Contents
What does blood in urine mean
Blood in the urine, also called hematuria, is common. It might be detected on a urine test, or you might notice it yourself. If you think you might have blood in your urine, see a doctor.
There are two kinds of blood in urine (hematuria):
- Microscopic hematuria or trace of blood in urine, is when blood in the urine is invisible to the naked eye; it only shows up under a microscope. Most people with microscopic hematuria do not have any symptoms. In many cases, microscopic hematuria goes away without causing any problems. In fact, people might never know they have it unless they get a urine test. In many patients with microscopic hematuria, a specific cause or pathology is not found 1.
- Gross hematuria may sound nasty, but it’s usually not — in medicine, “gross” is just a word that describes when something is large or happens in bigger amounts. Gross hematuria just means that enough red blood cells are in a person’s urine to turn it red, pink or brown. Like microscopic hematuria, gross hematuria often clears up on its own with no problems. Sometimes, though, it can be a sign of a more serious condition.
There are many causes, including infections, stones and tumors, however most causes are not serious. If you ever see blood in your urine, don’t panic. Chances are, it’s no big deal. Nevertheless, formal evaluation is critical, because malignancies are detected in up to 5% of patients with microscopic hematuria and in up to 30% to 40% of patients with gross hematuria 2. So make sure to see a doctor. If you need treatment, it’s good to get started right away.
Urinating is one way your body gets rid of waste products. The process starts in the kidneys, which remove excess fluids and waste from the blood and turn them into urine. The urine then flows through tubes called ureters into the bladder, where it’s stored until you pee it out. If blood cells leak into the urine at any part of the process, it causes hematuria.
Researchers have not found that eating, diet, and nutrition play a role in causing or preventing hematuria.
In its 2011 recommendation statement, the U.S. Preventive Services Task Force did not find sufficient evidence for or against screening for bladder cancer in asymptomatic adults 3. Despite this, microscopic hematuria is often found incidentally during routine health screenings, with a prevalence of about 2% to 31% 4.
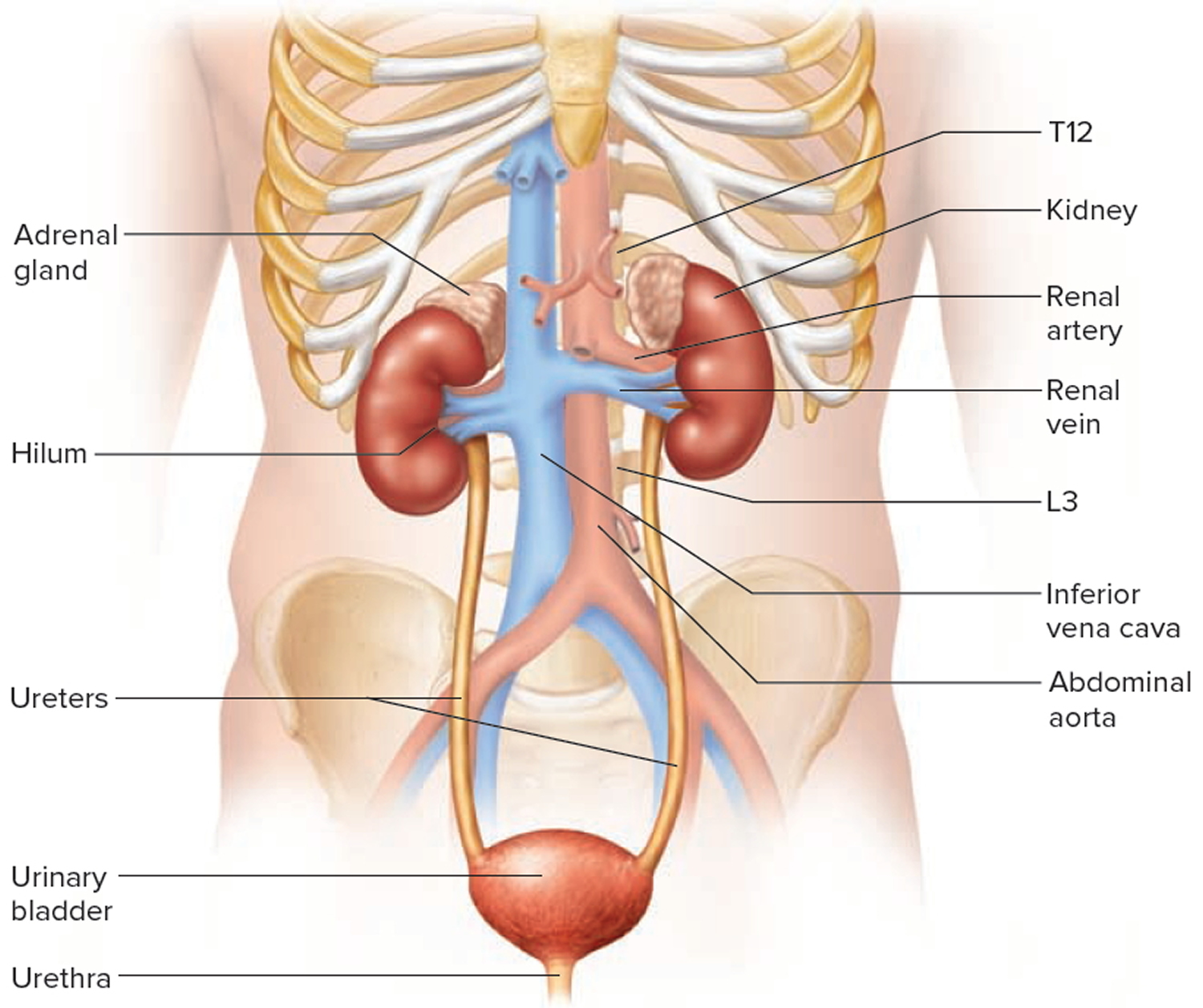
What is the urinary tract?
The urinary tract is the body’s drainage system for removing wastes and extra fluid. The urinary tract includes
- two kidneys
- two ureters
- the bladder
- the urethra
The kidneys are two bean-shaped organs, each about the size of a fist. They are located just below the rib cage, one on each side of the spine. Every day, the kidneys filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine, composed of wastes and extra fluid. Children produce less urine than adults. The urine flows from the kidneys to the bladder through tubes called ureters. The bladder stores urine until releasing it through urination. When the bladder empties, urine flows out of the body through a tube called the urethra at the bottom of the bladder.
Figure 1. Urinary tract anatomy
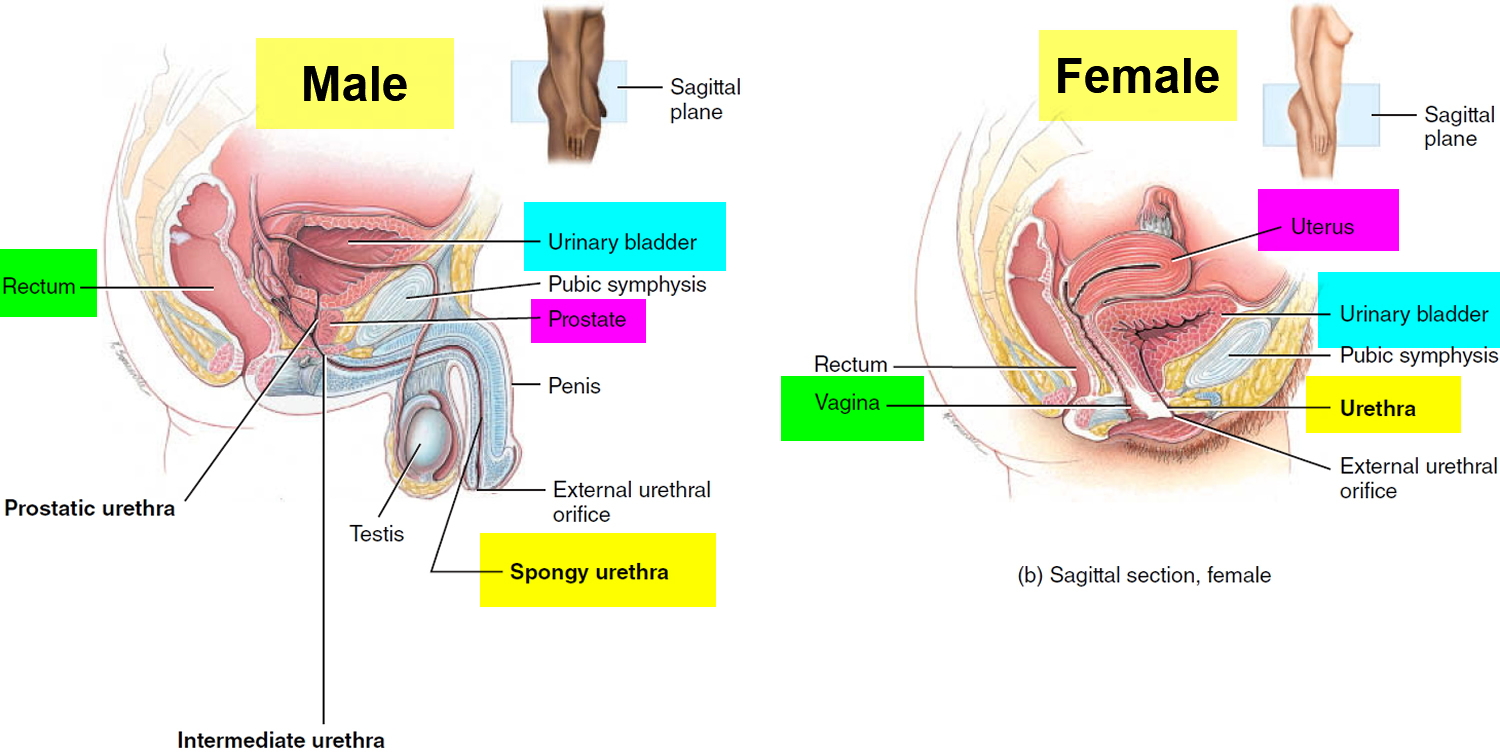
Figure 2. Urinary bladder anatomy
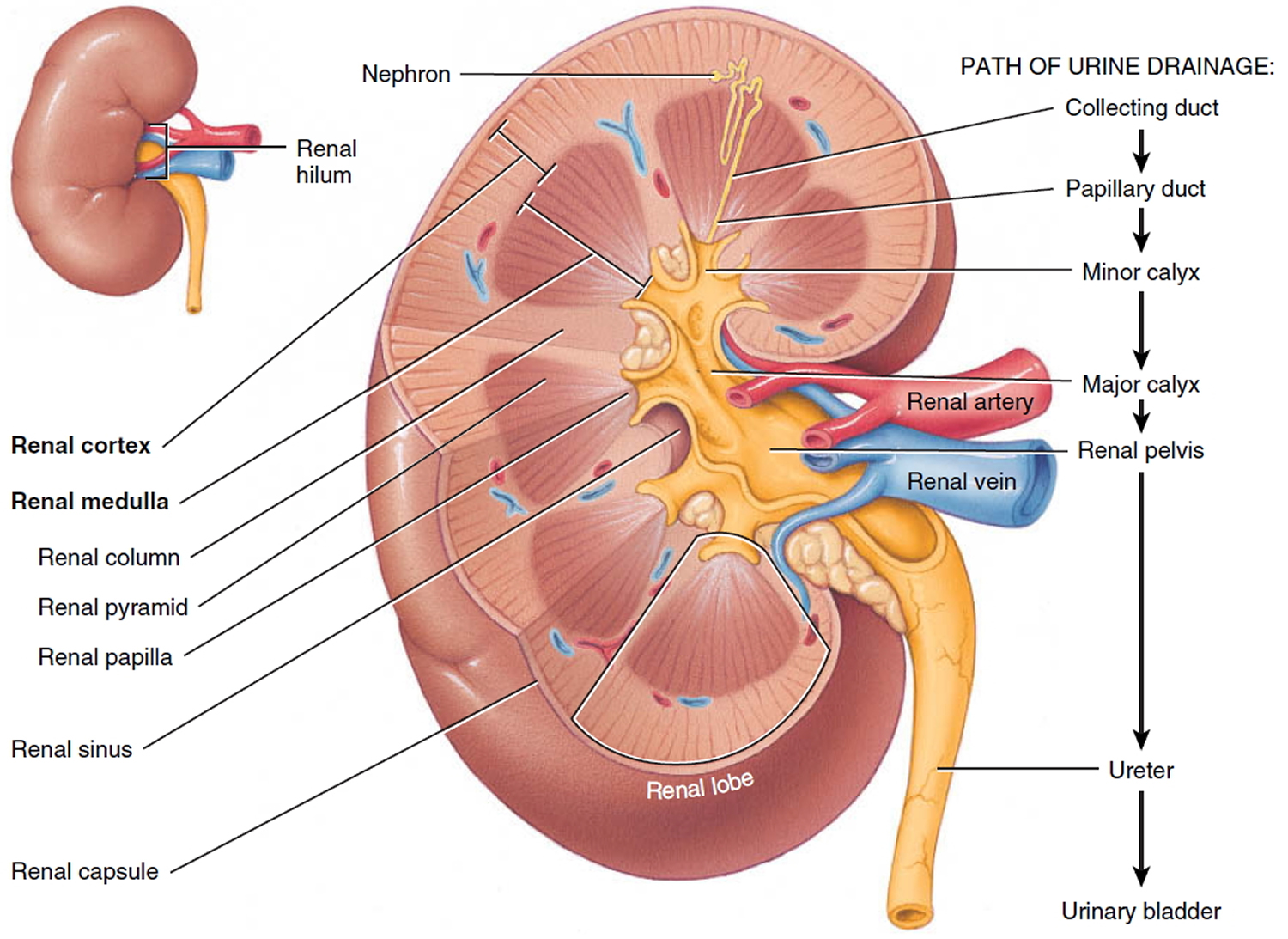
Figure 3. Kidney anatomy
 Blood in urine causes
Blood in urine causes
Hundreds of diseases have been shown to cause hematuria. In the small percentage of patients for whom an etiology is identified, causes may include urinary tract infection, benign prostatic hyperplasia, medical renal disease, urinary calculi, urethral stricture disease, and urologic malignancy 5. Table 1 lists the most common causes after initial evaluation of microscopic hematuria 4. The risk of urologic cancer increases significantly in men, persons older than 35 years, and persons with a history of smoking 3, 5. Table 2 lists other factors that have been shown to increase the risk of urologic malignancy in patients with asymptomatic microscopic hematuria 5.
The more common causes of blood in urine are:
- bladder infection (cystitis) or kidney infections (pyelonephritis)
- infection in the prostate (prostatitis)
- defects in the structure of the urinary tract
- inherited diseases
- mineral imbalances in the urine, like too much calcium
- kidney stones
- kidney diseases
- trauma to the kidney, ureter, bladder or urethra
- vigorous exercise
- viral illness, such as hepatitis—a virus that causes liver disease and inflammation of the liver
- sexual activity
- taking certain medicines, like some over-the-counter pain relievers
- endometriosis—a problem in women that occurs when the kind of tissue that normally lines the uterus grows somewhere else, such as the bladder
Other reasons why people get hematuria are menstruation, vigorous exercise, and injuries to the kidneys or urinary tract. Many athletes, especially distance runners, get hematuria from time to time.
In rare cases in children, hematuria can be a sign of kidney cancer or bladder cancer, a blood disease, or a blood clot. If something like that is going on, hematuria will usually be one of many other symptoms.
Very occasionally, what looks like hematuria might be something else. It’s possible (though unlikely) that things like food dye, some foods (like beets or blackberries), or certain prescription medicines can make a person’s urine look red.
More serious reasons people may have hematuria include:
- bladder or kidney cancer
- inflammation of the kidney, urethra, bladder, or prostate—a walnut-shaped gland in men that surrounds the urethra and helps make semen
- blood-clotting disorders, such as hemophilia
- sickle cell disease—a genetic disorder in which a person’s body makes abnormally shaped red blood cells
- polycystic kidney disease—a genetic disorder in which many cysts grow on a person’s kidneys.
Urinary tract infections
These occur when bacteria enter your body through the urethra and multiply in your bladder. Symptoms can include a persistent urge to urinate, pain and burning with urination, and extremely strong-smelling urine. For some people, especially older adults, the only sign of illness might be microscopic blood in the urine.
Kidney infections (pyelonephritis)
These can occur when bacteria enter your kidneys from your bloodstream or move from your ureters to your kidney(s). Signs and symptoms are often similar to bladder infections, though kidney infections are more likely to cause a fever and flank pain.
A bladder or kidney stone
The minerals in concentrated urine sometimes form crystals on the walls of your kidneys or bladder. Over time, the crystals can become small, hard stones.
The stones are generally painless, so you probably won’t know you have them unless they cause a blockage or are being passed. Then there’s usually no mistaking the symptoms — kidney stones, especially, can cause excruciating pain. Bladder or kidney stones can also cause both gross and microscopic bleeding.
Enlarged prostate
The prostate gland — which is just below the bladder and surrounding the top part of the urethra — often enlarges as men approach middle age. It then compresses the urethra, partially blocking urine flow. Signs and symptoms of an enlarged prostate (benign prostatic hyperplasia, or BPH) include difficulty urinating, an urgent or persistent need to urinate, and either visible or microscopic blood in the urine. Infection of the prostate (prostatitis) can cause the same signs and symptoms.
Kidney disease
Microscopic urinary bleeding is a common symptom of glomerulonephritis, an inflammation of the kidneys’ filtering system. Glomerulonephritis may be part of a systemic disease, such as diabetes, or it can occur on its own. Viral or strep infections, blood vessel diseases (vasculitis), and immune problems such as IgA nephropathy, which affects the small capillaries that filter blood in the kidneys (glomeruli), can trigger glomerulonephritis.
Cancer
Visible urinary bleeding may be a sign of advanced kidney, bladder or prostate cancer. Unfortunately, you might not have signs or symptoms in the early stages, when these cancers are more treatable.
Inherited disorders
Sickle cell anemia — a hereditary defect of hemoglobin in red blood cells — causes blood in urine, both visible and microscopic hematuria. So can Alport syndrome, which affects the filtering membranes in the glomeruli of the kidneys.
Kidney injury
A blow or other injury to your kidneys from an accident or contact sports can cause visible blood in your urine.
Medications
The anti-cancer drug cyclophosphamide and penicillin can cause urinary bleeding. Visible urinary blood sometimes occurs if you take an anticoagulant, such as aspirin and the blood thinner heparin, and you also have a condition that causes your bladder to bleed.
Strenuous exercise
It’s rare for strenuous exercise to lead to gross hematuria, and the cause is unknown. It may be linked to trauma to the bladder, dehydration or the breakdown of red blood cells that occurs with sustained aerobic exercise.
Runners are most often affected, although anyone can develop visible urinary bleeding after an intense workout. If you see blood in your urine after exercise, don’t assume it’s from exercising. See your doctor.
Often the cause of hematuria can’t be identified.
Table 1. Common Causes of Microscopic Hematuria
| Diagnosis | Frequency (%) |
|---|---|
Unknown | 43 to 68 |
Urinary tract infection | 4 to 22 |
Benign prostatic hyperplasia | 10 to 13 |
Urinary calculi | 4 to 5 |
Bladder cancer | 2 to 4 |
Renal cystic disease | 2 to 3 |
Renal disease | 2 to 3 |
Kidney cancer | < 1 |
Prostate cancer | < 1 |
Urethral stricture disease | < 1 |
Table 2. Common Risk Factors for Urinary Tract Malignancy in Patients with Microscopic Hematuria
Age older than 35 years | |
Analgesic abuse | |
Exposure to chemicals or dyes (benzenes or aromatic amines) | |
Male sex | |
Past or current smoking | |
History of any of the following: | |
Chronic indwelling foreign body | |
Chronic urinary tract infection | |
Exposure to known carcinogenic agents or alkylating chemotherapeutic agents | |
Gross hematuria | |
Irritative voiding symptoms | |
Pelvic irradiation | |
Urologic disorder or disease | |
Risk factors for hematuria
Almost anyone — including children and teens — can have red blood cells in the urine. Factors that make this more likely include:
- Age. Many men older than 50 have occasional hematuria due to an enlarged prostate gland.
- A recent infection. Kidney inflammation after a viral or bacterial infection (post-infectious glomerulonephritis) is one of the leading causes of visible urinary blood in children.
- Family history. You might be more prone to urinary bleeding if you have a family history of kidney disease or kidney stones.
- Certain medications. Aspirin, nonsteroidal anti-inflammatory pain relievers and antibiotics such as penicillin are known to increase the risk of urinary bleeding.
- Strenuous exercise. Long-distance runners are especially prone to exercise-induced urinary bleeding. In fact, the condition is sometimes called jogger’s hematuria. But anyone who works out strenuously can develop symptoms.
Who is more likely to develop hematuria?
People who are more likely to develop hematuria may
- have an enlarged prostate
- have urinary stones
- take certain medications, including blood thinners, aspirin and other pain relievers, and antibiotics
- do strenuous exercise, such as long-distance running
- have a bacterial or viral infection, such as streptococcus or hepatitis
- have a family history of kidney disease
- have a disease or condition that affects one or more organs.
People who are more likely to develop hematuria may have a family history of kidney disease, have an enlarged prostate, or have bladder or kidney stones, among other reasons.
Blood in urine symptoms
Gross hematuria produces pink, red or cola-colored urine due to the presence of red blood cells. It takes a small amount of blood in the urine to produce red urine, and the bleeding usually isn’t painful. In most cases, people with gross hematuria do not have other signs and symptoms. People with gross hematuria that includes blood clots in the urine may have bladder pain or pain in the back.
Bloody urine often occurs without other signs or symptoms.
Figure 4. Diagnosis and Management of microscopic hematuria
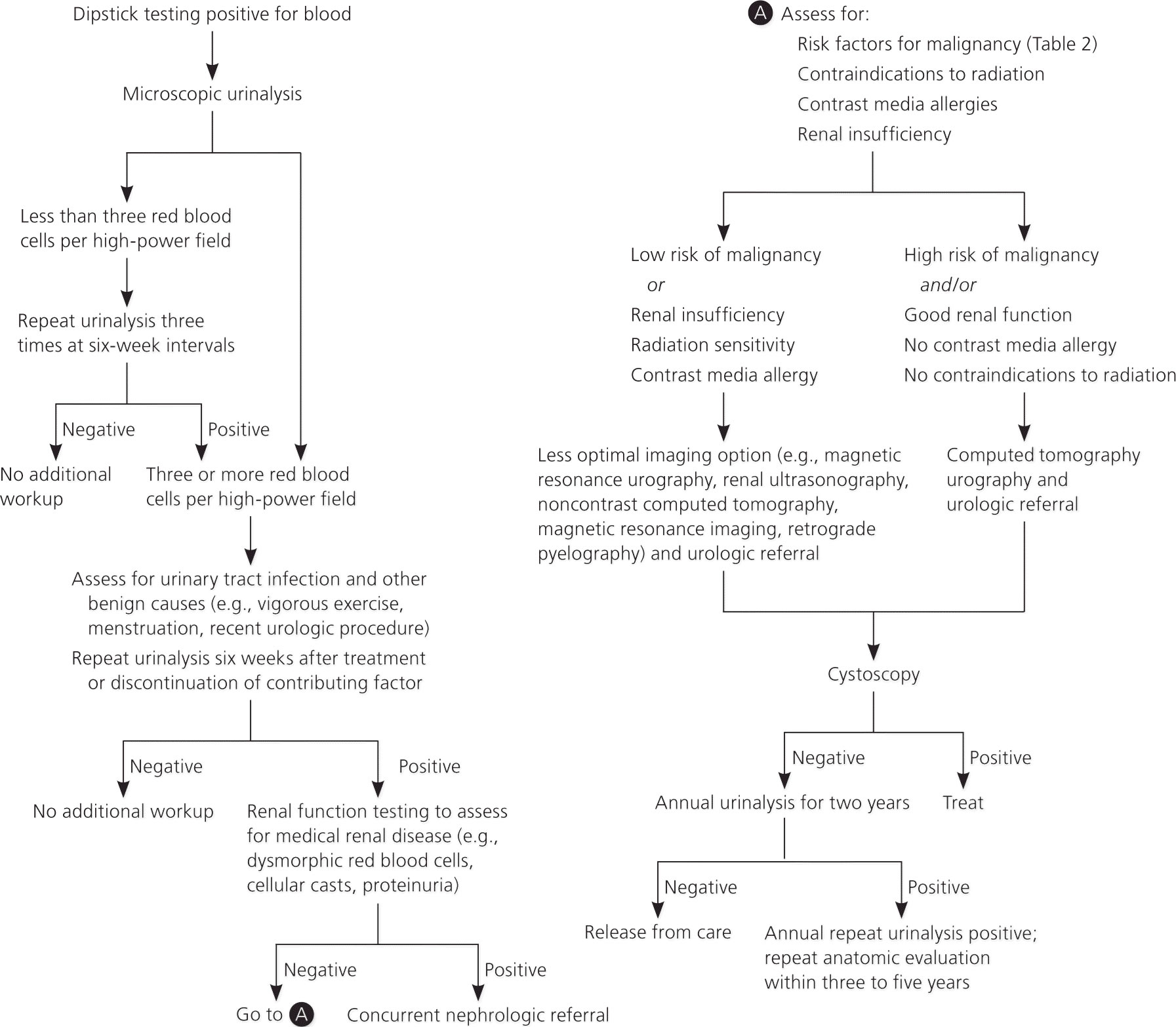 [Source 6]
[Source 6]
Blood in urine diagnosis
The most important test in the evaluation of hematuria is a microscopic examination of the urine 5.
A health care professional diagnoses hematuria or the cause of the hematuria with:
- a medical history
- a physical exam
- urinalysis
- additional testing
Sometimes, the cause of urinary bleeding can’t be found. In that case, your doctor might recommend regular follow-up tests, especially if you have risk factors for bladder cancer, such as smoking, exposure to environmental toxins or a history of radiation therapy.
Medical History
If you see a doctor about blood in your urine or if microscopic hematuria shows up on a urine test, the doctor will take a medical history to help the doctor diagnose the cause of hematuria. He or she will ask you to provide a medical history of symptoms, and a list of prescription and over-the-counter medications. The health care professional will also ask about current and past medical conditions. He or she will ask you questions about recent activities and family medical history.
Physical Exam
The doctor will give you a physical examination. During a physical exam, a health care professional most often taps on the abdomen and back, checking for pain or tenderness in the bladder and kidney area. A health care professional may perform a digital rectal exam on a man to look for any prostate problems. A health care professional may perform a pelvic exam on a woman to look for the source of possible red blood cells in the urine.
- Digital rectal exam. A digital rectal exam is a physical exam of a man’s prostate and rectum. To perform the exam, the health care professional has the man bend over a table or lie on his side while holding his knees close to his chest. The health care professional slides a gloved, lubricated finger into the patient’s rectum and feels the part of the prostate that lies in front of the rectum. The digital rectal exam is used to check for prostate inflammation, an enlarged prostate, or prostate cancer.
- Pelvic exam. A pelvic exam is a visual and physical exam of a woman’s pelvic organs. The health care professional has the woman lie on her back on an exam table and place her feet on the corners of the table or in supports. The health care professional looks at the pelvic organs and slides a gloved, lubricated finger into the vagina to check for problems that may be causing blood in the urine.
Positive Dipstick Test and Negative Microscopic Results
The health care professional can test the urine in the office using a dipstick or can send it out to a lab for analysis. Prior to obtaining a urine sample, the health care professional may ask a woman when she last menstruated. Sometimes blood from a woman’s menstrual period can get into her urine sample and can result in a false-positive test for hematuria. The test should be repeated after the woman stops menstruating.
The use of a simple urine dipstick test for identifying microscopic hematuria has a sensitivity greater than 90%; however, there is a considerable false-positive rate (up to 35%) 8, necessitating follow-up microscopic analysis for all positive results. Referral to a subspecialist should not be initiated until the hematuria is confirmed 9. False-positive results on a urine dipstick test can occur in the presence of hemoglobinuria, myoglobinuria, semen, highly alkaline urine (pH greater than 9), and concentrated urine 10. Ascorbic acid (vitamin C) has been shown to cause false-negative results on dipstick testing because of its reducing properties; therefore, patients taking vitamin C supplements and undergoing urinary evaluation may benefit from up-front microscopic examination 11.
What if tests show you have microscopic hematuria?
If the urine test comes back negative, the doctor will probably want another urine sample 1-2 weeks later to make sure the urine is free of red blood cells. If hematuria only happens once, there’s usually no need for any treatment.
If you don’t have any symptoms like pain or fever, you haven’t had a recent injury, and there’s no protein in your urine, your doctor will do 3 additional microscopic urine tests to rule out hematuria over a few months to see if you still have blood in your urine.
If one of these repeat test results is positive on microscopic analysis, the patient is considered to have microscopic hematuria. If all three specimens are negative on microscopy, the patient does not require further evaluation for hematuria 5 and other causes of a positive dipstick test result, such as hemoglobinuria and myoglobinuria, should be considered.
If urine samples point to something more serious or you’ve had a recent injury, you’ll probably need additional tests, such as a urine culture (more peeing in a cup!), or imaging tests like a kidney ultrasound, an MRI, or a CT scan. Occasionally, doctors need to remove a tiny piece of kidney tissue for testing (biopsy) or use instruments to check inside the body.
Blood in urine with urinary tract infections
If a patient has microscopic hematuria in the presence of pyuria (white blood cells in urine) or bacteriuria (the presence of bacteria in urine), a urine culture should be obtained to rule out urinary tract infection. Culture-directed antibiotics should be administered, and a microscopic urinalysis should be repeated in six weeks to assess for resolution of the hematuria 5. If the hematuria has resolved after the infection has cleared, no further workup is needed. If hematuria persists, diagnostic evaluation should commence 5.
Additional Testing
Sometimes, a health care professional will test the patient’s urine again. If the urine samples detect too many red blood cells, a health care professional may order additional tests:
- Blood test. A blood test involves drawing blood at a health care professional’s office or a commercial facility and sending the sample to a lab for analysis. A blood test can detect high levels of creatinine, a waste product of normal muscle breakdown, which may indicate kidney disease. Other blood tests may detect signs of autoimmune diseases, such as lupus, or other diseases, such as prostate cancer, which can cause hematuria.
- Computed tomography (CT) scan. CT scans use a combination of x-rays and computer technology to create images of the urinary tract, especially the kidneys. A health care professional may give the patient a solution to drink and an injection of contrast medium. CT scans require the patient to lie on a table that slides into a tunnel-shaped device that takes the x-rays. An x-ray technician performs the procedure in an outpatient center or a hospital, and a radiologist interprets the images. The patient does not need anesthesia. CT scans can help a doctor diagnose stones in the urinary tract, obstructions, infections, cysts, tumors, and traumatic injuries.
- Cystoscopy. Cystoscopy is a procedure that a urologist—a doctor who specializes in urinary problems—performs to see inside the patient’s bladder and urethra using a cystoscope, a tubelike instrument. The health care professional performs cystoscopy in his or her office, in an outpatient center, or in a hospital. The patient may need pain medication. A cystoscopy can detect cancer in a patient’s bladder.
- Kidney biopsy. Kidney biopsy is a procedure that involves taking a small piece of tissue from the kidney. A health care professional performs the biopsy in an outpatient center or a hospital. The health care professional will give the patient light sedation and local anesthetic. In some cases, the patient will require general anesthesia. A pathologist—a doctor who specializes in diagnosing diseases—examines the tissue in a lab. The biopsy can help diagnose if the hematuria is due to kidney disease.
- Magnetic resonance imaging (MRI). MRI is a test that takes pictures of the patient’s internal organs and soft tissues without using x-rays. A specially trained technician performs the procedure in an outpatient center or a hospital, and a radiologist interprets the images. The patient does not need anesthesia, although patients with a fear of confined spaces may receive light sedation. An MRI may include the injection of contrast medium. With most MRI machines, the patient will lie on a table that slides into a tunnel-shaped device that may be open-ended or closed at one end. Some machines allow the patient to lie in a more open space. During an MRI, the patient should remain perfectly still while the technician takes the images. During the procedure, the patient will hear loud mechanical knocking and humming noises coming from the machine. An MRI can help diagnose problems in individual internal organs, such as the bladder or kidney.
Blood in urine treatment
There are many different treatments for blood in the urine, and it depends on the cause. It may involve antibiotics, or surgery, or treatment for the condition which caused the blood in the urine. Some causes of blood in urine don’t need any treatment.
- It is important to have regular follow-ups with your doctor to ensure complete recovery.
Follow-up
If appropriate workup does not reveal nephrologic or urologic disease, then annual urinalysis should be performed for at least two years after initial referral. If these two urinalyses do not show persistent hematuria, the risk of future malignancy is less than 1% 12, 13, and the patient may be released from care. However, if asymptomatic microscopic hematuria persists on follow-up urinalysis, a full repeat evaluation should be considered within three to five years of the initial evaluation.6 Patients’ risk factors for urologic malignancy should guide clinical decision making about reevaluation 13.
- Elias K, Svatek RS, Gupta S, Ho R, Lotan Y. High-risk patients with hematuria are not evaluated according to guideline recommendations. Cancer. 2010;116(12):2954–2959.[↩]
- Khadra MH, Pickard RS, Charlton M, Powell PH, Neal DE. A prospective analysis of 1,930 patients with hematuria to evaluate current diagnostic practice. J Urol. 2000;163(2):524–527.[↩]
- Chou R, Dana T. Screening adults for bladder cancer: a review of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2010;153(7):461–468.[↩][↩]
- Hiatt RA, Ordoñez JD. Dipstick urinalysis screening, asymptomatic microhematuria, and subsequent urological cancers in a population-based sample [published correction appears in Cancer Epidemiol Biomarkers Prev. 1994;3(6):523]. Cancer Epidemiol Biomarkers Prev. 1994;3(5):439–443.[↩][↩]
- Davis R, Jones JS, Barocas DA, et al. Diagnosis, evaluation and follow-up of asymptomatic microhematuria (AMH) in adults: AUA guideline. American Urological Association Education and Research, Inc., 2012:1–30.[↩][↩][↩][↩][↩][↩][↩]
- Assessment of Asymptomatic Microscopic Hematuria in Adults. Am Fam Physician. 2013 Dec 1;88(11):747-754. https://www.aafp.org/afp/2013/1201/p747.html[↩][↩]
- Davis R, Jones JS, Barocas DA, et al. Diagnosis, evaluation and follow-up of asymptomatic microscopic hematuria (AMH) in adults: AUA guideline. American Urological Association Education and Research, Inc., 2012:5.[↩]
- Rao PK, Jones JS. How to evaluate ‘dipstick hematuria’: what to do before you refer. Cleve Clin J Med. 2008;75(3):227–233.[↩]
- Shaw ST Jr, Poon SY, Wong ET. ‘Routine urinalysis.’ Is the dipstick enough? JAMA. 1985;253(11):1596–1600.[↩]
- Gerber GS, Brendler CB. Evaluation of the urologic patient: history, physical examination, and urinalysis. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, eds. Campbell-Walsh Urology. 10th ed. Philadelphia, Pa.: Saunders; 2011:86–87.[↩]
- Brigden ML, Edgell D, McPherson M, Leadbeater A, Hoag G. High incidence of significant urinary ascorbic acid concentrations in a west coast population—implications for routine urinalysis. Clin Chem. 1992;38(3):426–431.[↩]
- Madeb R, Golijanin D, Knopf J, et al. Long-term outcome of patients with a negative work-up for asymptomatic microhematuria. Urology. 2010;75(1):20–25.[↩]
- Edwards TJ, et al. Patient-specific risk of undetected malignant disease after investigation for haematuria, based on a 4-year follow-up. BJU Int. 2011;107(2):247–252.[↩][↩]