Contents
What is vitiligo
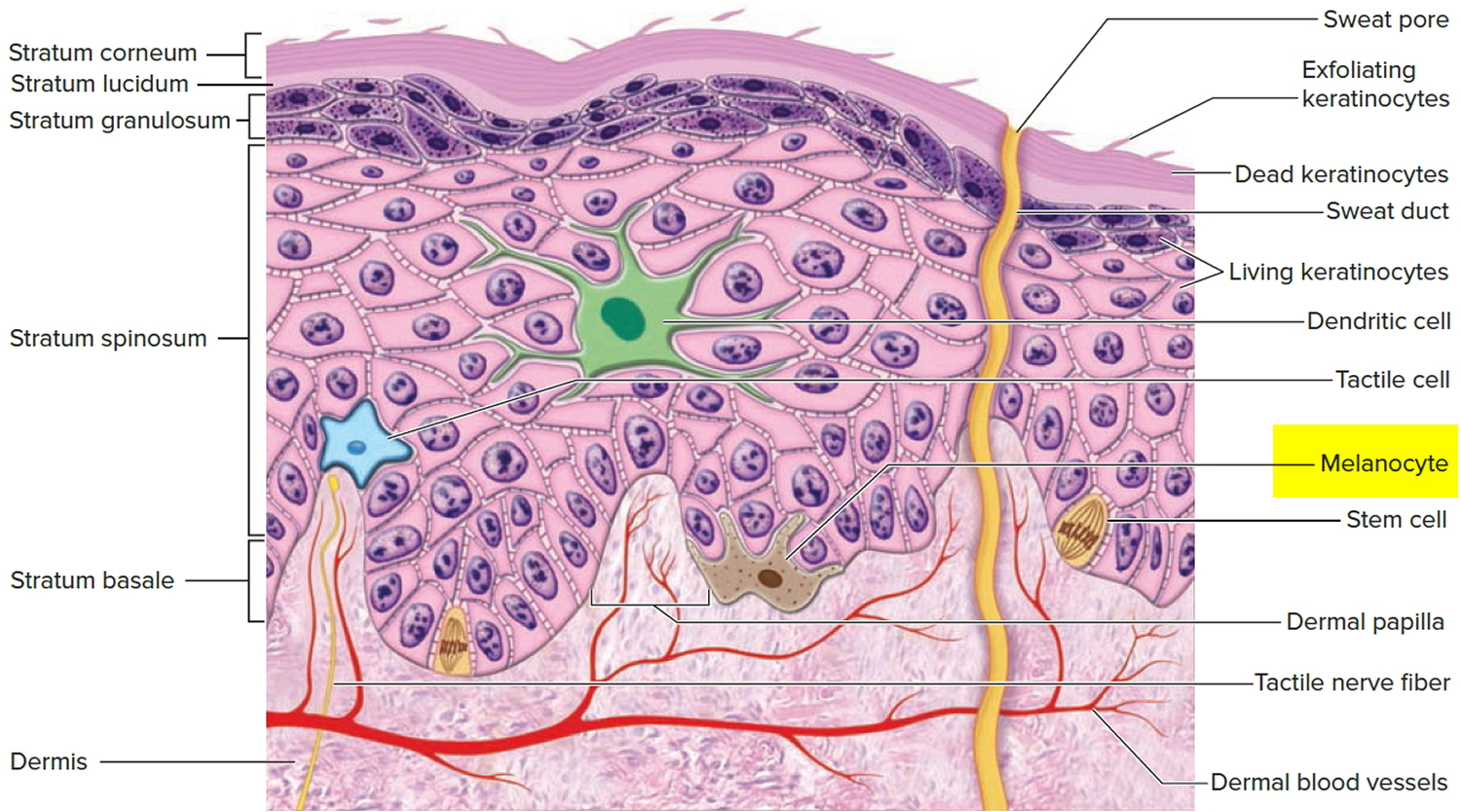
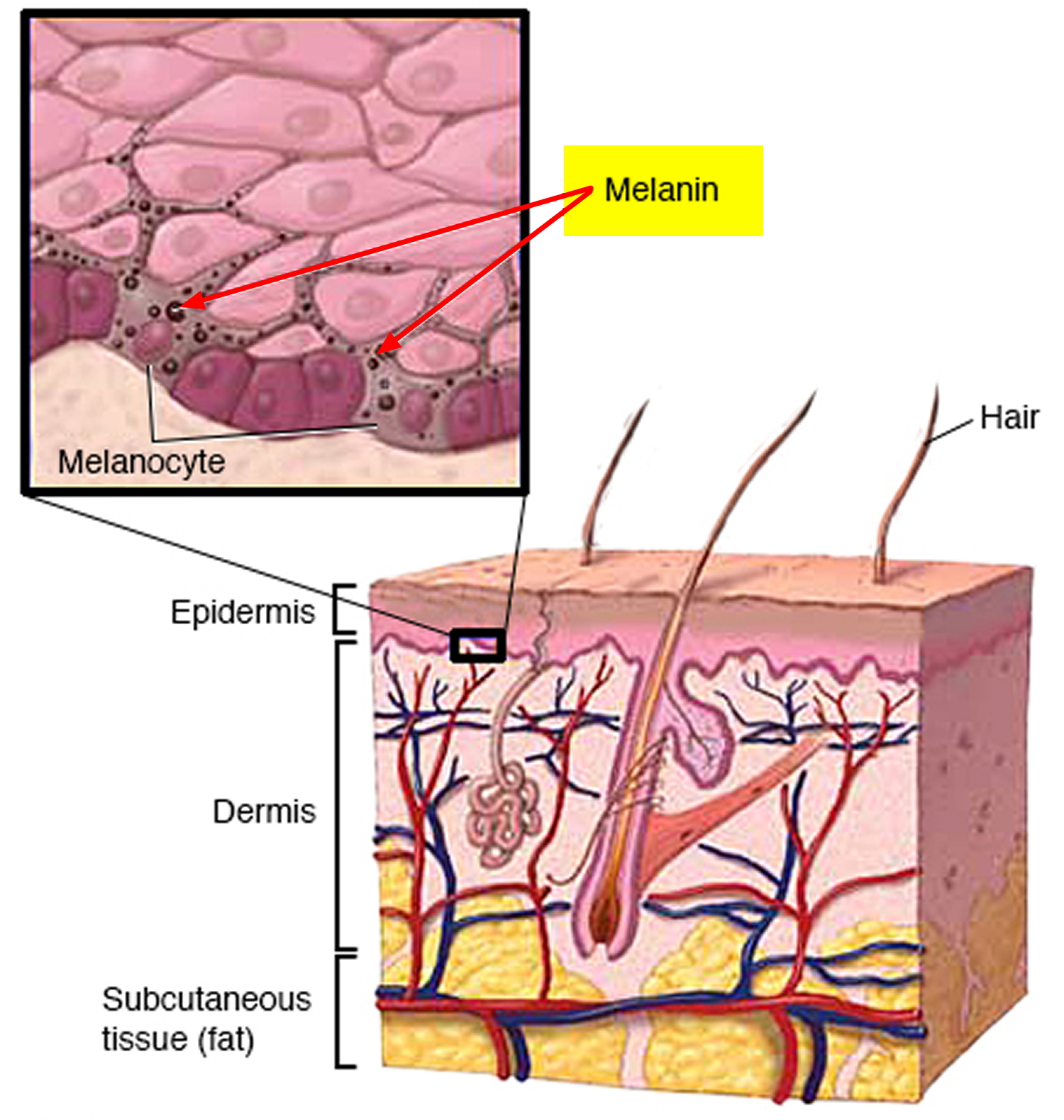
Vitiligo is a skin condition that causes patchy loss of skin coloring (pigmentation) resulting in pale white patches to develop on the skin (see Figures 2 – 4 below). Vitiligo occurs when the cells that produce melanin (melanocytes) die or stop functioning. The average age of onset of vitiligo is in the mid-twenties, but it can appear at any age. Vitiligo tends to progress over time, with larger areas of the skin losing pigment. Some people with vitiligo also have patches of pigment loss affecting the hair on their scalp or body. The extent and rate of color loss from vitiligo is unpredictable.
Figure 1. Skin anatomy
Vitiligo is a common disorder, affecting between 1 percent and 2 percent of the population worldwide. While the condition may be more noticeable in dark-skinned people, it occurs with similar frequency in all ethnic groups. Vitiligo can start at any age, but often appears before age 20.
Vitiligo isn’t caused by an infection and you can’t catch it from someone else who has it. Vitiligo is not life-threatening.
It’s difficult to predict how your disease will progress. Sometimes the patches stop forming without treatment. In most cases, pigment loss spreads and eventually involves most of your skin. Rarely, the skin gets its color back.
Researchers have identified several forms of vitiligo. Generalized vitiligo (also called nonsegmental vitiligo), which is the most common form, involves loss of pigment (depigmentation) in patches of skin all over the body. Depigmentation typically occurs on the face, neck, and scalp, and around body openings such as the mouth and genitals. Sometimes pigment is lost in mucous membranes, such as the lips. Loss of pigmentation is also frequently seen in areas that tend to experience rubbing, impact, or other trauma, such as the hands, arms, and places where bones are close to the skin surface (bony prominences). Another form called segmental vitiligo is associated with smaller patches of depigmented skin that appear on one side of the body in a limited area; this occurs in about 10 percent of affected individuals.
The pale areas of skin are more vulnerable to sunburn, so it’s important to take extra care when in the sun and use a broadspectrum sunscreen with a high sun protection factor (SPF) of SPF 50+.
Vitiligo is generally considered to be an autoimmune disorder. Autoimmune disorders occur when the immune system attacks the body’s own tissues and organs. In people with vitiligo the immune system appears to attack the pigment cells (melanocytes) in the skin. About 15 to 25 percent of people with vitiligo are also affected by at least one other autoimmune disorder, particularly autoimmune thyroid disease, rheumatoid arthritis, type 1 diabetes, psoriasis, pernicious anemia, Addison disease, myasthenia gravis or systemic lupus erythematosus.
In the absence of other autoimmune conditions, vitiligo does not affect general health or physical functioning. However, concerns about appearance and ethnic identity are significant issues for many affected individuals.
The white patches caused by vitiligo are usually permanent, although treatment options are available to improve the appearance of your skin.
If the patches are relatively small, skin camouflage cream can be used to cover them up. In general, combination treatments, such as phototherapy (treatment with light) and medication, give the best results. Although treatment may help restore color to your skin, the effect doesn’t usually last. Treatment can’t stop the condition spreading.
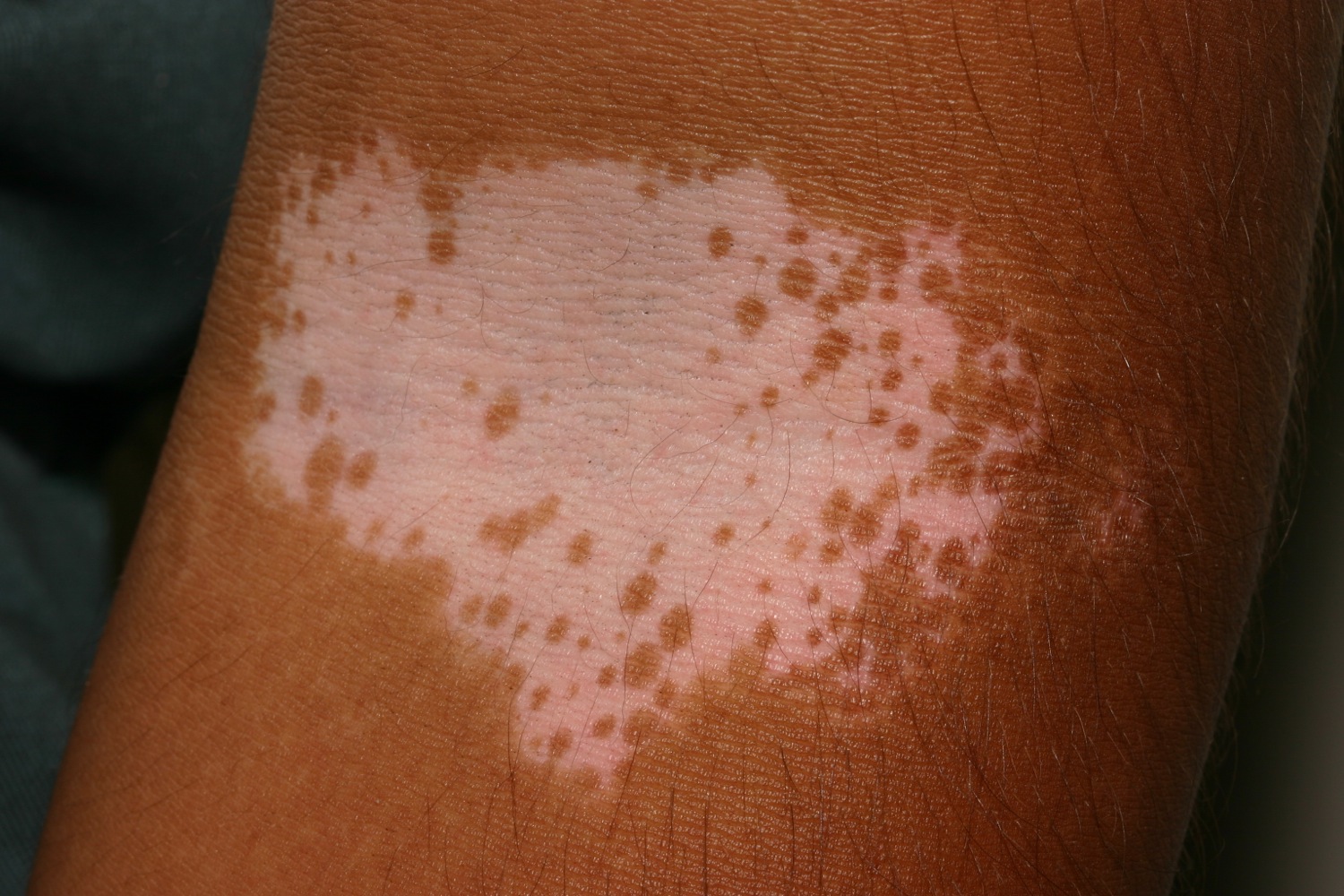
Figure 2. Vitiligo
Vitiligo types
There are two main types of vitiligo:
- Non-segmental vitiligo
- Segmental vitiligo
In rare cases, it’s possible for vitiligo to affect your whole body. This is known as universal or complete vitiligo.
Non-segmental vitiligo
In non-segmental vitiligo (also called bilateral or generalized vitiligo), the symptoms often appear on both sides of your body as symmetrical white patches (Figure 3).
Symmetrical patches can appear on the:
- backs of your hands
- arms
- skin around body openings, such as the eyes
- knees
- elbows
- feet
Non-segmental vitiligo is the most common type of vitiligo, affecting around 9 out of 10 people with the condition.
Figure 3. Vitiligo skin (non-segmental vitiligo)
Segmental vitiligo
In segmental vitiligo (also known as unilateral or localized vitiligo), the white patches only affect one area of your body.
Segmental vitiligo is less common than non-segmental vitiligo, although it’s more common in children. It usually starts earlier and affects 3 in 10 children with vitiligo.
Figure 4. Localized vitiligo (segmental vitiligo)
Vitiligo complications
Vitiligo can sometimes cause other problems.
Because of a lack of melanin, your skin will be more vulnerable to the effects of the sun. Make sure you use a strong sunscreen to avoid sunburn.
Vitiligo may also be associated with problems with your eyes, such as inflammation of the iris (iritis), and a partial loss of hearing (hypoacusis).
Problems with confidence and self-esteem are common in people with vitiligo, particularly if it affects areas of skin that are frequently exposed.
Vitiligo causes
Vitiligo is caused by the lack of a pigment called melanin in the skin. Melanin is produced by skin cells called melanocytes, and it gives your skin its color.
In vitiligo, there aren’t enough working melanocytes (melanin producing cells) to produce enough melanin in your skin. This causes white patches to develop on your skin or hair. It’s not clear exactly why the melanocytes disappear or die from the affected areas of skin.
Vitiligo may be related to:
- A disorder in which your immune system attacks and destroys the melanocytes in the skin
- Family history (heredity)
- A trigger event, such as sunburn, stress or exposure to industrial chemicals
It is unclear what specific circumstances trigger the immune system to attack melanocytes in the skin. Research suggests that the immune system of affected individuals may react abnormally to melanocytes that are stressed by factors such as chemicals or ultraviolet radiation. In addition, the melanocytes of people with vitiligo may be more susceptible to stress than those of the general population and therefore may be more likely to be attacked by the immune system. The condition probably results from a combination of genetic and environmental factors, most of which have not been identified.
Autoimmune conditions
Non-segmental vitiligo (the most common type) is thought to be an autoimmune condition.
In autoimmune conditions, the immune system doesn’t work properly. Instead of attacking foreign cells, such as viruses, your immune system attacks your body’s healthy cells and tissue.
If you have non-segmental vitiligo, your immune system destroys the melanocyte skin cells that make melanin.
Vitiligo is also associated with other autoimmune conditions, such as hyperthyroidism (an overactive thyroid gland), but not everyone with vitiligo will develop these conditions.
Risk factors for developing non-segmental vitiligo
You may be at increased risk of developing non-segmental vitiligo if:
- other members of your family have it
- there’s a family history of other autoimmune conditions – for example, if one of your parents has pernicious anaemia (an autoimmune condition that affects the stomach)
- you have another autoimmune condition
- you have melanoma (a type of skin cancer) or cutaneous T-cell lymphoma (cancer of the lymphatic system)
- you have particular changes in your genes that are known to be linked to non-segmental vitiligo
Neurochemicals
Segmental vitiligo (the less common type) is thought to be caused by chemicals released from the nerve endings in your skin. These chemicals are poisonous to the melanocyte skin cells.
Triggers
It’s possible that vitiligo may be triggered by particular events, such as:
- stressful events, like childbirth
- skin damage, such as severe sunburn or cuts (this is known as the Koebner response)
- exposure to certain chemicals – for example, at work.
Vitiligo symptoms
The areas most commonly affected by vitiligo include:
- the skin around your mouth and eyes
- fingers and wrists
- armpits
- groin
- genitals
- inside your mouth
It can also sometimes develop where there are hair roots, such as on your scalp. The lack of melanin in your skin can turn the hair in the affected area white or grey.
Vitiligo often starts as a pale patch of skin that gradually turns completely white. The centre of a patch may be white, with pale skin around it. If there are blood vessels under the skin, the patch may be slightly pink, rather than white.
The edges of the patch may be smooth or irregular. They’re sometimes red and inflamed, or there’s brownish discolouration (hyperpigmentation).
Vitiligo doesn’t cause discomfort to your skin, such as dryness, but the patches may occasionally be itchy.
The condition varies from person to person. Some people only get a few small, white patches, but others get bigger white patches that join up across large areas of their skin.
There’s no way of predicting how much skin will be affected. The white patches are usually permanent.
Vitiligo diagnosis
Your doctor will be able to diagnose vitiligo after examining the affected areas of skin.
They may ask whether:
- there’s a history of vitiligo in your family
- there’s a history of other autoimmune conditions in your family
- you’ve injured the affected areas of skin – for example, whether you’ve had sunburn or a severe rash there
- you tan easily in the sun, or whether you burn
- any areas of skin have got better without treatment, or whether they’re getting worse
- you’ve tried any treatments already
Your doctor may also ask you about the impact vitiligo has on your life. For example, how much it affects your confidence and self-esteem, and whether it affects your job.
Wood’s lamp
If available, your doctor may use an ultraviolet (UV) lamp called a Wood’s lamp to look at your skin in more detail. You’ll need to be in a dark room and the lamp will be held 10 to 13cm (4 to 5in) away from your skin.
The patches of vitiligo will be easier to see under the UV light, which will help your doctor distinguish vitiligo from other skin conditions, such as pityriasis versicolor (where there’s a loss of pigment due to a fungal infection).
Other autoimmune conditions
As non-segmental vitiligo is closely associated with other autoimmune conditions, you may be assessed to see whether you have any symptoms that could suggest an autoimmune condition, such as:
- being tired and lacking energy (signs of Addison’s disease)
- being thirsty and needing to urinate frequently (signs of diabetes)
A blood test may also be needed to check how well your thyroid gland is functioning and to look for underlying autoimmune conditions, such as anemia or diabetes.
Vitiligo treatment
Treatment for vitiligo is based on improving the appearance of the skin by restoring its color.
However, the effects of treatment aren’t usually permanent, and it can’t always control the spread of the condition.
Your doctor may recommend:
- sun safety advice
- camouflage creams
- topical corticosteroids
Further treatment may not be necessary if, for example, you only have a small patch of vitiligo or you have very fair skin anyway.
You may be referred to a dermatologist (a specialist in treating skin conditions) if further treatment is needed.
Protection from the sun
Sunburn is a real risk if you have vitiligo. You must protect your skin from the sun and avoid using sunbeds.
When skin is exposed to sunlight, it produces a pigment called melanin to help protect it from ultraviolet light. However, if you have vitiligo there isn’t enough melanin in your skin, so it isn’t protected.
Always apply a high-factor sunscreen, ideally with a sun protection factor (SPF) of 30 or above, to protect your skin from sunburn and long-term damage. This is particularly important if you have fair skin.
Protecting your skin from the sun will also mean you don’t tan as much, which will make your vitiligo less noticeable.
Vitamin D
If your skin isn’t exposed to the sun, there’s an increased risk of vitamin D deficiency. Vitamin D is essential for keeping bones and teeth healthy.
Sunlight is the main source of vitamin D, although it’s also found in some foods, such as oily fish.
It might be difficult to get enough vitamin D from food and sunlight alone. You should therefore consider taking a daily supplement containing 10 micrograms (10 mcg) of vitamin D.
Skin camouflage
Skin camouflage creams can be applied to the white patches of skin. The creams are specially made to match your natural skin color. The cream blends in the white patches with the rest of your skin, making them less noticeable.
Cosmetic camouflage can disguise vitiligo. Options include:
- Make-up, dyes and stains
- Waterproof products
- Dihydroxyacetone-containing products “tan without sun”
- Micropigmentation or tattooing for stable vitiligo
Camouflage creams are waterproof and can be applied anywhere on the body. They last for up to four days on the body and 12 to 18 hours on the face.
You can also get skin camouflage cream that contains sun block or has an sun protection factor (SPF) rating.
Self-tanning lotion (fake tan) may also help cover vitiligo. Some types can last several days before they need to be reapplied. Self-tanning lotion is available from most pharmacies.
Don’t get a tattoo. Avoid tattooing that’s not related to treating your vitiligo. Damage to your skin, such as that caused by a tattoo, may cause a new patch of vitiligo to appear within two weeks.
How to use cosmetic camouflage
There are 3 basic approaches to cosmetic camouflage.
- Concealing – concealers are often thicker and more opaque than regular foundation makeup. They effectively cover healed incision lines from surgery, scars and/or bruises on your face or body. Concealers are usually creamy products and come in a variety of shades to match the natural color of the skin. Sometimes they are blended with color correctors to achieve a good color match. Liquid color-matched concealers are also available that can closely resemble normal skin.
- Color correcting – color correctors are used to disguise the yellowish shade of a bruise or the overall redness from a burn. Color correctors come in tints, purple corrector blended with concealer neutralizes yellow skin tones, while green corrector yields a brown tone to neutralize redness.
- Contouring – contouring corrects the irregular facial surface contours by creating dimension using light and shadow. Dark colors make swellings or protrusions appear to recede, while light colours make surface depressions appear shallower. To achieve contouring you need a highlighter, which is about 2 shades lighter than your concealer, and a contour shadow, which is about 2 shades darker. Powdered blush-type products are best suited for contouring.
Camouflage makeup needs to be removed from your face and neck every night before you go to bed. Because of their waterproof nature, an oily cleansing cream or lotion may be needed to wipe off the makeup. Follow by cleaning with soap and water or your normal facial cleansing routine. Liquid camouflage products and camouflage cosmetics used elsewhere on the body can be left on for 3 or 4 days before removing them and re-applying.
Topical corticosteroids
Topical corticosteroids are a type of medication that contain steroids. You apply them to your skin as a cream or ointment.
They can sometimes stop the spread of the white patches and may restore some of your original skin color.
A topical corticosteroid may be prescribed to adults if:
- you have non-segmental vitiligo on less than 10% of your body
- you want further treatment (sun protection advice and camouflage creams are enough for some people)
- you aren’t pregnant
- you understand and accept the risk of side effects
Topical corticosteroids can be used on the face, but care should be taken in selecting and using this type of medication on your face.
Using topical corticosteroids
Your doctor may prescribe a cream or an ointment, depending on what you prefer and where it will be used. Ointments tend to be greasier. Creams are better in your joints – for example, inside your elbows.
Possible corticosteroids that may be prescribed include:
- fluticasone propionate
- betamethasone valerate
- hydrocortisone butyrate
Your doctor will tell you how to apply the cream or ointment to the patches and how much you should use. You normally need to apply the treatment once a day.
Topical corticosteroids are measured in a standard unit called the fingertip unit (FTU). One fingertip unit is the amount of topical steroid squeezed along an adult’s fingertip. One fingertip unit is enough to treat an area of skin twice the size of an adult’s hand.
Follow-up
After one month, you’ll have a follow-up appointment so your doctor can check how well the treatment is working and whether you have any side effects. If the treatment is causing side effects, you may need to stop using corticosteroids.
After another month or two, your doctor will check how much your vitiligo has improved. If there’s no improvement, you may be referred to a dermatologist.
If it’s improved slightly, you may continue treatment, but have a break from treatment every few weeks. You may also be referred to a dermatologist.
Treatment will be stopped if your vitiligo has improved significantly.
Your doctor may take photos of your vitiligo throughout your treatment to monitor any signs of improvement. You may also want to take photos yourself.
Side effects of topical corticosteroids
Side effects of topical corticosteroids include:
- streaks or lines in your skin (striae)
- thinning of your skin (atrophy)
- visible blood vessels appearing (telangiectasia)
- excess hair growth (hypertrichosis)
- contact dermatitis (inflammation of your skin)
- acne
Referral to a dermatologist
Your doctor may refer you to a dermatologist if:
- they’re unsure about your diagnosis
- you’re pregnant and need treatment
- more than 10% of your body is affected by vitiligo
- you’re distressed about your condition
- your face is affected and you want further treatment
- you can’t use topical corticosteroids because of the risk of side effects
- you have segmental vitiligo and want further treatment
- treatment with topical corticosteroids hasn’t worked
Children with vitiligo who need treatment will also be referred to a dermatologist.
In some cases, you may be prescribed strong topical corticosteroids while you’re waiting to be seen by a dermatologist.
Some treatments your dermatologist may recommend are described below.
Topical pimecrolimus or tacrolimus
Pimecrolimus and tacrolimus are a type of medicine called calcineurin inhibitors, which are normally used to treat eczema.
Pimecrolimus and tacrolimus are unlicensed for treating vitiligo, but they can be used to help restore skin pigment in adults and children with vitiligo.
They can cause side effects, such as:
- a burning or painful sensation when applied to the skin
- making the skin more sensitive to sunlight
- facial flushing (redness) and skin irritation if you drink alcohol
However, unlike corticosteroids, pimecrolimus and tacrolimus don’t cause thinning of the skin.
Phototherapy
Phototherapy (treatment with light) may be used for children or adults if:
- topical treatments haven’t worked
- the vitiligo is widespread
- the vitiligo is having a significant impact on quality of life
Evidence suggests that phototherapy, particularly when combined with other treatments, has a positive effect on vitiligo.
During phototherapy, your skin is exposed to ultraviolet A (UVA) or ultraviolet B (UVB) light from a special lamp. You may first take a medicine called psoralen, which makes your skin more sensitive to the light. Psoralen can be taken by mouth (orally), or it can be added to your bath water.
This type of treatment is sometimes called PUVA (psoralen and UVA light).
Phototherapy may increase the risk of skin cancer because of the extra exposure to UVA rays. The risk of skin cancer is lower with UVB light. Your dermatologist should discuss the risk with you before you decide to have phototherapy.
Phototherapy probably works in vitiligo by 2 mechanisms.
- Immune suppression—preventing destruction of the melanocytes
- Stimulation of cytokines (growth factors)
Treatment is usually given twice weekly for a trial period of 3–4 months. If repigmentation is observed, treatment is continued until repigmentation is complete or for a maximum of 1–2 years.
- Phototherapy is unsuitable for very fair skinned people.
- The treatment intensity aims for the vitiligo skin to be a light “carnation” pink
- If repigmentation is observed, treatment is continued until repigmentation is complete or for a maximum of 1–2 years.
- Treatment times are generally brief. The aim is to cause the treated skin to appear very slightly pink the following day.
- It is important to avoid burning (red, blistered, peeling, itchy or painful skin), as this could cause the vitiligo to get worse.
A meta-analysis included 35 unique studies reporting outcome after phototherapy for generalised vitiligo. Marked or clinically useful response was achieved in 36% after 12 months of NBUVB and in 62% after 12 months of PUVA. Face and neck responded better than trunk, which responded better than extremities. It was not very effective on hands and feet.
Sunlamps that you can buy to use at home for light therapy aren’t recommended. They’re not as effective as the phototherapy you’ll receive in hospital. The lamps are also not regulated, so may not be safe.
Systemic therapy
Systemic treatments for vitiligo include:
- Oral minocycline, a tetracycline antibiotic with anti-inflammatory properties
- Mini-pulses of oral steroids for 3 to 6 months, e.g., dexamethasone 2.5 mg, 2 days per week
- Subcutaneous afamelanotide
It is anticipated that monoclonal antibody biologic agents will be developed to treat vitiligo.
Surgical treatment of stable vitiligo
Surgical treatment for stable and segmental vitiligo requires removal of the top layer of vitiligo skin (by shaving, dermabrasion, sandpapering or laser) and replacement with pigmented skin removed from another site.
Techniques include:
- Non-cultured melanocyte-keratinocyte cell suspension transplantation.
- Punch grafting
- Blister grafts, formed by suction or cryotherapy
- Split skin grafting
- Cultured autografts of melanocytes grown in tissue culture
Skin grafts
A skin graft is a surgical procedure where healthy skin is removed from an unaffected area of the body and used to cover an area where the skin has been damaged or lost. To treat vitiligo, a skin graft can be used to cover the white patch.
Skin grafts may be considered for adults in areas that are affecting your appearance if:
- no new white patches have appeared in the last 12 months
- the white patches haven’t got worse in the last 12 months
- your vitiligo wasn’t triggered by skin damage, such as severe sunburn (known as the Koebner response)
An alternative to skin grafting involves taking a sample of normal skin, removing the melanocytes from it and then transplanting them onto the areas of vitiligo.
These types of treatments are time-consuming, carry a risk of scarring and aren’t suitable for children.
Depigmentation
Depigmentation may be recommended for adults who have vitiligo on more than 50% of their bodies, although it may not be widely available.
During depigmentation, a lotion is painted on to the normal skin to bleach away the remaining pigment and make it the same color as the depigmented (white) skin. A hydroquinone-based medication is used, which has to be applied continuously to prevent the skin from re-pigmenting.
Hydroquinone can cause side effects, such as:
- redness
- itching
- stinging
Depigmentation is usually permanent and leaves the skin with no protection from the sun. Re-pigmentation (when the color returns) can occur and may differ from your original skin color. Applying depigmenting treatments in one area of skin can sometimes cause loss of pigmentation of skin on other parts of the body.
Other treatments
Your dermatologist may recommend trying more than one treatment, such as phototherapy combined with a topical treatment. Other possible treatments include:
- excimer lasers – high-energy beams of light that are used in laser eye treatment, but may also be used in phototherapy.
- vitamin D analogues – such as calcipotriol, which may also be used with phototherapy
- azathioprine – a medicine that suppresses your immune system (the body’s natural defence system)
- oral prednisolone – a type of corticosteroid, which has also been used with phototherapy; it can cause side effects.
Potential future treatments
Treatments being studied include:
- A drug to stimulate color-producing cells (melanocytes). Called afamelanotide, this potential treatment is implanted under the skin to promote the growth of melanocytes.
- A drug that helps control melanoctyes. Prostaglandin E2 is being tested as a way to restore skin color in people with localized vitiligo that isn’t spreading. It’s applied to the skin as a gel.
- A drug that reverses loss of color. Tofacitinib, an oral drug typically used to treat rheumatoid arthritis, has shown some potential as a treatment for vitiligo.
Complementary therapies
Some complementary therapies claim to relieve or prevent vitiligo. However, there’s no evidence to support their effectiveness, so more research is needed before they can be recommended.
There’s very limited evidence that ginkgo biloba, a herbal remedy, may benefit people with non-segmental vitiligo. There’s currently not enough evidence to recommend it.
Check with your doctor if you decide to use herbal remedies. Some remedies can react unpredictably with other medication or make them less effective.
Coping and support
You may feel stressed, self-conscious, sad, ashamed or even devastated by the change in your appearance caused by vitiligo. You may feel that the condition limits your ability to go about your daily activities, especially if it’s widespread or affects visible areas of your body, such as the face, hands, arms and feet.
These tips may help you cope with vitiligo:
- Make a good connection. Find a doctor who knows a lot about the condition. A dermatologist is a doctor who specializes in the care of skin.
- Learn all about it. Find out as much as you can about the condition and your treatment options so that you can help decide what steps to take.
- Communicate your feelings. Let your doctor know if you’re feeling depressed. He or she can refer you to a mental health provider who specializes in helping people with depression.
- Talk with others. Ask your doctor about psychotherapy or support groups in your area for people with vitiligo.
- Confide in loved ones. Seek understanding and support from your family and friends.