Contents
- Congestive Heart failure
- How your Heart Works
- What is ejection fraction?
- Types of ejection fraction
- What’s an unhealthy ejection fraction?
- What is the formula for ejection fraction?
- Who should have their ejection fraction measured?
- What are the tests used to measure ejection fraction?
- Is ejection fraction the only test for heart failure?
- How often should my ejection fraction be measured?
- How will I know if my ejection fraction is improving?
- Who is at Risk for Congestive Heart failure?
- Types of Congestive Heart failure
- Right-sided heart failure
- Left-sided heart failure
- Heart failure with preserved ejection fraction
- Heart failure with preserved ejection fraction causes
- Heart failure with preserved ejection fraction pathophysiology
- Heart failure with preserved ejection fraction symptoms
- Heart failure with preserved ejection fraction diagnosis
- Heart failure with preserved ejection fraction treatment
- Heart failure with preserved ejection fraction prognosis
- Heart failure with reduced ejection fraction
- Heart failure with mid-range ejection fraction
- Congestive heart failure stages
- Congestive heart failure causes
- Congestive heart failure prevention
- Congestive heart failure symptoms
- Congestive heart failure complications
- Congestive heart failure diagnosis
- Congestive heart failure treatment
- Lifestyle and home remedies
- Medications
- Surgery and medical devices
- Cardiac rehabilitation
- Stage A heart failure treatment
- Stage B heart failure treatment
- Stage C heart failure treatment
- Stage D heart failure treatment
- Stages C and D heart failure with preserved ejection fraction treatment
- End-of-life care and heart failure
- Congestive heart failure prognosis
- Congestive heart failure life expectancy
- Living with congestive heart failure
Congestive Heart failure
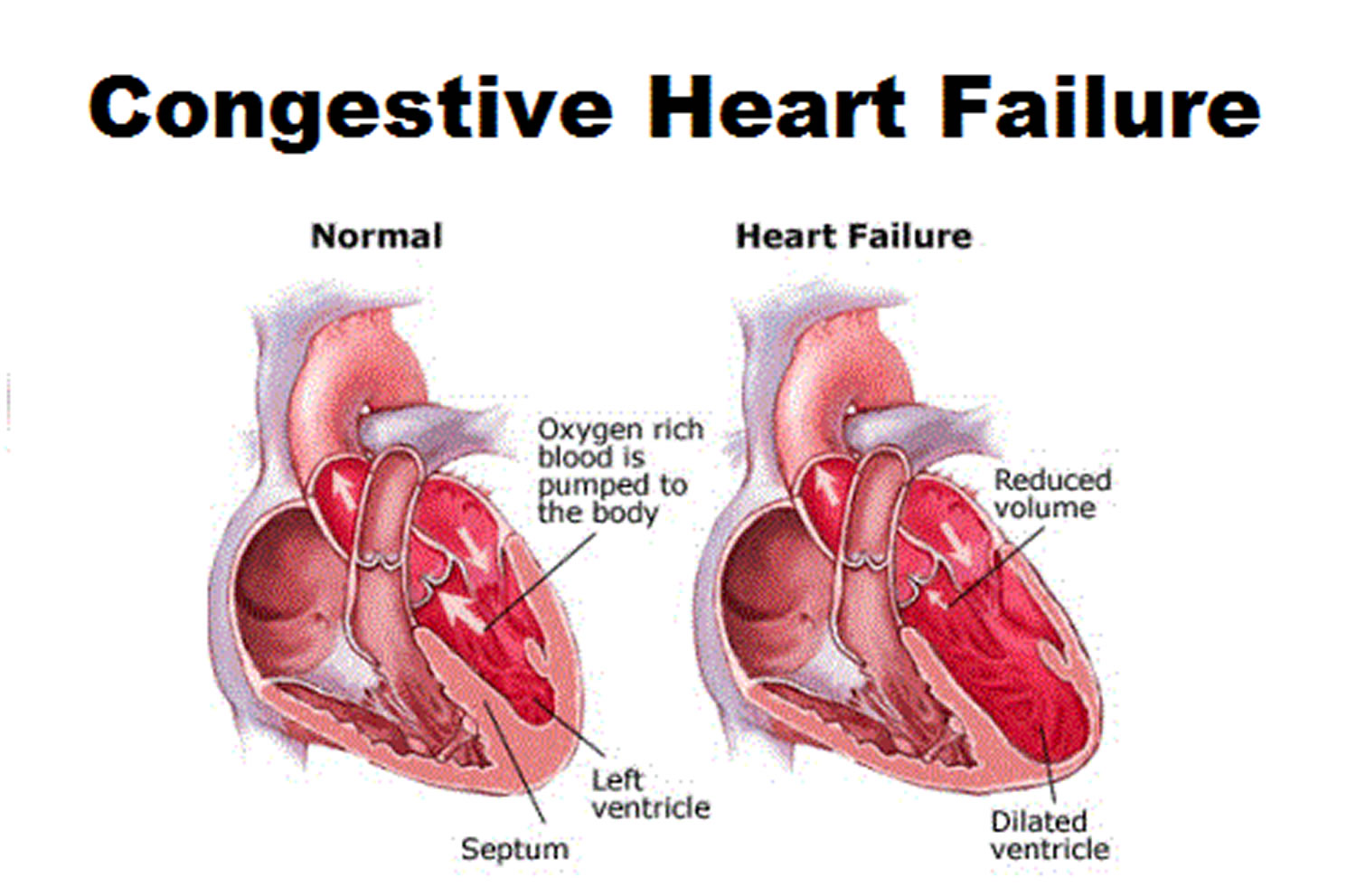
Congestive Heart Failure (CHF) also known as heart failure is a heart condition that develops when your heart muscle has become too weak to pump blood and oxygen effectively through your body to support the muscles and organs in your body. Heart failure can also happen if your heart becomes too stiff to fill up with blood properly, so not enough blood and oxygen is pumped around your body. As a result, your muscles and organs don’t get enough oxygen and nutrients. This may cause fluid to build up in your body, legs and make you feel breathless or tired. The term “heart failure” does not mean that your heart has stopped. However, heart failure is a serious condition that needs medical care.
Other names for Heart Failure
- Congestive heart failure.
- Left-side heart failure. This is when the heart can’t pump enough oxygen-rich blood to the body.
- Right-side heart failure. This is when the heart can’t fill with enough blood.
- Cor pulmonale. This term refers to right-side heart failure caused by high blood pressure in the pulmonary arteries and right ventricle (lower right heart chamber).
In 2024, more than 6.7 million adults 20 years old or older in the United States have heart failure, according to the American Heart Association 1.
Heart failure can develop suddenly (the acute kind) or over time as your heart gets weaker (the chronic kind). Heart failure is usually an ongoing (chronic) condition — unlike heart attacks, which occur suddenly and require immediate treatment (acute). However, both conditions can be related: a heart attack can cause ongoing muscle weakness and stiffness making your heart not able to fill up with enough blood that leads to long-term heart failure. In some cases, symptoms of heart failure can also start suddenly.
Heart failure can affect one or both sides of your heart. Left-sided and right-sided heart failure may have different causes. Most often, heart failure is caused by another medical condition that damages your heart. This includes coronary heart disease, heart inflammation, high blood pressure, cardiomyopathy, or an irregular heartbeat. Heart failure may not cause symptoms right away. But eventually, you may feel tired and short of breath and notice fluid buildup in your lower body, around your stomach, or your neck.
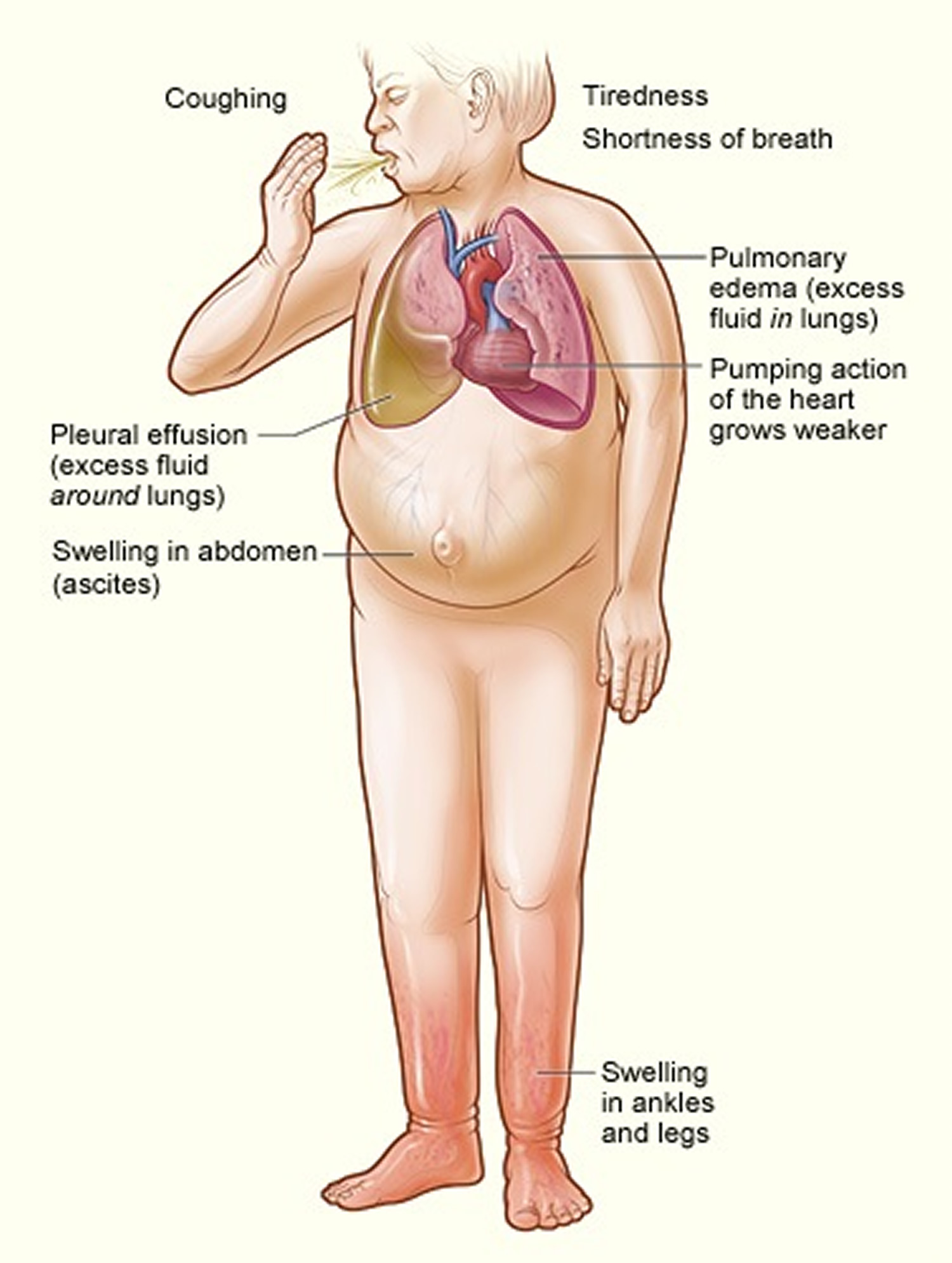
Your body depends on the heart’s pumping action to deliver oxygen- and nutrient-rich blood to the body’s cells. When the cells are nourished properly, the body can function normally. Heart failure, sometimes known as congestive heart failure, occurs when your heart muscle doesn’t pump blood as well as it should and the heart can’t pump enough blood to meet the body’s needs 2. With heart failure, the weakened heart can’t supply the cells with enough blood. This results in fatigue and shortness of breath and some people have coughing. Everyday activities such as walking, climbing stairs or carrying groceries can become very difficult. This inability may also result in fluid retention, which causes swelling, for example, in the legs, feet, or abdomen.
The term “heart failure” makes it sound like the heart is no longer working at all and there’s nothing that can be done, but that is not the case at all. Heart failure also doesn’t mean that your heart has stopped or is about to stop working.
Congestive heart failure is a type of heart failure which requires seeking timely medical attention, although sometimes heart failure and congestive heart failure, the two terms are used interchangeably.
As blood flow out of the heart slows, blood returning to the heart through the veins backs up, causing congestion in the body’s tissues. Often swelling (edema) results. Most often there’s swelling in the legs and ankles, but it can happen in other parts of the body, too.
Sometimes fluid collects in the lungs and interferes with breathing, causing shortness of breath, especially when a person is lying down. This is called pulmonary edema and if left untreated can cause respiratory distress.
Heart failure also affects the kidneys’ ability to dispose of sodium and water. This retained water also increases swelling in the body’s tissues (edema).
Congestive heart failure is a serious medical condition in which the heart cannot pump enough blood to meet the body’s needs. As blood flow out of the heart slows, blood returning to the heart through the veins backs up, causing congestion in the body’s tissues. Often swelling (edema) results. Most often there’s swelling in the legs and ankles, but it can happen in other parts of the body, too 3.
Sometimes fluid collects in the lungs and interferes with breathing, causing shortness of breath, especially when a person is lying down. This is called pulmonary edema and if left untreated can cause respiratory distress 3.
Heart failure also affects the kidneys’ ability to dispose of sodium and water. This retained water also increases swelling in the body’s tissues (edema) 3.
Congestive heart failure is often caused by hypertension, diabetes, or coronary heart disease, gradually leave your heart too weak or stiff to fill and pump efficiently.
It is estimated that 6.7 million adults in the United States have congestive heart failure 2 and at least 10 million in Europe 4. Congestive heart failure is one of the most common reasons those aged 65 and over are hospitalized 5.
- There were 1 million hospitalizations for congestive heart failure in 2000 and in 2010.
- About half of people who develop heart failure die within 5 years of diagnosis 6.
- Most congestive heart failure hospitalizations were for those aged 65 and over, but the proportion under age 65 increased significantly from 23% in 2000 to 29% in 2010.
- The overall rate of congestive heart failure hospitalization per 10,000 population did not change significantly from 2000 to 2010 (35.5 compared with 32.8), but the trends were different for those under and over age 65.
- From 2000 to 2010, the rate of congestive heart failure hospitalization for males under age 65 increased significantly while the rate for females aged 65 and over decreased significantly.
- In both 2000 and in 2010, a greater share of inpatients under age 65, compared with those aged 65 and over, were discharged to their homes.
Heart failure can damage your liver or kidneys. Other conditions it can lead to include pulmonary hypertension or other heart conditions, such as an irregular heartbeat, heart valve disease, and sudden cardiac arrest. One way to prevent heart failure is to control conditions that cause heart failure, such as coronary artery disease, high blood pressure, diabetes or obesity.
Some common symptoms of heart failure include:
- Chest pain (angina).
- Dizziness.
- Fatigue.
- Shortness of breath (dyspnea).
- Swollen hands or feet (edema).
Your doctor will diagnose heart failure based on your medical and family history, a physical exam, and results from imaging and blood tests.
Currently, heart failure is a serious condition and not all conditions that lead to heart failure can be reversed, but treatments can improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes — such as exercising, reducing salt in your diet, managing stress and losing weight — can improve your quality of life.
Heart failure therapies treat the underlying cause of low ejection fraction. In some cases of heart failure, the heart can’t fill with enough blood. In other cases, the heart can’t pump blood to the rest of the body with enough force. Some people have both problems. For heart failure due to an arrhythmia, you may benefit from a biventricular pacemaker. People with heart failure due to other causes, like high blood pressure, may need medications.
Heart failure treatments include:
- Biventricular pacemaker.
- Heart failure medications.
- Heart transplant.
- Heart valve repair or replacement.
- Implantable cardioverter defibrillator (ICD).
You can take additional steps to relieve strain on your heart and get the most out of treatment. Many people with mild heart failure enhance their quality of life by doing these:
- Increasing physical activity. A cardiac rehabilitation program can help you safely get started. Talk to your doctor before starting a new exercise routine if you haven’t been physically active.
- Maintaining a healthy weight.
- Limiting the amount of sodium and volume of fluids you consume.
- Quitting unhealthy habits, such as smoking, recreational drugs and alcohol. Limit caffeine.
- Track your daily fluid intake. You may need a diuretic medication to help get rid of extra fluid in your body.
- Eat a heart-healthy diet. A dietitian or nutritionist can help you build a healthy, filling meal plan.
- Manage stress, either through yoga, meditation or other stress management techniques.
- Get plenty of sleep at night.
Figure 1. Congestive Heart Failure
Figure 2. Congestive heart failure signs and symptoms
[Source 7 ]See your doctor if you think you might have symptoms of heart failure. Call your local emergency services number and get emergency medical help if you have any of the following:
- Chest pain.
- Fainting or severe weakness.
- Rapid or irregular heartbeat with shortness of breath, chest pain or fainting.
- Sudden, severe shortness of breath and coughing up white or pink, foamy mucus.
These symptoms may be due to heart failure. But there are many other possible causes. Don’t try to diagnose yourself.
At the emergency room, doctors do tests to learn if your symptoms are due to heart failure or something else.
See your doctor right away if you have heart failure and:
- Your symptoms suddenly get worse.
- You develop a new symptom.
- You gain 5 pounds (2.3 kilograms) or more within a few days.
Such changes could mean that existing heart failure is getting worse or that treatment isn’t working.
How your Heart Works
Your heart is a muscular organ that pumps blood to your body. Your heart is at the center of your circulatory system. The circulatory system consists of a network of blood vessels, such as arteries, veins, and capillaries. These blood vessels carry blood to and from all areas of your body.
An electrical system controls your heart and uses electrical signals to contract the heart’s walls. When the heart walls contract, blood is pumped into your circulatory system. Inlet and outlet valves in your heart chambers ensure that blood flows in the right direction.
Your heart is vital to your health and nearly everything that goes on in your body. Without your heart’s pumping action, blood can’t move throughout your body.
Your blood carries the oxygen and nutrients that your organs need to work well. Blood also carries carbon dioxide (a waste product) to your lungs so you can breathe it out.
A healthy heart supplies your body with the right amount of blood and oxygen at the rate needed to work well. If disease or injury weakens your heart, your body’s organs won’t receive enough blood to work normally.
Your heart has 2 sides, separated by an inner wall called the septum. The right side of the heart pumps blood to your lungs to pick up oxygen. The left side of your heart receives the oxygen-rich blood from the lungs and pumps it to the body.
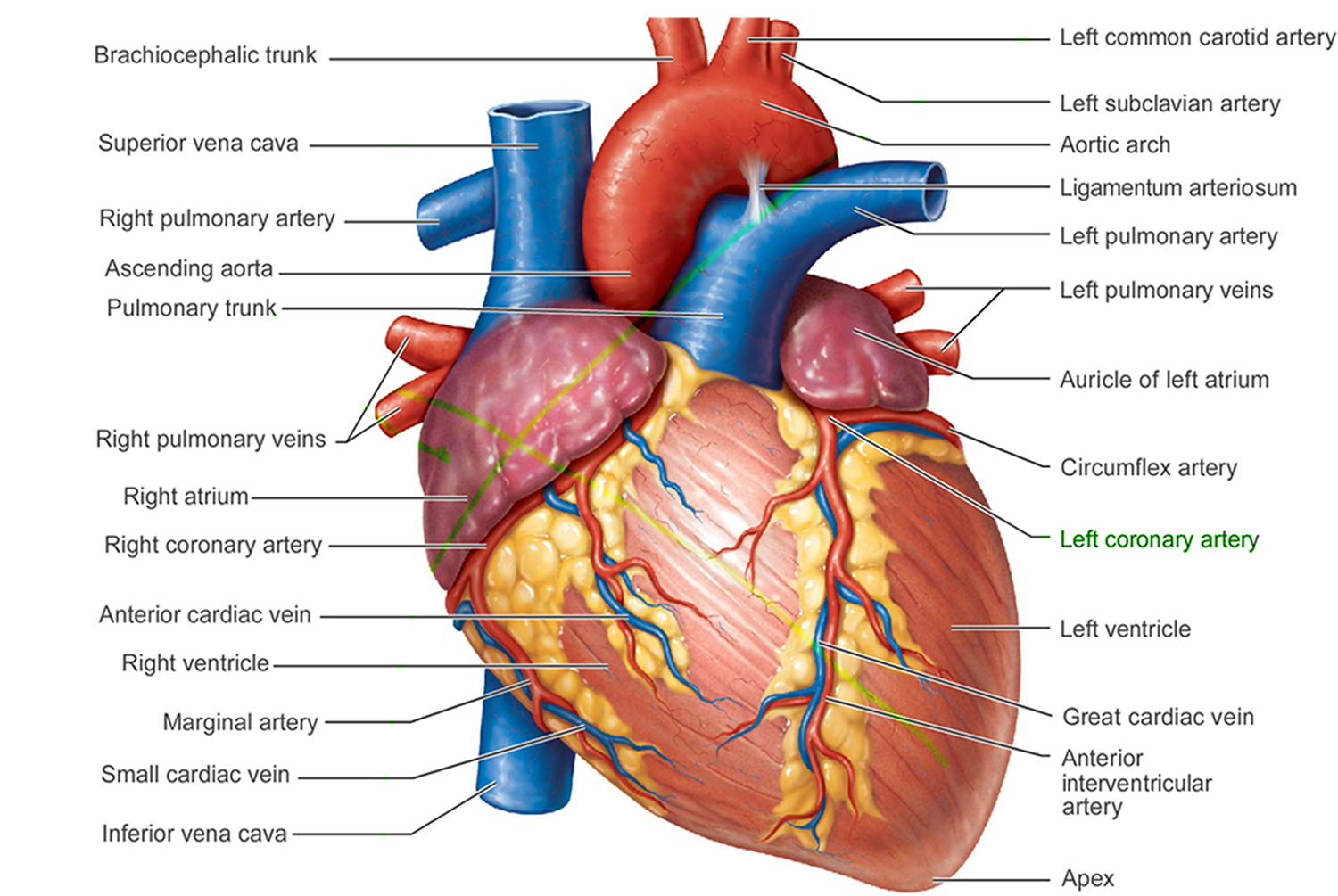
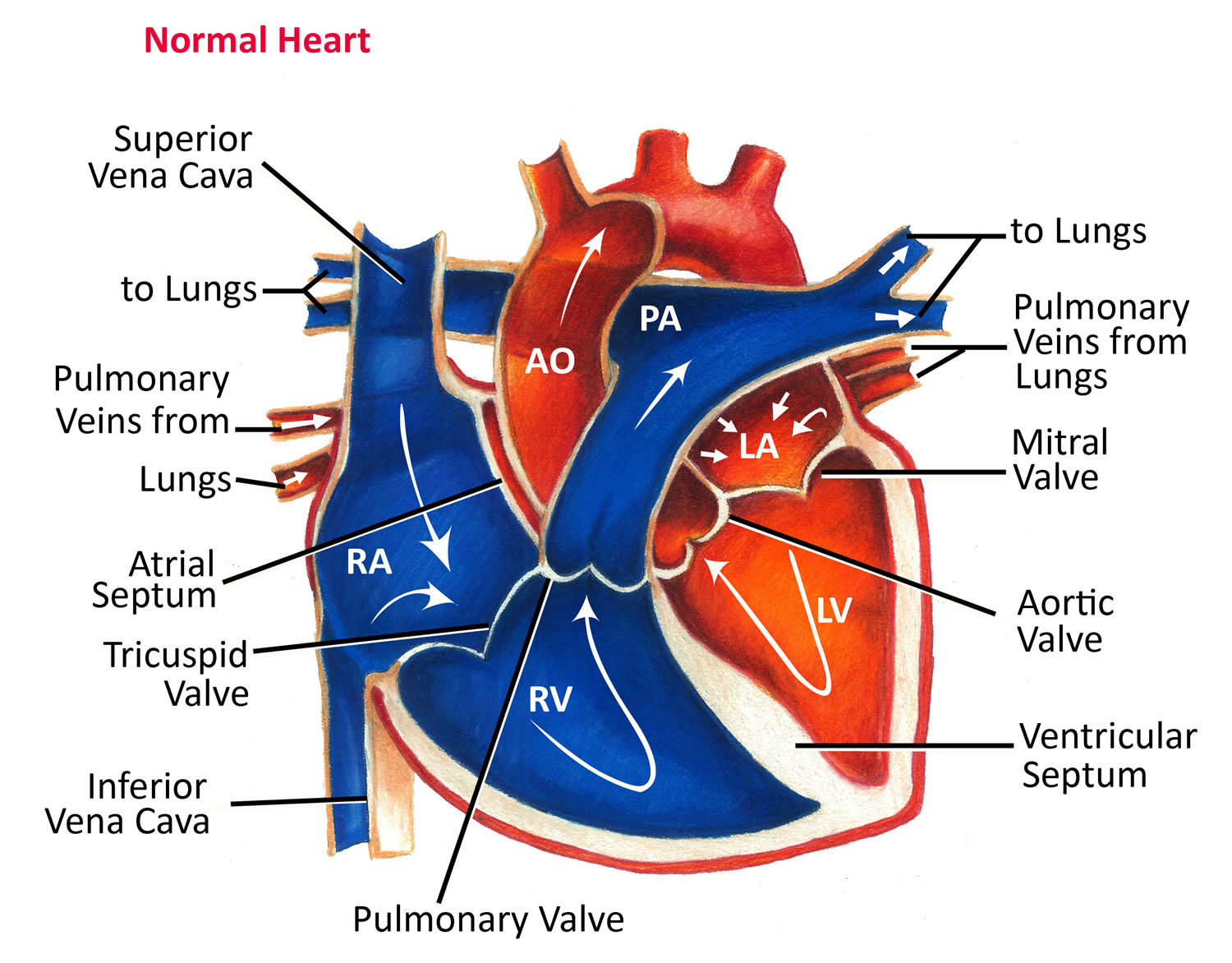
Figure 3. The anatomy of human heart
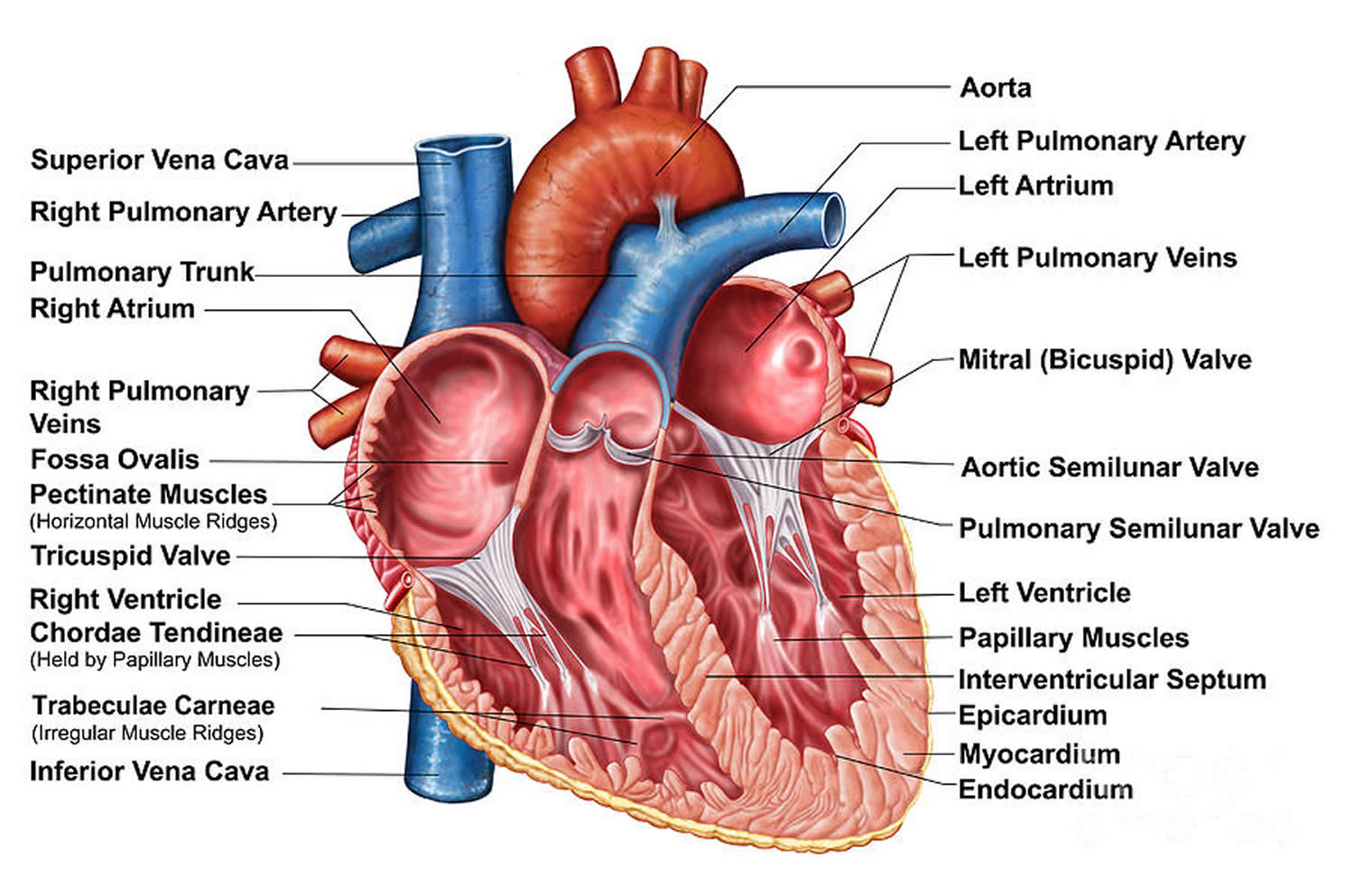
Figure 4. The anatomy of the heart chambers
Figure 5. Normal heart blood flow
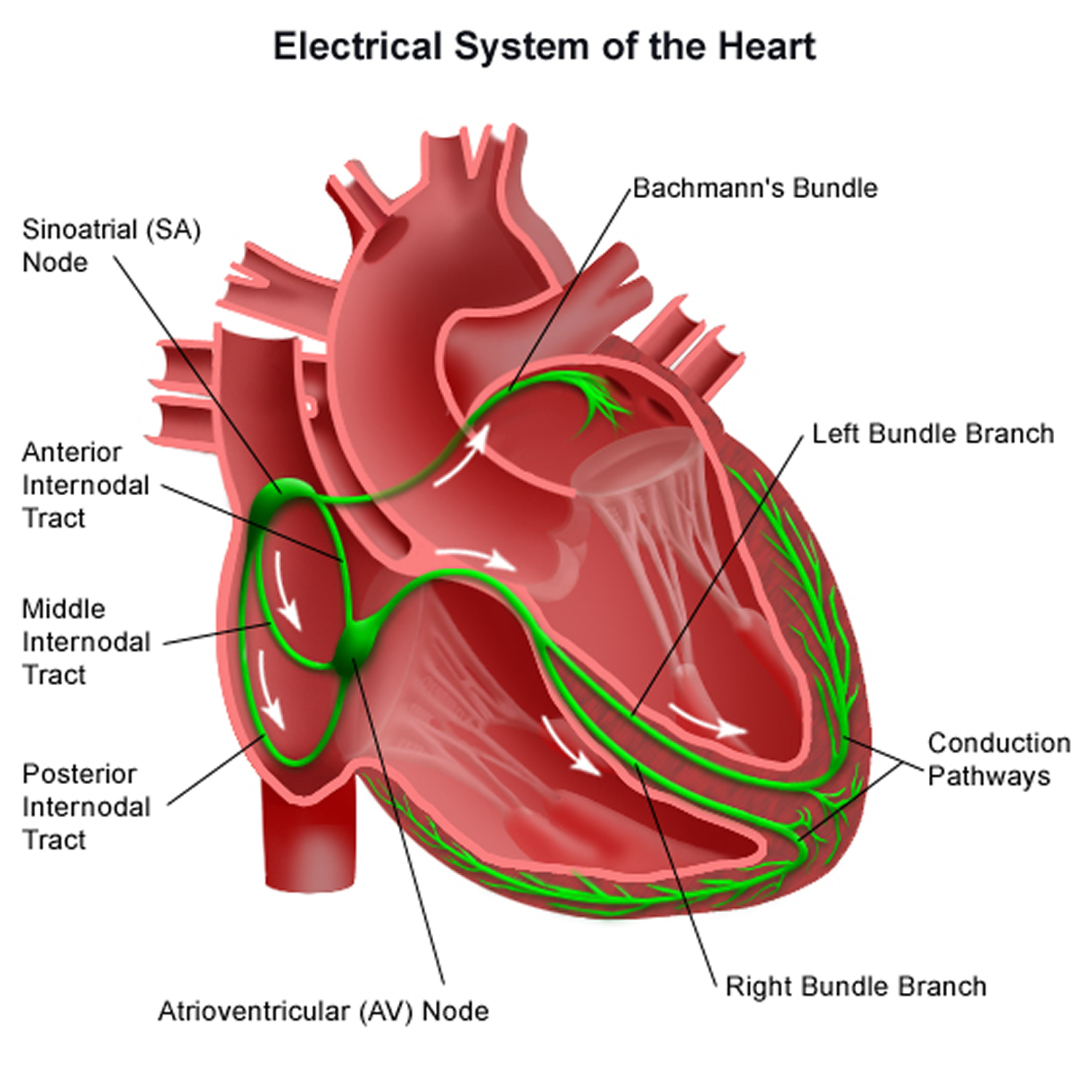
Figure 6. The heart’s electrical system
Heart Chambers
Your heart has 4 chambers 8, 2 on the right and 2 on the left:
- 2 upper chambers are called atrium (two is called an atria). The atria collect blood as it flows into your heart.
- 2 lower chambers are called ventricles.
- Right ventricle (RV) pumps Deoxygenated blood out of your heart to your lungs. Deoxygenated blood, also known as venous blood, is blood that has a lower oxygen concentration and a higher concentration of carbon dioxide than oxygenated blood.
- Left ventricle (LV) pumps Oxygenated blood out of your heart to other parts of your body. Oxygenated blood, also known as arterial blood, is blood rich in oxygen, typically bright red, that is pumped from the left ventricle of your heart to your body through arteries (aorta) after picking up oxygen in your lungs.
Your heart also has 4 valves that open and close to let blood flow from the atria to the ventricles and from the ventricles into the two large arteries connected to the heart in only one direction when the heart contracts (beats). The four heart valves are:
- Tricuspid valve, located between the right atrium and right ventricle
- Pulmonary or pulmonic valve, between the right ventricle and the pulmonary artery. The pulmonary artery carries blood from your heart to your lungs.
- Mitral valve, between the left atrium and left ventricle
- Aortic valve, between the left ventricle and the aorta. This aorta carries blood from the heart to the body.
Each valve has a set of flaps also called leaflets or cusps. The mitral valve has two flaps; the others have three. Valves are like doors that open and close. They open to allow blood to flow through to the next chamber or to one of the arteries. Then they shut to keep blood from flowing backward. Blood flow occurs only when there’s a difference in pressure across the valves, which causes them to open. Under normal conditions, the valves permit blood to flow in only one direction.
Your heart 4 chambers and 4 valves and is connected to various blood vessels. Veins are blood vessels that carry blood from the body to your heart. Arteries are blood vessels that carry blood away from your heart to your body.
Your heart pumps blood to your lungs and to all the body’s tissues by a sequence of highly organized contractions of the four chambers. For your heart to function properly, the four chambers must beat in an organized way.
When your heart’s valves open and close, they make a “lub-DUB” sound that a doctor can hear using a stethoscope 9.
- The First heart sound (S1) — the “lub” —is made by the mitral and tricuspid valves closing at the beginning of systole. Systole is when the ventricles contract, or squeeze, and pump blood out of the heart.
- The Second heart sound (S2) — the “DUB” —is made by the aortic and pulmonary valves closing at the beginning of diastole. Diastole is when the ventricles relax and fill with blood pumped into them by the atria.
Arteries
The arteries are major blood vessels connected to your heart.
- Pulmonary artery carries blood from the right side of the heart to the lungs to pick up a fresh supply of oxygen.
- Aorta is the main artery that carries oxygen-rich blood from the left side of the heart to the body.
- Coronary arteries are the other important arteries attached to the heart. They carry oxygen-rich blood from the aorta to the heart muscle, which must have its own blood supply to function.
Veins
The veins also are major blood vessels connected to your heart.
- Pulmonary veins carry oxygen-rich blood from the lungs to the left side of the heart so it can be pumped to the body.
- Superior vena cava (SVC) and inferior vena cava (IVC) are large veins that carry oxygen-poor blood (deoxygenated blood or venous blood) from the body back to the heart.
Blood Flow
The Right Side of Your Heart
In figure 5 above, the superior vena cava (SVC) and inferior vena cava (IVC) are shown in blue to the left of the heart muscle as you look at the picture. The superior vena cava (SVC) and inferior vena cava (IVC) are the largest veins in your body.
After your body’s organs and tissues have used the oxygen in your blood, the vena cavae carry the oxygen-poor blood (deoxygenated blood or venous blood) back to the right atrium of your heart.
- The superior vena cava (SVC) carries oxygen-poor blood from the upper parts of your body, including your head, chest, arms, and neck.
- The inferior vena cava (IVC) carries oxygen-poor blood from the lower parts of your body from the abdomen and lower extremities back to the right side of your heart for oxygenation.
The oxygen-poor blood (deoxygenated blood or venous blood) from the vena cavae flows into your heart’s right atrium. From the right atrium, blood is pumped into the right ventricle. And then from the right ventricle, blood is pumped to your lungs through the pulmonary arteries (shown in blue in the center of figure 5).
Once in the lungs, the blood travels through many small, thin blood vessels called capillaries. There, the blood picks up more oxygen and transfers carbon dioxide to the lungs—a process called gas exchange.
The oxygen-rich blood passes from your lungs back to your heart through the pulmonary veins (shown in red to the left of the right atrium in figure 5).
The Left Side of Your Heart
Oxygen-rich blood from your lungs passes through the pulmonary veins (shown in red to the right of the left atrium in figure 5 above). The blood enters the left atrium and is pumped into the left ventricle.
From the left ventricle, the oxygen-rich blood is pumped to the rest of your body through the aorta. The aorta is the main artery that carries oxygen-rich blood to your body.
Like all of your organs, your heart needs oxygen-rich blood. As blood is pumped out of your heart’s left ventricle, some of it flows into the coronary arteries (shown in red in figure 5).
Your coronary arteries are located on your heart’s surface at the beginning of the aorta. They carry oxygen-rich blood to all parts of your heart.
For the heart to work well, your blood must flow in only one direction. Your heart’s valves make this possible. Both of your heart’s ventricles have an “in” (inlet) valve from the atria and an “out” (outlet) valve leading to your arteries.
Healthy valves open and close in exact coordination with the pumping action of your heart’s atria and ventricles. Each valve has a set of flaps called leaflets or cusps that seal or open the valve. This allows blood to pass through the chambers and into your arteries without backing up or flowing backward.
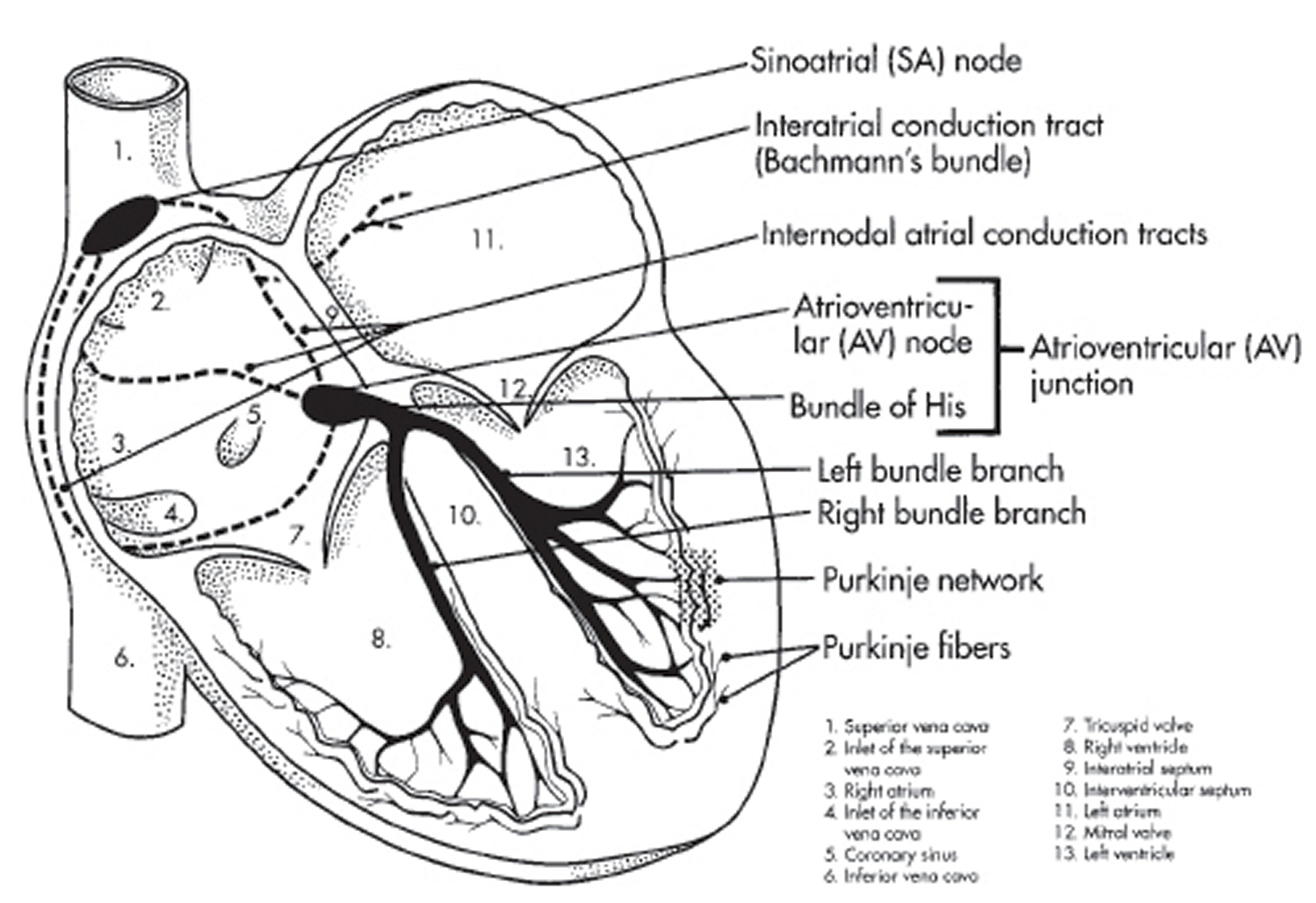
Heart’s Electrical System
To understand arrhythmias, it helps to understand the heart’s internal electrical system. The heart’s electrical system controls the rate and rhythm of the heartbeat.
With each heartbeat, an electrical signal spreads from the top of the heart to the bottom. As the signal travels, it causes the heart to contract and pump blood.
Your heart’s electrical system controls all the events that occur when your heart pumps blood 10. The electrical system also is called the cardiac conduction system. If you’ve ever seen the heart test called an EKG (electrocardiogram), you’ve seen a graphical picture of the heart’s electrical activity.
Your heart’s electrical system is made up of three main parts:
- Sinoatrial (SA) node, located in the right atrium of your heart
- Atrioventricular (AV) node, located on the interatrial septum close to the tricuspid valve
- His-Purkinje system, located along the walls of your heart’s ventricles
A heartbeat is a complex series of events. These events take place inside and around your heart. A heartbeat is a single cycle in which your heart’s chambers relax and contract to pump blood. This cycle includes the opening and closing of the inlet and outlet valves of the right and left ventricles of your heart.
Each heartbeat has two basic parts: diastole and systole. During diastole, the atria and ventricles of your heart relax and begin to fill with blood.
At the end of diastole, your heart’s atria contract (atrial systole) and pump blood into the ventricles. The atria then begin to relax. Your heart’s ventricles then contract (ventricular systole), pumping blood out of your heart.
Each electrical signal begins in a group of cells called the sinus node or sinoatrial (SA) node. The SA node is located in the heart’s upper right chamber, the right atrium. In a healthy adult heart at rest, the SA node fires off an electrical signal to begin a new heartbeat 60 to 100 times a minute. In a normal, healthy heart, each beat begins with a signal from the SA node. This is why the SA node sometimes is called your heart’s natural pacemaker. Your pulse, or heart rate, is the number of signals the SA node produces per minute.
The signal is generated as the vena cavae fill your heart’s right atrium with blood from other parts of your body. The signal spreads across the cells of your heart’s right and left atria.
From the SA node, the electrical signal travels through special pathways in the right and left atria. This causes the atria to contract and pump blood through the open valves from the atria into heart’s two lower chambers, the ventricles.
The electrical signal then moves down to a group of cells called the atrioventricular (AV) node, located between the atria and the ventricles. Here, the signal slows down just a little, allowing your heart’s right and left ventricles time to finish filling with blood.
The electrical signal then leaves the AV node and travels along a pathway called the bundle of His. This pathway divides into a right bundle branch and a left bundle branch. The signal goes down these branches to the ventricles, causing them to contract and pump blood to the lungs and the rest of the body.
From the bundle of His, the signal fibers divide into left and right bundle branches through the Purkinje fibers. These fibers connect directly to the cells in the walls of your heart’s left and right ventricles.
The signal spreads across the cells of your ventricle walls, and both ventricles contract. However, this doesn’t happen at exactly the same moment.
The left ventricle contracts an instant before the right ventricle. This pushes blood through the pulmonary valve (for the right ventricle) to your lungs, and through the aortic valve (for the left ventricle) to the rest of your body.
As the signal passes, the walls of the ventricles relax and await the next signal.
This process continues over and over as the atria refill with blood and more electrical signals come from the SA node.
A problem with any part of this process can cause an arrhythmia. For example, in atrial fibrillation, a common type of arrhythmia, electrical signals travel through the atria in a fast and disorganized way. This causes the atria to quiver instead of contract.
What is ejection fraction?
Ejection fraction (EF) is a measurement of your heart’s ability to pump oxygen-rich blood out to your body, expressed as a percentage (%), of how much oxygen-rich blood the left ventricle (LV) pumps out with each heart contraction 11. Ejection fraction (EF) refers to how well your heart pumps blood. Ejection fraction (EF) is the amount of blood pumped out of your heart’s lower chambers (ventricles) each time it contracts. An ejection fraction (EF) of 60 percent means that 60 percent of the total amount of blood in the left ventricle (LV) is pushed out with each heartbeat. A normal heart’s ejection fraction (normal EF) is between 50 and 70 percent 11. With each heartbeat, 50% to 70% of the blood in your left ventricle gets pumped out to your body. However, it is important to note that you can have a normal ejection fraction measurement and still have heart failure. This is called heart failure with preserved ejection fraction (HFpEF) previously known as diastolic heart failure. Heart failure with preserved ejection fraction (HFpEF) happens when your heart’s muscle has become so thick and stiff that the ventricle holds a smaller than usual volume of blood. In this case, your heart might still have an ejection fraction that falls in the normal range (EF≥50%) because your heart is pumping out a normal percentage of the blood that enters it. But in heart failure with preserved ejection fraction (HFpEF), the total amount of blood pumped isn’t enough to meet your body’s needs.
To understand ejection fraction (EF), it’s helpful to understand how blood flows through your heart:
- Blood enters your heart through the top right section (right atrium).
- Between heartbeats, there’s a short pause (diastole, the phase of the heartbeat when your heart muscle relaxes and allows heart chambers to fill with blood). This is when blood flows through a valve down to the left ventricle.
- Once the ventricle is full, the next heartbeat pumps out (ejects) a portion of the blood out to the body. Also called systole, the phase of the heartbeat when your heart muscle contracts and pumps blood from the heart chambers into the arteries.
Table 1. Ejection Fraction Percentage
| Sex | Normal | Mildly Abnormal | Moderately Abnormal | Severely Abnormal |
|---|---|---|---|---|
| Male | 52% to 72% | 41% to 51% | 30% to 40% | Below 30% |
| Female | 54% to 74% | 41% to 53% | 30% to 40% | Below 30% |
Types of ejection fraction
There are 2 types of ejection fraction: left ventricular ejection fraction (LVEF) and right ventricular ejection fraction (RVEF). Left ventricular ejection fraction (LVEF) measures how much blood gets pumped from the left ventricle with each contraction. Typically, ejection fraction refers to left ventricular. Right ventricular ejection fraction (RVEF) measures how much blood is pumped out of the right side of the heart, to the lungs.
Left ventricular ejection fraction (LVEF)
Ejection fraction (EF) typically refers to the left side of your heart or left ventricular ejection fraction (LVEF). It shows how much oxygen-rich blood is pumped out of the left ventricle (LV) to most of your body’s organs with each contraction. Left ventricular ejection fraction (LVEF) helps determine the severity of dysfunction on the left side of your heart.
Right ventricular ejection fraction (RVEF)
Right ventricular ejection fraction (RVEF) measures the amount of oxygen-poor blood or deoxygenated blood or venous blood pumped out of the right side of your heart to your lungs for oxygen. Right ventricular ejection fraction (RVEF) is important if you have right-sided heart failure. But this condition is not as common as left-sided heart failure.
What’s an unhealthy ejection fraction?
Ejection fraction (EF) refers to how well your heart pumps blood. The ejection fraction is the percentage of blood pumped out of the ventricle after a heart contraction. Ejection fraction (EF) is the amount of blood pumped out of your heart’s lower chambers (ventricles) each time it contracts. Your ejection fraction is an indicator of how well your heart is working. A low ejection fraction typically means you have or are at risk for heart failure. An ejection fraction (EF) from 41 to 49 percent (EF from 41% to 49%) might be considered too low. The lower your heart’s ejection fraction, the weaker your heart’s pumping action is. This occurs in people with severe heart failure. You can also have a low ejection fraction in the earlier stages of heart failure. However, ejection fraction (EF) does not always indicate that a person is developing heart failure, but it could indicate damage, perhaps from a previous heart attack. Some people with a normal ejection fraction also have heart failure. This is known as heart failure with preserved ejection fraction (HFpEF). An ejection fraction measurement under 40 percent (EF<40%) might be evidence of heart failure or cardiomyopathy (disease of the heart muscle that makes it harder for the heart to pump blood). In severe cases, ejection fraction (EF) can be even lower than 40.
According to the American Heart Association:
- Ejection fraction 50 to 70% (EF = 50% to 70%): Normal heart function.
- Ejection fraction 41 to 49% (EF = 41% to 49%): A mildly reduced left ventricle (LV) ejection fraction. Can indicate previous heart damage from heart attack or cardiomyopathy. You might not experience heart failure symptoms. Or, you may have symptoms with physical activity but not at rest.
- Ejection fraction less than 40% (EF < 40%): Your heart pumping ability is below normal. The lower the ejection fraction, the higher the risk of life-threatening complications, like cardiac arrest. Symptoms may be severe and may affect you even when sitting still.
- Ejection fraction greater than 75% (EF > 75%): Can indicate a heart condition like hypertrophic cardiomyopathy (HCM), a genetic heart condition where the heart muscle thickens, making it harder for the heart to pump blood effectively. This thickening can lead to various symptoms and complications, including shortness of breath, chest pain, and an increased risk of arrhythmias and a common cause of sudden cardiac arrest.
The lower your ejection fraction, the more severe your heart failure symptoms may be. You might experience:
- Confusion.
- Fatigue.
- Heart palpitations.
- Nausea.
- Shortness of breath (dyspnea).
- Water retention in your abdomen or feet.
- Weakness.
Some things that may cause a reduced ejection fraction are:
- Weakness of the heart muscle, such as cardiomyopathy.
- Heart attack that damaged the heart muscle.
- Heart valve disease.
- Long-term, uncontrolled high blood pressure.
What is the formula for ejection fraction?
The ejection fraction (EF) formula equals the amount of blood pumped out of the ventricle with each contraction (stroke volume or SV) divided by the end-diastolic volume (EDV), the total amount of blood in the ventricle. To express as a percentage, you would multiply by 100.
- Ejection fraction (EF) = (stroke volume [SV]/end-diastolic volume [EDV]) x 100
Stroke volume (SV) is the volume of blood pumped out of the heart’s left ventricle during each systolic cardiac contraction. Ventricular stroke volume (SV) is often thought of as the amount of blood (mL) ejected per beat by the left ventricle into the aorta (or from the right ventricle into the pulmonary artery). Moreover, a more precise definition for stroke volume (SV) and one that is used in echocardiography when assessing ventricular function is the difference between the ventricular end-diastolic volume (EDV) and the end-systolic volume (ESV). The end-diastolic volume (EDV) is the filled volume of the ventricle before contraction, and the end-systolic volume (ESV) is the residual volume of blood remaining in the ventricle after ejection. In a typical heart, the end-diastolic volume (EDV) is about 120 mL of blood and the end-systolic volume (ESV) is about 50 mL of blood 13. The difference in the end-diastolic volume (EDV) and the end-systolic volume (ESV), 70 mL, that is Stroke volume (SV) = end-diastolic volume (EDV) – end-systolic volume (ESV). Therefore, any factor that alters either the EDV or the ESV will change the SV. For example, an increase in EDV increases SV, whereas an increase in ESV decreases SV.
Who should have their ejection fraction measured?
It’s helpful to know your ejection fraction if you have or are at risk for a condition that can lead to heart failure.
This includes:
- ATTR amyloidosis (transthyretin amyloidosis), which can affect the heart. ATTR amyloidosis or transthyretin amyloidosis, is a rare, progressive disease where misfolded transthyretin (TTR) protein deposits as amyloid in organs and tissues, primarily affecting the heart and nerves, and can lead to heart failure
- Cancer or other conditions requiring chemotherapy, which sometimes causes heart damage (cardiotoxicity).
- Congenital heart disease. Congenital heart disease refers to heart problems present at birth, caused by abnormal development of the heart or blood vessels during fetal development. It’s the most common type of birth defect, affecting about 1 in 100 live-born babies.
- Heart attack. A heart attack also known as a myocardial infarction, occurs when a coronary artery, which supplies blood to your heart, becomes blocked, usually by a blood clot, depriving your heart muscle of oxygen, potentially causing damage or death. It’s a medical emergency requiring immediate treatment
- Heart valve disease.
- Myocarditis. Myocarditis is inflammation of the heart muscle (myocardium) that can weaken your heart and its ability to pump blood effectively, potentially leading to irregular heart rhythms or heart failure.
- Severe high blood pressure. Severe high blood pressure also called malignant hypertension or hypertensive crisis (blood pressure 180/120 mmHg or higher), is a medical emergency requiring immediate attention, potentially leading to heart attack, stroke, or other life-threatening complications
- Ventricular arrhythmia. Ventricular arrhythmias are abnormal heart rhythms originating in the heart’s lower chambers (ventricles), potentially causing a fast, irregular heartbeat and potentially life-threatening conditions like ventricular fibrillation.
What are the tests used to measure ejection fraction?
There are several reasons why your doctor might want to test your ejection fraction. For example, if you have symptoms like fatigue or shortness of breath, your doctor may want to see if your heart is failing. Your doctor also may want to test your ejection fraction if you have a history of heart disease, high blood pressure or diabetes. Testing your ejection fraction can help your doctor figure out if you have heart failure and how severe it is. It also can help guide treatment decisions.
Your doctor may order these tests to determine your ejection fraction:
- Echocardiography (echocardiogram) also known as an “echo”, is a non-invasive ultrasound test that uses sound waves to create images of your heart, allowing doctors to assess its structure and function. Echocardiography (echocardiogram) is the most common test used to measure ejection fraction.
- Cardiac catheterization: Cardiac catheterization is a medical procedure that involves inserting a thin, flexible tube (catheter) into a blood vessel, typically in the groin or arm, and guiding it to the heart to diagnose and/or treat heart conditions.
- Heart MRI scan, also called a cardiac MRI. This test uses magnetic fields and radio waves to create detailed images of the heart.
- Multigated acquisition scan (MUGA), also called a nuclear stress test or radionuclide ventriculography (RNVG) or equilibrium radionuclide angiocardiography (ERNA). A multigated acquisition (MUGA) scan is an imaging test to evaluate how your heart pumps blood. A MUGA scan measures your ejection fraction (EF). A multigated acquisition (MUGA) scan uses an injection of a substance called a radionuclide and a specialized camera. As the radionuclide travels through your blood, your doctor takes pictures of your heart. A multigated acquisition (MUGA) scan measures how your heart muscle contracts and relaxes while you rest or exercise.
- Cardiac computed tomography (CT) scan. A cardiac computed tomography (CT) scan is a procedure that utilizes multiple X-ray beams from different angles to acquire high-quality, three-dimensional (3D) images of your heart, along with your great vessels and surrounding structures. This quick but detailed and high-resolution scan shows your doctor problems with your heart structure, valves, arteries, aorta and more.
Is ejection fraction the only test for heart failure?
Ejection fraction is one of many parameters your heart doctor use to assess heart failure. Additional testing makes it possible to pinpoint the cause so that you receive appropriate therapies.
Additional tests your heart doctor use to diagnose heart disease include:
- Angiography or angiogram. An angiogram is a diagnostic procedure that uses X-ray images to look for blockages or narrow spots in your blood vessels (arteries or veins). An injected contrast material makes it easy to see where blood is moving and where blockages are. Your doctor can use X-rays or other types of imaging for your angiogram. Doctor use an angiogram of your heart, neck, kidneys, legs or other areas to locate the source of an artery or vein issue. Your doctor may want to do an angiogram procedure when you have signs of blocked, damaged or abnormal blood vessels.
- Chest X-ray. A chest X-ray is a test that creates an image of your heart, lungs and bones. Doctors use chest X-rays to diagnose or treat conditions like heart disease, pneumonia, emphysema or COPD.
- Echocardiogram.
- Electrocardiogram (EKG). Electrocardiogram (ECG/EKG) is a quick, noninvasive test diagnostic tool that records your heart’s electrical activity. Doctors use ECG for many reasons, like to diagnose heart rhythm issues or to monitor how well a treatment is working.
- Exercise stress test. An exercise stress test helps determine how well your heart responds during times when it’s working its hardest. It typically involves walking on a treadmill or pedaling on a stationary bike while hooked up to an EKG (ECG) to monitor your heart’s activity. If you can’t exercise, you receive medications that make your heart pump harder and faster or dilate the artery supplying blood to your heart (coronary arteries).
How often should my ejection fraction be measured?
Your heart doctor may be concerned about your ejection fraction if you:
- Have symptoms of heart failure.
- Experience a heart attack or other condition that affects your heart function.
- Are living with a condition that raises your risk of heart failure.
The frequency of testing after a heart failure diagnosis depends on a variety of factors, including how low your initial ejection fraction reading was. If your ejection fraction continues worsening, you’ll need it checked more frequently. If it is stable, you might not need it checked as often.
How will I know if my ejection fraction is improving?
If you have a low ejection fraction, you’ll have frequent appointments with your heart specialist to monitor it. It’s essential to go to all your appointments, even if you don’t feel sick.
If your symptoms are fading, it may be a sign that ejection fraction is improving. But it’s also possible for symptoms to worsen or for new ones to appear. These issues may indicate a worsening ejection fraction.
Contact your heart specialist immediately — do not wait until your next appointment — if you experience:
- Difficulty breathing, especially when lying down.
- A heartbeat that feels unusually fast.
- Loss of appetite or vomiting.
- Sudden weight change, which could be a sign of fluid retention.
- Unexplained weakness or dizziness.
Who is at Risk for Congestive Heart failure?
About 6.7 million adults 20 years old or older in the United States have heart failure 14. The number of people who have heart failure is growing.
Heart failure is more common in:
- People who are age 65 or older. Aging can weaken the heart muscle. Older people also may have had diseases for many years that led to heart failure. Heart failure is a leading cause of hospital stays among people on Medicare. Heart failure is rare in people younger than 50. Studies have shown that around 2% of the population younger than 54 years old have heart failure. The number increases to around 8% — about 1 in 12 — for people over 75.
- Blacks are more likely to have heart failure than people of other races. They’re also more likely to have symptoms at a younger age, have more hospital visits due to heart failure, and die from heart failure.
- People who are overweight. Excess weight puts strain on the heart. Being overweight also increases your risk of heart disease and type 2 diabetes. These diseases can lead to heart failure.
- People who have had a heart attack. Damage to the heart muscle from a heart attack and can weaken the heart muscle.
Children who have congenital heart defects also can develop heart failure. These defects occur if the heart, heart valves, or blood vessels near the heart don’t form correctly while a baby is in the womb. Congenital heart defects can make the heart work harder. This weakens the heart muscle, which can lead to heart failure. Children don’t have the same symptoms of heart failure or get the same treatments as adults.
Types of Congestive Heart failure
Heart failure can involve the heart’s left side, right side or both sides. However, it usually affects the left side first.
Right-sided heart failure
The right heart’s pumping action moves “used” deoxygenated blood or venous blood that returns to the heart through the veins through the right atrium into the right ventricle. The right ventricle then pumps the blood back out of the heart into the lungs to be replenished with oxygen.
Right-sided heart failure also called right ventricular heart failure or right heart failure means your heart’s right ventricle is too weak to pump enough blood to the lungs. As a result:
- Blood builds up in your veins, vessels that carry blood from your body back to your heart.
- This buildup increases pressure in your veins.
- The pressure pushes fluid out of your veins and into other tissue.
- Fluid builds up in your legs, abdomen or other areas of your body, causing swelling.
Right-sided heart failure usually occurs as a result of left-sided failure. When the left ventricle fails, increased fluid pressure is, in effect, transferred back through the lungs, ultimately damaging the heart’s right side. When the right side loses pumping power, blood backs up in the body’s veins. This usually causes swelling or congestion in the legs, ankles and swelling within the abdomen such as the gastrointestinal tract and liver causing ascites (accumulation of fluid in the peritoneal cavity, causing abdominal swelling).
Right-sided heart failure treatment focuses on managing symptoms so the disease doesn’t worsen. Healthy lifestyle habits, along with cardiac rehab, improve symptoms for many people. Other treatment options include cardiac devices and surgery. If you have shortness of breath, swelling or chest discomfort, talk to your doctor.
Right-sided heart failure prevention
You may not always be able to prevent heart failure. But you can sometimes treat conditions that cause heart failure.
If you treat these conditions early, you may be able to stop heart failure before it starts:
- Abnormal heart rhythms.
- Alcohol use disorder.
- Anemia.
- Coronary artery blockage.
- Heart valve disorders.
- High blood pressure.
- Obesity.
- Obstructive sleep apnea.
- Thyroid disorders.
Right-sided heart failure causes
Most right-sided heart failure occurs because of left-sided heart failure. The entire heart gradually weakens.
Left-sided heart failure results from another heart condition, such as:
Sometimes, right-sided heart failure can be caused by:
- High blood pressure in the lungs (pulmonary hypertension). Pulmonary hypertension specifically refers to high blood pressure in the pulmonary arteries, the blood vessels that carry blood from your heart to your lungs. Pulmonary hypertension is characterized by abnormally high blood pressure in the arteries of the lungs, which can lead to heart failure and requires specialist treatment. Pulmonary hypertension can be caused by various conditions, including lung diseases (like COPD or pulmonary fibrosis), heart problems, blood clots in the lungs (pulmonary embolism), or even certain medications. One type, pulmonary arterial hypertension (PAH), involves narrowing or blockage of the blood vessels in the lungs. Pulmonary arterial hypertension (PAH) can be idiopathic (cause unknown), heritable (genetic), or associated with other medical conditions. Autoimmune diseases, birth defects of the heart, and chronic low oxygen levels in the blood can also contribute to pulmonary hypertension.
- Pulmonary embolism (PE). A pulmonary embolism (PE) is a life-threatening condition that occurs when a blood clot blocks an artery in your lung. It can cause permanent lung damage and death. Blood clots most commonly come from the deep veins of your legs, a condition known as deep vein thrombosis. In many cases, multiple clots are involved.
- Lung diseases such as chronic obstructive pulmonary disease (COPD). Chronic obstructive pulmonary disease (COPD) is an umbrella term for a group of lung diseases that cause airflow obstruction and difficulty breathing, often caused by prolonged exposure to irritants like cigarette smoke.
Right-sided heart failure symptoms
The main sign of right-sided heart failure is fluid buildup. This buildup leads to swelling (edema) in your:
- Feet, ankles and legs.
- Lower back.
- Gastrointestinal tract and liver (causing ascites).
Other signs include:
- Breathlessness.
- Chest pain and discomfort.
- Heart palpitations.
Where you accumulate fluid depends on how much extra fluid and your position. If you’re standing, fluid typically builds up in your legs and feet. If you’re lying down, it may build up in your lower back. And if you have a lot of excess fluid, it may even build up in your belly.
Fluid build up in your liver or stomach may cause:
- Nausea.
- Bloating.
- Appetite loss.
Once right-sided heart failure becomes advanced, you can also lose weight and muscle mass. Doctors call these effects cardiac cachexia (a form of malnutrition and muscle wasting that can occur in people with advanced heart failure, leading to unintentional weight loss, fatigue, and reduced quality of life, often associated with a poor prognosis).
Right-sided heart failure diagnosis
To diagnose heart failure, your doctor will:
- Ask you about your symptoms. Often, this can be enough for your doctor to suspect heart failure.
- Perform a physical exam. Your doctor will take your pulse and blood pressure, listen to your heart and lungs and look for signs of swelling.
Your doctor will test your heart function using:
- Chest X-ray.
- Electrocardiogram (EKG).
- Echocardiogram.
- Blood tests, especially to measure substances called natriuretic peptides (NPs).
To confirm a diagnosis of heart failure or rule out other conditions causing your symptoms, you may need:
- Heart MRI.
- Heart CT.
- Cardiac catheterization.
- Stress test.
- Nuclear exercise stress test.
Right-sided heart failure treatment
Right-sided heart failure treatment is directed at the underlying cause of your heart failure, and not all causes of right-sided heart failure are curable. But you can treat heart failure and improve your symptoms. Often, a combination of lifestyle changes, medications and heart devices can help you manage heart failure and live an active life.
Cardiac rehabilitation, or rehab, is a program supervised by health professionals. It can help slow the progression of heart failure. Cardiac rehab usually includes:
- Exercise training, including an activity program tailored to fit your health goals.
- Education on heart-healthy living, nutrition, medication and how to manage your condition.
- Counseling to help reduce stress.
Medications treat right heart failure
Your heart doctor will determine the right medication or combination of medications that will help you feel your best. These may include:
- Angiotensin-converting enzyme (ACE) inhibitors, angiotensin 2 receptor blockers (ARBs) and angiotensin-receptor neprilysin inhibitors (ARNIs) to lower blood pressure.
- Channel blocker and beta blockers to reduce heart rate.
- Aldosterone antagonists and diuretics to get rid of excess fluid.
Your heart doctor may also prescribe:
- Anticoagulants (blood thinners).
- Cholesterol-lowering drugs.
- Digoxin is sometimes used to treat arrhythmia (irregular heartbeat).
For severe heart failure, your heart doctor may recommend:
- Implantable cardioverter-defibrillator (ICD).
- Cardiac resynchronization therapy (CRT), a type of pacemaker.
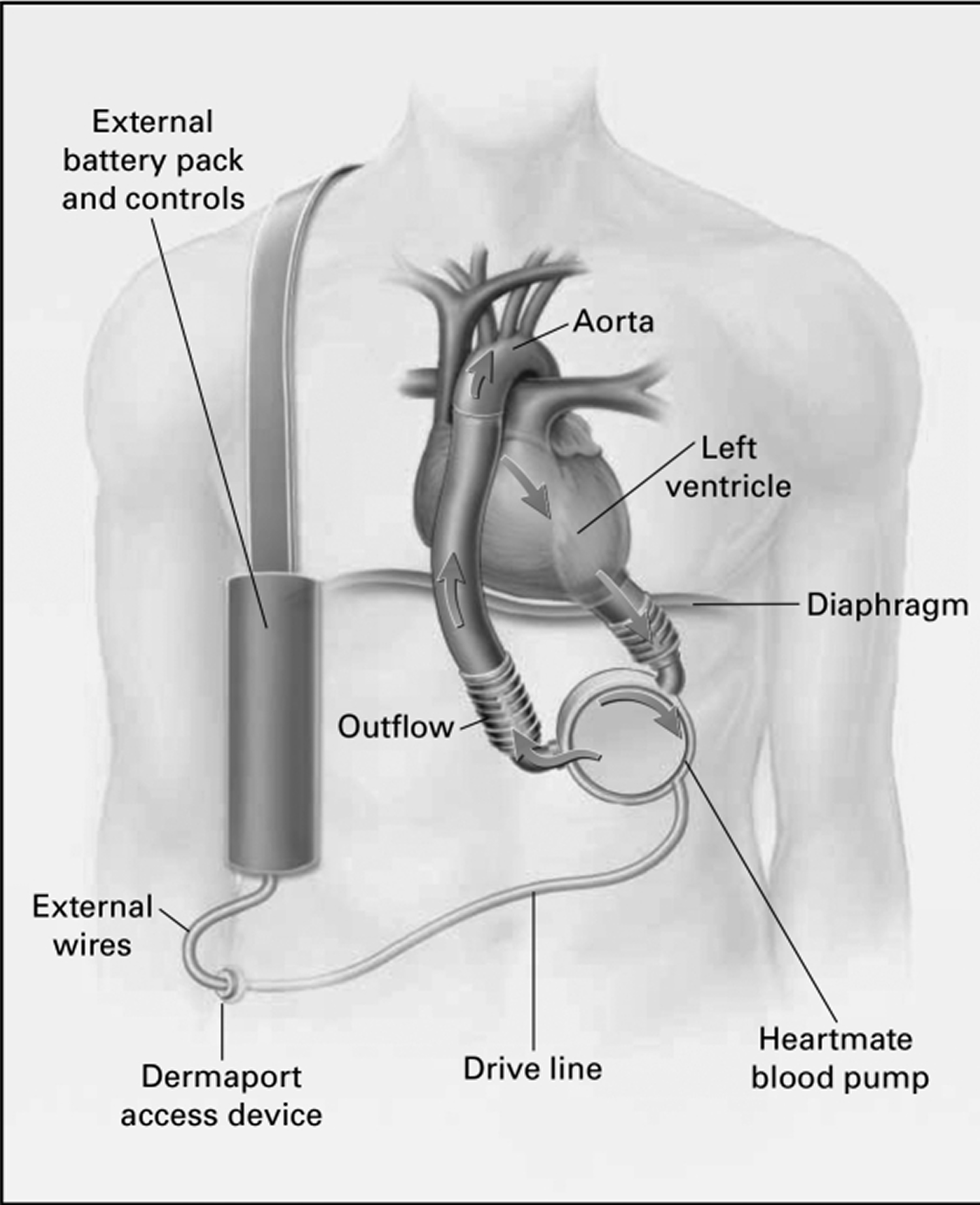
- Left ventricular assist device (LVAD).
If nonsurgical methods aren’t working, your heart doctor may talk to you about surgery for heart failure. There’s no procedure specifically for heart failure. But sometimes heart doctors identify a problem that surgery can correct. For example, surgery can repair a problem with your heart valve or coronary artery.
Heart failure surgery options may include:
- Percutaneous coronary intervention.
- Coronary artery bypass.
- Valve replacement.
- Heart transplant.
Right-sided heart failure prognosis
For many people, the right combination of medications and lifestyle changes can slow or stop the heart failure and improve symptoms. They can lead full, active lives. About 1 in 10 American adults who live with heart failure have advanced heart failure. That means treatments aren’t working, and symptoms are getting worse. You may feel symptoms, such as shortness of breath, even when you’re sitting. If you have advanced heart failure, talk with your heart specialist about palliative care and important care decisions. Palliative care focuses on improving the quality of life for individuals with serious illnesses and their families by addressing physical, psychological, social, and spiritual needs, and can be provided alongside curative treatments or as a primary focus.
Left-sided heart failure
The left side of your heart pumps fresh oxygen-rich blood from your lungs to the left atrium, then on to the left ventricle, which pumps it to the rest of your body. The left ventricle supplies most of your heart’s pumping power because it has to pump blood through your whole body, so the left ventricle is larger and stronger than the right ventricle. In left-sided heart failure or left ventricular heart failure, the left side of the heart must work harder to pump the same amount of blood. When people have left-sided heart failure, their heart’s left side has to work harder to pump the same amount of blood. Left-sided heart failure is the most common cause of right-sided heart failure.
When the left ventricle stops working efficiently:
- The left ventricle pumps less blood out to the body.
- The reduced blood flow causes blood to back up behind the left ventricle, into the left atrium, lungs and eventually the right ventricle.
- The backup causes higher blood pressure, which damages the right side of the heart. The damaged right side stops pumping efficiently, and blood builds up in the veins.
- As pressure increases in the veins, it pushes fluid into surrounding tissues.
- The fluid buildup causes swelling and congestion throughout your body.
There are 2 types of left-sided heart failure 15. Drug treatments are different for the two types:
- Heart failure with reduced ejection fraction (HFrEF), also called systolic failure: The left ventricle loses its ability to contract normally. The heart can’t pump with enough force to push enough blood into circulation. When this occurs, the heart is pumping less than or equal to 40% EF (ejection fraction).
- Heart failure with preserved ejection fraction (HFpEF), also called diastolic failure or diastolic dysfunction: The left ventricle loses its ability to relax normally because the muscle has become stiff. The heart can’t properly fill with blood during the resting period between each beat. When this occurs, the heart is pumping greater than or equal to 50%.
- Heart failure with mid-range ejection fraction (HFmrEF) is a newer concept. In this type of heart failure, the left ventricle pumps between 41% and 49% EF (ejection fraction). This places people with HFmrEF between the heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF) groups.
Left-sided heart failure causes
Left-sided heart failure may occur in people with:
- Coronary artery disease.
- Heart attack.
- High blood pressure.
- Valvular heart disease.
- Abnormal heart rhythms.
- Infiltrative diseases such as amyloidosis and sarcoidosis.
Other risk factors for left-sided heart failure include:
- Certain chemotherapy treatments for cancer that cause cardiotoxicity (heart toxicity).
- Diabetes.
- Obesity.
- Sleep apnea.
- Older age.
- Smoking.
- Toxins to your heart such as certain drugs and energy drinks.
- Less commonly, certain medications that are used to treat different disease processes, like autoimmune diseases and attention-deficit/hyperactivity disorder (ADHD).
Left-sided heart failure prevention
Living a heart-healthy lifestyle can lower your risk of left-sided heart failure. If you’ve already have left-sided heart failure, healthy habits can help you avoid future issues.
Steps you can take to prevent left-sided heart failure include:
- Manage your blood pressure or coronary artery disease.
- Regular physical activity and a good night’s sleep.
- Maintain a healthy weight and eat fruits and vegetables.
- Manage stress with deep breathing or relaxation techniques.
- Quitting tobacco if you use it and avoiding secondhand smoke.
Left-sided heart failure symptoms
Left-sided heart failure symptoms may be mild at first or you may think it’s a cold or allergy. You might not even notice them. But as your heart function worsens, you may experience:
- Constant coughing.
- Shortness of breath with walking or bending over.
- Waking up short of breath or unable to lie flat at night.
- Weight gain.
- Swelling (edema) in your ankles, legs or abdomen.
Over time, your heart works harder to do its job. This causes complications that may include:
- Cardiogenic shock. Cardiogenic shock is a life-threatening condition where the heart’s pumping function is severely impaired to meet the body’s needs, leading to organ damage and potentially death if not treated immediately
- Enlarged heart. An enlarged heart, also known as cardiomegaly, is a condition where the heart becomes larger than normal, often as a result of underlying conditions that make the heart work harder, such as high blood pressure or heart valve disease.
- Abnormal heart rates and rhythms (arrhythmia).
Left-sided heart failure complications
Complications of left-sided heart failure depend on your age, overall health and the severity of your heart disease. They may include:
- Kidney damage or failure. Heart failure can reduce the blood flow to the kidneys. Untreated, this can cause kidney failure. Kidney damage from heart failure can require dialysis for treatment.
- Other heart changes. Heart failure can cause changes in the heart’s size and function. These changes may damage heart valves and cause irregular heartbeats.
- Liver damage. Heart failure can cause fluid buildup that puts too much pressure on the liver. This fluid backup can lead to scarring, which makes it more difficult for the liver to work properly.
- Sudden cardiac death. If your heart is weak, there is a risk of dying suddenly due to a dangerous irregular heart rhythm.
- Arrhythmias or abnormal heart rhythms such as ventricular tachycardia and atrial fibrillation (Afib).
- Obstructive and central sleep apnea.
- Heart valve disease (leaky valves).
- Right-sided heart failure.
- Frailty and muscle weakness.
- Anemia.
- Depression or anxiety.
Left-sided heart failure diagnosis
To diagnose heart failure, your doctor examines you and asks questions about your symptoms and medical history. Your doctor checks to see if you have risk factors for heart failure, such as high blood pressure, coronary artery disease or diabetes.
Your doctor will listen to your lungs and heart with a device called a stethoscope. A whooshing sound called a murmur may be heard when listening to your heart. Your doctor may look at the veins in your neck and check for swelling in your legs and belly.
Tests that may be done to diagnose heart failure may include:
- Blood tests. Blood tests can help diagnose diseases that can affect the heart. Blood tests also can look for a specific protein made by the heart and blood vessels. In heart failure, the level of this protein goes up.
- Chest X-ray. X-ray images can show the condition of the lungs and heart.
- Electrocardiogram (ECG or EKG). This quick and painless test records the electrical signals in the heart. It can show how fast or how slowly the heart is beating.
- Echocardiogram. Sound waves create images of the beating heart. This test shows the size and structure of the heart and heart valves and blood flow through the heart.
- Ejection fraction. Ejection fraction is a measurement of the percentage of blood leaving your heart each time it squeezes. This measurement is taken during an echocardiogram. The result helps classify heart failure and guides treatment. An ejection fraction of 50% or higher is considered ideal. But you can still have heart failure even if the number is considered ideal.
- Exercise tests or stress tests. These tests often involve walking on a treadmill or riding a stationary bike while the heart is monitored. Exercise tests can show how the heart responds to physical activity. If you can’t exercise, you might be given medicines.
- CT scan of the heart also called cardiac CT scan, this test uses X-rays to create cross-sectional images of the heart.
- Heart MRI scan, also called a cardiac MRI. This test uses magnetic fields and radio waves to create detailed images of the heart.
- Coronary angiogram. This test helps spot blockages in the heart arteries. The healthcare professional inserts a long, thin flexible tube called a catheter into a blood vessel, usually in the groin or wrist. It’s then guided to the heart. Dye flows through the catheter to arteries in the heart. The dye helps the arteries show up more clearly on X-ray images and video.
- Myocardial biopsy. In this test, a heart doctor removes very small pieces of the heart muscle for examination. This test may be done to diagnose certain types of heart muscle diseases that cause heart failure.
Left-sided heart failure treatment
Treatment of heart failure depend on the cause. Treatment often includes lifestyle changes and medicines. If another health condition is causing your heart to fail, treating it may reverse your heart failure. Some people with heart failure need surgery to open blocked arteries or to place a device to help the heart work better. With treatment, symptoms of heart failure may improve.
Medications
A combination of medicines may be used to treat heart failure. The specific medicines used depend on the cause of your heart failure and the symptoms. Medicines to treat heart failure include:
- Angiotensin-converting enzyme (ACE) inhibitors. These medicines relax blood vessels to lower blood pressure, improve blood flow and decrease the strain on the heart. Examples include enalapril (Vasotec, Epaned), lisinopril (Zestril, Qbrelis) and captopril.
- Angiotensin 2 receptor blockers (ARBs). These medicines have many of the same benefits as ACE inhibitors. They may be an option for people who can’t tolerate ACE inhibitors. They include losartan (Cozaar), valsartan (Diovan) and candesartan (Atacand).
- Angiotensin receptor plus neprilysin inhibitors (ARNIs). This medicine uses two blood pressure medicines to treat heart failure. The combination medicine is sacubitril-valsartan (Entresto). It’s used to treat some people with heart failure with reduced ejection fraction. It may help prevent the need for a hospital stay in those people.
- Beta blockers. These medicines slow the heart rate and lower blood pressure. They reduce the symptoms of heart failure and help the heart work better. If you have heart failure, beta blockers may help you live longer. Examples include carvedilol (Coreg), metoprolol (Lopressor, Toprol-XL, Kapspargo Sprinkle) and bisoprolol.
- Diuretics or water pills, these medicines make you urinate more frequently. This helps prevent fluid buildup in your body. Diuretics, such as furosemide (Lasix, Furoscix), also decrease fluid in the lungs, so it’s easier to breathe. Some diuretics make the body lose potassium and magnesium. Your doctor may recommend supplements to treat this. If you’re taking a diuretic, you may have regular blood tests to check your potassium and magnesium levels.
- Potassium-sparing diuretics also called aldosterone antagonists, these medicines include spironolactone (Aldactone, CaroSpir) and eplerenone (Inspra). They may help people with severe heart failure with reduced ejection fraction (HFrEF) live longer. Unlike some other diuretics, these medicines can raise the level of potassium in the blood to dangerous levels. Talk with your doctor about your diet and potassium intake.
- Sodium-glucose cotransporter-2 (SGLT2) inhibitors. These medicines help lower blood sugar. They are often prescribed with diet and exercise to treat type 2 diabetes. But they’re also one of the first treatments for heart failure. That’s because several studies showed that sodium-glucose cotransporter-2 (SGLT2) inhibitors lowered the risk of hospital stays and death in people with certain types of heart failure — even if they didn’t have diabetes. Sodium-glucose cotransporter-2 (SGLT2) inhibitors medicines include canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance).
- Digoxin (Lanoxin) also called digitalis, helps the heart squeeze better to pump blood. It also tends to slow the heartbeat. Digoxin reduces heart failure symptoms in people with HFrEF. It may be more likely to be given to someone with a heart rhythm disorder, such as atrial fibrillation.
- Hydralazine and isosorbide dinitrate (BiDil). This combination of medicines helps relax blood vessels. It may be added to your treatment plan if you have severe heart failure symptoms and ACE inhibitors or beta blockers haven’t helped.
- Vericiguat (Verquvo). This medicine for chronic heart failure is taken once a day by mouth. It’s a type of medicine called an oral soluble guanylate cyclase stimulator. In studies, people with high-risk heart failure who took this medicine had fewer hospital stays for heart failure and heart disease-related deaths compared with those who got a dummy pill.
- Positive inotropes. These medicines may be given by IV to people with certain types of severe heart failure who are in the hospital. Positive inotropes can help the heart pump blood better and maintain blood pressure. Long-term use of these medicines has been linked to an increased risk of death in some people. Talk with your doctor about the benefits and risks of these medicines.
- Other medicines. Your doctor may prescribe other medicines to treat specific symptoms. For example, some people may receive nitrates for chest pain, statins to lower cholesterol or blood thinners to help prevent blood clots.
Your doctor may need to change your medicine doses frequently. This is more common when you’ve just started a new medicine or when your condition is getting worse.
You may need to stay in the hospital if you have a flare-up of heart failure symptoms. While in the hospital, you may receive:
- Medicines to relieve your symptoms.
- More medicines to help your heart pump better.
- Oxygen through a mask or small tubes placed in your nose.
If you have severe heart failure, you may need to use supplemental oxygen for a long time.
Surgery and other procedures
Surgery or other treatment to place a heart device may be recommended to treat the condition that led to heart failure.
Surgery or other procedures for heart failure may include:
- Coronary artery bypass graft surgery (CABG). You may need this surgery if severely blocked arteries are causing your heart failure. The surgery involves taking a healthy blood vessel from the leg, arm or chest and connecting it below and above the blocked arteries in the heart. The new pathway improves blood flow to the heart muscle.
- Heart valve repair or replacement. If a damaged heart valve causes heart failure, your care professional may recommend repairing or replacing the valve. There are many different types of heart valve surgery. The type needed depends on the cause of the heart valve disease. Heart valve repair or replacement may be done as open-heart or minimally invasive surgery.
- Implantable cardioverter-defibrillator (ICD). An implantable cardioverter-defibrillator (ICD) is used to prevent complications of heart failure. It isn’t a treatment for heart failure itself. An implantable cardioverter-defibrillator (ICD) is a device similar to a pacemaker. It’s implanted under the skin in the chest with wires leading through the veins and into the heart. The implantable cardioverter-defibrillator (ICD) checks the heartbeat. If the heart starts beating at a dangerous rhythm, the implantable cardioverter-defibrillator (ICD) tries to correct the beat. If the heart stops, the device shocks it back into regular rhythm. An ICD can also work as a pacemaker and speed up a slow heartbeat.
- Cardiac resynchronization therapy (CRT) also called biventricular pacing, cardiac resynchronization therapy (CRT) is a treatment for heart failure in people whose lower heart chambers aren’t pumping in sync with each other. A device sends electrical signals to the lower heart chambers. The signals tell the chambers to squeeze in a more coordinated way. This improves the pumping of blood out of the heart. Cardiac resynchronization therapy (CRT) may be used with an implantable cardioverter-defibrillator (ICD).
- Ventricular assist device (VAD). A ventricular assist device (VAD) helps pump blood from the lower chambers of the heart to the rest of the body. It’s also called a mechanical circulatory support device. Although a ventricular assist device (VAD) can be placed in one or both lower chambers of the heart, it’s usually placed in the lower left one. Your doctor may recommend a ventricular assist device (VAD) if you’re waiting for a heart transplant. Sometimes, a ventricular assist device (VAD) is used as a permanent treatment for people who have heart failure but who aren’t good candidates for a heart transplant.
- Heart transplant. Some people have such severe heart failure that surgery or medicines don’t help. These people may need to have their hearts replaced with a healthy donor heart. A heart transplant isn’t the right treatment for everyone. A team of doctors at a transplant center helps determine whether the procedure may be safe and beneficial for you.
Left-sided heart failure prognosis
Your outlook can be excellent as long you keep routine appointments with your heart doctor and take medications as recommended by your heart doctor.
Heart failure with preserved ejection fraction
Heart failure with preserved ejection fraction (HFpEF) previously known as diastolic heart failure is a type of heart failure where the left ventricle (the heart’s main pumping chamber) has difficulty relaxing and filling with blood during the resting period between beats, even though it can pump blood effectively during contraction 16, 17, 18, 19, 20. In heart failure with preserved ejection fraction (HFpEF), your heart might still have an ejection fraction (EF) that falls in the normal range (ejection fraction≥50%) because your heart is pumping out a normal percentage of the blood that enters it 21. But in heart failure with preserved ejection fraction (HFpEF), the total amount of blood pumped isn’t enough to meet your body’s needs 21.
Historically, heart failure with preserved ejection fraction (HFpEF) was termed diastolic heart failure; however, recent investigations suggest a more complex and heterogeneous pathophysiology 22, 23, 24, 25, 26, 27, 28. Ventricular diastolic and systolic reserve abnormalities, chronotropic incompetence, stiffening of ventricular tissue, atrial dysfunction, pulmonary hypertension, impaired vasodilation, and endothelial dysfunction are all implicated 29, 30. Frequently, these abnormalities are noted only when the circulatory system is stressed.
Nearly half of all patients with heart failure have heart failure with preserved ejection fraction (HFpEF) 31. The prevalence of heart failure with preserved ejection fraction (HFpEF) or diastolic heart failure, continues to increase in the developed world, likely because of the increasing prevalence of common risk factors, including older age, female sex, high blood pressure (hypertension), metabolic syndrome, kidney disease and obesity.
High blood pressure (hypertension) in particular is a strong risk factor for heart failure with preserved ejection fraction (HFpEF) or diastolic heart failure. 80 to 90 percent of patients with heart failure with preserved ejection fraction (HFpEF) or diastolic heart failure are hypertensive.
The diagnosis of heart failure with preserved ejection fraction (HFpEF) can be challenging, particularly in patients with overt signs or symptoms of congestion 32. Hemodynamic exercise testing has emerged as the gold standard to definitively establish or refute the diagnosis heart failure with preserved ejection fraction (HFpEF) 24, 26, 33, but estimates from community-based studies still show that many patients with shortness of breath (dyspnea) due to heart failure with preserved ejection fraction (HFpEF) remain undiagnosed 34.
Heart failure with preserved ejection fraction causes
Heart failure with preserved ejection fraction (HFpEF) occurs in nearly 50% of all heart failure cases, and prevalence is growing due to longer life, hypertension, diabetes, obesity, coronary artery disease, hyperlipidemia and other cardiac conditions.
You may be at risk for heart failure with preserved ejection fraction (HFpEF) if you have:
- Cardiac tamponade. Cardiac tamponade is a life-threatening condition where excessive fluid buildup in the pericardial sac (the sac that surrounds your heart). This fluid buildup increases pressure around your heart, preventing it from filling and emptying properly and impairing its ability to pump blood effectively, leading to a decrease in cardiac output and potentially causing shock requiring immediate medical attention.
- Cardiac tamponade can be caused by various factors, including:
- Trauma: Injuries to the chest that damage the heart or surrounding tissues.
- Infections: Pericarditis (inflammation of the pericardium) or other infections that cause fluid buildup.
- Medical conditions: Certain conditions, like uremia (kidney failure) or autoimmune diseases, can lead to pericardial effusion.
- Cancer: Malignant tumors that spread to the pericardium.
- Post-cardiac surgery: Complications from heart surgery can lead to fluid accumulation
- Cardiac tamponade can be caused by various factors, including:
- Coronary artery disease. Coronary artery disease also known as coronary heart disease, occurs when the coronary arteries that supply blood to your heart become narrowed or blocked, often due to plaque buildup, restricting blood flow and potentially leading to heart attack or other complications.
- Causes and risk factors for coronary artery disease or coronary heart disease include:
- Atherosclerosis: Atherosclerosis is the buildup of fats, cholesterol and other substances in and on the artery walls. This buildup is called plaque. The plaque can cause arteries to narrow, blocking blood flow. The plaque also can burst, leading to a blood clot. The most common cause of coronary artery disease (coronary heart disease) is atherosclerosis.
- High cholesterol (especially LDL or “bad” cholesterol)
- High blood pressure
- Smoking
- Diabetes
- Obesity
- Lack of physical activity
- Family history of heart disease
- Age (risk increases with age)
- Causes and risk factors for coronary artery disease or coronary heart disease include:
- Heart valve disease.
- High blood pressure (hypertension).
Cardiovascular and noncardiovascular conditions that may induce the acute decompensation of patients with heart failure with preserved ejection fraction (HFpEF) include but are not limited to 35:
- Acute kidney injury or worsening chronic kidney disease
- Anemia
- Chronic pulmonary disease, or the exacerbation thereof
- Dysrhythmia, particularly tachyarrhythmia, especially new-onset atrial fibrillation
- Infection
- Ischemia
- Increased salt intake or water retention
- Medication noncompliance, including antihypertensive or diuretics
- Poorly controlled or uncontrolled hypertension.
Heart failure with preserved ejection fraction pathophysiology
At a cellular level, heart muscle cells (cardiac myocytes) in patients with heart failure with preserved ejection fraction (HFpEF) are thicker and shorter than normal heart muscle cells (myocytes), and collagen content is increased. Recent histologic studies have shown reductions in myocardial capillary density that may contribute. At the organ level, affected individuals may have concentric remodeling with or without hypertrophy, although many people have normal ventricular geometry. Increases in heart muscle cells (myocytes) stiffness are mediated in part by relative hypophosphorylation of the sarcomeric molecule titin, due to cyclic guanosine monophosphate (cGMP) deficiency thought to arise primarily as a consequence of increased nitroso-oxidative stress induced by comorbid conditions such as obesity, metabolic syndrome and aging. Cellular and tissue characteristics may become more pronounced as the disease progresses.
Most studies suggest that the rate of left ventricular (LV) pressure decay during isovolumic relaxation is prolonged, increasing left ventricle (LV) and left atrial (LA) pressure, especially with elevated heart rates, as during exercise.
Normal ventricular filling is achieved in large part by ventricular suction, the early active component of diastole, which is generated by:
- Intraventricular pressure gradients
- Mitral annular longitudinal motion
- Early diastolic left ventricle (LV) “untwisting”
- Elastic recoil induced by contraction to a smaller end systolic volume in the preceding contraction cycle.
Each of these four elements is impaired in patients with heart failure with preserved ejection fraction (HFpEF), especially with stress, so filling becomes dependent on high left atrial (LA) pressure to actively push blood into the left ventricle (LV), as opposed to the action of a normal left ventricle (LV), which “pulls” blood in during early diastole. Passive left ventricle (LV) end-diastolic stiffness (Eed) is quantified by the slope and position of the diastolic pressure-volume relationship. Left ventricle (LV) end-diastolic stiffness (Eed) increases with normal aging, but this increase is exaggerated in individuals with heart failure with preserved ejection fraction (HFpEF) in most, but not all studies.
Although systolic function is relatively preserved, individuals with heart failure with preserved ejection fraction (HFpEF) typically exhibit subtle abnormalities in systolic performance, which become more dramatic during exercise. Limited stroke volume reserve and chronotropic incompetence markedly limit cardiac output in response to exercise. Mechanical dyssynchrony is common even though electrical dyssynchrony is not. Atrial fibrillation is extremely common in heart failure with preserved ejection fraction (HFpEF) (seen at some point in two-thirds of patients) and poorly tolerated because of the importance of LA contractile function in maintaining adequate LV chamber filling.
Pulmonary hypertension is common in patients with heart failure with preserved ejection fraction (HFpEF). Increased left atrial (LA) pressure adds in series with increased resistive and pulsatile pulmonary arterial loading to increase right ventricle (RV) afterload. This then leads to right ventricle (RV) dysfunction, which seems to be tightly correlated with the development of atrial fibrillation. With right ventricle (RV) failure, progressive systemic congestion occurs, manifested by malabsorption, congestive hepatopathy, cardiorenal syndrome, systemic inflammation and cardiac cachexia (a form of malnutrition and muscle wasting that can occur in people with advanced heart failure, leading to unintentional weight loss, fatigue, and reduced quality of life, often associated with a poor prognosis).
Increased right ventricle (RV) and left atrial (LA) size and subsequent increases in total cardiac volume can lead to pericardial restraint, preventing additional preload recruitment during exercise or saline loading and contributing to elevation in filling pressures and cardiac output plateau.
Heart failure with preserved ejection fraction symptoms
Patients with heart failure with preserved ejection fraction (HFpEF) typically exhibit intolerance to physical activity characterized by exertional dyspnea (98%) and fatigue (59%) 36, 37. With the progression of heart failure with preserved ejection fraction (HFpEF), these symptoms will occur with lower activity levels and may be accompanied by evidence of congestion 36, 37. Some patients with heart failure with preserved ejection fraction (HFpEF) are clinically asymptomatic, or their symptoms are so mild they go unnoticed.
The remaining clinical manifestations of heart failure with preserved ejection fraction (HFpEF) are typically the same as seen in other heart failure subtypes, including heart failure with reduced ejection fraction (HFrEF). Obtaining a thorough medical history and performing a comprehensive physical examination facilitate the classification of heart failure, which helps guide therapeutic interventions. The signs and symptoms of heart failure overlap with many other disease processes. Worsening ventricular dysfunction results in more severe symptoms and apparent signs. However, there is no single sign or symptom pathognomonic for heart failure.
It is reasonable to suspect heart failure with preserved ejection fraction (HFpEF) as a possible diagnosis in any patient with shortness of breath during physical activity (exertional dyspnea) and one of the following clinical parameters not otherwise explained by an alternative diagnosis 35:
- Age 60 or older
- Atrial fibrillation 38
- Chronic kidney disease
- Coronary artery disease
- Diabetes
- Hypertension
- Overweight/obesity 21
The exact pathogenic role of each risk factor is poorly understood.
Heart failure with preserved ejection fraction diagnosis
Heart failure with preserved ejection fraction (HFpEF) most common complaints at presentation are shortness of breath during physical activity (exertional dyspnea) and fatigue.
Diagnostic algorithms such as the HFA-PEFF (Heart Failure Association. Pretest Assessment, Echocardiography and natriuretic peptide, Functional testing, Final etiology) and H2FPEF (Heavy, 2 or more hypertensive drugs, atrial Fibrillation, Pulmonary hypertension, Elder older than 60, elevated Filling pressures) have been developed and evaluated to identify heart failure with preserved ejection fraction (HFpEF) noninvasively. Additional testing, such as echocardiography and measurement of natriuretic peptides, is required to apply these algorithms and confirm a diagnosis of heart failure with preserved ejection fraction (HFpEF) 39.
An evidence-based diagnostic approach to patients with suspected heart failure with preserved ejection fraction (HFpEF) is outlined in the 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure 21. For patients presenting with a sign or symptom of heart failure with preserved ejection fraction (HFpEF), additional testing is recommended to establish the diagnosis and, if possible, the specific etiology; the presence of underlying comorbidities should also be determined and documented.
Currently, 3 criteria must be met to establish the diagnosis 32:
- Clinical symptoms consistent with heart failure
- Preserved ejection fraction (ejection fraction at least 50 percent)
- Evidence of cardiac dysfunction
Objective evidence of cardiac dysfunction is the most controversial point and a topic of intense investigation. Potential findings that demonstrate cardiac dysfunction include evidence of congestion on physical examination or chest X-ray; atrial fibrillation; echocardiographic evidence of diastolic dysfunction (left atrial enlargement, engorged inferior vena cava, pulmonary hypertension or elevated E/e´ filling velocity); and elevated brain natriuretic peptide (BNP).
If the diagnosis remains uncertain after testing, invasive hemodynamic evaluation may be revealing. Elevated filling pressures at rest support the diagnosis of heart failure with preserved ejection fraction (HFpEF); however, many individuals demonstrate hemodynamic compromise only with stress. In these patients, it is critical to perform hemodynamic measurements during exercise.
Heart failure with preserved ejection fraction treatment
The goals of therapy for heart failure with preserved ejection fraction (HFpEF) are to reduce symptoms, improve quality of life, prevent disease progression, reduce hospitalizations, and effectively manage underlying comorbidities 35. To this end, lifestyle and behavioral modifications are a cornerstone of therapeutic intervention 35.
Lifestyle interventions
Several studies have demonstrated that exercise training improves cardiorespiratory fitness and quality of life in patients with heart failure with preserved ejection fraction (HFpEF) 40. Exercise training, exercise-based cardiac rehabilitation, and weight loss improve functional status, exercise performance, rates of heart failure-specific hospitalization, and quality of life in patients with heart failure with preserved ejection fraction (HFpEF) 41. Calorie restriction and exercise training may have positive additive effects in patients with heart failure with preserved ejection fraction (HFpEF), especially if they are older with concomitant obesity 42. In addition to calorie restriction, at least 1 study has demonstrated that sodium restriction as part of the Dietary Approaches to Stop Hypertension (DASH) diet improves ventricular diastolic function and arterial elastance in patients with heart failure with preserved ejection fraction (HFpEF) and hypertension 43.
Antihypertensive therapies
Diuretics, angiotensin receptor–neprilysin inhibitors (ARNIs), angiotensin receptor blockers (ARBs), and mineralocorticoid antagonists (MRAs) are the preferred pharmacologic interventions if blood pressure is uncontrolled in a patient with heart failure with preserved ejection fraction (HFpEF). The currently recommended blood pressure goal is below 130/80 mm Hg 44. The nonrandomized Optimize-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure) registry demonstrated improved 30-day mortality and decreased hospitalization for heart failure with diuretic use compared to no diuretic therapy after hospital discharge for heart failure 45. Bumetanide and torsemide have better bioavailability than furosemide. Some patients may require a combination of diuretic classes, such as thiazide or thiazide-like diuretics. Diuretic resistance is a common problem and may be due to excessive dietary sodium consumption, using medications that negatively affect diuretic action, such as nonsteroidal anti-inflammatory drugs, or underlying chronic kidney disease.
A meta-analysis of 11 trials of 14,262 patients in sinus rhythm, including 244 patients with heart failure with preserved ejection fraction (HFpEF), demonstrated that beta blockers reduce mortality and have beneficial effects 46. Patients with heart failure with preserved ejection fraction (HFpEF) and concomitant coronary artery disease also benefit from beta-blocker administration. The Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist (TOPCAT) trial was a randomized, double-blind trial of 3445 patients with symptomatic heart failure and an left ventricle EF of greater than 45% that demonstrated some reduction in hospitalization rates for heart failure 47. This was particularly true for patients with an left ventricle EF of less than 55% to 60% and those with elevated brain natriuretic peptide (BNP) 48.
A prespecified subgroup analysis of patients in the Prospective Comparison of angiotensin receptor plus neprilysin inhibitor (ARNI) with angiotensin 2 receptor blocker (ARB) Global Outcomes in heart failure with preserved ejection fraction (HFpEF) (PARAGON-HF) demonstrated that sacubitril-valsartan, as compared with valsartan, has a tendency to lower the risk of heart failure-related hospitalizations overall, but more so in women with heart failure with preserved ejection fraction (HFpEF) than men; the average left ventricle EF in study participants was 57% 49.
Sodium-glucose cotransporter 2 inhibitor therapy
The effects of sodium-glucose cotransporter 2 inhibitor (SGLT2i) therapy on cardiovascular mortality and hospitalization in patients with heart failure with preserved ejection fraction (HFpEF) has been demonstrated in the Dapagliflozin Evaluation to Improve the Lives of Patients with Preserved Ejection Fraction Heart Failure (DELIVER) and Empagliflozin in Heart Failure with a Preserved Ejection Fraction (EMPEROR-PRESERVED) trials 50. The DELIVER trial 51 demonstrated that dapagliflozin decreased the risk of worsening heart failure or cardiovascular death among patients with heart failure with preserved ejection fraction (HFpEF). The EMPEROR-PRESERVED trial 52 demonstrated significant reductions in cardiovascular mortality, heart failure-related hospitalizations, decline in kidney function, and improved quality of life in patients with heart failure with preserved ejection fraction (HFpEF). The effects of sodium-glucose cotransporter 2 inhibitor (SGLT2i) therapy are consistent for patients with heart failure with preserved ejection fraction (HFpEF) across all age groups, and increasing age has not been associated with an increase in adverse events 53, 54. Sodium-glucose cotransporter 2 inhibitor (SGLT2i) therapy should be considered in all patients with heart failure with preserved ejection fraction (HFpEF), with or without underlying type 2 diabetes, as early as index hospitalization after initial medical stabilization 51.
In patients with heart failure with preserved ejection fraction (HFpEF), obesity, and underlying type 2 diabetes, glucagon-like peptide (GLP-1) analogs or glucose-dependent insulinotropic polypeptide (GIP) receptor antagonists are beneficial if dual therapy is required 44.
Rate control in atrial fibrillation
Atrial fibrillation is very common in patients with heart failure with preserved ejection fraction (HFpEF). Beta blockers and nondihydropyridine calcium channel blockers are the preferred therapies for rate control in patients with atrial fibrillation and heart failure with preserved ejection fraction (HFpEF). Digoxin may be considered in hypotensive patients. Atrial fibrillation in patients with heart failure with preserved ejection fraction (HFpEF) and hypertrophic cardiomyopathy, cardiac amyloidosis, rheumatic mitral valve stenosis, or a mechanical mitral valve requires anticoagulation regardless of CHA2DS2-VASc score. The 2023 ACC/AHA Guideline for the Diagnosis and Management of Atrial Fibrillation recommends catheter ablation as a first-line therapy to improve symptoms of paroxysmal atrial fibrillation in younger patients with fewer comorbidities 55.
Additional therapies
In patients with heart failure with preserved ejection fraction (HFpEF) and suspected sleep apnea, consultation with sleep medicine for possible polysomnography is recommended. Fatigue is a common symptom of heart failure, and daytime sleepiness is a common symptom of sleep apnea; obesity is a risk factor for both disease processes.
Using CardioMEMS, a pulmonary artery pressure hemodynamic monitoring system, improves quality of life and decreases hospitalizations in patients with heart failure with preserved ejection fraction (HFpEF) and frequent hospitalizations 56. Additionally, CardioMEMS utilization has been shown to improve underlying metabolic comorbidities in tandem with improving pulmonary artery pressures 56.
Coronary angiogram and revascularization should be considered if ischemia is driving symptoms of heart failure with preserved ejection fraction (HFpEF) 57.
The 2022 ACC/AHA Guideline for the Management of Heart Failure recommends that all patients with a diagnosis of heart failure receive palliative and supportive care 21. In the context of patients with heart failure with preserved ejection fraction (HFpEF), palliative care is defined as “patient- and family-centered care that optimizes health-related quality of life by anticipating, preventing, and treating suffering” 21. Primary palliative care should begin early in the course of illness, and the interdisciplinary team can address many primary needs 58. Components of primary palliative care include high-quality communication, anticipatory guidance, advance care planning, home and case management assistance, care coordination, and addressing barriers to care such as food insecurity and transportation needs 21, 58.
Acute Decompensation of Heart Failure with Preserved Ejection Fraction
Multidisciplinary shock team assessment and intervention can improve 30-day all-cause mortality and reduce in-hospital mortality in patients with clinical and hemodynamics-proven cardiogenic shock of any cause 59. Intravenous vasopressor support can temporarily improve hemodynamics in patients with cardiogenic shock and improve end-organ perfusion; norepinephrine is preferred except in patients with tachyarrhythmias who benefit from phenylephrine. Vasopressor support allows time for diuresis and correction of precipitating factors like arrhythmia and ischemia.
Appropriate ventilatory support and diuresis are the cornerstones of therapy for patients with acutely decompensated heart failure with preserved ejection fraction (HFpEF). In most cases, loop diuretics are preferred to thiazide diuretics; there is no scientific evidence to support one loop diuretic over another in acutely decompensated patients with heart failure with preserved ejection fraction (HFpEF). The Diuretic Optimization Strategies Evaluation (DOSE) trial 60 revealed no clinically significant differences in symptomatic improvement between bolus or continuous intravenous loop diuretics. Some patients may require a combination of diuretic classes, such as thiazide, thiazide-like, or acetazolamide. Adding metolazone increases the risk of hypokalemia, hyponatremia, worsening renal function, and mortality compared to loop diuretics alone 61. Contrarily, the Acetazolamide in Decompensated Heart Failure with Volume OveRload (ADVOR) trial 62 demonstrated that adding acetazolamide to loop diuretics increases the incidence of successful decongestion in patients with acute heart failure within three days compared to placebo.
Following the initial stabilization of hemodynamics and ventilation, assessing and managing ischemia, arrhythmia, and other precipitating factors and comorbidities is paramount. Urgent revascularization is preferred in the setting of acute coronary syndrome. Intravenous or topical nitroglycerin is preferred in patients with hypertensive urgency or emergency and pulmonary edema; nitroglycerin decreases preload in patients with pulmonary edema.
Short-term renal replacement therapy or ultrafiltration should be considered in symptomatic hypervolemic patients with poor renal function and minimal urine output, irrespective of supportive therapy and stable hemodynamics. Patients with poor baseline renal function or end-stage renal disease are at a significantly increased risk for requiring renal replacement therapy.
There is no substantial evidence supporting the early initiation of angiotensin-converting enzyme (ACE) inhibitors, ARBs, ARNIs, MRAs, SGLT2i therapy, or beta blockers to prevent major adverse cardiac events in unstable patients with acutely decompensated heart failure with preserved ejection fraction (HFpEF). Thiazolidinediones and dipeptidyl peptidase-4 (DPP-4) inhibitors such as sitagliptin or saxagliptin are contraindicated in acutely decompensated heart failure with preserved ejection fraction (HFpEF).
Heart failure with preserved ejection fraction prognosis
Patients with heart failure with preserved ejection fraction (HFpEF) have increased rates of morbidity and mortality compared to patients without heart failure, but with outcomes comparable to heart failure with reduced ejection fraction (HFrEF) 63, 21, 64, 65. The presence and severity of common comorbidities such as hypertension, atrial fibrillation, diabetes, and chronic kidney disease significantly influence the prognosis of patients with heart failure with preserved ejection fraction (HFpEF) 64, 66. Biomarkers like BNP, NT-pro BNP, and high-sensitivity troponin are associated with prognosis in heart failure with preserved ejection fraction (HFpEF); elevated biomarker levels may indicate increased cardiovascular risk.
Independent predictors of mortality in patients with heart failure with preserved ejection fraction (HFpEF) confer a poor prognosis 20, 67, 68, 69, 66:
- Older age
- Male sex
- NYHA class C or D
- Lower LVEF and the degree of diastolic dysfunction
- Extent of coronary artery disease
- Peripheral artery disease
- Diabetes
- Functional renal impairment
- Pulmonary hypertension
- Right ventricular dysfunction
- Atrial fibrillation
- Increased red cell distribution width.
However, therapeutic interventions are available to reduce symptoms, improve functional status and quality of life, and reduce hospital admission rates 44, Clinical understanding of heart failure with preserved ejection fraction (HFpEF) continues to evolve, and clinical trials to improve outcomes for patients with heart failure with preserved ejection fraction (HFpEF) are ongoing.
Heart failure with reduced ejection fraction
Heart failure with reduced ejection fraction (HFrEF) also called systolic heart failure, is a type of left-sided heart failure with ejection fraction ≤40% (EF ≤40%) 21. The left ventricle can’t squeeze as strong as it should. The heart isn’t strong enough to pump enough blood to the body.
Heart failure with mid-range ejection fraction
Heart failure with mid-range ejection fraction (HFmrEF) is a newer concept. In heart failure with mid-range ejection fraction (HFmrEF), the left ventricle pumps between 41% and 49% ejection fraction (EF 41% to 49%) 21. This places people with HFmrEF between the heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF) groups.
Congestive heart failure stages
Heart failure is a chronic, progressive condition in which the heart muscle is unable to pump enough blood through to meet the body’s needs for blood and oxygen 70. Basically, the heart can’t keep up with its workload.
At first the heart tries to make up for this by 70:
- Enlarging. The heart stretches to contract more strongly and keep up with the demand to pump more blood. Over time this causes the heart to become enlarged.
- Developing more muscle mass. The increase in muscle mass occurs because the contracting cells of the heart get bigger. This lets the heart pump more strongly, at least initially.
- Pumping faster. This helps to increase the heart’s output.
The body also tries to compensate in other ways 70:
- The blood vessels narrow to keep blood pressure up, trying to make up for the heart’s loss of power.
- The body diverts blood away from less important tissues and organs (like the kidneys), the heart and brain.
- The kidneys retain more salt and water rather than excrete it through urine. This creates increased volume of blood, which helps to maintain blood pressure and allows the heart to pump stronger. But over time this extra volume can overtask the heart, making heart failure worse.
These temporary measures mask the problem of heart failure, but they don’t solve it. Heart failure continues and worsens until these substitute processes no longer work 70.
Eventually the heart and body just can’t keep up, and the person experiences the fatigue, breathing problems or other symptoms that usually prompt a trip to the doctor.
The body’s compensation mechanisms help explain why some people may not become aware of their condition until years after their heart begins its decline. It’s also a good reason to have a regular checkup with your doctor 70.
Heart failure can progress, so the American College of Cardiology and the American Heart Association have identified 4 stages of heart failure — stage A, B, C and D. Heart doctors also classify heart failure when it has progressed to stages C and D. This classification measures a patient’s overall heart function and severity of symptoms.
Stage A: At risk for heart failure
- People who are at risk for heart failure but do not yet have symptoms or structural or functional heart disease. Risk factors for people in stage A include hypertension, coronary vascular disease, diabetes, obesity, exposure to cardiotoxic agents, genetic variants for cardiomyopathy and family history of cardiomyopathy
Stage B: Pre-heart failure
- People without current or previous symptoms of heart failure but with either structural heart disease, increased filling pressures in the heart or other risk factors
Stage C: Symptomatic heart failure
- People with current or previous symptoms of heart failure
Stage D: Advanced heart failure
- People with heart failure symptoms that interfere with daily life functions or lead to repeated hospitalizations
Doctors usually classify or “stage” patients’ heart failure according to the severity of their symptoms 71. The most commonly used classification system, the New York Heart Association (NYHA) Functional Classification1, places patients in one of four categories based on limitations of physical activity. The table below describes the most commonly used classification system, the New York Heart Association (NYHA) Functional Classification 72. The NYHA Functional Classification places patients in one of four categories based on how much they are limited during physical activity.
Table 2. New York Heart Association (NYHA) Functional Classification of Heart Failure
| Class | Patient Symptoms |
|---|---|
| 1 (I) | No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, shortness of breath (dyspnea). |
| 2 (II) | Slight limitation of physical activity. Comfortable at rest. Ordinary physical activity results in fatigue, palpitation, shortness of breath (dyspnea). |
| 3 (III) | Marked limitation of physical activity. Comfortable at rest. Less than ordinary activity causes fatigue, palpitation, or shortness of breath (dyspnea). |
| 4 (IV) | Unable to carry on any physical activity without discomfort. Symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases. |
Table 3. American College of Cardiology/American Heart Association Guidelines of Heart Failure
| Class | Objective Assessment |
|---|---|
| A | No objective evidence of cardiovascular disease. No symptoms and no limitation in ordinary physical activity. |
| B | Objective evidence of minimal cardiovascular disease. Mild symptoms and slight limitation during ordinary activity. Comfortable at rest. |
| C | Objective evidence of moderately severe cardiovascular disease. Marked limitation in activity due to symptoms, even during less-than-ordinary activity. Comfortable only at rest. |
| D | Objective evidence of severe cardiovascular disease. Severe limitations. Experiences symptoms even while at rest. |
Footnotes: American College of Cardiology/American Heart Association Guidelines of Heart Failure – the system includes a category for people who are at risk of developing heart failure. For example, a person who has several risk factors for heart failure but no signs or symptoms of heart failure is Stage A. A person who has heart disease but no signs or symptoms of heart failure is Stage B. Someone who has heart disease and is experiencing or has experienced signs or symptoms of heart failure is Stage C. A person with advanced heart failure requiring specialized treatments is Stage D. Doctors use this classification system to identify your risk factors and begin early, more aggressive treatment to help prevent or delay heart failure. These scoring systems are not independent of each other. Your doctor often will use them together to help decide your most appropriate treatment options. Ask your doctor about your score if you’re interested in determining the severity of your heart failure. Your doctor can help you interpret your score and plan your treatment based on your condition.
[Source 71 ]What is advanced heart failure?
In the American Heart Association and American College of Cardiology’s A-to-D staging system, advanced heart failure is stage D. The New York Heart Association (NYHA), advanced heart failure is class 4 (IV) – unable to carry on any physical activity without discomfort; symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases.
In its early stages of heart failure, medication and a healthy lifestyle can help manage heart failure. But as your heart failure progresses and your heart becomes weaker, treatment gets more complex. When heart failure progresses to an advanced stage, difficult decisions must be made with your family and your health care professional about the care you want to receive. Do I want to receive aggressive treatment? Is quality of life more important than living as long as possible? How do I feel about resuscitation?
For advanced heart failure patients and their health care professional, making good decisions requires teamwork. Through shared decision-making, health care professionals and patients consider both the options and the patient’s preferences before charting a treatment course.
Living with advanced heart failure is difficult, and the medical decisions can be complicated. With shared decision-making, you can avoid heat-of-the-moment decisions and instead take time to figure out what’s best for you.
Congestive heart failure causes
Conditions that damage or overwork your heart muscle can cause heart failure 73. Certain lifestyle factors – smoking, being overweight, eating foods high in fat and cholesterol and physical inactivity – can contribute to heart failure because they increase your risk of developing heart conditions associated with heart failure. Your heart muscle can be damaged by certain infections, heavy alcohol use, recreational drug use and some chemotherapy medicines. Your genes also can play a role. Over time, your heart weakens. It isn’t able to fill with and/or pump blood as well as it should. As the heart weakens, certain proteins and substances might be released into the blood. These substances have a toxic effect on the heart and blood flow, and they worsen heart failure.
Any of the following conditions also can damage or weaken the heart and cause heart failure:
- Coronary heart disease. Coronary artery disease is the most common cause of heart failure. Coronary artery disease results from the buildup of fatty deposits in the arteries. The deposits narrow the arteries. This reduces blood flow and can lead to heart attack.
- Heart attack. A heart attack occurs suddenly when an artery feeding the heart becomes completely blocked. Damage to the heart muscle from a heart attack may mean that the heart can no longer pump as well as it should.
- High blood pressure. Also called hypertension, this condition forces the heart to work harder than it should to pump blood through the body. Over time, the extra work can make the heart muscle too stiff or too weak to properly pump blood.
- Heart valve disease. Heart valves keep blood flowing the right way. If a heart valve isn’t working properly, the heart must work harder to pump blood. This can weaken the heart over time. Treating some types of heart valve disease may reverse heart failure.
- Inflammation of the heart muscle (myocarditis). Myocarditis is most commonly caused by a virus and can lead to left-sided heart failure.
- Congenital heart defect. A heart condition that you’re born with is called a congenital heart defect. If the heart and its chambers or valves haven’t formed correctly, the other parts of the heart have to work harder to pump blood. This may lead to heart failure.
- Irregular heart rhythms (arrhythmias). Irregular heart rhythms may cause the heart to beat too fast, creating extra work for the heart. A slow heartbeat also may lead to heart failure. Treating an irregular heart rhythm may reverse heart failure in some people.
- Other heart conditions or diseases
- Other diseases. Some long-term diseases may contribute to chronic heart failure. Examples are diabetes, HIV infection, an overactive or underactive thyroid, or a buildup of iron or protein.
Causes of sudden heart failure also include:
- Allergic reactions.
- Any illness that affects the whole body.
- Blood clots in the lungs.
- Severe infections.
- Use of certain medicines.
- Viruses that attack the heart muscle.
Coronary Heart Disease
Coronary heart disease is a condition in which a waxy substance called plaque builds up inside the coronary arteries. These arteries supply oxygen-rich blood to your heart muscle.
Plaque narrows the arteries and reduces blood flow to your heart muscle. The buildup of plaque also makes it more likely that blood clots will form in your arteries. Blood clots can partially or completely block blood flow. Coronary heart disease can lead to chest pain or discomfort called angina, a heart attack, and heart damage.
Diabetes
Diabetes is a disease in which the body’s blood glucose (sugar) level is too high. The body normally breaks down food into glucose and then carries it to cells throughout the body. The cells use a hormone called insulin to turn the glucose into energy.
In diabetes, the body doesn’t make enough insulin or doesn’t use its insulin properly. Over time, high blood sugar levels can damage and weaken the heart muscle and the blood vessels around the heart, leading to heart failure.
High Blood Pressure
Blood pressure is the force of blood pushing against the walls of the arteries. If this pressure rises and stays high over time, it can weaken your heart and lead to plaque buildup.
Blood pressure is considered high if it stays at or above 140/90 mmHg over time. (The mmHg is millimeters of mercury—the units used to measure blood pressure.) If you have diabetes or chronic kidney disease, high blood pressure is defined as 130/80 mmHg or higher.
Other Heart Conditions or Diseases
Other conditions and diseases also can lead to heart failure, such as:
- Arrhythmia. Happens when a problem occurs with the rate or rhythm of the heartbeat.
- Cardiomyopathy. Happens when the heart muscle becomes enlarged, thick, or rigid.
- Congenital heart defects. Problems with the heart’s structure are present at birth.
- Heart valve disease. Occurs if one or more of your heart valves doesn’t work properly, which can be present at birth or caused by infection, other heart conditions, and age.
Other Factors
Other factors also can injure the heart muscle and lead to heart failure. Examples include:
- Alcohol abuse or cocaine and other illegal drug use
- HIV/AIDS
- Thyroid disorders (having either too much or too little thyroid hormone in the body)
- Too much vitamin E
- Treatments for cancer, such as radiation and chemotherapy.
Risk factors for congestive heart failure
Diseases and conditions that increase your risk of heart failure include:
- Coronary artery disease. Narrowed arteries may limit the heart’s supply of oxygen-rich blood, resulting in weakened heart muscle.
- Heart attack. A heart attack is a form of coronary artery disease that occurs suddenly. Damage to the heart muscle from a heart attack may mean the heart can no longer pump as well as it should.
- Heart valve disease. Having a heart valve that doesn’t work properly raises the risk of heart failure.
- High blood pressure. The heart works harder than it has to when blood pressure is high.
- Irregular heartbeats. Irregular heartbeats, especially if they are very frequent and fast, can weaken the heart muscle and cause heart failure.
- Congenital heart disease. Some people who develop heart failure were born with changes in the structure or function of their heart.
- Diabetes. Having diabetes increases the risk of high blood pressure and coronary artery disease.
- Sleep apnea. This inability to breathe properly during sleep results in low blood-oxygen levels and an increased risk of irregular heartbeats. These things can lead to a weakened heart.
- Obesity. People who have obesity have a higher risk of developing heart failure.
- Viral infections. Some viral infections can damage to the heart muscle.
Medicines that may increase the risk of heart failure include:
- Some diabetes medicines. The diabetes medicines rosiglitazone (Avandia) and pioglitazone (Actos) have been found to increase the risk of heart failure in some people. Don’t stop taking these medicines without first talking to your doctor.
- Other medicines that may lead to heart failure or heart conditions include nonsteroidal anti-inflammatory drugs (NSAIDs) and some medicines used to treat high blood pressure, cancer, blood conditions, irregular heartbeats, nervous system diseases, mental health conditions, lung and urinary conditions, and infections.
Other risk factors for heart failure include:
- Aging. The heart’s ability to work decreases with age, even in healthy people.
- Alcohol use. Drinking too much alcohol may weaken the heart muscle and lead to heart failure.
- Smoking or using tobacco. If you smoke, quit. Using tobacco increases the risk of heart disease and heart failure.
Congestive heart failure prevention
The key to preventing heart failure is to reduce your risk factors. You can control or eliminate many of the risk factors for heart disease — high blood pressure and coronary artery disease, for example — by making lifestyle changes along with the help of any needed medications.
Lifestyle changes you can make to help prevent heart failure include:
- Not smoking
- Controlling certain conditions, such as high blood pressure and diabetes
- Staying physically active
- Eating healthy foods
- Maintaining a healthy weight
- Reducing and managing stress.
Congestive heart failure symptoms
If you have heart failure, your heart can’t supply enough blood to meet your body’s needs. Symptoms may develop slowly. Sometimes, heart failure symptoms start suddenly.
The most common signs and symptoms of heart failure are 74:
- Shortness of breath (dyspnea) or trouble breathing when you exert yourself or when you lie down
- Fatigue, tiredness and weakness
- Swelling (edema) in your legs, ankles and feet
- Rapid or irregular heartbeat
- Reduced ability to exercise
- Wheezing.
- A cough that doesn’t go away or a cough that brings up white or pink mucus with spots of blood.
- Increased need to urinate at night
- Swelling of your abdomen (ascites)
- Sudden weight gain from fluid retention
- Lack of appetite and nausea
- Difficulty concentrating or decreased alertness
- Sudden, severe shortness of breath and coughing up pink, foamy mucus
- Chest pain if your heart failure is caused by a heart attack
- Prominent veins in the neck
All of these symptoms are the result of fluid buildup in your body. When symptoms start, you may feel tired and short of breath after routine physical effort, like climbing stairs.
As your heart grows weaker, symptoms get worse. You may begin to feel tired and short of breath after getting dressed or walking across the room. Some people have shortness of breath while lying flat.
Fluid buildup from heart failure also causes weight gain, frequent urination, and a cough that’s worse at night and when you’re lying down. This cough may be a sign of acute pulmonary edema. This is a condition in which too much fluid builds up in your lungs. The condition requires emergency treatment.
Cardiac asthma
Congestive heart failure complications
If you have heart failure, your outlook depends on the cause and the severity, your overall health, and other factors such as your age. Complications can include:
- Kidney damage or failure. Heart failure can reduce the blood flow to your kidneys, which can eventually cause kidney failure if left untreated. Kidney damage from heart failure can require dialysis for treatment.
- Heart valve problems. The valves of your heart, which keep blood flowing in the proper direction through your heart, may not function properly if your heart is enlarged or if the pressure in your heart is very high due to heart failure.
- Heart rhythm problems. Heart rhythm problems (arrhythmias) can be a potential complication of heart failure.
- Sudden cardiac death. If the heart is weak, there is a risk of dying suddenly due to a dangerous irregular heart rhythm.
- Liver damage. Heart failure can lead to a buildup of fluid that puts too much pressure on the liver. This fluid backup can lead to scarring, which makes it more difficult for your liver to function properly.
- Malnutrition.
Some people’s symptoms and heart function will improve with proper treatment. However, heart failure can be life-threatening. People with heart failure may have severe symptoms, and some may require heart transplantation or support with a ventricular assist device.
Congestive heart failure diagnosis
To diagnose heart failure, your doctor will take a careful medical history, review your symptoms and perform a physical examination. Your doctor will also check for the presence of risk factors, such as high blood pressure, coronary artery disease or diabetes.
Using a stethoscope, your doctor can listen to your lungs for signs of congestion. The stethoscope also picks up abnormal heart sounds that may suggest heart failure. The doctor may examine the veins in your neck and check for fluid buildup in your abdomen and legs.
After the physical exam, your doctor may also order some of these tests:
- Blood tests: Your doctor may take a sample of your blood to check your kidney, liver and thyroid function and to look for indicators of other diseases that affect the heart. A BNP blood test to check for a chemical called N-terminal pro-B-type natriuretic peptide (NT-proBNP) may help in diagnosing heart failure if the diagnosis isn’t certain when used in addition to other tests.
- Chest X-ray: Chest X-ray images help your doctor see the condition of your lungs and heart. In heart failure, your heart may appear enlarged and fluid buildup may be visible in your lungs. Your doctor can also use an X-ray to diagnose conditions other than heart failure that may explain your signs and symptoms.
- Electrocardiogram (EKG or ECG): This test records the electrical activity of your heart through electrodes attached to your skin. Impulses are recorded as waves and displayed on a monitor or printed on paper. This test helps your doctor diagnose heart rhythm problems and damage to your heart from a heart attack that may be underlying heart failure.
- Echocardiogram: An important test for diagnosing heart failure is the echocardiogram. An echocardiogram helps distinguish systolic heart failure from diastolic heart failure in which the heart is stiff and can’t fill properly. An echocardiogram uses sound waves to produce a video image of your heart. This test can help doctors see the size and shape of your heart and how well your heart is pumping. The echocardiogram also can help doctors look for valve problems or evidence of previous heart attacks, other heart abnormalities, and some unusual causes of heart failure. Your ejection fraction is measured during an echocardiogram and can also be measured by nuclear medicine tests, cardiac catheterization and cardiac MRI. This is an important measurement of how well your heart is pumping and is used to help classify heart failure and guide treatment.
- Doppler Ultrasound: A Doppler ultrasound uses sound waves to measure the speed and direction of blood flow. This test often is done with echo to give a more complete picture of blood flow to the heart and lungs. Doctors often use Doppler ultrasound to help diagnose right-side heart failure.
- Holter Monitor: A Holter monitor records your heart’s electrical activity for a full 24- or 48-hour period, while you go about your normal daily routine. You wear small patches called electrodes on your chest. Wires connect the patches to a small, portable recorder. The recorder can be clipped to a belt, kept in a pocket, or hung around your neck.
- Multigated Acquisition Scan (MUGA scan): A MUGA scan measures how your heart muscle contracts and relaxes while you rest or exercise. A MUGA scan uses an injection of a substance called technetium-99m-pertechnetate (Tc-99m) and a specialized camera. As the radionuclide (Tc-99m) travels through your blood, your doctor takes pictures of your heart. A nuclear heart scan can show where the heart muscle is healthy and where it’s damaged. A MUGA scan measures your ejection fraction (EF). EF is how much blood your heart pumps out each time it squeezes (contracts). The tracer you receive is safe for most people. Your body will get rid of it through your kidneys within about 24 hours. There is a risk of radiation exposure, bleeding and allergic reaction. If you’re pregnant or think you might be pregnant, or if you’re a nursing mother, don’t have this test. It could harm your baby.
- PET scan. A positron emission tomography (PET) scan is a type of nuclear heart scan. It shows the level of chemical activity in areas of your heart. This test can help your doctor see whether enough blood is flowing to these areas. A PET scan can show blood flow problems that other tests might not detect.
- Exercise tests or stress tests: Stress tests measure how your heart and blood vessels respond to exertion. You may walk on a treadmill or pedal a stationary bike while attached to an ECG machine. Or you may receive a drug intravenously that stimulates your heart similar to exercise. Sometimes the stress test can be done while wearing a mask that measures the ability of your heart and lungs to take in oxygen and breathe out carbon dioxide. Stress tests help doctors see if you have coronary artery disease. Stress tests also determine how well your body is responding to your heart’s decreased pumping effectiveness and can help guide long-term treatment decisions. If your doctor also wants to see images of your heart while you’re exercising, he or she may order a nuclear stress test or a stress echocardiogram. It’s similar to an exercise stress test, but it also uses imaging techniques to visualize your heart during the test.
- Cardiac computerized tomography (CT) scan. In a cardiac CT scan, you lie on a table inside a doughnut-shaped machine. An X-ray tube inside the machine rotates around your body and collects images of your heart and chest.
- Cardiac magnetic resonance imaging (MRI) also called heart MRI scan. In a cardiac MRI, you lie on a table inside a long tube-like machine that produces a magnetic field. The magnetic field aligns atomic particles in some of your cells. When radio waves are broadcast toward these aligned particles, they produce signals that vary according to the type of tissue they are. The signals create images of your heart.
- Cardiac catheterization (cardiac cath or heart cath): During cardiac catheterization, a long, thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck and threaded to your heart. This allows your doctor to look inside your coronary (heart) arteries. During this procedure, your doctor can check the pressure and blood flow in your heart chambers, collect blood samples, and use x rays to look at your coronary arteries. Cardiac catheterization is one of the most common heart procedures performed in the U.S. Cardiac cath is usually very safe. Major complications are very rare. Some minor risks include:
- Bruises where the catheter was inserted (puncture site)
- Bleeding at the puncture site
- Reaction to the contrast dye
- Infection
- Side effects, such as nausea or vomiting, from the medications given to help you relax or sleep during the procedure
- Some other risks include:
- Abnormal heart rhythm
- Blood clots
- Damage to a blood vessel or heart from the catheter
- Heart attack
- Side effects from X-rays
- Stroke
- Coronary Angiogram: In this test, a thin, flexible tube (catheter) is inserted into a blood vessel at your groin or in your arm and guided through the aorta into your coronary arteries. A dye injected through the catheter makes the arteries supplying your heart visible on an X-ray. This test helps doctors identify narrowed arteries to your heart (coronary artery disease) that can be a cause of heart failure. The test may include a ventriculogram — a procedure to determine the strength of the heart’s main pumping chamber (left ventricle) and the health of the heart valves.
- Myocardial biopsy: In this test, your doctor inserts a small, flexible biopsy cord into a vein in your neck or groin, and small pieces of the heart muscle are taken. This test may be performed to diagnose certain types of heart muscle diseases that cause heart failure.
- Genetic Testing. A DNA test (genetic testing) is a medical test that can identify mutations in your genes, chromosomes or proteins. Genetic testing looks for changes in your genes, chromosomes and proteins. DNA tests can give you lots of information about the genes that make up who you are. They can confirm if you have or don’t have a specific disease. DNA tests can also identify your risk for developing a certain condition or passing on a genetic disorder.
Results of these tests help doctors determine the cause of your signs and symptoms and develop a program to treat your heart. Your heart doctor may tell you the stage of your heart failure.
There are 2 main ways to determine the stage of heart failure:
New York Heart Association (NYHA) classification
New York Heart Association (NYHA) classification system groups heart failure into four categories by number. You may see Roman numerals used for these category names.
- Class 1 (I) heart failure. There are no heart failure symptoms.
- Class 2 (II) heart failure. Everyday activities can be done without difficulty. But exertion causes shortness of breath or fatigue.
- Class 3 (III) heart failure. It’s difficult to complete everyday activities.
- Class 4 (IV) heart failure. Shortness of breath occurs even at rest. This category includes the most severe heart failure.
American College of Cardiology/American Heart Association classification
American College of Cardiology/American Heart Association classification system uses letters A to D 21. It includes a category for people who are at risk of developing heart failure.
Stage A: At risk for heart failure
- People who are at risk for heart failure but do not yet have symptoms or structural or functional heart disease. Risk factors for people in stage A include hypertension, coronary vascular disease, diabetes, obesity, exposure to cardiotoxic agents, genetic variants for cardiomyopathy and family history of cardiomyopathy
Stage B: Pre-heart failure
- People without current or previous symptoms of heart failure but with either structural heart disease, increased filling pressures in the heart or other risk factors
Stage C: Symptomatic heart failure
- People with current or previous symptoms of heart failure
Stage D: Advanced heart failure
- People with heart failure symptoms that interfere with daily life functions or lead to repeated hospitalizations. Advanced heart failure requires specialized treatments.
Congestive heart failure treatment
Early diagnosis and treatment can help people who have heart failure live longer, more active lives. Treatment of heart failure depends on the cause, the type and severity of the heart failure. Treatment often includes lifestyle changes and medicines. If another health condition is causing the heart to fail, treating it may reverse heart failure.
Heart failure is a chronic disease needing lifelong management. However, with treatment, signs and symptoms of heart failure can improve, and the heart sometimes becomes stronger. Treatment may help you live longer and reduce your chance of dying suddenly.
Doctors sometimes can correct heart failure by treating the underlying cause. Some people with heart failure need surgery to open blocked arteries or to place a device to help the heart work better. For example, repairing a heart valve or controlling a fast heart rhythm may reverse heart failure. But for most people, the treatment of heart failure involves a balance of the right medications and, in some cases, use of devices that help the heart beat and contract properly.
The goals of treatment for all stages of heart failure include:
- Treating the condition’s underlying cause, such as coronary heart disease, high blood pressure, or diabetes
- Reducing symptoms
- Stopping the heart failure from getting worse
- Increasing your lifespan and improving your quality of life
Treatments usually include heart-healthy lifestyle changes, medicines, and ongoing care. If you have severe heart failure, you also may need medical procedures or surgery.
Lifestyle and home remedies
Making lifestyle changes can often help relieve signs and symptoms of heart failure and prevent the disease from worsening. These changes may be among the most important and beneficial you can make. Lifestyle changes your doctor may recommend include:
- Stop smoking. Smoking damages your blood vessels, raises blood pressure, reduces the amount of oxygen in your blood and makes your heart beat faster.
If you smoke, ask your doctor to recommend a program to help you quit. You can’t be considered for a heart transplant if you continue to smoke. Avoid secondhand smoke, too.
- Discuss weight monitoring with your doctor. Discuss with your doctor how often you should weigh yourself. Ask your doctor how much weight gain you should notify him or her about. Weight gain may mean that you’re retaining fluids and need a change in your treatment plan.
- Check your legs, ankles and feet for swelling daily. Check for any changes in swelling in your legs, ankles or feet daily. Check with your doctor if the swelling worsens.
- Eat a healthy diet. Aim to eat a diet that includes fruits and vegetables, whole grains, fat-free or low-fat dairy products, and lean proteins.
- Restrict salt in your diet. Too much sodium contributes to water retention, which makes your heart work harder and causes shortness of breath and swollen legs, ankles and feet.
Check with your doctor for the sodium restriction recommended for you. Keep in mind that salt is already added to prepared foods, and be careful when using salt substitutes.
- Maintain a healthy weight. If you’re overweight, your dietitian will help you work toward your ideal weight. Even losing a small amount of weight can help.
- Consider getting vaccinations. If you have heart failure, you may want to get influenza and pneumonia vaccinations. Ask your doctor about these vaccinations.
- Limit fats and cholesterol. In addition to avoiding high-sodium foods, limit the amount of saturated fat, trans fat and cholesterol in your diet. A diet high in fat and cholesterol is a risk factor for coronary artery disease, which often underlies or contributes to heart failure.
- Limit alcohol and fluids. Your doctor likely will recommend that you don’t drink alcohol if you have heart failure, since it can interact with your medication, weaken your heart muscle and increase your risk of abnormal heart rhythms.
- Getting medical care for other related conditions is important. If you have diabetes or high blood pressure, work with your health care team to control these conditions. Have your blood sugar level and blood pressure checked. Talk with your doctor about when you should have tests and how often to take measurements at home.
If you have severe heart failure, your doctor may also suggest you limit the amount of fluids you drink.
- Be active. Moderate aerobic activity helps keep the rest of your body healthy and conditioned, reducing the demands on your heart muscle. Before you start exercising though, talk to your doctor about an exercise program that’s right for you. Your doctor may suggest a walking program.
Check with your local hospital to see if it offers a cardiac rehabilitation program; if it does, talk to your doctor about enrolling in the program.
- Reduce stress. When you’re anxious or upset, your heart beats faster, you breathe more heavily and your blood pressure often goes up. This can make heart failure worse, since your heart is already having trouble meeting the body’s demands.
Find ways to reduce stress in your life. To give your heart a rest, try napping or putting your feet up when possible. Spend time with friends and family to be social and help keep stress at bay.
- Sleep easy. If you’re having shortness of breath, especially at night, sleep with your head propped up using a pillow or a wedge. If you snore or have had other sleep problems, make sure you get tested for sleep apnea.
To improve your sleep at night, prop up your head with pillows. Also, discuss with your doctor changing the time for taking medications, especially diuretics. Taking diuretics earlier in the day may decrease the need to urinate as often during the night.
Medications
Doctors usually treat heart failure with a combination of medications. Depending on your symptoms, you might take one or more medications, including:
- Angiotensin-converting enzyme (ACE) inhibitors. These medicines relax blood vessels to lower blood pressure, improve blood flow and decrease the strain on the heart. Examples include enalapril (Vasotec, Epaned), lisinopril (Zestril, Qbrelis) and captopril.
- Angiotensin 2 receptor blockers (ARBs). These medicines have many of the same benefits as ACE inhibitors. They may be an option for people who can’t tolerate ACE inhibitors. They include losartan (Cozaar), valsartan (Diovan) and candesartan (Atacand).
- Angiotensin receptor plus neprilysin inhibitors (ARNIs). This medicine uses two blood pressure medicines to treat heart failure. The combination medicine is sacubitril-valsartan (Entresto). It’s used to treat some people with heart failure with reduced ejection fraction. It may help prevent the need for a hospital stay in those people.
- Beta blockers. These medicines slow the heart rate and lower blood pressure. They reduce the symptoms of heart failure and help the heart work better. If you have heart failure, beta blockers may help you live longer. Examples include carvedilol (Coreg), metoprolol (Lopressor, Toprol-XL, Kapspargo Sprinkle) and bisoprolol.
- Ivabradine (Corlanor): This medication is known as an If channel blocker. This drug slows the heart rate differently from beta-blockers, without lowering blood pressure.
- Diuretics or water pills, these medicines make you urinate more frequently. This helps prevent fluid buildup in your body. Diuretics, such as furosemide (Lasix, Furoscix), also decrease fluid in the lungs, so it’s easier to breathe. Some diuretics make the body lose potassium and magnesium. Your doctor may recommend supplements to treat this. If you’re taking a diuretic, you may have regular blood tests to check your potassium and magnesium levels.
- Potassium-sparing diuretics also called aldosterone antagonists, these medicines include spironolactone (Aldactone, CaroSpir) and eplerenone (Inspra). They may help people with severe heart failure with reduced ejection fraction (HFrEF) live longer. Unlike some other diuretics, these medicines can raise the level of potassium in the blood to dangerous levels. Talk with your doctor about your diet and potassium intake.
- Sodium-glucose cotransporter-2 (SGLT2) inhibitors. These medicines help lower blood sugar. They are often prescribed with diet and exercise to treat type 2 diabetes. But they’re also one of the first treatments for heart failure. That’s because several studies showed that the medicine lowered the risk of hospital stays and death in people with certain types of heart failure — even if they didn’t have diabetes. Sodium-glucose cotransporter-2 (SGLT2) inhibitors include canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance).
- Digoxin (Lanoxin) also called digitalis, helps the heart squeeze better to pump blood. It also tends to slow the heartbeat. Digoxin reduces heart failure symptoms in people with heart failure with reduced ejection fraction (HFrEF). It may be more likely to be given to someone with a heart rhythm disorder, such as atrial fibrillation. The level of digoxin in the body must be checked using a blood test. If too much digoxin builds up in your blood, side effects may occur, including loss of appetite, nausea, vomiting and headaches. The heart rhythm can also become too fast or too slow. Always report any side effects of Digoxin to your doctor right away.
- Hydralazine and isosorbide dinitrate (BiDil). This combination of medicines helps relax blood vessels. It may be added to your treatment plan if you have severe heart failure symptoms and ACE inhibitors or beta blockers haven’t helped.
- Vericiguat (Verquvo). This medicine for chronic heart failure is taken once a day by mouth. This medication is known as a soluble guanylate cyclase (SGc) inhibitor. It works by increasing the amount of nitric oxide, which is a natural chemical in the body that helps to widen blood vessels. This helps reduce the workload on the heart. In studies, people with high-risk heart failure who took this medicine had fewer hospital stays for heart failure and heart disease-related deaths compared with those who got a dummy pill.
- Positive inotropes. These medicines may be given by IV to people with certain types of severe heart failure who are in the hospital. Positive inotropes can help the heart pump blood better and maintain blood pressure. Long-term use of these medicines has been linked to an increased risk of death in some people. Talk with your doctor about the benefits and risks of these medicines.
You may need to take two or more medications to treat heart failure. Your doctor may prescribe other heart medications as well — such as nitrates for chest pain, a statin to lower cholesterol or blood-thinning medications to help prevent blood clots — along with heart failure medications.
Your doctor may need to change your medicine doses frequently. This is more common when you’ve just started a new medicine or when your condition is getting worse.
You may be hospitalized if you have a flare-up of heart failure symptoms. While in the hospital, you may receive additional medications to help your heart pump better and relieve your symptoms. You may also receive supplemental oxygen through a mask or small tubes placed in your nose. If you have severe heart failure, you may need to use supplemental oxygen long term.
Your doctor may also prescribe other medications for additional health conditions that may occur with heart failure. These include:
- Potassium and magnesium supplements: Diuretics can remove potassium and magnesium from the body. Your doctor may prescribe potassium and/or magnesium supplements to ensure these levels remain normal while you are being treated.
- Anticoagulants also known as blood thinners: Anticoagulants are used in heart failure patients with atrial fibrillation, an artificial heart valve, blood clots or in people at high risk for blood clots. They help prevent blood clots from forming and blocking blood flow. Clots may form in the legs, lungs or heart. If a clot breaks off and gets stuck inside a blood vessel that supplies the brain, a stroke can result.
- Cholesterol-lowering drugs (statins): Your doctor may prescribe this class of medication if you have high cholesterol or have had a heart attack. They are not used to treat heart failure but other conditions as indicated. These medications help prevent the formation of plaque, which helps reduce the risk of heart attack and stroke.
- Oxygen therapy delivers concentrated oxygen to the lungs. This helps increase the amount of oxygen that can get into the blood. Oxygen therapy can improve shortness of breath and increase a person’s ability to be physically active.
- Some people may receive nitrates for chest pain.
Surgery and medical devices
In some cases, doctors recommend surgery to treat the underlying problem that led to heart failure. Some treatments being studied and used in certain people include:
- Coronary artery bypass graft surgery (CABG). If severely blocked coronary arteries are contributing to your heart failure, your doctor may recommend coronary artery bypass surgery. In this procedure, blood vessels from your leg, arm or chest bypass a blocked artery in your heart to allow blood to flow through your heart more freely.
- Heart valve repair or replacement. If a damaged heart valve causes your heart failure, your doctor may recommend repairing or replacing the heart valve. The surgeon can modify the original valve (valvuloplasty) to eliminate backward blood flow. Surgeons can also repair the valve by reconnecting valve leaflets or by removing excess valve tissue so that the leaflets can close tightly. Sometimes repairing the heart valve includes tightening or replacing the ring around the valve (annuloplasty). The type of heart valve surgery you need depends on the cause of your heart valve disease. Valve replacement is done when valve repair isn’t possible. In valve replacement surgery, the damaged valve is replaced by an artificial (prosthetic) valve. Certain types of heart valve repair or replacement can now be done without open heart surgery, using either minimally invasive surgery or cardiac catheterization techniques.
- Implantable cardioverter-defibrillator (ICD). An implantable cardioverter-defibrillator (ICD) is a device similar to a pacemaker. It’s implanted under the skin in your chest with wires leading through your veins and into your heart. The implantable cardioverter-defibrillator (ICD) monitors the heart rhythm. If the heart starts beating at a dangerous rhythm, or if your heart stops, the implantable cardioverter-defibrillator tries to pace your heart or shock it back into normal rhythm. An implantable cardioverter-defibrillator (ICD) can also function as a pacemaker and speed your heart up if it is going too slow.
- Cardiac resynchronization therapy (CRT) also called biventricular pacing, cardiac resynchronization therapy (CRT) is a treatment for heart failure in people whose lower heart chambers aren’t pumping in sync with each other. A biventricular pacemaker sends timed electrical impulses to both of the heart’s lower chambers (the left and right ventricles) so that they pump in a more efficient, coordinated manner. The signals tell the chambers to squeeze in a more coordinated way. This improves the pumping of blood out of the heart. Many people with heart failure have problems with their heart’s electrical system that cause their already-weak heart muscle to beat in an uncoordinated fashion. This inefficient muscle contraction may cause heart failure to worsen. Often a cardiac resynchronization therapy (CRT) or biventricular pacemaker is combined with an implantable cardioverter-defibrillator (ICD) for people with heart failure.
- Ventricular assist device (VAD) also called a mechanical circulatory support device. Ventricular assist devices are implanted into your abdomen or chest and attached to a weakened heart to help it pump blood to the rest of your body. A ventricular assist device (VAD) helps pump blood from the lower chambers of the heart to the rest of the body. Although a ventricular assist device (VAD) can be placed in one or both ventricles of the heart, it’s usually placed in the heart’s left ventricle. Your doctor may recommend a ventricular assist device (VAD) if you’re waiting for a heart transplant. Sometimes, a ventricular assist device (VAD) is used as a permanent treatment for people who have heart failure but who aren’t good candidates for a heart transplant. Doctors first used heart pumps to help keep heart transplant candidates alive while they waited for a donor heart. Ventricular assist devices are now sometimes used as an alternative to transplantation. Implanted heart pumps can significantly extend and improve the lives of some people with severe heart failure who aren’t eligible for or able to undergo heart transplantation or are waiting for a new heart. Major complications associated with left ventricular assist devices include bleeding, infection, and device malfunction. Temporary right ventricular failure immediately following an left ventricular assist device placement can occur in 30% of patients requiring inotropes or right ventricular assist device 75.
- Heart transplant. Some people have such severe heart failure that surgery or medicines don’t help. These people may need to have their hearts replaced with a healthy donor heart. A heart transplant isn’t the right treatment for everyone. A team of doctors at a transplant center helps determine whether the procedure may be safe and beneficial for you. Usually, patients <50 years of age who are brain dead are potential cardiac donors. Contraindications for heart donation include significant heart dysfunction, congenital heart disease, malignancies (except basal cell and squamous cell carcinomas of skin, primary tumors of the central nervous system with low metastatic potential), or transmissible diseases 75. Heart transplants can dramatically improve the survival and quality of life of some people with severe heart failure. However, candidates for transplantation often have to wait a long time before a suitable donor heart is found. Some transplant candidates improve during this waiting period through drug treatment or device therapy and can be removed from the transplant waiting list. Heart transplantation is the treatment of choice for patients with heart failure refractory to medical therapy. Data from the 2008 report from the registry of the International Society for Heart and Lung Transplant showed that patient survival at 1 and 3 years for patients who received cardiac transplantation was approximately 85% and 79%, respectively 76. Recent advances in medical and device therapies have also improved the survival of heart failure patients comparable to that for post-heart transplant 77. More patients need heart transplantation than there are donor hearts available. Heart transplantation is limited to patients who are most likely to benefit with a significant improvement in symptoms and life expectancy.
- Stem Cells – Experimental Approaches: Early clinical studies in patients with heart failure have shown the feasibility of transfer of distinct stem and progenitor cell populations to the heart, and have demonstrated beneficial effects on cardiac function and/or tissue viability 78. However, due to small study sizes, lack of randomised control groups, poor understanding of the mechanisms of action of transplanted cells, lack of information on procedural issues (that is, optimal cell type, cell dosage, timing of cell transfer, optimal route of application), and safety concerns with some progenitors (such as the arrhythmogenicity associated with skeletal myoblast grafts), further basic research and the initiation of large, double‐blind, placebo‐controlled, randomised clinical trials with hard end‐points (including mortality) are warranted before the role of cell‐based therapy of heart failure can be judged.
Figure 7. An intracorporeal left ventricular assist device and its components
Cardiac rehabilitation
Cardiac rehabilitation is a medically supervised program to help heart patients improve overall physical, mental and social function. The goal is to stabilize, slow or even reverse the progression of heart failure. This can help reduce the risk of heart disease, another cardiac event or death.
Cardiac rehab programs usually provide:
- A medical evaluation to determine your needs and limitations.
- A physical activity program tailored to your needs and limits.
- Counseling and education to help you understand your condition and how to manage it.
- Support and training to help you return to work or your normal activities.
- Counseling on modifying risk factors through nutrition and the use of prescribed medications.
Unfortunately, not everyone is eligible for or covered for cardiac rehab. Many people feel they can’t afford to spend the time and effort needed to complete cardiac rehab. But cardiac rehab programs save lives. There are other benefits too, both physical and emotional.
Patients repeatedly acknowledge that the benefits of cardiac rehab are worth the investment of time and energy. Even if you can’t attend rehab as often as you’d like, going when you can is beneficial.
Stage A heart failure treatment
Treatment for people with Stage A heart failure includes:
- Regular exercise, such as walking every day.
- No tobacco products.
- Treatment for high blood pressure (medication, low-sodium diet, active lifestyle).
- Treatment for high cholesterol.
- No alcohol or recreational drugs.
- Angiotensin-converting enzyme inhibitor (ACE-I) or an angiotensin II receptor blocker (ARB) if you have coronary artery disease, diabetes, high blood pressure or other vascular or cardiac conditions.
Stage B heart failure treatment
Treatment for people with Stage B heart failure includes:
- Treatments for Stage A.
- Angiotensin-converting enzyme inhibitor (ACE-I) or angiotensin II receptor blocker (ARB) if your EF is 40% or lower.
- Beta-blocker if you’ve had a heart attack and your EF is 40% or lower (if you aren’t already taking one).
- Aldosterone antagonist if you’ve had a heart attack or if you have an EF of 35% or less.
- Possible surgery or intervention as a treatment for coronary artery blockage, heart attack, valve disease (valve repair or replacement) or congenital heart disease.
Stage C heart failure treatment
Treatment for people with Stage C heart failure with reduced ejjection fraction (HFrEF) also referred to as systolic heart failure includes:
- Treatments from Stages A and B.
- Beta-blocker.
- Aldosterone antagonist.
- Sodium-glucose transport 2 inhibitors (SGLT2i).
- Hydralazine/nitrate combination if other treatments don’t stop your symptoms and you’re African American.
- Medications that slow your heart rate if your heart rate is faster than 70 beats per minute and you still have symptoms.
- A diuretic (“water pill”) if symptoms continue.
- Restriction of sodium (salt) in your diet.
- Weight tracking every day. Tell your doctor if you gain or lose more than 4 pounds.
- Possible fluid restriction.
- Possible cardiac resynchronization therapy (biventricular pacemaker).
- Possible implantable cardiac defibrillator (ICD) therapy.
If the treatment improves or stops your symptoms, you still need to continue treatment to slow the progression to Stage D.
Stage D heart failure treatment
Treatment for people who have Stage D heart failure includes treatments for Stages A, B and C. In addition, it includes evaluation for more advanced treatment options, including:
- Heart transplant.
- Ventricular assist devices.
- Heart surgery.
- Continuous infusion of inotropic drugs.
- Palliative or hospice care.
Stages C and D heart failure with preserved ejection fraction treatment
Treatment for people with Stage C and Stage D heart failure and preserved EF (HFpEF) also referred to as diastolic heart failure includes:
- Treatments for Stages A and B.
- Medications for the treatment of medical conditions that can cause heart failure or make it worse, such as atrial fibrillation, high blood pressure, diabetes, obesity, coronary artery disease, chronic lung disease, high cholesterol and kidney disease.
- Diuretic (“water pill”) to reduce or relieve symptoms.
It’s very important for you to manage your other health conditions, such as:
- Diabetes.
- Kidney disease.
- Anemia.
- High blood pressure.
- Thyroid disease.
- Asthma.
- Chronic lung disease.
Some conditions have signs and symptoms similar to congestive heart failure. If you have new or worsening nonurgent symptoms, tell your doctor.
End-of-life care and heart failure
Even with the number of treatments available for heart failure, it’s possible that your heart failure may worsen to the point where medications are no longer working and a heart transplant or device isn’t an option. If this occurs, you may need to enter hospice care. Hospice care provides a special course of treatment to terminally ill people.
Hospice care allows family and friends — with the aid of nurses, social workers and trained volunteers — to care for and comfort a loved one at home or in hospice residences. Hospice care provides emotional, psychological, social and spiritual support for people who are ill and those closest to them.
Although most people under hospice care remain in their own homes, the program is available anywhere — including nursing homes and assisted living centers. For people who stay in a hospital, specialists in end-of-life care can provide comfort, compassionate care and dignity.
Although it can be difficult, discuss end-of-life issues with your family and medical team. Part of this discussion will likely involve advance directives — a general term for oral and written instructions you give concerning your medical care should you become unable to speak for yourself.
If you have an implantable cardioverter-defibrillator, one important consideration to discuss with your family and doctors is turning off the defibrillator so that it can’t deliver shocks to make your heart continue beating.
Congestive heart failure prognosis
Congestive heart failure is a chronic, or lifelong, condition. You’ll need to treat it for the rest of your life. Heart failure is frequently a progressive disease process, and progression is associated with decreased survival, regardless of underlying cause 21, 79. With the right care, congestive heart failure won’t stop you from doing the things you enjoy.
Your prognosis, or outlook for the future, will depend on:
- How well your heart muscle is working.
- Your symptoms.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
One study says that people with congestive heart failure have a life span 10 years shorter than those who don’t have heart failure. Another study showed that the survival rates of people with chronic heart failure were:
- 80% to 90% for one year.
- 50% to 60% for year five.
- 30% for 10 years.
A different study found that people who had heart failure had expected life spans ranging from three to 20 years after their hospital stay, depending on various factors like age and sex. It’s important to look at your specific situation when considering your prognosis.
Congestive heart failure life expectancy
Currently, heart failure is a serious condition and has no cure. But many people with heart failure lead a full, enjoyable life when the condition is managed with heart failure medications and healthy lifestyle changes. It’s also helpful to have the support of family and friends who understand your condition.
Eighty percent of men and 70% of women <65 years of age diagnosed with heart failure will die within 8 years 75. Following an initial hospitalization for heart failure, there is a 50% readmission rate at 6 months and nearly 20% incidence of death within 12 months 80.
Patients with end stage heart failure fall into stage D of the ABCD classification of the American College of Cardiology/American Heart Association and class III–IV of the New York Heart Association functional classification; they are characterised by advanced structural heart disease and pronounced symptoms of heart failure at rest or upon minimal physical exertion, despite maximal medical treatment according to current guidelines 4, 81. This patient population has a 1‐year mortality rate of approximately 50% and requires special therapeutic interventions 82.
Treatments—such as medicines and lifestyle changes—can help people who have the condition live longer and more active lives. Researchers continue to study new ways to treat heart failure and its complications.
Managing heart failure requires an open dialogue between you and your doctor. Be honest about whether you’re following recommendations concerning your diet, lifestyle and taking medications. Your doctor often can suggest strategies to help you get and stay on track.
You and your doctor can work together to help make your life more comfortable. Pay attention to your body and how you feel, and tell your doctor when you’re feeling better or worse. This way, your doctor will know what treatment works best for you. Don’t be afraid to ask your doctor questions about living with heart failure.
Steps that may help you manage your condition include:
- Keep track of the medications you take. Make a list and share it with any new doctors treating you. Carry the list with you all the time. Don’t stop taking any medications without talking to your doctor. If you experience side effects to medications, discuss them with your doctor.
- Avoid certain over-the-counter medications. Some over-the-counter medications, such as ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and diet pills, may worsen heart failure and lead to fluid buildup.
- Be careful about supplements. Some dietary supplements may interfere with heart failure medications or could worsen your condition. Talk to your doctor about any supplements you are taking.
- Keep track of your weight and bring the record to visits with your doctor. An increase in weight can be a sign you’re building up fluids. Your doctor may tell you to take extra diuretics if your weight has increased by a certain amount in a day.
- Keep track of your blood pressure. Consider purchasing a home blood pressure monitor. Keep track of your blood pressure between doctor appointments and bring the record with you to visits.
- Write down your questions for your doctor. Before a doctor appointment, prepare a list of any questions or concerns. For example, is it safe for you and your partner to have sex? Most people with heart failure can continue sexual activity once symptoms are under control. Ask for clarification, if necessary. Be sure you understand everything your doctor wants you to do.
- Know your doctor’s contact information. Keep your doctor’s phone number, the hospital’s phone number, and directions to the hospital or clinic on hand. You’ll want to have these available in case you have questions for your doctor or you need to go to the hospital.
Living with congestive heart failure
With the right care and treatment plan, many adults still enjoy life even though congestive heart failure limits their activities. The most important thing is to make healthy lifestyle habits part of your daily routine. The more you make healthy living part of your new lifestyle, the better you’ll feel. Try to:
- Work with a nutritionist or dietitian to create a nutritious, filling meal plan you can stick with long-term.
- Find an exercise routine you enjoy so you’ll be motivated to get moving every day. Try some type of physical activity 30 minutes each day, three days a week.
- Track and manage your symptoms. Report any changes to your healthcare provider.
- Take medications as instructed.
- People with congestive heart failure may need to limit how much salt and/or fluid they consume each day. Your doctor can give you guidelines for this.
You need emergency treatment when your heart failure suddenly gets worse. Doctors call this acute decompensated heart failure. Your doctor can give you medicine and oxygen to improve your condition.
Dealing with new emotions
You’re probably feeling many emotions connected with your condition. You may feel alone, angry, scared or different from the person you were before you learned you have heart failure. These feelings are common. They may go away as you learn to understand and manage your condition. The important thing to remember is that your emotions can affect managing your heart failure symptoms. It’s important to understand your feelings, recognize problems and ask for help if you need it.
Seeking support
As you become healthier, reach out again to family and friends. Don’t be discouraged if friends seem distant or uncomfortable at first. They may be afraid to talk about your condition. They might even say or do insensitive things. Keep in mind, their intent is not to hurt you. Big changes take getting used to, for them as well as you.
Staying connected with friends and family
Don’t assume that people no longer desire your company. What if someone you love had heart failure instead of you? Would you stop being interested in that person? Chances are you’d still want to have a close and active relationship.
Family and friends are likely to feel the same way about you. You’re worthy of love now, just as you were before your diagnosis. As you manage your symptoms and begin to feel better, be sure to stay engaged in life. You might start by accepting short visits. When you feel up to it, you can add more daily social activity.
Identifying your activity goals
Managing your heart failure symptoms is about returning to function. It’s also about doing things that make you satisfied with life. You might want to start by visiting with a friend. Or you might go for a short walk with a family member. As you start to feel better and become more active, you’ll be more able to handle life outside your home.
- Now is a good time to think about the things that matter most to you. What do you need to do? What do you want to do?
- Overall, take your time. Make a gradual return to your normal daily activities.
- Now that you have a better understanding of the tools you’ll need to manage heart failure, take the time to list your goals.
Dealing with advanced heart failure
Advanced heart failure means the condition has progressed to where traditional therapies and symptom management are no longer working. Of the more than 6 million American adults living with heart failure, about 10% have advanced heart failure. Their treatment decisions can become more complex.
When heart failure progresses to an advanced stage, difficult decisions must be made. Do I want to receive aggressive treatment? Is quality of life more important than living as long as possible? How do I feel about resuscitation?
For advanced heart failure patients and their health care professional, making good decisions requires teamwork. Through shared decision-making, doctors and patients consider both the options and the patient’s preferences before charting a treatment course.
- Martin SS, Aday AW, Almarzooq ZI, et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation. 2024 Feb 20;149(8):e347-e913. https://www.ahajournals.org/doi/10.1161/CIR.0000000000001209 Erratum in: Circulation. 2024 May 7;149(19):e1164. doi: 10.1161/CIR.0000000000001247[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Heart Failure. https://www.nhlbi.nih.gov/health/health-topics/topics/hf[↩][↩]
- American Heart Association. Types of Heart Failure. http://www.heart.org/HEARTORG/Conditions/HeartFailure/AboutHeartFailure/Types-of-Heart-Failure_UCM_306323_Article.jsp[↩][↩][↩]
- Guidelines for therapy of chronic heart failure. Hoppe UC, Böhm M, Dietz R, Hanrath P, Kroemer HK, Osterspey A, Schmaltz AA, Erdmann E, Vorstand der Deutschen Gesellschaft fur Kardiologie–Herz- und Kreislaufforschung e.V. Z Kardiol. 2005 Aug; 94(8):488-509. https://www.ncbi.nlm.nih.gov/pubmed/16049651/[↩][↩]
- Hall MJ, DeFrances CJ, Williams SN, et al. National Hospital Discharge Survey: 2007 summary. National health statistics reports; no 29. Hyattsville, MD: National Center for Health Statistics. 2010. https://www.cdc.gov/nchs/data/nhsr/nhsr029.pdf[↩]
- Mozzafarian D, Benjamin EJ, Go AS, et al. on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:e38-e360.[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. What Are the Signs and Symptoms of Heart Failure ? https://www.nhlbi.nih.gov/health/health-topics/topics/hf/signs[↩]
- American Heart Association. About Arrhythmia. http://www.heart.org/HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/About-Arrhythmia_UCM_002010_Article.jsp[↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Congenital Heart Defects (CHDs). https://www.cdc.gov/ncbddd/heartdefects/index.html[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Your Heart’s Electrical System. https://www.nhlbi.nih.gov/health/health-topics/topics/hhw/electrical[↩]
- Ejection Fraction Heart Failure Measurement. https://www.heart.org/en/health-topics/heart-failure/diagnosing-heart-failure/ejection-fraction-heart-failure-measurement[↩][↩]
- Ejection Fraction. https://my.clevelandclinic.org/health/articles/16950-ejection-fraction[↩]
- Regulation of Stroke Volume. https://cvphysiology.com/cardiac-function/cf002[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Who Is at Risk for Heart Failure ? https://www.nhlbi.nih.gov/health/health-topics/topics/hf/atrisk[↩]
- Types of Heart Failure. https://www.heart.org/en/health-topics/heart-failure/what-is-heart-failure/types-of-heart-failure[↩]
- Anker SD, Butler J, Filippatos G, et al. ; EMPEROR-Preserved Trial Investigators . Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385(16):1451-1461. doi: 10.1056/NEJMoa2107038[↩]
- Nassif ME, Windsor SL, Borlaug BA, et al. The SGLT2 inhibitor dapagliflozin in heart failure with preserved ejection fraction: a multicenter randomized trial. Nat Med. 2021;27(11):1954-1960. doi: 10.1038/s41591-021-01536-x[↩]
- Solomon SD, McMurray JJV, Anand IS, et al. ; PARAGON-HF Investigators and Committees . Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381(17):1609-1620. doi: 10.1056/NEJMoa1908655[↩]
- Tromp J, Shen L, Jhund PS, Anand IS, Carson PE, Desai AS, Granger CB, Komajda M, McKelvie RS, Pfeffer MA, Solomon SD, Køber L, Swedberg K, Zile MR, Pitt B, Lam CSP, McMurray JJV. Age-Related Characteristics and Outcomes of Patients With Heart Failure With Preserved Ejection Fraction. J Am Coll Cardiol. 2019 Aug 6;74(5):601-612. doi: 10.1016/j.jacc.2019.05.052[↩]
- Melenovsky V, Hwang SJ, Redfield MM, Zakeri R, Lin G, Borlaug BA. Left atrial remodeling and function in advanced heart failure with preserved or reduced ejection fraction. Circ Heart Fail. 2015 Mar;8(2):295-303. doi: 10.1161/CIRCHEARTFAILURE.114.001667[↩][↩]
- Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022 May 3;79(17):e263-e421. doi: 10.1016/j.jacc.2021.12.012. Erratum in: J Am Coll Cardiol. 2023 Apr 18;81(15):1551. doi: 10.1016/j.jacc.2023.03.002[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Shah SJ, Borlaug BA, Kitzman DW, et al. Research priorities for heart failure with preserved ejection fraction: National Heart, Lung, and Blood Institute Working Group summary. Circulation. 2020;141(12):1001-1026. doi: 10.1161/CIRCULATIONAHA.119.041886[↩]
- Redfield MM. Heart Failure with Preserved Ejection Fraction. N Engl J Med. 2017 Mar 2;376(9):897. doi: 10.1056/NEJMc1615918[↩]
- Pieske B, Tschöpe C, de Boer RA, et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J. 2019;40(40):3297-3317. doi: 10.1093/eurheartj/ehz641[↩][↩]
- Borlaug BA. Evaluation and management of heart failure with preserved ejection fraction. Nat Rev Cardiol. 2020;17(9):559-573. doi: 10.1038/s41569-020-0363-2[↩]
- Obokata M, Kane GC, Reddy YN, Olson TP, Melenovsky V, Borlaug BA. Role of diastolic stress testing in the evaluation for heart failure with preserved ejection fraction: a simultaneous invasive-echocardiographic study. Circulation. 2017;135(9):825-838. doi: 10.1161/CIRCULATIONAHA.116.024822[↩][↩]
- Reddy YNV, Carter RE, Obokata M, Redfield MM, Borlaug BAA. A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction. Circulation. 2018;138(9):861-870. doi: 10.1161/CIRCULATIONAHA.118.034646[↩]
- Obokata M, Reddy YNV, Borlaug BA. Diastolic dysfunction and heart failure with preserved ejection fraction: understanding mechanisms by using noninvasive methods. JACC Cardiovasc Imaging. 2020;13(1 Pt 2):245-257. doi: 10.1016/j.jcmg.2018.12.034[↩]
- Andersen, M.J., Borlaug, B.A. Heart Failure with Preserved Ejection Fraction: Current Understandings and Challenges. Curr Cardiol Rep 16, 501 (2014). https://doi.org/10.1007/s11886-014-0501-8[↩]
- Borlaug, B. The pathophysiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 11, 507–515 (2014). https://doi.org/10.1038/nrcardio.2014.83[↩]
- Virani SS, Alonso A, Benjamin EJ, et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020 Mar 3;141(9):e139-e596. doi: 10.1161/CIR.0000000000000757[↩]
- Reddy YNV, Kaye DM, Handoko ML, van de Bovenkamp AA, Tedford RJ, Keck C, Andersen MJ, Sharma K, Trivedi RK, Carter RE, Obokata M, Verbrugge FH, Redfield MM, Borlaug BA. Diagnosis of Heart Failure With Preserved Ejection Fraction Among Patients With Unexplained Dyspnea. JAMA Cardiol. 2022 Sep 1;7(9):891-899. doi: 10.1001/jamacardio.2022.1916[↩][↩]
- Borlaug BA, Nishimura RA, Sorajja P, Lam CS, Redfield MM. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail. 2010;3(5):588-595. doi: 10.1161/CIRCHEARTFAILURE.109.930701[↩]
- Selvaraj S, Myhre PL, Vaduganathan M, et al. Application of diagnostic algorithms for heart failure with preserved ejection fraction to the community. JACC Heart Fail. 2020;8(8):640-653. doi: 10.1016/j.jchf.2020.03.013[↩]
- Golla MSG, Shams P. Heart Failure With Preserved Ejection Fraction (HFpEF) [Updated 2024 Mar 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK599960[↩][↩][↩][↩]
- Pfeffer MA, Shah AM, Borlaug BA. Heart Failure With Preserved Ejection Fraction In Perspective. Circ Res. 2019 May 24;124(11):1598-1617. doi: 10.1161/CIRCRESAHA.119.313572[↩][↩]
- Solomon SD, Rizkala AR, Lefkowitz MP, et al. Baseline Characteristics of Patients With Heart Failure and Preserved Ejection Fraction in the PARAGON-HF Trial. Circ Heart Fail. 2018 Jul;11(7):e004962. doi: 10.1161/CIRCHEARTFAILURE.118.004962[↩][↩]
- Leggat J, Bidault G, Vidal-Puig A. Lipotoxicity: a driver of heart failure with preserved ejection fraction? Clin Sci (Lond). 2021 Oct 15;135(19):2265-2283. doi: 10.1042/CS20210127[↩]
- Faxen UL, Venkateshvaran A, Shah SJ, Lam CSP, Svedlund S, Saraste A, Beussink-Nelson L, Lagerstrom Fermer M, Gan LM, Hage C, Lund LH. Generalizability of HFA-PEFF and H2FPEF Diagnostic Algorithms and Associations With Heart Failure Indices and Proteomic Biomarkers: Insights From PROMIS-HFpEF. J Card Fail. 2021 Jul;27(7):756-765. doi: 10.1016/j.cardfail.2021.02.005[↩]
- Pandey A, Parashar A, Kumbhani D, Agarwal S, Garg J, Kitzman D, Levine B, Drazner M, Berry J. Exercise training in patients with heart failure and preserved ejection fraction: meta-analysis of randomized control trials. Circ Heart Fail. 2015 Jan;8(1):33-40. doi: 10.1161/CIRCHEARTFAILURE.114.001615[↩]
- Mueller S, Winzer EB, Duvinage A, et al. OptimEx-Clin Study Group. Effect of High-Intensity Interval Training, Moderate Continuous Training, or Guideline-Based Physical Activity Advice on Peak Oxygen Consumption in Patients With Heart Failure With Preserved Ejection Fraction: A Randomized Clinical Trial. JAMA. 2021 Feb 9;325(6):542-551. doi: 10.1001/jama.2020.26812[↩]
- Kitzman DW, Brubaker P, Morgan T, Haykowsky M, Hundley G, Kraus WE, Eggebeen J, Nicklas BJ. Effect of Caloric Restriction or Aerobic Exercise Training on Peak Oxygen Consumption and Quality of Life in Obese Older Patients With Heart Failure With Preserved Ejection Fraction: A Randomized Clinical Trial. JAMA. 2016 Jan 5;315(1):36-46. doi: 10.1001/jama.2015.17346[↩]
- Hummel SL, Seymour EM, Brook RD, Sheth SS, Ghosh E, Zhu S, Weder AB, Kovács SJ, Kolias TJ. Low-sodium DASH diet improves diastolic function and ventricular-arterial coupling in hypertensive heart failure with preserved ejection fraction. Circ Heart Fail. 2013 Nov;6(6):1165-71. doi: 10.1161/CIRCHEARTFAILURE.113.000481[↩]
- Kittleson MM, Panjrath GS, Amancherla K, Davis LL, Deswal A, Dixon DL, Januzzi JL Jr, Yancy CW. 2023 ACC Expert Consensus Decision Pathway on Management of Heart Failure With Preserved Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2023 May 9;81(18):1835-1878. doi: 10.1016/j.jacc.2023.03.393[↩][↩][↩]
- Faselis C, Arundel C, Patel S, Lam PH, Gottlieb SS, Zile MR, Deedwania P, Filippatos G, Sheriff HM, Zeng Q, Morgan CJ, Wopperer S, Nguyen T, Allman RM, Fonarow GC, Ahmed A. Loop Diuretic Prescription and 30-Day Outcomes in Older Patients With Heart Failure. J Am Coll Cardiol. 2020 Aug 11;76(6):669-679. doi: 10.1016/j.jacc.2020.06.022[↩]
- Cleland JGF, Bunting KV, Flather MD, et al. Beta-blockers in Heart Failure Collaborative Group. Beta-blockers for heart failure with reduced, mid-range, and preserved ejection fraction: an individual patient-level analysis of double-blind randomized trials. Eur Heart J. 2018 Jan 1;39(1):26-35. doi: 10.1093/eurheartj/ehx564[↩]
- Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, Clausell N, Desai AS, Diaz R, Fleg JL, Gordeev I, Harty B, Heitner JF, Kenwood CT, Lewis EF, O’Meara E, Probstfield JL, Shaburishvili T, Shah SJ, Solomon SD, Sweitzer NK, Yang S, McKinlay SM; TOPCAT Investigators. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014 Apr 10;370(15):1383-92. doi: 10.1056/NEJMoa1313731[↩]
- Pfeffer MA, Claggett B, Assmann SF, Boineau R, Anand IS, Clausell N, Desai AS, Diaz R, Fleg JL, Gordeev I, Heitner JF, Lewis EF, O’Meara E, Rouleau JL, Probstfield JL, Shaburishvili T, Shah SJ, Solomon SD, Sweitzer NK, McKinlay SM, Pitt B. Regional variation in patients and outcomes in the Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist (TOPCAT) trial. Circulation. 2015 Jan 6;131(1):34-42. doi: 10.1161/CIRCULATIONAHA.114.013255[↩]
- McMurray JJV, Jackson AM, Lam CSP, Redfield MM, et al. Effects of Sacubitril-Valsartan Versus Valsartan in Women Compared With Men With Heart Failure and Preserved Ejection Fraction: Insights From PARAGON-HF. Circulation. 2020 Feb 4;141(5):338-351. doi: 10.1161/CIRCULATIONAHA.119.044491[↩]
- Rist A, Sevre K, Wachtell K, Devereux RB, Aurigemma GP, Smiseth OA, Kjeldsen SE, Julius S, Pitt B, Burnier M, Kreutz R, Oparil S, Mancia G, Zannad F. The current best drug treatment for hypertensive heart failure with preserved ejection fraction. Eur J Intern Med. 2024 Feb;120:3-10. doi: 10.1016/j.ejim.2023.10.008[↩]
- Solomon SD, McMurray JJV, Claggett B, de Boer RA, et al. DELIVER Trial Committees and Investigators. Dapagliflozin in Heart Failure with Mildly Reduced or Preserved Ejection Fraction. N Engl J Med. 2022 Sep 22;387(12):1089-1098. doi: 10.1056/NEJMoa2206286[↩][↩]
- Anker SD, Butler J, Filippatos G, Ferreira JP, et al. EMPEROR-Preserved Trial Investigators. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N Engl J Med. 2021 Oct 14;385(16):1451-1461. doi: 10.1056/NEJMoa2107038[↩]
- Anker SD, Usman MS, Anker MS, Butler J, et al. Patient phenotype profiling in heart failure with preserved ejection fraction to guide therapeutic decision making. A scientific statement of the Heart Failure Association, the European Heart Rhythm Association of the European Society of Cardiology, and the European Society of Hypertension. Eur J Heart Fail. 2023 Jul;25(7):936-955. doi: 10.1002/ejhf.2894[↩]
- Böhm M, Butler J, Filippatos G, Ferreira JP, Pocock SJ, Abdin A, Mahfoud F, Brueckmann M, Gollop ND, Iwata T, Ponikowski P, Wanner C, Zannad F, Packer M, Anker SD; EMPEROR-Preserved Trial Committees and Investigators. Empagliflozin Improves Outcomes in Patients With Heart Failure and Preserved Ejection Fraction Irrespective of Age. J Am Coll Cardiol. 2022 Jul 5;80(1):1-18. doi: 10.1016/j.jacc.2022.04.040[↩]
- Joglar JA, Chung MK, Armbruster AL, et al. Peer Review Committee Members. 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2024 Jan 2;149(1):e1-e156. doi: 10.1161/CIR.0000000000001193 Erratum in: Circulation. 2024 Jun 11;149(24):e1413. doi: 10.1161/CIR.0000000000001263[↩]
- Alam A, Van Zyl J, Nayyar N, Hall S, Jermyn R. Improvement in Metabolic Co-Morbidities after Implantation of CardioMEMS in Patients with Heart Failure with Preserved Ejection Fraction Phenotype. J Clin Med. 2021 Sep 22;10(19):4308. doi: 10.3390/jcm10194308[↩][↩]
- Golla MSG, Brown KN, Gupta N. Percutaneous Transluminal Coronary Arteriography. [Updated 2023 Mar 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538158[↩]
- Datla S, Verberkt CA, Hoye A, Janssen DJA, Johnson MJ. Multi-disciplinary palliative care is effective in people with symptomatic heart failure: A systematic review and narrative synthesis. Palliat Med. 2019 Sep;33(8):1003-1016. doi: 10.1177/0269216319859148[↩][↩]
- Waagstein F, Caidahl K, Wallentin I, Bergh CH, Hjalmarson A. Long-term beta-blockade in dilated cardiomyopathy. Effects of short- and long-term metoprolol treatment followed by withdrawal and readministration of metoprolol. Circulation. 1989 Sep;80(3):551-63. doi: 10.1161/01.cir.80.3.551[↩]
- Felker GM, Lee KL, Bull DA, Redfield MM, Stevenson LW, Goldsmith SR, LeWinter MM, Deswal A, Rouleau JL, Ofili EO, Anstrom KJ, Hernandez AF, McNulty SE, Velazquez EJ, Kfoury AG, Chen HH, Givertz MM, Semigran MJ, Bart BA, Mascette AM, Braunwald E, O’Connor CM; NHLBI Heart Failure Clinical Research Network. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011 Mar 3;364(9):797-805. doi: 10.1056/NEJMoa1005419[↩]
- Brisco-Bacik MA, Ter Maaten JM, Houser SR, Vedage NA, Rao V, Ahmad T, Wilson FP, Testani JM. Outcomes Associated With a Strategy of Adjuvant Metolazone or High-Dose Loop Diuretics in Acute Decompensated Heart Failure: A Propensity Analysis. J Am Heart Assoc. 2018 Sep 18;7(18):e009149. doi: 10.1161/JAHA.118.009149[↩]
- Mullens W, Dauw J, Martens P, Verbrugge FH, Nijst P, Meekers E, Tartaglia K, Chenot F, Moubayed S, Dierckx R, Blouard P, Troisfontaines P, Derthoo D, Smolders W, Bruckers L, Droogne W, Ter Maaten JM, Damman K, Lassus J, Mebazaa A, Filippatos G, Ruschitzka F, Dupont M; ADVOR Study Group. Acetazolamide in Acute Decompensated Heart Failure with Volume Overload. N Engl J Med. 2022 Sep 29;387(13):1185-1195. doi: 10.1056/NEJMoa2203094[↩]
- Shah KS, Xu H, Matsouaka RA, Bhatt DL, Heidenreich PA, Hernandez AF, Devore AD, Yancy CW, Fonarow GC. Heart Failure With Preserved, Borderline, and Reduced Ejection Fraction: 5-Year Outcomes. J Am Coll Cardiol. 2017 Nov 14;70(20):2476-2486. doi: 10.1016/j.jacc.2017.08.074[↩]
- Tsao CW, Lyass A, Enserro D, Larson MG, Ho JE, Kizer JR, Gottdiener JS, Psaty BM, Vasan RS. Temporal Trends in the Incidence of and Mortality Associated With Heart Failure With Preserved and Reduced Ejection Fraction. JACC Heart Fail. 2018 Aug;6(8):678-685. doi: 10.1016/j.jchf.2018.03.006[↩][↩]
- Kitai T, Miyakoshi C, Morimoto T, Yaku H, Murai R, Kaji S, Furukawa Y, Inuzuka Y, Nagao K, Tamaki Y, Yamamoto E, Ozasa N, Tang WHW, Kato T, Kimura T. Mode of Death Among Japanese Adults With Heart Failure With Preserved, Midrange, and Reduced Ejection Fraction. JAMA Netw Open. 2020 May 1;3(5):e204296. doi: 10.1001/jamanetworkopen.2020.4296[↩]
- Jones RC, Francis GS, Lauer MS. Predictors of mortality in patients with heart failure and preserved systolic function in the Digitalis Investigation Group trial. J Am Coll Cardiol. 2004 Sep 1;44(5):1025-9. doi: 10.1016/j.jacc.2004.05.077[↩][↩]
- Vanderpool RR, Saul M, Nouraie M, Gladwin MT, Simon MA. Association Between Hemodynamic Markers of Pulmonary Hypertension and Outcomes in Heart Failure With Preserved Ejection Fraction. JAMA Cardiol. 2018 Apr 1;3(4):298-306. doi: 10.1001/jamacardio.2018.0128. Erratum in: JAMA Cardiol. 2018 Jul 1;3(7):665. doi: 10.1001/jamacardio.2018.1559[↩]
- Gorter TM, van Veldhuisen DJ, Bauersachs J, et al.Right heart dysfunction and failure in heart failure with preserved ejection fraction: mechanisms and management. Position statement on behalf of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018 Jan;20(1):16-37. doi: 10.1002/ejhf.1029[↩]
- Mohammed SF, Hussain I, AbouEzzeddine OF, Takahama H, Kwon SH, Forfia P, Roger VL, Redfield MM. Right ventricular function in heart failure with preserved ejection fraction: a community-based study. Circulation. 2014 Dec 23;130(25):2310-20. doi: 10.1161/CIRCULATIONAHA.113.008461. Epub 2014 Nov 12. Erratum in: Circulation. 2015 Apr 28;131(17):e424. doi: 10.1161/CIR.0000000000000202.. Abou Ezzeddine, Omar F [corrected to AbouEzzeddine, Omar F].[↩]
- American Heart Association. What is Heart Failure ? http://www.heart.org/HEARTORG/Conditions/HeartFailure/AboutHeartFailure/What-is-Heart-Failure_UCM_002044_Article.jsp[↩][↩][↩][↩][↩]
- American Heart Association. Classes of Heart Failure. http://www.heart.org/HEARTORG/Conditions/HeartFailure/AboutHeartFailure/Classes-of-Heart-Failure_UCM_306328_Article.jsp[↩][↩][↩]
- Dolgin M, Association NYH, Fox AC, Gorlin R, Levin RI, New York Heart Association. Criteria Committee. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9th ed. Boston, MA: Lippincott Williams and Wilkins; March 1, 1994.[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. What Causes Heart Failure ? https://www.nhlbi.nih.gov/health/health-topics/topics/hf/causes[↩]
- Mayo Foundation for Medical Education and Research. Heart Failure Symptoms. http://www.mayoclinic.org/diseases-conditions/heart-failure/basics/symptoms/con-20029801[↩]
- Gaddam KK, Yelamanchili P, Sedghi Y, Ventura HO. Advanced Heart Failure and Management Strategies. The Ochsner Journal. 2009;9(4):227-233. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3096284/[↩][↩][↩][↩]
- Registry of the International Society for Heart and Lung Transplantation: twenty-fifth official adult heart transplant report–2008. Taylor DO, Edwards LB, Aurora P, Christie JD, Dobbels F, Kirk R, Rahmel AO, Kucheryavaya AY, Hertz MI. J Heart Lung Transplant. 2008 Sep; 27(9):943-56. https://www.ncbi.nlm.nih.gov/pubmed/18765186/[↩]
- Selection of patients for heart transplantation in the current era of heart failure therapy. Butler J, Khadim G, Paul KM, Davis SF, Kronenberg MW, Chomsky DB, Pierson RN 3rd, Wilson JR. J Am Coll Cardiol. 2004 Mar 3; 43(5):787-93. https://www.ncbi.nlm.nih.gov/pubmed/14998618/[↩]
- Cell-based therapy for heart failure. Wollert KC, Drexler H. Curr Opin Cardiol. 2006 May; 21(3):234-9. https://www.ncbi.nlm.nih.gov/pubmed/16601463/[↩]
- Ammar KA, Jacobsen SJ, Mahoney DW, Kors JA, Redfield MM, Burnett JC Jr, Rodeheffer RJ. Prevalence and prognostic significance of heart failure stages: application of the American College of Cardiology/American Heart Association heart failure staging criteria in the community. Circulation. 2007 Mar 27;115(12):1563-70. doi: 10.1161/CIRCULATIONAHA.106.666818[↩]
- Heart disease and stroke statistics–2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, Hailpern SM, Ho M, Howard V, Kissela B, Kittner S, Lloyd-Jones D, McDermott M, Meigs J, Moy C, Nichol G, O’Donnell C, Roger V, Sorlie P, Steinberger J, Thom T, Wilson M, Hong Y, American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008 Jan 29; 117(4):e25-146. http://circ.ahajournals.org/content/117/4/e25.long[↩]
- ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). Hunt SA, American College of Cardiology., American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol. 2005 Sep 20; 46(6):e1-82. https://www.ncbi.nlm.nih.gov/pubmed/16168273/[↩]
- Is the prognosis of heart failure improving ? Cleland JG, Gemmell I, Khand A, Boddy A. Eur J Heart Fail. 1999 Aug; 1(3):229-41. https://www.ncbi.nlm.nih.gov/pubmed/10935669/[↩]