Contents
What are tonsil stones
Tonsil stones are also known as tonsilloliths, are small white or yellow lumps of hardened material that can form in the palatine tonsils 1. Tonsil stones are formed by calcified accumulates of food, microorganism aggregates and cellular debris that can build up in the crypts of the palatine tonsils 2. Calcium hydroxyapatite and calcium carbonate along with other minerals including phosphorus, ammonia, and magnesium are the common types of stones identified in histology studies of tonsil stones 3. Tonsil stones can cause bad breath (halitosis). Tonsil stones are not harmful and may not need to be treated, but surgical options are available if they are a problem.
Tonsil stones are more common in adults than in children. The age of patients with tonsil stones ranges between 10 and 77 years with a median age of 50 years with a male to female ratio of 1:1 4.
Tonsil stones are usually small; it is rare to have a large tonsil stone.
Your tonsils are glands found at the back of your throat that help protect you against infection. The tonsil glands contain folds known as tonsillar crypts. Most tonsil stones are small, just 1 to 2 mm across. But they can be up to 1 cm across.
If your tonsillar crypts are enlarged, minerals like calcium can be trapped and harden or calcify into stones. Bacteria or fungi that cause tonsillitis can also cause tonsil stones to form.
Tonsil stones formation (tonsillolithiasis) is thought to occur mainly due to repeated inflammation of the tonsillar crypts with recurrent tonsillitis and calcification 1.
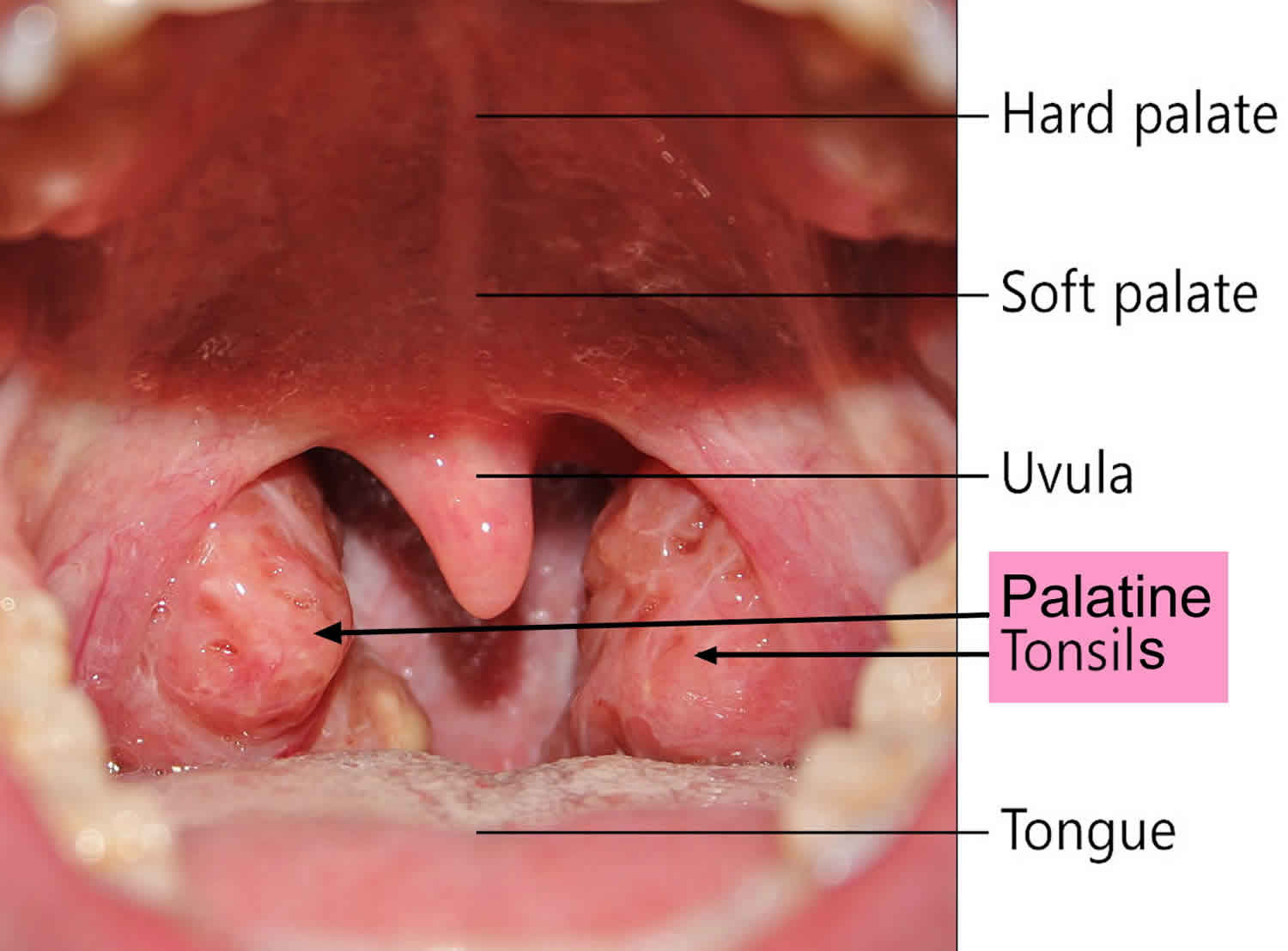
Figure 1. Normal healthy throat tonsils
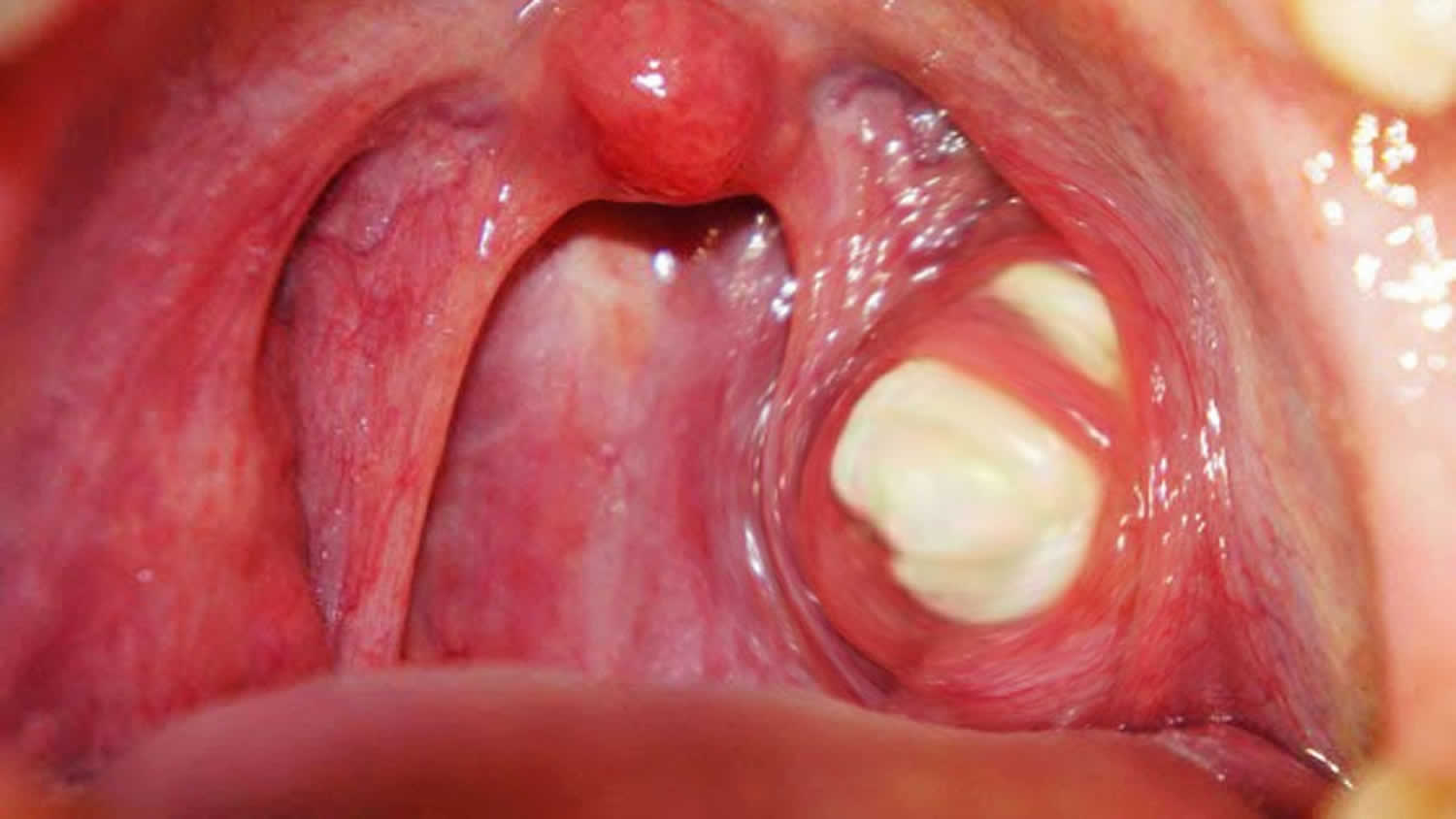
Figure 2. Tonsil stones
What do tonsils do
The tonsils are part of your body’s defense system. The tonsils serve immune acquisition and immune defence by antigen presentation, which is why they contain T-lymphocytes, macrophages and germinal centres of B-lymphocytes 5. Because of their location at the throat and palate, they have a kind of guardian function. They come into contact with germs especially soon after they enter through the mouth or the nose. Tonsils are the first and easiest-to-reach station of the mucosa associated lymphoid tissue system (MALT) in humans 6. This allows them to activate the immune system early. The greatest immunological activity of the tonsils is found between the ages of 3 and 10 years 7. As a result, the tonsils are most prominent during this period of childhood and subsequently demonstrate age-dependent involution 8. Since the main phase of the immune acquisition continues until the age of 6, the palatine tonsils are physiologically enlarged at this time 9. Then there is shrinkage, which is reflected mostly in a regression until the age of 12 10.
The oral cavity and especially the furrowed tonsil is a reservoir for multiple pathogens (viruses and bacteria), parasites 11 and fungi 12. However, all these microbes belong to the transient flora and we live in symbiosis with them for aeons 13. Jensen A. et al. 14 were able to detect more than 100 bacteria in the tonsils of children and adults with and without recurrent tonsillitis. 52 different bacterial strains form the basis were detectable in each patient, whether child or adult, whether sick or healthy. These represent 90% of the total pathogen load 14.
What are tonsillar crypts
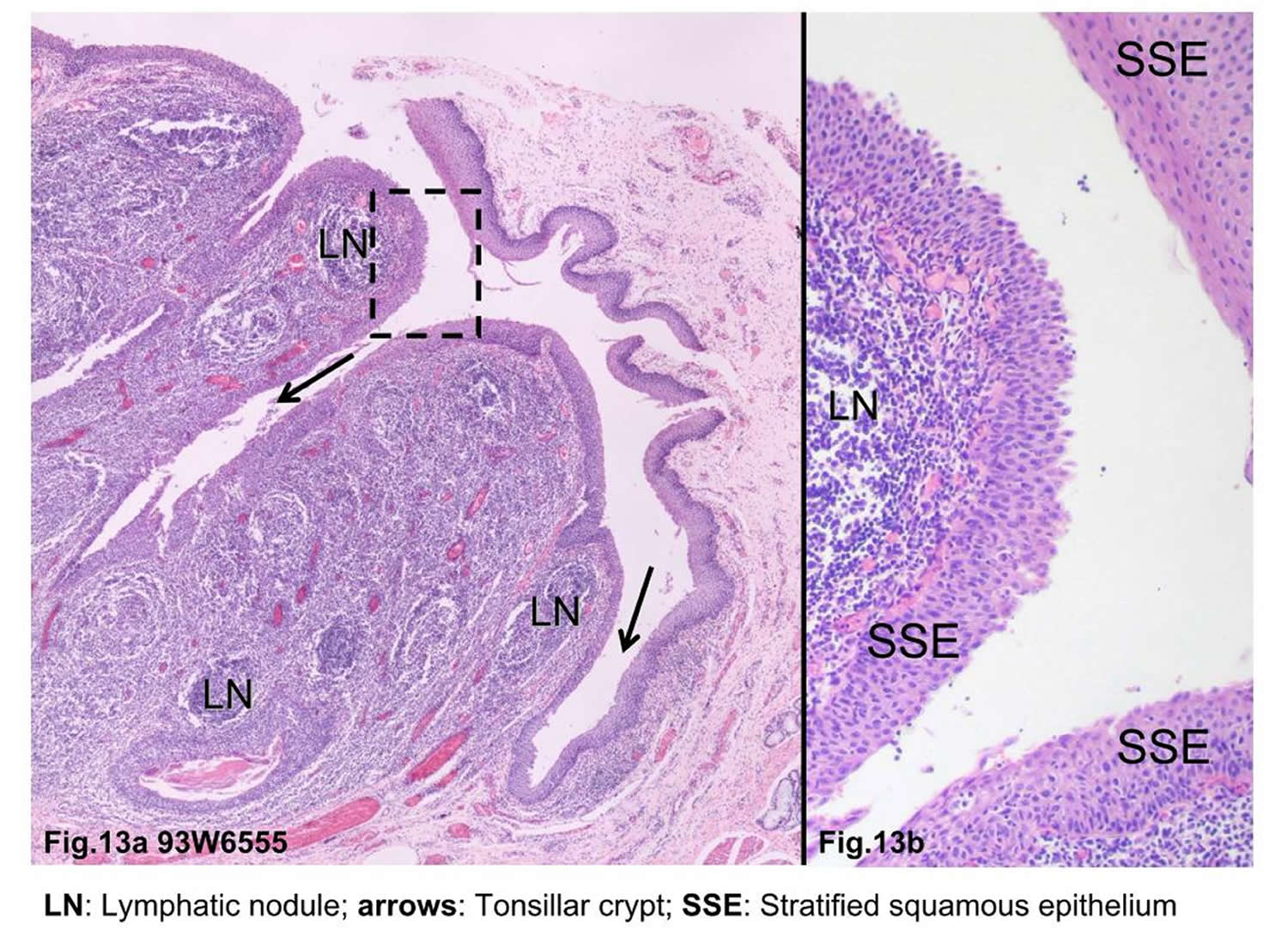
In a studies on the human palatine tonsils, scientists observed the crypts of the palatine tonsil contain many pores, ranging in diameter from 10 to 100 microns, on the luminal surface of the crypts 15. All of the crypt surface except at the sites of pores was covered by epithelial cells. Non-epithelial round cells, mostly lymphocytes, were exposed directly to the crypt lumen through these pores. In the lumen of palatine tonsillar crypts, numerous round cells were present which evidently pass through these pores from the parenchyma. This finding indicates that the tonsillar tissue is directly open to the crypt. Similar findings were obtained in the recess of the pharyngeal tonsil (adenoid).
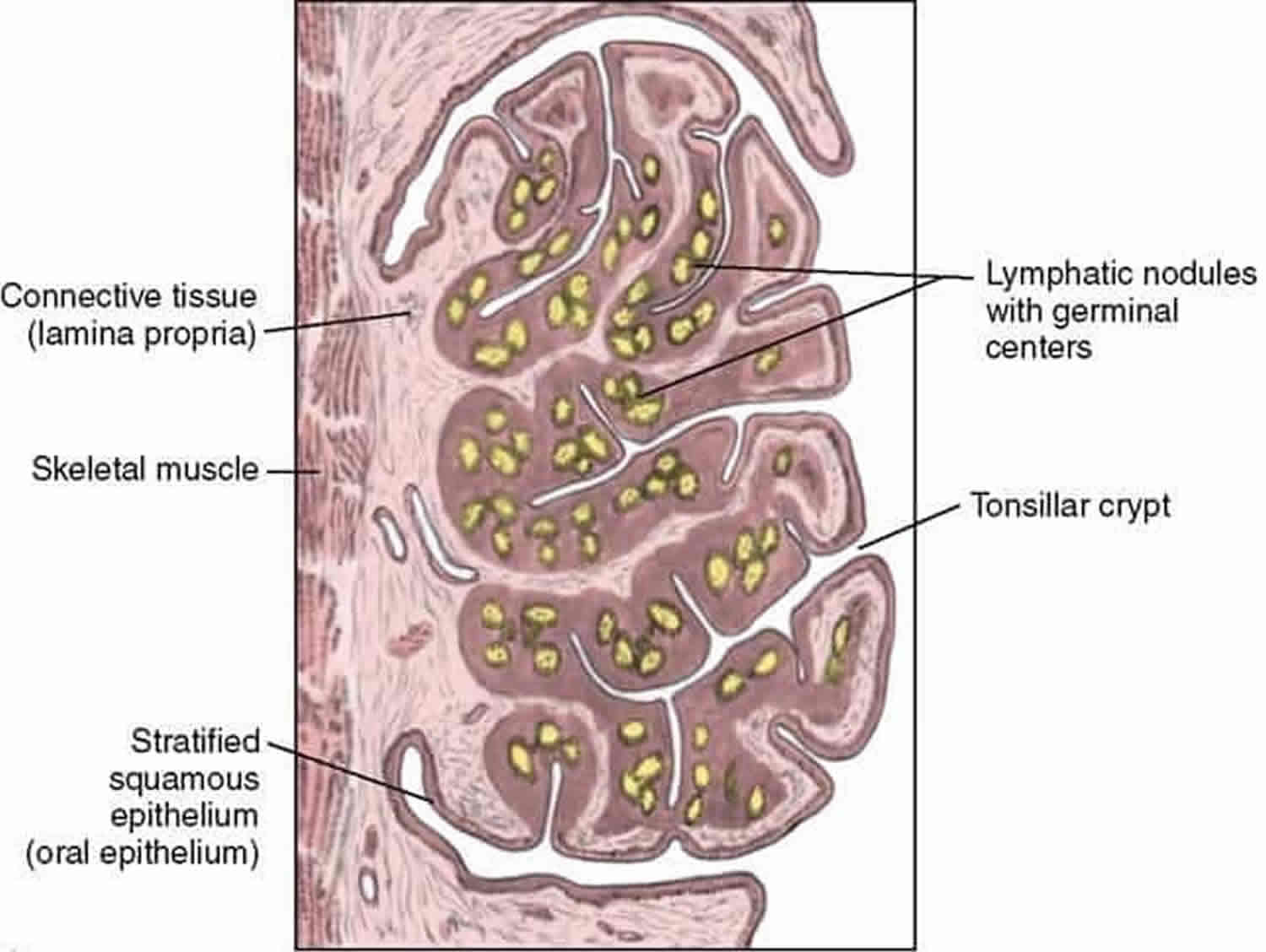
Figure 3. Tonsillar crypts
The epithelium of the human palatine tonsil is a site of interest because it overlies a mass of lymphoid tissue that forms a first line of defence in protecting the oropharyngeal isthmus, and as such is constantly exposed both to airborne and alimentary antigens. The surface area of the tonsillar epithelium available for this defensive role is maximised by the 10-30 blind-ending crypts and their rami extending through the full thickness of the tonsil almost to reach its hemicapsule.
The epithelium lining the tonsillar crypts is a highly modified form of the stratified squamous epithelium (SSE) called the “lymphoepithelium” that covers the oropharyngeal surface of the tonsil 16. The epithelium lining the crypts varied in structure from a stratified squamous epithelium (SSE) to a psuedostratified ciliated columnar epithelium (associated with the glands) or a single to double layer of round/cuboidal cells with round/oval nuclei 17. In places the epithelium appeared absent, its position being occupied by concentrations of lymphoid tissue. Lymphocytes were observed to traverse both the psuedostratified ciliated columnar epithelium and the epithelium composed of round/cuboidal cells. In places this took the form of individual or small groups of lymphocytes distorting the base of the epithelial lining cells and forming small pockets in which they were housed. These features were typical of specialised epithelial cells, the M cells, the presence of which, together with the infiltrating lymphocytes, is indicative of a lymphoepithelium or follicle-associated epithelium 18. These “M” cells cells take up antigens into vesicles and transport them to the extrafollicular region or the lymphoid follicles. In the extrafollicular region, interdigitating dendritic cells and macrophages process the antigens and present them to helper T lymphocytes. These lymphocytes stimulate proliferation of follicular B lymphocytes and their development into either antibody-expressing B memory cells capable of migration to the nasopharynx and other sites or plasma cells that produce antibodies and release them into the lumen of the crypt 19.
The presence, and sometimes the predominance, of nonepithelial cells was characteristic of the reticulated epithelium. T and B lymphocytes often infiltrated the whole epithelial thickness, and many plasma cells were located around intraepithelial vessels, while macrophages and interdigitating cells showed a patchy distribution. It is proposed that the major functions of the reticulated epithelium are: (1) to provide a favorable environment for the intimate contact between the effector cells of immune responses; (2) to facilitate direct transport of antigens; (3) to synthesize the secretory component continually; and (4) to contain a pool of immunoglobulins. Thus the reticulated epithelium lining the tonsillar crypts represents a specialized compartment, important in the immunological functions of the tonsil as a whole.
The lymphoid tissue was well vascularised and the capillaries and venules were lined by endothelial cells with round to oval, pale nuclei. Many lymphocytes were present in the lumen of the blood vessels, showing a high degree of trafficking. Lymph nodules were surrounded by a delicate layer of connective tissue.
It is now recognized that crypts epithelium are usually infiltrated by lymphocytes 20. This observations are later confirmed that the function of the palatine tonsil was ‘protection and defence’. Scientists likened the network of epithelial cells to a sponge, which holds the lymphoid cells in its interstices.
While all 5 immunoglobulin (Ig) isotypes are produced in the palatine tonsils, IgA is arguably the most important product of the tonsillar immune system. In its dimeric form, IgA may attach to the transmembrane secretory component to form secretory IgA, a critical component of the mucosal immune system of the upper airway. Although the secretory component is produced only in the extratonsillar epithelium, the tonsils do produce immunocytes bearing the J (joining) chain carbohydrate 21. This component is necessary for binding of IgA monomers to each other and to the secretory component and is an important product of B-cell activity in the follicles of the tonsil.
What causes tonsil stones
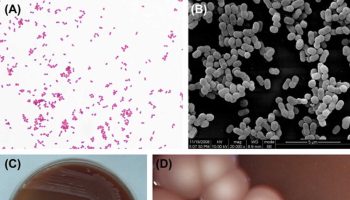
The exact mechanism of development of tonsillar stones is not well understood. However, several hypotheses exist to explain formation of tonsil stones. One hypothesis attributes stone formation to recurrent tonsillitis and subsequent crypt fibrosis that lead to epithelial cell retention, which creates an environment for microorganism overgrowth and calcification due to deposition of inorganic salts from salivary gland secretions 22. Stoodley et al 23 concluded that tonsilloliths share common characteristics with biofilms. Biofilms are aggregates of aerobic and non-aerobic microorganisms enclosed in an extracellular matrix. Due to the nature of biofilms, it is difficult to treat the microorganisms with antibiotics. In fact, a biofilm serves as a nidus for acute infections rendering it a source of recurrent ear nose and throat infections 24.
Tonsil stones symptoms
Tonsil stones commonly cause bad breath. Tonsil stones can also cause an irritable cough, earache, sore throat or a foul taste in your mouth.
If you have tonsil stones, you might find it hard to swallow. It might feel like there’s something stuck at the back of your throat. You might be able to see small patches of white on your tonsils.
Tonsil stones can also trigger infections and be difficult to treat with antibiotics.
Tonsil stones don’t always cause symptoms. Sometimes, tonsil stones are found on a scan or x-ray, or during a dental examination.
Tonsil stones diagnosis
If you think you might have tonsil stones, your doctor will talk to you and examine you. Tonsil stones might or might not be visible. A scan might help to find them if they are not obvious.
If the stones are dislodged and examined, they will usually smell foul.
Tonsil stones treatment
While you can manage the symptoms of tonsil stones, such as bad breath, there is no specific treatment for them. Good oral hygiene is important. This includes gargling with warm salt water and brushing your teeth regularly.
During vigorous gargling, the tonsil stones may become detached. Some people choose to dislodge them with a dental pick or swab. Be gentle if you decide to do this.
You might, however, decide you want them surgically removed. This option is best discussed with your doctor, who can refer you to an ear, nose and throat (ENT) specialist. The specialist will examine your tonsil stones and provide advice on the best course of action.
- Alfayez A, Albesher MB, Alqabasani MA. A giant tonsillolith. Saudi Med J. 2018;39(4):412-414. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5938656/[↩][↩]
- Giant tonsillolith. Hung CC, Lee JC, Kang BH, Lin YS. Otolaryngol Head Neck Surg. 2007 Oct; 137(4):676-7.[↩]
- Giant tonsillolith – a rare cause of dysphagia. Dykes M, Izzat S, Pothula V. J Surg Case Rep. 2012 Apr 1; 2012(4):4.[↩]
- Tonsillolith. Case report and review of the literature. Mesolella M, Cimmino M, Di Martino M, Criscuoli G, Albanese L, Galli V. Acta Otorhinolaryngol Ital. 2004 Oct; 24(5):302-7.[↩]
- Westermann J. Organe des Abwehrsystems. Berlin, Heidelberg: Springer; 2010. pp. 361–362.[↩]
- Morphology and immunology of the human palatine tonsil. Nave H, Gebert A, Pabst R. Anat Embryol (Berl). 2001 Nov; 204(5):367-73. https://www.ncbi.nlm.nih.gov/pubmed/11789984/[↩]
- Richardson, MA. Sore throat, tonsillitis, and adenoiditis. Med Clin North Am. 1999;83:75–83.[↩]
- Jung, KY, Lim, HH, Choi, G. Age-related changes of IgA immunocytes and serum and salivary IgA after tonsillectomy. Acta Otolaryngol Suppl. 1996;523:115–119.[↩]
- Early stage impacts of tonsillectomy on immune functions of children. Kaygusuz I, Gödekmerdan A, Karlidag T, Keleş E, Yalçin S, Aral I, Yildiz M. Int J Pediatr Otorhinolaryngol. 2003 Dec; 67(12):1311-5. https://www.ncbi.nlm.nih.gov/pubmed/14643474/[↩]
- Evaluation of long-term impacts of tonsillectomy on immune functions of children: a follow-up study. Kaygusuz I, Alpay HC, Gödekmerdan A, Karlidag T, Keles E, Yalcin S, Demir N. Int J Pediatr Otorhinolaryngol. 2009 Mar; 73(3):445-9. https://www.ncbi.nlm.nih.gov/pubmed/19150575/[↩]
- [The microbe colonization of the palatine tonsils of healthy school age children]. Mücke W, Huber HC, Ritter U. Zentralbl Hyg Umweltmed. 1994 Aug; 196(1):70-4. https://www.ncbi.nlm.nih.gov/pubmed/7802898/[↩]
- Tonsil surface and core cultures in recurrent tonsillitis: prevalence of anaerobes and beta-lactamase producing organisms. Mitchelmore IJ, Reilly PG, Hay AJ, Tabaqchali S. Eur J Clin Microbiol Infect Dis. 1994 Jul; 13(7):542-8. https://www.ncbi.nlm.nih.gov/pubmed/7805681/[↩]
- Molecular mapping to species level of the tonsillar crypt microbiota associated with health and recurrent tonsillitis. Jensen A, Fagö-Olsen H, Sørensen CH, Kilian M. PLoS One. 2013; 8(2):e56418. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3578847/[↩]
- Jensen A, Fagö-Olsen H, Sørensen CH, Kilian M. Molecular Mapping to Species Level of the Tonsillar Crypt Microbiota Associated with Health and Recurrent Tonsillitis. Xu P, ed. PLoS ONE. 2013;8(2):e56418. doi:10.1371/journal.pone.0056418. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3578847/[↩][↩]
- Pores of the palatine tonsillar crypt and pharyngeal tonsillar recess–a scanning electron microscopic study. Auris Nasus Larynx. 1979;6(1):23-30. https://www.ncbi.nlm.nih.gov/pubmed/549561[↩]
- The cells in tonsillar crypts. Clin Otolaryngol Allied Sci. 1982 Feb;7(1):35-44. https://www.ncbi.nlm.nih.gov/pubmed/7060282[↩]
- Functional morphology of tonsillar crypts in recurrent tonsillitis. Acta Otolaryngol Suppl. 1984;416:7-19. https://www.ncbi.nlm.nih.gov/pubmed/6598276[↩]
- Brandtzaeg, P. In: Immune functions and immunopathology of palatine and nasopharyngeal tonsils. Bernstein, JM, Ogra, PL, eds. Immunology of the Ear. New York, NY: Raven Press; 1987:63–106. [↩]
- Brandtzaeg, P. In: Immune functions and immunopathology of palatine and nasopharyngeal tonsils. Bernstein, JM, Ogra, PL, eds. Immunology of the Ear. New York, NY: Raven Press; 1987:63–106.[↩]
- Perry ME. The specialised structure of crypt epithelium in the human palatine tonsil and its functional significance. Journal of Anatomy. 1994;185(Pt 1):111-127. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1166820/pdf/janat00135-0110.pdf[↩]
- Brandtzaeg, P. Immunology of tonsils and adenoids: everything the ENT surgeon needs to know. Int J Pediatr Otorhinolaryngol. 2003;67:S69–S76.[↩]
- Thakur JS, Minhas RS, Thakur A, Sharma DR, Mohindroo NK. Giant tonsillolith causing odynophagia in a child: a rare case report. Cases J. 2008;1:50.[↩]
- Stoodley P, Debeer D, Longwell M, Nistico L, Hall-Stoodley L, Wenig B, et al. Tonsillolith: not just a stone but a living biofilm. Otolaryngol Head Neck Surg. 2009;141:316–321.[↩]
- Krespi YP, Shrime MG, Kacker A. The relationship between oral malodor and volatile sulfur compound-producing bacteria. Otolaryngol Head Neck Surg. 2006;135:671–676[↩]