Contents
- Anal cancer
- Types of anal cancer
- Anal cancer causes
- Anal cancer prevention
- Anal cancer signs and symptoms
- Anal cancer complications
- Anal cancer diagnosis
- Anal Cancer Stages
- Anal cancer treatment
- Living with anal cancer
- Anal Cancer Survival Rates
- Anal cancer prognosis
Anal cancer
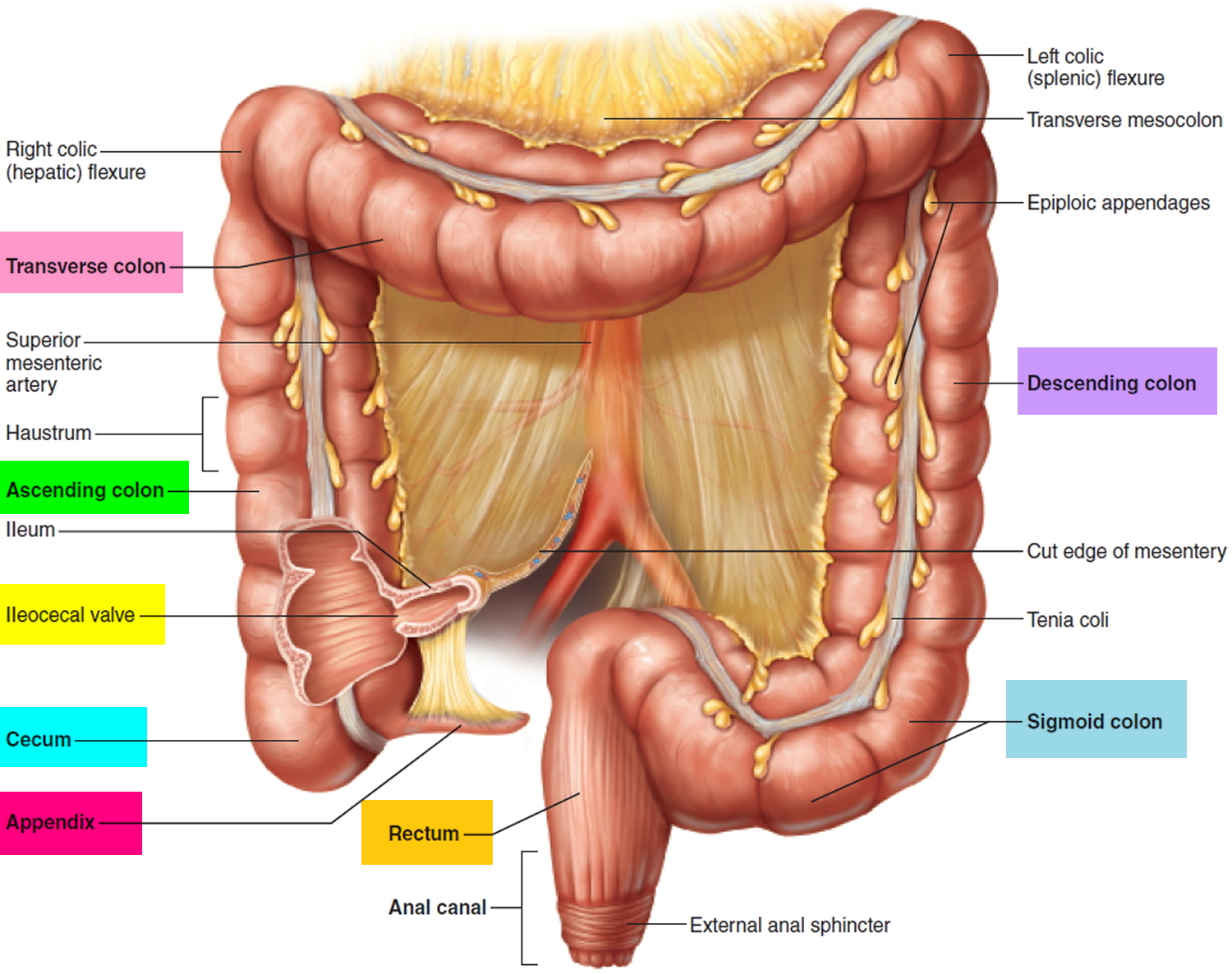
Anal cancer is a rare cancer that forms in tissues of the anus – the very end of the large bowel (large intestine or the colon) (see Figures 1 and 2 below). The anus is the part of the large bowel (large intestine) that opens to the outside of the body. It’s where the end of the intestines connect to the outside of the body. The anus is the tube that your poop (feces) passes through when you go to the toilet to empty your bowel. The anus makes up part of your digestive system. It is about 3 cm long, and is at the end of your back passage (rectum). The anal canal connects the rectum to the anus.
Anal cancers are often divided into 2 groups, which are sometimes treated differently (see Figure 2 below):
- Cancers of the anal canal (above the anal verge)
- Cancers of the anal margin (below the anal verge)
Sometimes anal cancers extend from one area into the other, so it’s hard to know exactly where they started.
The anal canal is surrounded by a sphincter (the anal sphincters), which are circular muscles (internal and external anal sphincter) that keeps stool from coming out until it relaxes during a bowel movement.
Anal cancer is rare – much less common than cancer of the colon or rectum. Anal cancer is more common in smokers and people over 50. You are also at higher risk if you have human papilloma virus (HPV), have anal sex, or have many sexual partners.
The American Cancer Society estimates for anal cancer in the United States for 2023 are 1, 2:
- About 9,760 new cases (3,180 in men and 6,580 in women)
- About 1,870 deaths (860 in women and 1,010 in men)
- 5-Year Relative Survival: 70.4%. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
- Anal cancer deaths as a percentage of All Cancer Deaths: 0.3%.
- Rate of New Cases and Deaths per 100,000: The rate of new cases of anal cancer was 1.9 per 100,000 men and women per year. The death rate was 0.3 per 100,000 men and women per year. These rates are age-adjusted and based on 2016–2020 cases and deaths.
- Lifetime Risk of Developing cervical cancer: Approximately 0.2 percent of men and women will be diagnosed with anal cancer at some point during their lifetime, based on 2017–2019 data.
- In 2020, there were an estimated 79,091 people living with anal cancer in the United States.
The number of new anal cancer cases has been rising for many years. There is a larger increase of anal cancer cases for women than men. Anal cancer is also more common in white women and black men 1. Anal cancer is rare in people younger than 35 and is found mainly in older adults, with an average age being in the early 60s.
The risk of being diagnosed with anal cancer during one’s lifetime is about 1 in 500 1. The risk is slightly higher in women than in men. The risk is also higher in people with certain risk factors for anal cancer.
Symptoms of anal cancer include rectal bleeding, anal pain or lumps in the anal area. Anal itching and discharge can also be signs of anal cancer.
Doctors use tests that examine the anus to diagnose anal cancer. They include a physical exam, endoscopy, ultrasound, and biopsy.
Anal cancer treatments include radiation therapy, chemotherapy, and surgery.
Most people with anal cancer are treated with a combination of chemotherapy and radiation (chemoradiation). Though combining anal cancer treatments increases the chance of a cure, the combined treatments also increase the risk of side effects.
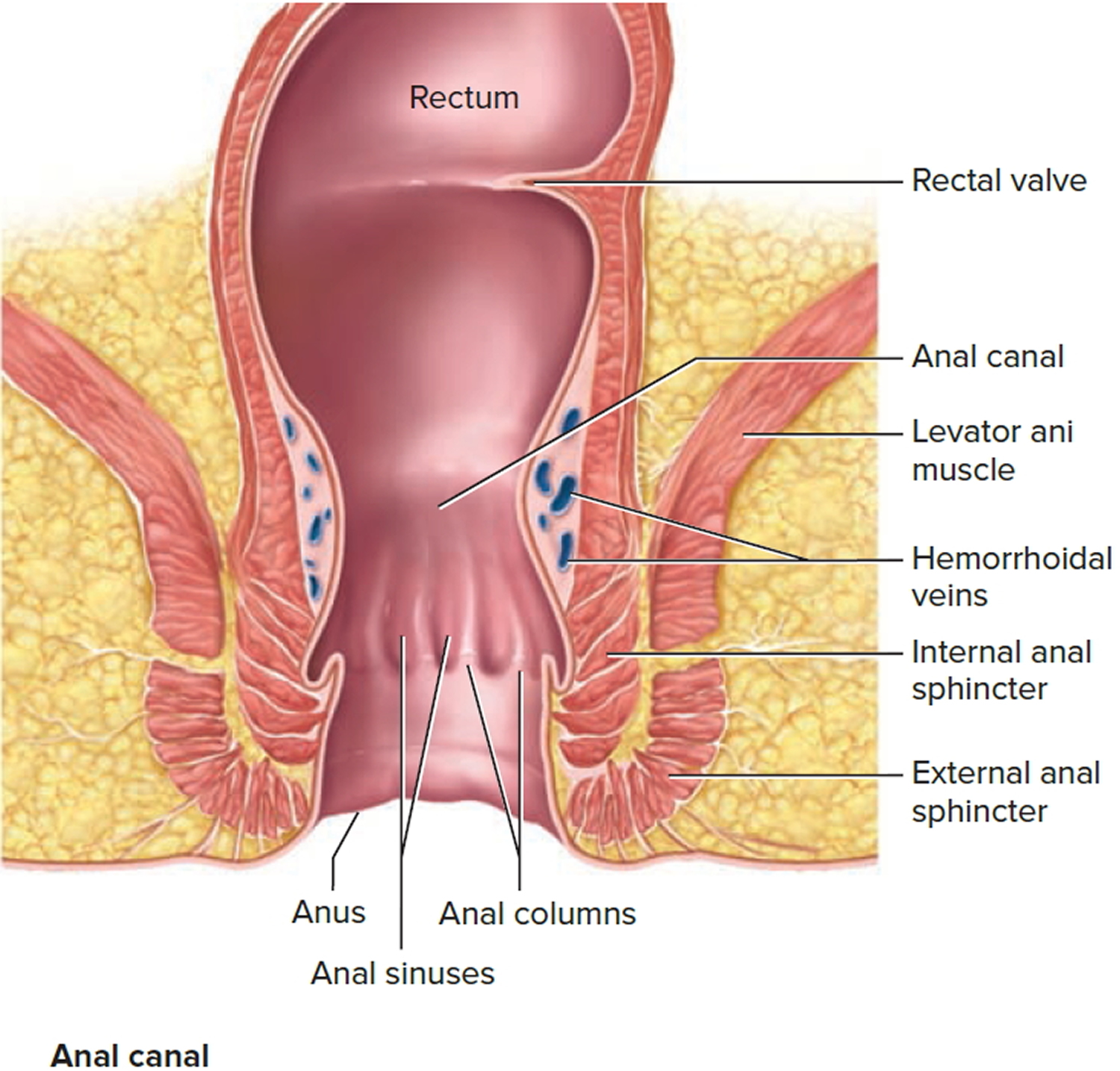
The anus
The anus is connected to the rectum by the anal canal. The anus is the continuation of the large intestine (the colon or large bowel) inferior to the rectum. It’s where the end of the intestines connect to the outside of the body.
The anal canal is about 1-1/2 inches (about 3 to 5 cm) long, it begins where the rectum passes through the levator ani (the muscle that forms the pelvic floor) and goes to the anal verge. The anal verge is where the anal canal connects to the outside skin at the anus. This skin around the anal verge is called the perianal skin (previously called the anal margin). The anal canal has two ring-shaped muscles (called sphincter muscles – an internal and external anal sphincter) that keep the anus closed and prevent stool from leaking out.
As food is digested, it passes from the stomach to the small intestine. It then moves from the small intestine into the main part of the large intestine (called the colon). The colon absorbs water and salt from the digested food. The waste matter that’s left after going through the colon is known as feces or stool. Stool is stored in the last part of the large intestine, called the rectum. From there, stool is passed out of the body through the anus as a bowel movement.
The inner lining of the anal canal is the mucosa. Most anal cancers start from cells in the mucosa. Glands and ducts (tubes leading from the glands) are found under the mucosa. The glands make mucus, which acts as a lubricating fluid. Anal cancers that start from cells in the glands are called adenocarcinomas.
The anal canal changes as it goes from the rectum to the anal verge. The parts of the anus include the:
- Cells above the anal canal (in the rectum) and in the part of the anal canal close to the rectum are shaped like tiny columns.
- Most cells near the middle of the anal canal are shaped like cubes and are called transitional cells. This area is called the transitional zone – this is where the rectum meets the anal canal.
- About midway down the anal canal is the dentate line, which is where most of the anal glands empty into the anus.
- Below the dentate line are flat (squamous) cells.
- At the anal verge, the squamous cells of the lower anal canal merge with the skin just outside the anus. This skin around the anal verge called the perianal skin or the anal margin, is also made up of squamous cells, but it also contains sweat glands and hair follicles, which are not found in the lining of the lower anal canal. The anal margin is the lower part of the anal canal and it contains muscles called the anal sphincters. You have an internal and external anal sphincter. They are the muscles that control your bowel movements.
Figure 1. Rectum
Figure 2. Rectum anatomy and Anus (anal canal)
Where does anal cancer start?
Anal cancer can start in any part of your anus. And it can start in different types of cell. There are different types of anal cancer depending on which type of cell the cancer starts in. The cell type and position of your cancer can affect what treatment you have.
- Anal cancer can start in the anal margin, the anal canal or the transitional zone.
- Anal margin cancers are more common in men than women. Cancers of the anal margin usually look more like normal cells. Doctors call these well differentiated tumors.
- Cancers that start higher up in the anal canal are more common in women.
Sometimes, treatment may be different, depending on where the cancer is located. But anal cancers can sometimes extend from one area into the other, so it’s hard to know exactly where they started.
Cell type
Cancer can start in the following cell types:
- Squamous cell cancers start in squamous cells that make up the lining of the anal canal – most anal cancers are squamous cell cancers
- Adenocarcinoma of the anus starts in glandular cells that make the mucus that helps stools (feces) pass through the anus smoothly – adenocarcinoma of the anus is less common
- Melanoma starts in cells in the skin called melanocytes – this is another rare type of anal cancer
Types of anal cancer
The type of anal cancer you have depends on the type of cell the cancer started in. Most anal cancers start in a type of cell called squamous cells. Other rare types include adenocarcinoma and melanoma.
Carcinoma in situ
Sometimes abnormal cells on the inner surface layer of the anus look like cancer cells but have not grown into any of the deeper layers. This is known as carcinoma in situ or CIS. Another name for this is Bowen disease.
Some doctors see this as the earliest form of anal cancer. Others consider it the most advanced type of anal intraepithelial neoplasia (AIN), which is a pre-cancer that might develop into cancer in the future, but not a true cancer.
Anal intraepithelial neoplasia (AIN) is also called anal squamous intraepithelial lesions (SILs) means there are abnormal cells in the lining of your anus. This is because most of the abnormal cells are a type of cell called squamous cells.
The cells might be inside your anal canal or in the skin around the back passage (perianal skin).
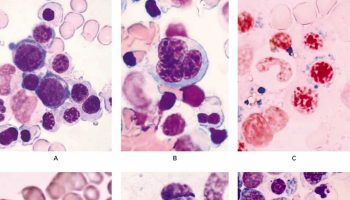
A pathologist looks at your cells under a microscope to check whether your anal cells look different to normal anal cells.
Invasive anal cancers
These are the different types of cancer that can start in the anal region:
Squamous cell carcinomas
Most anal cancers (nearly 9 out of 10 cases) in the United States are squamous cell carcinomas. These tumors start in the squamous cells that line most of the anal canal and the anal margin. Squamous cell carcinomas are also called epidermoid cancers.
Squamous cell carcinomas in the anal canal have grown beyond the surface and into the deeper layers of the lining (as opposed to carcinoma in situ which is only in the surface cells).
There are 3 types of squamous cell cancer. Many anal cancers have a mix of all 3 cell types. Your treatment depends on the position of the cancer in your anus. Cancers that start in the anal canal might have different treatment to cancers that start in the anal margin.
Cloacogenic carcinomas (also called basaloid or transitional cell carcinomas) are a type of squamous cell cancer. They develop in the transitional zone, also called the cloaca. These cancers look slightly different under a microscope, but they behave and are treated like other squamous cell carcinomas of the anal canal.
Squamous cell cancers of the anal margin (perianal skin) can be treated as an anal cancer or like squamous cell cancer of the skin. It is important to see an expert if you are diagnosed with perianal cancer to determine the best course of treatment.
Adenocarcinomas
A small number of anal cancers are known as adenocarcinomas. These start in cells that line the upper part of the anus near the rectum. They can also start in the glands under the anal mucosa that produce mucus into the anal canal. Most anal adenocarcinomas are treated the same as rectal cancer (rectal carcinomas).
Adenocarcinomas can also start in apocrine glands (a type of sweat gland of the perianal skin). Paget’s disease is a type of apocrine gland carcinoma that spreads through the surface layer of the skin. Paget’s disease can affect skin anywhere in the body but most often affects skin of the perianal area, vulva, or breast. This should not be confused with Paget’s disease of the bone , which is not cancer and a different disease.
Basal cell carcinomas
Basal cell carcinomas are a type of skin cancer that can develop in the perianal skin. These tumors are much more common in areas of skin exposed to the sun, such as the face and hands, and account for very few anal cancers. They are often treated with surgery to remove the cancer.
Melanomas
Melanoma is another type of skin cancer, it is very rare. These cancers start in cells in the skin or anal lining that make the brown pigment called melanin. Only a very small portion of anal cancers are melanomas. Melanomas are far more common on the skin in other parts of the body. If melanomas are found at an early stage (before they have grown deeply into the skin or spread to lymph nodes) they can be removed with surgery, and the outlook for long-term survival is very good. Early stage anal melanomas are treated with surgery to remove the tumor and a rim of surrounding normal tissue (local excision). If the tumor is large or has grown into deeper tissues (such as the sphincter muscle) a bigger operation, such as an abdominoperineal resection (APR) might be needed. But because anal melanomas are hard to see, most are found at a later stage. If possible, the entire tumor is removed with surgery. If all of the tumor can be removed, a cure is possible. If the melanoma has spread too far to be removed completely, other treatments may be given. If the melanoma has spread to other organs, it’s treated like skin melanoma that has spread, often with immunotherapy or targeted therapy drugs.
Gastrointestinal stromal tumors (GISTs)
These cancers are much more common in the stomach or small intestine, but rarely they can start in the anal region. When these tumors are found at an early stage, they are removed with surgery. If they have spread beyond the anus, they can be treated with drug therapy.
Potentially pre-cancerous anal conditions
Some changes in the anal mucosa are harmless at first, but might later develop into a cancer. These are called pre-cancerous conditions. A common term for these potentially pre-cancerous conditions is dysplasia. Some warts, for example, contain areas of dysplasia that can develop into cancer.
Dysplasia in cells of the anus is also called anal intraepithelial neoplasia (AIN) or anal squamous intraepithelial lesions (SILs). Depending on how the cells look, AIN or anal SIL can be divided into 2 groups:
Low-grade AIN (sometimes called AIN1 or low-grade anal SIL)
- The cells in low-grade AIN look like normal cells in many ways.
- Low-grade AIN often goes away without treatment. It has a low chance of turning into cancer.
High-grade AIN (sometimes called AIN2 or AIN3, or high-grade anal SIL)
- The cells in high-grade AIN look much more abnormal.
- High-grade AIN is less likely to go away without treatment and, with time, could become cancer. It needs to be watched closely. Some cases of high-grade AIN need to be treated.
Anal cancer causes
The exact cause of anal cancer is unknown, although a number of factors can increase your risk of developing anal cancer. These include:
- Infection with human papilloma virus (HPV) – a common and usually harmless group of viruses spread through sexual contact, which can affect the moist membranes lining your body
- Having anal sex or lots of sexual partners – possibly because this increases your risk of developing HPV
- Having a history of cervical, vaginal or vulval cancer
- Smoking
- Having a weakened immune system – for example, if you have HIV. HIV — the virus that causes AIDS — suppresses the immune system and increases the risk of anal cancer.
- Drugs or conditions that suppress your immune system. People who take drugs to suppress their immune systems (immunosuppressive drugs), including people who have received organ transplants, may have an increased risk of anal cancer.
It’s important to remember that some people with anal cancers do not have any known risk factors and the causes of their cancers are not known.
Your risk of developing anal cancer increases as you get older, with half of all cases diagnosed in people aged 65 or over. Anal cancer is also slightly more common in women than men.
HPV infection
Most anal cancers seem to be linked to a sexually transmitted infection called human papillomavirus (HPV) mainly HPV serotypes 16 and 18 3. In a Scandinavian study, HPV serotype 16 was detected in 73% of anal cancer specimens and HPV serotypes 16, 18, or both were present in 84% of the specimens 3. While HPV (human papillomavirus) infection seems to be important in the development of anal cancer, the vast majority of people with HPV infections do not get anal cancer 4.
Most squamous cell anal cancers are linked to infection with the human papillomavirus (HPV), the same virus that causes cervical cancer, as well as many other kinds of cancer. In fact, women with a history of cervical cancer (or pre-cancer) have an increased risk of anal cancer. They are called papillomaviruses because some of them cause papillomas, which are more commonly known as warts. The 2 types of HPV that cause most cases of anal and genital warts are HPV-6 and HPV-11.
HPV is a group of more than 150 related viruses. The subtype known as HPV-16 is often found in squamous cell carcinoma and is also found in some anal warts. Another subtype, HPV-18, is found less often. Most anal warts are caused by HPV-6 and HPV-11. Warts containing HPV-6 or HPV-11 are much less likely to become cancerous than those containing HPV-16. While anal warts themselves are unlikely to develop into anal cancer, people who have had anal warts are more likely to get anal cancer. This is because people who are infected with HPV subtypes that cause anal and genital warts are also more likely to be infected HPV subtypes that cause anal cancer.
HPV makes proteins (E6 and E7) that can shut down 2 important tumor suppressor proteins in normal cells. These proteins – p53 and Rb – normally work to keep cells from growing out of control. When these proteins are not active, cells are more likely to become cancerous.
HPV is passed from one person to another during skin-to-skin contact with an infected area of the body. HPV can be spread during sexual activity – including vaginal, anal, and oral sex – but sex doesn’t have to occur for the infection to spread. All that’s needed is for there to be skin-to-skin contact with an area of the body infected with HPV. The virus can be spread through genital-to-genital contact, or even hand-to-genital contact. An HPV infection can also spread from one part of the body to another. For example, an HPV infection might start in the genitals and then spread to the anus.
It can be very hard to avoid being exposed to HPV. It might be possible to prevent genital HPV infection by not allowing others to have contact with your anal or genital area, but even then there could be other ways to become infected that aren’t yet clear.
Infection with HPV is common, and in most cases the body can clear the infection on its own. But in some people the infection doesn’t go away and becomes chronic. Chronic infection, especially with high-risk HPV types, can cause certain cancers over time, including anal cancer.
A great deal of research is now being done to learn how HPV might cause anal cancer. There is good evidence that HPV causes many anal squamous cell carcinomas. But the role of this virus in causing anal adenocarcinomas is less certain.
Lowered immunity
When the body is less able to fight off infections, viruses like HPV can become more active, which might trigger the development of anal cancer. HIV, the virus that causes AIDS, weakens the body’s immune system, as can medicines used to prevent rejection in patients with organ transplants.
Smoking
Most people know that smoking is the main cause of lung cancer. But few realize that the cancer-causing chemicals in tobacco smoke can travel from the lungs to the rest of the body, causing other types of cancer. Smoking also seems to make the immune system less effective in fighting HPV infections. Many studies have noted an increased rate of anal cancer in smokers, and the effect of smoking is especially important in people with other risk factors for anal cancer.
Risk Factors for Anal Cancer
Several factors can affect your risk of anal cancer. But having a risk factor, or even several risk factors, does not mean that you will get cancer. Many people with risk factors never develop anal cancer, while others with this disease may have few or no known risk factors.
- Human papillomavirus (HPV) infection
- Infection with HPV is common, and in most cases, the body can clear the infection by itself. Sometimes, however, the infection does not go away and becomes chronic. Chronic infection, especially when it is caused by certain high-risk HPV types, can eventually cause certain cancers, such as anal cancer.
- Anal warts
- People who have had anal warts are more likely to get anal cancer. This is because people who are infected with HPV subtypes that cause anal and genital warts are also more likely to be infected with HPV subtypes that cause anal cancer.
- Having certain other cancers
- Women who have had cancer of the cervix, vagina, or vulva are at increased risk of anal cancer. This is probably because these cancers are also caused by infection with HPV.
- In men, it would seem likely that having had penile cancer, which is also linked to HPV infection, would increase the risk of anal cancer, but this link has not been shown in studies.
- HIV infection
- People infected with the human immunodeficiency virus (HIV), the virus that causes AIDS, are much more likely to get anal cancer than those not infected with this virus.
- Sexual activity
- Having multiple sex partners increases the risk of infection with HIV and HPV. It also increases the risk of anal cancer.
- Receptive anal sex also increases the risk of anal cancer in both men and women. Because of this, men who have sex with men have a high risk of this cancer.
- Smoking
- Smoking increases the risk of anal cancer. Current smokers are several times more likely to have cancer of the anus compared with people who do not smoke. Quitting smoking seems to reduce the risk. People who used to smoke but have quit are only slightly more likely to develop this cancer compared with people who never smoked.
- Lowered immunity
- Higher rates of anal cancer occur among people with reduced immunity, such as people with AIDS or people who have had an organ transplant and must take medicines that suppress their immune system.
- Drugs or conditions that suppress your immune system
- People who take drugs to suppress their immune systems (immunosuppressive drugs), including people who have received organ transplants, may have an increased risk of anal cancer. HIV — the virus that causes AIDS — suppresses the immune system and increases the risk of anal cancer.
- Older age
- Most cases of anal cancer occur in people age 50 and older. Around 25 out of 100 people (around 25%) diagnosed with anal cancer each year are aged 75 and over. But as anal cancer is a rare cancer the risk is still small.
- Gender and race/ethnicity
- Anal cancer is more common in women than men overall, but this varies in racial/ethnic groups and can vary with age. For instance, in African Americans younger than age 60, it’s more common in men than in women, but after age 60 it’s more common in women.
Anal cancer prevention
Since the cause of many cases of anal cancer is unknown, it’s not possible to prevent this disease completely. But there are things you can do that might lower your risk of anal cancer.
Infection with HPV increases the risk of anal cancer. HPV infection can be present for years without causing any symptoms, so the absence of visible warts can’t be used to tell if someone has HPV. Even when someone doesn’t have warts (or any other symptom), he (or she) can still be infected with HPV and pass it on to somebody else.
In order to reduce your risk of anal cancer:
- Practice safer sex. Abstaining from sex or practicing safe sex may help prevent HPV and HIV, two sexually transmitted viruses that may increase your risk of anal cancer. If you choose to have anal sex, use condoms.
- Get vaccinated against HPV. Two HPV vaccines — 9-valent HPV vaccine (Gardasil 9), quadrivalent HPV vaccine (Gardasil), and bivalent HPV vaccine (Cervarix) — are given to protect against HPV infection. Both boys and girls can be vaccinated against HPV.
- Stop smoking. Smoking increases your risk of anal cancer. Don’t start smoking. Stop if you currently smoke.
HPV vaccines
Vaccines are available that protect against certain HPV infections. HPV vaccines protect against infection with HPV subtypes 16 and 18. Some can also protect against infections with other HPV subtypes, including some types that cause anal and genital warts.
HPV vaccines can only be used to help prevent HPV infection – they do not help treat an existing infection. To work best, HPV vaccine should be given before a person becomes sexually active.
HPV vaccine is recommended for adolescents, including both boys and girls, but may be given to adults, too 5:
- Children ages 11–12 years should get two doses of HPV vaccine, given 6 to 12 months apart. HPV vaccines can be given starting at age 9.
- Children who start the HPV vaccine series on or after their 15th birthday need three doses, given over 6 months.
- Everyone through age 26 years should get HPV vaccine if they were not fully vaccinated already.
HPV vaccination is NOT recommended for everyone older than age 26 years 5.
- Some adults ages 27 through 45 years who were not already vaccinated might choose to get HPV vaccine after speaking with their doctor about their risk for new HPV infections and possible benefits of vaccination for them.
- HPV vaccination of adults provides less benefit, because more people in this age range have been exposed to HPV already.
Condom use
Condoms may provide some protection against HPV (and HIV), but they don’t prevent infection completely. Given this, it is unclear if condom use can reduce the risk of anal cancer.
One study found that when condoms are used correctly they can lower the genital HPV infection rate in women – but they must be used every time sex occurs. This study did not look at the effect of condom use on anal HPV infection.
Condoms can’t protect completely because they don’t cover every possible HPV-infected area of the body, such as skin of the genital or anal area. HPV can still be passed from one person to another by skin to skin contact with an HPV-infected area of the body that is not covered by a condom. Still, condoms may provide some protection against HPV. Male condom use also seems to help genital HPV infections clear (go away) faster in both women and men.
Condom use is also important because it can help protect against AIDS and other sexually transmitted illnesses that can be passed on through some body fluids.
Treating HIV
For people infected with HIV, it’s very important to take medicines (known as highly active antiretroviral therapy, or HAART) to help keep the infection under control and prevent it from progressing to AIDS. This also lowers the risk of long-term HPV infection and anal intraepithelial neoplasia (a kind of anal pre-cancer), which might help lower the risk of anal cancer.
Not smoking
Smoking is a known risk factor for anal cancer. Stopping smoking greatly reduces the risk of developing anal cancer and many other cancers.
Screening in people at high risk
Looking for a disease like cancer in someone with no symptoms is called screening. The goal of screening is to find cancer at an early stage, when treatment is likely to be most helpful. Anal cancer is not common in the United States, so screening the general public for anal cancer is not widely recommended at this time.
Still, some people at increased risk for anal intraepithelial neoplasia (AIN, a potentially pre-cancerous condition) and anal cancer might benefit from screening. This includes men who have sex with men (regardless of HIV status), women who have had cervical cancer or vulvar cancer, anyone who is HIV-positive, and anyone who has received an organ transplant. Some experts also recommend screening for anyone with a history of anal warts.
For these people, some experts recommend screening with regular digital rectal examinations and anal cytology testing (also known as an anal Pap test or anal Pap smear because it is much like a Pap test for cervical cancer). For an anal Pap test, the anal lining is swabbed, and cells that come off on the swab are looked at under the microscope.
The anal Pap test has not been studied enough to know how often it should be done, or if it actually reduces the risk of anal cancer by catching intraepithelial neoplasia (AIN) early. Some experts recommend that the test be done every year in men who have sex with men who are HIV-positive, and every 2 to 3 years if the men are HIV-negative. But there is no widespread agreement on the best screening schedule, or even exactly which groups of people can benefit from screening.
Patients with positive results on an anal Pap test should be referred for a biopsy. If AIN is found on the biopsy, it might need to be treated (especially if it is high-grade).
Anal cancer signs and symptoms
The symptoms of anal cancer are often similar to more common and less serious conditions affecting the anus, such as piles (hemorrhoids) and anal fissures (small tears or sores).
Sometimes anal cancer causes no symptoms at all. But bleeding is often the first sign of anal cancer. The bleeding is usually minor. At first, most people assume the bleeding is caused by hemorrhoids (painful, swollen veins in the anus and rectum that may bleed). They are a benign and fairly common cause of rectal bleeding.
Symptoms of anal cancer can include:
- bleeding from the bottom (rectal bleeding)
- itching and pain around the anus
- small lumps around the anus
- a discharge of mucus from the anus
- loss of bowel control (bowel incontinence)
- swollen lymph nodes in the anal or groin areas
However, some people with anal cancer don’t have any symptoms. About 20 out of 100 people (20%) diagnosed with anal cancer don’t have any symptoms.
See your doctor if you develop any of the above symptoms. While they’re unlikely to be caused by anal cancer, it’s best to get them checked out.
Anal cancer complications
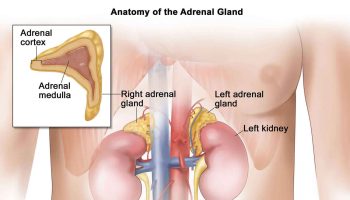
Anal cancer rarely spreads (metastasizes) to distant parts of the body. Only a small percentage of tumors are found to have spread, but those that do are especially difficult to treat. Anal cancer that metastasizes most commonly spreads to the liver and the lungs.
Anal cancer complications are chiefly related to treatment and include the following 3:
- Side effects of radiation
- Adverse effects of chemotherapy
- Decreased libido
- Bowel dysfunction
- Proctitis
- Rectal bleeding
- Surgery-associated strictures, fistulas, and wound infections
Anal cancer diagnosis
Tests and procedures used to diagnose anal cancer include:
- Digital rectal examination (DRE). Examining your anal canal and rectum for abnormalities. During a digital rectal exam, your doctor inserts a gloved, lubricated finger into your rectum. He or she feels for anything unusual, such as growths.
- Visually inspecting your anal canal and rectum. Your doctor may use a short, lighted tube (anoscope) to inspect your anal canal and rectum for anything unusual.
- Taking sound wave pictures (ultrasound) of your anal canal. To create a picture of your anal canal, your doctor inserts a probe, similar to a thick thermometer, into your anal canal and rectum. The probe emits high-energy sound waves, called ultrasound waves, which bounce off tissues and organs in your body to create a picture. Your doctor evaluates the picture to look for anything abnormal.
- Removing a sample of tissue for laboratory testing. If your doctor discovers any unusual areas, he or she may take small samples of affected tissue (biopsy) and send the samples to a laboratory for analysis. By looking at the cells under a microscope, doctors can determine whether the cells are cancerous.
- Blood tests. If you have risk factors for HIV, your doctor might order a HIV blood test to check for it. This information is important because HIV positive patients might need to start treatment for HIV so that their immune system is as normal as possible, before starting cancer treatment.
Endoscopy
Endoscopy uses a thin tube with a lens or tiny video camera on the end to look inside part of the body. Many types of endoscopy can be used to look for the cause of anal symptoms. They can also be used to get tissue samples from inside the anal canal (described below under Biopsy). Drugs may be used to make you sleepy during these tests.
Anoscopy
For anoscopy the doctor uses a short, hollow tube called an anoscope. It’s 3 to 4 inches long and about 1 inch in diameter and may have a light on the end of it. The doctor coats the anoscope with a lubricant and then gently pushes it into the anus and rectum. By shining a light into this tube, the doctor has a clear view of the lining of the lower rectum and anus. This exam usually doesn’t hurt.
Rigid proctosigmoidoscopy
The rigid proctosigmoidoscope is a lot like an anoscope, except that it’s longer (about 10 inches long). It lets the doctor see the rectum and the lower part of the sigmoid colon. You might need to take laxatives or have an enema before this test to make sure your bowels are empty.
Ultrasound
Ultrasound uses sound waves to make pictures of internal organs or masses. This test can be used to see how deep the cancer has grown into the tissues near the anus.
For most ultrasound exams a wand-like transducer is moved around on the skin. But for anal cancer, the transducer is put right into the rectum. This is called a transrectal or endorectal ultrasound. The test can be uncomfortable, but it usually doesn’t hurt.
Biopsy
If a change or growth is seen during an endoscopic exam, your doctor will need to take out a piece of it to see if it’s cancer. This is called a biopsy. If the growth is in the anal canal, this can often be done through the scope itself. Drugs may be used to numb the area before the biopsy is taken. Then, a small piece of the tissue is cut out and sent to a lab. If the tumor is very small, your doctor might try to remove the entire tumor during the biopsy.
A doctor called a pathologist will look at the tissue sample under a microscope. If cancer is present, the pathologist will send back a report describing the cell type and extent of the cancer.
Anal cancer sometimes spreads to nearby lymph nodes (bean-sized collections of immune system cells). Swollen lymph nodes in the groin can be a sign that cancer has spread. Lymph nodes may also become swollen from an infection. Biopsies may be needed to check for cancer spread to nearby lymph nodes.
There are many different ways to do a biopsy. A type called fine-needle aspiration (FNA) is often used to check lymph nodes that might have cancer in them. To do this, a small sample of fluid and tissue is taken out of the lymph node using a thin, hollow needle. A pathologist checks this fluid for cancer cells. If cancer is found in a lymph node, surgery may be done to remove the lymph nodes in that area.
Determining the extent of the cancer
Once it’s confirmed that you have anal cancer, your doctor may recommend additional tests to determine whether your cancer has spread to your lymph nodes or to other areas of your body.
Tests may include:
- Computerized tomography (CT)
- Magnetic resonance imaging (MRI)
- Positron emission tomography (PET)
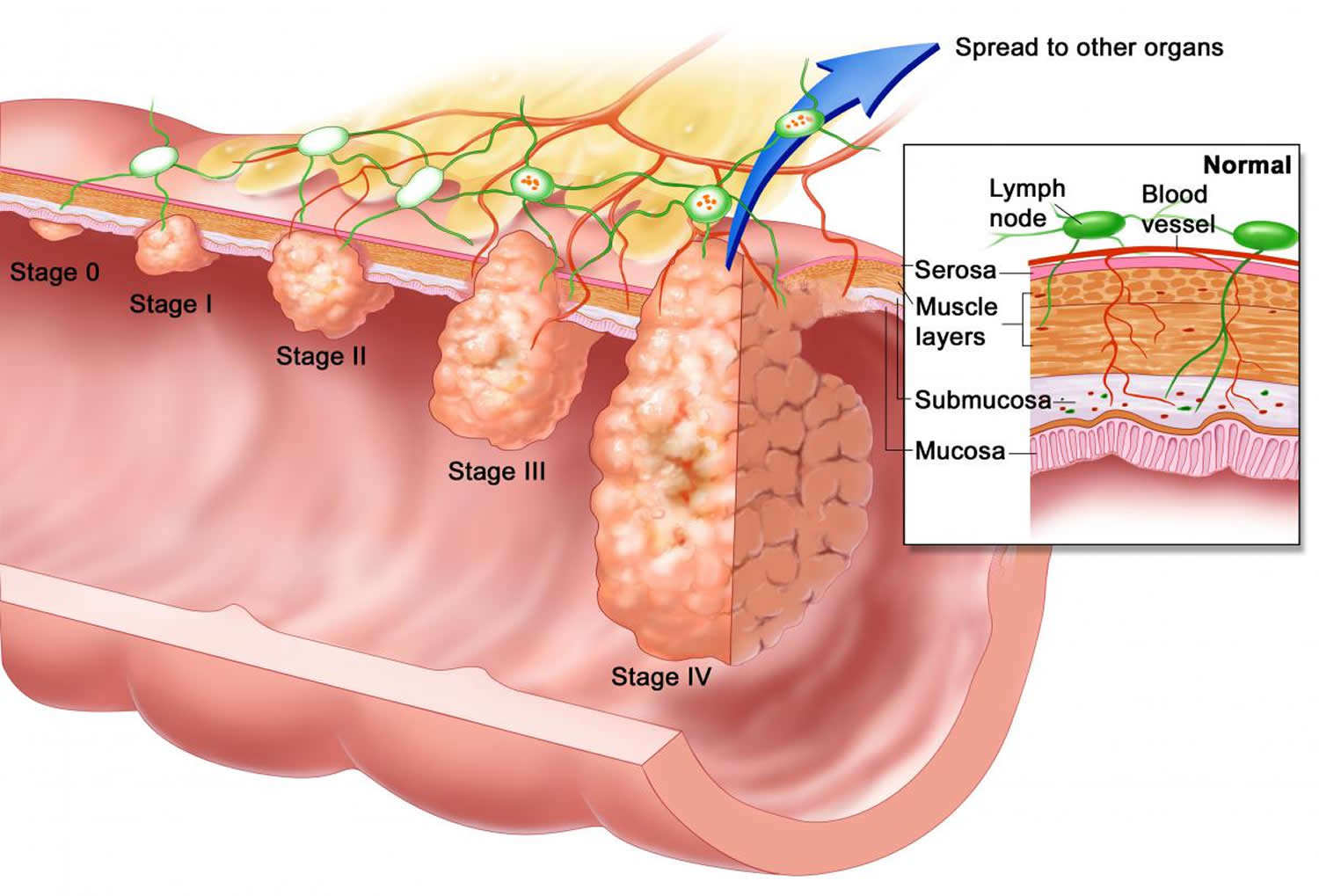
Your doctor uses the information from the procedures to assign your cancer a stage. The stages of anal cancer are indicated using Roman numerals ranging from 0 to IV, with the lowest stages indicating that the cancer is small and confined to the anus (see Table 1 below). By stage IV, the cancer has spread to distant areas of the body.
The cancer staging system continues to evolve and is becoming more complex as doctors improve cancer diagnosis and treatment. Your doctor uses your cancer stage to select the treatments that are right for you.
Computed tomography (CT) scan
CT scans use x-rays to make detailed cross-sectional images of your body. This is a common test for people with anal cancer. It can be used to help tell if the cancer has spread into the lymph nodes or to other parts of the body, such as the liver, lungs, or other organs.
Instead of taking one picture, like a standard x-ray, a CT scanner takes many pictures as it rotates around you. A computer then combines these into an image of a slice of your body.
CT-guided needle biopsy: CT scans can also be used to guide a biopsy needle right into a change that could be cancer. To do this, you stay on the CT scanning table while the doctor moves a biopsy needle through your skin and toward the tumor. CT scans are repeated until the needle is in the tumor. A biopsy sample is then taken out and sent to a lab to be looked at under a microscope.
Magnetic resonance imaging (MRI)
MRI scans use radio waves and strong magnets instead of x-rays. The energy from the radio waves is absorbed by the body and then released in a specific pattern formed by the type of tissue and by certain diseases. A computer translates the pattern into detailed images of parts of the body.
This test is sometimes used to see if nearby lymph nodes are enlarged, which might be a sign the cancer has spread there.
Chest x-ray
A regular x-ray might be done to find out if the cancer has spread to the lungs. It isn’t needed if a CT scan of the chest is done.
Positron emission tomography (PET) scan
For a PET scan, a form of radioactive sugar (known as fluorodeoxyglucose or FDG) is injected into your blood. Cancer cells are very active, so they absorb large amounts of the radioactive sugar. After about an hour, you’ll be moved onto a table in the PET scanner. A special camera creates pictures of areas where the radioactivity has collected. The picture is not finely detailed like a CT or MRI scan, but it provides helpful information about your whole body.
Often a PET scan is done in a machine that can do a CT scan at the same time (a PET/CT scan). It lets the doctor compare areas of higher radioactivity on the PET scan with the more detailed image of that area on the CT scan.
PET/CT scans can be useful:
- If your doctor thinks the cancer might have spread but doesn’t know where. They can show spread of cancer to the liver, bones, lymph nodes in the pelvis, or other organs. They are not as useful for looking at the brain or spinal cord.
- In staging anal cancer when you are first diagnosed. But their role in checking whether treatment is working or after completion of treatment is unproven. Most doctors do not recommend PET/CT scans for routine follow up after anal cancer treatment, and most often will order CT or MRI scans to watch for cancer recurrence.
Anal Cancer Stages
The staging system most often used for anal cancer is the American Joint Committee on Cancer (AJCC) TNM system, which is based on 3 key pieces of information:
- The extent (size) of the tumor (T): What is the size of the cancer? Has the cancer reached nearby structures or organs?
- The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes?
- The spread (metastasis) to distant sites (M): Has the cancer spread to distant lymph nodes or distant organs such as the liver or lungs?
Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced. Once a person’s T, N, and M categories have been determined, this information is combined in a process called stage grouping to assign an overall stage.
Anal cancer is usually staged based on the results of a physical exam, biopsy, and imaging tests. This is called a clinical stage. If surgery is done, the pathologic stage (also called the surgical stage) is determined by examining tissue removed during an operation. This is also known as surgical staging.
The system described below is the most recent AJCC system effective January 2023. It is used for tumors in the anal canal and perianal (formally anal margin) area.
Cancer staging can be complex, so ask your doctor to explain it to you in a way you understand.
Table 1. Anal cancer stages
| AJCC Stage | Stage grouping | Stage description* |
|---|---|---|
| 1 | T1 N0 M0 | The cancer is no more than 2 cm (about 4/5 inch) across (T1). It has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| 2A | T2 N0 M0 | The cancer is more than 2 cm (about 4/5 inch) but not more than 5 cm (about 2 inches) across (T2). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| 2B | T1-T2 N1 M0 | The cancer is no more than 5 cm (about 2 inches) across (T1 or T2) AND it has spread to lymph nodes near the rectum (N1) but not to distant parts of the body (M0). |
| 3A | T3 N0 M0 | The cancer is larger than 5 cm (about 2 inches) across (T3). It has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| OR | ||
| T3 N1 M0 | The cancer is larger than 5 cm (about 2 inches) across (T3) AND it has spread to lymph nodes near the rectum (N1) but not to distant parts of the body (M0). | |
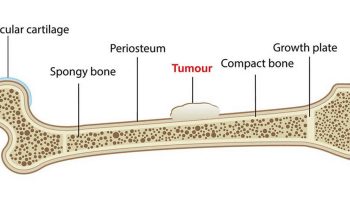
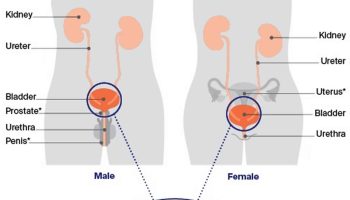
| 3B | T4 N0 M0 | The cancer is any size and is growing into nearby organ(s), such as the vagina, urethra (the tube that carries urine out of the bladder), prostate gland, or bladder (T4). It has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| 3C | T4 N1 M0 | The cancer is any size and is growing into nearby organ(s), such as the vagina, urethra (the tube that carries urine out of the bladder), prostate gland, or bladder (T4) AND it has spread to lymph nodes near the rectum (N1) but not to distant parts of the body (M0). |
| 4 | Any T Any N M1 | The cancer can be any size and may or may not have grown into nearby organs (any T). It may or may not have spread to nearby lymph nodes (any N). It has spread to distant organs, such as the liver or lungs (M1). |
Footnote: * The following additional categories are not listed on the table above:
- TX: Main tumor cannot be assessed due to lack of information.
- T0: No evidence of a primary tumor.
- NX: Regional lymph nodes cannot be assessed due to lack of information.
Anal cancer treatment
If you’re diagnosed with anal cancer, you’ll be cared for by a multidisciplinary team. This is a team of different specialists who work together to provide the best treatment and care. Your treatment options depend on many factors. The location, type, and the stage (extent of spread) of the tumor are important. In choosing your treatment plan, you and your cancer care team will also take into account your age, your overall health, and your personal preferences.
The main treatments used for anal cancer are:
- Chemoradiation – a combination of chemotherapy and radiotherapy
- Chemotherapy. Chemotherapy drugs are injected into a vein or taken as pills. The chemicals travel throughout your body, killing rapidly growing cells, such as cancer cells. Unfortunately they also damage healthy cells that grow rapidly, including those in your gastrointestinal tract and in your hair follicles. This causes side effects such as nausea, vomiting and hair loss.
- Radiation therapy. Radiation therapy uses high-powered beams, such as X-rays and protons, to kill cancer cells. During radiation therapy, you’re positioned on a table and a large machine moves around you, directing radiation beams to specific areas of your body to target your cancer. Radiation may damage healthy tissue near where the beams are aimed. Side effects may include skin redness and sores in and around your anus, as well as hardening and shrinking of your anal canal.
- Surgery – to remove a tumor or a larger section of bowel
Doctors usually treat anal cancer with a combination of chemotherapy and radiation (also called chemoradiation or chemoradiotherapy). Together, these two treatments enhance each other and improve chances for a cure.
- Chemoradiotherapy is the most common treatment for anal cancer if your cancer hasn’t spread to other parts of your body.
- You might have surgery after chemoradiotherapy if it hasn’t been successful or your cancer comes back.
In cases where the cancer has spread and can’t be cured, chemotherapy alone may be considered to help relieve symptoms. This is known as palliative care.
The main treatments are described in more detail below.
Chemoradiation
Chemoradiation is a treatment that combines chemotherapy (cancer-killing medication) and radiotherapy (where radiation is used to kill cancer cells).
Chemoradiation is currently the most effective treatment for anal cancer. You don’t usually need to stay in hospital when you’re having chemoradiation.
Your exact treatment plan will depend on what your treatment team thinks is best for you.
Chemotherapy for anal cancer is usually given in two cycles, each lasting four to five days, with a four-week gap between the cycles. In most cases, 2 or more chemotherapy drugs are used at the same time to shrink the cancer. The most common treatment is a combination of the chemotherapy drugs mitomycin C and fluorouracil (5FU). You have these drugs through a drip.
- The combination of 5-FU (fluorouracil) and cisplatin can also be used, especially in people who can’t get mitomycin or for advanced anal cancer.
- In certain people who may be older or can’t tolerate 2 chemotherapy drugs, 5-FU (fluorouracil) alone may be given with radiation.
For advanced anal cancer or anal cancer that has already been treated with 5-FU and mitomycin, other options for chemotherapy include:
- Carboplatin with paclitaxel (Taxol)
- 5-FU with cisplatin
- Oxaliplatin, Leucovorin and 5-FU
- Docetaxel (Taxotere), cisplatin and 5-FU
- Cisplatin, Leucovorin and 5-FU
In these treatments, the 5-FU is given into a vein 24 hours a day for 4 or 5 days. In many cases, part of the chemotherapy is delivered through a small tube called a peripherally inserted central catheter in your arm, which can stay in place until your treatment has finished. The tube means you don’t need to stay in hospital during each of the cycles of chemotherapy. However, you’ll be attached to a small plastic pump, which you take home with you. The other drugs are given more quickly on certain other days in the treatment cycle.
A few hospitals now offer tablet chemotherapy for anal cancer, which avoids the need for the pump and peripherally inserted central catheter. Sometimes, the oral drug capecitabine might be given in place of 5-FU. Talk to your treatment team about your treatment plan and how and where you will get chemo.
Radiation is given 5 days a week for at least 5 weeks. You typically undergo radiation therapy for anal cancer for five or six weeks. Chemotherapy is typically administered during the first week and the fifth week. Your doctor tailors your treatment schedule based on characteristics of your cancer and your overall health.
Though combining chemotherapy and radiation increases the effectiveness of the two treatments, it also makes side effects more likely. Discuss with your doctor what side effects to expect.
Both chemotherapy and radiotherapy often cause significant side effects, including:
- tiredness
- sore skin around the anus
- sore skin around the penis and scrotum in men or vulva in women
- hair loss – limited hair loss from the head, but total loss from the pubic area
- feeling sick
- nausea and vomiting
- loss of appetite or weight changes
- hair loss
- diarrhea
- mouth sores
- a greater chance of infection (from low white blood cell counts)
- easy bleeding or bruising (from low blood platelet counts)
- fatigue or shortness of breath (from low red blood cell counts)
These side effects are usually temporary, but there’s also a risk of longer-term problems, such as infertility.
If you’re concerned about the potential side effects of treatment, you should discuss this with your care team before treatment begins.
Other possible long-term side effects can include:
- bowel control problems
- long-term (chronic) diarrhea
- erectile dysfunction
- vaginal pain when having sex
- dry and itchy skin around the groin and anus
- bleeding from the anus, rectum, vagina or bladder
Along with the risks above, some chemo drugs can cause other, less common side effects.
For instance, cisplatin, paclitaxel, oxaliplatin, or docetaxel might cause nerve damage (called peripheral neuropathy). This can lead to numbness, tingling, sensitivity to cold, or pain in the hands and feet.
DPD deficiency: Between 2 and 8 out of 100 people (2 to 8%) have low levels of an enzyme called dihydropyrimidine dehydrogenase (DPD) in their bodies. A lack of DPD can mean you’re more likely to have severe side effects from capecitabine or fluorouracil. It might take you a bit longer to recover from the chemotherapy. These side effects can rarely be life threatening. Before starting treatment with capecitabine or fluorouracil you have a blood test to check levels of dihydropyrimidine dehydrogenase (DPD). So you may start treatment with a lower amount (dose) of the drug or have a different treatment. Your doctor or nurse will talk to you about this.
Most side effects get better over time once treatment stops, but some can last a long time or even be permanent. If you’re going to get chemo, be sure to discuss the drugs that will be used and their possible side effects.
Tell your doctor or nurse about any side effects as soon as you notice them so they can be treated promptly. For example, drugs can be used to help control nausea and vomiting. In some cases, changing the treatment dosage or delaying or stopping treatment may keep the side effects from getting worse.
Surgery
Surgery is a less common treatment option for anal cancer. It’s usually only considered if the tumor is small and can be easily removed, or if chemoradiation hasn’t worked.
If the tumor is very small and clearly defined, it may be cut out during a procedure called a local excision. This is a relatively simple procedure, carried out under general anesthetic, that usually only requires a stay in hospital of a few days.
Potential side effects of surgery depend on many things, including the extent of the operation and the person’s health before surgery. Most people will have at least some pain after the operation, but it usually can be controlled with medicines. Other problems can include reactions to anesthesia, damage to nearby organs, bleeding, blood clots in the legs, and infection.
Surgery to remove early-stage anal cancers
Very small anal cancers may be removed through surgery. During this procedure, the surgeon removes the tumor and a small amount of healthy tissue that surrounds it. Because the tumors are small, early-stage cancers can sometimes be removed without damaging the anal sphincter muscles that surround the anal canal. Anal sphincter muscles control bowel movements, so doctors work to keep the muscles intact. Depending on your cancer, your doctor may also recommend chemotherapy and radiation after surgery.
Surgery for late-stage anal cancers or anal cancers that haven’t responded to other treatments
If your cancer hasn’t responded to chemotherapy and radiation (chemoradiation) or if your cancer is advanced, your doctor may recommend a more complex operation called abdominoperineal resection, which is sometimes referred to as an AP resection or APR. An abdominoperineal resection (APR) involves removing your anus, rectum, part of the colon, some surrounding muscle tissue, and sometimes some of the surrounding lymph nodes (small glands that form part of the immune system) to reduce the risk of the cancer returning. The surgeon then attaches the remaining portion of your colon to an opening (stoma) in your abdomen through which your stools will leave your body and collect in a colostomy bag. You’ll usually need to stay in hospital for up to 10 days after this type of surgery. Before and after the operation, you’ll see a specialist nurse who can offer support and advice to help you adapt to life with a colostomy. Adjusting to life with a colostomy can be challenging, but most people become accustomed to it over time.
Abdominoperineal resection (APR) tends to cause more side effects, many of which are long-lasting. For instance, after an abdominoperineal resection (APR), you might develop scar tissue (called adhesions) in your belly that can cause organs or tissues to stick together. This might cause pain or problems with food moving through the bowels, which can lead to digestive problems.
People also need a permanent colostomy after an abdominoperineal resection (APR). This can take some time to get used to and may mean some lifestyle changes.
An abdominoperineal resection (APR) can sometimes damage the ureters or urethra (tubes that collect your urine) making it difficult to urinate (pee). This might mean more surgery.
For men, an APR may cause erection problems, trouble having an orgasm, or less intense orgasms. An abdominoperineal resection (APR) can also damage the nerves that control ejaculation, leading to “dry” orgasms (orgasms without semen).
APR usually does not cause a loss of sexual function for women, but abdominal adhesions (scar tissue) may sometimes cause pain during sex.
Immunotherapy
Immunotherapy is the use of medicines to stimulate your immune system to recognize and destroy cancer cells more effectively. Your body’s disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that make them undetectable by the immune system cells. Immunotherapy works by interfering with that process. Immunotherapy treatments are generally reserved for people with advanced anal cancer.
Immune checkpoint inhibitors
An important part of your immune system is its ability to keep itself from attacking normal cells in the body. To do this, it uses “checkpoints” – proteins on immune cells that need to be turned on (or off) to start an immune response. Cancer cells sometimes use these checkpoints to avoid being attacked by the immune system. But drugs that target these checkpoints can be used to treat some people with anal cancer.
Nivolumab (Opdivo) and pembrolizumab (Keytruda) target PD-1, a protein on certain immune cells (called T cells) that normally helps keep these cells from attacking other cells in the body 7. By blocking PD-1, these drugs boost the immune response against cancer cells. This can shrink some tumors or slow their growth.
Nivolumab and pembrolizumab can be used in people with anal cancer that has spread (metastasized) and whose cancer starts growing after getting at least one type of chemotherapy.
Nivolumab can be given as an intravenous (IV) infusion every 2 or 4 weeks. Pembrolizumab can be given as an intravenous (IV) infusion every 3 or 6 weeks.
Possible side effects of checkpoint inhibitors
Side effects of checkpoint inhibitors can include fatigue, cough, nausea, itching, skin rash, loss of appetite, constipation, joint pain, and diarrhea.
Other, more serious side effects occur less often:
- Infusion reactions: Some people might have an infusion reaction while getting these drugs. This is like an allergic reaction, and can include fever, chills, flushing of the face, rash, itchy skin, feeling dizzy, wheezing, and trouble breathing. It’s important to tell your doctor or nurse right away if you have any of these symptoms while getting these drugs.
- Autoimmune reactions: These drugs work by basically removing one of the defenses on the body’s immune system. Sometimes the immune system starts attacking other parts of the body, which can cause serious or even life-threatening problems in the lungs, intestines, liver, hormone-making glands, kidneys, or other organs.
It’s very important to report any new side effects to your health care team as soon as possible. If serious side effects do occur, treatment may need to be stopped and you may get high doses of corticosteroids to suppress your immune system.
Treatment of anal cancer by stage
The type of treatment your cancer care team will recommend depends on the type of anal cancer, where it is, and how far it has spread (the stage).
Perianal tumors (previously called anal margin cancers) are sometimes treated differently from anal canal cancers.
Stage 0
At this stage, the pre-cancer cells are still only in the inner lining of the anus and have not grown into deeper layers.
Stage 0 tumors can often be removed completely by surgery (local resection). The goal is to take out all of the pre-cancer as well as an edge (margin) of healthy tissue around it. Radiation therapy and chemotherapy (chemo) are rarely needed.
Stages 1 and 2
These cancers have grown into the anal wall but have not grown into nearby organs or spread to nearby lymph nodes. Most often they have not spread to nearby lymph nodes.
Surgery (local resection) might be used to remove some small tumors (usually less than 2 centimeter or 1 inch) that do not involve the sphincter muscle. In some cases, this may be followed with chemo and radiation therapy.
The standard treatment for anal cancers that cannot be removed without harming the anal sphincter is external beam radiation therapy (EBRT) combined with chemo (called chemoradiation). In chemoradiation, the 2 treatments are given over the same time period. The chemo is usually 5-FU with mitomycin. This combination of chemo is typically given during the first week and around the fifth week of treatment. The external beam radiation therapy is given daily, Monday through Friday, for 5 to 7 weeks.
If the cancer hasn’t gone away completely after chemoradiation is done, more treatment might be needed. But it’s important to know that it may take months to see the full effects of chemoradiation. Because of this, it is important to continue follow-up appointments with your doctors to monitor the cancer through digital rectal examination and anoscopy. Your doctors may watch any remaining cancer for up to 6 months. It may continue to shrink and even go away without more treatment.
At 6 months, if cancer is still found, more treatment is often needed. Most of the time, a surgery called an abdominoperineal resection (APR) might be recommended. In certain cases, only a local resection might be needed.
Stages 3A, 3B, and 3C
These cancers have grown into nearby organs or spread to nearby lymph nodes, but they have not spread to distant parts of the body.
In most cases, the first treatment will be radiation therapy combined with chemo (chemoradiation). In chemoradiation, both treatments are given over the same time period. The chemo is usually 5-FU with mitomycin. This combination of chemo is typically given during the first week and then around the fifth week of treatment. The radiation is given daily, Monday through Friday, for 5 to 7 weeks.
If some cancer remains after the chemoradiation, it may be watched closely for up to 6 months because it can take months to see the full effects of treatment.
If more treatment is needed because all of the cancer has not gone away by 6 months, most often a surgery called an abdominoperineal resection (APR) might be recommended. If the cancer has spread to or is still present in nearby lymph nodes, they may be removed with surgery or treated with radiation therapy.
Stage 4
In this stage, the cancer has spread to distant organs. Most often, anal cancer first spreads to the liver, but it can also spread to places such as the lungs, bones, and far away lymph nodes.
Treatment is very unlikely to cure these cancers. Instead, treatment is aimed at controlling the disease for as long as possible and relieving symptoms as much as possible. Chemotherapy, sometimes along with radiation, is usually the standard treatment.
Radiation might be used alone for cancer that has spread to the bones, brain or spinal cord. It might also be used for cancer that has spread to far away lymph nodes.
For some advanced anal cancers that have grown on chemotherapy, immunotherapy might be an option.
Because these cancers can be hard to treat, you might also want to think about taking part in a clinical trial of newer treatments.
Recurrent anal cancer
Cancer is called recurrent when it comes back after treatment. Recurrence can be local (in or near the same place it started) or distant (spread to organs like the lungs or liver).
If cancer returns in the anus or nearby lymph nodes after treatment, treatment depends on what treatment you had the first time. For example, if you had surgery alone, you may get radiation therapy and chemo (chemoradiation). If you first had chemoradiation, then you might be treated with surgery and/or chemo. Treating recurrent anal cancer often requires a surgery called an abdominoperineal resection (APR).
For some people, the cancer will come back in distant sites or organs in the body. The most common sites are the liver and lungs. The main treatment for this is usually chemo. Chemo might not cure the cancer, but it can often help control it and reduce any symptoms it’s causing. In other cases, surgery or radiation therapy might be options to help treat these cancers. But as with chemo, they are unlikely to cure these cancers, so be sure you understand the goal of any treatments offered.
Treating HIV-infected patients
Most people with HIV infection can be given the same treatment as others with anal cancer, and they can have a good outcome. People with advanced HIV disease and weakened immune systems might need to have less intensive chemotherapy.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care. Palliative care can be used while undergoing other aggressive treatments, such as surgery, chemotherapy or radiation therapy.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
Coping and support
A cancer diagnosis can be overwhelming and frightening. You can help yourself to feel more in control by taking an active role in your health care. To help you cope, try to:
- Learn enough about anal cancer to make decisions about your care. Ask your doctor about your anal cancer, including the stage of your cancer, your treatment options and, if you like, your prognosis. As you learn more about anal cancer, you may become more confident in making treatment decisions.
- Keep friends and family close. Keeping your close relationships strong will help you deal with your anal cancer. Friends and family can provide the practical support you’ll need, such as helping take care of your house if you’re in the hospital. And they can serve as emotional support when you feel overwhelmed by cancer.
Find someone to talk with. Find a good listener with whom you can talk about your hopes and fears. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Ask your doctor about support groups in your area. Or check your phone book, library or a cancer organization, such as the National Cancer Institute or the American Cancer Society.
Living with anal cancer
For many people with anal cancer, treatment can remove or destroy the cancer. Completing treatment can be both stressful and exciting. You may be relieved to finish treatment, but it’s hard not to worry about cancer coming back. This is very common if you’ve had cancer.
For other people, anal cancer may never go away completely. Some people may need to get treatments to try to control the cancer for as long as possible. Learning to live with cancer that doesn’t go away can be difficult and very stressful.
Survivors of anal cancer should also stay away from tobacco products. Smoking increases the risk of many cancers and might further increase the risk of many of the second cancers seen after anal cancer.
To help maintain good health, anal cancer survivors should also:
- Get to and stay at a healthy weight
- Keep physically active and limit the time you spend sitting or lying down
- Follow a healthy eating pattern that includes plenty of fruits, vegetables, and whole grains, and limits or avoids red and processed meats, sugary drinks, and highly processed foods
- Don’t drink alcohol. If you drink, have no more than 1 drink per day for women or 2 per day for men
These steps may also lower the risk of some other cancers.
Follow-up care
When you have completed treatment, your doctors will still want to watch you closely. It’s very important to go to all of your follow-up appointments. During these visits, your doctors will ask if you are having any problems and may do a physical exam, which will include a rectal exam, an exam of the anus, and an exam to see if any nearby lymph nodes are enlarged. Blood tests and imaging tests such as CT scans may also be ordered. These exams and tests are meant to look for signs of the cancer returning or side effects from treatment.
Almost any cancer treatment can have side effects. Some might only last for a few days or weeks to months, but others might last a long time. Some side effects might not even show up until years after you have finished treatment. Your doctor visits are a good time to ask questions and to talk about any changes or problems you notice or concerns you have.
Doctor visits and tests
For people with no signs of anal cancer, many doctors recommend follow-up visits (which may include an anoscopy) with physical exams every 3 to 6 months for at least the first 3 years after treatment. CT scans or MRIs are also often done regularly for a certain period of time. These visits may be less often (about every 6 months) for the next several years. Some doctors may advise different follow-up schedules.
Close follow-up is very important in the first several months after chemoradiation treatment, especially if not all of the cancer is gone. Some tumors continue to shrink after chemoradiation, so the doctor will want to watch the cancer closely during this time to see if more treatment might still be needed.
Can I lower my risk of the anal cancer progressing or coming back?
If you have (or have had) anal cancer, you probably want to know if there are things you can do that might lower your risk of the cancer growing or coming back, such as exercising, eating a certain type of diet, or taking nutritional supplements. Unfortunately, it’s not yet clear if there are things you can do that will help.
Adopting healthy behaviors such as not smoking, eating well, getting regular physical activity, and staying at a healthy weight might help, but no one knows for sure. However, we do know that these types of changes can have positive effects on your health that can extend beyond your risk of anal cancer or other cancers. Stopping smoking may also help you tolerate treatments like chemotherapy and radiation much better.
If you have a colostomy
Most people treated for anal cancer don’t need extensive surgery known as an abdominoperineal resection, or APR. But if you do have an abdominoperineal resection (APR), you will need to have a permanent colostomy.
If you have a colostomy, follow-up is important. You might feel worried or isolated from normal activities. A wound, ostomy, continence nurse (WOCN) or enterostomal therapist (a health care professional trained to help people with their colostomies) can teach you how to care for your colostomy.
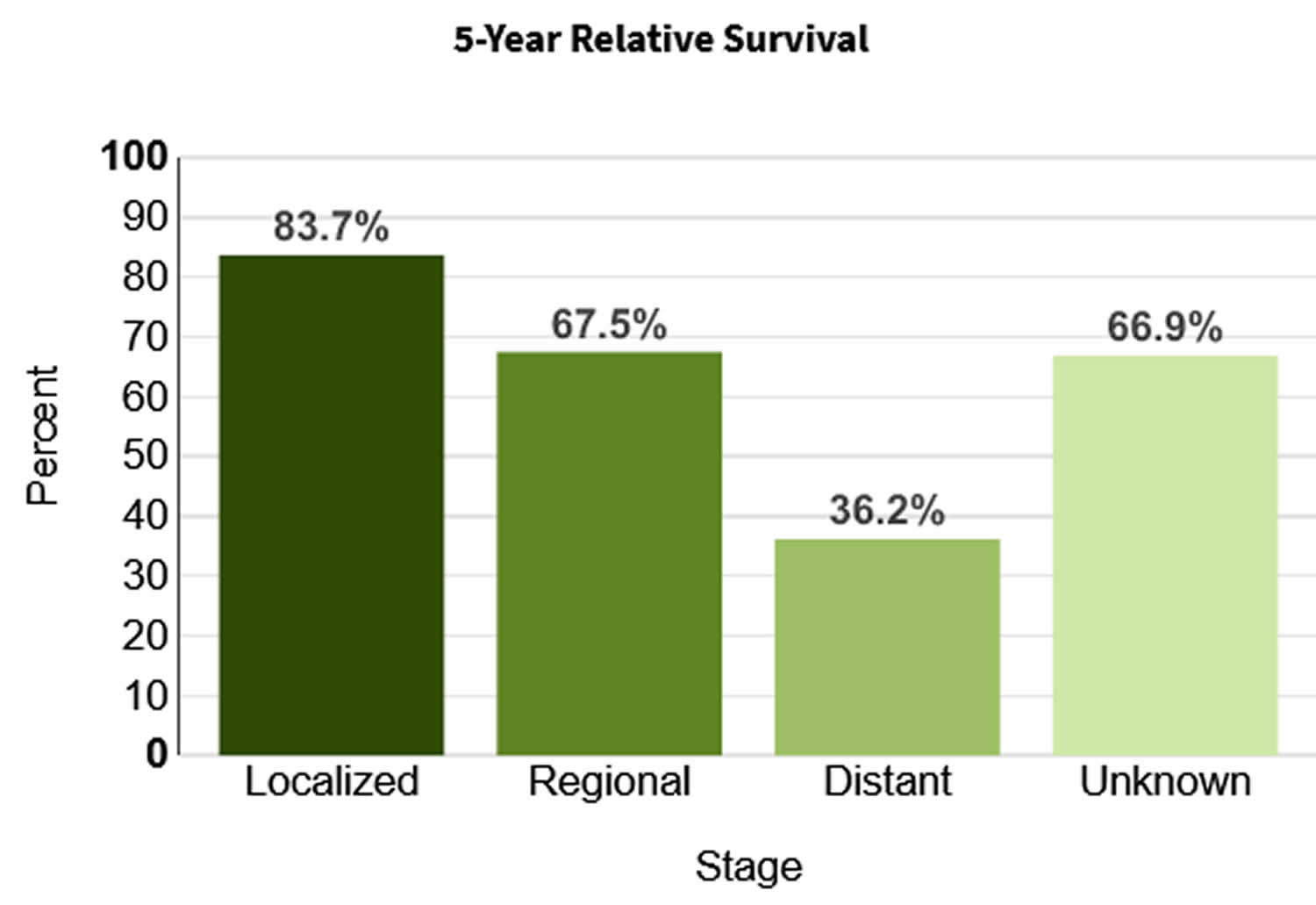
Anal Cancer Survival Rates
Survival rates can give you an idea of what percentage of people with the same type and stage of cancer are still alive a certain amount of time (usually 5 years) after they were diagnosed. They can’t tell you how long you will live, but they may help give you a better understanding of how likely it is that your treatment will be successful. Keep in mind that survival rates are estimates and are often based on previous outcomes of large numbers of people who had a specific cancer, but they can’t predict what will happen in any particular person’s case. These statistics can be confusing and may lead you to have more questions. Your doctor is familiar with your situation; ask how these numbers may apply to you.
A relative survival rate compares people with the same type and stage of cancer to people in the overall population. For example, if the 5-year relative survival rate for a specific stage of anal cancer is 70.4%, it means that people who have that cancer are, on average, about 70.4% as likely as people who don’t have that cancer to live for at least 5 years after being diagnosed.
The SEER (Surveillance, Epidemiology, and End Results) database tracks 5-year relative survival rates for anal cancer in the United States, based on how far the cancer has spread 2. The SEER database, however, does not group cancers by American Joint Committee on Cancer (AJCC) TNM system stages (stage 1, stage 2, stage 3, etc.). Instead, it groups cancers into localized, regional, and distant stages 2:
- Localized: There is no sign that the cancer has spread outside of the anal area.
- Regional: The cancer has spread outside the anal area to nearby structures or lymph nodes.
- Distant: The cancer has spread to distant parts of the body, such as the liver or lungs.
Figure 3. Anal cancer 5-year relative survival rates
[Source 2 ]Table 2. Anal cancer survival rates
| 5-year observed survival for anal cancer | ||
| Stage | Squamous cancers | Non-squamous cancers |
| 1 | 77% | 71% |
| 2 | 67% | 59% |
| 3A | 58% | 50% |
| 3B | 51% | 35% |
| 4 | 15% | 7% |
Table 3. 5-year relative survival rates for anal cancer
| SEER stage | 5-year relative survival rate |
|---|---|
| Localized | 83% |
| Regional | 67% |
| Distant | 36% |
| All SEER stages combined | 70% |
Footnotes: These numbers are based on people diagnosed with anal cancer between 2012 and 2018 from the SEER (Surveillance, Epidemiology, and End Results maintained by the National Cancer Institute) database. The SEER tracks 5-year relative survival rates for anal cancer in the United States, based on how far the cancer has spread and does not group cancers by AJCC TNM stages (stage 1, stage 2, stage 3, etc.). Instead, the SEER groups cancers into localized, regional, and distant stages:
- Localized: There is no sign that the cancer has spread outside of the anal area.
- Regional: The cancer has spread outside the anal area to nearby structures or lymph nodes.
- Distant: The cancer has spread to distant parts of the body, such as the liver or lungs.
A relative survival rate compares people with the same type and stage of cancer to people in the overall population. For example, if the 5-year relative survival rate for a specific stage of anal cancer is 83%, it means that people who have that cancer are, on average, about 83% as likely as people who don’t have that cancer to live for at least 5 years after being diagnosed.
[Source 8 ]Anal cancer prognosis
Localized anal cancer has a good prognosis, while metastatic disease has a poor prognosis 3.
- Key Statistics for Anal Cancer. https://www.cancer.org/cancer/anal-cancer/about/what-is-key-statistics.html[↩][↩][↩]
- Anal Cancer — Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/anus.html[↩][↩][↩][↩]
- Babiker HM, Kashyap S, Mehta SR, et al. Anal Cancer. [Updated 2023 Jun 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441891[↩][↩][↩][↩]
- What Causes Anal Cancer? https://www.cancer.org/cancer/types/anal-cancer/causes-risks-prevention/what-causes.html[↩]
- HPV Vaccine. https://www.cdc.gov/hpv/parents/vaccine-for-hpv.html[↩][↩]
- Anal Cancer Stages. https://www.cancer.org/cancer/types/anal-cancer/detection-diagnosis-staging/staging.html[↩]
- Immunotherapy for Anal Cancer. https://www.cancer.org/cancer/anal-cancer/treating/immunotherapy.html[↩]
- Anal Cancer Survival Rates. https://www.cancer.org/cancer/anal-cancer/detection-diagnosis-staging/survival-rates.html[↩]