Contents
- Small intestine cancer
- Diet and health history can affect the risk of developing small intestine cancer
- Small intestine cancer survival rate
- Stage Information for Small Intestine Cancer
- Small intestine cancer signs and symptoms
- Tests that examine the small intestine are used to detect (find), diagnose, and stage small intestine cancer
- Small intestine cancer treatment
- Gastrointestinal stromal tumor
- Signs and symptoms of gastrointestinal stromal tumors
- Stages of Gastrointestinal Stromal Tumors
- Treatment Options for Gastrointestinal stromal tumor
- Resectable Gastrointestinal Stromal Tumors
- Unresectable Gastrointestinal Stromal Tumors
- Metastatic and Recurrent Gastrointestinal Stromal Tumors
- Refractory Gastrointestinal Stromal Tumors
- Gastrointestinal Carcinoid Tumors
- Health history can affect the risk of gastrointestinal carcinoid tumors.
- Some gastrointestinal carcinoid tumors have no signs or symptoms in the early stages.
- The following tests and procedures may be used:
- Certain factors affect prognosis (chance of recovery) and treatment options.
- There are different types of treatment for patients with gastrointestinal carcinoid tumors.
- New types of treatment are being tested in clinical trials.
- Carcinoid Tumors in the Small Intestine
- Metastatic Gastrointestinal Carcinoid Tumors
- Recurrent Gastrointestinal Carcinoid Tumors
Small intestine cancer
Small intestine cancer is a rare disease in which malignant (cancer) cells form in the tissues of the small intestine 1.
The small intestine (also called small bowel) is part of the body’s digestive system, which also includes the esophagus, stomach, and large intestine. The digestive system removes and processes nutrients (vitamins, minerals, carbohydrates, fats, proteins, and water) from foods and helps pass waste material out of the body.
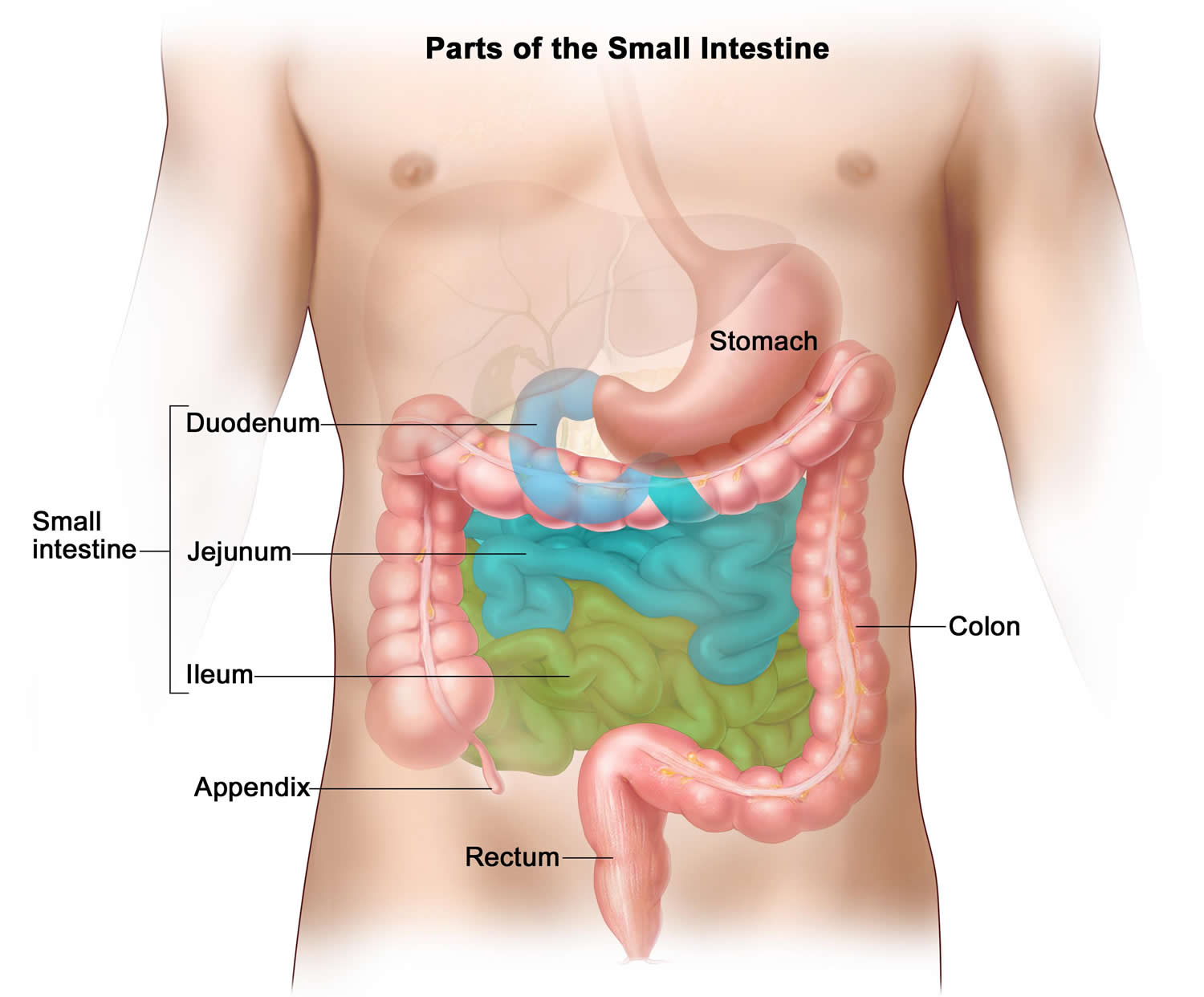
The small intestine is a long tube that connects the stomach to the large intestine. It folds many times to fit inside the abdomen. The small intestine consists of three parts: the duodenum, the jejunum, and the ileum (Figure 1). The duodenum, about 25 centimeters long and 5 centimeters in diameter, lies posterior to the parietal peritoneum and is the most fixed portion of the small intestine. It follows a C-shaped path as it passes anterior to the right kidney and the upper three lumbar vertebrae. The remainder of the small intestine is mobile and lies free in the peritoneal cavity. The proximal two-fifths of this portion of the small intestine is the jejunum, and the remainder is the ileum. The jejunum and ileum are not easily distinguished as separate parts; however, the diameter of the jejunum is typically greater than that of the ileum, and its wall is thicker, more vascular, and more active.
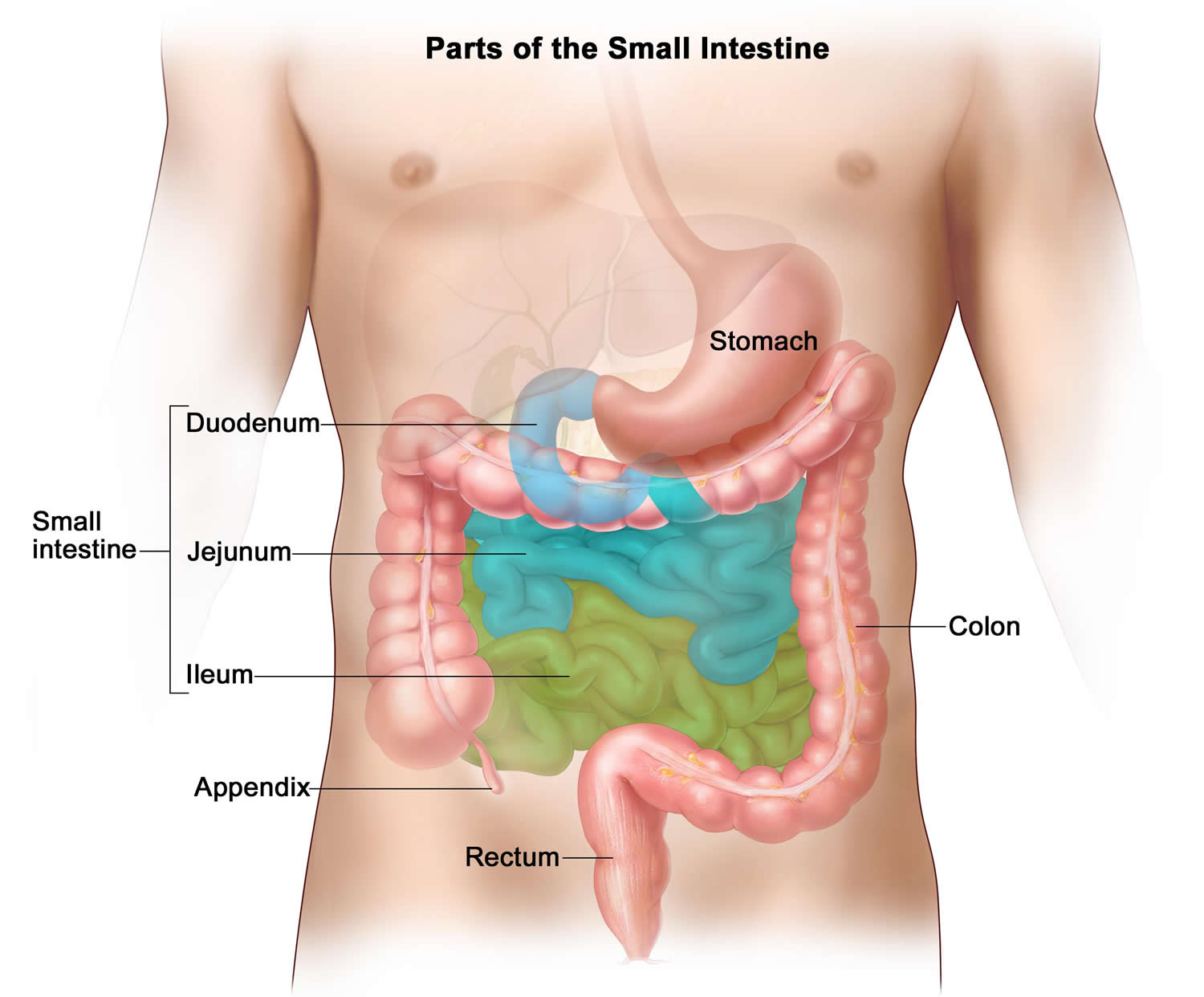
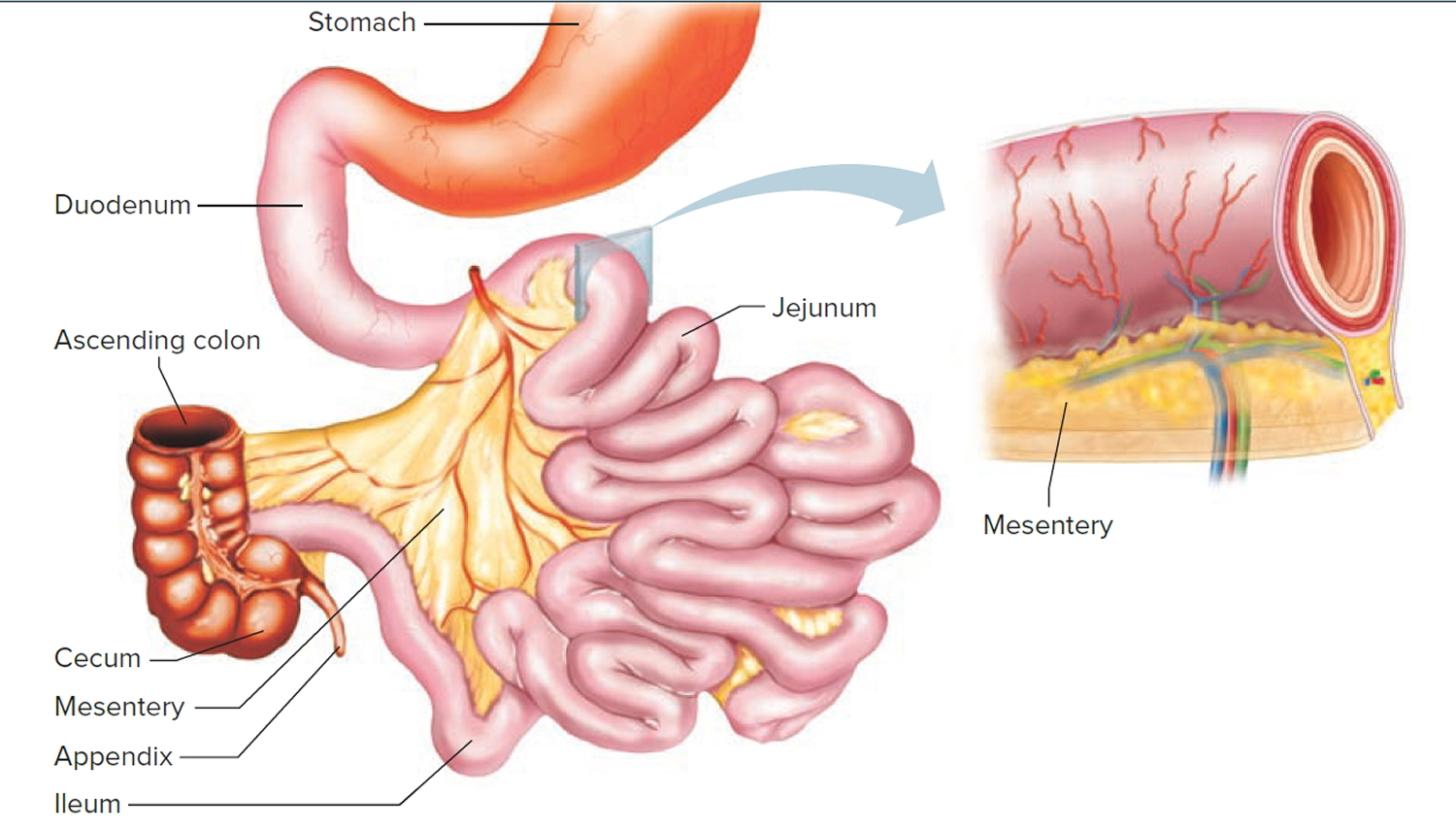
A double-layered fold of peritoneal membrane called mesentery suspends the jejunum and ileum from the posterior abdominal wall (Figure 2). The mesentery supports the blood vessels, nerves, and lymphatic vessels that supply the intestinal wall. A filmy, double fold of peritoneal membrane called the greater omentum drapes like an apron from the stomach over the transverse colon and the folds of the small intestine.
Estimated new cases and deaths from small intestine cancer in the United States in 2017 2:
- New cases: 10,190.
- Deaths: 1,390.
There are five types of small intestine cancer. The types of cancer found in the small intestine are:
- Adenocarcinoma (majority of cases).
- Lymphoma (uncommon), which is usually of the non-Hodgkin type.
- Sarcoma (most commonly leiomyosarcoma and more rarely angiosarcoma or liposarcoma).
- Gastrointestinal stromal tumor.
- Carcinoid tumors.
Approximately 25% to 50% of the primary malignant tumors in the small intestine are adenocarcinomas, and most occur in the duodenum 3. Small intestine carcinomas may occur synchronously (existing at the same time) or metachronously (multiple separate occurrences at different intervals) at multiple sites 4.
Leiomyosarcoma starts in the smooth muscle cells of the small intestine. Most of these tumors occur in the part of the small intestine near the large intestine most often in the ileum 4.
Some 20% of malignant lesions of the small intestine are carcinoid tumors, which occur more frequently in the ileum than in the duodenum or jejunum and may be multiple 4.
It is uncommon to find malignant lymphoma as a solitary small intestine lesion 4.
Together they account for the majority of small intestine malignancies, which, as a whole, account for only 1% to 2% of all gastrointestinal malignancies 5, 6, 7, 8.
Diet and health history can affect the risk of developing small intestine cancer
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer. Talk with your doctor if you think you may be at risk. Risk factors for small intestine cancer include the following:
- Eating a high-fat diet.
- Having Crohn disease.
- Having celiac disease.
- Having familial adenomatous polyposis.
Small intestine cancer survival rate
The prognosis (chance of recovery) and treatment options depend on the following:
- The type of small intestine cancer.
- Whether the cancer is in the inner lining of the small intestine only or has spread into or beyond the wall of the small intestine.
- Whether the cancer has spread to other places in the body, such as the lymph nodes, liver, or peritoneum (tissue that lines the wall of the abdomen and covers most of the organs in the abdomen).
- Whether the cancer can be completely removed by surgery.
- Whether the cancer is newly diagnosed or has recurred.
As in other gastrointestinal malignancies, the predominant modality of treatment is surgery when resection is possible, and cure relates to the ability to completely resect the cancer. The overall 5-year survival rate for resectable adenocarcinoma is only 20%. The 5-year survival rate for resectable leiomyosarcoma, the most common primary sarcoma of the small intestine, is approximately 50% 1.
Figure 1. Parts of the small intestine
Figure 2. Small intestines
Stage Information for Small Intestine Cancer
Staging is used to find out how far the cancer has spread, but treatment decisions are not based on stage.
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
The American Joint Committee on Cancer has designated staging by TNM classification to define small intestine cancer 3.
Table 1. Primary Tumor (T)
| TX | Primary tumor cannot be assessed. |
| T0 | No evidence of primary tumor. |
| Tis | Carcinoma in situ. |
| T1a | Tumor invades lamina propria. |
| T1b | Tumor invades submucosa. (a) |
| T2 | Tumor invades muscularis propria. |
| T3 | Tumor invades through the muscularis propria into the subserosa or into the nonperitonealized perimuscular tissue (mesentery or retroperitoneum) with extension ≤2 cm. (a) |
| T4 | Tumor perforates the visceral peritoneum or directly invades other organs or structures (includes other loops of small intestine, mesentery, or retroperitoneum >2 cm, and abdominal wall by way of serosa; for duodenum only, invasion of pancreas or bile duct). |
(a): The nonperitonealized perimuscular tissue is, for jejunum and ileum, part of the mesentery and, for duodenum in areas where serosa is lacking, part of the interface with the pancreas.
[Source 3]Table 2. Regional Lymph Nodes (N)
| NX | Regional lymph nodes cannot be assessed. |
| N0 | No regional lymph node metastasis. |
| N1 | Metastasis in 1–3 regional lymph nodes. |
| N2 | Metastases in ≥4 regional lymph nodes. |
Table 3. Distant Metastasis (M)
| M0 | No distant metastasis. |
| M1 | Distant metastasis. |
Table 4. Anatomic Stage/Prognostic Groups
| Stage | T | N | M |
|---|---|---|---|
| 0 | Tis | N0 | M0 |
| I | T1 | N0 | M0 |
| T2 | N0 | M0 | |
| IIA | T3 | N0 | M0 |
| IIB | T4 | N0 | M0 |
| IIIA | Any T | N1 | M0 |
| IIIB | Any T | N2 | M0 |
| IV | Any T | Any N | M1 |
Cancer may spread from where it began to other parts of the body.
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumor) and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor (metastatic tumor) in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumor (metastatic tumor) in another part of the body.
The metastatic tumor is the same type of cancer as the primary tumor. For example, if small intestine cancer spreads to the liver, the cancer cells in the liver are actually small intestine cancer cells. The disease is metastatic small intestine cancer, not liver cancer.
Small intestine cancer is grouped according to whether or not the tumor can be completely removed by surgery.
Treatment depends on whether the tumor can be removed by surgery and if the cancer is being treated as a primary tumor or is metastatic cancer.
- Recurrent Small Intestine Cancer
Recurrent small intestine cancer is cancer that has recurred (come back) after it has been treated. The cancer may come back in the small intestine or in other parts of the body.
Small intestine cancer signs and symptoms
Signs and symptoms of small intestine cancer include unexplained weight loss and abdominal pain.
These and other signs and symptoms may be caused by small intestine cancer or by other conditions. Check with your doctor if you have any of the following:
- Pain or cramps in the middle of the abdomen.
- Weight loss with no known reason.
- A lump in the abdomen.
- Blood in the stool.
Tests that examine the small intestine are used to detect (find), diagnose, and stage small intestine cancer
Procedures that make pictures of the small intestine and the area around it help diagnose small intestine cancer and show how far the cancer has spread. The process used to find out if cancer cells have spread within and around the small intestine is called staging.
In order to plan treatment, it is important to know the type of small intestine cancer and whether the tumor can be removed by surgery. Tests and procedures to detect, diagnose, and stage small intestine cancer are usually done at the same time. The following tests and procedures may be used:
- Physical exam and history : An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
- Blood chemistry studies : A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- Liver function tests : A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by the liver. A higher than normal amount of a substance can be a sign of liver disease that may be caused by small intestine cancer.
- Endoscopy : A procedure to look at organs and tissues inside the body to check for abnormal areas. There are different types of endoscopy:
Upper endoscopy : A procedure to look at the inside of the esophagus, stomach, and duodenum (first part of the small intestine, near the stomach). An endoscope is inserted through the mouth and into the esophagus, stomach, and duodenum. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer.
Capsule endoscopy : A procedure to look at the inside of the small intestine. A capsule that is about the size of a large pill and contains a light and a tiny wireless camera is swallowed by the patient. The capsule travels through the digestive tract, including the small intestine, and sends many pictures of the inside of the digestive tract to a recorder that is worn around the waist or over the shoulder. The pictures are sent from the recorder to a computer and viewed by the doctor who checks for signs of cancer. The capsule passes out of the body during a bowel movement.
Double balloon endoscopy : A procedure to look at the inside of the small intestine. A special instrument made up of two tubes (one inside the other) is inserted through the mouth or rectum and into the small intestine. The inside tube (an endoscope with a light and lens for viewing) is moved through part of the small intestine and a balloon at the end of it is inflated to keep the endoscope in place. Next, the outer tube is moved through the small intestine to reach the end of the endoscope, and a balloon at the end of the outer tube is inflated to keep it in place. Then, the balloon at the end of the endoscope is deflated and the endoscope is moved through the next part of the small intestine. These steps are repeated many times as the tubes move through the small intestine. The doctor is able to see the inside of the small intestine through the endoscope and use a tool to remove samples of abnormal tissue. The tissue samples are checked under a microscope for signs of cancer. This procedure may be done if the results of a capsule endoscopy are abnormal. This procedure is also called double balloon enteroscopy.
- Laparotomy : A surgical procedure in which an incision (cut) is made in the wall of the abdomen to check the inside of the abdomen for signs of disease. The size of the incision depends on the reason the laparotomy is being done. Sometimes organs or lymph nodes are removed or tissue samples are taken and checked under a microscope for signs of disease.
- Biopsy : The removal of cells or tissues so they can be viewed under a microscope to check for signs of cancer. This may be done during an endoscopy or laparotomy. The sample is checked by a pathologist to see if it contains cancer cells.
- Upper GI series with small bowel follow-through: A series of x-rays of the esophagus, stomach, and small bowel. The patient drinks a liquid that contains barium (a silver-white metallic compound). The liquid coats the esophagus, stomach, and small bowel. X-rays are taken at different times as the barium travels through the upper GI tract and small bowel.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
Small intestine cancer treatment
Different types of treatments are available for patients with small intestine cancer 9. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Three types of standard treatment are used:
Surgery
Surgery is the most common treatment of small intestine cancer. One of the following types of surgery may be done:
- Resection: Surgery to remove part or all of an organ that contains cancer. The resection may include the small intestine and nearby organs (if the cancer has spread). The doctor may remove the section of the small intestine that contains cancer and perform an anastomosis (joining the cut ends of the intestine together). The doctor will usually remove lymph nodes near the small intestine and examine them under a microscope to see whether they contain cancer.
- Bypass: Surgery to allow food in the small intestine to go around (bypass) a tumor that is blocking the intestine but cannot be removed.
Even if the doctor removes all the cancer that can be seen at the time of the surgery, some patients may be given radiation therapy after surgery to kill any cancer cells that are left. Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the cancer.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
The way the radiation therapy is given depends on the type of the cancer being treated. External radiation therapy is used to treat small intestine cancer.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy). The way the chemotherapy is given depends on the type and stage of the cancer being treated.
New types of treatment are being tested in clinical trials
Not every new treatment being studied are listed here because new treatment modalities are constantly being added.
Biologic therapy
Biologic therapy is a treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer. This type of cancer treatment is also called biotherapy or immunotherapy.
Radiation therapy with radiosensitizers
Radiosensitizers are drugs that make tumor cells more sensitive to radiation therapy. Combining radiation therapy with radiosensitizers may kill more tumor cells.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today’s standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Speak to your healthcare provider about the treatment options available including being involved as part of treatment clinical trials.
Follow-up tests may be needed.
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Small Intestine Adenocarcinoma Treatment
When possible, treatment of small intestine adenocarcinoma will be surgery to remove the tumor and some of the normal tissue around it 10.
Treatment of small intestine adenocarcinoma that cannot be removed by surgery may include the following:
- Surgery to bypass the tumor.
- Radiation therapy as palliative therapy to relieve symptoms and improve the patient’s quality of life.
- A clinical trial of radiation therapy with radiosensitizers, with or without chemotherapy.
- A clinical trial of new anticancer drugs.
- A clinical trial of biologic therapy.
Speak to your healthcare provider about the treatment options available including being involved as part of treatment clinical trials.
Small Intestine Leiomyosarcoma Treatment
When possible, treatment of small intestine leiomyosarcoma will be surgery to remove the tumor and some of the normal tissue around it.
Treatment of small intestine leiomyosarcoma that cannot be removed by surgery may include the following:
- Surgery (to bypass the tumor) and radiation therapy.
- Surgery, radiation therapy, or chemotherapy as palliative therapy to relieve symptoms and improve the patient’s quality of life.
- A clinical trial of new anticancer drugs.
- A clinical trial of biologic therapy.
Speak to your healthcare provider about the treatment options available including being involved as part of treatment clinical trials.
Recurrent Small Intestine Cancer
At the present time, no standard effective chemotherapy exists for patients with recurrent metastatic adenocarcinoma or leiomyosarcoma of the small intestine. These types of patients should be considered candidates for clinical trials evaluating the use of new anticancer drugs or biologic therapy in phase I and phase II trials 11.
Treatment of locally recurrent small intestine cancer may include the following:
- Surgery.
- Radiation therapy or chemotherapy as palliative therapy to relieve symptoms and improve the patient’s quality of life.
- A clinical trial of radiation therapy with radiosensitizers, with or without chemotherapy.
Speak to your healthcare provider about the treatment options available including being involved as part of treatment clinical trials.
Gastrointestinal stromal tumor
Gastrointestinal stromal tumor is a disease in which abnormal cells form in the tissues of the gastrointestinal tract 12. Gastrointestinal stromal tumors may be malignant (cancer) or benign (not cancer) 12. They are most common in the stomach and small intestine but may be found anywhere in or near the gastrointestinal tract. Some scientists believe that gastrointestinal stromal tumors begin in cells called interstitial cells of Cajal, in the wall of the gastrointestinal tract 12.
Although they comprise fewer than 1% of all gastrointestinal tumors, gastrointestinal stromal tumor are the most common mesenchymal tumors of the gastrointestinal tract 13. It has been estimated that there are 3,300 to 6,000 new gastrointestinal stromal tumor cases per year in the United States 14. A study based on Surveillance, Epidemiology and End Results registry data found that the age-adjusted yearly incidence of gastrointestinal stromal tumor in the United States was 6.8 per million from 1992 to 2000 15. However, the true incidence is not known, in part because many tumors have not been tested for the characteristic KIT or platelet-derived growth factor receptor alpha gene mutations. In addition, small, indolent gastrointestinal stromal tumor, only a few millimeters in diameter, are common in the general population and are not included in cancer registries 16. Gastrointestinal stromal tumor are equally distributed across all geographic and ethnic groups and men and women are equally affected. Most patients present between the ages of 50 and 80 17. The vast majority of gastrointestinal stromal tumor are sporadic, but there are rare familial forms associated with the characteristic heritable mutations in the KIT gene (or, rarely, in succinate dehydrogenase genes in Carney-Stratakis syndrome). Familial gastrointestinal stromal tumor may present as multiple primary tumors.
Gastrointestinal stromal tumor may be part of a genetic syndrome, but this is rare. A genetic syndrome is a set of symptoms or conditions that occur together and is usually caused by abnormal genes. The following genetic syndromes have been linked to gastrointestinal stromal tumor:
- Neurofibromatosis type 1 (NF1).
- Carney triad.
Gastrointestinal stromal tumor can occur anywhere along the GI tract, but most often are found in the stomach or small intestine. The American Joint Committee on Cancer Cancer Staging Manual lists the following approximate distributions 18:
- Stomach (60%).
- Small intestine (30%).
- Rectum (3%).
- Colon (1–2%).
- Esophagus (<1%).
- Omentum/mesentery (rare).
Less frequently, gastrointestinal stromal tumor may arise in the appendix, gallbladder, pancreas, retroperitoneum, and paravaginal and periprostatic tissues 19. Approximately 20% to 25% of gastric gastrointestinal stromal tumor and 40% to 50% of small intestinal gastrointestinal stromal tumor are clinically aggressive 20. It has been estimated that approximately 10% to 25% of patients present with metastatic disease 21.
Signs and symptoms of gastrointestinal stromal tumors
The clinical presentation of patients with GIST varies depending on the anatomic location of the tumor and the tumor size and aggressiveness 22. The most common presentation of GIST is GI bleeding, which may be acute (melena or hematemesis) or chronic and results in anemia 20. Signs and symptoms of gastrointestinal stromal tumors include blood in the stool or vomit.
These and other signs and symptoms may be caused by a gastrointestinal stromal tumor or by other conditions. Check with your doctor if you have any of the following:
- Blood (either bright red or very dark) in the stool or vomit.
- Pain in the abdomen, which may be severe.
- Feeling very tired.
- Trouble or pain when swallowing.
- Feeling full after only a little food is eaten.
Tests that examine the GI tract are used to detect (find) and diagnose gastrointestinal stromal tumors.
The following tests and procedures may be used:
- Physical exam and history : An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- Endoscopic ultrasound and biopsy : Endoscopy and ultrasound are used to make an image of the upper GI tract and a biopsy is done. An endoscope (a thin, tube-like instrument with a light and a lens for viewing) is inserted through the mouth and into the esophagus, stomach, and first part of the small intestine. A probe at the end of the endoscope is used to bounce high-energy sound waves (ultrasound) off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. This procedure is also called endosonography. Guided by the sonogram, the doctor removes tissue using a thin, hollow needle. A pathologist views the tissue under a microscope to look for cancer cells.
If cancer is found, the following tests may be done to study the cancer cells:
- Immunohistochemistry : A test that uses antibodies to check for certain antigens in a sample of tissue. The antibody is usually linked to a radioactive substance or a dye that causes the tissue to light up under a microscope. This type of test may be used to tell the difference between different types of cancer.
- Mitotic rate : A measure of how fast the cancer cells are dividing and growing. The mitotic rate is found by counting the number of cells dividing in a certain amount of cancer tissue.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) and treatment options depend on the following:
- How quickly the cancer cells are growing and dividing.
- The size of the tumor.
- Where the tumor is in the body.
- Whether the tumor can be completely removed by surgery.
- Whether the tumor has spread to other parts of the body.
Stages of Gastrointestinal Stromal Tumors
After a gastrointestinal stromal tumor has been diagnosed, tests are done to find out if cancer cells have spread within the gastrointestinal tract or to other parts of the body.
The process used to find out if cancer has spread within the gastrointestinal (GI) tract or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. The following tests and procedures may be used in the staging process:
- PET scan (positron emission tomography scan): A procedure to find malignant tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- Chest x-ray : An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- Bone scan : A procedure to check if there are rapidly dividing cells, such as cancer cells, in the bone. A very small amount of radioactive material is injected into a vein and travels through the bloodstream. The radioactive material collects in the bones and is detected by a scanner.
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
Cancer may spread from where it began to other parts of the body.
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumor) and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor (metastatic tumor) in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumor (metastatic tumor) in another part of the body.
The metastatic tumor is the same type of tumor as the primary tumor. For example, if a gastrointestinal stromal tumor (GIST) spreads to the liver, the tumor cells in the liver are actually GIST cells. The disease is metastatic GIST, not liver cancer.
The results of diagnostic and staging tests are used to plan treatment.
For many cancers it is important to know the stage of the cancer in order to plan treatment. However, the treatment of GIST is not based on the stage of the cancer. Treatment is based on whether the tumor can be removed by surgery and if the tumor has spread to other parts of the abdomen or to distant parts of the body.
Treatment is based on whether the tumor is:
- Resectable: These tumors can be removed by surgery .
- Unresectable: These tumors cannot be completely removed by surgery.
- Metastatic and recurrent: Metastatic tumors have spread to other parts of the body. Recurrent tumors have recurred (come back) after treatment.
- Recurrent GISTs may come back in the gastrointestinal tract or in other parts of the body. They are usually found in the abdomen, peritoneum, and/or liver.
- Refractory: These tumors have not gotten better with treatment.
Treatment Options for Gastrointestinal stromal tumor
Different types of treatments are available for patients with gastrointestinal stromal tumors (GISTs). Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Speak to your healthcare provider about the treatment options available including being involved as part of treatment clinical trials.
Four types of standard treatment are used:
- Surgery
If the GIST has not spread and is in a place where surgery can be safely done, the tumor and some of the tissue around it may be removed. Sometimes surgery is done using a laparoscope (a thin, lighted tube) to see inside the body. Small incisions (cuts) are made in the wall of the abdomen and a laparoscope is inserted into one of the incisions. Instruments may be inserted through the same incision or through other incisions to remove organs or tissues.
- Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells.
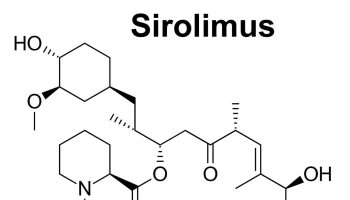
Tyrosine kinase inhibitors (TKIs) are targeted therapy drugs that block signals needed for tumors to grow. TKIs may be used to treat GISTs that cannot be removed by surgery or to shrink GISTs so they become small enough to be removed by surgery. Imatinib mesylate and sunitinib are two TKIs used to treat GISTs. TKIs are sometimes given for as long as the tumor does not grow and serious side effects do not occur.
- Watchful waiting
Watchful waiting is closely monitoring a patient’s condition without giving any treatment until signs or symptoms appear or change.
- Supportive care
If a GIST gets worse during treatment or there are side effects, supportive care is usually given. The goal of supportive care is to prevent or treat the symptoms of a disease, side effects caused by treatment, and psychological, social, and spiritual problems related to a disease or its treatment. Supportive care helps improve the quality of life of patients who have a serious or life-threatening disease. Radiation therapy is sometimes given as supportive care to relieve pain in patients with large tumors that have spread.
- New types of treatment are being tested in clinical trials
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today’s standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Speak to your healthcare provider about the treatment options available including being involved as part of treatment clinical trials.
Follow-up tests may be needed.
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Follow-up for GISTs that were removed by surgery may include CT scan of the liver and pelvis or watchful waiting. For GISTs that are treated with tyrosine kinase inhibitors, follow-up tests, such as CT, MRI, or PET scans, may be done to check how well the targeted therapy is working.
Resectable Gastrointestinal Stromal Tumors
Resectable gastrointestinal stromal tumors (GISTs) can be completely or almost completely removed by surgery. Treatment may include the following:
- Surgery to remove tumors that are 2 centimeters or larger. Laparoscopic surgery may be done if the tumor is 5 cm or smaller. If there are cancer cells remaining at the edges of the area where the tumor was removed, watchful waiting or targeted therapy with imatinib mesylate may follow.
- A clinical trial of targeted therapy with imatinib mesylate following surgery, to decrease the chance the tumor will recur (come back).
Unresectable Gastrointestinal Stromal Tumors
Unresectable GISTs cannot be completely removed by surgery because they are too large or in a place where there would be too much damage to nearby organs if the tumor is removed. Treatment is usually a clinical trial of targeted therapy with imatinib mesylate to shrink the tumor, followed by surgery to remove as much of the tumor as possible.
Metastatic and Recurrent Gastrointestinal Stromal Tumors
Treatment of GISTs that are metastatic (spread to other parts of the body) or recurrent (came back after treatment) may include the following:
- Targeted therapy with imatinib mesylate.
- Targeted therapy with sunitinib, if the tumor begins to grow during imatinib mesylate therapy or if the side effects are too bad.
- Surgery to remove tumors that have been treated with targeted therapy and are shrinking, stable (not changing), or that have slightly increased in size.
- Targeted therapy may continue after surgery.
- Surgery to remove tumors when there are serious complications, such as bleeding, a hole in the gastrointestinal (GI) tract, a blocked GI tract, or infection.
- A clinical trial of a new treatment.
Refractory Gastrointestinal Stromal Tumors
Many GISTs treated with a tyrosine kinase inhibitor (TKI) become refractory (stop responding) to the drug after a while. Treatment is usually a clinical trial with a different TKI or a clinical trial of a new drug.
Gastrointestinal Carcinoid Tumors
A gastrointestinal carcinoid tumor is cancer that forms in the lining of the gastrointestinal tract 23.
Gastrointestinal carcinoid tumors form from a certain type of neuroendocrine cell (a type of cell that is like a nerve cell and a hormone -making cell). These cells are scattered throughout the chest and abdomen but most are found in the gastrointestinal tract. Neuroendocrine cells make hormones that help control digestive juices and the muscles used in moving food through the stomach and intestines. A gastrointestinal carcinoid tumor may also make hormones and release them into the body.
Gastrointestinal carcinoid tumors are rare and most grow very slowly. Most of them occur in the small intestine, rectum, and appendix. Sometimes more than one tumor will form.
Health history can affect the risk of gastrointestinal carcinoid tumors.
Anything that increases a person’s chance of developing a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer. Talk to your doctor if you think you may be at risk.
Risk factors for GI carcinoid tumors include the following:
- Having a family history of multiple endocrine neoplasia type 1 (MEN1) syndrome or neurofibromatosis type 1 (NF1) syndrome.
- Having certain conditions that affect the stomach’s ability to make stomach acid, such as atrophic gastritis, pernicious anemia, or Zollinger-Ellison syndrome.
Some gastrointestinal carcinoid tumors have no signs or symptoms in the early stages.
Signs and symptoms may be caused by the growth of the tumor and/or the hormones the tumor makes. Some tumors, especially tumors of the stomach or appendix, may not cause signs or symptoms. Carcinoid tumors are often found during tests or treatments for other conditions.
Carcinoid tumors in the small intestine (duodenum, jejunum, and ileum), colon, and rectum sometimes cause signs or symptoms as they grow or because of the hormones they make. Other conditions may cause the same signs or symptoms. Check with your doctor if you have any of the following:
Duodenum
Signs and symptoms of GI carcinoid tumors in the duodenum (first part of the small intestine, that connects to the stomach) may include the following:
- Abdominal pain.
- Constipation.
- Diarrhea.
- Change in stool color.
- Nausea.
- Vomiting.
- Jaundice (yellowing of the skin and whites of the eyes).
- Heartburn.
Jejunum and ileum
Signs and symptoms of GI carcinoid tumors in the jejunum (middle part of the small intestine) and ileum (last part of the small intestine, that connects to the colon) may include the following:
- Abdominal pain.
- Weight loss for no known reason.
- Feeling very tired.
- Feeling bloated
- Diarrhea.
- Nausea.
- Vomiting.
Colon
Signs and symptoms of GI carcinoid tumors in the colon may include the following:
- Abdominal pain.
- Weight loss for no known reason.
Rectum
Signs and symptoms of GI carcinoid tumors in the rectum may include the following:
- Blood in the stool.
- Pain in the rectum.
- Constipation.
Carcinoid syndrome may occur if the tumor spreads to the liver or other parts of the body.
The hormones made by gastrointestinal carcinoid tumors are usually destroyed by liver enzymes in the blood. If the tumor has spread to the liver and the liver enzymes cannot destroy the extra hormones made by the tumor, high amounts of these hormones may remain in the body and cause carcinoid syndrome. This can also happen if tumor cells enter the blood. Signs and symptoms of carcinoid syndrome include the following:
- Redness or a feeling of warmth in the face and neck.
- Abdominal pain.
- Feeling bloated.
- Diarrhea.
- Wheezing or other trouble breathing.
- Fast heartbeat.
These signs and symptoms may be caused by gastrointestinal carcinoid tumors or by other conditions. Talk to your doctor if you have any of these signs or symptoms.
Imaging studies and tests that examine the blood and urine are used to detect (find) and diagnose gastrointestinal carcinoid tumors.
The following tests and procedures may be used:
- Physical exam and history : An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
- Blood chemistry studies : A procedure in which a blood sample is checked to measure the amounts of certain substances, such as hormones, released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease. The blood sample is checked to see if it contains a hormone produced by carcinoid tumors. This test is used to help diagnose carcinoid syndrome.
- Tumor marker test : A procedure in which a sample of blood, urine, or tissue is checked to measure the amounts of certain substances, such as chromogranin A, made by organs, tissues, or tumor cells in the body. Chromogranin A is a tumor marker. It has been linked to neuroendocrine tumors when found in increased levels in the body.
- Twenty-four-hour urine test: A test in which urine is collected for 24 hours to measure the amounts of certain substances, such as 5-HIAA or serotonin (hormone). An unusual (higher or lower than normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. This test is used to help diagnose carcinoid syndrome.
- MIBG scan : A procedure used to find neuroendocrine tumors, such as carcinoid tumors. A very small amount of radioactive material called MIBG (metaiodobenzylguanidine) is injected into a vein and travels through the bloodstream. Carcinoid tumors take up the radioactive material and are detected by a device that measures radiation.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging
- PET scan (positron emission tomography scan): A procedure to find malignant tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells.
- Endoscopic ultrasound: A procedure in which an endoscope is inserted into the body, usually through the mouth or rectum. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. A probe at the end of the endoscope is used to bounce high-energy sound waves (ultrasound) off internal tissues or organs, such as the stomach, small intestine, colon, or rectum, and make echoes. The echoes form a picture of body tissues called a sonogram. This procedure is also called endosonography.
- Upper endoscopy : A procedure to look at organs and tissues inside the body to check for abnormal areas. An endoscope is inserted through the mouth and passed through the esophagus into the stomach. Sometimes the endoscope also is passed from the stomach into the small intestine. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of disease.
- Colonoscopy : A procedure to look inside the rectum and colon for polyps, abnormal areas, or cancer. A colonoscope is inserted through the rectum into the colon. A colonoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove polyps or tissue samples, which are checked under a microscope for signs of cancer.
- Capsule endoscopy : A procedure used to see all of the small intestine. The patient swallows a capsule that contains a tiny camera. As the capsule moves through the gastrointestinal tract, the camera takes pictures and sends them to a receiver worn on the outside of the body.
- Biopsy : The removal of cells or tissues so they can be viewed under a microscope to check for signs of cancer. Tissue samples may be taken during endoscopy and colonoscopy.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) and treatment options depend on the following:
- Where the tumor is in the gastrointestinal tract.
- The size of the tumor.
- Whether the cancer has spread from the stomach and intestines to other parts of the body, such as the liver or lymph nodes.
- Whether the patient has carcinoid syndrome or has carcinoid heart syndrome.
- Whether the cancer can be completely removed by surgery.
- Whether the cancer is newly diagnosed or has recurred.
The plan for cancer treatment depends on where the carcinoid tumor is found and whether it can be removed by surgery.
For many cancers it is important to know the stage of the cancer in order to plan treatment. However, the treatment of gastrointestinal carcinoid tumors is not based on the stage of the cancer. Treatment depends mainly on whether the tumor can be removed by surgery and if the tumor has spread.
Treatment is based on whether the tumor:
- Can be completely removed by surgery.
- Has spread to other parts of the body.
- Has come back after treatment. The tumor may come back in the stomach or intestines or in other parts of the body.
- Has not gotten better with treatment.
There are different types of treatment for patients with gastrointestinal carcinoid tumors.
Different types of treatment are available for patients with gastrointestinal carcinoid tumor. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Four types of standard treatment are used:
Surgery
Treatment of GI carcinoid tumors usually includes surgery. One of the following surgical procedures may be used:
- Endoscopic resection: Surgery to remove a small tumor that is on the inside lining of the GI tract. An endoscope is inserted through the mouth and passed through the esophagus to the stomach and sometimes, the duodenum. An endoscope is a thin, tube-like instrument with a light, a lens for viewing, and a tool for removing tumor tissue.
- Local excision: Surgery to remove the tumor and a small amount of normal tissue around it.
- Resection: Surgery to remove part or all of the organ that contains cancer. Nearby lymph nodes may also be removed.
- Cryosurgery: A treatment that uses an instrument to freeze and destroy carcinoid tumor tissue. This type of treatment is also called cryotherapy. The doctor may use ultrasound to guide the instrument.
- Radiofrequency ablation: The use of a special probe with tiny electrodes that release high-energy radio waves (similar to microwaves) that kill cancer cells. The probe may be inserted through the skin or through an incision (cut) in the abdomen.
- Liver transplant: Surgery to remove the whole liver and replace it with a healthy donated liver.
- Hepatic artery embolization: A procedure to embolize (block) the hepatic artery, which is the main blood vessel that brings blood into the liver. Blocking the flow of blood to the liver helps kill cancer cells growing there.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the cancer.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
Radiopharmaceutical therapy is a type of internal radiation therapy. Radiation is given to the tumor using a drug that has a radioactive substance, such as iodine I 131, attached to it. The radioactive substance kills the tumor cells.
External and internal radiation therapy are used to treat gastrointestinal carcinoid tumors that have spread to other parts of the body.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping the cells from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy).
Chemoembolization of the hepatic artery is a type of regional chemotherapy that may be used to treat a gastrointestinal carcinoid tumor that has spread to the liver. The anticancer drug is injected into the hepatic artery through a catheter (thin tube). The drug is mixed with a substance that embolizes (blocks) the artery, and cuts off blood flow to the tumor. Most of the anticancer drug is trapped near the tumor and only a small amount of the drug reaches other parts of the body. The blockage may be temporary or permanent, depending on the substance used to block the artery. The tumor is prevented from getting the oxygen and nutrients it needs to grow. The liver continues to receive blood from the hepatic portal vein, which carries blood from the stomach and intestine.
The way the chemotherapy is given depends on the type and stage of the cancer being treated.
Hormone therapy
Hormone therapy with a somatostatin analogue is a treatment that stops extra hormones from being made. GI carcinoid tumors are treated with octreotide or lanreotide which are injected under the skin or into the muscle. Octreotide and lanreotide may also have a small effect on stopping tumor growth.
Treatment for carcinoid syndrome may also be needed.
Treatment of carcinoid syndrome may include the following:
- Hormone therapy with a somatostatin analogue stops extra hormones from being made. Carcinoid syndrome is treated with octreotide or lanreotide to lessen flushing and diarrhea. Octreotide and lanreotide may also help slow tumor growth.
- Interferon therapy stimulates the body’s immune system to work better and lessens flushing and diarrhea. Interferon may also help slow tumor growth.
- Taking medicine for diarrhea.
- Taking medicine for skin rashes.
- Taking medicine to breathe easier.
- Taking medicine before having anesthesia for a medical procedure.
Other ways to help treat carcinoid syndrome include avoiding things that cause flushing or difficulty breathing such as alcohol, nuts, certain cheeses and foods with capsaicin, such as chili peppers. Avoiding stressful situations and certain types of physical activity can also help treat carcinoid syndrome.
For some patients with carcinoid heart syndrome, a heart valve replacement may be done.
New types of treatment are being tested in clinical trials.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. Several types of targeted therapy are being studied in the treatment of GI carcinoid tumors.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today’s standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Speak to your healthcare provider about the treatment options available including being involved as part of treatment clinical trials.
Follow-up tests may be needed.
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Carcinoid Tumors in the Small Intestine
It is not clear what the best treatment is for GI carcinoid tumors in the duodenum (first part of the small intestine, that connects to the stomach). Treatment may include the following:
- Endoscopic surgery (resection) for small tumors.
- Surgery (local excision) to remove slightly larger tumors.
- Surgery (resection) to remove the tumor and nearby lymph nodes.
Treatment of GI carcinoid tumors in the jejunum (middle part of the small intestine) and ileum (last part of the small intestine, that connects to the colon) may include the following:
- Surgery (resection) to remove the tumor and the membrane that connects the intestines to the back of the abdominal wall. Nearby lymph nodes are also removed.
- A second surgery to remove the membrane that connects the intestines to the back of the abdominal wall, if any tumor remains or the tumor continues to grow.
- Hormone therapy.
Clinical trials are taking place in many parts of the country. Speak to your healthcare provider about the treatment options available including being involved as part of treatment clinical trials.
Metastatic Gastrointestinal Carcinoid Tumors
Distant metastases
Treatment of distant metastases of GI carcinoid tumors is usually palliative therapy to relieve symptoms and improve quality of life. Treatment may include the following:
- Surgery (resection) to remove as much of the tumor as possible.
- Hormone therapy.
- Radiopharmaceutical therapy.
- External radiation therapy for cancer that has spread to the bone, brain, or spinal cord.
- A clinical trial of a new treatment.
Liver metastases
Treatment of cancer that has spread to the liver may include the following:
- Surgery (local excision) to remove the tumor from the liver.
- Hepatic artery embolization.
- Cryosurgery.
- Radiofrequency ablation.
- Liver transplant.
Clinical trials are taking place in many parts of the country. Speak to your healthcare provider about the treatment options available including being involved as part of treatment clinical trials.
Recurrent Gastrointestinal Carcinoid Tumors
Treatment of recurrent GI carcinoid tumors may include the following:
- Surgery (local excision) to remove part or all of the tumor.
- A clinical trial of a new treatment.
Clinical trials are taking place in many parts of the country. Speak to your healthcare provider about the treatment options available including being involved as part of treatment clinical trials.
- Small Intestine Cancer Treatment. National Cancer Institute. https://www.cancer.gov/types/small-intestine/patient/small-intestine-treatment-pdq[↩][↩]
- American Cancer Society: Cancer Facts and Figures 2017. Atlanta, Ga: American Cancer Society, 2017. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf[↩]
- Small intestine. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 127-32.[↩][↩][↩][↩][↩][↩]
- Cellular Classification of Small Intestine Cancer. National Cancer Institute. https://www.cancer.gov/types/small-intestine/hp/small-intestine-treatment-pdq#section/_3[↩][↩][↩][↩]
- Zureikat AH, Heller MT, Zeh HJ III: Cancer of the small intestine. In: DeVita VT Jr, Lawrence TS, Rosenberg SA: Cancer: Principles and Practice of Oncology. 9th ed. Philadelphia, Pa: Lippincott Williams & Wilkins, 2011, pp 1048-59.[↩]
- Serour F, Dona G, Birkenfeld S, et al.: Primary neoplasms of the small bowel. J Surg Oncol 49 (1): 29-34, 1992. https://www.ncbi.nlm.nih.gov/pubmed/1548877[↩]
- Matsuo S, Eto T, Tsunoda T, et al.: Small bowel tumors: an analysis of tumor-like lesions, benign and malignant neoplasms. Eur J Surg Oncol 20 (1): 47-51, 1994. https://www.ncbi.nlm.nih.gov/pubmed/8131869[↩]
- Chow JS, Chen CC, Ahsan H, et al.: A population-based study of the incidence of malignant small bowel tumours: SEER, 1973-1990. Int J Epidemiol 25 (4): 722-8, 1996. https://www.ncbi.nlm.nih.gov/pubmed/8921448[↩]
- North JH, Pack MS: Malignant tumors of the small intestine: a review of 144 cases. Am Surg 66 (1): 46-51, 2000. https://www.ncbi.nlm.nih.gov/pubmed/10651347[↩]
- Rose DM, Hochwald SN, Klimstra DS, et al.: Primary duodenal adenocarcinoma: a ten-year experience with 79 patients. J Am Coll Surg 183 (2): 89-96, 1996. https://www.ncbi.nlm.nih.gov/pubmed/8696551[↩]
- Recurrent Small Intestine Cancer. National Cancer Institute. https://www.cancer.gov/types/small-intestine/hp/small-intestine-treatment-pdq#section/_72[↩]
- Gastrointestinal Stromal Tumors. National Cancer Institute. https://www.cancer.gov/types/soft-tissue-sarcoma/hp/gist-treatment-pdq[↩][↩][↩]
- Judson I, Demetri G: Advances in the treatment of gastrointestinal stromal tumours. Ann Oncol 18 (Suppl 10): x20-4, 2007. https://www.ncbi.nlm.nih.gov/pubmed/17761719[↩]
- Corless CL, Heinrich MC: Molecular pathobiology of gastrointestinal stromal sarcomas. Annu Rev Pathol 3: 557-86, 2008. https://www.ncbi.nlm.nih.gov/pubmed/18039140[↩]
- Tran T, Davila JA, El-Serag HB: The epidemiology of malignant gastrointestinal stromal tumors: an analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol 100 (1): 162-8, 2005. https://www.ncbi.nlm.nih.gov/pubmed/15654796[↩]
- Agaimy A, Wünsch PH, Hofstaedter F, et al.: Minute gastric sclerosing stromal tumors (GIST tumorlets) are common in adults and frequently show c-KIT mutations. Am J Surg Pathol 31 (1): 113-20, 2007. https://www.ncbi.nlm.nih.gov/pubmed/17197927[↩]
- Nowain A, Bhakta H, Pais S, et al.: Gastrointestinal stromal tumors: clinical profile, pathogenesis, treatment strategies and prognosis. J Gastroenterol Hepatol 20 (6): 818-24, 2005. https://www.ncbi.nlm.nih.gov/pubmed/15946127[↩]
- Gastrointestinal stromal tumor. In: Edge SB, Byrd DR, Compton CC, et al., eds.: AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer, 2010, pp 175-80.[↩]
- Corless CL, Fletcher JA, Heinrich MC: Biology of gastrointestinal stromal tumors. J Clin Oncol 22 (18): 3813-25, 2004. https://www.ncbi.nlm.nih.gov/pubmed/15365079[↩]
- Miettinen M, Lasota J: Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis. Arch Pathol Lab Med 130 (10): 1466-78, 2006. https://www.ncbi.nlm.nih.gov/pubmed/17090188[↩][↩]
- DeMatteo RP, Lewis JJ, Leung D, et al.: Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg 231 (1): 51-8, 2000. https://www.ncbi.nlm.nih.gov/pubmed/10636102[↩]
- Demetri GD: Gastrointestinal stromal tumor. In: DeVita VT Jr, Lawrence TS, Rosenberg SA: Cancer: Principles and Practice of Oncology. 9th ed. Philadelphia, Pa: Lippincott Williams & Wilkins, 2011, pp 1060-73.[↩]
- Gastrointestinal Carcinoid Tumors. National Cancer Institute. https://www.cancer.gov/types/gi-carcinoid-tumors/hp/gi-carcinoid-treatment-pdq[↩]