Contents
What is cardiac tamponade
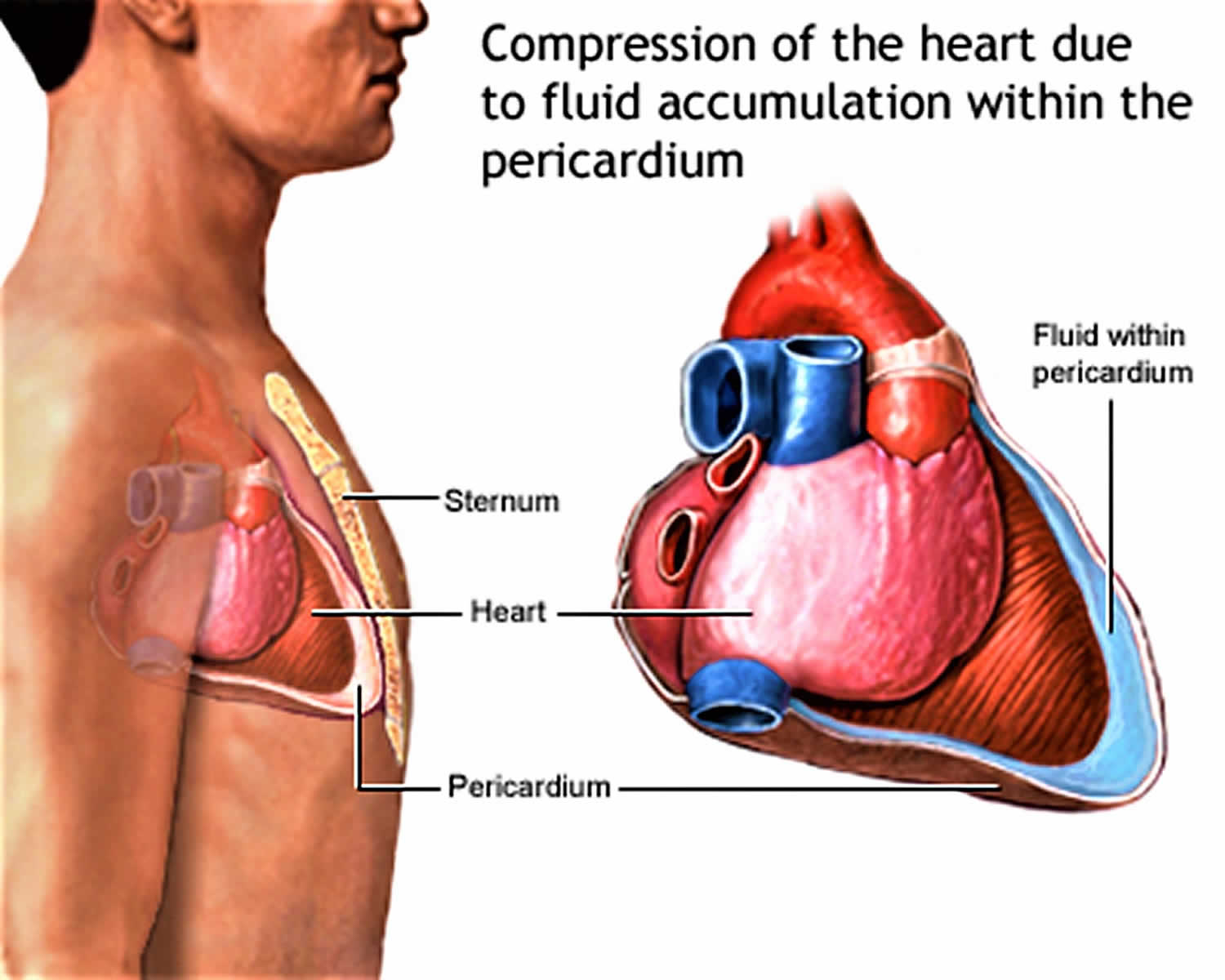
Cardiac tamponade is a emergency condition that needs to be treated in the hospital due to compression of the heart caused by the accumulation of pericardial fluid or pericardial effusion (transudate, exudate, or blood) in the space between the heart muscle and the outer covering sac of the heart 1). The accumulation of pericardial fluid or pericardial effusion prevents the heart ventricles from expanding fully. The excess pressure from the fluid prevents the heart from working properly. As a result, the body does not get enough blood. Slow accumulation such as in infection (tuberculosis [TB], myocarditis), autoimmune diseases, cancers, uremia, and other inflammatory diseases of the pericardium (pericarditis) is better tolerated than rapid accumulation as seen in hemorrhages, for example, a hemorrhage from a penetrating wound to the heart or ventricular wall rupture after a heart attack (myocardial infarction) or following a pacemaker insertion complication 2). Once cardiac tamponade is diagnosed, treatment is required. Without treatment, cardiac tamponade is universally fatal 3). Data show that cardiac tamponade following open heart surgery is often fatal 4). In all cases, the underlying cause must be treated. When the cause of the pericardial effusion is a cancer, it carries an 80% mortality within 12 months, whereas patients with a non-malignant cause have a mortality rate of less than 15% 5).
Cardiac tamponade is a medical emergency that happens when enough fluid accumulates in the pericardial sac compressing the heart and leading to a decrease in cardiac output and shock 6). Cardiac tamponade can rapidly lead to hypotension, shock, and death. The diagnosis of cardiac tamponade is a clinical diagnosis that requires prompt recognition and treatment to prevent cardiovascular collapse and cardiac arrest. Once the cardiac tamponade is diagnosed, the patient is best monitored in the ICU until the fluid is evacuated from the pericardial sac. Oxygen is usually required, and the patient is placed at bed rest with the feet elevated. The treatment of cardiac tamponade can be performed at the bedside or in the operating room 7). After treatment, the patient needs to be monitored to ensure that the fluid does not re-accumulate. If a drain is left in the pericardial sac, the nurse should monitor the drainage. A follow-up echocardiogram is usually done prior to discharge 8).
Diagnosis of pericardial effusion with tamponade can be difficult using clinical exam alone 9). A point-of-care echocardiogram can be very useful to confirm the diagnosis and determine the need for intervention. Remember, cardiac tamponade is ultimately a clinical diagnosis requiring both hemodynamically unstable patient and pericardial effusion.
Patients suspected of having cardiac tamponade due to medical causes should be monitored closely and acted on promptly as they can deteriorate quickly. These patients are by definition unstable and should be watched in the hospital following treatment. Further testing may better explain the cause of the pericardial effusion. Pericardiocentesis, while effective, is not without risk. Complications include damage the nearby vessels (including puncturing a coronary vessel, internal mammary vessels), inadvertent puncture to the right ventricle or laceration of the liver. These complications may be reduced by using point-of-care ultrasound for guidance during pericardiocentesis, but this has not been well studied.
Penetrating traumatic pericardial tamponade require prompt surgical intervention: pericardial window if the patient has vital signs, or emergency department thoracotomy if the patient has no pulse. Hemopericardium in blunt traumatic arrest is considered a non-survivable injury, and further resuscitation is not usually warranted 10).
Patients with cardiac tamponade present similar to patients with other forms of cardiogenic or obstructive shock 11). Patients with cardiac tamponade may have vague symptoms of chest pain, palpitations, shortness of breath, or in more severe cases, dizziness, syncope and altered mental status 12). Patients with cardiac tamponade may also present in a pulseless electrical activity cardiac arrest 13). The classic physical findings in cardiac tamponade are included in Beck’s cardiac tamponade triad of hypotension, jugular venous distension, and muffled heart sounds 14). Pulses paradoxus, which is a decrease in systolic blood pressure by more than 10 mm Hg with inspiration is an important physical exam finding that suggests a pericardial effusion is causing cardiac tamponade 15). When fluid compresses the heart and impairs filling, the interventricular septum bows toward the left ventricle during inspiration due to increased venous return to the right side of the heart. This further decreases the of the left ventricle leading to decreased left ventricular preload and stroke volume. The challenge with making the diagnosis of tamponade with clinical signs alone is difficult since they are neither sensitive nor specific 16).
Evaluation includes electrocardiogram (ECG), chest X-ray, complete blood count (to rule out infection), Basic metabolic panel (to rule out uremia), ESR, CRP (markers of inflammation), bedside echocardiogram to rule out large pericardial effusion, impending hemodynamic compromise or cardiac tamponade, computed tomography (CT) and cardiovascular magnetic resonance (CMR).
The fluid around the heart must be drained as quickly as possible. A procedure that uses a needle to remove fluid from the tissue that surrounds the heart, pericardiocentesis, will be done.
A surgical procedure to cut and remove part of the covering of the heart (pericardium) may also be done. This is known as surgical pericardiectomy or pericardial window.
Fluids are given to keep blood pressure normal until the fluid can be drained from around the heart. Medicines that increase blood pressure may also help keep the person alive until the fluid is drained.
Oxygen may be given to help reduce the workload on the heart by decreasing tissue demands for blood flow.
The cause of tamponade must be found and treated.
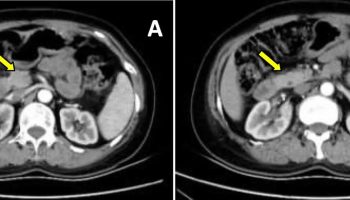
Figure 1. Cardiac tamponade
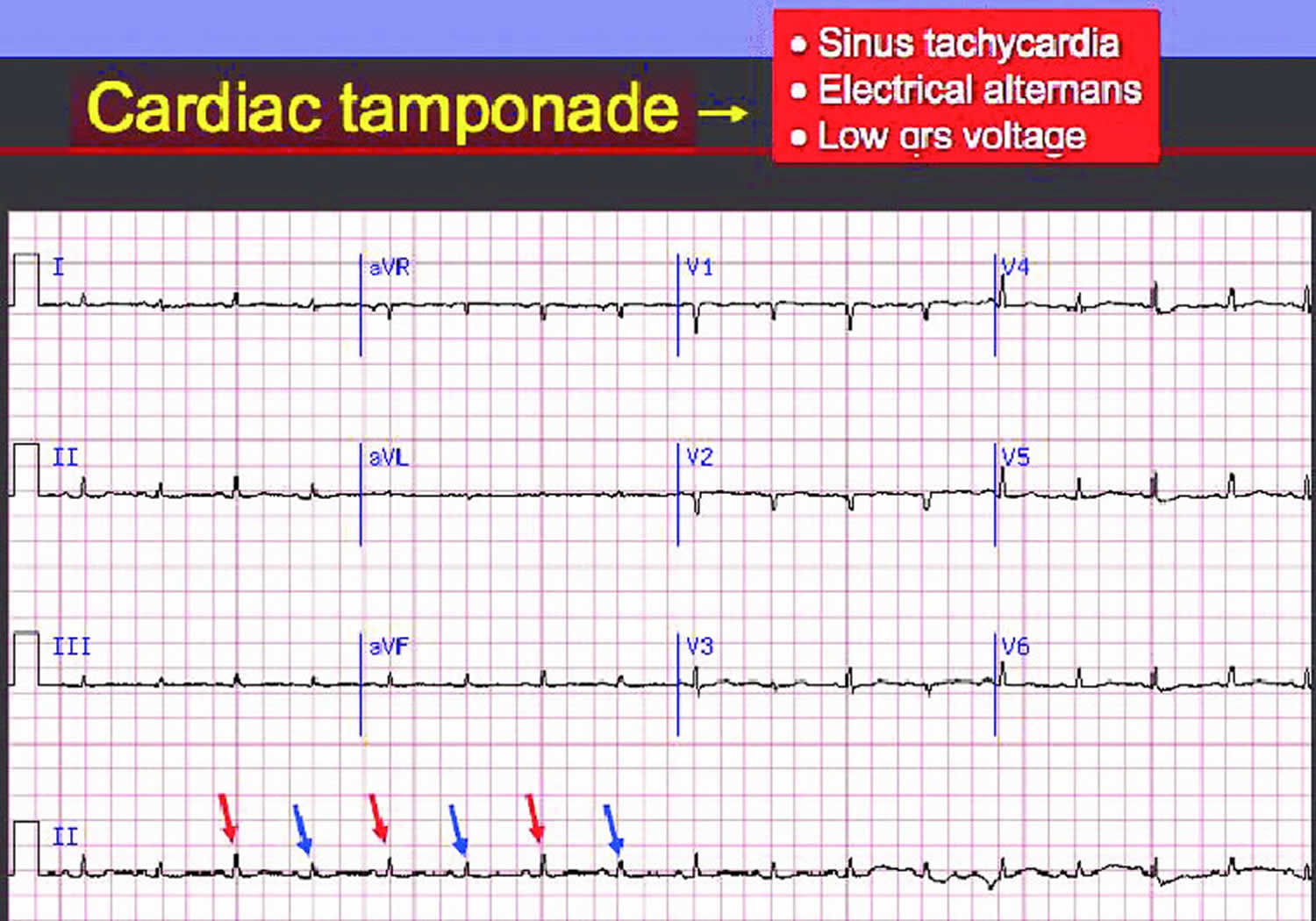
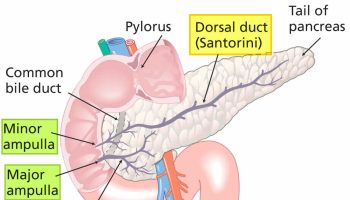
Figure 2. Cardiac tamponade ECG
Footnote: ECG showing sinus tachycardia with low QRS voltage and electrical alternans in a patient with cardiac tamponade.
Electrical alternans may be present. When the word alternans is used, the underlying pathophysiology that is most often thought of is alternans due to motion of the heart and its shifting position in relationship to the surface electrodes. The pathophysiologic mechanism underlying the alternation in the height or amplitude of the QRS complex is the swinging or shifting or the electrical axis of the heart. It should be noted that there can also be P wave and T wave alternans attributable to the motion of the heart.
While electrical alternans is frequently thought of in association with pericardial effusion, it should be noted that not all pericardial effusions cause electrical alternans, and that total electrical alternans (involving the p wave, QRS complex and the T wave) is present in just 5-10% of cases of cardiac tamponade.
[Source 17) ]Cardiac tamponade vs Pericardial effusion
Cardiac tamponade is pressure on the heart caused by the accumulation of pericardial fluid or pericardial effusion. Pericardial effusion (fluid around the heart) is an abnormal accumulation of fluid in the pericardial cavity. Because of the limited amount of space in the pericardial cavity, fluid accumulation will lead to an increased intrapericardial pressure and this can negatively affect heart function. When there is a pericardial effusion with enough pressure to adversely affect heart function, this is called cardiac tamponade. Pericardial effusion usually results from a disturbed equilibrium between the production and re-absorption of pericardial fluid, or from a structural abnormality that allows fluid to enter the pericardial cavity. Normal levels of pericardial fluid are from 15 to 50 mL.
Pericardial effusion can be classified broadly into three types, namely transudative, exudative and hemorrhagic. A fluid secreting malignancy could also be the cause of a pericardial effusion.
Pericardial effusion usually results from a disturbed equilibrium between the production and reabsorption of pericardial fluid. This can occur in infections and inflammations where there is increased production of pericardial fluid or in malignancy and hypothyroidism where there is inadequate drainage of the fluid.
Most pericardial effusions are caused by inflammation of the pericardium, a condition called pericarditis. As the pericardium becomes inflamed, extra fluid is produced, leading to a pericardial effusion. Viral infections are one of the main causes of pericarditis and pericardial effusions. Infections causing pericardial effusions include cytomegalovirus, coxsackie virus, echovirus, and HIV. However, other conditions like injury to the pericardium or heart from a medical procedure, myocardial infarction, uremia, autoimmune disease and cancer should be considered in differential diagnosis of pericardial effusion.
What causes cardiac tamponade
Cardiac tamponade is caused by the buildup of pericardial fluid or pericardial effusion (exudate, transudate, or blood) that can accumulate for several reasons. Hemorrhage, such as from a penetrating wound to the heart or ventricular wall rupture after an heart attack (myocardial infarction), can lead to a rapid increase in pericardial volume. Other risk factors, which tend to produce a slower growing effusion, include infection (tuberculosis [TB], myocarditis), autoimmune diseases, neoplasms, uremia, and other inflammatory diseases (pericarditis). The pericardial fluid that builds up slowly is better tolerated in patients than rapid accumulations. Hence, traumatic causes (hemopericardium) require small volumes to causes hemodynamic instability versus pericardial effusions from medical causes such as malignancy where large volumes of fluid may accumulate in pericardial sac before patients become symptomatic 18).
Normally, a small, physiologic amount of fluid surrounds the heart within the pericardium. When the volume of fluid builds up fast enough, the chambers of the heart are compressed, and tamponade physiology develops rapidly with much smaller volumes. The classical example is the traumatic cardiac injury resulting in hemp-pericardium. Under this pressure, the chambers of the heart are unable to relax leading to decreased venous return, filling and cardiac output.
Slow growing effusions, such as those due to autoimmune disease or cancers, allow for stretching of the pericardium, and effusions can become quite large before leading to tamponade physiology 19).
Cardiac tamponade can occur due to:
- Dissecting aortic aneurysm (thoracic)
- End-stage lung cancer
- Heart attack (acute MI)
- Heart surgery
- Pericarditis caused by bacterial or viral infections
- Wounds to the heart
Other possible causes include:
- Heart tumors
- Underactive thyroid gland
- Kidney failure
- Leukemia
- Placement of central lines
- Radiation therapy to the chest
- Recent invasive heart procedures
- Systemic lupus erythematosus (SLE)
- Dermatomyositis
- Heart failure
Cardiac tamponade due to disease occurs in about 2 out of 10,000 people. However, there are sub-groups of patients with a higher incidence of pericardial effusions. These include HIV-positive patients, patients with end-stage renal disease, those with known or occult malignancies, a history of congestive heart failure, tuberculosis, autoimmune diseases like lupus, or penetrating traumatic injury to central chest “cardiac box” 20).
Cardiac tamponade signs and symptoms
Symptoms of cardiac tamponade
Patients with pericarditis commonly present with sudden onset, severe chest pain, pleuritic in nature, improves when leaning forward and worsens on lying down. On the other hand, cardiac tamponade patients present with forms of cardiogenic or obstructive shock. They may have vague symptoms of chest pain, palpitations, shortness of breath, or in more severe cases, dizziness, syncope, and altered mental status 21). They may also present in a pulseless electrical activity, cardiac arrest.
Cardiac tamponade symptoms may include:
- Anxiety, restlessness
- Sharp chest pain that is felt in the neck, shoulder, back, or abdomen
- Chest pain that gets worse with deep breathing or coughing
- Problems breathing
- Discomfort, sometimes relieved by sitting upright or leaning forward
- Fainting, lightheadedness
- Pale, gray, or blue skin
- Palpitations
- Rapid breathing
- Swelling of the legs or abdomen
- Jaundice
Other cardiac tamponade symptoms that may occur with this disorder:
- Dizziness
- Drowsiness
- Weak or absent pulse
Signs of cardiac tamponade
The classic physical findings in cardiac tamponade are included in Beck’s triad of hypotension, jugular venous distension, and muffled heart sounds. Pulses paradoxus, which is a decrease in systolic blood pressure by more than 10 mm Hg with inspiration is an important physical exam finding that suggests a pericardial effusion is causing cardiac tamponade. When fluid compresses the heart and impairs filling, the interventricular septum bows toward the left ventricle during inspiration due to increased venous return to the right side of the heart. This further decreases the left ventricle space leading to decreased left ventricular preload and stroke volume. The challenge with making the diagnosis of tamponade with clinical signs alone is difficult since they are neither sensitive nor specific 22).
Cardiac tamponade prognosis
Death due to cardiac tamponade can occur quickly if the fluid or blood is not removed promptly from the pericardium.
The outcome is often good if the condition is treated promptly. However, tamponade may come back.
Cardiac tamponade possible complications
Complications of cardiac tamponade may include:
- Heart failure
- Pulmonary edema
- Bleeding
- Shock
- Death
Cardiac tamponade diagnosis
The diagnosis of cardiac tamponade can be suspected on history and physical exam findings. ECG may be helpful, especially if it shows low voltages or electrical alternans, which is the classic ECG finding in cardiac tamponade due to the swinging of the heart within the pericardium that is filled with fluid. This is a rare ECG finding, and most commonly the ECG finding of cardiac tamponade is sinus tachycardia. A chest x-ray may show an enlarged heart and may strongly suggest pericardial effusion if a prior chest radiograph with a normal cardiac silhouette is available for comparison. CT chest can also pick up pericardial effusion 23).
A physical exam may show:
- Blood pressure that falls when breathing deeply
- Rapid breathing
- Heart rate over 100 (normal is 60 to 100 beats per minute)
- Heart sounds are only faintly heard through a stethoscope
- Neck veins that may be bulging (distended) but the blood pressure is low
- Weak or absent peripheral pulses
Echocardiogram is the best imaging modality to use at the bedside, whether it is a point-of-care echo or a cardiology echo study. Echocardiography can not only confirm there is a pericardial effusion, but determine its size, and whether it is causing compromise of cardiac function (right ventricular diastolic collapse, right atrial systolic collapse, plethoric IVC – a decrease in the proximal venal caval diameter by <50% during deep inspiration).
Other tests may include:
- Chest CT or MRI of chest
- Chest x-ray
- Coronary angiography
- ECG
- Right heart catheterization
Cardiac tamponade treatment
The treatment of cardiac tamponade is the removal of pericardial fluid (pericardiocentesis) to help relieve the pressure surrounding the heart 24). This can be done by performing a needle pericardiocentesis at the bedside, performed either using traditional landmark technique in a sub-xiphoid window or using a point-of-care echocardiogram to guide needle placement in real-time. Often the removal of the first small amounts of fluid can make a large improvement in hemodynamics, but leaving a catheter within the pericardium can allow for further drainage 25). However, hemodynamically unstable patients warrant the use of pericardiocentesis without imaging. Rule out type A aortic dissection with the help of echocardiogram or CT angiography prior to pericardiocentesis. Surgical drainage is required if the heart cannot be reached by a needle, clotted hemopericardium, intrapericardial bleeding, or thoracic conditions that make needle drainage difficult or ineffective 26).
Surgical options include creating a pericardial window or removing the pericardium. Emergency department resuscitative thoracotomy and the opening of the pericardial sac is therapy that can be used in traumatic arrests with suspected or confirmed cardiac tamponade. These options are preferable to needle pericardiocentesis for traumatic pericardial effusions.
Volume resuscitation and pressor support may be helpful; however, these are temporizing measures that should be performed while preparing for definitive treatment with one of the above procedures.
References [ + ]