Contents
- What is seborrheic dermatitis
- Seborrheic dermatitis causes
- Seborrheic dermatitis pathophysiology
- Seborrheic dermatitis prevention
- Seborrheic dermatitis signs and symptoms
- Seborrheic dermatitis complications
- Seborrheic dermatitis diagnosis
- Seborrheic dermatitis differential diagnosis
- Seborrheic dermatitis treatment
- Seborrheic dermatitis prognosis
What is seborrheic dermatitis
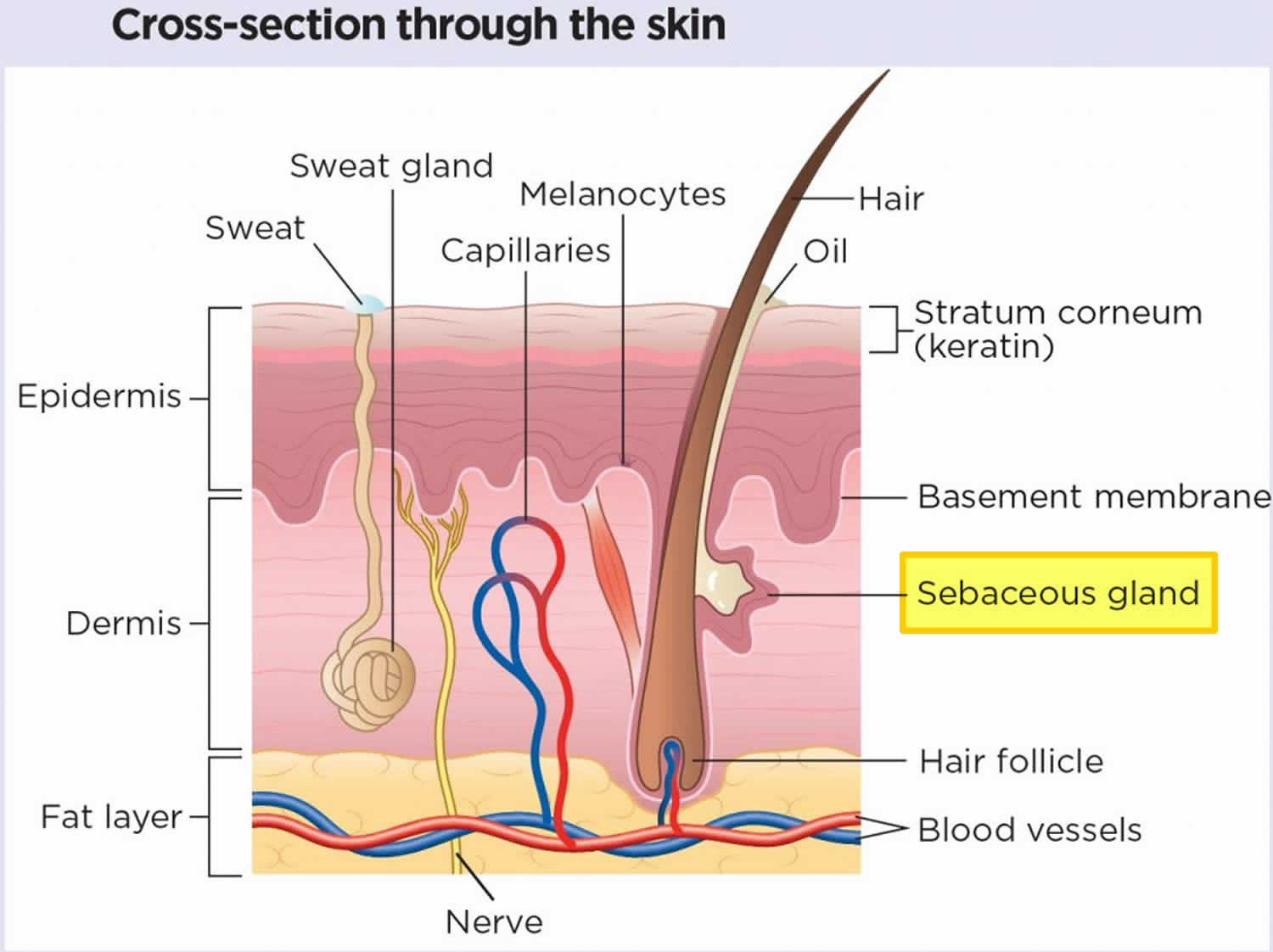
Seborrheic dermatitis also called seborrhoeic dermatitis or seborrheic eczema is a common, longterm (chronic) or relapsing form of dermatitis (inflammatory skin condition) or chronic form of eczema that mainly affects the sebaceous gland (oil-producing) rich regions of your body, including your scalp, face, eyebrows, eyelids, ears and trunk 1, 2, 3, 4. Seborrheic dermatitis appears as itchy red patches, greasy scales with white or yellow crusty or powdery flakes on your scalp and other parts of your body, but its not contagious. Seborrheic dermatitis can occur with or without redness. Its presence doesn’t mean the skin is unclean or infected. “Seborrheic” refers to the “sebaceous glands” while “dermatitis” means “inflammatory skin condition”. Sebaceous glands are microscopic oil glands found in your hair follicles that secrete sebum. Sebum is an oily substance that protects your skin from drying out. There are infantile and adult forms of seborrheic dermatitis. Seborrheic dermatitis on the scalp of teenagers or adults is called “dandruff” or “pityriasis capitis” and “cradle cap” when seborrheic dermatitis is on a baby’s scalp 5, 6. Dandruff presents as diffuse bran-like scaly patches within hair-bearing areas of the scalp without underlying redness. Dandruff may be asymptomatic or mildly itchy. Cradle cap (pityriasis capitis) is the common term for seborrheic dermatitis on the scalp of infants. Cradle cap is seen most commonly in infants aged between 3 weeks and 12 months with peak prevalence at 3 months of age 7. Seborrheic dermatitis is sometimes associated with psoriasis and is known as sebopsoriasis.
The exact cause of seborrheic dermatitis is unknown, but it may be due to an overproduction of skin oil combined with irritation from Malassezia yeast (sometimes called Pityrosporum ovale) which are normal skin organism of humans. The Malessezia overgrows and the immune system seems to overreact to it, leading to a fungal infection that results in skin changes. Factors that might increase your risk of seborrheic dermatitis include family history, stress, fatigue, use of alcohol-containing lotions, skin disorders, obesity, HIV, and certain neurologic conditions. In patients with HIVand AIDS, 35% of those with early HIV infection have seborrheic dermatitis, and 85% in patients with AIDS 8. Risk factors for seborrheic dermatitis include immunodeficiency, neurological diseases including Alzheimer’s disease and Parkinson disease, increased sebaceous gland activity, and exposures to drug treatment, including lithium, immunosuppressants, and dopamine antagonists 9.
Seborrheic dermatitis causes no serious harm to your skin, including your hair. Seborrheic dermatitis is a lifelong condition that appears, disappears with treatment, and flares up from time to time. In teenagers and adults, seborrheic dermatitis usually doesn’t disappear on its own without treatment. In adults, seborrheic dermatitis is frequently chronic and long-term maintenance treatment is often necessary. Cradle cap in infants usually takes a few weeks or months to disappear. If seborrheic dermatitis in babies persists beyond 12 months, the diagnosis should be reconsidered. The most common problems associated with both infant seborrheic dermatitis and adult seborrheic dermatitis relate to misdiagnosis of the condition 10.
Seborrheic dermatitis treatment depends on the area of your body that is affected and how severe your seborrheic dermatitis is. The goal of treatment is to reduce the visible signs of seborrheic dermatitis and itching and redness. Treatment includes use of over-the-counter (OTC) products and prescription medications. Prescription drugs include topical antifungals, calcineurin inhibitors and corticosteroids. Ongoing maintenance treatment is often needed. You may need to use a combination of these treatments:
- Scalp treatment
- Cradle cap (infants). Cradle cap usually clears up without treatment when the child is between eight and 12 months old. It may be treated daily with a mild baby shampoo. Massage or brush the scalp with a soft brush several times a day and after each shampoo. Sorbolene cream or lotion and a soft-bristled toothbrush can soften and remove the cradle cap scales. Be careful not to cause a break in the skin, which can lead to infection. If the cradle cap continues, or the baby seems uncomfortable and scratches the scalp, contact your pediatrician or dermatologist. He or she may prescribe a prescription shampoo or lotion. Other areas of affected skin may be treated with a gentle steroid lotion.
- Adolescents and adults. For mild cases, look for over-the-counter dandruff shampoos that contain selenium, zinc pyrithione, ketoconazole, salicylic acid or coal tar. Shampoo with it twice a week or as directed on the label of the product. For long-term control, your doctor may prescribe antifungal shampoos that contain ciclopirax (Loprox) or ketoconazole (Nizoral). These shampoos are used from daily to two or three times a week for several weeks until the dandruff has cleared, then once every week to two weeks to prevent flare-ups. Your doctor will give you specific directions for use.
- For moderate to severe cases, your doctor may prescribe a shampoo containing betamethasone valerate (Luxiq), clobetasol (Clobex), fluocinolone (Capex) or fluocinolone solution (Synalar). Shampoo your hair as directed. Some products are used daily, others are used twice daily for two weeks then two times a week.
- Ask your skin doctor about what side effects to watch for while using these shampoos.
- Face and Body treatment
- Treatments for seborrheic dermatitis of the face and body include topical antifungals, corticosteroids and calcineurin inhibitors.
- Topical antifungals include ciclopirox, ketoconazole or sertaconazole. These products, available in creams, foams or gels, are usually applied to the affected areas twice daily for up to eight weeks and then as needed.
- Topical corticosteroids include betamethasone valerate, desonide, fluocinolone or hydrocortisone. These products come in creams, lotions, foams, gels, ointments, oil or solution. They are taken once or twice a day. Your skin doctor might prescribe these products if antifungal products aren’t successful in clearing your seborrheic dermatitis or for treating flare-ups. Corticosteroids can cause a thinning of your skin and should not be used continuously for weeks and months at a time without a break.
- Topical calcineurin inhibitors are an alternative to corticosteroids. These products include pimecrolimus cream (Elidel) or tacrolimus ointment (Protopic). They are applied to the affected area twice daily.
- If your seborrheic dermatitis is severe, your skin specialist may prescribe an oral (pill) antifungal agent or phototherapy (a specific wavelength of ultraviolet light to decrease inflammation in the skin).
- Treatments for seborrheic dermatitis of the face and body include topical antifungals, corticosteroids and calcineurin inhibitors.
Ask your skin specialist about the side effects of these medications and what to watch for. Follow your skin doctor’s instructions about how to take these medications. You and your skin specialist will work closely together to select products and develop a treatment plan that will be most helpful to treat your unique case of seborrheic dermatitis.
Figure 1. Skin anatomy
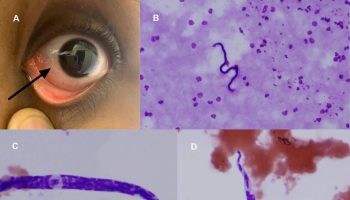
Figure 2. Seborrheic dermatitis face
Figure 3. Seborrheic dermatitis scalp
Figure 4. Seborrheic dermatitis newborn
Figure 5. Seborrheic dermatitis hairline
Figure 6. Seborrheic dermatitis nose
Figure 7. Seborrheic dermatitis eyebrows
Figure 8. Seborrheic dermatitis beard
Who gets seborrheic dermatitis?
Seborrheic dermatitis is a common benign and noncontagious inflammatory skin condition that affects 3% to 12% of the population. Seborrheic dermatitis affects approximately 5% of the global population, while its noninflammatory form affects closer to 50% of individuals 11. Seborrheic dermatitis prefers males of all ethnicities and peaks in the first 3 months of life and again at puberty, where it then reaches an apex at 40-60 years and later declines 12, 13, 14:
- Infantile seborrheic dermatitis also called cradle cap affects babies under the age of 3 months and usually resolves by 6-12 months of age. Infants are usually extensively affected by seborrheic dermatitis (cradle cap), which often appears as firm, greasy scales on the crown and frontal regions of the scalp that can cause significant parental anxiety.
- Adult seborrheic dermatitis tends to begin in late adolescence. Prevalence is greatest in young adults and in older people. Adult seborrheic dermatitis is more common in males than in females. Adult seborrheic dermatitis is characterized by a relapsing and remitting pattern of disease and is ranked third behind atopic and contact dermatitis for its potential to impair patients’ quality of life 15.
Seborrheic dermatitis often occurs in otherwise healthy patients. However, the following factors are sometimes associated with severe adult seborrheic dermatitis 6:
- Oily skin (seborrhea)
- Familial tendency to seborrheic dermatitis or a family history of psoriasis
- Immunosuppression: organ transplant recipients, human immunodeficiency virus (HIV) infection, and patients with lymphoma
- Neurological and psychiatric diseases: Parkinson’s disease, tardive dyskinesia, depression, epilepsy, facial nerve palsy, spinal cord injury, and congenital disorders such as Down syndrome
- Use of neuroleptic medications
- Treatment for psoriasis with psoralen and ultraviolet A (PUVA) therapy
- Lack of sleep, and stressful events.
What’s the difference between seborrheic dermatitis and psoriasis?
Psoriasis and seborrheic dermatitis can mimic each other. Psoriasis is an inflammatory skin disease that affects 2% to 4% of the population. Psoriasis and seborrheic dermatitis can have patches of red skin with flakes. Both can be found on your scalp and back. The scales of psoriasis are often thicker than that of seborrheic dermatitis. The edges of those scales are very well-defined. On the scalp, psoriasis scales are closer to a silver color than white or yellow. There is a condition called sebopsoriasis where seborrheic dermatitis and psoriasis overlap. In that case you have the symptoms of both: both white flakes and silver flakes, both on the scalp or back, both itchy.
If you’re concerned about whether you have psoriasis or seborrheic dermatitis, consult your doctor.
Your skin doctor (dermatologist) will likely be able to tell you if you have scalp psoriasis, seborrheic dermatitis or both by looking at your skin, scalp and nails.
Scalp psoriasis and seborrheic dermatitis are common conditions that affect the scalp. And they share some symptoms, such as inflamed, scaly skin.
Most often, the scales of psoriasis look thicker and drier than the scales of seborrheic dermatitis. Psoriasis tends to extend beyond the hairline. And psoriasis usually affects more than one area of the body. If you have scalp psoriasis, you may have mild psoriasis on your elbows, knees or lower back too. Or you may notice nail changes, such as pitting.
- Scalp psoriasis
- Inflamed skin covered with scales or with oily, crusted patches called plaques
- Patches that may extend beyond the hairline or appear on other parts of the body
- Itching
- Seborrheic dermatitis of the scalp
- Inflamed skin covered with scales or crusted patches
- Skin flakes, called dandruff, on the scalp and hair
- Itching
Scalp psoriasis and seborrheic dermatitis of the scalp share some similar treatments, including medicated shampoos and corticosteroid lotions. Scalp psoriasis is often persistent and more difficult to treat than is seborrheic dermatitis of the scalp. Other treatments, such as light therapy, may be needed to help control psoriasis.
Does the weather make seborrheic dermatitis worse?
Dry air during the winter months will make your seborrheic dermatitis worse. Seborrheic dermatitis behaves best during the summertime. The sun’s UV-A and UV-B light have been shown to kill the type of yeast that overgrows on the skin of people who get seborrheic dermatitis.
Do certain foods trigger or reduce seborrheic dermatitis?
Although there are theories out there, experts have yet to find that food causes or reduces seborrheic dermatitis. Diet high in fruit intake is associated with less seborrheic dermatitis whereas stress may precipitate flare-ups. This study found that patients with higher fruit intake had a decreased likelihood of seborrheic dermatitis 16. These results align with research on other inflammatory skin diseases, including eczema incidence, which is negatively associated with increased fruit intake 17. Fruits contain high levels of vitamins and flavonoids, which reduce inflammation and may modulate the inflammatory response in seborrheic dermatitis that contributes to skin barrier dysfunction 17.
Does seborrheic dermatitis cause hair loss?
No, seborrheic dermatitis does not cause hair loss (alopecia). Hair loss is not a symptom of seborrheic dermatitis and if you are experiencing hair loss, you probably have a different underlying condition.
Seborrheic dermatitis and acne can appear at the same time, in the same places on your body. Both are affected by oils in your skin. People who have acne are more likely to have dandruff.
Seborrheic dermatitis causes
There are multiple factors associated with the development of seborrheic dermatitis, but its exact cause is not completely understood 14. The onset of seborrheic dermatitis appears linked to the interplay of normal microscopic skin flora especially Malassezia yeast also called Pityrosporum ovale (Malassezia yeast are basidiomycetous yeasts that form part of the normal skin flora of humans), the composition of oil on the skin surface, problem with your immune system and individual susceptibility e.g. hormone levels (andoregens and adrenal corticosteroids), fungal infections, nutritional deficits, neurogenic factors 18, 19, 13. Neither the level of sebum produced nor the amount of yeast appears to be significant factors 20. Several studies suggest that nutrition can influence other inflammatory skin diseases, such as acne vulgaris, hidradenitis suppurativa, and psoriasis 21, 22, 23. Therefore obesity (BMI 30 or higher) and nutrition may play a role in influencing the seborrheic dermatitis clinical course 24, 25, 26, 1. Numerous inflammatory markers are higher in those with obesity, which may contribute to initiating or aggravating seborrheic dermatitis 27. Abdominal obesity can also lead to dyslipidemia, another factor associated with seborrheic dermatitis 24, 25, 28.
If you are born with naturally oily skin, you are more likely to get seborrheic dermatitis. Overgrowth of Malassezia yeast (Pityrosporum ovale), which is present on everyone’s skin, is believed to play a role. The lipases and phospholipases produced by Malassezia yeast cleave free fatty acids from triglycerides present in sebum. This may induce inflammation 14. Differences in skin barrier lipid content and function may account for individual presentations 14.
Other factors that trigger or worsen seborrheic dermatitis include:
- Stress.
- Cold and dry climate.
- Oily skin.
- An increased level of androgens (a hormone).
- Using alcohol-based lotions.
- History of other skin disorders, including rosacea, psoriasis and acne.
- A history of psoriasis or dermatitis in your family makes you vulnerable as well.
If you have other health issues, you’re more prone to seborrheic dermatitis:
- Immunosuppressions
- Organ transplant recipients.
- Adult Hodgkin’s Lymphoma.
- Adult Non-Hodgkin’s Lymphoma.
- HIV (human immunodeficiency virus).
- Psychiatric disorders
- Depression.
- Neurological diseases
- Parkinson’s disease.
- Tardive dyskinesia.
- Epilepsy.
- Facial nerve palsy.
- Spinal cord injury.
- Congenital disorders
- Down syndrome.
You’re also more prone to seborrheic dermatitis if you take these psychotropic medications 14:
- Lithium.
- Buspirone.
- Haloperidol decanoate.
- Chlorpromazine.
Risk factors for seborrheic dermatitis
Risk factors for the development of seborrheic dermatitis include 14:
- Age. Seborrheic dermatitis occurs most often in infants younger than 3 months old and in adults ages 30 to 60.
- Male sex. Seborrheic dermatitis is more common in men than in women, and in Caucasians more than African Americans.
- Stress. Stress relief is often the lifestyle change which will have the biggest impact on seborrheic dermatitis.
- Recovery from stressful medical conditions, such as a heart attack.
- Fatigue or tiredness
- A change of season
- Increased sebaceous gland activity
- Immune system disorders 29:
- Lymphoma
- Organ transplant recipients
- Kidney transplantation
- HIV-AIDS
- Neurological and psychiatric diseases 30:
- Parkinson disease 31
- Stroke
- Alzheimer’s disease
- Major depression
- Tardive Dyskinesia
- Epilepsy
- Facial nerve palsy
- Spinal cord injury
- Autonomic dysfunction
- Exposure to certain drugs:
- Dopamine antagonists
- Immunosuppressants
- Psoralen and psoralen plus ultraviolet A (PUVA)
- Lithium
- Buspirone
- Haloperidol decanoate
- Chlorpromazine
- Low ambient humidity and low ambient temperature
Seborrheic dermatitis pathophysiology
The proposed mechanisms for the pathogenesis of seborrheic dermatitis include 14:
- Disruption of the skin’s microbiota
- An impaired immune reaction to Malassezia species associated with a diminished T-cell response and activation of complement
- The increased presence of unsaturated fatty acids on the skin surface
- Disruption of cutaneous neurotransmitters
- Abnormal shedding of keratinocytes
- Epidermal barrier disturbances associated with genetic factors 32
The role of Malassezia species (Pityrosporum ovale) also includes the degradation of sebum and consumption of saturated fatty acids, disrupting the lipid balance on the skin surface 33. Further evidence for the involvement of Malassezia species (Pityrosporum ovale) includes their isolation from seborrheic dermatitis lesions and the significant resolution of seborrheic dermatitis with antifungal treatment 14.
Seborrheic dermatitis prevention
Because the exact cause of seborrheic dermatitis is not completely understood, there’s little that can be done to prevent it. Cradle cap is a natural, harmless condition. It can be simply treated at home. If you are a teenager or an adult with seborrheic dermatitis, you might be more prone if you have higher than normal levels of androgens (male sex hormones), a higher level of lipids in your skin or have an overgrowth of the yeast that is always present on your skin’s surface.
Some simple healthy things you can do to reduce your risk of developing seborrheic dermatitis include getting plenty of rest, controlling your emotional stress and getting a daily small doses (minutes) of sunshine (UV light). Stay away from the midday sun.
Always follow your doctor’s instructions for using medicated shampoos and skin products. Under treatment or inappropriate treatment can result in flare-ups of your seborrheic dermatitis.
Seborrheic dermatitis signs and symptoms
Seborrheic dermatitis can occur in areas of your body with the most sebaceous (oil) gland activity: your upper back and chest, face/forehead, the creases at the base of your nose, behind your ears, navel (belly button), eyebrows, under your breasts and in the creases/bends of your arms, legs and groin.
Seborrheic dermatitis signs and symptoms may include:
- Itchy white flakes of skin on your scalp (dandruff) on your scalp, hair, eyebrows, beard or mustache. When scratched, the flakes come loose, mix in with your hair, or fall onto your neck and shoulders.
- Patches of greasy skin covered with flaky white or yellow scales or crust on the scalp, face, sides of the nose, eyebrows, ears, eyelids, chest, armpits, groin area or under the breasts
- Red scales on your skin.
- Crusty yellow scales on infants’ heads (cradle cap). Cradle cap shouldn’t itch, but scratching may cause additional inflammation in the area and break the skin, leading to bleeding or mild infections.
- Blepharitis (scaly redness on the edges of your eyelids).
- Pinkish plaques (thick skin) of scales on both sides of your face.
- Flaky patches on your chest and at your hairline that are shaped like a flower petal or a ring.
- Redness in the folds and creases of your genitals, armpits and beneath your breasts.
- Inflamed hair follicles on your cheeks and the upper half of your trunk.
- Rash that may look darker or lighter in people with brown or Black skin and redder in those with white skin.
- Ring-shaped (annular) rash, for a type called petaloid seborrheic dermatitis.
- Itchiness (pruritus)
Usually, one or two areas of your skin are involved, but seborrheic dermatitis can be extensive, involving:
- Scalp: On the scalp it can range from a mild flaking of the skin (dandruff) to inflamed, scaly areas, which can sometimes weep.
- Face: Typically, the skin around the sides of the nose and in the creases, and sometimes the cheeks, can become red or lighter or darker than the surrounding skin (depending on your skin tone), and scaly. The inner half of the eyebrows can develop ‘dandruff’. Sometimes the eyelids and eyelashes become involved, a condition known as ‘blepharitis’.
- Ears: Seborrheic dermatitis may occur around the ears. Eczema can occur in the ear canal (otitis externa), on the earlobe or behind the ears.
- Generalized: Very rarely, seborrheic dermatitis can become severe and extensive, covering large areas of the body and needing more aggressive management.
The signs and symptoms of seborrheic dermatitis tend to flare with stress, fatigue or a change of season.
Infant seborrheic dermatitis
Infant seborrheic dermatitis causes cradle cap (diffuse, greasy scaling on the scalp). The rash may spread to affect armpit and groin folds (a type of napkin dermatitis). There are salmon-pink patches that may flake or peel. Children with darker skin types often do not experience the classic cradle cap appearance of seborrheic dermatitis, but instead have redness, flaking, and hypopigmentation of the affected areas and folds of skin.
Infant seborrheic dermatitis is not especially itchy, so the baby often appears undisturbed by the rash, even when generalized.
Adult seborrheic dermatitis
Seborrheic dermatitis commonly affects areas of the skin with high sebum production, such as the scalp, nasolabial folds, glabella, eyebrows, beard, ears, retroauricular skin, sternum, and other skin folds.
Seborrheic dermatitis typical features include:
- Winter flares, improving in summer following sun exposure
- Minimal itch most of the time
- Combination oily and dry mid-facial skin
- Ill-defined localised scaly patches or diffuse scale in the scalp
- Blepharitis: scaly red eyelid margins
- Salmon-pink, thin, scaly, and ill-defined plaques in skin folds on both sides of the face
- Petal or ring-shaped flaky patches on the hairline and on anterior chest
- Rash in the armpits, under the breasts, in the groin folds, and genital creases
- Malassezia folliculitis (inflamed hair follicles) on the cheeks and upper trunk.
People of darker skin may present with scaly hypopigmented macules and patches in typical areas of involvement. Arcuate or petal-like patches may be seen, termed petaloid seborrheic dermatitis 6.
Extensive seborrheic dermatitis affecting the scalp, neck, and trunk is sometimes called pityriasiform seborrhoeide 6.
Seborrheic dermatitis complications
Seborrheic dermatitis usually takes a benign course, and serious complications are very rare.
Seborrheic dermatitis complications may include 6:
- Secondary bacterial or fungal infection
- Skin thinning, dilated blood vessels, and steroid-induced telangiectasia
- Psychosocial impact due to appearance of skin.
The intertriginous areas (areas between skin folds) and eyelids are prone to secondary bacterial infections, especially during acute flares, and the diaper region is particularly prone to overgrowth with Candida fungus.
Erythroderma (inflammatory skin disease with redness and scaling) has been reported in immunosuppressed babies with generalized infant seborrheic dermatitis, but it is more frequently a feature in adults seborrheic dermatitis with HIV-AIDS 14. However, research has not firmly established that seborrheic dermatitis causes erythroderma per se, given its preference for sebaceous-rich skin 30, 34.
Seborrheic dermatitis diagnosis
The diagnosis of seborrheic dermatitis is a clinical diagnosis based on the location where it appears on your body, appearance on the affected skin and behaviour of the lesions. No blood, urine or allergy tests are needed, but HIV serology should be checked in cases of severe seborrheic dermatitis, especially where the onset is sudden 35. Your dermatologist may perform a skin biopsy to rule out other diseases if your condition does not respond to treatment. Because some medications can trigger or worsen seborrheic dermatitis, your medications require a review as well.
The following tests may be helpful in the diagnosis of seborrheic dermatitis and its associated pathologies 14:
- Potassium hydroxide (KOH) examination of skin scrapings
- Swab for microscopy, culture, and sensitivities. As Malassezia yeast are a normal component of skin flora, their presence on microscopy of skin scrapings is not diagnostic.
- Histology and direct immunofluorescence
- HIV serology; Venereal Disease Research Laboratory (VDRL)
- Serum zinc levels
- Antinuclear antibodies (ANA); extractable nuclear antigens (ENA); erythrocyte sedimentation rate (ESR)
Histopathology
The dermatopathology of seborrheic dermatitis is nonspecific, but the surface and infundibular epidermis usually show a superficial perivascular infiltrate of lymphocytes, acanthosis, focal spongiosis, and focal parakeratosis 33, 36. “Shoulder parakeratosis” refers to scale-crust accumulation around the infundibular ostia, which is appreciated in patients. Malassezia species may be present in the stratum corneum.
Histological progression from acute to chronic seborrheic dermatitis characteristically demonstrates a transition from spongiosis to psoriasiform hyperplasia and the development of a lichenoid lymphocytic infiltrate 14. Severe seborrheic dermatitis is often associated with keratinocyte necrosis, focal interface destruction, and leukocytoclasia.
Seborrheic dermatitis differential diagnosis
Adult seborrheic dermatitis differential diagnosis include 14:
- Scalp
- Psoriasis: Mostly not itchy and tends to affect the back of the head (occipital) and the front of the head (frontal), whereas seborrheic dermatitis tends to affect the crown or highest point of the head (vertex) and temple (parietal) regions
- Contact eczema (contact dermatitis): Due to the use of different shampoos and hair dye
- Darier disease: Yellowish-brown clusters of rough dome-shaped papules in seborrheic distribution; acanthosis; peculiar odor
- Face
- Psoriasis: Rarely occurs in isolation; pitted nails
- Lupus erythematosus (LE): Discoid lupus erythematosus is associated with skin atrophy and scarring hair loss
- Rosacea: Look for erythema and telangiectasia; may cause meibomianitis along the posterior lid line
- Acne vulgaris: Look for comedones (hallmark feature)
- Staphylococcal blepharitis (anterior lash line)
- Contact eczema (contact dermatitis): Eyelids commonly involved (versus irritant eczema [dry, scaly skin] or allergic eczema [swollen, vesicular skin rash])
- Darier disease: Nail changes
- Trunk
- Psoriasis: Sharply-defined red plaques with a loose, silvery lamella scale
- Pityriasis rosea: Herald spot; collarette scale; Christmas tree distribution
- Pityriasis versicolor: Not symmetrical; hypo- or hyperpigmentation
- Subacute lupus erythematosus: Photosensitive distribution
- Nummular eczema: Intense itch
- Tinea corporis: Raised leading edges and central clearing; uncommon in infants
- Erythema annulare centrifugum: Recurrent polycyclic lesions that slowly expand and disappear
- Darier’s disease: Greasy wart-like papules and plaques
- Grover’s disease (transient acantholytic dermatosis): Acanthosis
- Drug reaction: Drug history (neuroleptic; immunosuppressant; PUVA; lithium)
- Parapsoriasis: Elderly; very slow growing; resistant to treatment
- Pemphigus foliaceus: Fragile, painful blisters; Nikolsky sign is positive
- Secondary syphilis: Lesions on the palms and soles; a history of chancre
- Intertriginous areas (areas where two skin areas may touch or rub together i.e., armpit of the arm, the anogenital region, skin folds of the breasts and between fingers and toes)
- Psoriasis (inverse): Sharply-defined border
- Contact eczema (contact dermatitis): Itchy; vesicular
- Tinea cruris: Advancing border; very uncommon in infants
- Erythrasma: Coral-red fluorescence under Wood Lamp
- Candidiasis: Satellite lesions; obesity; a history of immunodeficiency
- Hailey-Hailey disease (familial benign pemphigus): Acanthosis
Infant seborrheic dermatitis differential diagnosis include 14:
- Cradle cap
- Tinea capitis: Look for broken hairs or “black dots”; very uncommon in adults
- Impetigo: Yellow, honey-colored crusting
- Diaper region
- Irritant contact dermatitis: Tends to spare the skin folds
- Candidiasis: Either secondary or from colonization with fecal yeast; look for satellite lesions
- Infantile psoriasis: Sharply-defined red plaques with silver scale
- Histiocytosis X (Langerhans cell histiocytosis): Tends to be confined to the skin folds with a purpuric rash on the body
- Acrodermatitis enteropathica: Look for periorificial involvement and check zinc levels
Seborrheic dermatitis treatment
Seborrheic dermatitis treatment varies according to the your age, the area of your body that is affected, the distribution and severity your seborrheic dermatitis. The goal of treatment is to reduce the visible signs of seborrheic dermatitis and itching and redness. Treatment includes use of over-the-counter (OTC) products and prescription medications. Prescription drugs include topical antifungals, calcineurin inhibitors and corticosteroids. Ongoing maintenance treatment is often needed. Furthermore, treatment rotation may be more effective and associated with fewer adverse reactions than persisting with monotherapy 14.
For adolescents and adults, the main treatments for seborrheic dermatitis are medicated shampoos, creams and lotions. If nonprescription products and self-care habits don’t help, your doctor might suggest that you try one or more of these treatments:
- Scalp treatment
- Cradle cap (infants). Cradle cap usually clears up without treatment when the child is between eight and 12 months old. It may be treated daily with a mild baby shampoo. Massage or brush the scalp with a soft brush several times a day and after each shampoo. Sorbolene cream or lotion and a soft-bristled toothbrush can soften and remove the cradle cap scales. Be careful not to cause a break in the skin, which can lead to infection. If the cradle cap continues, or the baby seems uncomfortable and scratches the scalp, contact your pediatrician or dermatologist. He or she may prescribe a prescription shampoo or lotion. Other areas of affected skin may be treated with a gentle steroid lotion.
- Adolescents and adults. For mild cases, look for over-the-counter dandruff shampoos that contain selenium, zinc pyrithione or coal tar. Shampoo with it twice a week or as directed on the label of the product. For long-term control, your doctor may prescribe antifungal shampoos that contain ciclopirax (Loprox) or ketoconazole (Nizoral). These shampoos are used from daily to two or three times a week for several weeks until the dandruff has cleared, then once every week to two weeks to prevent flare-ups. Your doctor will give you specific directions for use.
- For moderate to severe cases, your doctor may prescribe a shampoo containing betamethasone valerate (Luxiq), clobetasol (Clobex), fluocinolone (Capex) or fluocinolone solution (Synalar). Shampoo your hair as directed. Some products are used daily, others are used twice daily for two weeks then two times a week.
- Ask your skin doctor about what side effects to watch for while using these shampoos.
- Face and Body treatment
- Treatments for seborrheic dermatitis of the face and body include topical antifungals, corticosteroids and calcineurin inhibitors.
- Topical antifungals include ciclopirox, ketoconazole or sertaconazole. These products, available in creams, foams or gels, are usually applied to the affected areas twice daily for up to eight weeks and then as needed.
- Topical corticosteroids include betamethasone valerate, desonide, fluocinolone or hydrocortisone. These products come in creams, lotions, foams, gels, ointments, oil or solution. They are taken once or twice a day. Your skin doctor might prescribe these products if antifungal products aren’t successful in clearing your seborrheic dermatitis or for treating flare-ups. Corticosteroids can cause a thinning of your skin and should not be used continuously for weeks and months at a time without a break.
- Topical calcineurin inhibitors are an alternative to corticosteroids. These products include pimecrolimus cream (Elidel) or tacrolimus ointment (Protopic). They are applied to the affected area twice daily.
- If your seborrheic dermatitis is severe, your skin specialist may prescribe an oral (pill) antifungal agent or phototherapy (a specific wavelength of ultraviolet light to decrease inflammation in the skin).
- Treatments for seborrheic dermatitis of the face and body include topical antifungals, corticosteroids and calcineurin inhibitors.
In 2023, the FDA approved Roflumilast (Zoryve foam 0.3%), a topical, non-steroidal PDE4 inhibitor (phosphodiesterase inhibitor) available for the treatment of seborrheic dermatitis in patients 9 years of age and older. Roflumilast (Zoryve) is also available as a cream (0.15%) for the treatment of mild to moderate atopic dermatitis in adults and children ages 6 years and older.
Ask your skin specialist about the side effects of these medications and what to watch for. Follow your skin doctor’s instructions about how to take these medications. You and your skin specialist will work closely together to select products and develop a treatment plan that will be most helpful to treat your unique case of seborrheic dermatitis.
Seborrheic dermatitis medication
Treatment of seborrheic dermatitis often involves several of the following medications:
- Keratolytics: used to remove scale when necessary, e.g. salicylic acid, lactic acid, urea, propylene glycol.
- Topical antifungal agents: applied to reduce Malassezia yeast e.g. ketoconazole, or ciclopirox shampoo and/or cream. Note, some strains of Malassezia are resistant to azole antifungals. Try zinc pyrithione or selenium sulphide.
- Mild topical corticosteroids: for 1–3 weeks to reduce the inflammation of an acute flare.
- Topical calcineurin inhibitors: Pimecrolimus cream, tacrolimus ointment are indicated if topical corticosteroids are needing to be used frequently, as they have fewer side effects on facial skin with long term use.
Topical Creams, Ointments, and Lotions
- 2% salicylic acid + 2% sulfur in sorbolene cream or emulsifying ointment 37
- 2% ketoconazole cream
- 1% clotrimazole + 1% hydrocortisone cream
- 10% sulfacetamide + 5% sulfur lotion 38
- Betamethasone dipropionate 0.05% lotion
- 0.03% and 0.1% tacrolimus ointment
Shampoos
- 1% zinc pyrithione
- 1% to 2.5% selenium sulfide
- 2% ketoconazole
- 1% ciclopirox
- 5% coal tar + 2% salicylic acid
- 0.1% and 0.03% tacrolimus
Oral Anti-fungal Medications
- Itraconazole
- Fluconazole
- Terbinafine
In resistant cases in adults, oral itraconazole, tetracycline antibiotics, or phototherapy may be recommended. Low-dose oral isotretinoin has also been shown to be effective for severe or moderate disease.
In 2023, the FDA approved Roflumilast (Zoryve foam 0.3%), a topical, non-steroidal PDE4 inhibitor (phosphodiesterase inhibitor) available for the treatment of seborrheic dermatitis in patients 9 years of age and older. Roflumilast (Zoryve) is also available as a cream (0.15%) for the treatment of mild to moderate atopic dermatitis in adults and children ages 6 years and older.
If you’re considering over the counter treatment or prescription medications, you will want to discuss the best path with your doctor or skin doctor. It might also be a good idea to discuss any lifestyle changes or skin and hair products with your doctor before taking them.
You should see a dermatologist if your symptoms get worse or you experience a flare-up. Your skin doctor may need to change your dosage, add a different medication to your treatment regimen or change medications.
Antifungal gels, creams, lotions, foams or shampoos alternated with another medication
Your skin doctor might suggest you try a product with 2% ketoconazole or 1% ciclopirox (Loprox). Or you might rotate between two or more products. Ketoconzole can worsen the dryness of tightly coiled or chemically treated hair and increase the risk of breakage. To ease this effect, use it only once a week with a moisturizing conditioner.
How often you shampoo or apply other antifungal products will depend on your hair-grooming practices and symptoms. Medicated shampoos can be used once a day or 2 to 3 times a week for several weeks. Let the product sit on your scalp for a few minutes — see package directions — so it has time to work. Then rinse. After your symptoms clear up, use a medicated shampoo just once a week or once every two weeks. This will help prevent a relapse.
For scalp and nonscalp seborrheic dermatitis treatment, evidence supports topical 1% to 2% ketoconazole, 1% ciclopirox, 1% zinc pyrithione, and 1% hydrocortisone 39. Intermittent use of a mild topical corticosteroid and imidazole antifungal combination is convenient and can be very effective, but a potent corticosteroid may be necessary for the short-term treatment of adult scalp seborrheic dermatitis 14.
Shampoos usually contain combinations of agents such as pine or coal tar (antipruritic/keratolytic), salicylic acid (keratolytic), sulfur (antimicrobial/keratolytic), and sulfacetamide (antiinflammatory/antibacterial) 14. You can apply these to your scalp and other areas of your body and wash them off after 5 to 10 minutes. Given the lack of safety and efficacy data for such treatment, care should be taken when using topical salicylic acid, selenium, or zinc for treating infant seborrheic dermatitis 14. Topical ketoconazole has been shown to be safe in infants, with minimal systemic absorption detected 14.
Side effects associated with topical corticosteroids should be reduced by intermittent use of site-appropriate potencies or steroid-sparing preparations such as topical 1% pimecrolimus 14. Another strategy is to employ the antiinflammatory effect of the topical antifungals, estimated to be equivalent to 1% hydrocortisone 40.
Creams, lotions, shampoos or ointments that control inflammation
Your skin doctor might prescribe a prescription-strength corticosteroid you apply to the scalp or other affected area. These include hydrocortisone, fluocinolone (Capex, Synalar), clobetasol (Clobex, Temovate) and desonide (Desowen, Desonate). They are effective and easy to use. And use them only until symptoms clear up. If used for many weeks or months without a break, they can cause side effects. These include loss of skin color, thinning skin, and skin showing streaks or lines.
Creams or ointments with a calcineurin inhibitor such as tacrolimus (Protopic) or pimecrolimus (Elidel) may be effective. Another benefit is that they have fewer side effects than corticosteroids do. But they are not first-choice treatments because the Food and Drug Administration has concerns about a possible association with cancer. In addition, tacrolimus and pimecrolimus cost more than mild corticosteroid medications.
Antifungal medication you take as a pill
If your seborrheic dermatitis isn’t improving with other treatments (refractory disease) or is severe or generalized, your skin doctor may prescribe an antifungal medication in pill form. The antifungal with antiinflammatory properties include ketoconazole (monitor liver function; Black Box warning), itraconazole (check for CYP450 drug interactions; can worsen heart failure), and fluconazole (adjust the dose according to renal function) 14. Itraconazole has the greatest antiinflammatory effect, whereas oral terbinafine may be more effective than oral fluconazole in severe seborrheic dermatitis 14. Low-dose isotretinoin is noninferior to the topical standard of care but is commonly associated with significant mucocutaneous side effects 41.
Itraconazole is safe and effective for controlling the flares of seborrheic dermatitis and preventing relapses 40. It has also been shown to improve the quality of life in patients with moderate-to-severe seborrheic dermatitis 42. However, given the absence of high-quality safety and efficacy data, a specialist team review is recommended before commencing oral treatment for infant seborrheic dermatitis 14.
In HIV-AIDS, antiretroviral treatment frequently improves seborrheic dermatitis, and seborrheic dermatitis may improve with L-dopa therapy in Parkinson disease 43.
Future therapies for seborrheic dermatitis could target improving skin barrier function or restoring the skin’s surface lipid composition 14.
Scalp treatment
- Medicated shampoos containing ketoconazole, ciclopirox, selenium sulfide, zinc pyrithione, coal tar, and salicylic acid, used twice weekly for at least a month and if necessary, indefinitely.
- Steroid scalp applications reduce itching and should be applied daily for a few days every so often.
- Calcineurin inhibitors such as tacrolimus can be used as steroid alternatives.
- Coal tar cream can be applied to scaling areas and removed several hours later by shampooing.
- Combination therapy is often advisable.
- Alternative treatments, such as tea tree oil shampoo, may be used.
Face, ears, chest, and back
- Cleanse the affected skin thoroughly once or twice each day using a non-soap cleanser.
- Apply ketoconazole or ciclopirox cream once daily for 2 to 4 weeks, repeated as necessary.
- Hydrocortisone cream can also be used, applied up to twice daily for 1 or 2 weeks. Occasionally a more potent topical steroid may be prescribed.
- Topical calcineurin inhibitors such as pimecrolimus cream or tacrolimus ointment may be used instead of topical steroids.
- A variety of herbal remedies are commonly used, but their efficacy is uncertain.
Management in infants
The initial approach, especially in mild and localized seborrheic dermatitis of the scalp, should be conservative, involving either application of gentle aqueous cream or repeated shampooing, followed by gentle brushing using a soft toothbrush or comb to remove the scales. Sorbolene cream or lotion and a soft-bristled toothbrush can soften and remove the cradle cap scales. White petrolatum may be useful.
More extensive (depending on the extent of the rash) or resistant seborrheic dermatitis may be treated with topical antifungal agents (e.g., ketoconazole, clotrimazole and miconazole) and a low-potency topical steroid (eg, hydrocortisone 1%) or azole (eg ketoconazole 2%) for 1–2 weeks. Topical steroid may be preferred if there is a significant inflammatory component 3, 44.
Home remedies for seborrheic dermatitis
If you have seborrheic dermatitis of the scalp, you may be able to control seborrheic dermatitis with lifestyle changes and home remedies. You can try some of the over-the-counter dandruff shampoos that contain selenium, zinc pyrithione, ketoconazole, salicylic acid or coal tar. Many of these are sold in nonprescription forms. If one shampoo doesn’t work, look at the active ingredient and try another product with a different active ingredient. Shampoos should remain on your scalp for at least five minutes before rinsing off. Shampoo with it twice a week or as directed on the label of the product. You may need to try different products or a combination of products before your condition improves.
The best approach for you depends on your skin type, hair-grooming practices and your symptoms. But even if your condition clears up, it’s likely to come back at some point. Watch for the symptoms and resume treating the condition when it recurs. Or use nonprescription antidandruff products in your self-care routine to prevent flare-ups.
If you think you have seborrheic dermatitis on your face or body, see your doctor or dermatologist. They will examine you to determine the extent and severity of your condition. You will work together to develop the best treatment approach to get your condition under control and manage flare-ups. Follow all instructions and never hesitate to call your doctor if you have questions or concerns.
For long-term control, your doctor may prescribe antifungal shampoos that contain ciclopirax (Loprox) or ketoconazole (Nizoral). These shampoos are used from daily to two or three times a week for several weeks until the dandruff has cleared, then once every week to two weeks to prevent flare-ups. Your doctor will give you specific directions for use.
For moderate to severe cases, your doctor may prescribe a shampoo containing betamethasone valerate (Luxiq), clobetasol (Clobex), fluocinolone (Capex) or fluocinolone solution (Synalar). Shampoo your hair as directed. Some products are used daily, others are used twice daily for two weeks then two times a week.
Lifestyle changes
Healthy lifestyle habits, like managing stress and getting plenty of sleep, can also improve skin. Stress relief is often the lifestyle change which will have the biggest impact on seborrheic dermatitis. Some particularly effective stress relief techniques include:
- Perform light exercise, such as yoga or a gentle walk;
- Journal about stress and negative feelings;
- Develop a mediation or breathwork practice;
- Spend time in nature, even if it’s just five minutes.
There are many other ways you can reduce stress. What matters most is finding an enjoyable technique that allows you to slow down and devote time to self care.
Wash your scalp regularly
If regular shampoo doesn’t help with dandruff, try nonprescription dandruff shampoos. They are classified according to the active ingredient they contain:
- Pyrithione zinc (DermaZinc, Head & Shoulders, others), also sold as bar soap
- Selenium sulfide (Head & Shoulders, Selsun Blue, others)
- Ketoconazole 1% (Nizoral A-D)
- Tar (Denorex Extra Strength, DHS Tar, others)
- Salicylic acid (Denorex, DHS Sal, others)
How often you shampoo or apply other antifungal products will depend on your hair-grooming practices and symptoms. Medicated shampoos can be used once a day or 2 to 3 times a week for several weeks. After your symptoms clear up, use a medicated shampoo just once a week or once every two weeks. This will help prevent a relapse. Shampoo that contains tar or selenium sulfide can discolor light-colored hair.
Sometimes a shampoo that has helped loses its effectiveness over time. If that’s the case, try alternating between two or more types. Be sure to leave your shampoo on for the full recommended time — this allows its ingredients to work. Then rinse. These shampoos may be rubbed gently on the face, ears and chest and rinsed off well.
Other home remedies
The following nonprescription treatments and self-care tips may help you control seborrheic dermatitis:
- Soften and remove scales from your hair. Apply mineral oil, peanut oil or olive oil to your scalp. Leave it in for 1 to 3 hours. Then comb or brush your hair and wash it.
- Wash your skin regularly. Use warm, not hot, water and a gentle soap or nonsoap cleanser. Rinse thoroughly. Pat dry and apply a moisturizer while your skin is still damp.
- Apply a medicated cream. First try a mild corticosteroid cream, foam, ointment or oil (Scalpicin Scalp Itch) on affected areas, keeping it away from the eyes. If that doesn’t work, try the antifungal cream ketoconazole.
- Don’t use styling products. Stop using hair sprays, gels and other styling products while you’re treating the condition.
- Don’t use skin and hair products that contain alcohol. These can cause the disease to flare up.
- If you have a beard or mustache, shampoo facial hair regularly. Seborrheic dermatitis can be worse under mustaches and beards. Shampoo with 1% ketoconazole daily until your symptoms improve. Then switch to shampooing once a week or once every two weeks. Or shaving might ease your symptoms.
- Gently clean your eyelids. If your eyelids are inflamed or scaly, wash them each night. Use a few drops of baby shampoo mixed with two capfuls of warm water. Wipe away scales with a cotton swab. Warm, damp cloths pressed to your eyelids also may help.
- Gently wash your baby’s scalp. If your infant has mild cradle cap, wash the scalp with a mild baby shampoo once a day. Gently loosen the scales with a cloth or an infant hairbrush before rinsing out the shampoo. If scaling persists, first apply mineral oil or olive oil to the scalp for an hour or two. Cradle cap usually disappears in a few weeks or months.
Alternative medicine
Many alternative therapies, including those listed below, have helped some people manage their seborrheic dermatitis. But evidence for their effectiveness isn’t proved. It’s always a good idea to check with your doctor before adding any alternative medicines to your self-care routine.
- Tea tree oil. A shampoo with 5% tea tree oil may be used on the affected area. Some studies suggest that tea tree oil can trigger an allergic reaction.
- Aloe. Apply aloe vera gel to the affected area. Aloe is an ingredient in many products, or you can use it directly from the leaf of an aloe plant.
- Low levels of serum zinc, vitamin D, and vitamin E in patients with seborrheic dermatitis suggest the benefits of supplementation.
Zinc is an essential trace element that assists in cell growth, development, and differentiation and plays catalytic and structural roles in transcription factors, receptors, growth factors, cytokines, and enzymes 45. Zinc also possesses anti-inflammatory properties, including inhibiting polynuclear neutrophils chemotaxis and altering the production of interleukin-6 and tumor necrosis factor alpha, 2 proinflammatory cytokines produced by skin cells 46, 47. Zinc also possesses antiandrogen activity by inhibiting 5 alpha-reductase type 1 expression 48. These inflammatory and androgenic pathways are essential to the pathogenesis of seborrheic dermatitis, therefore lower serum zinc levels in patients with seborrheic dermatitis may represent a precipitating factor to disease development 49. Importantly, there was no correlation between serum zinc levels and disease severity graded by SEborrheic Dermatitis Area and Severity Index (SEDASI), so it may only be involved in the development of seborrheic dermatitis rather than progression 49. The authors postulated that this is due to the study’s small sample size and their inclusion of only mild seborrheic dermatitis 49. More studies are needed to identify if this relationship holds true for severe seborrheic dermatitis and if oral zinc supplementation is of clinical benefit.
Vitamin E is a fat-soluble vitamin and an important antioxidant that helps protect cell membranes from lipid peroxidation, minimizing oxidative damage 50. Therefore, the low levels of vitamin E in patients with seborrheic dermatitis may contribute to an increased oxidative burden 51. Supplementation with oral vitamin E showed early promising results in improving other inflammatory skin diseases, including atopic dermatitis and psoriasis 50. Further research is needed to elucidate the role of vitamin E supplementation as an adjunctive therapy in seborrheic dermatitis.
Vitamin D plays a role in multiple skin processes, ranging from keratinocyte proliferation, differentiation, and apoptosis to immunoregulatory processes and barrier maintenance 52. Vitamin D enhances the synthesis of structural proteins and mediates immunosuppressive action in the skin 52. Thus, the lower 25-hydroxyvitamin D levels in patients with seborrheic dermatitis found by Rahimi et al 53 and Borda and Wikramanayake 54 may decrease these protective functions, generating epidermal barrier dysfunction in seborrheic dermatitis. Vitamin D deficiency also plays a role in other inflammatory skin pathologies, such as psoriasis and atopic dermatitis; supplementation of vitamin D3 and vitamin D analogs is effective against psoriasis 52. Further research is needed to determine the significance of vitamin D deficiency in seborrheic dermatitis and the efficacy of interventional supplementation.
Prebiotics and probiotics possess antimicrobial properties and play a role in the inflammatory response and skin barrier function 55. Probiotics are live microorganisms while prebiotics are nondigestible carbohydrates that induce the growth of probiotic bacteria 55. Prebiotics and probiotics are beneficial for several dermatologic conditions, including dandruff and seborrhea, but their use in seborrheic dermatitis is limited 56. Triphala, a polyphenol-rich prebiotic, is one of the few dietary supplements that has been tested as a seborrheic dermatitis treatment 57. Triphala has antioxidant properties and acts as a skin protectant for human skin cells in test tube study 58. The study was limited by a small sample size, but Triphala is a potential adjunctive treatment for seborrheic dermatitis, but more extensive clinical trials are necessary to fully understand its efficacy and safety.
If you’re considering dietary supplements or other alternative therapies, talk with your skin doctor about their pros and cons.
Seborrheic dermatitis prognosis
Infant seborrheic dermatitis usually affects the scalp of babies (cradle cap) and is mild and self-limiting, whereas adult seborrheic dermatitis presents a chronic pattern of skin disease characterized by relapses and remissions throughout life 14. Infant seborrheic dermatitis is generally a harmless condition that doesn’t cause pain, itching or discomfort. It appears within the first weeks to months of life and is rarely seen after 12 months of age in most babies. Cradle cap is benign and self-limiting. It usually resolves without intervention over the course of weeks to several months. If disease persists beyond 12 months, the diagnosis should be reconsidered. Infant seborrheic dermatitis can be easily managed with simple at-home care. Adult seborrheic dermatitis is very controllable with treatment but not curable 14. Adult seborrheic dermatitis improves quickly with regular treatment. See a skin doctor if your condition doesn’t respond to self-treatment, or if the affected area becomes painful, forms crusts, or drains fluid or pus. Although seborrheic dermatitis does take a toll on the well-being of patients, timely management can help increase your quality of life 59.
- Woolhiser E, Keime N, Patel A, Weber I, Adelman M, Dellavalle RP. Nutrition, Obesity, and Seborrheic Dermatitis: Systematic Review. JMIR Dermatol. 2024 Aug 5;7:e50143. doi: 10.2196/50143[↩][↩]
- Heath CR, Usatine RP. Seborrheic dermatitis. J Fam Pract. 2021 Nov;70(9):E3-E4. doi: 10.12788/jfp.0315[↩]
- Okokon EO, Verbeek JH, Ruotsalainen JH, Ojo OA, Bakhoya VN. Topical antifungals for seborrhoeic dermatitis. Cochrane Database Syst Rev. 2015 May 2;(5):CD008138. doi: 10.1002/14651858.CD008138.pub3[↩][↩]
- Gupta A, Bluhm R. Seborrheic dermatitis. J Eur Acad Dermatol Venereol. 2004;18(1):13–26. doi: 10.1111/j.1468-3083.2004.00693.x.693[↩]
- Seborrheic Dermatitis. https://my.clevelandclinic.org/health/diseases/14403-seborrheic-dermatitis[↩]
- Seborrhoeic dermatitis. https://dermnetnz.org/topics/seborrhoeic-dermatitis[↩][↩][↩][↩][↩]
- Foley P, Zuo Y, Plunkett A, Merlin K, Marks R. The frequency of common skin conditions in preschool-aged children in Australia: seborrheic dermatitis and pityriasis capitis (cradle cap). Arch Dermatol. 2003 Mar;139(3):318-22. doi: 10.1001/archderm.139.3.318[↩]
- Scognamiglio P, Chiaradia G, De Carli G, Giuliani M, Mastroianni CM, Aviani Barbacci S, Buonomini AR, Grisetti S, Sampaolesi A, Corpolongo A, Orchi N, Puro V, Ippolito G, Girardi E; SENDIH Study Group. The potential impact of routine testing of individuals with HIV indicator diseases in order to prevent late HIV diagnosis. BMC Infect Dis. 2013 Oct 10;13:473. doi: 10.1186/1471-2334-13-473[↩]
- Dessinioti C, Katsambas A. Seborrheic dermatitis: etiology, risk factors, and treatments: facts and controversies. Clin Dermatol. 2013;31(4):343–351. doi: 10.1016/j.clindermatol.2013.01.001.S0738-081X(13)00002-3[↩]
- Schwartz JL, Clinton TS. Darier’s disease misdiagnosed as severe seborrheic dermatitis. Mil Med. 2011 Dec;176(12):1457-9. doi: 10.7205/milmed-d-11-00147[↩]
- Palamaras I, Kyriakis K, Stavrianeas N. Seborrheic dermatitis: lifetime detection rates. J Eur Acad Dermatol Venereol. 2012 Apr;26(4):524–6. doi: 10.1111/j.1468-3083.2011.04079.x[↩]
- Sanders MGH, Pardo LM, Franco OH, Ginger RS, Nijsten T. Prevalence and determinants of seborrhoeic dermatitis in a middle-aged and elderly population: the Rotterdam study. Br J Dermatol. 2018;178(1):148–153. doi: 10.1111/bjd.15908[↩]
- Sampaio ALSB, Mameri ACA, Vargas TJDS, Ramos-e-Silva M, Nunes AP, Carneiro SCDS. Seborrheic dermatitis. An Bras Dermatol. 2011;86(6):1061–1071. doi: 10.1590/s0365-05962011000600002.S0365-05962011000600002[↩][↩]
- Tucker D, Masood S. Seborrheic Dermatitis. [Updated 2024 Mar 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551707[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Sampogna F, Linder D, Piaserico S, Altomare G, Bortune M, Calzavara-Pinton P, Vedove CD, Girolomoni G, Peserico A, Sala R, Abeni D. Quality of life assessment of patients with scalp dermatitis using the Italian version of the Scalpdex. Acta Derm Venereol. 2014 Jul;94(4):411-4. doi: 10.2340/00015555-1731[↩]
- Sanders MGH, Pardo LM, Ginger RS, Kiefte-de Jong JC, Nijsten T. Association between Diet and Seborrheic Dermatitis: A Cross-Sectional Study. J Invest Dermatol. 2019 Jan;139(1):108-114. doi: 10.1016/j.jid.2018.07.027[↩]
- Cepeda AM, Del Giacco SR, Villalba S, Tapias E, Jaller R, Segura AM, Reyes G, Potts J, Garcia-Larsen V. A Traditional Diet Is Associated with a Reduced Risk of Eczema and Wheeze in Colombian Children. Nutrients. 2015 Jun 25;7(7):5098-110. doi: 10.3390/nu7075098[↩][↩]
- Wikramanayake TC, Borda LJ, Miteva M, Paus R. Seborrheic dermatitis-Looking beyond Malassezia. Exp Dermatol. 2019 Sep;28(9):991-1001. doi: 10.1111/exd.14006[↩]
- Lin Q, Panchamukhi A, Li P, Shan W, Zhou H, Hou L, Chen W. Malassezia and Staphylococcus dominate scalp microbiome for seborrheic dermatitis. Bioprocess Biosyst Eng. 2021 May;44(5):965-975. doi: 10.1007/s00449-020-02333-5[↩]
- Zani MB, Soares RC, Arruda AC, de Arruda LH, Paulino LC. Ketoconazole does not decrease fungal amount in patients with seborrhoeic dermatitis. Br J Dermatol. 2016 Aug;175(2):417-21. doi: 10.1111/bjd.14501[↩]
- Dall’Oglio F, Nasca MR, Gerbino C, Micali G. An overview of the diagnosis and management of seborrheic dermatitis. Clin Cosmet Investig Dermatol. 2022;15:1537–1548. doi: 10.2147/CCID.S284671[↩]
- Bowe WP, Joshi SS, Shalita AR. Diet and acne. J Am Acad Dermatol. 2010;63(1):124–141. doi: 10.1016/j.jaad.2009.07.043.S0190-9622(09)00967-0[↩]
- Barrea L, Fabbrocini G, Annunziata G, Muscogiuri G, Donnarumma M, Marasca C, Colao A, Savastano S. Role of nutrition and adherence to the mediterranean diet in the multidisciplinary approach of hidradenitis suppurativa: evaluation of nutritional status and its association with severity of disease. Nutrients. 2018;11(1):57. doi: 10.3390/nu11010057[↩]
- Akbaş A, Kılınç F, Şener S, Hayran Y. Investigation of the relationship between seborrheic dermatitis and metabolic syndrome parameters. J Cosmet Dermatol. 2022;21(11):6079–6085. doi: 10.1111/jocd.15121[↩][↩]
- Savaş Erdoğan S, Falay Gür T, Özkur E, Doğan B. Insulin resistance and metabolic syndrome in patients with seborrheic dermatitis: a case-control study. Metab Syndr Relat Disord. 2022;20(1):50–56. doi: 10.1089/met.2021.0063[↩][↩]
- Hou X, Chen S, Hu G, Chen P, Wu J, Ma X, Yang Z, Yang W, Jia W, China National Diabetes. Metabolic Disorders Study Group Stronger associations of waist circumference and waist-to-height ratio with diabetes than BMI in Chinese adults. Diabetes Res Clin Pract. 2019;147:9–18. doi: 10.1016/j.diabres.2018.07.029.S0168-8227(18)30133-5[↩]
- Cox AJ, West NP, Cripps AW. Obesity, inflammation, and the gut microbiota. Lancet Diabetes Endocrinol. 2015;3(3):207–215. doi: 10.1016/S2213-8587(14)70134-2.S2213-8587(14)70134-2[↩]
- Imamoglu B, Hayta SB, Guner R, Akyol M, Ozcelik S. Metabolic syndrome may be an important comorbidity in patients with seborrheic dermatitis. Arch Med Sci Atheroscler Dis. 2016;1(1):e158–e161. doi: 10.5114/amsad.2016.65075. doi: 10.5114/amsad.2016.65075.29072[↩]
- Lally A, Casabonne D, Imko-Walczuk B, Newton R, Wojnarowska F. Prevalence of benign cutaneous disease among Oxford renal transplant recipients. J Eur Acad Dermatol Venereol. 2011 Apr;25(4):462-70. doi: 10.1111/j.1468-3083.2010.03814.x[↩]
- Dessinioti C, Katsambas A. Seborrheic dermatitis: etiology, risk factors, and treatments: facts and controversies. Clin Dermatol. 2013 Jul-Aug;31(4):343-351. doi: 10.1016/j.clindermatol.2013.01.001[↩][↩]
- Niemann N, Billnitzer A, Jankovic J. Parkinson’s disease and skin. Parkinsonism Relat Disord. 2021 Jan;82:61-76. doi: 10.1016/j.parkreldis.2020.11.017[↩]
- Adalsteinsson JA, Kaushik S, Muzumdar S, Guttman-Yassky E, Ungar J. An update on the microbiology, immunology and genetics of seborrheic dermatitis. Exp Dermatol. 2020 May;29(5):481-489. doi: 10.1111/exd.14091[↩]
- Schwartz JR, Messenger AG, Tosti A, Todd G, Hordinsky M, Hay RJ, Wang X, Zachariae C, Kerr KM, Henry JP, Rust RC, Robinson MK. A comprehensive pathophysiology of dandruff and seborrheic dermatitis – towards a more precise definition of scalp health. Acta Derm Venereol. 2013 Mar 27;93(2):131-7. doi: 10.2340/00015555-1382[↩][↩]
- Gaitanis G, Magiatis P, Hantschke M, Bassukas ID, Velegraki A. The Malassezia genus in skin and systemic diseases. Clin Microbiol Rev. 2012 Jan;25(1):106-41. doi: 10.1128/CMR.00021-11[↩]
- Forrestel AK, Kovarik CL, Mosam A, Gupta D, Maurer TA, Micheletti RG. Diffuse HIV-associated seborrheic dermatitis – a case series. Int J STD AIDS. 2016 Dec;27(14):1342-1345. doi: 10.1177/0956462416641816[↩]
- Sampaio AL, Mameri AC, Vargas TJ, Ramos-e-Silva M, Nunes AP, Carneiro SC. Seborrheic dermatitis. An Bras Dermatol. 2011 Nov-Dec;86(6):1061-71; quiz 1072-4. English, Portuguese. doi: 10.1590/s0365-05962011000600002[↩]
- Piquero-Casals J, La Rotta-Higuera E, Francisco Mir-Bonafé J, Rozas-Muñoz E, Granger C. Non-Steroidal Topical Therapy for Facial Seborrheic Dermatitis. J Drugs Dermatol. 2020 Jun 1;19(6):658-660. doi: 10.36849/JDD.2020.10.36849/JDD.2020.5121[↩]
- Gupta AK, Versteeg SG. Topical Treatment of Facial Seborrheic Dermatitis: A Systematic Review. Am J Clin Dermatol. 2017 Apr;18(2):193-213. doi: 10.1007/s40257-016-0232-2[↩]
- Cheong WK, Yeung CK, Torsekar RG, Suh DH, Ungpakorn R, Widaty S, Azizan NZ, Gabriel MT, Tran HK, Chong WS, Shih IH, Dall’Oglio F, Micali G. Treatment of Seborrhoeic Dermatitis in Asia: A Consensus Guide. Skin Appendage Disord. 2016 May;1(4):187-96. doi: 10.1159/000444682[↩]
- Das A, Panda S. Use of Topical Corticosteroids in Dermatology: An Evidence-based Approach. Indian J Dermatol. 2017 May-Jun;62(3):237-250. doi: 10.4103/ijd.IJD_169_17[↩][↩]
- Kamamoto CSL, Nishikaku AS, Gompertz OF, Melo AS, Hassun KM, Bagatin E. Cutaneous fungal microbiome: Malassezia yeasts in seborrheic dermatitis scalp in a randomized, comparative and therapeutic trial. Dermatoendocrinol. 2017 Oct 23;9(1):e1361573. doi: 10.1080/19381980.2017.1361573[↩]
- Abbas Z, Ghodsi SZ, Abedeni R. Effect of itraconazole on the quality of life in patients with moderate to severe seborrheic dermatitis: a randomized, placebo-controlled trial. Dermatol Pract Concept. 2016 Jul 31;6(3):11-6. doi: 10.5826/dpc.0603a04[↩]
- Skorvanek M, Bhatia KP. The Skin and Parkinson’s Disease: Review of Clinical, Diagnostic, and Therapeutic Issues. Mov Disord Clin Pract. 2016 Sep 8;4(1):21-31. doi: 10.1002/mdc3.12425[↩]
- Wananukul S, Chatproedprai S, Charutragulchai W. Randomized, double-blind, split-side comparison study of moisturizer containing licochalcone vs. 1% hydrocortisone in the treatment of infantile seborrhoeic dermatitis. J Eur Acad Dermatol Venereol. 2012 Jul;26(7):894-7. doi: 10.1111/j.1468-3083.2011.04187.x[↩]
- Ogawa Y, Kawamura T, Shimada S. Zinc and skin biology. Arch Biochem Biophys. 2016;611:113–119. doi: 10.1016/j.abb.2016.06.003.S0003-9861(16)30189-8[↩]
- Sainte-Marie I, Jumbou O, Tenaud I, Dreno B. Comparative study of the in vitro inflammatory activity of three nickel salts on keratinocytes. Acta Derm Venereol. 1998;78(3):169–172. doi: 10.1080/000155598441459[↩]
- Dreno B, Trossaert M, Boiteau HL, Litoux P. Zinc salts effects on granulocyte zinc concentration and chemotaxis in acne patients. Acta Derm Venereol. 1992 Aug;72(4):250-2.[↩]
- Brocard A, Knol AC, Khammari A, Dréno B. Hidradenitis suppurativa and zinc: a new therapeutic approach. a pilot study. Dermatology. 2007;214(4):325–327. doi: 10.1159/000100883.000100883[↩]
- Aktaş Karabay E, Aksu Çerman A. Serum zinc levels in seborrheic dermatitis: a case-control study. Turk J Med Sci. 2019 Oct 24;49(5):1503-1508. doi: 10.3906/sag-1906-72[↩][↩][↩]
- Berardesca E, Cameli N. Vitamin E supplementation in inflammatory skin diseases. Dermatol Ther. 2021;34(6):e15160. doi: 10.1111/dth.15160[↩][↩]
- Jahan I, Islam MR, Islam MR, Ali R, Rahman SMM, Nahar Z, Hasnat A, Islam MS. Altered serum elements, antioxidants, MDA, and immunoglobulins are associated with an increased risk of seborrheic dermatitis. Heliyon. 2021 Mar 28;7(3):e06621. doi: 10.1016/j.heliyon.2021.e06621[↩]
- Umar M, Sastry KS, Al Ali F, Al-Khulaifi M, Wang E, Chouchane AI. Vitamin D and the pathophysiology of inflammatory skin diseases. Skin Pharmacol Physiol. 2018;31(2):74–86. doi: 10.1159/000485132[↩][↩][↩]
- Rahimi S, Nemati N, Shafaei-Tonekaboni SS. Serum levels of 25-hydroxyvitamin D in patients with seborrheic dermatitis: a case-control study. Dermatol Res Pract. 2021;2021:6623271. doi: 10.1155/2021/6623271[↩]
- Borda LJ, Wikramanayake TC. Seborrheic Dermatitis and Dandruff: A Comprehensive Review. J Clin Investig Dermatol. 2015 Dec;3(2):10.13188/2373-1044.1000019. doi: 10.13188/2373-1044.1000019[↩]
- Baquerizo Nole KL, Yim E, Keri JE. Probiotics and prebiotics in dermatology. J Am Acad Dermatol. 2014;71(4):814–821. doi: 10.1016/j.jaad.2014.04.050.S0190-9622(14)01407-8[↩][↩]
- Reygagne P, Bastien P, Couavoux M, Philippe D, Renouf M, Castiel-Higounenc I, Gueniche A. The positive benefit of Lactobacillus paracasei NCC2461 ST11 in healthy volunteers with moderate to severe dandruff. Benef Microbes. 2017;8(5):671–680. doi: 10.3920/BM2016.0144[↩]
- Zareie E, Mansouri P, Hosseini H, Sadeghpour O, Shirbeigi L, Hejazi S, Emtiazy M. Effect of oral administration of triphala, a polyphenol-rich prebiotic, on scalp sebum in patients with scalp seborrhea a randomized clinical trial. J Dermatolog Treat. 2022;33(2):1011–1016. doi: 10.1080/09546634.2020.1800568[↩]
- Varma SR, Sivaprakasam TO, Mishra A, Kumar LM, Prakash NS, Prabhu S, Ramakrishnan S. Protective Effects of Triphala on Dermal Fibroblasts and Human Keratinocytes. PLoS One. 2016 Jan 5;11(1):e0145921. doi: 10.1371/journal.pone.0145921[↩]
- Araya M, Kulthanan K, Jiamton S. Clinical Characteristics and Quality of Life of Seborrheic Dermatitis Patients in a Tropical Country. Indian J Dermatol. 2015 Sep-Oct;60(5):519. doi: 10.4103/0019-5154.164410[↩]