Contents
Upper respiratory infection
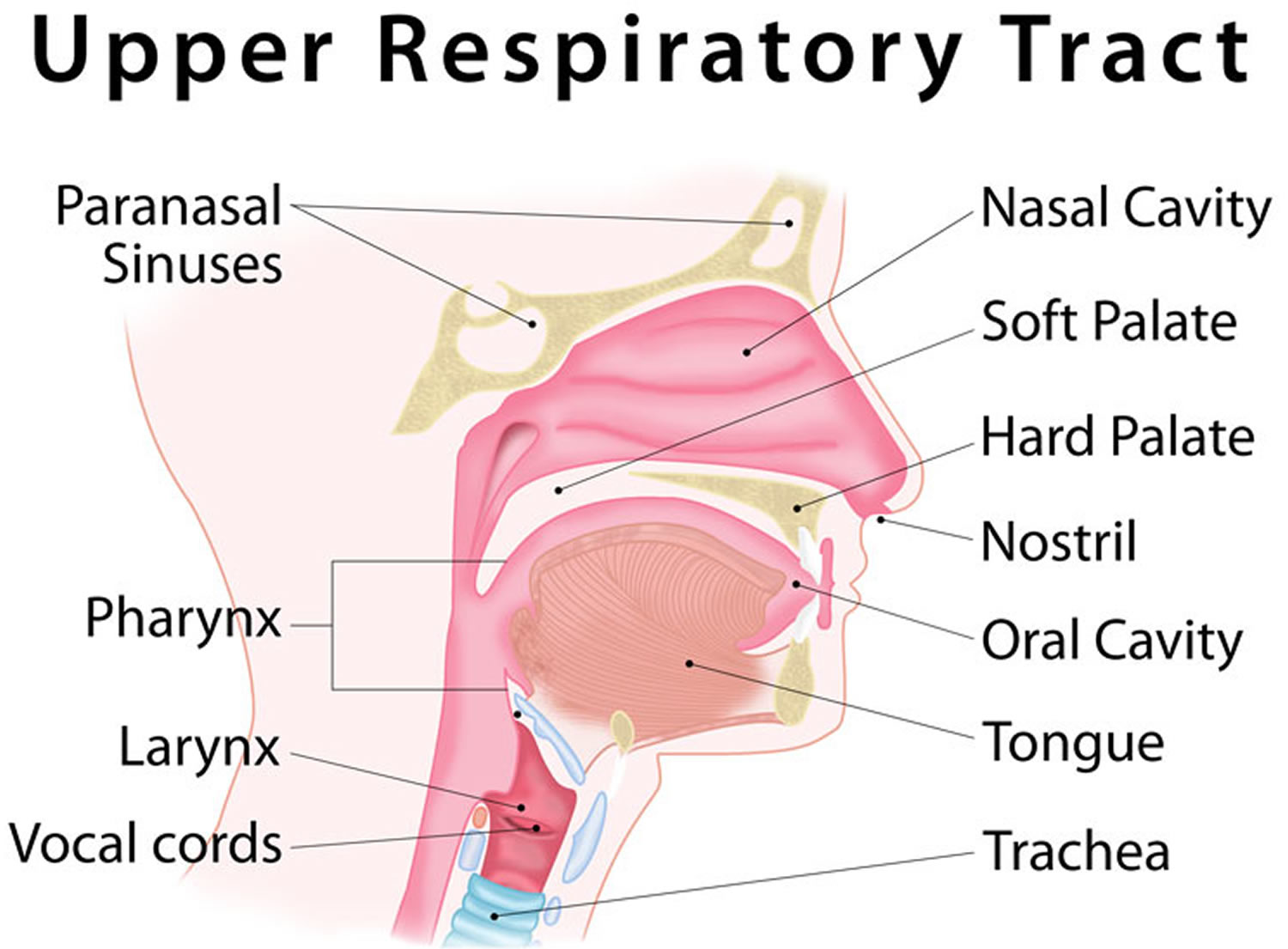
Upper respiratory tract infection also called “URTI”, upper respiratory infection (URI) or “the common cold” is an infection of the nose, sinuses (sinusitis), throat (pharyngitis), epiglottis (epiglottitis) or larynx and trachea (laryngotracheitis). Defining most of these upper respiratory infection diseases is difficult because the presentations connected with upper respiratory tract infections (URIs) commonly overlap and their causes are similar. Upper respiratory infections are usually caused by several families of virus; these are the rhinovirus, coronavirus, parainfluenza, respiratory syncytial virus (RSV), adenovirus, human metapneumovirus and influenza 1, that is spread by coughs, sneezes, and direct contact. These cause a variety of patient diseases including acute bronchitis, the common cold, influenza, and respiratory distress syndromes 2. Occasionally the enterovirus is implicated in summer. Recently, the newly discovered bocavirus (related to the parvovirus) has also been linked to upper respiratory infection 3. The common cold is the most frequent kind of upper respiratory infection. The flu and sinus infections are other kinds of upper respiratory infections.
The term upper respiratory tract infection is probably a misnomer as it incorrectly implies an absence of lower respiratory tract symptoms. Upper respiratory tract infection (URTI) occurs commonly in both children and adults and is a major cause of mild illness. Upper respiratory tract infections account for an estimated 10 million outpatient appointments a year. Adults get a common cold around two to three times yearly whereas children can have up to eight cases yearly 4. Respiratory infections are more common in the fall and winter when school starts and indoor crowding facilitates transmission. Fall months see a peak in incidence of common cold caused by the rhinovirus. Upper respiratory tract infections are accountable for greater than 20 million missed days of school and greater than 20 million days of work lost, thus generating a large economic burden 5.
Infections of the respiratory tract are grouped according to their symptomatology and anatomic involvement. Acute upper respiratory infections (URI) include the common cold, pharyngitis, epiglottitis, and laryngotracheitis. These infections are usually benign, transitory and self-limited, although epiglottitis and laryngotracheitis can be serious diseases in children and young infants.
Almost all upper respiratory infections are caused by viruses, so antibiotics won’t cure them. But you can do things at home to help your child get better. With most upper respiratory infections, your child should feel better in 4 to 10 days.
Figure 1. Upper respiratory infection
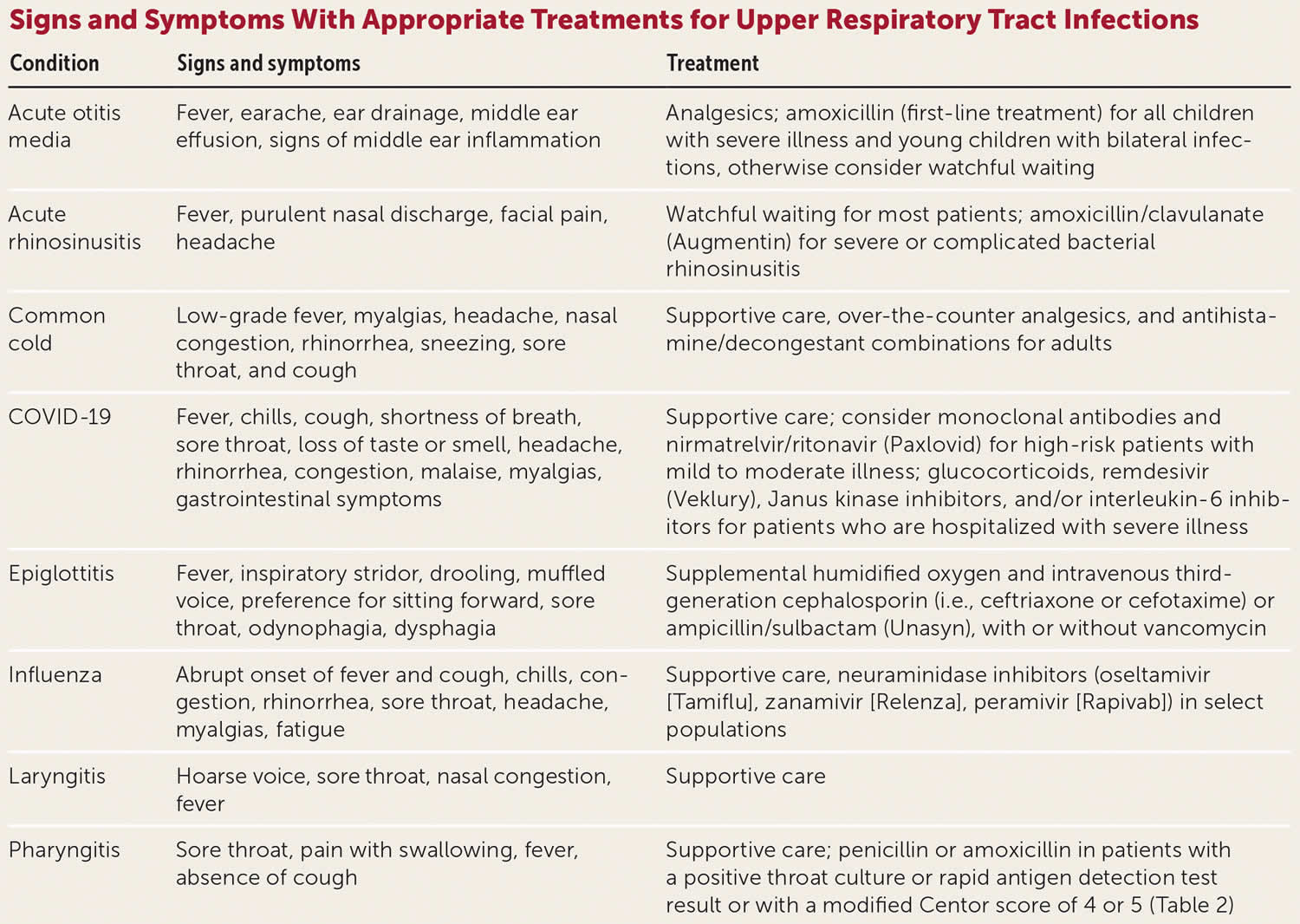
Figure 2. Upper respiratory infections treatment guidelines
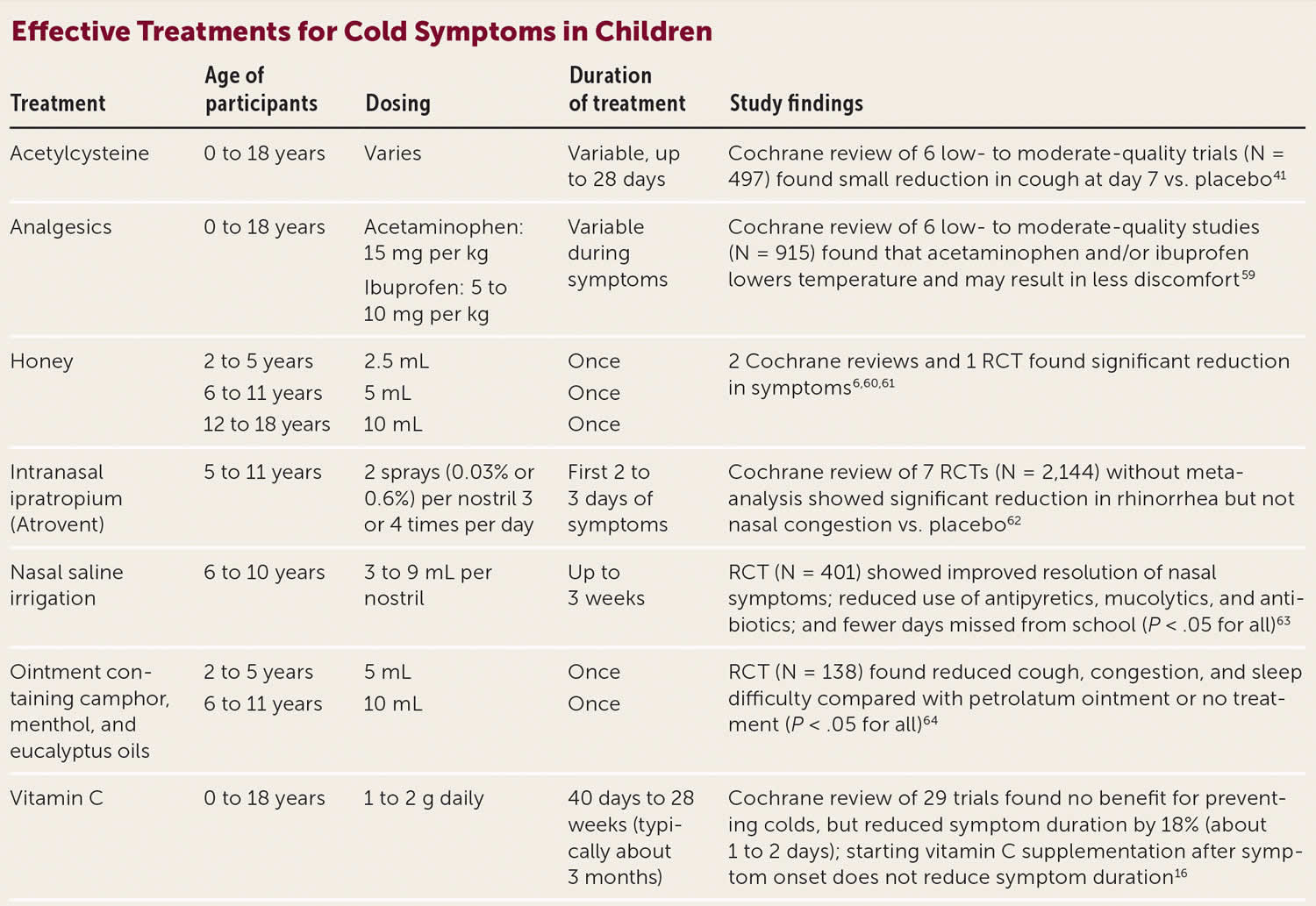
[Source 6 ]Figure 3. Effective treatments for cold symptoms in children
[Source 6 ]See a doctor if you have an upper respiratory infection and:
- you feel very unwell or your symptoms get worse
- you cough up blood or bloodstained mucus
- you have had a cough for more than 3 weeks
- you’re pregnant
- you’re over 65
- you have a weakened immune system – for example, because you have a condition like diabetes or you’re having chemotherapy
- you have a long-term health condition, such as a heart, lung or kidney condition
You may have pneumonia if your symptoms are severe.
Call your local emergency services number anytime you think your child may need emergency care. For example, call if:
- Your child has severe trouble breathing. Symptoms may include:
- Using the belly muscles to breathe.
- The chest sinking in or the nostrils flaring when your child struggles to breathe.
Call your doctor or nurse call line now or seek immediate medical care if:
- Your child has new or worse trouble breathing.
- Your child has a new or higher fever.
- Your child seems to be getting much sicker.
- Your child has a new rash.
Watch closely for changes in your child’s health, and be sure to contact your doctor if:
- Your child is coughing more deeply or more often, especially if you notice more mucus or a change in the color of the mucus.
- Your child has a new symptom, such as a sore throat, an earache, or sinus pain.
- Your child is not getting better as expected.
What are antibiotics?
Antibiotics are medicines that can fight or prevent bacterial infections. Upper respiratory infections are caused by two types of germs—bacteria and viruses. Antibiotics do not work against infections caused by a virus. A virus causes most coughs, colds, sore throats, and sinus infections. When you have a virus, ask your doctor what you can do to feel better. For example, if you have common cold caused by rhinovirus, respiratory syncytial virus (RSV), influenza virus, parainfluenza virus, adenovirus or enterovirus 7, treatments in adults are limited to over-the-counter analgesics, zinc, nasal decongestants with or without antihistamines, and ipratropium for cough 8. The American Academy of Pediatrics Choosing Wisely recommendation states that cough and cold medicines should be avoided for respiratory illness in children younger than four years 9. And the only established safe and effective treatments for children are acetylcysteine, honey (for children one year and older), nasal saline irrigation, intranasal ipratropium, and topical application of ointment containing camphor, menthol, and eucalyptus oils 8.
The majority of acute upper respiratory infections (URIs) are caused by viruses and the use of antibiotic treatment is ineffective, inappropriate and potentially harmful 10, 11. However, proven upper respiratory infection caused by Group A Streptococcal disease (Strep throat) and pertussis (whooping cough) should be treated with antibiotic therapy. Symptomatic treatment for acute upper respiratory infections should be directed to maximize relief of the most prominent symptom(s).
How do antibiotics work?
Antibiotics kill off the weaker bacteria the first few times you take them. At first you will start to feel better. However, the stronger bacteria are still alive. If you stop taking these medicines too soon (as soon as you start to feel better), the stronger bacteria can keep growing, and the antibiotic won’t work anymore.
When do I need antibiotics?
You need antibiotics to stop an infection caused by bacteria, such as Strep throat (Group A Streptococcal disease), pertussis (whooping cough) and some sinus and ear infections (see Figure 2).
Upper respiratory infection causes
Most upper respiratory infections are caused by viruses, such as rhinovirus, coronavirus, parainfluenza, respiratory syncytial virus (RSV), adenovirus, human metapneumovirus and influenza. Bacteria may cause roughly 15% of sudden onset pharyngitis presentations. The most common is Streptococcus pyogenes, a Group A streptococcus 12. Epiglottitis and laryngotracheitis are likely caused by Haemophilus influenzae type b 2. Haemophilus influenzae type b vaccine is commercially available and is now a basic component of childhood immunization program. These organisms gain entry to the respiratory tract by inhalation of droplets and invade the upper respiratory mucosa. Epithelial destruction may ensue, along with redness, edema, hemorrhage and sometimes an exudate.
Influenza
The incubation period for influenza is 1 to 4 days, and the time interval between symptom onset is estimated to be 3 to 4 days. Viral shedding can occur 1 day before the onset of symptoms. It is believed that influenza can be transferred among humans by direct contact, indirect contact, droplets, or aerosolization. Short distances (<1 meter) are generally required for contact and droplet transmission to occur between the source person and the susceptible individual. Airborne transmission may occur over longer distances (>1 m). Most evidence-based data suggest that direct contact and droplet transfer are the predominant modes of transmission for influenza 13.
Common Cold
Common colds are the most prevalent entity of all respiratory infections and are the leading cause of patient visits to the physician, as well as work and school absenteeism. Most colds are caused by viruses. The pathogens responsible for causing the common cold include rhinovirus, adenovirus, parainfluenza virus, respiratory syncytial virus, enterovirus, and coronavirus. The rhinovirus with more than 100 serotypes, a species of the Enterovirus genus of the Picornaviridae family, is the most common cause of the common cold and causes up to 80% of all respiratory infections during peak seasons 14. Dozens of rhinovirus serotypes and frequent antigenic changes among them make identification, characterization, and eradication complex. After deposition in the anterior nasal mucosa, rhinovirus replication and infection are thought to begin upon mucocilliary transport to the posterior nasopharynx and adenoids. As soon as 10 to 12 hours after inoculation, symptoms may begin. The mean duration of symptoms is 7 to 10 days, but symptoms can persist for as long as 3 weeks. Nasal mucosal infection and the host’s subsequent inflammatory response cause vasodilation and increased vascular permeability. These events result in nasal obstruction and rhinorrhea whereas cholinergic stimulation prompts mucus production and sneezing.
Coronaviruses may be responsible for more than 10% of cases. Parainfluenza viruses, respiratory syncytial virus, adenoviruses and influenza viruses have all been linked to the common cold syndrome. All of these organisms show seasonal variations in incidence. The cause of 30% to 40% of cold syndromes has not been determined.
Sinusitis
Sinusitis is an acute inflammatory condition of one or more of the paranasal sinuses. Infection plays an important role in this affliction. Sinusitis often results from infections of other sites of the respiratory tract since the paranasal sinuses are contiguous to, and communicate with, the upper respiratory tract.
Acute sinusitis most often follows a common cold which is usually of viral origin. Vasomotor and allergic rhinitis may also precede to the development of sinusitis. Obstruction of the sinusal ostia due to deviation of the nasal septum, presence of foreign bodies, polyps or tumors can predispose to sinusitis. Infection of the maxillary sinuses may follow dental extractions or an extension of infection from the roots of the upper teeth. The most common bacterial agents responsible for acute sinusitis are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Other organisms including Staphylococcus aureus, Streptococcus pyogenes, gram-negative organisms and anaerobes have also been recovered. Chronic sinusitis is commonly a mixed infection of aerobic and anaerobic organisms.
Infections caused by viruses or bacteria impair the ciliary activity of the epithelial lining of the sinuses and increased mucous secretions. This leads to obstruction of the paranasal sinusal ostia which impedes drainage. With bacterial multiplication in the sinus cavities, the mucus is converted to mucopurulent exudates. The pus further irritates the mucosal lining causing more edema, epithelial destruction and ostial obstruction. When acute sinusitis is not resolved and becomes chronic, mucosal thickening results and the development of mucoceles and polyps may ensue.
Pharyngitis
Pharyngitis is an inflammation of the pharynx involving lymphoid tissues of the posterior pharynx and lateral pharyngeal bands. The etiology can be bacterial, viral and fungal infections as well as noninfectious etiologies such as smoking. Most cases are due to viral infections and accompany a common cold or influenza. Type A coxsackieviruses can cause a severe ulcerative pharyngitis in children (herpangina), and adenovirus and herpes simplex virus, although less common, also can cause severe pharyngitis. Pharyngitis is a common symptom of Epstein-Barr virus and cytomegalovirus infections.
Group A beta-hemolytic streptococcus or Streptococcus pyogenes is the most important bacterial agent associated with acute pharyngitis and tonsillitis. Corynebacterium diphtheriae causes occasional cases of acute pharyngitis, as do mixed anaerobic infections (Vincent’s angina), Corynebacterium haemolyticum, Neisseria gonorrhoeae, and Chlamydia trachomatis. Outbreaks of Chlamydia pneumoniae causing pharyngitis or pneumonitis have occurred in military recruits. Mycoplasma pneumoniae and Mycoplasma hominis have been associated with acute pharyngitis. Candida albicans, which causes oral candidiasis or thrush, can involve the pharynx, leading to inflammation and pain.
As with common cold, viral pathogens in pharyngitis appear to invade the mucosal cells of the nasopharynx and oral cavity, resulting in edema and hyperemia of the mucous membranes and tonsils. Bacteria attach to and, in the case of group A beta-hemolytic streptococci, invade the mucosa of the upper respiratory tract. Many clinical manifestations of infection appear to be due to the immune reaction to products of the bacterial cell. In diphtheria, a potent bacterial exotoxin causes local inflammation and cell necrosis.
Epiglottitis and Laryngotracheitis
Inflammation of the upper airway is classified as epiglottitis or laryngotracheitis (croup) on the basis of the location, clinical manifestations, and pathogens of the infection. Haemophilus influenzae type b is the most common cause of epiglottitis, particularly in children age 2 to 5 years. Epiglottitis is less common in adults. Some cases of epiglottitis in adults may be of viral origin. Most cases of laryngotracheitis are due to viruses. More serious bacterial infections have been associated with H influenzae type b, group A beta-hemolytic streptococcus and C diphtheriae. Parainfluenza viruses are most common but respiratory syncytial virus, adenoviruses, influenza viruses, enteroviruses and Mycoplasma pneumoniae have been implicated.
A viral upper respiratory infection may precede infection with H influenzae in episodes of epiglottitis. However, once H influenzae type b infection starts, rapidly progressive erythema and swelling of the epiglottis ensue, and bacteremia is usually present. Viral infection of laryngotracheitis commonly begins in the nasopharynx and eventually moves into the larynx and trachea. Inflammation and edema involve the epithelium, mucosa and submucosa of the subglottis which can lead to airway obstruction.
The syndrome of epiglottitis begins with the acute onset of fever, sore throat, hoarseness, drooling, dysphagia and progresses within a few hours to severe respiratory distress and prostration. The clinical course can be fulminant and fatal. The pharynx may be inflamed, but the diagnostic finding is a “cherry-red” epiglottis.
A history of preceding cold-like symptoms is typical of laryngotracheitis, with rhinorrhea, fever, sore throat and a mild cough. Tachypnea, a deep barking cough and inspiratory stridor eventually develop. Children with bacterial tracheitis appear more ill than adults and are at greater risk of developing airway obstruction.
Haemophilus influenzae type b is isolated from the blood or epiglottis in the majority of patients with epiglottis; therefore a blood culture should always be performed. Sputum cultures or cultures from pharyngeal swabs may be used to isolate pathogens in patients with laryngotracheitis. Serologic studies to detect a rise in antibody titers to various viruses are helpful for retrospective diagnosis. Newer, rapid diagnostic techniques, using immunofluorescent-antibody staining to detect virus in sputum, pharyngeal swabs, or nasal washings, have been successfully used. Enzyme-linked immunosorbent assay (ELISA), DNA probe and polymerase chain reaction procedures for detection of viral antibody or antigens are now available for rapid diagnosis.
Upper respiratory infection prevention
To keep your respiratory system (and especially your lungs) healthy:
- don’t smoke
- avoid harmful environmental factors such as smoke, dusts and chemicals
- exercise (check with your doctor first if you have a health condition), preferably away from busy roads with high air-pollution
- wash your hands regularly to prevent infections
- eat a healthy, vitamin-rich diet
- drink plenty of water
- introduce plants into your living spaces
- practise good hygiene
- consider having the flu vaccine each year
Upper respiratory infection signs and symptoms
Initial symptoms of a cold are runny, stuffy nose and sneezing, usually without fever. Other upper respiratory infections may have fever. Children with epiglottitis may have difficulty in breathing, muffled speech, drooling and stridor. Children with serious laryngotracheitis (croup) may also have tachypnea, stridor and cyanosis.
Acute upper respiratory tract infections include rhinitis, pharyngitis, tonsillitis, and laryngitis. Symptoms of upper respiratory infections commonly include:
- Cough – you may bring up mucus (phlegm)
- Sore throat
- Runny nose
- Nasal congestion
- Breathlessness, tight chest or wheezing
- Headaches
- Low-grade fever
- Facial pressure
- Sneezing
- Malaise
- Myalgias (muscle aches)
- Feeling generally unwell
The onset of symptoms usually begins one to three days after exposure and lasts 7–10 days, and can persist up to 3 weeks.
Upper respiratory infection complications
Complications of upper respiratory tract infections are relatively rare, except with influenza. Complications of influenza infection include primary influenza viral pneumonia; secondary bacterial pneumonia; sinusitis; otitis media; coinfection with bacterial agents; and exacerbation of preexisting medical conditions, particularly asthma and chronic obstructive pulmonary disease. Pneumonia is one of the most common complications of influenza illness in children and contributes significantly to morbidity and mortality.
Upper respiratory infection treatment
Most upper respiratory infections pass within 1 to 2 weeks. You can usually treat your symptoms at home. Viral infections are treated symptomatically. Epiglottitis is a medical emergency, especially in children. All children with this diagnosis should be observed carefully and be intubated to maintain an open airway as soon as the first sign of respiratory distress is detected. Antibacterial therapy should be directed at H influenzae. Patients with croup are usually successfully managed with close observation and supportive care, such as fluid, humidified air, and racemic epinephrine. For prevention, Haemophilus influenzae type b conjugated vaccine is recommended for all pediatric patients, as is immunization against diphtheria. Streptococcal pharyngitis and epiglottitis caused by Haemophilus influenzae are treated with antibacterials.
Most upper respiratory infections go away in a few days. Some things you can do to take care of yourself with an upper respiratory infection include:
- Get plenty of rest
- Drink lots of water to loosen any mucus and make it easier to cough up
- Drink a hot lemon and honey drink to help soothe a cough (not suitable for babies)
- Gargle with warm salty water if you have a sore throat (children shouldn’t try this)
- Use an air humidifier or inhale steam from a bowl of hot water (adults only) – you can add menthol or eucalyptus oil
- Raise your head up while sleeping using extra pillows to make breathing easier and clear your chest of mucus
- Use painkillers to bring down a fever and help ease a sore throat, headaches and muscle pain
- Over-the-counter (OTC) cold and cough medicines may help ease symptoms in adults and older children. They do not make your cold go away faster, but can help you feel better. These OTC medicines are not recommended for children under age 4.
- Antibiotics should not be used to treat a common cold.
- Many alternative treatments have been tried for colds, such as vitamin C, zinc supplements, and echinacea. Talk to your health care provider before trying any herbs or supplements.
DON’T
- DO NOT let children breathe in steam from a bowl of hot water as there’s a risk of scalding
- DO NOT give aspirin to children under 16
- DO NOT smoke – it can make your symptoms worse
Medicine for upper respiratory infection
Analgesics (pain relievers) such as nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., ibuprofen) have been shown to reduce headache, ear pain, muscle pain, joint pain, and sneezing but do not improve cough, cold duration, or total symptom score 15. Ibuprofen is more effective than acetaminophen (paracetamol) for reducing fever-related discomfort 16. Acetaminophen (paracetamol) may provide short-term relief of runny nose (rhinorrhea) and nasal obstruction but has no effect on sore throat, malaise, sneezing, or cough 17.
Nasal decongestants (oral and intranasal) may relieve nasal congestion, but there is no evidence that they reduce cough 18. Topical oxymetazoline, which is included in many over-the-counter intranasal decongestants, reduces the duration and severity of nasal congestion after multiple doses 19. Patients should be warned about the risk of rhinitis when intranasal oxymetazoline is used for more than three days 20.
Combination antihistamine medications such as antihistamines combined with oral decongestants and/or analgesics may provide some relief of cold symptoms, although the effect on cough is limited 21, 22, 23. Anti-histamines (H1-receptor antagonists) may offer a modest reduction of rhinorrhea (runny nose) and sneezing during the first 2 days of a cold treatment in adults 24, 25. First-generation antihistamines are sedating, so advise the patient about caution during their use. Topical and oral nasal decongestants (i.e., topical oxymetazoline, oral pseudoephedrine) have moderate benefit in adults and adolescents in reducing nasal airway resistance 26. When started on the first day of symptoms, medications containing ibuprofen and pseudoephedrine may reduce the severity of cold symptoms 27. Antihistamine monotherapy is not effective for relieving cough 21, 22.
Evidence-based data does not support the use of antibiotics in the treatment of the common cold because they do not improve symptoms or shorten the course of illness 26. There is also a lack of convincing evidence supporting the use of dextromethorphan for acute cough.
Intranasal ipratropium is the only medication that improves persistent cough related to upper respiratory infection in adults 28, 29. Inhaled ipratropium in combination with albuterol improves cough during the first 10 days of treatment, but there is no benefit at 20 days compared with placebo 30.
According to a Cochrane Review 31, 32, vitamin C used as daily prophylaxis at doses of 200 milligrams or more had a “modest but consistent effect” on the duration and severity of common cold symptoms (8% and 14% decreases in duration for adults and children, respectively). In children, 1 to 2 gram/day vitamin C shortened colds by 18% 32. The severity of colds was also reduced by regular vitamin C administration 32. When taken therapeutically after the onset of symptoms, however, high-dose vitamin C has not shown clear benefit in trials 31, 32.
Neither steam nor vitamin D supplementation improves symptoms of the common cold 16, 33, 34. Vitamin E can actually make symptoms worse in older adults aged 60 years or older 35. Although echinacea was previously thought to provide benefit, high-quality studies have not shown that echinacea reduces the duration or severity of cold symptoms 36, 37, 38, 39. Based on low-quality evidence, Pelargonium sidoides (South African geranium) does not shorten time to resolution of cold symptoms in adults 40.
Early antiviral treatment for influenza infection shortens the duration of influenza symptoms, decreases the length of hospital stays, and reduces the risk of complications. Recommendations for the treatment of influenza are updated frequently by the Centers for Disease Control and Prevention based on epidemiologic data and antiviral resistance patterns. Give antiviral therapy for influenza within 48 hours of symptom onset (or earlier), and do not delay treatment for laboratory confirmation if a rapid test is not available. Antiviral treatment can provide benefit even after 48 hours in pregnant and other high-risk patients 41.
Vaccination is the most effective method of preventing influenza illness. Antiviral chemoprophylaxis is also helpful in preventing influenza (70% to 90% effective) and should be considered as an adjunct to vaccination in certain scenarios or when vaccination is unavailable or not possible. Generally, antiviral chemoprophylaxis is used during periods of influenza activity for (1) high-risk persons who cannot receive vaccination (due to contraindications) or in whom recent vaccination does not, or is not expected to, afford a sufficient immune response; (2) controlling outbreaks among high-risk persons in institutional settings; and (3) high-risk persons with influenza exposures 42.
How you can care for your child at home
Safe and effective treatment options for symptoms of the common cold in children vary somewhat from those for adults (see Figure 3). Nasal saline irrigation, analgesics, and time are the mainstays of treatment for upper respiratory infections in children. Avoid cough preparations in children 26.
To help your child cope with a cough or cold:
- Give your child acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) for fever, pain, sore throat or fussiness. Although ibuprofen and acetaminophen reduce fever-related discomfort, ibuprofen may be more effective 43. If you give your child a pain reliever, follow the dosing guidelines carefully. Always read and follow all instructions on the label. Alternating these medications may reduce daycare absences in children with fever. For children younger than 3 months old, don’t give acetaminophen until your baby has been seen by a doctor. Don’t give ibuprofen to a child younger than 6 months old or to children who are vomiting constantly or are dehydrated. Also, use caution when giving aspirin to children or teenagers. Though aspirin is approved for use in children older than age 3, children and teenagers recovering from chickenpox or flu-like symptoms should never take aspirin. This is because aspirin has been linked to Reye’s syndrome, a rare but potentially life-threatening condition, in such children.
- Acetylcysteine. The mucolytic acetylcysteine may safely decrease cough after six to seven days in children two years and older 44.
- Intranasal ipratropium may decrease runny nose (rhinorrhea) but not nasal congestion related to upper respiratory infections in children five years and older. It should not be used in children younger than five years. The main adverse effects are nosebleeds, nasal dryness, and headache, although these are self-limited 45.
- Nasal saline irrigation. Over-the-counter saline can keep nasal passages moist and loosen mucus. Rinsing your child’s nasal passages with saline (nasal irrigation) is a quick and effective way to relieve nasal congestion. One large trial found that children who use saline nasal washes six times per day have faster resolution of nasal secretions and nasal obstruction and reduced use of antipyretics, decongestants, and antibiotics 46. This regimen also reduces school absences. Saline irrigation solutions can be purchased ready-made or as kits to add to water. You can also use a homemade solution. Look for a squeeze bottle or a neti pot — a small container with a spout designed for nose rinsing — at your pharmacy or health food store. To make up the saline irrigation solution, do not use tap water, as it can contain organisms that could cause infection. Use water that’s distilled or sterile. You can also use water that was boiled and cooled. Another option is using water that has been filtered using a filter with an absolute pore size of 1 micron or smaller. To prevent infections, wash the bottle or pot with hot soapy water and rinse it after every use and leave it open to air-dry. Do not share a container with other people.
- In younger children, apply saline nasal drops, wait for a short period and then use a suction bulb to draw mucus out of each nostril.
- For older children, use a saline nasal spray or saline nasal irrigation.
- Complementary and alternative treatments. Application of ointment containing camphor, menthol, and eucalyptus oils on the chest and neck of children at bedtime can relieve nasal congestion and reduce nighttime cough frequency and severity, improving sleep for both the child and parents 47. The use of menthol alone may also improve perceived nasal patency but may not help with cough 48. Menthol is safe for use in children two years and older. The use of honey before bedtime may also reduce the frequency and severity of cough 49, 50. Honey should not be given to children younger than 12 months because of the risk of exposure to botulinum spores.
- Be careful with cough and cold medicines. Don’t give them to children younger than 6, because they don’t work for children that age and can even be harmful. For children 6 and older, always follow all the instructions carefully. Make sure you know how much medicine to give and how long to use it. And use the dosing device if one is included.
- Be careful when giving your child over-the-counter cold or flu medicines and Tylenol at the same time. Many of these medicines have acetaminophen, which is Tylenol. Read the labels to make sure that you are not giving your child more than the recommended dose. Too much acetaminophen (Tylenol) can be harmful.
- Over-the-counter cough and cold medicines are intended to treat the symptoms of coughs and colds, not the underlying disease. Research suggests that these medicines haven’t been proved to work any better than inactive medicine (placebo). More important, these medications have potentially serious side effects, including fatal overdoses in children younger than 2 years old.
- Don’t use over-the-counter medicines, except for fever reducers and pain relievers, to treat coughs and colds in children younger than 6 years old. Also, consider avoiding use of these medicines for children younger than 12 years old.
- Make sure your child rests. Keep your child at home if he or she has a fever.
- Run a cool-mist humidifier. Place a humidifier near your child’s bed or close to your child. This can add moisture to the air, which might decrease the drying of the nasal passages and throat. This may make it easier for your child to breathe. Follow the directions for cleaning the machine. Clean the humidifier after every use.
- Keep your child away from smoke. Do not smoke or let anyone else smoke around your child or in your house.
- Wash your hands and your child’s hands regularly so that you don’t spread the disease.
- Give your child lots of fluids, enough so that the urine is light yellow or clear like water. This is very important if your child is vomiting or has diarrhea. Liquids such as water, juice and broth might help thin secretions. Give your child sips of water or drinks such as Pedialyte or Gastrolyte. These drinks contain a mix of salt, sugar, and minerals. You can buy them at drugstores or grocery stores. Give these drinks as long as your child is throwing up or has diarrhea. Do not use them as the only source of liquids or food for more than 12 to 24 hours. Warm liquids, such as tea or chicken soup, might have a soothing effect, increase the flow of nasal mucus and loosen respiratory secretions.
- Offer cold or frozen drinks or foods. Ice cream, frozen fruit pops, ice or cold beverages might feel good on a sore throat.
- Encourage gargling with salt water. For children age 6 years and older, gargling with warm salt water might soothe throat pain.
- Offer hard candy. For children age 5 years and older, sucking on a piece of hard candy might soothe throat pain. Hard candy is probably as effective as medicated lozenges and less likely to have harmful effects. However, hard candy is a choking hazard and shouldn’t be given to younger children.
What about antibiotics?
Antibiotics can be used to combat bacterial infections but have no effect on viruses, which cause colds. If your child has a cold, antibiotics won’t help. Remember, the more your child uses antibiotics, the more likely he or she is to get sick with an antibiotic-resistant infection in the future.
Is codeine OK?
No. The Food and Drug Administration (FDA) limits the use of prescription cough and cold medicines containing the opioids codeine or hydrocodone to adults age 18 and older. This is due to the potential for slowed or difficult breathing, misuse, risky use, addiction, overdose and even death.
- Cotton M, Innes S, Jaspan H, Madide A, Rabie H. Management of upper respiratory tract infections in children. S Afr Fam Pract (2004). 2008;50(2):6–12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3098742[↩]
- Thomas M, Bomar PA. Upper Respiratory Tract Infection. [Updated 2018 Nov 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532961[↩][↩]
- Human bocavirus. Allander T. J Clin Virol. 2008 Jan; 41(1):29-33.[↩]
- Simasek M, Blandino DA. Treatment of the common cold. Am Fam Physician. 2007 Feb 15;75(4):515-20 [↩]
- Adams PF, Hendershot GE, Marano MA., Centers for Disease Control and Prevention/National Center for Health Statistics. Current estimates from the National Health Interview Survey, 1996. Vital Health Stat 10. 1999 Oct;(200):1-203[↩]
- Antibiotic Use in Acute Upper Respiratory Tract Infections. Am Fam Physician. 2022;106(6):628-636. https://www.aafp.org/pubs/afp/issues/2022/1200/antibiotics-upper-respiratory-tract-infections.html[↩][↩]
- Kirkpatrick GL. The common cold. Prim Care. 1996 Dec;23(4):657-75. doi: 10.1016/s0095-4543(05)70355-9[↩]
- DeGeorge KC, Ring DJ, Dalrymple SN. Treatment of the Common Cold. Am Fam Physician. 2019 Sep 1;100(5):281-289. https://www.aafp.org/pubs/afp/issues/2019/0901/p281.html[↩][↩]
- Choosing Wisely. Cough and cold medicines should not be prescribed, recommended or used for respiratory illnesses in young children. https://www.choosingwisely.org/clinician-lists/american-academy-pediatrics-cough-and-cold-medicines-for-children-under-four/[↩]
- Hersh AL, Shapiro DJ, Pavia AT, Shah SS. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011 Dec;128(6):1053-61. doi: 10.1542/peds.2011-1337[↩]
- Avoid prescribing antibiotics for upper respiratory infections. Infectious Diseases Society of America February 23, 2015. https://www.choosingwisely.org/clinician-lists/infectious-diseases-society-antbiotics-for-upper-respiratory-infections/?highlight=upper%20respiratory%20infection[↩]
- Dasaraju PV, Liu C. Infections of the Respiratory System. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 93. Available from: https://www.ncbi.nlm.nih.gov/books/NBK8142[↩]
- Brankston G, Gitterman L, Hirji Z, Lemieux C, Gardam M. Transmission of influenza A in human beings. Lancet Infect Dis. 2007 Apr;7(4):257-65[↩]
- Heikkinen T, Järvinen A. The common cold. Lancet. 2003 Jan 04;361(9351):51-9[↩]
- Kim SY, Chang YJ, Cho HM, Hwang YW, Moon YS. Non-steroidal anti-inflammatory drugs for the common cold. Cochrane Database Syst Rev. 2015 Sep 21;2015(9):CD006362. doi: 10.1002/14651858.CD006362.pub4[↩]
- Little P, Moore M, Kelly J, Williamson I, Leydon G, McDermott L, Mullee M, Stuart B; PIPS Investigators. Ibuprofen, paracetamol, and steam for patients with respiratory tract infections in primary care: pragmatic randomised factorial trial. BMJ. 2013 Oct 25;347:f6041. doi: 10.1136/bmj.f6041[↩][↩]
- Li S, Yue J, Dong BR, Yang M, Lin X, Wu T. Acetaminophen (paracetamol) for the common cold in adults. Cochrane Database Syst Rev. 2013 Jul 1;2013(7):CD008800. doi: 10.1002/14651858.CD008800.pub2[↩]
- Deckx L, De Sutter AI, Guo L, Mir NA, van Driel ML. Nasal decongestants in monotherapy for the common cold. Cochrane Database Syst Rev. 2016 Oct 17;10(10):CD009612. doi: 10.1002/14651858.CD009612.pub2[↩]
- Reinecke S, Tschaikin M. Untersuchung der Wirksamkeit von Oxymetazolin auf die Rhinitisdauer. Ergebnisse einer plazebokontrollierten Doppelblindstudie bei akuter Rhinitis [Investigation of the effect of oxymetazoline on the duration of rhinitis. results of a placebo-controlled double-blind study in patients with acute rhinitis]. MMW Fortschr Med. 2005 Oct 6;147 Suppl 3:113-8. German.[↩]
- Dykewicz MS, Fineman S, Skoner DP, Nicklas R, Lee R, Blessing-Moore J, Li JT, Bernstein IL, Berger W, Spector S, Schuller D. Diagnosis and management of rhinitis: complete guidelines of the Joint Task Force on Practice Parameters in Allergy, Asthma and Immunology. American Academy of Allergy, Asthma, and Immunology. Ann Allergy Asthma Immunol. 1998 Nov;81(5 Pt 2):478-518. doi: 10.1016/s1081-1206(10)63155-9[↩]
- Smith SM, Schroeder K, Fahey T. Over-the-counter (OTC) medications for acute cough in children and adults in community settings. Cochrane Database Syst Rev. 2014 Nov 24;2014(11):CD001831. doi: 10.1002/14651858.CD001831.pub5[↩][↩]
- De Sutter AI, van Driel ML, Kumar AA, Lesslar O, Skrt A. Oral antihistamine-decongestant-analgesic combinations for the common cold. Cochrane Database Syst Rev. 2012 Feb 15;(2):CD004976. doi: 10.1002/14651858.CD004976.pub3. Update in: Cochrane Database Syst Rev. 2022 Jan 21;1:CD004976[↩][↩]
- Irwin RS, Baumann MH, Bolser DC, Boulet LP, Braman SS, Brightling CE, Brown KK, Canning BJ, Chang AB, Dicpinigaitis PV, Eccles R, Glomb WB, Goldstein LB, Graham LM, Hargreave FE, Kvale PA, Lewis SZ, McCool FD, McCrory DC, Prakash UBS, Pratter MR, Rosen MJ, Schulman E, Shannon JJ, Hammond CS, Tarlo SM. Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest. 2006 Jan;129(1 Suppl):1S-23S[↩]
- Arroll B. Common cold. BMJ Clin Evid. 2008 Jun 09;2008[↩]
- Sterrantino C, Duarte G, Costa J, Vaz-Carneiro A. Análise da Revisão Cochrane: Antihistamínicos para a Constipação. Cochrane Database Syst Rev. 2015;11:CD009345 [Analysis of the Cochrane Review: Antihistamines for the Common Cold. Cochrane Database Syst Rev. 2015;11:CD009345]. Acta Med Port. 2016 Mar;29(3):164-7. Portuguese. doi: 10.20344/amp.7526[↩]
- Fashner J, Ericson K, Werner S. Treatment of the common cold in children and adults. Am Fam Physician. 2012 Jul 15;86(2):153-9[↩][↩][↩]
- Klimek L, Schumacher H, Schütt T, Gräter H, Mueck T, Michel MC. Factors associated with efficacy of an ibuprofen/pseudoephedrine combination drug in pharmacy customers with common cold symptoms. Int J Clin Pract. 2017 Feb;71(2):e12907. doi: 10.1111/ijcp.12907[↩]
- Holmes PW, Barter CE, Pierce RJ. Chronic persistent cough: use of ipratropium bromide in undiagnosed cases following upper respiratory tract infection. Respir Med. 1992 Sep;86(5):425-9. doi: 10.1016/s0954-6111(06)80010-7[↩]
- Bolser DC. Cough suppressant and pharmacologic protussive therapy: ACCP evidence-based clinical practice guidelines. Chest. 2006 Jan;129(1 Suppl):238S-249S. doi: 10.1378/chest.129.1_suppl.238S[↩]
- Zanasi A, Lecchi M, Del Forno M, Fabbri E, Mastroroberto M, Mazzolini M, Pisani L, Pandolfi P, Nava S, Morselli-Labate AM. A randomized, placebo-controlled, double-blind trial on the management of post-infective cough by inhaled ipratropium and salbutamol administered in combination. Pulm Pharmacol Ther. 2014 Dec;29(2):224-32. doi: 10.1016/j.pupt.2014.07.008[↩]
- Douglas RM, Hemilä H, Chalker E, Treacy B. Vitamin C for preventing and treating the common cold. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD000980[↩][↩]
- Hemilä H, Chalker E. Vitamin C for preventing and treating the common cold. Cochrane Database Syst Rev. 2013 Jan 31;2013(1):CD000980. doi: 10.1002/14651858.CD000980.pub4[↩][↩][↩][↩]
- Singh M, Singh M, Jaiswal N, Chauhan A. Heated, humidified air for the common cold. Cochrane Database Syst Rev. 2017 Aug 29;8(8):CD001728. doi: 10.1002/14651858.CD001728.pub[↩]
- Murdoch DR, Slow S, Chambers ST, Jennings LC, Stewart AW, Priest PC, Florkowski CM, Livesey JH, Camargo CA, Scragg R. Effect of vitamin D3 supplementation on upper respiratory tract infections in healthy adults: the VIDARIS randomized controlled trial. JAMA. 2012 Oct 3;308(13):1333-9. doi: 10.1001/jama.2012.12505[↩]
- Graat JM, Schouten EG, Kok FJ. Effect of daily vitamin E and multivitamin-mineral supplementation on acute respiratory tract infections in elderly persons: a randomized controlled trial. JAMA. 2002 Aug 14;288(6):715-21. doi: 10.1001/jama.288.6.715[↩]
- Karsch-Völk M, Barrett B, Kiefer D, Bauer R, Ardjomand-Woelkart K, Linde K. Echinacea for preventing and treating the common cold. Cochrane Database Syst Rev. 2014 Feb 20;2014(2):CD000530. doi: 10.1002/14651858.CD000530.pub3[↩]
- Barrett BP, Brown RL, Locken K, Maberry R, Bobula JA, D’Alessio D. Treatment of the common cold with unrefined echinacea. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2002 Dec 17;137(12):939-46. doi: 10.7326/0003-4819-137-12-200212170-00006[↩]
- Woelkart K, Linde K, Bauer R. Echinacea for preventing and treating the common cold. Planta Med. 2008 May;74(6):633-7. doi: 10.1055/s-2007-993766[↩]
- Yale SH, Liu K. Echinacea purpurea therapy for the treatment of the common cold: a randomized, double-blind, placebo-controlled clinical trial. Arch Intern Med. 2004 Jun 14;164(11):1237-41. doi: 10.1001/archinte.164.11.1237[↩]
- Timmer A, Günther J, Motschall E, Rücker G, Antes G, Kern WV. Pelargonium sidoides extract for treating acute respiratory tract infections. Cochrane Database Syst Rev. 2013 Oct 22;(10):CD006323. doi: 10.1002/14651858.CD006323.pub3[↩]
- Siston AM, Rasmussen SA, Honein MA, Fry AM, Seib K, Callaghan WM, Louie J, Doyle TJ, Crockett M, Lynfield R, Moore Z, Wiedeman C, Anand M, Tabony L, Nielsen CF, Waller K, Page S, Thompson JM, Avery C, Springs CB, Jones T, Williams JL, Newsome K, Finelli L, Jamieson DJ., Pandemic H1N1 Influenza in Pregnancy Working Group. Pandemic 2009 influenza A(H1N1) virus illness among pregnant women in the United States. JAMA. 2010 Apr 21;303(15):1517-25[↩]
- Harper SA, Bradley JS, Englund JA, File TM, Gravenstein S, Hayden FG, McGeer AJ, Neuzil KM, Pavia AT, Tapper ML, Uyeki TM, Zimmerman RK., Expert Panel of the Infectious Diseases Society of America. Seasonal influenza in adults and children–diagnosis, treatment, chemoprophylaxis, and institutional outbreak management: clinical practice guidelines of the Infectious Diseases Society of America. Clin. Infect. Dis. 2009 Apr 15;48(8):1003-32[↩]
- Wong T, Stang AS, Ganshorn H, Hartling L, Maconochie IK, Thomsen AM, Johnson DW. Combined and alternating paracetamol and ibuprofen therapy for febrile children. Cochrane Database Syst Rev. 2013 Oct 30;2013(10):CD009572. doi: 10.1002/14651858.CD009572.pub2[↩]
- Chalumeau M, Duijvestijn YC. Acetylcysteine and carbocysteine for acute upper and lower respiratory tract infections in paediatric patients without chronic broncho-pulmonary disease. Cochrane Database Syst Rev. 2013 May 31;(5):CD003124. doi: 10.1002/14651858.CD003124.pub4[↩]
- AlBalawi ZH, Othman SS, Alfaleh K. Intranasal ipratropium bromide for the common cold. Cochrane Database Syst Rev. 2013 Jun 19;2013(6):CD008231. doi: 10.1002/14651858.CD008231.pub3[↩]
- Slapak I, Skoupá J, Strnad P, Horník P. Efficacy of isotonic nasal wash (seawater) in the treatment and prevention of rhinitis in children. Arch Otolaryngol Head Neck Surg. 2008 Jan;134(1):67-74. doi: 10.1001/archoto.2007.19[↩]
- Paul IM, Beiler JS, King TS, Clapp ER, Vallati J, Berlin CM Jr. Vapor rub, petrolatum, and no treatment for children with nocturnal cough and cold symptoms. Pediatrics. 2010 Dec;126(6):1092-9. doi: 10.1542/peds.2010-1601[↩]
- Kenia, P., Houghton, T. and Beardsmore, C. (2008), Does inhaling menthol affect nasal patency or cough?. Pediatr. Pulmonol., 43: 532-537. https://doi.org/10.1002/ppul.20797[↩]
- Paul IM, Beiler J, McMonagle A, Shaffer ML, Duda L, Berlin CM Jr. Effect of honey, dextromethorphan, and no treatment on nocturnal cough and sleep quality for coughing children and their parents. Arch Pediatr Adolesc Med. 2007 Dec;161(12):1140-6. doi: 10.1001/archpedi.161.12.1140[↩]
- Oduwole O, Udoh EE, Oyo-Ita A, Meremikwu MM. Honey for acute cough in children. Cochrane Database Syst Rev. 2018 Apr 10;4(4):CD007094. doi: 10.1002/14651858.CD007094.pub5[↩]