Contents
- What is heart pain ?
- Types of Angina
- Stable Angina
- Unstable Angina
- Variant (Prinzmetal’s) Angina
- Microvascular Angina
- Causes of microvascular angina:
- Symptoms of microvascular angina:
- Coronary Microvascular Disease
- What Causes Coronary Microvascular Disease ?
- Understand Your Risk for Coronary Microvascular Disease ?
- What Are the Signs and Symptoms of Coronary Microvascular Disease ?
- Diagnosis of Coronary Microvascular Disease
- Diagnostic Tests for Coronary Microvascular Disease
- Treatment of Coronary Microvascular Disease
- Prevention of Coronary Microvascular Disease
- Angina in Women
- What Is Pulmonary Embolism ?
- What is Aortic Dissection
- What is Aortic Valve Stenosis
- What is Hypertrophic cardiomyopathy
- What is Pericarditis
- What is Panic Attack
What is heart pain ?
Heart pain or angina is chest pain or discomfort caused when your heart muscle doesn’t get enough oxygen-rich blood 1. It may feel like pressure or squeezing in your chest 2. The discomfort also can occur in your shoulders, arms, neck, jaw, or back. Angina pain may even feel like indigestion 1.
But, angina is not a disease. Heart pain or angina is a symptom of an underlying heart problem, usually coronary heart disease (coronary artery disease). There are many types of angina, including microvascular angina, Prinzmetal’s angina, stable angina, unstable angina and variant angina.
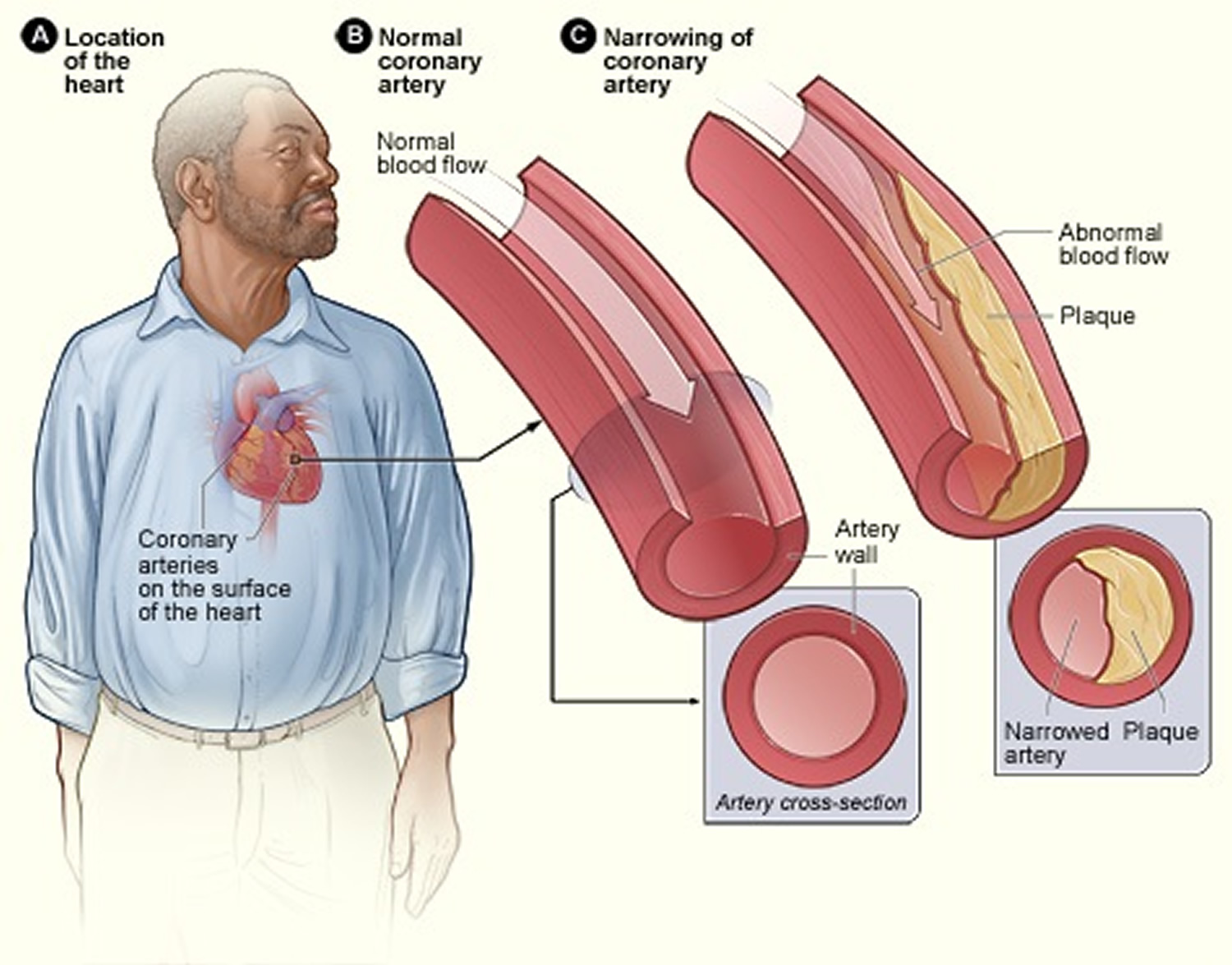
Coronary heart disease (coronary artery disease) is the most common type of heart disease in adults. It occurs if a waxy substance called plaque builds up on the inner walls of your coronary arteries. These arteries carry oxygen-rich blood to your heart. Heart pain or angina usually happens because one or more of the coronary arteries is narrowed or blocked, also called ischemia.
Experts believe that nearly 7 million people in the United States suffer from angina 2. The condition occurs equally among men and women 2.
Angina can be a sign of coronary heart disease (coronary artery disease), even if initial tests don’t point to the disease. However, not all chest pain or discomfort is a sign of coronary heart disease (coronary artery disease) 2.
Heart pain symptoms
Pain and discomfort are the main symptoms of angina. Angina often is described as pressure, squeezing, burning, or tightness in the chest. The pain or discomfort usually starts behind the breastbone.
Pain from angina also can occur in the arms, shoulders, neck, jaw, throat, or back. The pain may feel like indigestion. Some people say that angina pain is hard to describe or that they can’t tell exactly where the pain is coming from.
Signs and symptoms such as nausea (feeling sick to your stomach), fatigue (tiredness), shortness of breath, sweating, light-headedness, and weakness also may occur.
Women are more likely to feel discomfort in the neck, jaw, throat, abdomen, or back. Shortness of breath is more common in older people and those who have diabetes. Weakness, dizziness, and confusion can mask the signs and symptoms of angina in elderly people.
Symptoms also vary based on the type of angina you have.
Because angina has so many possible symptoms and causes, all chest pain should be checked by a doctor. Chest pain that lasts longer than a few minutes and isn’t relieved by rest or angina medicine may be a sign of a heart attack. Call your local emergency number right away.
Stable Angina
The pain or discomfort:
- Occurs when the heart must work harder, usually during physical exertion
- Doesn’t come as a surprise, and episodes of pain tend to be alike
- Usually lasts a short time (5 minutes or less)
- Is relieved by rest or medicine
- May feel like gas or indigestion
- May feel like chest pain that spreads to the arms, back, or other areas
Unstable Angina
The pain or discomfort:
- Often occurs at rest, while sleeping at night, or with little physical exertion
- Comes as a surprise
- Is more severe and lasts longer than stable angina (as long as 30 minutes)
- Usually isn’t relieved by rest or medicine
- May get worse over time
- May mean that a heart attack will happen soon
Variant Angina
The pain or discomfort:
- Usually occurs at rest and during the night or early morning hours
- Tends to be severe
- Is relieved by medicine
Microvascular Angina
The pain or discomfort:
- May be more severe and last longer than other types of angina pain
- May occur with shortness of breath, sleep problems, fatigue, and lack of energy
- Often is first noticed during routine daily activities and times of mental stress
Causes of heart pain
Angina usually is a symptom of coronary heart disease (coronary artery disease). This means that the underlying causes of angina generally are the same as the underlying causes of coronary heart disease (coronary artery disease).
Research suggests that coronary heart disease (coronary artery disease) starts when certain factors damage the inner layers of the coronary arteries. These factors include:
- Smoking
- High amounts of certain fats and cholesterol in the blood
- High blood pressure
- High amounts of sugar in the blood due to insulin resistance or diabetes
Plaque may begin to build up where the arteries are damaged. When plaque builds up in the arteries, the condition is called atherosclerosis. Plaque narrows or blocks the arteries, reducing blood flow to the heart muscle. Some plaque is hard and stable and causes the arteries to become narrow and stiff. This can greatly reduce blood flow to the heart and cause angina. Other plaque is soft and more likely to rupture (break open) and cause blood clots. Blood clots can partially or totally block the coronary arteries and cause angina or a heart attack.
Other conditions also can cause chest pain, such as 2:
- Pulmonary embolism (a blockage in a lung artery)
- A lung infection
- Aortic dissection (tearing of a major artery)
- Aortic stenosis (narrowing of the heart’s aortic valve)
- Hypertrophic cardiomyopathy (heart muscle disease)
- Pericarditis (inflammation in the tissues that surround the heart)
- A panic attack
All chest pain should be checked by a doctor !
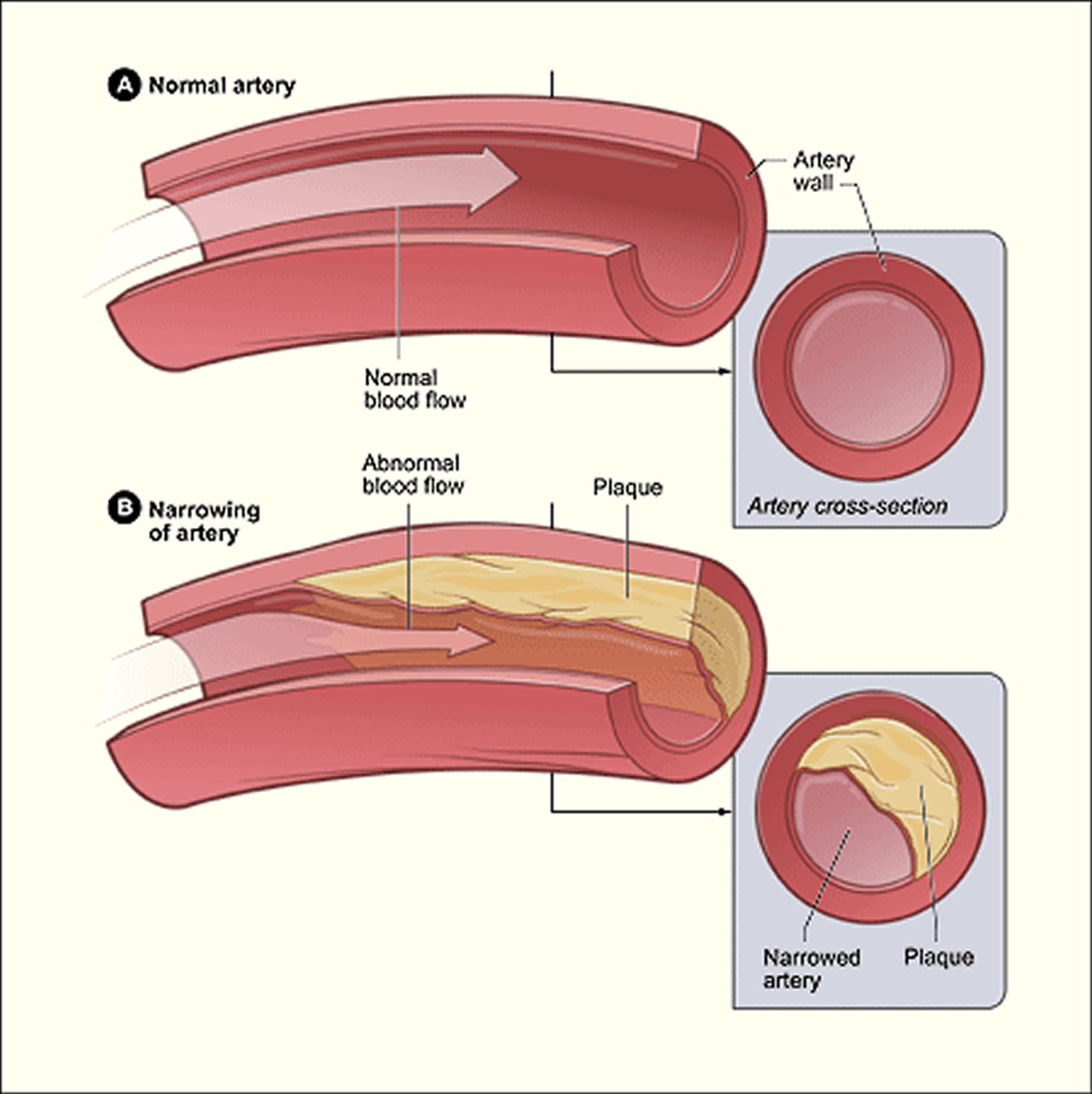
Plaque Buildup in an Artery
Plaque is made up of fat, cholesterol, calcium, and other substances found in the blood. Over time, plaque hardens and narrows your arteries. This limits the flow of oxygen-rich blood to your organs and other parts of your body.
When plaque builds up in the arteries, the condition is called atherosclerosis. Atherosclerosis can lead to serious problems, including heart attack, stroke, or even death.
Atherosclerosis is a disease in which plaque builds up inside your arteries. The buildup of plaque occurs over many years.
Atherosclerosis plaque narrows the coronary arteries and reduces blood flow to your heart muscle. Plaque narrows and stiffens the coronary arteries. This reduces the flow of oxygen-rich blood to the heart muscle, causing chest pain.
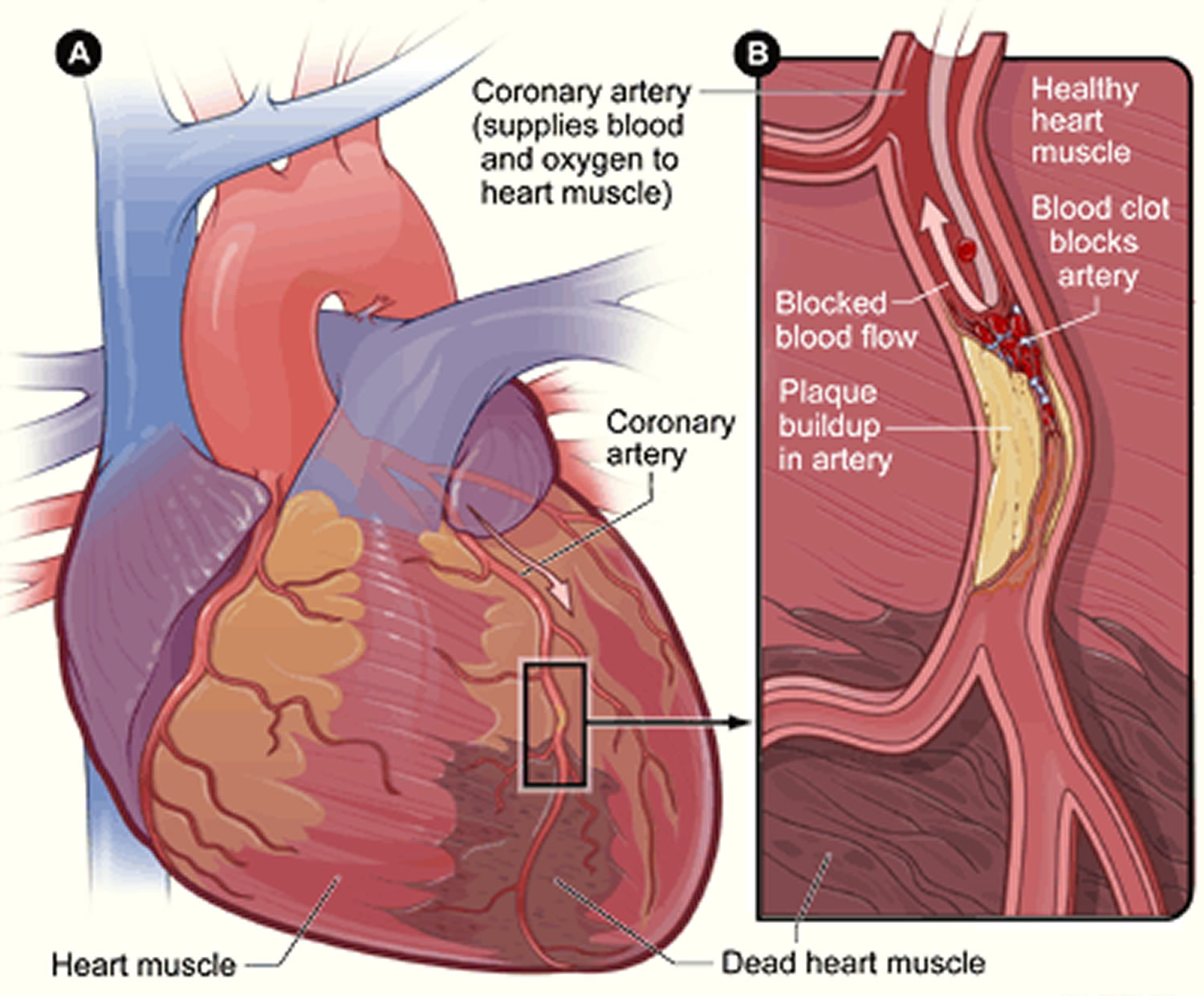
Plaque buildup also makes it more likely that blood clots will form in your arteries. Blood clots can partially or completely block blood flow, which can cause a heart attack.
- If blood flow to your heart muscle is reduced or blocked, you may have angina (chest pain or discomfort) or a heart attack.
When plaque narrows and stiffens the coronary arteries. This reduces the flow of oxygen-rich blood to the heart muscle, causing chest pain. Plaque buildup also makes it more likely that blood clots will form in your arteries. Blood clots can partially or completely block blood flow, which can cause a heart attack.
Angina also can be a symptom of coronary microvascular disease. This disease is called coronary microvascular disease. In coronary microvascular disease, plaque doesn’t cause blockages in the arteries as it does in coronary heart disease. Studies have shown that coronary microvascular disease is more likely to affect women than men. Coronary microvascular disease also is called cardiac syndrome X and nonobstructive coronary heart disease.
Risk for Angina
If you’re at risk for heart disease or coronary microvascular disease, you’re also at risk for angina. The major risk factors for heart disease and coronary microvascular disease include:
- Unhealthy cholesterol levels
- High blood pressure
- Smoking
- Diabetes
- Overweight or obesity
- Metabolic syndrome
- Inactivity
- Unhealthy diet
- Older age (The risk increases for men after 45 years of age and for women after 55 years of age.)
- Family history of early heart disease
Figure 1. Atherosclerosis plaque
[Source 3]Figure 2. Atherosclerosis blocking the coronary artery in your heart
[Source 3]Figure 3. Heart With Muscle Damage and a Blocked Left Coronary Artery
[Source 4]Types of Angina
The major types of angina are stable, unstable, variant (Prinzmetal’s), and microvascular. Knowing how the types differ is important. This is because they have different symptoms and require different treatments.
Stable Angina
Stable angina (angina pectoris) is the most common type of angina 2. It occurs when the heart is working harder than usual 2. Angina often occurs when the heart muscle itself needs more blood than it is getting, for example, during times of physical activity or strong emotions 5. Severely narrowed arteries may allow enough blood to reach the heart when the demand for oxygen is low, such as when you’re sitting. But, with physical exertion—like walking up a hill or climbing stairs—the heart works harder and needs more oxygen.
Stable angina has a regular pattern. (“Pattern” refers to how often the angina occurs, how severe it is, and what factors trigger it.)
If you have stable angina, you can learn its pattern and predict when the pain will occur. The pain usually goes away a few minutes after you rest or take your angina medicine 2.
Stable angina isn’t a heart attack, but it suggests that a heart attack is more likely to happen in the future.
Symptoms of Stable Angina – The pain or discomfort:
- Occurs when the heart must work harder, usually during physical exertion
- Doesn’t come as a surprise, and episodes of pain tend to be alike
- Usually lasts a short time (5 minutes or less)
- Is relieved by rest or medicine
- May feel like gas or indigestion
- May feel like chest pain that spreads to the arms, back, or other areas
Possible triggers of stable angina include:
- Emotional stress – learn stress management
- Exposure to very hot or cold temperatures – learn how cold and hot weather affect the heart.
- Heavy meals
- Smoking.
Treatment of Stable Angina
People with stable angina or sometimes referred to as angina pectoris have episodes of chest pain. The discomfort that are usually predictable and manageable. You might experience it while running or if you’re dealing with stress.
Normally this type of chest discomfort is relieved with rest, nitroglycerin or both. Nitroglycerin relaxes the coronary arteries and other blood vessels, reducing the amount of blood that returns to the heart and easing the heart’s workload. By relaxing the coronary arteries, it increases the heart’s blood supply.
If you experience chest discomfort, be sure and visit your doctor for a complete evaluation and, possibly, tests. If you have stable angina and start getting chest pain more easily and more often, see your doctor immediately as you may be experiencing early signs of unstable angina.
Unstable Angina
Unstable angina, sometimes referred to as acute coronary syndrome causes unexpected chest pain, doesn’t follow a pattern 6. It may occur more often and be more severe than stable angina. Unstable angina also can occur with or without physical exertion, and rest or medicine may not relieve the pain.
The most common cause is reduced blood flow to the heart muscle because the coronary arteries are narrowed by fatty buildups (atherosclerosis) which can rupture causing injury to the coronary blood vessel resulting in blood clotting which blocks the flow of blood to the heart muscle.
Unstable angina should be treated as an emergency. If you have new, worsening or persistent chest discomfort, you need to go to the emergency department. You could be having a heart attack which puts you at increased risk for severe cardiac arrhythmias or cardiac arrest, which could lead to sudden death.
- Unstable angina is very dangerous and requires emergency treatment. This type of angina is a sign that a heart attack may happen soon.
Causes of Unstable Angina: Blood clots that block an artery partially or totally are what causes unstable angina. Blood clots may form, partially dissolve, and later form again and angina can occur each time a clot blocks blood flow in an artery. Learn more about excessive blood clotting.
Symptoms of Unstable Angina – The pain or discomfort 6:
- Often occurs while you may be resting, sleeping, or with little physical exertion
- Comes as a surprise
- May last longer than stable angina
- Rest or medicine usually do not help relieve it
- May get worse over time
- Can lead to a heart attack
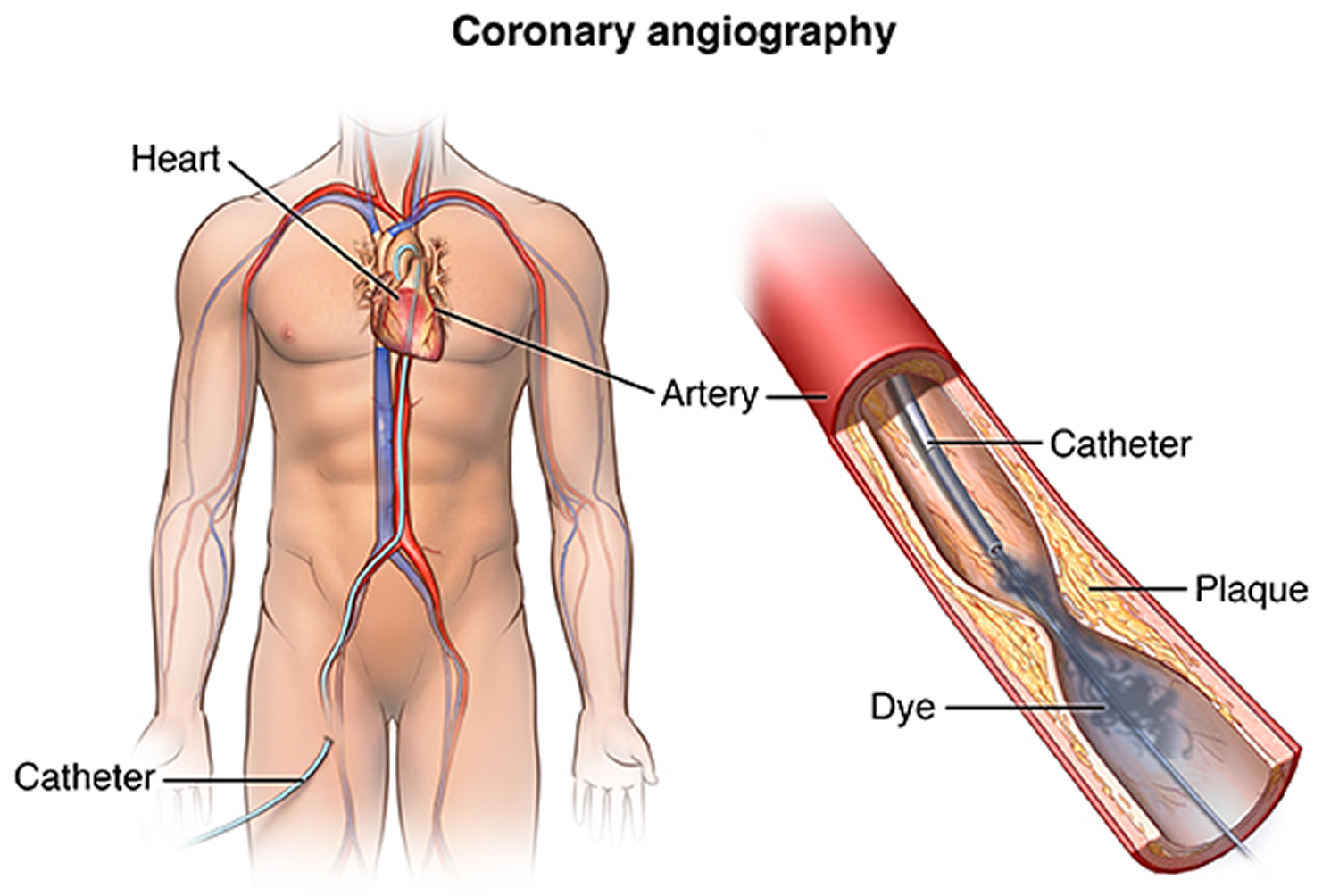
Treatment for Unstable Angina
First, your healthcare provider will need to find the blocked part or parts of the coronary arteries by performing a cardiac catheterization. In this procedure, a catheter is guided through an artery in the arm or leg and into the coronary arteries, then injected with a liquid dye through the catheter. High-speed X-ray movies record the course of the dye as it flows through the arteries, and doctors can identify blockages by tracing the flow. An evaluation of how well your heart is working also can be done during cardiac catheterization.
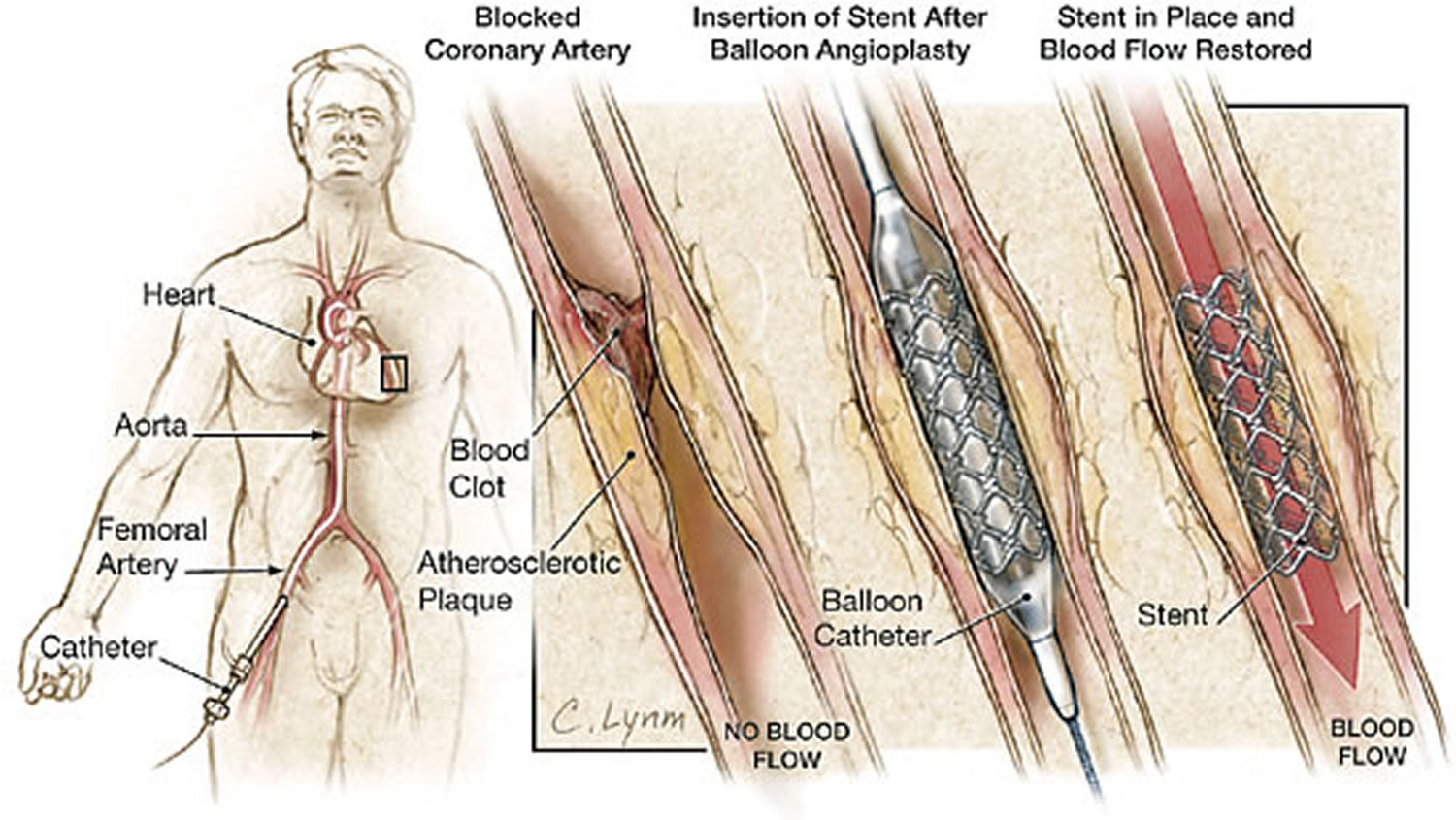
Figure 4. Cardiac Catheterization
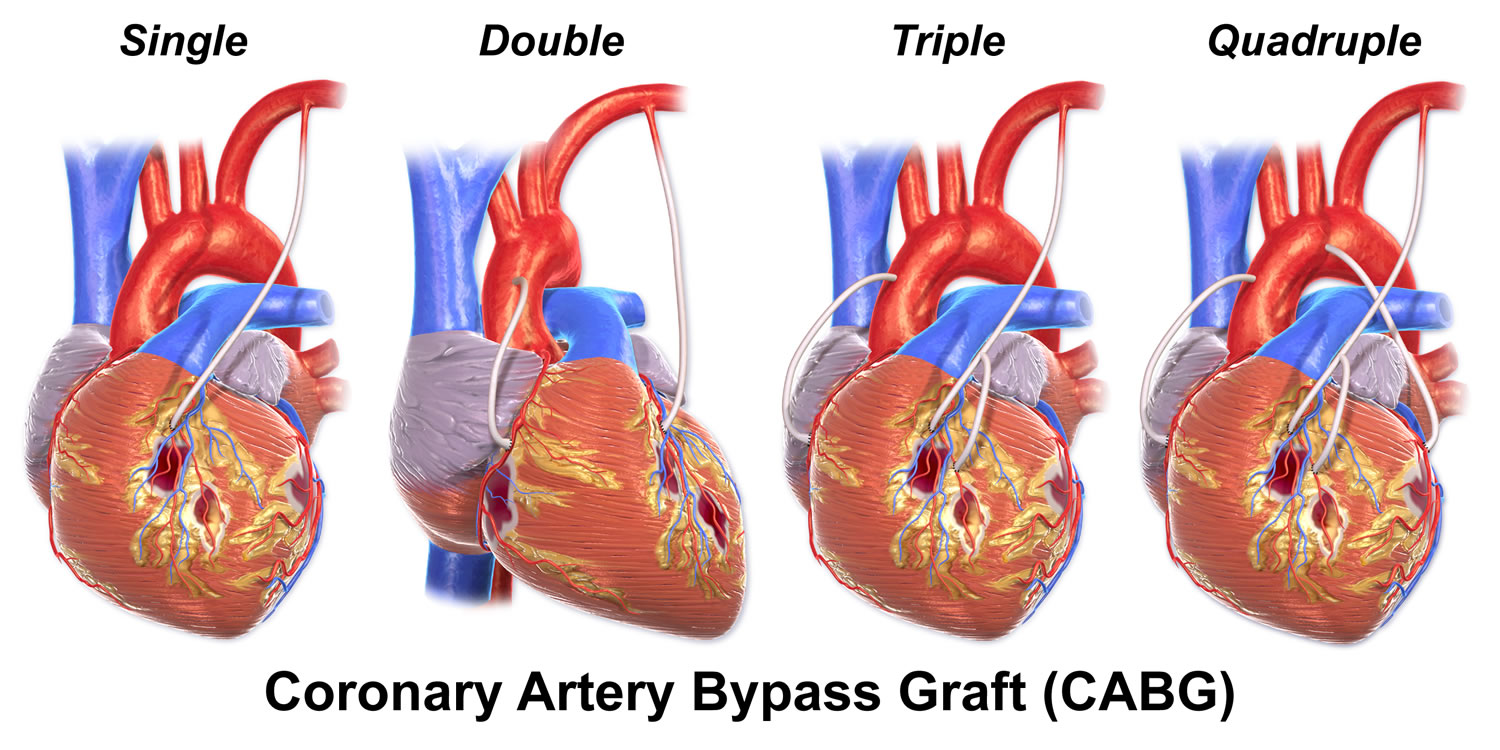
Next, based on the extent of the coronary artery blockage(s) your doctor will discuss with you the following treatment options:
- Percutaneous coronary intervention (heart stent surgery) may be required to open a blocked coronary artery. Briefly, this procedure involves undergoing cardiac catheterization followed by using a catheter with a small inflatable balloon at the tip. The balloon is inflated, squeezing open the fatty plaque deposit located on the inner lining of the coronary artery. Then the balloon is deflated and the catheter is withdrawn. This procedure is often followed by insertion of a stent to then keep the coronary artery vessel propped open to allow for improved blood flow to the heart muscle.
- Coronary artery bypass graft surgery may be indicated depending on the extent of coronary artery blockages and medical history. In this procedure, a blood vessel is used to route blood around the blocked part of the artery, forming a kind of detour.
Before any of these procedures, a doctor must find the blocked part or parts of the coronary arteries. He or she will guide a catheter through an artery in the arm or leg and into the coronary arteries, then inject a liquid dye through the catheter. High-speed X-ray movies record the course of the dye as it flows through the arteries, and doctors can identify blockages by tracing the flow. An evaluation of how the heart works also can be done during cardiac catheterization.
For more information, talk to your doctor.
Figure 5. Heart stent surgery (percutaneous coronary intervention)
Figure 6. Coronary artery bypass grafting
Variant (Prinzmetal’s) Angina
Variant angina or Prinzmetal’s angina is rare, representing about two out of 100 cases of angina, and usually occurs in younger patients than those who have other kinds of angina 7. A spasm in a coronary artery causes this type of angina. Variant angina almost always occurs while you’re at rest, and the pain can be severe. It usually happens between midnight and early morning. These attacks can be very painful. Medicine can relieve this type of angina.
Causes of Variant (Prinzmetal) Angina:
The pain from variant angina is caused by a spasm in the coronary arteries (which supply blood to the heart muscle).
The coronary arteries can spasm as a result of:
- Exposure to cold weather
- Stress
- Medicines that tighten or narrow blood vessels
- Smoking
- Cocaine use
Symptoms of Variant (Prinzmetal) Angina:
The pain or discomfort:
- Usually occurs while resting and during the night or early morning hours
- Are usually severe
- Can be relieved by taking medication
Treatment of Variant Angina (Prinzmetal’s Angina)
Medicines can help control the spasms. Drugs such as calcium antagonists and nitrates are the mainstays of treatment.
The spasms tend to come in cycles – appearing for a time, then going away. After six to 12 months of treatment, doctors may gradually reduce the medication.
Prinzmetal’s angina is a chronic condition that will need to be followed by your healthcare provider even though the prognosis is generally good.
Microvascular Angina
Microvascular angina or chest pain, can be more severe and last longer than other types of angina. Medicine may not relieve this type of angina.
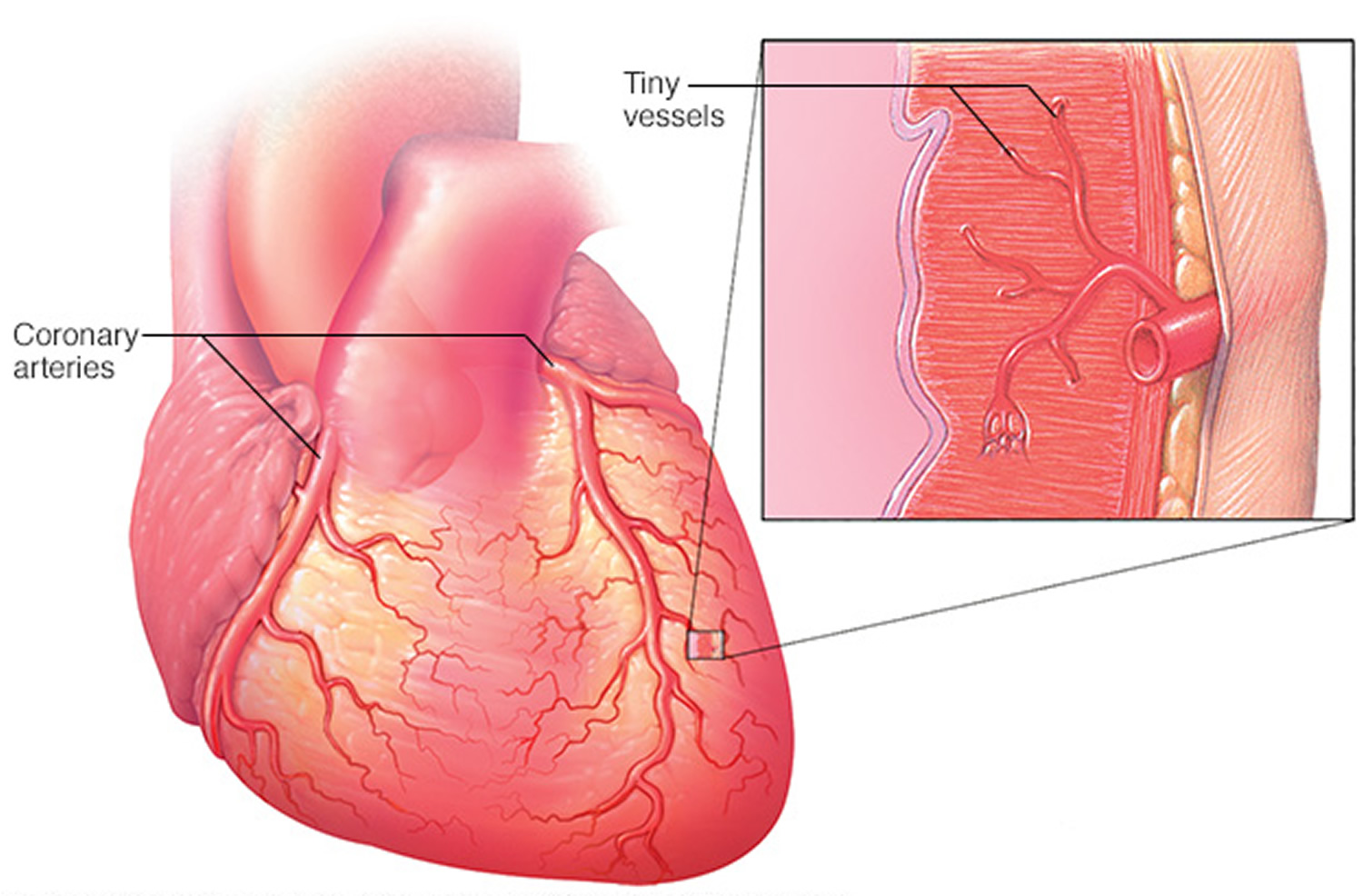
This type of angina may be a symptom of coronary microvascular disease. Coronary microvascular disease is heart disease that affects the heart’s smallest coronary artery blood vessels.
Causes of microvascular angina:
Spasms within the walls of these very small arterial blood vessels causes reduced blood flow to the heart muscle leading to a type of chest pain referred to as microvascular angina.
Symptoms of microvascular angina:
Angina that occurs in coronary microvascular disease may differ from the typical angina that occurs in heart disease in that the chest pain usually lasts longer than 10 minutes, and it can last longer than 30 minutes. If you have been diagnosed with microvascular disease, follow the directions from your healthcare provider regarding how to treat your symptoms and when to seek emergency assistance.
The pain or discomfort:
- May be more severe and last longer than other types of angina pain
- May occur with shortness of breath, sleep problems, fatigue, and lack of energy
- Often is first noticed during routine daily activities and times of mental stress
Figure 7. Microvascular coronary artery disease
Coronary Microvascular Disease
Coronary microvascular disease (sometimes called small artery disease or small vessel disease) is heart disease that affects the walls and inner lining of tiny coronary artery blood vessels that branch off from the larger coronary arteries 8. Coronary heart disease, also called coronary artery disease, involves plaque formation that can block blood flow. In coronary microvascular disease, the heart’s tiny coronary artery blood vessels may not have plaque, but damage to the inner walls of the blood vessels that can lead to spasms and decrease blood flow to the heart muscle. According to the National Heart, Lung, and Blood Institute’s Wise study (Women’s Ischemia Syndrome Evaluation), as many as 3 million U.S. women with coronary heart disease, cholesterol plaque may not build up into major blockages, but instead spreads evenly throughout the artery wall 9. As a result, diagnostic coronary angiography reveals that these women have “clear” arteries no blockages incorrectly indicating low risk. Despite this, many of these women have a high risk for heart attack, according to newly published research from the National Institutes of Health 10.
In women with this condition, called coronary microvascular syndrome, plaque accumulates in very small arteries of the heart, causing narrowing, reduced oxygen flow to the heart, and pain that can be similar to that of people with blocked arteries, but the plaque does not show up when physicians use standard tests. As a result, many women go undiagnosed. Research is ongoing to learn more about the role of hormones in heart disease and to find better ways to diagnose coronary microvascular disease.
Women more frequently develop coronary microvascular disease and it occurs particularly in younger women; however, men and women who have coronary microvascular disease often have diabetes, high blood pressureor a family history of cardiomyopathy.
Diagnosing coronary microvascular disease has been a challenge for doctors 8. Standard tests used to diagnose coronary heart disease are not designed to detect coronary microvascular disease, so more research is needed to find the best diagnostic tests and treatments for the disease.
Other Names for Coronary Microvascular Disease
- Cardiac syndrome X
- Nonobstructive coronary heart disease
What Causes Coronary Microvascular Disease ?
The same risk factors that cause atherosclerosis may cause coronary microvascular disease. Atherosclerosis is a disease in which plaque builds up inside the arteries.
Risk factors for atherosclerosis include:
- Unhealthy blood cholesterol levels
- High blood pressure
- Smoking
- Diabetes
- Overweight and obesity
- Inactivity
- Unhealthy diet
- Older age
- Family history of heart disease
Understand Your Risk for Coronary Microvascular Disease ?
Women may be at risk for coronary microvascular disease if they have lower than normal estrogen levels at any point in their adult lives. Low estrogen levels before menopause can raise younger women’s risk for coronary microvascular disease and can be caused by stress and also a functioning problem with the ovaries.
Women who have high blood pressure before menopause, especially high systolic blood pressure, are at increased risk for coronary microvascular disease. After menopause, women tend to have more of the traditional risk factors for atherosclerosis, which also puts them at higher risk for coronary microvascular disease.
Women who have heart disease are more likely to have a worse outcome, such as a heart attack, if they also have anemia because anemia is thought to slow the growth of cells needed to repair damaged blood vessels.
What Are the Signs and Symptoms of Coronary Microvascular Disease ?
Women with coronary microvascular disease often have chest pain called angina, also called microvascular angina usually lasting longer than 10 minutes, and it can last longer than 30 minutes.
Other signs and symptoms of coronary microvascular disease are:
- shortness of breath
- sleep problems
- fatigue
- lack of energy
People that experience coronary microvascular disease symptoms often first notice them during their routine daily activities and times of mental stress but less often during physical activity or exertion. This differs from heart disease, in which symptoms often first appear while a person is being physically active. If you have coronary microvascular disease, learn the warning signs of a heart attack and the warning signs of a heart attack in women.
Diagnosis of Coronary Microvascular Disease
Your healthcare provider will diagnose coronary microvascular disease based on your medical history, a physical exam, and test results. They will also check to see whether you have any risk factors for heart disease. For example, your doctor may measure your weight and height to check for overweight or obesity. He or she also may recommend tests for high cholesterol, metabolic syndrome, and diabetes.
Diagnostic Tests for Coronary Microvascular Disease
The risk factors for coronary microvascular disease and traditional heart disease often are the same. Thus, your doctor may recommend tests for heart disease, such as:
- Coronary angiography
- Stress test
- Magnetic Resonance Imaging (MRI)
Unfortunately, standard tests for coronary heart disease aren’t designed to detect coronary microvascular disease. These tests look for blockages in the large coronary arteries. Coronary microvascular disease affects the tiny coronary arteries. If test results show that you don’t have heart disease, your doctor might still diagnose you with coronary microvascular disease. This could happen if signs are present that not enough oxygen is reaching your heart’s tiny arteries.
Coronary microvascular disease symptoms often first occur during routine daily tasks. Because of this, your doctor may ask you to fill out a questionnaire called the Duke Activity Status Index (DASI). The will ask you how well you’re able to do daily activities, such as shopping, cooking, and going to work.
The Duke Activity Status Index (DASI) results will help your doctor decide which kind of stress test you should have. The results also give your doctor information about how well blood is flowing through your coronary arteries.
Duke Activity Status Index (DASI)
The Duke Activity Status Index is a self-administered questionnaire that measures a patient’s functional capacity 8. It can be used to get a rough estimate of a patient’s peak oxygen uptake.
- Can you take care of yourself (eating, dressing, bathing or using the toilet)?
- Can you walk indoors, such as around your house?
- Can you walk a block or two on level ground?
- Can you climb a flight of stairs or walk up a hill?
- Can you run a short distance?
- Can you do light work around the house, such as dusting or washing dishes?
- Can you do moderate work around the house, such as vacuuming, sweeping floors or carrying in groceries?
- Can you do heavy work around the house, such as scrubbing floors or lifting and moving heavy furniture?
- Can you do yard work, such as raking leaves, weeding or pushing a power mower?
- Can you have sexual relations?
- Can you participate in moderate recreational activities, such as golf, bowling, dancing, doubles tennis or throwing a baseball or football?
- Can you participate in strenuous sports, such as swimming, singles tennis, football, basketball or skiing?
Duke Activity Status Index (DASI) = sum of “Yes” replies ___________
VO2peak = (0.43 x DASI) + 9.6
VO2peak = ___________ ml/kg/min ÷ 3.5 ml/kg/min = __________ METS
———————————————————————————————————————————————————————————-
Your doctor also may recommend blood tests, including a test for anemia. Anemia is thought to slow the growth of cells needed to repair damaged blood vessels.
Research is ongoing for better ways to detect and diagnose coronary microvascular disease. Currently, researchers have not agreed on the best way to diagnose the disease.
Treatment of Coronary Microvascular Disease
Relieving pain is one of the main goals of treating coronary microvascular disease. Treatments also are used to control risk factors and other symptoms.
Treatments may include medicines such as:
- Cholesterol medication to improve cholesterol levels
- Antithrombotic medications to lower blood pressure and decrease the heart’s workload
- Medication to help prevent blood clots or control inflammation
- Nitroglycerin to relax blood vessels, improve blood flow to the heart muscle, and treat chest pain
Prevention of Coronary Microvascular Disease
No specific studies have been done on how to prevent coronary microvascular disease. Researchers don’t yet known how or in what way preventing coronary microvascular disease differs from preventing heart disease. Lifestyle changes and ongoing care can help you lower your risk for heart disease.
- Lifestyle Changes – If lifestyle changes aren’t enough, your doctor may prescribe medicines to control your risk factors. Take all of your medicines as your doctor advises.
- Know your body mass index (BMI)
- Know your family history of heart disease
Angina in Women
Heart disease in men is more often due to blockages in their coronary arteries, referred to as obstructive coronary artery disease (coronary heart disease). Women more frequently develop heart disease within the very small arteries that branch out from the coronary arteries. This is referred to as microvascular disease and occurs particularly in younger women. Up to 50 percent of women with anginal symptoms who undergo cardiac catheterization don’t have the obstructive type of coronary artery disease (coronary heart disease).
Cardiovascular disease is the No. 1 killer of women in the United States, affecting one out of every three in the United States. Nearly half of African-American women have cardiovascular disease.
Recognizing the signs and seeking treatment is the first step. Understanding your risk factors, such as a family history, is also important to staying in tune with changes in your health.
What Is Pulmonary Embolism ?
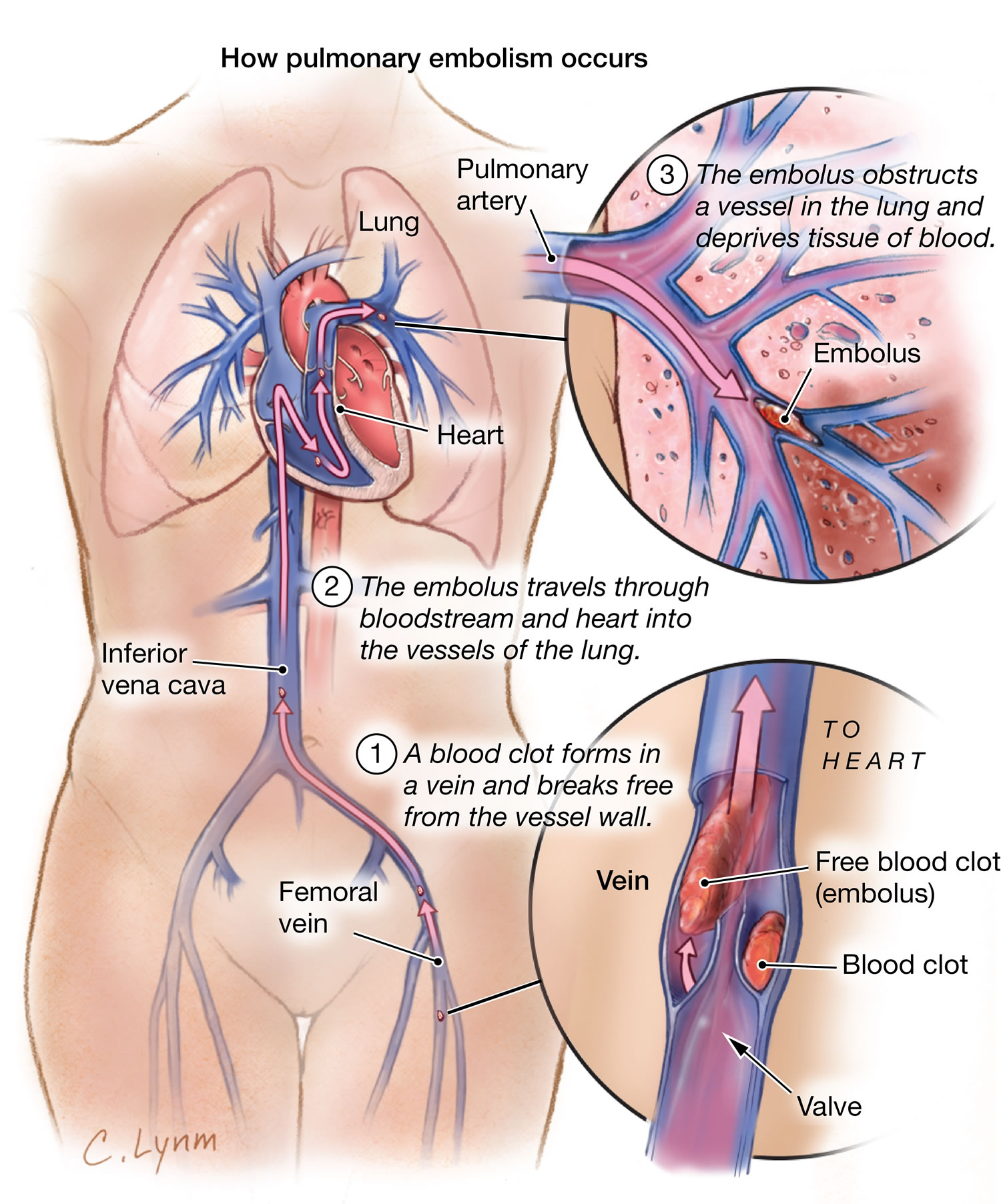
Pulmonary embolism is a sudden blockage in a lung artery. The blockage usually is caused by a blood clot that travels to the lung from a vein in the leg 11.
A clot that forms in one part of the body and travels in the bloodstream to another part of the body is called an embolus.
Pulmonary embolism most often is a complication of a condition called deep vein thrombosis (DVT). In deep vein thrombosis (DVT), blood clots form in the deep veins of the body—most often in the legs. These clots can break free, travel through the bloodstream to the lungs, and block an artery.
Deep vein clots are not like clots in veins close to the skin’s surface. Those clots remain in place and do not cause pulmonary embolism.
Blood clots can form in the deep veins of the legs if blood flow is restricted and slows down. This can happen if you don’t move around for long periods, such as:
- After some types of surgery
- During a long trip in a car or airplane
- If you must stay in bed for an extended time
Blood clots are more likely to develop in veins damaged from surgery or injured in other ways. Rarely, an air bubble, part of a tumor, or other tissue travels to the lungs and causes pulmonary embolism. Also, if a large bone in the body (such as the thigh bone) breaks, fat from the bone marrow can travel through the blood. If the fat reaches the lungs, it can cause pulmonary embolism.
Pulmonary embolism is a serious condition that can:
- Damage part of your lung because of a lack of blood flow to your lung tissue. This damage may lead to pulmonary hypertension (increased pressure in the pulmonary arteries).
- Cause low oxygen levels in your blood.
- Damage other organs in your body because of a lack of oxygen.
If a blood clot is large, or if there are many clots, pulmonary embolism can cause death.
Figure 8. Pulmonary embolism
Outlook for Pulmonary embolism
The exact number of people affected by deep vein thrombosis and pulmonary embolism isn’t known. Estimates suggest these conditions affect 300,000 to 600,000 people in the United States each year.
If left untreated, about 30 percent of patients who have pulmonary embolism will die 11. Most of those who die do so within the first few hours of the event.
The good news is that a prompt diagnosis and proper treatment can save lives and help prevent the complications of pulmonary embolism.
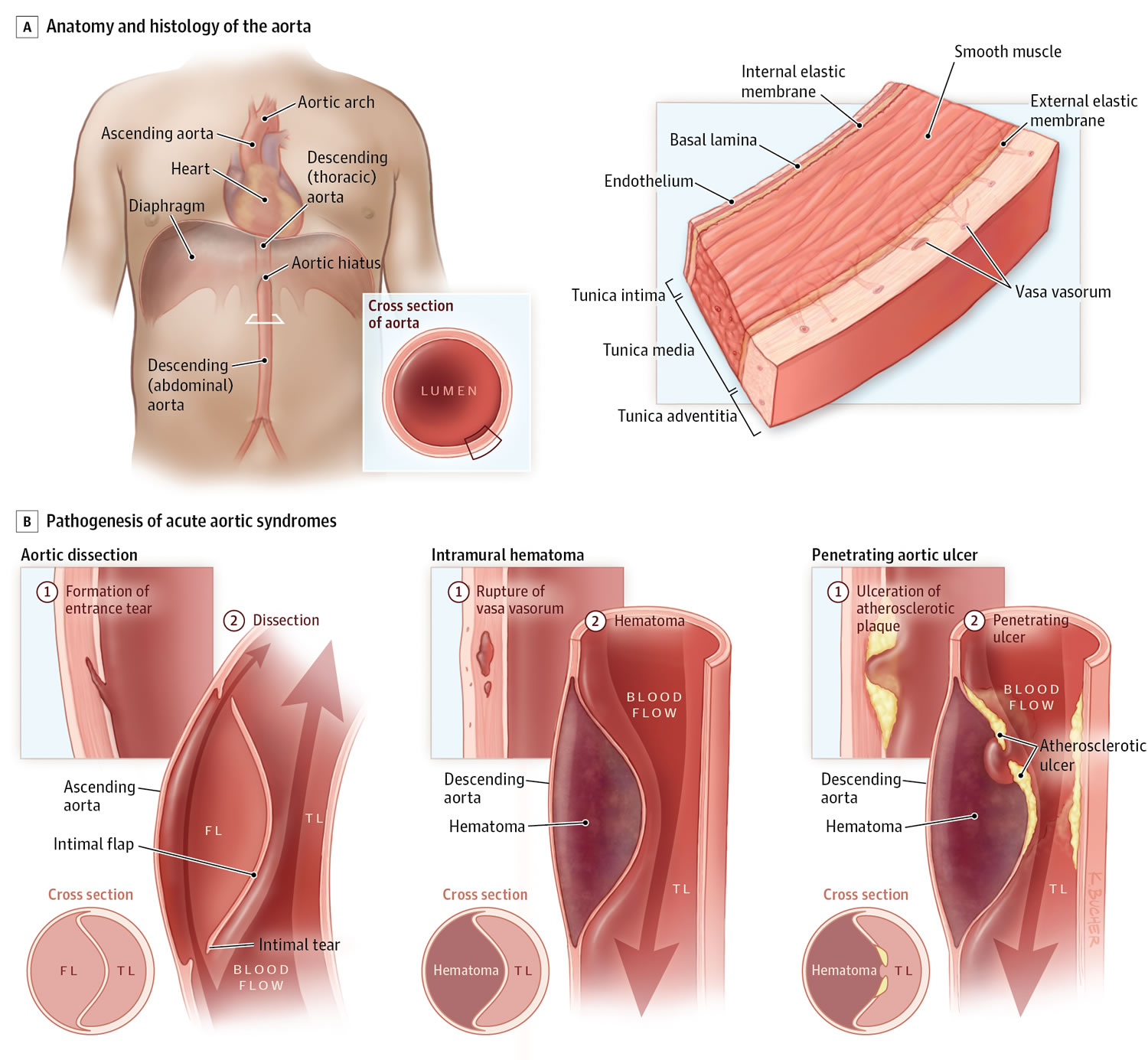
What is Aortic Dissection
Aortic dissection is a serious condition in which there is a tear in the wall of the major artery carrying blood out of the heart (aorta). As the tear extends along the wall of the aorta, blood can flow in between the layers of the blood vessel wall (dissection). This can lead to aortic rupture or decreased blood flow (ischemia) to organs.
Aortic dissection occurs in about 2 out of every 10,000 people. It can affect anyone, but is most often seen in men ages 40 to 70.
Causes of Aortic dissection
When it leaves the heart, the aorta first moves up through the chest towards the head (the ascending aorta). It then bends or arches, and finally moves down through the chest and abdomen (the descending aorta).
Aortic dissection most often happens because of a tear or damage to the inner wall of the aorta. This very often occurs in the chest (thoracic) part of the artery, but it may also occur in the abdominal aorta.
When a tear occurs, it creates 2 channels:
- One in which blood continues to travel
- Another where blood stays still
If the channel with non-traveling blood gets bigger, it can push on other branches of the aorta. This can narrow the other branches and reduce blood flow through them.
An aortic dissection may also cause abnormal widening or ballooning of the aorta (aneurysm).
The exact cause is unknown, but more common risks include:
- Aging
- Atherosclerosis
- Blunt trauma to the chest, such as hitting the steering wheel of a car during an accident
- High blood pressure
Other risk factors and conditions linked to aortic dissection include:
- Bicuspid aortic valve
- Coarctation (narrowing) of the aorta
- Connective tissue disorders (such as Marfan syndrome and Ehlers-Danlos syndrome) and rare genetic disorders
- Heart surgery or procedures
- Pregnancy
- Swelling of the blood vessels due to conditions such as arteritis and syphilis.
Figure 9. Aortic dissection
Symptoms of Aortic Dissection
In most cases, the symptoms begin suddenly, and include severe chest pain. The pain may feel like a heart attack.
- Pain can be described as sharp, stabbing, tearing, or ripping.
- It is felt below the chest bone, and then moves under the shoulder blades or to the back.
- Pain can move to the shoulder, neck, arm, jaw, abdomen, or hips.
- The pain changes position, often moving to the arms and legs as the aortic dissection gets worse.
Symptoms are caused by a decrease of blood flowing to the rest of the body, and can include:
- Anxiety and a feeling of doom
- Fainting or dizziness
- Heavy sweating (clammy skin)
- Nausea and vomiting
- Pale skin (pallor)
- Rapid, weak pulse
- Shortness of breath and trouble breathing when lying flat (orthopnea)
Other symptoms may include:
- Pain in the abdomen
- Stroke symptoms
- Swallowing difficulties from pressure on the esophagus
Exams and Tests for Aortic Dissection
The health care provider will take your family history and listen to your heart, lungs, and abdomen with a stethoscope. The exam may find:
- A “blowing” murmur over the aorta, heart murmur, or other abnormal sound
- A difference in blood pressure between the right and left arms, or between the arms and legs
- Low blood pressure
- Signs resembling a heart attack
- Signs of shock, but with normal blood pressure
Aortic dissection or aortic aneurysm may be seen on:
- Aortic angiography
- Chest x-ray
- Chest MRI
- CT scan of chest with dye
- Doppler ultrasonography (occasionally performed)
- Echocardiogram
- Transesophageal echocardiogram (TEE)
Blood work to rule out a heart attack is needed.
Treatment of Aortic Dissection
Aortic dissection is a life-threatening condition and needs to be treated right away.
- Dissections that occur in the part of the aorta that is leaving the heart (ascending) are treated with surgery.
- Dissections that occur in other parts of the aorta (descending) may be managed with surgery or medicines.
Two techniques may be used for surgery:
- Standard, open surgery. This requires a surgical incision that is made in the chest or abdomen.
- Endovascular aortic repair. This surgery is done without any major surgical incisions.
Drugs that lower blood pressure may be prescribed. These drugs may be given through a vein (intravenously). Beta-blockers are the first drugs of choice. Strong pain relievers are very often needed.
If the aortic valve is damaged, valve replacement is needed. If the heart arteries are involved, a coronary bypass is also performed.
Outlook (Prognosis) for Aortic Dissection
Aortic dissection is life threatening. The condition can be managed with surgery if it is done before the aorta ruptures. Less than one half of people with a ruptured aorta survive.
Those who survive will need lifelong, aggressive treatment of high blood pressure. They will need to be followed up with CT scans every few months to monitor the aorta.
Possible Complications of Aortic Dissection
Aortic dissection may decrease or stop the blood flow to many different parts of the body. This may result in short-term or long-term problems, or damage to the:
- Brain
- Heart
- Intestines or bowels
- Kidneys
- Legs
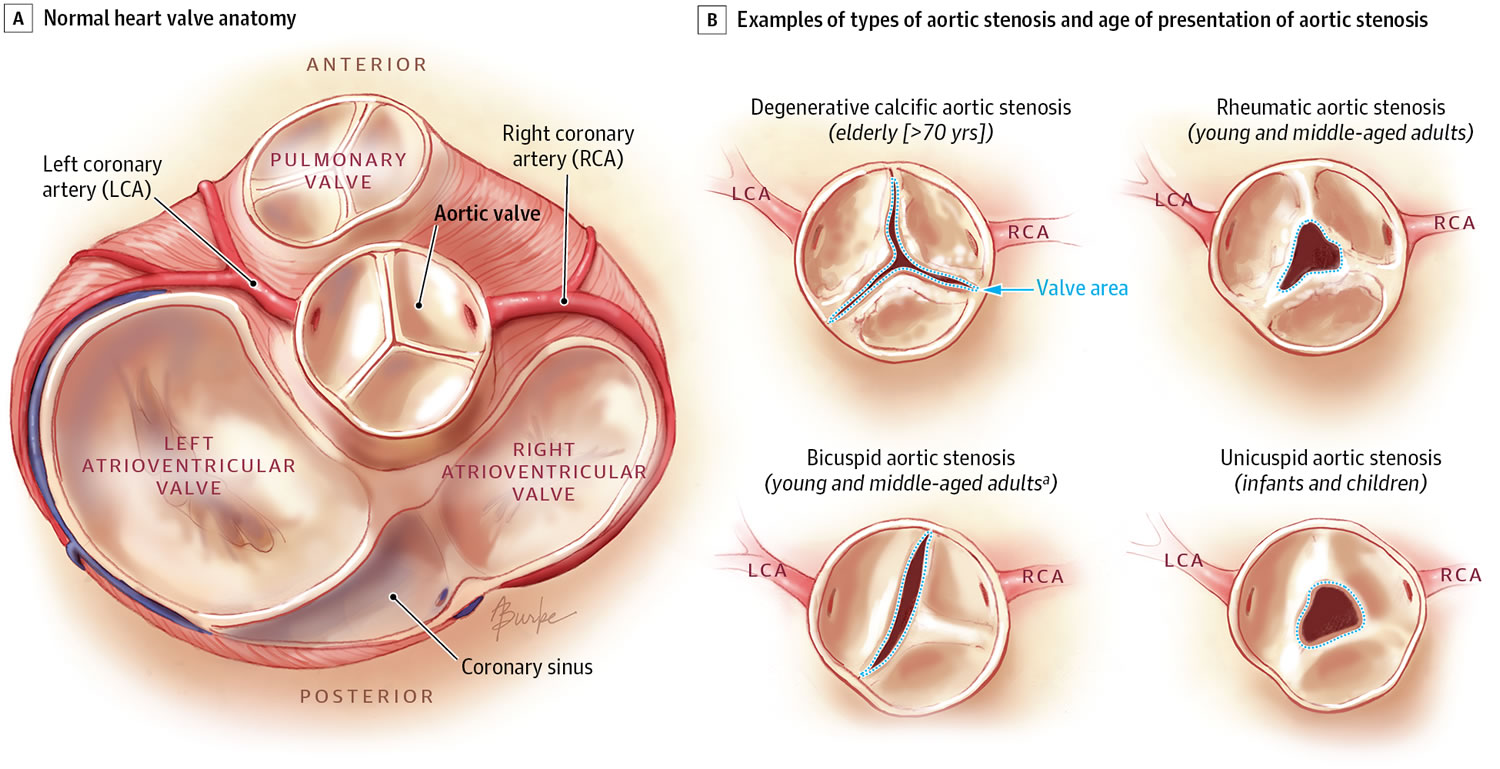
What is Aortic Valve Stenosis
The aorta is the main artery that carries blood out of the heart to the rest of the body. Blood flows out of the heart and into the aorta through the aortic valve. A normal aortic valve has three leaflets or cusps (tricuspid). About 1 percent of the population is born with a valve that only has two leaflets (bicuspid) and narrows or leaks over time. In aortic stenosis, the aortic valve does not open fully. This decreases blood flow from the heart 12.
Some infants are born with severely narrowed aortic valves need early treatment. However, most bicuspid aortic valves work normally for a long time — sometimes a lifetime. In other patients, the valve can become thick and narrowed/obstructed (stenotic) or curled at the edges and leaky (regurgitant or insufficient). When the valve is obstructed the left ventricle pumps at a higher pressure than normal to push the blood through the narrow opening. In response, the heart muscle gets thicker. This can lead to chest pain. When the valve primarily leaks, the ventricle has to pump more blood and the ventricle enlarges.
As the pressure continues to rise, blood may back up into the lungs. Severe aortic stenosis can limit the amount of blood that reaches the brain and the rest of the body.
With mild obstruction, patients usually have no symptoms. The problem is detected by the presence of a clicking sound in the heart and a murmur. When the valve opening narrows to about one-fourth its original size, symptoms are common. The most common symptom of an obstructed or leaky aortic valve is shortness of breath with exertion. This usually develops gradually over time, and some patients will just feel “out of shape.” Chest pain, lightheadedness or fainting may also occur. Recurrent fevers may indicate the valve is infected.
Figure 10. Aortic Valve Stenosis
Causes of Aortic Stenosis
Aortic stenosis may be present from birth (congenital), but most often it develops later in life. Children with aortic stenosis may have other conditions present from birth.
Aortic stenosis mainly occurs due to the buildup of calcium deposits that narrow the valve. This is called calcific aortic stenosis. The problem mostly affects older people.
Calcium buildup of the valve happens sooner in people who are born with abnormal aortic or bicuspid valves. In rare cases, calcium buildup can develop more quickly when a person has received chest radiation (such as for cancer treatment).
Another cause is rheumatic fever. This condition can develop after strep throat or scarlet fever. Valve problems do not develop for 5 to 10 years or longer after rheumatic fever occurs. Rheumatic fever is becoming rarer in the United States.
Aortic stenosis occurs in about 2% of people over 65 years of age. It occurs more often in men than in women.
Symptoms of Aortic Stenosis
Most people with aortic stenosis do not develop symptoms until the disease is advanced. The diagnosis may have been made when the health care provider heard a heart murmur and performed tests.
Symptoms of aortic stenosis include:
- Chest discomfort: The chest pain may get worse with activity and reach into the arm, neck, or jaw. The chest may also feel tight or squeezed.
- Cough, possibly bloody.
- Breathing problems when exercising.
- Becoming easily tired.
- Feeling the heartbeat (palpitations).
- Fainting, weakness, or dizziness with activity.
In infants and children, symptoms include:
- Becoming easily tired with exertion (in mild cases)
- Failure to gain weight
- Poor feeding
- Serious breathing problems that develop within days or weeks of birth (in severe cases)
Children with mild or moderate aortic stenosis may get worse as they get older. They are also at risk for a heart infection called bacterial endocarditis.
Exams and Tests forAortic Stenosis
A heart murmur, click, or other abnormal sound is almost always heard through a stethoscope. The provider may be able to feel a vibration or movement when placing a hand over the heart. There may be a faint pulse or changes in the quality of the pulse in the neck.
Blood pressure may be low.
Aortic stenosis is most often detected and then followed using a test called a transthoracic echocardiogram (TTE).
The following tests may also be performed:
- ECG
- Exercise stress testing
- Left cardiac catheterization
- MRI of the heart
- Transesophageal echocardiogram (TEE)
Treatment of Aortic Stenosis
Regular checkups by a provider may be all that is needed if your symptoms are not severe. The provider should ask about your health history, do a physical exam, and perform an echocardiogram.
People with severe aortic stenosis may be told not to play competitive sports, even if they have no symptoms. If symptoms do occur, strenuous activity must often be limited.
Medicines are used to treat symptoms of heart failure or abnormal heart rhythms (most commonly atrial fibrillation). These include diuretics (water pills), nitrates, and beta-blockers. High blood pressure should also be treated. If aortic stenosis is severe, this treatment must be done carefully so blood pressure does not drop too far.
In the past, most people with heart valve problems were given antibiotics before dental work or a procedure such as colonoscopy. The antibiotics were given to prevent an infection of the damaged heart. However, antibiotics are now used much less often before dental work and other procedures. Check with your health care provider to find out whether you need antibiotics.
People with this and other heart conditions should stop smoking and be tested for high cholesterol.
Surgery to repair or replace the valve is often done for adults or children who develop symptoms. Even if symptoms are not very bad, the doctor may recommend surgery based on test results.
A less invasive procedure called balloon valvuloplasty may be done instead of or before surgery.
A balloon is placed into an artery in the groin, threaded to the heart, placed across the valve, and inflated. However, narrowing often occurs again after this procedure.
A newer procedure done at the same time as valvuloplasty can implant an artificial valve. This procedure is most often done in patients who cannot have surgery, but it is becoming more common.
Some children may need aortic valve repair or replacement. Children with mild aortic stenosis may be able to take part in most activities.
Outlook (Prognosis) of Aortic Stenosis
The outcome varies. The disorder may be mild and not produce symptoms. Over time, the aortic valve may become narrower. This may result in more severe heart problems such as:
- Atrial fibrillation and atrial flutter
- Blood clots to the brain (stroke), intestines, kidneys, or other areas
- Fainting spells (syncope)
- Heart failure
- High blood pressure in the arteries of the lungs (pulmonary hypertension)
The results of aortic valve replacement are often excellent. To get the best treatment, go to a center that regularly performs this type of surgery.
Ongoing Care for Aortic Stenosis
Medical
Everyone with an aortic valve defect needs routine follow-up, whether before or after surgery. Progression occurs over time. Even with the best surgery, the patient is never “cured.” The severity of your valve problem will dictate how often you’ll need to visit the doctor and how often echocardiograms are needed. Medicines might be useful to lower blood pressure or maintain the health of the left ventricle. You should also consult a cardiologist experienced in caring for adults with congenital heart disease if you are undergoing any type of non-heart surgery or invasive procedure.
Activity Restrictions
If you have a severely obstructed valve, vigorous exercise is not a good idea (for more information see the Physical Activity and Exercise section.) Your cardiologist may tell you to limit your activity if this is the case. Ask your cardiologist about your exercise limits.
Endocarditis Prevention
People with even mildly abnormal aortic valves are at risk for bacterial endocarditis. That’s why it’s important for you to keep your mouth clean and healthy with regular dental check ups. Getting antibiotics before dental procedures isn’t proven to be beneficial and so isn’t universally recommended any more. But if you have a prosthetic valve, you’ll need to take antibiotics before dental work. See the section on Endocarditis for more information.
Problems You May Have
Most patients feel well. Aortic stenosis (obstruction) and insufficiency (leak) usually cause symptoms only when these defects are severe. Symptoms include shortness of breath, exercise intolerance, dizziness, chest pain or occasionally abnormal heart rhythms. Patients may also develop an enlarged aorta over time, which may eventually require surgery. There are usually no symptoms associated with this, which can only be detected with imaging.
Pregnancy
The risk from pregnancy depends on how severely the valve is obstructed or how much it’s leaking.
If you have mild or moderate stenosis and your left heart muscle (ventricle) is functioning normally, you can have a safe pregnancy, but you need medical supervision throughout the pregnancy. Sometimes balloon valvuloplasty can be done to relieve symptoms if they occur during pregnancy but only when symptoms can’t be controlled by medication and bed rest.
If your stenosis is severe and you have symptoms, avoid conception until you’ve had your heart valve repaired or replaced. If you’re considering pregnancy and you have aortic valve stenosis, you should meet with a multidisciplinary medical team that can give you more information about the risk of pregnancy to you and your baby.
Pregnancy in aortic regurgitation is better tolerated, but if the regurgitation has weakened the heart muscle and signs of heart failure are present before pregnancy, the risk posed by pregnancy is higher.
In patients who have had their heart valve replaced with a metal (mechanical) heart valve, they may be taking warfarin (Coumadin) which can cause risk to the fetus and alternative means of blood thinning may be required. In aortic insufficiency, women may be taking medicines such as ACE inhibitors such as lisinopril (Zestril) or enalapril (Vasotec). These drugs are dangerous to the developing fetus (see the section on Pregnancy) and need to be changed before conception.
It’s best to talk with your doctor before you plan to become pregnant.
Will you need more surgery ?
If you already had an operation on your aortic valve, chances are high that you may need another. This may be to replace a valve or an enlarging aorta. No surgical fix is ever perfect, so regular follow-up with a doctor who is informed about this particular problem is recommended.
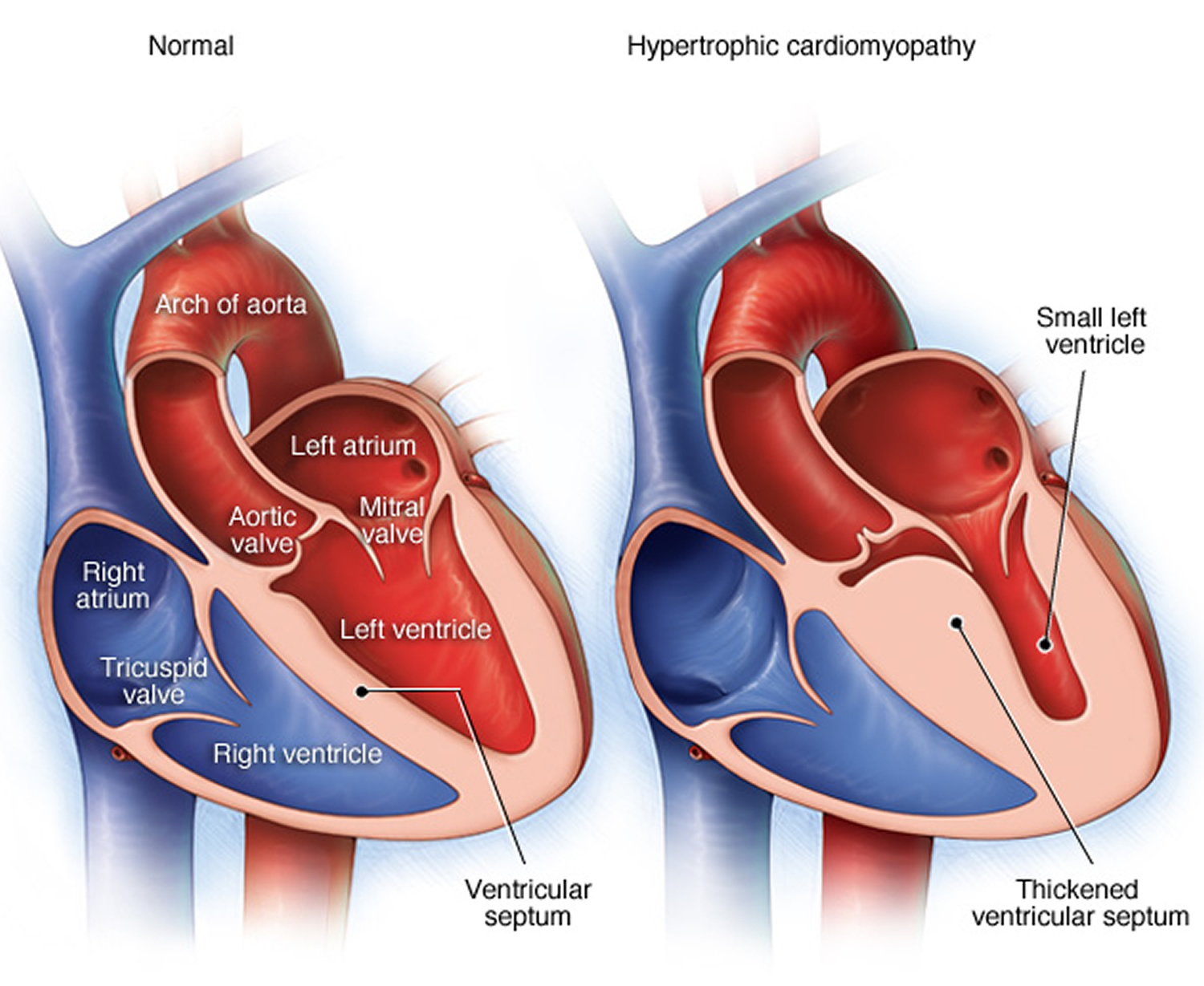
What is Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy is a condition in which the heart muscle becomes thick 13. Often, only 1 part of the heart is thicker than the other parts.
The thickening can make it harder for blood to leave the heart, forcing the heart to work harder to pump blood. It also can make it harder for the heart to relax and fill with blood.
Figure 11. Hypertrophic cardiomyopathy
Causes of Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy is most often passed down through families (inherited). It is thought to result from defects in the genes that control heart muscle growth.
Younger people are likely to have a more severe form of hypertrophic cardiomyopathy. However, the condition is seen in people of all ages.
Symptoms of Hypertrophic cardiomyopathy
Some people with the condition may have no symptoms. They may first find out they have the problem during a routine medical exam.
In many young adults, the first symptom of hypertrophic cardiomyopathy is sudden collapse and possible death. This can be caused by highly abnormal heart rhythms (arrhythmias). It may also be due to a blockage that prevents the outflow of blood from the heart to the rest of the body.
Common symptoms include:
- Chest pain
- Dizziness
- Fainting, especially during exercise
- Fatigue
- Lightheadedness, especially with or after activity or exercise
- Sensation of feeling the heart beat fast or irregularly (palpitations)
- Shortness of breath with activity or after lying down (or being asleep for a while)
Exams and Tests for Hypertrophic cardiomyopathy
The health care provider will perform a physical exam and listen to the heart and lungs with a stethoscope. Signs may include:
- Abnormal heart sounds or a heart murmur. These sounds may change with different body positions.
- High blood pressure.
- The pulse in your arms and neck will also be checked. The provider may feel an abnormal heartbeat in the chest.
Tests used to diagnose heart muscle thickness, problems with blood flow, or leaky heart valves (mitral valve regurgitation) may include:
- Echocardiography
- ECG
- 24-hour Holter monitor (heart rhythm monitor)
- Cardiac catheterization
- Chest x-ray
- MRI of the heart
- Transesophageal echocardiogram (TEE)
Blood tests may be done to rule out other diseases.
Close family members of people who have been diagnosed with hypertrophic cardiomyopathy may be screened for the condition.
Treatment for Hypertrophic cardiomyopathy
Always follow your provider’s advice about exercise if you have hypertrophic cardiomyopathy. You may be told to avoid strenuous exercise. Also, see your provider for regularly scheduled checkups.
If you have symptoms, you may need medicines such as beta-blockers and calcium channel blockers to help the heart contract and relax correctly. These drugs may relieve chest pain or shortness of breath when exercising.
People with arrhythmias may need treatment, such as:
- Medicines to treat the abnormal rhythm.
- Blood thinners to reduce the risk of blood clots (if the arrhythmia is due to atrial fibrillation).
- A permanent pacemaker to control the heartbeat.
- An implanted defibrillator that recognizes life-threatening heart rhythms and sends an electrical pulse to stop them. Sometimes a defibrillator is placed, even if the patient has not had an arrhythmia but is at high risk for a deadly arrhythmia (for example, if the heart muscle is very sick or the patient has a relative who has died suddenly).
When blood flow out of the heart is severely blocked, symptoms can become severe. An operation called surgical myectomy may be done. In some cases, people may be given an injection of alcohol into the arteries that feed the thickened part of the heart (alcohol septal ablation). People who have this procedure often show much improvement.
You may need surgery to repair the heart’s mitral valve if it is leaking.
Outlook (Prognosis) for Hypertrophic cardiomyopathy
Some people with hypertrophic cardiomyopathy may not have symptoms and will have normal lifespan. Others may get worse slowly or quickly. In some cases, the condition may develop into dilated cardiomyopathy.
People with hypertrophic cardiomyopathy are at higher risk for sudden death than people without the condition. Sudden death can occur at a young age.
There are different types of hypertrophic cardiomyopathy, which have different prognoses. The outlook may be better when the disease occurs in older people or when there is a particular pattern of thickness in the heart muscle.
- Hypertrophic cardiomyopathy is a well-known cause of sudden death in athletes. Almost half of deaths due to this condition happen during or just after some type of physical activity.
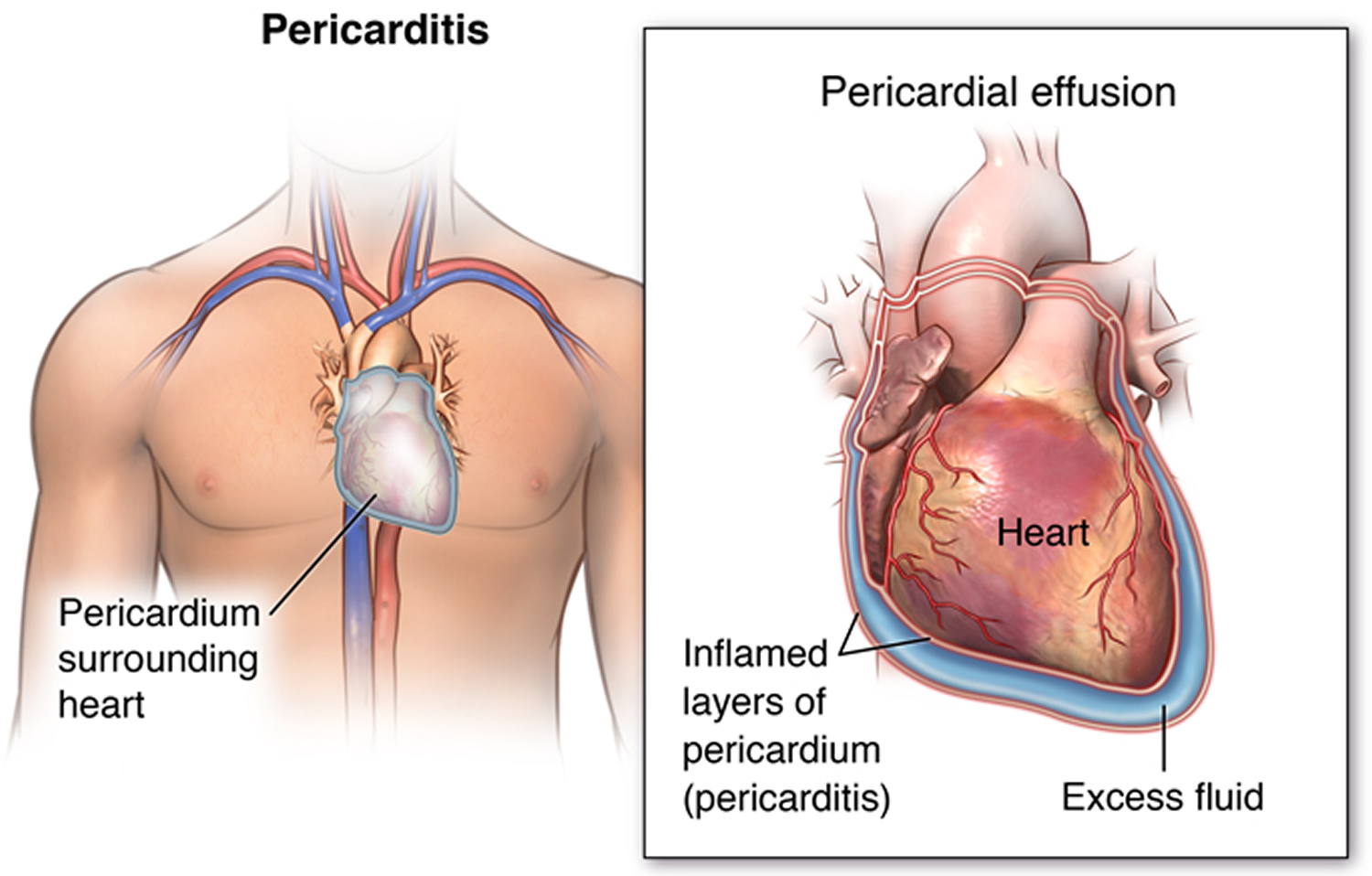
What is Pericarditis
Pericarditis is a condition in which the sac-like covering around the heart (pericardium) becomes inflamed 14.
Causes of Pericarditis
The cause of pericarditis is unknown or unproven in many cases. It mostly affects men ages 20 to 50 years.
Pericarditis is often the result of an infection such as:
- Viral infections that cause a chest cold or pneumonia
- Infections with bacteria (less common)
- Some fungal infections (rare)
The condition may be seen with diseases such as:
- Cancer (including leukemia)
- Disorders in which the immune system attacks healthy body tissue by mistake
- HIV infection and AIDS
- Underactive thyroid gland
- Kidney failure
- Rheumatic fever
- Tuberculosis (TB)
Other causes include:
- Heart attack
- Heart surgery or trauma to the chest, esophagus, or heart
- Certain medicines, such as procainamide, hydralazine, phenytoin, isoniazid, and some drugs used to treat cancer or suppress the immune system
- Swelling or inflammation of the heart muscle
- Radiation therapy to the chest.
Figure 12. Pericarditis
Symptoms of Pericarditis
Chest pain is almost always present. The pain:
- May be felt in the neck, shoulder, back, or abdomen
- Often increases with deep breathing and lying flat, and may increase with coughing and swallowing
- Can feel sharp and stabbing
- Is often relieved by sitting up and leaning or bending forward
You may have fever, chills, or sweating if the condition is caused by an infection.
Other symptoms may include:
- Ankle, feet, and leg swelling
- Anxiety
- Breathing difficulty when lying down
- Dry cough
- Fatigue
Exams and Tests for Pericarditis
When listening to the heart with a stethoscope, the health care provider can hear a sound called a pericardial rub. The heart sounds may be muffled or distant. There may be other signs of excess fluid in the pericardium (pericardial effusion).
If the disorder is severe, there may be:
- Crackles in the lungs
- Decreased breath sounds
- Other signs of fluid in the space around the lungs
The following imaging tests may be done to check the heart and the tissue layer around it (pericardium):
- Chest MRI scan
- Chest x-ray
- Echocardiogram
- Electrocardiogram
- Heart MRI or heart CT scan
- Radionuclide scanning
To look for heart muscle damage, the provider may order a troponin I test. Other laboratory tests may include:
- Antinuclear antibody (ANA)
- Blood culture
- CBC
- C-reactive protein
- Erythrocyte sedimentation rate (ESR)
- HIV test
- Rheumatoid factor
- Tuberculin skin test
Treatment for Pericarditis
The cause of pericarditis should be identified, if possible.
High doses of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen are often given with a medicine called colchicine. These medicines will decrease your pain and reduce the swelling or inflammation in the sac around your heart.
If the cause of pericarditis is an infection:
- Antibiotics will be used for bacterial infections
- Antifungal medicines will be used for fungal pericarditis
Other medicines that may be used are:
- Corticosteroids such as prednisone (in some people)
- “Water pills” (diuretics) to remove excess fluid
If the buildup of fluid makes the heart function poorly, treatment may include:
- Draining the fluid from the sac. This procedure, called pericardiocentesis, may be done using an echocardiography-guided needle.
- Cutting a small hole (window) in the pericardium (subxiphoid pericardiotomy) to allow the infected fluid to drain into the abdominal cavity
Surgery called pericardiectomy may be needed if the pericarditis is long-lasting, comes back after treatment, or causes scarring or tightening of the tissue around the heart. The operation involves cutting or removing part of the pericardium.
Outlook (Prognosis) for Pericarditis
Pericarditis can range from mild illness that gets better on its own, to a life-threatening condition. Fluid buildup around the heart and poor heart function can complicate the disorder.
The outcome is good if pericarditis is treated right away. Most people recover in 2 weeks to 3 months. However, pericarditis may come back. This is called recurrent, or chronic, if symptoms or episodes continue.
Scarring and thickening of the sac-like covering and the heart muscle may occur when the problem is severe. This is called constrictive pericarditis. It can cause long-term problems similar to those of heart failure.
What is Panic Attack
Panic disorder is a type of anxiety disorder in which you have repeated attacks of intense fear that something bad will happen 15.
A panic attack is a sudden episode of intense fear that triggers severe physical reactions when there is no real danger or apparent cause 16. Panic attacks can be very frightening. When panic attacks occur, you might think you’re losing control, having a heart attack or even dying.
Many people have just one or two panic attacks in their lifetimes, and the problem goes away, perhaps when a stressful situation ends. But if you’ve had recurrent, unexpected panic attacks and spent long periods in constant fear of another attack, you may have a condition called panic disorder.
Although panic attacks themselves aren’t life-threatening, they can be frightening and significantly affect your quality of life. But treatment can be very effective.
Panic attacks typically begin suddenly, without warning. They can strike at any time — when you’re driving a car, at the mall, sound asleep or in the middle of a business meeting. You may have occasional panic attacks or they may occur frequently.

Causes of Panic Disorder
The cause is unknown. Genes may play a role. Other family members may have the disorder. But panic disorder often occurs when there is no family history.
Panic disorder is twice as common in women as it is in men. Symptoms often begin before age 25, but may occur in the mid-30s. Children can also have panic disorder, but it is often not diagnosed until they are older.
A panic attack is a sudden episode of intense fear that triggers severe physical reactions when there is no real danger or apparent cause. Panic attacks can be very frightening. When panic attacks occur, you might think you’re losing control, having a heart attack or even dying.
Many people have just one or two panic attacks in their lifetimes, and the problem goes away, perhaps when a stressful situation ends. But if you’ve had recurrent, unexpected panic attacks and spent long periods in constant fear of another attack, you may have a condition called panic disorder.
Although panic attacks themselves aren’t life-threatening, they can be frightening and significantly affect your quality of life. But treatment can be very effective.
Panic attacks typically begin suddenly, without warning. They can strike at any time — when you’re driving a car, at the mall, sound asleep or in the middle of a business meeting. You may have occasional panic attacks or they may occur frequently.
Panic attacks have many variations, but symptoms usually peak within minutes. You may feel fatigued and worn out after a panic attack subsides.
Factors that may increase the risk of developing panic attacks or panic disorder include:
- Family history of panic attacks or panic disorder
- Major life stress, such as the death or serious illness of a loved one
- A traumatic event, such as sexual assault or a serious accident
- Major changes in your life, such as a divorce or the addition of a baby
- Smoking or excessive caffeine intake
- History of childhood physical or sexual abuse
Left untreated, panic attacks and panic disorder can affect almost every area of your life. You may be so afraid of having more panic attacks that you live in a constant state of fear, ruining your quality of life.
Complications that panic attacks may cause or be linked to include:
- Development of specific phobias, such as fear of driving or leaving your home
- Frequent medical care for health concerns and other medical conditions
- Avoidance of social situations
- Problems at work or school
- Depression, anxiety disorder and other psychiatric disorders
- Increased risk of suicide or suicidal thoughts
- Alcohol or other substance misuse
- Financial problems
For some people, panic disorder may include agoraphobia — avoiding places or situations that cause you anxiety because you fear not being able to escape or get help if you have a panic attack. Or you may become reliant on others to be with you in order to leave your home.
If you’ve had signs or symptoms of a panic attack, make an appointment with your primary care provider. After an initial evaluation, your doctor may refer you to a psychiatrist or psychologist for treatment.
Symptoms of Panic attack
A panic attack begins suddenly, and most often peaks within 10 to 20 minutes. Some symptoms continue for an hour or more. A panic attack may be mistaken for a heart attack.
A person with panic disorder often lives in fear of another attack, and may be afraid to be alone or far from medical help.
People with panic disorder have at least 4 of the following symptoms during an attack:
- Chest pain or discomfort
- Dizziness or feeling faint
- Fear of dying
- Fear of losing control or impending doom
- Feeling of choking
- Feelings of detachment
- Feelings of unreality
- Nausea or upset stomach
- Numbness or tingling in the hands, feet, or face
- Palpitations, fast heart rate, or pounding heart
- Sensation of shortness of breath or smothering
- Sweating, chills, or hot flashes
- Trembling or shaking
Panic attacks may change behavior and function at home, school, or work. People with the disorder often worry about the effects of their panic attacks.
People with panic disorder may abuse alcohol or other drugs. They may feel sad or depressed.
Panic attacks cannot be predicted. At least in the early stages of the disorder, there is no trigger that starts the attack. Recalling a past attack may trigger panic attacks.
Exams and Tests for Panic attack
Many people with panic disorder first seek treatment in the emergency room. This is because the panic attack often feels like a heart attack.
The health care provider will perform a physical exam and a mental health assessment.
Blood tests will be done. Other medical disorders must be ruled out before panic disorder can be diagnosed. Disorders related to substance use will be considered because symptoms can resemble panic attacks.
Treatment for Panic attack
The goal of treatment is to help you function well during everyday life. Using both medicines and talk therapy works best.
Certain medicines, usually used to treat depression, may be very helpful for this disorder. They work by preventing your symptoms or making them less severe. You must take these medicines every day. DO NOT stop taking them without talking with your provider.
Medicines called sedatives or hypnotics may also be prescribed.
- These medicines should only be taken under a doctor’s direction.
- Your doctor will prescribe a limited amount of these drugs. They should not to be used everyday.
- They may be used when symptoms become very severe or when you are about to be exposed to something that always brings on your symptoms.
- If you are prescribed a sedative, do not drink alcohol while on this medicine.
Talk therapy (cognitive-behavioral therapy, or CBT) helps you understand your behaviors and how to change them. During therapy you will learn how to:
- Understand and control distorted views of life stressors, such as other people’s behavior or life events.
- Recognize and replace thoughts that cause panic and decrease the sense of helplessness.
- Manage stress and relax when symptoms occur.
- Imagine the things that cause the anxiety, starting with the least fearful. Practice in real-life situations to help you overcome your fears.
The following may also help reduce the number or severity of panic attacks:
- Not drinking alcohol
- Eating at regular times
- Getting plenty of exercise
- Getting enough sleep
- Reducing or avoiding caffeine, certain cold medicines, and stimulants
Support Groups for Panic Attack and Panic Disorder
You can ease the stress of having panic disorder by joining a support group. Sharing with others who have common experiences and problems can help you not feel alone.
Support groups are usually not a good substitute for talk therapy or taking medicine, but can be a helpful addition.
Resources for more information include:
- Anxiety and Depression Association of America: www.adaa.org
- National Institute of Mental Health: www.nimh.nih.gov/health/publications/panic-disorder-when-fear-overwhelms/index.shtml
- Angina (Chest Pain). American Heart Association. http://www.heart.org/HEARTORG/Conditions/HeartAttack/DiagnosingaHeartAttack/Angina-Chest-Pain_UCM_450308_Article.jsp[↩][↩]
- Angina. National Heart, Lung and Blood Institute, National Institutes of Health. https://www.nhlbi.nih.gov/health/health-topics/topics/angina[↩][↩][↩][↩][↩][↩][↩][↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Coronary Heart Disease. https://www.nhlbi.nih.gov/health/health-topics/topics/cad[↩][↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Heart Attack. https://www.nhlbi.nih.gov/health/health-topics/topics/heartattack[↩]
- Angina Pectoris (Stable Angina). American Heart Association. http://www.heart.org/HEARTORG/Conditions/HeartAttack/DiagnosingaHeartAttack/Angina-Pectoris-Stable-Angina_UCM_437515_Article.jsp[↩]
- Unstable Angina. American Heart Association. http://www.heart.org/HEARTORG/Conditions/HeartAttack/DiagnosingaHeartAttack/Unstable-Angina_UCM_437513_Article.jsp[↩][↩]
- Prinzmetal’s or Prinzmetal Angina, Variant Angina and Angina Inversa. American Heart Association. http://www.heart.org/HEARTORG/Conditions/HeartAttack/DiagnosingaHeartAttack/Prinzmetals-or-Prinzmetal-Angina-Variant-Angina-and-Angina-Inversa_UCM_435674_Article.jsp[↩]
- Coronary Microvascular Disease (MVD). American Heart Association. http://www.heart.org/HEARTORG/Conditions/HeartAttack/DiagnosingaHeartAttack/Coronary-Microvascular-Disease-MVD_UCM_450320_Article.jsp[↩][↩][↩]
- WISE Study of Women and Heart Disease Yields Important Findings On Frequently Undiagnosed Coronary Syndrome. National Heart, Lung and Blood Institute, National Institutes of Health. https://www.nhlbi.nih.gov/news/press-releases/2006/wise-study-of-women-and-heart-disease-yields-important-findings-on-frequently-undiagnosed-coronary-syndrome[↩]
- Women and Cardiovascular Heart Disease: Clinical Implications From the Women’s Ischemia Syndrome Evaluation (WISE) Study. Journal of the American College of Cardiology Feb 2006, 47 (3 Supplement) S59-S62; DOI: 10.1016/j.jacc.2004.10.083. http://www.onlinejacc.org/content/47/3_Supplement/S59[↩]
- Pulmonary Embolism. National Heart, Lung and Blood Institute, National Institutes of Health. https://www.nhlbi.nih.gov/health/health-topics/topics/pe[↩][↩]
- Aortic stenosis. Medline Plus, U.S. National Library of Medicine. https://medlineplus.gov/ency/article/000178.htm[↩]
- Hypertrophic cardiomyopathy. Medline Plus, U.S. National Library of Medicine. https://medlineplus.gov/ency/article/000192.htm[↩]
- Pericarditis. Medline Plus, U.S. National Library of Medicine. https://medlineplus.gov/ency/article/000182.htm[↩]
- Panic disorder. Medline Plus, U.S. National Library of Medicine. https://medlineplus.gov/ency/article/000924.htm[↩]
- Panic attacks and panic disorder. Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/panic-attacks/basics/definition/CON-20020825?p=1[↩]