What is a diaphragm
The diaphragm is the major muscles of respiration. And the other respiratory muscles are the intercostal muscles.
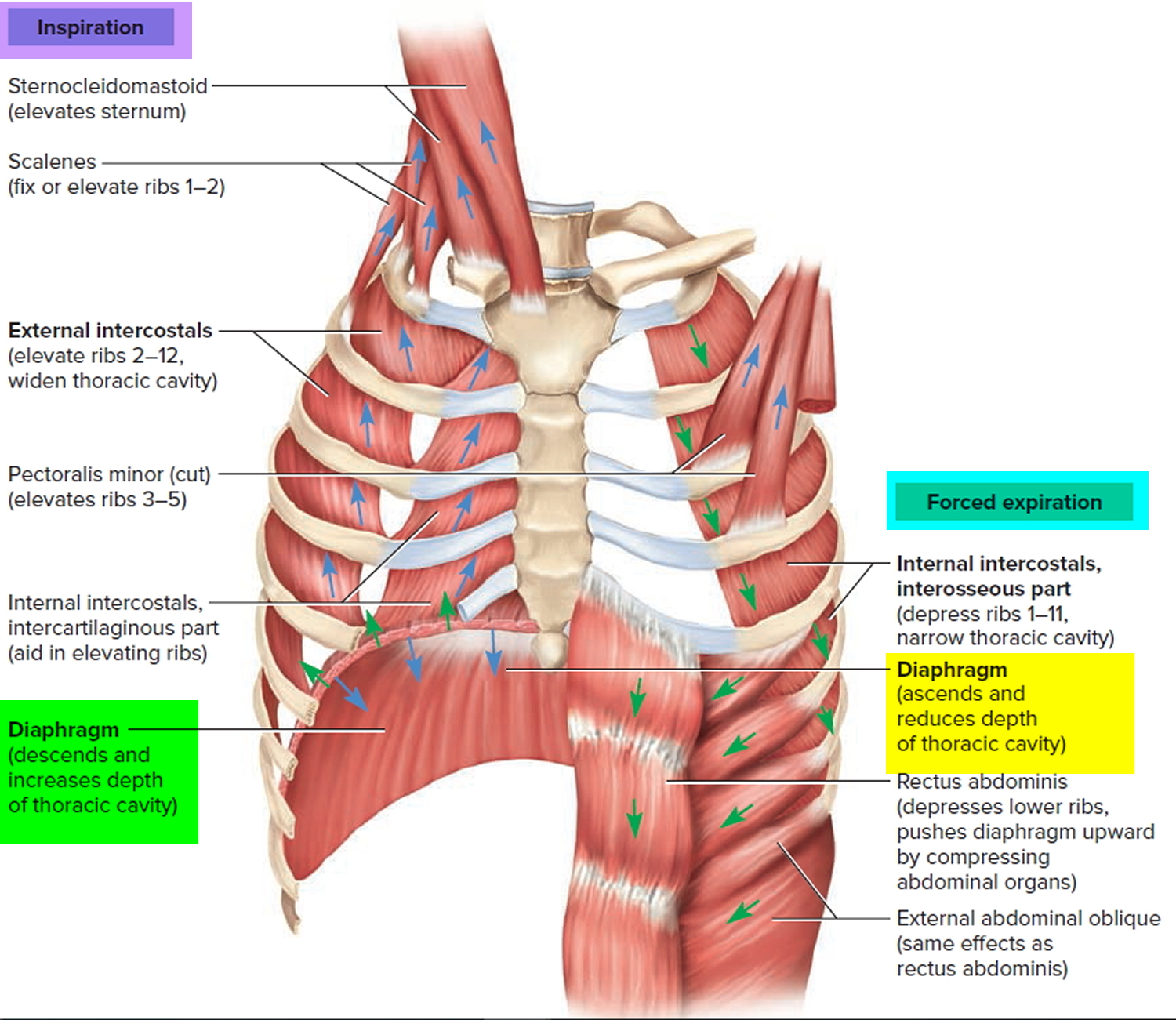
Breathing in is called inhalation (inspiration). Just before each inhalation, the air pressure inside the lungs is equal to the air pressure of the atmosphere, which at sea level is about 760 millimeters of mercury (mmHg), or 1 atmosphere (atm). For air to flow into the lungs, the pressure inside the lung (lungs alveoli) must become lower than the atmospheric pressure. This condition is achieved by increasing the size of the lungs. For inhalation to occur, the lungs must expand, which increases lung volume and thus decreases the pressure in the lungs to below atmospheric pressure. The first step in expanding the lungs during normal quiet inhalation involves contraction of the main muscle of inhalation, the diaphragm, with resistance from external intercostal muscles.
The most important muscle of inhalation is the diaphragm, the dome-shaped skeletal muscle that forms the floor of the thoracic cavity (Figure 1). It is innervated by fibers of the phrenic nerves, which emerge from the spinal cord at cervical levels 3, 4, and 5. When relaxed, the diaphragm bulges upward to its farthest extent, pressing against the base of the lungs. Contraction of the diaphragm causes it to flatten, lowering its dome. This increases the vertical diameter of the thoracic cavity and lowers its internal pressure and produces an inflow of air. During normal quiet inhalation, the diaphragm descends about 1-1.5 cm (0.4 in.), producing a pressure difference of 1–3 mmHg and the inhalation of about 500 mL of air. In strenuous breathing, the diaphragm may descend 10-12 cm (4 in.), which produces a pressure difference of 100 mmHg and the inhalation of 2–3 liters of air. Contraction of the diaphragm is responsible for about 75% of the air that enters the lungs during quiet breathing. Advanced pregnancy, excessive obesity, or confining abdominal clothing can prevent complete descent of the diaphragm. When the diaphragm relaxes, it bulges upward again, compresses the lungs and expels air.
Figure 1. Diaphragm muscle
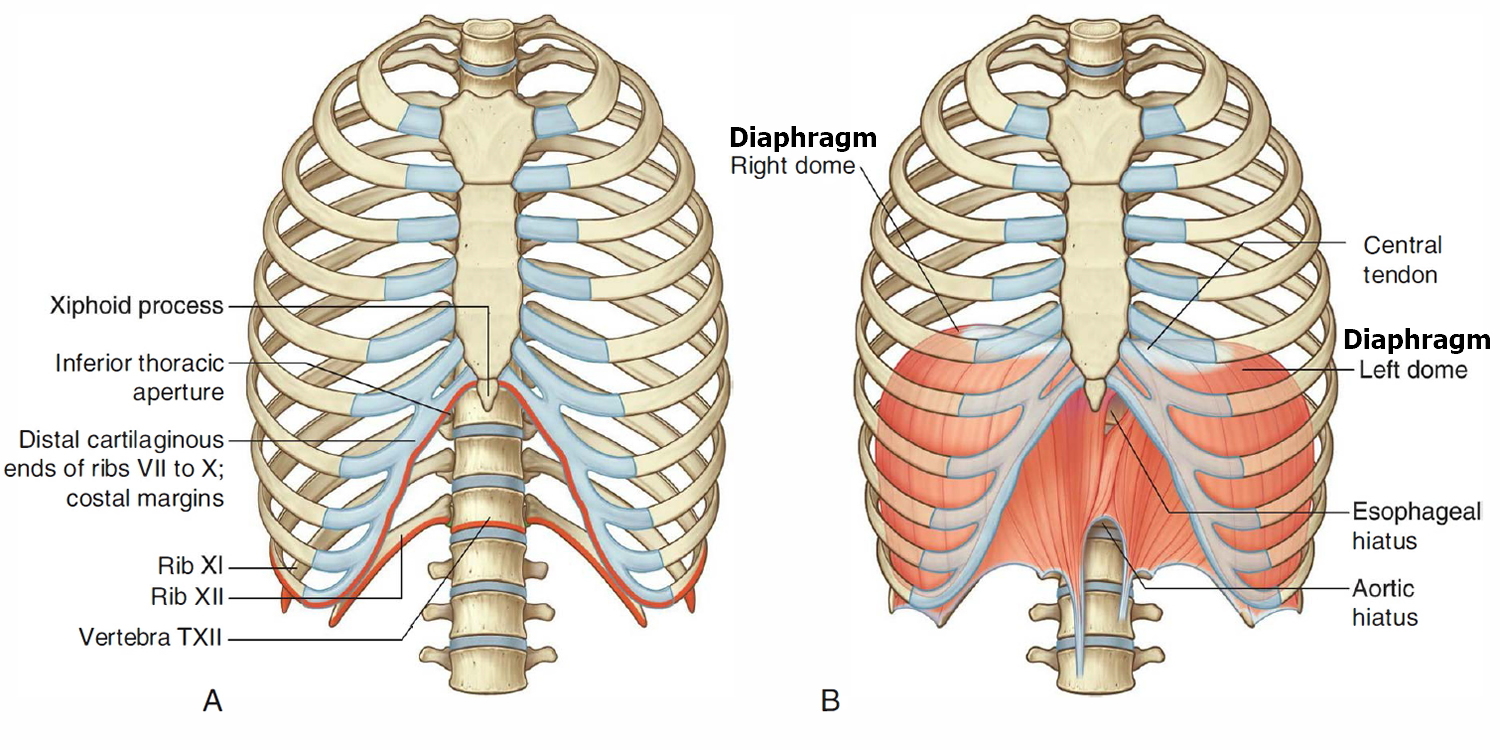 Note: A. Inferior thoracic aperture. B. Diaphragm.
Note: A. Inferior thoracic aperture. B. Diaphragm.The next most important muscles of inhalation are the external intercostal muscles. When these muscles contract, they elevate the ribs (Figure 2). As a result, there is an increase in the anteroposterior and lateral diameters of the chest cavity. Contraction of the external intercostal muscles is responsible for about 25% of the air that enters the lungs during normal quiet breathing.
Several other muscles aid the diaphragm as synergists. Chief among these are the internal and external intercostal muscles between the ribs. Their primary function is to stiffen the thoracic cage during respiration and prevent it from caving inward when the diaphragm descends. However, they also contribute to enlargement and contraction of the thoracic cage and add about one-third of the air that ventilates the lungs. During quiet breathing, the scalene muscles of the neck fix ribs 1 and 2 (hold them stationary), while the external intercostal muscles pull the other ribs upward.
Since most ribs are anchored at both ends—by their attachment to the vertebral column at the proximal (posterior) end and their attachment through the costal cartilage to the sternum at the distal (anterior) end—they swing upward like the handles on a bucket and thrust the sternum forward. These actions increase both the transverse (left to right) and anteroposterior diameters of the chest. In deep breathing, the anteroposterior dimension can increase as much as 20%.
Other muscles of the chest and abdomen also aid in breathing, especially during forced respiration; thus they are considered accessory muscles of respiration. Deep inspiration is aided by the erector spinae, which arches the back and increases chest diameter and by several muscles that elevate the upper ribs: the sternocleidomastoids and scalenes of the neck; the pectoralis minor, pectoralis major, serratus anterior, and serratus posterior superior of the chest; and the intercartilaginous part of the internal intercostals (the anterior part between the costal cartilages). Although the scalenes merely fix the upper ribs during quiet respiration, they elevate them during forced inspiration.
Breathing out, called exhalation (expiration), is also due to a pressure gradient, but in this case the gradient is in the opposite direction: The pressure in the lungs is greater than the pressure of the atmosphere. Normal exhalation during quiet breathing, unlike inhalation, is a passive process because no muscular contractions are involved. Instead, exhalation results from elastic recoil of the chest wall and lungs, both of which have a natural tendency to spring back after they have been stretched. Two inwardly directed forces contribute to elastic recoil: (1) the recoil of elastic fibers that were stretched during inhalation and (2) the inward pull of surface tension due to the film of intrapleural fluid between the visceral and parietal pleurae.
Exhalation starts when the inspiratory muscles relax. As the diaphragm relaxes, its dome moves superiorly owing to its elasticity. As the external intercostals relax, the ribs are depressed. These movements decrease the vertical, lateral, and anteroposterior diameters of the thoracic cavity, which decreases lung volume. In turn, the alveolar pressure increases to about 762 mmHg. Air then flows from the area of higher pressure in the alveoli to the area of lower pressure in the atmosphere.
Exhalation becomes active only during forceful breathing, as occurs while playing a wind instrument or during exercise. During these times, muscles of exhalation—the abdominal and internal intercostals—contract, which increases pressure in the abdominal region and thorax. Contraction of the abdominal muscles moves the inferior ribs downward and compresses the abdominal viscera, thereby forcing the diaphragm superiorly. Contraction of the internal intercostals, which extend inferiorly and posteriorly between adjacent ribs, pulls the ribs inferiorly. Although intrapleural pressure is always less than alveolar pressure, it may briefly exceed atmospheric pressure during a forceful exhalation, such as during a cough. These actions reduce the chest dimensions and expel air more rapidly and thoroughly than usual. Other lumbar, abdominal, and even pelvic muscles contribute to forced expiration by raising the pressure in the abdominal cavity and pushing some of the viscera, such as the stomach and liver, up against the diaphragm. This increases the pressure in the thoracic cavity and thus helps to expel air. Such “abdominal breathing” is particularly important in singing and public speaking.
Not only does abdominal pressure affect thoracic pressure, but the opposite is also true. Depression of the diaphragm raises abdominal pressure and helps to expel the contents of certain abdominal organs, thus aiding in childbirth, urination, defecation, and vomiting. During such actions, we often consciously or unconsciously employ the Valsalva maneuver. This consists of taking a deep breath, holding it by closing the glottis, and then contracting the abdominal muscles to raise abdominal pressure and push the organ contents out.
The Heimlich maneuver is an action designed to expel an obstruction from the trachea by applying compression to the abdomen just inferior to the diaphragm. This is done by grasping the fist from behind with the other hand, and forcefully thrusting inward and upward to force the diaphragm upward, forcing air into the trachea to dislodge the object.
Figure 2. Muscles of respiration – the diaphragm and intercostal muscles.
Note: Muscles listed on the left are active during inspiration and those on the right are active during forced expiration. Note that the diaphragm is active in both phases, and different parts of the internal intercostal muscles serve for inspiration and expiration.
Figure 3. Diaphragm muscle anatomy
Diaphragm muscle
The musculotendinous diaphragm seals the inferior thoracic aperture (Figure 1). Generally, muscle fibers of the diaphragm arise radially, from the margins of the inferior thoracic aperture, and converge into a large central tendon. Because of the oblique angle of the inferior thoracic aperture, the posterior attachment of the diaphragm is inferior to the anterior attachment.
The diaphragm is not flat; rather, it “balloons” superiorly, on both the right and left sides, to form domes. The right dome is higher than the left, reaching as far as rib V. As the diaphragm contracts , the height of the domes decreases and the volume of the thorax increases. The esophagus and inferior vena cava penetrate the diaphragm; the aorta passes posterior to the diaphragm.
What Controls Your Breathing ?
A respiratory control center at the base of your brain controls your breathing. This center sends ongoing signals down your spine and to the muscles involved in breathing.
These signals ensure your breathing muscles contract (tighten) and relax regularly. This allows your breathing to happen automatically, without you being aware of it.
To a limited degree, you can change your breathing rate, such as by breathing faster or holding your breath. Your emotions also can change your breathing. For example, being scared or angry can affect your breathing pattern.
Your breathing will change depending on how active you are and the condition of the air around you. For example, you need to breathe more often when you do physical activity. In contrast, your body needs to restrict how much air you breathe if the air contains irritants or toxins.
To adjust your breathing to changing needs, your body has many sensors in your brain, blood vessels, muscles, and lungs.
Sensors in the brain and in two major blood vessels (the carotid artery and the aorta) detect carbon dioxide or oxygen levels in your blood and change your breathing rate as needed.
Sensors in the airways detect lung irritants. The sensors can trigger sneezing or coughing. In people who have asthma, the sensors may cause the muscles around the airways in the lungs to contract. This makes the airways smaller.
Sensors in the lungs alveoli (air sacs) can detect fluid buildup in the lung tissues. These sensors are thought to trigger rapid, shallow breathing.
Sensors in your joints and muscles detect movement of your arms or legs. These sensors may play a role in increasing your breathing rate when you’re physically active.