Contents
What is anaphylaxis
Anaphylaxis is a severe and potentially life-threatening reaction to a trigger such as an allergy. It’s also known as anaphylactic shock.
- Anaphylaxis is a medical emergency that requires immediate medical assistance and treatment.
- Anaphylaxis can occur within seconds or minutes of exposure to something you’re allergic to, such as peanuts or bee stings.
Anaphylaxis causes your immune system to release a flood of chemicals that can cause you to go into shock — your blood pressure drops suddenly and your airways narrow, blocking breathing. Signs and symptoms include a rapid, weak pulse; a skin rash; and nausea and vomiting. Common triggers include certain foods, some medications, insect venom and latex.
Anaphylaxis requires an injection of epinephrine and a follow-up trip to an emergency room. If you don’t have epinephrine, you need to go to an emergency room immediately. If anaphylaxis isn’t treated right away, it can be fatal.
- Trouble breathing or noisy breathing
- Difficulty talking more than a few words and/or hoarse voice
- Wheeze
- Cough
- Swelling and tightness of the throat
- Collapse
- Light-headedness or dizziness
- Diarrhea
- Tingling in the hands, feet, lips or scalp
- Swelling of tongue
- Pale and floppy (in young children)
A severe allergic reaction (anaphylaxis) is a medical emergency. Call your local emergency immediately. Lay the person down. If they have an adrenaline injector and you are able to administer it, do so.
Anaphylaxis is a medical emergency. It can be very serious if not treated quickly.
If someone has symptoms of anaphylaxis, you should:
- Call your local emergency number for an ambulance immediately – mention that you think the person has anaphylaxis
- Remove any trigger if possible – for example, carefully remove any wasp or bee sting stuck in the skin
- Lie the person down flat and elevate his or her legs – unless they’re unconscious, pregnant or having breathing difficulties
- Use an adrenaline auto-injector if the person has one – but make sure you know how to use it correctly first
- Check the person’s pulse and breathing and, if necessary, administer CPR (cardiopulmonary resuscitation) or other first-aid measures
- Give another injection after 5-15 minutes if the symptoms don’t improve and a second auto-injector is available
If you’re having an anaphylactic reaction, you can follow these steps yourself if you feel able to.
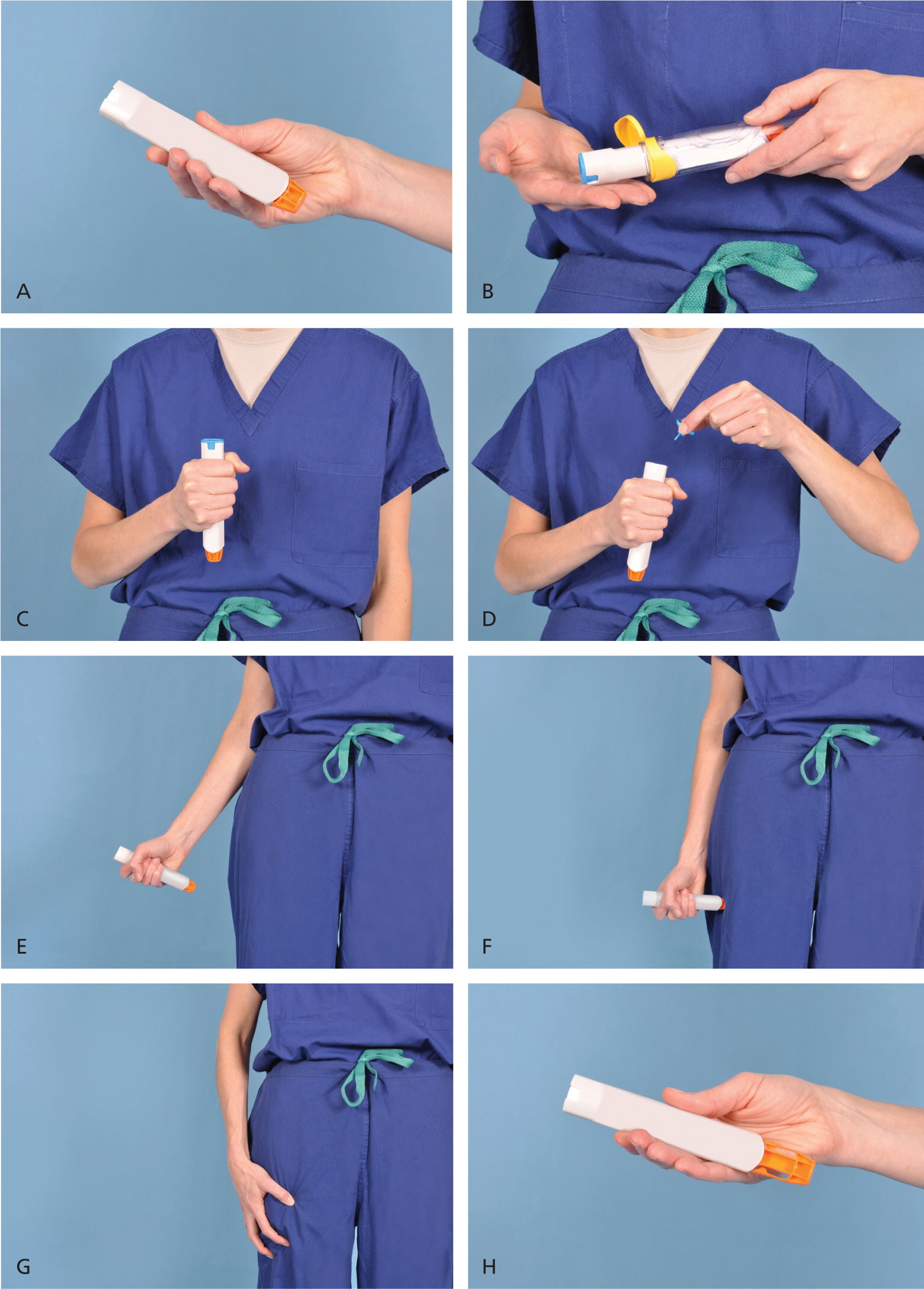
How to use Adrenaline auto-injectors
People with potentially serious allergies will often be given an adrenaline auto-injector to carry at all times. This can help stop an anaphylactic reaction becoming life threatening.
This should be used as soon as a serious reaction is suspected, either by the person experiencing anaphylaxis or someone helping them.
If you’ve been given an auto-injector, make sure you’re aware how to use it correctly.
There are three main types of adrenaline auto-injector, which are used in slightly different ways.
These are:
- EpiPen – see Figure 1 on how to use Epipen
- Jext
- Emerade
Instructions are also included on the side of each injector if you forget how to use it or someone else needs to give you the injection.
Figure 1. How to use the Epipen
Demonstration of appropriate deployment of the (A) Epipen (released in 2008). For demonstration purposes, a trainer device is being used instead of a live device; however, the coloring of key components is the same as the actual adult device. (B) Open the yellow cap of the carrying case and remove the device from its storage tube (the Epipen Jr. has a green cap). (C) Grasp and form a fist around the unit with the orange tip facing down. (D) With the other hand, remove the blue safety release. (E) Aim the orange tip toward the outer thigh. (F) Swing the arm and jab the device firmly into the outer thigh, at a 90-degree angle, until the device clicks. The needle will deploy at this time into thigh (the autoinjector is designed to work through clothing). Hold the device firmly against the thigh for 10 seconds, so the entire dose will be delivered. (G) Remove the device from the thigh and massage the injection area for 10 seconds. (H) The safety feature of the device, extension of the orange tip that locks into place, will completely cover the needle immediately after use. The used device should be taken to the hospital emergency department with the patient for disposal.
Positioning and resuscitation
Someone experiencing anaphylaxis should be placed in a comfortable position.
- Most people should lie flat.
- Pregnant women should lie on their left side to avoid putting too much pressure on the large vein that leads to the heart.
- People having trouble breathing should sit up to help make breathing easier.
- People who are unconscious should be placed in the recovery position to ensure the airway remains open and clear – place them on their side, making sure they’re supported by one leg and one arm, and open their airway by lifting their chin.
- Avoid a sudden change to an upright posture such as standing or sitting up – this can cause a dangerous fall in blood pressure.
If the person’s breathing or heart stops, cardiopulmonary resuscitation (CPR) should be performed immediately.
How to perform a Cardiopulmonary Resuscitation (CPR)
Hands-only CPR
To carry out a chest compression:
- Place the heel of your hand on the breastbone at the center of the person’s chest. Place your other hand on top of your first hand and interlock your fingers.
- Position yourself with your shoulders above your hands.
- Using your body weight (not just your arms), press straight down by 5-6cm (2-2.5 inches) on their chest.
- Keeping your hands on their chest, release the compression and allow the chest to return to its original position.
- Repeat these compressions at a rate of 100 to 120 times per minute until an ambulance arrives or you become exhausted.
When you call for an ambulance, telephone systems now exist that can give basic life-saving instructions, including advice about CPR. These are now common and are easily accessible with mobile phones.
Cardiopulmonary Resuscitation (CPR) with rescue breaths
If you’ve been trained in CPR, including rescue breaths, and feel confident using your skills, you should give chest compressions with rescue breaths. If you’re not completely confident, attempt hands-only CPR instead (see above).
Adults
- Place the heel of your hand on the center of the person’s chest, then place the other hand on top and press down by 5-6cm (2-2.5 inches) at a steady rate of 100 to 120 compressions per minute.
- After every 30 chest compressions, give two rescue breaths.
- Tilt the casualty’s head gently and lift the chin up with two fingers. Pinch the person’s nose. Seal your mouth over their mouth and blow steadily and firmly into their mouth for about one second. Check that their chest rises. Give two rescue breaths.
- Continue with cycles of 30 chest compressions and two rescue breaths until they begin to recover or emergency help arrives.
Children over one year old
- Open the child’s airway by placing one hand on the child’s forehead and gently tilting their head back and lifting the chin. Remove any visible obstructions from the mouth and nose.
- Pinch their nose. Seal your mouth over their mouth and blow steadily and firmly into their mouth, checking that their chest rises. Give five initial rescue breaths.
- Place the heel of one hand on the center of their chest and push down by 5cm (about two inches), which is approximately one-third of the chest diameter.
- The quality (depth) of chest compressions is very important. Use two hands if you can’t achieve a depth of 5cm using one hand.
- After every 30 chest compressions at a rate of 100 to 120 per minute, give two breaths.
- Continue with cycles of 30 chest compressions and two rescue breaths until they begin to recover or emergency help arrives.
Infants under one year old
- Open the infant’s airway by placing one hand on their forehead and gently tilting the head back and lifting the chin. Remove any visible obstructions from the mouth and nose.
- Place your mouth over the mouth and nose of the infant and blow steadily and firmly into their mouth, checking that their chest rises. Give five initial rescue breaths.
- Place two fingers in the middle of the chest and push down by 4cm (about 1.5 inches), which is approximately one-third of the chest diameter. The quality (depth) of chest compressions is very important. Use the heel of one hand if you can’t achieve a depth of 4cm using the tips of two fingers.
- After 30 chest compressions at a rate of 100 to 120 per minute, give two rescue breaths.
- Continue with cycles of 30 chest compressions and two rescue breaths until they begin to recover or emergency help arrives.
Recovery position
If a person is unconscious but is breathing and has no other life-threatening conditions, they should be placed in the recovery position.
Putting someone in the recovery position will keep their airway clear and open. It also ensures that any vomit or fluid won’t cause them to choke.
Figure 2. Recovery position
The video shows a step-by-step guide to putting someone in the recovery position.
Or you can follow these steps:
- with the person lying on their back, kneel on the floor at their side
- place the arm nearest you at a right angle to their body with their hand upwards, towards the head
- tuck their other hand under the side of their head, so that the back of their hand is touching their cheek
- bend the knee farthest from you to a right angle
- carefully roll the person onto their side by pulling on the bent knee
- the top arm should be supporting the head and the bottom arm will stop you rolling them too far
- open their airway by gently tilting their head back and lifting their chin, and check that nothing is blocking their airway
- stay with the person and monitor their condition until help arrives.
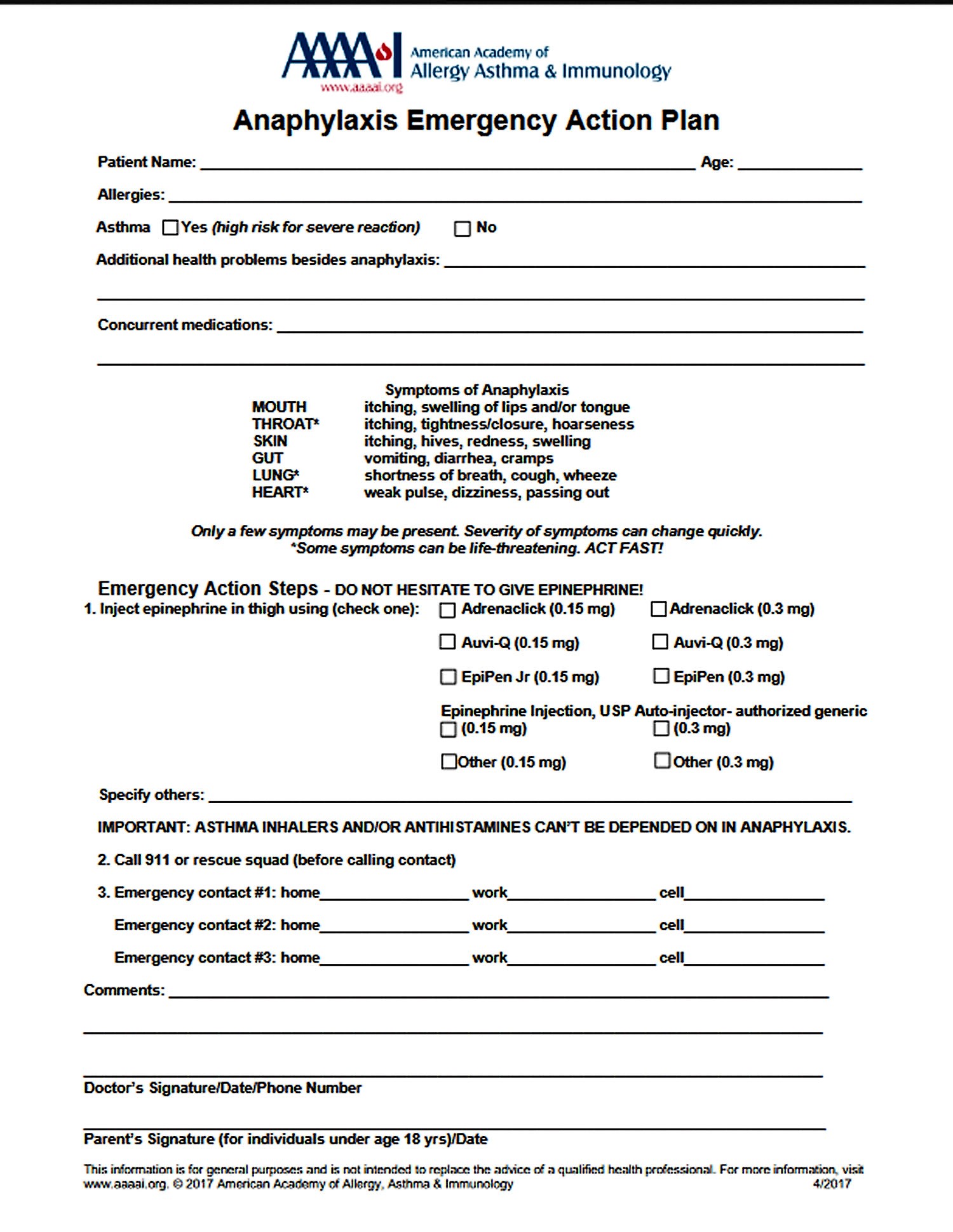
Figure 3. Anaphylaxis Emergency Action Plan
Triggers of anaphylaxis
Anaphylaxis is the result of the immune system – the body’s natural defence system – overreacting to a trigger.
This is often something you’re allergic to, but isn’t always.
The most common anaphylaxis triggers in children are food allergies, such as to peanuts, and tree nuts, fish, shellfish and milk. Besides allergy to peanuts, nuts, fish and shellfish, anaphylaxis triggers in adults include:
- Foods – including nuts, milk, fish, shellfish, eggs and some fruits
- Medicines – including some antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin
- Insect stings – particularly wasp and bee stings
- General anesthetic
- Contrast agents – special dyes used in some medical tests to help certain areas of your body show up better on scans
- Latex – a type of rubber found in some rubber gloves and condoms
In some cases, there’s no obvious trigger. This is known as idiopathic anaphylaxis.
Exercise induced anaphylaxis
Although not common, some people develop anaphylaxis from aerobic exercise, such as jogging, or even less intense physical activity, such as walking. Eating certain foods before exercise or exercising when the weather is hot, cold or humid also has been linked to anaphylaxis in some people. Talk with your doctor about precautions to take when exercising.
If you don’t know what triggers your allergy attack, certain tests can help identify the allergen. In some cases, the cause of anaphylaxis is never identified (idiopathic anaphylaxis).
Risk factors for anaphylaxis
There aren’t many known risk factors for anaphylaxis, but some things that might increase your risk include:
- Previous anaphylaxis. If you’ve had anaphylaxis once, your risk of having this serious reaction increases. Future reactions might be more severe than the first reaction.
- Allergies or asthma. People who have either condition are at increased risk of having anaphylaxis.
- Certain other conditions. These include heart disease and an abnormal accumulation of a certain type of white blood cell (mastocytosis).
Preventing anaphylaxis
If you have a serious allergy or have experienced anaphylaxis before, it’s important to try to prevent future episodes.
The following can help reduce your risk:
- Identify any triggers – you may be referred to an allergy clinic for allergy tests to check for anything that could trigger anaphylaxis
- Avoid triggers whenever possible – for example, you should be careful when food shopping or eating out if you have a food allergy
- If you have food allergies, carefully read the labels of all the foods you buy and eat. Manufacturing processes can change, so it’s important to periodically recheck the labels of foods you commonly eat.
- When eating out, ask how each dish is prepared, and find out what ingredients it contains. Even small amounts of food you’re allergic to can cause a serious reaction.
- If you’re allergic to stinging insects, use caution around them. Wear long-sleeved shirts and pants; don’t walk barefoot on grass; avoid bright colors; don’t wear perfumes, colognes or scented lotions; and don’t drink from open soda cans outdoors. Stay calm when near a stinging insect. Move away slowly and avoid slapping at the insect.
- Carry your adrenaline auto-injector at all times – give yourself an injection whenever you think you may be experiencing anaphylaxis, even if you’re not completely sure.
- If you have an epinephrine autoinjector, check the expiration date and be sure to refill your prescription before it expires.
- Wear a medical alert necklace or bracelet to indicate you have an allergy to specific drugs or other substances.
- Be sure to alert all your doctors to medication reactions you’ve had.
Identify triggers
Finding out if you’re allergic to anything that could trigger anaphylaxis can help you avoid these triggers in the future.
If you’ve had anaphylaxis and haven’t already been diagnosed with an allergy, you should be referred to an allergy clinic for tests to identify any triggers.
The most commonly used tests are:
- a skin prick test – your skin is pricked with a tiny amount of a suspected allergen to see if it reacts
- a blood test – a sample of your blood is taken to test its reaction to a suspected allergen
Avoid triggers
If a trigger has been identified, you’ll need to take steps to avoid it in the future whenever possible. See below for advice about avoiding some specific triggers.
Food
You can reduce the chances of being exposed to a food allergen by:
- checking food labels and ingredients
- letting staff at a restaurant know what you’re allergic to so it’s not included in your meal
- remembering some types of food may contain small traces of potential allergens – for example, some sauces contain wheat and peanuts
Insect stings
You can reduce your risk of being stung by an insect by taking basic precautions, such as:
- moving away from wasps, hornets or bees slowly without panicking – don’t wave your arms around or swat at them
- using an insect repellent if you spend time outdoors, particularly in the summer
- being careful drinking out of cans when there are insects around – insects may fly or crawl inside the can and sting you in the mouth when you take a drink
- not walking around outside with bare feet
Some specialist allergy centers can also offer special treatment to help desensitize you to insect stings (immunotherapy).
Medicines
If you’re allergic to certain types of medicines, there are normally alternatives that can be safely used.
For example, if you’re allergic to:
- penicillin – you can normally safely take a different group of antibiotics known as macrolides
- non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin – you can normally safely take paracetamol; read the ingredients of things like colds medicines carefully to make sure they don’t contain NSAIDs
- one type of general anesthetic – others are available, or it may be possible to perform surgery using a local anaesthetic or an epidural injection
Always tell any healthcare professional about medicine allergies you have, as they may not be aware of them.
Be prepared
Even if you’re careful, at some point you’ll likely be exposed to what you’re allergic to. Fortunately, you can respond quickly and effectively to an allergy emergency by knowing the signs and symptoms of an anaphylactic reaction and having a plan to quickly treat those symptoms.
It’s important to remember the following:
- carry an auto-injector at all times – there should be no exceptions; you may also be advised to get an emergency card or bracelet with full details of your allergy and doctor’s contact details to alert others
- extremes of heat can make adrenaline less effective – so don’t leave your auto-injector in the fridge or your car’s glove compartment, for example
check the expiry date regularly – an out-of-date injector will offer limited protection - manufacturers offer a reminder service, where you can be contacted near the expiry date – check the information leaflet that comes with your medicine for more information
- don’t delay injecting yourself if you think you may be experiencing anaphylaxis, even if your initial symptoms are mild – it’s better to use adrenaline early and then find out it was a false alarm than delay treatment until you’re sure you’re experiencing severe anaphylaxis
If your child has an auto-injector, they will need to change over to an adult dose once they reach 30kg (approximately 4.5 stone).
Anaphylaxis signs and symptoms
Anaphylaxis signs and symptoms can include:
- trouble breathing or noisy breathing
- difficulty talking more than a few words and/or hoarse voice
- wheeze
- cough
- swelling and tightness of the throat
- collapse
- light-headedness or dizziness
- diarrhea
- tingling in the hands, feet, lips or scalp
- swelling of tongue
- pale and floppy (in young children)
A severe allergic reaction (anaphylaxis) is a medical emergency. Call your local emergency immediately. Lay the person down. If they have an adrenaline injector and you are able to administer it, do so.
Anaphylaxis Diagnosis
Your doctor will ask you questions about previous allergic reactions, including whether you’ve reacted to:
- Particular foods
- Medications
- Latex
- Insect stings
To help confirm the diagnosis:
- You might be given a blood test to measure the amount of a certain enzyme (tryptase) that can be elevated up to three hours after anaphylaxis
- You might be tested for allergies with skin tests or blood tests to help determine your trigger
Many conditions have signs and symptoms similar to those of anaphylaxis. Your doctor will want to rule out other conditions.
Anaphylaxis treatment
During an anaphylactic attack, you might receive cardiopulmonary resuscitation (CPR) if you stop breathing or your heart stops beating. You might also be given medications, including:
- Epinephrine (adrenaline) to reduce your body’s allergic response
- Oxygen, to help you breathe
- Intravenous (IV) antihistamines and cortisone to reduce inflammation of your air passages and improve breathing
- A beta-agonist (such as albuterol) to relieve breathing symptoms
The preferred route of administration for epinephrine is intramuscular injection because it provides more reliable and quicker rise to effective plasma levels than the subcutaneous route 1. An intramuscular 1:1,000 aqueous solution of epinephrine at a dose of 0.01 mg per kg (maximal dose of 0.3 mg in children and 0.5 mg in adults) is given every five to 15 minutes until the patient is without symptoms of respiratory or vascular compromise 2. The onset of action is usually three to five minutes. The use of a commercially made autoinjector is preferred, because dosing errors are common when drawing epinephrine from a vial. Commercial devices allow for a set dose with the correct dilution (e.g., 0.15 mg for patients weighing less than 66 lb [30 kg]; 0.3 mg for patients weighing more than 66 lb) 3. Intravenous epinephrine may be used to manage refractory anaphylaxis in consultation with an intensivist, because dosing requires close cardiovascular monitoring 4.
Epinephrine activates the α1 adrenergic receptors and β1 and β2 adrenergic receptors, leading to immediate vasoconstriction, increased peripheral resistance, decreased mucosal edema, increased cardiac inotropy/chronotropy, and bronchodilation, reversing the airway obstruction and vascular collapse 1. In a retrospective review of food-induced anaphylaxis in 13 children, all seven of the surviving patients received epinephrine within five minutes of severe respiratory symptoms, whereas the six who died did not 5.
- You will need to go to hospital for observation – usually for 6-12 hours – as the symptoms can occasionally return during this period.
In most cases of anaphylaxis, symptoms completely abate with intramuscular epinephrine. Your physician will need to determine the length of postreaction monitoring. The unpredictable nature of biphasic reactions makes this decision difficult, and no guidelines address this issue 6. Reaction severity is not a predictor of biphasic reactions 2. The patient’s ability to recognize symptoms and to self-administer epinephrine using an autoinjector should drive this decision. Ten hours of observation is probably adequate in most situations, but some investigators recommend a minimum of 24 hours 6.
While in hospital:
- an oxygen mask may be used to help breathing
- fluids may be given directly into a vein to help increase blood pressure
- additional medications such as antihistamines and steroids may be used to help relieve symptoms
- blood tests may be carried out to confirm anaphylaxis
You should be able to go home when the symptoms are under control and it’s thought they won’t return quickly. This will usually be after a few hours, but may be longer if the reaction was severe.
You may be asked to take antihistamine and steroid tablets for a few days after leaving hospital to help stop your symptoms returning.
You will also probably be asked to attend a follow-up appointment with an allergy specialist so you can be given advice about how you can avoid further episodes of anaphylaxis.
An adrenaline auto-injector may be provided for emergency use between leaving hospital and attending the follow-up appointment.
Using an autoinjector
Many people at risk of anaphylaxis carry an autoinjector. This device is a combined syringe and concealed needle that injects a single dose of medication when pressed against the thigh. Always replace epinephrine before its expiration date, or it might not work properly.
Using an autoinjector immediately can keep anaphylaxis from worsening and could save your life. Be sure you know how to use the autoinjector. Also, make sure the people closest to you know how to use it.
Long-term treatment
If insect stings trigger your anaphylactic reaction, a series of allergy shots (immunotherapy) might reduce your body’s allergic response and prevent a severe reaction in the future.
Unfortunately, in most other cases there’s no way to treat the underlying immune system condition that can lead to anaphylaxis. But you can take steps to prevent a future attack — and be prepared if one occurs.
- Try to avoid your allergy triggers.
- Carry self-administered epinephrine. During an anaphylactic attack, you can give yourself the drug using an autoinjector (EpiPen, others).
- Kemp SF, Lockey RF, Simons FE. Epinephrine: the drug of choice for ananphylaxis. A statement of the World Allergy Organization. Allergy. 2008;63(8):1061–1070.[↩][↩]
- Oswalt ML, Kemp SF. Anaphylaxis: office management and prevention Immunol Allergy Clin North Am. 2007;27(2):177–191vi.[↩][↩]
- Baker TW, Stolfi A, Johnson TL. Use of epinephrine autoinjectors for treatment of anaphylaxis: which commercially available autoinjector do patients prefer? Ann Allergy Asthma Immunol. 2009;103(4):356–358.[↩]
- McLean-Tooke AP, Bethune CA, Fay AC, Spickett GP. Adrenaline in the treatment of anaphylaxis: what is the evidence? BMJ. 2003;327(7427):1332–1335.[↩]
- Sampson HA, Mendelson L, Rosen JP. Fatal and nearfatal anaphylactic reactions to food in children and adolescents. N Engl J Med. 1992;327(6):380–384.[↩]
- Kemp SF. The post-anaphylaxis dilemma: how long is long enough to observe a patient after resolution of symptoms? Curr Allergy Asthma Rep. 2008;8(1):45–48.[↩][↩]