Contents
What is an absence seizure
Absence seizures are characterized by sudden, brief (lasting a few seconds), frequent periods of unconsciousness, which may be accompanied by automatic movements (simple automatisms or clonic, atonic, or autonomic components) 1. Absence seizure was previously known as ‘petit mal seizure’. Typical absence seizures are often confused with complex partial seizures — especially in cases of prolonged seizure with automatisms. However, the abrupt ending of typical absence seizures, without a postictcal phase, is the most useful clinical feature in distinguishing the two types.
Typical absence seizures should not be confused with atypical absence seizures — which differ markedly in EEG findings and ictal behaviour, and usually present with other seizure types in a child with a background of learning disability and severe epilepsy. Typical absence seizures may be the sole seizure type experienced by a child. If this is the case, and the child is of normal development and has no structural lesions, the child is said to have childhood absence epilepsy. Alternatively, typical absence seizures may coexist in children with other epileptic syndromes — such as juvenile myoclonic epilepsy or juvenile absence epilepsy, in which other seizure types are also present. This differentiation into typical versus atypical seizures is important, as the natural history and response to treatment vary between the two groups.
Absence seizures may occur alone or may coexist with other types of seizures in a child with other epileptic syndromes. They’re more common in children than in adults. Some children who have them also develop other seizures. Many children outgrow absence seizures in their teens.
About 10% of seizures in children with epilepsy are typical absence seizures. Annual incidence has been estimated at 0.7 to 4.6/100,000 people in the general population, and 6 to 8/100,000 in children aged 0 to 15 years 1. Prevalence is 5 to 50/100,000 people in the general population. Similar figures were found in the USA (Connecticut) and in Europe-based (Scandinavia, France) population studies. Age of onset ranges from 3 to 13 years, with a peak at 6 to 7 years 1.
- Absence seizures have a typical spike and wave pattern on the EEG – showing regular symmetrical generalized spike and wave complexes with a frequency of 3 Hz, and usually occur in children with normal development and intelligence. Atypical absence seizures have different EEG changes and clinical manifestations, and have a different natural history and response to treatment.
- Absence seizures can be differentiated from complex partial seizures by their abrupt ending and lack of a postictal phase.
- About 10% of seizures in children with epilepsy are typical absence seizures, with genetic factors considered to be the main cause. Where they are the only manifestation of epilepsy, they generally resolve spontaneously by the age of 12 years.
Generalized absence seizures usually start in childhood, but can occur in adults. Absence seizures are brief and characterized by staring, loss of expression, unresponsiveness and stopping activity. Sometimes eye blinking or upward eye movements are seen. The person usually recovers immediately and resumes their previous activity, with no memory of the event.
Someone having an absence seizure may look like he or she is staring blankly into space for a few seconds. Then, there is a quick return to a normal level of alertness. This type of seizure usually doesn’t lead to physical injury.
Absence seizures usually can be controlled with anti-seizure medications.
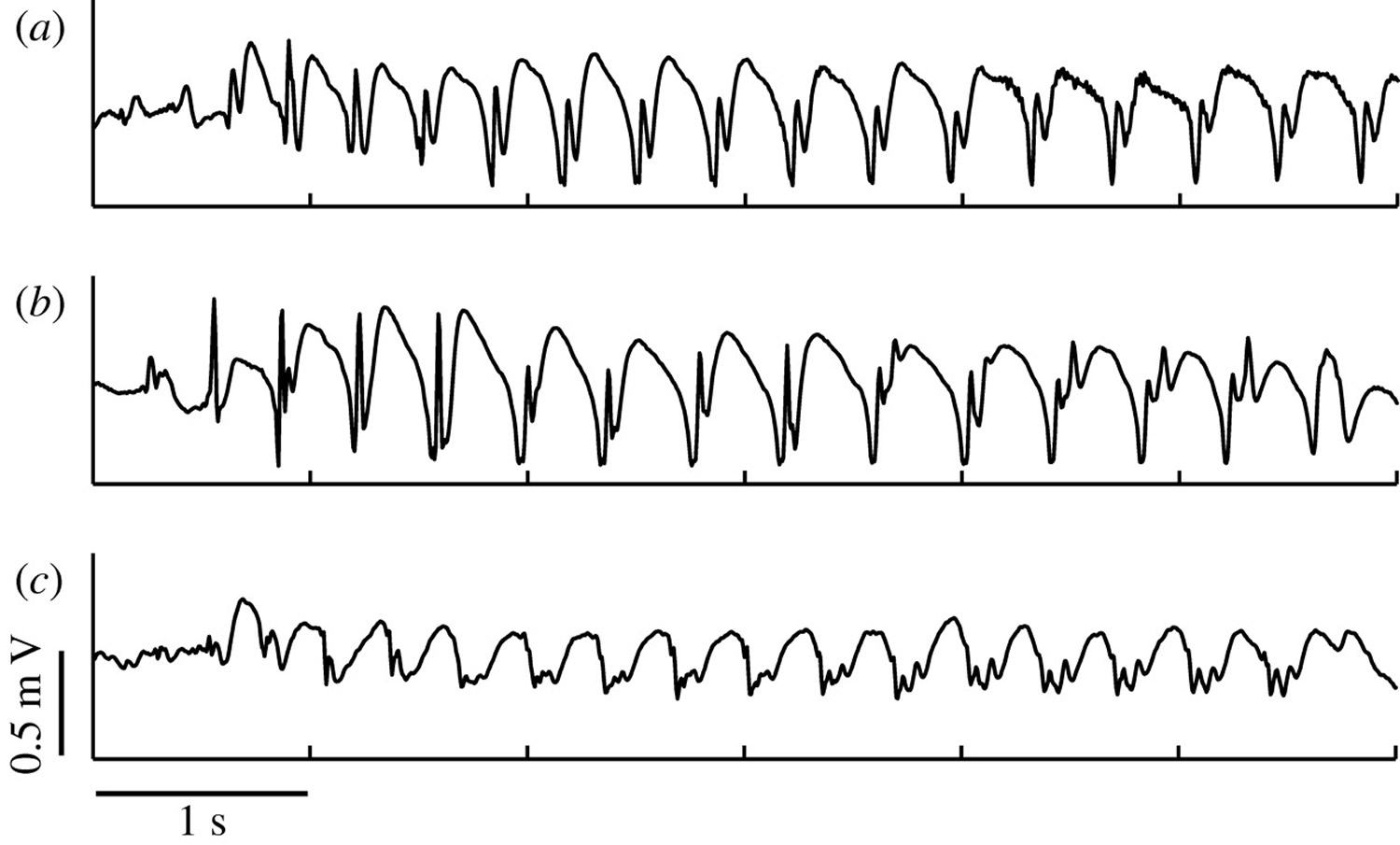
Figure 1. Absence seizure EEG
Note: The EEG recordings of three different patients with childhood absence epilepsy. (a) A typical spike–wave oscillation. (b) During a seizure, the EEG profile can show additional spikes. (c) A similar EEG recording as in (b). Again observe a polyspike–wave pattern; however, it is difficult to discern whether the spikes are leading the wave or vice versa.
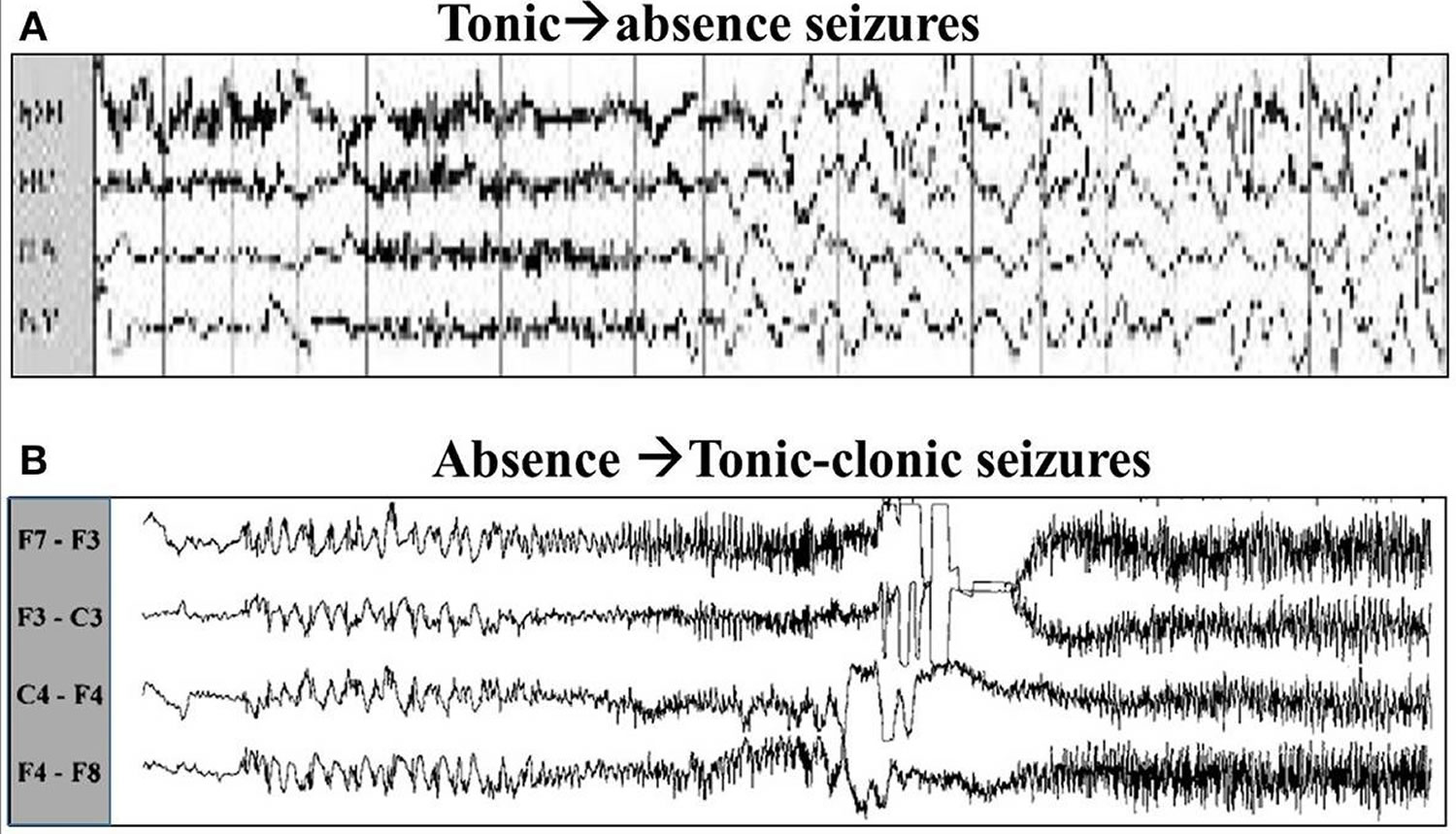
[Source 2]Figure 2. Absence seizures EEG
[Sources 3, 4]Absence seizure prognosis
In childhood absence epilepsy, in which typical absence seizures are the only type of seizures suffered by the child, seizures generally cease spontaneously by 12 years of age or sooner. Less than 10% of children develop infrequent generalized tonic clonic seizures and it is rare for them to continue having absence seizures. In other epileptic syndromes (in which absence seizures may coexist with other types of seizure) prognosis is varied, depending on the syndrome. Absence seizures have a significant impact on quality of life. The episode of unconsciousness may occur at any time and usually without warning. Affected children need to take precautions to prevent injury during absences and should refrain from activities that would put them at risk if seizures occurred (e.g., climbing heights, swimming unsupervised, or cycling on busy roads). Often, school staff members are the first to notice the recurrent episodes of absence seizures, and treatment is generally initiated because of the adverse impact on learning.
Absence seizure complications
While most children outgrow absence seizures, some:
- Must take anti-seizure medications throughout life to prevent seizures
- Eventually have full convulsions, such as generalized tonic-clonic seizures
Other complications can include:
- Learning difficulties
- Behavior problems
- Social isolation
Absence seizure causes
Many children appear to have a genetic predisposition to absence seizures.
In general, seizures are caused by abnormal electrical impulses from nerve cells (neurons) in the brain. The brain’s nerve cells normally send electrical and chemical signals across the synapses that connect them.
In people who have seizures, the brain’s usual electrical activity is altered. During an absence seizure, these electrical signals repeat themselves over and over in a three-second pattern.
People who have seizures may also have altered levels of the chemical messengers that help the nerve cells communicate with one another (neurotransmitters).
Risk factors for absence seizures
Certain factors are common to children who have absence seizures, including:
- Age. Absence seizures are more common in children between the ages of 4 and 14.
- Sex. Absence seizures are more common in girls.
- Family members who have seizures. Nearly half of children with absence seizures have a close relative who has seizures.
Absence seizure signs and symptoms
An indication of simple absence seizure is a vacant stare, which may be mistaken for a lapse in attention that lasts about 10 seconds, though it may last as long as 20 seconds, without any confusion, headache or drowsiness afterward.
Most absence seizures last only a few seconds. They often involve staring episodes. The episodes may:
- Occur many times a day
- Occur for weeks to months before being noticed
- Interfere with school and learning
- Be mistaken for lack of attention, daydreaming or other misbehavior
Unexplained difficulties in school and learning difficulties may be the first sign of absence seizures.
Signs and symptoms of absence seizures usually include:
- Sudden stop in motion without falling
- Lip smacking
- Eyelid flutters
- Chewing motions
- Finger rubbing
- Small movements of both hands
Afterward, there’s no memory of the incident. Some people have many episodes daily, which interfere with school or daily activities.
A child may have absence seizures for some time before an adult notices the seizures, because they’re so brief. A decline in a child’s learning ability may be the first sign of this disorder. Teachers may comment about a child’s inability to pay attention or that a child is often daydreaming.
During the seizure, the person may:
- Stop walking and start again a few seconds later
- Stop talking in mid-sentence and start again a few seconds later
The person usually does not fall during the seizure.
Right after the seizure, the person is usually:
- Wide awake
- Thinking clearly
- Unaware of the seizure
Specific symptoms of typical absence seizures may include:
- Changes in muscle activity, such as no movement, hand fumbling, fluttering eyelids, lip smacking, chewing
- Changes in alertness (consciousness), such as staring episodes, lack of awareness of surroundings, sudden halt in movement, talking, and other awake activities
Some absence seizures begin slower and last longer. These are called atypical absence seizures. Symptoms are similar to regular absence seizures, but muscle activity changes may be more noticeable.
Absence seizures diagnosis
Your doctor will ask for a detailed description of the seizures and conduct a physical exam. Tests may include:
- Electroencephalography (EEG). This painless procedure measures waves of electrical activity in the brain. Brain waves are transmitted to the EEG machine via small electrodes attached to the scalp with paste or an elastic cap. Rapid breathing (hyperventilation) during an EEG study can trigger an absence seizure. During a seizure, the pattern on the EEG differs from the normal pattern.
- Brain scans. In absence seizures, brain-imaging studies, such as head CT or magnetic resonance imaging (MRI), will be normal. But tests such as MRI can produce detailed images of the brain, which can help rule out other problems, such as a stroke or a brain tumor. Because your child will need to hold still for long periods, talk with your doctor about the possible use of sedation.
- Blood tests may also be ordered to check for other health problems that may be causing the seizures.
Absence seizure treatment
Your doctor likely will start at the lowest dose of anti-seizure medication possible and increase the dosage as needed to control the seizures. Children may be able to taper off anti-seizure medications, under a doctor’s supervision, after they’ve been seizure-free for two years.
Absence seizure medication
- Ethosuximide (Zarontin). This is the drug most doctors start with for absence seizures. In most cases, seizures respond well to this drug. Possible side effects include nausea, vomiting, sleepiness, trouble sleeping, hyperactivity. Ethosuximide has been associated with aplastic anaemia, skin reactions, and renal and hepatic impairment.
- Valproic acid (Depakene). Girls who continue to need medication into adulthood should discuss potential risks of valproic acid with their doctors. Valproic acid has been associated with higher risk of birth defects in babies, and doctors advise women against using it during pregnancy or while trying to conceive. Doctors may recommend the use of valproic acid in children who have both absence and grand mal (tonic-clonic) seizures. Valproate has been associated with behavioral and cognitive abnormalities, liver necrosis, and pancreatitis.
- Lamotrigine (Lamictal). Some studies show this drug to be less effective than ethosuximide or valproic acid, but it has fewer side effects. Side effects may include skin rash and nausea.
Lifestyle and home remedies
Dietary therapy
Following a diet that’s high in fat and low in carbohydrates, known as a ketogenic diet, can improve seizure control. This is used only if traditional medications fail to control the seizures.
This diet isn’t easy to maintain, but is successful at reducing seizures for some people. Variations on a high-fat, low-carbohydrate diet, such as the glycemic index and modified Atkins diets, though less effective, aren’t as restrictive as the ketogenic diet and may also provide benefit.
Additional options
Here are other steps you might take to help with seizure control:
- Take medication correctly. Don’t adjust the dosage before talking to your doctor. If you feel your medication should be changed, discuss it with your doctor.
- Get enough sleep. Lack of sleep can trigger seizures. Be sure to get adequate rest every night.
- Wear a medical alert bracelet. This will help emergency personnel know how to treat you correctly if you have another seizure.
- Ask your doctor about driving or recreation restrictions. Someone with a seizure disorder will have to be seizure-free for reasonable lengths of time (intervals vary from state to state) before being able to drive. Don’t bathe or swim unless someone else is nearby to help if needed.
Coping and support
If you’re living with a seizure disorder, you may feel anxious or stressed about what your future holds. Stress can affect your mental health, so it’s important to talk with your doctor about your feelings and seek resources for help.
At home
Your family members can provide much-needed support. Tell them what you know about the seizure disorder. Let them know they can ask you questions, and be open to conversations about their worries. Help them understand the condition by sharing any educational materials or other resources that your doctor has given you.
At school
Talk with your child’s teachers and coaches about your child’s seizure disorder and how it affects your child at school. Discuss what your child might need from them if a seizure happens at school.
You’re not alone
Remember, you don’t have to go it alone. Reach out to family and friends. Ask your doctor about local support groups or join an online support community. Don’t be afraid to ask for help. Having a strong support system is important to living with any medical condition.
- Posner E. Absence seizures in children. BMJ Clinical Evidence. 2008;2008:0317. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2907950[↩][↩][↩]
- Marten F., Rodrigues S., Benjamin O., Richardson M. P., Terry J. R. (2009). Onset of polyspike complexes in a mean-field model of human electroencephalography and its application to absence epilepsy. Philos. Trans. Roy. Soc. Lond. A Math. Phys. Eng. Sci. 367, 1145–1161. 10.1098/rsta.2008.0255 http://rsta.royalsocietypublishing.org/content/367/1891/1145.long[↩]
- Absence seizures with evolution into generalized tonic-clonic activity: clinical and EEG features. Mayville C, Fakhoury T, Abou-Khalil B. Epilepsia. 2000 Apr; 41(4):391-4. https://www.ncbi.nlm.nih.gov/pubmed/10756402[↩]
- Shih T. T., Hirsch L. J. (2003). Tonic-absence seizures: an underrecognized seizuretype. Epilepsia 44, 461–465. 10.1046/j.1528-1157.2003.39602.x https://www.ncbi.nlm.nih.gov/pubmed/12614405[↩]