Contents
What is atelectasis
Atelectasis is a condition in which one or more areas of your lungs collapse or don’t inflate properly. Lung atelectasis can be a complete or partial collapse of a lung or lobe of a lung. If only a small area or a few small areas of the lungs are affected, you may have no signs or symptoms. If a large area or several large areas of the lungs are affected, they may not be able to deliver enough oxygen to your blood. This can cause symptoms and complications.
Lung atelectasis develops when the tiny air sacs (alveoli) within the lung become deflated. Atelectasis can be a breathing (respiratory) complication after surgery. Almost everyone who has surgery has some atelectasis from anesthesia. Anesthesia changes your regular pattern of breathing and the absorption of gases and pressures, which may combine to cause some degree of collapse of the tiny air sacs (alveoli) in your lungs. Atelectasis is particularly prominent after heart bypass surgery.
Atelectasis is also a possible complication of other respiratory problems, including cystic fibrosis, inhaled foreign objects, lung tumors, fluid in the lung, respiratory weakness and chest injuries.
The amount of lung tissue involved in atelectasis is variable, depending on the cause. Atelectasis can make breathing difficult and lower oxygen particularly if lung disease is already present.
The outlook for atelectasis depends on its cause. In adults, atelectasis often is short term. The collapsed air sacs slowly refill with air once the cause of the atelectasis is resolved.
If atelectasis persists, it may prevent the lung from properly clearing mucus. This can lead to infections (such as pneumonia).
Atelectasis usually isn’t life threatening. However, if it affects a large area of the lungs—especially in a baby, small child, or someone who has another lung disease or illness—it can be fatal if not treated quickly.
Treatment of atelectasis depends on the cause and severity of the collapse.
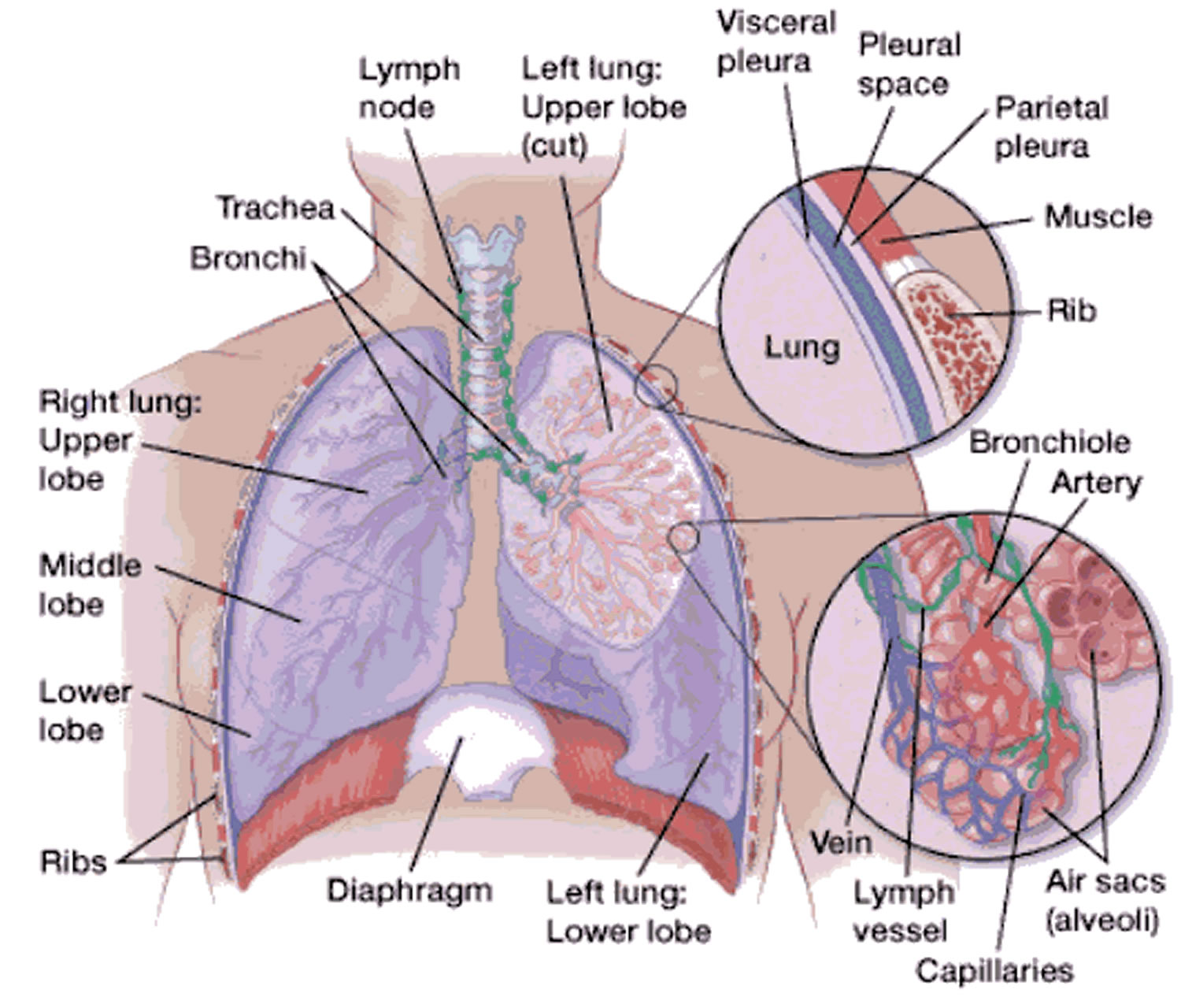
How the Lungs Work
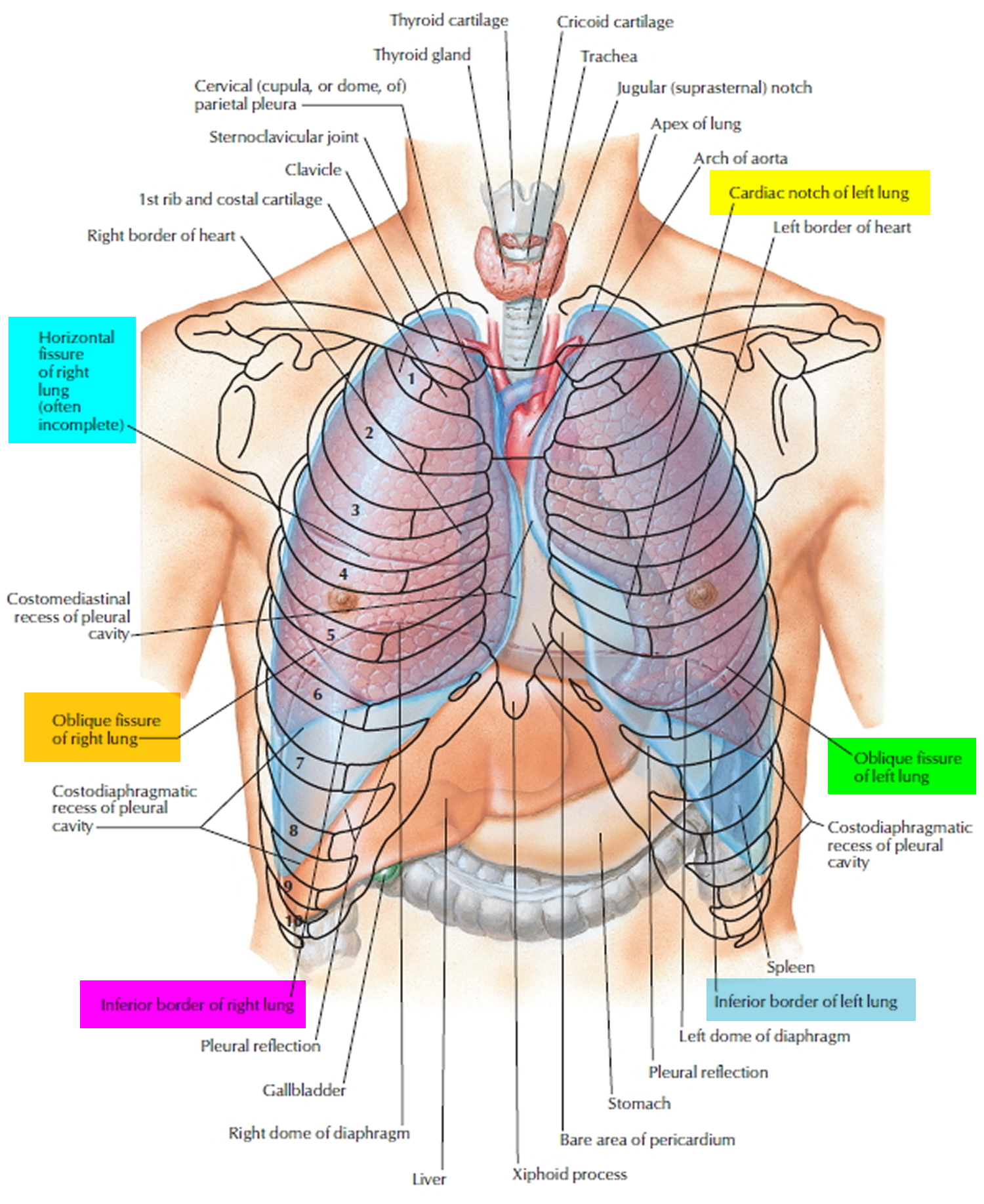
The lungs are soft, spongy, cone-shaped organs in the thoracic (chest) cavity. The lungs consist largely of air tubes and spaces. The balance of the lung tissue, its stroma, is a framework of connective tissue containing many elastic fibers. As a result, the lungs are light, soft, spongy, elastic organs that each weigh only about 0.6 kg (1.25 pounds). The elasticity of healthy lungs helps to reduce the effort of breathing.
Your lungs are organs in your chest that allow your body to take in oxygen from the air. They also help remove carbon dioxide (a waste gas that can be toxic) from your body.
The lungs’ intake of oxygen and removal of carbon dioxide is called gas exchange. Gas exchange is part of breathing. Breathing is a vital function of life; it helps your body work properly.
The left and right lungs are situated in the left and right pleural cavities inside the thoracic cavity. They are separated from each other by the heart and other structures of the mediastinum, which divides the thoracic cavity into two anatomically distinct chambers. As a result, if trauma causes one lung to collapse, the other may remain expanded. Below the lungs, a thin, dome-shaped muscle called the diaphragm separates the chest from the abdomen. When you breathe, the diaphragm moves up and down, forcing air in and out of the lungs. The thoracic cage encloses the rest of the lungs.
Each lung occupies most of the space on its side of the thoracic cavity. A bronchus and some large blood vessels suspend each lung in the cavity. These tubular structures enter the lung on its medial surface.
Parietal refers to a membrane attached to the wall of a cavity; visceral refers to a membrane that is deeper—toward the interior—and covers an internal organ, such as a lung. Within the thoracic (chest) cavity, the compartments that contain the lungs, on either side of the mediastinum, are lined with a membrane called the parietal pleura. A similar membrane, called the visceral pleura, covers each lung.
The parietal and visceral pleural membranes are separated only by a thin film of watery fluid (serous fluid), which they secrete. Although no actual space normally exists between these membranes, the potential space between them is called the pleural cavity.
A thin lining layer called the pleura surrounds the lungs. The pleura protects your lungs and helps them slide back and forth against the chest wall as they expand and contract during breathing. A layer of serous membrane, the visceral pleura, firmly attaches to each lung surface and folds back to become the
parietal pleura. The parietal pleura, in turn, borders part of the mediastinum and lines the inner wall of the thoracic cavity and the superior surface of the diaphragm.
In certain conditions, the pleural cavities may fill with air (pneumothorax), blood (hemothorax), or pus. Air in the pleural cavities, most commonly introduced in a surgical opening of the chest or as a result of a stab or gunshot wound, may cause the lungs to collapse (atelectasis). This collapse of a part of a lung, or rarely an entire lung, is called atelectasis. The goal of treatment is the evacuation of air (or blood) from the pleural space, which allows the lung to reinflate. A small pneumothorax may resolve on its own, but it is oft en necessary to insert a chest tube to assist in evacuation.
The thoracic (chest) cavity is divided by a thick wall called the mediastinum. This is the region between the lungs, extending from the base of the neck to the diaphragm. It is occupied by the heart, the major blood vessels connected to it, the esophagus, the trachea and bronchi, and a gland called the thymus.
Figure 1. Lungs anatomy
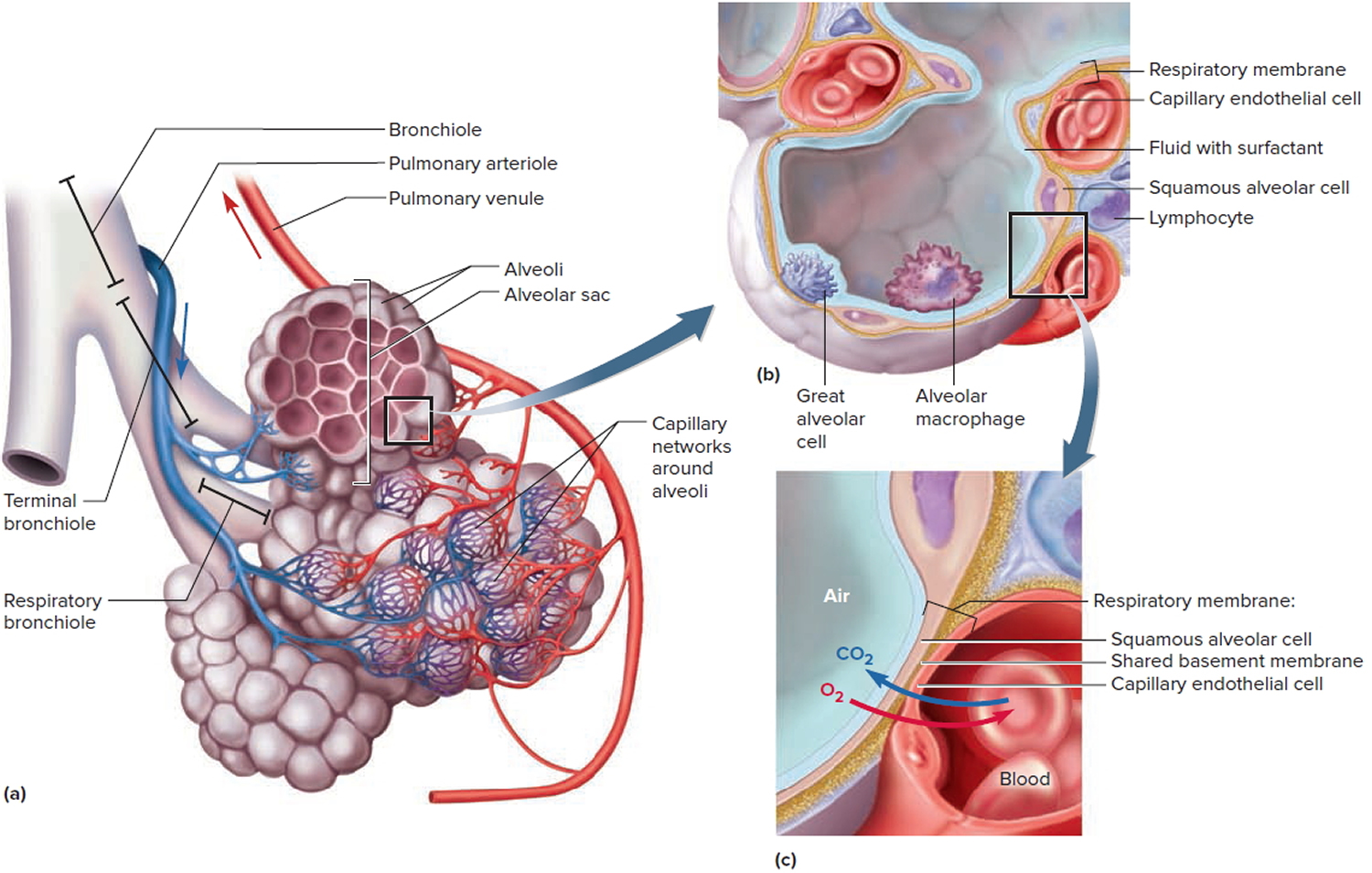
 Lung Alveoli
Lung Alveoli
Each human lung is a spongy mass composed of 150 million little sacs, the alveoli. These provide about 70 m², per lung, of gas-exchange surface—about equal to the floor area of a handball court or a room about 8.4 m (25 ft) square.
An alveolus is a pouch about 0.2 to 0.5 mm in diameter.
When you breathe, air passes through your nose and mouth into your windpipe. The air then travels to your lungs’ air sacs. These sacs are called alveoli.
Small blood vessels called capillaries run through the walls of the air sacs. When air reaches the air sacs, the oxygen in the air passes through the air sac walls into the blood in the capillaries. At the same time, carbon dioxide moves from the capillaries into the air sacs. This process is called gas exchange.
The air sacs must remain open and filled with air for this process to work right. Surfactant, a liquid that coats the inside of the lungs, helps the air sacs stay open. Deep breathing and coughing also help keep the air sacs open. (Coughing helps clear mucus and other substances from your airways.)
In atelectasis, part of the lung collapses or doesn’t inflate. The air sacs in that part of the lung are no longer filled with air. As a result, they can’t take part in gas exchange.
If only a small area or a few small areas of the lungs are affected, you may have no signs or symptoms. This is because the rest of the lung can bring in enough oxygen to make up for the collapsed part of the lung.
If atelectasis affects a large area or several large areas of the lungs, your body’s organs and tissues may not get enough oxygen-rich blood.
Conditions and factors that keep the lungs from properly expanding and filling with air can cause atelectasis. For example, atelectasis is very common after surgery.
The medicine used during surgery to temporarily put you to sleep can decrease or stop your normal effort to breathe and urge to cough. Sometimes, especially after chest or abdominal surgery, pain may keep you from wanting to take deep breaths. As a result, part of your lungs may collapse or not inflate right.
Figure 2. Lungs alveoli
Note: (a) Clusters of alveoli and their blood supply. (b) Structure of an alveolus. (c) Structure of the respiratory membrane.
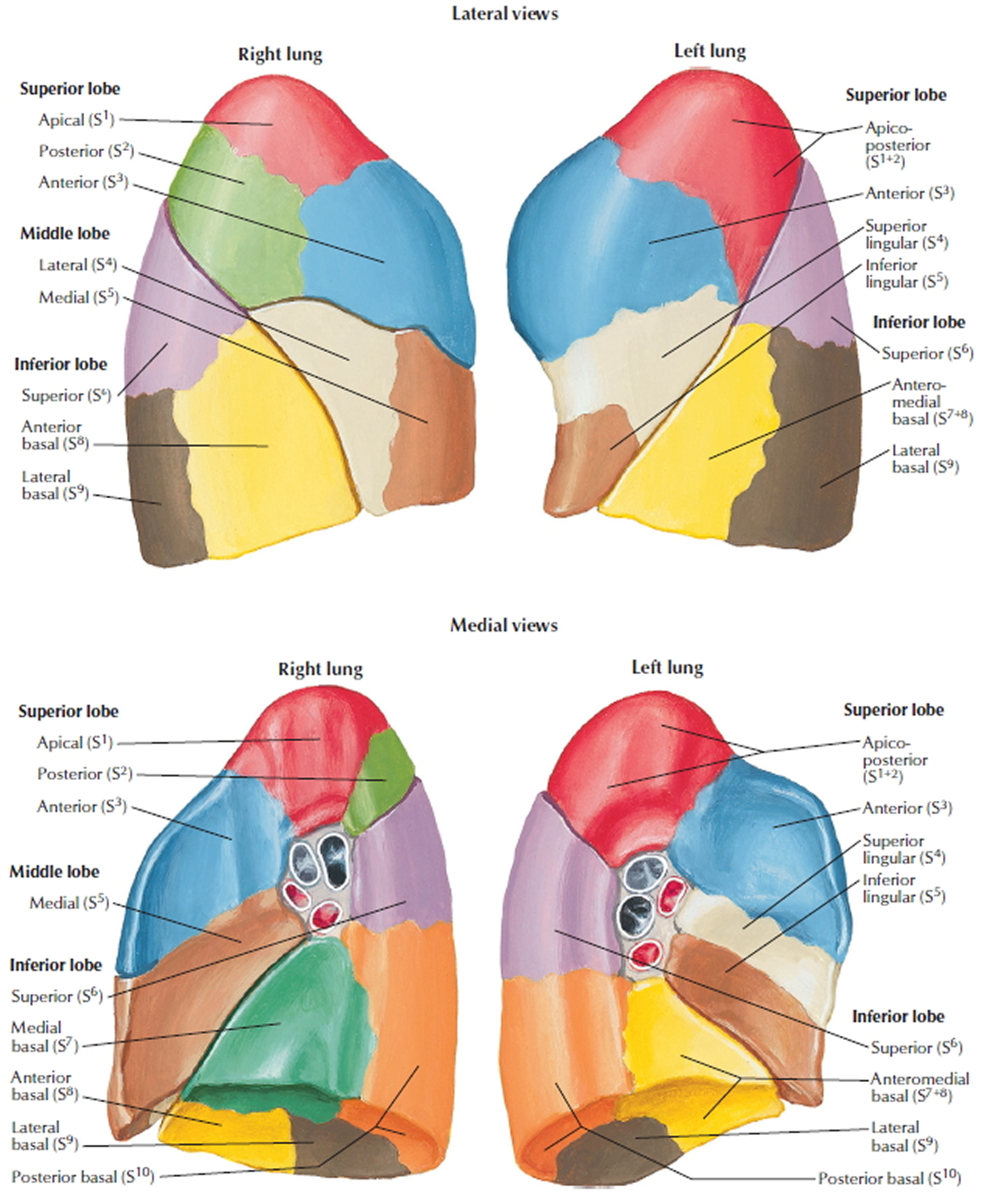
Figure 4. Bronchopulmonary segments
Discoid atelectasis
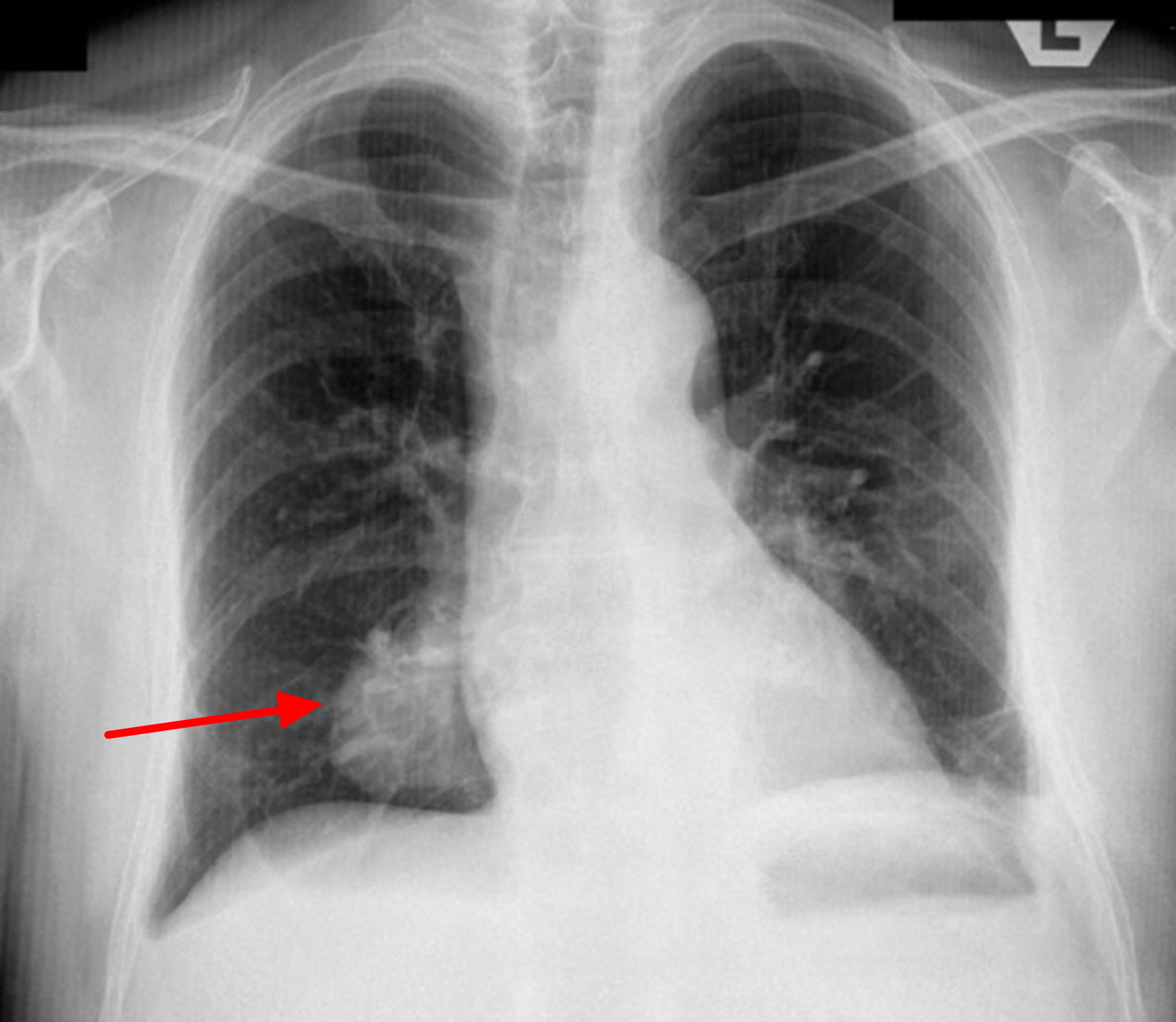
Discoid atelectasis also known as rounded atelectasis or Blesovsky syndrome, represents folded atelectatic lung tissue with fibrous bands and adhesions to the visceral pleura. Incidence is high in asbestos workers (65-70% of cases), most likely due to a high degree of pleural disease. Affected patients typically are asymptomatic, and the mean age at presentation is 60 years. Discoid atelectasis may mimic a neoplastic tumor. The comet tail sign or talon sign is its distinguishing radiographic characteristic.
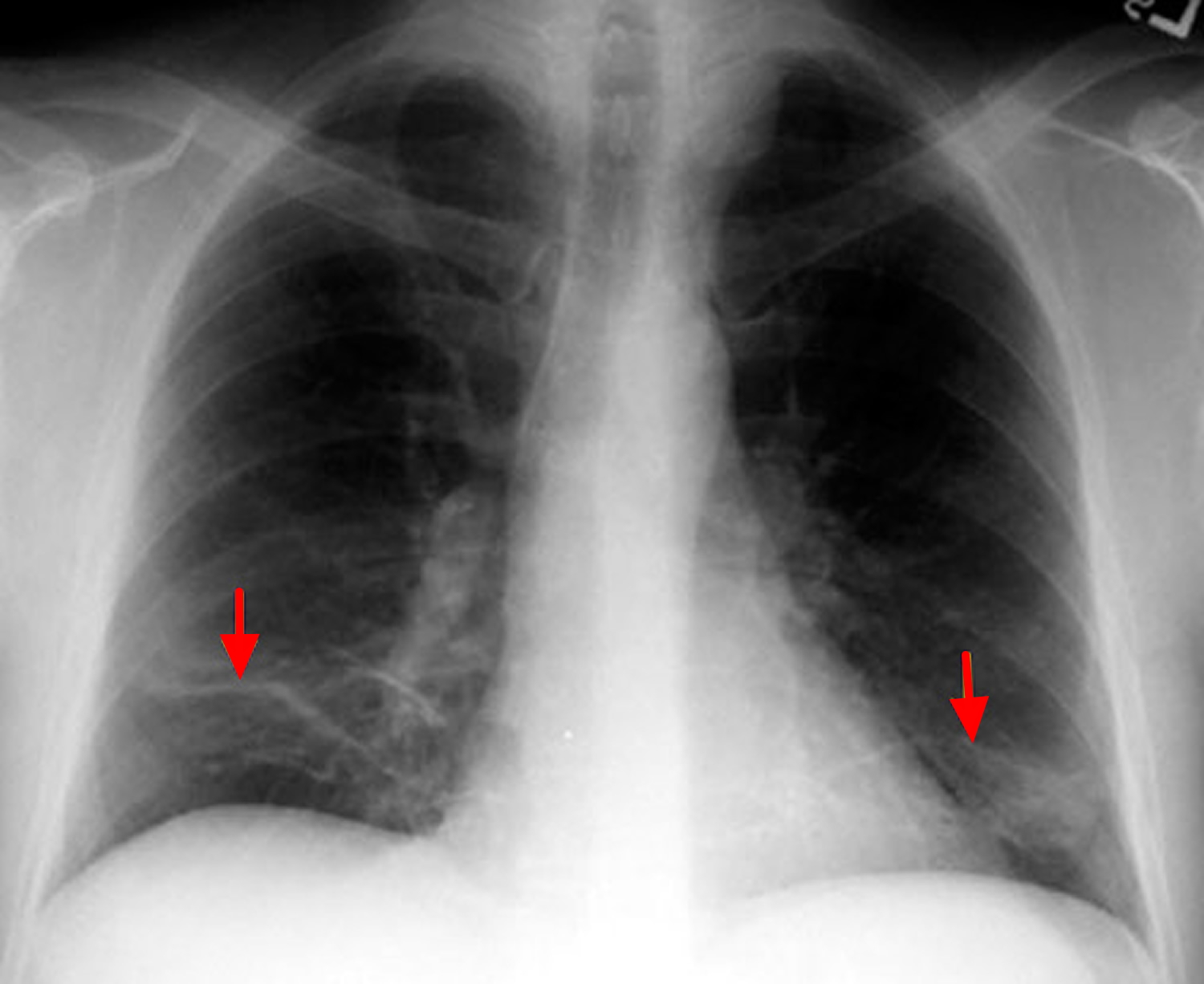
Figure 5. Discoid atelectasis (chest x-ray)
Two theories have been put forward on the pathology of discoid atelectasis. The second theory is more favored while the multi-factorial aetiology suggests both mechanisms probably operate in different patients:
Hanke and Kretzschmar
- underlying pleural effusion causes local atelectasis in the adjacent lung
- a cleft or infolding of the visceral pleura will then form if the rate of pleural fluid formation exceeds alveolar air absorption
- this then causes the lung to tilt on the cleft
- the lung then curls on itself in a concentric fashion
- fibrous adhesions suspending the atelectatic segment (and usually tilt the lung cranially) develop
- as the effusion resorbs, the aerated lung fills in the space between the area of round atelectasis
- organisation of the fibrinous exudate and fibrous contraction lead to additional lung parenchymal distortion
Schneider et al.
- a local pleuritis caused by irritants such as asbestos
- in the event of a benign asbestos-related pleural effusion, the pleura contracts and thickens with shrinkage of the underlying lung, and atelectasis develops in a round configuration
Aetiology 1
- exposure to mineral dust: asbestos, pneumoconiosis
- exudative pleuritis: tuberculosis, haemothorax
- less commonly seen in histoplasmosis, legionella, end-stage renal disease
- sarcoidosis
Associations
It can be associated with:
- asbestos lung exposure: most commonly
- therapeutic pneumothorax in the treatment of tuberculosis 2
- congestive heart failure 3
- pulmonary infarction 3
- parapneumonic effusion
Location: distribution
There may be a predilection towards the lower lobes 4.
Radiographic features
CT scan
- almost always seen adjacent to a pleural surface
- there is associated adjacent pleural thickening
- comet tail sign: produced by the pulling of bronchovascular bundles giving the shape of a comet tail
- crow feet sign
Rounded atelectasis can occasionally increase in size on serial scan 5.
Nuclear medicine
FDG-PET: not metabolically active. May play a role in differentiating from malignancy when there are few or atypical features on chest radiographs and CT scan 6.
Linear atelectasis
Relatively thin, linear densities in the lung bases oriented parallel to the diaphragm (known as Fleischner’s lines).
Figure 6. Linear atelectasis
Figure 7. Bibasilar atelectasis (both lung bases above the diaphragm are collapsed)
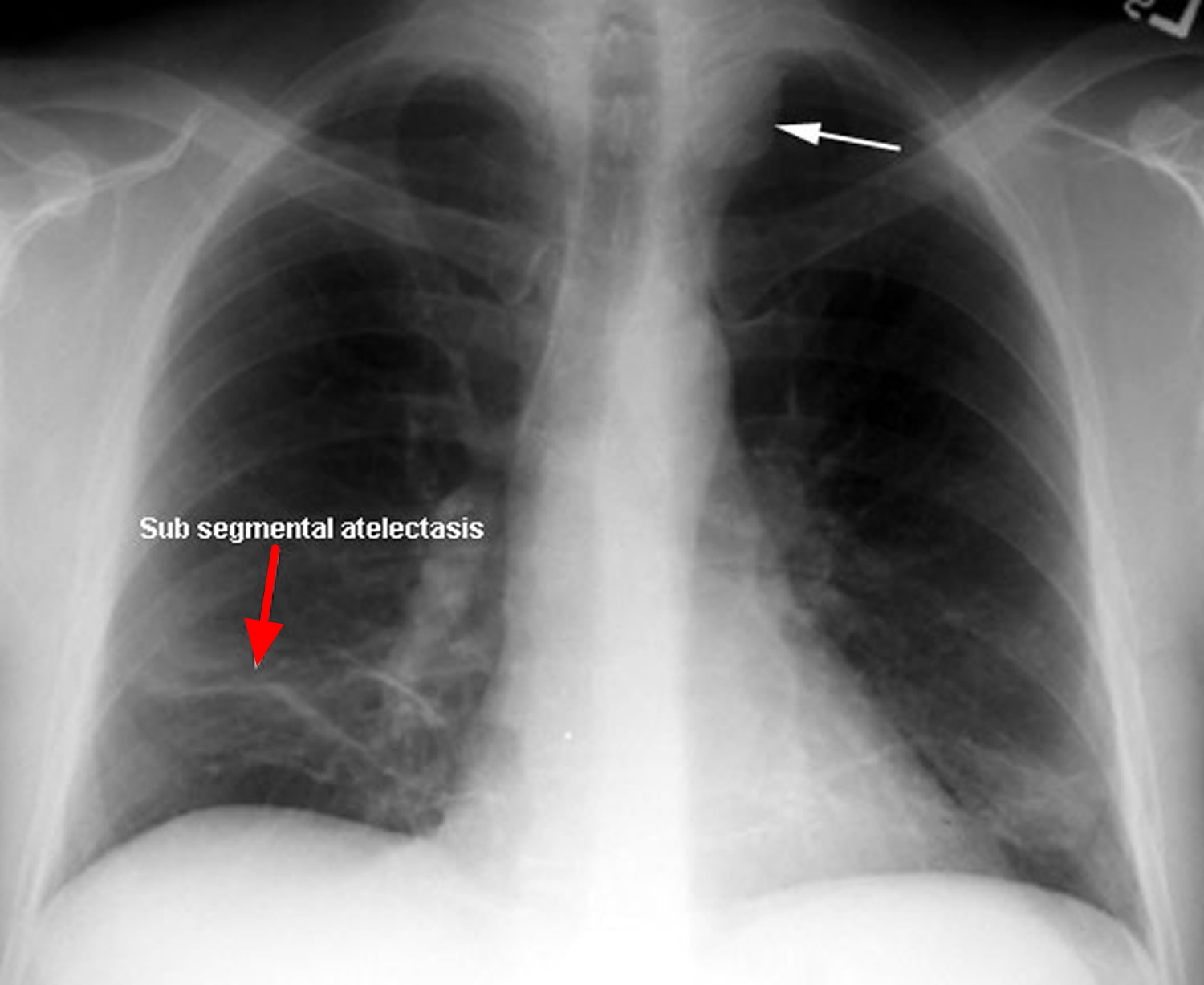
Subsegmental atelectasis
Subsegmental atelectasis refers to collapse of one bronchopulmonary segment of a lung lobe (see Figure 4 above and 8 below). It is a morphological subtype of lung atelectasis. It is better appreciated on CT and its radiographic appearance can range from being a thin linear to a wedge shaped opacity then does not abut an interlobar fissure.
Figure 8. Subsegmental atelectasis
Atelectasis causes
Atelectasis can occur if the lungs can’t fully expand and fill with air. Atelectasis has many causes.
Nonobstructive atelectasis
Nonobstructive atelectasis can be caused by loss of contact between the parietal and visceral pleurae, compression, loss of surfactant, and replacement of parenchymal tissue by scarring or infiltrative disease. Examples of nonobstructive atelectasis are described below.
Conditions and factors that prevent deep breathing and coughing can cause atelectasis. For example, if you’re taking shallow breaths or breathing with the help of a ventilator, your lungs don’t fill with air in the normal way.
Normally, when you take a deep breath, the base (bottom) and the back of your lungs fill with air first. However, if you’re taking shallow breaths or using a ventilator, air may not make it all the way to the air sacs at the bottom of your lungs. Thus, these air sacs won’t inflate properly.
Atelectasis is very common after surgery. The medicine used during surgery to temporarily put you to sleep can decrease or stop your normal effort to breathe and urge to cough. Sometimes, especially after chest or abdominal surgery, pain may keep you from wanting to take deep breaths. As a result, part of your lung may collapse or not inflate right.
Pressure from outside the lungs also may make it hard to take deep breaths. A number of factors can cause pressure outside the lungs. Examples include a tumor, a tight body cast, a bone deformity, or pleural effusion (fluid buildup between the ribs and the lungs).
Lung conditions and other medical disorders that affect your ability to breathe deeply or cough and clear mucus from your lungs also may lead to atelectasis. One example is respiratory distress syndrome.
Respiratory distress syndrome (RDS) is a breathing disorder that affects some newborns. It’s more common in premature infants because their lungs aren’t able to make enough surfactant. Surfactant is a liquid that coats the inside of the lungs and helps keep the air sacs open. Without enough surfactant, part of the lungs may collapse.
Other lung conditions and medical disorders that can cause atelectasis include pneumonia, lung cancer, and neuromuscular diseases. Rarely, asthma, COPD (chronic obstructive pulmonary disease), and cystic fibrosis are associated with atelectasis.
Migrating atelectasis in newborns is rare and may be caused by neuromuscular diseases. “Migrating” means that the part of the lung that collapses will change depending on the position of the baby.
Other possible causes of nonobstructive atelectasis include:
- Injury. Chest trauma — from a fall or car accident, for example — can cause you to avoid taking deep breaths (due to the pain), which can result in compression of your lungs.
- Pleural effusion. This is a buildup of fluid between the tissues (pleura) that line the lungs and the inside of the chest wall.
- Pneumonia. Different types of pneumonia, an infection of your lungs, may temporarily cause atelectasis.
- Pneumothorax. Air leaks into the space between your lungs and chest wall, indirectly causing some or all of a lung to collapse.
- Scarring of lung tissue. Scarring could be caused by injury, lung disease or surgery. In these rare cases, the atelectasis is minor compared with the damage to the lung tissue from the scarring.
- Tumor. A large tumor can press against and deflate the lung, as opposed to blocking the air passages.
Obstructive atelectasis
Obstructive atelectasis or absorption atelectasis, is the most common type and results from reabsorption of gas from the alveoli when communication between the alveoli and the trachea is obstructed. An airway blockage may be due to a foreign object (such as an inhaled peanut), a mucus plug, lung cancer or a poorly placed breathing tube from a ventilator.
Obstructive atelectasis may be caused by:
- Mucus plug. Accumulation of mucus in your airways, often occurring during and after surgery because you can’t cough, is a common cause of atelectasis. Drugs given during surgery make the lungs inflate less fully than usual, so normal secretions collect in the airways. Suctioning the lungs during surgery helps clear away these secretions, but they may continue to build up afterward. Mucus plugs also are common in children, people with cystic fibrosis and during severe asthma attacks.
- Foreign body. Atelectasis is common in children who have inhaled an object, such as a peanut or small toy part, into their lungs.
- Narrowing of major airways from disease. Chronic infections, including fungal infections, tuberculosis and other diseases, can scar and constrict major airways.
- Tumor in a major airway. An abnormal growth can narrow the airway.
- Blood clot. This occurs only if there’s significant bleeding into the lungs that can’t be coughed out.
When a blockage occurs, the air that’s already in the air sacs is absorbed into the bloodstream. New air can’t get past the blockage to refill the air sacs, so the affected area of lung deflates.
Risk Factors for atelectasis
You might be at risk for atelectasis if you can’t take deep breaths or cough, or if you have an airway blockage.
Conditions that can increase your risk for atelectasis include:
- Surgery in which you’re given medicine to make you sleep (general anesthesia). This medicine can decrease or stop your normal effort to breathe and urge to cough.
- Use of a breathing tube
- Any condition or factor that causes pain when you breathe. Examples include surgery on your chest or abdomen, trauma, broken ribs, or pleurisy (inflammation of the membrane that surrounds your lungs and lines your chest cavity).
- Being on a ventilator (a machine that supports breathing).
- A blockage in your airway due to a foreign object, a mucus plug, lung cancer, or a poorly placed breathing tube.
- Lung conditions and other medical disorders that affect your ability to breathe deeply or cough. Examples include respiratory distress syndrome, pneumonia, lung cancer, and neuromuscular diseases. Rarely, asthma, COPD (chronic obstructive pulmonary disease), and cystic fibrosis are associated with atelectasis.
- Age — being younger than 3 or older than 60 years of age.
- Confinement to bed with infrequent changes of position.
- Impaired swallowing function, particularly in older adults — aspirating secretions into the lungs is a major source of infections.
- Lung disease, such as asthma in children, COPD, bronchiectasis or cystic fibrosis.
- Pressure on the lung caused by a buildup of fluid between the ribs and the lungs (called a pleural effusion)
- Premature birth.
- Recent abdominal or chest surgery.
- Respiratory muscle weakness, due to muscular dystrophy, spinal cord injury or another neuromuscular condition.
- Any cause of shallow breathing — including medications and their side effects, or mechanical limitations, such as abdominal pain or rib fracture, for example.
People who have one of the conditions above and who smoke or are obese are at greater risk for atelectasis than people who don’t smoke or aren’t obese.
Infants and toddlers (birth to 3 years old) who have risk factors for atelectasis seem to develop the condition more easily than adults.
Atelectasis prevention
Not smoking before surgery can lower your risk of atelectasis. If you smoke, ask your doctor how far in advance of your surgery you should quit smoking.
After surgery, your doctor may recommend that you take the following steps to fully expand your lungs:
- Perform deep breathing exercises. These exercises are very important after surgery. While in the hospital, you may use a device called an incentive spirometer. This device measures how much air you’re breathing in and how fast you’re breathing in. Using this device encourages you to breathe deeply and slowly.
- Change your position. Sit up or walk around as soon as possible after surgery (with your doctor’s permission).
- Make an effort to cough. Coughing helps clear mucus and other substances from your airways.
- Atelectasis in children is often caused by a blockage in the airway. To decrease atelectasis risk, keep small objects out of reach of children.
If deep breathing is painful, your doctor may prescribe medicines to control the pain. This can make it easier for you to take deep breaths and fully expand your lungs.
Your doctor also might suggest using positive end-expiratory pressure (PEEP) or continuous positive airway pressure (CPAP). Both devices use mild air pressure to help keep the airways and air sacs open.
Atelectasis prognosis (outlook)
In an adult, atelectasis in a small area of the lung is usually not life threatening. The rest of the lung can make up for the collapsed area, bringing in enough oxygen for the body to function.
Large areas of atelectasis may be life threatening, often in a baby or small child, or in someone who has another lung disease or illness.
The collapsed lung usually reinflates slowly if the airway blockage has been removed. Scarring or damage may remain.
The outlook depends on the underlying disease. For example, people with extensive cancer often don’t do well, while those with simple atelectasis after surgery have a very good outcome.
Atelectasis symptoms
Atelectasis likely won’t cause signs or symptoms if it only affects a small area of lung.
If atelectasis affects a large area of lung, especially if it occurs suddenly, it may cause a low level of oxygen in your blood. As a result, you may feel short of breath. Your heart rate and breathing rate may increase, and your skin and lips may turn blue.
If you do have signs and symptoms, they may include:
- Difficulty breathing (dyspnea)
- Rapid, shallow breathing
- Coughing
Other symptoms might be related to the underlying cause of the atelectasis (for example, chest pain due to surgery).
If your child has atelectasis, you may notice that he or she seems agitated, anxious, or scared.
Atelectasis complications
The following complications may result from atelectasis:
- Low blood oxygen (hypoxemia). Atelectasis hampers your lungs’ ability to get oxygen to the alveoli.
- Pneumonia. You’re at greater risk of developing pneumonia until the atelectasis has been cleared. Mucus in a collapsed lung may lead to infection.
- Respiratory failure. A small area of atelectasis, especially in an adult, usually is treatable. But loss of a lobe or a whole lung, particularly in an infant or in someone with lung disease, can be life-threatening.
Atelectasis diagnosis
Your doctor will diagnose atelectasis based on your signs and symptoms and the results from tests and procedures.
Oximetry. This simple test uses a small device placed on one of your fingers to measure the oxygen saturation in your blood.Atelectasis might be detected as a result of a chest x ray done for an underlying lung condition.
Atelectasis usually is diagnosed by a radiologist, pulmonologist (lung specialist), emergency medicine physician, or a primary care doctor (such as a pediatrician, internal medicine specialist, or family practitioner).
Diagnostic Tests and Procedures
The most common test used to diagnose atelectasis is a chest x ray. A chest x ray is a painless test that creates pictures of the structures inside your chest, such as your heart, lungs, and blood vessels.
Your doctor also may recommend a chest computed tomography scan, or chest CT scan. This test creates precise pictures of the structures in your chest. A chest CT scan is a type of x ray. However, the pictures from a chest CT scan show more details than pictures from a standard chest x ray.
Atelectasis often resolves without treatment. If the condition is severe or lasts a long time and your doctor thinks it’s caused by an airway blockage, he or she may use bronchoscopy. This procedure is used to look inside your airway.
During the procedure, your doctor passes a thin, flexible tube called a bronchoscope through your nose (or sometimes your mouth), down your throat, and into your airway. If you have a breathing tube, the bronchoscope can be passed through the tube to your airway.
A light and small camera on the bronchoscope allow your doctor to see inside your airway. Your doctor also can remove blockages during the procedure.
Atelectasis treatment
The main goals of treating atelectasis are to treat the cause of the condition and to reexpand the collapsed lung tissue. Treatment may vary based on the underlying cause of the atelectasis.
Atelectasis Caused by Surgery
If atelectasis is caused by surgery, your doctor may recommend that you take the following steps to fully expand your lungs:
- Perform deep breathing exercises. This is very important after surgery. While in the hospital, you may use a device called an incentive spirometer. This device measures how much air you’re breathing in and how fast you’re breathing in. Using this device encourages you to breathe in deeply and slowly.
- Change your position. Sit up or walk around as soon as possible after surgery with your doctor’s permission.
- Make an effort to cough. Coughing helps clear mucus and other substances from your airways.
Your doctor also may suggest using positive end-expiratory pressure (PEEP) or continuous positive airway pressure (CPAP). Both devices use mild air pressure to help keep the airways and air sacs open.
Chest physiotherapy
Techniques that help people breathe deeply after surgery to re-expand collapsed lung tissue are very important. These techniques are best learned before surgery.
They include:
- Coughing.
- Clapping (percussion) on your chest over the collapsed area to loosen mucus. You can also use mechanical mucus-clearance devices, such as an air-pulse vibrator vest or a hand-held instrument.
- Performing deep-breathing exercises (incentive spirometry) and using a device to assist with deep coughing may be helpful.
- Positioning your body so that your head is lower than your chest (postural drainage). This allows mucus to drain better from the bottom of your lungs.
Supplemental oxygen can help relieve shortness of breath.
Atelectasis Caused by Pressure From Outside the Lungs
If pressure from outside the lungs causes atelectasis, your doctor will treat the cause of the pressure. For example, if the cause is a tumor or fluid buildup, your doctor will remove the tumor or fluid. This will allow your lung to fully expand.
Atelectasis Caused by a Blockage
If a blockage causes atelectasis, you’ll receive treatment to remove the blockage or relieve it. If the blockage is from an inhaled object, such as a peanut, your doctor will remove it during bronchoscopy.
If a mucus plug is blocking your airways, your doctor may use suction to remove it. Other treatments also can help clear excess mucus from the lungs, such as:
- Chest clapping or percussion. This treatment involves pounding your chest and back over and over with your hands or a device to loosen the mucus from your lungs so you can cough it up.
- Postural drainage. For this treatment, your bed may be tilted so that your head is lower than your chest. This allows mucus to drain more easily.
- Medicines. Your doctor may prescribe medicines to help open your airways or to loosen mucus.
Atelectasis Caused by a Lung Condition or Other Medical Disorder
If a lung condition or other medical disorder causes atelectasis, your doctor will treat the underlying cause with medicines, procedures, or other therapies.
- Sobocińska M, Sobociński B, Jarzemska A, Serafin Z. Rounded atelectasis of the lung: A pictorial review. Polish journal of radiology. 79: 203-9. doi:10.12659/PJR.889983 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4102604/[↩]
- Mchugh K, Blaquiere RM. CT features of rounded atelectasis. AJR Am J Roentgenol. 1989;153 (2): 257-60. AJR Am J Roentgenol (abstract) https://www.ncbi.nlm.nih.gov/pubmed/2750607[↩]
- Partap VA. The comet tail sign. Radiology. 1999;213 (2): 553-4. http://pubs.rsna.org/doi/full/10.1148/radiology.213.2.r99nv08553[↩][↩]
- Müller NL, Silva CI. Imaging of the chest. (2008) ISBN:141604048X.[↩]
- Silverman SP, Marino PL. Unusual case of enlarging pulmonary mass. Chest. 1987;91 (3): 457-8. https://www.ncbi.nlm.nih.gov/pubmed/3816324[↩]
- McAdams HP, Erasums JJ, Patz EF et-al. 18F. J Comput Assist Tomogr. 1998;22 (4): 601-4. https://www.ncbi.nlm.nih.gov/pubmed/9676452[↩]