Contents
What is acl injury
Tearing of the anterior cruciate ligament (ACL) is a very common sporting injury. Many people hear or feel a “pop” in the knee when an ACL injury occurs. Your knee may swell, feel unstable and become too painful to bear weight.
Anterior cruciate ligament (ACL) injuries have an incidence of approximately 252,000 yearly 1. Approximately half of ACL injuries occur in combination with damage to the meniscus, articular cartilage, or other ligaments. Additionally, patients may have bruises of the bone beneath the cartilage surface. These may be seen on a magnetic resonance imaging (MRI) scan and may indicate injury to the overlying articular cartilage. Persons who experience ACL injuries have an increased risk of arthritis.
Women are two to eight times more likely to have an ACL injury than men. It has been proposed that this is due to differences in physical conditioning, muscular strength, and neuromuscular control. Other hypothesized causes of this gender-related difference in ACL injury rates include pelvis and lower extremity (leg) alignment, increased ligamentous laxity, and the effects of estrogen on ligament properties.
An ACL tear can happen when you change direction rapidly, slow down when running, land after a jump, or receive a direct blow to your knee. Athletes who participate in high demand sports like soccer, skiing and basketball are sports where ACL knee injuries can happen.
Injuries to the posterior cruciate ligament are less common. It can be injured during a direct blow to the tibia when the knee is bent, or when the knee is over-straightened.
Depending on the severity of your ACL injury and your activity level, treatment may include rest and rehabilitation exercises to help you regain strength and stability or surgery to replace the torn ligament followed by rehabilitation. A proper training program may help reduce the risk of an ACL injury.
ACL knee injury
About half of all injuries to the anterior cruciate ligament occur along with damage to other structures in the knee, such as articular cartilage, meniscus, or other ligaments.
Injured ligaments are considered “sprains” and are graded on a severity scale.
- Grade 1 Sprains. The ligament is mildly damaged in a Grade 1 Sprain. It has been slightly stretched, but is still able to help keep the knee joint stable.
- Grade 2 Sprains. A Grade 2 Sprain stretches the ligament to the point where it becomes loose. This is often referred to as a partial tear of the ligament.
- Grade 3 Sprains. This type of sprain is most commonly referred to as a complete tear of the ligament. The ligament has been split into two pieces, and the knee joint is unstable.
Partial tears of the anterior cruciate ligament are rare; most ACL injuries are complete or near complete tears.
Complications of ACL injury
People who experience an ACL injury are at higher risk of developing knee osteoarthritis, in which joint cartilage deteriorates and its smooth surface roughens. Arthritis may occur even if you have surgery to reconstruct the ligament.
Multiple factors likely influence the risk of arthritis, such as the severity of the original injury, the presence of related injuries in the knee joint or the level of activity after treatment.
The Knee Joint
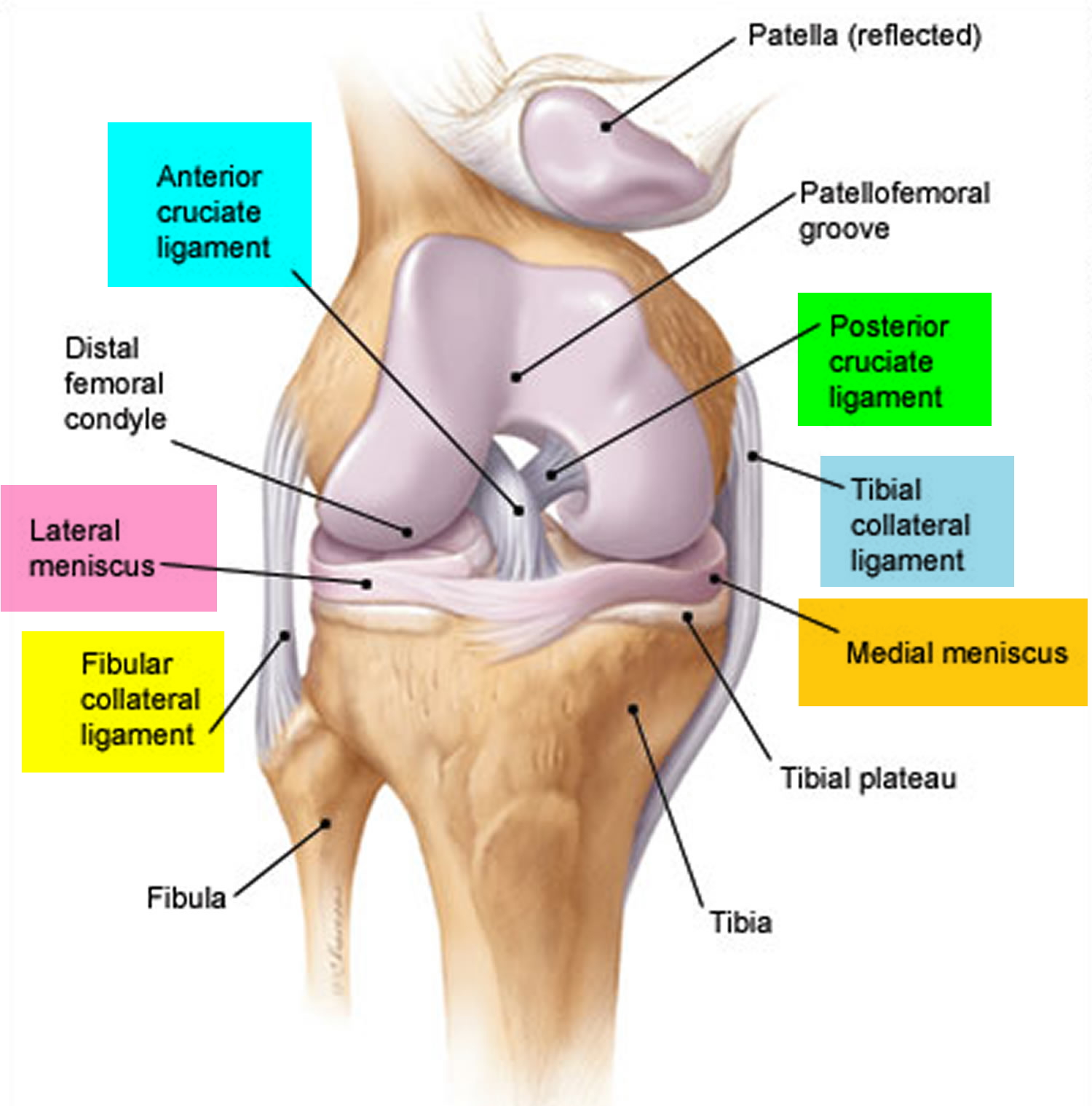
Three bones meet to form your knee joint: your thighbone (femur), shinbone (tibia), and kneecap (patella). Your kneecap sits in front of the joint to provide some protection.
The knee joint (tibiofemoral joint) is the largest and most complex joint of the body (Figures 1) and its evaluation can present a challenge. It is a modified hinge joint (because its primary movement is a uniaxial hinge movement) that consists of three joints within a single synovial cavity:
- Laterally is a tibiofemoral joint, between the lateral condyle of the femur, lateral meniscus, and lateral condyle of the tibia, which is the weight-bearing bone of the leg.
- Medially is another tibiofemoral joint, between the medial condyle of the femur, medial meniscus, and medial condyle of the tibia.
- An intermediate patellofemoral joint is between the patella and the patellar surface of the femur.
Bones are connected to other bones by ligaments. There are four primary ligaments in your knee. They act like strong ropes to hold the bones together and keep your knee stable.
- The lateral collateral ligament strengthens the knee joint on the outer side of the knee. It runs between your femur (thigh bone) and the top of your fibula — the long, thin bone adjacent to the tibia.
- The medial collateral ligament strengthens the knee joint on the inner side of the knee. It runs between your femur and the upper inside edge of your tibia (shin bone).
Together the collateral ligaments resist side-to-side movement of the knee joint and help prevent rotation between your thigh bone and your shin and brace it against unusual movement.
Knee Joint Anatomical Components
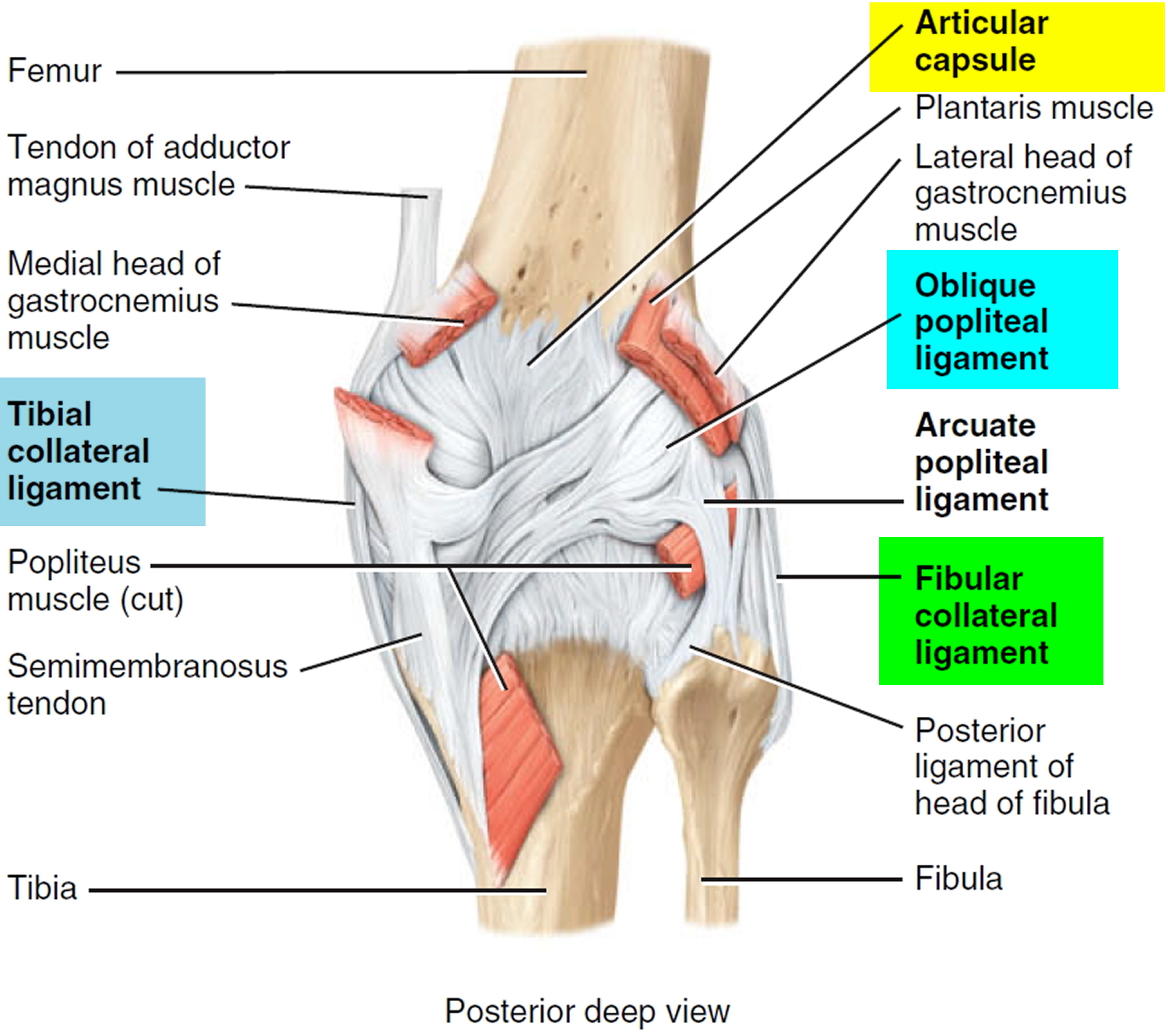
- Articular capsule. Independent capsule unites the bones of the knee joint. The ligamentous sheath surrounding the kneww joint consists mostly of muscle tendons or their expansions. There are, however, some capsular fibers connecting the articulating bones.
- Medial and lateral patellar retinacula. Fused tendons of insertion of the quadriceps femoris muscle and the fascia lata (fascia of thigh) that strengthen the anterior surface of the joint.
- Patellar ligament. Continuation of common tendon of insertion of quadriceps femoris muscle that extends from the patella to the tibial tuberosity. Also strengthens the anterior surface of the joint. Posterior surface of the ligament is separated from the synovial membrane of the joint by an infrapatellar fat pad.
- Oblique popliteal ligament. Broad, flat ligament that extends from the intercondylar fossa and lateral condyle of the femur to the head and medial condyle of the tibia. The ligament strengthens the posterior surface of the joint.
- Arcuate popliteal ligament. Extends from lateral condyle of femur to styloid process of the head of the fibula. Strengthens the lower lateral part of the posterior surface of the joint.
- Tibial collateral ligament. Broad, flat ligament on the medial surface of the joint that extends from the medial condyle of the femur to the medial condyle of the tibia. Tendons of the sartorius, gracilis, and semitendinosus muscles, all of which strengthen the medial aspect of the joint, cross the ligament. The tibial collateral ligament is firmly attached to the medial meniscus.
- Fibular collateral ligament. Strong, rounded ligament on the lateral surface of the joint that extends from the lateral condyle of the femur to the lateral side of the head of the fibula. It strengthens the lateral aspect of the joint. The ligament is covered by the tendon of the biceps femoris muscle. The tendon of
the popliteal muscle is deep to the ligament. - Intracapsular ligaments. Ligaments within capsule connecting tibia and femur. The anterior and posterior cruciate ligaments are named based on their
origins relative to the intercondylar area of the tibia. From their origins, they cross on their way to their destinations on the femur.- Anterior cruciate ligament (ACL). Extends posteriorly and laterally from a point anterior to the intercondylar area of the tibia to the posterior part of the medial surface of the lateral condyle of the femur. The Anterior cruciate ligament (ACL) limits hyperextension of the knee (which normally does not occur at this joint) and prevents the anterior sliding of the tibia on the femur. This ligament is stretched or torn in about 70% of all serious knee injuries.
- Posterior cruciate ligament (PCL). Extends anteriorly and medially from a depression on the posterior intercondylar area of the tibia and lateral meniscus to the anterior part of the lateral surface of the medial condyle of the femur. The posterior cruciate ligament (PCL) prevents the posterior sliding of the tibia (and anterior sliding of the femur) when the knee is flexed. This is very important when walking down stairs or a steep incline.
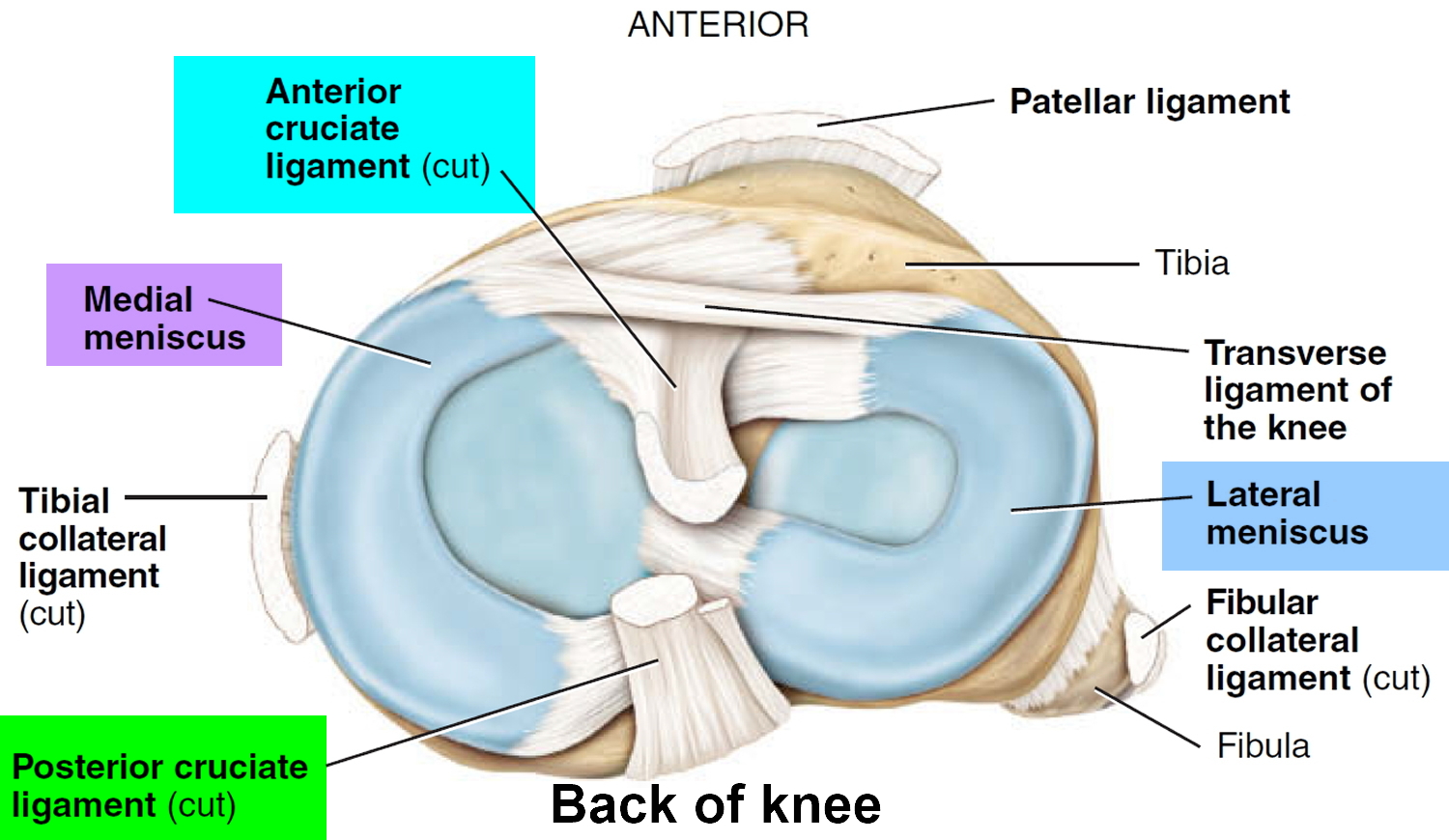
- Articular discs (menisci). Two fibrocartilage discs between the tibial and femoral condyles help compensate for the irregular shapes of the bones and circulate synovial fluid.
- Medial meniscus. Semicircular piece of fibrocartilage (C-shaped). Its anterior end is attached to the anterior intercondylar fossa of the tibia, anterior to the anterior cruciate ligament. Its posterior end is attached to the posterior intercondylar fossa of the tibia between the attachments of the posterior cruciate ligament and lateral meniscus.
- Lateral meniscus. Nearly circular piece of fibrocartilage (approaches an incomplete O in shape). Its anterior end is attached anteriorly to the intercondylar eminence of the tibia, and laterally and posteriorly to the anterior cruciate ligament. Its posterior end is attached posteriorly to the intercondylar eminence of the tibia, and anteriorly to the posterior end of the medial meniscus. The anterior surfaces of the medial and lateral menisci are connected to each other by the transverse ligament of the knee and to the margins of the head of the tibia by the coronary ligaments.
- The more important bursae of the knee include the following:
- Prepatellar bursa between the patella and skin.
- Infrapatellar bursa between superior part of tibia and patellar ligament.
- Suprapatellar bursa between inferior part of femur and deep surface of quadriceps femoris muscle.
Figure 1. Knee joint
Figure 2. Knee joint ligaments
Figure 3. Knee joint ligaments (posterior view)
ACL injury causes
Most ACL injuries happen during sports and fitness activities that can put stress on the knee:
- Changing direction rapidly
- Stopping suddenly
- Slowing down while running
- Landing from a jump incorrectly
- Direct contact or collision, such as a football tackle
Several studies have shown that female athletes have a higher incidence of ACL injury than male athletes in certain sports. It has been proposed that this is due to differences in physical conditioning, muscular strength, and neuromuscular control. Other suggested causes include differences in pelvis and lower extremity (leg) alignment, increased looseness in ligaments, and the effects of estrogen on ligament properties.
Risk factors for acl injury
Women are more likely to have an ACL injury than are men who participate in the same sports. Studies have suggested some reasons for these differences in risk.
In general, women athletes exhibit a strength imbalance in their thighs with the muscles at the front of the thigh (quadriceps) being stronger than the muscles at the back (hamstrings). The hamstrings help prevent the shinbone from moving too far forward — movement that can overextend the ACL.
Studies comparing jumping and landing techniques among men and women athletes have shown that women athletes are more likely to land from a jump in a way that increases stress on their knees.
Research suggests that training to strengthen muscles of the legs, hips and lower torso — as well as training to improve jumping and landing techniques — may reduce the higher ACL injury risk associated with women athletes.
ACL injury prevention
Proper training and exercise can help reduce the risk of ACL injury. A physical therapist, athletic trainer or other specialist in sports medicine can provide assessment, instruction and feedback that can help you reduce risks. Programs to reduce ACL injury include:
- Exercises that strengthen leg muscles, particularly hamstring exercises, to ensure an overall balance in leg muscle strength
- Exercises to strengthen the core: hips, pelvis and lower abdomen
- Training and exercise for proper techniques and knee position in jumping and landing
- Training to improve techniques for pivoting and cutting
Gear
Wear footwear and padding that is appropriate for your sport to help prevent injury. If you downhill ski, make sure your ski bindings are adjusted correctly by a trained professional so that your skis will release appropriately when you fall.
Wearing a knee brace does not appear to prevent ACL injury or reduce the risk of recurring injury after surgery.
ACL knee injury symptoms
When you injure your anterior cruciate ligament, you might hear a “popping” noise and you may feel your knee give out from under you. Other typical symptoms include:
- Pain with swelling. Within 24 hours, your knee will swell. If ignored, the swelling and pain may resolve on its own. However, if you attempt to return to sports, your knee will probably be unstable and you risk causing further damage to the cushioning cartilage (meniscus) of your knee.
- Loss of full range of motion
- Tenderness along the joint line
- Discomfort while walking
- A feeling of instability or “giving way” with weight bearing
ACL injury diagnosis
During the physical exam, your doctor will check your knee for swelling and tenderness — comparing your injured knee to your uninjured knee. He or she also may move your knee into a variety of positions to assess range of motion and overall function of the joint.
Physical Examination and Patient History
During your first visit, your doctor will talk to you about your symptoms and medical history.
During the physical examination, your doctor will check all the structures of your injured knee, and compare them to your non-injured knee. Most ligament injuries can be diagnosed with a thorough physical examination of the knee.
In addition to performing special tests for identifying meniscus tears and injury to other ligaments of the knee, the physician will often perform the Lachman’s test to see if the ACL is intact.
If the ACL is torn, the examiner will feel increased forward (upward or anterior) movement of the tibia in relation to the femur (especially when compared to the normal leg) and a soft, mushy endpoint (because the ACL is torn) when this movement ends.
Lachman Test
Imaging Tests
Other tests which may help your doctor confirm your diagnosis include:
X-rays. Although they will not show any injury to your anterior cruciate ligament, x-rays can show whether the injury is associated with a broken bone.
Magnetic resonance imaging (MRI) scan. This study creates better images of soft tissues like the anterior cruciate ligament. However, an MRI is usually not required to make the diagnosis of a torn ACL.
ACL injury treatment
A tear of the anterior cruciate ligament tends to be a more serious injury than an equivalent tear to any of the other knee ligaments, as joint stability is more profoundly affected, and surgery is often necessary.
Partial or even complete tears of the posterior cruciate or the collateral ligaments can often heal with a prescribed rehabilitation programme. However, if more than one ligament is injured, surgery is often needed.
Treatment for an ACL tear will vary depending upon the patient’s individual needs. For example, the young athlete involved in agility sports will most likely require surgery to safely return to sports. The less active, usually older, individual may be able to return to a quieter lifestyle without surgery.
Prompt first-aid care
Prompt first-aid care can reduce pain and swelling immediately after an injury to your knee. Follow the R.I.C.E. model of self-care at home:
- Rest. General rest is necessary for healing and limits weight bearing on your knee.
- Ice. When you’re awake, try to ice your knee at least every two hours for 20 minutes at a time.
- Compression. Wrap an elastic bandage or compression wrap around your knee.
- Elevation. Lie down with your knee propped up on pillows.
Natural history of ACL injury
What happens naturally with an ACL injury without surgical intervention varies from patient to patient and depends on the patient’s activity level, degree of injury and instability symptoms.
The prognosis for a partially torn ACL is often favorable, with the recovery and rehabilitation period usually at least 3 months. However, some patients with partial ACL tears may still have instability symptoms. Close clinical follow-up and a complete course of physical therapy helps identify those patients with unstable knees due to partial ACL tears.
Complete ACL ruptures have a much less favorable outcome without surgical intervention. After a complete ACL tear, some patients are unable to participate in cutting or pivoting-type sports, while others have instability during even normal activities, such as walking. There are some rare individuals who can participate in sports without any symptoms of instability. This variability is related to the severity of the original knee injury, as well as the physical demands of the patient.
About half of ACL injuries occur in combination with damage to the meniscus, articular cartilage or other ligaments. Secondary damage may occur in patients who have repeated episodes of instability due to ACL injury. With chronic instability, a large majority of patients will have meniscus damage when reassessed 10 or more years after the initial injury. Similarly, the prevalence of articular cartilage lesions increases in patients who have a 10-year-old ACL deficiency.
Nonsurgical Treatment
A torn ACL will not heal without surgery. But nonsurgical treatment may be effective for patients who are elderly or have a very low activity level. If the overall stability of the knee is intact, your doctor may recommend simple, nonsurgical options.
Bracing. Your doctor may recommend a brace to protect your knee from instability. To further protect your knee, you may be given crutches to keep you from putting weight on your leg.
Physical therapy. As the swelling goes down, a careful rehabilitation program is started. Specific exercises will restore function to your knee and strengthen the leg muscles that support it.
In nonsurgical treatment, progressive physical therapy and rehabilitation can restore the knee to a condition close to its pre-injury state and educate the patient on how to prevent instability. This may be supplemented with the use of a hinged knee brace. However, many people who choose not to have surgery may experience secondary injury to the knee due to repetitive instability episodes.
Surgical treatment is usually advised in dealing with combined injuries (ACL tears in combination with other injuries in the knee). However, deciding against surgery is reasonable for select patients.
Nonsurgical management of isolated ACL tears is likely to be successful or may be indicated in patients:
- With partial tears and no instability symptoms
- With complete tears and no symptoms of knee instability during low-demand sports who are willing to give up high-demand sports
- Who do light manual work or live sedentary lifestyles
- Whose growth plates are still open (children)
Surgical Treatment
ACL tears are not usually repaired using suture to sew it back together, because repaired ACLs have generally been shown to fail over time. Therefore, the torn ACL is generally replaced by a substitute graft made of tendon.
- Patellar tendon autograft (autograft comes from the patient)
- Hamstring tendon autograft
- Quadriceps tendon autograft
- Allograft (taken from a cadaver) patellar tendon, Achilles tendon, semitendinosus, gracilis, or posterior tibialis tendon
Patient Considerations
Active adult patients involved in sports or jobs that require pivoting, turning or hard-cutting as well as heavy manual work are encouraged to consider surgical treatment. This includes older patients who have previously been excluded from consideration for ACL surgery. Activity, not age, should determine if surgical intervention should be considered.
In young children or adolescents with ACL tears, early ACL reconstruction creates a possible risk of growth plate injury, leading to bone growth problems. The surgeon can delay ACL surgery until the child is closer to skeletal maturity or the surgeon may modify the ACL surgery technique to decrease the risk of growth plate injury.
A patient with a torn ACL and significant functional instability has a high risk of developing secondary knee damage and should therefore consider ACL reconstruction.
It is common to see ACL injuries combined with damage to the menisci, articular cartilage, collateral ligaments, joint capsule, or a combination of the above. The “unhappy triad,” frequently seen in football players and skiers, consists of injuries to the ACL, the MCL, and the medial meniscus.
In cases of combined injuries, surgical treatment may be warranted and generally produces better outcomes. As many as half of meniscus tears may be repairable and may heal better if the repair is done in combination with the ACL reconstruction.
Rebuilding the ligament. Most ACL tears cannot be sutured (stitched) back together. To surgically repair the ACL and restore knee stability, the ligament must be reconstructed. Your doctor will replace your torn ligament with a tissue graft. This graft acts as a scaffolding for a new ligament to grow on.
Patellar tendon autograft
The middle third of the patellar tendon of the patient, along with a bone plug from the shin and the kneecap is used in the patellar tendon autograft. Occasionally referred to by some surgeons as the “gold standard” for ACL reconstruction, it is often recommended for high-demand athletes and patients whose jobs do not require a significant amount of kneeling.
In studies comparing outcomes of patellar tendon and hamstring autograft ACL reconstruction, the rate of graft failure was lower in the patellar tendon group. In addition, most studies show equal or better outcomes in terms of postoperative tests for knee laxity (Lachman’s, anterior drawer and instrumented tests) when this graft is compared to others. However, patellar tendon autografts have a greater incidence of postoperative patellofemoral pain (pain behind the kneecap) complaints and other problems.
The pitfalls of the patellar tendon autograft are:
- Postoperative pain behind the kneecap
- Pain with kneeling
- Slightly increased risk of postoperative stiffness
- Low risk of patella fracture
Hamstring tendon autograft
The semitendinosus hamstring tendon on the inner side of the knee is used in creating the hamstring tendon autograft for ACL reconstruction. Some surgeons use an additional tendon, the gracilis, which is attached below the knee in the same area. This creates a two- or four-strand tendon graft. Hamstring graft proponents claim there are fewer problems associated with harvesting of the graft compared to the patellar tendon autograft including:
- Fewer problems with anterior knee pain or kneecap pain after surgery
- Less postoperative stiffness problems
- Smaller incision
- Faster recovery
The graft function may be limited by the strength and type of fixation in the bone tunnels, as the graft does not have bone plugs. There have been conflicting results in research studies as to whether hamstring grafts are slightly more susceptible to graft elongation (stretching), which may lead to increased laxity during objective testing. Recently, some studies have demonstrated decreased hamstring strength in patients after surgery.
There are some indications that patients who have intrinsic ligamentous laxity and knee hyperextension of 10 degrees or more may have increased risk of postoperative hamstring graft laxity on clinical exam. Therefore, some clinicians recommend the use of patellar tendon autografts in these hypermobile patients.
Additionally, since the medial hamstrings often provide dynamic support against valgus stress and instability, some surgeons feel that chronic or residual medial collateral ligament laxity (grade 2 or more) at the time of ACL reconstruction may be a contraindication for use of the patient’s own semitendinosus and gracilis tendons as an ACL graft.
Quadriceps tendon autograft
The quadriceps tendon autograft is often used for patients who have already failed ACL reconstruction. The middle third of the patient’s quadriceps tendon and a bone plug from the upper end of the knee cap are used. This yields a larger graft for taller and heavier patients. Because there is a bone plug on one side only, the fixation is not as solid as for the patellar tendon graft. There is a high association with postoperative anterior knee pain and a low risk of patella fracture. Patients may find the incision is not cosmetically appealing.
Allografts
Allografts are grafts taken from cadavers and are becoming increasingly popular. These grafts are also used for patients who have failed ACL reconstruction before and in surgery to repair or reconstruct more than one knee ligament. Advantages of using allograft tissue include elimination of pain caused by obtaining the graft from the patient, decreased surgery time and smaller incisions. The patellar tendon allograft allows for strong bony fixation in the tibial and femoral bone tunnels with screws.
However, allografts are associated with a risk of infection, including viral transmission (HIV and Hepatitis C), despite careful screening and processing. Several deaths linked to bacterial infection from allograft tissue (due to improper procurement and sterilization techniques) have led to improvements in allograft tissue testing and processing techniques. There have also been conflicting results in research studies as to whether allografts are slightly more susceptible to graft elongation (stretching), which may lead to increased laxity during testing.
Some published literature may point to a higher failure rate with the use of allografts for ACL reconstruction. Higher failure rates for allografts have been reported in young, active patients returning to high-demand sporting activities after ACL reconstruction, compared with autografts.
The reason for this higher failure rate is unclear. It could be due to graft material properties (sterilization processes used, graft donor age, storage of the graft). It could possibly be due to an ill-advised earlier return to sport by the athlete because of a faster perceived physiologic recovery, when the graft is not biologically ready to be loaded and stressed during sporting activities. Further research in this area is indicated and is ongoing.
Surgical Procedure
Before any surgical treatment, the patient is usually sent to physical therapy. Patients who have a stiff, swollen knee lacking full range of motion at the time of ACL surgery may have significant problems regaining motion after surgery. It usually takes three or more weeks from the time of injury to achieve full range of motion. It is also recommended that some ligament injuries be braced and allowed to heal prior to ACL surgery.
The patient, the surgeon, and the anesthesiologist select the anesthesia used for surgery. Patients may benefit from an anesthetic block of the nerves of the leg to decrease postoperative pain.
The surgery usually begins with an examination of the patient’s knee while the patient is relaxed due the effects of anesthesia. This final examination is used to verify that the ACL is torn and also to check for looseness of other knee ligaments that may need to be repaired during surgery or addressed postoperatively.
If the physical exam strongly suggests the ACL is torn, the selected tendon is harvested (for an autograft) or thawed (for an allograft) and the graft is prepared to the correct size for the patient.
After the graft has been prepared, the surgeon places an arthroscope into the joint. Small (one-centimeter) incisions called portals are made in the front of the knee to insert the arthroscope and instruments and the surgeon examines the condition of the knee. Meniscus and cartilage injuries are trimmed or repaired and the torn ACL stump is then removed.
In the most common ACL reconstruction technique, bone tunnels are drilled into the tibia and the femur to place the ACL graft in almost the same position as the torn ACL. A long needle is then passed through the tunnel of the tibia, up through the femoral tunnel, and then out through the skin of the thigh. The sutures of the graft are placed through the eye of the needle and the graft is pulled into position up through the tibial tunnel and then up into the femoral tunnel. The graft is held under tension as it is fixed in place using interference screws, spiked washers, posts, or staples. The devices used to hold the graft in place are generally not removed.
Variations on this surgical technique include the “two-incision,” “over-the-top,” and “double-bundle” types of ACL reconstructions, which may be used because of the preference of the surgeon or special circumstances (revision ACL reconstruction, open growth plates).
Before the surgery is complete, the surgeon will probe the graft to make sure it has good tension, verify that the knee has full range of motion and perform tests such as the Lachman’s test to assess graft stability. The skin is closed and dressings (and perhaps a postoperative brace and cold therapy device, depending on surgeon preference) are applied. The patient will usually go home on the same day of the surgery.
Surgical Complications
- Infection. The incidence of infection after arthroscopic ACL reconstruction is very low. There have also been reported deaths linked to bacterial infection from allograft tissue due to improper procurement and sterilization techniques.
- Viral transmission. Allografts specifically are associated with risk of viral transmission, including HIV and Hepatitis C, despite careful screening and processing. The chance of obtaining a bone allograft from an HIV-infected donor is calculated to be less than 1 in a million.
- Bleeding, numbness. Rare risks include bleeding from acute injury to the popliteal artery, and weakness or paralysis of the leg or foot. It is not uncommon to have numbness of the outer part of the upper leg next to the incision, which may be temporary or permanent.
- Blood clot. Although rare, blood clot in the veins of the calf or thigh is a potentially life-threatening complication. A blood clot may break off in the bloodstream and travel to the lungs, causing pulmonary embolism or to the brain, causing stroke.
- Instability. Recurrent instability due to rupture or stretching of the reconstructed ligament or poor surgical technique is possible.
- Stiffness. Knee stiffness or loss of motion has been reported by some patients after surgery.
- Extensor mechanism failure. Rupture of the patellar tendon (patellar tendon autograft) or patella fracture (patellar tendon or quadriceps tendon autografts) may occur due to weakening at the site of graft harvest.
- Growth plate injury. In young children or adolescents with ACL tears, early ACL reconstruction creates a possible risk of growth plate injury, leading to bone growth problems. The ACL surgery can be delayed until the child is closer to reaching skeletal maturity. Alternatively, the surgeon may be able to modify the technique of ACL reconstruction to decrease the risk of growth plate injury.
- Kneecap pain. Postoperative anterior knee pain is especially common after patellar tendon autograft ACL reconstruction. The incidence of pain behind the kneecap varies greatly in studies, whereas the incidence of kneeling pain is often higher after patellar tendon autograft ACL reconstruction.
Rehabilitation
Whether your treatment involves surgery or not, rehabilitation plays a vital role in getting you back to your daily activities. A physical therapy program will help you regain knee strength and motion.
If you have surgery, physical therapy with exercises beginning immediately after the surgery focuses on returning motion to the joint and surrounding muscles. This is followed by a strengthening program designed to protect the new ligament. This strengthening gradually increases the stress across the ligament. The final phase of rehabilitation is aimed at a functional return tailored for the athlete’s sport.
Much of the success of ACL reconstructive surgery depends on the patient’s dedication to rigorous physical therapy. With new surgical techniques and stronger graft fixation, current physical therapy uses an accelerated course of rehabilitation.
Postoperative Course. In the first 10 to 14 days after surgery, the wound is kept clean and dry, and early emphasis is placed on regaining the ability to fully straighten the knee and restore quadriceps control.
The knee is iced regularly to reduce swelling and pain. The surgeon may dictate the use of a postoperative brace and the use of a machine to move the knee through its range of motion. Weight-bearing status (use of crutches to keep some or all of the patient’s weight off of the surgical leg) is also determined by physician preference, as well as other injuries addressed at the time of surgery.
Rehabilitation. The goals for rehabilitation of ACL reconstruction include reducing knee swelling, maintaining mobility of the kneecap to prevent anterior knee pain problems, regaining full range of motion of the knee, as well as strengthening the quadriceps and hamstring muscles.
The patient may return to sports when there is no longer pain or swelling, when full knee range of motion has been achieved, and when muscle strength, endurance and functional use of the leg have been fully restored.
The patient’s sense of balance and control of the leg must also be restored through exercises designed to improve neuromuscular control. This usually takes 4 to 6 months. The use of a functional brace when returning to sports is ideally not needed after a successful ACL reconstruction, but some patients may feel a greater sense of security by wearing one.
- Management of ACL Injuries: Clinical Practice Guideline from the AAOS. Am Fam Physician. 2015 Aug 1;92(3):232-234. https://www.aafp.org/afp/2015/0801/p232.html[↩]