Contents
What is a wart
A viral wart is a very common growth of the skin caused by infection with human papillomavirus (HPV). A wart is also called a verruca or papilloma and warty lesions may be described as verrucous. Warts usually go away on their own but may take months or even years.
A wart will usually have a flesh colored appearance and the skin forming the wart will be rough.
Warts don’t cause you any harm but some people find them itchy, painful or embarrassing. Warty lesions (verrucas) are more likely to be painful – like standing on a needle.
There are several different types of warts, each with a slightly different appearance:
Cutaneous warts have a hard, keratinous surface. A tiny black dot may be observed in the middle of each scaly spot, due to a thrombosed capillary blood vessel.
- Common warts – these are small, raised areas of skin, usually round (papules), with a rough surface of skin often looking like the top of a cauliflower (known as butcher’s warts) — papillomatous and hyperkeratotic surface ranging in size from 1 mm to larger than 1 cm. These warts often appear on backs of fingers or toes, your hands, around the nails —where they can distort nail growth, elbows and knees.
- Flat or Plane warts – these are flat warts that are usually yellow in color (see Figure 6 below). They are often numerous. They are most common in children and can often spread and group together. Multiple flat-topped, flesh-colored papules are typical. Flat warts distribution is grouped and assymetric, helping to distinguish them from seborrheic keratosis in the adult. Flat warts tend to occur on sun-exposed skin, e.g. the back of the hands, the forehead and shins. It appears the immune suppressive nature of sunlight predisposes to flat wart infection. Shaving (or scratching) the legs or beard area can cause multiple lesions through auto-innoculation. Linear flat warts distribution (pseudo-Koebner response) are common. In some cases, the lesions are brown and resemble nevi (freckles). Flat warts are mostly caused by HPV types 3 and 10.
- Plantar warts (verrucas) are warts that appear on your feet, usually on the sole, heel or toes — include tender inwardly growing and painful ‘myrmecia’ on the sole of the foot, and clusters of less painful mosaic warts. The weight of your body causes the wart to be pushed into the skin so a verruca will usually not be raised like other warts and may even cause some discomfort when walking. You may notice a white area of skin with a tiny black dot in the center. Plantar epidermoid cysts are associated with warts. Persistent plantar warts may rarely be complicated by the development of verrucous carcinoma.
- Filiform warts – filiform warts (finger like) are on a long stalk like a thread that usually appear on your eyelids, armpits or neck. Filiform warts commonly appear on the face. Filiform warts are also described as digitate warts.
- Mosaic warts – these grow in clusters and are most common on your hands and feet.
- Mucosal warts – Oral warts can affect the lips and even inside the cheeks, where they may be called squamous cell papillomas. They are softer than cutaneous warts.
Most warts will usually disappear within two years if left untreated, but they can sometimes cause discomfort and can look unpleasant. Warts are also contagious.
You can treat warts if they bother you, keep coming back or are painful. There are treatments available to buy over-the-counter without prescription from pharmacies and some supermarkets. Please speak to your doctor about other treatment options for warts and verrucas.
See a doctor if:
- you’re worried about a growth on your skin
- you aren’t sure whether the growths are warts
- the growths are bothersome and interfere with activities
- you also have a weakened immune system because of immune-suppressing drugs, HIV/AIDS or other immune system disorders
- you have a wart or verruca that keeps coming back
- you have a very large or painful wart or verruca
- a wart bleeds or changes in how it looks
- you have a wart on your face or genitals
- the growths are painful or change in appearance or color
- you’ve tried treating the warts, but they persist, spread or recur
Are warts contagious
Yes. Warts are caused by a virus known as the human papilloma virus (HPV) and warts can be spread to other people from contaminated surfaces or through close skin contact. You’re more likely to spread a wart or verruca if your skin is wet or damaged.
It can take months for a wart or verruca to appear after contact with the virus.
Mucosal HPV is spread mainly by direct skin-to-skin contact during vaginal, oral, or anal sexual activity. It’s not spread through blood or body fluids. It can be spread even when an infected person has no visible signs or symptoms.
Anyone who has had sexual contact can get HPV, even if it was only with only one person, but infections are more likely in people who have had many sex partners.
The virus can also be spread by genital contact without sex, but this is not common. Oral-genital and hand-genital spread of some genital HPV types have been reported. And there may be other ways to become infected with HPV that aren’t yet clear.
You DO NOT get HPV from:
- Toilet seats
- Hugging or holding hands
- Swimming in pools or hot tubs
- Sharing food or utensils
- Being unclean
Transmission from mother to newborn during birth is rare, but it can happen, too. When it does, it can cause warts (papillomas) in the infant’s breathing tubes (trachea and bronchi) and lungs, which is called respiratory papillomatosis. These papillomas can also grow in the voice box, which is called laryngeal papillomatosis. Both of these infections can cause life-long problems.
DO
- wash your hands after touching a wart or verruca
- change your socks daily if you have a verruca
- cover warts and verrucas with a plaster when swimming
- take care not to cut a wart when shaving
DON’T
- share towels, flannels, socks or shoes if you have a wart or verruca
- bite your nails or suck fingers with warts on
- walk barefoot in public places if you have a verruca
- scratch or pick a wart
Warts are particularly common in:
- School-aged children, but they may arise at any age
- Eczema (dermatitis), due to a defective skin barrier
- People who are immune suppressed with medications such as azathioprine or cyclosporin, or with human immunodeficiency virus (HIV) infection. In these patients, the warts may never disappear — despite treatment.
No treatment is universally effective at eradicating viral warts. In children, even without treatment, 50% of warts disappear within 6 months, and 90% are gone in 2 years. They are more persistent in adults but they clear up eventually. They are likely to recur in patients that are immune suppressed, e.g, organ transplant recipients. Recurrence is more frequent in tobacco smokers.
Viral warts are very widespread in people with the rare inherited disorder epidermodysplasia verruciformis.
Malignant change is rare in common warts, and causes verrucous carcinoma.
Oncogenic strains of HPV, the cause of some anogenital warts and warts arising in the oropharynx, are responsible for intraepithelial and invasive neoplastic lesions including cervical, anal, penile and vulval cancer.
Figure 1. Warts on hands
Figure 2. Wart on finger
Figure 3. Warts on face
Figure 4. Filiform warts
Figure 5. Wart on foot
Figure 6. Flat warts
Figure 7. Periungual warts are warts about the nails. They are particularly common in children who bite their nails or pick at their cuticles.
What causes warts
Common warts are caused by an infection with the human papillomavirus (HPV). More than 200 types of human papillomavirus (HPV) exist, but only a few cause warts or papillomas on your hands, which are non-cancerous tumors. The most common subtypes of human papillomavirus (HPV) are types 2, 3, 4, 27, 29, and 57. Human papillomavirus (HPV) is spread by direct skin-to-skin contact or autoinoculation. This means if a wart is scratched or picked, the viral particles may be spread to another area of skin. The incubation period can be as long as twelve months.
Other types of human papillomavirus (HPV) are more likely to cause warts on your feet and other areas of your skin and mucous membranes. Most types of HPV cause relatively harmless conditions such as common warts, while others about 40 of those human papillomavirus (HPV) types affect the genitals and may cause serious disease such as cancer of the cervix. Genital warts are spread through sexual contact (sexually transmitted infections) with an infected partner. Some of those can put you at risk or known to cause cancer, including cancers of the cervix (the base of the womb at the top of the vagina), vagina, vulva (the area around the outside of the vagina), penis, anus, and parts of the mouth and throat. Women are somewhat more likely than men to develop genital warts. Like warts that appear elsewhere on your body, genital warts are caused by the human papillomavirus (HPV). Some strains of genital HPV can cause genital warts, while others can cause cancer. About 14 million new genital HPV infections occur each year 1. In fact, the Centers for Disease Control and Prevention (CDC) estimates that more than 90% and 80%, respectively, of sexually active men and women will be infected with at least one type of HPV at some point in their lives 2. Around one-half of these infections are with a high-risk HPV type 3. Vaccines can help protect against certain strains of genital HPV.
You can get warts from skin-to-skin contact with people who have warts. If you have warts, you can spread the virus to other places on your own body. You can also get the wart virus indirectly by touching something that another person’s wart touched, such as a towel or exercise equipment. The virus usually spreads through breaks in your skin, such as a hangnail or a scrape. Biting your nails also can cause warts to spread on your fingertips and around your nails.
Each person’s immune system responds to the HPV virus differently, so not everyone who comes in contact with HPV develops warts.
Figure 8. Genital warts in mouth
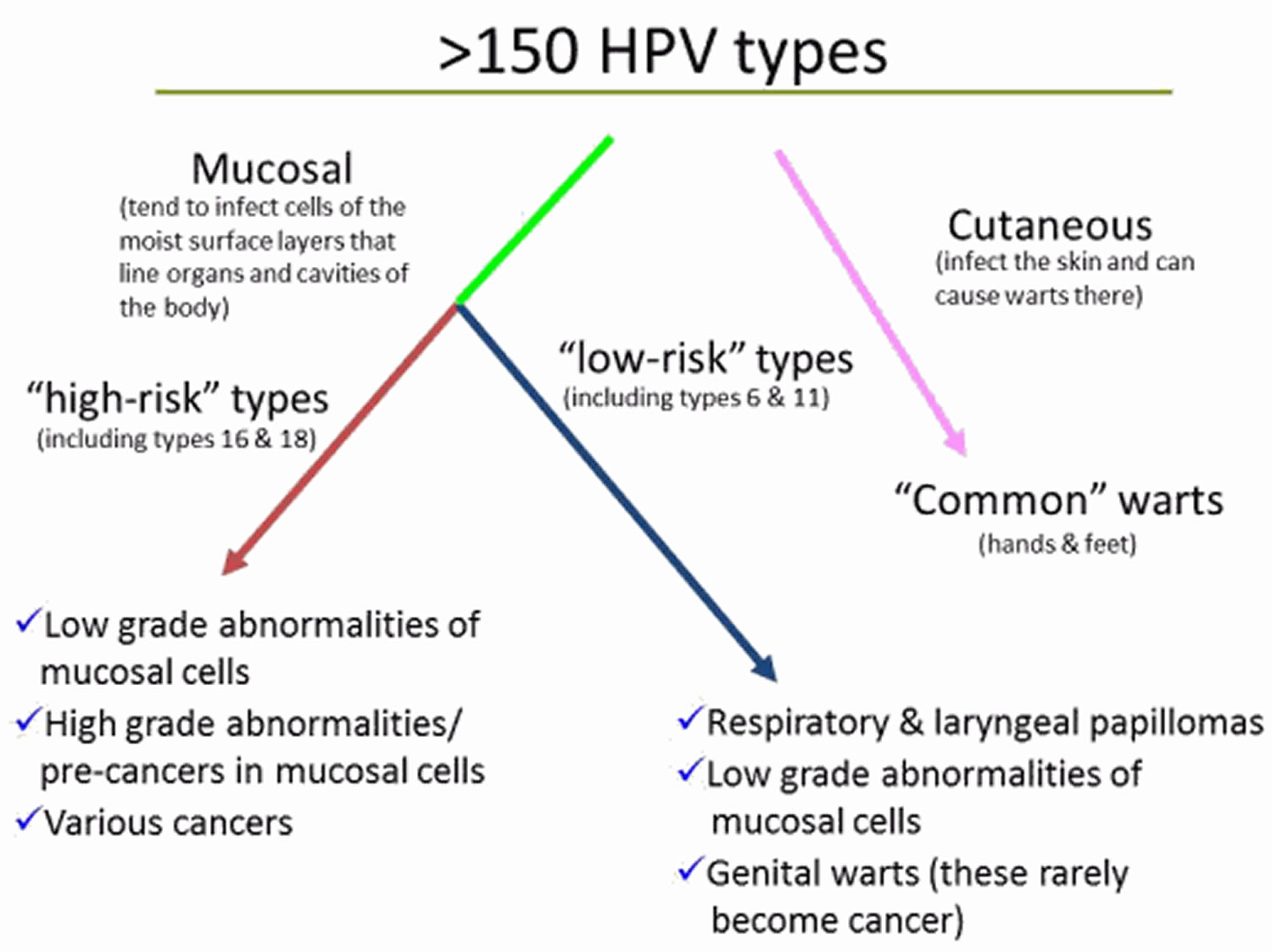
This diagram shows the different groups of human papillomavirus (HPV) types and the problems each group can cause.
Risk factors for common warts
People at higher risk of developing common warts include:
- Children and young adults
- People with weakened immune systems, such as those with HIV/AIDS or people who’ve had organ transplants.
To reduce your risk of common warts:
- Avoid direct contact with warts. This includes your own warts.
- Don’t pick at warts. Picking may spread the virus.
- Don’t use the same emery board, pumice stone or nail clipper on your warts as you use on your healthy skin and nails.
- Don’t bite your fingernails. Warts occur more often in skin that has been broken. Nibbling the skin around your fingernails opens the door for the virus.
- Groom with care. Use a disposable emery board. And avoid brushing, clipping or shaving areas that have warts. If you must shave, use an electric razor.
- Wash your hands carefully after touching your warts or surfaces such as shared exercise equipment.
HPV is very common, so the only way to keep from becoming infected may be to completely avoid any contact of the areas of your body that can become infected (like the mouth, anus, and genitals) with those of another person. This means not having vaginal, oral, or anal sex, but it also means not allowing those areas to come in contact with someone else’s skin.
HPV vaccines can prevent infection with the types of HPV most likely to cause cancer and genital warts, although the vaccines are most effective when given at a younger age (in older children and teens). The Food and Drug Administration (FDA) has approved three vaccines to prevent HPV infection: Gardasil®, Gardasil® 9, and Cervarix®. These vaccines provide strong protection against new HPV infections, but they are not effective at treating established HPV infections or disease caused by HPV 4. Anecdotally, HPV vaccines have been reported to result in clearance of non-genital warts in some people.
If you are sexually active, limiting the number of sex partners and avoiding sexual activity with people who have had many other sex partners can help lower your risk of exposure to genital HPV. But again, HPV is very common, so having sexual contact with even one other person can put you at risk.
Condoms can offer some protection from HPV infection, but HPV might be on skin that’s not covered by the condom. And condoms must be used every time, from start to finish. The virus can spread during direct skin-to-skin contact before the condom is put on, and male condoms don’t protect the entire genital area, especially for women. The female condom covers more of the vulva in women, but hasn’t been studied as carefully for its ability to protect against HPV. Condoms are very helpful, though, in protecting against other infections that can be spread through sexual activity.
It’s usually not possible to know who has a mucosal HPV infection, and HPV is so common that even using these measures doesn’t guarantee that a person won’t get infected, but they can help lower the risk.
Tests are rarely needed to diagnosis viral warts, as they are so common and have a characteristic appearance.
- Pinpoint dots (clotted capillaries) are revealed when the top of the wart is removed.
- Dermatoscopic examination is sometimes helpful to distinguish viral warts from other verrucous lesions such as seborrhoeic keratosis and skin cancer.
- Sometimes, viral warts are diagnosed on skin biopsy. The histopathological features of verruca vulgaris differ from that of plane warts.
How to get rid of warts
Many people don’t bother to treat viral warts because treatment can be more uncomfortable than the warts—they are hardly ever a serious problem. Warts that are very small and not troublesome can be left alone and in some cases they will regress on its own.
However, warts may be painful, and they often look ugly so cause embarrassment.
To get rid of them, you have to stimulate your body’s own immune system to attack the wart virus. Persistence with the treatment and patience is essential!
Topical treatment
Topical treatment includes wart paints containing salicylic acid or similar compounds, which work by removing the dead surface skin cells. Podophyllin is a cytotoxic agent used in some products, and must not be used in pregnancy or in women considering pregnancy.
The paint is normally applied once daily. Treatment with wart paint usually makes the wart smaller and less uncomfortable; 70% of warts resolve within twelve weeks of daily applications.
- Soften the wart by soaking in a bath or bowl of hot soapy water.
- Rub the wart surface with a piece of pumice stone or emery board.
- Apply wart paint or gel accurately, allowing it to dry.
- Covered with plaster or duct tape.
If the wart paint makes the skin sore, stop treatment until the discomfort has settled, then recommence as above. Take care to keep the chemical off normal skin.
Cryotherapy
Cryotherapy is normally repeated at one to two–week intervals. It is uncomfortable and may result in blistering for several day or weeks. Success is in the order of 70% after 3-4 months of regular freezing.
A hard freeze using liquid nitrogen might cause a permanent white mark or scar. It can also cause temporary numbness.
An aerosol spray with a mixture of dimethyl ether and propane (DMEP) can be purchased over the counter to freeze common and plantar warts. It is important to read and follow the instructions carefully.
Combining Immunotherapy with cryotherapy reduces the number of cryotherapy sessions.
Electrosurgery
Electrosurgery (curettage and cautery) is used for large and resistant warts. Under local anaesthetic, the growth is pared away and the base burned. The wound heals in two weeks or longer; even then 20% of warts can be expected to recur within a few months. This treatment leaves a permanent scar.
Other treatments
Other experimental treatments for recurrent, resistant or extensive warts include:
- Topical retinoids, such as tretinoin cream or adapalene gel
- The immune modulator, imiquimod cream
- Fluorouracil cream
- Bleomycin injections
- Oral retinoids
- Pulsed dye laser destruction of feeding blood vessels
- Photodynamic therapy
- Laser vaporisation
- H2 receptor antagonists
- Oral zinc oxide and zinc sulfate
- Applications of raw garlic or tea tree oil
- Immune stimulation using diphencyprone, squaric acid
- Immunotherapy with Candida albicans or tuberculin PPD
- Hypnosis
- Hyperthermia
- Occlusion with duct tape
Flat wart treatment
- Treatment is not needed. Flat warts have the highest frequency of spontaneous resolution of all warts so observation is appropriate.
- Freezing is okay but caution about color change and that kids don’t like the treatment.
- Sunscreen if in sun-exposed area.
- Tretinoin nightly or imiquimod nightly or alternate the two.
- 5-fluorouricil 5% topically applied twice daily.
- Curettage in appropriate setting.
- Laser therapy
Liquid nitrogen therapy every 1-3 weeks may be performed until all lesions have resolved. If on the legs, cessation of shaving is preferred. If in a sun-exposed area, sun protection is desirable, as it may be that UV suppresses the immune system and prolongs the condition. Topical imiquimod nightly may be tried.
Topical imiquimod every other night alternating with a topical retinoid (e.g., tretinoin) the other nights may be beneficial. Other therapies that have been tried include 5-FU 5% topically applied twice daily for 2-3 weeks. The patient must be informed of all the typical side effects. Topical imiquimod 3 times per week completely cleared the recalcitrant, facial, flat warts after 3 weeks.
Topical immunotherapy with diphenylcyclopropenone was successfully used in one case 5.
Lidocaine followed by light curettage is appropriate and effective in older patients (not young children who don’t like needles), and when the warts are fewer in number. Treatment every 3-4 weeks until gone may be done.
The YAG laser has been employed successfully for flat warts. Photodynamic therapy (PDT) utilises photosensitising agents, oxygen and light, to create a photochemical reaction that selectively destroys cancer cells. Photosensitising agents are drugs that are administered into the body through topical, oral or intravenous methods. In the body, they concentrate in cancer cells and only become active when light of a certain wavelength is directed onto the area where the cancer is. The photodynamic reaction between the photosensitising agent, light and oxygen kills the cancer cells. Photodynamic therapy (PDT) is commonly used and 10% ALA (nanoemulsion formulation containing 10% aminolaevulinic acid hydrochloride) is particularly beneficial 6. The pulsed dye laser was used to treat recalcitrant flat, common, plantar/palmar and periungual warts in one study 7. Flat warts were most responsive.
Oral isotretinoin 30 mg/day for 12 weeks cleared all 16 patients (15 placebo) in a randomized, blinded study 8.
Plantar wart removal
How to get rid of plantar warts
- Observation with intermittent paring to prevent pain.
- Salicylic acid
- Cryotherapy
- Lidocaine, then curettage.
- 5-fluorouricil under occlusion
Observation
Plantar warts need not be treated. Plantar warts can be painful depending upon their thickness and location. The patient should be encouraged to do periodic paring if this is the case.
Salicylic Acid
The wart may be treated alone with salicylic acid by the patient/parent. The patient/parent may be told to do the following:
Do the following for any warts NOT on the face or anogenitals: Soak the wart in water for 5-10 minutes and then abrade the surface with e.g., a pumice stone or emery board, to remove the surface white layer. Let dry and then apply two to four drops of 17% salicylic acid (e.g., DuoFilm) directly to the wart once a day. Each drop should be permitted to dry before the next is added. Try to keep the salicylic acid off normal skin. When finished, you can cover with a bandage or duct tape. Repeat daily. If the wart gets significantly inflamed (e.g., red and tender), hold treatment on that lesion and wait to see if the wart goes away. Sometimes when the body succeeds in killing the wart, the wart will suddenly turn black and then fall off in several days.
Alternatively, the application daily of salicylic acid and paring every 2-3 days is a helpful adjunct to cryotherapy. This is because lesions on the soles are driven deep into the skin by the pressure of walking. Removing the hyperkeratotic covering helps expose the wart to therapy. Some suggest the higher the concentration (going as high as 50%), the better. See also combination of SA and imiquimod below in imiquimod section.
Salicylic Acid and 5-Fluorouricil
The combination of 5-Fluorouricil and Salicylic Acid is an effective and beneficial therapy for common and plantar warts 9. WartPeel is one such product.
Paring, Cryotherapy
For these and a variety of other treatment options, see verruca.
Aggressive Curettage
Often, plantar warts are resistant to cryotherapy. One useful technique is to anesthetize first with lidocaine (warn patients that this is painful) and then use a disposable, very sharp curette to core out the wart. Bleeding will occur but can be controlled with light electrocautery or a topical hemostatic agent (e.g., aluminum chloride). Then, a light freeze to the base should be done. This procedure is more aggressive and the patient should agree to the increased pain and longer healing time. S/he should be told of the hole that is created and the potential for limping for a few days. Due to the longer healing time, this procedure may be repeated monthly.
5-Fluorouracil
In a study comparing 5% 5-Fluorouricil cream under tape occlusion versus tape occlusion alone in 40 patients with plantar warts 10, the following was found: “Nineteen out of 20 patients (95%) randomized to 5% 5-FU with tape occlusion had complete eradication of all plantar warts within 12 weeks of treatment. The average time to cure occurred at 9 weeks of treatment. Three patients (15%) had a recurrence at the 6-month follow-up visit; accordingly, an 85% sustained cure rate was observed. It is concluded that use of topical 5% 5-fluorouracil cream for plantar warts is safe, efficacious, and accepted by the patient.”
Adapalene
In a study of 50 patients with 424 plantar warts treated with adapalene gel 0.1% twice daily under occlusion using plastic wrap or weekly cryotherapy 11, the following was found: all the warts in 24 of 25 patients treated with adapalene disappeared in an average of 37 ± 19 days. All the warts in 24 of 25 patients treated with cryotherapy disappeared in 52 ± 30 days in an average of 1.88 sittings of cryo-therapy. During the study, the patients were seen weekly and and it appears from the report that paring was done at those visits. Also, the cryotherapy was performed for 1-2 minutes using an N2O gas operated machine at a temperature of −94°C. The authors postulate that the treatment works by inducing cell-mediated immunity against the wart 12.
Verruca Vulgaris Warts Treatment
- Observe
- Cryotherapy every 1-3 weeks
- Intralesional injection Candida
- Intralesional injection MMR vaccine
- Intralesional injection Vitamin D
- Topical 5-Fluorouracil (5-FU) nightly
- Salicylic Acid 17% home treatment (see plantar warts)
- Squaric Acid
- Measure serum zinc level and treat if low.
- Lidocaine followed by curettage, then freezing base (see plantar warts)
- Laser
Observation
No treatment is needed for these benign lesions. However, they are contagious, both to the patient and to others.
Cryotherapy
The mainstay of treatment is cryotherapy performed every 2-3 weeks. A single 10 second freeze seems optimum, based upon studies (see below). A second freeze-thaw added benefit only for plantar warts in one study 13. Waiting more than 3 weeks between treatments allows the wart time to grow back. Two weeks between treatments seems to be optimum for most patients. However, one study of external genital warts 14 found that double freeze-thaw every 7-8 days required fewer sessions and cleared quicker than every 14-21 days.
It is not unusual for the patient to need 6-10 treatments in order to clear the warts. Thus, the patient should be told that one treatment rarely does it–multiple treatments are needed.
Freeze Longer?
An interesting study compared the traditional freeze-thaw (freeze until the wart and a surrounding 1-2 mm halo of normal skin turns white and then stop) to a 10-second freeze (same as traditional, but keep spraying to keep white for 10 seconds) each done every 2 weeks for a maximum of 5 weeks 15. The 10-second freeze was significantly more effective and cleared 64% of non-defaulters compared to 39% in the traditional group. There was more pain, blistering and other side effects, however. Some patients are exquisitely sensitive to cryotherapy and this seems to be idiosyncratic. Thus, perhaps the best approach is to use the traditional method on the first visit and move up to 10 seconds on subsequent visits as tolerated. An alternative published approach is to remove the tip from the cryogun, making it a cryoblast. This increased clearance rates in one study.
Freezing in Children
The use of the spray gun can be frightening to children. A good alternative is to use a cup of the liquid nitrogen to soak a hemostat or forceps for fifteen seconds, then grab the wart for ten seconds. There is no scary spray, nor dripping of the liquid nitrogen (compared with using a cotton-tipped applicator).
Candida Antigen Injection
Immunotherapy with candida antigen is a safe and effective treatment of warts in children. The main drawback is the pain and fear experienced by the patient. In one retrospective review of 220 children who were treated with intralesional injection of Candida every 3 weeks 16, 70% of treated wart cleared in an average of 2.73 treatments. The cure rate is high, but all warts may need to be treated for complete clearing.
MMR Antigen Injection
Using the MMR vaccine instead of the Candida antigen seems just as effective. In one study, the MMR vaccine 0.5 cc was injected intralesionally into each wart in the MMR group, whereas normal saline was used in the second group. These injections were repeated every 2 weeks for a maximum of 3 injections. Eighteen of 24 patients cleared in the MMR group (75%) vs. only 6 of 24 in the saline group (25%) 17.
Intralesional Vitamin D
In a recent study, intralesional injections of 0.2- to 0.5-mL vitamin D3 solution (600,000 IU; 15 mg/mL) at 3-week intervals were used to treat recalcitrant warts in 60 patients. The majority of patients (90%) had complete clearing. Complete resolution required an average of 3.66 injections. Of the 35% of patients with distant warts, all experienced complete resolution of these in addition to resolution of the primary lesion. Up to 5 warts were injected at each visit 18.
Intralesional Bleomycin
Intralesional bleomycin can be highly efficacious, even for treatment-resistant warts. Usually the 1 U/ml concentration is used, and the wart injected till it blanches. 0.1-0.2 ml per wart is typical. Pain can be significant and last up to a week. The patient should be told to expect the wart to turn black several days after treatment and then falls off in 2-4 weeks. Treatment may be done every 3 weeks, but at most 2 treatments are usually needed. Warts on the fingers may not be best suited for Bleomycin as nail dystrophy, Raynauds and even digital necrosis are rare side effects there.
5-Fluorouracil
5-FU may be applied to a wart nightly. (Off label). In a study of 39 children treated with 5-FU once or twice daily under occlusion for 6 weeks 19 the following was found: “Eighty-eight percent of treated warts improved after 6 weeks of treatment, and 41% of subjects had complete resolution of at least one wart. Treatment response did not differ between once or twice daily applications. Tolerability and patient satisfaction were excellent. No subject had clinically significant blood levels of 5-fluorouracil. At 6 month follow-up, 87% of complete responders had no wart recurrence. Topical 5% 5-fluorouracil is a safe, effective, and well-tolerated treatment for warts in children.”
5-FU can cause pigmentation of the nail (usually reversible). See periungual warts. Some combine 5-FU with imiquimod, one in the morning and one at night.
Duct Tape
Occluding a digital wart with duct tape for 6.5 days to make it “mushy” (and some theorize better allowing the immune system to recognize the wart) can be effective. On the seventh day, the duct tape is removed and the wart pared down and allowed to dry. The tape is then reapplied. Repeat as necessary as long as progress is being made.
Laser
The CO2 or pulsed dye laser is often employed in recalcitrant cases.
Cidofovir
3% cidofovir cream applied twice daily with occlusion for a period of about 12 weeks completely cleared 53% of recalcitrant warts in one study 20. This included patients with genital, periungual and plantar warts. Local irritation erythema and/or pruritus occurred in about 14% of patients. Topical 3% cidofovir has also been used with success in immunocompromised children applied daily and occluded 21.
Ignemol for warts
Ingenol mebutate appears highly effective in the treatment of anogenital warts with just one application. In one report of 10 patients using either 0.015% or 0.05% ingenol mebutate (IM) or placebo, all warts cleared within 3-7 days. No sites treated with vehicle cleared. There were no recurrences in three months at sites which cleared. There was mild to moderate burning x 1-2 days 22. In a similar study 23, a single application of either 0.015% or 0.05% gel cleared 13/17 patients with anogenital warts. Up to three applications cleared 16/17.
Imiquimod
Imiquimod has been used in recalcitrant warts in various locations in children. Sixteen of 18 children cleared with twice daily therapy after a mean of 6 months of use 24. In another study compared with cryotherapy every 2 weeks, plantar warts in children were more likely to clear with imiquimod and salicylic acid compared with cryotherapy alone (83% vs 30% clearance at 3 months) 25. Specifically the parentrs applied 5% imiquimod every morning for 5 days/week and filling of warts every evening followed by 15% salicylic acid.
Squaric Acid
The topical application of squaric acid induces an allergic contact dermatitis and can clear recalcitrant warts in children. A retrospective chart review 26 found that 40 of 48 (83%) patients in whom treatment outcomes could be obtained reported complete resolution of their warts. Age range was 3-18 years, and the average treatment duration was 6-12 months. Various protocols are used [e.g., The Permanente Medical Group 27].
Adapalene
One study showed 24 of 25 plantar warts cleared in 37 ± 19 (56-17) days with topical adapalene 0.1% gel applied twice daily under occlusion using plastic wrap 28.
Salicylic Acid, 5-Fluorouracil and Imiquimod for Plantar Warts
One may pare the top of the plantar wart and then treat with salicylic acid and 5-fluorouracil plaster in the morning and imiquimod under occlusion nightly for 8 to 12 weeks.
Zinc
Topical, oral and intralesonal zinc have been used successfully for warts as reported in a variety of small studies. Indeed, zinc deficiency appears to be associated with treatment-resistant warts 29. Measuring serum zinc and if low, treating with one of the above regimens appears reasonable. Nausea is the main potential side effect of oral zinc.
In one placebo-controlled trial, oral zinc at a dose of 10 mg/kg/day up to 600 mg/day resulted in complete clearance of warts in 20 patients (86.9%) after 2 months of treatment compared with zero in the placebo group. However, it must be noted that all patients were zinc deficient and according to the article “the response to treatment was directly related to the increment in serum zinc level” 30. In another randomized study 31, 78.1% (25/32) of patients cleared after a 2-month course of treatment with zinc sulfate 10 mg/kg/day up to 600 mg/day compared to 13% (3/23) in the control group.
In one study of vulvar warts, the addition of 400 mg oral zinc sulfate daily to crotherapy, podophyllin or imiquimod did not speed clearance, but did reduced recurrence 32.
Relapse after successful wart treatment
Pulsed dye laser induces the lowest rate of recurrence of plantar warts, as compared to other treatments (e.g. freezing, CO2, keratolytics). There is a higher risk of relapse of non-genital warts in subjects older than 25 years and a 5-fold increased risk in smokers, as compared to non-smokers. Smoking is also related to time to initial healing and to time to complete healing at follow-up 33.
Periungual warts treatment
Periungual warts are warts about the nails. They are particularly common in children who bite their nails or pick at their cuticles.
- Freezing
- Duct tape
- Intralesional Candida
- Topical fluorouracil
- Laser
- Intralesional bleomycin
The patient must be told that any destructive treatment of the wart may result in permanent nail dystrophy. See common wart treatment ideas above as well.
Cryotherapy, observation, and Candida injection may all be done.
Duct Tape
A benign therapy which has been reported to work is to wrap the finger with duct or other occlusive tape first longitudinally and then circumferentially twice. Have the patient remove the tape in 6.5 days and leave off for 12 hours. Then reapply. Tell the patient you are trying to “smother” the wart 34. Chronic warts unresponsive to therapy, especially in patients over 25 years of age, should be biopsied to rule out squamous cell carcinoma.
Lidocaine, Then Curettage with a Disposable Curette
This destructive procedure is aggressive, but can be very effective for periungual warts. It is often performed every month. The patient must accept a significant hole that will need to fill in. Bleeding, infection, and scarring are potential sequelae. As noted above, permanent nail dystrophy may follow. The area is cleansed, then infiltrated with lidocaine (okay to use epinephrine) and then curettage performed with a disposable curette (disposable curettes are sharper than reusable). Bleeding may be controlled with aluminum chloride and light cautery. Light cryotherapy may be done after all the visible wart is removed. The patient should keep the digit covered and greasy, with e.g., Vaseline, until healed. Clean with soap and water daily.
Intralesional Immunotherapy
One to several warts may be injected with either Candida or other agents to stimulate the immune system. One study 35 used Mycobacterium w vaccine. Twenty-eight out of 30 patients with a variety of warts including periungual were completely cleared. Their method as paraphrased is as follows: Injection was done with 0.1 ml of killed Mycobacterium w vaccine intralesionally in a single wart. Thereafter, a single injection of 0.1 ml of vaccine was given at intervals of four weeks in a single wart until there was complete resolution of the warts or a maximum of 10 injections. Treatment was stopped if there was no response after three injections.”
Topical Fluorouracil
Topical 5-FU can clear periungual warts. The 5% cream is applied nightly to each wart. Pigmentation of the nail may rarely occur (see image below) 36.
Cidofovir
3% cidofovir cream applied twice daily with occlusion for a period of about 12 weeks completely cleared 53% of recalcitrant warts in one study 20. This included patients with genital, periungual and plantar warts. Local irritation erythema and/or pruritus occurred in about 14% of patients. Topical 3% cidofovir has also been used with success in immunocompromised children applied daily and occluded 21.
Laser
Various lasers have been used.
Intralesional Bleomycin
See Management of ungual warts 37
- Satterwhite CL, Torrone E, Meites E, et al. Sexually transmitted infections among US women and men: Prevalence and incidence estimates, 2008. Sexually Transmitted Diseases 2013; 40(3):187-193. https://www.ncbi.nlm.nih.gov/pubmed/23403598[↩]
- Chesson HW, Dunne EF, Hariri S, Markowitz LE. The estimated lifetime probability of acquiring human papillomavirus in the United States. Sexually Transmitted Diseases 2014; 41(11):660-664. https://www.ncbi.nlm.nih.gov/pubmed/25299412[↩]
- Hariri S, Unger ER, Sternberg M, et al. Prevalence of genital human papillomavirus among females in the United States, the National Health and Nutrition Examination Survey, 2003–2006. Journal of Infectious Diseases 2011; 204(4):566–573. https://www.ncbi.nlm.nih.gov/pubmed/21791659[↩]
- Schiller JT, Castellsague X, Garland SM. A review of clinical trials of human papillomavirus prophylactic vaccines. Vaccine 2012; 30 Suppl 5:F123-138. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4636904/[↩]
- Eur J Derm 1998;8;488[↩]
- JEADV 2016;30;1700[↩]
- Cutis 1995;56;230[↩]
- J Dermatol Treatment 2015;26;78-82[↩]
- J Dtsch Dermatol Ges. 2004 Mar;2(3):187-93[↩]
- J Drugs Dermatol. 2006 May;5(5):418-24[↩]
- Indian J Dermatol. 2015;60;102[↩]
- Indian J Dermatol. 2011;56;513[↩]
- BJD 1994;131;883[↩]
- Dermatologica Sinica 2014;32;154-156[↩]
- BJD 2001;145;554[↩]
- Pediatr Dermatol 2015 Sep 07[↩]
- Adv Biomed Res. 2014 Mar 31;3:107[↩]
- J Cutan Med Surg 2017 Apr 06[↩]
- Pediatr Dermatol. 2009 May-Jun;26(3):279-85[↩]
- JEADV 2016;30;1218[↩][↩]
- PD 2017;34;e24[↩][↩]
- J Invest Dermatol 2014;134:S90-107[↩]
- JEADV 2016;30;1041[↩]
- Ped Dermatol 2002 May-Jun;19(3):263-6[↩]
- J Dermatolog Treat 2016 Jan 01;27;80-82[↩]
- Pediatr Dermatol. 2015 Jan-Feb;32(1):85-90[↩]
- https://mydoctor.kaiserpermanente.org/ncal/Images/Squaric%20Acid%20protocal%20for%20Warts_tcm75-456602.pdf[↩]
- Indian Journal of Dermatology, Vol. 60, No. 1, January-February 2015, pp. 102[↩]
- J Coll Physicians Surg Pak. 2010 Feb;20(2):83-6[↩]
- Br J Dermatol 2002;146:423[↩]
- JAAD 2009;60;706[↩]
- J Obstet Gynaecol Res. 2014 Oct;40(10):2110-3[↩]
- JEADV 2017;31;712[↩]
- Cutis 1978;22;673[↩]
- J Cutan Aesthet Surg. 2014 Oct-Dec; 7(4): 203–208[↩]
- BJD 1985;112:621[↩]
- Management of ungual warts. Dermatol Ther. 2012 Nov-Dec;25(6):545-50. doi: 10.1111/j.1529-8019.2012.01509.x. http://onlinelibrary.wiley.com/wol1/doi/10.1111/j.1529-8019.2012.01509.x/full[↩]
















