Contents
Central sleep apnea
Central sleep apnea is a sleep-related breathing disorder in which your breathing repeatedly stops and starts during sleep. Central sleep apnea occurs because your brain doesn’t send proper signals to the muscles that control your breathing 1, 2, 3, 4. A single central apnea event is a ≥10-second pause in breathing with no associated respiratory effort; greater than five such events per hour are considered abnormal. Central sleep apnea is present when a patient has greater than five central apneas per hour of sleep with associated symptoms of disrupted sleep (such as excessive daytime somnolence). Central sleep apnea (CSA) is different from obstructive sleep apnea (OSA), in which you can’t breathe normally because of upper airway obstruction. Central sleep apnea is less common than obstructive sleep apnea. As opposed to obstructive sleep apnea (OSA), central sleep apnea is characterized by repetitive cessation of breathing during sleep resulting from lack of ventilatory effort or drive to breathe from your brain. While obstructive sleep apnea (OSA) and central sleep apnea (CSA) are two different sleep-related breathing disorders, sometimes they coexist, and most people with sleep apnea will have a combination of both types. The hallmark symptom of sleep apnea is excessive daytime sleepiness.
Central sleep apnea often occurs in people who have certain medical problems. For example, it can develop in someone who has a problem with an area of the brain called the brainstem, which controls breathing. Central sleep apnea may occur as a result of other conditions, such as heart failure and stroke. Sleeping at a high altitude also may cause central sleep apnea.
Conditions that can cause or lead to central sleep apnea include 4, 5, 6, 7:
- Problems that affect the brainstem, including brain infection, stroke, or conditions of the cervical spine (neck) or spinal cord injury
- Certain medicines, such as narcotic painkillers
- Being at high altitude
If the sleep apnea is not associated with another disease, it is called idiopathic central sleep apnea.
A condition called Cheyne-Stokes Breathing (CSB) or Cheyne-Stokes Respiration (CBR) can affect people with severe heart failure and can be associated with central sleep apnea 8. Unlike obstructive sleep apnea (OSA), which can be the cause of heart failure, Cheyne-Stokes respiration (Cheyne-Stokes breathing) is believed to be a result of heart failure 8. The presence of Cheyne-Stokes respiration in patients with heart failure also predicts worse outcomes and increases the risk of sudden cardiac death 8. Cheyne-Stokes Breathing pattern involves alternating deep and heavy breathing with shallow, or even not breathing, usually while sleeping. The American Academy of Sleep Medicine (AASM) recommends to score a respiratory event as Cheyne-Stokes breathing if both of the following criteria are met:
- There are episodes of at least three consecutive central apneas and/or central hypopneas separated by a crescendo and decrescendo change in breathing amplitude with a cycle length of at least 40 seconds (typically 45 to 90 seconds).
- There are five or more central apneas and/or central hypopneas per hour associated with the crescendo/decrescendo breathing pattern recorded over a minimum of two hours of monitoring.
Despite increasing recognition and growing knowledge, Cheyne-Stokes respiration remains elusive, and patients have very limited treatment options 9, 10, 11, 12.
Central sleep apnea is not the same as obstructive sleep apnea (OSA). With obstructive sleep apnea, breathing stops and starts because the upper airway is narrowed or blocked. Central sleep apnea and obstructive sleep apnea can be present in the same person.
Though the prevalence of central sleep apnea is lower than obstructive sleep apnea (OSA), both conditions often coexist, and patients can exhibit features of both states 4. The prevalence of central sleep apnea (CSA) tends to increase with age and is higher in the elderly population above 65 years of age. A cross-sectional study reported the prevalence of central sleep apnea (CSA) in men aged 65 years and older as 2.7% by using a modified form of the International Classification of Sleep Disorders – Third Edition (ICSD-3) classification 13.
The International Classification of Sleep Disorders – Third Edition (ICSD-3) has divided central sleep apnea into several categories based on distinct clinical and polysomnographic features 14:
- Primary central sleep apnea (CSA). Diagnosis of primary central sleep apnea can be made if polysomnography (PSG) reveals ≥5 central apneas and/or central hypopneas per hour of sleep, with a total number of these central events being >50% of total respiratory events in the apnea-hypopnea index with no evidence of Cheyne-Stokes breathing (CSB) 15. Additionally, there must be at least one complaint related to disrupted sleep, i.e., sleepiness, insomnia, awakening with shortness of breath, snoring, or witnessed apneas.
- Central sleep apnea (CSA) with Cheyne-Stokes Breathing (CSB). Diagnosis of central sleep apnea with with Cheyne-Stokes Breathing (CSB) requires the criteria of primary central sleep apnea with three or more consecutive central apneas or hypopneas separated by a crescendo–decrescendo respiratory pattern with a cycle length of ≥40 seconds 4.
- Central sleep apnea (CSA) due to a medical disorder without Cheyne-Stokes Breathing (CSB)
- Central sleep apnea (CSA) due to a periodic high-altitude breathing
- Central sleep apnea (CSA) due to a medication or substance
- Treatment-emergent central sleep apnea (CSA) also known as complex sleep apnea, which happens when someone has obstructive sleep apnea (OSA) converts to central sleep apnea (CSA) while using continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea (OSA) 16. Diagnosis of treatment-emergent central apnea requires to have a primary diagnosis of OSA (with an apnea-hypopnea index [AHI] ≥ 5 obstructive respiratory events per hour of sleep) followed by resolution of the obstructive apnea and emergence or persistence of central sleep apnea (not explained by the presence of other disease or substance) during positive airway pressure (PAP) titration study 4. Previous studies have noted that the prevalence of treatment-emergent central sleep apnea varies between 3.5% and 20% 17, 18, 19, 20, 21, 22, 23, 24, 25.
When your sleep is interrupted throughout the night, you can be drowsy during the day. Left untreated, central sleep apnea can be life threatening. People with central sleep apnea are at higher risk for car crashes, work-related accidents, and other medical problems. Central sleep apnea also appears to put individuals at risk for a major health issue associated with different forms of cardiovascular disease including high blood pressure (hypertension), coronary artery disease (coronary heart disease), heart attack, heart failure, irregular heartbeat and stroke and transient ischemic attack (TIA) also known as “mini-stroke” 26.
Doctors diagnose central sleep apnea based on your medical and family histories, a physical exam, and sleep study also called polysomnography results. Nocturnal polysomnography (PSG) is the gold standard diagnostic test in evaluating central apnea during which patients need to sleep overnight at a sleep laboratory 4. However, more recently home sleep testing is increasingly being used to diagnose sleep apnea. The most commonly used type of home sleep testing device records airflow, respiratory effort, oxygen saturation, and heart rate 27. Although home sleep apnea tests are widely utilized, the accuracy of the diagnosis or severity estimation of central sleep apnea with these devices is reduced 28.
If you have central sleep apnea, it is important to get treatment. There are a variety of treatments for central sleep apnea, depending on your medical history and the severity of your sleep apnea. Treatments for central sleep apnea involve treating existing condition that is causing central sleep apnea, using a device to assist breathing, using supplemental oxygen or phrenic nerve stimulation. Oxygen treatment may help ensure the lungs get enough oxygen while sleeping. Devices used during sleep to aid breathing may be recommended. These include nasal continuous positive airway pressure (CPAP), bilevel positive airway pressure (BiPAP) or adaptive servo-ventilation (ASV). Some types of central sleep apnea are treated with medicines that stimulate breathing. If narcotic medicine is causing the apnea, the dosage may need to be lowered or the medicine changed.
Can you die from central sleep apnea?
It depends on what is causing your central sleep apnea. Central sleep apnea is most commonly associated with congestive heart failure or stroke. Central sleep apnea can also be due to end stage kidney disease, in people who have a problem with an area of the brain called the brainstem, which controls breathing or in people taking taking certain medications such as opioids, see central sleep apnea causes below for more details. In addition, sudden drops in blood oxygen levels (hypoxemia) that occur during central sleep apnea may adversely affect your heart health. If you have an underlying heart disease, these repeated multiple episodes of low blood oxygen (hypoxia or hypoxemia) worsen prognosis and increase the risk of abnormal heart rhythms (arrhythmias).
Untreated sleep apnea may lead to or worsen heart disease, including:
- Heart arrhythmias
- Heart failure
- Heart attack
- High blood pressure
- Stroke
Consult a medical professional if you experience — or if your partner observes — any signs or symptoms of central sleep apnea, particularly the following:
- Shortness of breath that awakens you from sleep
- Intermittent pauses in your breathing during sleep
- Difficulty staying asleep
- Excessive daytime drowsiness, which may cause you to fall asleep while you’re working, watching television or even driving
Ask your doctor about any sleep problem that leaves you chronically fatigued, sleepy and irritable. Excessive daytime drowsiness may be due to other disorders, such as not allowing yourself time to get enough sleep at night (chronic sleep deprivation), sudden attacks of sleep (narcolepsy) or obstructive sleep apnea.
Central vs Obstructive sleep apnea
Obstructive sleep apnea (OSA) is a problem in which your breathing pauses during sleep because of narrowed or blocked airways. On the other hand, central sleep apnea is characterized by repetitive cessation of breathing during sleep resulting from the brain temporarily stops sending signals to the muscles that control breathing. Whereas obstructive sleep apnea (OSA) is extremely common in the adult population, central sleep apnea affects less than 10% of patients referred to sleep laboratories. However, central apneas also may occur in an individual with obstructive apneas, a person can have both conditions, such as with a medical problem called obesity hypoventilation syndrome (OHS). Clinicians may struggle to determine if central sleep apnea or obstructive sleep apnea (OSA) is the principal problem, or if a combination of the 2 disorders may need therapy. Obesity hypoventilation syndrome is a condition in some obese people in which poor breathing leads to lower oxygen and higher carbon dioxide levels in the blood. The exact cause of obesity hypoventilation syndrome is not known. Researchers believe obesity hypoventilation syndrome (OHS) results from a defect in the brain’s control over breathing. Excess weight against the chest wall also makes it harder for the muscles to draw in a deep breath and to breathe quickly enough. As a result, the blood contains too much carbon dioxide and not enough oxygen. Untreated, obesity hypoventilation syndrome (OHS) can lead to serious heart and blood vessel problems, severe disability, or death.
Treatment for obesity hypoventilation syndrome (OHS) involves breathing assistance using special machines (mechanical ventilation). Options include:
- Noninvasive mechanical ventilation such as continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BPAP) through a mask that fits tightly over the nose or nose and mouth (mainly for sleep)
- Oxygen therapy
- Breathing help through an opening in the neck (tracheostomy) for severe cases
- Other treatments are aimed at weight loss, which can reverse obesity hypoventilation syndrome (OHS).
Treatment is started in the hospital or as an outpatient.
Obstructive sleep apnea causes
When you sleep, all of the muscles in your body become more relaxed. This includes the muscles that help keep your throat open so air can flow into your lungs.
Normally, your throat remains open enough during sleep to let air pass by. Some people have a narrow throat. When the muscles in their upper throat relax during sleep, the tissues close in and block the airway. This stop in breathing is called apnea.
Loud snoring is a telltale symptom of obstructive sleep apnea. Snoring is caused by air squeezing through the narrowed or blocked airway. Not everyone who snores has sleep apnea though.
Other factors also may increase your risk of obstructive sleep apnea:
- A lower jaw that is short compared to your upper jaw
- Certain shapes of the roof of your mouth (palate) or airway that cause it to collapse more easily
- Large neck or collar size, 17 inches (43 centimeters) or more in men and 16 inches (41 centimeters) or more in women
- Large tongue, which may fall back and block the airway
- Obesity
- Large tonsils and adenoids that can block the airway
Sleeping on your back can also cause your airway to become blocked or narrowed.
Obstructive sleep apnea symptoms
If you have obstructive sleep apnea, you usually begin snoring heavily soon after falling asleep.
- The snoring often becomes very loud.
- Snoring is interrupted by a long silent period while your breathing stops.
- The silence is followed by a loud snort and gasp, as you attempt to breathe.
- This pattern repeats throughout the night.
Most people with obstructive sleep apnea do not know their breathing starts and stops during the night. Usually, a sleep partner or other family members hear the loud snoring, gasping, and snorting. Snoring can be loud enough to hear through walls. Sometimes, people with obstructive sleep apnea wake up gasping for air.
People with sleep apnea may:
- Wake up unrefreshed in the morning
- Feel sleepy or drowsy throughout the day
- Act grumpy, impatient, or irritable
- Be forgetful
- Fall asleep while working, reading, or watching TV
- Feel sleepy while driving or even fall asleep while driving
- Have hard-to-treat headaches
Other problems that may occur include:
- Depression
- Hyperactive behavior, especially in children
- Difficult to treat high blood pressure
- Leg swelling (if apnea is severe)
Obstructive sleep apnea possible complications
Untreated obstructive sleep apnea may lead to or worsen heart disease, including:
- Heart arrhythmias
- Heart failure
- Heart attack
- High blood pressure
- Stroke
Obstructive sleep apnea treatment
Treatment helps keep your airway open while you sleep so your breathing does not stop.
Lifestyle changes may help relieve symptoms in people with mild sleep apnea, such as:
- Avoid alcohol or medicines that make you sleepy before bedtime. They can make symptoms worse.
- Avoid sleeping on your back.
- Lose excess weight.
Continuous positive airway pressure (CPAP) devices work best to treat obstructive sleep apnea in most people.
- You wear a mask over your nose or over your nose and mouth while you sleep.
- The mask is connected by a hose to a small machine that sits at the side of your bed.
- The machine pumps air under pressure through the hose and mask and into your airway while you sleep. This helps keep your airway open.
It can take some time to get used to sleeping with continuous positive airway pressure (CPAP) therapy. Good follow-up and support from a sleep center can help you overcome any problems using CPAP.
Dental devices may help some people. You wear them in your mouth while you sleep to keep your jaw forward and the airway open.
Other treatments may be available, but there is less evidence that they work. It is best to talk with a doctor who specializes in sleep problems before trying them.
Surgery may be an option for some people. It is often a last resort if other treatments did not work and you have severe symptoms. Surgery may be used to:
- Remove extra tissue at the back of the throat.
- Correct problems with the structures in the face.
- Create an opening in the windpipe to bypass the blocked airway if there are physical problems.
- Remove the tonsils and adenoids.
Surgery may not completely cure obstructive sleep apnea and may have long-term side effects.
Obstructive sleep apnea prognosis
If not treated, sleep apnea may cause:
- Anxiety and depression
- Loss of interest in sex
- Poor performance at work or school
Daytime sleepiness because of sleep apnea can increase the risk of:
- Motor vehicle accidents from driving while sleepy
- Industrial accidents from falling asleep on the job
In most cases, treatment completely relieves symptoms and problems from sleep apnea.
Central sleep apnea causes
Central sleep apnea occurs when your brain fails to transmit signals to your breathing muscles. Central sleep apnea can be caused by a number of conditions that affect the ability of your brainstem — which links your brain to your spinal cord and controls many functions such as heart rate and breathing — to control your breathing. Problems that affect your brainstem, including brain infection, stroke, or conditions of the cervical spine (neck).
The cause varies with the type of central sleep apnea you have. Types include:
- Cheyne-Stokes breathing (Cheyne-Stokes respiration). Cheyne-Stokes breathing pattern involves alternating deep and heavy breathing with shallow, or even not breathing, usually while sleeping. Cheyne-Stokes breathing is characterized by a gradual increase and then decrease in breathing effort and airflow. During the weakest breathing effort, a total lack of airflow (central sleep apnea) can occur. This type of central sleep apnea is most commonly associated with congestive heart failure or stroke.
- Drug-induced apnea. Taking certain medications such as opioids — including morphine (Ms Contin, Kadian, others), oxycodone (Roxicodone, Oxycontin, others) or codeine — may cause your breathing to become irregular, to increase and decrease in a regular pattern, or to temporarily stop completely.
- High-altitude periodic breathing. A Cheyne-Stokes breathing pattern may occur if you’re exposed to a very high altitude. The change in oxygen at this altitude is the reason for the alternating rapid breathing (hyperventilation) and underbreathing.
- Treatment-emergent central sleep apnea. Some people with obstructive sleep apnea (OSA) develop central sleep apnea while using continuous positive airway pressure (CPAP) for their sleep apnea treatment. This condition is known as treatment-emergent central sleep apnea and is a combination of obstructive and central sleep apneas.
- Medical condition-induced central sleep apnea. Several medical conditions, including end-stage kidney disease and stroke, may give rise to central sleep apnea and doesn’t involve Cheyne-Stokes breathing.
- Severe obesity
- Idiopathic (primary) central sleep apnea. The cause of this uncommon type of central sleep apnea isn’t known.
Risk factors for central sleep apnea
Certain factors put you at increased risk of central sleep apnea:
- Being male. Males are more likely to develop central sleep apnea than are females.
- Being older. Central sleep apnea is more common among older adults, especially adults older than age 65, possibly because they may have other medical conditions or sleep patterns that are more likely to cause central sleep apnea 29.
- Family history and genetics. Your genes can affect how your brain controls your breathing during sleep. Genetic conditions such as congenital central hypoventilation syndrome can raise your risk.
- Drinking alcohol and smoking can affect how your brain controls sleep or the muscles involved in breathing.
- Heart disorders. People with irregular heartbeats (atrial fibrillation) or whose heart muscles don’t pump enough blood for the body’s needs (congestive heart failure) are at greater risk of central sleep apnea.
- Stroke, brain tumor or a structural brainstem lesion. Having had a stroke increases the risk of central sleep apnea. These brain conditions can impair the brain’s ability to regulate breathing.
- High altitude. Sleeping at an altitude higher than you’re accustomed to may increase your risk of sleep apnea. High-altitude sleep apnea is no longer a problem a few weeks after returning to a lower altitude.
- Opioid use. Opioid pain medicines, especially long-acting ones such as methadone an cause problems with how your brain controls sleep, increasing your risk of central sleep apnea.
- Health conditions. Some conditions that affect how your brain controls your airway and chest muscles can raise your risk. These include amyotrophic lateral sclerosis (ALS), and myasthenia gravis. Also, your hormone levels can affect how your brain controls your breathing.
- Premature birth. Babies born before 37 weeks of pregnancy have a higher risk of breathing problems during sleep. In most cases, the risk gets lower as the baby gets older.
- Continuous positive airway pressure (CPAP). Some people with obstructive sleep apnea (OSA) develop central sleep apnea (CSA) while using continuous positive airway pressure (CPAP). This condition is known as treatment-emergent central sleep apnea or complex sleep apnea. It is a combination of obstructive and central sleep apneas. For most people, treatment-emergent central sleep apnea goes away with continued use of a continuous positive airway pressure (CPAP) device. Other people may be treated with a different kind of positive airway pressure therapy.
Central sleep apnea symptoms
Central sleep apnea common signs and symptoms include:
- Observed episodes of stopped breathing or abnormal breathing patterns during sleep
- Sudden awakenings accompanied by shortness of breath
- Shortness of breath that’s relieved by sitting up
- Difficulty staying asleep (insomnia)
- Excessive daytime sleepiness (hypersomnia)
- Chest pain at night
- Difficulty concentrating
- Mood changes
- Morning headaches
- Snoring. Although snoring suggests some degree of a blocked airway, snoring also can occur in people with central sleep apnea. However, snoring may not be as prominent with central sleep apnea as it is with obstructive sleep apnea.
- Lower tolerance for exercise
Other symptoms may include:
- Chronic fatigue
- Daytime sleepiness
- Morning headaches
- Restless sleep
Other symptoms may occur if the apnea is due to a problem with the nervous system. Symptoms depend on the parts of the nervous system that are affected, and may include:
- Shortness of breath
- Swallowing problems
- Voice changes
- Weakness or numbness throughout the body
Although snoring indicates some degree of airflow obstruction, snoring also may be heard in the presence of central sleep apnea. However, snoring may not be as prominent with central sleep apnea as it is with obstructive sleep apnea.
Central sleep apnea complications
Central sleep apnea is a serious medical condition. Some complications include:
- Fatigue. The repeated awakenings associated with sleep apnea make normal, restorative sleep impossible. People with central sleep apnea often experience severe fatigue, daytime drowsiness and irritability. You may have difficulty concentrating and find yourself falling asleep at work, while watching television or even when driving.
- Cardiovascular problems. In addition, sudden drops in blood oxygen levels that occur during central sleep apnea may adversely affect heart health. If there’s underlying heart disease, these repeated multiple episodes of low blood oxygen (hypoxia or hypoxemia) worsen prognosis and increase the risk of abnormal heart rhythms.
Central sleep apnea diagnosis
Your doctor may make an evaluation based on your signs and symptoms or may refer you to a sleep specialist in a sleep disorder center.
Your doctor will take your medical history and do a physical exam.
- Your doctor will check your mouth, neck, and throat.
- You may be asked about daytime sleepiness, how well you sleep, and bedtime habits.
You will need to have a sleep study or polysomnography to confirm central sleep apnea. This testing can be done in your home or in a sleep lab.
Other tests that may be performed include:
- Arterial blood gases
- Electrocardiogram (ECG)
- Echocardiogram
- Thyroid function studies
- Lung function testing
- MRI of the brain, spine, or neck
A sleep specialist can help you decide on your need for further evaluation. Such an evaluation often involves overnight monitoring of your breathing and other body functions during a sleep study called polysomnography. During polysomnography, you’re connected to equipment that monitors your heart, lung and brain activity (EEG), breathing patterns, arm and leg movements, and blood oxygen levels while you sleep. You may have a full-night or split-night sleep study.
In a split-night sleep study, you’re monitored during the first half of the night. If you’re diagnosed with central sleep apnea, staff may wake you and give you positive airway pressure for the second half of the night.
Polysomnography can help your doctor diagnose central sleep apnea. It also can help your doctor rule out other sleep disorders, such as obstructive sleep apnea, repetitive movements during sleep (periodic limb movements) or sudden attacks of sleep (narcolepsy), which can cause excessive daytime sleepiness but require different treatment.
Doctors trained in nervous system diseases (neurologists), heart diseases (cardiologists) and others may be involved in evaluating your condition. Doctors may also order imaging of your head or heart to look for contributing conditions.
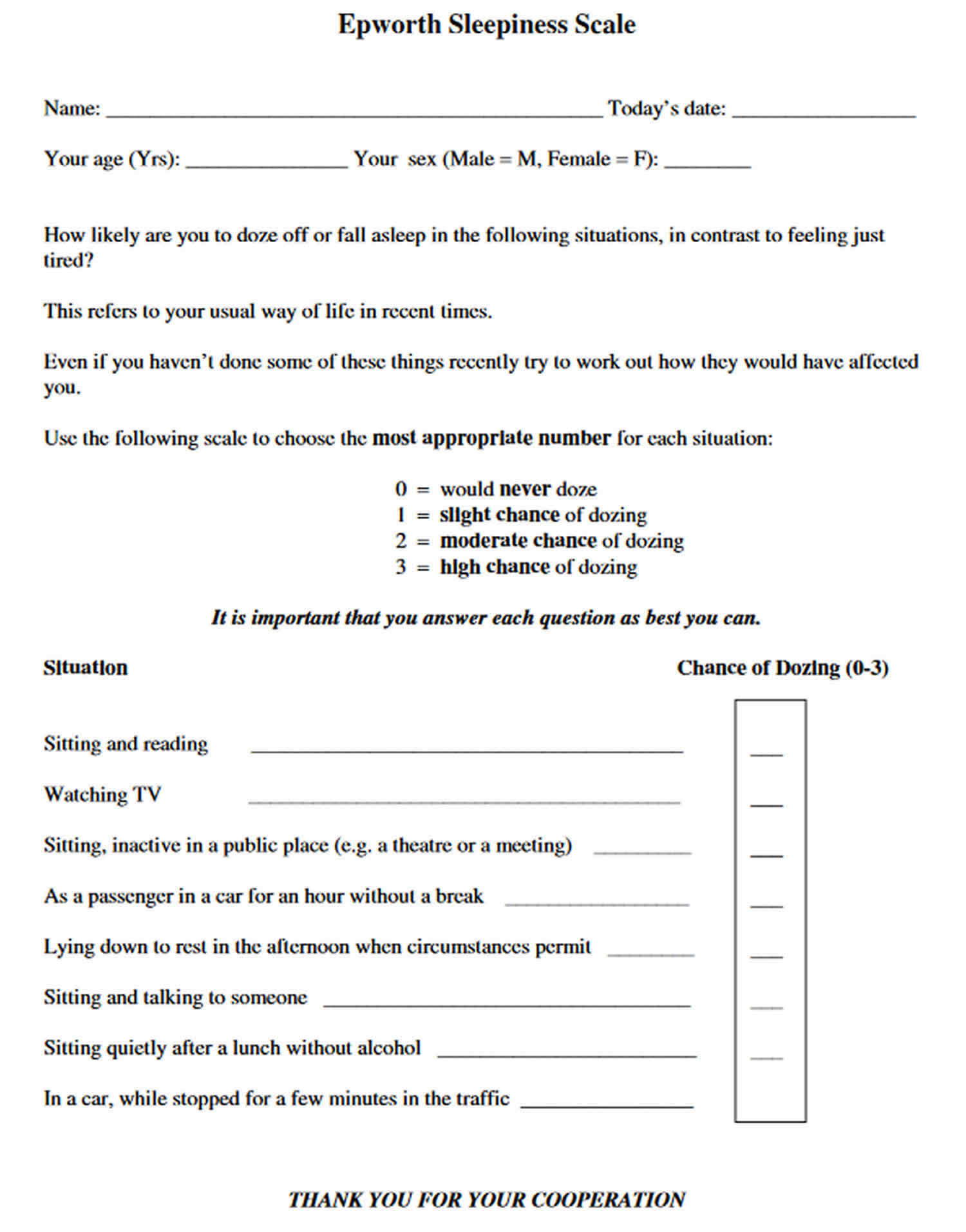
It may also help to fill out an Epworth Sleepiness Scale questionnaire. This asks how likely you’ll be to doze off in a number of different situations, such as watching TV or sitting in a meeting. The final score will help your doctor determine whether you may have a sleep disorder. For example, a score of 16-24 means you’re excessively sleepy and should consider seeking medical attention. A score of eight to nine is considered average during the daytime.
Figure 1. Epworth Sleepiness Scale
Central sleep apnea diagnostic criteria
The diagnostic criteria for central sleep apnea were published by the International Classification of Sleep Disorders – Third Edition (ICSD-3) 14 and varies according to the type of central sleep apnea 30. The diagnostic criteria for central sleep apnea generally requires evidence of recurrent central apneas on polysomnography recording and exclusion of alternative diagnoses 14. Central apnea is defined as a cessation of flow during sleep for at least 10 seconds without effort 15:
- Diagnosis of primary central sleep apnea (CSA) can be made if polysomnography reveals ≥5 central apneas and/or central hypopneas per hour of sleep, with a total number of these central events being >50% of total respiratory events in the apnea-hypopnea index with no evidence of Cheyne-Stokes breathing 15. Additionally, there must be at least one complaint related to disrupted sleep, i.e., sleepiness, insomnia, awakening with shortness of breath, snoring, or witnessed apneas.
- Diagnosis of central sleep apnea (CSA) with Cheyne-Stokes breathing (CSB) requires the criteria of primary central sleep apnea with 3 or more consecutive central apneas or hypopneas separated by a crescendo–decrescendo respiratory pattern with a cycle length of ≥40 seconds.
- Diagnosis of treatment-emergent central apnea (TECSA) requires to have a primary diagnosis of obstructive sleep apnea (OSA) with an apnea-hypopnea index [AHI] ≥ 5 obstructive respiratory events per hour of sleep followed by resolution of the obstructive sleep apnea (OSA) and emergence or persistence of central sleep apnea (CSA) (not explained by the presence of other disease or substance) during positive airway pressure (PAP) titration study.
Central sleep apnea treatment
Central sleep apnea treatments may include:
- Addressing associated medical problems. Possible causes of central sleep apnea include other disorders, and treating those conditions may help your central sleep apnea. For example, if central sleep apnea is due to heart failure, the goal is to treat the heart failure itself.
- Reduction of opioid medications. If opioid medications are causing your central sleep apnea, your doctor may gradually reduce your dose of those medications.
- Continuous positive airway pressure (CPAP). This method, also used to treat obstructive sleep apnea, involves wearing a mask over your nose or your nose and mouth while you sleep. CPAP is usually the first treatment given for central sleep apnea. The mask is attached to a small pump that supplies a continuous amount of pressurized air to hold open your upper airway. CPAP may prevent the airway closure that can trigger central sleep apnea. As with obstructive sleep apnea, it’s important that you use the device only as directed. If your mask is uncomfortable or the pressure feels too strong, talk with your doctor. Several types of masks are available. Doctors can also adjust the air pressure.
- Adaptive servo-ventilation (ASV). If CPAP hasn’t effectively treated your condition, you may be given adaptive servo-ventilation (ASV). Like CPAP, adaptive servo-ventilation also delivers pressurized air. Unlike CPAP, adaptive servo-ventilation adjusts the amount of pressure during inhalation on a breath-by-breath basis to smooth out the breathing pattern. The device may also automatically deliver a breath if you haven’t taken a breath within a certain number of seconds. Adaptive servo-ventilation (ASV) isn’t recommended for people with symptomatic heart failure 30. A multicenter largest trial (SERVE-HF) revealed that the use of adaptive servo-ventilation (ASV) was associated with increased the risk of death in heart failure patients with reduced ejection fraction 31. Therefore, adaptive servo-ventilation (ASV) is not recommended for the treatment of central sleep apnea in people with heart failure.
- Bilevel positive airway pressure (BPAP). Like adaptive servo-ventilation, bilevel positive airway pressure (BPAP) delivers pressure when you breathe in and a different amount of pressure when you breathe out. Unlike adaptive servo-ventilation, the amount of pressure during inspiration is fixed rather than variable. Bilevel positive airway pressure (BPAP) can also be configured to deliver a breath if you haven’t taken a breath within a certain number of seconds. Dohi et al. 32 suggested the effectiveness of BPAP in patients with heart failure and central sleep apnea with Cheyne-Stokes Breathing (CSB). BPAP acts to normalize the apnea-hypopnea index (AHI) by increasing ventilation and augmenting alveolar volume. A longitudinal cross-section study also suggested using CPAP and BiPAP to treat opioid-related central sleep apnea 33. Be sure to talk to your doctor about the potential risks of BPAP if your doctor is considering this therapy and you have heart failure.
- Supplemental oxygen. Using supplemental oxygen while you sleep may help if you have central sleep apnea. Various devices are available to deliver oxygen to your lungs.
- Medications. Certain medications, such as acetazolamide (Diamox) or theophylline (Theo-24, Theochron), have been used to stimulate breathing in people with central sleep apnea. These medications may be prescribed to help your breathing as you sleep if you can’t tolerate positive airway pressure. These medications may also be used to prevent central sleep apnea in high altitude.
Central sleep apnea mechanical devices
Continuous positive airway pressure (CPAP) has been recommended as the first-line therapy for central sleep apnea (CSA). Available literature and data support CPAP’s beneficial effect on central sleep apnea 34, 35. It can be explained by its ability to maintain airway patency, stabilizing the compensatory ventilatory output. In concurrent obstructive episodes, CPAP is a reasonable therapeutic option. The Canadian CPAP (CANPAP) trial was the most extensive randomized controlled study to evaluate the effect of CPAP on morbidity and mortality in patients with central sleep apnea (CSA) and heart failure 36. The study did reveal a modest reduction in mean apnea-hypopnea index (AHI) to 19 events per hour of sleep without significant effect on mortality. A subsequent post hoc analysis (a statistical analysis specified after a study has been concluded and the data collected) showed a reduction in mortality rate in those patients who responded to CPAP therapy 37.
Bilevel positive airway pressure (BPAP) can be a viable option in hypercapnic central sleep apnea, especially if the patient is unresponsive to CPAP. Dohi et al. 32 suggested the effectiveness of bilevel positive airway pressure (BPAP) in patients with heart failure and central sleep apnea (CSA) with Cheyne-Stokes Breathing (CSB). Bi-level positive airway pressure ventilation (BPAP) acts to normalize the apnea-hypopnea index (AHI) by increasing ventilation and augmenting alveolar volume. A longitudinal cross-section study also suggested using CPAP and BPAP to treat opioid-related central sleep apnea (CSA) 33
Adaptive servo-ventilation (ASV) is a form of positive airway pressure that provides ventilatory support individualized to the patient’s effort. A servo-controlled inspiratory pressure is delivered over positive end-expiratory pressure based on the detection of apneas. It remains a therapeutic option for central sleep apnea (CSA) patients with preserved ejection fraction and improves AHI and left ventricular ejection fraction (LVEF) 30. A multicenter largest trial (SERVE-HF) revealed that the use of adaptive servo-ventilation (ASV) was associated with increased mortality in heart failure patients with reduced ejection fraction 31. Therefore, adaptive servo-ventilation (ASV) is not recommended for the treatment of central sleep apnea (CSA) in this particular group of patients 31.
Nocturnal oxygen therapy in previous trials has decreased the number of apneic episodes during sleep times for patients with congestive heart failure. It also improved NYHA functional class quality of life, and ejection fraction was noted at the end of 12-week in patients with central sleep apnea (CSA) 38. These findings were confirmed over 52 weeks in a similar trial, ensuring improved quality of life 39.
Unilateral placement of phrenic nerve stimulators is another treatment option for patients with central sleep apnea (CSA). A recent study suggested that phrenic nerve stimulation therapy was associated with decreased disease severity and improved quality of life 40. It also resulted in significant improvement in the arousal index, improved quality of life, and a decreased self-reported daytime sleepiness. These benefits were independent of heart failure status 40. Peripheral nerve stimulation works by restoring the normal physiological mechanics of breathing.
Different medications have been studied as a potential treatment for central sleep apnea. However, these medications remain investigational, and there is no approved pharmacological treatment for central sleep apnea (CSA). Hypnotics such as triazolam and zolpidem can reduce wakefulness and unstable sleep 41. These medications may lead to increased total sleep, decreased central apnea index, and a decrease in brief arousals 41.
Respiratory stimulants such as acetazolamide, a carbonic anhydrase inhibitor, work by causing mild metabolic acidosis, resulting in increased respiratory drive decreases the frequency of central apneas 42. Recently, other medications such as Buspirone and Mirtazapine have been studied 43, 44. Both drugs reduced the susceptibility to developing hypocapnic central apnea in individuals with spinal cord injuries. Theophylline, a non-selective adenosine receptors antagonist, has been used in the context of central sleep apneas in patients with heart failure, and the benefit may be attributed to inhibition of adenosine receptors located in the medulla leading to increasing ventilatory stimulation 45. A recent experimental study demonstrated that selective adenosine A1 receptor blockade could alleviate the cervical spinal cord injury sleep disordered breathing to significantly reduce apnea-hypopnea index following induced cervical spinal cord injury in rats 46.
Surgery or other procedures
A new therapy for people with symptomatic heart failure who have moderate to severe sleep apnea involves stimulation of the phrenic nerve that runs from the brain to the diaphragm called transvenous phrenic nerve stimulation. A nerve stimulator, which is implanted in under your skin in the upper chest, acts like a pacemaker to help you breathe normally during sleep. The device monitors your breathing and stimulates the phrenic nerve to generate a breath if you’ve gone too long without breathing during sleep. A device approved by the U.S. Food and Drug Administration (FDA) known as Remede System delivers an electrical pulse to the phrenic nerve that controls the diaphragm during sleep. Used for moderate to severe central sleep apnea, this system produces a steady breathing pattern. More study is needed.
Sleep apnea monitoring
If you have been diagnosed with sleep apnea, you will need to schedule regular check-ups to make sure that your treatment is working and whether you have any complications. You may need to repeat your sleep study to monitor your symptoms while using your treatment, especially if you gain or lose a lot of weight. You may also need treatment for other health conditions that caused your sleep apnea or can make it worse.
Central sleep apnea prognosis
How well you do depends on the medical condition causing central sleep apnea. The prognosis is usually favorable for people with idiopathic central sleep apnea.
If not treated, central sleep apnea may cause:
- Anxiety and depression
- Loss of interest in sex
- Poor performance at work or school
Daytime sleepiness because of central sleep apnea can increase the risk of:
- Motor vehicle accidents from driving while sleepy
- Industrial accidents from falling asleep on the job.
Patients with sleep apnea syndrome are at increased risk of systemic complications, including systemic hypertension, pulmonary hypertension, arrhythmias including atrial fibrillation, sleep disturbances accompanied with excessive daytime sleepiness, mood disorders, chronic respiratory failure, narcolepsy, and hypercapnic respiratory failure 47. Heart failure patients with central sleep apnea (CSA) and Cheyne-Stokes breathing tend to have a worse prognosis, and treatment often includes optimization of heart failure therapy 48.
Adaptive servo-ventilation (ASV) is a therapy modality that delivers servo-controlled inspiratory pressure support on top of expiratory positive airway pressure. A recent study in 2015 showed that in patients with heart failure with reduced ejection fraction, adaptive servo-ventilation (ASV) was associated with increased all-cause and cardiovascular mortality without any significant benefit 4. There was no improvement in either symptoms or quality of life 49. There has been reportedly increased mortality in patients with heart failure with reduced ejection fraction in whom adaptive servo-ventilation was used 50.
- Badr, M.S., Javaheri, S. Central Sleep Apnea: a Brief Review. Curr Pulmonol Rep 8, 14–21 (2019). https://doi.org/10.1007/s13665-019-0221-z[↩]
- Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP. Pathophysiology of sleep apnea. Physiol Rev. 2010 Jan;90(1):47-112. doi: 10.1152/physrev.00043.2008. Erratum in: Physiol Rev.2010 Apr;90(2):797-8.[↩]
- Wellman A, Jordan AS, Malhotra A, Fogel RB, Katz ES, Schory K, Edwards JK, White DP. Ventilatory control and airway anatomy in obstructive sleep apnea. Am J Respir Crit Care Med. 2004 Dec 1;170(11):1225-32. doi: 10.1164/rccm.200404-510OC[↩]
- Rana AM, Sankari A. Central Sleep Apnea. [Updated 2023 Jun 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK578199[↩][↩][↩][↩][↩][↩][↩]
- Sankari A, Bascom A, Oomman S, Badr MS. Sleep disordered breathing in chronic spinal cord injury. J Clin Sleep Med. 2014 Jan 15;10(1):65-72. doi: 10.5664/jcsm.3362[↩]
- Sankari A, Bascom AT, Chowdhuri S, Badr MS. Tetraplegia is a risk factor for central sleep apnea. J Appl Physiol (1985). 2014 Feb 1;116(3):345-53. doi: 10.1152/japplphysiol.00731.2013. Epub 2013 Oct 10. Erratum in: J Appl Physiol (1985). 2014 Oct 15;117(8):940.[↩]
- Javaheri S, Barbe F, Campos-Rodriguez F, Dempsey JA, Khayat R, Javaheri S, Malhotra A, Martinez-Garcia MA, Mehra R, Pack AI, Polotsky VY, Redline S, Somers VK. Sleep Apnea: Types, Mechanisms, and Clinical Cardiovascular Consequences. J Am Coll Cardiol. 2017 Feb 21;69(7):841-858. doi: 10.1016/j.jacc.2016.11.069[↩]
- Rudrappa M, Modi P, Bollu PC. Cheyne Stokes Respirations. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448165[↩][↩][↩]
- Vargas-Ramirez L, Gonzalez-Garcia M, Franco-Reyes C, Bazurto-Zapata MA. Severe sleep apnea, Cheyne-Stokes respiration and desaturation in patients with decompensated heart failure at high altitude. Sleep Sci. 2018 May-Jun;11(3):146-151. doi: 10.5935/1984-0063.20180028[↩]
- Granitza P, Kraemer JF, Schoebel C, Penzel T, Kurths J, Wessel N. Is dynamic desaturation better than a static index to quantify the mortality risk in heart failure patients with Cheyne-Stokes respiration? Chaos. 2018 Oct;28(10):106312. doi: 10.1063/1.5039601[↩]
- Tinoco A, Mortara DW, Hu X, Sandoval CP, Pelter MM. ECG derived Cheyne-Stokes respiration and periodic breathing are associated with cardiorespiratory arrest in intensive care unit patients. Heart Lung. 2019 Mar-Apr;48(2):114-120. doi: 10.1016/j.hrtlng.2018.09.003[↩]
- Kim Y, Kim S, Ryu DR, Lee SY, Im KB. Factors Associated with Cheyne-Stokes Respiration in Acute Ischemic Stroke. J Clin Neurol. 2018 Oct;14(4):542-548. doi: 10.3988/jcn.2018.14.4.542[↩]
- Donovan LM, Kapur VK. Prevalence and Characteristics of Central Compared to Obstructive Sleep Apnea: Analyses from the Sleep Heart Health Study Cohort. Sleep. 2016 Jul 1;39(7):1353-9. doi: 10.5665/sleep.5962[↩]
- Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014 Nov;146(5):1387-1394. doi: 10.1378/chest.14-0970[↩][↩][↩]
- Berry RB, Brooks R, Gamaldo C, Harding SM, Lloyd RM, Quan SF, Troester MT, Vaughn BV. AASM Scoring Manual Updates for 2017 (Version 2.4). J Clin Sleep Med. 2017 May 15;13(5):665-666. doi: 10.5664/jcsm.6576[↩][↩][↩]
- Nigam G, Riaz M, Chang ET, Camacho M. Natural history of treatment-emergent central sleep apnea on positive airway pressure: A systematic review. Ann Thorac Med. 2018 Apr-Jun;13(2):86-91. doi: 10.4103/atm.ATM_321_17[↩]
- Endo Y, Suzuki M, Inoue Y, Sato M, Namba K, Hasegawa M, Matsuura M. Prevalence of complex sleep apnea among Japanese patients with sleep apnea syndrome. Tohoku J Exp Med. 2008 Aug;215(4):349-54. doi: 10.1620/tjem.215.349[↩]
- Gilmartin GS, Daly RW, Thomas RJ. Recognition and management of complex sleep-disordered breathing. Curr Opin Pulm Med. 2005 Nov;11(6):485-93. doi: 10.1097/01.mcp.0000183061.98665.b0[↩]
- Kuzniar TJ, Pusalavidyasagar S, Gay PC, Morgenthaler TI. Natural course of complex sleep apnea–a retrospective study. Sleep Breath. 2008 May;12(2):135-9. doi: 10.1007/s11325-007-0140-z[↩]
- Javaheri S, Smith J, Chung E. The prevalence and natural history of complex sleep apnea. J Clin Sleep Med. 2009 Jun 15;5(3):205-11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2699163[↩]
- Dernaika T, Tawk M, Nazir S, Younis W, Kinasewitz GT. The significance and outcome of continuous positive airway pressure-related central sleep apnea during split-night sleep studies. Chest. 2007 Jul;132(1):81-7. doi: 10.1378/chest.06-2562[↩]
- Cassel W, Canisius S, Becker HF, Leistner S, Ploch T, Jerrentrup A, Vogelmeier C, Koehler U, Heitmann J. A prospective polysomnographic study on the evolution of complex sleep apnoea. Eur Respir J. 2011 Aug;38(2):329-37. doi: 10.1183/09031936.00162009[↩]
- Yaegashi H, Fujimoto K, Abe H, Orii K, Eda S, Kubo K. Characteristics of Japanese patients with complex sleep apnea syndrome: a retrospective comparison with obstructive sleep apnea syndrome. Intern Med. 2009;48(6):427-32. doi: 10.2169/internalmedicine.48.1459[↩]
- Morgenthaler TI, Kagramanov V, Hanak V, Decker PA. Complex sleep apnea syndrome: is it a unique clinical syndrome? Sleep. 2006 Sep;29(9):1203-9. doi: 10.1093/sleep/29.9.1203[↩]
- Lehman S, Antic NA, Thompson C, Catcheside PG, Mercer J, McEvoy RD. Central sleep apnea on commencement of continuous positive airway pressure in patients with a primary diagnosis of obstructive sleep apnea-hypopnea. J Clin Sleep Med. 2007 Aug 15;3(5):462-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1978327[↩]
- Tietjens JR, Claman D, Kezirian EJ, De Marco T, Mirzayan A, Sadroonri B, Goldberg AN, Long C, Gerstenfeld EP, Yeghiazarians Y. Obstructive Sleep Apnea in Cardiovascular Disease: A Review of the Literature and Proposed Multidisciplinary Clinical Management Strategy. J Am Heart Assoc. 2019 Jan 8;8(1):e010440. doi: 10.1161/JAHA.118.010440[↩]
- Bazoukis G, Bollepalli SC, Chung CT, Li X, Tse G, Bartley BL, Batool-Anwar S, Quan SF, Armoundas AA. Application of artificial intelligence in the diagnosis of sleep apnea. J Clin Sleep Med. 2023 Jul 1;19(7):1337-1363. doi: 10.5664/jcsm.10532[↩]
- Kapoor M, Greenough G. Home Sleep Tests for Obstructive Sleep Apnea (OSA). J Am Board Fam Med. 2015 Jul-Aug;28(4):504-9. doi: 10.3122/jabfm.2015.04.140266[↩]
- Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A. Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med. 1998 Jan;157(1):144-8. doi: 10.1164/ajrccm.157.1.9706079[↩]
- Aurora RN, Chowdhuri S, Ramar K, Bista SR, Casey KR, Lamm CI, Kristo DA, Mallea JM, Rowley JA, Zak RS, Tracy SL. The treatment of central sleep apnea syndromes in adults: practice parameters with an evidence-based literature review and meta-analyses. Sleep. 2012 Jan 1;35(1):17-40. doi: 10.5665/sleep.1580[↩][↩][↩]
- Cowie MR, Woehrle H, Wegscheider K, Angermann C, d’Ortho MP, Erdmann E, Levy P, Simonds AK, Somers VK, Zannad F, Teschler H. Adaptive Servo-Ventilation for Central Sleep Apnea in Systolic Heart Failure. N Engl J Med. 2015 Sep 17;373(12):1095-105. doi: 10.1056/NEJMoa1506459[↩][↩][↩]
- Dohi T, Kasai T, Narui K, Ishiwata S, Ohno M, Yamaguchi T, Momomura S. Bi-level positive airway pressure ventilation for treating heart failure with central sleep apnea that is unresponsive to continuous positive airway pressure. Circ J. 2008 Jul;72(7):1100-5. doi: 10.1253/circj.72.1100[↩][↩]
- Schoebel C, Ghaderi A, Amra B, Soltaninejad F, Penzel T, Fietze I. Comparison of Therapeutic Approaches to Addicted Patients with Central Sleep Apnea. Tanaffos. 2018 Mar;17(3):155-162. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6428378[↩][↩]
- Hoffstein V, Slutsky AS. Central sleep apnea reversed by continuous positive airway pressure. Am Rev Respir Dis. 1987 May;135(5):1210-2. doi: 10.1164/arrd.1987.135.5.1210[↩]
- Sin DD, Logan AG, Fitzgerald FS, Liu PP, Bradley TD. Effects of continuous positive airway pressure on cardiovascular outcomes in heart failure patients with and without Cheyne-Stokes respiration. Circulation. 2000 Jul 4;102(1):61-6. doi: 10.1161/01.cir.102.1.61[↩]
- Bradley TD, Logan AG, Kimoff RJ, Sériès F, Morrison D, Ferguson K, Belenkie I, Pfeifer M, Fleetham J, Hanly P, Smilovitch M, Tomlinson G, Floras JS; CANPAP Investigators. Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med. 2005 Nov 10;353(19):2025-33. doi: 10.1056/NEJMoa051001[↩]
- Arzt M, Floras JS, Logan AG, Kimoff RJ, Series F, Morrison D, Ferguson K, Belenkie I, Pfeifer M, Fleetham J, Hanly P, Smilovitch M, Ryan C, Tomlinson G, Bradley TD; CANPAP Investigators. Suppression of central sleep apnea by continuous positive airway pressure and transplant-free survival in heart failure: a post hoc analysis of the Canadian Continuous Positive Airway Pressure for Patients with Central Sleep Apnea and Heart Failure Trial (CANPAP). Circulation. 2007 Jun 26;115(25):3173-80. doi: 10.1161/CIRCULATIONAHA.106.683482[↩]
- Sakakibara M, Sakata Y, Usui K, Hayama Y, Kanda S, Wada N, Matsui Y, Suto Y, Shimura S, Tanabe T. Effectiveness of short-term treatment with nocturnal oxygen therapy for central sleep apnea in patients with congestive heart failure. J Cardiol. 2005 Aug;46(2):53-61.[↩]
- Sasayama S, Izumi T, Matsuzaki M, Matsumori A, Asanoi H, Momomura S, Seino Y, Ueshima K; CHF-HOT Study Group. Improvement of quality of life with nocturnal oxygen therapy in heart failure patients with central sleep apnea. Circ J. 2009 Jul;73(7):1255-62. doi: 10.1253/circj.cj-08-1210[↩]
- Fudim M, Spector AR, Costanzo MR, Pokorney SD, Mentz RJ, Jagielski D, Augostini R, Abraham WT, Ponikowski PP, McKane SW, Piccini JP. Phrenic Nerve Stimulation for the Treatment of Central Sleep Apnea: A Pooled Cohort Analysis. J Clin Sleep Med. 2019 Dec 15;15(12):1747-1755. doi: 10.5664/jcsm.8076[↩][↩]
- Bonnet MH, Dexter JR, Arand DL. The effect of triazolam on arousal and respiration in central sleep apnea patients. Sleep. 1990 Feb;13(1):31-41. doi: 10.1093/sleep/13.1.31[↩][↩]
- Ginter G, Sankari A, Eshraghi M, Obiakor H, Yarandi H, Chowdhuri S, Salloum A, Badr MS. Effect of acetazolamide on susceptibility to central sleep apnea in chronic spinal cord injury. J Appl Physiol (1985). 2020 Apr 1;128(4):960-966. doi: 10.1152/japplphysiol.00532.2019[↩]
- Prowting J, Maresh S, Vaughan S, Kruppe E, Alsabri B, Badr MS, Sankari A. Mirtazapine reduces susceptibility to hypocapnic central sleep apnea in males with sleep-disordered breathing: a pilot study. J Appl Physiol (1985). 2021 Jul 1;131(1):414-423. doi: 10.1152/japplphysiol.00838.2020[↩]
- Maresh S, Prowting J, Vaughan S, Kruppe E, Alsabri B, Yarandi H, Badr MS, Sankari A. Buspirone decreases susceptibility to hypocapnic central sleep apnea in chronic SCI patients. J Appl Physiol (1985). 2020 Oct 1;129(4):675-682. doi: 10.1152/japplphysiol.00435.2020[↩]
- Javaheri S, Parker TJ, Wexler L, Liming JD, Lindower P, Roselle GA. Effect of theophylline on sleep-disordered breathing in heart failure. N Engl J Med. 1996 Aug 22;335(8):562-7. doi: 10.1056/NEJM199608223350805[↩]
- Sankari A, Minic Z, Farshi P, Shanidze M, Mansour W, Liu F, Mao G, Goshgarian HG. Sleep disordered breathing induced by cervical spinal cord injury and effect of adenosine A1 receptors modulation in rats. J Appl Physiol (1985). 2019 Dec 1;127(6):1668-1676. doi: 10.1152/japplphysiol.00563.2019[↩]
- Chaudhary BA, Speir WA Jr. Sleep apnea syndromes. South Med J. 1982 Jan;75(1):39-45. doi: 10.1097/00007611-198201000-00011[↩]
- Terziyski K, Draganova A. Central Sleep Apnea with Cheyne-Stokes Breathing in Heart Failure – From Research to Clinical Practice and Beyond. Adv Exp Med Biol. 2018;1067:327-351. doi: 10.1007/5584_2018_146[↩]
- Cowie MR, Woehrle H, Wegscheider K, Vettorazzi E, Lezius S, Koenig W, Weidemann F, Smith G, Angermann C, d’Ortho MP, Erdmann E, Levy P, Simonds AK, Somers VK, Zannad F, Teschler H. Adaptive servo-ventilation for central sleep apnoea in systolic heart failure: results of the major substudy of SERVE-HF. Eur J Heart Fail. 2018 Mar;20(3):536-544. doi: 10.1002/ejhf.1048[↩]
- Iftikhar IH, Khayat RN. Central sleep apnea treatment in patients with heart failure with reduced ejection fraction: a network meta-analysis. Sleep Breath. 2022 Sep;26(3):1227-1235. doi: 10.1007/s11325-021-02512-y[↩]





