Contents
- What is a tuberculosis test
- What is tuberculosis?
- How to test for tuberculosis
- Tuberculosis test results
- Who should be tested for tuberculosis
- Diagnosing latent tuberculosis infection & tuberculosis disease
- Tuberculosis test side effects
What is a tuberculosis test
There are two kinds of tests that are used to detect tuberculosis bacteria in the body: the tuberculosis skin test (PPD) and tuberculosis blood tests (IGRAs). A positive tuberculosis skin test or tuberculosis blood test only tells that a person has been infected with tuberculosis bacteria. It does not tell whether the person has latent tuberculosis infection or has progressed to tuberculosis disease. Other tests, such as a chest x-ray and a sample of sputum, are needed to see whether the person has tuberculosis disease.
You should get tested for tuberculosis if:
- You have spent time with a person known or suspected to have tuberculosis disease; or
- You have HIV infection or another condition that weakens your immune system and puts you at high risk for tuberculosis disease; or
- You have symptoms of tuberculosis disease; or
- You are from a country where tuberculosis disease is very common (most countries in Latin America and the Caribbean, Africa, Asia, Eastern Europe, and Russia); or
- You live somewhere in the United States where tuberculosis disease is more common such as a homeless shelter, migrant farm camp, prison or jail, and some nursing homes; or
- You inject illegal drugs.
How does a tuberculosis test work?
Once inhaled the Mycobacterium tuberculosis bacteria reach the lung and grow slowly over several weeks. The body’s immune system is stimulated, which can be shown by a PPD skin test or tuberculosis blood test (an interferon gamma-release assay or IGRA). Tuberculosis blood test (interferon gamma-release assay) measures a person’s immune reactivity to Mycobacterium tuberculosis. White blood cells from most persons that have been infected with Mycobacterium tuberculosis will release interferon-gamma (IFN-g) when mixed with antigens (substances that can produce an immune response) derived from Mycobacterium tuberculosis. Tuberculosis blood tests (IGRAs) – have been developed using the tuberculosis antigens ‘early secretion antigen target 6′ (ESAT-6) and ‘culture filtrate protein 10′ (CFP-10), as well as tb7.7 in the QuantiFERON Gold and Gold in Tube assays, which are not present in BCG (tuberculosis vaccine), and are found in only a few species of environmental mycobacteria.
What is tuberculosis?
Tuberculosis (TB) is a serious bacterial infection with Mycobacterium tuberculosis. The Mycobacterium tuberculosis bacteria usually attack your lungs, but tuberculosis bacteria can attack any part of your body such as the kidney, spine, and brain. Not everyone infected with tuberculosis bacteria becomes sick. As a result, two tuberculosis-related conditions exist: latent tuberculosis infection and tuberculosis disease (active tuberculosis).
In most people the immune system either kills the Mycobacterium tuberculosis bacteria or builds a defensive barrier around the infection but the tuberculosis bacteria are not killed and lie dormant. This is called latent tuberculosis; the person is not ill and is not infectious. Sometimes at the time of the initial infection, bacteria get into the blood stream and can be carried to other parts of the body, such as bones, lymph glands or the brain, before the defensive barrier is built. It is estimated that one third of the world’s population, two billion people, have latent tuberculosis.
If the immune system fails to build the defensive barrier, or the barrier fails later, latent tuberculosis can spread within the lung (pulmonary tuberculosis) or develop in the other part(s) of the body it has spread to (extrapulmonary tuberculosis). Only some of those with latent tuberculosis will develop symptoms (‘active tuberculosis’). About half the cases of active tuberculosis develop within a few years of the original infection, particularly in children and young adults. The other half of active tuberculosis cases arise from reactivation of the latent infection many years later. Active tuberculosis infection causes serious illness and death, and can be difficult to treat. If not treated properly, tuberculosis disease (active tuberculosis) can be fatal.
Tuberculosis (TB) can also spread to other people.
Who catches tuberculosis?
Anyone can catch tuberculosis but those at particular risk are those who have been exposed to tuberculosis bacteria, and those who are less able to fight latent infection. They include:
- close contacts of infectious cases;
- those who have lived in, travel to or receive visitors from places where tuberculosis is still very common;
- those who live in ethnic minority communities originating from places where tuberculosis is very common;
- those with immune systems weakened by HIV infection or other medical problems;
- infants, young children and the elderly, as their immune systems are less robust;
- those with chronic poor health and nutrition because of lifestyle problems such as homelessness or problem drug or alcohol use;
- those living in poor or crowded housing conditions, including those living in hostels;
- those who have spent time in prison.
How tuberculosis spreads
tuberculosis bacteria are spread through the air from one person to another. The tuberculosis bacteria are put into the air when a person with tuberculosis disease of the lungs or throat coughs, speaks, or sings. People nearby may breathe in these bacteria and become infected.
Tuberculosis is NOT spread by:
- shaking someone’s hand
- sharing food or drink
- touching bed linens or toilet seats
- sharing toothbrushes
- kissing
When a person breathes in tuberculosis bacteria, the bacteria can settle in the lungs and begin to grow. From there, they can move through the blood to other parts of the body, such as the kidney, spine, and brain.
tuberculosis disease in the lungs or throat can be infectious. This means that the bacteria can be spread to other people. tuberculosis in other parts of the body, such as the kidney or spine, is usually not infectious.
People with tuberculosis disease are most likely to spread it to people they spend time with every day. This includes family members, friends, and coworkers or schoolmates.
What to do if you have been exposed to tuberculosis
You may have been exposed to tuberculosis bacteria if you spent time near someone with tuberculosis disease. The tuberculosis bacteria are put into the air when a person with active tuberculosis disease of the lungs or throat coughs, sneezes, speaks, or sings.
You CANNOT get tuberculosis from:
- Clothes
- Drinking glass
- Eating utensils
- Handshake
- Toilet
- Other surfaces
If you think you have been exposed to someone with tuberculosis disease, you should contact your doctor or local health department about getting a tuberculosis skin test or a special tuberculosis blood test. Be sure to tell the doctor or nurse when you spent time with the person who has tuberculosis disease.
It is important to know that a person who is exposed to tuberculosis bacteria is not able to spread the bacteria to other people right away. Only persons with active tuberculosis disease can spread tuberculosis bacteria to others. Before you would be able to spread tuberculosis to others, you would have to breathe in tuberculosis bacteria and become infected. Then the active bacteria would have to multiply in your body and cause active tuberculosis disease. At this point, you could possibly spread tuberculosis bacteria to others. People with tuberculosis disease are most likely to spread the bacteria to people they spend time with every day, such as family members, friends, coworkers, or schoolmates.
Some people develop tuberculosis disease soon (within weeks) after becoming infected, before their immune system can fight the tuberculosis bacteria. Other people may get sick years later, when their immune system becomes weak for another reason. Many people with tuberculosis infection never develop tuberculosis disease.
Preventing exposure to tuberculosis disease while traveling abroad
In many countries, tuberculosis is much more common than in the United States. Travelers should avoid close contact or prolonged time with known tuberculosis patients in crowded, enclosed environments (for example, clinics, hospitals, prisons, or homeless shelters).
Although multidrug-resistant and extensively drug-resistant tuberculosis are occurring globally, they are still rare. HIV-infected travelers are at greatest risk if they come in contact with a person with multidrug-resistant or extensively drug-resistant tuberculosis.
Air travel itself carries a relatively low risk of infection with tuberculosis of any kind. Travelers who will be working in clinics, hospitals, or other health care settings where tuberculosis patients are likely to be encountered should consult infection control or occupational health experts. They should ask about administrative and environmental procedures for preventing exposure to tuberculosis. Once those procedures are implemented, additional measures could include using personal respiratory protective devices.
Travelers who anticipate possible prolonged exposure to people with tuberculosis (for example, those who expect to come in contact routinely with clinic, hospital, prison, or homeless shelter populations) should have a tuberculosis skin test (PPD skin test) or a tuberculosis blood test (interferon gamma release assay or IGRA) before leaving the United States. If the test reaction is negative, they should have a repeat test 8 to 10 weeks after returning to the United States. Additionally, annual testing may be recommended for those who anticipate repeated or prolonged exposure or an extended stay over a period of years. Because people with HIV infection are more likely to have an impaired response to tuberculosis tests, travelers who are HIV positive should tell their physicians about their HIV infection status.
What is latent tuberculosis infection and tuberculosis disease
Not everyone infected with tuberculosis bacteria becomes sick. As a result, two tuberculosis-related conditions exist: latent tuberculosis infection and tuberculosis disease.
Table 1. Difference between Latent Tuberculosis Infection (LTBI) and Tuberculosis Disease
| A Person with Latent Tuberculosis Infection (LTBI) | A Person with Tuberculosis Disease |
|---|---|
| Has NO symptoms |
|
| Does not feel sick | Usually feels sick |
| Cannot spread TB bacteria to others | May spread TB bacteria to others |
| Usually has a skin test or blood test result indicating TB infection | Usually has a skin test or blood test result indicating TB infection |
| Has a normal chest x-ray and a negative sputum smear | May have an abnormal chest x-ray, or positive sputum smear or culture |
| Needs treatment for latent TB infection to prevent TB disease | Needs treatment to treat TB disease |
Latent tuberculosis infection
Tuberculosis bacteria can live in the body without making you sick. This is called latent tuberculosis infection. In most people who breathe in tuberculosis bacteria and become infected, the body is able to fight the bacteria to stop them from growing. People who have latent tuberculosis infection do not feel sick, do not have any symptoms, and cannot spread tuberculosis to others.
People with latent tuberculosis infection:
- Have no symptoms
- Don’t feel sick
- Can’t spread tuberculosis bacteria to others
- Usually have a positive tuberculosis skin test reaction or positive tuberculosis blood test
- May develop tuberculosis disease if they do not receive treatment for latent tuberculosis infection
Many people who have latent tuberculosis infection never develop tuberculosis disease. In these people, the tuberculosis bacteria remain inactive for a lifetime without causing disease. But in other people, especially people who have a weak immune system, the bacteria become active, multiply, and cause tuberculosis disease.
Preventing latent tuberculosis infection from progressing to tuberculosis disease (active tuberculosis)
Many people who have latent tuberculosis infection never develop tuberculosis disease. But some people who have latent tuberculosis infection are more likely to develop tuberculosis disease than others. Those at high risk for developing tuberculosis disease include:
- People with HIV infection
- People who became infected with tuberculosis bacteria in the last 2 years
- Babies and young children
- People who inject illegal drugs
- People who are sick with other diseases that weaken the immune system
- Elderly people
- People who were not treated correctly for tuberculosis in the past
If you have latent tuberculosis infection and you are in one of these high-risk groups, you should take medicine to keep from developing tuberculosis disease. There are several treatment options for latent tuberculosis infection. You and your health care provider must decide which treatment is best for you. If you take your medicine as instructed, it can keep you from developing tuberculosis disease. Because there are less bacteria, treatment for latent tuberculosis infection is much easier than treatment for tuberculosis disease. A person with tuberculosis disease has a large amount of tuberculosis bacteria in the body. Several drugs are needed to treat tuberculosis disease.
Tuberculosis disease (active tuberculosis)
Tuberculosis bacteria become active if your immune system can’t stop them from growing. When tuberculosis bacteria are active (multiplying in your body), this is called tuberculosis disease (active tuberculosis). People with tuberculosis disease are sick. They may also be able to spread the bacteria to people they spend time with every day.
Many people who have latent tuberculosis infection never develop tuberculosis disease. Some people develop tuberculosis disease soon after becoming infected (within weeks) before their immune system can fight the tuberculosis bacteria. Other people may get sick years later when their immune system becomes weak for another reason.
For people whose immune systems are weak, especially those with HIV infection, the risk of developing tuberculosis disease is much higher than for people with normal immune systems.
Symptoms of tuberculosis disease (active tuberculosis infection) depend on where in the body the tuberculosis bacteria are growing. tuberculosis bacteria usually grow in the lungs (pulmonary tuberculosis). Tuberculosis disease (active tuberculosis infection) in the lungs may cause symptoms such as:
- a bad cough that lasts 3 weeks or longer
- pain in the chest
- coughing up blood or sputum (phlegm from deep inside the lungs)
Other symptoms of tuberculosis disease(active tuberculosis infection) are:
- weakness or fatigue
- weight loss
- no appetite
- chills
- fever
- sweating at night
Symptoms of tuberculosis disease in other parts of the body depend on the area affected. Tuberculosis disease (active tuberculosis) often involves the lungs, but can involve any part of the body including the skin (cutaneous tuberculosis).
Tuberculosis Prevention
Bacille Calmette-Guérin (BCG) is a vaccine for tuberculosis disease. Bacille Calmette-Guérin (BCG) vaccine is not widely used in the United States, but it is often given to infants and small children in other countries where tuberculosis is common. Bacille Calmette-Guérin (BCG) does not always protect people from getting tuberculosis.
BCG Recommendations
In the United States, BCG should be considered for only very select people who meet specific criteria and in consultation with a tuberculosis expert. Health care providers who are considering BCG vaccination for their patients are encouraged to discuss this intervention with the tuberculosis control program in their area.
Children
BCG vaccination should only be considered for children who have a negative tuberculosis test and who are continually exposed, and cannot be separated from adults who:
- Are untreated or ineffectively treated for tuberculosis disease, and the child cannot be given long-term primary preventive treatment for tuberculosis infection; or
- Have tuberculosis disease caused by strains resistant to isoniazid and rifampin.
Health Care Workers
BCG vaccination of health care workers should be considered on an individual basis in settings in which:
- A high percentage of tuberculosis patients are infected with tuberculosis strains resistant to both isoniazid and rifampin;
- There is ongoing transmission of drug-resistant tuberculosis strains to health care workers and subsequent infection is likely; or
- Comprehensive tuberculosis infection-control precautions have been implemented, but have not been successful.
Health care workers considered for BCG vaccination should be counseled regarding the risks and benefits associated with both BCG vaccination and treatment of latent tuberculosis infection.
Testing for tuberculosis in BCG-Vaccinated People
Many people born outside of the United States have been BCG-vaccinated.
People who were previously vaccinated with BCG may receive a PPD skin test (tuberculosis skin test) to test for tuberculosis infection. Vaccination with BCG may cause a positive reaction to a tuberculosis skin test. A positive reaction to a tuberculosis skin test may be due to the BCG vaccine itself or due to infection with tuberculosis bacteria.
Tuberculosis blood tests IGRA (interferon gamma release assay), unlike the tuberculosis skin test, are not affected by prior BCG vaccination and are not expected to give a false-positive result in people who have received BCG.
For children under the age of five, the tuberculosis skin test is preferred over tuberculosis blood tests.
A positive tuberculosis skin test or tuberculosis blood test only tells that a person has been infected with tuberculosis bacteria. It does not tell whether the person has latent tuberculosis infection or has progressed to tuberculosis disease. Other tests, such as a chest x-ray and a sample of sputum, are needed to see whether the person has tuberculosis disease.
Tuberculosis testing during pregnancy
There is a greater risk to a pregnant woman and her baby if tuberculosis disease is not diagnosed and treated.
Tuberculosis skin testing is considered both valid and safe throughout pregnancy. Tuberculosis blood tests also are safe to use during pregnancy, but have not been evaluated for diagnosing tuberculosis infection in pregnant women. Other tests are needed to show if a person has tuberculosis disease.
How is tuberculosis treated?
Tuberculosis is completely curable if the correct drugs are taken for the correct length of time. Before drug treatment for tuberculosis nearly half of all persons with active tuberculosis died from it. Several antibiotics need to be taken over a number of months to prevent resistance developing to the tuberculosis drugs. The great majority of tuberculosis bacteria are sensitive to the antibiotics used (rifampicin, isoniazid, pyrazinamide and ethambutol). A minority of cases, 7.8% in the UK in 2013, are resistant to one of the first line antibiotics 2. Isoniazid and rifampicin are ineffective in 1% of cases. These cases are said to be of multi-drug resistant tuberculosis (MDR tuberculosis), which is harder to treat.
Tuberculosis bacteria grow very slowly and divide only occasionally when the antibiotics start to kill them, so treatment usually has to be continued for six months to ensure all active and dormant bacteria are killed and the person with tuberculosis is cured. People with pulmonary tuberculosis are usually not infectious after two weeks of treatment. Drug-resistant forms of the bacteria require treatment for longer than six months. Multi-drug resistant tuberculosis is particularly serious, requiring significantly prolonged (up to 24 months) treatment, with the infectious period lasting much longer.
In latent tuberculosis there are many thousand times fewer tuberculosis bacteria than in active tuberculosis. Treatment with a single drug (isoniazid) for six months, or two drugs (isoniazid and rifampicin) for a shorter time, is sufficient to kill most or all of the dormant bacteria, reducing the risk that the person will develop active tuberculosis later in their life.
Following tuberculosis treatment, the disease can return (relapse) in a small number of people, because not all bacteria have been killed. This is obviously much more likely if the course of treatment has been interrupted, not completed or otherwise not followed. However, it is also possible to catch tuberculosis a second time, unlike some other infectious diseases.
How to test for tuberculosis
There are two types of tests for tuberculosis infection: the tuberculosis skin test (PPD skin test or Mantoux test) and the tuberculosis blood test (interferon gamma release assay or IGRA). A person’s health care provider should choose which tuberculosis test to use. Factors in selecting which test to use include the reason for testing, test availability, and cost. Generally, it is not recommended to test a person with both a tuberculosis skin test and a tuberculosis blood test.
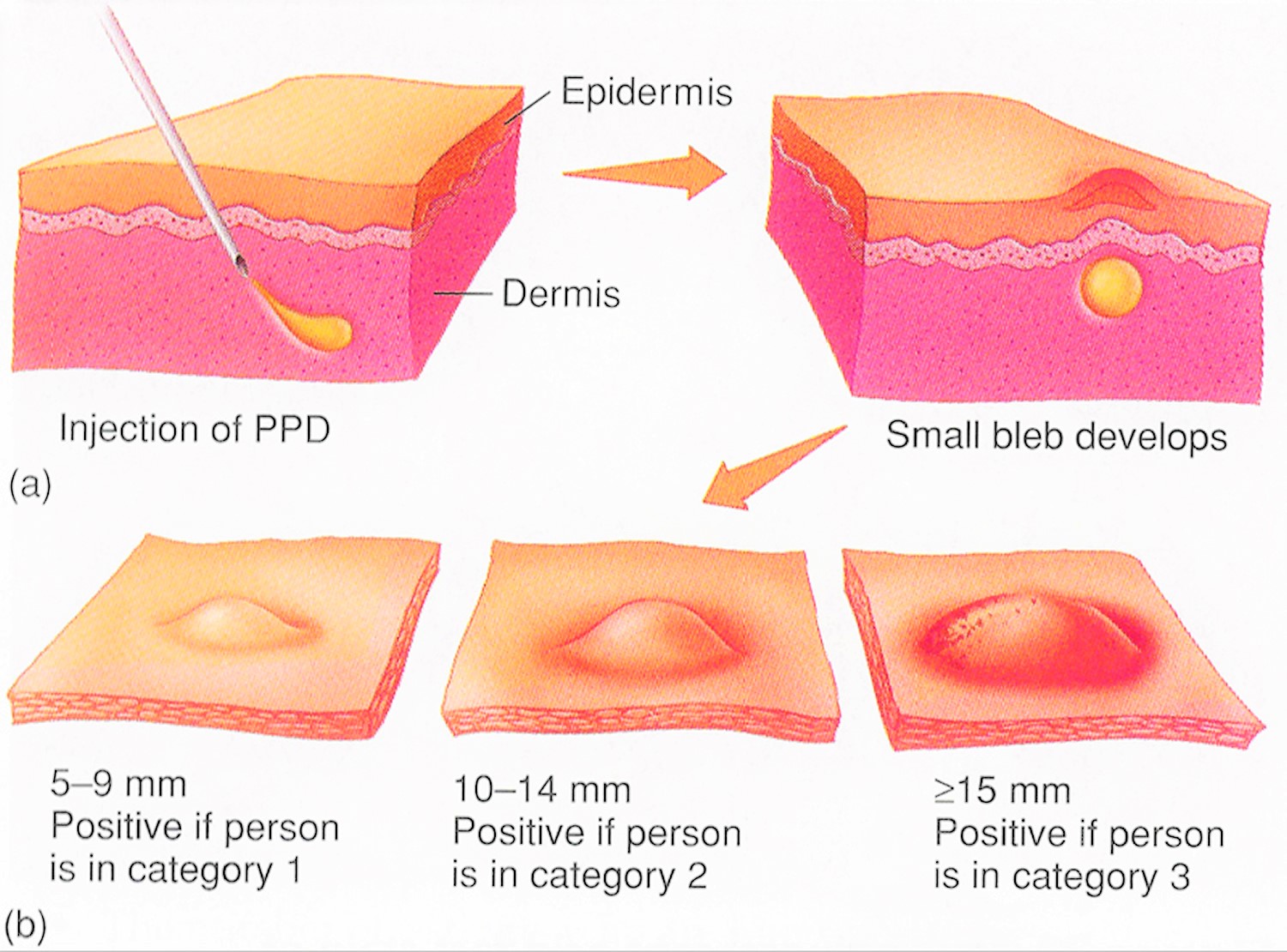
PPD skin test
The PPD (purified protein derivative) of tuberculosis bacteria skin test is also called the Mantoux test or the tuberculin skin test, involves injecting a small amount of PPD (purified protein derivative) of tuberculosis bacteria (tuberculin) into the skin of your forearm. Tuberculin is also called tuberculin PPD (purified protein derivative), is a solution of Mycobacterium tuberculosis complex antigens 3. PPD skin test, Mantoux test or tuberculin skin test, is a skin test to detect if you have been infected with tuberculosis bacteria (Mycobacterium tuberculosis). A PPD skin test or tuberculin skin test is used to screen for tuberculosis infection when someone has potentially been exposed to tuberculosis. PPD skin test is also used as a diagnostic tool when someone is showing symptoms of tuberculosis disease. The PPD skin test is conducted by injecting a small amount of testing fluid called tuberculin into the inside of your forearm and measuring the resulting swelling several days later. The PPD skin test material does not contain live bacteria and cannot cause tuberculosis. The test is undertaken by specially trained laboratory technicians and other healthcare workers.
- The PPD skin test is usually undertaken on the inner aspect of a forearm
- The selected area is first cleaned using an alcohol swab
- 0.1 ml tuberculin is injected intradermally, raising a bleb 6–10 mm in diameter
- A person given the tuberculin skin test must return within 48 to 72 hours to have a trained health care worker look for a reaction on the arm.
A tuberculin skin test or PPD skin test is used to detect exposure to tuberculosis bacteria by measuring your immune response to an inactivated or killed version of Mycobacterium tuberculosis.
A tuberculin skin test detects if a patient has ever been infected with tuberculosis bacteria (Mycobacterium tuberculosis) but does not determine if a patient currently has tuberculosis infection or tuberculosis disease. Further testing is required to confirm or rule-out a diagnosis of tuberculosis disease.
If you have had prior exposure to the tuberculosis bacteria (Mycobacterium tuberculosis), antibodies are formed and remain in your body. During the tuberculin purified protein derivative (PPD) skin test, the tuberculosis antigen (inactivated or killed version of Mycobacterium tuberculosis) is injected under your skin and if antibodies are present, your body will have an immune response. There will be an area of inflammation at the site of the injection. Reliable administration and reading of the tuberculin skin test requires standardization of procedures, training, supervision, and practice.
There are two tuberculosis-related conditions.
- The first is called tuberculosis infection or latent tuberculosis infection. Tuberculosis infection describes a stage of tuberculosis in which a person’s immune system is able to control the infection. Patients with tuberculosis infection or latent tuberculosis infection don’t become ill or spread tuberculosis to others, but may develop tuberculosis disease if left untreated.
- The second is referred to as tuberculosis disease, active tuberculosis, or reactivation tuberculosis. Tuberculosis disease occurs in 5 to 10% of people with tuberculosis infection. Patients with tuberculosis disease usually develop symptoms of tuberculosis and can spread tuberculosis to others.
A tuberculin skin test may be performed to screen for tuberculosis infections or to assist in diagnosing tuberculosis disease:
- Screening for tuberculosis infection: Screening for tuberculosis infection means testing for TB in a patient without symptoms. Screening is often conducted when someone has a high risk of having tuberculosis and would benefit from treatment if a tuberculosis infection is diagnosed.
- Diagnosing tuberculosis disease: Diagnostic tests are used when a patient has symptoms of tuberculosis. A positive tuberculin skin test supports a diagnosis of tuberculosis disease. In addition to the results of a tuberculin skin test, doctors consider a patient’s medical history and the results of a physical exam, imaging, and other lab tests to diagnose tuberculosis disease.
A tuberculin skin test requires two visits with a health care provider. On the first visit the tuberculin purified protein derivative (PPD) skin test is placed; on the second visit the health care provider reads the test result. A person given the tuberculin skin test must return within 48 to 72 hours to have a trained health care worker look for a reaction on the arm.
The tuberculin skin test is performed by injecting 0.1 ml of tuberculin purified protein derivative (PPD) into the inner surface of the forearm. The injection should be made with a tuberculin syringe, with the needle bevel facing upward. The tuberculin skin test is an intradermal injection. When placed correctly, the injection should produce a pale elevation of the skin (a wheal) 6 to 10 mm in diameter.
The tuberculin skin test reaction should be read between 48 and 72 hours after administration. A patient who does not return within 72 hours will need to be rescheduled for another tuberculin skin test as soon as possible.
The reaction should be measured in millimeters of the induration (palpable, raised, hardened area or swelling). The reader should not measure erythema (redness). The diameter of the indurated area should be measured across the forearm (perpendicular to the long axis).
The result of the tuberculin skin test depends on the size of the raised, hard area or swelling.
- Positive tuberculin skin test: This means the person’s body was infected with tuberculosis bacteria. Additional tests are needed to determine if the person has latent tuberculosis infection or tuberculosis disease. Other tests, such as a chest x-ray and a sample of sputum, are needed to see whether the person has tuberculosis disease.
- Negative tuberculin skin test: This means the person’s body did not react to the test, and that latent tuberculosis infection or tuberculosis disease is not likely.
There is no problem in repeating a tuberculosis skin test. If repeated, the additional test should be placed in a different location on the body (e.g., other arm).
The tuberculosis skin test is the preferred tuberculosis test for children under the age of five.
Figure 1. PPD skin test
The PPD skin test result depends on the size of the raised, hard area or swelling. The diameter of hard skin thickening (induration) is recorded in millimeters.
- Positive PPD skin test or abnormal (more than 5 mm induration): This means the person’s body was infected with tuberculosis bacteria. Abnormal tests may take weeks to subside and can leave a mark or scar.
- Additional tests are needed to determine if the person has latent tuberculosis infection or tuberculosis disease.
- Negative PPD skin test is classified as negative (no induration or less than 5 mm induration ): This means the person’s body did not react to the test, and that latent tuberculosis infection or tuberculosis disease is not likely. Or tuberculosis bacteria are not showing up in your body at this time. Sometimes the test may have been done too soon to show the tuberculosis bacteria.
- False negative results can occur due to anything reducing immunity, particularly co-infection with HIV but also treatments such as TNF-α antagonists. Extensive tuberculosis (pulmonary or miliary) can itself also temporarily depress the immunity, and can lead to a paradoxically negative PPD skin tests.
There is no problem in repeating a tuberculosis skin test. If repeated, the additional test should be placed in a different location on the body (e.g., other arm).
If your tuberculosis skin test is negative, you still may need to have more tests (diagnostic tests) if:
- You have been around someone with tuberculosis disease.
- Your tuberculosis skin test was within 8 weeks of your exposure to tuberculosis.
- You have signs of tuberculosis disease, like coughing, chest pain, fever, weight loss, or tiredness.
- You have HIV infection, since the tuberculosis skin test may not react the way it should.
Once you have a positive tuberculosis skin test you will always have a positive tuberculosis skin test, even if you complete treatment. Ask your doctor for a written record of your positive skin test result. This will be helpful if you are asked to have another tuberculosis skin test in the future.
Latent tuberculosis is where you’ve been infected with tuberculosis bacteria, but don’t have any symptoms. For example, you may need to have a test if you’ve been in close contact with someone known to have active tuberculosis disease involving the lungs, or if you’ve recently spent time in a country where tuberculosis levels are high. If you’ve just moved to the US from a country where tuberculosis is common, you should be given information and advice about the need for testing. Your doctor may suggest having a PPD tuberculin skin test when you register as a patient.
If you have a latent tuberculosis infection, your skin will be sensitive to PPD tuberculin and a small, hard red bump will develop at the site of the injection, usually within 48 to 72 hours of having the test.
- If you have a very strong skin reaction, you may need a chest X-ray to confirm whether you have active tuberculosis disease.
If you don’t have a latent infection, your skin won’t react to the PPD skin test. However, as tuberculosis can take a long time to develop, you may need to be screened again at a later stage.
Many people born outside of the United States have been given a vaccine called Bacille Calmette-Guérin (BCG). People who were previously vaccinated with Bacille Calmette-Guérin (BCG) may receive a tuberculosis skin test to test for tuberculosis infection. Vaccination with BCG may cause a false positive reaction to a PPD skin test, you may have a mild skin reaction to the PPD skin test. A positive reaction to a tuberculosis skin test may be due to the BCG vaccine itself or due to infection with tuberculosis bacteria.
PPD skin test (tuberculin skin test) should not be given within 1 month to patients who have received live vaccines. These vaccines include measles, mumps, rubella, oral polio, yellow fever, and varicella.
What does a positive tuberculosis test look like
Figure 2. Tuberculosis test pictures
Figure 3. Positive PPD skin test
Tuberculosis blood test
The usual tuberculosis blood test is interferon gamma release assay (IGRA). Two tuberculosis blood tests are approved by the U.S. Food and Drug Administration (FDA) and are available in the United States: the QuantiFERON®–TB Gold In-Tube test (QFT-GIT) and the T-SPOT®.tuberculosis test (T-Spot). One advantage of IGRA (interferon gamma release assay) tuberculosis blood test over skin testing is that it is not positive after BCG vaccination, unlike the PPD skin test (tuberculosis skin test). Tuberculosis blood tests are the preferred method of tuberculosis testing for people who have received the BCG vaccine. The interferon gamma release assay (IGRA) is a blood test for TB that’s becoming more widely available.
Advantages of tuberculosis blood test (IGRA):
- Requires a single patient visit to conduct the test.
- Results can be available within 24 hours.
- Does not boost responses measured by subsequent tests.
- Prior BCG (bacille Calmette-Guérin) vaccination does not cause a false-positive tuberculosis blood test (IGRA) test result.
Disadvantages and limitations of tuberculosis blood test (IGRA):
- A disadvantage of tuberculosis blood test is the difficulty and expense of conducting the test accurately.
- Blood samples must be processed within 8-30 hours after collection while white blood cells are still viable.
- Errors in collecting or transporting blood specimens or in running and interpreting the assay can decrease the accuracy of tuberculosis blood test (IGRA).
- Limited data on the use of tuberculosis blood test (IGRA) to predict who will progress to tuberculosis disease in the future.
A health care provider will draw a patient’s blood and send it to a laboratory for analysis and results.
Tuberculosis blood test results may be:
- Positive tuberculosis blood test: This means that the person has been infected with tuberculosis bacteria. Additional tests are needed to determine if the person has latent tuberculosis infection or tuberculosis disease.
- Negative tuberculosis blood test: This means that the person’s blood did not react to the test and that latent tuberculosis infection or tuberculosis disease is not likely.
- Indeterminate or borderline (uncertain).
Tuberculosis blood tests are the preferred tuberculosis test for:
- People who have received the tuberculosis vaccine bacille Calmette–Guérin (BCG).
- People who have a difficult time returning for a second appointment to look for a reaction to the PPD skin test.
Tuberculosis blood tests (interferon gamma release assay) may be used to help diagnose latent tuberculosis:
- if you have a positive PPD skin test (Mantoux test or tuberculin skin test)
- if you previously had the BCG vaccination – the PPD skin test (Mantoux test or tuberculin skin test) may not be reliable in these cases
- as part of your tuberculosis screening if you’ve just moved to the US from a country where tuberculosis is common
- as part of a health check when you register with a doctor
- if you’re about to have treatment that will suppress your immune system
- if you’re a healthcare worker
As with PPD skin test (tuberculin skin test), live virus vaccines (measles, mumps, rubella, oral polio, yellow fever, and varicella) might affect tuberculosis blood test (interferon gamma release assay) results. However, the effect of live virus vaccination on tuberculosis blood test (interferon gamma release assay) has not been studied. Until additional information is available, tuberculosis blood test (interferon gamma release assay) testing in the context of live virus vaccine administration should be done as follows:
- Either on the same day as vaccination with live-virus vaccine or 4-6 weeks after the administration of the live-virus vaccine
- At least one month after smallpox vaccination
Tuberculosis test results
Tuberculosis test positive
Positive tuberculosis PPD skin test or tuberculosis blood test only tells that a person has been infected with tuberculosis bacteria. It does not tell whether the person has latent tuberculosis infection or has progressed to tuberculosis disease. Other tests, such as a chest x-ray and a sample of sputum, are needed to see whether the person has tuberculosis disease.
- Positive PPD skin test or abnormal (more than 5 mm induration): This means the person’s body was infected with tuberculosis bacteria. Abnormal tests may take weeks to subside and can leave a mark or scar.
- Additional tests are needed to determine if the person has latent tuberculosis infection or tuberculosis disease.
- Positive tuberculosis blood test: This means that the person has been infected with tuberculosis bacteria. Additional tests are needed to determine if the person has latent tuberculosis infection or tuberculosis disease.
Tuberculosis test negative
- Negative PPD skin test is classified as negative (no induration or less than 5 mm induration ): This means the person’s body did not react to the test, and that latent tuberculosis infection or tuberculosis disease is not likely.
- Negative tuberculosis blood test: This means that the person’s blood did not react to the test and that latent tuberculosis infection or tuberculosis disease is not likely.
Who should be tested for tuberculosis
Certain people should be tested for tuberculosis infection because they are at higher risk for being infected with tuberculosis bacteria, including:
- People who have spent time with someone who has tuberculosis disease
- People from a country where tuberculosis disease is common (most countries in Latin America, the Caribbean, Africa, Asia, Eastern Europe, and Russia)
- People who live or work in high-risk settings (for example: correctional facilities, long-term care facilities or nursing homes, and homeless shelters)
- Health-care workers who care for patients at increased risk for tuberculosis disease
- Infants, children and adolescents exposed to adults who are at increased risk for latent tuberculosis infection or tuberculosis disease
Many people who have latent tuberculosis infection never develop tuberculosis disease. But some people who have latent tuberculosis infection are more likely to develop tuberculosis disease than others. Those at high risk for developing tuberculosis disease include:
- People with HIV infection
- People who became infected with tuberculosis bacteria in the last 2 years
- Babies and young children
- People who inject illegal drugs
- People who are sick with other diseases that weaken the immune system
- Elderly people
- People who were not treated correctly for tuberculosis in the past
Tuberculosis tests are generally not needed for people with a low risk of infection with tuberculosis bacteria.
Tuberculosis risk factors
Some people develop tuberculosis disease soon after becoming infected (within weeks) before their immune system can fight the tuberculosis bacteria. Other people may get sick years later, when their immune system becomes weak for another reason.
Overall, about 5 to 10% of infected persons who do not receive treatment for latent tuberculosis infection will develop tuberculosis disease (active tuberculosis infection) at some time in their lives. For persons whose immune systems are weak, especially those with HIV infection, the risk of developing tuberculosis disease (active tuberculosis infection) is much higher than for persons with normal immune systems.
Generally, persons at high risk for developing tuberculosis disease (active tuberculosis infection) fall into two categories:
- Persons who have been recently infected with tuberculosis bacteria
- Persons with medical conditions that weaken the immune system
Persons who have been recently infected with tuberculosis bacteria
This includes:
- Close contacts of a person with infectious tuberculosis disease
- Persons who have immigrated from areas of the world with high rates of tuberculosis
- Children less than 5 years of age who have a positive tuberculosis test
- Groups with high rates of tuberculosis transmission, such as homeless persons, injection drug users, and persons with HIV infection
- Persons who work or reside with people who are at high risk for tuberculosis in facilities or institutions such as hospitals, homeless shelters, correctional facilities, nursing homes, and residential homes for those with HIV
Persons with medical conditions that weaken the immune system
Babies and young children often have weak immune systems. Other people can have weak immune systems, too, especially people with any of these conditions:
- HIV infection (the virus that causes AIDS)
- Substance abuse
- Silicosis
- Diabetes mellitus
- Severe kidney disease
- Low body weight
- Organ transplants
- Head and neck cancer
- Medical treatments such as corticosteroids or organ transplant
- Specialized treatment for rheumatoid arthritis or Crohn’s disease
Diagnosing latent tuberculosis infection & tuberculosis disease
Most persons, but not everyone, with tuberculosis disease have one or more symptoms of tuberculosis disease. All persons with either symptoms or a positive tuberculosis test result should be evaluated for tuberculosis disease. If a person has symptoms, but a negative tuberculosis test result, they should still be evaluated for tuberculosis disease.
Diagnosis of latent tuberculosis infection
A diagnosis of latent tuberculosis infection is made if a person has a positive tuberculosis test result and a medical evaluation does not indicate tuberculosis disease. The decision about treatment for latent tuberculosis infection will be based on a person’s chances of developing tuberculosis disease by considering their risk factors.
Diagnosis of tuberculosis disease (active tuberculosis infection)
Tuberculosis disease (active tuberculosis infection) is diagnosed by medical history, physical examination, chest x-ray, and other laboratory tests. Tuberculosis disease (active tuberculosis infection) is treated by taking several drugs as recommended by a health care provider.
Tuberculosis disease (active tuberculosis infection) should be suspected in persons who have any of the following symptoms:
- Unexplained weight loss
- Loss of appetite
- Night sweats
- Fever
- Fatigue
If tuberculosis disease (active tuberculosis infection) is in the lungs (pulmonary), symptoms may include:
- Coughing for longer than 3 weeks
- Hemoptysis (coughing up blood)
- Chest pain
If tuberculosis disease (active tuberculosis infection) is in other parts of the body (extrapulmonary), symptoms will depend on the area affected.
People suspected of having tuberculosis disease should be referred for a complete medical evaluation, which will include the following:
1. Medical History
Clinicians should ask about the patient’s history of tuberculosis exposure, infection, or disease. It is also important to consider demographic factors (e.g., country of origin, age, ethnic or racial group, occupation) that may increase the patient’s risk for exposure to tuberculosis or to drug-resistant tuberculosis. Also, clinicians should determine whether the patient has medical conditions, such as HIV infection or diabetes, that increase the risk of latent tuberculosis infection progressing to tuberculosis disease.
2. Physical Examination
A physical exam can provide valuable information about the patient’s overall condition and other factors that may affect how tuberculosis is treated, such as HIV infection or other illnesses.
3. Test for tuberculosis Infection
The PPD tuberculin skin test (Mantoux test) or the tuberculosis blood test (interferon gamma release assay or IGRA) can be used to test for Mycobacterium tuberculosis infection. Additional tests are required to confirm tuberculosis disease.
4. Chest Radiograph
A posterior-anterior chest radiograph is used to detect chest abnormalities. Lesions may appear anywhere in the lungs and may differ in size, shape, density, and cavitation. These abnormalities may suggest tuberculosis, but cannot be used to definitively diagnose tuberculosis. However, a chest radiograph may be used to rule out the possibility of pulmonary tuberculosis in a person who has had a positive reaction to a PPD skin or tuberculosis blood test and no symptoms of disease.
5. Diagnostic Microbiology
The presence of acid-fast-bacilli (AFB) on a sputum smear or other specimen often indicates tuberculosis disease. Acid-fast microscopy is easy and quick, but it does not confirm a diagnosis of tuberculosis because some acid-fast-bacilli are not M. tuberculosis. Therefore, a culture is done on all initial samples to confirm the diagnosis. (However, a positive culture is not always necessary to begin or continue treatment for tuberculosis.) A positive culture for Mycobacterium tuberculosis confirms the diagnosis of tuberculosis disease. Culture examinations should be completed on all specimens, regardless of acid-fast-bacilli (AFB) smear results. Laboratories should report positive results on smears and cultures within 24 hours by telephone or fax to the primary health care provider and to the state or local tuberculosis control program, as required by law.
6. Drug Resistance
For all patients, the initial Mycobacterium tuberculosis isolate should be tested for drug resistance. It is crucial to identify drug resistance as early as possible to ensure effective treatment. Drug susceptibility patterns should be repeated for patients who do not respond adequately to treatment or who have positive culture results despite 3 months of therapy. Susceptibility results from laboratories should be promptly reported to the primary health care provider and to the state or local tuberculosis control program.
Tuberculosis test side effects
You should not receive PPD skin test if you have had an allergic reaction to a previous tuberculin skin test. You should not receive PPD skin test if you have extensive skin burns or eczema or if you have active tuberculosis or history of treatment for tuberculosis.
Along with its needed effects, PPD skin test may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Pregnancy Category C (all Trimesters): Animal studies have shown an adverse effect and there are no adequate studies in pregnant women OR no animal studies have been conducted and there are no adequate studies in pregnant women.
Studies in women suggest that PPD skin test poses minimal risk to the infant when used during breastfeeding.
Check with your doctor or nurse immediately if any of the following side effects occur:
Incidence not known
- bleeding at the injection site (occurring up to 3 days after the skin test)
- blistering, crusting, or scabbing at the injection site
- cough
- deep, dark purple bruise at the injection site (occurring up to 3 days after the skin test)
- difficult or labored breathing
- dizziness
- fainting
- fast heartbeat
- fever
- hard lump at the injection site
- hives
- itching, pain, redness, or swelling at the injection site
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- noisy breathing
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- scar at the injection site
- unusual tiredness or weakness
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Incidence not known
- pain, discomfort, or itching at the injection site
- redness or rash at the injection site (occurring within 12 hours after skin test)
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
- Latent TB Infection and TB Disease. https://www.cdc.gov/tb/topic/basics/tbinfectiondisease.htm[↩]
- Public Health England. Tuberculosis in the UK 2014 report. Public Health England; London: 2014.[↩]
- Furin J. Advances in the diagnosis, treatment, and prevention of tuberculosis in children. Expert Rev Respir Med. 2019 Mar;13(3):301-311[↩]