to T2) AND any of the following:
It has not spread to distant sites (M0). |
| II | T0, T1 or T2 N2 M0 | The cancer is no larger than 4 cm (about 1 1/2 inches) (T0 to T2) AND it has spread to one or more lymph nodes on the opposite side of the primary cancer or both sides of the neck, none larger than 6cm (N2). It has not spread to distant sites (M0). |
| OR | ||
| T3 or T4 N0 or N1 M0 | The cancer is larger than 4 cm (about 1 1/2 inches) (T3) OR is growing into the epiglottis (the base of the tongue) (T3) OR is growing into the larynx (voice box), the tongue muscle, or bones such as the medial pterygoid plate, the hard palate, or the jaw (T4) any of the following:
It has not spread to distant sites (M0). | |
| III
| T3 or T4 N2 M0 | The cancer is larger than 4 cm (about 1 1/2 inches) (T3) OR is growing into the epiglottis (the base of the tongue) (T3) OR is growing into the larynx (voice box), the tongue muscle, or bones such as the medial pterygoid plate, the hard palate, or the jaw (T4) AND it has spread to one or more lymph nodes on the opposite side of the primary cancer or both sides of the neck, none larger than 6cm (N2). It has not spread to distant sites (M0). |
| IV | Any T Any N M1 | The cancer is any size and may have grown into nearby structures (Any T) AND the it might or might not have spread to nearby lymph nodes (Any N). It has spread to distant sites such as the lungs or bones (M1). |
* The following additional categories are not described in the table above:
- TX: Main tumor cannot be assessed due to lack of information.
- T0: No evidence of a primary tumor.
- NX: Regional lymph nodes cannot be assessed due to lack of information.
Survival Rates for Oral Cavity and Oropharyngeal Cancer by Stage
The following survival statistics come from the National Cancer Institute’s SEER program. They are based on large numbers of patients diagnosed between 2000 and 2014. SEER doesn’t provide recent statistics by AJCC stage. Instead, cancers are divided into the summary stages:
- Local: the cancer is only in the area where it started. This includes stages I and II, as well as some stage III cancers that haven’t spread to any lymph nodes.
- Regional: the cancer has spread to nearby tissues and/or lymph nodes. This includes some stage III cancers, as well as stage IV cancers that haven’t spread to distant sites
- Distant: the cancer has spread to distant sites
Also, these statistics are based on the stage of the cancer when it was first diagnosed. They do not apply to cancers that have come back.
For cancers of the oropharynx and tonsil, the relative 5-year survival rate was 66%, but survival by stage is not available
For cancers of the gums and other parts of the mouth, the relative survival was 60%, but survival by stage is not available.
Lip
| Stage | 5-Year Relative Survival Rate |
| Local | 93% |
| Regional | 48% |
| Distant | 52% |
Tongue
| Stage | 5-Year Relative Survival Rate |
| Local | 78% |
| Regional | 63% |
| Distant | 36% |
Floor of the mouth
| Stage | 5-Year Relative Survival Rate |
| Local | 75% |
| Regional | 38% |
| Distant | 20% |
Oral Cavity and Oropharyngeal Cancer Treatment
The main treatment options for people with oral and oropharyngeal cancers are:
- Surgery
- Radiation therapy
- Chemotherapy
- Targeted therapy
- Palliative treatment
These may be used either alone or in combination, depending on the stage and location of the tumor. In general, surgery is the first treatment for cancers of the oral cavity, and may be followed by radiation or combined chemotherapy and radiation. Oropharyngeal cancers are usually treated with a combination of chemotherapy and radiation.
Laryngeal and Hypopharyngeal Cancers
Cancers that start in the larynx are called laryngeal cancers. Cancers that start in the hypopharynx are called hypopharyngeal cancers. Both types of cancers are covered here because these 2 structures are so close to each other.
Squamous cell carcinomas
Almost all cancers in the larynx or hypopharynx develop from thin, flat cells called squamous cells, which are in the epithelium, the innermost layer lining these 2 structures. Cancer that starts in this layer of cells is called squamous cell carcinoma or squamous cell cancer.
Most squamous cell cancers of the larynx and hypopharynx start as a pre-cancer called dysplasia. When seen under a microscope, these cells look abnormal but not quite like cancer cells. Most of the time, dysplasia doesn’t turn into cancer. It often goes away without any treatment, especially if the underlying cause (like smoking) is stopped. Most pre-cancers of the larynx and hypopharynx do not cause problems unless they’re on the vocal cord(s).
Sometimes dysplasia will progress to carcinoma in situ (CIS). Carcinoma in situ (CIS) is the earliest form of cancer. In CIS, the cancer cells are only seen in the epithelium lining the larynx or hypopharynx. They haven’t grown into deeper layers or spread to other parts of the body. Most of these early cancers can be cured, but if carcinoma in situ (CIS) isn’t treated, it can develop into an invasive squamous cell cancer that will destroy nearby tissues and spread to other parts of the body.
Other cancers
Other rare types of cancer can also start in the larynx or hypopharynx.
Minor salivary gland cancers: Some parts of the larynx and hypopharynx have tiny glands called minor salivary glands beneath their lining layer. These glands make mucus and saliva to lubricate and moisten the area. Cancer rarely develops in the cells of these glands.
Sarcomas: The shape of the larynx and hypopharynx depends on a framework of connective tissues and cartilage. Cancers like chondrosarcomas or synovial sarcomas can develop from connective tissues of the larynx or hypopharynx, but this is extremely rare.
Melanomas: These cancers usually start in the skin, but in rare cases they can start on inner (mucosal) surfaces of the body, such as in the larynx or hypopharynx.
The American Cancer Society’s most recent estimates for laryngeal cancer in the United States for 2018 are:
- About 13,150 new cases of laryngeal cancer (10,490 in men and 2,660 in women)
- About 3,710 people (2,970 men and 740 women) will die from laryngeal cancer
About 60% of laryngeal cancers start in the glottis (the area containing the vocal cords themselves), while about 35% develop in the supraglottic area (above the vocal cords). The rest develop in either the subglottis (below the vocal cords) or overlap more than one area so that it is hard to tell where they started.
The rate of new cases of laryngeal cancer is falling by about 2% to 3% a year, most likely because fewer people are smoking.
About 3,000 cancers will start in the hypopharynx.
What Causes Laryngeal and Hypopharyngeal Cancers?
Doctors don’t know what causes each case of laryngeal or hypopharyngeal cancer.
Scientists believe that some risk factors, such as tobacco or heavy alcohol use, cause these cancers by damaging the DNA of the cells that line the inside of the larynx and hypopharynx.
Some people inherit DNA mutations (changes) from their parents that greatly increase their risk for developing certain cancers. But inherited gene mutations are not believed to cause very many cancers of the larynx or hypopharynx.
Gene changes related to these cancers usually happen during life, rather than being inherited. These acquired mutations often result from exposure to cancer-causing chemicals, like those found in tobacco smoke. An acquired change in the p16 tumor suppressor gene seems to be important in laryngeal and hypopharyngeal cancers, although not all these cancers have this change. Several different gene changes are probably needed for cancer to develop, and not all of these changes are understood at this time.
Inherited mutations of oncogenes or tumor suppressor genes rarely cause these cancers, but some people seem to inherit a reduced ability to detoxify (break down) certain types of cancer-causing chemicals. These people are more sensitive to the cancer-causing effects of tobacco smoke, alcohol, and certain industrial chemicals. Researchers are developing tests that may help identify such people, but these tests are not yet reliable enough for routine use.
Some forms of human papillomavirus (HPV) are important causes of some throat cancers (including cancers of the hypopharynx). The outlook for people with these cancers appears to be better than for people whose cancers are the result of tobacco or alcohol use.
Risk Factors for Laryngeal and Hypopharyngeal Cancers
Laryngeal and hypopharyngeal cancers are often grouped with other cancers of the mouth and throat (commonly called head and neck cancers). These cancers often have many of the same risk factors, which are listed below.
Tobacco and alcohol use
Tobacco use is the most important risk factor for head and neck cancers (including cancers of the larynx and hypopharynx). The risk for these cancers is much higher in smokers than in nonsmokers. Most people with these cancers have a history of smoking or other tobacco exposure. The more you smoke, the greater your risk. Smoke from cigarettes, pipes, and cigars all increase your risk of getting these cancers.
Some studies have also found that long-term exposure to secondhand smoke might increase the risk of these cancers, but more research is needed to confirm this.
Moderate or heavy alcohol use (more than 1 drink a day) also increases the risk of these cancers, although not as much as smoking.
People who use both tobacco and alcohol have the highest risk of all. Combining these 2 habits doesn’t just add both risks together, it actually multiplies them. People who smoke and drink are many times more likely to get head and neck cancer than are people with neither habit.
Poor nutrition
Poor nutrition may increase the risk of getting head and neck cancer. The exact reason for this isn’t clear. Heavy drinkers often have vitamin deficiencies, which may help explain the role of alcohol in increasing risk of these cancers.
Researchers have been comparing eating habits and risk. It’s been suggested that eating fewer fried foods and processed foods and eating more plant-based foods might help reduce laryngeal cancer risk.
Human papillomavirus infection
Human papillomavirus (HPV) is a group of over 150 related viruses. They are called papilloma viruses because some of them cause a type of growth called a papilloma, more commonly known as a wart.
Infection with certain types of HPV can also cause some forms of cancer, including cancers of the penis, cervix, vulva, vagina, anus, and throat. Other types of HPV cause warts in different parts of the body.
HPV infection of the throat seems to be a factor in some throat cancers, such as some cancers of the tonsils and some cancers of the hypopharynx. HPV infection is very rarely a factor in laryngeal cancer.
Genetic syndromes
People with syndromes caused by inherited gene defects (mutations) have a very high risk of throat cancer, including cancer of the hypopharynx.
Fanconi anemia: People with this syndrome often have blood problems at an early age, which may lead to leukemia or aplastic anemia. They also have a very high risk of cancer of the mouth and throat.
Dyskeratosis congenita: This genetic syndrome can cause aplastic anemia, skin rashes, and abnormal fingernails and toenails. People with this syndrome have a very high risk of developing cancer of the mouth and throat when they are young.
Workplace exposures
Long and intense exposures to wood dust, paint fumes, and certain chemicals used in the metalworking, petroleum, plastics, and textile industries can increase the risk of laryngeal and hypopharyngeal cancers.
Asbestos is a mineral fiber that was often used as an insulating material in many products in the past. Exposure to asbestos is an important risk factor for lung cancer and mesothelioma (cancer that starts in the lining of the chest or abdomen). Some studies have suggested a link between asbestos exposure and laryngeal cancer, but not all studies agree.
Gender
Cancers of the larynx and hypopharynx are about 4 times more common in men than women. This is likely because the main risk factors − smoking and heavy alcohol use − are more common in men. But in recent years, as these habits have become more common among women, their risks for these cancers have increased as well.
Age
Cancers of the larynx and hypopharynx usually develop over many years, so they are not common in young people. Over half of patients with these cancers are 65 or older when the cancers are first found.
Race
Cancers of the larynx and hypopharynx are more common among African Americans and whites than among Asians and Latinos.
Gastroesophageal reflux disease (GERD)
When acid from the stomach backs up into the esophagus it’s called gastroesophageal reflux disease (GERD). GERD can cause heartburn and increase the chance of cancer of the esophagus. Studies are being done to see if it increases the risk of laryngeal and hypopharyngeal cancers, too.
Signs and Symptoms of Laryngeal and Hypopharyngeal Cancers
In most cases, laryngeal and hypopharyngeal cancers are found because of the symptoms they cause.
Hoarseness or voice changes
Laryngeal cancers that form on the vocal cords (glottis) often cause hoarseness or a change in the voice. This can lead to them being found at a very early stage. People who have voice changes (like hoarseness) that do not improve within 2 weeks should see their health care provider right away.
For cancers that don’t start on the vocal cords, hoarseness occurs only after these cancers reach a later stage or have spread to the vocal cords. These cancers are sometimes not found until they have spread to the lymph nodes and the person notices a growing mass in the neck.
Other symptoms
Cancers that start in the area of the larynx above the vocal cords (supraglottis), the area below the vocal cords (subglottis), or the hypopharynx do not usually cause voice changes, and are therefore more often found at later stages.
Symptoms of these cancers may include:
- A sore throat that does not go away
- Constant coughing
- Pain when swallowing
- Trouble swallowing
- Ear pain
- Trouble breathing
- Weight loss
- A lump or mass in the neck (due to spread of the cancer to nearby lymph nodes)
Many of these symptoms are more likely to be caused by conditions other than laryngeal or hypopharyngeal cancer. Still, if you have any of these symptoms, it is very important to have them checked by a doctor so that the cause can be found and treated, if needed.
Laryngeal Cancer Stages
The staging system most often used for laryngeal cancer is the American Joint Committee on Cancer (AJCC) TNM system, which is based on 3 key pieces of information:
- The extent of the main tumor (T): Where is the tumor? How far has it grown into the larynx and nearby structures? Has it affected vocal cord movement?
- The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes in the neck? If so, how many are affected, and how large are they?
- The spread (metastasis) to distant sites (M): Has the cancer spread to distant parts of the body? (The most common sites of spread are the lungs, liver, or bones.)
Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced.
Once the T, N, and M categories of the cancer have been determined, this information is combined in a process called stage grouping to assign an overall stage.
The system described below is the most recent AJCC system, effective January 2018.
Laryngeal cancer is typically given a clinical stage based on the results of any exams, biopsies, and imaging tests that might have been done. If surgery has been done, the pathologic stage (also called the surgical stage) can be determined.
The stages of laryngeal cancer are slightly different, based on which part of the larynx the cancer starts in:
- The supraglottis (the area above the vocal cords)
- The glottis (the area that includes the vocal cords)
- The subglottis (the area below the vocal cords)
Laryngeal cancer staging can be complex, so ask your doctor to explain it to you in a way you understand.
Table 4. Stages of supraglottic laryngeal cancer
| AJCC stage | Stage grouping | Stage description* |
| 0 | Tis N0 M0 | The tumor is only in the top layer of cells lining the inside of the larynx and has not grown any deeper (Tis). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| I | T1 N0 M0 | The tumor has grown deeper, but it is only in one part of the supraglottis, and the vocal cords move normally (T1). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| II | T2 N0 M0 | The tumor has grown deeper, and it has grown into more than one part of the supraglottis (or glottis), and the vocal cords move normally (T2). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| III | T3 N0 M0 | The tumor is still only in the larynx, but it has caused a vocal cord to stop moving, OR the tumor is growing into nearby areas such as the postcricoid area, paraglottic space, pre-epiglottic (in front of the epiglottis) tissues, or the inner part of the thyroid cartilage (firm tissue that separates the thyroid gland from the front of the larynx) (T3). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| OR | ||
| T1 to T3 N1 M0 | The tumor might or might not have grown into structures just outside the larynx, and it might or might not have affected a vocal cord (T1 to T3). The cancer has spread to a single lymph node on the same side of the neck as the tumor, which is no larger than 3 centimeters (cm) across (N1). The cancer has not spread to distant parts of the body (M0). | |
| IVA | T4a N0 or N1 M0 | The tumor has grown through the thyroid cartilage and/or is growing into tissues beyond the larynx (such as the thyroid gland, trachea, esophagus, tongue muscles, or neck muscles). This is also known as moderately advanced local disease (T4a). The cancer has not spread to nearby lymph nodes (N0), or it has spread to a single lymph node on the same side of the neck as the tumor, which is no larger than 3 centimeters (cm) across (N1). The cancer has not spread to distant parts of the body (M0). |
| OR | ||
| T1-T4a N2 M0 | The tumor might or might not have grown into structures outside the larynx (as far as moderately advanced disease), and it might or might not have affected a vocal cord (T1 to T4a). The cancer is N2:
The cancer has not spread to distant parts of the body (M0). | |
| IVB | T4b Any N M0 | The tumor is growing into the area in front of the spine in the neck (the prevertebral space), surrounds a carotid artery, or is growing down into the space between the lungs. This is also known as very advanced local disease (T4b). The cancer might or might not have spread to nearby lymph nodes (any N). It has not spread to distant parts of the body (M0). |
| OR | ||
| Any T N3 M0 | The tumor might or might not have grown into structures outside the larynx, and it might or might not have affected a vocal cord (any T). The cancer has spread to at least one lymph node that is larger than 6 cm across, OR it has spread to a lymph node and then grown outside of the lymph node (N3). It has not spread to distant parts of the body (M0). | |
| IVC | Any T Any N M1 | The tumor might or might not have grown into structures outside the larynx, and it might or might not have affected a vocal cord (any T). The cancer might or might not have spread to nearby lymph nodes (any N). The cancer has spread to distant parts of the body (M1). |
* The following additional categories are not listed on the table above:
- TX: Main tumor cannot be assessed due to lack of information.
- NX: Regional lymph nodes cannot be assessed due to lack of information.
Table 5. Stages of glottic laryngeal cancer
| AJCC stage | Stage grouping | Stage description* |
| 0 | Tis N0 M0 | The tumor is only in the top layer of cells lining the inside of the larynx and has not grown any deeper (Tis). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| I | T1 N0 M0 | The tumor has grown deeper, but it is only in the vocal cords, and they move normally (T1). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| II | T2 N0 M0 | The tumor has grown into the supraglottis or subglottis, and/or the vocal cords do not move normally (T2). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| III | T3 N0 M0 | The tumor is still only in the larynx, but it has caused a vocal cord to stop moving, OR the tumor is growing into the paraglottic space, OR the tumor is growing into the inner part of the thyroid cartilage (firm tissue that separates the thyroid gland from the front of the larynx) (T3). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| OR | ||
| T1 to T3 N1 M0 | The tumor might or might not have grown into structures just outside the larynx, and it might or might not have affected a vocal cord (T1 to T3). The cancer has spread to a single lymph node on the same side of the neck as the tumor, which is no larger than 3 centimeters (cm) across (N1). The cancer has not spread to distant parts of the body (M0). | |
| IVA | T4a N0 or N1 M0 | The tumor has grown through the thyroid cartilage and/or is growing into tissues beyond the larynx (such as the thyroid gland, trachea, cricoid cartilage, esophagus, tongue muscles, or neck muscles). This is also known as moderately advanced local disease (T4a). The cancer has not spread to nearby lymph nodes (N0), or it has spread to a single lymph node on the same side of the neck as the tumor, which is no larger than 3 centimeters (cm) across (N1). The cancer has not spread to distant parts of the body (M0). |
| OR | ||
| T1-T4a N2 M0 | The tumor might or might not have grown into structures outside the larynx (as far as moderately advanced disease), and it might or might not have affected a vocal cord (T1 to T4a). The cancer is N2:
The cancer has not spread to distant parts of the body (M0). | |
| IVB | T4b Any N M0 | The tumor is growing into the area in front of the spine in the neck (the prevertebral space), surrounds a carotid artery, or is growing down into the space between the lungs. This is also known as very advanced local disease (T4b). The cancer might or might not have spread to nearby lymph nodes (any N). It has not spread to distant parts of the body (M0). |
| OR | ||
| Any T N3 M0 | The tumor might or might not have grown into structures outside the larynx, and it might or might not have affected a vocal cord (any T). The cancer has spread to at least one lymph node that is larger than 6 cm across, OR it has spread to a lymph node and then grown outside of the lymph node (N3). It has not spread to distant parts of the body (M0). | |
| IVC | Any T Any N M1 | The tumor might or might not have grown into structures outside the larynx, and it might or might not have affected a vocal cord (any T). The cancer might or might not have spread to nearby lymph nodes (any N). The cancer has spread to distant parts of the body (M1). |
* The following additional categories are not listed on the table above:
- TX: Main tumor cannot be assessed due to lack of information.
- NX: Regional lymph nodes cannot be assessed due to lack of information.
Table 6. Stages of subglottic laryngeal cancer
| AJCC stage | Stage grouping | Stage description* |
| 0 | Tis N0 M0 | The tumor is only in the top layer of cells lining the inside of the larynx and has not grown any deeper (Tis). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| I | T1 N0 M0 | The tumor has grown deeper, but it is only in the subglottis (T1). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| II | T2 N0 M0 | The tumor has grown into the vocal cords, which might or might not move normally (T2). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| III | T3 N0 M0 | The tumor is still only in the larynx, but it has caused a vocal cord to stop moving, OR the tumor is growing into the paraglottic space, OR the tumor is growing into the inner part of the thyroid cartilage (firm tissue that separates the thyroid gland from the front of the larynx) (T3). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| OR | ||
| T1 to T3 N1 M0 | The tumor might or might not have grown into structures just outside the larynx, and it might or might not have affected a vocal cord (T1 to T3). The cancer has spread to a single lymph node on the same side of the neck as the tumor, which is no larger than 3 centimeters (cm) across (N1). The cancer has not spread to distant parts of the body (M0). | |
| IVA | T4a N0 or N1 M0 | The tumor is growing through the cricoid or thyroid cartilage and/or is growing into structures beyond the larynx (such as the thyroid gland, trachea, esophagus, tongue muscles, or neck muscles). This is also known as moderately advanced local disease (T4a). The cancer has not spread to nearby lymph nodes (N0), or it has spread to a single lymph node on the same side of the neck as the tumor, which is no larger than 3 centimeters (cm) across (N1). The cancer has not spread to distant parts of the body (M0). |
| OR | ||
| T1-T4a N2 M0 | The tumor might or might not have grown into structures outside the larynx (as far as moderately advanced disease), and it might or might not have affected a vocal cord (T1 to T4a). The cancer is N2:
The cancer has not spread to distant parts of the body (M0). | |
| IVB | T4b Any N M0 | The tumor is growing into the area in front of the spine in the neck (the prevertebral space), surrounds a carotid artery, or is growing down into the space between the lungs. This is also known as very advanced local disease (T4b). The cancer might or might not have spread to nearby lymph nodes (any N). It has not spread to distant parts of the body (M0). |
| OR | ||
| Any T N3 M0 | The tumor might or might not have grown into structures outside the larynx, and it might or might not have affected a vocal cord (any T). The cancer has spread to at least one lymph node that is larger than 6 cm across, OR it has spread to a lymph node and then grown outside of the lymph node (N3). It has not spread to distant parts of the body (M0). | |
| IVC | Any T Any N M1 | The tumor might or might not have grown into structures outside the larynx, and it might or might not have affected a vocal cord (any T). The cancer might or might not have spread to nearby lymph nodes (any N). The cancer has spread to distant parts of the body (M1). |
* The following additional categories are not listed on the table above:
- TX: Main tumor cannot be assessed due to lack of information.
- NX: Regional lymph nodes cannot be assessed due to lack of information.
Hypopharyngeal Cancer Stages
Table 7. Stages of hypopharyngeal cancer
| AJCC Stage | Stage grouping | Stage description* |
| 0 | Tis N0 M0 | The tumor is only in the top layer of cells lining the inside of the hypopharynx and has not grown any deeper (Tis). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| I | T1 N0 M0 | The tumor has grown deeper, but it is only in one part of the hypopharynx, and it is no more than 2 centimeters (cm) across (T1). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| II | T2 N0 M0 | The tumor has grown into more than one part of the hypopharynx, OR it has grown into a nearby area, OR it is larger than 2 but no larger than 4 cm across and has not affected the vocal cords (T2). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
|
III | T3 N0 M0 | The tumor is larger than 4 cm across, OR the tumor is affecting the movement of the vocal cords, OR the tumor has grown into the esophagus (T3). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| OR | ||
| T1 to T3 N1 M0 | The tumor can be any size and might or might not have grown into structures outside the hypopharynx, and it might or might not have affected a vocal cord (T1 to T3). The cancer has spread to a single lymph node on the same side of the neck as the tumor, which is no larger than 3 centimeters (cm) across (N1). The cancer has not spread to distant parts of the body (M0). | |
|
IVA | T4a N0 or N1 M0 | The tumor has grown into the thyroid or cricoid cartilage, the hyoid bone, the thyroid gland, or nearby areas of muscle or fat. This is also known as moderately advanced local disease (T4a). The cancer has not spread to nearby lymph nodes (N0), or it has spread to a single lymph node on the same side of the neck as the tumor, which is no larger than 3 centimeters (cm) across (N1). The cancer has not spread to distant parts of the body (M0). |
| OR | ||
| T1-T4a N2 M0 | The tumor can be any size and might or might not have grown into structures outside the hypopharynx (as far as moderately advanced disease), and it might or might not have affected a vocal cord (T1 to T4a). The cancer is N2:
The cancer has not spread to distant parts of the body (M0). | |
|
IVB | T4b Any N M0 | The tumor is growing into the area in front of the spine in the neck, surrounds a carotid artery, or is growing down into the space between the lungs. This is also known as very advanced local disease (T4b). The cancer might or might not have spread to nearby lymph nodes (any N). It has not spread to distant parts of the body (M0). |
| OR | ||
| Any T N3 M0 | The tumor can be any size and might or might not have grown into structures outside the hypopharynx, and it might or might not have affected a vocal cord (any T). The cancer has spread to at least one lymph node that is larger than 6 cm across, OR it has spread to a lymph node and then grown outside of the lymph node (N3). It has not spread to distant parts of the body (M0). | |
| IVC | Any T Any N M1 | The tumor can be any size and might or might not have grown into structures outside the hypopharynx, and it might or might not have affected a vocal cord (any T). The cancer might or might not have spread to nearby lymph nodes (any N). The cancer has spread to distant parts of the body (M1). |
*The following additional categories are not listed on the table above:
- TX: Main tumor cannot be assessed due to lack of information.
- NX: Regional lymph nodes cannot be assessed due to lack of information.
Survival Rates for Laryngeal and Hypopharyngeal Cancers by Stage
These numbers are from the National Cancer Data Base, based on patients diagnosed in 1998-1999, and published in 2010 in the AJCC Cancer Staging Manual, Seventh Edition. For laryngeal cancers, survival rates differ based on which part of the larynx the cancer started in (supraglottis, glottis, or subglottis).
Remember, these survival rates are only estimates – they can’t predict what will happen to any individual . We understand that these statistics can be confusing. If you have more questions, talk with your doctor to better understand your situation.
Supraglottis (part of the larynx above the vocal cords)
| Stage | 5-year relative survival rate |
| I | 59% |
| II | 59% |
| III | 53% |
| IV | 34% |
Glottis (part of the larynx including the vocal cords)
| Stage | 5-year relative survival rate |
| I | 90% |
| II | 74% |
| III | 56% |
| IV | 44% |
Subglottis (part of the larynx below the vocal cords)
(These numbers are less accurate because of the small number of patients.)
| Stage | 5-year relative survival rate |
| I | 65% |
| II | 56% |
| III | 47% |
| IV | 32% |
Hypopharynx
Remember, these survival rates are only estimates – they can’t predict what will happen to any individual . We understand that these statistics can be confusing. If you have more questions, talk with your doctor to better understand your situation.
Treating Laryngeal and Hypopharyngeal Cancer
Treatment for laryngeal or hypopharyngeal cancer may include:
- Surgery
- Radiation therapy
- Chemotherapy
- Targeted therapy
Throat cancer causes
Throat cancer occurs when cells in your throat develop genetic mutations. These mutations cause cells to grow uncontrollably and continue living after healthy cells would normally die. The accumulating cells can form a tumor in your throat.
It’s not clear what causes the mutation that causes throat cancer. But doctors have identified factors that may increase your risk.
You are at an increased risk of throat cancer if you smoke (cigarettes, cigars or pipes) and drink alcohol, especially if you have 3 or more drinks a day.
Other risk factors include:
- Viruses, such as human papillomavirus (HPV) or Epstein-Barr virus (EBV)
- A diet low in fruits and vegetables and vitamin A.
- Gastroesophageal reflux disease (GERD)
Throat cancer prevention
There’s no proven way to prevent throat cancer from occurring. But in order to reduce your risk of throat cancer, you can:
- Stop smoking or don’t start smoking. If you smoke, quit. If you don’t smoke, don’t start. Stopping smoking can be very difficult, so get some help. Your doctor can discuss the benefits and risks of the many stop-smoking strategies, such as medications, nicotine replacement products and counseling.
- Drink alcohol only in moderation, if at all. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women of all ages and men older than age 65, and up to two drinks a day for men age 65 and younger.
- Choose a healthy diet full of fruits and vegetables. The vitamins and antioxidants in fruits and vegetables may reduce your risk of throat cancer. Eat a variety of colorful fruits and vegetables.
- Protect yourself from HPV. Some throat cancers are thought to be caused by the sexually transmitted infection human papillomavirus (HPV). You can reduce your risk of HPV by limiting your number of sexual partners and using a condom every time you have sex. Also consider the HPV vaccine, which is available to boys, girls, and young women and men.
Throat cancer signs and symptoms
Signs and symptoms of throat cancer may include:
- Pain in the throat or around the breastbone
- A sore throat
- Cough that won’t go away
- Changes in your voice, such as hoarseness or not speaking clearly
- Trouble swallowing
- blood in their phlegm
- Difficulty swallowing
- Ear pain
- A lump or sore that doesn’t heal
- Weight loss
Throat cancer stages
Once throat cancer is diagnosed, the next step is to determine the extent (stage) the cancer. Knowing the stage helps determine your treatment options.
The stage of throat cancer is characterized with the Roman numerals I through IV. Each subtype of throat cancer has its own criteria for each stage. In general, stage I throat cancer indicates a smaller tumor confined to one area of the throat. Later stages indicate more advanced cancer, with stage IV being the most advanced.
Throat cancer diagnosis
Your doctor will talk to you and examine you. You might be referred to a specialist such as an ear nose and throat specialist or a head and neck surgeon.
You might have an endoscopic examination of your throat and larynx. This could be a nasendoscopy, laryngoscopy or brochoscopy.
Your doctor might send you for tests such as:
- Small tissue sample (biopsy) from your throat. If abnormalities are found during an endoscopy or laryngoscopy, your doctor can pass surgical instruments through the scope to collect a tissue sample (biopsy). The sample is sent to a laboratory for testing. Your doctor may also order a sample of a swollen lymph node using a technique called fine-needle aspiration.
- Computerized tomography (CT) scan
- Magnetic resonance imaging (MRI) scan
- Positron emission tomography (PET) scan
- Ultrasound
- X-ray.
Throat cancer treatment
Your treatment options are based on many factors, such as the location and stage of your throat cancer, the type of cells involved, your overall health, and your personal preferences. Discuss the benefits and risks of each of your options with your doctor. Together you can determine what treatments will be most appropriate for you.
The main treatment for throat cancer is surgery or radiotherapy. Chemotherapy might also be offered, usually with radiotherapy.
Radiation therapy
Radiation therapy uses high-energy beams from sources such as X-rays and protons to deliver radiation to the cancer cells, causing them to die.
Radiation therapy can come from a large machine outside your body (external beam radiation), or radiation therapy can come from small radioactive seeds and wires that can be placed inside your body, near your cancer (brachytherapy).
For early-stage throat cancers, radiation therapy may be the only treatment necessary. For more-advanced throat cancers, radiation therapy may be combined with chemotherapy or surgery. In very advanced throat cancers, radiation therapy may be used to reduce signs and symptoms and make you more comfortable.
Surgery
The types of surgical procedures you may consider to treat your throat cancer depend on the location and stage of your cancer. Options may include:
- Surgery for early-stage throat cancer. Throat cancer that is confined to the surface of the throat or the vocal cords may be treated surgically using endoscopy. Your doctor may insert a hollow endoscope into your throat or voice box and then pass special surgical tools or a laser through the scope. Using these tools, your doctor can scrape off, cut out or, in the case of the laser, vaporize very superficial cancers.
- Surgery to remove all or part of the voice box (laryngectomy). For smaller tumors, your doctor may remove the part of your voice box that is affected by cancer, leaving as much of the voice box as possible. Your doctor may be able to preserve your ability to speak and breathe normally. For larger, more-extensive tumors, it may be necessary to remove your entire voice box. Your windpipe is then attached to a hole (stoma) in your throat to allow you to breathe (tracheotomy). If your entire larynx is removed, you have several options for restoring your speech. You can work with a speech pathologist to learn to speak without your voice box.
- Surgery to remove part of the throat (pharyngectomy). Smaller throat cancers may require removing only small parts of your throat during surgery. Parts that are removed may be reconstructed in order to allow you to swallow food normally.
- Surgery to remove cancerous lymph nodes (neck dissection). If throat cancer has spread deep within your neck, your doctor may recommend surgery to remove some or all of the lymph nodes to see if they contain cancer cells.
Surgery carries a risk of bleeding and infection. Other possible complications, such as difficulty speaking or swallowing, will depend on the specific procedure you undergo.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. Chemotherapy is often used along with radiation therapy in treating throat cancers. Certain chemotherapy drugs make cancer cells more sensitive to radiation therapy. But combining chemotherapy and radiation therapy increases the side effects of both treatments. Discuss with your doctor the side effects you’re likely to experience and whether combined treatments will offer benefits that outweigh those effects.
Targeted drug therapy
Targeted drugs treat throat cancer by taking advantage of specific defects in cancer cells that fuel the cells’ growth.
Cetuximab (Erbitux) is one targeted therapy approved for treating throat cancer in certain situations. Cetuximab stops the action of a protein that’s found in many types of healthy cells, but is more prevalent in certain types of throat cancer cells.
Other targeted drugs are being studied in clinical trials. Targeted drugs can be used in combination with chemotherapy or radiation therapy.
Rehabilitation after treatment
Treatment for throat cancer often causes complications that may require working with specialists to regain the ability to swallow, eat solid foods and talk. During and after throat cancer treatment, your doctor may have you seek help for:
- Eating difficulties
- Swallowing difficulties
- Stiffness and pain in your neck
- Speech problems
Your doctor can discuss the potential side effects and complications of your treatments with you.
Living with throat cancer
You may feel your cancer experience doesn’t end on the last day of treatment. Take time to adjust to the physical and emotional changes and re-establish a new daily routine at your own pace. Your doctor will continue to monitor your health and confirm the cancer hasn’t come back.
If you have surgery to treat your throat cancer, you might have problems after surgery, such as:
- a sore throat
- breathing difficulties, which might mean you need a breathing hole (tracheostomy) in your lower neck
- problems eating, which might mean you need a feeding tube inserted
- trouble swallowing
- scars and wounds that need time to heal.
If you have more extensive surgery, you might have to adjust to greater changes. Talk to your doctor about what to expect or for referral to support services and resources.
Lifestyle and home remedies
Quit smoking
Throat cancers are closely linked to smoking. Not everyone with throat cancer smokes. But if you do smoke, now is the time to stop because:
- Smoking makes treatment less effective.
- Smoking makes it harder for your body to heal after surgery.
- Smoking increases your risk of getting another cancer in the future.
Stopping smoking can be very difficult. And it’s that much harder when you’re trying to cope with a stressful situation, such as a cancer diagnosis. Your doctor can discuss all of your options, including medications, nicotine replacement products and counseling.
Quit drinking alcohol
Alcohol, particularly when combined with smoking or chewing tobacco, greatly increases the risk of throat cancer. If you drink alcohol, stop now. This may help reduce your risk of a second cancer. Stopping drinking may also help you better tolerate your throat cancer treatments.
Coping and support
Being diagnosed with cancer can be devastating. Throat cancer affects a part of your body that is vital to everyday activities, such as breathing, eating and talking. In addition to worrying about how these basic activities may be affected, you may also be concerned about your treatments and chances for survival.
Though you may feel like your life — your survival — is out of your hands, you can take steps to feel more in control and to cope with your throat cancer diagnosis. To cope, try to:
- Learn enough about throat cancer to make treatment decisions. Write down a list of questions to ask your doctor at your next appointment. Ask your doctor about further sources of information about your cancer. Knowing more about your specific condition may help you feel more comfortable when making treatment decisions.
- Find someone to talk with. Seek out sources of support that can help you deal with the emotions you’re feeling. You may have a close friend or family member who is a good listener. Clergy members and counselors are other options. Consider joining a support group for people with cancer. Contact your local chapter of the American Cancer Society or Support for People with Oral and Head and Neck Cancer. The American Cancer Society’s Cancer Survivors Network offers online message boards and chatrooms that you can use to connect with others with throat cancer.
- Take care of yourself during cancer treatment. Make keeping your body healthy during treatment a priority. Avoid extra stress. Get enough sleep each night so that you wake feeling rested. Take a walk or find time to exercise when you feel up to it. Make time for relaxing, such as listening to music or reading a book.
- Go to all of your follow-up appointments. Your doctor will schedule follow-up exams every few months during the first two years after treatment, and then less frequently after that. These exams allow your doctor to monitor your recovery and check for a cancer recurrence.
Follow-up exams can make you nervous, since they may remind you of your initial diagnosis and treatment. You may fear that your cancer has come back. Expect some anxiety around the time of each follow-up appointment. Plan ahead by finding relaxing activities that can help redirect your mind away from your fears.
- Throat cancer. https://www.mayoclinic.org/diseases-conditions/throat-cancer/symptoms-causes/syc-20366462[↩]