Contents
- What is insulin ?
- Types of Insulin
- Comparing human insulin and insulin analogues
- What is the Pancreas ?
- The different types of insulin
- Insulin’s Role in Blood Glucose Control
- What happens with insulin resistance ?
- What causes insulin resistance ?
- What is Prediabetes ?
- How does Insulin Resistance relate to type 2 Diabetes and Prediabetes ?
- What are the symptoms of insulin resistance and prediabetes ?
- Who should be tested for prediabetes ?
- How are insulin resistance and prediabetes diagnosed ?
- Why should a person be tested for diabetes ?
- Can insulin resistance and prediabetes be reversed ?
What is insulin ?
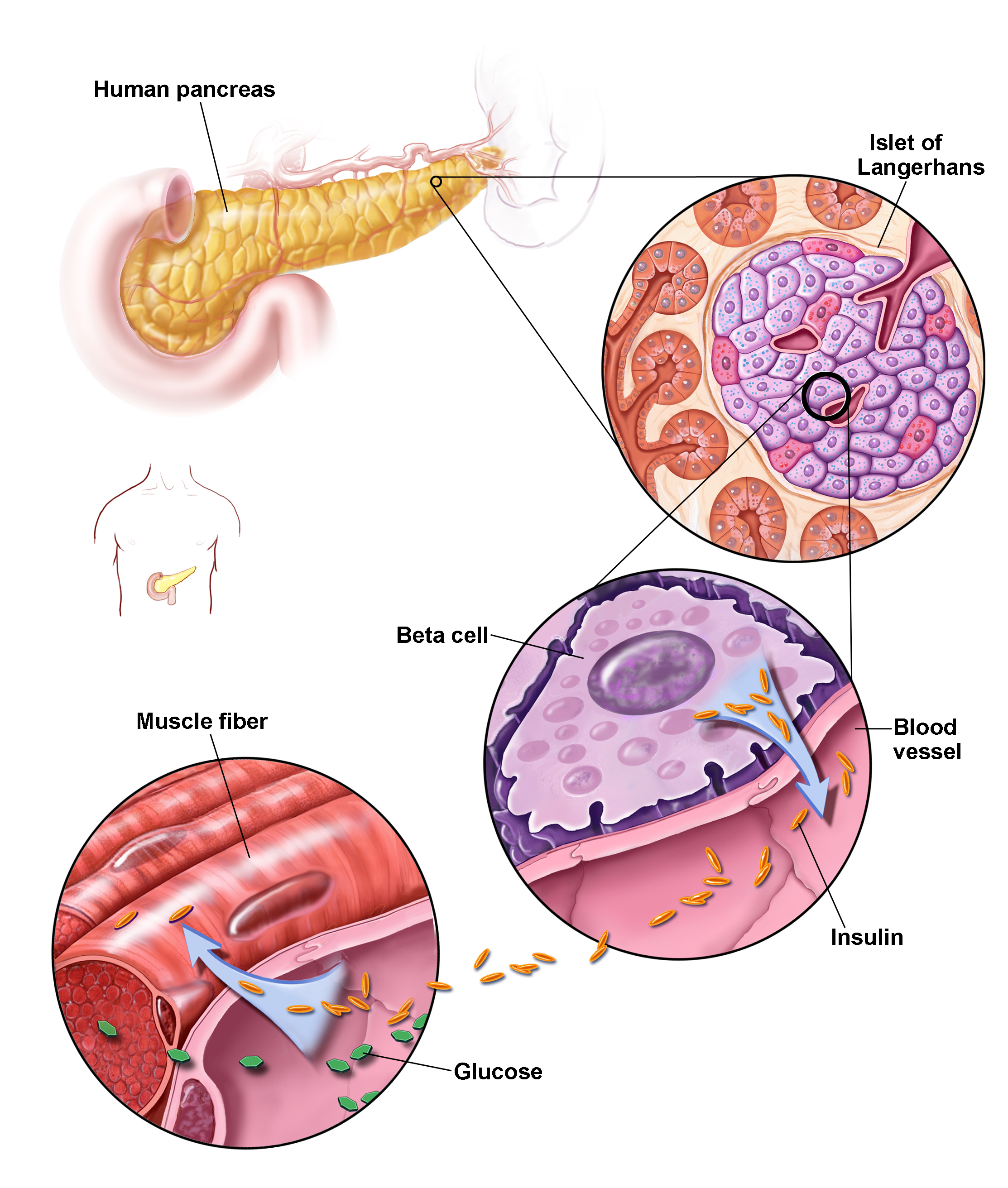
Insulin is a hormone made in the pancreas, an organ located behind the stomach. The pancreas contains clusters of cells called islets. Beta cells within the islets make insulin and release it into the blood. When the body cannot make enough insulin, insulin is taken by injection or other means 1.
Insulin is a hormone that helps your body use glucose for energy.
Insulin plays a major role in metabolism—the way the body uses digested food for energy. The digestive tract breaks down carbohydrates—sugars and starches found in many foods—into glucose. Glucose is a form of sugar that enters the bloodstream. With the help of insulin, cells throughout the body absorb glucose and use it for energy.
Insulin resistance is when your body’s inability to respond to and use the insulin it produces. In insulin resistance, muscle, fat, and liver cells do not respond properly to insulin and thus cannot easily absorb glucose from the bloodstream. As a result, your body needs higher levels of insulin to help glucose enter cells.
Insulin resistance may be linked to obesity, hypertension, and high levels of fat in the blood.
Types of Insulin
Insulin therapy is essential for everyone who has type 1 diabetes and some people who have type 2 diabetes. Various types of insulin are available. They differ in terms of how long their effect lasts, as well as their chemical structure 2.
Some types of insulin work quickly (short-acting insulin or rapid-acting insulin), while others only start to work after a certain amount of time, and then work over a longer time period (long-acting or basal insulin).
Insulin can be extracted from the pancreas cells of pigs (porcine insulin) or cattle (bovine insulin) and prepared for use in humans. But nowadays most people use genetically engineered insulin for the treatment of diabetes. One type of synthetic insulin is called “human insulin.” Human insulin mimics the insulin made in the human body. There are also other types of synthetic insulin called “insulin analogues.” Their chemical structure is different to that of other kinds of insulin.
Comparing human insulin and insulin analogues
Insulin analogues were introduced to the market in the 1990s. Compared to human insulin, they start lowering blood sugar somewhat sooner after being injected. For many years now there has been a debate about whether people with diabetes benefit from this. But research has not found any evidence to suggest they do 2.
If, for instance, a particular type of insulin were shown to prevent complications caused by poorly controlled blood sugar levels, that type of insulin would offer a clear advantage. It would also be an advantage if the insulin prevented strong fluctuations in blood sugar levels that lead to noticeably low or high blood sugar (hypoglycemia or hyperglycemia). Or if it made it easier for people to follow their daily treatment plan. But studies in this area suggest that insulin analogues and human insulin are equally effective in the treatment of diabetes 2.
What is the Pancreas ?
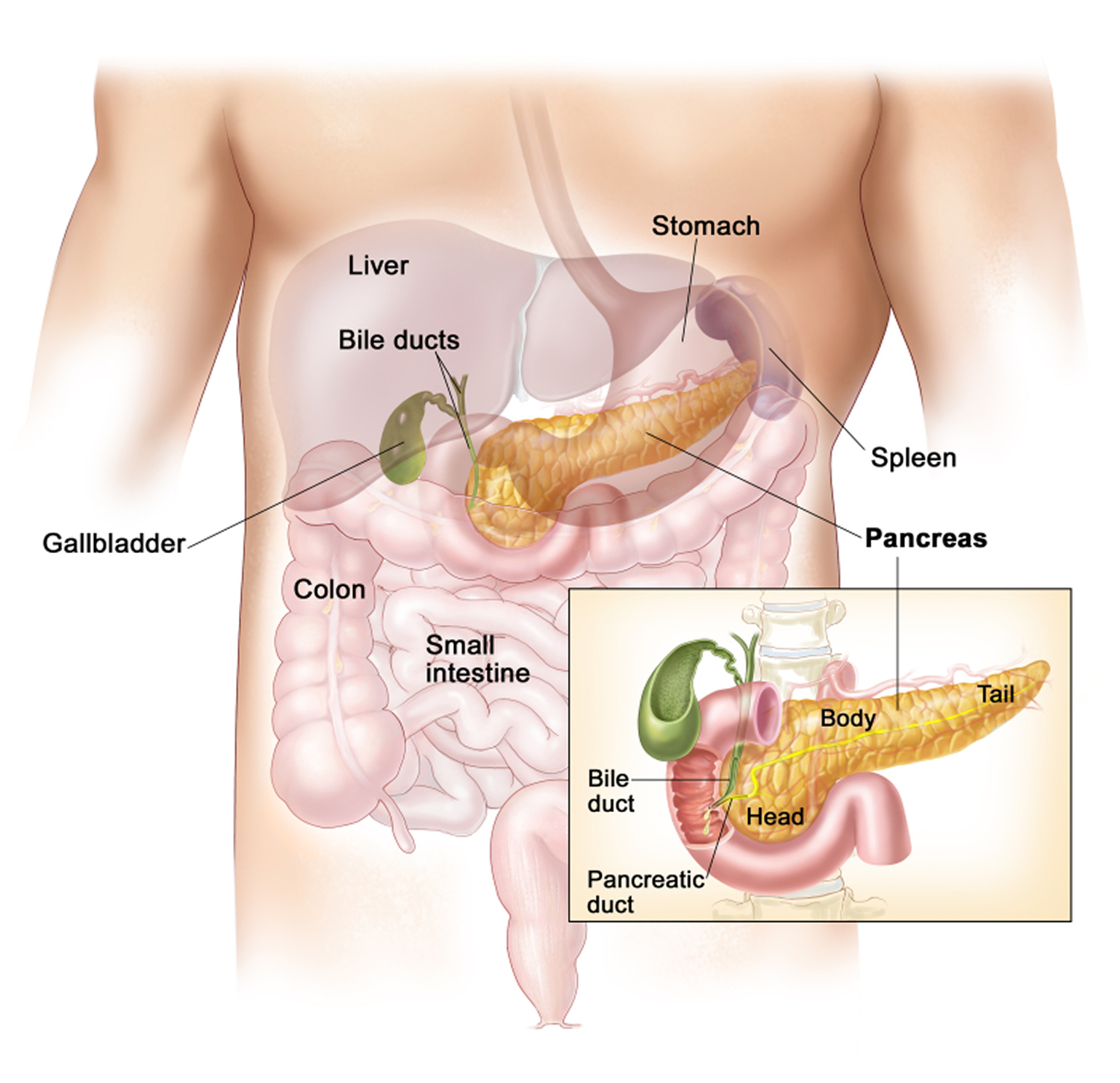
The pancreas is 12 to 18 centimeters (about 4.7 to 7.1 inches) long and weighs about 70 to 100 grams. The pancreas is made up of a head, a body and a pointy tail. It is located in the upper abdomen behind the stomach 3. The organ has two major functions. It produces
- the enzymes that break down foods in the intestine, and
- the hormones such as insulin, which maintain a constant blood sugar level.
Over 99% of the exocrine pancreas cells produce digestive juices – about 1.5 to 2 liters per day. They are called exocrine (“secreting externally”) because they secrete digestive juice “externally” into the small intestine. This clear, colorless juice is mainly made up of water and also contains salt, sodium bicarbonate and digestive enzymes. There are enzymes for breaking down fats (lipases), proteins (proteases), and carbohydrates (amylases). Proteases are inactive while inside the pancreas. They are activated once they have been secreted into the small intestine. The sodium bicarbonate neutralizes the acidic gastric (stomach) juice in the mass of semi-digested food to help the digestive enzymes work better.
The digestive juices flows from the pancreas through an excretory duct into the small intestine. In most people, this duct joins up with the the excretory duct of the gallbladder before reaching the small intestine. A sphincter muscle at the end of the duct controls the flow of digestive juice into the small intestine.
In case of pancreatitis, enzymes may be activated inside the pancreas before reaching the small intestine, causing the gland to start “digesting itself.”
Endocrine pancreas cells
Groups of endocrine cells are spread over the surface of the pancreas. They are called islets of Langerhans, because they are scattered like small islands and were discovered by pathologist Paul Langerhans. These islet cells produce insulin, glucagon and other hormones. They are called endocrine (“secreting internally”) cells, because they secrete hormones directly into the blood. These hormones help to regulate blood sugar levels and keep them from getting too high or too low.
When the blood sugar levels rise, as they might after a meal, insulin is released by the islets of Langerhans. The insulin is then able to transport sugar from the blood into the cells of the body, where it can be converted into energy. Insulin also allows the liver and the muscles to store more sugar, as well as keeping the liver from producing more sugar. This has the effect of lowering blood sugar levels.
When blood sugar levels are too low, the pancreas releases glucagon into the bloodstream. This hormone acts as an antagonist to insulin. It causes the liver cells of the liver to release stored sugar and to convert proteins into sugar to make them available as a source of energy too. The flow of glucagon is stopped once blood sugar levels rise 3.
The different types of insulin
The following types of insulin products are classified according to how quickly and how long they are effective, and their chemical structure:
- Short-acting insulin:
+ Insulin analogues:
+ Start working: about 5 to 10 minutes after injection
+ Peak activity: about 1 to 1.5 hours after injection
+ Effective for: about 2 to 3 hours
+ Regular insulin (human insulin, porcine insulin, bovine insulin):
+ Starts working: about 15 to 30 minutes after injection
+ Peak activity: about 1.5 to 3 hours after injection
+ Effective for: about 4 to 8 hours
- Intermediate-acting insulin (insulin analogues, human insulin or porcine insulin with delayed action due to addition of NPH (neutral protamine Hagedorn) or zinc):
+ Starts working: about 2 hours after injection
+ Peak activity: about 4 to 6 hours after injection
+ Effective for: about 12 to 14 hours
- Long-acting insulin (insulin analogues, human insulin, porcine insulin):
+ Slow onset of action.
+ Peak activity and how long it is effective depends on the way in which the action is delayed. Usually works for up to 24 hours.
- Premixed insulin (insulin analogues, human insulin, porcine insulin):
+ Short-acting insulin and intermediate-acting or long-acting insulin that has already been mixed.
Short-acting insulin – including regular insulin, insulin analogues and premixed insulin – is normally injected before meals. Some people wait a certain amount of time following the injection before they eat. Others vary the time interval between injecting and eating depending on their blood sugar levels.
Many people find fixed injection-meal intervals bothersome and difficult to stick to in everyday life. So far there is no evidence to show that blood sugar levels are better controlled if you stick to fixed injection-meal intervals.
Insulin’s Role in Blood Glucose Control
When blood glucose levels rise after a meal, the pancreas releases insulin into the blood. Insulin and glucose then travel in the blood to cells throughout the body.
- Insulin helps muscle, fat, and liver cells absorb glucose from the bloodstream, lowering blood glucose levels.
- Insulin stimulates the liver and muscle tissue to store excess glucose. The stored form of glucose is called glycogen.
- Insulin also lowers blood glucose levels by reducing glucose production in the liver.
In a healthy person, these functions allow blood glucose and insulin levels to remain in the normal range.
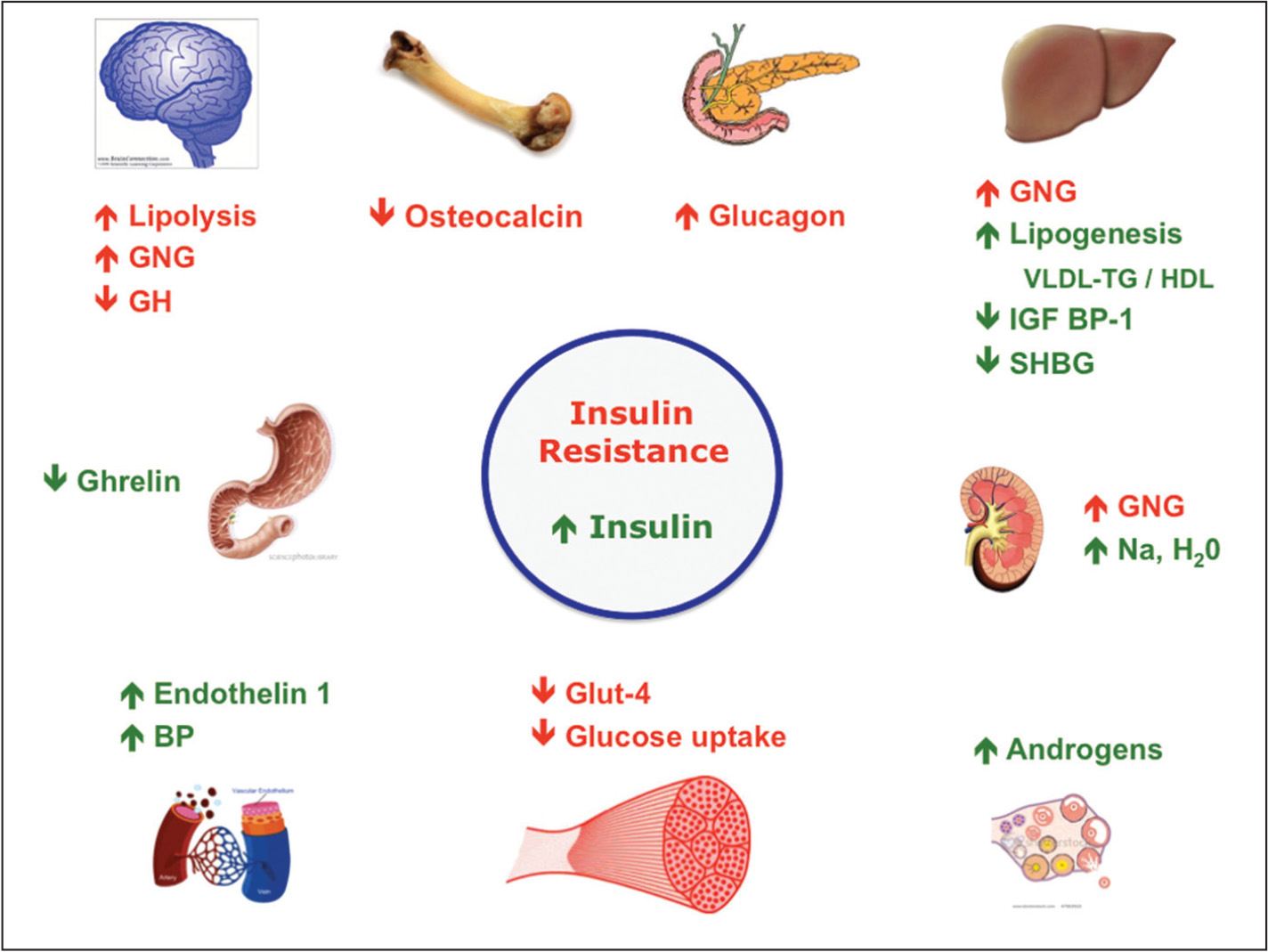
What happens with insulin resistance ?
In insulin resistance, muscle, fat, and liver cells do not respond properly to insulin and thus cannot easily absorb glucose from the bloodstream. As a result, the body needs higher levels of insulin to help glucose enter cells.
The beta cells in the pancreas try to keep up with this increased demand for insulin by producing more. As long as the beta cells are able to produce enough insulin to overcome the insulin resistance, blood glucose levels stay in the healthy range.
Over time, insulin resistance can lead to type 2 diabetes and prediabetes because the beta cells fail to keep up with the body’s increased need for insulin. Without enough insulin, excess glucose builds up in the bloodstream, leading to diabetes, prediabetes, and other serious health disorders 4.
What causes insulin resistance ?
Although the exact causes of insulin resistance are not completely understood, scientists think the major contributors to insulin resistance are excess weight (obesity) and physical inactivity. Insulin resistance may be linked to obesity, hypertension, and high levels of fat in the blood 5.
1) Excess Weight
Some experts believe obesity, especially excess fat around the waist, is a primary cause of insulin resistance. Scientists used to think that fat tissue functioned solely as energy storage. However, studies have shown that belly fat produces hormones and other substances that can cause serious health problems such as insulin resistance, high blood pressure, imbalanced cholesterol, and cardiovascular disease (CVD).
Belly fat plays a part in developing chronic, or long-lasting, inflammation in the body. Chronic inflammation can damage the body over time, without any signs or symptoms. Scientists have found that complex interactions in fat tissue draw immune cells to the area and trigger low-level chronic inflammation. This inflammation can contribute to the development of insulin resistance, type 2 diabetes, and CVD. Studies show that losing the weight can reduce insulin resistance and prevent or delay type 2 diabetes.

2) Physical Inactivity
Many studies have shown that physical inactivity is associated with insulin resistance, often leading to type 2 diabetes. In the body, more glucose is used by muscle than other tissues. Normally, active muscles burn their stored glucose for energy and refill their reserves with glucose taken from the bloodstream, keeping blood glucose levels in balance.
Studies show that after exercising, muscles become more sensitive to insulin, reversing insulin resistance and lowering blood glucose levels. Exercise also helps muscles absorb more glucose without the need for insulin. The more muscle a body has, the more glucose it can burn to control blood glucose levels.
3) Other Causes
Other causes of insulin resistance may include ethnicity; certain diseases; hormones; steroid use; some medications; older age; sleep problems, especially sleep apnea; and cigarette smoking.
Does sleep matter ?
Yes. Studies show that untreated sleep problems, especially sleep apnea, can increase the risk of obesity, insulin resistance, and type 2 diabetes. Night shift workers may also be at increased risk for these problems. Sleep apnea is a common disorder in which a person’s breathing is interrupted during sleep. People may often move out of deep sleep and into light sleep when their breathing pauses or becomes shallow. This results in poor sleep quality that causes problem sleepiness, or excessive tiredness, during the day.
Many people aren’t aware of their symptoms and aren’t diagnosed. People who think they might have sleep problems should talk with their health care provider.
What is Prediabetes ?
Prediabetes is a condition in which blood glucose (HB A1C levels) —which reflect average blood glucose levels—are higher than normal but not high enough for a diagnosis of diabetes. In prediabetes, the beta cells can no longer produce enough insulin to overcome insulin resistance, causing blood glucose levels to rise above the normal range. Prediabetes is becoming more common in the United States. The U.S. Department of Health and Human Services estimates that at least 86 million U.S. adults ages 20 or older had prediabetes in 2012 6.
Having prediabetes is a risk factor for getting type 2 diabetes and CVD, which can lead to heart attack or stroke.
People with prediabetes may be retested each year. Within the prediabetes A1C range of 5.7 to 6.4 percent, the higher the A1C, the greater the risk of diabetes. Those with prediabetes are likely to develop type 2 diabetes within 10 years, but they can take steps to prevent or delay diabetes.
How does Insulin Resistance relate to type 2 Diabetes and Prediabetes ?
Insulin resistance increases your risk of developing type 2 diabetes and prediabetes. Prediabetes usually occurs in people who already have insulin resistance. Although insulin resistance alone does not cause type 2 diabetes, it often sets the stage for the disease by placing a high demand on the insulin-producing beta cells. In prediabetes, the beta cells can no longer produce enough insulin to overcome insulin resistance, causing blood glucose levels to rise above the normal range.
Once a person has prediabetes, continued loss of beta cell function usually leads to type 2 diabetes. People with type 2 diabetes have high blood glucose. Over time, high blood glucose damages nerves and blood vessels, leading to complications such as heart disease, stroke, blindness, kidney failure, and lower-limb amputations.
Studies have shown that most people with prediabetes develop type 2 diabetes within 10 years, unless they change their lifestyle. Lifestyle changes include losing 5 to 7 percent of their body weight—10 to 14 pounds for people who weigh 200 pounds—by making changes in their diet and level of physical activity.
What are the symptoms of insulin resistance and prediabetes ?
Insulin resistance and prediabetes usually have no symptoms. People may have one or both conditions for several years without knowing they have them. Even without symptoms, health care providers can identify people at high risk by their physical characteristics, also known as risk factors.
People with a severe form of insulin resistance may have dark patches of skin, usually on the back of the neck. Sometimes people have a dark ring around their neck. Dark patches may also appear on elbows, knees, knuckles, and armpits. This condition is called acanthosis nigricans.
Who should be tested for prediabetes ?
The American Diabetes Association (ADA) recommends that testing to detect prediabetes be considered in adults who are overweight or obese and have one or more additional risk factors for diabetes. The section “Body Mass Index (BMI)” explains how to determine if a person is overweight or obese. However, not everyone who is overweight will get type 2 diabetes. People without these risk factors should begin testing at age 45.
Risk factors for prediabetes—in addition to being overweight or obese or being age 45 or older—include the following:
- being physically inactive
- having a parent or sibling with diabetes
- having a family background that is African American, Alaska Native, American Indian, Asian American, Hispanic/Latino, or Pacific Islander American
- giving birth to a baby weighing more than 9 pounds
- being diagnosed with gestational diabetes—diabetes that develops only during pregnancy
- having high blood pressure—140/90 mmHg or above—or being treated for high blood pressure
- HDL cholesterol level below 35 mg/dL or a triglyceride level above 250 mg/dL
- having polycystic ovary syndrome (PCOS)
- having prediabetes, impaired fasting glucose (IFG), or impaired glucose tolerance (IGT) on an earlier testing
- having other conditions associated with insulin resistance, such as obesity or acanthosis nigricans
- having cardiovascular disease (CVD)
If test results are normal, testing should be repeated at least every 3 years. Testing is important for early diagnosis. Catching prediabetes early gives people time to change their lifestyle and prevent type 2 diabetes and CVD. Health care providers may recommend more frequent testing depending on initial results and risk status.
In addition to weight, the location of excess fat on the body can be important. A waist measurement of 40 inches or more for men and 35 inches or more for women is linked to insulin resistance and increases a person’s risk for type 2 diabetes. This is true even if a person’s BMI falls within the normal range.
How are insulin resistance and prediabetes diagnosed ?
Health care providers use blood tests to determine whether a person has prediabetes, but they do not usually test specifically for insulin resistance. Insulin resistance can be assessed by measuring the level of insulin in the blood.
However, the test that most accurately measures insulin resistance, called the euglycemic clamp, is too costly and complicated to be used in most health care providers’ offices. The clamp is a research tool used by scientists to learn more about glucose metabolism. Research has shown that if blood tests indicate prediabetes, insulin resistance most likely is present.
Blood Tests for Prediabetes
All blood tests involve drawing blood at a health care provider’s office or commercial facility and sending the sample to a lab for analysis. Lab analysis of blood is needed to ensure test results are accurate. Glucose measuring devices used in a health care provider’s office, such as finger-stick devices, are not accurate enough for diagnosis but may be used as a quick indicator of high blood glucose.
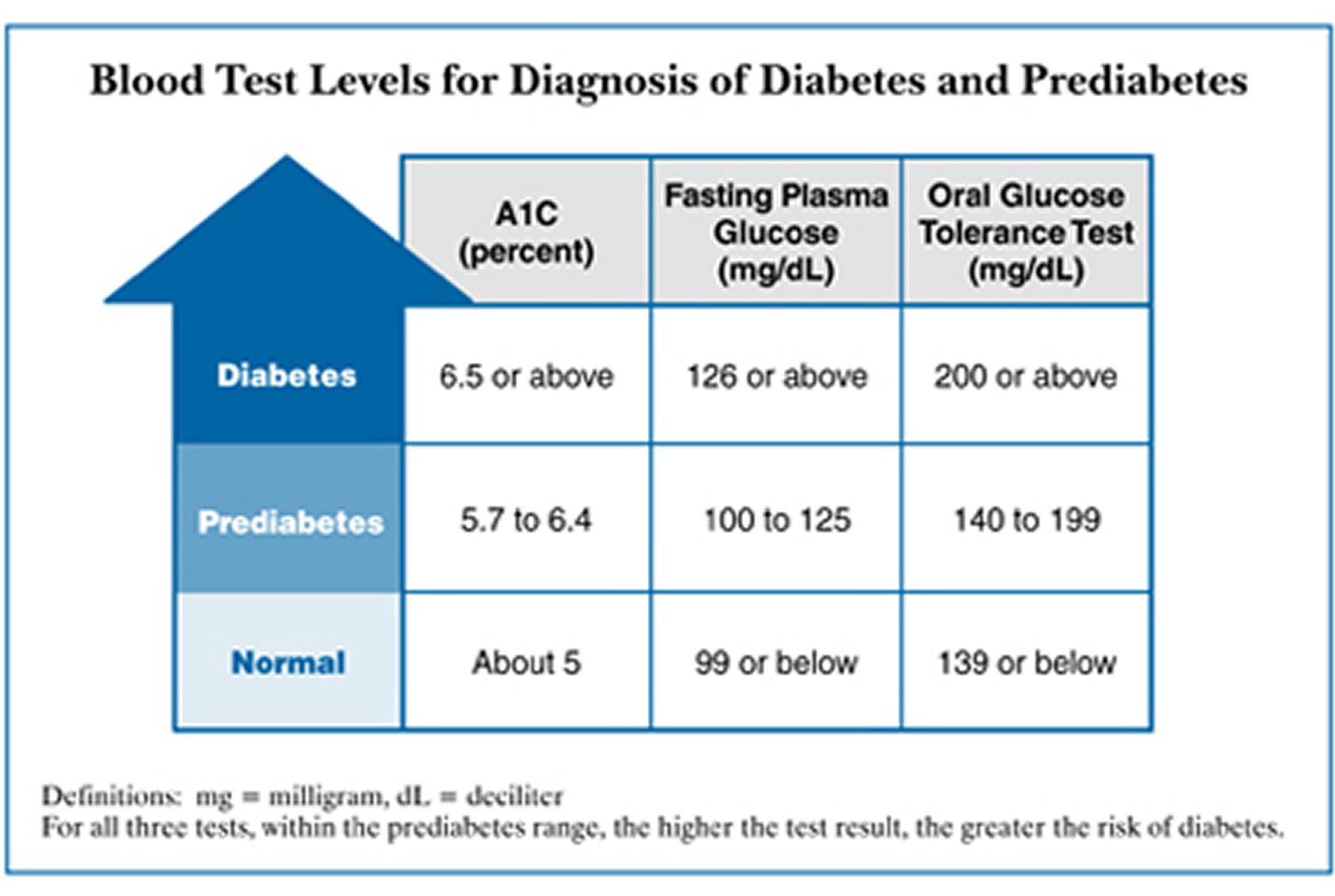
Prediabetes can be detected with one of the following blood tests:
- The HB A1C test
- The fasting plasma glucose (FPG) test
- The oral glucose tolerance test (OGTT)
1) HB A1C test. Sometimes called hemoglobin A1c, HbA1c, or glycohemoglobin test, this test reflects average blood glucose levels over the past 3 months. This test is the most reliable test for prediabetes, but it is not as sensitive as the other tests. In some individuals, it may miss prediabetes that could be caught by glucose tests.
The A1C test is based on the attachment of glucose to hemoglobin, the protein in red blood cells that carries oxygen. In the body, red blood cells are constantly forming and dying, but typically they live for about 3 months. Thus, the A1C test reflects the average of a person’s blood glucose levels over the past 3 months. The A1C test result is reported as a percentage. The higher the percentage, the higher a person’s blood glucose levels have been. A normal A1C level is below 5.7 percent.
Although some health care providers can quickly measure A1C in their office, that type of measurement—called a point-of-care test—is not considered reliable for diagnosis. For diagnosis of prediabetes, the A1C test should be analyzed in a laboratory.
The HB A1C test can be unreliable for diagnosing prediabetes in people with certain conditions that are known to interfere with the results. Interference should be suspected when A1C results seem very different from the results of a blood glucose test. People of African, Mediterranean, or Southeast Asian descent, or people with family members with sickle cell anemia or a thalassemia, are particularly at risk of interference. People in these groups may have a less common type of hemoglobin, known as a hemoglobin variant, that can interfere with some A1C tests.
A HB A1C of 5.7 to 6.4 percent indicates prediabetes.
| Diagnosis* | A1C Level |
|---|---|
| Normal | below 5.7 percent |
| Diabetes | 6.5 percent or above |
| Prediabetes | 5.7 to 6.4 percent |
Can the A1C test be used to diagnose type 2 diabetes and prediabetes ?
Yes. In 2009, an international expert committee recommended the A1C test as one of the tests available to help diagnose type 2 diabetes and prediabetes 7. Previously, only the traditional blood glucose tests were used to diagnose diabetes and prediabetes.
Because the A1C test does not require fasting and blood can be drawn for the test at any time of day, experts are hoping its convenience will allow more people to get tested—thus, decreasing the number of people with undiagnosed diabetes. However, some medical organizations continue to recommend using blood glucose tests for diagnosis.
2) Fasting plasma glucose test. This test measures blood glucose in people who have not eaten anything for at least 8 hours. This test is most reliable when done in the morning. Prediabetes found with this test is called IFG.
Fasting glucose levels of 100 to 125 mg/dL indicate prediabetes.
3) The Oral Glucose Tolerance Test (OGTT). This test measures blood glucose after people have not eaten (fasting) for at least 8 hours and 2 hours after they drink a sweet liquid provided by a health care provider or laboratory. Prediabetes found with this test is called IGT.
A blood glucose level between 140 and 199 mg/dL indicates prediabetes.
The following table lists the blood test levels for a diagnosis of prediabetes.
Why should a person be tested for diabetes ?
Testing is especially important because early in the disease diabetes has no symptoms. Although no test is perfect, the A1C and blood glucose tests are the best tools available to diagnose diabetes—a serious and lifelong disease.
Testing enables health care providers to find and treat diabetes before complications occur and to find and treat prediabetes, which can delay or prevent type 2 diabetes from developing.
Can insulin resistance and prediabetes be reversed ?
Yes. Physical activity and weight loss help the body respond better to insulin. The Diabetes Prevention Program was a federally funded study of 3,234 people at high risk for diabetes.
The Diabetes Prevention Program and other large studies proved that people with prediabetes can often prevent or delay diabetes if they lose a modest amount of weight by cutting fat and calorie intake and increasing physical activity—for example, walking 30 minutes a day, 5 days a week.
People at High Risk for Diabetes
The Diabetes Prevention Program study participants were overweight and had prediabetes. Many had family members with type 2 diabetes. Prediabetes, obesity, and a family history of diabetes are strong risk factors for type 2 diabetes. About half of the Diabetes Prevention Program participants were from minority groups with high rates of diabetes, including African Americans, Alaska Natives, American Indians, Asian Americans, Hispanics/Latinos, and Pacific Islander Americans.
The Diabetes Prevention Program participants also included others at high risk for developing type 2 diabetes, such as women with a history of gestational diabetes and people ages 60 and older.
Approaches to Preventing Diabetes
The Diabetes Prevention Program tested three approaches to preventing diabetes:
- Making lifestyle changes. People in the lifestyle change group exercised, usually by walking 5 days a week for about 30 minutes a day, and lowered their intake of fat and calories.
- Taking the diabetes medication metformin. Those who took metformin also received information about physical activity and diet.
- Receiving education about diabetes. The third group only received information about physical activity and diet and took a placebo—a pill without medication in it.
People in the lifestyle change group showed the best outcomes. However people who took metformin also benefited. The results showed that by losing an average of 15 pounds in the first year of the study, people in the lifestyle change group reduced their risk of developing type 2 diabetes by 58 percent over 3 years.
Lifestyle change was even more effective in those ages 60 and older. People in this group reduced their risk by 71 percent.
People in the metformin group also benefited, reducing their risk by 31 percent.
Lasting Results
The Diabetes Prevention Program Outcomes Study (DPPOS) has shown that the benefits of weight loss and metformin last for at least 10 years. The DPPOS has continued to follow most DPP participants since the DPP ended in 2001. The DPPOS showed that 10 years after enrolling in the Diabetes Prevention Program.
- people in the lifestyle change group reduced their risk for developing diabetes by 34 percent
- those in the lifestyle change group ages 60 or older had even greater benefit, reducing their risk of developing diabetes by 49 percent
- participants in the lifestyle change group also had fewer heart and blood vessel disease risk factors, including lower blood pressure and triglyceride levels, even though they took fewer medications to control their heart disease risk
- those in the metformin group reduced their risk of developing diabetes by 18 percent
Even though controlling weight with lifestyle changes is challenging, it produces long-term health rewards by lowering the risk for type 2 diabetes, lowering blood glucose levels, and reducing other heart disease risk factors.
What steps can help reverse insulin resistance and prediabetes ?
By losing weight and being more physically active, people can reverse insulin resistance and prediabetes, thus preventing or delaying type 2 diabetes. People can decrease their risk by:
- Eating a healthy diet and reaching and maintaining a healthy weight
- Increasing physical activity
- Not smoking
- Not drinking alcohol
A) Eating, Diet, and Nutrition
Adopting healthy eating habits can help people lose a modest amount of weight and reverse insulin resistance. Experts encourage people to slowly adopt healthy eating habits that they can maintain, rather than trying extreme weight-loss solutions. People may need to get help from a dietitian or join a weight-loss program for support.
In general, people should lose weight by choosing healthy foods, controlling portions, eating less fat and refined sugar, and increasing physical activity. People are better able to lose weight and keep it off when they learn how to adapt their favorite foods to a healthy eating plan.
B) Physical Activity
Regular physical activity tackles several risk factors at once. Regular physical activity helps the body use insulin properly.
Regular physical activity also helps a person
- lose weight
- control blood glucose levels
- control blood pressure
- control cholesterol levels
People in the Diabetes Prevention Program who were physically active for 30 minutes a day, 5 days a week, reduced their risk of type 2 diabetes. Many chose brisk walking as their physical activity.
Most people should aim for at least 30 minutes of exercise most days of the week. For best results, people should do both aerobic activities, which use large muscle groups and make the heart beat faster, and muscle strengthening activities.
Aerobic activities include brisk walking, climbing stairs, swimming, dancing, and other activities that increase the heart rate.
Muscle strengthening activities include lifting weights and doing sit-ups or push-ups.
People who haven’t been physically active recently should talk with their health care provider about which activities are best for them and have a checkup before starting an exercise program.
Not Smoking
Those who smoke should quit. A health care provider can help people find ways to quit smoking. Studies show that people who get help have a better chance of quitting.
Points to Remember
- Insulin is a hormone that helps cells throughout the body absorb glucose and use it for energy. Insulin resistance is a condition in which the body produces insulin but does not use it effectively.
- Insulin resistance increases the risk of developing type 2 diabetes and prediabetes.
- The major contributors to insulin resistance are excess weight, especially around the waist, and physical inactivity.
- Prediabetes is a condition in which blood glucose or A1C levels—which reflect average blood glucose levels—are higher than normal but not high enough for a diagnosis of diabetes.
- The Diabetes Prevention Program (DPP) study and its follow-up study, the Diabetes Prevention Program Outcomes Study (DPPOS), confirmed that people with prediabetes can often prevent or delay diabetes if they lose a modest amount of weight by cutting fat and calorie intake and increasing physical activity.
- By losing weight and being more physically active, people can reverse insulin resistance and prediabetes, thus preventing or delaying type 2 diabetes.
- People with insulin resistance and prediabetes can decrease their risk for diabetes by eating a healthy diet and reaching and maintaining a healthy weight, increasing physical activity, not smoking, and not drinking alcohol.
- National Center for Biotechnology Information, PubMed Health. Insulin. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024496/[↩]
- National Center for Biotechnology Information, PubMed Health. Type 1 diabetes: Types of insulin. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072520/[↩][↩][↩]
- National Center for Biotechnology Information, PubMed Health. Pancreas. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0015631/[↩][↩]
- The National Institute of Diabetes and Digestive and Kidney Diseases, Health Information Center. Prediabetes & Insulin Resistance. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance[↩]
- National Center for Biotechnology Information, PubMed Health. Insulin Resistance. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0023068/[↩]
- Centers for Disease Control and Prevention. 2014 National Diabetes Statistics Report. https://www.cdc.gov/diabetes/data/statistics/2014statisticsreport.html[↩]
- The International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32(7):1327–1334.[↩]