Contents
- What is uterus pain ?
- How Do Doctors Narrow the Diagnosis to Focus on Important Common Conditions of Pelvic Pain ?
What is uterus pain ?
Pain in the uterus area (uterus pain) is commonly called pelvic pain – which is pain in the lowest part of your abdomen and pelvis 1.
Pelvic pain is a general term used to describe pain that occurs mostly or only in the region below a woman’s belly button. This region includes the lower stomach, lower back, buttocks, and genital area 2.
Pelvic pain is chronic if it lasts for more than 6 months and affects a woman’s quality of life 3. This condition is a common reason why women seek medical care 4.
There are many possible causes of pelvic pain, and it may be difficult to figure out the specific cause or causes 2. A woman’s pelvic pain may result from multiple causes occurring all at the same time. In many cases, pelvic pain indicates a problem with one or more of the organs in the pelvic area, such as the uterus, vagina, intestine, bladder or from musculoskeletal sources. Problems may include infection, inflammation, or conditions such as endometriosis. And a woman with one chronic pain condition is at increased risk for other types of chronic pain.
The intensity of a woman’s pelvic pain may not relate to the severity of the problem or condition causing the pain 5. For example, a woman with only small areas of endometriosis may experience intense pain.
How many women have pelvic pain ?
Researchers are not sure exactly how many women in the United States have chronic pelvic pain.
Because it is often linked to other disorders, such as endometriosis or vulvodynia, chronic pelvic pain may be misdiagnosed as another condition, making it difficult to estimate reliable prevalence rates for pelvic pain 6. According to one study, about 15% of women of childbearing age in the United States reported having pelvic pain that lasted at least 6 months 7. Worldwide, the rates of chronic pelvic pain for women of childbearing age range from 14% to 32% 7. Between 13% and 32% of these women have pain that is severe enough to cause them to miss work 8.
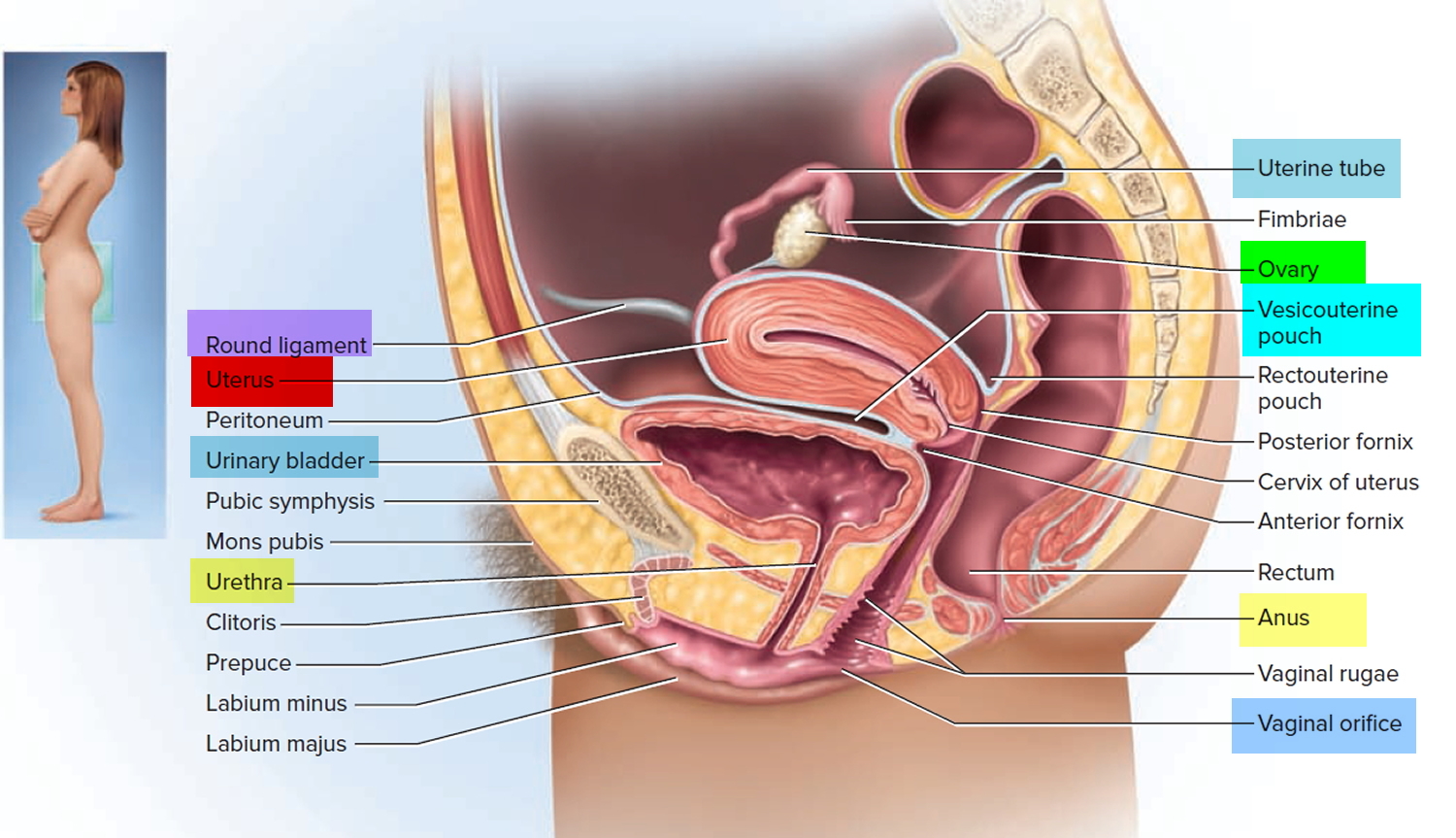
Figure 1. Uterus anatomy and location
Uterus pain causes
Depending on its source, pelvic pain can be dull or sharp; it might be constant or off and on (intermittent); and it might be mild, moderate or severe. Pelvic pain can sometimes radiate to your lower back, buttocks or thighs. Sometimes, you might notice pelvic pain only at certain times, such as when you urinate or during sexual activity.
Pelvic pain can occur suddenly, sharply and briefly (acute) or over the long term (chronic). Chronic pelvic pain refers to any constant or intermittent pelvic pain that has been present for six months or more.
Several types of diseases and conditions can cause pelvic pain. Chronic pelvic pain can result from more than one condition.
Pelvic pain can arise from your digestive, reproductive or urinary system. Recently, doctors have recognized that some pelvic pain, particularly chronic pelvic pain, can also arise from muscles and connective tissue (ligaments) in the structures of the pelvic floor. Occasionally, pelvic pain might be caused by irritation of nerves in the pelvis.
Female reproductive system
Pelvic pain arising from the female reproductive system might be caused by conditions such as:
- Adenomyosis
- Ectopic pregnancy (or other pregnancy-related conditions)
- Endometriosis
- Menstrual cramps (dysmenorrhea)
- Miscarriage (before the 20th week) or intrauterine fetal death
- Mittelschmerz (ovulation pain)
- Ovarian cancer
- Ovarian cysts
- Pelvic inflammatory disease (PID)
- Salpingitis (inflammation of the fallopian tubes)
- Uterine fibroids
- Vulvodynia
Other causes in women (and men):
Examples of other possible causes of pelvic pain — in women (and men) — include:
- Appendicitis
- Crohn’s disease
- Chronic constipation
- Colon cancer
- Diverticulitis
- Intestinal obstruction
- Enlarged spleen (splenomegaly)
- Fibromyalgia
- Inguinal hernia
- Interstitial cystitis (also called painful bladder syndrome)
- Kidney stones
- Past physical or sexual abuse
- Pelvic floor muscle spasms
- Prostatitis
- Psychological factors
- Ulcerative colitis
The following problems can cause or contribute to pelvic pain:
Adhesions
Adhesions are bands of scar tissue that form between internal tissues and organs 2, 3. They can form as a result of surgery or infections, such as pelvic inflammatory disease. There is disagreement about whether adhesions can cause pain. It has been proposed that pain may occur when adhesions prevent normal movement of internal organs, such as the bowel.3
Endometriosis
Endometriosis is condition that occurs when tissues that normally grow inside the uterus grow somewhere else in the body, usually in other parts of the pelvis, such as on the outside of the uterus, ovaries, or fallopian tubes (uterine tubes). The two most common symptoms of endometriosis are pain and infertility.
Interstitial cystitis/painful bladder syndrome
Interstitial cystitis/painful bladder syndrome is associated with pain in the region of the bladder as well as the need to urinate frequently and urgently 9. This pain may be a burning or sharp pain in the bladder or at the opening where urine leaves the body (urethra), and it is often relieved by emptying the bladder.
Irritable bowel syndrome
Irritable bowel syndrome (IBS) is a digestive problem that can cause pain, bloating, constipation, or diarrhea. Researchers have yet to find a specific cause for irritable bowel syndrome but stress or certain foods can trigger symptoms in some people 10.
Pelvic floor disorders
Pelvic floor disordersoccur when the muscles and connective tissues that hold the pelvic organs in place weaken or are injured, such as may occur during childbirth. These organs include the uterus, bladder, and rectum. Pelvic floor disorders can cause discomfort as well as functional problems, such as the uncontrolled loss of urine (urinary incontinence) or stool (fecal incontinence). With pelvic floor disorders, pain may also be caused by spasms or an increase in pelvic floor muscle tone.
Uterine fibroids
Uterine fibroids consist of an overgrowth of muscle cells within the wall of the uterus. These noncancerous tumors may cause heavy, irregular, or painful periods and local pressure symptoms, including frequent urination, trouble defecating, and lower back pain.
Vulvodynia
Vulvodynia is a condition that involves pain or discomfort of the vulva (the external female genitalia)), especially during intercourse. The pain may range from sharp pain to burning to itching. Although the vulvar pain is outside the pelvis, health care providers who see patients with pelvic pain may also care for patients with this disorder.
What are the symptoms of pelvic pain ?
Although pain is the core symptom of pelvic pain, the specifics of that pain and other symptoms vary from woman to woman. Pelvic pain can be severe enough that it interferes with normal activities, such as going to work, exercising, or having sex.
Women describe pelvic pain in many ways. Pelvic pain can be steady, or it can come and go. It can be a sharp and stabbing pain felt in a specific spot, or a dull pain that is spread out. Some women have pain that occurs only during their menstrual periods. Some women feel pain when they need to use the bathroom, and some feel pain when lifting something heavy. Some women have pain in the vulva (the external genitals), which is called vulvodynia, during sex or when inserting a tampon 11, 3.
How is pelvic pain diagnosed ?
To find out the cause of a woman’s pain, her health care provider will 2:
- Ask questions about the woman’s pain and health history. How a woman describes her pain can help her health care provider figure out the pain type and what might be causing it.
- Perform a physical exam. The health care provider will examine the abdomen and pelvis, and check the woman’s organs, muscles, and tissues in the pelvic region for tenderness or abnormalities that suggest a pain disorder.
The information the doctor gathers from the questions and physical exam will help the doctor decide whether additional tests or procedures are needed to help diagnose the cause of the pelvic pain. These tests or procedures may include 2, 12:
- Lab tests, such as blood work or a urine test
- Pelvic ultrasound, a procedure that uses sound waves to look at organs and structures inside the pelvic region3
- Pelvic laparoscopy, a minor surgery in which the doctor inserts a viewing instrument called a laparoscope through a small cut in the skin below the belly button to look inside the pelvis4
- Pelvic MRI (magnetic resonance imaging) scan, an imaging test that uses powerful magnets and radio waves to create pictures of the pelvis5
- Cystoscopy, looking into the bladder by inserting a viewing instrument6
- Colonoscopy, looking into the bowel by inserting a viewing instrument7
Finding the cause of pelvic pain can be challenging and can take time. Some women must check with more than one doctor or with a specialist to get help for their pain. Sometimes, the cause of the pain is not found. But failure to locate the cause does not mean that the pain a woman feels is not real or that it cannot be treated 2. Understanding what triggers the pain also can be helpful.
How is pelvic pain treated ?
Treatment depends on the cause of pelvic pain, how intense the pain is, and how often the pain occurs. No single treatment approach has been shown to be better than another in all cases 13.
Some treatment options include:
- Medicines. Many types of medicine are used to treat pelvic pain. These include pain relievers that are swallowed or injected, muscle relaxants, and antidepressants 9, 10.
- Hormonal treatment. Hormones can help pain related to endometriosis and menstruation 14. These include hormones that are swallowed, injected, or placed in the uterus, such as birth control pills, gonadotropin-releasing hormone injections, or progestin-releasing intrauterine devices. Hormonal treatment for pelvic pain is not the same as hormone therapy that is sometimes used to treat the symptoms of menopause.
- Lifestyle changes. Some women’s pain is helped by changes in diet, improved posture, and regular physical activity.
- Physical therapy. Some types of pain, such as muscle and connective tissue pain, respond well to physical therapy. This type of therapy might involve massage, stretching, strengthening, or learning to relax or control pelvic muscles 3.
- Surgery. Some women may need surgery to remove adhesions,6fibroids, and/or endometriosis. In some cases, the surgery might also reduce or relieve pelvic pain. Some women may have surgery to cut or destroy nerves to interrupt pain signals,1 but such pain surgeries often are not successful. Depending on the cause of the pain, a woman’s health care provider might recommend a hysterectomy, surgery to remove a woman’s uterus, to help relieve or reduce pelvic pain.
- Counseling. Counseling or “talk therapy” may help treat pain. In fact, talk therapy, when combined with medical treatment, appears to work better for improving some symptoms than does medical treatment alone.1
Finding a treatment that works can take time. Some women want to try alternative therapies to relieve their pain. Learning healthy ways to cope with pain is an important aspect of any treatment approach.
Can there be more than one reason for your pain ?
Yes. Studies have found a good deal of overlap among pain conditions 13, 15. For instance, a woman may have endometriosis, irritable bowel syndrome, and depression at the same time—each of which may contribute to the overall pain she feels.
Having more than one pain condition can complicate diagnosis and treatment. To be effective, treatment needs to address all the conditions that are contributing to your uterus pain.
Can pelvic pain affect your ability to become pregnant ?
Some pelvic conditions that are associated with pain also are associated with difficulty getting pregnant.
These include:
- Endometriosis. Up to 30% to 50% of women with endometriosis are not able to get pregnant,1 making this condition one of the top three causes of female infertility.
- Pelvic adhesions. Adhesions that form on the ovaries, fallopian tubes, or uterus can make it difficult or impossible to get pregnant 16.
- Uterine fibroids. Most women with fibroids do not have problems with fertility and can get pregnant. If a woman’s fibroid is located in the uterine cavity, she may face an increased risk of early pregnancy loss. Some women with fibroids may not be able to get pregnant naturally, but advances in treatments for infertility may help some of them get pregnant.
Some treatments for pelvic pain also can affect a woman’s ability to get pregnant. For example, hormonal birth control commonly is used to treat endometriosis. Hysterectomy, which is surgery to remove a woman’s uterus, may be an option for women who are not helped by other treatments, but it makes pregnancy impossible. However, a woman may still be able to become a mother through other means, such as a surrogate carrier.
Can alternative therapies treat your pelvic pain ?
Some women choose alternative medicine to treat their pain. Although there is little evidence on how effective these remedies are for treating pain, alternative treatments may help in some cases 17.
For instance, the following approaches may help relieve menstrual pain 2:
- Vitamin B1 or magnesium supplements
- Acupuncture, acupressure, and nerve stimulation therapies
If you are thinking about trying an alternative product or therapy to cope with your pain, make sure to talk to your health care providers first. Ask them what the scientific evidence indicates about the safety of the product or therapy and how well it works. Keep in mind that dietary supplements can interact with other medicines you might be using or can cause problems if not used correctly 18.
How Do Doctors Narrow the Diagnosis to Focus on Important Common Conditions of Pelvic Pain ?
Doctors usually categorize female patients presenting with uterus pain (acute pelvic pain) according to age (e.g., is she in her reproductive years or postmenopausal ?). If the patient is of reproductive age, possible diagnoses are next categorized by whether she is pregnant or attempting pregnancy.
Non-pregnant Reproductive Aged-Women
The typical diagnoses made in nonpregnant reproductive-aged women who present with acute pelvic pain include the following (from most to least common) 19, 20:
- Idiopathic (unknown cause or origin) pelvic pain,
- Pelvic inflammatory disease. Pelvic inflammatory disease is an infection and inflammation of the uterus, ovaries, and other female reproductive organs. It is usually caused by sexually transmitted infections e.g. gonorrhea and chlamydia
- Acute appendicitis,
- Conditions related to ovarian cysts, and
- Endometriosis.
Other less common causes of acute pelvic pain in this population are listed in Table 1 below.
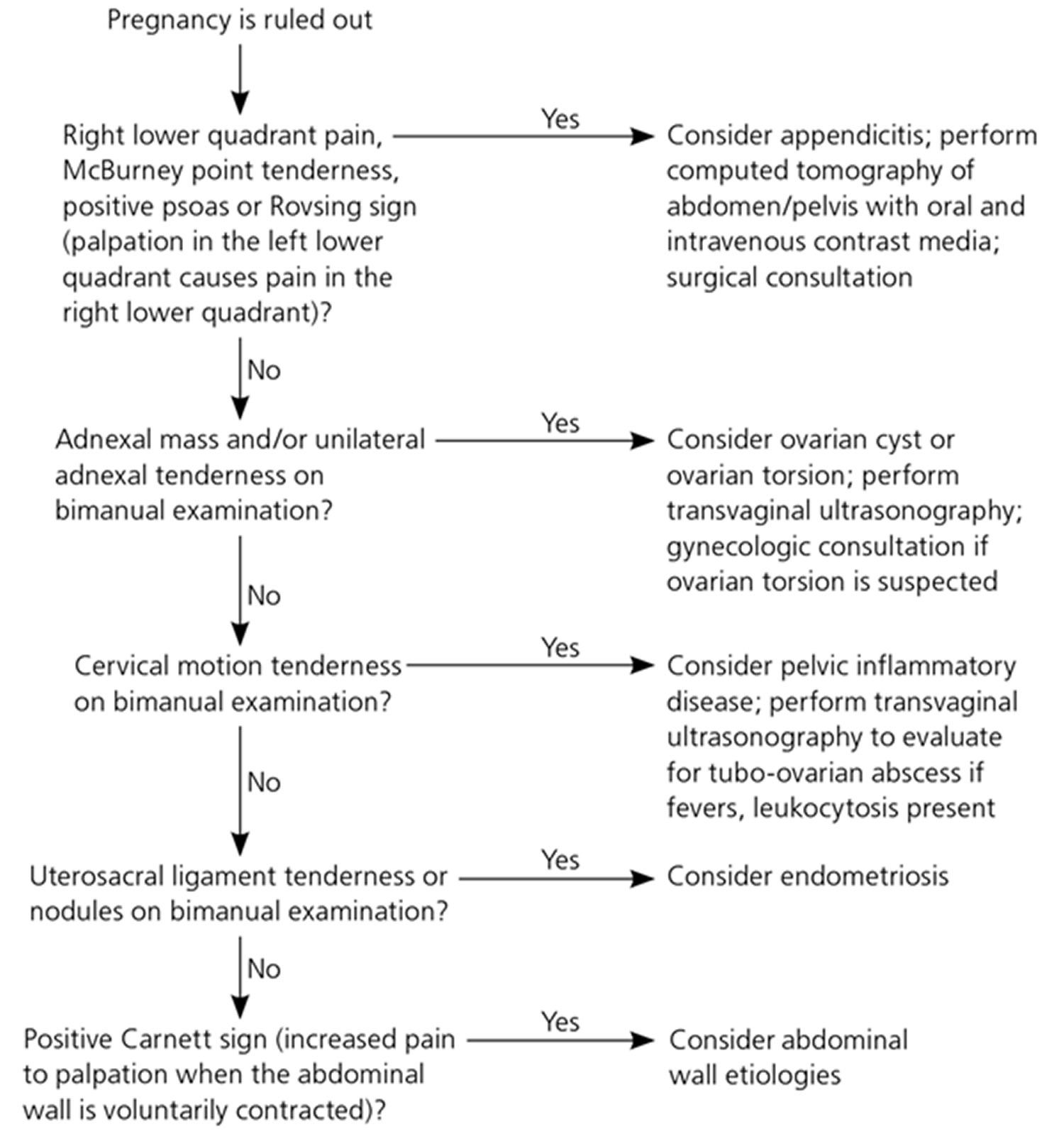
Table 1. Conditions Causing Acute Pelvic Pain in Different Populations
| Patient category | Common diagnoses | Less common diagnoses | Rare diagnoses |
|---|---|---|---|
Reproductive age (not pregnant) | Endometriosis (ruptured endometrioma) | Adenomyosis | Endosalpingiosis |
Idiopathic (no cause identified) | Dysmenorrhea | Round ligament mass (lipoma, teratoma) | |
Ovarian cyst, ruptured | Endometritis (postprocedure) | Transverse vaginal septum | |
Ovarian torsion | Imperforate hymen | ||
PID, tubo-ovarian abscess | Intrauterine device perforation | ||
Leiomyoma (degenerating) | |||
Mittelschmerz | |||
Reproductive age (pregnancy related) | Corpus luteum cyst | Leiomyoma (degenerating) | Incarcerated gravid uterus |
Ectopic pregnancy | Pubic symphysis separation | Ovarian vein thrombosis | |
Endometritis (postpartum) | Subchorionic hemorrhage | PID (rare after first trimester) | |
Normal labor | Uterine rupture | ||
Ovarian torsion | |||
PID (first trimester) | |||
Placental abruption | |||
Preterm labor | |||
Spontaneous abortion | |||
Reproductive age (undergoing fertility treatment) | Ectopic pregnancy | — | Heterotopic pregnancy |
Ovarian follicular cyst | |||
Ovarian hyperstimulation syndrome | |||
Ovarian torsion | |||
Postmenopausal | Malignancy | Ischemic colitis | Endometriosis |
PID, tubo-ovarian abscess | |||
Retained intrauterine device | |||
All groups | Appendicitis | Bowel obstruction | Mesenteric adenitis |
Diverticulitis | Inguinal hernia | ||
Inflammatory bowel disease | Interstitial cystitis | ||
Irritable bowel syndrome | Pelvic adhesive disease (postoperative scarring) | ||
Musculoskeletal (abdominal wall) pain | Perirectal abscess | ||
Urinary tract infection | Urethral diverticulum | ||
Urolithiasis | Urinary retention |
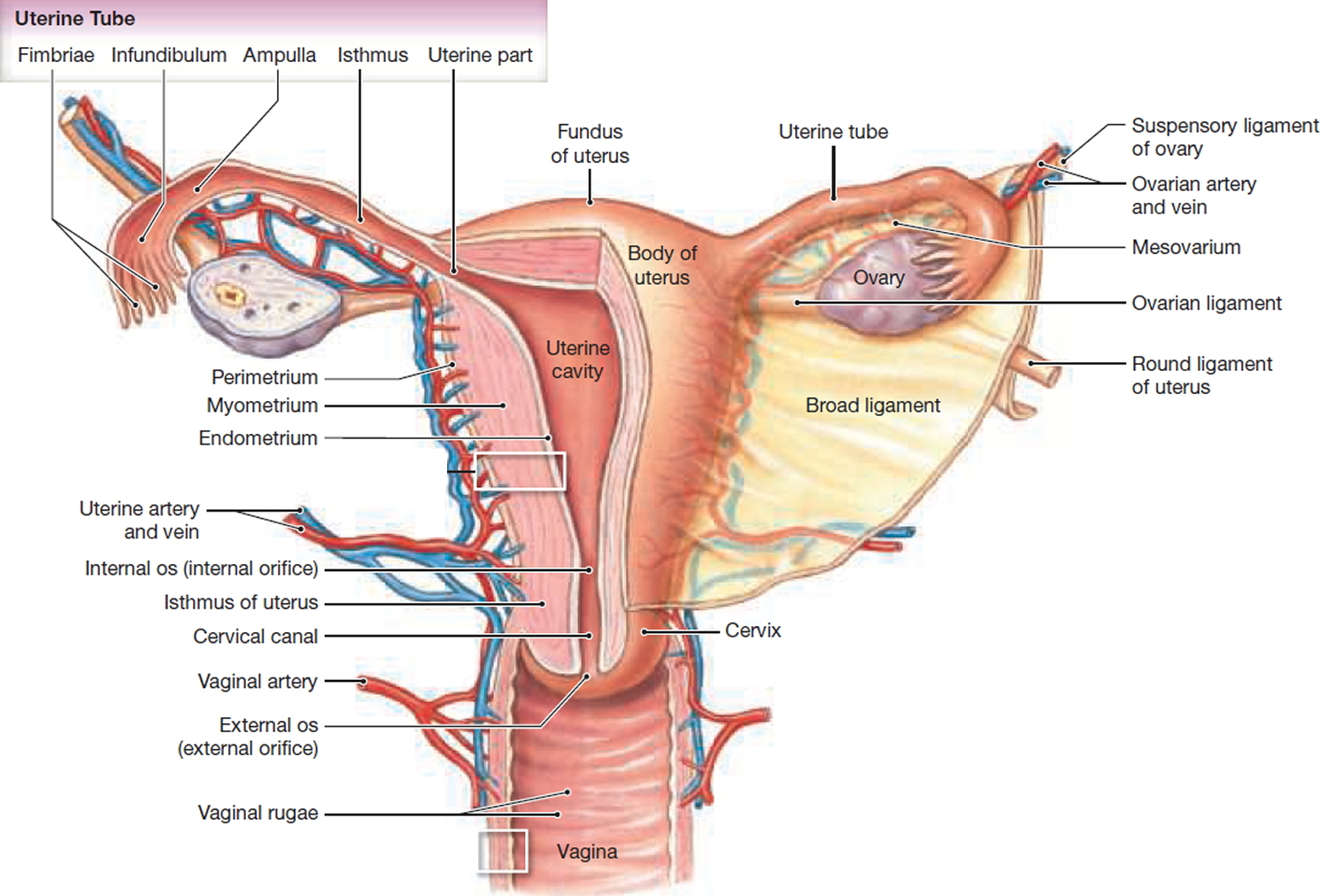
Figure 2. An algorithm for using physical examination findings to evaluate selected common causes of pelvic pain in nonpregnant women
Note: McBurney’s point = is the name given to the point over the right side of the abdomen that is one-third of the distance from the anterior superior iliac spine to the umbilicus (navel), this point roughly corresponds to the most common location of the base of the appendix where it is attached to the cecum, deep tenderness at McBurney’s point, known as McBurney’s sign, is a sign of acute appendicitis; Rovsing sign = is a sign of appendicitis, if palpation of the left lower quadrant of a person’s abdomen increases the pain felt in the right lower quadrant, the patient is said to have a positive Rovsing’s sign and may have appendicitis; Positive Carnett’s sign = is a finding on clinical examination in which (acute) abdominal pain remains unchanged or increases when the muscles of the abdominal wall are tensed. A positive test increases the likelihood that the abdominal wall and not the abdominal cavity is the source of the pain (for example, due to rectus sheath hematoma instead of appendicitis).
[Source 21]Reproductive-aged women who are pregnant or attempting pregnancy
Women who are pregnant or attempting pregnancy through fertility treatments have other common causes of acute pelvic pain (Table 1). For pregnant women, the clinical scenario narrows the list of possible causes, but it is critical to detect serious or life-threatening conditions, such as ectopic pregnancy in the early weeks of pregnancy and placental abruption in the later stages of pregnancy. Nongynecologic conditions, such as appendicitis, can also occur during pregnancy.
Women undergoing infertility treatments through ovarian stimulation or in vitro fertilization have unique risks, such as ovarian hyperstimulation syndrome (i.e., ovarian enlargement with multiple ovarian cysts and leakage of fluid from the ovary into the abdominal/pelvic space), ovarian torsion, and heterotopic pregnancy (i.e., simultaneous ectopic and intrauterine pregnancy) 22.
Postmenopausal women
Cancer must be primarily considered in a postmenopausal woman with acute pelvic pain. Other rare causes are postmenopausal endometriosis 23 and, on occasion, a retained intrauterine device that the patient had forgotten to remove 24.
Pain in right side of uterus
Acute appendicitis
- Complete blood count demonstrating leukocytosis
- Contrast CT of the abdomen and pelvis
Ectopic pregnancy
- Qualitative urine β-hCG can detect a pregnancy at four weeks’ gestation
- Quantitative serum β-hCG can determine if pregnancy is above the discriminatory level such that an intrauterine pregnancy should be visible on pelvic ultrasonography to rule out ectopic gestation.
- Blood type to determine Rh status; if bleeding and pregnant, will need Rho(D) immune globulin (RhoGam)
- Pelvic ultrasonography
Ovarian torsion
- Presence of risk factors (nausea, vomiting, pregnancy)
- Pelvic ultrasonography with Doppler flow study
- Consider urgent referral for surgical evaluation and treatment
Pain in uterus area
Bilateral pain, particularly if associated with mucopurulent vaginal discharge
Pelvic inflammatory disease
- Testing for sexually transmitted infections
- Complete blood count to test for leukocytosis or left shift
Adenomyosis (endometrial tissue grown into the uterine wall)
- History of intrauterine instrumentation, multiple cesarean deliveries, or other uterine surgeries
- Magnetic resonance imaging
Pelvic adhesions
- History of intrauterine instrumentation, multiple cesarean deliveries, or other uterine surgeries
- Consider non-urgent referral to gynecologist or general surgeon in absence of other findings
Menstrual abnormalities
Amenorrhea (abnormal absence of menstruation)
- Imperforate hymen – Pelvic examination
- Transverse vaginal septum – Pelvic ultrasonography
Dysmenorrhea (painful menstruation)
- Endometriosis, ovarian cyst – Pelvic ultrasonography (to assess for ovarian cyst)
Urinary symptoms
Dysuria (painful or difficult urination)
- Urinary tract infection – Urinalysis demonstrating white blood cells, bacteria, leukocyte esterase, or nitrites
Gross hematuria (blood in urine)
- Urolithiasis (urinary bladder or urinary tract stone) – Abdominal ultrasonography.
- Pelvic pain. Mayo Clinic. https://www.mayoclinic.org/symptoms/pelvic-pain/basics/definition/sym-20050898[↩]
- American College of Obstetricians and Gynecologists. (2004). ACOG practice bulletin no. 51. Chronic pelvic pain. Obstetrics & Gynecology, 103, 589–605.[↩][↩][↩][↩][↩][↩][↩]
- UCSF Medical Center. (n.d.). Pelvic pain. https://www.ucsfhealth.org/conditions/pelvic_pain/[↩][↩][↩][↩]
- Reiter, R. C. (1996). A profile of women with chronic pelvic pain. Clinical Obstetrics and Gynecology, 33, 130–136.[↩]
- What causes pelvic pain ? National Institute of Child Health and Human Development. https://www.nichd.nih.gov/health/topics/pelvicpain/conditioninfo/Pages/causes.aspx[↩]
- Andrews J, Yunker A, Reynolds WS, et al. Noncyclic Chronic Pelvic Pain Therapies for Women: Comparative Effectiveness [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2012 Jan. (Comparative Effectiveness Reviews, No. 41.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK84586/[↩]
- Mathias, S. D., Kuppermann, M., Liberman, R. F., Lipschutz, R. C., & Steege, J. F. (1996). Chronic pelvic pain: Prevalence, health-related quality of life, and economic correlates. Obstetrics & Gynecology, 87, 321–327.[↩][↩]
- Ahangari, A. (2014). Prevalence of chronic pelvic pain among women: An updated review. Pain Physician, 17, E141–E147. http://www.painphysicianjournal.com/current/pdf?article=MjA2NQ%3D%3D&journal=81[↩]
- National Kidney and Urologic Diseases Information Clearinghouse. (2013). Interstitial cystitis/painful bladder syndrome. https://www.niddk.nih.gov/health-information/urologic-diseases/interstitial-cystitis-painful-bladder-syndrome[↩][↩]
- National Digestive Diseases Clearinghouse. (n.d.). Irritable bowel syndrome. https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome[↩][↩]
- International Pelvic Pain Society. (2008). Pelvic pain assessment form. http://pelvicpain.org/docs/resources/forms/history-and-physical-form-english.aspx[↩]
- Radiological Society of North America. (2015). Ultrasound—pelvis. https://www.radiologyinfo.org/en/info.cfm?pg=pelvus[↩]
- Andrews, J., Yunker, A., Reynolds, W. S., Likis, F. E., Sathe, N. A., & Jerome, R. N. (2012). Noncyclic chronic pelvic pain therapies for women: Comparative effectiveness (Comparative Effectiveness Review No. 41). Rockville, MD: Agency for Healthcare Research and Quality.[↩][↩]
- American College of Obstetricians and Gynecologists, ACOG Committee on Practice Bulletins—Gynecology. (2004). ACOG practice bulletin no. 51. Chronic pelvic pain. Obstetrics & Gynecology, 103(3), 589–605[↩]
- Rodriguez, M. A., Afari, N., Buchwald, D. S., & National Institute of Diabetes and Digestive and Kidney Diseases Working Group on Urological Chronic Pelvic Pain. (2009). Evidence for overlap between urological and nonurological unexplained clinical conditions. Journal of Urology,182, 2123–2131.[↩]
- American Society for Reproductive Medicine. (2008). Adhesions: What are they and how can they be prevented ? http://www.missourifertility.com/uploads/3/8/7/5/38755215/adhesions-what_are_they….pdf[↩]
- National Center for Complementary and Integrative Medicine. (2017). Chronic Pain: In Depth. https://nccih.nih.gov/health/pain/chronic.htm[↩]
- National Center for Complementary and Alternative Medicine. (2015). 5 Tips: What Consumers Need To Know About Dietary Supplements. https://nccih.nih.gov/health/tips/supplements[↩]
- Yeh JM, Hook EW III, Goldie SJ. A refined estimate of the average lifetime cost of pelvic inflammatory disease. Sex Transm Dis. 2003;30(5):369–378.[↩]
- Morino M, Pellegrino L, Castagna E, Farinella E, Mao P. Acute nonspecific abdominal pain: a randomized, controlled trial comparing early lap-aroscopy versus clinical observation. Ann Surg. 2006;244(6):881–888.[↩]
- Common Questions About the Evaluation of Acute Pelvic Pain. Am Fam Physician. 2016 Jan 1;93(1):41-48A. http://www.aafp.org/afp/2016/0101/p41.html[↩][↩]
- Svare J, Norup P, Grove Thomsen S, et al. Heterotopic pregnancies after in-vitro fertilization and embryo transfer—a Danish survey. Hum Reprod. 1993;8(1):116–118.[↩]
- Oxholm D, Knudsen UB, Kryger-Baggesen N, Ravn P. Postmenopausal endometriosis. Acta Obstet Gynecol Scand. 2007;86(10):1158–1164.[↩]
- Wagner CA, Gimpelson RJ. Postmenopausal bleeding due to a Cu-7 intrauterine device retained for thirty years. JSLS. 2012;16(2):329–332.[↩]