Contents
- Age-related macular degeneration
- Dry macular degeneration
- Wet macular degeneration
- Age-related macular degeneration causes
- Age-related macular degeneration prevention
- Age-related macular degeneration signs and symptoms
- Age-related macular degeneration stages
- Age-related macular degeneration diagnosis
- Age-related macular degeneration treatment
- Medications to stop growth of abnormal blood vessels
- Photodynamic therapy
- Photocoagulation therapy
- Vitamin supplements
- What are lutein, zeaxanthin, and beta-carotene?
- How do lutein and zeaxanthin compare to beta-carotene?
- What are omega-3 fatty acids?
- What is the function of copper in the Age-Related Eye Disease Study (AREDS) and AREDS2 supplements?
- What is the basis for the concentration of zinc in the AREDS supplements?
- What is the risk of lung cancer from taking beta-carotene?
- The dose of vitamin E in the Age-Related Eye Disease Study (AREDS) formulation is higher than the recommended dietary allowance. Is this safe?
- Do the Age-Related Eye Disease Study (AREDS) or AREDS2 formulations interfere with other medications?
- Does the high-dose vitamin E in the AREDS formulations affect the risk of prostate cancer?
- Low vision rehabilitation
- Lifestyle and home remedies
- Coping and support
- Age-related macular degeneration prognosis
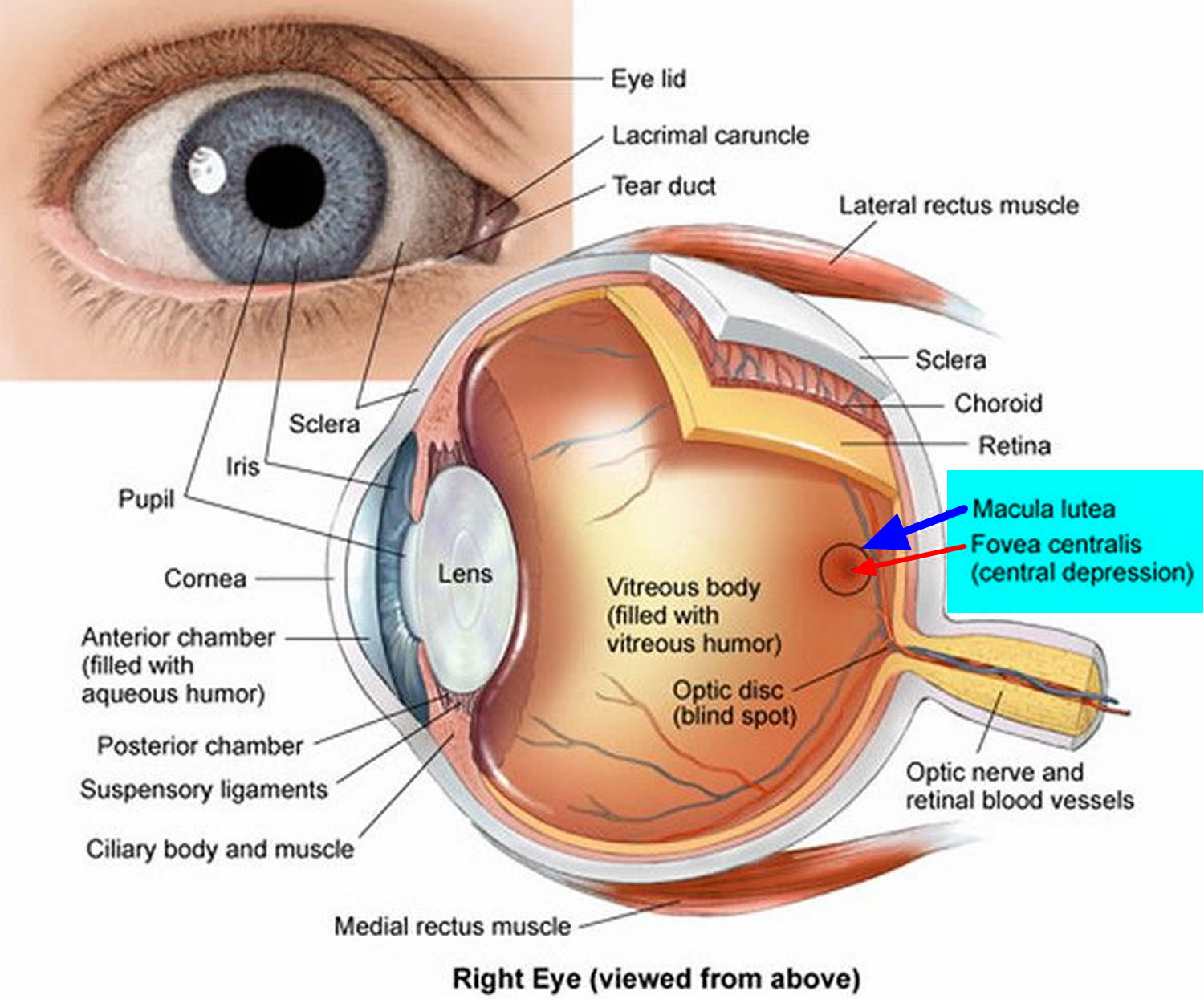
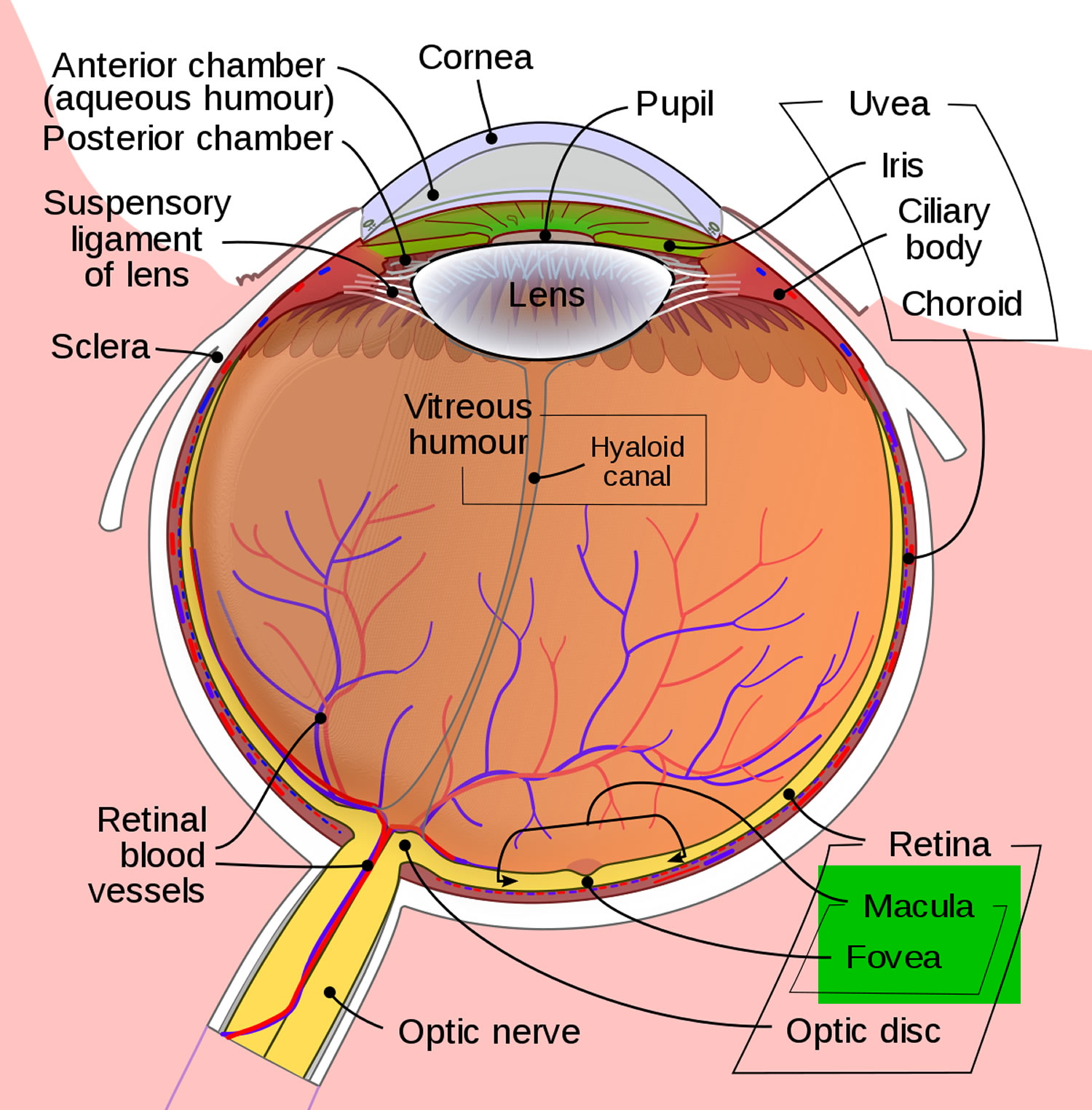
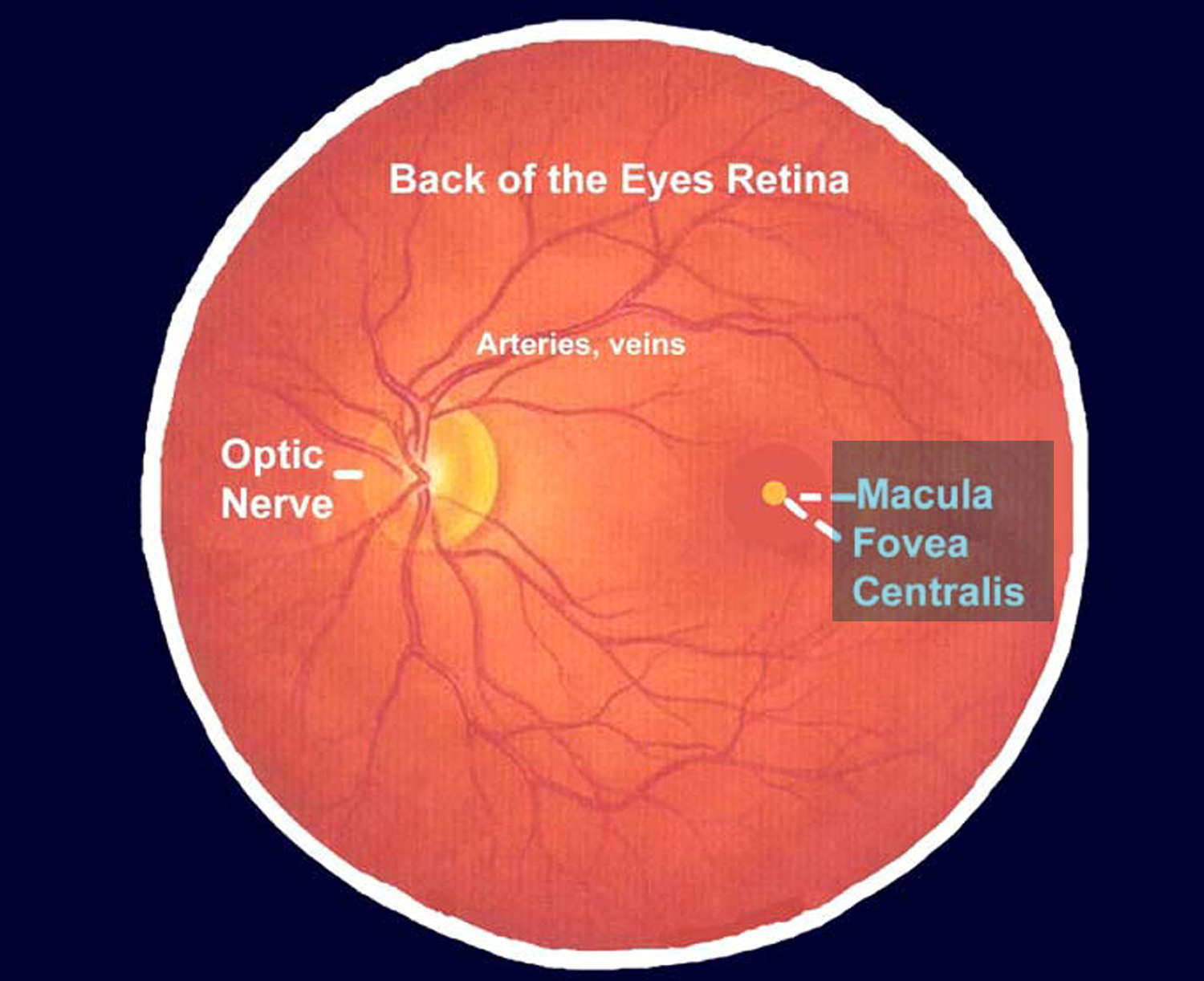
Age-related macular degeneration (AMD) is a complex, multifactorial and progressive retinal eye disease affecting millions of people over 60 years of age worldwide 1, 2, 3, 4. Age-related macular degeneration (AMD) is a progressive eye condition that affects the macula, a small but crucial part of the retina that is located on the inside back layer of your and is eye responsible for sharp central vision. Age-related macular degeneration (AMD) slowly blurs your central vision, making it challenging to see fine details whether looking at something close or far and perform daily tasks like reading, driving, and recognizing faces. But your peripheral (side) vision will stay normal. For instance, imagine you are looking at a fan. With AMD, you might see the wings of the fan but not the central part. In developed countries, age-related macular degeneration (AMD) is the leading cause of central loss of vision and legal blindness among the elderly; it accounts for 8.7% of all blindness worldwide, a percentage that translates to about 30–50 million people 5, 6, 7. Age-related macular degeneration (AMD) is estimated to affect around 196 million people by 2020 and 288 million people by 2040 6.
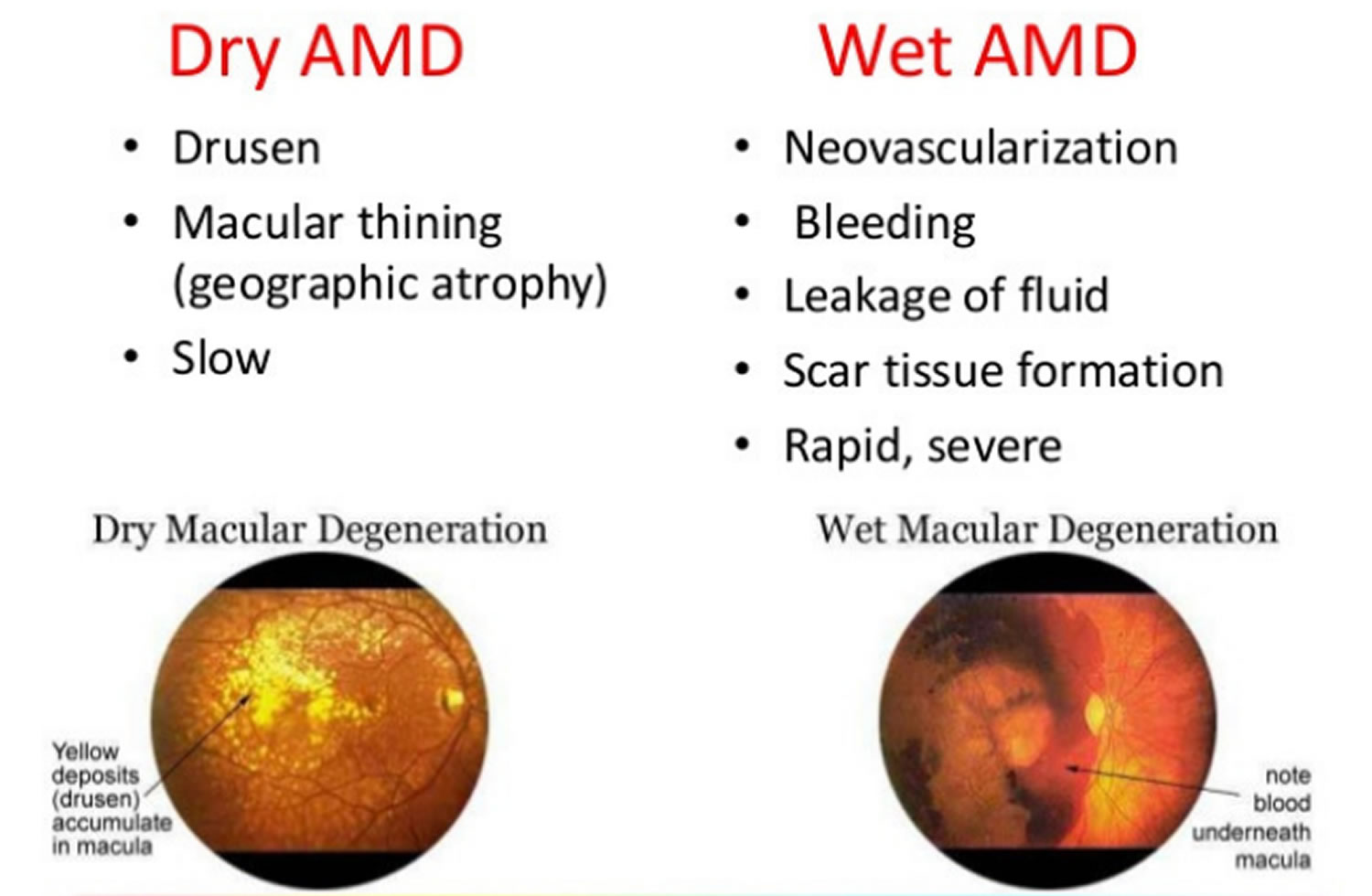
There are two types of age related macular degeneration (AMD): wet macular degeneration and dry macular degeneration 1.
- Wet age-related macular degeneration (wet AMD) also called neovascular AMD happens when abnormal blood vessels grow from the choroid underneath the macula. This is called choroidal neovascularization. “Neovascularization” means “new blood vessels”. Wet AMD happens when a protein called vascular endothelial growth factor (VEGF) makes abnormal blood vessels grow in the wrong place in the back of your eye. These new abnormal blood vessels often leak blood and fluid leading to distorted vision. This is the most serious kind. Wet age-related macular degeneration damages the macula quickly. That makes straight lines look zigzag and wavy, as well as blind spots and loss of central vision. These abnormal blood vessels and bleeding from them eventually form a scar, leading to permanent loss of central vision.
- Dry age-related macular degeneration (dry AMD) also known as non-neovascular AMD or atrophic AMD happens when the light-sensitive cells in the macula slowly break down. The “dry” form of macular degeneration is identified by the presence of yellow deposits called drusen in the macula. It is the most common kind. About 80 percent (8 out of 10) of people who have age-related macular degeneration (AMD) have the dry form. A few small drusen may not cause any changes in vision. However, as they grow in numbers and size, they may lead to a dimming or distortion of vision. Then people start noticing when they read. A common early symptom is that straight lines appear crooked. In the later stages of dry macular degeneration, there is also a thinning of the light-sensitive layer of cells in the macula leading to atrophy, or tissue death. Atrophy of the retinal pigment epithelium occurs in the advanced stage of the disease known as geographic atrophy. Geographic atrophy on involving the center of the macula leads to significant visual loss. In the atrophic form of dry macular degeneration, patients may have blind spots in the center of their vision. In more advanced stages, patients lose central vision.
Most patients have the dry macular degeneration and can lose some form of central vision. Still, you must keep in mind that the dry form of macular degeneration can lead to the wet macular degeneration. Although only about 10% of people with macular degeneration develop the wet macular degeneration, they make up the majority of those who experience serious vision loss from age-related macular degeneration (AMD).
The symptoms of AMD depend on the stage. Dry age-related macular degeneration (dry AMD) happens in 3 stages: early, intermediate, and late. Age-related macular degeneration (AMD) is a progressive disease, that means symptoms usually get worse over time.
- Early dry AMD doesn’t cause any symptoms.
- In intermediate dry AMD, some people still have no symptoms. Others may notice mild symptoms, like mild blurriness in their central vision or trouble seeing in low lighting.
- In late AMD (wet or dry type), many people notice that straight lines start to look wavy or crooked. You may also notice a blurry area near the center of your vision. Over time, this blurry area may get bigger or you may see blank spots. Colors may also seem less bright than before, and you may have more trouble seeing in low lighting.
Straight lines looking wavy is a warning sign for late AMD. If you notice this symptom, see your eye doctor (ophthalmologist) right away.
Risk Factors for macular degeneration
Macular degeneration tends to have a higher incidence of occurrence when the following risk factors are present:
- Age: Macular degeneration can occur at any age; however, the chance of its occurrence increases nearly five-fold after the age of sixty-five.
- Heredity: Macular degeneration tends to “run in families.” This means that there is a genetic factor that predisposes a person toward developing the condition. Anytime a “bloodline” relative has macular degeneration, you run an increased chance of developing the condition.
- Gender: Women have a slightly higher incidence of developing macular degeneration than men.
- Race and Ethnicity: Fair-skinned people of northern European ancestry (Scandinavian, English, or German descent) have a higher chance of developing macular degeneration. Early AMD is more common in individuals of European ancestry than in Asians, whereas the prevalence of late AMD is the same between the two populations.
- Eye Color: Blue-eyed individuals are more prone to develop the condition than brown-eyed persons.
- Cardiovascular History: A history of heart disease or stroke is associated with a higher incidence of macular degeneration.
- Smoking: Macular degeneration tends to occur more frequently in persons who smoke. Even after treatment, smokers are reported to have a greater chance of having macular problems recur.
Eye doctors (ophthalmologists) can check for AMD as part of a comprehensive dilated eye exam. The exam is simple and painless — your eye doctor will give you some eye drops to dilate (widen) your pupil and then check your eyes for AMD and other eye problems. Your eye doctor may also recommend doing a test called optical coherence tomography (OCT). In an OCT test, your eye doctor will take pictures of the inside of your eye with a special machine.
Early detection of AMD is very important because there are treatments available that can delay or reduce the severity of the disease. Age-related macular degeneration (AMD) can be detected in a routine eye examination. An eye doctor (ophthalmologist) would easily be able to detect the presence of drusen — tiny yellow deposits under the retina — or pigment clumping, during an eye exam. Your eye doctor may also ask you to look at an Amsler grid (see Figure 6 below). A pattern of straight lines resembling a checkerboard. If any of the straight lines appear wavy to you, or you notice some of the lines as missing. These can be signs of macular degeneration.
Treatment for age-related macular degeneration depends on the stage and type. There’s currently no treatment for early AMD, so your eye doctor will probably just keep track of how your eyes are doing with regular eye exams. Eating healthy, getting regular exercise, and quitting smoking can also help.
If you have intermediate AMD in 1 or both eyes, special dietary supplements (vitamins and minerals) may be able to stop it from turning into late AMD. If you have late AMD in only 1 eye, these supplements may slow down AMD in your other eye.
For people with intermediate or advanced age-related macular degeneration, taking a high-dose formulation of antioxidant vitamins and minerals may help reduce the risk of vision loss. Research from the Age-Related Eye Disease Study (AREDS) and AREDS2 have shown these vitamins to prevent progression to advanced AMD in patients with an intermediate or advanced disease in 1 eye 8, 9:
- 500 milligrams (mg) of vitamin C
- 400 international units (IU) of vitamin E
- 10 mg of lutein
- 2 mg of zeaxanthin
- 80 mg of zinc (as zinc oxide)
- 2 mg of copper (as cupric oxide)
Ask your eye doctor if taking antioxidant vitamins and minerals supplements is right for you.
If you have wet AMD, there are 2 treatment options that can slow down or stop vision loss from wet AMD (neovascular AMD):
- Anti-VEGF injections (intravitreal anti-VEGF shots). Anti-VEGF medicines help stop bleeding and leaking from blood vessels in the back of your eye. Most people with wet AMD will get anti-VEGF injections as their only treatment. Currently used anti-VEGF medicines prevent visual loss and may also improve vision in some cases 10. Anti-VEGF injections usually only work for a short time, so most people need to get them many times. At first, most people need injections once a month. After that, your eye doctor will tell you how often you need injections to help stop vision loss from AMD.
- Photodynamic therapy (PDT). Photodynamic therapy (PDT), a combination of injections and laser treatment. Photodynamic therapy (PDT) is a much less common treatment for wet AMD that doctors sometimes use along with anti-VEGF injections. Photodynamic therapy works by using a light-sensitive medicine called verteporfin (Visudyne) that “turns on” when hit by a specific type of laser sometimes called a cold laser. Your eye doctor will shine the laser on a very small area in the back of your eye, causing the verteporfin to break down the blood vessels that are causing your vision loss. When you get photodynamic therapy (PDT), your eye doctor will:
- Give a shot of verteporfin in your arm
- Put numbing medicine in your eye
- Place a special contact lens on your eye to help guide the laser
- Shine the laser onto the extra blood vessels in the back of your eye
- Some people will need to get PDT more than once. Talk to your eye doctor to find out if you will need more treatments to help stop vision loss from AMD.
Untreated wet AMD leads to irreversible vision loss in most patients. However, vision loss can still occur even with treatment. Patients with vision loss from AMD often report a diminished quality of life 11. These individuals report significantly more emotional distress, poorer health, and less independence in daily activities compared to those with other chronic illnesses 12.
Patients already with severe vision loss may benefit from visual rehabilitation and referral to a low-vision clinic where they can obtain educational resources to help them function with their limited vision. Several low-vision tools may be offered, including handheld magnifiers, closed-circuit television viewers, and accessibility applications on standard electronic devices, such as smartphones and tablets. Patients should be informed about the availability of large-print periodicals, audiobooks, and other resources offered by their local library. These individuals may also benefit from a referral to social services to help preserve their independence as much as possible.
Figure 1. Structure of the human eye
Figure 2. Macula
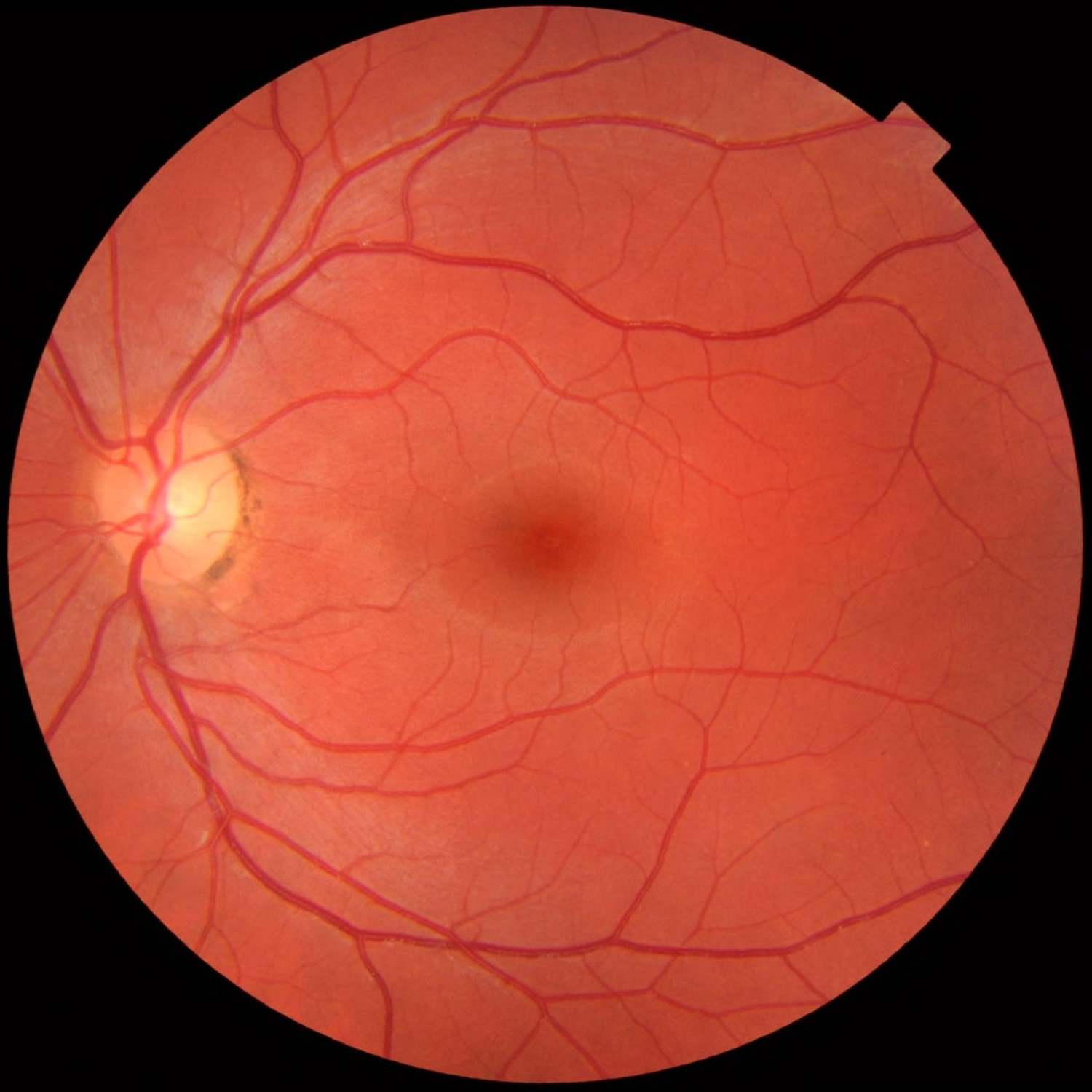
Figure 3. Normal macula and retina (left eye)
Figure 4. Age related macular degeneration
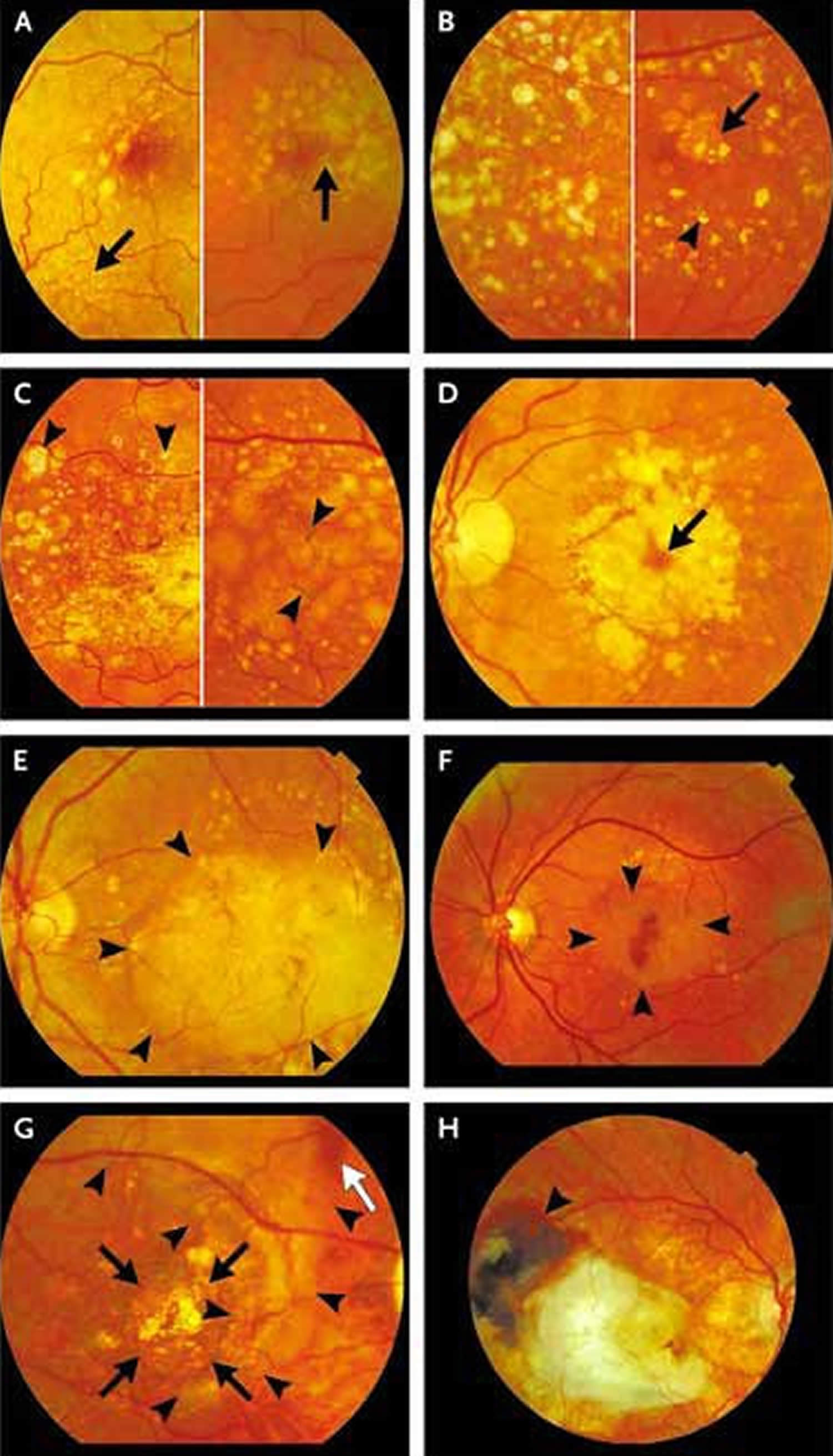
Figure 5. Progression from early to late age-related macular degeneration
Footnotes: Panel A shows early age-related macular degeneration in two maculas: the macula shown on the left-hand side contains small drusen (arrow) and some large, indistinctly bordered drusen in the fovea; the macula shown on the right-hand side contains more drusen and focal hyperpigmentation (arrow). The left-hand side of Panel B shows early age-related macular degeneration characterized by extensive small and large drusen in and around the macula; the right-hand side shows crystalline drusen (arrowhead) and a small patch of late dry age-related macular degeneration (arrow). The left-hand side of Panel C shows early age-related macular degeneration, with crystalline and calcified drusen (arrowheads); on the right-hand side (also early age-related macular degeneration) are large confluent drusen leading to a drusenoid detachment of the RPE, with hyperpigmentation (arrowheads). Panel D (late age-related macular degeneration) shows dry age-related macular degeneration, with a central island in which photoreceptors are still functioning (arrow); this eye has a complete ring scotoma around a small central visual-field remnant. Panel E (late age-related macular degeneration) shows wet age-related macular degeneration in the form of a large serous detachment of the RPE (with borders marked by arrowheads) caused by fluid leaking from a subretinal neovascular membrane. Panel F (late age-related macular degeneration) shows the development of wet age-related macular degeneration with a subfoveal hemorrhage surrounded by detachment of the RPE (arrowheads). Panel G (late age-related macular degeneration) shows dry age-related macular degeneration (black arrows), in which the orange lines are large choroidal vessels, surrounded by glial scar tissue (arrowheads) resulting from a large subretinal hemorrhage with a small remnant (white arrow). Panel H (late age-related macular degeneration) shows cicatricial wet age-related macular degeneration, with glial scarring in the macula and remnants of hemorrhages at its temporal border (arrowhead).
[Source 1 ]Age is a major risk factor for age-related macular degeneration. The disease is most likely to occur after age 60, but it can occur earlier.
Other risk factors for age-related macular degeneration include:
- Smoking. Research shows that smoking doubles the risk of age-related macular degeneration.
- Race. age-related macular degeneration is more common among Caucasians than among African-Americans or Hispanics/Latinos.
- Family history and Genetics. People with a family history of age-related macular degeneration are at higher risk. At last count, researchers had identified nearly 20 genes that can affect the risk of developing age-related macular degeneration. Many more genetic risk factors are suspected. You may see offers for genetic testing for age-related macular degeneration. Because age-related macular degeneration is influenced by so many genes plus environmental factors such as smoking and nutrition, there are currently no genetic tests that can diagnose age-related macular degeneration, or predict with certainty who will develop it. The American Academy of Ophthalmology 13 currently recommends against routine genetic testing for age-related macular degeneration, and insurance generally does not cover such testing.
Researchers have found links between age-related macular degeneration and some lifestyle choices, such as smoking. You might be able to reduce your risk of age-related macular degeneration or slow its progression by making these healthy choices:
- Avoid smoking
- Exercise regularly
- Maintain normal blood pressure and cholesterol levels
- Eat a healthy diet rich in green, leafy vegetables and fish
See your eye doctor if:
- You notice changes in your central vision
- Your ability to see colors and fine detail becomes impaired
These changes may be the first indication of macular degeneration, particularly if you’re older than age 50.
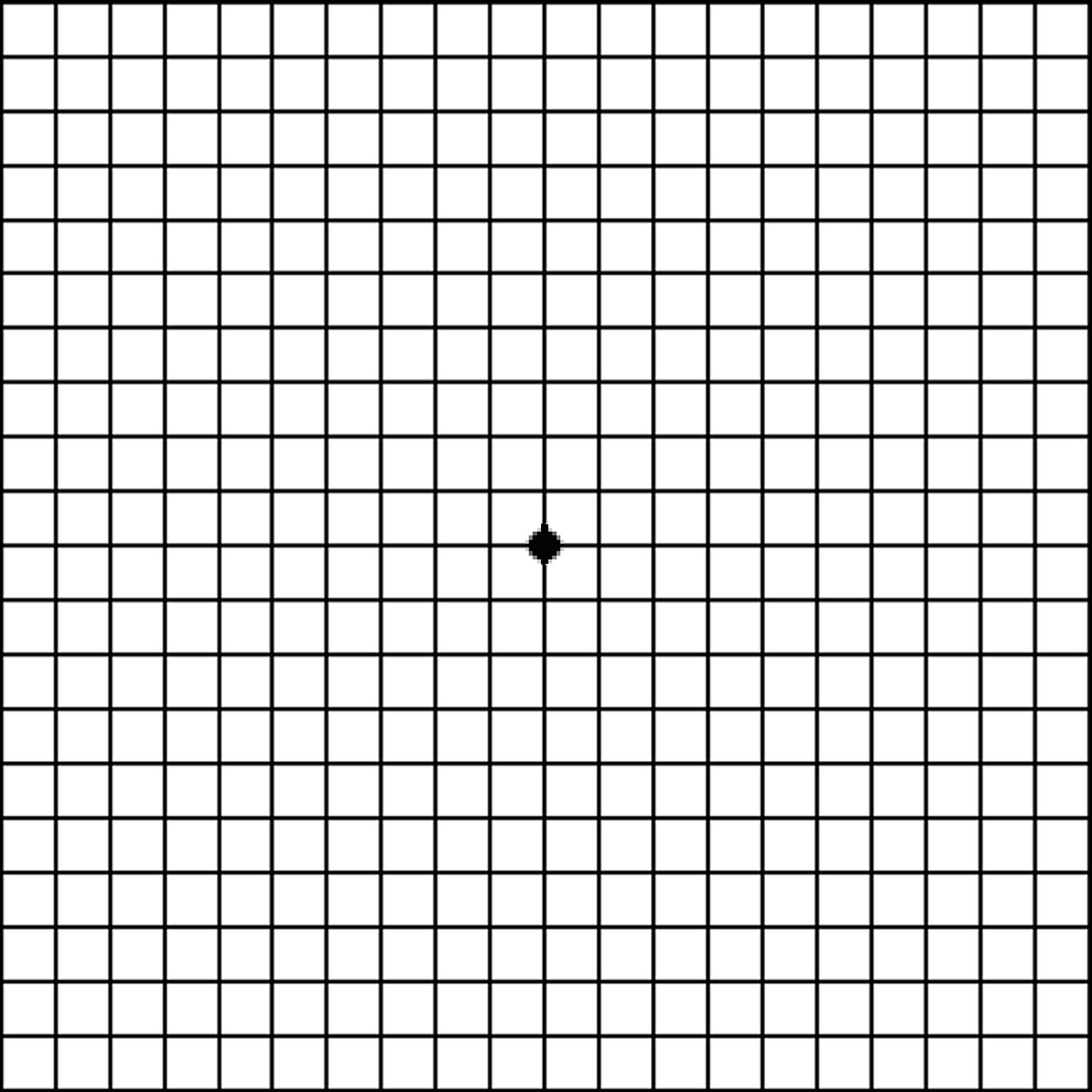
Amsler Grid Test
Amsler Grid test helps detect macular degeneration. If you normally wear glasses for reading, wear them for this test. If you wear bifocals, look through the bottom reading portion.
Do the Amsler Grid test with each eye separately, first the right and then the left. Hold the test grid right in front of you, 14 inches (35 centimeters) away from your eye. Look at the dot in the center of the grid, not at the grid pattern.
While looking at the dot, you will see the rest of the grid in your peripheral vision. All the lines, both vertical and horizontal, should appear straight and unbroken. They should meet at all the crossing points with no missing areas. If any lines appear distorted or broken, note their location on the grid using a pen or pencil.
Figure 6. Amsler grid
Dry macular degeneration
Dry age-related macular degeneration (dry AMD) also known as non-neovascular AMD or atrophic AMD is a common eye disorder among people over 50. About 80 percent (8 out of 10) of people who have age-related macular degeneration (AMD) have the dry macular degeneration. Dry AMD causes blurred or reduced central vision, due to thinning of the macula. The macula is the part of the retina responsible for clear vision in your direct line of sight. Dry age-related macular degeneration (AMD) is when parts of the macula get thinner with age and tiny clumps of protein called drusen grow. People with dry AMD may have drusen, pigment abnormalities, or atrophy of the retinal pigment epithelium occurs in the advanced stage of the disease known as geographic atrophy. Geographic atrophy involving the center of the macula leads to significant visual loss.
Drusen (yellowish subretinal deposits) are the hallmark feature of early and intermediate AMD and are characterized by accumulations of extracellular material that build up in the space between Bruch’s membrane and the retinal pigment epithelium (RPE) 14, 15, 16. Drusen can be hard (definite boundaries) or soft (indistinct boundaries), or they may confluence into larger drusen and may evolve into drusenoid RPE detachments (PED) 4.
The progression and pathogenesis of AMD have not been fully understood, but the calcification of drusen is considered an indicator of increased risk of late age-related macular degeneration (AMD) 14, 15, 17, 18, 19, 20. Moreover, there is no agreement as to whether drusen in the absence of other ocular abnormalities always point to early age-related macular degeneration 21, 22.
Drusen can be classified according to size, appearance, biochemical composition, and examination technique 23, 24. With increasing age, drusen become confluent and larger, sometimes crystalline, less circumscribed, or accompanied by hyperpigmentations or hypopigmentations of the retinal pigment epithelium (RPE). As seen through the ophthalmoscope, drusen are dots ranging in color from white to yellow, sometimes with a crystalline, glittering aspect 1.
Dry macular degeneration may first develop in one eye before developing in the other eye. It also may develop in both eyes at the same time. Over time your vision worsens, which may affect your ability to do things such as read, drive and recognize faces. But having dry macular degeneration doesn’t mean you’ll lose all your sight. Vision loss is typically central, and people retain their peripheral vision. Some people have only mild central vision loss. In others, it can be more severe.
Early detection and self-care measures may delay vision loss due to dry macular degeneration.
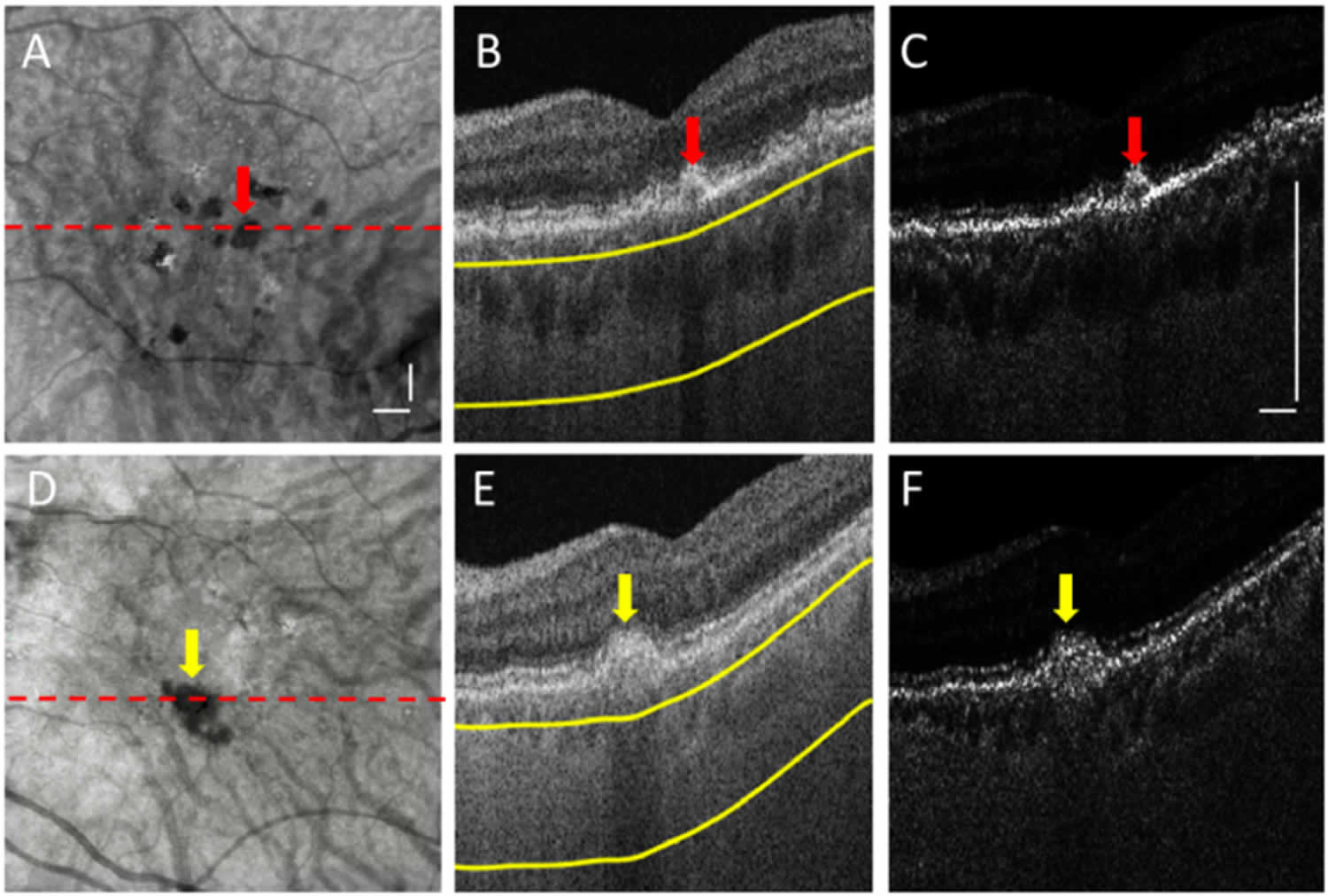
Figure 7. Calcified drusen on OCT scans
Footnotes: (A-C) an eye with calcified drusen with a hyperreflective cap and a hypo-reflective core (Red arrow), and (D-F) an eye with calcified drusen with hyperreflective contents but without a hypo-reflective core (Yellow arrow). (A, D) enface sub-retinal pigment epithelium (RPE) OCT image obtained from a slab defined by 64 µm to 400 µm below the Bruch’s membrane (BM) shown as yellow lines in (B, E), where choroidal hypotransmission defects (hypoTDs) appear as the dark foci. (B, E) Representative B-scans passing through calcified drusen at the locations highlighted by dashed lines in (A, D), and (C, F) correspondingly converted optical attenuation coefficient (OAC) B-scans, respectively. Scale bar represents 500 µm.
[Source 25 ]Dry macular degeneration symptoms
Dry macular degeneration symptoms usually develop gradually and without pain. They may include:
- Visual distortions, such as straight lines seeming bent.
- Reduced central vision in one or both eyes.
- The need for brighter light when reading or doing close-up work.
- Increased difficulty adapting to low light levels, such as when entering a dimly lit restaurant or theater.
- Increased blurriness of printed words.
- Decreased intensity or brightness of colors.
- Difficulty recognizing faces.
- A well-defined blurry spot or blind spot in the field of vision.
Dry macular degeneration can affect one or both eyes. If only one eye is affected, you may not notice any changes in your vision. This is because your good eye may compensate for the affected eye. And the condition doesn’t affect the side vision, so it does not cause total blindness.
Dry macular degeneration is one of two types of age-related macular degeneration (AMD). It can progress to wet macular degeneration, which is when abnormal blood vessels grow and leak under the retina. The dry type is more common, but it usually progresses slowly over years. The wet type is more likely to cause a relatively sudden change in vision resulting in serious vision loss.
Dry macular degeneration complications
People whose dry macular degeneration has progressed to central vision loss have a higher risk of depression and social isolation. With profound loss of vision, people may see visual hallucinations. This condition is called Charles Bonnet syndrome. Dry macular degeneration may progress to wet macular degeneration, which can quickly cause vision loss if left untreated.
Dry macular degeneration causes
No one knows exactly what causes dry macular degeneration. Research indicates that it may be a combination of family genes and environmental factors, including smoking, obesity and unhealthy diet.
Dry macular degeneration develops as the eye ages. Dry macular degeneration affects the macula — an area of the retina that’s responsible for clear vision in your direct line of sight. Over time, tissue in the macula may thin and lose cells responsible for vision.
Dry macular degeneration risk factors
Factors that may increase your risk of macular degeneration include 26:
- Age. Age-related macular degeneration (AMD) is most common in people over 65.
- Family history and genetics. Age-related macular degeneration (AMD) has a hereditary component. Researchers have identified several genes that are related to developing the condition.
- Race. Macular degeneration is more common in whites than it is in other people.
- Smoking. Smoking cigarettes or being regularly exposed to tobacco smoke significantly increases your risk of macular degeneration.
- Obesity. Research indicates that being obese may increase your chance that early or intermediate macular degeneration will progress to the more severe form of the disease.
- Cardiovascular disease. If you have heart or blood vessel disease, you may be at higher risk of macular degeneration.
Dry macular degeneration prevention
It’s important to have regular eye exams to identify early signs of macular degeneration. The following measures may help reduce your risk of developing dry macular degeneration:
- Have routine eye exams. Ask your eye doctor how often you need to undergo routine eye exams. A dilated eye exam can identify macular degeneration.
- Manage your other medical conditions. For example, if you have cardiovascular disease or high blood pressure, take your medication and follow your doctor’s instructions for controlling the condition.
- Don’t smoke. Smokers are more likely to develop macular degeneration than are nonsmokers. Ask your doctor for help to stop smoking.
- Maintain a healthy weight and exercise regularly. If you need to lose weight, reduce the number of calories you eat and increase the amount of exercise you get each day. Maintain a healthy weight by exercising regularly and controlling your diet.
- Choose a diet rich in fruits and vegetables. Choose a healthy diet that’s full of a variety of fruits and vegetables. These foods contain antioxidant vitamins that reduce your risk of developing macular degeneration.
- Include fish in your diet. Omega-3 fatty acids, which are found in fish, may reduce the risk of macular degeneration. Nuts, such as walnuts, also contain omega-3 fatty acids.
Dry macular degeneration diagnosis
Your doctor may diagnose your condition by reviewing your medical and family history and conducting a complete eye exam. He or she may also do several other tests, including:
- Examination of the back of your eye. Your eye doctor will put drops in your eyes to dilate them and use a special instrument to examine the back of your eye. He or she will look for a mottled appearance that’s caused by drusen — yellow deposits that form under the retina. People with macular degeneration often have many drusen.
- Test for defects in the center of your vision. During an eye examination, your eye doctor may use an Amsler grid to test for defects in the center of your vision. Macular degeneration may cause some of the straight lines in the grid to look faded, broken or distorted.
- Fluorescein angiography. During this test, your doctor injects a colored dye into a vein in your arm. The dye travels to and highlights the blood vessels in your eye. A special camera takes several pictures as the dye travels through the blood vessels. The images will show if you have abnormal blood vessel or retinal changes.
- Indocyanine green angiography. Like fluorescein angiography, this test uses an injected dye. It may be used to confirm the findings of a fluorescein angiography or to identify specific types of macular degeneration.
- Optical coherence tomography (OCT). This noninvasive imaging test displays detailed cross-sectional images of the retina. It identifies areas of retina thinning, thickening or swelling. These can be caused by fluid accumulations from leaking blood vessels in and under your retina.
- Optical coherence tomography angiography (OCTA). Optical coherence tomography angiography (OCTA) is a newer technology that creates images of the retinal circulation by obtaining sequential B-scans from a single area, and decorrelation signals are generated to show only areas with movement, such as flow-through vessels 27. Optical coherence tomography angiography (OCTA) may facilitate the earlier diagnosis of choroidal neovascularization (CNV), potentially identifying lesions before they are visible on conventional OCT or fluorescein angiography 28.
Dry macular degeneration treatment
For now, there’s no way to reverse damage from dry macular degeneration. If your condition is diagnosed early, you can take steps to help slow its progression, such as taking vitamin supplements, eating healthfully and not smoking.
Vitamin supplements
For people with intermediate or advanced dry AMD, taking a high-dose formulation of antioxidant vitamins and minerals may help reduce the risk of vision loss. Research from the Age-Related Eye Disease Study 2 (AREDS2) has shown benefit in a formulation that includes 29, 30:
- 500 milligrams (mg) of vitamin C
- 400 international units (IU) of vitamin E
- 10 mg of lutein
- 2 mg of zeaxanthin
- 80 mg of zinc (as zinc oxide)
- 2 mg of copper (as cupric oxide)
Furthermore, the use of antioxidant vitamins (e.g., vitamin C, vitamin E), lutein, zeaxanthin, and zinc in an otherwise well-nourished population with intermediate age related macular degeneration has been demonstrated to reduce the progression toward more advanced stages of age related macular degeneration by approximately 25% at 5 years 31, 32.
However, the evidence doesn’t show benefit in these supplements for people with early-stage dry macular degeneration. In addition, high doses of vitamin E may increase the risk of heart failure and other complications. Ask your doctor if taking supplements is right for you.
Low vision rehabilitation
Age-related macular degeneration doesn’t affect your side (peripheral) vision and usually doesn’t cause total blindness. But it can reduce or eliminate your central vision — which is necessary for driving an automobile, reading and recognizing people’s faces. It may help for you to get care from a low vision rehabilitation specialist, an occupational therapist, your eye doctor and others trained in low vision rehabilitation. They can help you find ways to adapt to your changing vision.
Surgery to implant a telescopic lens
For selected people with advanced dry macular degeneration in both eyes, an option to improve vision may be surgery to implant a telescopic lens in one eye. The telescopic lens, which looks like a tiny plastic tube, is equipped with lenses that magnify your field of vision. The telescopic lens implant may improve both distance and close-up vision, but it has a very narrow field of view. It can be particularly useful in an urban environment to aid in identifying street signs.
Lifestyle and home remedies
Even after receiving a diagnosis of dry macular degeneration, you can take steps that may help slow vision loss.
- Don’t smoke. If you smoke, ask your doctor for help to quit.
- Choose a healthy diet. The antioxidant vitamins in fruits and vegetables contribute to eye health. Kale, spinach, broccoli, peas and other vegetables have high levels of antioxidants, including lutein and zeaxanthin, which may benefit people with macular degeneration. Foods containing high levels of zinc may also be of particular value in patients with macular degeneration. These include high-protein foods, such as beef, pork and lamb. Nonmeat sources include milk, cheese, yogurt, whole-grain cereals and whole-wheat bread.
- Another good choice is healthy unsaturated fats, such as olive oil. And research studies have shown that a diet high in omega-3 fatty acids, such as found in salmon, tuna and walnuts, may lower the risk for advanced AMD. But the same benefit is not shown from taking omega-3 supplements, such as fish oil pills.
- Manage your other medical conditions. If you have cardiovascular disease or high blood pressure, for example, take your medication and follow your doctor’s instructions for controlling the condition.
- Maintain a healthy weight and exercise regularly. If you need to lose weight, reduce the number of calories you eat and increase the amount of exercise you get each day. Maintain a healthy weight by exercising regularly and controlling your diet.
- Have routine eye exams. Ask your eye doctor about the recommended schedule for follow-up exams. In between checkups, you can do a self-assessment of your vision using an Amsler grid. These steps will help identify if your condition develops into wet macular degeneration, which can be treated with drugs.
Coping and support
These tips may help you cope with your changing vision:
- Ask your eye doctor to check your eyeglasses. If you wear contacts or glasses, be sure your prescription is up to date.
- Use magnifiers. A variety of magnifying devices can help you with reading and other close-up work, such as sewing. Such devices include hand-held magnifying lenses or magnifying lenses you wear like glasses. You may also use a closed-circuit television system that uses a video camera to magnify reading material and project it on a video screen.
- Change your computer display and add audio systems. Adjust the font size in your computer’s settings. And adjust your monitor to show more contrast. You may also add speech-output systems or other technologies to your computer.
- Use electronic reading aids and voice interface. Try large-print books, tablet computers and audio books. Some tablet and smartphone apps are designed to help people with low vision. And many of these devices now come with a voice recognition system, which can be a helpful low vision aid.
- Select special appliances made for low vision. Some clocks, radios, telephones and other appliances have extra-large numbers. You may find it easier to watch a television with a larger high-definition screen, or you may want to sit closer to the screen.
- Use brighter lights in your home. Better lighting helps with reading and other daily activities, and it may also reduce the risk of falling.
- Consider your transportation options. If you drive, check with your doctor to see if it’s safe to continue doing so. Be extra cautious in certain situations, such as driving at night, in heavy traffic or in bad weather. Use public transportation or ask family members to help, especially with night driving. Make arrangements to use local van or shuttle services, volunteer driving networks, or rideshares.
- Get support. Having macular degeneration can be difficult, and you may need to make changes in your life. You may go through many emotions as you adjust. Consider talking to a counselor or joining a support group. Spend time with supportive family members and friends.
Wet macular degeneration
Wet macular degeneration (wet AMD) also called neovascular AMD or exudative AMD is a chronic eye disease that causes blurred vision or a blind spot in your visual field. It’s generally caused by abnormal blood vessels that leak fluid or blood into the macula. The macula is in the part of the retina responsible for central vision 33.
Wet macular degeneration is one of two types of age-related macular degeneration. The other type — dry macular degeneration (dry AMD) — which is more common and less severe. The wet AMD always begins as the dry AMD. Approximately 10% of patients with age-related macular degeneration (AMD) develop choroidal neovascularization, which is the hallmark of wet age-related macular degeneration (wet AMD).
Early detection and treatment of wet macular degeneration may help reduce vision loss and, in some instances, recover vision. Regular administration of intravitreal anti-VEGF medications may prevent blindness in most patients with wet AMD 34. In the absence of such treatment, patients experience severe, irreversible vision loss 35. In the absence of anti-VEGF therapy, around 79% to 90% of affected eyes eventually become legally blind due to complications from neovascularization 36.
Wet macular degeneration symptoms
Wet macular degeneration symptoms usually appear suddenly and worsen rapidly. They may include:
- Visual distortions, such as straight lines seeming bent
- Reduced central vision in one or both eyes
- The need for brighter light when reading or doing close-up work.
- Difficulty adjusting to low light levels, such as when entering a dimly lit restaurant or theater.
- Decreased intensity or brightness of colors
- A well-defined blurry spot or blind spot in your field of vision
- A general haziness in your overall vision
- Increased blurriness of printed words.
- Difficulty recognizing faces.
- Abrupt onset and rapid worsening of symptoms
Macular degeneration doesn’t affect side (peripheral) vision, so it rarely causes total blindness.
Wet macular degeneration complication
People whose wet macular degeneration has progressed to central vision loss have a higher risk of depression and social isolation. With profound loss of vision, people may see visual hallucinations. This condition is known as Charles Bonnet syndrome.
Wet macular degeneration causes
No one knows the exact cause of wet macular degeneration, but it develops in people who have had dry macular degeneration. Of all people with age-related macular degeneration (AMD), about 20 percent have the wet AMD.
Wet macular degeneration can develop in different ways:
- Vision loss caused by abnormal blood vessel growth. Sometimes abnormal new blood vessels grow from the choroid under and into the macula called choroidal neovascularization (CNV). The choroid is the layer of blood vessels between the retina and the outer, firm coat of the eye called the sclera. These abnormal blood vessels may leak fluid or blood, interfering with the retina’s function.
- Vision loss caused by fluid buildup in the back of the eye. When fluid leaks from the choroid, it can collect between the choroid and a thin cell layer called the retinal pigment epithelium (RPE) and the retina or within the layers of the retina. This may cause irregularities in the macula layers, resulting in vision loss or distortion.
Vascular endothelial growth factor (VEGF) plays a critical role in the development of choroidal neovascularization (CNV), where new vessels grow under or through the retinal pigment epithelium (RPE), often through breaks in the Bruch membrane, leading to complications such as bleeding under the retina, retinal pigment epithelium detachment or atrophy, hard exudate deposition, or subretinal or subretinal pigment epithelium fluid accumulation with associated vision loss 37.
Dr. John Donald MacIntyre Gass classified choroidal neovascularization (CNV) into 2 types based on their anatomic histopathological location 38:
- Type 1 choroidal neovascularization is located below the retinal pigment epithelium (RPE). This type is typically observed in AMD and correlates with occult choroidal neovascularization (CNV) in fluorescein angiography 39
- Type 2 choroidal neovascularization is subretinal, occurring between the retina and the retinal pigment epithelium (RPE). This type is typically noted with choroidal neovascularization (CNV) secondary to presumed ocular histoplasmosis syndrome. Classic choroidal neovascularization (CNV) in wet AMD is a type 2 choroidal neovascularization (CNV).
Type 3 neovascularization (retinal angiomatous proliferation or RAP) starts intraretinally and then reaches the subretinal or sub-RPE area 40, 41. The origin of neovascularization may vary and may not start in the choroid itself. Thus, according to the Consensus Nomenclature for Reporting Neovascular Age-Related Macular Degeneration, these subtypes are currently included under the broad term macular neovascularization (MNV).
Macular neovascularization (MNV) is further classified into 3 types based on multimodal imaging characteristics, including optical coherence tomography (OCT), OCT angiography, fluorescein angiography, and indocyanine green angiography (ICGA).
- Type 1 macular neovascularization the neovascularization process starts at the choriocapillaris and grows into and within the sub-RPE space, leading to different types of pigment epithelial detachment (PED). Polypoidal choroidal vasculopathy (PCV) is a subtype of type 1 macular neovascularization.
- Type 2 macular neovascularization originates in the choroid and passes through the Bruch membrane and RPE to reach the subretinal space, where it proliferates.
- Type 3 macular neovascularization, the new vessel starts from the retinal circulation, typically in the deep retinal capillary plexus, and then grows toward the outer retina.[21]
Wet macular degeneration risk factors
Factors that may increase your risk of macular degeneration include:
- Age. Age-related macular degeneration (AMD) is most common in people over 65.
- Family history and genetics. Age-related macular degeneration (AMD) has a hereditary component. Researchers have identified several genes related to developing the condition.
- Race. Macular degeneration is more common in white people.
- Smoking. Smoking cigarettes or being regularly exposed to tobacco smoke significantly increases your risk of macular degeneration.
- Obesity. Research indicates that being obese increases the chance that early or intermediate macular degeneration will progress to a more severe form of the disease.
- Cardiovascular disease. If you have diseases that affect your heart and blood vessels, you may be at higher risk of macular degeneration.
Wet macular degeneration prevention
The following measures may help reduce your risk of developing wet macular degeneration:
- Have routine eye exams. Ask your eye doctor how often you need to undergo routine eye exams. A dilated eye exam can identify macular degeneration. In between checkups, you can do a self-assessment of your vision using an Amsler grid.
- Manage your other medical conditions. For example, if you have cardiovascular disease or high blood pressure, take your medication and follow your doctor’s instructions for controlling the condition.
- Don’t smoke. Smokers are more likely to develop macular degeneration than are nonsmokers. Ask your doctor for help to stop smoking.
- Maintain a healthy weight and exercise regularly. If you need to lose weight, reduce the number of calories you eat and increase the amount of exercise you get each day. Maintain a healthy weight by exercising regularly and controlling your diet.
- Choose a healthy diet. Include fruits, leafy greens, nuts and fish high in omega-3 fatty acids, such as salmon. Nuts such as walnuts also contain omega-3 fatty acids. These foods contain antioxidant vitamins that reduce your risk of developing macular degeneration.
- Take certain nutritional supplements. If you have intermediate or advanced macular degeneration, taking supplements with high levels of vitamins C and E, zinc and copper may reduce the risk of vision loss, the American Academy of Ophthalmology says. Ask your doctor if taking supplements is right for you.
Vitamin supplements
For people with intermediate or advanced disease, taking a high-dose formulation of antioxidant vitamins and minerals may help reduce the risk of vision loss, the American Academy of Ophthalmology says 42. Research shows benefit in a formulation that includes:
- 500 milligrams (mg) of vitamin C
- 400 international units (IU) of vitamin E
- 10 mg of lutein
- 2 mg of zeaxanthin
- 80 mg of zinc (as zinc oxide)
- 2 mg of copper (as cupric oxide)
Furthermore, the use of antioxidant vitamins (e.g., vitamin C, vitamin E), lutein, zeaxanthin, and zinc in an otherwise well-nourished population with intermediate age related macular degeneration has been demonstrated to reduce the progression toward more advanced stages of age related macular degeneration by approximately 25% at 5 years 31, 32.
However, the evidence doesn’t show benefit in these supplements for people with early-stage dry macular degeneration. In addition, high doses of vitamin E may increase the risk of heart failure and other complications. Ask your doctor if taking supplements is right for you.
Wet macular degeneration diagnosis
Your doctor will review your medical and family history and conduct a complete eye exam. To confirm a diagnosis of macular degeneration, he or she may do several other tests, including:
- Examination of the back of your eye. Your eye doctor will put drops in your eyes to dilate them and use a special instrument to examine the back of your eye. He or she will look for fluid or blood or a mottled appearance that’s caused by drusen. People with macular degeneration often have many drusen — yellow deposits that form under the retina.
- Test for defects in the center of your vision. During an eye exam, your eye doctor may use an Amsler grid to test for defects in your central vision. If you have macular degeneration, some of the straight lines in the grid will look faded, broken or distorted.
- Fluorescein angiography. During this test, your doctor injects a colored dye into a vein in your arm. The dye travels to and highlights the blood vessels in your eye. A special camera takes pictures as the dye travels through the blood vessels. The images will show if you have abnormal blood vessels or retinal changes.
- Indocyanine green angiography. Like fluorescein angiography, this test uses an injected dye. It may be used to confirm the findings of a fluorescein angiography or to identify specific types of macular degeneration.
- Optical coherence tomography (OCT). This noninvasive imaging test displays detailed cross-sections of the retina. It identifies areas of thinning, thickening or swelling. This test is also used to help monitor how the retina responds to macular degeneration treatments.
- Optical coherence tomography angiography (OCTA). Optical coherence tomography angiography (OCTA) is a newer technology that creates images of the retinal circulation by obtaining sequential B-scans from a single area, and decorrelation signals are generated to show only areas with movement, such as flow-through vessels 27. Optical coherence tomography angiography (OCTA) may facilitate the earlier diagnosis of choroidal neovascularization (CNV), potentially identifying lesions before they are visible on conventional OCT or fluorescein angiography 28.
Wet AMD related choroidal neovascularization (CNV) has several different appearances on the dilated funduscopic examination 43:
- A gray-green membrane deep into the retina, often associated with an overlying neurosensory retinal detachment.
- Presence of blood, lipid, or subretinal fluid.
- Retinal pigment epithelium (RPE) detachment appears clinically as dome-shaped, sharply demarcated elevations of the retinal pigment epithelium (RPE), which may also be serous, fibrovascular, drusenoid, or hemorrhagic 44. A notch in serous pigment epithelial detachment (PED) may indicate the location of occult choroidal neovascularization (CNV) membranes 45.
- Massive subretinal hemorrhage with central vision loss or less commonly, breakthrough vitreous hemorrhage with peripheral vision loss.
- Retinal pigment epithelium (RPE) tear or rip 46.
- Disciform scars may be present, appearing as white or yellow subretinal membranes with or without RPE hyperplasia and pigmentation.
The use of blood thinners and hematological disorders should be ruled out in patients with massive subretinal hemorrhage (the size of at least 4 disc areas).
Wet macular degeneration treatment
Treatments are available that may help slow disease progression, preserve existing vision and, if started early enough, recover some lost vision.
Medications to stop growth of abnormal blood vessels
Medications may help stop growth of new blood vessels called anti-VEGF drugs, may help stop the growth of new blood vessels by blocking the effects of growth signals the body sends to generate new blood vessels. These drugs are considered the first line treatment for all stages of wet macular degeneration.
Medications used to treat wet macular degeneration include:
- Bevacizumab (Avastin)
- Ranibizumab (Lucentis)
- Aflibercept (Eylea)
- Brolucizumab (Beovu)
- Ranibizumab injection for intravitreal use via ocular implant (SUSVIMO)
- Faricimab-svoa (Vabysmo)
Your eye doctor injects these medicines into the affected eye. You may need injections every 4 to 6 weeks to maintain the beneficial effect of the medication. In some instances, you may partially recover vision as the blood vessels shrink and the fluid under the retina absorbs, allowing retinal cells to regain some function.
Possible risks of eye injections include conjunctival hemorrhage, eye pain, floaters, increased eye pressure and eye inflammation. Some of these medications may increase the risk of stroke.
Possible risks of eye injections include:
- Conjunctival hemorrhage.
- Increased eye pressure.
- Infection.
- Retinal detachment.
- Eye inflammation.
Intravitreal anti-VEGF agents come with several risks. Common adverse events include subconjunctival hemorrhage and discomfort during or after the procedure, often due to the iodine-based antiseptic used to clean the ocular surface. Floaters may be caused by bubbles in the syringe or the medication itself. Serious adverse events rarely occur and can include vitreous hemorrhage or endophthalmitis 47.
Several studies have also explored potential systemic adverse events related to intravitreal anti-VEGF administration, including the risk of myocardial infarction, stroke, nonocular hemorrhage, and thromboembolic events. Current evidence does not suggest an increase in systemic morbidity or mortality from the intravitreal administration of anti-VEGF agents 48. However, this theoretical risk is still important to discuss with patients, especially those deemed to be at higher risk.
Anti-VEGF treatment regimens
Anti-VEGF drugs are administered according to various regimens 33:
- Most anti-VEGF drugs are approved for fixed dosage with the following possible schedules:
- Monthly or every 28 days (ranibizumab 0.5 mg)
- Bimonthly after the initial 3 monthly (every 28 days) injections (aflibercept 2 mg)
- Every 8 to 12 weeks (brolucizumab 6 mg) after the initial 3 monthly (every 25-31 days) doses
- Up to every 16 weeks (faricimab 6 mg) after a loading dose of 4 monthly (every 28±7 days) injections
- A pro re nata (PRN or as needed) schedule where a patient receives injections only when the disease appears active, such as in subretinal or intraretinal fluid on OCT, retinal hemorrhage, or leakage on fluorescein angiography 49
- A treat-and-extend (TAE) protocol, where injection frequency is slowly extended as long as disease activity remains controlled 50, 51
- A treat-extend-stop protocol, where the patient receives an anti-VEGF agent every month for at least 3 months until the OCT confirms dry macula. If the fovea remains dry, as per the TAE protocol, the interval between injections can increase by 1 to 2 weeks until a 12-week interval is reached. The injections are stopped in patients with at least 7 injections and dry macula at the third 12-week visit. Monthly evaluations are performed to monitor for choroidal neovascularization (CNV) recurrence in approximately 30% of patients 52
- A treat-extend-pause-and-monitor protocol initially follows a treat-and-extend (TAE) protocol 53. Injections were paused in stable patients who had reached 12-weekly injections and started a pro re nata (PRN) protocol. The patient was contacted 6 weeks after the last injection (18 weeks from the previous visit). If stable, no injection was given, and the patient was scheduled for a follow-up evaluation 12 weeks later.
Although monthly injections are more effective compared to pro re nata (PRN) regimens, evidence comparing PRN to treat-and-extend (TAE) regimens remains inconclusive. Endophthalmitis is more likely with monthly injections, and patients receive more injections with monthly and treat-and-extend (TAE) dosing compared to pro re nata (PRN). However, PRN regimens require more frequent clinic visits compared to TAE dosing 54.
Long-term data suggest that PRN dosing may result in slightly worse visual outcomes compared to monthly injections after a year. This difference may be clinically insignificant after a year but may become crucial after several years of treatment. Ultimately, the clinician and patient should work together to choose the best treatment option.
Using light to activate an injected medication (photodynamic therapy)
Photodynamic therapy is sometimes used to treat abnormal blood vessels at the center of your macula in wet macular degeneration (wet AMD). However, it is much less common than treatment with anti-VEGF injections.
During photodynamic therapy, your eye doctor injects a medicine called verteporfin (Visudyne) into a vein in your arm. The medicine then travels to blood vessels in your eye. Your eye doctor shines a focused light from a special laser on the problem blood vessels in your eye. This activates the verteporfin, causing the problem blood vessels to close. This stops the leakage.
Photodynamic therapy may improve your vision and reduce the rate of vision loss. You may need repeated treatments over time, as the treated blood vessels may reopen.
After photodynamic therapy, you’ll need to avoid direct sunlight and bright lights until the drug has cleared your body, which may take a few days.
Using a laser to destroy abnormal blood vessels (photocoagulation therapy)
During laser photocoagulation therapy, your doctor uses a high-energy laser beam to seal abnormal blood vessels under the macula. The laser causes scarring that can create a blind spot, but the procedure is used to stop the vessels from bleeding with the aim of minimizing further damage to the macula. Even with this treatment, blood vessels may regrow, requiring further treatment.
Few people who have wet macular degeneration are candidates for this treatment. It generally isn’t an option if you have abnormal blood vessels directly under the center of the macula. Also, the more damaged your macula is, the lower the likelihood of success.
Low vision rehabilitation
Age-related macular degeneration doesn’t affect your side (peripheral) vision and usually doesn’t cause total blindness. But it can reduce or eliminate your central vision — which is necessary for driving, reading and recognizing people’s faces. It may be beneficial for you to work with a low vision rehabilitation specialist, an occupational therapist, your eye doctor and others trained in low vision rehabilitation. They can help you find ways to adapt to your changing vision.
Lifestyle and home remedies
Even after receiving a diagnosis of wet macular degeneration, you can take steps that may help slow vision loss.
- Don’t smoke. If you smoke, ask your doctor for help quitting.
- Choose a healthy diet. The antioxidant vitamins in fruits and vegetables contribute to eye health. Kale, spinach, broccoli, squash and other vegetables have high levels of antioxidants, including lutein and zeaxanthin. These nutrients may benefit people with macular degeneration. Eating foods containing high levels of zinc also may be helpful for people with macular degeneration. These include high-protein foods, such as beef, pork and lamb. Nonmeat sources include milk, cheese, yogurt, whole-grain cereals and whole-wheat bread. Another good choice is healthy unsaturated fat, such as in olive oil. And research studies have shown that a diet high in omega-3 fatty acids, such as in salmon, tuna and walnuts, may lower the risk of advanced macular degeneration. But the same benefit is not shown from taking omega-3 supplements, such as fish oil pills.
- Manage your other medical conditions. If you have cardiovascular disease or high blood pressure, for example, take your medicine and follow your health care provider’s instructions for controlling the condition.
- Maintain a healthy weight and exercise regularly. If you need to lose weight, reduce the number of calories you eat and increase the amount of exercise you get each day.
- Have regular eye exams. Ask your eye doctor about the recommended schedule for follow-up exams. In between checkups, you can do a self-assessment of your vision using an Amsler grid.
Coping and support
Vision loss from macular degeneration can affect your ability to do things such as read, recognize faces and drive. These tips may help you cope with your changing vision:
- Ask your eye doctor to check your eyeglasses. If you wear contacts or glasses, be sure your prescription is up to date.
- Use magnifiers. A variety of magnifying devices can help you with reading and other close-up work, such as sewing. Such devices include hand-held magnifying lenses or magnifying lenses you wear like glasses. You may also use a closed-circuit television system that uses a video camera to magnify reading material and project it on a video screen.
- Change your computer display and add audio systems. Adjust the font size in your computer’s settings. And adjust your monitor to show more contrast. You may also add speech-output systems or other technologies to your computer.
- Use electronic reading aids and voice interface. Try large-print books, tablet computers and audio books. Some tablet and smartphone apps are designed to help people with low vision. And many of these devices now come with a voice recognition feature.
- Select special appliances made for low vision. Some clocks, radios, telephones and other appliances have extra-large numbers. You may find it easier to watch a television with a larger high definition screen, or you may want to sit closer to the screen.
- Use brighter lights in your home. Better lighting helps with reading and other daily activities, and it may also reduce the risk of falling.
- Consider your transportation options. If you drive, check with your doctor to see if it’s safe to continue doing so. Be extra cautious in certain situations, such as driving at night, in heavy traffic or in bad weather. Use public transportation or ask a friend or family member to help, especially with night driving.
- Make arrangements to use local van or shuttle services, volunteer driving networks, or rideshares.
Get support. Having macular degeneration can be difficult, and you may need to make changes in your life. You may go through many emotions as you adjust. Consider talking to a counselor or joining a support group. Spend time with supportive family members and friends.
Wet macular degeneration prognosis
If left untreated for 2 to 3 years, around 50% to 60% of eyes with wet AMD and subfoveal choroidal neovascularization (CNV) lose 6 or more lines of vision, compared to 20% to 30% of eyes with any submacular choroidal neovascularization (CNV) 55, 56, 57. Classic choroidal neovascularization (CNV) is associated with poorer visual outcomes compared to occult or minimally classic CNV, and up to 50% of the patients without classic lesions on initial presentation may develop classic CNV within 1 year after diagnosis 58, 59.
Eyes with large subretinal hemorrhages that involve the fovea often have poor visual outcomes. However, some eyes have surprisingly good visual recovery, suggesting that prompt treatment, such as intravitreal anti-VEGF medications or surgery, is still beneficial 60. Retinal pigment epithelium (RPE) tears involving the fovea also generally result in poor visual acuity and an elevated risk of vision loss from an retinal pigment epithelium (RPE) tear in the fellow eye 61.
The cause of age-related macular degeneration (AMD) is not known. But age-related macular degeneration (AMD) is more common in people who smoke, who are overweight, who eat an unhealthy diet or who have a condition that affects their blood vessels, like high cholesterol or diabetes.
There are two types of age related macular degeneration (AMD): wet macular degeneration and dry macular degeneration 1.
- Wet age-related macular degeneration (wet AMD) also called neovascular AMD happens when abnormal blood vessels grow from the choroid underneath the macula. This is called choroidal neovascularization. “Neovascularization” means “new blood vessels”. These new abnormal blood vessels often leak blood and fluid leading to distorted vision. This is the most serious kind. Wet age-related macular degeneration damages the macula quickly. That makes straight lines look zigzag and wavy, as well as blind spots and loss of central vision. These abnormal blood vessels and bleeding from them eventually form a scar, leading to permanent loss of central vision.
- Dry age-related macular degeneration (dry AMD) also known as non-neovascular AMD or atrophic AMD happens when the light-sensitive cells in the macula slowly break down. The “dry” form of macular degeneration is identified by the presence of yellow deposits called drusen in the macula. It is the most common kind. About 80 percent (8 out of 10) of people who have age-related macular degeneration (AMD) have the dry form. A few small drusen may not cause any changes in vision. However, as they grow in numbers and size, they may lead to a dimming or distortion of vision. Then people start noticing when they read. A common early symptom is that straight lines appear crooked. In the later stages of dry macular degeneration, there is also a thinning of the light-sensitive layer of cells in the macula leading to atrophy, or tissue death. Atrophy of the retinal pigment epithelium occurs in the advanced stage of the disease known as geographic atrophy. Geographic atrophy on involving the center of the macula leads to significant visual loss. In the atrophic form of dry macular degeneration, patients may have blind spots in the center of their vision. In more advanced stages, patients lose central vision.
Wet age-related macular degeneration (wet AMD) is differentiated from early or dry AMD by the presence of choroidal neovascularization (CNV), where new blood vessels from the choroid penetrate through the Bruch membrane and proliferate either between the Bruch membrane and the retinal pigment epithelium (RPE) or in the subretinal space 62. Various factors contribute to the development of choroidal neovascularization (CNV) and vision loss in patients with wet AMD 63. These factors include the following:
- Vascular endothelial growth factor (VEGF) plays a critical role in the development of choroidal neovascularization (CNV), where new vessels grow under or through the retinal pigment epithelium (RPE), often through breaks in the Bruch membrane, leading to complications such as bleeding under the retina, retinal pigment epithelium detachment or atrophy, hard exudate deposition, or subretinal or subretinal pigment epithelium fluid accumulation with associated vision loss 37.
- Growth of new blood vessels with the proliferation of fibrous tissue
- Leakage of fluid, proteins, and lipids from the new vessels
- Bleeding from the fragile new vessels
- Fibrovascular scar formation, with the death of the neurosensory retina and vision loss
AMD is a multifactorial disease, and numerous risk factors have been identified. The main risk factors for the development of advanced age-related macular degeneration (AMD) are increasing age, ethnicity, and genetics. Although a number of modifiable risk factors have been investigated, cigarette smoking is the main modifiable risk factor that has been consistently identified in numerous studies 64. Importantly, it is essential to recognize that the associations found in observational studies that analyze risk factors should not be interpreted as cause and effect. Such associations may not necessarily translate into treatment recommendations, as there may be multiple confounding variables that are not accounted for in the studies.
Risk factors for developing early age related macular degeneration (AMD) include 65, 66, 4, 26, 67:
- Older age. AMD is more common in older adults. Age-related macular degeneration (AMD) is the leading cause of severe vision loss in adults above the age of 60.
- Ethnic Background: Fair-skinned people of northern European ancestry (Scandinavian, English, or German descent) have a higher chance of developing macular degeneration. Early AMD is more common in individuals of European ancestry than in Asians, whereas the prevalence of late AMD is the same between the two populations. Both early and late age-related macular degeneration are known to be common among non-Hispanic whites when compared to blacks and Hispanics 68.
- Presence of AMD in the other eye
- Family history of AMD. Macular degeneration tends to “run in families”. This means that there is a genetic factor that predisposes a person toward developing the condition. Anytime a “bloodline” relative has macular degeneration, you run an increased chance of developing the condition. A genetic predisposition to AMD is evident as at least 34 genetic loci and 52 gene mutations are associated with age-related macular degeneration 69. Consult with your eye doctor about your risk.
- Women tend to develop AMD earlier than men.
- Diet low in omega 3 and 6 fatty acids, vitamins, carotenoid and minerals
- Diet high in saturated fat
- Lifestyle factors
- Smoking. Macular degeneration tends to occur more frequently in persons who smoke. Even after treatment, smokers are reported to have a greater chance of having macular problems recur 70
- Poor diet and nutrition
- Obesity (BMI of 30 kg/m2 or higher)
- Alcohol consumption
- Lack of exercise
- Sunlight exposure. Long-term bright light exposure may be a risk factor for AMD. The Chesapeake Bay Waterman Study suggested that fisherman exposed to daily bright sunlight may have an increased risk. Certainly, staring at bright light such as the sun, for even a few minutes, can cause permanent damage to the retina. Many ophthalmologists recommend the use of sunglasses and a hat to protect against potentially harmful bright sunlight.
- Medical risk factors
- High blood pressure (hypertension). High blood pressure is a risk factor for developing wet AMD. High blood pressure, like smoking, leads to a constriction, or narrowing, of the blood vessels that nourish the retina, negatively affecting its health.
- Hypercholesterolemia
- Hypertriglyceridemia
- Coronary artery and blood vessel disease (atherosclerosis) 71
- Cerebrovascular disease
- Diabetes
- Family history
- Studies have suggested that inflammation plays a role in the pathogenesis of drusen and wet AMD. Various complement-related genetic variants are associated with AMD, most notably, polymorphisms of complement factor H (CFH) gene, which normally inhibits the alternative complement pathway, are among the best-known mutations in AMD 72, 73. These include Y402H in the complement factor H gene and other variants in factor B /complement component 2, complement component 3, and complement Factor I 74.
It’s important to have regular eye exams to identify early signs of macular degeneration. The following measures may help reduce your risk of developing age-related macular degeneration (AMD) 65:
- Don’t smoke. Smokers are more likely to develop macular degeneration than are nonsmokers. Smoking is a definite risk factor for AMD, as well as other serious diseases. Anyone who smokes should stop, especially if they already have signs of AMD. It will help save your vision.
- Maintain a healthy weight and exercise regularly. If you need to lose weight, reduce the number of calories you eat and increase the amount of exercise you get each day.
- Choose a diet rich in fruits and vegetables. These foods contain antioxidant vitamins that reduce your risk of developing macular degeneration.
- Increased vitamin E intake
- Increased zinc intake
- Increased combined intake of vitamin C, vitamin E, beta-carotene and zinc
- Include fish in your diet. Omega-3 fatty acids, which are found in fish, may reduce the risk of macular degeneration. Nuts such as walnuts also contain omega-3 fatty acids.
- Hormone replacement therapy (HRT) or estrogen therapy in women after menopause has been found to have a potential protective effect 75.
- Manage all medical conditions. For example, if you have cardiovascular disease or high blood pressure, take your medicine and follow your health care provider’s instructions for controlling the condition.
The Age-Related Eye Disease Study (AREDS) documented that antioxidant and zinc supplementation decreases the risk of AMD progression and vision loss 76.
AREDS 2 supplements are made of large amounts of certain vitamins and minerals 76:
- 500 milligrams (mg) of vitamin C
- 400 international units (IU) of vitamin E
- 10 mg of lutein
- 2 mg of zeaxanthin
- 80 mg of zinc (as zinc oxide)
- 2 mg of copper (as cupric oxide)
The symptoms of age-related macular degeneration depend on the stage.
Dry AMD happens in 3 stages: early, intermediate, and late. AMD is a progressive disease — that means symptoms usually get worse over time.
- Early dry AMD doesn’t cause any symptoms.
- In intermediate dry AMD, some people still have no symptoms. Others may notice mild symptoms, like mild blurriness in their central vision or trouble seeing in low lighting.
- In late AMD (wet or dry type), many people notice that straight lines start to look wavy or crooked. You may also notice a blurry area near the center of your vision. Over time, this blurry area may get bigger or you may see blank spots. Colors may also seem less bright than before, and you may have more trouble seeing in low lighting.
In its early stages, age-related macular degeneration (AMD) may not have symptoms and may be unrecognized until it progresses or affects both eyes. The first symptom of macular degeneration is usually distortion of straight lines or blurred vision with a dim, blurry spot in the center of your vision. This spot may get bigger or darker with time.
Symptoms of age-related macular degeneration (AMD) include:
- Straight lines start to appear distorted, or the center of vision becomes distorted. Straight lines looking wavy is a warning sign for late AMD. If you notice this symptom, see your eye doctor right away.
- Decreased quality or resolution of vision with blurriness and difficulty in reading the fine print, driving, etc.
- Dark, blurry areas or white out appears in the center of vision
- Reduced or altered color perception.
If you experience any of these symptoms, see an eye doctor (ophthalmologist) as soon as possible.
Dry macular degeneration symptoms
Dry macular degeneration symptoms usually develop gradually and without pain. They may include:
- Visual distortions, such as straight lines seeming bent.
- Reduced central vision in one or both eyes.
- The need for brighter light when reading or doing close-up work.
- Increased difficulty adapting to low light levels, such as when entering a dimly lit restaurant or theater.
- Increased blurriness of printed words.
- Decreased intensity or brightness of colors.
- Difficulty recognizing faces.
- A well-defined blurry spot or blind spot in the field of vision.
Dry macular degeneration can affect one or both eyes. If only one eye is affected, you may not notice any changes in your vision. This is because your good eye may compensate for the affected eye. And the condition doesn’t affect the side vision, so it does not cause total blindness.
Dry macular degeneration is one of two types of age-related macular degeneration (AMD). It can progress to wet macular degeneration, which is when abnormal blood vessels grow and leak under the retina. The dry type is more common, but it usually progresses slowly over years. The wet type is more likely to cause a relatively sudden change in vision resulting in serious vision loss.
Wet macular degeneration symptoms
Wet macular degeneration symptoms usually appear suddenly and worsen rapidly. They may include:
- Visual distortions, such as straight lines seeming bent
- Reduced central vision in one or both eyes
- The need for brighter light when reading or doing close-up work.
- Difficulty adjusting to low light levels, such as when entering a dimly lit restaurant or theater.
- Decreased intensity or brightness of colors
- A well-defined blurry spot or blind spot in your field of vision
- A general haziness in your overall vision
- Increased blurriness of printed words.
- Difficulty recognizing faces.
- Abrupt onset and rapid worsening of symptoms
Macular degeneration doesn’t affect side (peripheral) vision, so it rarely causes total blindness.
Age-related macular degeneration (AMD) has been staged into 4 groups based on clinical examination of the macula 77:
- Group 1 (no AMD): no drusen or 5–15 small drusen (<63 microns in diameter) in the absence of any other stage of AMD.
- Group 2 (early-stage AMD): more than 15 small drusen or less than 20 medium-sized (63-124 micron in diameter) indistinct soft drusen or pigment abnormalities but not geographic atrophy.
- Group 3 (intermediate stage AMD): the presence of at least one large druse ( >125 microns in diameter), or presence of numerous medium-sized drusen (approximately 20 or more drusen with indistinct boundaries and 65 or more drusen with distinct boundaries) or presence of non-central geographic atrophy i.e., atrophy not involving the fovea.
- Group 4 (advanced stage AMD): central geographic atrophy that involves the fovea or presence of neovascular AMD.
Age-related macular degeneration (AMD) can be detected in a routine eye examination. Your eye doctor (ophthalmologist) may diagnose your macular degeneration by reviewing your medical and family history and conducting a complete eye exam. An eye doctor would easily be able to detect the presence of drusen — tiny yellow deposits under the retina — or pigment clumping, during an eye exam. Your eye doctor may also ask you to look at an Amsler grid. A pattern of straight lines resembling a checkerboard. If any of the straight lines appear wavy to you, or you notice some of the lines as missing. These can be signs of macular degeneration.
If your doctor detects AMD, other tests may be performed, including:
- Examination of the back of your eye. Your eye doctor puts drops in your eyes to dilate them and uses a special instrument to examine the back of your eye. The eye doctor looks for a mottled appearance that’s caused by yellow deposits that form under the retina, called drusen. People with macular degeneration often have many drusen.
- A test for changes in the center of your vision. During an eye examination, your eye doctor may use an Amsler grid to test for changes in the center of your vision. If you have macular degeneration, some of the straight lines in the grid may look faded, broken or distorted.
- Fluorescein angiography. In fluorescein angiography, your eye doctor injects a dye into a vein in your arm. The dye travels to and highlights the blood vessels in your eye. A special camera takes several pictures as the dye travels through the blood vessels. The images will show if you have retinal or blood vessel changes, which are a sign of wet macular degeneration. If any new vessels have developed or vessels are leaking fluid or blood in the macula, the photographs will show their exact location and type.
- Indocyanine green angiography. Like fluorescein angiography, this test uses an injected dye. It may be used alongside a fluorescein angiogram to identify specific types of macular degeneration.
- Optical coherence tomography (OCT). This noninvasive imaging test displays detailed cross-sectional images of the retina. Optical coherence tomography (OCT) identifies areas where the retina may be thinning, thickening or swelling. These can be caused by fluid buildup from leaking blood vessels in and under your retina.
- Optical coherence tomography angiography (OCTA). Optical coherence tomography angiography (OCTA) is a newer technology that creates images of the retinal circulation by obtaining sequential B-scans from a single area, and decorrelation signals are generated to show only areas with movement, such as flow-through vessels 27. Optical coherence tomography angiography (OCTA) may facilitate the earlier diagnosis of choroidal neovascularization (CNV), potentially identifying lesions before they are visible on conventional OCT or fluorescein angiography 28.
Geographic Atrophy
It is the advanced stage of dry age-related macular degeneration (dry AMD). It is defined as a sharply delineated round or oval area of hypopigmentation or depigmentation or absence of the retinal pigment epithelium (RPE). The choroidal vessels are more visible than in surrounding areas, and the atrophic patch must be at least 175 µm in diameter. Geographic atrophy is known to enlarge over time, and it tends to be bilateral disease. Persons with unilateral geographic atrophy are also at risk of developing neovascular or wet age-related macular degeneration (wet AMD) in the second eye.
Most commonly, drusen precede geographic atrophy. Larger drusen, confluent drusen, refractile deposits with hyperpigmentation have been documented to evolve into geographic atrophy. Geographic atrophy may also occur due to the collapse of drusenoid retinal pigment epithelium (RPE). The retinal pigment epithelium (RPE) and photoreceptors overlying the area of drusen progressively undergo degeneration.
Neovascular age-related macular degeneration (wet AMD) is characterized by a choroidal neovascular membrane (CNVM) and related features like pigment epithelial detachment (PED), retinal pigment epithelium (RPE) rip, or disciform scarring. On fundus examination, choroidal neovascularization (CNV) is seen as a grayish-green tissue below the retina along with fluid or blood in the intraretinal or subretinal plane 43.
Degenerative changes in the Bruch’s membrane weaken its integrity. Proangiogenic growth factors stimulate the growth of abnormal vascular networks from the choriocapillaris, which perforate the Bruch’s membrane and disrupt the normal retinal pigment epithelium (RPE)-photoreceptor complex. A fibrovascular complex forms, which either lies completely below the RPE ( Type 1 choroidal neovascular membrane) or breaches the RPE and lies in the subretinal plane (Type 2 choroidal neovascular membrane). This complex can exude fluid or blood into the subretinal and intraretinal space. This fluid or blood can also accumulate beneath the RPE, causing pigment epithelium detachment. This complex progresses to a fibrotic disciform scar in the worst-case scenario.
Symptoms noticed by the patients include blurring of vision and distortion, especially for near vision. Decreased vision, micropsia, metamorphopsia, or scotoma are other presenting complaints.
On fundus examination, pigment epithelial detachment is seen as a sharply demarcated dome-shaped elevation of the RPE. Overlying neurosensory detachment, lipid or blood, and sub retinal pigment epithelium (RPE) blood is a sign that a choroidal neovascularization (CNV) is underlying the pigment epithelial detachment (PED). Rarely, this blood can pass through the retina into the vitreous cavity, causing vitreous hemorrhage.
There are 4 types of pigment epithelial detachments (PEDs): Serous, fibrovascular, drusenoid, and hemorrhagic pigment epithelial detachment 44.
- Serous pigment epithelial detachment (PED) is defined as an area of smooth, sharply demarcated dome-shaped RPE elevation. On fundus evaluation, a reddish halo of subretinal fluid can be seen. The presence of blood or pigment at the dependent part of the pigment epithelial detachment (PED) or a notched configuration of the pigment epithelial detachment (PED) raises the suspicion of the presence of an underlying choroidal neovascular membrane (CNVM). The notch is the area where the CNVM adheres to the RPE and causes it to detach from the Bruch’s membrane.
- Fibrovascular pigment epithelial detachment (PED), is an area of irregular elevation of the RPE. Its name is derived from the underlying vascular and fibrous components.
- Drusenoid pigment epithelial detachment (PED) is a detachment of the RPE caused due to the confluence of soft drusens.
- Hemorrhagic pigment epithelial detachment (PED) is characterized by the blood beneath the retinal pigment epithelium (RPE).
Treatment for age-related macular degeneration depends on the stage and type. There’s currently no treatment for early AMD, so your eye doctor will probably just keep track of how your eyes are doing with regular eye exams. Eating healthy, getting regular exercise, and quitting smoking can also help.
If you have intermediate AMD in 1 or both eyes, special dietary supplements (vitamins and minerals) may be able to stop it from turning into late AMD. If you have late AMD in only 1 eye, these supplements may slow down AMD in your other eye.
If you have wet AMD, there are 2 treatment options that can slow down or stop vision loss from wet AMD (neovascular AMD):
- Anti-VEGF injections (intravitreal anti-VEGF shots). Anti-VEGF medicines help stop bleeding and leaking from blood vessels in the back of your eye. Most people with wet AMD will get anti-VEGF injections as their only treatment. Currently used anti-VEGF medicines prevent visual loss and may also improve vision in some cases 10. Anti-VEGF injections usually only work for a short time, so most people need to get them many times. At first, most people need injections once a month. After that, your eye doctor will tell you how often you need injections to help stop vision loss from AMD.
- Photodynamic therapy (PDT). Photodynamic therapy (PDT), a combination of injections and laser treatment. Photodynamic therapy (PDT) is a much less common treatment for wet AMD that doctors sometimes use along with anti-VEGF injections. Photodynamic therapy works by using a light-sensitive medicine called verteporfin (Visudyne) that “turns on” when hit by a specific type of laser sometimes called a cold laser. Your eye doctor will shine the laser on a very small area in the back of your eye, causing the verteporfin to break down the blood vessels that are causing your vision loss. When you get photodynamic therapy (PDT), your eye doctor will:
- Give a shot of verteporfin in your arm
- Put numbing medicine in your eye
- Place a special contact lens on your eye to help guide the laser
- Shine the laser onto the extra blood vessels in the back of your eye
- Some people will need to get PDT more than once. Talk to your eye doctor to find out if you will need more treatments to help stop vision loss from AMD.
Medications to stop growth of abnormal blood vessels
Medications may help stop growth of new blood vessels called anti-VEGF drugs, may help stop the growth of new blood vessels by blocking the effects of growth signals the body sends to generate new blood vessels. These drugs are considered the first line treatment for all stages of wet macular degeneration.
Medications used to treat wet macular degeneration include:
- Bevacizumab (Avastin)
- Ranibizumab (Lucentis)
- Aflibercept (Eylea)
- Brolucizumab (Beovu)
- Ranibizumab injection for intravitreal use via ocular implant (SUSVIMO)
- Faricimab-svoa (Vabysmo)
Your eye doctor injects these medicines into the affected eye. You may need injections every 4 to 6 weeks to maintain the beneficial effect of the medication. In some instances, you may partially recover vision as the blood vessels shrink and the fluid under the retina absorbs, allowing retinal cells to regain some function.
Possible risks of eye injections include conjunctival hemorrhage, eye pain, floaters, increased eye pressure and eye inflammation. Some of these medications may increase the risk of stroke.
Possible risks of eye injections include:
- Conjunctival hemorrhage.
- Increased eye pressure.
- Infection.
- Retinal detachment.
- Eye inflammation.
Intravitreal anti-VEGF agents come with several risks. Common adverse events include subconjunctival hemorrhage and discomfort during or after the procedure, often due to the iodine-based antiseptic used to clean the ocular surface. Floaters may be caused by bubbles in the syringe or the medication itself. Serious adverse events rarely occur and can include vitreous hemorrhage or endophthalmitis 47.
Several studies have also explored potential systemic adverse events related to intravitreal anti-VEGF administration, including the risk of myocardial infarction, stroke, nonocular hemorrhage, and thromboembolic events. Current evidence does not suggest an increase in systemic morbidity or mortality from the intravitreal administration of anti-VEGF agents 48. However, this theoretical risk is still important to discuss with patients, especially those deemed to be at higher risk.
Anti-VEGF treatment regimens
Anti-VEGF drugs are administered according to various regimens 33:
- Most anti-VEGF drugs are approved for fixed dosage with the following possible schedules:
- Monthly or every 28 days (ranibizumab 0.5 mg)
- Bimonthly after the initial 3 monthly (every 28 days) injections (aflibercept 2 mg)
- Every 8 to 12 weeks (brolucizumab 6 mg) after the initial 3 monthly (every 25-31 days) doses
- Up to every 16 weeks (faricimab 6 mg) after a loading dose of 4 monthly (every 28±7 days) injections
- A pro re nata (PRN or as needed) schedule where a patient receives injections only when the disease appears active, such as in subretinal or intraretinal fluid on OCT, retinal hemorrhage, or leakage on fluorescein angiography 49
- A treat-and-extend (TAE) protocol, where injection frequency is slowly extended as long as disease activity remains controlled 50, 51
- A treat-extend-stop protocol, where the patient receives an anti-VEGF agent every month for at least 3 months until the OCT confirms dry macula. If the fovea remains dry, as per the TAE protocol, the interval between injections can increase by 1 to 2 weeks until a 12-week interval is reached. The injections are stopped in patients with at least 7 injections and dry macula at the third 12-week visit. Monthly evaluations are performed to monitor for choroidal neovascularization (CNV) recurrence in approximately 30% of patients 52
- A treat-extend-pause-and-monitor protocol initially follows a treat-and-extend (TAE) protocol 53. Injections were paused in stable patients who had reached 12-weekly injections and started a pro re nata (PRN) protocol. The patient was contacted 6 weeks after the last injection (18 weeks from the previous visit). If stable, no injection was given, and the patient was scheduled for a follow-up evaluation 12 weeks later.
Although monthly injections are more effective compared to pro re nata (PRN) regimens, evidence comparing PRN to treat-and-extend (TAE) regimens remains inconclusive. Endophthalmitis is more likely with monthly injections, and patients receive more injections with monthly and treat-and-extend (TAE) dosing compared to pro re nata (PRN). However, PRN regimens require more frequent clinic visits compared to TAE dosing 54.
Long-term data suggest that PRN dosing may result in slightly worse visual outcomes compared to monthly injections after a year. This difference may be clinically insignificant after a year but may become crucial after several years of treatment. Ultimately, the clinician and patient should work together to choose the best treatment option.
Photodynamic therapy
Photodynamic therapy is a possible treatment for the irregular blood vessel growth in wet macular degeneration (wet AMD). However, it is much less common than treatment with anti-VEGF shots. During photodynamic therapy, your eye doctor injects a medicine called verteporfin (Visudyne) into a vein in your arm. The medicine then travels to blood vessels in your eye. Your eye doctor shines a focused light from a special laser on the problem blood vessels in your eye. This activates the verteporfin, causing the problem blood vessels to close. This stops the leakage.
Photodynamic therapy may improve your vision and reduce the rate of vision loss. You may need repeated treatments over time, as the treated blood vessels may reopen.
After photodynamic therapy, you’ll need to avoid direct sunlight and bright lights until the drug has cleared your body. This may take a few days.
Photocoagulation therapy
During photocoagulation therapy, your eye doctor uses a high-energy laser beam to seal problem blood vessels under the macula. This procedure helps stop the vessels from bleeding, with the aim of minimizing further damage to the macula. Even with this treatment, blood vessels may regrow, requiring further treatment. The laser also can cause scarring that creates a blind spot.
Few people who have wet macular degeneration get this treatment. It generally isn’t an option if you have problem blood vessels directly under the center of the macula. Also, the more damaged your macula is, the lower the likelihood of success.
Vitamin supplements
For people with intermediate or advanced age-related macular degeneration, taking a high-dose formulation of antioxidant vitamins and minerals may help reduce the risk of vision loss. Research from the Age-Related Eye Disease Study 2 (AREDS2) has shown benefit in a formulation that includes:
- 500 milligrams (mg) of vitamin C
- 400 international units (IU) of vitamin E
- 10 mg of lutein
- 2 mg of zeaxanthin
- 80 mg of zinc (as zinc oxide)
- 2 mg of copper (as cupric oxide)
Ask your eye doctor if taking antioxidant vitamins and minerals supplements is right for you.
What are lutein, zeaxanthin, and beta-carotene?
Lutein, zeaxanthin, and beta-carotene belong to a family of nutrients known as carotenoids. Carotenoids are made by plants and are enriched in green leafy vegetables. They can be stored in animal tissues and are found at relatively low levels in animal-based foods. In the body, beta-carotene is used to make vitamin A, which is required by the retina to detect light and convert it into electrical signals. Beta-carotene itself is not found in the eye. In contrast, lutein and zeaxanthin are found in the retina and lens, where they may act as natural antioxidants and help absorb damaging, high-energy blue and ultraviolet light.
How do lutein and zeaxanthin compare to beta-carotene?
During the Age-Related Eye Disease Study (AREDS) and AREDS2 trials beta-carotene may increase lung cancer risk among people who smoke. Lutein and zeaxanthin are in the same family of nutrients as beta-carotene and are believed to have important functions in the retina. Lutein and zeaxanthin have not been associated with increased cancer risk.
Some studies prior to AREDS2 found that dietary intake of lutein, zeaxanthin and omega-3 fatty acids is associated with a lower risk of developing advanced AMD 30, 78, 79, 80, 81, 82, 83. Analysis from the AREDS2 trial suggests that lutein + zeaxanthin offers similar or better protective benefits against advanced AMD compared with beta-carotene. In AREDS2 trial, participants who took an AREDS formulation containing lutein + zeaxanthin lacking beta-carotene had an 18% lower risk of progressing to advanced AMD compared with those who took AREDS containing beta-carotene (no lutein or zeaxanthin). Among participants who had the lowest dietary intake of lutein and zeaxanthin, those who took AREDS with lutein + zeaxanthin had a 26% lower risk of progressing to advanced AMD compared to participants taking the original AREDS formula.
What are omega-3 fatty acids?
Omega-3 fatty acids are made by marine algae and enriched in fish oils. They are believed to be responsible for the health benefits associated with regularly eating fish, including lower rates of cardiovascular disease. The AREDS2 study focused on the omega-3 fatty acids docosahexanoic acid (DHA) and its precursor eicosapentanoic acid (EPA). DHA is needed for the integrity of retinal cells and has been shown to promote retinal development and repair in prior studies.
What is the function of copper in the Age-Related Eye Disease Study (AREDS) and AREDS2 supplements?
In Age-Related Eye Disease Study (AREDS) and AREDS2 trials, copper (as cupric oxide) was added to supplement formulas containing zinc. The goal was to reduce the risk of copper deficiency anemia, a condition associated with high levels of zinc intake. The studies showed clear benefits for patients who took an AREDS formula with zinc, with no evidence of anemia. There was no evidence that 2 mg copper was harmful, nor reason to suspect that it would be. So, in the AREDS investigators’ hands, the use of copper was safe and may have helped balance the effects of zinc.
What is the basis for the concentration of zinc in the AREDS supplements?
In the Age-Related Eye Disease Study (AREDS) trial, the 80 mg zinc dose (alone or in combination with antioxidant vitamins) was found to be effective compared to a placebo. Although zinc was found to be an essential component of the AREDS formulation, some nutritional experts recommended a lower dose. In the AREDS2 trial, there was no placebo control. Instead, participants were given the option to take the original formula or to be randomly assigned to receive a modified version, such as a formula containing 25 mg zinc. The investigators did not find a difference in the effects of 80 mg vs. 25 mg zinc. Because AREDS2 did not include a placebo control, results from AREDS, placebo-controlled trial, are still considered the gold standard.
Zinc is found in vegetables, grains, and meat. Vegetables and grains contain other molecules that can prevent zinc absorption and thus reduce its bioavailability. Supplements contain purified zinc, without these competing molecules. Although the chemical form of zinc affects its rate of absorption in the stomach, it is not clear how this affects bioavailability (i.e., the amount of zinc that reaches the retina).
What is the risk of lung cancer from taking beta-carotene?
In the AREDS2 trial, current smokers or those who had quit smoking less than a year before enrollment were excluded from receiving beta-carotene. Despite this precaution, lung cancers were observed in 2% of participants who took an AREDS formulation with beta-carotene, compared with 0.9% of participants who took AREDS without beta-carotene. Across both groups, about 91% of participants who developed lung cancer were former smokers.
The dose of vitamin E in the Age-Related Eye Disease Study (AREDS) formulation is higher than the recommended dietary allowance. Is this safe?
The recommended dietary allowance (RDA) of vitamin E for adults over 14 years old is 22.4 IU; but it is not the maximum dose. Rather, it is the dose that nutrition experts have decided is sufficient for most people to remain healthy. The Age-Related Eye Disease Study (AREDS) formula contains 400 IU to provide vitamin E beyond usual dietary intake.
The AREDS and AREDS2 trials found no adverse effects of 400 IU/day vitamin E. Other studies of adults taking more than 1,500 IU/day from natural vitamin E and 1,100 IU/day for synthetic vitamin E observed increased risk of bleeding, including brain bleeds. Most studies of vitamin E supplementation below these levels have shown beneficial or no effects on heart disease.
However, vitamin E can interact with some medications, including blood thinners, chemotherapeutic agents, and lipid-lowering drugs.
Do the Age-Related Eye Disease Study (AREDS) or AREDS2 formulations interfere with other medications?
High-dose nutritional supplements can sometimes interfere with medications and compete with other vital nutrients for absorption into the body. People who are considering taking an Age-Related Eye Disease Study (AREDS) formulation should make a list of all the medications they take to share with their doctor. The list should include supplements and over-the-counter drugs.
Does the high-dose vitamin E in the AREDS formulations affect the risk of prostate cancer?
Age-Related Eye Disease Study (AREDS) and AREDS2 found no effect of high-dose vitamin E on prostate cancer risk. However, data from other studies on the relationship between vitamin E and prostate cancer conflict:
- In 1994, the Alpha-Tocopherol, Beta Carotene (ATBC) trial found a 35% reduced risk of prostate cancer in men taking 50 mg of vitamin E (synthetic, equivalent to 56 IU) daily for a follow-up of six years 84
- In 2009, the Physicians Health Study II (PHS II) found that 400 IU of vitamin E every other day for a follow-up of eight years had no effect on the incidence of prostate cancer 85.
- In 2011, the Selenium and Vitamin E Cancer Prevention Trial (SELECT) found a 17% increase in prostate cancer risk among men taking 400 IU of vitamin E daily for a follow-up of seven years 86. That risk equates to 1-2 more prostate cancers per 1,000 patients who took high-dose vitamin E for one year. For unclear reasons, men who took both vitamin E and selenium did not have an increased rate of prostate cancer.
Many factors influence prostate cancer risk, including age, family history and race.
Low vision rehabilitation
Age-related macular degeneration (AMD) doesn’t affect your side vision and doesn’t cause total blindness. But it can reduce or eliminate your central vision, which is necessary for reading, driving and recognizing people’s faces. It may help for you to get care from a low vision rehabilitation specialist, an occupational therapist, your eye doctor and others trained in low vision rehabilitation. They can help you find ways to adapt to your changing vision.
Lifestyle and home remedies
Even after receiving a diagnosis of age related macular degeneration, you can take steps that may help slow vision loss.
- Don’t smoke. If you smoke, ask your health care provider for help quitting.
- Choose a healthy diet. The antioxidant vitamins in fruits and vegetables contribute to eye health. Kale, spinach, broccoli, squash and other vegetables have high levels of antioxidants, including lutein and zeaxanthin, which may benefit people with macular degeneration. Eating foods containing high levels of zinc also may be helpful for people with macular degeneration. These include high-protein foods, such as beef, pork and lamb. Nonmeat sources include milk, cheese, yogurt, whole-grain cereals and whole-wheat bread. Another good choice is healthy unsaturated fat, such as in olive oil. And research studies have shown that a diet high in omega-3 fatty acids, such as in salmon, tuna and walnuts, may lower the risk of advanced age-related macular degeneration (AMD). But the same benefit is not shown from taking omega-3 supplements, such as fish oil pills.
- Manage your other medical conditions. If you have cardiovascular disease or high blood pressure, for example, take your medicine and follow your provider’s instructions for controlling the condition.
- Maintain a healthy weight and exercise regularly. If you need to lose weight, reduce the number of calories you eat and increase the amount of exercise you get each day.
- Have regular eye exams. Ask your eye doctor about the recommended schedule for follow-up exams. In between checkups, you can do a self-assessment of your vision using an Amsler grid. These steps will help tell you if your condition develops into wet macular degeneration, which can be treated with medicines.
Coping and support
These tips may help you cope with your changing vision:
- Ask your eye doctor to check your eyeglass prescription. If you wear contacts or glasses, be sure your prescription is up to date. If new glasses don’t help, ask for a referral to a low vision specialist.
- Use magnifiers. A variety of magnifying devices can help you with reading and other close-up work, such as sewing. Such devices include hand-held magnifying lenses or magnifying lenses you wear like glasses. You also may use a closed-circuit television (CCTV) system that uses a video camera to magnify reading material and project it on a video screen.
- Change your computer display and add audio systems. Adjust the font size in your computer’s settings. And adjust your monitor to show more contrast. You also may add speech-output systems or other technologies to your computer.
- Use electronic reading aids and voice interfaces. Try large-print books, tablet computers and audiobooks. Some tablet and smartphone apps are designed to help people with low vision. And many of these devices now come with voice recognition systems, which can be a helpful low vision aid.
- Select special appliances made for low vision. Some clocks, radios, telephones and other appliances have extra-large numbers. You may find it easier to watch a television with a larger high-definition screen, or you may want to sit closer to the screen.
- Use brighter lights in your home. Better lighting helps with reading and other daily activities, and it also may reduce the risk of falling.
- Consider your transportation options. If you drive, check with your doctor to see if it’s safe to continue doing so. Be extra cautious in certain situations, such as driving at night, in heavy traffic or in bad weather. Use public transportation or ask family members to help, especially with night driving. Or use local van or shuttle services, volunteer driving networks, or rideshares.
- Get support. Having macular degeneration can be difficult, and you may need to make changes in your life. You may go through many emotions as you adjust. Consider talking to a counselor or joining a support group. Spend time with supportive family members and friends.
Age-related macular degeneration A(MD) is primarily an age-related retinal condition that affects a person’s central vision. In AMD a part of the retina called the macula is damaged. In advanced stages, people lose their ability to drive, to see faces, and to read smaller print. In its early stages, AMD may have no signs or symptoms, so people may not suspect they have it.
There are two types of macular degeneration — wet and dry AMD.
- Dry AMD. Dry macular degeneration is the most common. About 80% of those with AMD have the dry macular degeneration. Its exact cause is unknown, although both genetic and environmental factors are thought to play a role. This happens as the light-sensitive cells in the macula slowly break down, generally one eye at a time. The loss of vision in this condition is usually slow and gradual. It is believed that the age-related damage of an important support membrane under the retina contributes to dry age-related macular degeneration.
- Wet AMD. Wet macular degeneration is less common, it usually leads to more severe vision loss in patients than dry AMD. It is the most common cause of severe loss of vision. Wet AMD happens when abnormal blood vessels start to grow beneath the retina (choroidal neovascularization [CNV]). They leak fluid and blood — hence the name wet AMD — and can create a large blind spot in the center of the visual field. If left untreated for 2 to 3 years, around 50% to 60% of eyes with wet AMD and subfoveal choroidal neovascularization (CNV) lose 6 or more lines of vision, compared to 20% to 30% of eyes with any submacular choroidal neovascularization (CNV) 55, 56, 57. Classic choroidal neovascularization (CNV) is associated with poorer visual outcomes compared to occult or minimally classic CNV, and up to 50% of the patients without classic lesions on initial presentation may develop classic CNV within 1 year after diagnosis 58, 59.
Eyes with large subretinal hemorrhages that involve the fovea often have poor visual outcomes. However, some eyes have surprisingly good visual recovery, suggesting that prompt treatment, such as intravitreal anti-VEGF medications or surgery, is still beneficial 60. Retinal pigment epithelium (RPE) tears involving the fovea also generally result in poor visual acuity and an elevated risk of vision loss from an retinal pigment epithelium (RPE) tear in the fellow eye 61.
- de Jong PT. Age-related macular degeneration. N Engl J Med. 2006 Oct 5;355(14):1474-85. https://www.nejm.org/doi/full/10.1056/NEJMra062326[↩][↩][↩][↩][↩]
- Fleckenstein M., Keenan T. D. L., Guymer R. H., Chakravarthy U., Schmitz-Valckenberg S., Klaver C. C., Wong W. T., Chew E. Y., “Age-related macular degeneration,” Nat Rev Dis Primers 7(1), 31 (2021). 10.1038/s41572-021-00265-2[↩]
- García-Onrubia L, Valentín-Bravo FJ, Coco-Martin RM, González-Sarmiento R, Pastor JC, Usategui-Martín R, Pastor-Idoate S. Matrix Metalloproteinases in Age-Related Macular Degeneration (AMD). Int J Mol Sci. 2020 Aug 18;21(16):5934. doi: 10.3390/ijms21165934[↩]
- Ruia S, Kaufman EJ. Macular Degeneration. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560778[↩][↩][↩]
- Ozaki E, Campbell M, Kiang AS, Humphries M, Doyle SL, Humphries P. Inflammation in age-related macular degeneration. Adv Exp Med Biol. 2014;801:229-35. doi: 10.1007/978-1-4614-3209-8_30[↩]
- Wong WL, Su X, Li X, Cheung CM, Klein R, Cheng CY, Wong TY. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014 Feb;2(2):e106-16. doi: 10.1016/S2214-109X(13)70145-1[↩][↩]
- Colijn JM, Buitendijk GHS, Prokofyeva E, et al. EYE-RISK consortium; European Eye Epidemiology (E3) consortium. Prevalence of Age-Related Macular Degeneration in Europe: The Past and the Future. Ophthalmology. 2017 Dec;124(12):1753-1763. doi: 10.1016/j.ophtha.2017.05.035[↩]
- Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001 Oct;119(10):1417-36. doi: 10.1001/archopht.119.10.1417. Erratum in: Arch Ophthalmol. 2008 Sep;126(9):1251.[↩]
- Age-Related Eye Disease Study 2 Research Group. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA. 2013 May 15;309(19):2005-15. doi: 10.1001/jama.2013.4997. Erratum in: JAMA. 2013 Jul 10;310(2):208.[↩]
- Kaiser SM, Arepalli S, Ehlers JP. Current and Future Anti-VEGF Agents for Neovascular Age-Related Macular Degeneration. J Exp Pharmacol. 2021 Sep 29;13:905-912. doi: 10.2147/JEP.S259298[↩][↩]
- Mangione CM, Gutierrez PR, Lowe G, Orav EJ, Seddon JM. Influence of age-related maculopathy on visual functioning and health-related quality of life. Am J Ophthalmol. 1999 Jul;128(1):45-53. doi: 10.1016/s0002-9394(99)00169-5[↩]
- Williams RA, Brody BL, Thomas RG, Kaplan RM, Brown SI. The psychosocial impact of macular degeneration. Arch Ophthalmol. 1998 Apr;116(4):514-20. doi: 10.1001/archopht.116.4.514[↩]
- Age-Related Macular Degeneration PPP – Updated 2015. https://www.aao.org/preferred-practice-pattern/age-related-macular-degeneration-ppp-2015[↩]
- Hirabayashi K., Yu H. J., Wakatsuki Y., Marion K. M., Wykoff C. C., Sadda S. R., “OCT risk factors for development of atrophy in eyes with intermediate age-related macular degeneration,” Ophthalmol. Retina (2022). 10.1016/j.oret.2022.09.007[↩][↩]
- Liu J., Laiginhas R., Shen M., Shi Y., Li J., Trivizki O., Waheed N. K., Gregori G., Rosenfeld P. J., “Multimodal imaging and en face OCT detection of calcified drusen in eyes with age-related macular degeneration,” Ophthalmol. Sci. 2(2), 100162 (2022). 10.1016/j.xops.2022.100162[↩][↩]
- Gregori G., Wang F., Rosenfeld P. J., Yehoshua Z., Gregori N. Z., Lujan B. J., Puliafito C. A., Feuer W. J., “Spectral domain optical coherence tomography imaging of drusen in nonexudative age-related macular degeneration,” Ophthalmology 118(7), 1373–1379 (2011). 10.1016/j.ophtha.2010.11.013[↩]
- Tan A. C. S., Pilgrim M. G., Fearn S., Bertazzo S., Tsolaki E., Morrell A. P., Li M., Messinger J. D., Dolz-Marco R., Lei J., Nittala M. G., Sadda S. R., Lengyel I., Freund K. B., Curcio C. A., “Calcified nodules in retinal drusen are associated with disease progression in age-related macular degeneration,” Sci. Transl. Med. 10(466), eaat4544 (2018). 10.1126/scitranslmed.aat4544[↩]
- Ouyang Y., Heussen F. M., Hariri A., Keane P. A., Sadda S. R., “Optical coherence tomography-based observation of the natural history of drusenoid lesion in eyes with dry age-related macular degeneration,” Ophthalmology 120(12), 2656–2665 (2013). 10.1016/j.ophtha.2013.05.029[↩]
- Bonnet C., Querques G., Zerbib J., Oubraham H., Garavito R. B., Puche N., Souied E. H., “Hyperreflective pyramidal structures on optical coherence tomography in geographic atrophy areas,” Retina 34(8), 1524–1530 (2014). 10.1097/IAE.0000000000000165[↩]
- Suzuki M., Curcio C. A., Mullins R. F., Spaide R. F., “Refractile drusen: clinical imaging and candidate histology,” Retina 35(5), 859–865 (2015). 10.1097/IAE.0000000000000503[↩]
- Sarks SH, Arnold JJ, Killingsworth MC, Sarks JP. Early drusen formation in the normal and aging eye and their relation to age related maculopathy: a clinicopathological study. Br J Ophthalmol. 1999 Mar;83(3):358-68. doi: 10.1136/bjo.83.3.358[↩]
- Crabb JW, Miyagi M, Gu X, Shadrach K, West KA, Sakaguchi H, Kamei M, Hasan A, Yan L, Rayborn ME, Salomon RG, Hollyfield JG. Drusen proteome analysis: an approach to the etiology of age-related macular degeneration. Proc Natl Acad Sci U S A. 2002 Nov 12;99(23):14682-7. doi: 10.1073/pnas.222551899[↩]
- Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD, de Jong PT, Klaver CC, Klein BE, Klein R, et al. An international classification and grading system for age-related maculopathy and age-related macular degeneration. The International ARM Epidemiological Study Group. Surv Ophthalmol. 1995 Mar-Apr;39(5):367-74. doi: 10.1016/s0039-6257(05)80092-x[↩]
- Hageman GS, Mullins RF. Molecular composition of drusen as related to substructural phenotype. Mol Vis. 1999 Nov 3;5:28. http://www.molvis.org/molvis/v5/a28[↩]
- Lu J, Cheng Y, Li J, Liu Z, Shen M, Zhang Q, Liu J, Herrera G, Hiya FE, Morin R, Joseph J, Gregori G, Rosenfeld PJ, Wang RK. Automated segmentation and quantification of calcified drusen in 3D swept source OCT imaging. Biomed Opt Express. 2023 Feb 28;14(3):1292-1306. doi: 10.1364/BOE.485999[↩]
- Tomany SC, Wang JJ, Van Leeuwen R, Klein R, Mitchell P, Vingerling JR, Klein BE, Smith W, De Jong PT. Risk factors for incident age-related macular degeneration: pooled findings from 3 continents. Ophthalmology. 2004 Jul;111(7):1280-7. doi: 10.1016/j.ophtha.2003.11.010[↩][↩]
- Jia Y, Tan O, Tokayer J, Potsaid B, Wang Y, Liu JJ, Kraus MF, Subhash H, Fujimoto JG, Hornegger J, Huang D. Split-spectrum amplitude-decorrelation angiography with optical coherence tomography. Opt Express. 2012 Feb 13;20(4):4710-25. doi: 10.1364/OE.20.004710[↩][↩][↩]
- Ma J, Desai R, Nesper P, Gill M, Fawzi A, Skondra D. Optical Coherence Tomographic Angiography Imaging in Age-Related Macular Degeneration. Ophthalmol Eye Dis. 2017 Mar 20;9:1179172116686075. doi: 10.1177/1179172116686075[↩][↩][↩]
- Agrón E, Domalpally A, Cukras CA, Clemons TE, Chen Q, Lu Z, Chew EY, Keenan TDL; AREDS and AREDS2 Research Groups. Reticular Pseudodrusen: The Third Macular Risk Feature for Progression to Late Age-Related Macular Degeneration: Age-Related Eye Disease Study 2 Report 30. Ophthalmology. 2022 Oct;129(10):1107-1119. doi: 10.1016/j.ophtha.2022.05.021[↩]
- Age-Related Eye Disease Study Research Group, SanGiovanni JP, Chew EY, et al. The relationship of dietary carotenoid and vitamin A, E, and C intake with age-related macular degeneration in a case-control study: AREDS Report No. 22. Arch Ophthalmol. 2007 Sep;125(9):1225-32. doi: 10.1001/archopht.125.9.1225[↩][↩]
- Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report number 8. Arch Ophthalmol 2001;119:1417-36.[↩][↩]
- Age-Related Eye Disease Study 2 (AREDS2) Research Group, Chew EY, SanGiovanni JP, Ferris FL, et al. Lutein/zeaxanthin for the treatment of age-related cataract: AREDS2 randomized trial report number 4. JAMA Ophthalmol 2013;131:843-50.[↩][↩]
- Hobbs SD, Tripathy K, Pierce K. Wet Age-Related Macular Degeneration (AMD) [Updated 2024 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572147[↩][↩][↩]
- Ba J, Peng RS, Xu D, Li YH, Shi H, Wang Q, Yu J. Intravitreal anti-VEGF injections for treating wet age-related macular degeneration: a systematic review and meta-analysis. Drug Des Devel Ther. 2015 Sep 28;9:5397-405. doi: 10.2147/DDDT.S86269[↩]
- Chew EY, Clemons TE, Agrón E, Sperduto RD, Sangiovanni JP, Davis MD, Ferris FL 3rd; Age-Related Eye Disease Study Research Group. Ten-year follow-up of age-related macular degeneration in the age-related eye disease study: AREDS report no. 36. JAMA Ophthalmol. 2014 Mar;132(3):272-7. doi: 10.1001/jamaophthalmol.2013.6636[↩]
- Ferris FL 3rd, Fine SL, Hyman L. Age-related macular degeneration and blindness due to neovascular maculopathy. Arch Ophthalmol. 1984 Nov;102(11):1640-2. doi: 10.1001/archopht.1984.01040031330019[↩]
- Spraul CW, Lang GE, Grossniklaus HE, Lang GK. Histologic and morphometric analysis of the choroid, Bruch’s membrane, and retinal pigment epithelium in postmortem eyes with age-related macular degeneration and histologic examination of surgically excised choroidal neovascular membranes. Surv Ophthalmol. 1999 Oct;44 Suppl 1:S10-32. doi: 10.1016/s0039-6257(99)00086-7[↩][↩]
- Gass JD. Biomicroscopic and histopathologic considerations regarding the feasibility of surgical excision of subfoveal neovascular membranes. Am J Ophthalmol. 1994 Sep 15;118(3):285-98. https://www.ajo.com/article/S0002-9394(14)72951-4/pdf[↩]
- Shaimov TB, Panova IE, Shaimov RB, Shaimovа VA, Shai Mova TA, Fomin AV, Shaimov TB, Panova IE, Shaimov RB, Shaimova VA, Shaimova TA, Fomin AV. [Optical coherence tomography angiography in the diagnosis of neovascular age-related macular degeneration]. Vestn Oftalmol. 2015 Sep-Oct;131(5):4-13. Russian. doi: 10.17116/oftalma201513154-12[↩]
- Freund KB, Ho IV, Barbazetto IA, Koizumi H, Laud K, Ferrara D, Matsumoto Y, Sorenson JA, Yannuzzi L. Type 3 neovascularization: the expanded spectrum of retinal angiomatous proliferation. Retina. 2008 Feb;28(2):201-11. doi: 10.1097/IAE.0b013e3181669504[↩]
- Yannuzzi LA, Freund KB, Takahashi BS. Review of retinal angiomatous proliferation or type 3 neovascularization. Retina. 2008 Mar;28(3):375-84. doi: 10.1097/IAE.0b013e3181619c55[↩]
- Age-Related Macular Degeneration PPP – Updated 2015. https://www.aao.org/preferred-practice-pattern/age-related-macular-degeneration-ppp-2015#references[↩]
- Bressler NM, Bressler SB, Gragoudas ES. Clinical characteristics of choroidal neovascular membranes. Arch Ophthalmol. 1987 Feb;105(2):209-13. doi: 10.1001/archopht.1987.01060020063030[↩][↩]
- Zayit-Soudry S, Moroz I, Loewenstein A. Retinal pigment epithelial detachment. Surv Ophthalmol. 2007 May-Jun;52(3):227-43. doi: 10.1016/j.survophthal.2007.02.008[↩][↩]
- Gass JD. Serous retinal pigment epithelial detachment with a notch. A sign of occult choroidal neovascularization. Retina. 1984 Fall-Winter;4(4):205-20. doi: 10.1097/00006982-198400440-00001[↩]
- Tripathy K, Chawla R, Kumar V, Sharma YR, Venkatesh P. A 56-year-old male with unilateral painless diminution of vision. Oman J Ophthalmol. 2016 May-Aug;9(2):119. doi: 10.4103/0974-620X[↩]
- Bakri SJ, Thorne JE, Ho AC, Ehlers JP, Schoenberger SD, Yeh S, Kim SJ. Safety and Efficacy of Anti-Vascular Endothelial Growth Factor Therapies for Neovascular Age-Related Macular Degeneration: A Report by the American Academy of Ophthalmology. Ophthalmology. 2019 Jan;126(1):55-63. doi: 10.1016/j.ophtha.2018.07.028. Epub 2018 Aug 2. Erratum in: Ophthalmology. 2019 Jun;126(6):915. doi: 10.1016/j.ophtha.2019.04.015[↩][↩]
- Moja L, Lucenteforte E, Kwag KH, Bertele V, Campomori A, Chakravarthy U, D’Amico R, Dickersin K, Kodjikian L, Lindsley K, Loke Y, Maguire M, Martin DF, Mugelli A, Mühlbauer B, Püntmann I, Reeves B, Rogers C, Schmucker C, Subramanian ML, Virgili G. Systemic safety of bevacizumab versus ranibizumab for neovascular age-related macular degeneration. Cochrane Database Syst Rev. 2014 Sep 15;9(9):CD011230. doi: 10.1002/14651858.CD011230.pub2[↩][↩]
- Lalwani GA, Rosenfeld PJ, Fung AE, Dubovy SR, Michels S, Feuer W, Davis JL, Flynn HW Jr, Esquiabro M. A variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: year 2 of the PrONTO Study. Am J Ophthalmol. 2009 Jul;148(1):43-58.e1. doi: 10.1016/j.ajo.2009.01.024[↩][↩]
- Augsburger M, Sarra GM, Imesch P. Treat and extend versus pro re nata regimens of ranibizumab and aflibercept in neovascular age-related macular degeneration: a comparative study. Graefes Arch Clin Exp Ophthalmol. 2019 Sep;257(9):1889-1895. doi: 10.1007/s00417-019-04404-0[↩][↩]
- Kertes PJ, Galic IJ, Greve M, Williams G, Baker J, Lahaie M, Sheidow T. Efficacy of a Treat-and-Extend Regimen With Ranibizumab in Patients With Neovascular Age-Related Macular Disease: A Randomized Clinical Trial. JAMA Ophthalmol. 2020 Mar 1;138(3):244-250. doi: 10.1001/jamaophthalmol.2019.5540[↩][↩]
- Adrean SD, Chaili S, Grant S, Pirouz A. Recurrence Rate of Choroidal Neovascularization in Neovascular Age-Related Macular Degeneration Managed with a Treat-Extend-Stop Protocol. Ophthalmol Retina. 2018 Mar;2(3):225-230. doi: 10.1016/j.oret.2017.07.00[↩][↩]
- Cao X, Sanchez JC, Dinabandhu A, Guo C, Patel TP, Yang Z, Hu MW, Chen L, Wang Y, Malik D, Jee K, Daoud YJ, Handa JT, Zhang H, Qian J, Montaner S, Sodhi A. Aqueous proteins help predict the response of patients with neovascular age-related macular degeneration to anti-VEGF therapy. J Clin Invest. 2022 Jan 18;132(2):e144469. doi: 10.1172/JCI144469[↩][↩]
- Li E, Donati S, Lindsley KB, Krzystolik MG, Virgili G. Treatment regimens for administration of anti-vascular endothelial growth factor agents for neovascular age-related macular degeneration. Cochrane Database Syst Rev. 2020 May 5;5(5):CD012208. doi: 10.1002/14651858.CD012208.pub2[↩][↩]
- Laser photocoagulation of subfoveal neovascular lesions in age-related macular degeneration. Results of a randomized clinical trial. Macular Photocoagulation Study Group. Arch Ophthalmol. 1991 Sep;109(9):1220-31. doi: 10.1001/archopht.1991.01080090044025[↩][↩]
- Laser photocoagulation of subfoveal neovascular lesions of age-related macular degeneration. Updated findings from two clinical trials. Macular Photocoagulation Study Group. Arch Ophthalmol. 1993 Sep;111(9):1200-9. doi: 10.1001/archopht.1993.01090090052019[↩][↩]
- Treatment of Age-Related Macular Degeneration With Photodynamic Therapy(TAP) Study Group. Photodynamic Therapy of Subfoveal Choroidal Neovascularization in Age-Related Macular Degeneration With Verteporfin: Two-Year Results of 2 Randomized Clinical Trials—TAP Report 2. Arch Ophthalmol. 2001;119(2):198–207. doi:10-1001/pubs.Ophthalmol.-ISSN-0003-9950-119-2-ecs00156[↩][↩]
- Bressler NM, Frost LA, Bressler SB, Murphy RP, Fine SL. Natural course of poorly defined choroidal neovascularization associated with macular degeneration. Arch Ophthalmol. 1988 Nov;106(11):1537-42. doi: 10.1001/archopht.1988.01060140705039[↩][↩]
- Bressler SB, Pieramici DJ, Koester JM, Bressler NM. Natural history of minimally classic subfoveal choroidal neovascular lesions in the treatment of age-related macular degeneration with photodynamic therapy (TAP) investigation: outcomes potentially relevant to management–TAP report No. 6. Arch Ophthalmol. 2004 Mar;122(3):325-9. doi: 10.1001/archopht.122.3.325[↩][↩]
- Hanscom TA, Diddie KR. Early surgical drainage of macular subretinal hemorrhage. Arch Ophthalmol. 1987 Dec;105(12):1722-3. doi: 10.1001/archopht.1987.01060120120037[↩][↩]
- Schoeppner G, Chuang EL, Bird AC. The risk of fellow eye visual loss with unilateral retinal pigment epithelial tears. Am J Ophthalmol. 1989 Dec 15;108(6):683-5. doi: 10.1016/0002-9394(89)90861-1[↩][↩]
- Green WR, Enger C. Age-related macular degeneration histopathologic studies. The 1992 Lorenz E. Zimmerman Lecture. Ophthalmology. 1993 Oct;100(10):1519-35. doi: 10.1016/s0161-6420(93)31466-1[↩]
- Ambati J, Ambati BK, Yoo SH, Ianchulev S, Adamis AP. Age-related macular degeneration: etiology, pathogenesis, and therapeutic strategies. Surv Ophthalmol. 2003 May-Jun;48(3):257-93. doi: 10.1016/s0039-6257(03)00030-4[↩]
- Tomany SC, Wang JJ, Van Leeuwen R, et al. Risk factors for incident age-related macular degeneration: pooled findings from 3 continents. Ophthalmology 2004;111:1280-7.[↩]
- Age-related macular degeneration: diagnosis and management. London: National Institute for Health and Care Excellence (NICE); 2018 Jan. (NICE Guideline, No. 82.) 6, Risk factors. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536467[↩][↩]
- Seddon JM, Reynolds R, Yu Y, Daly MJ, Rosner B. Risk models for progression to advanced age-related macular degeneration using demographic, environmental, genetic, and ocular factors. Ophthalmology. 2011 Nov;118(11):2203-11. doi: 10.1016/j.ophtha.2011.04.029[↩]
- Katsi VK, Marketou ME, Vrachatis DA, Manolis AJ, Nihoyannopoulos P, Tousoulis D, Vardas PE, Kallikazaros I. Essential hypertension in the pathogenesis of age-related macular degeneration: a review of the current evidence. J Hypertens. 2015 Dec;33(12):2382-8. doi: 10.1097/HJH.0000000000000766[↩]
- Friedman DS, Katz J, Bressler NM, Rahmani B, Tielsch JM. Racial differences in the prevalence of age-related macular degeneration: the Baltimore Eye Survey. Ophthalmology. 1999 Jun;106(6):1049-55. doi: 10.1016/S0161-6420(99)90267-1[↩]
- Black JR, Clark SJ. Age-related macular degeneration: genome-wide association studies to translation. Genet Med. 2016 Apr;18(4):283-9. doi: 10.1038/gim.2015.70[↩]
- Klein R, Klein BE, Tomany SC, Moss SE. Ten-year incidence of age-related maculopathy and smoking and drinking: the Beaver Dam Eye Study. Am J Epidemiol. 2002 Oct 1;156(7):589-98. doi: 10.1093/aje/kwf092[↩]
- Delcourt C, Michel F, Colvez A, Lacroux A, Delage M, Vernet MH; POLA Study Group. Associations of cardiovascular disease and its risk factors with age-related macular degeneration: the POLA study. Ophthalmic Epidemiol. 2001 Sep;8(4):237-49. doi: 10.1076/opep.8.4.237.1613[↩]
- Kauppinen A, Paterno JJ, Blasiak J, Salminen A, Kaarniranta K. Inflammation and its role in age-related macular degeneration. Cell Mol Life Sci. 2016 May;73(9):1765-86. doi: 10.1007/s00018-016-2147-8[↩]
- Schultz DW, Klein ML, Humpert AJ, Luzier CW, Persun V, Schain M, Mahan A, Runckel C, Cassera M, Vittal V, Doyle TM, Martin TM, Weleber RG, Francis PJ, Acott TS. Analysis of the ARMD1 locus: evidence that a mutation in HEMICENTIN-1 is associated with age-related macular degeneration in a large family. Hum Mol Genet. 2003 Dec 15;12(24):3315-23. doi: 10.1093/hmg/ddg348[↩]
- Johnson LV, Leitner WP, Staples MK, Anderson DH. Complement activation and inflammatory processes in Drusen formation and age related macular degeneration. Exp Eye Res. 2001 Dec;73(6):887-96. doi: 10.1006/exer.2001.1094[↩]
- Abramov Y, Borik S, Yahalom C, Fatum M, Avgil G, Brzezinski A, Banin E. The effect of hormone therapy on the risk for age-related maculopathy in postmenopausal women. Menopause. 2004 Jan-Feb;11(1):62-8. doi: 10.1097/01.GME.0000074701.19603.11[↩]
- Age-Related Eye Disease Study Research Group; SanGiovanni JP, Chew EY, Clemons TE, Ferris FL 3rd, Gensler G, Lindblad AS, Milton RC, Seddon JM, Sperduto RD. The relationship of dietary carotenoid and vitamin A, E, and C intake with age-related macular degeneration in a case-control study: AREDS Report No. 22. Arch Ophthalmol. 2007 Sep;125(9):1225-32. doi: 10.1001/archopht.125.9.1225[↩][↩]
- Age-Related Eye Disease Study Research Group. The Age-Related Eye Disease Study system for classifying age-related macular degeneration from stereoscopic color fundus photographs: the Age-Related Eye Disease Study Report Number 6. Am J Ophthalmol. 2001 Nov;132(5):668-81. doi: 10.1016/s0002-9394(01)01218-1[↩]
- Eye Disease Case-Control Study Group. Antioxidant status and neovascular age-related macular degeneration. Arch Ophthalmol. 1993 Jan;111(1):104-9. doi: 10.1001/archopht.1993.01090010108035[↩]
- Mares-Perlman JA, Fisher AI, et al. Lutein and zeaxanthin in the diet and serum and their relation to age-related maculopathy in the third national health and nutrition examination survey. Am J Epidemiol. 2001 Mar 1;153(5):424-32. doi: 10.1093/aje/153.5.424[↩]
- Seddon JM, Ajani UA, Sperduto RD, Hiller R, Blair N, Burton TC, Farber MD, Gragoudas ES, Haller J, Miller DT, et al. Dietary carotenoids, vitamins A, C, and E, and advanced age-related macular degeneration. Eye Disease Case-Control Study Group. JAMA. 1994 Nov 9;272(18):1413-20. Erratum in: JAMA 1995 Feb 22;273(8):622[↩]
- Snellen EL, Verbeek AL, et al. Neovascular age-related macular degeneration and its relationship to antioxidant intake. Acta Ophthalmol Scand. 2002 Aug;80(4):368-71. doi: 10.1034/j.1600-0420.2002.800404.x[↩]
- Moeller SM, Parekh N, et al; CAREDS Research Study Group. Associations between intermediate age-related macular degeneration and lutein and zeaxanthin in the Carotenoids in Age-related Eye Disease Study (CAREDS): ancillary study of the Women’s Health Initiative. Arch Ophthalmol. 2006 Aug;124(8):1151-62. doi: 10.1001/archopht.124.8.1151[↩]
- Tan JS, Wang JJ, et al. Dietary antioxidants and the long-term incidence of age-related macular degeneration: the Blue Mountains Eye Study. Ophthalmology. 2008 Feb;115(2):334-41. doi: 10.1016/j.ophtha.2007.03.083[↩]
- Lippman SM, Klein EA, Goodman PJ, et al. Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA. 2009 Jan 7;301(1):39-51. doi: 10.1001/jama.2008.864[↩]
- Gaziano JM, Glynn RJ, et al. Vitamins E and C in the prevention of prostate and total cancer in men: the Physicians’ Health Study II randomized controlled trial. JAMA. 2009 Jan 7;301(1):52-62. doi: 10.1001/jama.2008.862[↩]
- The ATBC Cancer Prevention Study Group. The alpha-tocopherol, beta-carotene lung cancer prevention study: design, methods, participant characteristics, and compliance. Ann Epidemiol. 1994 Jan;4(1):1-10. doi: 10.1016/1047-2797(94)90036-1[↩]