Contents
What is Wilms tumor
Wilms tumors also known as nephroblastoma, are the most common cancers in children that start in the kidneys. In children and adolescents younger than 15 years old, most kidney cancers are Wilms tumors. About 9 of 10 kidney cancers in children are Wilms tumors, but Wilms tumor can happen in adults too.
Having certain genetic conditions or birth defects can increase the risk of getting Wilms tumor. Children that are at risk should be screened for Wilms tumor every three months until they turn eight.
Each year, about 500 new cases of Wilms tumors are diagnosed in the United States. This number has been fairly stable for many years. About 5% of all cancers in children are Wilms tumors.
Wilms tumors tend to occur in young children. The average age at diagnosis is about 3 to 4 years. It becomes less common as children grow older and is uncommon after age 6. It’s very rare in adults, although cases have been reported.
Most Wilms tumors are unilateral, which means they affect only one kidney. Most often there is only one tumor, but 5% to 10% of children with Wilms tumors have more than one tumor in the same kidney. About 5% of children with Wilms tumors have bilateral disease (tumors in both kidneys).
Wilms tumors often become quite large before they are noticed. The average newly found Wilms tumor is many times larger than the kidney in which it started. Most Wilms tumors are found before they have spread (metastasized) to other organs. Wilms tumor may spread to the lungs, liver, bone, brain, or nearby lymph nodes.
Symptoms include a lump in the abdomen, blood in the urine, and a fever for no reason. Tests that examine the kidney and blood are used to find the tumor.
Even if a doctor thinks a child might have a cancer such as Wilms tumor based on a physical exam or imaging tests, they can’t be sure until a small piece of the tumor is checked in a lab.
Doctors usually diagnose and remove the tumor in surgery. Other treatments include chemotherapy and radiation and biologic therapies. Biologic therapy boosts your body’s own ability to fight cancer.
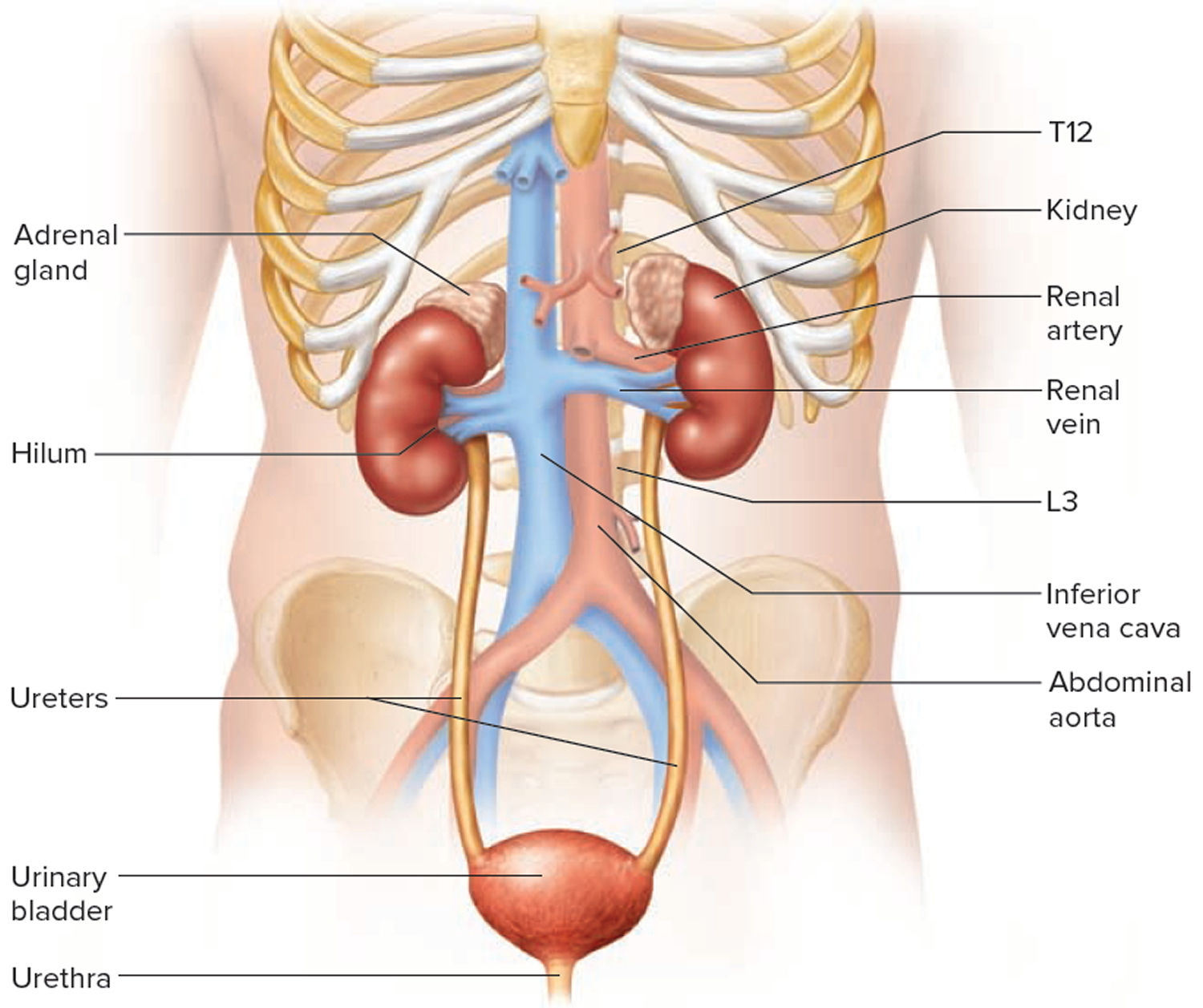
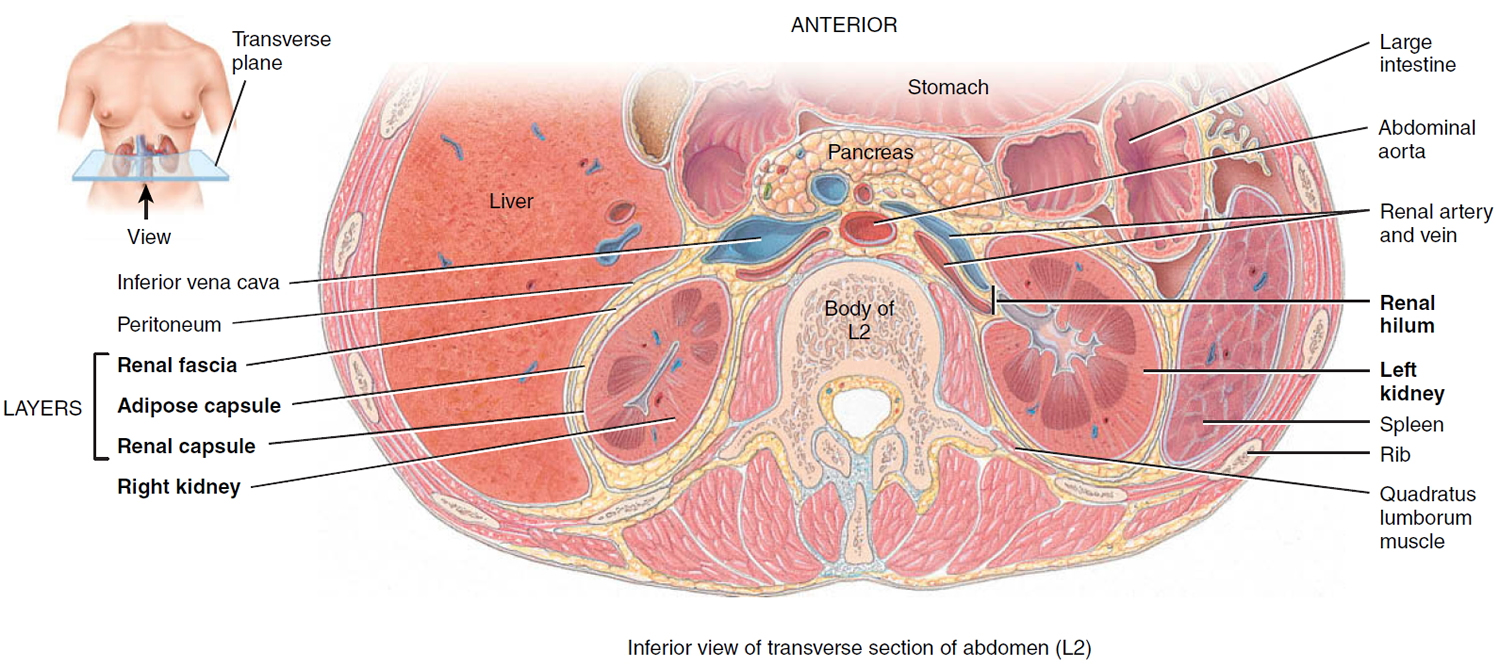
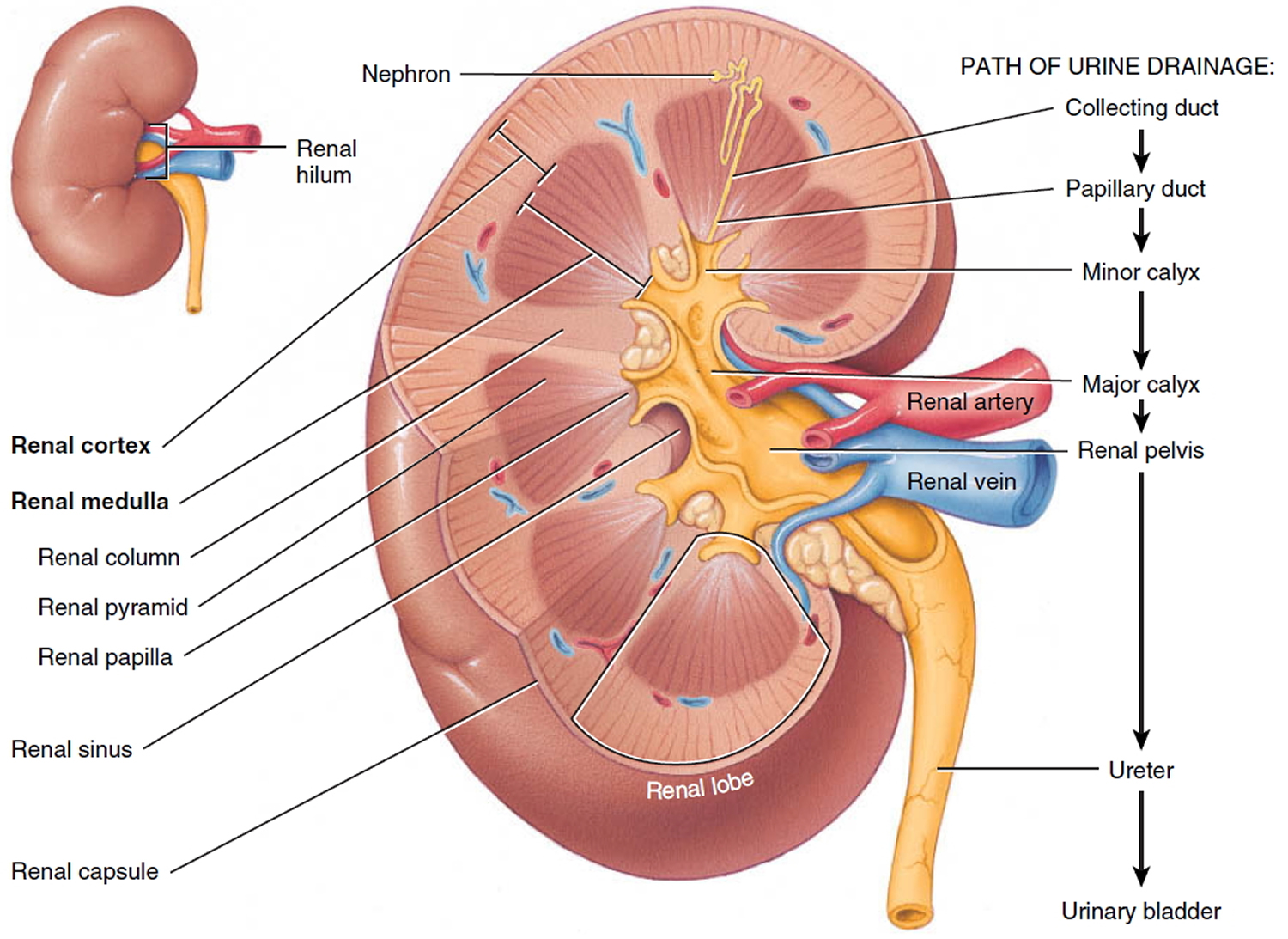
Kidneys
The main job of the kidneys is filtering blood coming in from the renal arteries to rid the body of excess water, salt, and waste products. These substances become urine. Urine leaves the kidneys through long, slender tubes called ureters that connect to the bladder. Urine flows down the ureters into the bladder, and is stored there until the person urinates.
The kidneys also have other jobs:
- They help control blood pressure by making a hormone called renin.
- They help make sure the body has enough red blood cells by making a hormone called erythropoietin. This hormone tells the bone marrow to make more red blood cells.
Your kidneys are important, but you actually need less than one complete kidney to do all of its basic functions. Many people in the United States live normal, healthy lives with just one kidney.
Figure 1. Kidney location
Figure 2. Kidney location (transverse section)
Figure 3. Kidney anatomy
Types of Wilms tumor
Wilms tumors (nephroblastoma) are grouped into 2 major types based on how they look under a microscope (their histology):
- Favorable histology: Although the cancer cells in these tumors don’t look quite normal, there is no anaplasia (see next paragraph). More than 9 of 10 Wilms tumors have a favorable histology. The chance of curing children with these tumors is very good.
- Unfavorable histology (anaplastic Wilms tumor): In these tumors, the look of the cancer cells varies widely, and the cells’ nuclei (the central parts that contain the DNA) tend to be very large and distorted. This is called anaplasia. The more anaplasia a tumor has, the harder it is to cure.
Other types of kidney cancers in children
Most kidney cancers in children are Wilms tumors, but in rare cases children can develop other types of kidney tumors.
- Mesoblastic nephroma
These tumors usually appear in the first few months of life. Children are usually cured with surgery, but sometimes chemotherapy is given as well. These tumors sometimes come back soon after treatment, so children who have had these tumors need to be watched closely for the first year afterward.
- Clear cell sarcoma of kidney
These tumors are much more likely to spread to other parts of the body than Wilms tumors, and they are harder to cure. Because these tumors are rare, treatment is often given as part of a clinical trial. It’s usually much like the intensive treatment used for Wilms tumors with unfavorable histology.
- Malignant rhabdoid tumor of the kidney
These tumors occur most often in infants and toddlers. They tend to spread to other parts of the body quickly, and most have already spread by the time they are found, which makes them hard to cure. Because these tumors are rare, treatment is often given as part of a clinical trial, and usually includes chemotherapy with several different drugs.
- Renal cell carcinoma
This is the most common type of kidney cancer in adults, but it also accounts for a small number of kidney tumors in children. It’s rare in young children, but it’s actually more common than Wilms tumor in older teens.
Surgery to remove the kidney is the main treatment for these cancers if it can be done. The outlook for these cancers depends largely on the extent (stage) of the cancer at the time it’s found, whether it can be removed completely with surgery, and its subtype (based on how the cancer cells look under a microscope). If the cancer is too advanced to be removed by surgery, other types of treatment may be needed.
What Causes Wilms Tumor?
Although there is a clear link between Wilms tumors and certain birth defect syndromes and genetic changes, most children with this type of cancer do not have any known birth defects or inherited gene changes.
Researchers do not yet know exactly why some children get Wilms tumors, but they have made great progress in understanding how normal kidneys develop, as well as how this process can go wrong, leading to a Wilms tumor.
The kidneys develop very early as a fetus grows in the womb. Changes (mutations) in certain genes in early kidney cells can lead to problems as the kidneys develop. Some of the cells that are supposed to develop into mature kidney cells stay as early kidney cells instead. Clusters of these early kidney cells sometimes remain after the baby is born. Usually, these cells mature by the time the child is 3 to 4 years old. If this doesn’t happen, the cells might somehow begin to grow out of control, which might result in a Wilms tumor.
Normal human cells grow and function based mainly on the information contained in each cell’s chromosomes (long strands of DNA in each cell). DNA carries the instructions for nearly everything our cells do. DNA is divided into units called genes.
Some genes control when your cells grow, divide into new cells, and die. Genes that help cells grow, divide, or stay alive are called oncogenes. Others that slow down cell division or cause cells to die at the right time are called tumor suppressor genes. Cancers can be caused by DNA changes that turn on oncogenes or turn off tumor suppressor genes. These gene changes can be inherited from a parent (as is sometimes the case with childhood cancers), or they may happen during a person’s lifetime as cells in the body divide to make new cells.
Changes in certain genes increase the chance that some kidney cells will remain in an early form and turn into a Wilms tumor.
For example, a small number of Wilms tumors are caused by changes (mutations) in or loss of the WT1 or WT2 genes, which are tumor suppressor genes found on chromosome 11. Changes in these genes and some other genes on chromosome 11 can lead to overgrowth of certain body tissues. This may explain why some other growth abnormalities.
Sometimes these gene changes are passed on from a parent to a child, but most Wilms tumors don’t seem to be caused by inherited gene mutations. Instead, they seem to result from gene changes that occur early in a child’s life, perhaps even before birth.
In a small number of Wilms tumors there is a change in a tumor suppressor gene known as WTX, which is found on the X chromosome. Another gene that is sometimes altered in Wilms tumor cells is known as CTNNB1. It’s not clear exactly what causes these genes to be altered.
Because the genes described above are not altered in all Wilms tumors, there must be gene changes that have not yet been found. In many cases, more than one gene change is involved.
Researchers now understand some of the gene changes that can occur in Wilms tumors, but it’s still not clear what causes these changes. Some gene changes can be inherited, but most Wilms tumors are not the result of known inherited syndromes. Other gene changes may just be random events that sometimes happen inside a cell, without having an outside cause. There are no known lifestyle-related or environmental causes of Wilms tumors, so it is important to know that there is nothing these children or their parents could have done to prevent these cancers.
Risk Factors for Wilms Tumor
A risk factor is anything that affects the chance of having a disease such as cancer. Different cancers have different risk factors.
Lifestyle-related risk factors such as body weight, physical activity, diet, and tobacco use play a major role in many adult cancers. But these factors usually take many years to influence cancer risk, and they are not thought to have much of an effect on the risk of childhood cancers, including Wilms tumors.
So far research has not found any strong links between Wilms tumor and environmental factors, either during a mother’s pregnancy or after a child’s birth.
Most Wilms tumors have no clear cause, but there are some factors that affect risk.
Age
Wilms tumors are most common in young children, with the average age being about 3 to 4 years. They are less common in older children, and rare in adults.
Race
In the United States, the risk of Wilms tumor is slightly higher in African-American children than in white children and is lowest among Asian-American children. The reason for this is not known.
Gender
Girls have a slightly higher risk of Wilms tumor than boys.
Family history of Wilms tumor
About 1% to 2% of children with Wilms tumors have one or more relatives with the same cancer. Scientists think that these children inherit chromosomes with an abnormal or missing gene from a parent that increases their risk of developing Wilms tumor. Surprisingly, the relative with Wilms tumor is not usually a parent.
Children with a family history of Wilms tumors are slightly more likely to have tumors in both kidneys. Still, in most children only one kidney is affected.
Certain genetic syndromes/birth defects
There is a strong link between Wilms tumors and certain kinds of birth defects. About 1 child in 10 with Wilms tumor also has birth defects. Most birth defects linked to Wilms tumors occur in syndromes. A syndrome is a group of symptoms, signs, malformations, or other abnormalities that occur together in the same person. Syndromes linked to Wilms tumor include:
WAGR syndrome
WAGR stands for the first letters of the physical and mental problems linked with this syndrome (although not all children have all of them):
- Wilms tumor
- Aniridia (complete or partial lack of the iris [colored area] of the eyes)
- Genitourinary tract abnormalities (defects of the kidneys, urinary tract, penis, scrotum, clitoris, testicles, or ovaries)
- Mental Retardation
Children with this syndrome have about a 30% to 50% chance of having a Wilms tumor. The cells in children with WAGR syndrome are missing part of chromosome 11, where the WT1 gene is normally found. Children with WAGR tend to get Wilms tumors at an earlier age and often have tumors in both kidneys.
Denys-Drash syndrome and Frasier syndrome
These rare syndromes have also been linked to changes (mutations) in the WT1 gene.
In Denys-Drash syndrome, the kidneys become diseased and stop working when the child is very young. Wilms tumors usually develop in the diseased kidneys. The reproductive organs don’t develop normally, and boys may be mistaken for girls. Because the risk of Wilms tumors is very high, doctors often advise removing the kidneys soon after this syndrome is diagnosed.
In Frasier syndrome the kidneys are also diseased, but they usually keep working into adolescence. As with Denys-Drash syndrome, the reproductive organs don’t develop normally. Children with Frasier syndrome are also at increased risk for Wilms tumors, although they are at even higher risk for cancers in the reproductive organs.
Beckwith-Wiedemann syndrome
Children with this syndrome tend to be big for their age. They also have larger than normal internal organs and often have an enlarged tongue. They may have an oversized arm and/or leg on one side of the body (called hemihypertrophy), as well as other medical problems. They have about a 5% risk of having Wilms tumors (or, less often, other cancers that develop during childhood). This syndrome is caused by a defect in chromosome 11 that affects the WT2 gene.
Other syndromes
Less often, Wilms tumor has been linked to other syndromes, including:
- Perlman syndrome
- Sotos syndrome
- Simpson-Golabi-Behmel syndrome
- Bloom syndrome
- Li-Fraumeni syndrome
- Trisomy 18
Certain birth defects
Wilms tumor is also more common in children with certain birth defects (without known syndromes):
- Aniridia (complete or partial lack of the iris [colored area] of the eyes)
- Hemihypertrophy (an oversized arm and/or leg on one side of the body)
- Cryptorchidism (failure of the testicles to descend into the scrotum) in boys
- Hypospadias (defect in boys where the urinary opening is on the underside of the penis)
Can Wilms Tumor Be Prevented?
The risk of many adult cancers can be reduced with certain lifestyle changes (such as staying at a healthy weight or quitting smoking), but at this time there are no known ways to prevent most cancers in children.
The only known risk factors for Wilms tumors (age, race, gender, and certain inherited conditions) can’t be changed. There are no known lifestyle-related or environmental causes of Wilms tumors, so at this time there is no way to protect against most of these cancers. Experts think these cancers come from cells that were in the fetus but failed to develop into mature kidney cells. This doesn’t seem to be caused by anything a mother could avoid during pregnancy.
In some very rare cases, such as in children with Denys-Drash syndrome who are almost certain to develop Wilms tumors, doctors may recommend removing the kidneys at a very young age (with a donor kidney transplant later on) to prevent tumors from developing.
Wilms tumor symptoms
Before being diagnosed with Wilms tumor, most children do not show any signs of having cancer, and usually act and play normally. Often, a parent may discover a firm, smooth lump in the child’s abdomen. It is not uncommon for the mass to grow quite large before it is discovered ― the average Wilms tumor is 1 pound at diagnosis.
Signs and Symptoms of Wilms Tumor
Swelling or a hard mass in the abdomen (belly): This is often the first sign of a Wilms tumor. Parents may notice this while bathing or dressing the child. It feels firm and is often large enough to be felt on both sides of the belly. It’s usually not painful, but it might cause belly pain in some children.
Other possible symptoms: Some children with Wilms tumor may also have:
- Fever
- Nausea
- Loss of appetite
- Shortness of breath
- Constipation
- Blood in the urine
Wilms tumors can also sometimes cause high blood pressure (hypertension). This does not usually cause symptoms on its own, but in rare cases blood pressure can get high enough to cause problems such as headaches, bleeding inside the eye, or even a change in consciousness.
Many of the signs and symptoms above are more likely to be caused by something other than a kidney tumor. Still, if your child has any of these symptoms, check with your child’s doctor so that the cause can be found and treated, if needed.
Even though Wilms tumors often are large when found, most have not spread to other areas of the body. This makes it easier to successfully treat than if the cancer cells have spread (metastasized) to other parts of the body.
Can Wilms Tumor Be Found Early?
Wilms tumors are usually found when they start to cause symptoms such as swelling in the abdomen (belly), but by this point they have often grown quite large. They can be found earlier in some children with tests such as an ultrasound of the abdomen. But because Wilms tumors are rare, it’s not practical to use ultrasound exams as a screening test (a test to look for disease in people with no signs or symptoms) in all children who are not at increased risk. There are no blood tests or other tests that are useful in screening otherwise healthy children for Wilms tumors.
On the other hand, screening for Wilms tumor is very important for children who have syndromes or birth defects known to be linked to this disease. For these children, most doctors recommend physical exams by a specialist and ultrasound exams on a regular basis (for example, about every 3 or 4 months at least until the age of 8) to find any kidney tumors when they are still small and have not yet spread to other organs.
Wilms tumor can also run in families, although this is rare. Talk to your doctor if you have any relatives who have had a Wilms tumor. If you do, the children in your family may need to have regular ultrasound exams of the abdomen. If a man or woman is known to have a WT1 gene mutation, testing can be done to see if they have passed the mutation on to their children. This can be done even before birth.
Wilms tumor diagnosis
Wilms tumors are usually found when a child is brought to a doctor because of symptoms he or she is having. The doctor might suspect a child has a Wilms tumor because of the physical exam or other test results, but the diagnosis can only be made for certain by taking out a small piece of the tumor and looking at it under a microscope.
Medical history and physical exam
If your child has signs or symptoms that suggest he or she may have a kidney tumor, the doctor will want to get a complete medical history to learn more about the symptoms and how long they have been there. The doctor may also ask if there’s a family history of cancer or birth defects, especially in the genitals or urinary system.
The doctor will examine your child for possible signs of a kidney tumor or other health problems. The focus will probably be on the abdomen (belly) and on any increase in blood pressure, which is another possible sign of a kidney tumor. Blood and urine samples might also be collected and tested.
Several tests are used to confirm a Wilms tumor diagnosis and determine the stage of the disease. Tests that might be used include:
- Ultrasonography (ultrasound or US), usually the first tool used to diagnose a Wilms tumor (or another type of tumor in the abdomen), uses sound waves instead of X-rays to generate an image of the area doctors wish to view. It’s also very useful when looking for tumor growing into the main veins coming out of the kidney. This can help in planning for surgery, if it’s needed.
- Computed tomography (CT or CAT scan) produces a detailed cross-sectional view of an organ through X-rays. It is extremely useful in detecting tumors and determining whether cancer has spread to other areas. It’s also helpful for checking whether a cancer has grown into nearby veins or has spread to organs beyond the kidney, such as the lungs. Your child will need to lie very still on a table while the scans are being done. Younger children may be given medicine to help keep them calm or even asleep during the test to help make sure the pictures are clear.
- Magnetic resonance imaging (MRI) uses radio waves and strong magnets to produce detailed pictures of the internal parts of the body. This provides more intricate images that allow doctors to see if the cancer has invaded any major blood vessels near the kidney. For example, it might be done if there’s a chance that a kidney tumor might have reached a major vein (the inferior vena cava) in the abdomen. An MRI scan might also be used to look for possible spread of cancer to the brain or spinal cord if doctors are concerned the cancer may have spread there. Your child may have to lie inside a narrow tube, which is confining and can be distressing. The test also requires a person to stay still for several minutes at a time. Younger children may be given medicine to help keep them calm or even asleep during the test.
- X-rays are used to look for any metastasized areas, especially in the lungs. This test might not be needed if a CT scan of the chest is done.
- Bone scans use small amounts of radioactive material to highlight areas of diseased bone, if any exist.
- Laboratory tests such as blood tests and urinalysis check the general health of a patient and to detect any adverse side effects (such as low red or white blood cell counts) of the treatment. A urine sample may be tested (urinalysis) to see if there are problems with the kidneys. Urine may also be tested for substances called catecholamines. This is done to make sure your child doesn’t have another kind of tumor called neuroblastoma. (Neuroblastomas often start in the adrenal glands, which are just on top of each kidney.)
- Kidney biopsy/surgery. Most of the time, imaging tests can give doctors enough information to decide if a child probably has a Wilms tumor, and therefore if surgery should be done. But the actual diagnosis of Wilms tumor is made when a small piece of the tumor is removed and checked under a microscope. The cells in Wilms tumors have a distinct appearance when looked at this way. Doctors also look at the sample to determine the histology of the Wilms tumor (favorable or unfavorable). In most cases, a sample is removed during surgery to treat the tumor. Sometimes if the doctors are less certain about the diagnosis or if they aren’t sure the tumor can be removed completely, a sample of the tumor may be taken during a biopsy as a separate procedure before surgery.
The chance of Wilms tumor being hereditary (“running in the family”) is so rare that there is no test to screen those who may pass the disease onto their offspring. However, certain genetic factors like birth defect syndromes can increase the likelihood of developing the disease. Those with a family history or personal history of Beckwith-Wiedemann syndrome (a condition associated with larger-than-normal internal organs), WAGR (marked by defects of the iris, kidneys, urinary tract, or genitalia), or Denys-Drash syndrome (a defect of the genitalia) are at risk.
Kids with risk factors for Wilms tumor should be screened for the disease through an ultrasound every 3 months until about age 6 or 7. Those at high risk may get undergo screening until they’re a little older.
Wilms tumor staging
The stage of a cancer describes how far it has spread. Your child’s treatment and prognosis (outlook) depend, to a large extent, on the cancer’s stage. Staging is based on the results of the physical exam and imaging tests (ultrasound, CT scans, etc.), as well as on the results of surgery to remove the tumor, if it has been done.
Children’s Oncology Group (COG) staging system
A staging system is a standard way for the cancer care team to sum up the extent of the tumor. In the United States, the Children’s Oncology Group staging system is used most often to describe the extent of spread of Wilms tumors. This system describes Wilms tumor stages using Roman numerals I through V (1 through 5).
Stage I
The tumor was contained within one kidney and was removed completely by surgery. The tissue layer surrounding the kidney (the renal capsule) was not broken during surgery. The cancer had not grown into blood vessels in or next to the kidney. The tumor was not biopsied before surgery to remove it.
About 40% to 45% of all Wilms tumors are stage I.
Stage II
The tumor has grown beyond the kidney, either into nearby fatty tissue or into blood vessels in or near the kidney, but it was removed completely by surgery without any apparent cancer left behind. Nearby lymph nodes (bean-sized collections of immune cells) do not contain cancer. The tumor was not biopsied before surgery.
About 20% of all Wilms tumors are stage II.
Stage III
This stage refers to Wilms tumors that may not have been removed completely. The cancer remaining after surgery is limited to the abdomen (belly). One or more of the following features may be present:
- The cancer has spread to lymph nodes in the abdomen or pelvis but not to more distant lymph nodes, such as those inside the chest.
- The cancer has grown into nearby vital structures so the surgeon could not remove it completely.
- Deposits of tumor (tumor implants) are found along the inner lining of the abdominal space.
- Cancer cells are found at the edge of the sample removed by surgery, a sign that some of the cancer still remains after surgery.
- Cancer cells “spilled” into the abdominal space before or during surgery.
- The tumor was removed in more than one piece – for example, the tumor was in the kidney and in the nearby adrenal gland, which was removed separately.
- A biopsy of the tumor was done before it was removed with surgery.
About 20% to 25% of all Wilms tumors are stage III.
Stage IV
The cancer has spread through the blood to organs away from the kidneys such as the lungs, liver, brain, or bones, or to lymph nodes far away from the kidneys.
About 10% of all Wilms tumors are stage IV.
Stage V
Tumors are found in both kidneys at diagnosis.
About 5% of all Wilms tumors are stage V.
Tumor histology
The other main factor in determining the prognosis and treatment for a Wilms tumor is the tumor’s histology, which is based on how the tumor cells look under a microscope. The histology can be either favorable or unfavorable (anaplastic).
Wilms tumor prognosis
Overall, about 9 of 10 children with Wilms tumor are cured. A great deal of progress has been made in treating this disease. Much of this progress in the United States has been because of the work of the National Wilms Tumor Study Group (now part of the Children’s Oncology Group), which runs clinical trials of new treatments for children with Wilms tumor. Today, most children with this cancer are treated in a clinical trial to try to improve on what doctors believe is the best treatment. The goal of these studies is to find ways to cure as many children as possible while limiting side effects by giving as little treatment as needed.
Because of major advances in treatment, most children treated for Wilms tumor are now surviving into adulthood. Doctors have learned that treatment can affect children’s health later in life, so watching for health effects as they get older has become more of a concern in recent years.
Just as the treatment of childhood cancer requires a very specialized approach, so does the care and follow-up after treatment. The earlier any problems can be recognized, the more likely it is they can be treated effectively. Young people treated for Wilms tumor are at risk, to some degree, for several possible late effects of their cancer treatment. It’s important to discuss what these possible effects might be with your child’s medical team so you know what to watch for and report to the doctor.
The risk of late effects depends on a number of factors, such as the specific treatments the child has, the doses of treatment, and the age of the child when being treated. These late effects may include:
- Reduced kidney function
- Heart or lung problems after getting certain chemotherapy drugs or radiation therapy to these parts of the body
- Slowed or delayed growth and development
- Changes in sexual development and ability to have children, especially in girls
- Increased risk of second cancers later in life (rare)
There may be other possible complications from treatment as well. Your child’s doctor should carefully review any possible problems with you before your child starts treatment.
Along with physical side effects, some childhood cancer survivors might have emotional or psychological issues. They might also have problems with normal functioning and school work. These can often be addressed with support and encouragement. If needed, doctors and other members of the health care team can recommend special support programs and services to help children after cancer treatment.
Long-term follow-up care
To help increase awareness of late effects and improve follow-up care of childhood cancer survivors throughout their lives, the Children’s Oncology Group (COG) has developed long-term follow-up guidelines for survivors of childhood cancers. These guidelines can help you know what to watch for, what type of screening tests should be done to look for problems, and how late effects can be treated.
Ask your child’s health care team about possible long-term complications and make sure there’s a plan in place to watch for these problems and treat them, if needed. To learn more, ask your child’s doctors about the COG survivor guidelines. You can also read them online at http://www.survivorshipguidelines.org. You may want to discuss them with your child’s doctor.
Wilms tumor survival rate
Survival rates are often used by doctors as a standard way of discussing a person’s prognosis (outlook). Some parents may want to know the survival statistics for children in similar situations, while others may not find the numbers helpful, or may even not want to know them. If you would rather not read about survival rates, don’t read any further.
The 4-year survival rate refers to the percentage of children who live at least 4 years after their cancer is diagnosed. Of course, many children live much longer than 4 years (and many are cured).
To get 4-year survival rates, doctors have to look at children who were treated at least 4 years ago. Improvements in treatment since then may result in a better outlook for children now being diagnosed with Wilms tumors.
These survival rates are based on the results of the National Wilms Tumor Studies, which included most of the children treated in the United States in the last few decades. The most important factors in determining a child’s outlook are the stage and histology of the tumor.
Some of these rates are based on only small numbers of children, so it’s hard to know if they are accurate.
Survival rates are based on previous outcomes of children who had the disease, but they can’t predict what will happen in any particular child’s case. Knowing the stage and histology of a Wilms tumor are important in estimating the child’s outlook. But other factors can also affect a child’s outlook, such as how well the tumor responds to treatment. Even when taking other factors into account, survival rates are only rough estimates. Your child’s doctor can tell you if the numbers below apply, as he or she knows your child’s situation best.
| Wilms Tumor 4-year Survival Rates | ||
| Tumor Stage | Favorable Histology | Unfavorable Histology (Anaplastic Wilms Tumor) |
| I | 99% | 83% |
| II | 98% | 81% |
| III | 94% | 72% |
| IV | 86% | 38% |
| V | 87% | 55% |
Wilms tumor treatment
Treatment is determined by many factors, the most important being the stage of the cancer at diagnosis, and the condition, or histology, of the cancer cells when observed under a microscope. “Favorable” histology is associated with a good chance of a cure; tumors with “unfavorable” histology are more aggressive and difficult to cure. About 95% of Wilms tumors have favorable histology.
Because Wilms tumors are rare, few doctors outside of those in children’s cancer centers have much experience in treating them. Children with Wilms tumors are treated with a team approach that includes the child’s pediatrician as well as specialists at a child’s cancer center. For Wilms tumors, the doctors on this team often include:
- A pediatric surgeon or pediatric urologist (doctor who treats urinary system problems in children [and genital problems in boys])
- A pediatric oncologist (doctor who uses chemotherapy and other medicines to treat childhood cancers)
- A pediatric radiation oncologist (doctor who uses radiation therapy to treat cancer in children)
Doctors use a staging system to describe the extent of a metastasized tumor. It is extremely useful in determining prognosis (possibility for a cure) and the best course of treatment. For example, a child with very aggressive disease should be given an intensive regimen of medication to achieve the best chance for a cure. A child with less-invasive disease should be given the least amount needed to reduce long-term side effects from toxicity.
The stages are:
- Stage I: Cancer is found in one kidney only and can be completely removed by surgery. About 41% of all Wilms tumors are stage I.
- Stage II: Cancer has spread beyond the kidney to the surrounding area, but can be completely removed by surgery. About 23% are stage II.
- Stage III: Cancer has not spread beyond the abdomen, but cannot be completely removed by surgery. About 23% are stage III.
- Stage IV: Cancer has spread to distant parts of the body; most commonly, the lungs, liver, bone, and/or brain. About 10% are stage IV.
- Stage V: Cancer is found in both kidneys at diagnosis (also called bilateral tumors). About 5% are stage V.
After your child’s tumor is found and its stage and histology are determined, the cancer care team will discuss treatment options with you. It’s important to discuss all of the options as well as their possible side effects with your child’s doctors so you can make an informed decision.
The main types of treatment for Wilms tumor are:
- Surgery
- Chemotherapy
- Radiation therapy
Most children will get more than one type of treatment.
In the United States, surgery is the first treatment for most Wilms tumors. In Europe, doctors often prefer to give a short course of chemotherapy before the surgery. There seems to be no difference in the results from these 2 approaches 2.
The first goal of treatment is to remove the primary (main) tumor, even if the cancer has spread to distant parts of the body. Sometimes the tumor might be hard to remove because it is very large, it has spread into nearby blood vessels or other vital structures, or it’s in both kidneys. For these children, doctors might use chemotherapy, radiation therapy, or a combination of the 2 to try to shrink the tumor(s) before surgery.
If any cancer is left after surgery, radiation therapy or more surgery may be needed.
Surgery is most often used to treat Wilms tumor. For stages I through IV, a radical nephrectomy ― removal of the cancer along with the entire kidney, ureter (tube that carries urine from the kidney to the bladder), adrenal gland (hormone-producing gland that sits on top of the kidney), and surrounding fatty tissue ― is done.
Since stage V patients have cancer involvement in both kidneys, removing both kidneys would result in kidney failure and the need for a kidney transplant. As a result, surgeons usually take out as much of the cancer as possible and preserve as much healthy kidney tissue as they can to avoid an organ transplant.
Surgery to remove all or part of a kidney
Treatment for Wilms’ tumor may begin with surgery to remove all or part of a kidney (nephrectomy). Surgery is also used to confirm the diagnosis — the tissue removed during surgery is sent to a lab to determine whether it’s cancerous and what type of cancer is in the tumor.
Surgery for Wilms’ tumor may include:
- Removing part of the affected kidney. Partial nephrectomy involves removal of the tumor and a small part of the kidney tissue surrounding it. Partial nephrectomy may be an option if the cancer is very small or if your child has only one functioning kidney.
- Removing the affected kidney and surrounding tissue. In a radical nephrectomy, doctors remove the kidney and surrounding tissues, including part of the ureter and sometimes the adrenal gland. Nearby lymph nodes also are removed. The remaining kidney can increase its capacity and take over the job of filtering the blood.
- Removing all or part of both kidneys. If the cancer affects both kidneys, the surgeon removes as much cancer as possible from both kidneys. In a small number of cases, this may mean removing both kidneys, and your child would then need kidney dialysis. If a kidney transplant is an option, your child would no longer need dialysis.
Chemotherapy
Chemotherapy uses powerful drugs to kill cancer cells throughout the body. Treatment for Wilms’ tumor usually involves a combination of drugs, given through a vein, that work together to kill cancer cells.
What side effects your child may experience will depend on which drugs are used. Common side effects include nausea, vomiting, loss of appetite, hair loss and higher risk of infections. Ask the doctor what side effects may occur during treatment, and if there are any potential long-term complications.
Chemotherapy may be used before surgery to shrink tumors and make them easier to remove. It may be used after surgery to kill any cancer cells that may remain in the body. Chemotherapy may also be an option for children whose cancers are too advanced to be removed completely with surgery.
For children who have cancer in both kidneys, chemotherapy is administered before surgery. This may make it more likely that surgeons can save at least one kidney in order to preserve kidney function.
Regardless of the stage and histology, all treatment plans usually include both surgery and chemotherapy, and the more advanced stages also may require radiation therapy. Chemotherapy uses drugs (administered either orally or intravenously) to enter the bloodstream, circulate throughout the body, and kill cancerous cells wherever they may be. Radiation uses high-energy X-ray beams to kill specific cells in different areas of the body.
Both treatments have short-term and long-term risks. Temporary or short-term discomfort may include nausea and vomiting, loss of appetite, mouth sores, fatigue, loss of hair, weakened immune system (leaving a patient vulnerable to infection), and bleeding or bruising.
Long-term effects may include the development of secondary cancers (like leukemia) or the weakening of some internal organs, such as the heart. However, these risks are minimal ― the benefits of treatment far outweighs potential risks.
Radiation therapy
Depending on the stage of the tumor, radiation therapy may be recommended. Radiation therapy uses high-energy beams to kill cancer cells.
During radiation therapy, your child is carefully positioned on a table and a large machine moves around your child, precisely aiming energy beams at the cancer. Possible side effects include nausea, diarrhea, tiredness and sunburn-like skin irritation.
Only a few centers in the United States, offer proton beam therapy — highly targeted precision beam therapy that destroys cancer while sparing healthy tissue.
Radiation therapy may be used after surgery to kill any cancer cells that weren’t removed during the operation. It may also be an option to control cancer that has spread to other areas of the body, depending on where the cancer has spread.
Clinical trials
Your child’s doctor may recommend participating in a clinical trial. These research studies allow your child a chance at the latest cancer treatments, but they can’t guarantee a cure.
Discuss the benefits and risks of clinical trials with your child’s doctor. The majority of children with cancer enroll in a clinical trial, if available. However, enrollment in a clinical trial is up to you and your child.
What Happens After Treatment for Wilms Tumor?
During and after treatment for Wilms tumors, the main concerns for most families are the short- and long-term effects of the tumor and its treatment, and concerns about the tumor still being there or coming back.
It’s certainly normal to want to put the tumor and its treatment behind you, and get back to a life that doesn’t revolve around cancer. But it’s important to realize that follow-up care is a central part of treatment that offers your child the best chance for long-term recovery.
Follow-up exams and tests
Your child’s health care team will set up a follow-up schedule, which will include physical exams and imaging tests (such as chest x-rays, ultrasounds, and CT scans) to look for the growth or return of the tumor, or any problems related to treatment.
Since most children have had a kidney removed, blood and urine tests will be done to check how well the remaining kidney is working. If your child received the drug doxorubicin (Adriamycin) during chemotherapy, the doctor may also order tests to check the function of your child’s heart.
The recommended schedule for follow-up exams and tests depends on the initial stage and histology (favorable or unfavorable) of the cancer, the type of treatment, and any problems that the child may have had during treatment. Doctor visits and tests will be more frequent at first (about every 6 to 12 weeks for the first couple of years), but the time between visits may be extended as time goes on.
During this time, it’s important to report any new symptoms to your child’s doctor right away, so that the cause can be found and treated, if needed. Your child’s doctor can give you an idea of what to watch for.
If the tumor does come back, or if it doesn’t respond to treatment, your child’s doctors will discuss the treatment options with you.
Children with bilateral Wilms tumors or Denys-Drash syndrome will also need regular tests to look for possible early signs of kidney failure (including urine tests, blood pressure checks, and blood tests of kidney function).
Caring for Your Child
As much as parents long to have their child out of the hospital, they often feel unsure of whether they can provide appropriate care after their child comes home. The doctors, nurses, and home health services should provide all the information and support needed to help a parent care for a child between hospital visits.
Depending on the treatment regimen (and a child’s general health and the doctor’s recommendations), appropriate at-home care can vary. Treatment for most children with Wilms tumor is not as intensive as treatment for other cancers (except for more advanced stages) so most kids won’t have tremendous restrictions on them.
Most kids undergoing treatment for Wilms don’t have special nutritional requirements or need medication for low blood cell counts, as most other cancer patients do. However, parents must watch for signs of distress, like fever, nausea, vomiting, or diarrhea. A child with a high fever should see a doctor right away.
Once a child is finished with therapy, the care team will provide a schedule of follow-up tests. Chest X-rays or CT scans may be taken every several months. Stage and histology of the cancer will determine the ultrasound schedule. Blood work and a physical exam may be required to check for adverse effects of the treatment.
For kids who relapse (the cancer returns), prognosis and treatment depend on their prior therapy, the cancer’s histology, and how long it’s been since the last treatment. The longer it’s been, the better. There are few late recurrences of Wilms tumor, so remaining cancer-free for at least 2 years after treatment is generally a very good sign.
Coping and support
Here are some suggestions to help you guide your family through cancer treatment.
At the hospital
When your child has medical appointments or stays in the hospital:
- Bring a favorite toy or book to office or clinic visits, to keep your child occupied while waiting.
- Stay with your child during a test or treatment, if possible. Use words that he or she will understand to describe what will happen.
- Include play time in your child’s schedule. Major hospitals usually have a playroom for children undergoing treatment. Often playroom staff members are part of the treatment team, with training in child development, recreation, psychology or social work. If your child must remain in his or her room, a child life specialist or recreational therapist may be available to make a bedside visit.
- Ask for support from clinic or hospital staff members. Seek out organizations for parents of children with cancer. Parents who have already been through this can provide encouragement and hope, as well as practical advice. Ask your child’s doctor about local support groups.
At home
After leaving the hospital:
- Monitor your child’s energy level outside of the hospital. If he or she feels well enough, gently encourage participation in regular activities. At times your child will seem tired or listless, particularly after chemotherapy or radiation, so make time for enough rest, too.
- Keep a daily record of your child’s condition at home — body temperature, energy level, sleeping patterns, drugs administered and any side effects. Share this information with your child’s doctor.
- Plan a normal diet unless your child’s doctor suggests otherwise. Prepare favorite foods when possible. If your child is undergoing chemotherapy, his or her appetite may dwindle. Make sure fluid intake increases to counter the decrease in solid food intake.
- Encourage good oral hygiene for your child. A mouth rinse can be helpful for sores or areas that are bleeding. Use lip balm to soothe cracked lips. Ideally, your child should have necessary dental care before treatment begins. Afterward check with your child’s doctor before scheduling visits to the dentist.
- Check with the doctor before any vaccinations, because cancer treatment affects the immune system.
- Be prepared to talk with your other children about the illness. Tell them about changes they might see in their sibling, such as hair loss and flagging energy, and listen to their concerns.