Contents
- What is Cholesterol ?
- Cellular Cholesterol Metabolism
- Cholesterol Facts 10
- A) LDL (Bad) Cholesterol
- B) Triglycerides
- C) HDL (Good) Cholesterol
- Total Blood (or serum) Cholesterol
- What should your Cholesterol Levels be ?
- What Affects Cholesterol Levels ?
- Where does Cholesterol come from ?
- What Is Your Risk of Developing Heart Disease or Having a Heart Attack ?
- Estimate of 10-Year Risk for Men
- Estimate of 10-Year Risk for Women
- What can you do if your LDL Cholesterol Level is High ? (see also Foods that can lower your cholesterol)
- What can you do if your Triglycerides Level is High ?
- What can you do if your HDL Cholesterol Level is Low ?
- Common Cholesterol Misconceptions 23, 24
- Why cholesterol matters ?
- Cholesterol-lowering Medication 25
- HMG-CoA Reductase Inhibitors (also called Statins)
- Bile Acid Sequestrants
- Fibrates
- Niacin
- Cholesterol Absorption Inhibitors
- Omega-3 Fatty Acid
- Combination Medicines
- Other Combination Medicines
What is Cholesterol ?
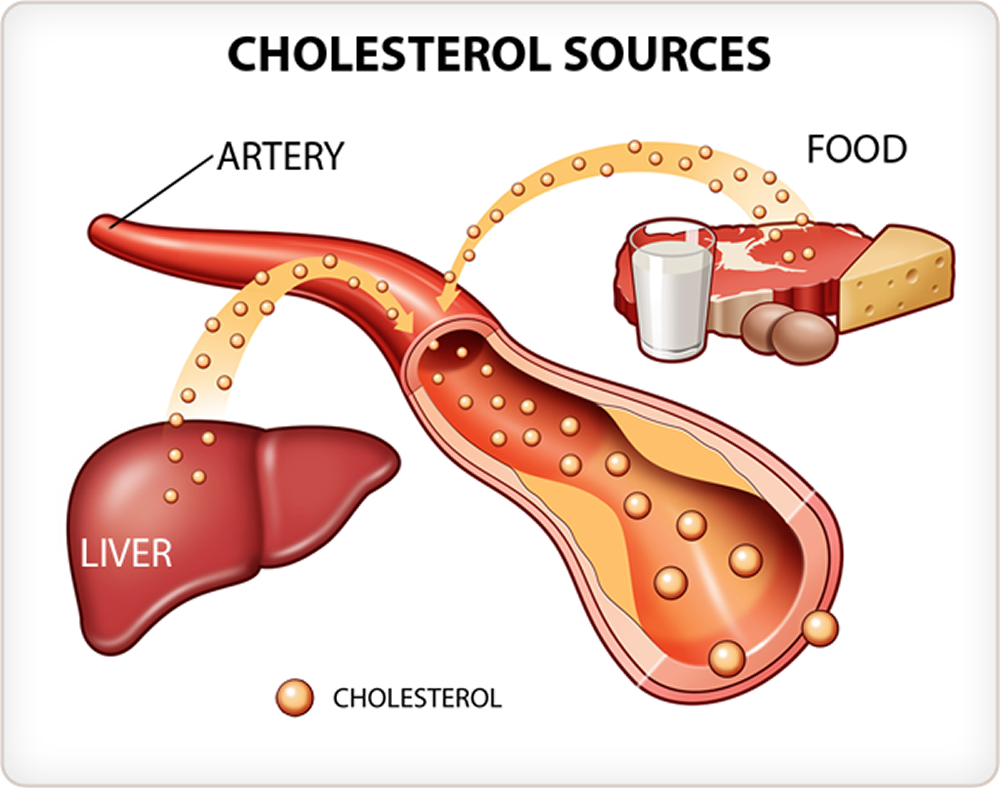
Cholesterol is a waxy, fat-like substance that occurs naturally in all parts of the body. Cholesterol isn’t just something that sits in your body like fat around your waist. Your bodies need cholesterol to make cell membranes, key hormones like testosterone and estrogen, the bile acids needed to digest and absorb fats and vitamin D. Cholesterol is so important to the body that the liver and intestines make it from scratch. However, cholesterol also is found in some of the foods you eat.
In humans, cholesterol is absorbed from the diet and synthesized by cells in various tissues. A healthy man weighing 60 kg contains approximately 140 g of cholesterol, but only 1% of the total cholesterol is involved in a dynamic metabolic cycle 1. In one study, the mean intake of dietary cholesterol was estimated to be 300–500 mg/day 2. They also reported that the dietary cholesterol aggregates into micelles with biliary cholesterol (800–1300 mg/day) in the duodenum 2. Physiologically, approximately 50% of the cholesterol is absorbed in the jejunum via a cholesterol transporter Niemann-Pick C1-like 1 (NPC1L1) expressed on the brush border membrane. The cholesterol is then transported to the liver in the form of chylomicrons and chylomicron remnants 3. NPC1L1, which may facilitate the liver accumulation of cholesterol, is expressed on the canalicular membrane of hepatocytes in humans. Another transporter pump system involving ATP-binding cassette (ABC) G5/G8 excretes cholesterol into bile 4.
Cholesterol is carried through your bloodstream by carriers made of fat (lipid) and proteins. These are called – lipoproteins.
Two types of lipoproteins carry cholesterol to and from cells. One is low-density lipoprotein or LDL. The other is high-density lipoprotein or HDL. The amount of each type of cholesterol in your blood can be measured by a blood test.
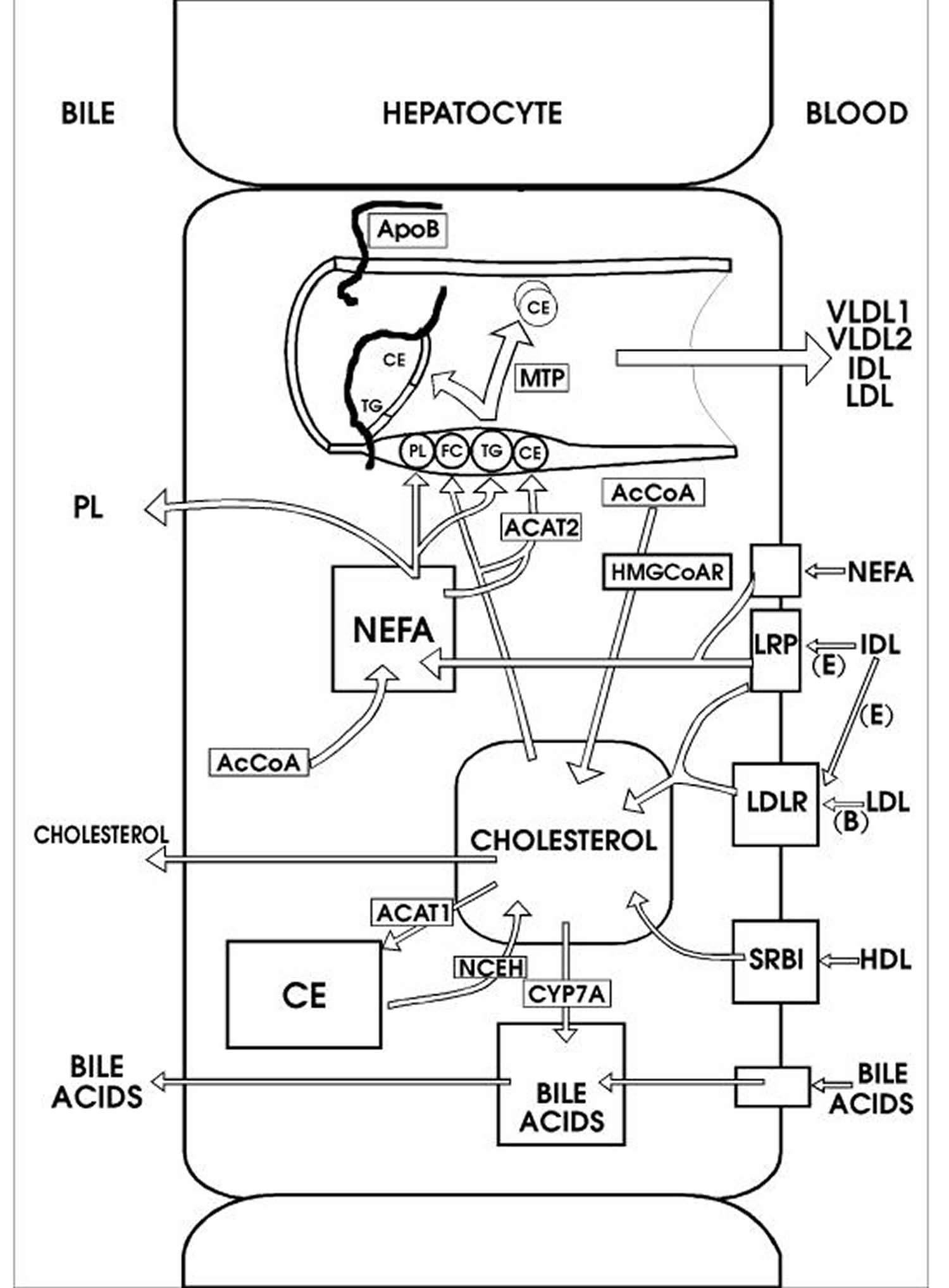
The main metabolic pathways of cholesterol in liver cells include (1) cholesterol de novo synthesis (acetyl-CoA-mevalonate-cholesterol pathway); (2) cholesterol uptake in the form of LDL and chylomicron remnants; (3) cholesterol excretion into the blood in the form of VLDL; (4) cholesterol excretion and uptake through bile via ABCG5/G8 and NPC1L1, respectively; (5) synthesis of bile acids and their excretion. Under normal conditions, these pathways interact with each other to maintain cholesterol levels within a specific range 5.
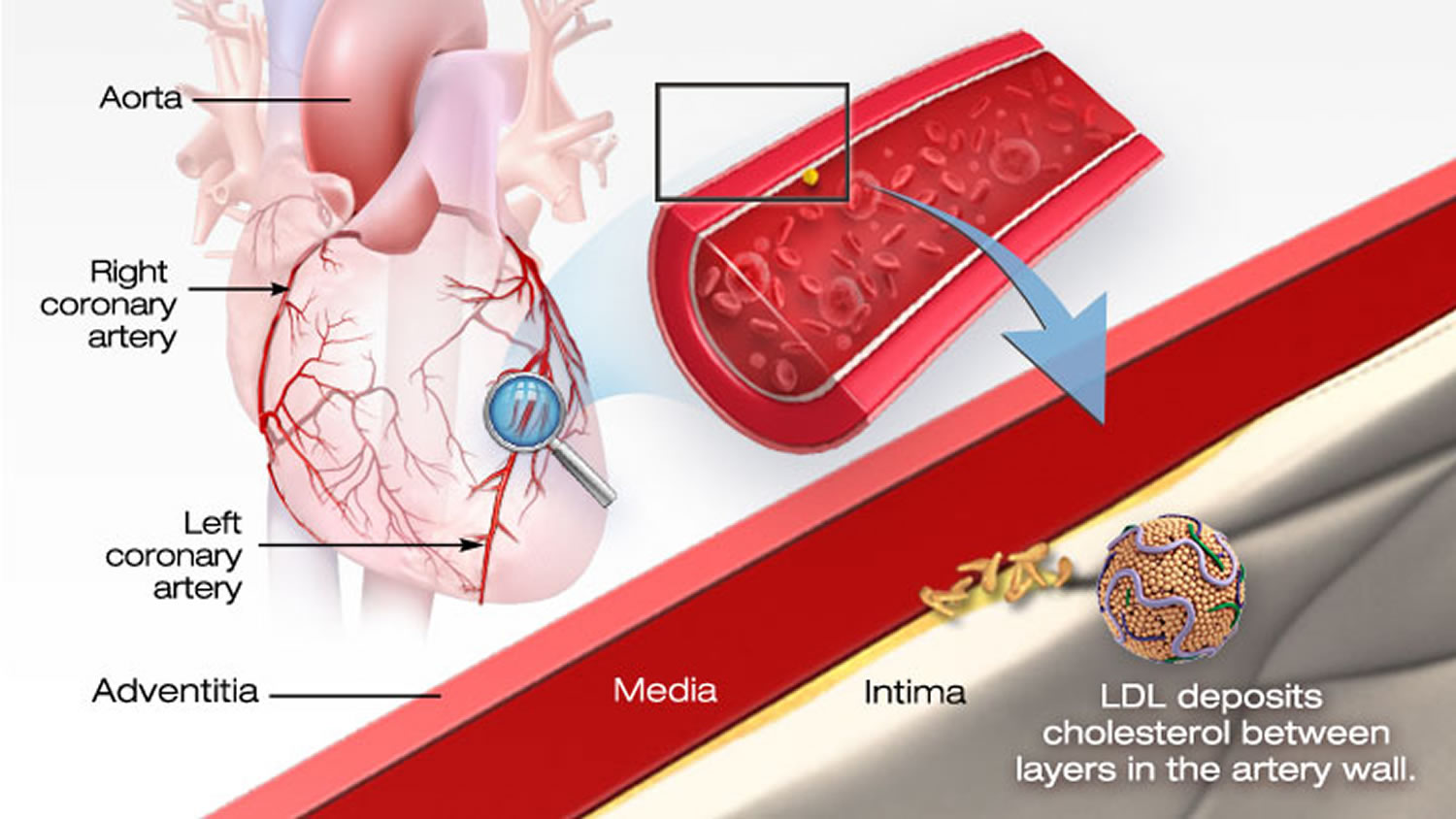
Your body needs some cholesterol to work properly. But if you have too much of bad cholesterol (LDL and Triglycerides) in your blood, it can combine with other substances in the blood and stick to the walls of your arteries. This is called plaque. Plaque can narrow your arteries or even block them.
The plaque buildup in arteries that LDL cholesterol and triglycerides contribute to is known as atherosclerosis (“hardening of the arteries”). When plaque builds up, it can partly or entirely block the blood flow of an artery in the heart, brain, pelvis, legs, arms or kidneys. This can lead to coronary heart disease, angina (chest pain), carotid artery disease, peripheral artery disease and chronic kidney disease.
Atherosclerosis can also lead to a heart attack or stroke. That’s because a couple of things can happen where plaque occurs:
- A piece of plaque may break off.
- A blood clot (thrombus) may form on the uneven surface of plaque buildup.
If either of these travels through the body, ultimately lodging in an artery to the heart, it causes a heart attack. If lodged in an artery to, or in, the brain, a stroke results.
Over time, plaque hardens and narrows your coronary arteries. This limits the flow of oxygen-rich blood to the heart. Eventually, an area of plaque can rupture (break open). This causes a blood clot to form on the surface of the plaque. If the clot becomes large enough, it can mostly or completely block blood flow through a coronary artery. A heart attack occurs if the flow of oxygen-rich blood to a section of heart muscle is cut off. If blood flow isn’t restored quickly, the section of heart muscle begins to die. Without quick treatment, a heart attack can lead to serious problems or death.
Plaque also can build up in other arteries in your body, such as the arteries that bring oxygen-rich blood to your brain and limbs. This can lead to problems such as carotid artery disease, stroke, and peripheral artery disease.
Coronary heart disease is a condition in which plaque builds up inside the coronary (heart) arteries. Plaque is made up of cholesterol, fat, calcium, and other substances found in the blood. When plaque builds up in the arteries, the condition is called atherosclerosis.
Cellular Cholesterol Metabolism
Cholesterol is an essential component of cell membranes but is also used by hepatocytes (liver cells) and enterocytes (cells of the intestinal lining) for the production of lipoproteins 6. The hepatocyte also secretes bile that contains cholesterol and bile acids that are derived from cholesterol. Adrenal and gonadal cells synthesise corticosteroid hormones from cholesterol. All nucleated cells can synthesise the enzymes to produce cholesterol 6. This synthetic pathway produces cholesterol as well as other isoprene products involved in the prenylation of proteins and the synthesis of ubiquinone. The rate-limiting enzyme in this pathway is 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase. The product of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, mevalonic acid, appears in plasma and urine and may be used as a guide to cholesterol synthetic activity. The plasma mevalonate concentration varies in a diurnal rhythm with the highest synthetic rate in the early hours of the morning.
There is a demand for cholesterol during cell growth and in cells that use cholesterol for specialised purposes. To meet such demands, the cell can synthesise cholesterol de novo, can import it through specialised receptors such as the LDL and related receptors, and can use cholesterol after cleavage of stored cholesterol ester by the action of neutral cholesterol ester hydrolase 6. The regulation of both cholesterol synthesis and importation by LDL receptors occurs by sensing the amount of cholesterol in the membranes. A depletion of membrane cholesterol will up-regulate transcription of both HMG-CoA reductase and the LDL receptor through a complex mechanism 7.
The upregulation of cholesterol synthesis and importation in the time of need is made possible by an interaction of a regulatory protein with the promoters of the genes for the LDL receptor, HMG-CoA reductase and HMG-CoA synthase. The LDL receptor promoter has three imperfect repeats. Repeat 2, consisting of 16 base pairs, forms a sterol regulatory element (SRE) that interacts with the SRE binding protein (SREBP) under cholesterol deprivation. SREBP has three isoforms in humans, each comprising approximately 1150 amino acids. SREBP has three domains: the amino-terminal domain contains a basic helix-loop-helix leucine zipper region that enables it to bind to DNA, a carboxy-terminal domain binding to sterol cleavage activating protein (SCAP) at the cell membrane, and an intermediate domain that contains two transmembrane portions linked by a loop of about 30 amino acids into the lumen of the endoplasmic reticulum (ER). SCAP is associated with SREBP in the membrane where the complex is stationary until cholesterol depletion permits its migration to the Golgi apparatus. In the Golgi apparatus two membrane-bound proteases process the SREBP:SCAP complex to create a cleavage product that migrates to the nucleus. Site 1 protease is a serine protease that cleaves the loop in the central domain of SREBP. Site 2 protease is a metalloprotease that cleaves the amino-terminal portion of SREBP that translocates to the nucleus. Additional complexity is introduced into the regulation of lipid metabolism by the three isoforms of SREBP. Alternative transcription start sites on chromosome 17 create differences in exon 1 of SREBP to produce SREBP1a and SREBP1c. SREBP2 is coded on chromosome 22. Whilst SREBP1a has broad specificity for all genes with SREBP response elements, SREBP1c favours promoters of genes for fatty acid synthesis and SREBP2 enhances cholesterol synthesis and importation into the cell 6.
Cholesterol importation into cells typically involves a high affinity, saturable process by means of the LDL receptor and a low affinity process of passive association with the cell membrane and internalisation. Additional receptors, such as the LDL receptor-related protein (LRP), may import lipoproteins in certain cells 8. Whilst the low affinity process accounts for very little uptake at low concentrations of LDL, higher concentrations of LDL may result in the internalisation of sufficient cholesterol to result in storage of cholesterol as its ester, to regulate cholesterol synthesis and possibly also LDL receptor expression. At least some contribution to low affinity clearance may be attributable to an interaction of fatty acids with cell membranes at physiologically appropriate concentration9 and some clearance may also take place by means of the scavenger receptor B1 (SRB1) even though this receptor has conventionally been viewed as a receptor for other lipoproteins 9.
Figure 1. Cholesterol metabolism and pathways in the liver cells
[Source 6]Notes to Figure 1: The cholesterol pool receives cholesterol from the blood through the LDL receptor (LDLR), LRP and SRB1. Additional inputs to the cholesterol pool are from cholesterol ester (CE) by NCEH and de novo synthesis from AcCoA involving HMG-CoA reductase. Outputs of cholesterol from the pool are to lipoproteins as free cholesterol (FC), and cholesterol ester (CE) by the reaction of cholesterol with non-esterified fatty acid (NEFA) catalysed by ACAT2. ACAT1 catalyses esterification of cholesterol for intracellular storage and cytochrome P4507A (CYP7A) initiates bile acid synthesis. Lipoprotein assembly in the lumen of the endoplasmic reticulum (ER) involves (PL) and TG, apoB and MTP. The lipoproteins synthesised by the liver include VLDL1 and VLDL2, IDL and LDL. The ligand for internalisation of IDL is apoE (E) and for internalisation of LDL is apoB100 (B).
Lipoprotein Synthesis
Lipoproteins, composed of lipid and apolipoproteins, are a means of transporting insoluble lipids, chiefly triacylglycerol (triglyceride), cholesterol ester (CE) and cholesterol. Different mechanisms exist to target TG and cholesterol within lipoproteins to cells that require fatty acids and/or cholesterol. Lipoproteins generally have a spherical shape but vary significantly in size, density, and constituent lipids and apoproteins. Greater lipid content makes for larger diameters and lower density, chiefly by triacylglycerol (triglyceride) content. The shell contains phospholipid (PL), cholesterol and apoproteins while the core contains triacylglycerol (triglyceride) and cholesterol ester (CE).
The enterocyte and hepatocyte are the sites of assembly for triacylglycerol-rich lipoproteins, using apoB for assembly of the lipoproteins. The triacylglycerol-rich lipoproteins secreted by the enterocyte are termed chylomicrons (CM) and those secreted by the hepatocytes are termed very low-density lipoproteins (VLDL). The enterocyte uses an edited mRNA of apoB100 to synthesise apoB48.15 chylomicrons contain one copy of apoB48 and VLDL contains one copy of apoB100.
Almost half of the cholesterol in the gut is absorbed but this efficiency varies amongst individuals. Enterocytes, like hepatocytes, express ACAT2 that produces cholesterol ester (CE) but in contrast to ACAT1, its catalytic site is on the lumenal aspect of the endoplasmic reticulum (ER). The CE globules as well as those of TG in the lumen of the endoplasmic reticulum (ER), are used in lipoprotein assembly. Both enterocytes and hepatocytes initiate lipoprotein assembly by adding a critical initial amount of neutral lipid to apoB so that this constitutively expressed protein is protected from ubiquitinylation and degradation. The critical protein responsible for this is microsomal TG transfer protein (MTP). Further remodelling of the lipoprotein takes place in the Golgi region before secretion.
As may be expected, there is in reality a range in size and content of lipoproteins secreted by lipoprotein-producing cells, especially by hepatocytes. These include: TG-rich VLDL with flotation rates of Sf 60–400 termed VLDL1, smaller CE-rich very low-density lipoproteins (VLDL) (Sf 20–60) termed VLDL2, intermediate-density lipoproteins (IDL, Sf 12–20) and LDL (Sf 0–12).
Lipoprotein Metabolism
A general scheme of lipoprotein metabolism is presented in Figure 2. CMs enter the venous circulation from the thoracic duct and lipoproteins made by the liver enter the hepatic venous system. Redistribution of apoproteins from especially high-density lipoprotein (HDL) supplies the bulk of the apoproteins on these TG-rich lipoproteins.
The circulating TG-rich lipoproteins attach briefly to proteoglycans in the vascular beds of muscle and adipose tissue. Lipoprotein lipase (LPL) also resident on the proteoglycans, is activated by apoC-II and inhibited by apoC-III. TG is hydrolysed by activated LPL to release fatty acids that will diffuse into the tissue or be sequestered on albumin. The lipolytic process results in a smaller core and the redundant shell around the core buds off with apoA-I to form HDL.
The remnants of chylomicron (CM) and very low-density lipoproteins (VLDL) return to the liver, being cleared by virtue of apoE that serves as the ligand for the LDL receptor, as well as the LRP. VLDL remnants, entering the IDL flotation range, are further hydrolysed by hepatic lipase (HL) to produce LDL. ApoB is the only apoprotein on LDL. Only on LDL will apoB serve as the ligand for the LDL receptor.
Whilst it is known that the liver can secrete a range of apoB-containing lipoproteins, the classical pathway is the production of mainly VLDL1 with subsequent conversion of this lipoprotein through VLDL2 to IDL before being removed into the liver from the circulation; but some IDL is metabolised to LDL. The half-lives of the lipoproteins increase down the lipolytic cascade, with LDL being the longest resident in plasma.
The larger lipoproteins are remodelled in the circulation by LPL as mentioned above. Smaller lipoproteins like IDL, LDL and HDL are modified by HL. An additional complexity is brought about by CE transfer protein (CETP) which exchanges neutral lipids between lipoproteins; TG being moved towards cholesterol-rich LDL and HDL, and CE being moved from these lipoproteins to CM and VLDL. The latter two apoB-containing lipoproteins can thus participate in the reverse cholesterol transport (RCT) of cholesterol from HDL to the liver. TG-rich LDL and HDL are substrates for HL, the action of which will decrease their size by hydrolysis of TG.
The lipoproteins that lack apoB constitute mainly HDL. This class of lipoproteins is important for RCT. The other functions of HDL include being a reservoir for apopoproteins A, C and E, CETP and lecithin:cholesterol acyltransferase (LCAT), the provision of anti-oxidant activity by paraoxonase, and modulation of endothelial function and immunity. Having accepted cholesterol from a cell, a small HDL particle will enlarge as a result of esterification of cholesterol by LCAT as CE migrates to the core and additional cholesterol that is now accommodated in the shell, also becomes esterified. Not only can HDL transfer CE to the TG-rich lipoproteins, but it can deliver it directly to the liver through SRB1.
Cholesterol Facts 10
- Cholesterol is a waxy, fat-like substance. Your body needs some cholesterol, but it can build up on the walls of your arteries and lead to heart disease and stroke when you have too much in your blood.
- Having high blood cholesterol puts you at risk of heart disease, the leading cause of death in the United States.
- You can have high cholesterol and not realize it. Most of the 65 million Americans with high cholesterol have no symptoms. So it’s important to have your blood cholesterol levels checked. All adults age 20 and older should have their cholesterol levels checked at least once every 5 years. If you have an elevated cholesterol, you’ll need to have it tested more often. Talk with your doctor to find out how often is best for you 11.
- People with high cholesterol have about twice the risk of heart disease as people with lower levels.
- 71 million American adults (33.5%) have high low-density lipoprotein (LDL), or “bad,” cholesterol.
- Only 1 out of every 3 adults with high LDL cholesterol has the condition under control.
- Less than half of adults with high LDL cholesterol get treatment.
- Lowering your cholesterol can reduce your risk of having a heart attack, needing heart bypass surgery or angioplasty, and dying of heart disease.
- Exercising, eating a healthy diet, and not smoking will help you prevent high cholesterol and reduce your levels.
- High cholesterol has no symptoms, so many people don’t know that their cholesterol is too high. Your doctor can do a simple blood test to check your levels.
- The National Cholesterol Education Program recommends that adults get their cholesterol checked every five years.
A) LDL (Bad) Cholesterol
LDL cholesterol is called “bad” cholesterol. LDL cholesterol makes up the majority of the body’s cholesterol. LDL is known as “bad” cholesterol because having high levels can lead to plaque buildup in your arteries and result in heart disease and stroke. Too much LDL in the bloodstream helps create the harmful cholesterol-filled plaques that grow inside arteries (atherosclerosis). Such plaque buildups narrow arteries and are responsible for angina (chest pain with exertion or stress), heart attacks, peripheral artery disease can narrowed arteries in the legs and most types of stroke.
The higher the level of LDL cholesterol in your blood, the GREATER your chance is of getting heart disease. The higher the level of HDL cholesterol in your blood, the LOWER your chance is of getting heart disease.
What causes a person’s LDL level to be high ? Most of the time diet is the key culprit. Eating foods rich in saturated fats, trans fats, and easily digested carbohydrates boost LDL. Genes are sometimes at the root of high cholesterol, and some medications can boost LDL.
Saturated fats: typical sources of saturated fat include animal products, such as red meat, whole-fat dairy products, and eggs, and also a few vegetable oils, such as palm oil, coconut oil, and cocoa butter. Saturated fat can increase your levels of “bad” LDL cholesterol. But it has some benefits, too — it lowers triglycerides and nudges up levels of “good” HDL cholesterol. The role of saturated fat in heart disease is currently under debate. For now, it’s best to limit your intake of saturated-fat-rich foods.

B) Triglycerides
Triglycerides are the most common type of fat in the body; they store excess energy from your diet. Normal triglyceride levels vary by age and sex. People with high triglycerides often have a high total cholesterol level, including a high LDL cholesterol level and a low HDL cholesterol level.
The plasma level of triglyceride is a well-established independent biomarker of cardiovascular disease risk 12 and triglyceride-rich lipoproteins have atherogenic properties. Triglyceride predicts cardiovascular disease in a wide range of circumstances. Its association with cardiovascular disease risk is partly attenuated by adjustment for HDL cholesterol, with which it is moderately correlated 13.
Genetic variation associated with lifelong low triglyceride levels is associated with a lower incidence of cardiovascular disease 14. Triglyceride is carried primarily within large lipoproteins, chylomicrons, and VLDL (very low density lipoprotein), which are also rich in cholesterol and like LDL can enter the arterial wall and stimulate atherosclerosis. These triglyceride-rich lipoproteins carry various atherogenic proteins such as apolipoprotein C-III, itself associated with atherosclerosis and cardiovascular disease 15.
Replacing 1% of daily energy intake from saturated fat with polyunsaturated or monounsaturated fat lowers triglyceride by 0.9 or 0.4 mg/dL 16 perhaps more in those with hypertriglyceridemia 17.
Replacing the 1% saturated fat with 1% carbohydrates raises serum triglycerides by ≈1 mg/dL. Dietary carbohydrates raise plasma triglyceride levels by increasing the production by the liver of triglycerides and subsequent incorporation into VLDL (very low density lipoprotein) 17. The magnitude that dietary carbohydrates increase plasma triglyceride is similar whether the carbohydrate has a high or low glycemic index 18.
Many people with heart disease or diabetes also have high triglyceride levels.
Elevated triglycerides can be caused by several factors. They are overweight and obesity, physical inactivity, cigarette smoking, excess alcohol consumption and a diet very high in carbohydrates (more than 60 percent of total calories). These causes can be addressed with lifestyle changes. Sometimes underlying diseases or genetic disorders cause high triglycerides, too.
A high triglyceride level combined with low HDL cholesterol or high LDL cholesterol is linked with fatty buildups in artery walls. This increases the risk of heart attack and stroke.

C) HDL (Good) Cholesterol
HDL cholesterol is “good” cholesterol. Think of it as the “healthy” cholesterol, so higher levels are better. Experts believe HDL acts as a scavenger, carrying LDL cholesterol away from the arteries and back to the liver. There it’s broken down and passed from the body.
Experts believe HDL cholesterol may act in a variety of helpful ways that tend to reduce the risk for heart disease:
- HDL cholesterol scavenges and removes LDL or “bad” cholesterol.
- HDL reduces, reuses, and recycles LDL cholesterol by transporting it to the liver where it can be reprocessed.
- HDL cholesterol acts as a maintenance crew for the inner walls (endothelium) of blood vessels. Damage to the inner walls is the first step in the process of atherosclerosis, which causes heart attacks and strokes. HDL scrubs the wall clean and keeps it healthy.
People with high blood triglycerides usually also have lower HDL cholesterol. Genetic factors, type 2 diabetes, smoking, being overweight and being sedentary can all lower HDL cholesterol. Women tend to have higher levels of HDL cholesterol than men do.
A healthy HDL cholesterol level may protect against heart attack and stroke. Studies show low levels of HDL cholesterol increase the risk of heart disease. HDL cholesterol does not completely eliminate LDL cholesterol. Only one-fourth to one-third of blood cholesterol is carried by HDL.

Total Blood (or serum) Cholesterol
Everyone should start getting tested for cholesterol and other risk factors at age 20. These measurements help to determine risk for a heart attack or stroke. In some cases, children can have high cholesterol levels. Evidence suggests these children are at greater risk for developing heart disease as adults. Lack of regular physical activity, poor dietary habits and genetics can all affect a child’s cholesterol levels. Parents and caregivers can help kids develop a heart-healthy lifestyle by serving foods low in saturated fat and trans fats; encouraging at least 60 minutes of physical activity on most (and preferably all) days; and stressing the importance of avoiding tobacco products.
If you’re between age 40 and 79, talk to your doctor about assessing your 10-year risk. Once you know your risk, you can take action to lower it. Your doctor may recommend diet and lifestyle changes and maybe medication, too. Follow all of your doctor’s instructions, and have your cholesterol and other risk factors rechecked every four to six years.
Keeping your cholesterol levels healthy is a great way to keep your heart healthy and lower your chances of getting heart disease or having a stroke. Cholesterol test report will show your cholesterol levels in milligrams per deciliter of blood (mg/dL). This isn’t a type of cholesterol, instead, it’s a composite of different types. A person’s total cholesterol score is calculated by adding their HDL and LDL cholesterol levels and 20 percent of their triglyceride level.
Nowadays, these ranges and your total cholesterol levels are considered in context with other risk factors, and treatment is recommended accordingly.
High blood cholesterol is a condition in which you have too much cholesterol in your blood. By itself, the condition usually has no signs or symptoms. Thus, many people don’t know that their cholesterol levels are too high. People who have high blood cholesterol have a greater chance of getting coronary heart disease, also called coronary artery disease.
The American Heart Association recommends that all adults age 20 or older have their cholesterol and other traditional risk factors checked every four to six years. After that, people should work with their healthcare providers to determine their risk for cardiovascular disease and stroke.
People who have cardiovascular disease or are at higher risk of it may need their cholesterol and other risk factors assessed more often.

What should your Cholesterol Levels be ?
Your ideal cholesterol level 19 will depend on your risk for heart disease.
- Total cholesterol level – less than 200 milligrams per deciliter (mg/dl) is best, but depends on your HDL and LDL levels
- LDL cholesterol levels – less than 130 mg/dl is best, but this depends on your risk for heart disease
- HDL cholesterol levels – 60 mg/dl or higher reduces your risk for heart disease
- Triglycerides – less than 150 milligrams per deciliter (mg/dl) is best
| Total Cholesterol Level | Category |
|---|---|
| Less than 200 mg/dL | Desirable |
| 200-239 mg/dL | Borderline High |
| 240 mg/dL and above | High |
Note: Cholesterol levels are measured in milligrams (mg) of cholesterol per deciliter (dL) of blood.
| LDL Cholesterol Level | LDL-Cholesterol Category |
|---|---|
| Less than 100 mg/dL | Optimal |
| 100-129 mg/dL | Near optimal/above optimal |
| 130-159 mg/dL | Borderline high |
| 160-189 mg/dL | High |
| 190 mg/dL and above | Very high |
| Desirable Cholesterol Levels | |
|---|---|
| Total cholesterol | Less than 200 mg/dL |
| LDL (“bad” cholesterol) | Less than 100 mg/dL |
| HDL (“good” cholesterol) | 60 mg/dL or higher |
| Triglycerides | Less than 150 mg/dL |
(Source 20).
Note: In general, HDL (good) cholesterol protects against heart disease, so for HDL, higher numbers are better. A level less than 40 mg/dL is low and is considered a major risk factor because it increases your risk for developing heart disease. HDL levels of 60 mg/dL or more help to lower your risk for heart disease.
Triglycerides can also raise heart disease risk. Levels that are borderline high (150-199 mg/dL) or high (200 mg/dL or more) may need treatment in some people.
What Affects Cholesterol Levels ?
A variety of things can affect cholesterol levels. These are things you can do something about:
- Diet. Saturated fat and cholesterol in the food you eat make your blood cholesterol level go up. Saturated fat is the main culprit, but cholesterol in foods also matters. Reducing the amount of saturated fat and cholesterol in your diet helps lower your blood cholesterol level.
- Weight. Being overweight is a risk factor for heart disease. It also tends to increase your cholesterol. Losing weight can help lower your LDL and total cholesterol levels, as well as raise your HDL and lower your triglyceride levels.
- Physical Activity. Not being physically active is a risk factor for heart disease. Regular physical activity can help lower LDL (bad) cholesterol and raise HDL (good) cholesterol levels. It also helps you lose weight. You should try to be physically active for 30 minutes on most, if not all, days.
Things you cannot do anything about also can affect cholesterol levels. These include:
- Age and Gender. As women and men get older, their cholesterol levels rise. Before the age of menopause, women have lower total cholesterol levels than men of the same age. After the age of menopause, women’s LDL levels tend to rise.
- Heredity. Your genes partly determine how much cholesterol your body makes. High blood cholesterol can run in families.
Where does Cholesterol come from ?
Cholesterol comes from two sources. Your body (specifically your liver) makes all the cholesterol you need. The rest you get from foods from animals. For example, meat, poultry and full-fat dairy products contain cholesterol (called dietary cholesterol). More importantly, these foods are high in saturated and trans fat. That’s a problem because these fats cause your liver to make more cholesterol than it otherwise would. For some people, this added production means they go from a normal cholesterol level to one that’s unhealthy.

Some tropical oils, such as palm oil, palm kernel oil and coconut oil, also can trigger your liver to make more cholesterol. These oils are often found in baked goods.
The saturated and trans fats you eat may raise your blood cholesterol level. Having too much cholesterol in your blood may lead to increased
risk for heart disease and stroke. High levels of cholesterol in the blood can increase your risk of heart disease. Your cholesterol levels tend to rise as you get older. There are usually no signs or symptoms that you have high blood cholesterol, but it can be detected with a blood test. You are likely to have high cholesterol if members of your family have it, if you are overweight or if you eat a lot of fatty foods.
You can lower your cholesterol by exercising more and eating more fruits and vegetables. You also may need to take medicine to lower your cholesterol.
What Is Your Risk of Developing Heart Disease or Having a Heart Attack ?
In general, the higher your LDL level and the more risk factors you have (other than LDL), the greater your chances of developing heart disease or having a heart attack. Some people are at high risk for a heart attack because they already have heart disease. Other people are at high risk for developing heart disease because they have diabetes (which is a strong risk factor) or a combination of risk factors for heart disease. Follow these steps to find out your risk for developing heart disease.
- Step 1: Check the table below to see how many of the listed risk factors you have; these are the risk factors that affect your LDL goal.
Major Risk Factors That Affect Your LDL Goal
- Cigarette smoking
- High blood pressure (140/90 mmHg or higher or on blood pressure medication)
- Low HDL cholesterol (less than 40 mg/dL)*
- Family history of early heart disease (heart disease in father or brother before age 55; heart disease in mother or sister before age 65)
- Age (men 45 years or older; women 55 years or older)
* If your HDL cholesterol is 60 mg/dL or higher, subtract 1 from your total count.
Even though obesity and physical inactivity are not counted in this list, they are conditions that need to be corrected.
- Step 2: How many major risk factors do you have? If you have 2 or more risk factors in the table above, use the attached risk scoring tables (which include your cholesterol levels) to find your risk score. Risk score refers to the chance of having a heart attack in the next 10 years, given as a percentage. My risk score is ________%.
Estimate of 10-Year Risk for Men
Framingham Point Scores by Age Group
| Age | Points |
|---|---|
| 20-34 | -9 |
| 35-39 | -4 |
| 40-44 | 0 |
| 45-49 | 3 |
| 50-54 | 6 |
| 55-59 | 8 |
| 60-64 | 10 |
| 65-69 | 11 |
| 70-74 | 12 |
| 75-79 | 13 |
Framingham Point Scores by Age Group and Total Cholesterol
| Total Cholesterol | Age 20-39 | Age 40-49 | Age 50-59 | Age 60-69 | Age 70-79 |
|---|---|---|---|---|---|
| <160 | 0 | 0 | 0 | 0 | 0 |
| 160-199 | 4 | 3 | 2 | 1 | 0 |
| 200-239 | 7 | 5 | 3 | 1 | 0 |
| 240-279 | 9 | 6 | 4 | 2 | 1 |
| 280+ | 11 | 8 | 5 | 3 | 1 |
Framingham Point Scores by Age and Smoking Status
| Age 20-39 | Age 40-49 | Age 50-59 | Age 60-69 | Age 70-79 | |
|---|---|---|---|---|---|
| Nonsmoker | 0 | 0 | 0 | 0 | 0 |
| Smoker | 8 | 5 | 3 | 1 | 1 |
Framingham Point Scores by HDL Level
| HDL | Points |
|---|---|
| 60+ | -1 |
| 50-59 | 0 |
| 40-49 | 1 |
| <40 | 2 |
Framingham Point Scores by Systolic Blood Pressure and Treatment Status
| Systolic BP | If Untreated | If Treated |
|---|---|---|
| <120 | 0 | 0 |
| 120-129 | 0 | 1 |
| 130-139 | 1 | 2 |
| 140-159 | 1 | 2 |
| 160+ | 2 | 3 |
10-Year Risk by Total Framingham Point Scores
| Point Total | 10-Year Risk |
|---|---|
| < 0 | < 1% |
| 0 | 1% |
| 1 | 1% |
| 2 | 1% |
| 3 | 1% |
| 4 | 1% |
| 5 | 2% |
| 6 | 2% |
| 7 | 3% |
| 8 | 4% |
| 9 | 5% |
| 10 | 6% |
| 11 | 8% |
| 12 | 10% |
| 13 | 12% |
| 14 | 16% |
| 15 | 20% |
| 16 | 25% |
| 17 or more | 30% |
Estimate of 10-Year Risk for Women
Framingham Point Scores by Age Group
| Age | Points |
|---|---|
| 20-34 | -7 |
| 35-39 | -3 |
| 40-44 | 0 |
| 45-49 | 3 |
| 50-54 | 6 |
| 55-59 | 8 |
| 60-64 | 10 |
| 65-69 | 12 |
| 70-74 | 14 |
| 75-79 | 16 |
Framingham Point Scores by Age Group and Total Cholesterol
| Total Cholesterol | Age 20-39 | Age 40-49 | Age 50-59 | Age 60-69 | Age 70-79 |
|---|---|---|---|---|---|
| <160 | 0 | 0 | 0 | 0 | 0 |
| 160-199 | 4 | 3 | 2 | 1 | 1 |
| 200-239 | 8 | 6 | 4 | 2 | 1 |
| 240-279 | 11 | 8 | 5 | 3 | 2 |
| 280+ | 13 | 10 | 7 | 4 | 2 |
Framingham Point Scores by Age and Smoking Status
| Age 20-39 | Age 40-49 | Age 50-59 | Age 60-69 | Age 70-79 | |
|---|---|---|---|---|---|
| Nonsmoker | 0 | 0 | 0 | 0 | 0 |
| Smoker | 9 | 7 | 4 | 2 | 1 |
Framingham Point Scores by HDL Level
| HDL | Points |
|---|---|
| 60+ | -1 |
| 50-59 | 0 |
| 40-49 | 1 |
| <40 | 2 |
Framingham Point Scores by Systolic Blood Pressure and Treatment Status
| Systolic BP | If Untreated | If Treated |
|---|---|---|
| <120 | 0 | 0 |
| 120-129 | 1 | 3 |
| 130-139 | 2 | 4 |
| 140-159 | 3 | 5 |
| 160+ | 4 | 6 |
10-Year Risk by Total Framingham Point Scores
| Point Total | 10-Year Risk |
|---|---|
| < 9 | < 1% |
| 9 | 1% |
| 10 | 1% |
| 11 | 1% |
| 12 | 1% |
| 13 | 2% |
| 14 | 2% |
| 15 | 3% |
| 16 | 4% |
| 17 | 5% |
| 18 | 6% |
| 19 | 8% |
| 20 | 11% |
| 21 | 14% |
| 22 | 17% |
| 23 | 22% |
| 24 | 27% |
| 25 or more | 30% |
(Source: National Institutes of Health, National Heart, Lung and Blood Institute. Estimate of 10-Year Risk for Coronary Heart Disease Framingham Point Scores. 21).
- Step 3: Use your medical history, number of risk factors, and risk score to find your risk of developing heart disease or having a heart attack in the table below.
| If You Have | You Are in Category |
|---|---|
| Heart disease, diabetes, or risk score more than 20%* | I. High Risk |
| 2 or more risk factors and risk score 10-20% | II. Next Highest Risk |
| 2 or more risk factors and risk score less than 10% | III. Moderate Risk |
| 0 or 1 risk factor | IV. Low-to-Moderate Risk |
* Means that more than 20 of 100 people in this category will have a heart attack within 10 years.
My risk category is ______________________.
What can you do if your LDL Cholesterol Level is High ? (see also Foods that can lower your cholesterol)
The main goal of cholesterol-lowering treatment is to lower your LDL level enough to reduce your risk of developing heart disease or having a heart attack. The higher your risk, the lower your LDL goal will be. To find your LDL goal, see the boxes below for your risk category. There are two main ways to lower your cholesterol:
- Therapeutic Lifestyle Changes (TLC)–includes a cholesterol-lowering diet (called the TLC diet), physical activity, and weight management. TLC is for anyone whose LDL is above goal.
- Drug Treatment–if cholesterol-lowering drugs are needed, they are used together with TLC treatment to help lower your LDL.
If you are in:
- Category I, Highest Risk, your LDL goal is less than 100 mg/dL. you will need to begin the TLC diet to reduce your high risk even if your LDL is below 100 mg/dL. If your LDL is 100 or above, you will need to start drug treatment at the same time as the TLC diet. If your LDL is below 100 mg/dL, you may also need to start drug treatment together with the TLC diet if your doctor finds our risk is very high, for example if you had a recent heart attack or have both heart disease and diabetes.
- Category II, Next Highest Risk, your LDL goal is less than 130 mg/dL. If your LDL is 130 mg/dL or above, you will need to begin treatment with the TLC diet. If your LDL is 130 mg/dL or more after 3 months on the TLC diet, you may need drug treatment along with the TLC diet. If your LDL is less than 130 mg/dL, you will need to follow the heart healthy diet for all Americans, which allows a little more saturated fat and cholesterol than the TLC diet.
- Category III, Moderate Risk, your LDL goal is less than 130 mg/dL. If your LDL is 130 mg/dL or above, you will need to begin the TLC diet. If your LDL is 160 mg/dL or more after you have tried the TLC diet for 3 months, you may need drug treatment along with the TLC diet. If your LDL is less than 130 mg/dL, you will need to follow the heart healthy diet for all Americans.
- Category IV, Low-to-Moderate Risk, your LDL goal is less than 160 mg/dL. If your LDL is 160 mg/dL or above, you will need to begin the TLC diet. If your LDL is still 160 mg/dL or more after 3 months on the TLC diet, you may need drug treatment along with the TLC diet to lower your LDL, especially if your LDL is 190 mg/dL or more. If your LDL is less than 160 mg/dL, you will need to follow the heart healthy diet for all Americans.
To reduce your risk for heart disease or keep it low, it is very important to control any other risk factors you may have such as high blood pressure and smoking.
Healthy foods and exercise can cut your LDL levels. Regular exercise, the kind that gets your heart pumping, also lowers your levels. Eat foods low in saturated fat, cholesterol, and simple carbs. (Simple carbs include foods like sugar, white bread, and white crackers.) You can lower your numbers even more if you add fiber and plant sterols (margarine or nuts) to your diet.
If healthy foods and exercise aren’t enough, your doctor may suggest medications. Some drugs, like statins, help block your body from making cholesterol. Other medicines lower the amount of cholesterol your body gets from food you eat. There are also drugs that you take as a shot rather than as a pill. These meds block a protein that interferes with the way your liver removes LDL from your blood. They’re recommended for people who can’t use statins or who have a severe form of high cholesterol.
Remember, many other things affect your chances of getting heart disease. Smoking, diabetes, high blood pressure, obesity, and lack of exercise also raise the risk. It’s important to lower your LDL, but don’t ignore these other health issues.
Hyperlipidemia (high blood cholesterol) can often be improved by lifestyle changes. This is true even if high cholesterol is due to genetics (familial hypercholesterolemia).
The four lifestyle changes you need to make are:
- Regular exercise
- Avoiding tobacco smoke
- Losing weight (if you’re overweight or obese)
- Eating a heart-healthy diet
1) Regular exercise
Becoming more physically active. A sedentary lifestyle lowers HDL cholesterol. Less HDL cholesterol means there’s less good cholesterol to remove LDL (bad) cholesterol from arteries.
Physical activity is important. Just 40 minutes of aerobic exercise of moderate to vigorous intensity done three to four times a week is enough to lower both cholesterol and high blood pressure. Brisk walking, swimming, bicycling or a dance class are examples.
2) Quitting smoking
Smokers can lower their cholesterol levels and help protect their arteries by quitting. Nonsmokers should avoid exposure to secondhand smoke.
3) Losing weight
Being overweight or obese tends to raise LDL cholesterol and lower HDL cholesterol.
Losing excess weight can improve cholesterol levels. A weight loss of 10 percent can go a long way toward lowering your risk of high cholesterol — or reversing it.
4) Eating a heart-healthy diet
The American Heart Association’s heart-healthy eating plan can help you manage your blood cholesterol level and reduce your risk of heart disease and stroke 22. The simple cooking tips below will help you prepare tasty, heart-healthy meals that improve your cholesterol by reducing excess saturated fat and trans fat.
- Reduce saturated fat in meat and poultry
The American Heart Association recommends a dietary pattern that emphasizes poultry and limits red meat. The amount of saturated fat in meats can vary widely, depending on the cut and how it’s prepared.
Here are some ways to reduce the saturated fat in meat:
+ Select lean cuts of meat with minimal visible fat. Lean beef cuts include the round, chuck, sirloin or loin. Lean pork cuts include the tenderloin or loin chop. Lean lamb cuts come from the leg, arm and loin.
+ Buy “choice” or “select” grades rather than “prime.” Select lean or extra lean ground beef.
+ Trim all visible fat from meat before cooking.
+ Broil rather than pan-fry meats such as hamburger, lamb chops, pork chops and steak.
+ Use a rack to drain off fat when broiling, roasting or baking. Instead of basting with drippings, keep meat moist with wine, fruit juices or an acceptable oil-based marinade.
+ Cook a day ahead of time. Stews, boiled meat, soup stock or other dishes in which fat cooks into the liquid can be refrigerated. Then, remove the hardened fat from the top.
+ When a recipe calls for browning the meat first, try browning it under the broiler instead of in a pan.
+ Eat chicken and turkey rather than duck and goose, which are higher in fat. Choose white meat most often when eating poultry.
+ Remove the skin from chicken or turkey before cooking. If your poultry dries out too much, first try basting with wine, fruit juices or an acceptable oil-based marinade. Or leave the skin on for cooking and remove it before eating.
+ Limit processed meats such as sausage, bologna, salami and hot dogs. Many processed meats — even those with “reduced fat” labels — are high in calories and saturated fat. Often they’re high in sodium, too. Read labels carefully and choose processed meats only occasionally.
- Eat more fish
Fish can be fatty or lean, but it’s still low in saturated fat. Choose oily fish such as salmon, trout and herring, which are high in omega-3 fatty acids. Prepare fish baked, broiled, grilled or boiled rather than breaded and fried, and without added salt, saturated fat and trans fat. Shrimp and crawfish have more cholesterol than most other types of seafood, but they’re lower in total fat and saturated fat than most meats and poultry.
- Eat Less meat
Try meatless meals featuring vegetables or beans. For example, think eggplant lasagna, a big grilled portobello mushroom on a bun instead of a burger, or beans-n-weenies without the weenies and salt. Or think of meat as a condiment in casseroles, stews, low-sodium soups and spaghetti — use it sparingly and just for flavor rather than as a main ingredient.
- Cook fresh vegetables the heart-healthy way
Try cooking vegetables in a tiny bit of vegetable oil and add a little water during cooking if needed, or use a vegetable oil spray. Just 1 to 2 teaspoons of oil is enough for a package of plain frozen vegetables without sauce or seasonings that serves four. Place in a skillet with tight cover, season and cook over a very low heat until the vegetables are done.
- Add herbs and spices to make vegetables even tastier. For example, these combinations add new and subtle flavors:
+ Rosemary with peas, cauliflower and squash
+ Oregano with zucchini
+ Dill with green beans
+ Marjoram with Brussels sprouts, carrots and spinach
+ Basil with tomatoes
Start with a small quantity (1/8 to 1/2 teaspoon to a package of frozen vegetables), then let your own and your family’s taste be your guide. Chopped parsley and chives, sprinkled on just before serving, also enhance the flavor of many vegetables.
- Use liquid vegetable oils in place of solid fats
Liquid vegetable oils such as canola, safflower, sunflower, soybean and olive can often be used instead of solid fats such as butter, lard or shortening. If you must use margarine, try the soft or liquid kind. Use a little liquid oil to:
+ Pan-fry fish and poultry.
+ Saute vegetables.
+ Make cream sauces and soups using low-fat or fat-free milk.
+ Add to whipped or scalloped potatoes using low-fat or fat-free milk.
+ Brown rice for Spanish, curried or stir-fried rice.
+ Cook dehydrated potatoes and other prepared foods that call for fat to be added.
+ Make pancakes or waffles.
- Puree fruits and veggies for baking
You can replace the oil in muffin, cookie, cake and snack bar recipes with pureed fruits or veggies to give your treats an extra healthy boost. For many recipes, use the specified amount of puree instead of oil. Check the mix’s package or your cookbook’s substitutions page for other conversions. You can:
+ Use applesauce in spice muffins or oatmeal cookies.
+ Include bananas in breads and muffins.
+ Try zucchini in brownies.
- Lower dairy fats
Low-fat (1%) or fat-free (skim) milk can be used in many recipes in place of whole milk or half-and-half. Some dishes like puddings may result in a softer set. You can also use low-fat, low-sodium cottage cheese, part-skim milk mozzarella or ricotta and other low-fat, low-sodium cheeses with little or no change in consistency.
- Sauces and gravies
Let your cooking liquid cool, then remove the hardened fat before making gravy. Or use a fat separator to pour off the good liquid from cooking stock, leaving the fat behind.
- Increase fiber and whole grains
+ Toast and crush or cube fiber-rich whole-grain bread to make breadcrumbs, stuffing or croutons.
+ Replace the breadcrumbs in your meatloaf with uncooked oatmeal.
+ Serve whole fruit at breakfast in place of juice.
+ Use brown rice instead of white rice and try whole grain pasta.
+ Add lots of colorful veggies to your salad — carrots, broccoli and cauliflower are high in fiber and give your salad a delicious crunch
What can you do if your Triglycerides Level is High ?
Studies have consistently linked high triglycerides levels with heart disease, heart attacks, and stroke, especially in people with low levels of “good” HDL cholesterol and in those with type 2 diabetes.
The good news is that there’s a lot you can do on your own to lower triglycerides and improve health.
- Get more physical activity. Exercise can have a big impact on triglyceride levels. Experts recommend that everybody get at least 30 minutes of exercise at least five times a week. If you’re out of shape, start slowly. Begin with a quick walk three times a week and then build up from there.
- Lose some weight. If you’re heavy, shed a few pounds and try to maintain an ideal body weight. Exercise will help, but you also need to focus on diet. The key is to eat fewer calories — whether they come from fats, carbs, or protein. Focus on a diet that’s high in fruits, vegetables, lean proteins, and low-fat dairy products. Cutting down on sugary foods — like sodas — could really help, too.
- Choose better fats. Pay more attention to the fats you eat. Eat fewer foods with unhealthy fats (found in meat, butter, and cheese) and trans fats (in processed foods and margarines), as well as cholesterol. Boost your intake of healthy monounsaturated and polyunsaturated fats, which are found in olive oil, nuts, and some fish. Studies have found that the omega-3s in fatty fish — like tuna, salmon, mackerel, and sardines — are particularly good at lowering triglyceride levels. Because even healthy fats are high in calories, you still need to eat these foods in moderation.
- Cut down on alcohol. Even small amounts of alcohol seem to cause big spikes in triglyceride levels. Limit alcohol intake to one drink a day.
- Fish oil with omega-3 fatty acids can help keep triglycerides under control.
- Niacin (nicotinic acid) can lower triglycerides by up to 50%. It’s available as a non-prescription supplement.
What can you do if your HDL Cholesterol Level is Low ?
If your HDL is low, you can take several steps to boost your HDL level and reduce your heart disease risk:
- Exercise . Aerobic exercise for 30 to 60 minutes on most days of the week can help pump up HDL.
- Quit smoking . Tobacco smoke lowers HDL, and quitting can increase HDL levels.
- Keep a healthy weight. Besides improving HDL levels, avoiding obesity reduces risk for heart disease and multiple other health conditions.
Common Cholesterol Misconceptions 23, 24
- High cholesterol isn’t a concern for children.
High cholesterol can be inherited (familial hypercholesterolemia). Children who have this genetic disorder are at very high risk of heart disease. This problem is underdiagnosed and undertreated worldwide. These kids need to be identified and aggressively treated with medications.
Cholesterol testing should be considered for children and adolescents who are at higher-than-normal risk, meaning those with:
+ A parent or grandparent who had evidence of coronary atherosclerosis, peripheral vascular disease or cerebrovascular disease; who had a coronary artery procedure; or who had a heart attack or sudden cardiac death before age 55.
+ A parent who has a history of high total cholesterol levels (240 mg/dL or higher).
All children–not just those at higher risk–will benefit from a healthy diet and lifestyle. Compelling evidence shows the atherosclerotic process (buildup of plaque in arteries) begins in childhood and progresses slowly into adulthood. Later in life, it often leads to coronary heart disease, the leading cause of death in the United States. Establishing the habits of healthy eating and physical activity early in life can reduce the risk of later cardiovascular problems.
To reduce fatty deposits in children’s arteries, it’s important to discourage cigarette smoking, encourage regular aerobic exercise, identify and treat high blood pressure, avoid or reduce overweight, diagnose and treat diabetes and encourage a healthy diet. Children ages 2 and older should be encouraged to eat a diet emphasizing fruits, vegetables, fish, whole grains, low sodium and few sugar-laden foods and drinks.
- You don’t need a cholesterol check until you’re middle aged.
Everyone should start getting tested for cholesterol and other risk factors at age 20. These measurements help to determine risk for a heart attack or stroke. In some cases, children can have high cholesterol levels. Evidence suggests these children are at greater risk for developing heart disease as adults. Lack of regular physical activity, poor dietary habits and genetics can all affect a child’s cholesterol levels. Parents and caregivers can help kids develop a heart-healthy lifestyle by serving foods low in saturated fat and trans fats; encouraging at least 60 minutes of physical activity on most (and preferably all) days; and stressing the importance of avoiding tobacco products.
If you’re between age 40 and 79, talk to your doctor about assessing your 10-year risk. Once you know your risk, you can take action to lower it. Your doctor may recommend diet and lifestyle changes and maybe medication, too. Follow all of your doctor’s instructions, and have your cholesterol and other risk factors rechecked every four to six years.
- Using margarine instead of butter will lower my cholesterol
Both margarine and butter are high in saturated fat, which increases LDL cholesterol, so use both in moderation. Limiting food high in saturated fat and trans fat may help reduce bad cholesterol. Most vegetable oils and soft or liquid margarines have less saturated and trans fat than solid spreads, and are preferable to the stick forms of margarine for a heart-healthy diet. When selecting a margarine, choose one that has 0 grams trans fat on the Nutrition Facts label.
- Thin people don’t have to worry about high cholesterol
Any body type can have high cholesterol. True, overweight people are more likely to have high cholesterol, but everybody, including thin people, should have their cholesterol checked regularly. People who do not gain weight easily are often less aware of how much saturated and trans fat they eat. Nobody can “eat anything they want” and stay heart-healthy.
- Since the food label on my favorite food says “low cholesterol,” I can be sure it is sure it is “heart-healthy.”
Many “low-cholesterol” foods contain high levels of saturated fat and/or trans fat — both of which contribute to raising LDL cholesterol. Some foods that claim to be “low-fat” may have a higher fat content than expected. Look for the amount of saturated fat, trans fat, and total calories in a serving of the product. Also check the size of one serving. Often it’s smaller than you think. The first item listed in the ingredients list is the one used most in the product, so choose products where fats and oils appear near the end of the list.
- High cholesterol is a man’s problem, not a woman’s.
Premenopausal women may have some protection from high LDL (bad) levels of cholesterol, compared to men. That’s because the female hormone estrogen is highest during the childbearing years and tends to raise HDL (good) cholesterol levels. This may help explain why premenopausal women are usually protected from developing heart disease.
But as people get older, gain weight or both, their triglyceride and cholesterol levels tend to rise. Postmenopausal women may find that, despite a heart-healthy diet and regular physical activity, their cholesterol still rises. This is why women nearing menopause should have their cholesterol levels checked and talk with their doctor about their risk factors and options.
At one time, it was thought that hormone replacement therapy (HRT) might lower a woman’s risk of heart disease and stroke. However, recent studies have shown that HRT does not reduce the risk of heart disease and stroke in postmenopausal women. That’s why the American Heart Association recommends it not be used for cardiovascular prevention.
- Diet and physical activity dictate your cholesterol level.
Diet and physical activity affect overall blood cholesterol levels, but other factors also contribute. Being overweight or obese tends to increase bad cholesterol (LDL) and lower good cholesterol (HDL). Getting older also causes LDL cholesterol to rise. For some, heredity may play a role. Even so, a heart-healthy diet and regular physical activity are important to everyone for maintaining cardiovascular health. Have your cholesterol tested and work with your healthcare professionals on the plan that’s best for you.
- If you take cholesterol meds, you don’t need to make lifestyle changes.
Drug therapy is important, but making diet and lifestyle changes are the best ways to reduce heart disease and stroke risk. To lower cholesterol, eat a heart-healthy diet and get 40 minutes of aerobic exercise of moderate to vigorous intensity three to four times a week. It’s also very important to take your medication exactly as your doctor has instructed so it can work most efficiently.
Remember that one change — like switching from butter to soft margarine — is a good step, but may not be enough to reduce your cholesterol to healthy levels. Other diet and lifestyle changes or medication may be needed, as your doctor recommends.
Why cholesterol matters ?
Cholesterol circulates in the blood, and as blood cholesterol levels rise, so does the risk to your health. That’s why it’s important to have your cholesterol tested so you can know your levels.
There are actually two types of cholesterol: “bad” and “good.” LDL cholesterol is the bad kind. HDL is the good kind. Too much of the bad kind — or not enough of the good kind — increases the chances that cholesterol will start to slowly build up in the inner walls of arteries that feed the heart and brain. We talk more about these two kinds of cholesterol here: LDL, HDL and Triglycerides.
Together with other substances, cholesterol can form a thick, hard deposit that can narrow the arteries and make them less flexible. This condition is known as atherosclerosis. If a clot forms and blocks a narrowed artery, a heart attack or stroke can result.
High cholesterol is one of the major controllable risk factors for coronary heart disease, heart attack and stroke. If you have other risk factors such as smoking, high blood pressure or diabetes, this risk increases even more. The more risk factors you have and the more severe they are, the more your overall risk rises.
If you have high cholesterol, making changes in your diet can help bring it down into the healthy range. Exercise can help boost the level of protective HDL. Several types of medication, notably the family of drugs known as statins, can powerfully lower LDL. Depending on your cardiovascular health, your doctor may recommend taking a statin.
Cholesterol-lowering Medication 25
If you have high low-density lipoprotein (LDL) cholesterol, your doctor may prescribe medicine in addition to lifestyle changes to control your LDL cholesterol level.
Your health care team will evaluate your cholesterol levels and other risk factors to determine your overall risk for heart disease and stroke and decide whether you need treatment to lower your cholesterol. Your doctor may prescribe medication if:
- You previously had a heart attack or stroke.
- Your LDL cholesterol level is 190 mg/dL or higher.
- You are 40–75 years old with diabetes and LDL cholesterol of 70 mg/dL or higher.
- You are 40–75 years old with a high risk for developing heart disease or stroke and LDL cholesterol of 70 mg/dL or higher.
Discuss with your health care team about your overall cardiovascular health and how you may be able to reduce your cardiovascular disease risk.
Cholesterol-lowering Medication
Several types of medications help lower LDL cholesterol. The chart below describes each type and how it works. The U.S. Food and Drug Administration (FDA) also provides a quick reference list of medicines to treat high LDL cholesterol 26.
| Type of Medicine | How it Works |
|---|---|
| Statins | HMG-CoA Reductase Inhibitors or Statin drugs lower LDL cholesterol by slowing down the liver’s production of cholesterol. They also increase the liver’s ability to remove LDL cholesterol that is already in the blood. The U.S. Food and Drug Administration (FDA) offers advice on the risks related to taking statins:
|
| Bile acid sequestrants | Bile acid sequestrants help remove cholesterol from the blood stream by removing bile acids. The body needs bile acids and makes them by breaking down LDL cholesterol. |
| Niacin, or nicotinic acid | Niacin is a B vitamin that can improve all lipoprotein levels. Nicotinic acid raises high-density lipoprotein (HDL) cholesterol levels while lowering total cholesterol, LDL cholesterol, and triglyceride levels. |
| Cholesterol Absorption Inhibitors | Inhibits the absorption of cholesterol by the small intestine |
| Fibrates | Fibrates mainly lower triglycerides and, to a lesser extent, increase HDL levels. |
| Omega-3 Fatty Acid | |
| Combination Medicines | Niacin and Lovastatin / Niacin and Simvastatin / Ezetimibe and Simvastatin |
| Other Combination Medicines | Amlodipine and Atorvastatin |
- Statins: What You Should Know
HMG-CoA Reductase Inhibitors (also called Statins)
| Brand Name | Generic Name |
|---|---|
| Altoprev | Lovastatin |
| Crestor | Rosuvastatin |
| Lescol | Fluvastatin |
| Lipitor | Atorvastatin |
| Livalo | Pitavastatin |
| Mevacor | Lovastatin |
| Pravachol | Pravastatin |
| Zocor | Simvastatin |
Warnings
+ Do not use these medicines if you have liver disease.
+ Do not use these medicines if you are pregnant or nursing.
+ Use these medicines with caution if you are also taking Gemfibrozil, Fenofibrates, Amiodarone, Verapamil, or blood thinners (anticoagulants).
+ People who use some HIV medicines, birth control pills (oral contraceptives), Nefazodone, and niacin should talk to their doctor about the specific risks of using Statins.
+ Drinking a quart or more of grapefruit juice everyday may affect these “Statin” medicines.
Common Side Effects
+ Gas
+ Dizziness
+ Constipation
+ Headache
+ Diarrhea
+ Upset stomach
Warning Signs
Call your doctor if you have any of these signs:
+ Fever
+ Dark urine
+ Muscle pain or weakness that happens without a good reason (like exercise or injury)
- Bile Acid Sequestrants: What You Should Know
Bile Acid Sequestrants
| Brand Name | Generic Name |
|---|---|
| Colestid | Colestipol |
| LoCholest (oral powder) | Cholestyramine |
| Prevalite (oral powder) | Cholestyramine |
| Questran (oral powder) | Cholestyramine |
| Welchol | Colesevelam |
Warnings
+ Do not use these drugs if you have problems with your liver or gallbladder.
+ People who have bleeding problems, heart disease, stomach ulcers, kidney disease, or an under-active thyroid should talk to their doctor about the risks of taking these medicines.
+ People who take Spironolactone should talk to their doctor before taking Colestipol (Colestid).
Common Side Effects
+ Heartburn
+ Constipation
+ Gas
+ Indigestion
+ Nausea
Warning Signs
Call your doctor if you have any of these signs:
+ Stomach pain
+ Vomiting
+ Sudden weight loss
+ Unusual bleeding from gums or rectum
- Fibrates: What You Should Know
Fibrates
| Brand Name | Generic Name |
|---|---|
| Antara | Fenofibrate |
| Fenoglide | Fenofibrate |
| Lipofen | Fenofibrate |
| Lopid | Gemfibrozil |
| Tricor | Fenofibrate |
| Triglide | Fenofibrate |
| Trilipix | Fenofibric Acid |
Warnings
+ People with kidney problems, gallbladder disease, or liver disease should not use these drugs.
+ Talk to your doctor before taking other medicines to control cholesterol called “Statins” (HMG-CoA Reductase Inhibitors).
+ Pregnant women or women who are breastfeeding should talk to their doctor about the risks of taking these drugs.
+ People who take diabetes medicines or blood thinners (anticoagulants) should talk to their doctor about the risks of taking these drugs.
Common Side Effects
+ Headache
+ Constipation or Diarrhea
+ Dizziness
+ Stomach pain
Warning Signs
Call your doctor if you have any of these signs:
+ Muscle pain
+ Weakness
+ Jaundice (skin or eyes look yellow)
- Niacin: What You Should Know
Niacin
| Brand Name | Generic Name |
|---|---|
| Niaspan | Niacin Nicotinic Acid |
Warnings
+ Do not use Niaspan if you have liver disease or if you are taking an immediate-release niacin pill.
+ Do not use Niaspan if you are pregnant or breastfeeding.
+ People who are taking aspirin, high blood pressure medicines, HMG CoA Reductase Inhibitors (“Statins”), or medicines to lower bile acid should talk to their doctor about the risks of taking Niacin (Niaspan).
+ People with kidney disease, peptic ulcer, diabetes, or chest pain should talk to their doctor about the risks of taking this drug.
+ People who have had a heart attack or gout should talk to their doctor about the risks of taking this drug.
Common Side Effects
+ Headache
+ Upset stomach
+ Heartburn
+ Diarrhea
+ Flushing (redness of the face or neck)
Warning Signs
Call your doctor if you have any of these signs:
+ Fast heartbeat
+ Fainting
+ Dizziness
+ Jaundice (skin or eyes look yellow)
- Cholesterol Absorption Inhibitors: What You Should Know
Cholesterol Absorption Inhibitors
| Brand Name | Generic Name |
|---|---|
| Zetia | Ezetimibe |
Warnings
+ Women who are pregnant or breastfeeding should not take Zetia with another cholesterol medicine.
+ People who have liver disease should not take Zetia with another cholesterol medicine.
+ Use caution if you are taking blood thinners (anticoagulants).
Common Side Effects
+ Feeling Tired
+ Stomach Pain
Warning Signs
Call your doctor if you have any of these signs:
+ Muscle Pain, Tenderness or Weakness
+ Stomach Pain
+ Swelling of the Face or Lips
+ Severe Itching
- Omega-3 Fatty Acid: What You Should Know
Omega-3 Fatty Acid
| Brand Name | Generic Name |
|---|---|
| Lovaza | Omega-3 Acid Ethyl Esters |
Warnings
+ Women who are breastfeeding, pregnant, or planning to become pregnant should talk to their doctor before taking Lovaza.
+ Tell your doctor if you have diabetes or liver, thyroid or pancreas problems.
+ Tell your doctor if you are allergic to fish.
+ Tell your doctor if you drink more than 2 glasses of alcohol each day.
+ Tell your doctor if you take blood thinners or anticoagulants including aspirin, warfarin, coumarin, and clopidogrel (Plavix).
Common Side Effects
+ Burping
+ Infection
+ Feeling like you have the flu
+ Upset stomach
+ Change in your sense of taste
+ Back pain
+ Skin rash
Other Side Effects
Lovaza may affect certain blood tests.
+ Test to check your liver (ALT)
+ Test to check your cholesterol (LDL-C)
- Combination Drugs: What You Should Know
Combination Medicines
| Brand Name | Generic Name |
|---|---|
| Advicor | Niacin and Lovastatin |
| Simcor | Niacin and Simvastatin |
| Vytorin | Ezetimibe and Simvastatin |
Warnings
- Do not take Vytorin or Advicor if you are pregnant or breastfeeding.
- Do not take Vytorin if you have liver disease.
- People taking Gemfibrozil (Lopid), Fenofibrate (Tricor), high blood pressure medicines, Protease Inhibitors (medicines to treat HIV) or blood thinners (anticoagulants) should use caution when taking these drugs.
- Drinking a quart or more of grapefruit juice everyday may affect these drugs.
Common Side Effects
- Headache
- Flushing (redness of the face or neck)
- Upset stomach
Warning Signs
Call your doctor if you have any of these signs:
- Dark urine
- Stomach pain
- Muscle pain, tenderness or weakness that happens without a good reason (like exercise or injury)
- Jaundice (skin or eyes look yellow)
Caduet is used to treat people who have both high blood pressure and high cholesterol.
Other Combination Medicines
| Brand Name | Generic Name |
|---|---|
| Caduet | Amlodipine and Atorvastatin |
Warnings
- Do not take Caduet if you are pregnant or planning to become pregnant.
- Do not take Caduet if you are breastfeeding.
- Do not take Caduet if you have liver problems.
Common Side Effects
- Swelling of the Legs or Ankles (edema)
- Muscle or Joint Pain
- Headache
- Diarrhea or Constipation
- Feeling Dizzy
- Feeling Tired or Sleepy
- Gas
- Rash
- Nausea
- Stomach Pain
- Fast or Irregular Heartbeat
- Face feels Hot or Warm (flushing)
Warning Signs
Call your doctor if you have any of these signs:
- Muscle problems like weakness, tenderness, or pain that happens without a good reason (like exercise or injury)
- Brown or Dark-colored Urine
- Skin or Eyes look yellow (jaundice)
- Feel more tired than usual
- A physiological method for estimation of hepatic secretion of biliary lipids in man. Grundy SM, Metzger AL. Gastroenterology. 1972 Jun; 62(6):1200-17. https://www.ncbi.nlm.nih.gov/pubmed/5050318/[↩]
- Evaluation of fatty acid metabolism-related gene expression in nonalcoholic fatty liver disease. Nakamuta M, Kohjima M, Morizono S, Kotoh K, Yoshimoto T, Miyagi I, Enjoji M. Int J Mol Med. 2005 Oct; 16(4):631-5. https://www.ncbi.nlm.nih.gov/pubmed/16142397/[↩][↩]
- Niemann-Pick C1 Like 1 protein is critical for intestinal cholesterol absorption. Altmann SW, Davis HR Jr, Zhu LJ, Yao X, Hoos LM, Tetzloff G, Iyer SP, Maguire M, Golovko A, Zeng M, Wang L, Murgolo N, Graziano MP. Science. 2004 Feb 20; 303(5661):1201-4. https://www.ncbi.nlm.nih.gov/pubmed/14976318/[↩]
- Coexpression of ATP-binding cassette proteins ABCG5 and ABCG8 permits their transport to the apical surface. Graf GA, Li WP, Gerard RD, Gelissen I, White A, Cohen JC, Hobbs HH. J Clin Invest. 2002 Sep; 110(5):659-69. https://www.ncbi.nlm.nih.gov/pubmed/12208867/[↩]
- Enjoji M, Yasutake K, Kohjima M, Nakamuta M. Nutrition and Nonalcoholic Fatty Liver Disease: The Significance of Cholesterol. International Journal of Hepatology. 2012;2012:925807. doi:10.1155/2012/925807. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3328950/[↩]
- Marais AD. Familial Hypercholesterolaemia. The Clinical Biochemist Reviews. 2004;25(1):49-68. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1853359/[↩][↩][↩][↩][↩]
- Horton JD, Goldstein JL, Brown MS. SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J Clin Invest. 2002;109:1125–31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC150968/[↩]
- Yu KCW, Chen W, Cooper AD. LDL receptor-related protein mediates cell-surface clustering and hepatic sequestration of chylomiron remnants in LDLR-deficient mice. J Clin Invest. 2001;107:1387–94. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC209318/[↩]
- Tai ES, Adiconis X, Ordovas JM, et al. Polymorphisms at the SRBI locus are associated with lipoprotein levels in subjects with heterozygous familial hypercholesterolemia. Clin Genet. 2003;63:53–8. https://www.ncbi.nlm.nih.gov/pubmed/12519372[↩]
- Centers for Disease Control and Prevention.Division for Heart Disease and Stroke Prevention. – Cholesterol Fact Sheet – https://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_cholesterol.htm[↩]
- National Institutes of Health, National Heart, Lung, and Blood Institute. YOUR GUIDE TO Lowering Your Cholesterol With TLC. https://www.nhlbi.nih.gov/files/docs/public/heart/chol_tlc.pdf[↩]
- Miller M, Stone NJ, Ballantyne C, Bittner V, Criqui MH, Ginsberg HN, et. al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123:2292–2333. doi: 10.1161/CIR.0b013e3182160726.[↩]
- Sarwar N, Danesh J, Eiriksdottir G, Sigurdsson G, Wareham N, Bingham S, Boekholdt SM, Khaw KT, Gudnason V. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation. 2007;115:450–458. doi: 10.1161/CIRCULATIONAHA.106.637793.[↩]
- TG and HDL Working Group of the Exome Sequencing Project, National Heart, Lung, and Blood Institute. Loss-of-function mutations in APOC3, triglycerides, and coronary disease. N Engl J Med.2014;371:22–31.[↩]
- Wyler von Ballmoos MC, Haring B, Sacks FM. The risk of cardiovascular events with increased apolipoprotein CIII: a systematic review and meta-analysis. J Clin Lipidol. 2015;9:498–510. doi: 10.1016/j.jacl.2015.05.002.[↩]
- Mensink RP. Effects of Saturated Fatty Acids on Serum Lipids and Lipoproteins: A Systematic Review and Regression Analysis. Geneva, Switzerland: World Health Organization; 2016.[↩]
- Miller M, Stone NJ, Ballantyne C, Bittner V, Criqui MH, Ginsberg HN, Goldberg AC, Howard WJ, Jacobson MS, Kris-Etherton PM, Lennie TA, Levi M, Mazzone T, Pennathur S; on behalf of the American Heart Association Clinical Lipidology, Thrombosis, and Prevention Committee of the Council on Nutrition, Physical Activity, and Metabolism; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Nursing; Council on the Kidney in Cardiovascular Disease. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123:2292–2333. doi: 10.1161/CIR.0b013e3182160726.[↩][↩]
- Sacks FM, Carey VJ, Anderson CA, Miller ER 3rd, Copeland T, Charleston J, Harshfield BJ, Laranjo N, McCarron P, Swain J, White K, Yee K, Appel LJ. Effects of high vs low glycemic index ofdietary carbohydrate on cardiovascular disease risk factors andinsulin sensitivity: the OmniCarb randomized clinical trial. JAMA.2014;312:2531–2541. doi: 10.1001/jama.2014.16658.[↩]
- Centers for Disease Control and Prevention.Division for Heart Disease and Stroke Prevention. – Know The Facts About High Cholesterol – https://www.cdc.gov/cholesterol/docs/ConsumerEd_Cholesterol.pdf[↩]
- National Cholesterol Education Program. Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. https://www.nhlbi.nih.gov/files/docs/guidelines/atp3xsum.pdf[↩]
- National Institutes of Health, National Heart, Lung and Blood Institute. Estimate of 10-Year Risk for Coronary Heart Disease Framingham Point Scores. https://www.nhlbi.nih.gov/health-pro/guidelines/current/cholesterol-guidelines/quick-desk-reference-html/10-year-risk-framingham-table[↩]
- American Heart Association. Cooking To Lower Cholesterol Updated:May 22,2017 . http://www.heart.org/HEARTORG/Conditions/Cholesterol/PreventionTreatmentofHighCholesterol/Cooking-To-Lower-Cholesterol_UCM_305630_Article.jsp[↩]
- American Heart Association. Why Cholesterol Matters. Published Summer 2017. http://heartinsight.heart.org/Summer-2017/Why-Cholesterol-Matters/[↩]
- American Heart Association. Common Misconceptions about Cholesterol. Updated:May 22,2017. http://www.heart.org/HEARTORG/Conditions/Cholesterol/AboutCholesterol/Common-Misconceptions-about-Cholesterol_UCM_305638_Article.jsp#.WNwSUW8rLRY[↩]
- Centers for Disease Control and Prevention. Cholesterol-lowering Medication. https://www.cdc.gov/cholesterol/treating_cholesterol.htm[↩]
- US Food and Drug Administration (FDA). High Cholesterol–Medicines To Help You. https://www.fda.gov/ForConsumers/ByAudience/ForWomen/ucm118595.htm[↩]