Contents
What is ankylosing spondylitis
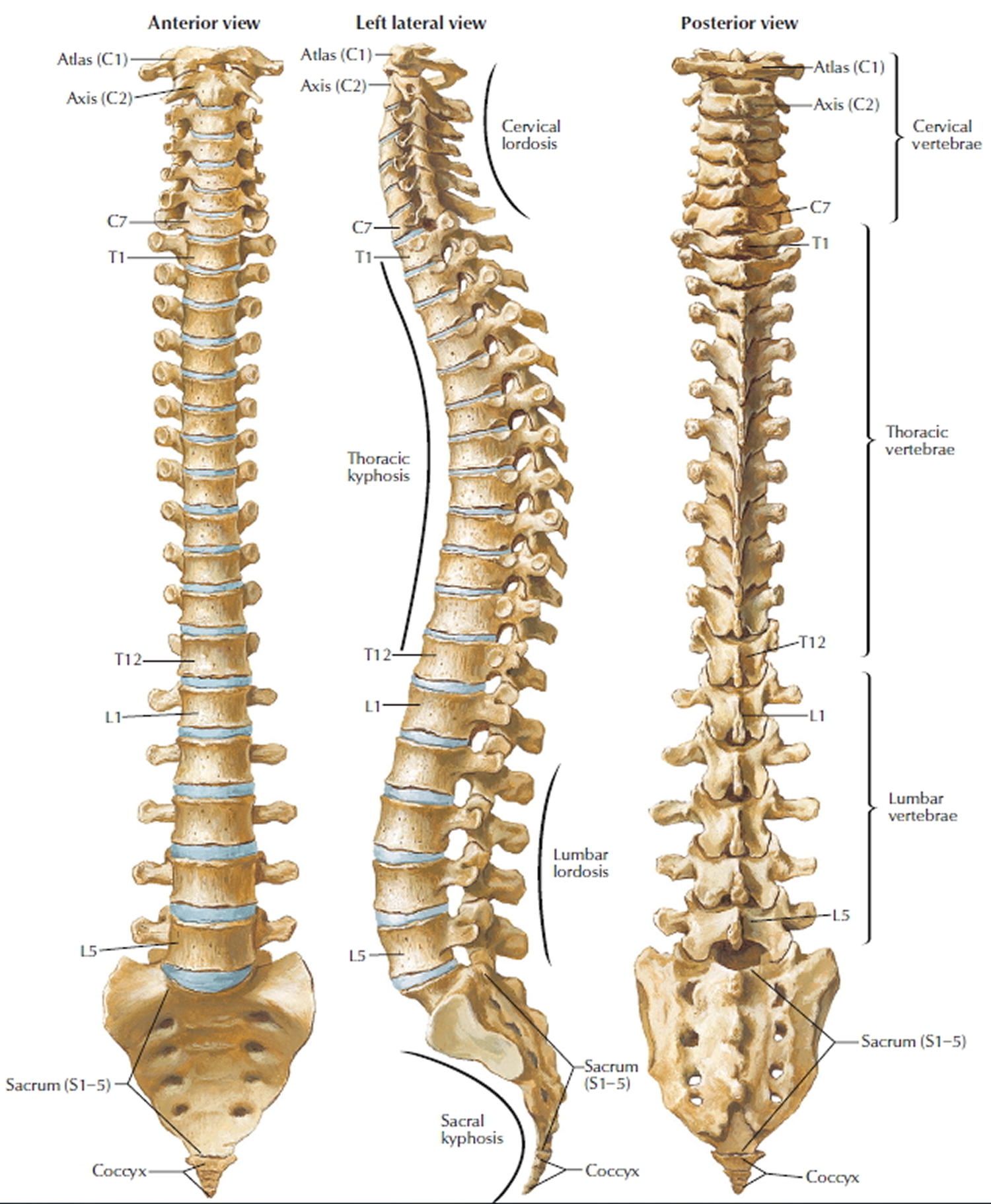
Ankylosing spondylitis is a kind of arthritis that primarily affects the joints and ligaments of your spine (vertebrae) and sacroiliac joints. ‘Ankylosing’ means stiff and ‘spondylo’ means vertebra. In more advanced cases this inflammation can lead to ankylosis — new bone formation in the spine — causing sections of the spine to fuse in a fixed, immobile position. The hallmark feature of ankylosing spondylitis is the involvement of the sacroiliac joints during the progression of the disease. The sacroiliac joints are located at the base of the spine, where the spine joins the pelvis.
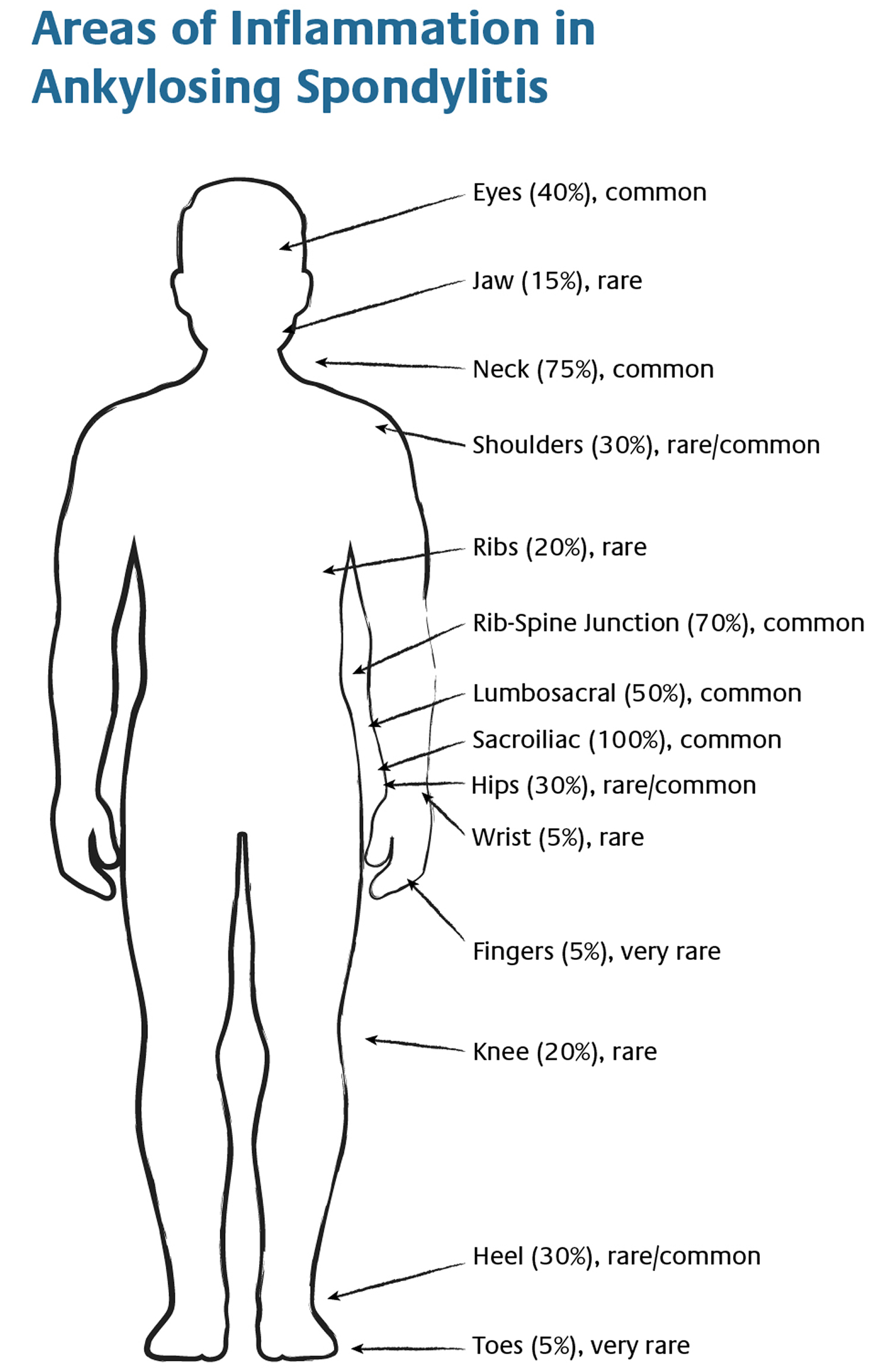
Ankylosing spondylitis can also affect other large joints – such as the shoulders, hips, ribs, heels, and small joints of the hands and feet and may also cause problems in your eyes (known as iritis or uveitis), skin, bowel, lungs and heart.
Ankylosing spondylitis affects 1 in 2,000 births. Males tend to be affected more severely and at an earlier age. Usual onset is between 15 and 25 years of age. Ankylosing spondylitis often runs in families. Relatives may have the disease, or another disease that is associated, for instance Reiter’s disease, psoriatic arthritis or enteropathic arthritis. The cause is unknown, but it is likely that both genes and factors in the environment play a role.
The hallmark feature of ankylosing spondylitis is the involvement of the sacroiliac (SI) joints during the progression of the disease in the late teens or early 20’s. The sacroiliac joints are located at the base of the spine, where the spine joins the pelvis. These problems often start in late adolescence or early adulthood. Early symptoms of ankylosing spondylitis include back pain and stiffness. Pain in one or both buttocks and lower back pain and stiffness are typically worse in the morning, and relieved by exercise. Over time, ankylosing spondylitis can fuse your vertebrae together, limiting movement. Some people have symptoms that come and go. Others have severe, chronic pain and discomfort.
Most people with ankylosing spondylitis are young men in their late teens or early 20s who complain of persistent back pain and early morning stiffness. A smaller number experience pain in their hands or feet. Pronounced stiffness of the spine is the most typical sign, with diminished movements in all directions.
In severe cases the entire backbone may be fixed in a rigid position (‘poker back’), and chest expansion on breathing is reduced. Sometimes the hip joints are involved and become completely fused with resulting loss of movement. Some people may also develop eye, heart and breathing complications.
A diagnosis of ankylosing spondylitis is based on your medical history and a physical examination. You may also have imaging or blood tests.
Ankylosing spondylitis has no cure, but medicines can relieve symptoms and may keep the disease from getting worse. Eating a healthy diet, not smoking, and exercising can also help. In rare cases, you may need surgery to straighten the spine.
Figure 1. Vertebral column
Figure 2. Ankylosing spondylitis areas of body involvement and inflammation
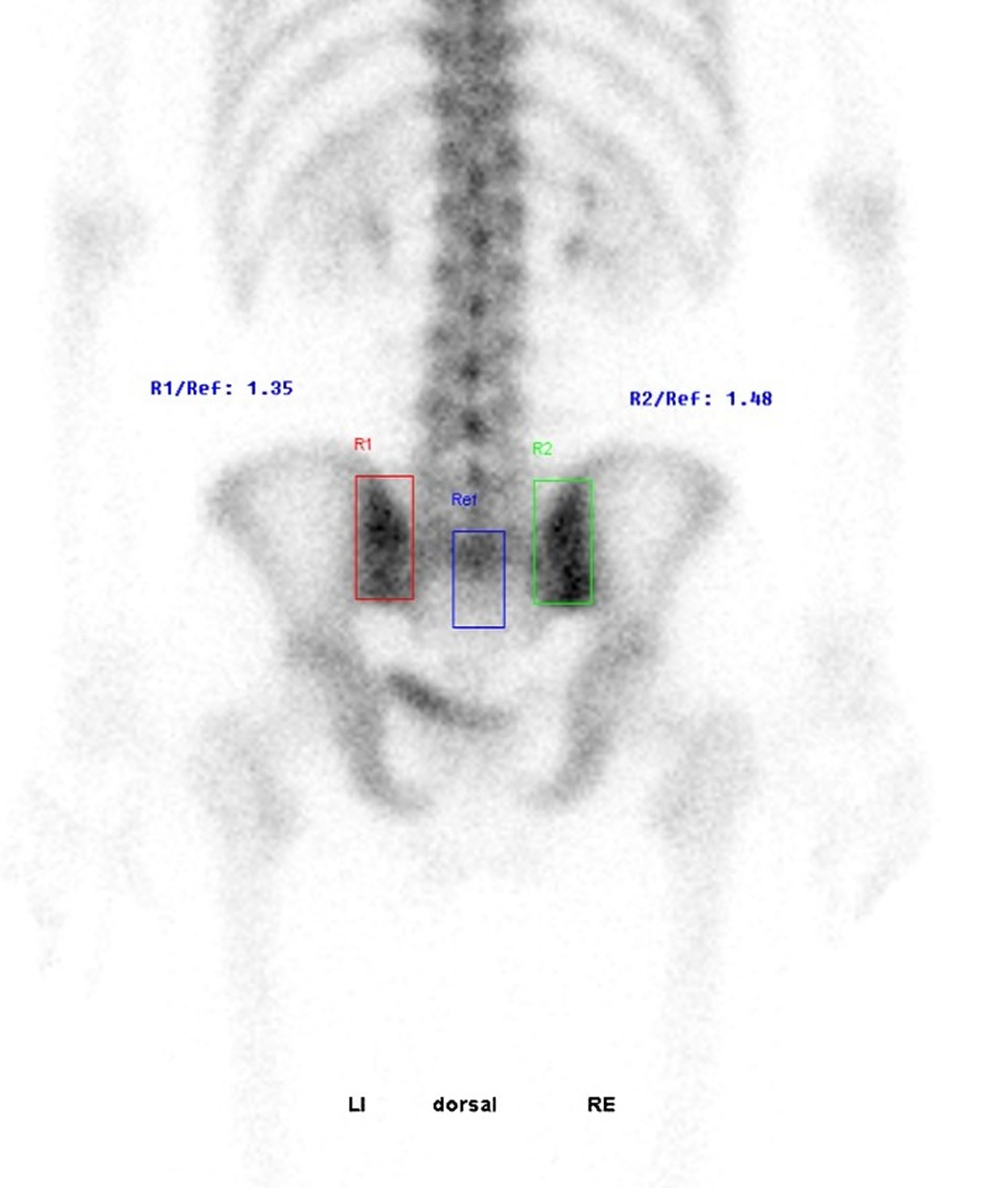
Figure 3. Ankylosing spondylitis in a 30 y.o male patient with chronic low back pain. HLA B27+ with active sacroiliitis
Figure 4. Ankylosing spondylitis sacroiliac joint inflammation (bone scan) – note high bone metabolic turnover at both sacroiliac joint indicating active inflammation.
Ankylosing spondylitis prognosis
The outlook for ankylosing spondylitis is highly variable. For some people the condition improves after an initial period of inflammation, whereas for others it can get progressively worse over time. With special exercises and pain relief, most patients are able to lead independent lives and be fully employed.
Around 70-90% of people with ankylosing spondylitis remain fully independent or minimally disabled in the long term.
Most patients never require hospitalization. However, some people eventually become severely disabled as a result of the bones in their spine fusing in a fixed position and damage to other joints, such as the hips or knees.
With modern treatments, ankylosing spondylitis doesn’t normally affect life expectancy significantly, although the condition is associated with an increased risk of other potentially life-threatening problems.
What Happens over Time
Back and Spine
It is the process of healing and repair following inflammation of the entheses (inflammation where the ligaments attach to the bone) that eventually can lead to scarring of the tissues, which subsequently can lead to extra bone formation. Thus, in someone with very severe disease, the process of inflammation can lead, over many years, to a bony fusion of the ligaments in the spine and sometimes in other joints as well, which is called ankylosis. This can cause an increased risk of spinal fracture because of the restricted range of movement and the fact that the bone formed during fusion is inherently weak. Not everyone will go on to this stage of spondylitis.
Fusion of the spine can sometimes lead to a forward curvature of the spine, called kyphosis, causing a forward-stooped posture. Although this can happen in the most severe cases of ankylosing spondylitis, it is now far less common given the advances in treatment.
It is important to follow your doctor’s instructions, take your medicine on schedule and maintain a daily exercise regimen, which, over time, will make you feel better and lead to better outcomes. It is also important to pay particular attention to your posture in order to avoid kyphosis. With the advent of the newer classes of medications, specifically the biologics anti-tumor necrosis factor-alpha agents), there is reason to believe that the natural course of spondylitis may be slowed or halted. More studies are needed to confirm this.
Figure 5. Ankylosing spondylitis spine
Hips and Shoulders
The hips and shoulders are affected in about one-third of people with ankylosing spondylitis. Hip involvement usually comes on gradually, and although the pain often is felt in the groin area, it can sometimes be felt in other areas of the body, such as the knees or the front of the thigh. When this happens, it is called “referred pain,” which can be very misleading to both a doctor and affected person. Hip involvement typically is more common in younger people when symptoms first begin. It often carries with it a more severe prognosis or course of disease. Generally speaking, shoulder involvement is mild.
The Chest
Adults with spondylitis often have chest pain (costochondritis) that mimics the heavy chest pain of unstable angina (acute heart attack) or pleurisy (the pain with deep breathing that occurs when the outer lining of the lung is inflamed). Anyone experiencing symptoms should seek medical attention to rule out a more serious condition. Over time, long-term inflammation of the joints between the ribs and spine, and where the ribs meet the breastbone in front of the chest, land scarring of tissue results in decreased chest expansion. If the pain is found to be spondylitis-related and you find yourself unable to practice critical deep-breathing exercises, which help maintain chest expansion, there are things that you can do to help yourself:
- Use ice packs on the affected areas for short periods
- Try gentle massage of the neck and shoulder area
- Try deep breathing exercises after a hot shower or warm bath
Talk to your doctor about trying different medications.
Once your doctor has ruled out more serious problems, it might be helpful to take one or two sessions with a physical therapist or respiratory therapist, who can provide instructions on how to maximize air intake by learning a technique called “diaphragm breathing.”
The Jaw
About 10 percent of people with spondylitis experience inflammation of the jaw. This can be particularly debilitating, causing difficulty in fully opening the mouth to eat.
Ankylosing spondylitis complications
In severe ankylosing spondylitis, new bone forms as part of the body’s attempt to heal. This new bone gradually bridges the gap between vertebrae and eventually fuses sections of vertebrae. Those parts of your spine become stiff and inflexible. Fusion can also stiffen your rib cage, restricting your lung capacity and function.
Other complications might include:
- Eye inflammation (iritis). Iritis (anterior uveitis) is a condition sometimes associated with ankylosing spondylitis where the front part of the eye becomes red and swollen. It usually only affects one eye, rather than both. If you have iritis, your eye may become red, painful and sensitive to light (photophobia). Your vision may also become blurred or cloudy. You should visit your doctor as soon as possible if you have ankylosing spondylitis and think you may have developed iritis, as the condition can cause the loss of some or all of your vision if not treated promptly. If your doctor thinks you have iritis, they’ll refer you urgently to an ophthalmologist, a medical doctor who specialises in eye problems, for treatment. Iritis can usually be treated with corticosteroid eye drops.
- Osteoporosis and compression spinal fractures. Some people’s bones thin during the early stages of ankylosing spondylitis. Weakened vertebrae (osteoporosis) can crumble, increasing the severity of your stooped posture. Vertebral fractures can put pressure on and possibly injure the spinal cord and the nerves that pass through the spine. Osteoporosis is where the bones become weak and brittle. In AS osteoporosis can develop in the spine and increase your risk of fracturing the bones in your backbone. The longer you have the condition, the more this risk increases. If you do develop osteoporosis, you’ll usually need to take medication to help strengthen your bones. There are a number of medications that can be used to treat osteoporosis, which can be taken by mouth (orally) as tablets or given by injection.
- Reduced flexibility. Although most people with ankylosing spondylitis remain fully independent or minimally disabled in the long term, some people with the condition eventually have severely restricted movement in their spine. This usually only affects the lower back and is the result of the bones in the spine joining up (fusing). Fusing of the spine can make it difficult to move your back and can mean your posture becomes fixed in one position, although it doesn’t lead to severe disability in most cases. In rare cases surgery may be recommended to correct severe bends in the spine.
- Heart problems. Ankylosing spondylitis can cause problems with your aorta, the largest artery in your body. The inflamed aorta can enlarge to the point that it distorts the shape of the aortic valve in the heart, which impairs its function.
- Cauda equina syndrome. Cauda equina syndrome is a very rare complication of ankylosing spondylitis that occurs when nerves at the bottom of your spine become compressed (compacted). Cauda equina syndrome causes:
- pain or numbness in your lower back and buttocks
- weakness in your legs – which can affect your ability to walk
- urinary incontinence or bowel incontinence – when you cannot control your bladder or bowels
- See your doctor as soon as possible if you have ankylosing spondylitis and you develop any of these symptoms.
- Chest infections
- Joint damage. ankylosing spondylitis can cause joints such as the hips and knees to become inflamed. This can damage the affected joints over time, making them painful and difficult to move. If a joint becomes particularly damaged, you may need surgery to replace it with an artificial one.
- Rarely, kidney disease
- Amyloidosis. In very rare cases it’s possible to develop a condition called amyloidosis as a complication of ankylosing spondylitis. Amyloid is a protein produced by cells in your bone marrow, the spongy material found in the centres of some hollow bones. Amyloidosis is a condition where amyloid builds up in organs such as your heart, kidneys and liver. It can cause a wide range of symptoms, including:
- fatigue
- weight loss
- fluid retention (oedema)
- shortness of breath
- numbness or tingling in the hands and feet
Ankylosing spondylitis causes
The causes of ankylosing spondylitis are not yet understood. However, doctors believe genetics may play a role, because ankylosing spondylitis tends to run in families. Also, most people with ankylosing spondylitis share the same gene (called HLA B27). However, only some people with the gene develop the condition.
HLA-B27 gene
Research has shown more than 9 out of 10 people with ankylosing spondylitis carry a particular gene known as human leukocyte antigen B27 (HLA-B27).
Having the HLA-B27 gene doesn’t necessarily mean you’ll develop ankylosing spondylitis. It’s estimated 8 in every 100 people in theCaucasian population have the HLA-B27 gene, but most don’t have ankylosing spondylitis. Generally speaking, no more than 2 percent of people born with HLA-B27 gene will eventually develop spondylitis.
It is important to note that the HLA-B27 test is not a diagnostic test for ankylosing spondylitis. Also, the association between ankylosing spondylitis and HLA-B27 varies among different ethnic and racial groups. It can be a very strong indicator in that more than 95 percent of people in the Caucasian population who have ankylosing spondylitis test positive for HLA-B27. However, close to 80 percent of ankylosing spondylitis patients from Mediterranean countries and only 50 percent of African American patients with ankylosing spondylitis are HLA-B27 positive.
It’s thought having this gene may make you more vulnerable to developing ankylosing spondylitis. The condition may be triggered by one or more environmental factors, although it’s not known what these are.
Testing for this gene may be carried out if ankylosing spondylitis is suspected. However, this test isn’t a very reliable method of diagnosing the condition because some people can have the HLA-B27 gene but not have ankylosing spondylitis.
Ankylosing spondylitis can run in families, and the HLA-B27 gene can be inherited from another family member.
- If you have ankylosing spondylitis and tests have shown you carry the HLA-B27 gene, the chance of any children you have developing the condition is less than 20%.
- If you have ankylosing spondylitis but don’t carry the HLA-B27 gene, the chance of any children you have developing the condition is less than 10%.
- If you have a close relative who has ankylosing spondylitis, such as a parent or a brother or sister, you’re three times more likely to develop the condition compared with someone who doesn’t have a relative with the condition.
Ankylosing spondylitis symptoms
Inflammation of the entheses, where joint capsules, ligaments, or tendons attach to bone, is a hallmark of ankylosing spondylitis. This can be felt in multiple areas of the body, where doctor can check for pain and tenderness. The sites are sometimes referred to as “hot spots.” They can lead to swelling and tenderness along the back, pelvic bones, sacroiliac joints, the chest, and the heel. The heel can be significantly affected, and the pain and tenderness can have a serious impact on a person’s mobility. The two areas of the foot that can be affected are the Achilles tendon, at the back of the heel and the plantar fascia, at the base of the heel.
It is important to note that the course of ankylosing spondylitis (ankylosing spondylitis) varies greatly from person to person. So too can the onset of symptoms. Although symptoms usually start to appear in late adolescence or early adulthood (ages 17 to 45), symptoms can occur in children or much later in life.
The symptoms of ankylosing spondylitis tend to come and go. The more common symptoms include:
- back pain or buttock pain, that may be worse in bed at night
- stiffness in the morning, or after long periods of rest
- other joint pain
- pain in tendons and ligaments, such as in the chest wall, soles of the feet, or heels
- problems with your heart, lungs, bowel, skin or eyes.
Many of these symptoms can be a sign of other conditions, so it’s best to seek medical advice to make a diagnosis.
The most common early symptoms of ankylosing spondylitis are frequent pain and stiffness in the lower back and buttocks, which comes on gradually over the course of a few weeks or months. At first, discomfort may only be felt on one side, or alternate sides. The pain is usually dull and diffuse, rather than localized. This pain and stiffness is usually worse in the mornings and during the night, but may be improved by a warm shower or light exercise. Also, in the early stages of ankylosing spondylitis, there may be mild fever, loss of appetite, and general discomfort. It is important to note that back pain from ankylosing spondylitis is inflammatory in nature and not mechanical.
The pain typically becomes persistent (chronic) and is felt on both sides, usually lasting for at least three months. Over the course of months or years, the stiffness and pain can spread up the spine and into the neck. Pain and tenderness spreading to the ribs, shoulder blades, hips, thighs, and heels is possible as well.
Note that ankylosing spondylitis can present differently at onset in some people. This tends to be the case in women more than men. For example, anecdotally from some women with ankylosing spondylitis that their symptoms started in the neck rather than in the lower back.
Varying levels of fatigue may also result from the inflammation caused by ankylosing spondylitis. The body must expend energy to deal with the inflammation, thus causing fatigue. Also, mild to moderate anemia, which may also result from the inflammation, can contribute to an overall feeling of tiredness.
In a minority of individuals, pain does not start in the lower back, or even the neck, but in a peripheral joint such as the hip, ankle, elbow, knee, heel, or shoulder. This pain is commonly caused by enthesitis, inflammation of the site where a ligament or tendon attaches to bone. Inflammation and pain in peripheral joints is more common in juveniles with ankylosing spondylitis. This can be confusing since, without the immediate presence of back pain, ankylosing spondylitis may look like some other form of arthritis.
Many people with ankylosing spondylitis also experience bowel inflammation, which may be associated with Crohn’s disease or ulcerative colitis.
Ankylosing spondylitis is often accompanied by iritis or uveitis (inflammation of the eyes). About one-third of people with ankylosing spondylitis will experience inflammation of the eye at least once. Signs of iritis or uveitis are: Eye(s) becoming painful, watery, and red, blurred vision, and sensitivity to bright light.
Ankylosing spondylitis diagnosis
A rheumatologist is commonly the physician who will diagnose ankylosing spondylitis, since they are doctors who are specially trained in diagnosing and treating disorders that affect the joints, muscles, tendons, ligaments, connective tissue, and bones. A thorough physical exam, including X-rays, individual medical history, and a family history of ankylosing spondylitis, as well as blood work (including a test for HLA-B27) are factors in making a diagnosis.
Note that ankylosing spondylitis can present differently at onset in some people. This tends to be the case in women more than men.
The following clinical features are taken into account when making an ankylosing spondylitis diagnosis:
- Onset is usually under 45 years of age.
- Pain persists for more than three months (i.e., it is chronic).
- Back pain and stiffness worsen with immobility, especially at night and early morning.
- Back pain and stiffness tend to ease with physical activity and exercise.
Varying levels of fatigue may also result from the inflammation caused by ankylosing spondylitis. The body must expend energy to deal with the inflammation, thus causing fatigue. Also, mild to moderate anemia, which may also result from the inflammation, can contribute to an overall feeling of tiredness.
The hallmark of ankylosing spondylitis is involvement of the sacroiliac (SI) joints. Some physicians still rely on X-ray to show erosion typical of sacroiliitis, which is inflammation of the sacroiliac joints. Using conventional X-rays to detect this involvement can be problematic because it can take seven to 10 years of disease progression for the changes in the sacroiliac joints to be serious enough to show up on conventional X-rays.
Another option is to use MRI to check for SI involvement, but MRI can be cost prohibitive in some cases.
Ankylosing spondylitis test
There are no specific lab tests to identify ankylosing spondylitis. Certain blood tests can check for markers of inflammation, but inflammation can be caused by many different health problems. Furthermore, elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are common indicators of inflammation, are not present in all ankylosing spondylitis patients and, when they are, it can be from other causes such as anemia, infection, or cancer. For example, it is estimated that less than 70 percent of people with ankylosing spondylitis have a raised ESR level.
Your blood can be tested for the HLA-B27 gene, but most people who have that gene don’t have ankylosing spondylitis, and fewer black people with the disease have the gene than do white people. HLA-B27 is a perfectly normal gene found in 8 percent of the Caucasian population. Generally speaking, no more than 2 percent of people born with this gene will eventually develop ankylosing spondylitis.
It is important to note that the HLA-B27 test is not a diagnostic test for ankylosing spondylitis. Also, the association between ankylosing spondylitis and HLA-B27 varies among different ethnic and racial groups. It can be a very strong indicator in that more than 95 percent of people in the Caucasian population who have ankylosing spondylitis test positive for HLA-B27. However, close to 80 percent of ankylosing spondylitis patients from Mediterranean countries and only 50 percent of African American patients with ankylosing spondylitis are HLA-B27 positive.
Since there is no single blood test for ankylosing spondylitis, laboratory work may, or may not, be of help. Elevated erythrocyte sedimentation rate (ESR), also known as SED rate, and C-reactive protein (CRP) are common indicators of inflammation. Elevated levels of these markers, however, are not present in all ankylosing spondylitis patients and, when they are, it can be from other causes such as anemia, infection, or cancer. For example, it is estimated that less than 70 percent of people with ankylosing spondylitis have a raised ESR level.
Finally, there is no association between ankylosing spondylitis and rheumatoid factor (associated with rheumatoid arthritis) and antinuclear antibodies (associated with lupus.)
Confirming ankylosing spondylitis
The hallmark of ankylosing spondylitis is involvement of the sacroiliac (SI) joints. Some physicians still rely on X-ray to show erosion typical of sacroiliitis, which is inflammation of the sacroiliac joints. Using conventional X-rays to detect this involvement can be problematic because it can take seven to 10 years of disease progression for the changes in the SI joints to be serious enough to show up on conventional X-rays.
Another option is to use MRI to check for SI involvement, but MRI can be cost prohibitive in some cases.
Although scans can sometimes show spinal inflammation and fusing of the spine (ankylosis), damage to the spine can’t always be picked up in the early stages of ankylosing spondylitis.
This is why diagnosis is often difficult. In many cases confirming a diagnosis is a long process that can take years.
A diagnosis of ankylosing spondylitis can usually be confirmed if an X-ray shows inflammation of the sacroiliac joints (sacroiliitis) and you have at least one of the following:
- at least three months of lower back pain that gets better with exercise and doesn’t improve with rest
- limited movement in your lower back (lumbar spine)
- limited chest expansion compared with what is expected for your age and sex
If you have all three of these features but don’t have sacroiliitis – or if you only have sacroiliitis – you’ll be diagnosed with probable ankylosing spondylitis.
Ankylosing spondylitis treatment
The aim of treatment is to reduce pain and stiffness, and prevent or delay spinal deformity or other complications. If you have ankylosing spondylitis, your doctor may suggest that you try physiotherapy, including different types of exercise to strengthen your back, encourage movement in the spine and reduce pain.
You may also be prescribed anti-inflammatories or other types of medications to relieve inflammation, pain and stiffness. Surgery may be recommended to replace or remove joints or thickened bone. However, most people with ankylosing spondylitis don’t need surgery.
The course of your condition can change over time, and you might have painful episodes (relapses) and periods of less pain (remissions) throughout your life. But most people are able to live productive lives despite a diagnosis of ankylosing spondylitis.
You might want to join an online or in-person support group of people with this condition, to share experiences and support.
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) — such as naproxen (Naprosyn) and indomethacin (Indocin) — are the medications doctors most commonly use to treat ankylosing spondylitis. They can relieve your inflammation, pain and stiffness. However, these medications might cause gastrointestinal bleeding.
If NSAIDs aren’t helpful, your doctor might suggest starting a biologic medication, such as a tumor necrosis factor (TNF) blocker or an interleukin 17 (IL-17) inhibitor. TNF blockers target a cell protein that causes inflammation in the body. IL-17 plays a role in your body’s defense against infection and also has a role in inflammation.
Tumor necrosis factor (TNF) blockers help reduce pain, stiffness, and tender or swollen joints. They are administered by injecting the medication under the skin or through an intravenous line.
The five TNF blockers approved by the Food & Drug Administration to treat ankylosing spondylitis are:
- Adalimumab (Humira)
- Certolizumab pegol (Cimzia)
- Etanercept (Enbrel)
- Golimumab (Simponi; Simponi Aria)
- Infliximab (Remicade)
Secukinumab (Cosentyx) is the first IL-17 inhibitor approved by the FDA for the treatment of ankylosing spondylitis.
TNF blockers and IL-17 inhibitors can reactivate latent tuberculosis and make you more prone to infection.
Ankylosing spondylitis exercise
Physical therapy is an important part of treatment and can provide a number of benefits, from pain relief to improved strength and flexibility. A physical therapist can design specific exercises for your needs. Taking regular exercise – 150 minutes of exercise a week can greatly increase your health.
Range-of-motion and stretching exercises can help maintain flexibility in your joints and preserve good posture. Proper sleep and walking positions and abdominal and back exercises can help maintain your upright posture.
Mobility exercises
The mobility section consists of exercises that slowly move the different parts of the spine to the limit of their movement. This is the most important section for keeping the spine mobile. Physical therapist recommend that you do these exercises every day.
Flexibility exercises
These exercises stretch the large muscle groups such as the hamstrings and quadriceps that are anchored around the spine. It is important that these muscles do not shorten or the spine be pulled into wrong positions. We recommend that you do these exercises every day.
Breathing exercises
These exercises are designed to maximize the volume of the chest and lungs. We recommend that you do these every day.
Surgery
Most people with ankylosing spondylitis don’t need surgery. However, your doctor might recommend surgery if you have severe pain or joint damage, or if your hip joint is so damaged that it needs to be replaced.
Ankylosing spondylitis diet
Today, magazine articles and web pages bombard us with claims about special diets, foods, or supplements that can cause or cure arthritis. It is appealing to think that there are simple answers to a complicated disease like ankylosing spondylitis, but unfortunately, most claims for cure-all diets or nutritional supplements have not been scientifically tested to determine if they work and if they are safe. Some are outright frauds, while others have undergone scientific studies that are often incomplete and show that they may be harmful instead of beneficial.
To date, few of these claims have been substantiated by rigorously controlled studies. That said, some people find that certain foods trigger changes in symptoms –– either for the better or the worse. If you find yourself noticing this type of pattern, try keeping a food diary for a few weeks to test if indeed what you eat makes a difference or if you have food sensitivities.
There is, in fact, evidence that certain foods tend to be inflammatory in nature, while others can help manage inflammation.
Whether a person is affected by a chronic illness or not, there are some straightforward guidelines that, if followed, would lead to improved health and well-being for almost everyone:
Both calcium and alcohol affect the strength of the bones, and it is a well-known fact that people with spondylitis are already at higher risk for osteoporosis, a dangerous thinning of the bones that can lead to fractures. Following a diet with adequate amounts of calcium and vitamin D will help reduce the risk of osteoporosis. Consuming more than two alcoholic drinks per day increases a person’s chances of developing weakened bones. In addition, alcohol mixed with certain medications can cause serious side effects to the gastrointestinal tract and major organs such as the liver and the kidneys.
It is important to find out from your doctor whether any medications that you take affect how your body uses what you eat. For instance, some medications cause a person to retain sodium, while others cause potassium loss. Methotrexate can lower folic acid levels, causing a variety of adverse symptoms that can be offset by taking additional supplements.
Experts agree that there are basic guidelines to good nutrition, which are:
- Eat a variety of healthy foods — avoid those that are not.
- Eat plenty of vegetables, fruits, and whole-grain products.
- Use fat (especially saturated fat found in animal products), cholesterol, sugar, and salt in moderation.
- Minimized processed foods, as well as those heavy in artificial preservatives and sweeteners.
- Drink eight to10 glasses of water a day.
- Most people receive daily requirements of vitamins and minerals by eating a well-balanced diet, but others need to take vitamin supplements.
Avoid alcohol or foods that can interact with your medication. Talk with your doctor and/or pharmacist about potential interactions.
Maintaining a Healthy Weight
Besides the well-known medical problems individuals can develop as a result of weight gain (high blood pressure, diabetes, cancer, stroke, and heart disease), extra weight puts additional stress on joints and bones. For example, the corticosteroid prednisone causes weight gain to some degree in nearly all patients who take the medication and can lead to redistribution of body fat to places like the face, back of the neck, and abdomen.
On the other hand, underweight people can suffer from medical problems, ranging from chronic fatigue and anemia to lowered resistance to infection and clinical depression. Inflammation, certain medications, and depression associated with a chronic illness may lessen your appetite or upset your stomach, making it difficult for some people with spondylitis to maintain a healthy weight. This is especially true for those who have spondylitis with inflammatory bowel disease or Crohn’s disease who experience gastrointestinal problems on top of arthritis symptoms. Any severe weight loss to should be reported to your doctor.