Contents
What is toxoplasmosis
Toxoplasmosis is a common infection caused by the protozoan parasite, Toxoplasma gondii, that you can catch from the poo of infected cats or infected meat. Toxoplasmosis is usually harmless but can cause serious problems in some people -pregnant women and individuals who have compromised immune systems.
You are more at risk of toxoplasmosis if:
- You are pregnant – toxoplasmosis can cause miscarriage or stillbirth. If Toxoplasma gondii parasite spreads to your baby it can cause serious complications, especially if you catch it early in pregnancy
- Your immune system is weakened – for example, if you have HIV or you are having chemotherapy. Toxoplasmosis infection may affect your eyes or brain
Toxoplasma gondii parasite can be found in:
- Undercooked or raw meat
- Raw eggs
- Cured meat, such as parma ham or salami
- Unpasteurized goat’s milk and dairy products made from it
- Cat feces
- Soil or cat litter that is contaminated with infected cat feces.
You can come in contact with the toxoplasmosis parasite that causes the infection through:
- Eating raw or undercooked meat
- Eating unwashed fruits and vegetables
- Touching cat poop
- Touching kitchen utensils and cutting boards used to prepare raw or undercooked meat and fruits and vegetables
- Touching dirt or sand
Toxoplasma gondii cannot be passed from person to person, other than in mother-to-child (congenital) transmission and very rare cases of blood transfusion or organ transplantation.
People typically become infected by three principal routes of transmission.
- Foodborne
- Animal-to-human (zoonotic)
- Mother-to-child (congenital)
- Rare instances
Toxoplasma gondii infects most species of warm blooded animals like most birds, domestic cats and their relatives and mammals, including humans and is considered to be a leading cause of death attributed to foodborne illness in the United States. More than 60 million men, women, and children in the U.S. carry the Toxoplasma gondii parasite, but very few have symptoms because your immune system usually keeps the parasite from causing illness. But toxoplasmosis can cause big health problems for your baby during pregnancy.
In the United States it is estimated that 11% of the population 6 years and older have been infected with Toxoplasma. In various places throughout the world, it has been shown that up to 95% of some populations have been infected with Toxoplasma. Infection is often highest in areas of the world that have hot, humid climates and lower altitudes.
Toxoplasmosis doesn’t usually cause any symptoms and most people don’t realize they have had it.
Some people get flu-like symptoms, such as:
- high temperature (fever)
- aching muscles
- tiredness
- feeling sick
- sore throat
- swollen lymph nodes
If you do have symptoms, they normally get better on their own within about 6 weeks. However, women newly infected with Toxoplasma during pregnancy and anyone with a compromised immune system should be aware that toxoplasmosis can have severe consequences.
Once you have had toxoplasmosis you are immune to it for the rest of your life.
Serologic prevalence data indicate that toxoplasmosis is one of the most common human infections throughout the world. A high prevalence of infection in France has been related to a preference for eating raw or undercooked meat, while a high prevalence in Central America has been related to the frequency of stray cats in a climate favoring survival of oocysts and soil exposure. The overall seroprevalence in the United States among adolescents and adults, as determined with specimens collected by the third National Health and Nutrition Examination Survey (NHANES III) between 1988 and 1994, was found to be 22.5%, with a seroprevalence among women of childbearing age (15 to 44 years) of 15%. In a more recent evaluation using data from National Health and Nutrition Examination Survey 2009-2010, the overall age-adjusted Toxoplasma gondii antibody seroprevalence among persons > 6 years of age was 12.4%, and among women 15–44 years of age was 9.1%.
Acquired infection with Toxoplasma in immunocompetent persons is generally an asymptomatic infection. However, 10% to 20% of patients with acute infection may develop cervical lymphadenopathy and/or a flu-like illness. The clinical course is usually benign and self-limited; symptoms usually resolve within a few weeks to months. In rare cases ocular infection with visual loss can occur. Immunodeficient patients often have central nervous system (CNS) disease but may have retinochoroiditis, pneumonitis, or other systemic disease. In patients with AIDS, toxoplasmic encephalitis is the most common cause of intracerebral mass lesions and is thought to usually be caused by reactivation of chronic infection. Toxoplasmosis in patients being treated with immunosuppressive drugs may be due to either newly acquired or reactivated latent infection.
Toxoplasmosis in humans
Toxoplasmosis doesn’t usually cause any symptoms and most people don’t realize they have had it.
Some people get flu-like symptoms, such as:
- high temperature (fever)
- aching muscles
- tiredness
- feeling sick
- sore throat
- swollen lymph nodes or glands
If you do have symptoms, they normally get better on their own within about 6 weeks.
Once you have had toxoplasmosis you are immune to it for the rest of your life.
What should I do if I think I am at risk for severe toxoplasmosis?
If you are planning to become pregnant, your health care provider may test you for Toxoplasma gondii. If the test is positive it means you have already been infected sometime in your life. There usually is little need to worry about passing the infection to your baby. If the test is negative, take necessary precautions to avoid infection (See Toxoplasmosis prevention below).
If you are already pregnant, you and your health care provider should discuss your risk for toxoplasmosis. Your health care provider may order a blood sample for testing.
If you have a weakened immune system, ask your doctor about having your blood tested for Toxoplasma. If your test is positive, your doctor can tell you if and when you need to take medicine to prevent the infection from reactivating. If your test is negative, it means you need to take precautions to avoid infection. (See Toxoplasmosis prevention below).
What should I do if I think I may have toxoplasmosis?
If you suspect that you may have toxoplasmosis, talk to your health care provider. Your provider may order one or more varieties of blood tests specific for toxoplasmosis. The results from the different tests can help your provider determine if you have a Toxoplasma gondii infection and whether it is a recent (acute) infection.
Toxoplasmosis complications
If you have a normal immune system, you’re not likely to experience complications of toxoplasmosis, although otherwise healthy people sometimes develop eye infections. Untreated, these infections can lead to blindness.
But if your immune system is weakened, especially as a result of HIV/AIDS, toxoplasmosis can lead to seizures and life-threatening illnesses such as encephalitis — a serious brain infection.
In people with AIDS, untreated encephalitis from toxoplasmosis is fatal. Relapse is a constant concern for people with toxoplasmosis who also have a weakened immune system.
Children with congenital toxoplasmosis may develop disabling complications, including hearing loss, mental disability and blindness.
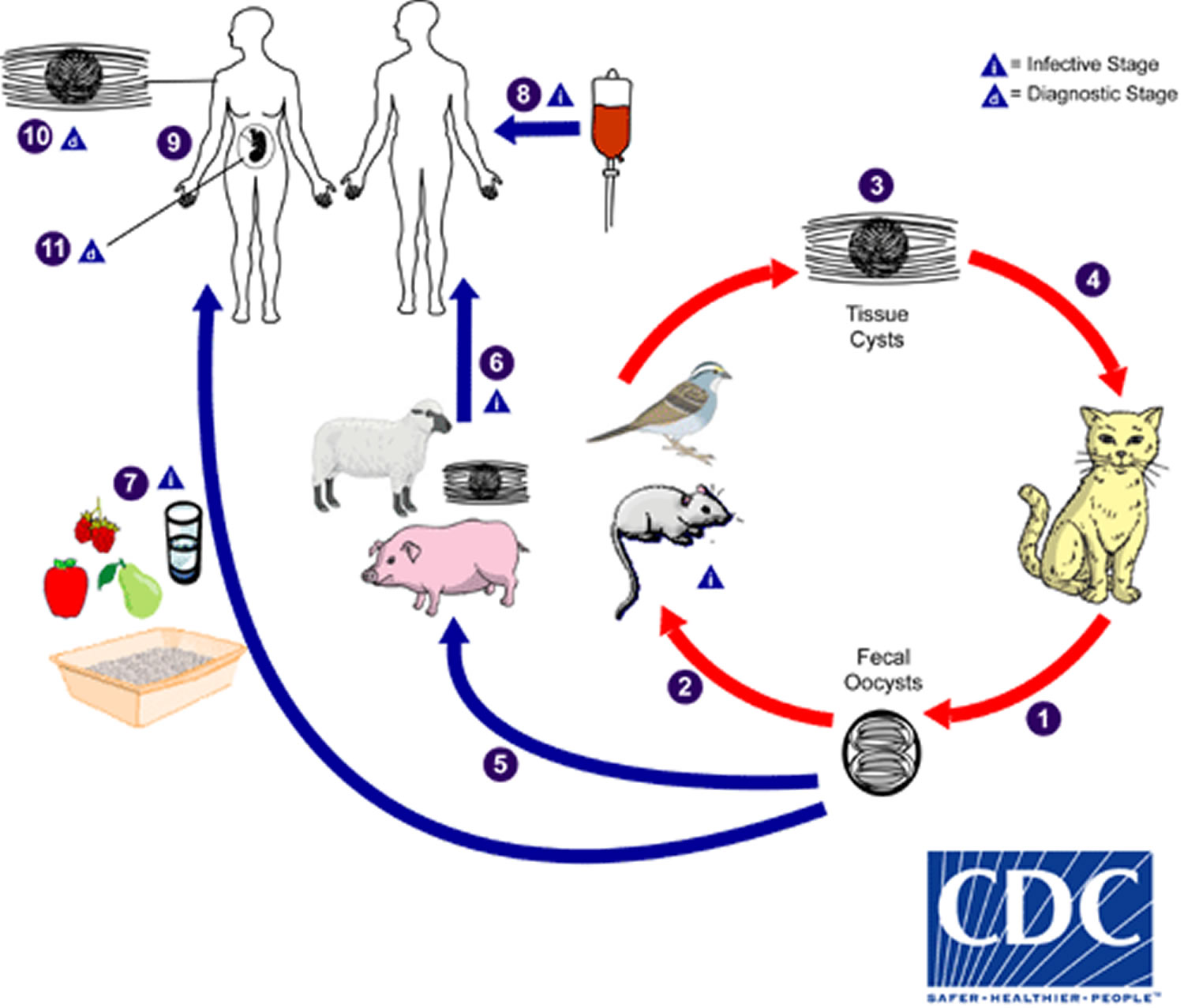
Toxoplasmosis Life Cycle
The only known definitive hosts for Toxoplasma gondii are members of family Felidae (domestic cats and their relatives).
- (1) Unsporulated oocysts are shed in the cat’s feces, although oocysts are usually only shed for 1–2 weeks, large numbers may be shed.
- (2) Intermediate hosts in nature (including birds and rodents) become infected after ingesting soil, water, or plant material contaminated with oocysts.
- (3) Oocysts transform into tachyzoites that localize in neural and muscle tissue and develop into tissue cyst bradyzoites.
- (4) Cats become infected after consuming intermediate hosts harboring tissue cysts or by ingestion of sporulated oocysts.
- (5) Animals bred for human consumption and wild game may also become infected with tissue cysts after ingestion of sporulated oocysts in the environment.
Humans can become infected by any of several routes:
- (6) eating undercooked meat of animals harboring tissue cysts.
- (7) consuming food or water contaminated with cat feces or by contaminated environmental samples (such as fecal-contaminated soil or changing the litter box of a pet cat).
- (8) blood transfusion or organ transplantation.
- (9) transplacentally from mother to fetus.
In the human host, the parasites form tissue cysts, most commonly in skeletal muscle, myocardium, brain, and eyes; these cysts may remain throughout the life of the host. Diagnosis is usually achieved by serology, although tissue cysts may be observed in stained biopsy specimens The number 10. Diagnosis of congenital infections can be achieved by detecting Toxoplasma gondii DNA in amniotic fluid using molecular methods such as PCR (11).
Figure 1. Toxoplasmosis Life Cycle
Foodborne transmission
The tissue form of the parasite (a microscopic cyst consisting of bradyzoites) can be transmitted to humans by food. People become infected by:
Eating undercooked, contaminated meat (especially pork, lamb, and venison)
Accidental ingestion of undercooked, contaminated meat after handling it and not washing hands thoroughly (Toxoplasma cannot be absorbed through intact skin)
Eating food that was contaminated by knives, utensils, cutting boards, or other foods that had contact with raw, contaminated meat
Animal-to-human (zoonotic) transmission
Cats play an important role in the spread of toxoplasmosis. They become infected by eating infected rodents, birds, or other small animals. The parasite is then passed in the cat’s feces in an oocyst form, which is microscopic.
Kittens and cats can shed millions of oocysts in their feces for as long as 3 weeks after infection. Mature cats are less likely to shed Toxoplasma if they have been previously infected. A Toxoplasma-infected cat that is shedding the parasite in its feces contaminates the litter box. If the cat is allowed outside, it can contaminate the soil or water in the environment as well.
People can accidentally swallow the oocyst form of the parasite. People can be infected by:
- Accidental ingestion of oocysts after cleaning a cat’s litter box when the cat has shed Toxoplasma in its feces
- Accidental ingestion of oocysts after touching or ingesting anything that has come into contact with a cat’s feces that contain Toxoplasma
- Accidental ingestion of oocysts in contaminated soil (e.g., not washing hands after gardening or eating unwashed fruits or vegetables from a garden)
- Drinking water contaminated with the Toxoplasma parasite
Mother-to-child (congenital) transmission
A woman who is newly infected with Toxoplasma during pregnancy can pass the infection to her unborn child (congenital infection). The woman may not have symptoms, but there can be severe consequences for the unborn child, such as diseases of the nervous system and eyes.
Rare instances of transmission
Organ transplant recipients can become infected by receiving an organ from a Toxoplasma-positive donor. Rarely, people can also become infected by receiving infected blood via transfusion. Laboratory workers who handle infected blood can also acquire infection through accidental inoculation.
Toxoplasmosis pregnancy
The risk of getting toxoplasmosis when you’re pregnant is very low.
If you get toxoplasmosis in the early stages of pregnancy, the risk of miscarriage is increased. It’s rare for the infection to pass to the baby during early pregnancy but if it does, it can cause serious health problems.
If you get toxoplasmosis during pregnancy, you have a 3 in 10 chance (30 percent) of passing the infection to your baby. The later in your pregnancy you get infected, the more likely it is that your baby gets infected. But the earlier in pregnancy you get infected, the more serious the baby’s problems may be after birth. For example, he could have microcephaly or vision problems. Some infected babies may die.
If you get toxoplasmosis for the first time when you’re pregnant, or up to three months before you conceive, there’s a risk that the infection can:
- pass to and damage your unborn baby (mother-to-child transmission)
- cause Preterm, Miscarriage or Stillbirth.
- Preterm birth – Birth before 37 weeks of pregnancy
- Stillbirth – This is when a baby dies in the womb after 20 weeks of pregnancy
The risk of problems varies, depending on when you become infected during your pregnancy.
In later pregnancy, the toxoplasmosis infection more commonly passes to the baby. For example:
- If you become infected around the time of conception, there is a less than 5% chance that your baby will also develop the infection.
- If you become infected during the third trimester of your pregnancy (from week 27 until the birth), there is about a 65% chance that your baby will also be infected.
- However, babies infected during later pregnancy are less likely to develop serious health problems.
If you have toxoplasmosis within 6 months of getting pregnant, you may be able to pass it to your baby during pregnancy. If you get toxoplasmosis in the early stages of pregnancy, the risk of miscarriage is increased and it can cause blindness and brain damage in an unborn baby. Talk to your health care provider about being tested.
Toxoplasmosis symptoms during pregnancy
You may not know if you have the infection. Lots of times there are no symptoms. For some people, it feels like the flu. Symptoms can include:
- Achy muscles
- Headache
- Fatigue (tiredness)
- Fever
- Discomfort
- Swollen glands
These symptoms can last for a month or longer. If you think you have toxoplasmosis, talk to your health care provider. Your provider can give you a blood test to find out if you have the infection. Even though blood tests are a regular part of prenatal care, you don’t’ usually get testing for toxoplasmosis. So be sure to talk to your provider if you think you have the infection.
If you have toxoplasmosis during pregnancy, your health care provider may suggest a test called amniocentesis (also called amnio) to see if your baby is infected. Amnio is a test that takes some amniotic fluid from around your baby in the uterus. You can get this test at 15 to 20 weeks of pregnancy.
The fluid can be tested to see if your baby has toxoplasmosis. It also can be tested for other problems with the baby, like birth defects or genetic problems. Birth defects are problems with a baby’s body that are present at birth. Genetic conditions may be passed from parents to children through genes and include certain diseases and birth defects.
What is amniocentesis?
Amniocentesis (also called amnio) is a prenatal test that takes amniotic fluid from around your baby in the uterus (also called womb). The fluid is tested to see if your baby has certain health conditions. A prenatal test is a medical test you get during pregnancy. Talk to your health care provider to see if amnio is right for you.
Amnio is a diagnostic test. This means that it tells you for sure whether or not your baby has a health condition. This is different from a screening test that tells if your baby’s more likely than others to have a certain condition. If results of a screening test aren’t normal, you may want to have a diagnostic test like amnio to diagnose (find out) if your baby has a condition. Amnio results almost always are correct.
Amnio is not recommended before 15 weeks because it has a higher risk of miscarriage and other complications. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy.
Having an amnio is your choice, even if you’re at risk of having a baby with a birth defect or genetic condition. Talk with your partner and obstetrician about your testing options.
How is amniocentesis done?
Here’s what happens when you have an amnio:
- You lie on your back on an exam table, and your provider covers your belly with a thin layer of gel.
- Your provider moves an ultrasound wand (also called transducer) across your belly to find your baby and the placenta. The placenta grows in your uterus and supplies your baby with food and oxygen through the umbilical cord. Ultrasound uses sound waves and a computer screen to show a picture of your baby inside the womb.
- Your provider cleans your belly with an antibacterial liquid that kills germs on your skin.
- Using ultrasound as a guide, your provider puts a thin needle through your belly and uterus into the amniotic sac. The amniotic sac (also called bag of waters) is the sac (bag) inside the uterus that holds your growing baby. It’s filled with amniotic fluid.
- Your provider uses the needle to remove a small amount of amniotic fluid (less than 1 ounce). The amniotic fluid contains cells from your baby.
- Once the fluid sample is taken, your provider uses the ultrasound to check that your baby’s heartbeat is healthy.
Your provider sends the sample to a lab where your baby’s cells are separated from the amniotic fluid. The cells grow for about 10 to 12 days at the lab and then they’re tested for birth defects and genetic conditions. The lab also can test the amniotic fluid for proteins like alpha-fetoprotein (also called AFP). AFP levels are often higher if your baby has a neural tube defect. Test results usually are available within 2 weeks.
If amnio shows that your baby has a health condition, talk to your provider about your options. For example, your baby may be able to be treated with medicines or surgery before or after birth. Knowing about a birth defect before birth may help you get ready to care for your baby. And you can make plans for your baby’s birth with your provider to make sure your baby gets special care or treatment he may need right after he’s born.
Are there any risks to having an amniocentesis?
Serious complications from amnio are rare. Most women have only mild discomfort during an amnio. You may have a stinging feeling when the needle enters your skin, feel cramping when the needle enters the uterus or feel pressure when the fluid is removed. After the test, your provider may tell you to take it easy for the rest of the day and not to exercise or have sex for a day or two.
Some women may have other complications from amnio, including:
- Miscarriage. Less than 1 in 200 women (less than 1 percent) have a miscarriage after an amnio.
- Infection in the uterus
- Cramping, spotting or leaking amniotic fluid. About 1 to 2 in 100 women (1 to 2 percent) have these problems.
- Passing infection to your baby. If you have an infection, like HIV or toxomplasmosis, you may pass it to your baby during amnio. HIV is the virus that causes AIDS. Toxoplasmosis is an infection you can get from eating undercooked meat or touching cat poop.
- Rh problems. Amnio may cause a small amount of your baby’s blood to mix with your blood. If you’re Rh-negative and your baby is Rh-positive, you may get a shot called Rh immune globulin after amnio to help protect your baby.
If you have any of these signs or symptoms after an amnio, call your obstetrician:
- Feeling a change in your baby’s movement
- Bleeding or leaking fluid from your vagina
- Fever
- Redness and swelling where your provider inserted the needle
- Strong belly cramps that last more than a few hours
Can toxoplasmosis during pregnancy harm your baby?
Most babies born with toxoplasmosis have no symptoms. But about 1 in 10 babies (10 percent) with the infection are born with problems, including:
- Eye infections
- Enlarged liver and spleen
- Jaundice (yellowing of the skin and the whites of the eyes)
- Pneumonia
Without treatment, 8 or 9 out of 10 newborns (85 percent) may develop problems later in life, even if they show no symptoms earlier. These problems include:
- Intellectual disabilities
- Vision problems
- Cerebral palsy (a group of disorders that can cause problems with brain development that can affect a person’s balance, posture and ability to move)
- Seizures
- Hearing loss
Each year, between 400 and 4,000 babies in the United States are born with toxoplasmosis. If you think you had toxoplasmosis during pregnancy, be sure your baby is tested. Your baby can have a blood test to check for this infection.
How is toxoplasmosis treated during pregnancy?
Getting treatment with certain antibiotics helps reduce the chance of your baby getting toxoplasmosis. Antibiotics are medicines that kill some types of organisms that cause infections. This treatment also helps reduce the seriousness of any symptoms your baby may have.
If you’re infected before 18 weeks of pregnancy, your provider may give you an antibiotic called spiramycin. This medicine helps reduce the chance of your baby getting the infection.
If you’re infected after 18 weeks of pregnancy, your provider may give you different antibiotics called pyrimethamine and sulfadiazine. These medicines are recommended for use after 18 weeks of pregnancy. This is because if you take them before 18 weeks of pregnancy, they may cause birth defects in your baby.
How is toxoplasmosis treated in your baby after birth?
If your baby shows symptoms of toxoplasmosis, he or she gets treated with the antibiotics pyrimethamine and sulfadiazine. He or she continues these antibiotic treatments through his/her first birthday, sometimes even longer.
Congenital toxoplasmosis
Congenital toxoplasmosis results from an acute primary infection acquired by the mother during pregnancy. Congenital toxoplasmosis has a wide spectrum of clinical manifestations, but it is subclinical in approximately 75% of infected newborns 1. The incidence and severity of congenital toxoplasmosis vary with the trimester during which infection was acquired —with first-trimester maternal infection leading to more severe manifestations. When clinically apparent, it may mimic other diseases of the newborn. In a proportion of cases, spontaneous abortion, prematurity, or stillbirth may result. Involvement of the central nervous system (CNS) is a hallmark of congenital Toxoplasma infection. The presence of chorioretinitis, intracranial calcifications, and hydrocephalus is considered the classic triad of congenital toxoplasmosis 1. Evidence of retinal infection may be found in 80-90% of known infected babies. Fever, hydrocephalus or microcephaly, hepatosplenomegaly, jaundice, convulsions, chorioretinitis (often bilateral), cerebral calcifications, and abnormal cerebrospinal fluid are the classic features of severe congenital toxoplasmosis 1. Other occasional findings included rash (maculopapular, petechial, or both), myocarditis, pneumonitis and respiratory distress, hearing defects, an erythroblastosis-like picture, thrombocytopenia, lymphocytosis, monocytosis, and nephrotic syndrome.
Some infected children without overt disease as neonates may escape serious sequelae of the infection; however, a significant number (14 to 85%) develop chorioretinitis, strabismus, blindness, hydrocephalus or microcephaly, cerebral calcifications, developmental delay, epilepsy, or deafness months or years later.
Many infants with subclinical infection at birth will subsequently develop signs or symptoms of congenital toxoplasmosis. Ocular Toxoplasma infection, an important cause of retinochoroiditis in the United States, can be the result of congenital infection, or infection after birth. In congenital infection, patients are often asymptomatic until the second or third decade of life, when lesions develop in the eye.
Because treatment of the mother may reduce the incidence of congenital infection and reduce sequelae in the infant, prompt and accurate diagnosis is important.
Current treatment regimens work primarily against the actively dividing tachyzoite form of Toxoplasma gondii and do not eradicate encysted organisms (bradyzoites). A significant paradigm shift over the past 20–30 years has been the realization that therapy begun prenatally and within the first 1–2 months after delivery can significantly ameliorate subsequent neurologic damage in infected children. For congenital infection, treatment regimens that include pyrimethamine and sulfadiazine with leukovorin—prolonged for at least 1 year and often initiated before birth—seem to be associated with substantially less frequent and severe sequelae. Further refining the optimal treatment regimen is an area requiring further research, especially as newer drugs (azithromycin, atovoquone, etc) with activity against the various stages of Toxoplasma are developed. Continued research is required to determine the impact of therapy during infancy upon recrudescent ocular disease in adolescents who were congenitally infected.
What happens to the eyes of babies born with congenital toxoplasmosis?
The infection causes inflammation of a small patch of retina which typically spontaneously resolves. However the infection can leave a localized scar (retina and underlying choroid) which contains the Toxoplasma organism in an inactive, encysted form. The chorioretinal scars do not affect vision unless the scar involves the central portion of the retina (the macula).
What are the long-term consequences of congenital ocular toxoplasmosis?
The chorioretinal scars of congenital ocular toxoplasmosis are generally inert. However, the encysted Toxoplasma organisms can reactivate causing inflammation, pain, redness, sensitivity to light, blurred vision, and increased intraocular pressure. Examination during reactivation reveals a cloud of white blood cells overlying the whitened patch of inflamed retina. In severe cases, the view into the eye is quite cloudy, and the underlying acute inflammation can be only dimly perceived.
Ocular toxoplasmosis
Ocular toxoplasmosis is an infection in the eye, a chorioretinal infection with Toxoplasma gondii parasite. Toxoplasmosis is the most common cause of back of the eye inflammation (posterior uveitis) in the world 2. Toxoplamosis can be acquired or present at birth (congenital), having crossed the placenta from a newly infected mother to her fetus. Most humans acquire toxoplasmosis by eating raw or undercooked meat, vegetables or milk products, or by coming into contact with infected cat litterbox or sandboxes. In humans, the infection usually causes no symptoms, and resolves without treatment in a few months. In individuals with compromised immune systems, Toxoplasma gondii can reactivate to cause disease 3.
Reactivation of a congenital infection was traditionally thought to be the most common cause of ocular toxoplasmosis, but an acquired infection is now considered to be more common 4. A toxoplasmosis infection that affects the eye usually attacks the retina and initially resolves without symptoms. However, the inactive parasite may later reactivate causing eye pain, blurred vision, and possibly permanent damage, including blindness. Although most cases of toxoplasmosis resolve on their own, for some, inflammation can be treated with antibiotics and steroids 5.
Visual symptoms during acute toxoplasma retinochoroiditis are typically secondary to vitritis or less frequently from the involvement of the macula or optic nerve. Vision loss may become permanent due to formation of a macular scar or optic atrophy, and up to 24% of patients may have 20/200 vision or less in at least one eye 6. A toxoplasmosis scar can be associated with severe visual field loss when it occurs close to the optic disk 7.
Ocular toxoplasmosis prognosis
The long-term outlook (prognosis) for ocular toxoplasmosis is dependent on what part of the eye is affected. Symptoms during an infection resulting in abnormal vision (blurriness, loss) are usually associated with involvement of the macula (the part of the eye needed for sharp, central vision) or the optic nerve. Vision loss may become permanent if a scar forms around the macula or if damage to the optic nerve occurs (optic nerve atrophy). If a scar forms around the optic disk (point of entry of the optic nerve in the eye), vision loss may be severe 4.
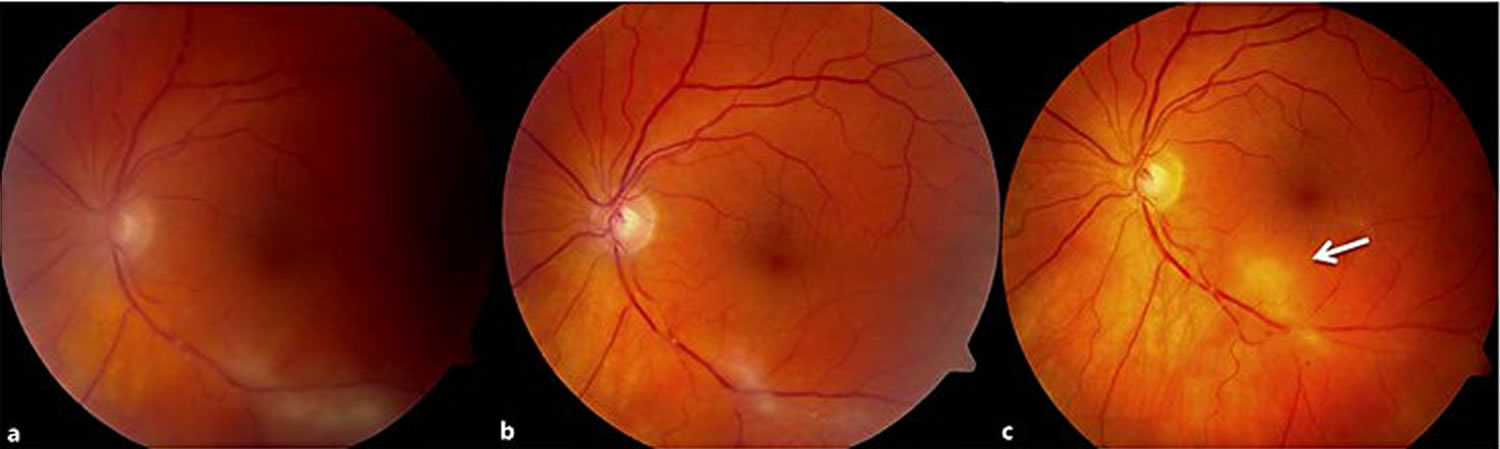
Figure 2. Ocular toxoplasmosis
Note: (a) Fundus photograph of a 63-year-old male patient with active ocular toxoplasmosis chorioretinitis with local vitritis along the inferior vascular arcade.( b) Resolved vitritis and resolving lesion 2 weeks after starting dual therapy with trimethoprim-sulfamethoxazole and prednisone. (c) Fibrosis and vitreoretinal adhesion with new focus of active retinitis closer to the fovea (white arrow). After the treatment of the new focus, trimethoprim-sulfamethoxazole prophylaxis continued for this patient.
Figure 3. Ocular toxoplasmosis
Note: (a) Primary manifestation of a peripheral retinochoroidal lesion in a 53-year-old immunocompetent male patient diagnosed with ocular toxoplasmosis by clinical appearance. (b) Active focal retinitis adjacent to the old scarred lesion in the same patient. (c) Recurrent manifestation was observed within 5 years presenting with ‘clustering’ appearance.
Ocular toxoplasmosis diagnosis
The diagnosis of ocular toxoplasmosis is usually evident based on typical clinical presentation. When the clinical diagnosis cannot be made definitely by a funduscopic examination, serological tests including serum anti-Toxoplasma titers of IgM and IgG may be needed to support the diagnosis. Toxoplasma gondii antibody titers in ocular fluids or polymerase chain reaction (PCR) of aqueous and vitreous samples are other newer tools with high sensitivity and specificity to confirm the diagnosis 8.
Most diagnostic laboratories are only capable of measuring IgG and IgM antibody levels using enzyme-linked immunosorbent assay (ELISA) or immunofluorescent antibody commercial kits. ELISA has an advantage over immunofluorescent antibody testing because it permits automation for simultaneous testing of large numbers of samples and the results are objective 9. The Sabin-Feldman dye test, the classic gold standard serology test, uses live Toxoplasma gondii tachyzoites to detect IgG antibodies 9. Despite its high sensitivity and specificity, this test is not frequently performed, owing to the risk for laboratory-acquired infections, and is available in very few reference laboratories in North America.
Serum IgM and IgG antibodies to Toxoplasma gondii develop within 1-2 weeks after infection 10. Patients suspected of acute toxoplasmosis may initially be analyzed for IgG serology primarily, and if the result is positive for IgG, IgM antibody levels may be measured. Nonreactive IgG rules out the toxoplasmosis diagnosis in an immunocompetent patient 11. IgM levels rise within the first week and become undetectable after 6-9 months. Elevated levels of antibodies alone should not be considered as an evidence of recent infection, nor should low serum IgG levels be considered as inactive disease. If the laboratory testing is unequivocal, levels of serological tests should be repeated in 15-21 days 9.
Asymptomatic patients with IgG reactivity alone may have latent infection with a history of primary exposure. This serological pattern is most important for immunosuppressed patients, including HIV infection and transplant recipients, and defines the risk for reactivation of disease 11. In patients with reactivation disease, IgM and IgG response may not be seen. In immunocompromised patients with seronegativity but strong clinical evidence, further tests to exclude Toxoplasma infection should be performed. These include IgG antibody testing or Toxoplasma gondii PCR of the vitreous and aqueous humor.
Serology is also used to assess the risk of transplacental transmission. IgG serology is performed in women considering pregnancy routinely in countries with endemic toxoplasmosis 12. Elevated levels of IgG before pregnancy in immunocompetent women indicate a low risk for transplacental transmission. Those with undetectable IgG levels are advised to avoid undercooked meat consumption or cat feces. Negative serology of IgM excludes acute infection in the last 6 months; if it is positive, it may persist up to 2 years after exposure to T. gondii. The IgG avidity test provides information about the time of exposure if serologies of IgG and IgM are reactive. An IgG avidity test resulting in high-avidity IgG antibodies in sera of patients in the first trimester indicates that the infection was acquired before conception, because high-avidity IgG antibodies take 3-4 months to appear 13. Low-avidity IgG antibodies should not be used to confirm the diagnosis of recent infection, due to persistence of these antibodies for many months after the acute infection 11.
Detection of Toxoplasma-specific antibodies or DNA of the parasite in ocular specimens is the main basis of the diagnosis 14. Intraocular antibody production is established by the Goldmann-Witmer coefficient (GWC), which compares the Toxoplasma-specific antibodies in ocular fluids and in serum 15. Although a ratio >1 should indicate intraocular antibody production, this may also occur in healthy controls, and therefore a ratio of at least 3 is often used to confirm diagnosis 16.
The contribution of PCR to help with the diagnosis is more controversial. In immunocompetent patients with the clinical diagnosis of ocular toxoplasmosis, DNA of Toxoplasma gondii could be amplified by PCR techniques only in 30-40% cases 17. However, in immunocompromised individuals, T. gondii DNA was amplified in 75% of the clinically diagnosed patients 18. Montoya et al. 19 reported that the diagnostic value of PCR in intraocular specimens for Toxoplasma gondii chorioretinitis was 67%. The sensitivity of PCR in patients meeting clinical diagnostic criteria for toxoplasmic chorioretinitis was lower in other studies, ranging from 27 to 36% 20. Despite low sensitivity, the specificity of PCR is 100% 21. PCR is a highly sensitive method of detecting nucleic acids, but no current standards are available to diagnose ocular toxoplasmosis, as reported by Garweg et al. 22 and this likely accounts for the wide range of PCR sensitivity in published reports. To improve the sensitivity of PCR, investigators are analyzing different DNA targets in patients with ocular toxoplasmosis. These studies are focused especially on Toxoplasma B1 gene, which is a promising genomic fragment, owing to the higher number of repeats and highly conserved DNA sequence 23. The sensitivity of PCR also depends on the immune status of the patient. When the clinical symptoms first manifest in immunocompetent patients, the intraocular inflammatory response reduces the parasitic burden in the aqueous humor and vitreous, thus decreasing the amount of target DNA for PCR amplification.
Fekkar et al. 17 reported that combining Goldmann-Witmer Coefficient with PCR significantly improved the diagnostic sensitivity from 81 to 93%. The sensitivity and the specificity of intraocular antibody detection have been reported to be 63 and 89% by others, and adding PCR as an additional laboratory test may be of value in some cases 21. In addition, Goldmann-Witmer Coefficient typically is more sensitive in immunocompetent patients, as the ocular antibody production is often unpredictable in immunocompromised patients. Rothova et al. 24 reported Goldmann-Witmer Coefficient sensitivity of 57% in immunocompromised patients, whereas the sensitivity was 93% in immunocompetent patients.
Ocular toxoplasmosis treatment
In individuals with a normally functioning immune system and mild symptoms that do not threaten the function of the eye, treatment may not be needed and symptoms may resolve within 4-8 weeks 25. Considering the natural history of this disease and the side effects of medications, the risk of treatment secondary to the potential toxicity of antiparasitic medications may be greater than any benefit provided. However, for cases in which there is a potential for vision loss, treatment may involve the use of anti-parasitic medications, steroids, and antibiotics. Typically, the anti-parasitic medication pyrimethamine is utilized in combination with the antibiotic sulfadiazine and corticosteroids. Other medications that have been used in individuals with ocular toxoplasmosis include the antibiotics clindamycin, azithromycin, and trimethoprim-sulfamethoxazole and the steroid dexamethasone 4. For example, “classic therapy” for ocular toxoplasmosis, adults: pyrimethamine 100 mg for 1 day as a loading dose, then 25 to 50 mg per day, plus sulfadiazine 1 gram four times per day, plus folinic acid (leucovorin) 5-25 mg with each dose of pyrimethamine; pediatric dose: pyrimethamine 2 mg/kg first day then 1 mg/kg each day, plus sulfadiazine 50 mg/kg two times per day, plus folinic acid (leucovorin) 7.5 mg per day) for 4 to 6 weeks followed by reevaluation of the patient’s condition. Leucovorin protects the bone marrow from the toxic effects of pyrimethamine. If the patient has a hypersensitivity reaction to sulfa drugs, pyrimethamine plus clindamycin can be used instead. The fixed combination of trimethoprim with sulfamethoxazole has been used as an alternative, as well as other drugs such as atovaquone and pyrimethamine plus azithromycin, which have not been extensively studied.
Toxoplasmosis causes
Toxoplasma gondii is a single-celled parasitic organism that can infect most animals and birds. Because Toxoplasma gondii infectious organisms are excreted only in cat feces, wild and domestic cats are the parasite’s ultimate host.
Although you can’t “catch” toxoplasmosis from an infected child or adult, you can become infected if you:
- Come into contact with cat feces that contain the parasite. You may accidentally ingest the parasites if you touch your mouth after gardening, cleaning a litter box or touching anything that has come in contact with infected cat feces. Cats who hunt or who are fed raw meat are most likely to harbor T. gondii.
- Eat or drink contaminated food or water. Lamb, pork and venison are especially likely to be infected with T. gondii. Occasionally, unpasteurized dairy products also may contain the parasite. Water contaminated with T. gondii isn’t common in the United States.
- Use contaminated knives, cutting boards or other utensils. Kitchen utensils that come into contact with raw meat can harbor the parasites unless the utensils are washed thoroughly in hot, soapy water.
- Eat unwashed fruits and vegetables. The surface of fruits and vegetables may contain the parasite. To be safe, thoroughly wash and peel all produce, especially any you eat raw.
- Receive an infected organ transplant or transfused blood. In rare cases, toxoplasmosis can be transmitted through an organ transplant or blood transfusion.
When a person becomes infected with Toxoplasma gondii, the parasite forms cysts that can affect almost any part of the body — often your brain and muscle tissue of different organs, including the heart.
If you’re generally healthy, your immune system keeps the parasites in check. They remain in your body in an inactive state, providing you with lifelong immunity so that you can’t become infected with the parasite again. But if your immune system is weakened by disease or certain medications, the infection can be reactivated, leading to serious complications.
Risk factors for toxoplasmosis
Anyone can become infected with toxoplasmosis. The parasite is found throughout the world.
You’re at risk of serious health problems from toxoplasmosis infection if:
- You have HIV/AIDS. Many people with HIV/AIDS also have toxoplasmosis, either a recent infection or an old infection that has reactivated.
- You’re undergoing chemotherapy. Chemotherapy affects your immune system, making it difficult for your body to fight even minor infections.
- You take steroids or other immunosuppressant drugs. Medications used to treat certain nonmalignant conditions suppress your immune system and make you more likely to develop complications of toxoplasmosis.
Toxoplasmosis prevention
The parasite that causes toxoplasmosis is found in the poo of infected cats and in infected meat. You can also catch it from soil that has been contaminated by cat poo.
If you are pregnant or have a weak immune system:
DO
- Wear gloves while gardening. Wash your hands afterwards.
- Wash your hands before preparing food and eating
- Wash hands, knives and chopping boards thoroughly after preparing raw meat
- Wash fruit and vegetables thoroughly to get rid of any traces of soil
- Wear gloves while emptying cat litter trays and empty them every day
- Don’t eat raw or undercooked meat, especially lamb or pork. Cooked meat should not look pink, and the juices should be clear.
- Wash your hands with soap and water after handling fruits, vegetables or raw meat.
- Don’t touch your eyes, nose or mouth when handling raw meat.
- Clean cutting boards, work surfaces and utensils with hot, soapy water after using them with fruits, vegetables or raw meat.
- Peel or thoroughly wash all raw fruits and vegetables before eating.
- Don’t let your cat go outside your home where it may come in contact with the parasite.
- Ask someone else to clean your cat’s litter box. If you have to do it yourself, wear gloves. Wash your hands thoroughly when you’re done emptying the litter.
- Stay away from children’s sandboxes. Cats like to use them as litter boxes.
Cook food to safe temperatures. A food thermometer should be used to measure the internal temperature of cooked meat. Do not sample meat until it is cooked. USDA recommends the following for meat preparation.
For Whole Cuts of Meat (excluding poultry)
- Cook to at least 145° F (63° C) as measured with a food thermometer placed in the thickest part of the meat, then allow the meat to rest* for three minutes before carving or consuming.
For Ground Meat (excluding poultry)
- Cook to at least 160° F (71° C); ground meats do not require a rest* time.
For All Poultry (whole cuts and ground)
Cook to at least 165° F (74° C), and for whole poultry allow the meat to rest* for three minutes before carving or consuming.
*According to USDA, “A ‘rest time’ is the amount of time the product remains at the final temperature, after it has been removed from a grill, oven, or other heat source. During the three minutes after meat is removed from the heat source, its temperature remains constant or continues to rise, which destroys pathogens.”
- Freeze meat for several days at sub-zero (0° F or minus 17.8 °C) temperatures before cooking to greatly reduce chance of infection.
- Peel or wash fruits and vegetables thoroughly before eating.
- Do not eat raw or undercooked oysters, mussels, or clams (these may be contaminated with Toxoplasma that has washed into sea water).
- Do not drink unpasteurized goat’s milk.
- Wash cutting boards, dishes, counters, utensils, and hands with hot soapy water after contact with raw meat, poultry, seafood, or unwashed fruits or vegetables.
- Wear gloves when gardening and during any contact with soil or sand because it might be contaminated with cat feces that contain Toxoplasma gondii. Wash hands with soap and water after gardening or contact with soil or sand.
- Teach children the importance of washing hands to prevent infection.
DON’T
- eat raw or undercooked meat, or cured meats like salami or Parma ham
- have unpasteurized goat’s milk or any products made from it
- touch or handle pregnant sheep or lambs
If I am at risk, can I keep my cat?
Yes, you may keep your cat if you are a person at risk for a severe infection (e.g., you have a weakened immune system or are pregnant); however, there are several safety precautions to avoid being exposed to Toxoplasma gondii :
- Ensure the cat litter box is changed daily. The Toxoplasma parasite does not become infectious until 1 to 5 days after it is shed in a cat’s feces.
- If you are pregnant or immunocompromised:
- Avoid changing cat litter if possible. If no one else can perform the task, wear disposable gloves and wash your hands with soap and water afterwards.
- Keep cats indoors.
- Do not adopt or handle stray cats, especially kittens. Do not get a new cat while you are pregnant.
- Feed cats only canned or dried commercial food or well-cooked table food, not raw or undercooked meats.
- Keep your outdoor sandboxes covered.
Your veterinarian can answer any other questions you may have regarding your cat and risk for toxoplasmosis.
Once infected with Toxoplasma is my cat always able to spread the infection to me?
No, cats only spread Toxoplasma in their feces for a few weeks following infection with the parasite. Like humans, cats rarely have symptoms when infected, so most people do not know if their cat has been infected. The Toxoplasma shedding in feces will go away on its own; therefore it does not help to have your cat or your cat’s feces tested for Toxoplasma.
Toxoplasmosis symptoms
Toxoplasmosis symptoms in humans
Symptoms of the infection vary.
- Most people who become infected with Toxoplasma gondii are not aware of it.
- Some people who have toxoplasmosis may feel as if they have the “flu” with swollen lymph glands or muscle aches and pains that last for a month or more.
- high temperature (fever)
- aching muscles
- tiredness
- feeling sick
- sore throat
- swollen lymph nodes or glands
- Severe toxoplasmosis, causing damage to the brain, eyes, or other organs, can develop from an acute Toxoplasma infection or one that had occurred earlier in life and is now reactivated. Severe cases are more likely in individuals who have weak immune systems, though occasionally, even persons with healthy immune systems may experience eye damage from toxoplasmosis.
- Signs and symptoms of ocular toxoplasmosis can include reduced vision, blurred vision, pain (often with bright light), redness of the eye, and sometimes tearing. Ophthalmologists sometimes prescribe medicine to treat active disease. Whether or not medication is recommended depends on the size of the eye lesion, the location, and the characteristics of the lesion (acute active, versus chronic not progressing). An ophthalmologist will provide the best care for ocular toxoplasmosis.
- Most infants who are infected while still in the womb have no symptoms at birth, but they may develop symptoms later in life. A small percentage of infected newborns have serious eye or brain damage at birth.
People who are most likely to develop severe toxoplasmosis include:
- Infants born to mothers who are newly infected with Toxoplasma gondii during or just before pregnancy.
- Persons with severely weakened immune systems, such as individuals with AIDS, those taking certain types of chemotherapy, and those who have recently received an organ transplant.
In people with weakened immune systems
If you have HIV/AIDS, are receiving chemotherapy or have recently had an organ transplant, a previous toxoplasma infection may reactivate. In that case, you may develop more-severe signs and symptoms of infection, including:
- Headache
- Confusion
- Poor coordination
- Seizures
- Lung problems that may resemble tuberculosis or Pneumocystis jiroveci pneumonia, a common opportunistic infection that occurs in people with AIDS
- Blurred vision caused by severe inflammation of your retina (ocular toxoplasmosis)
In babies
If you become infected for the first time just before or during your pregnancy, you can pass the infection to your baby (congenital toxoplasmosis), even if you don’t have signs and symptoms yourself.
Your baby is most at risk of contracting toxoplasmosis if you become infected in the third trimester and least at risk if you become infected during the first trimester. On the other hand, the earlier in your pregnancy the infection occurs, the more serious the outcome for your baby.
Many early infections end in stillbirth or miscarriage. Infants who survive are likely to be born with serious problems, such as:
- Seizures
- An enlarged liver and spleen
- Yellowing of the skin and whites of the eyes (jaundice)
- Severe eye infections
Only a small number of babies who have toxoplasmosis show signs of the disease at birth. Often, infants who are infected don’t develop signs — which may include hearing loss, mental disability or serious eye infections — until their teens or later.
Toxoplasmosis diagnosis
The diagnosis of toxoplasmosis may be documented by:
- Observation of parasites in patient specimens, such as bronchoalveolar lavage material from immunocompromised patients, or lymph node biopsy.
- Isolation of parasites from blood or other body fluids, by intraperitoneal inoculation into mice or tissue culture. The mice should be tested for the presence of Toxoplasma organisms in the peritoneal fluid 6 to 10 days post inoculation; if no organisms are found, serology can be performed on the animals 4 to 6 weeks post inoculation.
- Detection of parasite genetic material by PCR (polymerase chain reaction), especially in detecting congenital infections in utero. Polymerase chain reaction is a technique used in molecular biology to amplify a single copy or a few copies of a segment of DNA or RNA across several orders of magnitude, generating thousands to millions of copies of a particular DNA or RNA sequence.
- Serologic testing is the routine method of diagnosis.
Toxoplasmosis test
Antibody Detection
The detection of Toxoplasma-specific antibodies is the primary diagnostic method to determine infection with Toxoplasma. Toxoplasma antibody detection tests are performed by a large number of laboratories with commercially available kits.
An algorithm for the immunodiagnosis of toxoplasmosis for individuals greater than one year of age is shown table below. The immunofluorescence assay (IFA) and enzyme immunoassay (EIA) tests for IgG and IgM antibodies are the tests most commonly used today. Persons should be initially tested for the presence of Toxoplasma-specific IgG antibodies to determine their immune status. A positive IgG titer indicates infection with the organism at some time. If more precise knowledge of the time of infection is necessary, then an IgG positive person should have an IgM test performed by a procedure with minimal nonspecific reactions, such as IgM-capture EIA. A negative IgM test essentially excludes recent infection, but a positive IgM test is difficult to interpret because Toxoplasma-specific IgM antibodies may be detected by EIA for as long as 18 months after acute acquired infection.
A major problem with Toxoplasma-specific IgM testing is lack of specificity. Two situations occur frequently: i) persons with a positive IgM but negative IgG, and ii) individuals with positive IgG and IgM results. In the first situation, a positive IgM result with a negative IgG result in the same specimen should be viewed with great suspicion; the patient’s blood should be redrawn two weeks after the first and tested together with the first specimen. If the first specimen was drawn very early after infection, the patient should have highly positive IgG and IgM antibodies in the second sample. If the IgG is negative and the IgM is positive in both specimens, the IgM result should be considered to be a false positive and the patient should be considered to be not infected. In the second situation, a second specimen should be drawn and both specimens submitted together to a reference lab which employs a different IgM testing system for confirmation.
If the patient is pregnant, and IgG/IgM positive, an IgG avidity test should be performed. A high avidity result in the first 12 to 16 weeks of pregnancy (time dependent upon the commercial test kit) essentially rules out an infection acquired during gestation. A low IgG avidity result should not be interpreted as indicating recent infection, because some individuals have persistent low IgG avidity for many months after infection. Suspected recent infection in a pregnant woman should be confirmed prior to intervention by having samples tested at a toxoplasmosis reference laboratory. If the patient has clinical illness compatible with toxoplasmosis but the IgG titer is low, a follow-up titer two to three weeks later should show an increase in antibody titer if the illness is due to acute toxoplasmosis, assuming the host is not severely immunocompromised.
Table 1. Toxoplasmosis Laboratory Diagnosis
| IgG Result | IgM Result | Report/interpretation for humans* |
|---|---|---|
| Negative | Negative | No serological evidence of infection with Toxoplasma. |
| Negative | Equivocal | Possible early acute infection or false-positive IgM reaction. Obtain a new specimen for IgG and IgM testing. If results for the second specimen remain the same, the patient is probably not infected with Toxoplasma. |
| Negative | Positive | Possible acute infection or false-positive IgM result. Obtain a new specimen for IgG and IgM testing. If results for the second specimen remain the same, the IgM reaction is probably a false-positive. |
| Equivocal | Negative | Indeterminate: obtain a new specimen for testing or retest this specimen for IgG in a different essay. |
| Equivocal | Equivocal | Indeterminate: obtain a new specimen for both IgG and IgM testing. |
| Equivocal | Positive | Possible acute infection with Toxoplasma. Obtain a new specimen for IgG and IgM testing. If results for the second specimen remain the same or if the IgG becomes positive, both specimens should be sent to a reference laboratory with experience in diagnosis of toxoplasmosis for further testing. |
| Positive | Negative | Infected with Toxoplasma for six months or more. |
| Positive | Equivocal | Infected with Toxoplasma for probably more than 1 year or false-positive IgM reaction. Obtain a new specimen for IgM testing. If results with the second specimen remain the same, both specimens should be sent to a reference laboratory with experience in the diagnosis of toxoplasmosis for further testing. |
| Positive | Positive | Possible recent infection within the last 12 months, or false-positive IgM reaction. Send the specimen to a reference laboratory with experience in the diagnosis of toxoplasmosis for further testing. |
Note: *except infants
[Source 26]Newborn infants suspected of congenital toxoplasmosis should be tested by both an IgM- and an IgA-capture EIA. Detection of Toxoplasma-specific IgA antibodies is more sensitive than IgM detection in congenitally infected babies. None of the current commercial assays offered in the United States have been cleared by the Food and Drug Administration for in vitro diagnostic use for infants; consequently, all specimens from neonates suspected of having congenital toxoplasmosis should be sent to the Toxoplasma Serology Laboratory, Palo Alto, CA, USA which has the most experience with infant testing.
Serological determination of active central nervous system toxoplasmosis in immunocompromised patients is not possible at this time. Toxoplasma-specific IgG antibody levels in AIDS patients often are low to moderate, but occasionally no specific IgG antibodies can be detected. Tests for IgM antibodies are generally negative.
Several commercial kits for Toxoplasma serologic testing are available. However, the sensitivity and specificity of these kits may vary widely from one commercial brand to another. This is of concern because serology results can influence decisions on continuation or termination of pregnancies.
Toxoplasma Human Serum Panel
To help evaluate the accuracy of commercial Toxoplasma antibody test kits, CDC created a Toxoplasma serum panel, the ‘CDC 1998 Toxoplasma Human Serum Panel,’ that contains known positive and negative sera. FDA now requires that any new commercial Toxoplasma test kit performs adequately based on results obtained using this panel 27
A panel of 100 human specimens (1.0 ml each) has been assembled to include samples which are Toxoplasma antibody negative, Toxoplasma-specific IgG positive but IgM negative, Toxoplasma-specific IgG and IgM positive and Toxoplasma-specific IgG and IgA positive. Specimens with varying levels of reactivity were included. The panel was tested by the Toxoplasma Serology Laboratory, Palo Alto Research Institute, Palo Alto, CA, for IgG, IgM, and IgA by the Sabin-Feldman Dye Test, the IgM-ELISA, the IgA-ELISA, and the differential agglutination (AC/HS) tests. The panel has also been tested at the Centers for Disease Control and Prevention (CDC) by IFA-IgG and the CDC EIA-IgM.
This panel is available for purchase from CDC by device manufacturers / U.S. distributors for Toxoplasma human antibody detection assays. After the panel is tested with a device, the results will be sent to CDC for analysis. The submitter will receive a written analysis from CDC including sensitivity and specificity rates for each immunoglobulin subclass tested, limited results of IgG reproducibility, graphs of device positive results vs. standard tests for each immunoglobulin subclass tested, and information regarding IgM and IgA results vs. time post-infection for both the device and the standard tests.
Testing in severe cases
If you’ve developed a life-threatening illness such as encephalitis, you may need one or more imaging tests to check for lesions or cysts in your brain. These include:
- Magnetic resonance imaging (MRI). This test uses a magnetic field and radio (electromagnetic) waves to create cross-sectional images of your head and brain. During the procedure, you lie inside a large, doughnut-shaped machine that contains a magnet surrounded by coils that send and receive radio waves. In response to the radio waves, your body produces faint signals that are picked up by the coils and processed into images by a computer. MRI is noninvasive and poses minimal risks to your health.
- Brain biopsy. In rare cases, especially if you don’t respond to treatment, a neurosurgeon may take a small sample of brain tissue. The sample is then analyzed in a laboratory to check for toxoplasmosis cysts.
Toxoplasmosis treatment
Once a diagnosis of toxoplasmosis is confirmed, you and your health care provider can discuss whether treatment is necessary. In an otherwise healthy person who is not pregnant, treatment usually is not needed. If symptoms occur, they typically go away within a few weeks to months. For pregnant women or persons who have weakened immune systems, medications are available to treat toxoplasmosis.
If you’re otherwise healthy and have signs and symptoms of acute toxoplasmosis, your doctor may prescribe the following drugs:
- Pyrimethamine (Daraprim). This medication, typically used for malaria, is a folic acid antagonist. It may prevent your body from absorbing the B vitamin folate (folic acid, vitamin B-9), especially when you take high doses over a long period. For that reason, your doctor may recommend taking additional folic acid. Other potential side effects of pyrimethamine include bone marrow suppression and liver toxicity.
- Sulfadiazine. This antibiotic is used with pyrimethamine to treat toxoplasmosis.
Treating pregnant women and babies
If you’re pregnant and infected with toxoplasmosis, treatment may vary depending on where you receive medical care.
If infection occurred before the 16th week of pregnancy, you may receive the antibiotic spiramycin. Use of this drug may reduce your baby’s risk of neurological problems from congenital toxoplasmosis. Spiramycin is routinely used to treat toxoplasmosis in Europe, but is still considered experimental in the United States.
If infection occurred after the 16th week of pregnancy, or if tests show that your unborn child has toxoplasmosis, you may be given pyrimethamine and sulfadiazine and folinic acid (leucovorin). Your doctor will help you determine the optimal treatment.
If your infant has toxoplasmosis or is likely to have it, treatment with pyrimethamine and sulfadiazine and folinic acid (leucovorin) is recommended. Your baby’s doctor will need to monitor your baby while he or she is taking these medications.
Treating people with HIV/AIDS
If you have HIV/AIDS, the treatment of choice for toxoplasmosis is also pyrimethamine and sulfadiazine, with folinic acid (leucovorin). An alternative is pyrimethamine taken with clindamycin (Cleocin).
- McAuley JB. Congenital Toxoplasmosis. Journal of the Pediatric Infectious Diseases Society. 2014;3(Suppl 1):S30-S35. doi:10.1093/jpids/piu077. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4164182/[↩][↩][↩]
- Jabs DA: Ocular toxoplasmosis. Int Ophthalmol Clin 1990;30:264-270.[↩]
- Wu L, Roy H, et al. Ophthalmologic Manifestations of Toxoplasmosis. Medscape. https://emedicine.medscape.com/article/2044905-overview[↩]
- Ozgonul C., Besirli C.G.. Recent Developments in the Diagnosis and Treatment of Ocular Toxoplasmosis. Ophthalmic Research. October 11, 2016. https://www.karger.com/Article/FullText/449169[↩][↩][↩]
- Toxoplasmosis. American Association for Pediatric Ophthalmology and Strabismus. https://aapos.org/terms/conditions/106[↩]
- Bosch-Driessen LE, Berendschot TT, Ongkosuwito JV, Rothova A: Ocular toxoplasmosis: clinical features and prognosis of 154 patients. Ophthalmology 2002;109:869-878. https://www.ncbi.nlm.nih.gov/pubmed/11986090[↩]
- Kim SJ, Scott IU, Brown GC, et al: Interventions for toxoplasma retinochoroiditis: a report by the American Academy of Ophthalmology. Ophthalmology 2013;120:371-378. https://www.ncbi.nlm.nih.gov/pubmed/23062648[↩]
- Harper TW, Miller D, Schiffman JC, Davis JL: Polymerase chain reaction analysis of aqueous and vitreous specimens in the diagnosis of posterior segment infectious uveitis. Am J Ophthalmol 2009;147:140-147. e2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4142712/[↩]
- Suzuki LA, Rocha RJ, Rossi CL: Evaluation of serological markers for the immunodiagnosis of acute acquired toxoplasmosis. J Med Microbiol 2001;50:62-70. https://www.ncbi.nlm.nih.gov/pubmed/11192507[↩][↩][↩]
- Marcolino PT, Silva DA, Leser PG, et al: Molecular markers in acute and chronic phases of human toxoplasmosis: determination of immunoglobulin G avidity by Western blotting. Clin Diagn Lab Immunol 2000;7:384-389. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC95883/[↩]
- Montoya JG, Liesenfeld O: Toxoplasmosis. Lancet 2004;363:1965-1976. https://www.ncbi.nlm.nih.gov/pubmed/15194258[↩][↩][↩]
- Montoya JG, Remington JS: Management of Toxoplasma gondii infection during pregnancy. Clin Infect Dis 2008;47:554-566. https://www.ncbi.nlm.nih.gov/pubmed/18624630[↩]
- Montoya JG, Huffman HB, Remington JS: Evaluation of the immunoglobulin G avidity test for diagnosis of toxoplasmic lymphadenopathy. J Clin Microbiol 2004;42:4627-4631. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC522337/[↩]
- Maenz M, Schluter D, Liesenfeld O, et al: Ocular toxoplasmosis past, present and new aspects of an old disease. Prog Retin Eye Res 2014;39:77-106. https://www.ncbi.nlm.nih.gov/pubmed/24412517[↩]
- Goldmann H, Witmer R: Antibodies in the aqueous humor (in German). Ophthalmologica 1954;127:323-330.[↩]
- De Groot-Mijnes JD, Rothova A, Van Loon AM, et al: Polymerase chain reaction and Goldmann-Witmer coefficient analysis are complimentary for the diagnosis of infectious uveitis. Am J Ophthalmol 2006;141:313-318. https://www.ncbi.nlm.nih.gov/pubmed/16458686[↩]
- Fekkar A, Bodaghi B, Touafek F, et al: Comparison of immunoblotting, calculation of the Goldmann-Witmer coefficient, and real-time PCR using aqueous humor samples for diagnosis of ocular toxoplasmosis. J Clin Microbiol 2008;46:1965-1967. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2446865/[↩][↩]
- Garweg JG, de Groot-Mijnes JD, Montoya JG: Diagnostic approach to ocular toxoplasmosis. Ocul Immunol Inflamm 2011;19:255-261. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3154545[↩]
- Montoya JG, Parmley S, Liesenfeld O, et al: Use of the polymerase chain reaction for diagnosis of ocular toxoplasmosis. Ophthalmology 1999;106:1554-1563. https://www.ncbi.nlm.nih.gov/pubmed/10442904[↩]
- Fardeau C, Romand S, Rao NA, et al: Diagnosis of toxoplasmic retinochoroiditis with atypical clinical features. Am J Ophthalmol 2002;134:196-203. https://www.ncbi.nlm.nih.gov/pubmed/12140026[↩]
- Villard O, Filisetti D, Roch-Deries F, et al: Comparison of enzyme-linked immunosorbent assay, immunoblotting, and PCR for diagnosis of toxoplasmic chorioretinitis. J Clin Microbiol 2003;41:3537-3541. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC179817/[↩][↩]
- Garweg JG, de Groot-Mijnes JD, Montoya JG: Diagnostic approach to ocular toxoplasmosis. Ocul Immunol Inflamm 2011;19:255-261. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3154545/[↩]
- Steeples LR, Guiver M, Jones NP: Real-time PCR using the 529 bp repeat element for the diagnosis of atypical ocular toxoplasmosis. Br J Ophthalmol 2016;100:200-203. https://www.ncbi.nlm.nih.gov/pubmed/26174811[↩]
- Rothova A, de Boer JH, Ten Dam-van Loon NH, et al: Usefulness of aqueous humor analysis for the diagnosis of posterior uveitis. Ophthalmology 2008;115:306-311. https://www.ncbi.nlm.nih.gov/pubmed/17669497[↩]
- Butler NJ, Furtado JM, Winthrop KL, Smith JR: Ocular toxoplasmosis. II. Clinical features, pathology and management. Clin Exp Ophthalmol 2013;41:95-108. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4028599/[↩]
- Toxoplasmosis. https://www.cdc.gov/dpdx/toxoplasmosis/index.html[↩]
- Preventing Congenital Toxoplasmosis. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr4902a5.htm[↩]