Contents
What is avascular necrosis
Avascular necrosis also called osteonecrosis, aseptic necrosis, ischemic necrosis or femoral head necrosis, is the cellular death of the components of bone, including the bone marrow, due to the impairment of the bones own blood supply. Without blood, the bone tissue dies. This causes the bone to collapse. Avascular necrosis may also cause the joints that surround the bone to collapse. If you have avascular necrosis, you may have pain or be limited in your physical activity. Avascular necrosis is most common in the hip and shoulder, but can affect other large joints such as the knee, elbow, wrist and ankle. Avascular necrosis is a component of a number of conditions and usually the epiphysis of long bones, such as the femoral and humeral heads and the femoral condyles, but small bones have also been known to be affected.
Avascular necrosis can develop in any bone, most often in the:
- Thigh bone (femur) – hips.
- Upper arm bone (humerus).
- Knees.
- Shoulders.
- Ankles.
Avascular necrosis most often affects the hips and knees. Less often affected spots are the shoulders, hands and feet. Rarely, avascular necrosis can occur in the jaw. This can result in ulcers (sores) of gum tissue, exposed jaw bone and pain.
Osteonecrosis of the jaw may occur as a rare complication of treatment with medications called bisphosphonates. It mainly occurs in patients who are receiving frequent doses of intravenous bisphosphonates such as zoledronate or pamidronate to treat cancer in the bone. Most often, this problem occurred in people who recently had a dental procedure or had dental disease.
There are no symptoms in the early stages of avascular necrosis. As bone damage worsens, you may experience the following symptoms:
- Pain in the joint that may increase over time and becomes severe if the bone collapses
- Pain that occurs even at rest
- Limited range of motion
- Groin pain, if the hip joint is affected
- Limping, if the condition occurs in the leg
Patients with hip pain due to avascular necrosis often feel pain in the groin. Pain due to hip or knee avascular necrosis is most often worse with weight-bearing or walking.
Anyone can get avascular necrosis, but it is most common in men and people in their 30s, 40s, and 50s. The male-to-female ratio depends on the underlying cause, although primary avascular necrosis is more prevalent in men. The overall male-to-female ratio is 8:1. Most of the 10,000 to 20,000 Americans who develop avascular necrosis each year are between the ages of 20 and 50. Age at onset depends on the underlying cause. Primary avascular necrosis most often occurs during the fourth or fifth decade and is bilateral in 40-80% of cases. On average, women present almost 10 years later than men. These people most often have a history of serious trauma, corticosteroid use, excess alcohol intake or one of the other risk factors listed below. One Japanese survey estimated that 2500-3300 cases of avascular necrosis of the hip occur each year, of which, 34.7% were a result of corticosteroid abuse, 21.8% to alcohol abuse, and 37.1% to idiopathic mechanisms. A French study reported avascular necrosis in 4.3% of allogenic bone marrow transplant recipients.
The natural history of avascular necrosis is directly linked to the size and level of the necrosis. Very small lesions (involvement of less than 15% of the femoral head) may resolve without any further treatment. Conversely, lesions involving greater than 50% of the femoral head progress to collapse, and ultimately require in total hip arthroplasty.
The amount of disability that is resultant in sufferers of avascular necrosis depends on what part of the bone is affected, how large the affected area is, and how effectively the bone is able to rebuild itself. With early diagnosis and proper treatment, most people with avascular necrosis can lead almost normal, productive lives.
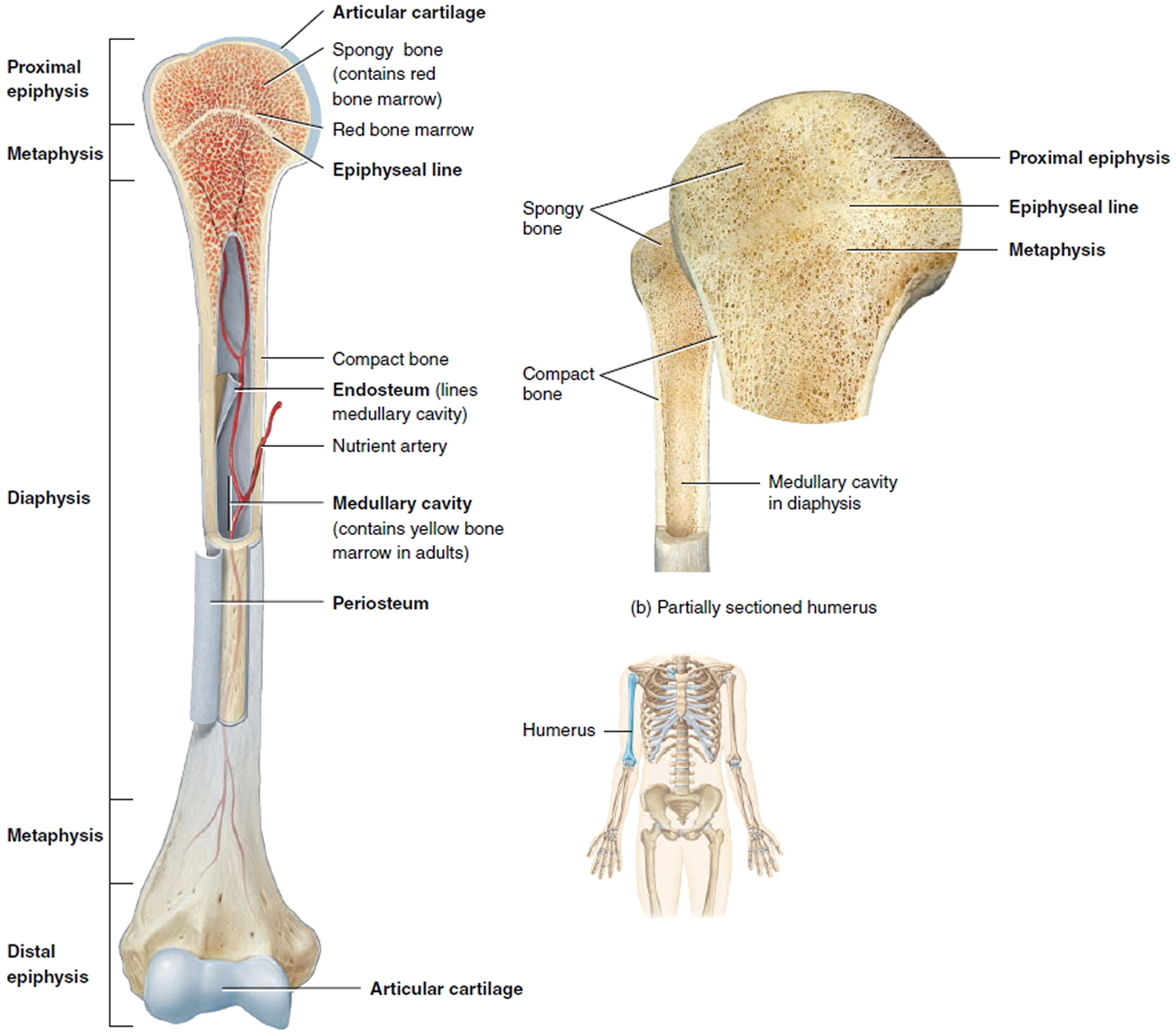
Figure 1. Parts of a long bone
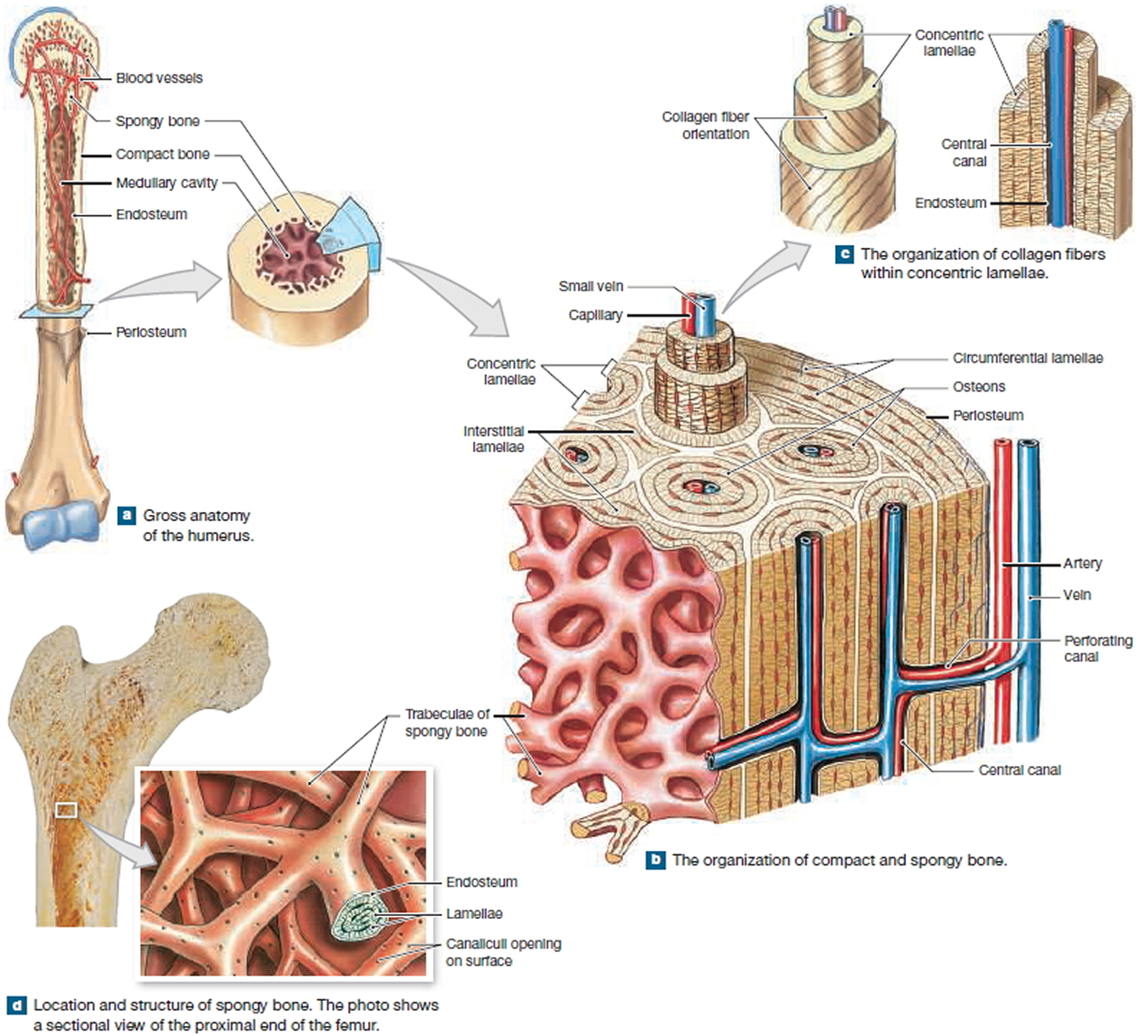
Figure 2. Internal organization of bones
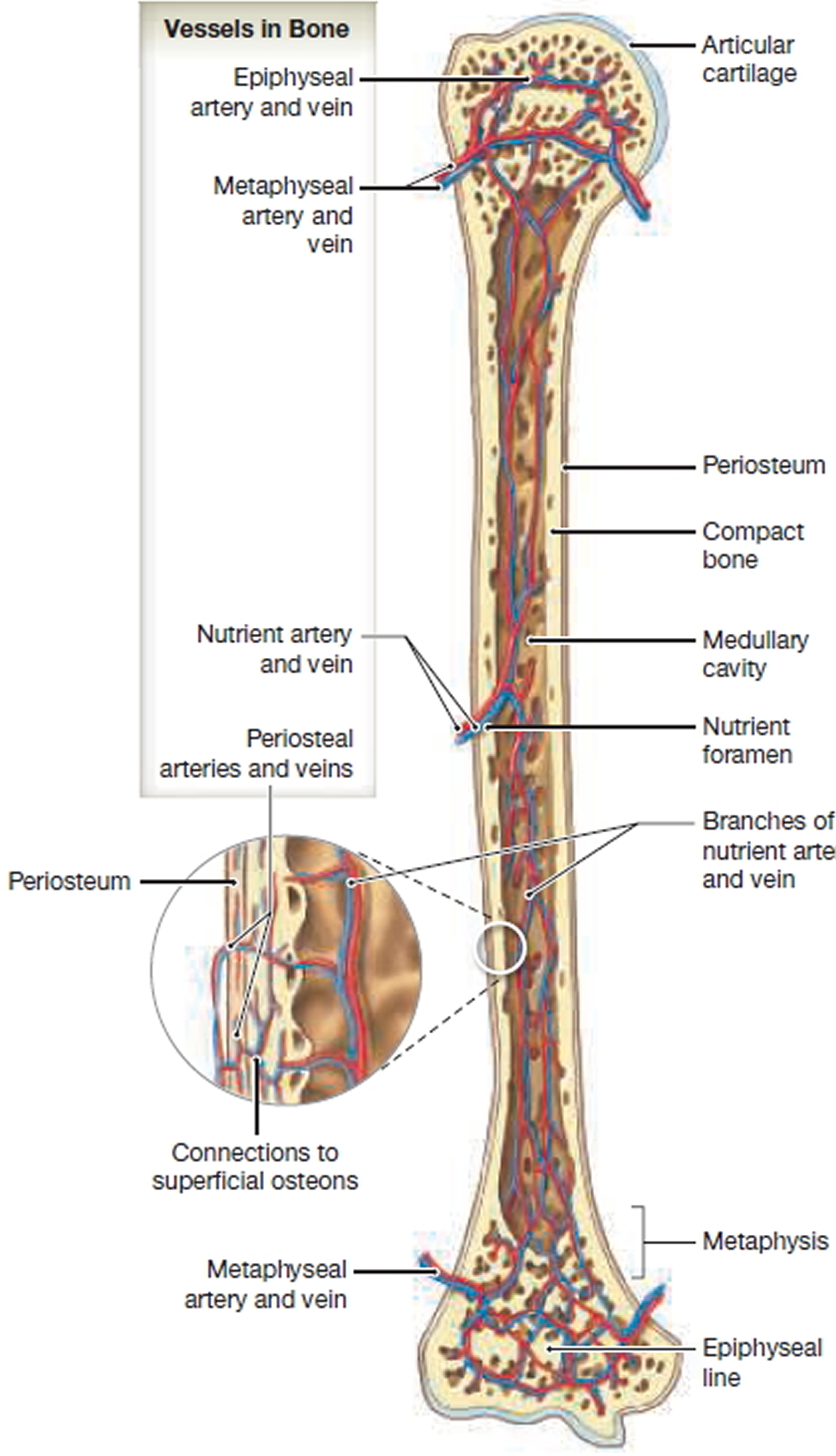
Figure 3. Blood supply to a Mature Bone
Figure 4. Avascular necrosis of knee (MRI image T1)
Avascular necrosis of hip
Avascular necrosis of the femoral head also called osteonecrosis of the femoral head is a series of pathological processes caused by blood supply disorders in part of the femoral head 1. Moya-Angeler et al. 2 reported that the number of patients with avascular necrosis of femoral head is increasing by 200,000-300,000 annually, and that the number of cumulative cases has attained 5-7.5 million in the United States. At the same time, the age of onset tends be earlier. A study by Harvard Medical School showed that the younger the patient, the more easily it is to have total hip replacement overhauling surgery 3. In addition, the high incidence of avascular necrosis of the femoral head is a heavy social and family burden. Therefore, intervention is particularly important before collapse of a necrotic femoral head.
The most common etiology of avascular necrosis of femoral head is use of corticosteroids (51%), followed by use of alcohol (31%) 4. About 5-25% of patients will be attacked by this disease if patients continually use corticosteroids for more than 1 month. Risk increases with the quantity and duration of use. Other possible causes include scuba diving or high-pressure disease, systemic lupus erythematosus and other connective tissue diseases, autoimmune diseases, hyperlipidemia, fat embolism syndrome, and metabolic bone diseases7. However, about 15% of patients exhibit no obvious cause, and thus have what is termed idiopathic osteonecrosis of the femoral head. The best time to treat avascular necrosis of femoral head is at the early stage; a variety of treatments are available before collapse of an osteonecrotic femoral head. However, obvious limitations appear once the head collapses 5. No method has been demonstrated to effectively stop progression of the disease before the femoral head collapses or to postpone progression of osteoarthritis after the femoral head has collapsed. In a study by Wang and colleagues 6 found that the distribution of osteoblastic and osteoclastic activities differs in the different regions of patients with late stage avascular necrosis of femoral head.
Figure 5. Avascular necrosis of femoral head (grade IV avascular necrosis)
Note: Bilaterally reduced joint space with remodelled femoral heads showing areas of sclerosis. Partial collapse of the femoral heads.
Avascular necrosis of hip treatment
The best time to treat avascular necrosis of femoral head is at the early stage; a variety of treatments are available before collapse of an osteonecrotic femoral head. However, obvious limitations appear once the head collapses. No method has been demonstrated to effectively stop progression of the disease before the femoral head collapses or to postpone progression of osteoarthritis after the femoral head has collapsed. In this preliminary study 7 involving 35 hips of men and women (mean age 43 years and body mass index 31 kg/m2) with corticosteroid-induced osteonecrosis, core hip decompression with injection of concentrated bone marrow plus platelet-rich plasma improved pain and function with > 90% of hips in that study were without collapse at a minimum of 2 years.
Avascular necrosis causes
Avascular necrosis occurs when part of the bone does not get blood and dies. After a while, the bone can collapse. If avascular necrosis is not treated, the joint deteriorates, leading to severe arthritis.
Avascular necrosis can be caused by disease or by severe trauma, such as a fracture or dislocation, that affects the blood supply to the bone. Avascular necrosis can also occur without trauma or disease. For about 25 percent of people with avascular necrosis, the cause of interrupted blood flow is unknown – this is called idiopathic — meaning it occurs without any known cause.
The most common causes of avascular necrosis are:
- Serious trauma (injury), which interrupts a bone’s blood supply
- Corticosteroid medications (such as prednisone, cortisone or methylprednisolone), mainly when a high dose is used for a prolonged period of time
- Excess alcohol consumption
- Systemic lupus erythematosus
Other less common risk factors for avascular necrosis include:
- Decompression disease (also called the “Bends” that can occur with scuba diving)
- Blood disorders such as sickle cell anemia, antiphospholipid antibody syndrome (APS) and lupus anticoagulant
- HIV infection (the virus that causes AIDS)
- Radiation therapy
- Bisphosphonates, which may be linked to avascular necrosis of the jaw
- Organ transplants
The following are possible causes of avascular necrosis:
Medicines or Medical Treatments
- Chemotherapy.
- Radiation therapy.
- High-dose steroids.
- Organ transplants.
- HIV drugs
Medical Conditions
- Cancer.
- Lupus.
- HIV/AIDS.
- Gaucher disease (disease in which harmful substance build up in the certain organs and the bone)
- Systemic lupus erythematosus (an autoimmune disease in which the body’s immune system mistakenly attacks healthy tissue such as the bone)
- Legg-Calve-Perthes disease (childhood disease in which the thigh bone in the hip doesn’t get enough blood, causing the bone to die)
- Decompression sickness, also know as divers’ disease, the bends, or caisson disease, from a lot of deep sea diving
- Gout.
- Vasculitis.
- Osteoarthritis.
- Osteoporosis.
- Blood disorders, such as sickle cell disease.
- Pancreatitis.
- Diabetes.
Alcohol Use
Excessive alcohol use causes fatty substances to build up in the blood vessels. This can cause a decreased blood supply to the bone, which can lead to avascular necrosis.
Injury
A broken or dislocated bone, or a joint injury, may damage the surrounding blood vessels. This can cause a decreased blood supply to the bone, which can lead to avascular necrosis.
When avascular necrosis occurs in the shoulder joint, it is usually due to long-term treatment with steroids, a history of trauma to the shoulder, or the person has sickle cell disease.
Risk factors for developing avascular necrosis
Risk factors for developing avascular necrosis include:
- Trauma. Injuries, such as hip dislocation or fracture, can damage nearby blood vessels and reduce blood flow to bones.
- Steroid use. High-dose use of corticosteroids, such as prednisone, is the most common cause of avascular necrosis that isn’t related to trauma. The exact reason is unknown, but one hypothesis is that corticosteroids can increase lipid levels in your blood, reducing blood flow and leading to avascular necrosis.
- Excessive alcohol use. Consuming several alcoholic drinks a day for several years also can cause fatty deposits to form in your blood vessels.
- Bisphosphonate use. Long-term use of medications to increase bone density may be a risk factor for developing osteonecrosis of the jaw. This complication has occurred in some people treated with these medications for cancers, such as multiple myeloma and metastatic breast cancer. The risk appears to be lower for women treated with bisphosphonates for osteoporosis.
- Certain medical treatments. Radiation therapy for cancer can weaken bone. Organ transplantation, especially kidney transplant, also is associated with avascular necrosis.
Avascular necrosis prevention
Many cases of avascular necrosis do not have a known cause, so prevention may not be possible. In some cases, you can reduce your risk by doing the following:
- Avoid drinking excessive amounts of alcohol.
- When possible, avoid high doses and long-term use of corticosteroids.
- Monitor steroid use. Make sure your doctor knows about any past or present use of high-dose steroids. Steroid-related bone damage appears to worsen with repeated courses of high-dose steroids.
- Follow safety measures when diving to avoid decompression sickness.
- Keep cholesterol levels low. Tiny bits of fat are the most common substance blocking blood supply to bones.
The key ways to prevent avascular necrosis are to avoid too much alcohol intake and avoid tobacco use, as smoking also raises the risk of avascular necrosis. Also, if you have to take corticosteroids, such as prednisone, work with your doctor to take the smallest dose for the shortest time possible that will control your symptoms.
Prevent avascular necrosis of the jaw with good dental hygiene. If you need any dental work, complete that before starting bisphosphonate treatment or as soon afterward as possible. See your dentist right away if you have any sign of dental infection (jaw pain or pain, swelling or redness of the gums).
Avascular necrosis outlook (prognosis)
How well you do depends on the following:
- The cause of the avascular necrosis
- How severe the disease is when diagnosed
- Amount of bone involved
- Your age and overall health
Outcome may vary from complete healing to permanent damage in the affected bone. Some people will develop osteoarthritis (also called degenerative arthritis or “wear and tear” of the joints) as a result of avascular necrosis. Working with a physical therapist on an exercise program may be helpful in treating the pain and stiffness from osteoarthritis.
Avascular necrosis possible complications
Advanced avascular necrosis can lead to osteoarthritis and permanent decreased mobility. Severe cases may require joint replacement.
Avascular necrosis signs and symptoms
Avascular necrosis does not always cause symptoms, especially when it first develops. As the disease gets worse, you may feel pain when you put your weight on a joint that is affected by avascular necrosis. Over time, you may feel pain in the joint even when you are resting.
Pain caused by avascular necrosis may be mild or severe. If it causes your bone and joint to collapse, you may have severe pain and not be able to use the joint. For instance, if you have avascular necrosis in the hip, you may not be able to walk. Pain associated with avascular necrosis of the hip may be focused in the groin, thigh or buttock. In addition to the hip, the areas likely to be affected are the shoulder, knee, hand and foot.
Avascular necrosis diagnosis
There is no single test for avascular necrosis. If your doctor suspects you have avascular necrosis, he or she will take your medical history and do a physical exam.
Many disorders can cause joint pain. Imaging tests can help pinpoint the source of pain. Your doctor may also order one or more tests to see which bones are affected. These tests include:
- X-ray.
- Magnetic resonance imaging (MRI).
- Computed tomography (CT) scan.
- Bone scan. A small amount of radioactive material is injected into your vein. This tracer travels to the parts of your bones that are injured or healing and shows up as bright spots on the imaging plate.
- Bone biopsy.
- Measure of the pressure inside the bone.
MRI
MRI is the most sensitive (~95%) modality and demonstrates changes well before plain films changes are visible.
- diffuse edema: Edema is not an early sign; instead, studies show that edema occurs in advanced stages and is directly correlated with pain
- reactive interface line is a focal serpentine low signal line with fatty centre (most common appearance and first sign on MRI)
- double line sign: serpiginous peripheral/outer dark (sclerosis) and inner bright (granulation tissue) on T2WI is diagnostic
- rim sign: osteochondral fragmentation:
- secondary degenerative change
Nuclear medicine
Bone scintigraphy is also quite sensitive (~85%) and is the second option after MRI. It is a choice when multiple sites of involvement must be assessed in patients with risk factors, such as sickle cell disease. The findings are different accordingly to the time of the scan:
- early disease: often represented by a cold area likely representing the vascular interruption
- late disease: may show a “doughnut sign”: a cold spot with surrounding high uptake ring (surrounding hyperaemia and adjacent synovitis)
Avascular necrosis treatment
Most people with avascular necrosis need treatment.
The goals of treatments are to:
- Improve use of the joint.
- Stop further damage.
- Protect bones and joints.
If your provider knows the cause of avascular necrosis, part of the treatment will be aimed at the underlying condition. For example, if a blood clotting disorder is the cause, treatment will consist, in part, of clot-dissolving medicine.
Your treatment options may include surgery or nonsurgical treatments, such as medicines. Your doctor will determine the best treatment for you based on several factors, including:
- Your age.
- The stage of the disease.
- Where and how much bone has avascular necrosis.
- The cause, if known. If the cause is steroid or alcohol use, treatment may not work unless you stop using those substances.
If the condition is caught early, you will take pain relievers and limit use of the affected area. This may include using crutches if your hip, knee, or ankle is affected. You may need to do range-of-motion exercises. Nonsurgical treatment can often slow the progression of avascular necrosis, but most people will need surgery.
Nonsurgical Treatments
Non-surgical treatments do not cure avascular necrosis, but they may help manage the disease. Your doctor may recommend one or more non-surgical treatments, especially if the disease is in its early stages.
Often, treatment starts with pain medications and by limiting weight-bearing (such as walking) on affected areas. This type of conservative treatment may work well for patients with early avascular necrosis in small areas of bone. Yet, it does not work for those with hip or knee avascular necrosis who are facing worsening disease and bone collapse. Instead, these patients may need surgical procedures to relieve pain and try to prevent bone collapse.
Treatment of jaw osteonecrosis: Most cases of osteonecrosis of the jaw improve with conservative treatment. This includes limited debridement (removing dead tissue) and use of antibiotics and medicated mouthwash.
Medications
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to reduce pain and swelling.
- If you have blood-clotting problems, blood thinners may be used to prevent clots that block the blood supply to the bone.
- If you take steroid medicines, cholesterol-lowering drugs may be used to reduce fat in the blood. Reducing the amount of cholesterol and fat in your blood may help prevent the vessel blockages that can cause avascular necrosis.
There is no proven medical therapy for avascular necrosis. Some studies suggest that short-term bisphosphonate treatment may slow, improve or even prevent bone collapse in the hip and knee.
Taking Weight Off the Joint
Your doctor may suggest you limit your activity or use crutches to take weight off joints with avascular necrosis. This may slow bone damage and allow some healing. If combined with NSAIDs, it may help you avoid or delay surgery.
Range-of-Motion Exercises
Your doctor may recommend you exercise the joints with avascular necrosis to help improve their range of motion.
Electrical Stimulation
Your doctor may recommend electrical stimulation therapy to help bone growth. Electrical stimulation can be used during surgery and applied directly to the damaged area. Or it can be administered through electrodes attached to your skin.
Surgery
Most people with avascular necrosis eventually need surgery as the disease worsens. Some people with early stage disease may need surgery if non-surgical treatments do not help.
Surgical options include:
- A bone graft
- A bone graft along with its blood supply (vascularized bone graft)
- Cutting the bone and changing its alignment to relieve stress on the bone or joint (osteotomy)
- Total joint replacement, which replaces the joint with a man-made one.
- Removing part of the inside of the bone (core decompression) to relieve pressure and allow new blood vessels to form and this increases blood flow to the bone.
- Regenerative medicine treatment. Bone marrow aspirate and concentration is a novel procedure that in the future might be appropriate for early stage avascular necrosis of the hip. Stem cells are harvested from your bone marrow. During surgery a core of dead hip bone is removed and stem cells inserted in its place, potentially allowing for growth of new bone.
- Gou WL, Lu Q, Wang X, Wang Y, Peng J, Lu SB. Key pathway to prevent the collapse of femoral head in osteonecrosis. European review for medical and pharmacological sciences. 2015;19:2766–74. https://www.ncbi.nlm.nih.gov/pubmed/26241528[↩]
- Tripathy SK, Goyal T, Sen RK. Management of femoral head osteonecrosis: Current concepts. Indian journal of orthopaedics. 2015;49:28–45. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4292325/[↩]
- Wright EA, Katz JN, Baron JA, Wright RJ, Malchau H, Mahomed N. et al. Risk factors for revision of primary total hip replacement: results from a national case-control study. Arthritis care & research. 2012;64:1879–85. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3510659/[↩]
- van der Jagt D, Mokete L, Pietrzak J, Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. The Journal of the American Academy of Orthopaedic Surgeons. 2015;23:69–70. https://www.ncbi.nlm.nih.gov/pubmed/25624358[↩]
- Okazaki S, Nagoya S, Tateda K, Katada R, Mizuo K, Watanabe S. et al. Weight bearing does not contribute to the development of osteonecrosis of the femoral head. International journal of experimental pathology. 2012;93:458–62. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3521902/[↩]
- Wang C, Meng H, Wang Y, et al. Analysis of early stage osteonecrosis of the human femoral head and the mechanism of femoral head collapse. International Journal of Biological Sciences. 2018;14(2):156-164. doi:10.7150/ijbs.18334. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5821037/[↩]
- Stem Cells Combined With Platelet-rich Plasma Effectively Treat Corticosteroid-induced Osteonecrosis of the Hip: A Prospective Study. Clin Orthop Relat Res. 2018 Feb;476(2):388-397. doi: 10.1007/s11999.0000000000000033. https://www.ncbi.nlm.nih.gov/pubmed/29529674[↩]