Contents
- What is cirrhosis of the liver
What is cirrhosis of the liver
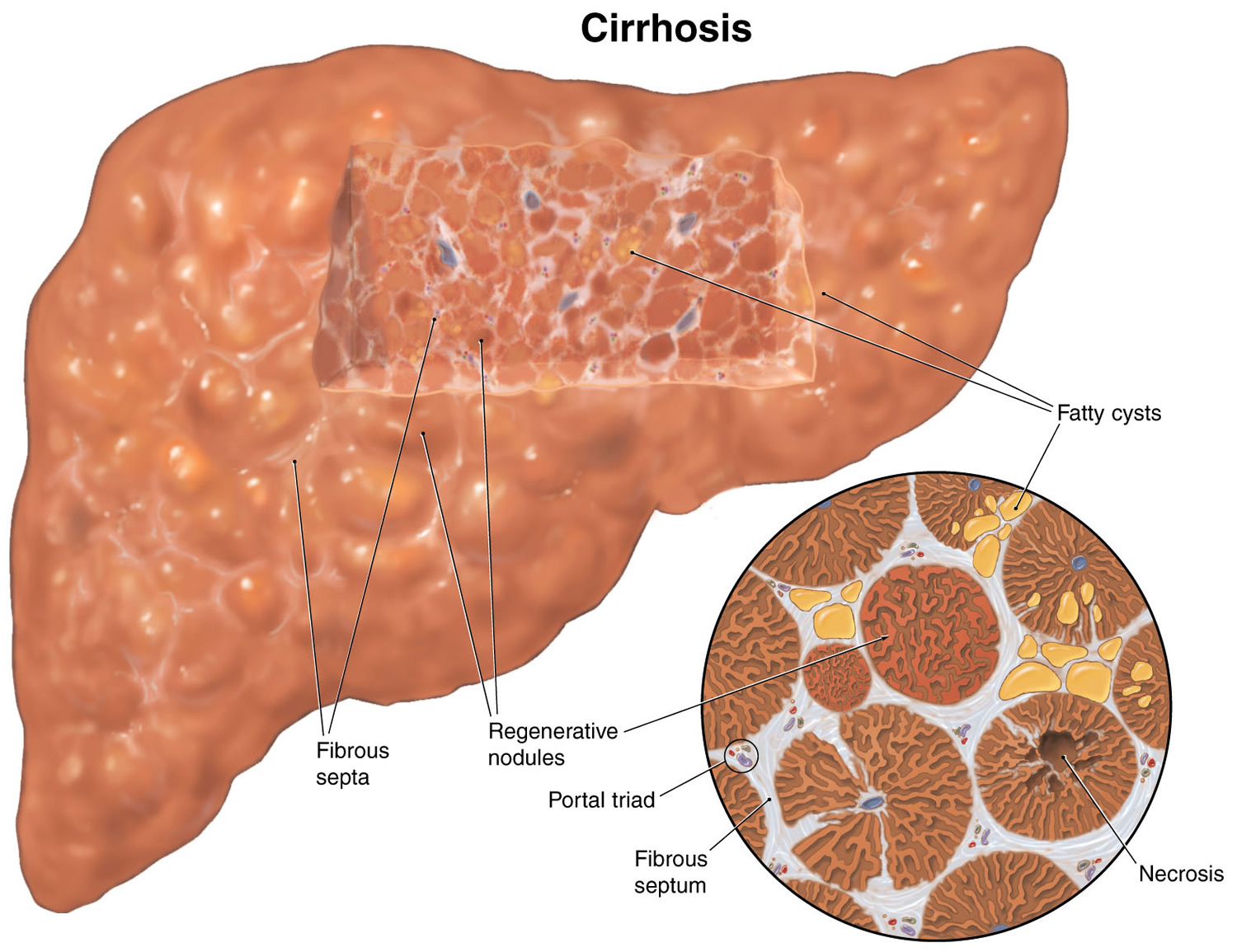
Cirrhosis is scarring of the liver 1. Scar tissue forms because of injury or long-term liver injury or disease. Scar tissue cannot do what healthy liver tissue does – make protein, help fight infections, clean the blood, help digest food and store energy.
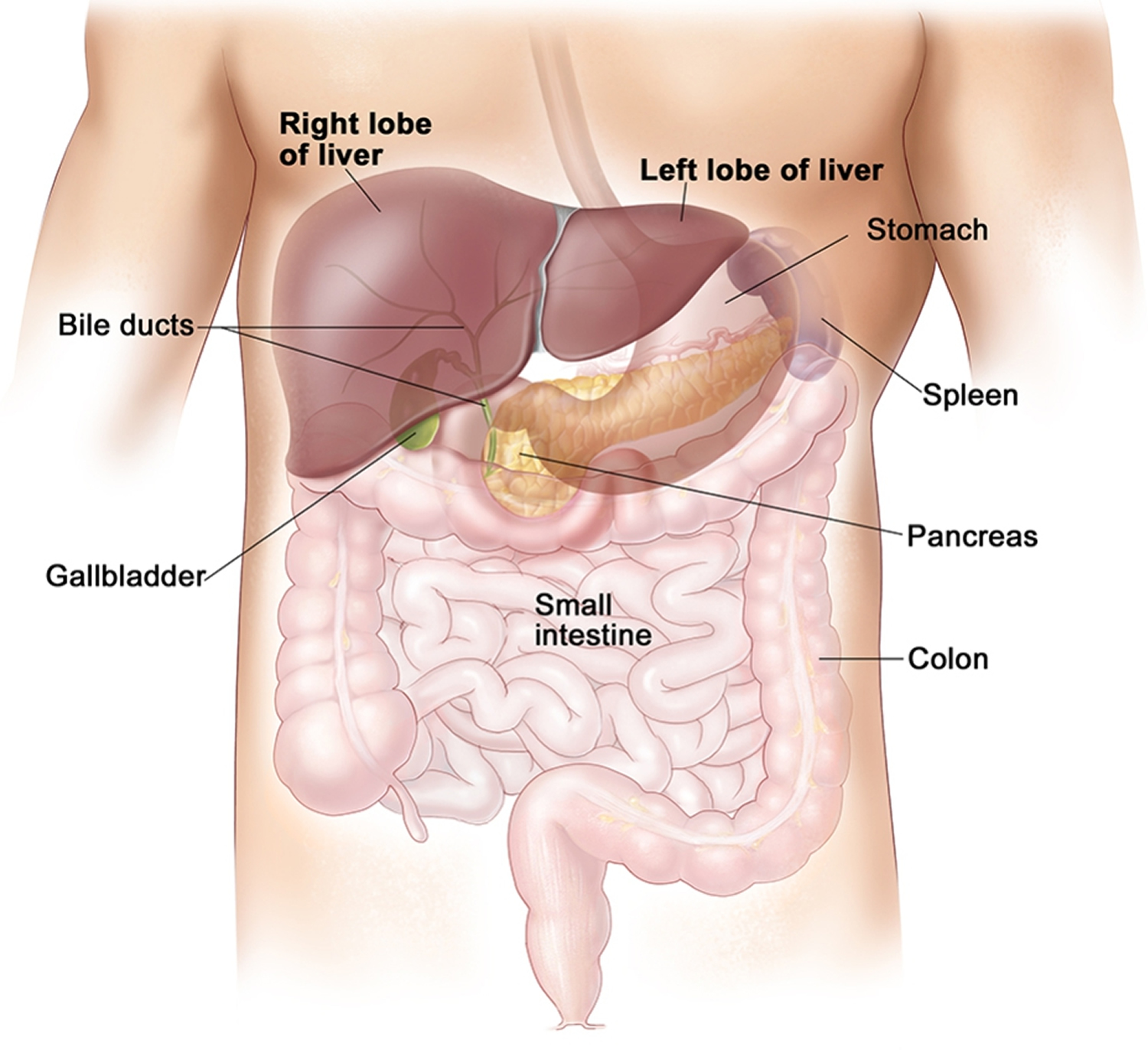
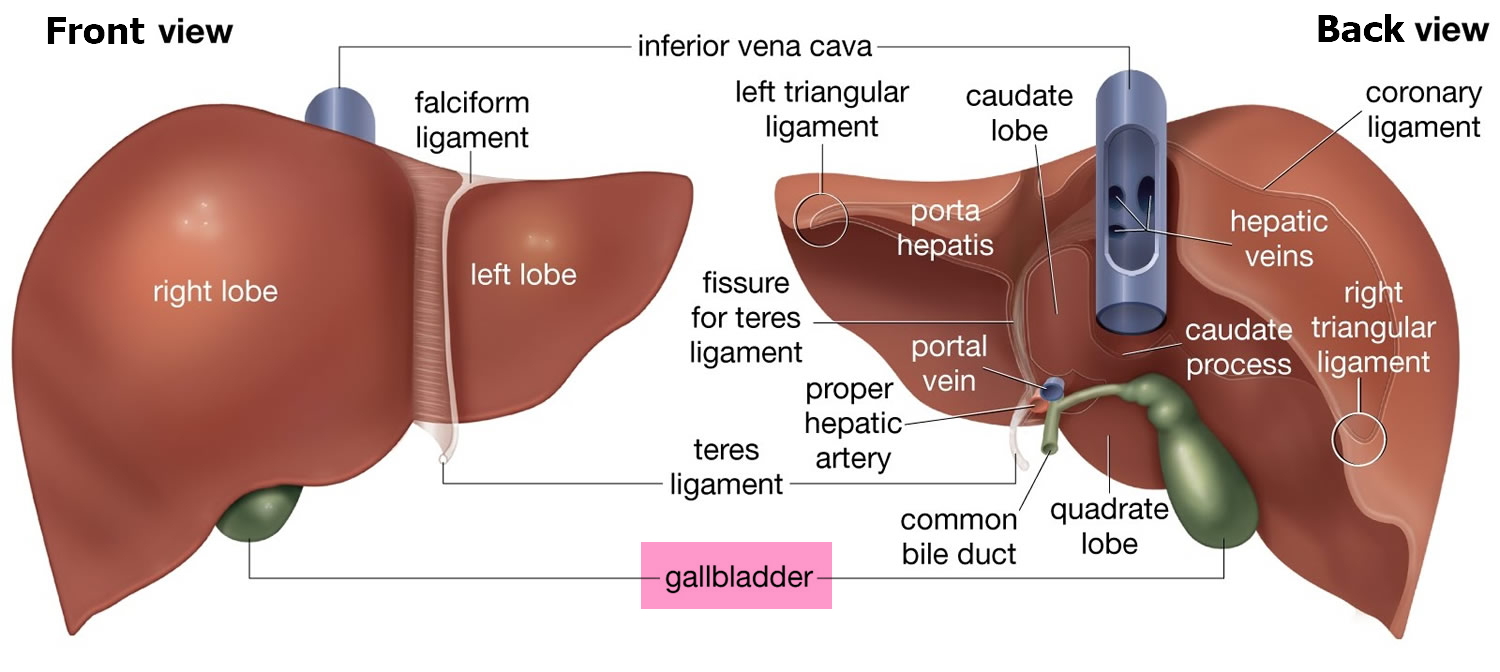
The liver is the body’s largest internal organ and you cannot live without your liver. Your liver is called the body’s metabolic factory because of the important role it plays in metabolism:
- It breaks down and stores many of the nutrients absorbed from the intestine that your body needs to function. Some nutrients must be changed (metabolized) in the liver before they can be used for energy or to build and repair body tissues.
- It makes most of the clotting factors that keep you from bleeding too much when you are cut or injured.
- It secretes bile into the intestines to help absorb nutrients (especially fats).
- It breaks down alcohol, drugs, and toxic wastes in the blood, which then pass from the body through urine and stool.
The liver carries on many important metabolic activities. The liver plays a key role in carbohydrate metabolism by helping maintain concentration of blood glucose within the normal range. Liver cells responding to the hormone insulin lower the blood glucose level by polymerizing glucose to glycogen. Liver cells responding to the hormone glucagon raise the blood glucose level by breaking down glycogen to glucose or by converting noncarbohydrates into glucose.
The liver’s effects on lipid metabolism include oxidizing (breaking down) fatty acids at an especially high rate; synthesizing lipoproteins, phospholipids, and cholesterol; and converting excess portions of carbohydrate molecules into fat molecules. The blood transports fats synthesized in the liver to adipose tissue for storage.
Other liver functions concern protein metabolism. They include deaminating amino acids; forming urea; synthesizing plasma proteins such as clotting factors; and converting certain amino acids into other amino acids.
The liver also stores many substances, including glycogen, iron, and vitamins A, D, and B12. In addition, macrophages in the liver help destroy damaged red blood cells and phagocytize foreign antigens. The liver also removes toxic substances such as alcohol and certain drugs from blood (detoxification).
A healthy liver is necessary for survival. The liver can regenerate most of its own cells when they become damaged. However, if injury to the liver is too severe or long lasting, regeneration is incomplete, and the liver creates scar tissue 2. Scarring of the liver, also called fibrosis, may lead to cirrhosis.
The buildup of scar tissue that causes cirrhosis is usually a slow and gradual process. In the early stages of cirrhosis, the liver continues to function. However, as cirrhosis gets worse and scar tissue replaces more healthy tissue, the liver will begin to fail. Chronic liver failure, which is also called end-stage liver disease, progresses over months, years, or even decades. With end-stage liver disease, the liver can no longer perform important functions or effectively replace damaged cells.
Cirrhosis is the 12th leading cause of death in the United States, accounting for nearly 32,000 deaths each year. More men die of cirrhosis than women 3.
Cirrhosis of the liver can lead to:
- Easy bruising or bleeding, or nosebleeds
- Swelling of the abdomen or legs
- Extra sensitivity to medicines
- High blood pressure in the vein entering the liver
- Enlarged veins called varices in the esophagus and stomach. Varices can bleed suddenly.
- Kidney failure
- Jaundice
- Severe itching
- Gallstones
A small number of people with cirrhosis get liver cancer.
Your doctor will diagnose cirrhosis with blood tests, imaging tests, or a biopsy.
Figure 1. Location of the human liver
Figure 2. Liver anatomy
Figure 3. Cirrhosis of the liver
What causes cirrhosis of the liver
Cirrhosis has many causes. In the United States, the most common causes are chronic alcoholism and hepatitis. Many people with cirrhosis have more than one cause of liver damage. Nothing will make the scar tissue disappear, but treating the cause can keep it from getting worse. If too much scar tissue forms, you may need to consider a liver transplant.
The list below shows common causes of cirrhosis in the United States 2. While chronic hepatitis C and alcohol-related liver disease are the most common causes of cirrhosis, the incidence of cirrhosis caused by nonalcoholic fatty liver disease is rising due to increasing rates of obesity.
Most Common Causes of Cirrhosis
Chronic hepatitis C
Hepatitis C is due to a viral infection that causes inflammation, or swelling, and damage to the liver. The hepatitis C virus spreads through contact with infected blood, such as from a needlestick accident, injection drug use, or receiving a blood transfusion before 1992. Less commonly, hepatitis C can be spread by sexual contact with an infected person or at the time of childbirth from an infected mother to her newborn.
Hepatitis C often becomes chronic, with long-term persistence of the viral infection. Chronic hepatitis C causes damage to the liver that, over years or decades, can lead to cirrhosis. Advanced therapies for chronic hepatitis C now exist, and health care providers should treat people with chronic hepatitis C before they develop severe fibrosis or cirrhosis. Unfortunately, many people first realize they have chronic hepatitis C when they develop symptoms of cirrhosis.
Alcoholism is the second most common cause of cirrhosis in the United States. Most people who consume alcohol do not suffer damage to the liver. However, heavy alcohol use over several years makes a person more likely to develop alcohol-related liver disease. The amount of alcohol it takes to damage the liver varies from person to person. Research suggests that drinking two or fewer drinks a day for women and three or fewer drinks a day for men may not injure the liver 4. Drinking more than these amounts leads to fat and inflammation in the liver, which over 10 to 12 years can lead to alcoholic cirrhosis 5.
Nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH)
In nonalcoholic fatty liver disease (NAFLD), fat builds up in the liver; however, the fat buildup is not due to alcohol use. When the fat accompanies inflammation and liver cell damage, the condition is called nonalcoholic steatohepatitis, or nonalcoholic steatohepatitis (NASH), with “steato” meaning fat, and “hepatitis” meaning inflammation of the liver. The inflammation and damage can cause fibrosis, which eventually can lead to cirrhosis.
Extra fat in the liver has many causes and is more common in people who:
- are overweight or obese.
- have diabetes—a condition characterized by high blood glucose, also called high blood sugar.
- have high blood cholesterol and triglycerides, called hyperlipidemia.
- have high blood pressure.
- have metabolic syndrome—a group of traits and medical conditions linked to being overweight and obese that makes people more likely to develop both cardiovascular disease and type 2 diabetes. Metabolic syndrome is defined as the presence of any three of the following: large waist size, high triglycerides in the blood, abnormal levels of cholesterol in the blood, high blood pressure, and higher than normal blood glucose levels. NASH may represent the liver component of the metabolic syndrome.
Nonalcoholic steatohepatitis (NASH) now ranks as the third most common cause of cirrhosis in the United States.
Chronic hepatitis B
Hepatitis B, like hepatitis C, is due to a viral infection that causes inflammation and damage to the liver. Chronic infection can lead to damage and inflammation, fibrosis, and cirrhosis. The hepatitis B virus spreads through contact with infected blood, such as by needlestick accident, injection drug use, or receiving a blood transfusion before the mid-1980s. Hepatitis B also spreads through sexual contact with an infected person and from an infected mother to child during childbirth.
In the United States, hepatitis B is somewhat uncommon, affecting less than 1 percent of the population, or fewer than one in 100 people.5 In many areas of the world, however, hepatitis B is common. In some parts of Africa and in most of Asia and the Pacific Islands, about 5 to 7 percent of the population has chronic hepatitis B. In some parts of Africa, more than 8 percent of the population has chronic hepatitis B.6 For these reasons, hepatitis B is likely the major cause of cirrhosis worldwide. However, in the United States, hepatitis B ranks well behind hepatitis C, alcohol-related liver disease, and nonalcoholic steatohepatitis (NASH).
Therapies for chronic hepatitis B now exist and health care providers should treat people with chronic hepatitis B before they develop severe fibrosis or cirrhosis. Unfortunately, many people first realize they have chronic hepatitis B when they develop symptoms of cirrhosis.
Hepatitis B is also a preventable disease. Since the 1980s, a hepatitis B vaccine has been available and should be given to newborns and children in the United States. Adults at higher risk of getting hepatitis B should also get the vaccine.
Less Common Causes of Cirrhosis
Less common causes of cirrhosis include the following:
Autoimmune hepatitis
In this form of hepatitis, the body’s immune system attacks liver cells and causes inflammation, damage, and eventually cirrhosis. Normally, the immune system protects people from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances. In autoimmune diseases, the body’s immune system attacks the body’s own cells and organs. Researchers believe genetics, or inherited genes, may make some people more likely to develop autoimmune diseases. At least 70 percent of those with autoimmune hepatitis are female 6.
Diseases that damage, destroy, or block the bile ducts. Several diseases can damage, destroy, or block the ducts that carry bile from the liver to the small intestine, causing bile to back up in the liver and leading to cirrhosis. In adults, the most common of these diseases is primary biliary cirrhosis, a chronic disease that causes the small bile ducts in the liver to become inflamed and damaged and ultimately disappear. Primary sclerosing cholangitis is a disease that causes irritation, scarring, and narrowing of the larger bile ducts of the liver.
In infants and children, causes of damage to or disappearance of bile ducts that can lead to cirrhosis include:
- Alagille syndrome, a collection of symptoms that indicates a genetic digestive disorder and leads to a loss of bile ducts in infancy.
- Biliary atresia, a life-threatening condition that affects newborns in which bile ducts are missing. The cause is unknown. Biliary atresia is the most common reason for liver transplantation in children 7.
- Cystic fibrosis, an inherited disease of the lungs, intestines, pancreas, and bile ducts in which the body does not produce enough fluid and mucus becomes thick and blocks off small bile ducts. This blockage of the bile ducts can lead to cirrhosis.
Long-term blockage of the bile ducts by gallstones can cause cirrhosis. Cirrhosis may also develop if the bile ducts are mistakenly tied off or injured during surgery on the gallbladder or liver.
Inherited diseases that affect the liver
Inherited diseases that interfere with how the liver produces, processes, and stores enzymes, proteins, metals, and other substances can cause cirrhosis. These diseases include alpha-1 antitrypsin deficiency, hemochromatosis, Wilson disease, galactosemia, and glycogen storage diseases.
Hepatitis D, or hepatitis delta, and hepatitis E are two rare viral infections of the liver. Hepatitis D infection occurs only in people who have hepatitis B. People infected with chronic hepatitis B and chronic hepatitis D are more likely to develop cirrhosis than people infected with chronic hepatitis B alone 8.
Hepatitis E is a virus found in domestic and wild animals, particularly pigs, and can cause hepatitis in humans. People with weakened immune systems, including people who are liver or kidney transplant recipients or who have acquired immune deficiency syndrome (AIDS), can develop chronic hepatitis E. Chronic hepatitis E can cause scarring of the liver and cirrhosis. Current treatments for chronic hepatitis D and E are experimental and only partially effective.
Other causes. Other causes of cirrhosis may include:
- reactions to medications taken over a period of time.
- prolonged exposure to toxic chemicals.
- parasitic infections.
- chronic heart failure with liver congestion, a condition in which blood flow out of the liver is slowed. Liver congestion can also occur after surgery to correct
- a congenital heart problem—a heart problem that is present at birth.
Trauma to the liver or other acute, or short term, causes of damage do not cause cirrhosis. Usually, years of chronic injury are required to cause cirrhosis.
Cirrhosis of the liver signs and symptoms
Many people with cirrhosis have no symptoms in the early stages of the disease. However, as the disease progresses, a person may experience the following symptoms:
- Fatigue or feeling tired
- Weakness
- Itching or itchy skin
- Loss of appetite
- Weight loss
- Nausea
- Bloating of the abdomen from ascites—a buildup of fluid in the abdomen
- Edema—swelling due to a buildup of fluid—in the feet, ankles, or legs
- Spider like blood vessels, called spider angiomas, on the skin
- Jaundice, a condition that causes the skin and whites of the eyes to turn yellow
- Bleeding easily
- Bruising easily
- Confusion, drowsiness and slurred speech (hepatic encephalopathy)
- Redness in the palms of the hands
- Testicular atrophy in men
- Breast enlargement in men
What are the complications of cirrhosis ?
As the liver fails, complications may develop. In some people, complications may be the first signs of the disease. Complications of cirrhosis may include the following:
Portal hypertension
The portal vein carries blood from the stomach, intestines, spleen, gallbladder, and pancreas to the liver. In cirrhosis, scar tissue partially blocks the normal flow of blood, which increases the pressure in the portal vein. This condition is called portal hypertension. Portal hypertension is a common complication of cirrhosis. This condition may lead to other complications, such as:
- fluid buildup leading to edema and ascites
- enlarged blood vessels, called varices, in the esophagus, stomach, or both
- an enlarged spleen, called splenomegaly
- mental confusion due to a buildup of toxins that are ordinarily removed by the liver, a condition called hepatic encephalopathy
Edema and ascites
Liver failure causes fluid buildup that results in edema and ascites. Ascites can lead to spontaneous bacterial peritonitis, a serious infection that requires immediate medical attention.
Varices
Portal hypertension may cause enlarged blood vessels in the esophagus, stomach, or both. These enlarged blood vessels, called esophageal or gastric varices, cause the vessel walls to become thin and blood pressure to increase, making the blood vessels more likely to burst. If they burst, serious bleeding can occur in the esophagus or upper stomach, requiring immediate medical attention.
Splenomegaly
Portal hypertension may cause the spleen to enlarge and retain white blood cells and platelets, reducing the numbers of these cells and platelets in the blood. A low platelet count may be the first evidence that a person has developed cirrhosis.
Hepatic encephalopathy
A failing liver cannot remove toxins from the blood, so they eventually accumulate in the brain. The buildup of toxins in the brain is called hepatic encephalopathy. This condition can decrease mental function and cause stupor and even coma. Stupor is an unconscious, sleeplike state from which a person can only be aroused briefly by a strong stimulus, such as a sharp pain.
Coma is an unconscious, sleep like state from which a person cannot be aroused. Signs of decreased mental function include:
- confusion
- personality changes
- memory loss
- trouble concentrating
- a change in sleep habits
Metabolic bone diseases
Some people with cirrhosis develop a metabolic bone disease, which is a disorder of bone strength usually caused by abnormalities of vitamin D, bone mass, bone structure, or minerals, such as calcium and phosphorous. Osteopenia is a condition in which the bones become less dense, making them weaker. When bone loss becomes more severe, the condition is referred to as osteoporosis. People with these conditions are more likely to develop bone fractures.
Gallstones and bile duct stones
If cirrhosis prevents bile from flowing freely to and from the gallbladder, the bile hardens into gallstones. Symptoms of gallstones include abdominal pain and recurrent bacterial cholangitis—irritated or infected bile ducts. Stones may also form in and block the bile ducts, causing pain, jaundice, and bacterial cholangitis.
Bruising and bleeding
When the liver slows the production of or stops producing the proteins needed for blood clotting, a person will bruise or bleed easily.
Sensitivity to medications.
Cirrhosis slows the liver’s ability to filter medications from the blood. When this slowdown occurs, medications act longer than expected and build up in the body. For example, some pain medications may have a stronger effect or produce more side effects in people with cirrhosis than in people with a healthy liver.
Insulin resistance and type 2 diabetes
Cirrhosis causes resistance to insulin. The pancreas tries to keep up with the demand for insulin by producing more; however, extra glucose builds up in the bloodstream, causing type 2 diabetes.
Liver cancer
Liver cancer is common in people with cirrhosis. Liver cancer has a high mortality rate. Current treatments are limited and only fully successful if a health care provider detects the cancer early, before the tumor is too large. For this reason, health care providers should check people with cirrhosis for signs of liver cancer every 6 to 12 months. Health care providers use blood tests, ultrasound, or both to check for signs of liver cancer.
Other complications
Cirrhosis can cause immune system dysfunction, leading to an increased chance of infection. Cirrhosis can also cause kidney and lung failure, known as hepatorenal and hepatopulmonary syndromes.
How is cirrhosis diagnosed ?
A health care provider usually diagnoses cirrhosis based on the presence of conditions that increase its likelihood, such as heavy alcohol use or obesity, and symptoms. A health care provider may test for cirrhosis based on the presence of these conditions alone because many people do not have symptoms in the early stages of the disease. A health care provider may confirm the diagnosis with:
- a medical and family history
- a physical exam
- a blood test
- imaging tests
- a liver biopsy
Medical and family history. Taking a medical and family history is one of the first things a health care provider may do to help diagnose cirrhosis. He or she will ask the patient to provide a medical and family history.
Physical exam. A physical exam may help diagnose cirrhosis. During a physical exam, a health care provider usually:
- examines a patient’s body
- uses a stethoscope to listen to sounds in the abdomen
- taps on specific areas of the patient’s body
The health care provider will perform a physical exam to look for signs of the disease. For example, the liver may feel hard or ascites may cause the abdomen to enlarge.
Blood test. A blood test involves drawing blood at a health care provider’s office or a commercial facility and sending the sample to a lab for analysis. Blood tests can show abnormal liver enzyme levels or abnormal numbers of blood cells or platelets.
Blood tests can help find the cause in people with diagnosed cirrhosis. For example, a health care provider may use blood tests to diagnose hepatitis B and C.
Health care providers use three blood tests to measure the severity of cirrhosis:
- bilirubin, which tests the amount of bile pigment in the blood
- creatinine, which tests kidney function
- international normalized ratio, which tests the blood’s ability to clot
The results of these blood tests are used to calculate the Model for End-stage Liver Disease (MELD) score 9. Experts developed the MELD score to predict the 90-day survival rate of people with end-stage liver disease. MELD scores usually range between 6 and 40, with a score of 6 indicating the best likelihood of 90-day survival. The MELD score is used to determine whether a person is eligible for liver transplantation.
Imaging tests. Imaging tests can show signs of advanced cirrhosis, such as irregularities in the liver surface, gastric varices, and splenomegaly. These tests can also detect signs of complications, such as ascites and liver cancer.
- Ultrasound uses a device, called a transducer, that bounces safe, painless sound waves off organs to create an image of their structure. A specially trained technician performs the procedure in a health care provider’s office, an outpatient center, or a hospital, and a radiologist—a doctor who specializes in medical imaging—interprets the images. A patient does not need anesthesia.
- Computerized tomography (CT) scans use a combination of x rays and computer technology to create images. For a CT scan, a technician may give the patient a solution to drink and an injection of a special dye, called contrast medium. CT scans require the patient to lie on a table that slides into a tunnelshaped device where the technician takes the x rays. An x-ray technician performs the procedure in an outpatient center or a hospital, and a radiologist interprets the images. A patient does not need anesthesia.
- Magnetic resonance imaging (MRI) machines use radio waves and magnets to produce detailed pictures of the body’s internal organs and soft tissues without using x rays. A specially trained technician performs the procedure in an outpatient center or a hospital, and a radiologist interprets the images. A patient does not need anesthesia, though a health care provider may use light sedation for patients with a fear of confined spaces. An MRI may include the injection of contrast medium. With most MRI machines, the patient lies on a table that slides into a tunnel-shaped device that may be open ended or closed at one end; some machines allow the patient to lie in a more open space.
- Elastography, also called liver stiffness measurement, uses either ultrasound or MRI to measure the stiffness of the liver. Scar tissue increases the stiffness of the liver. Elastography can show how much scarring is present with some reliability. Elastography is a relatively new test. However, this test promises to be helpful in showing how severe liver scarring is and whether the scarring is getting worse over time.
Liver biopsy. A liver biopsy is a procedure that involves taking a piece of liver tissue for examination with a microscope for signs of damage or disease. The health care provider may ask the patient to stop taking certain medications temporarily before the liver biopsy. The health care provider may ask the patient to fast for 8 hours before the procedure.
During the procedure, the patient lies on a table, right hand resting above the head. The health care provider applies a local anesthetic to the area where he or she will insert the biopsy needle. If needed, a health care provider will also give sedatives and pain medication. The health care provider uses a needle to take a small piece of liver tissue. He or she may use ultrasound, CT scans, or other imaging techniques to guide the needle. After the biopsy, the patient must lie on the right side for up to 2 hours and is monitored an additional 2 to 4 hours before being sent home.
A health care provider performs a liver biopsy at a hospital or an outpatient center. The health care provider sends the liver sample to a pathology lab, where the pathologist—a doctor who specializes in diagnosing diseases—looks at the tissue with a microscope and sends a report to the patient’s health care provider.
A liver biopsy can confirm the diagnosis of cirrhosis; however, a person does not always need this test. A health care provider will perform a biopsy if the result might help determine the cause or affect treatment. Sometimes a health care provider finds a cause of liver damage other than cirrhosis during biopsy.
How is cirrhosis of the liver treated ?
Treatment for cirrhosis depends on the cause of the disease and whether complications are present. In the early stages of cirrhosis, the goals of treatment are to slow the progression of tissue scarring in the liver and prevent complications. As cirrhosis progresses, a person may need additional treatments and hospitalization to manage complications. Treatment may include the following:
Avoiding Alcohol and Illegal Substances
People with cirrhosis should not drink any alcohol or take any illegal substances, as both will cause more liver damage.
Preventing Problems with Medications
People with cirrhosis should be careful about starting new medications and should consult a health care provider before taking prescription medications, over-the-counter medications, or vitamins. People with cirrhosis should avoid complementary and alternative medications, such as herbs.
Cirrhosis slows the liver’s ability to filter medications from the blood. When this slowdown occurs, medications act longer than expected and build up in the body. Some medications and vitamins may also affect liver function.
Viral Hepatitis Vaccination and Screening
All people with cirrhosis should consider vaccination against hepatitis A and B. An infection with one of these hepatitis viruses can cause cirrhosis to get worse.
Vaccination can easily prevent both infections.
People with cirrhosis should also get a screening blood test for hepatitis C.
Treating Causes of Cirrhosis
Health care providers can treat some causes of cirrhosis, for example, by prescribing antiviral medications for hepatitis B and C. In some instances, these medications cure the viral infection. Health care providers treat autoimmune hepatitis with corticosteroids and other medications that suppress the immune system. Health care providers can treat hemochromatosis and Wilson disease—inherited forms of liver disease caused by the buildup of iron or copper in the liver—if detected early. Health care providers usually treat liver diseases due to blockage or loss of bile ducts with ursodiol (Actigall, Urso). Ursodiol is a nontoxic bile acid that people can take orally. Ursodiol replaces the bile acids that are normally produced by the liver, which are toxic and build up in the liver when the bile ducts are blocked.
Eating, Diet, and Nutrition
A healthy diet is important in all stages of cirrhosis because malnutrition is common in people with this disease. Malnutrition is a condition that occurs when the body does not get enough nutrients. Cirrhosis may lead to malnutrition because it can cause:
- people to eat less because of symptoms such as loss of appetite
- changes in metabolism
- reduced absorption of vitamins and minerals
Health care providers can recommend a meal plan that is well balanced and provides enough calories and protein. If ascites develops, a health care provider or dietitian may recommend a sodium-restricted diet. To improve nutrition, the health care provider may prescribe a liquid supplement. A person may take the liquid by mouth or through a nasogastric tube—a tiny tube inserted through the nose and throat that reaches into the stomach.
A person with cirrhosis should not eat raw shellfish, which can contain a bacterium that causes serious infection. Cirrhosis affects the immune system, making people with cirrhosis more likely than healthy people to develop an infection after eating shellfish that contain this bacterium.
A health care provider may recommend calcium and vitamin D supplements to help prevent osteoporosis.
Home remedies to limit additional liver damage:
- Don’t drink alcohol. Whether your cirrhosis was caused by chronic alcohol use or another disease, avoid alcohol. Drinking alcohol may cause further liver damage.
- Eat a low-sodium diet. Excess salt can cause your body to retain fluids, worsening swelling in your abdomen and legs. Use herbs for seasoning your food, rather than salt. Choose prepared foods that are low in sodium.
- Eat a healthy diet. Cirrhosis leads to malnutrition and loss of muscle. The best defense against this development is to maintain a healthy diet, with a variety of fruits and vegetables. You also need protein, contrary to outdated but still circulating advice to limit this food group if you have cirrhosis. Choose lean protein, such as legumes, poultry or fish. Avoid raw seafood.
- Avoid infections. Cirrhosis makes it more difficult for you to fight off infections. Protect yourself by washing your hands frequently. Also, get vaccinated for hepatitis A and B, influenza, and pneumonia.
- Use over-the-counter medications carefully. Cirrhosis makes it more difficult for your liver to process drugs. For this reason, ask your doctor before taking any medications, including nonprescription drugs. Avoid drugs such as aspirin and ibuprofen (Advil, Motrin IB, others). If you have liver damage, your doctor may recommend you use a lower dose of acetaminophen (Tylenol, others).
- Alternative or herbal medicine include licorice root (glycyrrhiza), schisandra and astragalus have been used to treat liver diseases. However, there is not enough evidence of benefit from clinical trials to recommend the use of any herbal products to treat liver cirrhosis. In addition, herbal medications represent an increasing percentage of reported cases of drug-induced liver injury. Talk with your doctor if you’re interested in trying alternative medicine to help you cope with cirrhosis.
Treating Symptoms and Complications of Cirrhosis
Itching and abdominal pain. A health care provider may give medications to treat various symptoms of cirrhosis, such as itching and abdominal pain.
Portal hypertension. A health care provider may prescribe a beta-blocker or nitrate to treat portal hypertension. Beta-blockers lower blood pressure by helping the heart beat slower and with less force, and nitrates relax and widen blood vessels to let more blood flow to the heart and reduce the heart’s workload.
Varices. Beta-blockers can lower the pressure in varices and reduce the likelihood of bleeding. Bleeding in the stomach or esophagus requires an immediate upper endoscopy. This procedure involves using an endoscope—a small, flexible tube with a light—to look for varices. The health care provider may use the endoscope to perform a band ligation, a procedure that involves placing a special rubber band around the varices that causes the tissue to die and fall off. A gastroenterologist—a doctor who specializes in digestive diseases—performs the procedure at a hospital or an outpatient center. People who have had varices in the past may need to take medication to prevent future episodes.
Edema and ascites. Health care providers prescribe diuretics—medications that remove fluid from the body—to treat edema and ascites. A health care provider may remove large amounts of ascitic fluid from the abdomen and check for spontaneous bacterial peritonitis. A health care provider may prescribe bacteria-fighting medications called antibiotics to prevent infection. He or she may prescribe oral antibiotics; however, severe infection with ascites requires intravenous (IV) antibiotics.
Hepatic encephalopathy. A health care provider treats hepatic encephalopathy by cleansing the bowel with lactulose, a laxative given orally or as an enema—a liquid put into the rectum. A health care provider may also add antibiotics to the treatment. Hepatic encephalopathy may improve as other complications of cirrhosis are controlled.
Hepatorenal syndrome. Some people with cirrhosis who develop hepatorenal syndrome must undergo regular dialysis treatment, which filters wastes and extra fluid from the body by means other than the kidneys. People may also need medications to improve blood flow through the kidneys.
Osteoporosis. A health care provider may prescribe bisphosphonate medications to improve bone density.
Gallstones and bile duct stones. A health care provider may use surgery to remove gallstones. He or she may use endoscopic retrograde cholangiopancreatography, which uses balloons and basketlike devices, to retrieve the bile duct stones.
Liver cancer. A health care provider may recommend screening tests every 6 to 12 months to check for signs of liver cancer. Screening tests can find cancer before the person has symptoms of the disease. Cancer treatment is usually more effective when the health care provider finds the disease early. Health care providers use blood tests, ultrasound, or both to screen for liver cancer in people with cirrhosis. He or she may treat cancer with a combination of surgery, radiation, and chemotherapy.
Stages of cirrhosis of the liver
The Model for End-Stage Liver Disease (MELD) is a measure of the severity of liver dysfunction that is well established among clinicians caring cirrhotic patients 10. It is not uncommon to observe the score being obtained frequently as a prognostic tool in the ICU setting. Furthermore, the MELD score has appeal as a sequential predictor because its components, the serum creatinine, international normalized ratio (INR) and total bilirubin, fluctuate from day to day in ill patients 11.
The Model for End-Stage Liver Disease (MELD) score was initially created to predict survival in patients with complications of portal hypertension undergoing elective placement of transjugular intrahepatic portosystemic shunts (TIPS) 12. The model was subsequently validated as a predictor of survival in several independent cohorts of patients with varying levels of liver disease severity (e.g., hospitalized and ambulatory patients), as well as patients of geographically and temporally diverse origin 13. In a prospective study of candidates on the waiting list, MELD was an excellent predictor of waitlist mortality, 83% of the time, the model correctly predicts the first patient to die 14.
Components of the Model for End-Stage Liver Disease (MELD) score
Bilirubin
In patients with end stage liver disease, serum bilirubin concentration is a well-established marker of the ‘hepatic synthetic function,’ although in the strictest sense, it represents excretory function. Of the three MELD variables, serum bilirubin carries the most weight. It has essentially linear relationship with 90 day mortality in patients waiting for liver transplantation, despite lack of consideration for inter-laboratory variability in the measurement serum bilirubin 15.
In the MELD score, the serum total bilirubin concentration is used for the bilirubin variable. In theory, direct bilirubin is expected to be a better physiologic marker of liver function than total bilirubin, because indirect fraction of bilirubin is susceptible to other processes in the body, such as hemolysis and genetic variability in the bilirubin metabolism. In reality, however, in our evaluation of direct bilirubin as an alternative to total bilirubin.
Creatinine
It is common to see a substantial degree of variability in renal function in patients with end stage liver disease. More importantly, diminished renal function is an important predictor of survival in those patients 16. Incorporation of serum creatinine in the MELD score as a predictor of survival affords considerable advantage over other measures of liver disease such as the Child-Pugh score.
However, accuracy of non-invasive measurement of renal function, including serum creatinine has been shown to be suboptimal among cirrhotic patients 17. True, measured glomerular filtration rate (GFR, e.g., by iothalamate clearance measurement) is better at assessing prognosis than creatinine and mathematic equations containing creatinine. A multivariable model that incorporates calculated GFR and/or serum sodium is superior to the MELD score 18.
There has been a recent push for standardizing creatinine measurement in laboratories. The traditional colorimetric alkaline picric Jaffe method has several limitations, one of which is interference with bilirubin in high concentrations 19. In patients with high serum bilirubin (>25 mg/dL), serum creatinine can be overestimated, leading to imprecise calculation of the MELD score. Accordingly, the new standard is an enzymatic method for measuring serum creatinine. Preferential use of the latter method and standardization of measurement processes has been proposed, especially in patients with serum bilirubin >25 mg/dl 14.
INR
Prothrombin time and the INR reflect coagulopathy associated with synthetic dysfunction in patients with end stage liver disease. The liver plays an important role in the coagulation pathways by generating most of the clotting factors. In patients with end stage liver disease, decreased production of factors along the intrinsic pathway prolongs prothrombin time. Figure 1 shows that after adjusting for bilirubin and creatinine, INR is associated with a steep increase in mortality risk. However, once it reaches approximately 3, the risk does not seem to increase any further.
There remains a strong need for a reproducible and accurate measure of coagulopathy in liver patients, which may replace INR in MELD making it even more accurate 20. At the current time, however, INR remains a practically useful and statistically significant correlate of mortality risk in patients with end stage liver disease 21. It is also widely available and is likely continue to be used an indicator of survival in patients with end stage liver disease and a component of the MELD score 14.
Application of MELD in Liver Transplantation
Coinciding with the implementation of MELD-based liver allocation, there was an immediate 12% reduction in liver transplant waiting list registrations, especially in candidates with MELD scores of less than 10 22. More importantly, there was a 3.5% reduction in waiting list death rate 22, 18, 23, accompanied by a decrease in median waiting time from 656 days to 416 days 24. More recent data showed longer term benefits of the MELD system: between 2002 and 2008, the number of wait list candidates decreased by 3.4%, while the annual dropout rate from the waiting list remained stationary 25. Waiting time also decreased with a higher proportion of candidates being transplanted within 30 days (23% 2001 to 37% in 2008). Thus, the MELD score has been a pivotal element of the current allocation system, contributing to more effective allocation of the scarce donor organs and to a significant increase in the probability of receiving a liver transplantation 26.
When is a liver transplant considered for cirrhosis of the liver ?
A health care provider may consider a liver transplant when cirrhosis leads to liver failure or treatment for complications is ineffective. Liver transplantation is surgery to remove a diseased or an injured liver and replace it with a healthy whole liver or part of a liver from another person, called a donor.
Candidates for liver transplant undergo extensive testing to determine whether they are healthy enough to have a good outcome following surgery. Additionally, transplant centers typically require some period of abstinence alcohol for people with alcohol-related liver disease before they can receive transplants.
For adults in the United States, the most common reasons for needing a liver transplant in 2016 were 27:
- alcoholic liver disease
- cancers that start in the liver combined with cirrhosis
- fatty liver disease (nonalcoholic steatohepatitis)
- cirrhosis caused by chronic hepatitis C
Biliary atresia is the most common reason children need a liver transplant 27.
Doctors may consider a liver transplant to treat rare disorders such as urea cycle disorders and familial hypercholesterolemia.
What are the survival rates after a liver transplant ?
For patients receiving liver transplants from deceased donors, the survival rates are 27:
- 86 percent at 1 year
- 78 percent at 3 years
- 72 percent at 5 years
The 20-year survival rate is about 53 percent 28.
Your chances of a successful liver transplant and long-term survival depend on your personal situation.
- Cirrhosis. Medline Plus. https://medlineplus.gov/cirrhosis.html[↩]
- Cirrhosis. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/liver-disease/cirrhosis[↩][↩]
- Murphy SL, Xu J, Kochanek KD. Deaths: final data for 2010. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_04.pdf[↩]
- O’Shea RS, Dasarathy S, McCullough AJ. Alcoholic liver disease. Hepatology. 2010;51(1):307–328.[↩]
- Gyamfi MA, Wan YJ. Pathogenesis of alcoholic liver disease: the role of nuclear receptors. Experimental Biology and Medicine. 2010;235(5):547–560.[↩]
- Makol A, Watt KD, Chowdhary VR. Autoimmune hepatitis: a review of current diagnosis and treatment. Hepatitis Research and Treatment. 2011:2011;1–11.[↩]
- Boudi FB. Pediatric liver transplantation. http://emedicine.medscape.com/article/1012910-overview[↩]
- Lok ASF, McMahon BJ. Chronic hepatitis B. American Association for the Study of Liver Diseases. https://www.aasld.org[↩]
- Asrani SK, Kim WR. Model for End Stage Liver Disease: End of the First Decade. Clinics in liver disease. 2011;15(4):685-698. doi:10.1016/j.cld.2011.08.009. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3564596/[↩]
- Peeraphatdit T, Naksuk N, Thongprayoon C, et al. Model for End-Stage Liver Disease (MELD) Score Measurements on The Daily Basis in Critically Ill Cirrhotic Patients Do Not Provide Additional Prognostic Value. Mayo Clinic proceedings. 2015;90(9):1196-1206. doi:10.1016/j.mayocp.2015.06.017. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4567441/[↩]
- Coagulopathy of acute liver failure. Munoz SJ, Stravitz RT, Gabriel DA. Clin Liver Dis. 2009 Feb; 13(1):95-107. https://www.ncbi.nlm.nih.gov/pubmed/19150314/[↩]
- A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. Hepatology. 2000 Apr; 31(4):864-71. https://www.ncbi.nlm.nih.gov/pubmed/10733541/[↩]
- A model to predict survival in patients with end-stage liver disease. Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D’Amico G, Dickson ER, Kim WR. Hepatology. 2001 Feb; 33(2):464-70. https://www.ncbi.nlm.nih.gov/pubmed/11172350/[↩]
- The model for end-stage liver disease (MELD). Kamath PS, Kim WR, Advanced Liver Disease Study Group. Hepatology. 2007 Mar; 45(3):797-805. https://www.ncbi.nlm.nih.gov/pubmed/17326206/[↩][↩][↩]
- Do we need to MEND the MELD ? Gish RG. Liver Transpl. 2007 Apr; 13(4):486-7. https://www.ncbi.nlm.nih.gov/pubmed/17394144/[↩]
- Report of the first international liver transplantation society expert panel consensus conference on renal insufficiency in liver transplantation. Charlton MR, Wall WJ, Ojo AO, Ginès P, Textor S, Shihab FS, Marotta P, Cantarovich M, Eason JD, Wiesner RH, Ramsay MA, Garcia-Valdecasas JC, Neuberger JM, Feng S, Davis CL, Gonwa TA, International Liver Transplantation Society Expert Panel. Liver Transpl. 2009 Nov; 15(11):S1-34. https://www.ncbi.nlm.nih.gov/pubmed/19877213/[↩]
- The evaluation of renal function and disease in patients with cirrhosis. Francoz C, Glotz D, Moreau R, Durand F. J Hepatol. 2010 Apr; 52(4):605-13. https://www.ncbi.nlm.nih.gov/pubmed/20185192/[↩]
- Serum sodium, renal function, and survival of patients with end-stage liver disease. Lim YS, Larson TS, Benson JT, Kamath PS, Kremers WK, Therneau TM, Kim WR. J Hepatol. 2010 Apr; 52(4):523-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4546826/[↩][↩]
- Different methods of creatinine measurement significantly affect MELD scores. Cholongitas E, Marelli L, Kerry A, Senzolo M, Goodier DW, Nair D, Thomas M, Patch D, Burroughs AK. Liver Transpl. 2007 Apr; 13(4):523-9. https://www.ncbi.nlm.nih.gov/pubmed/17323365/[↩]
- Determining the model for end-stage liver disease with better accuracy: neutralizing the international normalized ratio pitfalls. Marlar RA. Hepatology. 2007 Aug; 46(2):295-6. https://www.ncbi.nlm.nih.gov/pubmed/17661420/[↩]
- A revised model for end-stage liver disease optimizes prediction of mortality among patients awaiting liver transplantation. Leise MD, Kim WR, Kremers WK, Larson JJ, Benson JT, Therneau TM. Gastroenterology. 2011 Jun; 140(7):1952-60. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4546828/[↩]
- Results of the first year of the new liver allocation plan. Freeman RB, Wiesner RH, Edwards E, Harper A, Merion R, Wolfe R, United Network for Organ Sharing Organ Procurement and Transplantation Network Liver and Transplantation Committee. Liver Transpl. 2004 Jan; 10(1):7-15. https://www.ncbi.nlm.nih.gov/pubmed/14755772/[↩][↩]
- Model for end-stage liver disease: did the new liver allocation policy affect waiting list mortality? Austin MT, Poulose BK, Ray WA, Arbogast PG, Feurer ID, Pinson CW. Arch Surg. 2007 Nov; 142(11):1079-85. https://www.ncbi.nlm.nih.gov/pubmed/18025337/[↩]
- Wiesner R, Lake JR, Freeman RB, et al. Model for end-stage liver disease (MELD) exception guidelines. Liver Transpl. 2006;12(12) Suppl 3:S85–S87. https://www.ncbi.nlm.nih.gov/pubmed/17123285[↩]
- Thuluvath PJ, Guidinger MK, Fung JJ, et al. Liver transplantation in the United States 1999–2008. Am J Transplant. 2010;10(4 Pt 2):1003–1019. https://www.ncbi.nlm.nih.gov/pubmed/20420649[↩]
- Impact of MELD on waitlist outcome of retransplant candidates. Kim HJ, Larson JJ, Lim YS, Kim WR, Pedersen RA, Therneau TM, Rosen CB. Am J Transplant. 2010 Dec; 10(12):2652-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4547838/[↩]
- Organ Procurement and Transplantation Network. Health Resources and Services Administration, U.S. Department of Health and Human Services. https://optn.transplant.hrsa.gov/data/view-data-reports/build-advanced[↩][↩][↩]
- Schoening WN, Buescher N, Rademacher S, et al. Twenty-year longitudinal follow-up after orthotopic liver transplantation: a single-center experience of 313 consecutive cases. American Journal of Transplantation. 2013;13(9):2384–2394.[↩]