Contents
- Congenital heart disease
- Types of congenital heart disease
- Holes in the Heart (Septal Defects)
- Atrial Septal Defect
- Ventricular Septal Defect
- Atrioventricular Septal Defect
- Patent Ductus Arteriosus
- Coarctation of the Aorta
- Dextro-Transposition of the Great Arteries
- Hypoplastic Left Heart Syndrome
- Narrowed Valves
- Pulmonary Atresia
- Tetralogy of Fallot
- Total Anomalous Pulmonary Venous Return
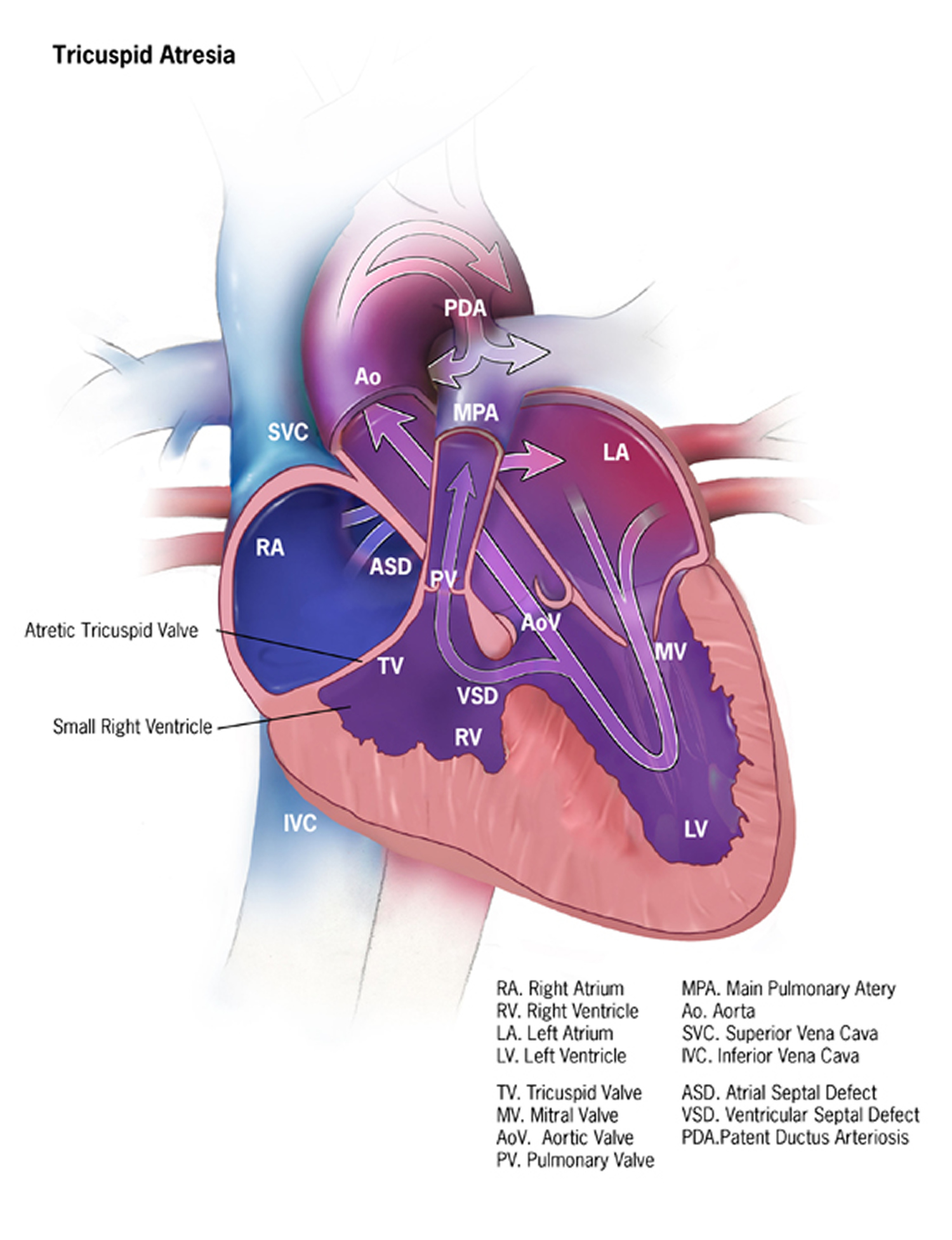
- Tricuspid Atresia
- Truncus Arteriosus
- Cyanotic congenital heart disease
- Double outlet right ventricle
- Ebstein anomaly
- Single ventricle spectrum
- Symptoms of cyanotic congenital heart disease
- Exams and Tests for cyanotic congenital heart disease
- Treatment for cyanotic congenital heart disease
- Outlook (Prognosis) for cyanotic congenital heart disease
- Possible Complications for cyanotic heart disease
- Prevention of cyanotic congenital heart disease
Congenital heart disease
Congenital heart defects are conditions that are present at birth and can affect the structure of a baby’s heart and the way it works 1. They are the most common type of birth defect 2. They affect 8 out of every 1,000 newborns. Each year, more than 35,000 babies in the United States are born with congenital heart defects 1.
The diagnosis and treatment of complex heart defects has greatly improved over the past few decades. As a result, almost all children who have complex heart defects survive to adulthood and can live active, productive lives.
Most people who have complex heart defects continue to need special heart care throughout their lives. They may need to pay special attention to how their condition affects issues such as health insurance, employment, birth control and pregnancy, and other health issues.
In the United States, more than 1 million adults are living with congenital heart defects 1.
These congenital heart defects can involve 1:
- The interior walls of the heart
- The valves inside the heart
- The arteries and veins that carry blood to the heart or the body
They can affect how blood flows through the heart and out to the rest of the body. Congenital heart defects can vary from mild with no symptoms (such as a small hole in the heart) to complex defects with severe life-threatening symptoms (such as missing or poorly formed parts of the heart). Many of these defects are simple conditions. They need no treatment or are easily fixed.
About 1 in 4 babies born with a heart defect has a critical congenital heart defect also known as critical congenital heart disease 3. Babies with a critical congenital heart defect need surgery or other procedures in the first year of life 3.
How the Heart Works
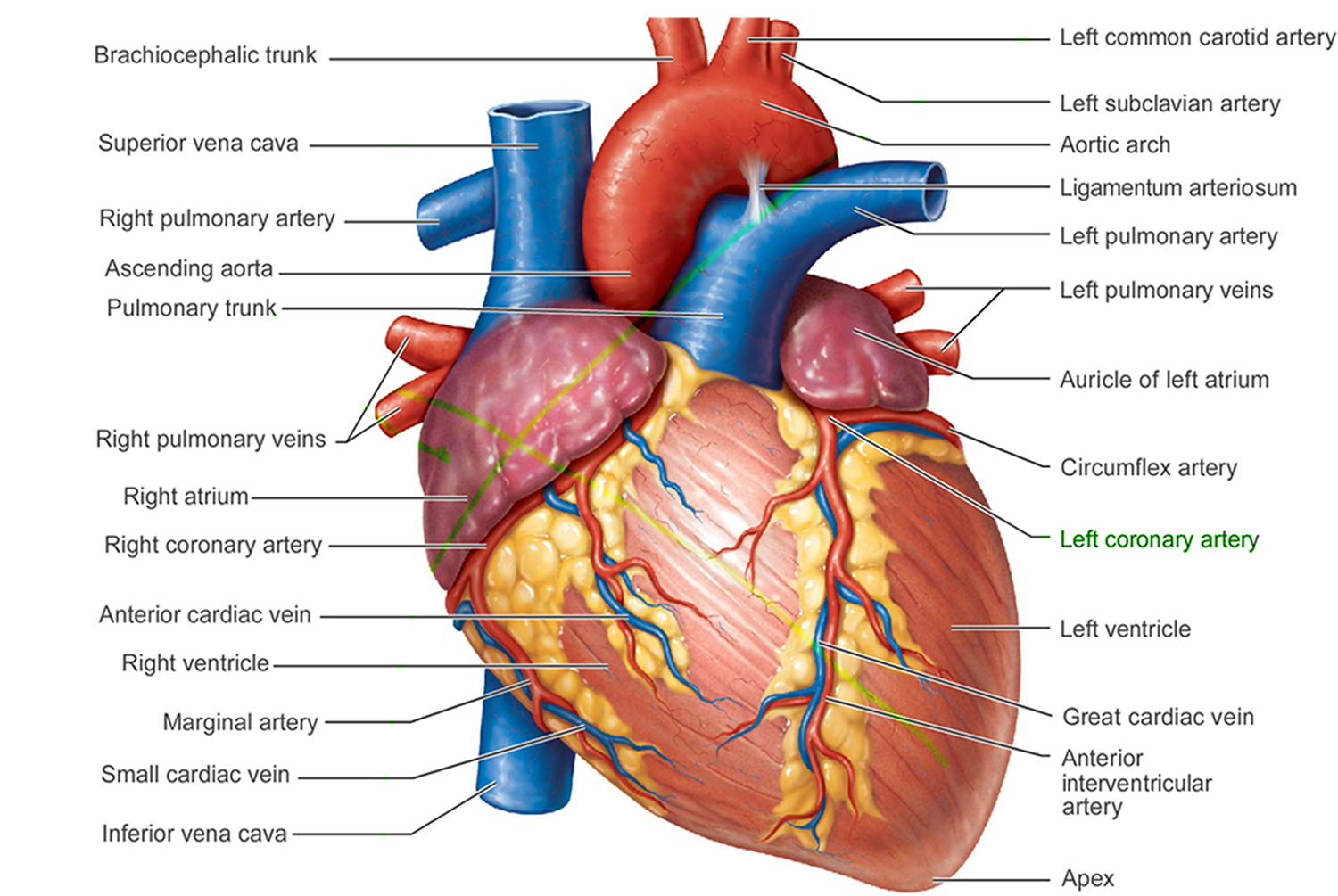
Figure 1. The anatomy of the heart
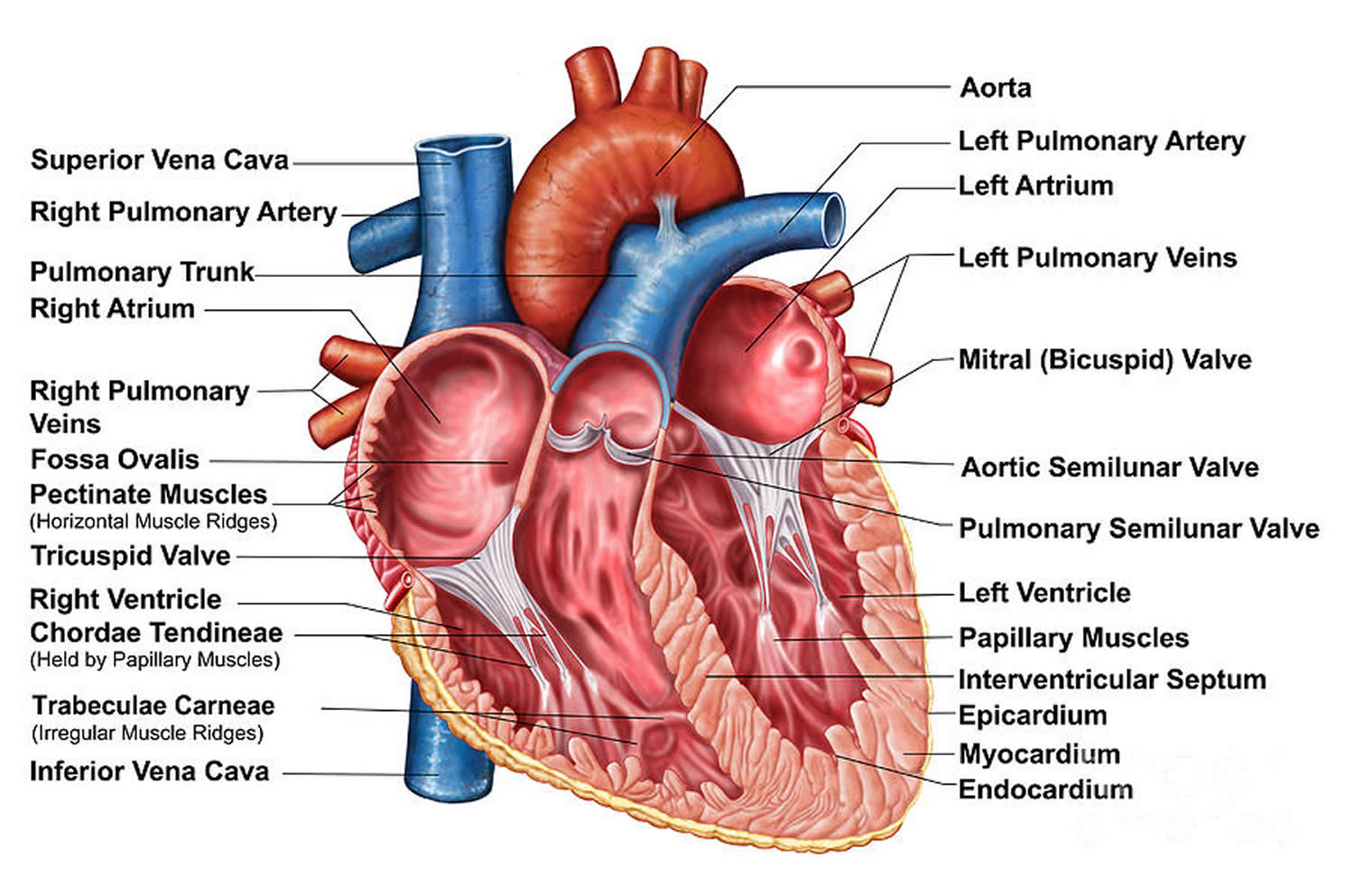
Figure 2. The anatomy of the heart chambers
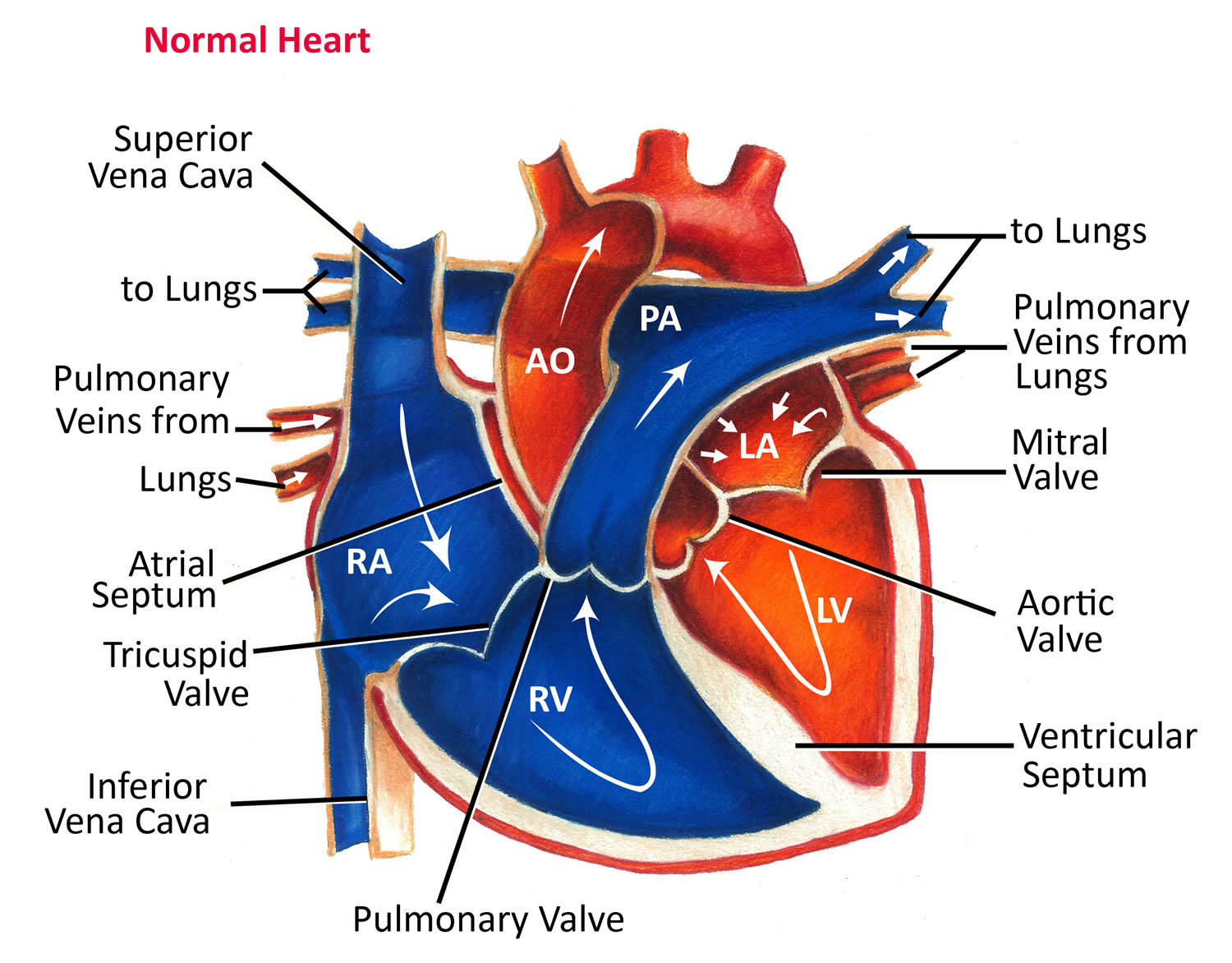
Figure 3. Normal heart blood flow
To understand congenital heart defects, it’s helpful to know how a healthy heart works. Your child’s heart is a muscle about the size of his or her fist 2. The heart works like a pump and beats 100,000 times a day 2.
The heart has two sides, separated by an inner wall called the septum. The right side of the heart pumps blood to the lungs to pick up oxygen. The left side of the heart receives the oxygen-rich blood from the lungs and pumps it to the body.
The heart has four chambers 4, two on the right and two on the left:
- Two upper chambers are called atrium (two is called an atria). The atria collect blood as it flows into the heart.
- Two lower chambers are called ventricles. The ventricles pump blood out of the heart to the lungs or other parts of the body.
The heart also has four valves that open and close to let blood flow from the atria to the ventricles and from the ventricles into the two large arteries connected to the heart in only one direction when the heart contracts (beats). The four heart valves are:
- Tricuspid valve, located between the right atrium and right ventricle
- Pulmonary or pulmonic valve, between the right ventricle and the pulmonary artery. This artery carries blood from the heart to the lungs.
- Mitral valve, between the left atrium and left ventricle
- Aortic valve, between the left ventricle and the aorta. This aorta carries blood from the heart to the body.
Each valve has a set of flaps (also called leaflets or cusps). The mitral valve has two flaps; the others have three. Valves are like doors that open and close. They open to allow blood to flow through to the next chamber or to one of the arteries. Then they shut to keep blood from flowing backward. Blood flow occurs only when there’s a difference in pressure across the valves, which causes them to open. Under normal conditions, the valves permit blood to flow in only one direction.
The heart four chambers and four valves and is connected to various blood vessels. Veins are blood vessels that carry blood from the body to the heart. Arteries are blood vessels that carry blood away from the heart to the body.
The heart pumps blood to the lungs and to all the body’s tissues by a sequence of highly organized contractions of the four chambers. For the heart to function properly, the four chambers must beat in an organized way.
When the heart’s valves open and close, they make a “lub-DUB” sound that a doctor can hear using a stethoscope 2.
- The first sound—the “lub”—is made by the mitral and tricuspid valves closing at the beginning of systole. Systole is when the ventricles contract, or squeeze, and pump blood out of the heart.
- The second sound—the “DUB”—is made by the aortic and pulmonary valves closing at the beginning of diastole. Diastole is when the ventricles relax and fill with blood pumped into them by the atria.
Arteries
The arteries are major blood vessels connected to your heart.
- The pulmonary artery carries blood from the right side of the heart to the lungs to pick up a fresh supply of oxygen.
- The aorta is the main artery that carries oxygen-rich blood from the left side of the heart to the body.
- The coronary arteries are the other important arteries attached to the heart. They carry oxygen-rich blood from the aorta to the heart muscle, which must have its own blood supply to function.
Veins
The veins also are major blood vessels connected to your heart.
- The pulmonary veins carry oxygen-rich blood from the lungs to the left side of the heart so it can be pumped to the body.
- The superior and inferior vena cavae are large veins that carry oxygen-poor blood from the body back to the heart.
Blood Flow
- The Right Side of Your Heart
In figure 3 above, the superior and inferior vena cavae are shown in blue to the left of the heart muscle as you look at the picture. These veins are the largest veins in your body.
After your body’s organs and tissues have used the oxygen in your blood, the vena cavae carry the oxygen-poor blood back to the right atrium of your heart.
The superior vena cava carries oxygen-poor blood from the upper parts of your body, including your head, chest, arms, and neck. The inferior vena cava carries oxygen-poor blood from the lower parts of your body.
The oxygen-poor blood from the vena cavae flows into your heart’s right atrium. From the right atrium, blood is pumped into the right ventricle. And then from the right ventricle, blood is pumped to your lungs through the pulmonary arteries (shown in blue in the center of figure 3).
Once in the lungs, the blood travels through many small, thin blood vessels called capillaries. There, the blood picks up more oxygen and transfers carbon dioxide to the lungs—a process called gas exchange.
The oxygen-rich blood passes from your lungs back to your heart through the pulmonary veins (shown in red to the left of the right atrium in figure 3).
- The Left Side of Your Heart
Oxygen-rich blood from your lungs passes through the pulmonary veins (shown in red to the right of the left atrium in figure 3 above). The blood enters the left atrium and is pumped into the left ventricle.
From the left ventricle, the oxygen-rich blood is pumped to the rest of your body through the aorta. The aorta is the main artery that carries oxygen-rich blood to your body.
Like all of your organs, your heart needs oxygen-rich blood. As blood is pumped out of your heart’s left ventricle, some of it flows into the coronary arteries (shown in red in figure 3).
Your coronary arteries are located on your heart’s surface at the beginning of the aorta. They carry oxygen-rich blood to all parts of your heart.
For the heart to work well, your blood must flow in only one direction. Your heart’s valves make this possible. Both of your heart’s ventricles have an “in” (inlet) valve from the atria and an “out” (outlet) valve leading to your arteries.
Healthy valves open and close in exact coordination with the pumping action of your heart’s atria and ventricles. Each valve has a set of flaps called leaflets or cusps that seal or open the valve. This allows blood to pass through the chambers and into your arteries without backing up or flowing backward.
Causes of congenital heart disease
The causes of congenital heart defects among most babies are unknown. Some babies have heart defects because of changes in their individual genes or chromosomes. Congenital heart defects also are thought to be caused by a combination of genes and other factors, such as things in the environment, the mother’s diet, the mother’s health conditions, or the mother’s medication use during pregnancy. For example, certain conditions a mother has, like pre-existing diabetes or obesity, have been linked to heart defects in the baby 5, 6. Smoking during pregnancy as well as taking certain medications have also been linked to heart defects 5, 6.
Congenital heart disease symptoms and signs
Signs and symptoms for congenital heart defects depend on the type and severity of the particular defect. Some defects might have few or no signs or symptoms. Others might cause a baby to have the following symptoms:
- Blue-tinted nails or lips
- Fast or troubled breathing
- Tiredness when feeding
- Sleepiness
Diagnosis of congenital heart disease
Some congenital heart defects may be diagnosed during pregnancy using a special type of ultrasound called a fetal echocardiogram, which creates ultrasound pictures of the heart of the developing baby. However, some congenital heart defects are not detected until after birth or later in life, during childhood or adulthood. If a healthcare provider suspects a congenital heart defect may be present, the baby can get several tests (such as an echocardiogram) to confirm the diagnosis.
Treatment of congenital heart disease
Treatment for congenital heart defects depends on the type and severity of the defect present. Some affected infants and children might need one or more surgeries to repair the heart or blood vessels. Some can be treated without surgery using a procedure called cardiac catheterization. A long tube, called a catheter, is threaded through the blood vessels into the heart, where a doctor can take measurements and pictures, do tests, or repair the problem. Sometimes the heart defect can’t be fully repaired, but these procedures can improve blood flow and the way the heart works.
Living with a congenital heart disease
As medical care and treatment have advanced, infants with congenital heart defects are living longer and healthier lives. Many children with congenital heart defects are now living into adulthood. It is estimated that more than two million individuals in the United States are living with a congenital heart defect. Many people with a congenital heart defect lead independent lives with little or no difficulty. Others might develop disability over time. Some people with a CHD have genetic problems or other health conditions that increase their risk for disability.
Even with improved treatments, many people with a congenital heart defect are not cured, even if their heart defect has been repaired. People with a congenital heart defect can develop other health problems over time, depending on their specific heart defect, the number of heart defects they have, and the severity of their heart defect. For example, some other health problems that might develop include irregular heart beat (arrhythmias), increased risk of infection in the heart muscle (infective endocarditis), or weakness in the heart (cardiomyopathy). People with a congenital heart defect need routine checkups with a cardiologist (heart doctor) to stay as healthy as possible. They also might need further operations after initial childhood surgeries. It is important for people with a congenital heart defect to visit their doctor on a regular basis and discuss their health, including their specific heart condition, with their doctor.
Types of congenital heart disease
With congenital heart defects, some part of the heart doesn’t form properly before birth. This changes the normal flow of blood through the heart.
There are many types of congenital heart defects. Some are simple, such as a hole in the septum. The hole allows blood from the left and right sides of the heart to mix. Another example of a simple defect is a narrowed valve that blocks blood flow to the lungs or other parts of the body.
Other heart defects are more complex. They include combinations of simple defects, problems with the location of blood vessels leading to and from the heart, and more serious problems with how the heart develops.
Listed below are examples of different types of congenital heart diseases. The types marked with a star (*) are considered critical congenital heart defects 2.
- Atrial Septal Defect
- Atrioventricular Septal Defect
- Patent Ductus Arteriosus
- Coarctation of the Aorta*
- Double-outlet right ventricle*
- d-Transposition of the great arteries*
- Ebstein anomaly*
- Hypoplastic Left Heart Syndrome*
- Interrupted aortic arch*
- Pulmonary atresia*
- Single ventricle*
- Tetralogy of Fallot*
- Total Anomalous Pulmonary Venous Return*
- Tricuspid atresia*
- Truncus Arteriosus*
- Ventricular Septal Defect
Examples of Simple Congenital Heart Defects
Holes in the Heart (Septal Defects)
The septum is the wall that separates the chambers on left and right sides of the heart. The wall prevents blood from mixing between the two sides of the heart. Some babies are born with holes in the septum. These holes allow blood to mix between the two sides of the heart.
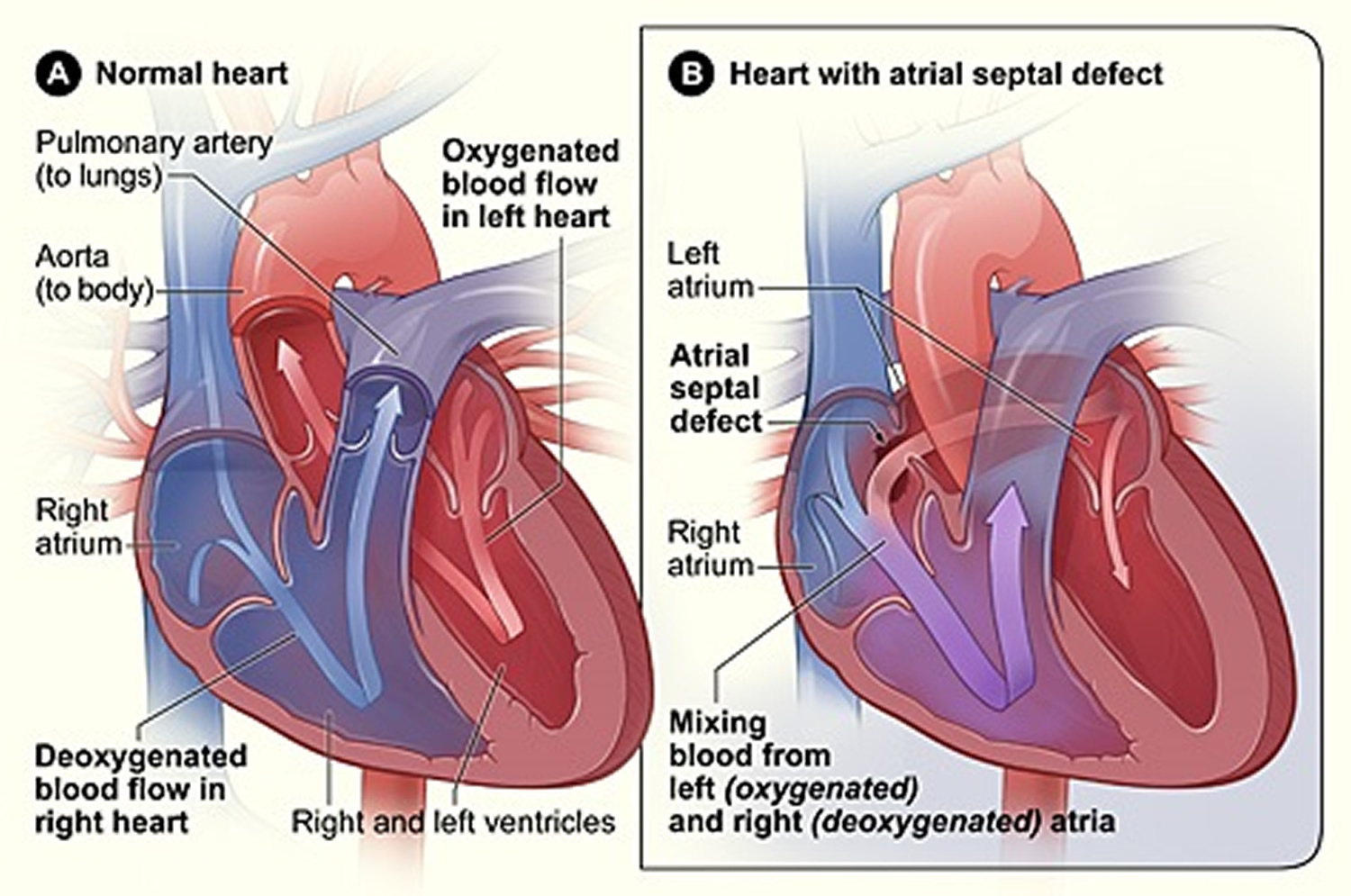
Atrial Septal Defect
Atrial septal defect is a birth defect of the heart in which there is a hole in the wall (septum) that separates the atria – the upper chambers of the heart (atria) 7. The hole allows oxygen-rich blood from the left atrium to flow into the right atrium, instead of flowing into the left ventricle as it should. Many children who have atrial septal defects have few, if any, symptoms 8.
As a baby develops during pregnancy, there are normally several openings in the wall dividing the upper chambers of the heart (atria) 7. These usually close during pregnancy or shortly after birth 7.
If one of these openings does not close, a hole is left, and it is called an atrial septal defect 7. The hole increases the amount of blood that flows through the lungs and over time, it may cause damage to the blood vessels in the lungs 7. Damage to the blood vessels in the lungs may cause problems in adulthood, such as high blood pressure in the lungs and heart failure. Other problems may include abnormal heartbeat, and increased risk of stroke 7.
A hole can vary in size and may close on its own or may require surgery 7.
Atrial Septal Defects can be small, medium, or large 8.
Small Atrial Septal Defects allow only a little blood to leak from one atrium to the other. They don’t affect how the heart works and don’t need any special treatment. Many small Atrial Septal Defects close on their own as the heart grows during childhood 8.
Medium and large Atrial Septal Defects allow more blood to leak from one atrium to the other. They’re less likely to close on their own 8.
About half of all Atrial Septal Defects close on their own over time. Medium and large Atrial Septal Defects that need treatment can be repaired using a catheter procedure or open-heart surgery 8.
Figure 4. Cross-Section of a Normal Heart and a Heart With an Atrial Septal Defect
[Source 8]Occurrence of Atrial Septal Defects
The Centers for Disease Control and Prevention recently estimated that each year about 1,966 babies in the United States are born with an atrial septal defect 9. It can also occur with other heart defects.
Causes and Risk Factors for Atrial Septal Defects
The causes of heart defects such as atrial septal defect among most babies are unknown 7. Some babies have heart defects because of changes in their genes or chromosomes. These types of heart defects also are thought to be caused by a combination of genes and other risk factors, such as things the mother comes in contact with in the environment or what the mother eats or drinks or the medicines the mother uses.
Diagnosis of Atrial Septal Defects
An atrial septal defect may be diagnosed during pregnancy or after the baby is born 7. In many cases, it may not be diagnosed until adulthood 7.
During Pregnancy with a Baby with Atrial Septal Defect
During pregnancy, there are screening tests (prenatal tests) to check for birth defects and other conditions. An atrial septal defect might be seen during an ultrasound (which creates pictures of the body), but it depends on the size of the hole and its location 7. If an atrial septal defect is suspected, a specialist will need to confirm the diagnosis.
After the Baby is Born with Atrial Septal Defect
An atrial septal defect is present at birth, but many babies do not have any signs or symptoms. Signs and symptoms of a large or untreated atrial septal defect may include the following:
- Frequent respiratory or lung infections
- Difficulty breathing
- Tiring when feeding (infants)
- Shortness of breath when being active or exercising
- Skipped heartbeats or a sense of feeling the heartbeat
- A heart murmur, or a whooshing sound that can be heard with a stethoscope
- Swelling of legs, feet, or stomach area
- Stroke
It is possible that an atrial septal defect might not be diagnosed until adulthood 7. One of the most common ways an atrial septal defect is found is by detecting a murmur when listening to a person’s heart with a stethoscope. If a murmur is heard or other signs or symptoms are present, the health care provider might request one or more tests to confirm the diagnosis. The most common test is an echocardiogram which is an ultrasound of the heart.
Treatments for Atrial Septal Defects
Treatment for an atrial septal defect depends on the age of diagnosis, the number of or seriousness of symptoms, size of the hole, and presence of other conditions. Sometimes surgery is needed to repair the hole. Sometimes medications are prescribed to help treat symptoms. There are no known medications that can repair the hole.
If a child is diagnosed with an atrial septal defect, the health care provider may want to monitor it for a while to see if the hole closes on its own. During this period of time, the health care provider might treat symptoms with medicine. A health care provider may recommend surgery for a child with a large atrial septal defect, even if there are few symptoms, to prevent problems later in life. Surgery may also be recommended for an adult who has many or severe symptoms. Surgery involves fixing the hole and may be done through cardiac catheterization or open-heart surgery. After surgery, follow-up care will depend on the size of the defect, person’s age, and whether the person has other birth defects.
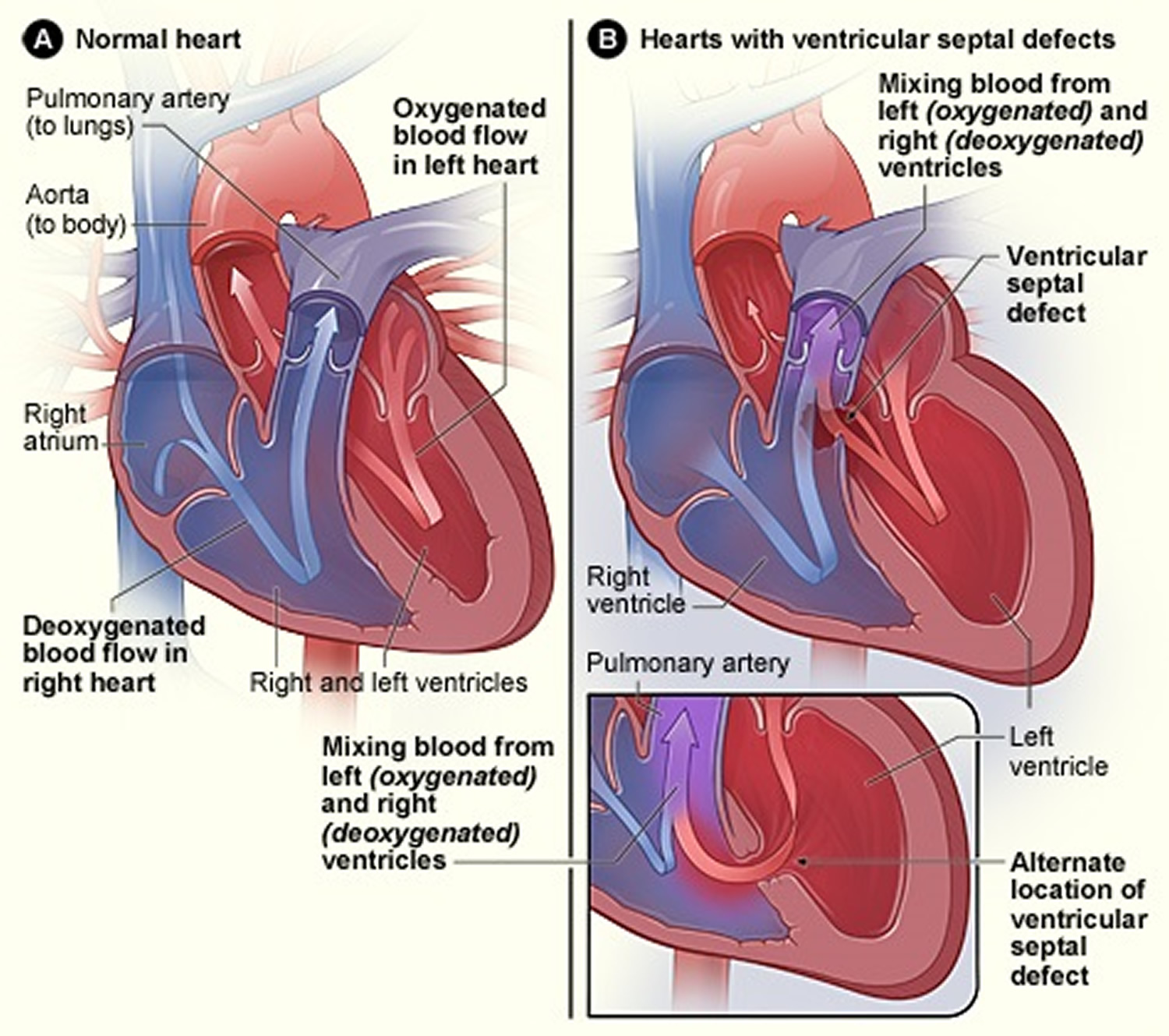
Ventricular Septal Defect
A ventricular septal defect (VSD) is a birth defect of the heart in which there is a hole in the wall (septum) that separates the two lower chambers (ventricles) of the heart 10. This wall also is called the ventricular septum. The hole allows oxygen-rich blood to flow from the left ventricle into the right ventricle, instead of flowing into the aorta and out to the body as it should.
A ventricular septal defect happens during pregnancy if the wall that forms between the two ventricles does not fully develop, leaving a hole.
Ventricular septal defects can be small, medium, or large. Small ventricular septal defects don’t cause problems and may close on their own. Medium ventricular septal defects are less likely to close on their own and may require treatment 8.
Large ventricular septal defects allow a lot of blood to flow from the left ventricle to the right ventricle. As a result, the left side of the heart must work harder than normal. Extra blood flow increases blood pressure in the right side of the heart and the lungs.
The heart’s extra workload can cause heart failure and poor growth. If the hole isn’t closed, high blood pressure can scar the arteries in the lungs 8. Over time, if not repaired, this defect can increase the risk for other complications, including heart failure, high blood pressure in the lungs (called pulmonary hypertension), irregular heart rhythms (called arrhythmia), or stroke 10.
Doctors use open-heart surgery to repair ventricular septal defects.
Figure 5. Cross-Section of a Normal Heart and a Heart With a Ventricular Septal Defect
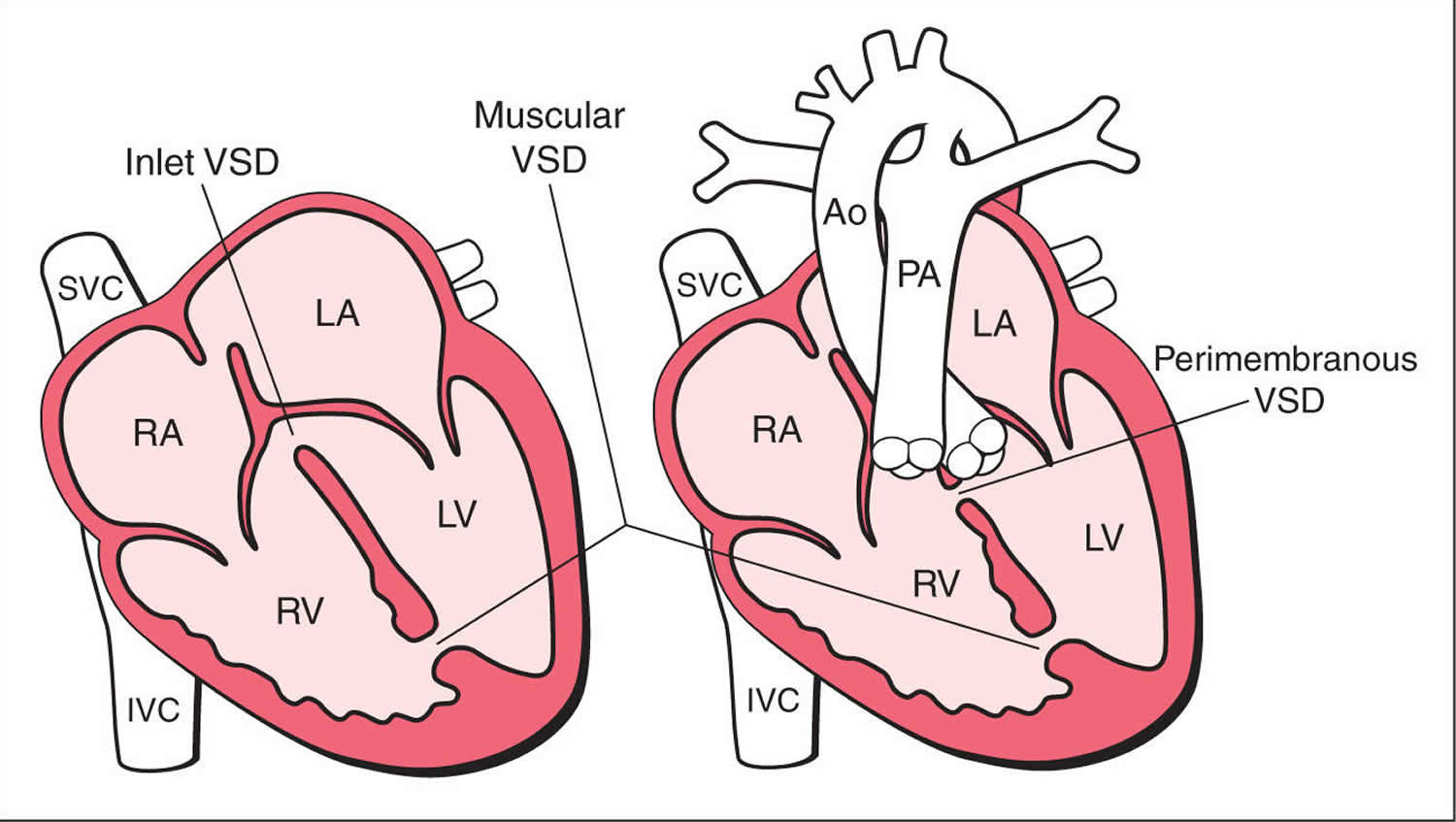
Types of Ventricular Septal Defects
An infant with a ventricular septal defect can have one or more holes in different places of the septum. There are several names for these holes. Some common locations and names are (see figure 6) 10:
- Conoventricular Ventricular Septal Defect
In general, this is a hole where portions of the ventricular septum should meet just below the pulmonary and aortic valves.
- Perimembranous Ventricular Septal Defect
This is a hole in the upper section of the ventricular septum.
- Inlet Ventricular Septal Defect
This is a hole in the septum near to where the blood enters the ventricles through the tricuspid and mitral valves. This type of ventricular septal defect also might be part of another heart defect called an atrioventricular septal defect (AVSD).
- Muscular Ventricular Septal Defect
This is a hole in the lower, muscular part of the ventricular septum and is the most common type of ventricular septal defect.
Figure 6. Ventricular Septal Defect Types
Occurrence of Ventricular Septal Defects
In a recent study in Atlanta, the Centers for Disease Control and Prevention estimated that 42 of every 10,000 babies born had a ventricular septal defect 11.
Causes and Risk Factors for Ventricular Septal Defects
The causes of heart defects (such as a ventricular septal defect) among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. Heart defects also are thought to be caused by a combination of genes and other risk factors, such as the things the mother comes in contact with in the environment or what the mother eats or drinks or the medicines the mother uses.
Diagnosis for Ventricular Septal Defects
A ventricular septal defect usually is diagnosed after a baby is born.
The size of the ventricular septal defect will influence what symptoms, if any, are present, and whether a doctor hears a heart murmur during a physical examination. Signs of a ventricular septal defect might be present at birth or might not appear until well after birth. If the hole is small, it usually will close on its own and the baby might not show any signs of the defect. However, if the hole is large, the baby might have symptoms, including:
- Shortness of breath,
- Fast or heavy breathing,
- Sweating,
- Tiredness while feeding, or
- Poor weight gain.
During a physical examination the doctor might hear a distinct whooshing sound, called a heart murmur. If the doctor hears a heart murmur or other signs are present, the doctor can request one or more tests to confirm the diagnosis. The most common test is an echocardiogram, which is an ultrasound of the heart that can show problems with the structure of the heart, show how large the hole is, and show how much blood is flowing through the hole.
Treatments for Ventricular Septal Defects
Treatments for a ventricular septal defect depend on the size of the hole and the problems it might cause. Many ventricular septal defects are small and close on their own; if the hole is small and not causing any symptoms, the doctor will check the infant regularly to ensure there are no signs of heart failure and that the hole closes on its own. If the hole does not close on its own or if it is large, further actions might need to be taken.
Depending on the size of the hole, symptoms, and general health of the child, the doctor might recommend either cardiac catheterization or open-heart surgery to close the hole and restore normal blood flow. After surgery, the doctor will set up regular follow-up visits to make sure that the ventricular septal defect remains closed. Most children who have a ventricular septal defect that closes (either on its own or with surgery) live healthy lives.
Medicines for Ventricular Septal Defects
Some children will need medicines to help strengthen the heart muscle, lower their blood pressure, and help the body get rid of extra fluid.
Nutrition for Ventricular Septal Defects
Some babies with a ventricular septal defect become tired while feeding and do not eat enough to gain weight. To make sure babies have a healthy weight gain, a special high-calorie formula might be prescribed. Some babies become extremely tired while feeding and might need to be fed through a feeding tube.
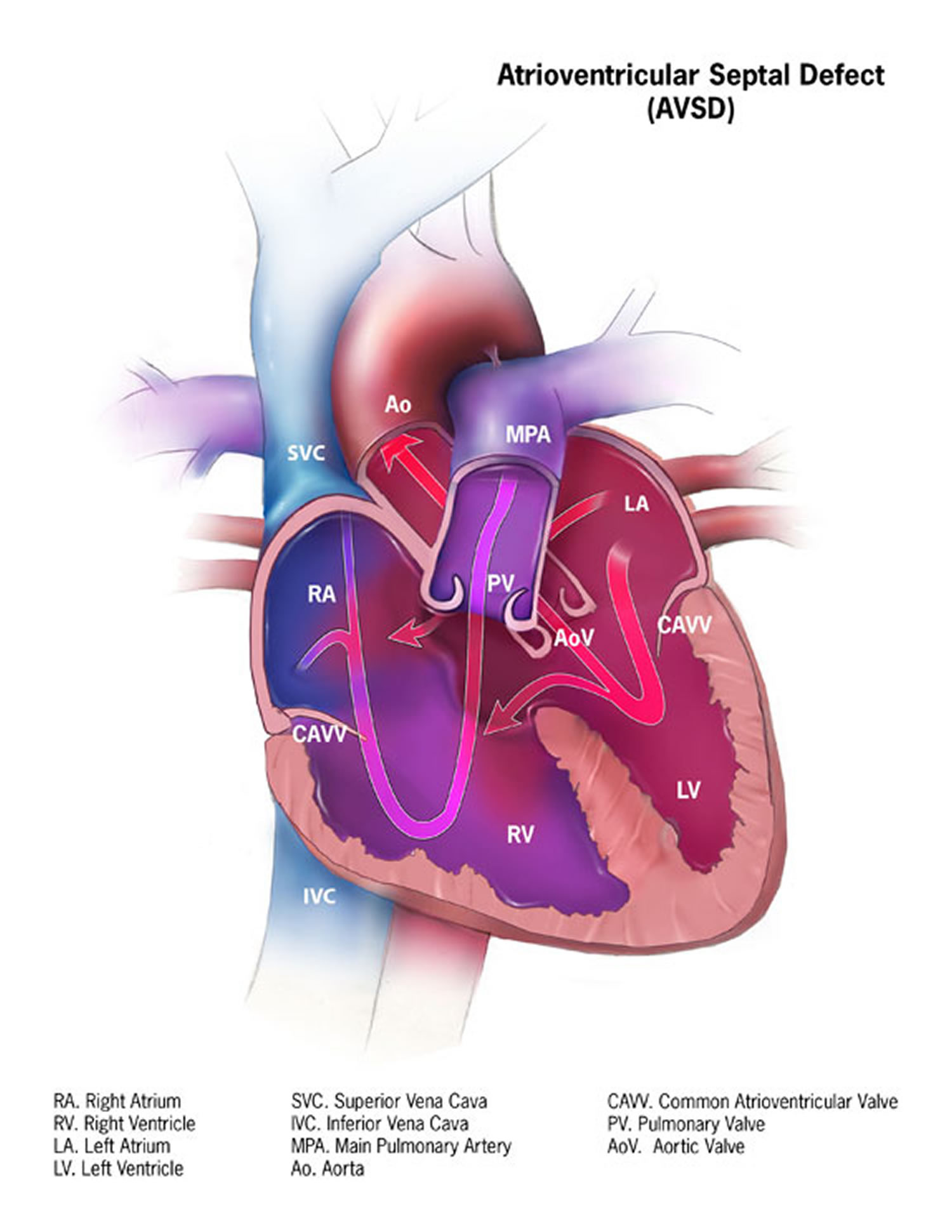
Atrioventricular Septal Defect
An atrioventricular septal defect is a heart defect in which there are holes between the chambers of the right and left sides of the heart, and the valves that control the flow of blood between these chambers may not be formed correctly 12. This condition is also called atrioventricular canal (AV canal) defect or endocardial cushion defect. In atrioventricular septal defect, blood flows where it normally should not go. The blood may also have a lower than normal amount of oxygen, and extra blood can flow to the lungs. This extra blood being pumped into the lungs forces the heart and lungs to work hard and may lead to congestive heart failure.
There are two general types of Atrioventricular Septal Defect that can occur, depending on which structures are not formed correctly:
Complete Atrioventricular Septal Defect
A complete Atrioventricular Septal Defect occurs when there is a large hole in the center of the heart which allows blood to flow between all four chambers of the heart. This hole occurs where the septa (walls) separating the two top chambers (atria) and two bottom chambers (ventricles) normally meet. There is also one common atrioventricular valve in the center of the heart instead of two separate valves – the tricuspid valve on the right side of the heart and the mitral valve on the left side of the heart. This common valve often has leaflets (flaps) that may not be formed correctly or do not close tightly. A complete Atrioventricular Septal Defect arises during pregnancy when the common valve fails to separate into the two distinct valves (tricuspid and mitral valves) and when the septa (walls) that split the upper and lower chambers of the heart do not grow all the way to meet in the center of the heart.
Partial or Incomplete Atrioventricular Septal Defect
A partial or incomplete Atrioventricular Septal Defect occurs when the heart has some, but not all of the defects of a complete Atrioventricular Septal Defect. There is usually a hole in the atrial wall or in the ventricular wall near the center of the heart. A partial Atrioventricular Septal Defect usually has both mitral and tricuspid valves, but one of the valves (usually mitral) may not close completely, allowing blood to leak backward from the left ventricle into the left atrium.
Figure 7. Atrioventricular Septal Defect
[Source 12]Occurrence of Atrioventricular Septal Defects
The Centers for Disease Control and Prevention estimates that about 2,000 babies (1 in 2,120 babies) are born with Atrioventricular Septal Defect every year in the United States 13.
Causes and Risk Factors for Atrioventricular Septal Defects
The causes of congenital heart defects, such as Atrioventricular Septal Defect, among most babies are unknown 12. Some babies have heart defects because of changes in their genes or chromosomes. In particular, Atrioventricular Septal Defect is common in babies with Down syndrome, a genetic condition that involves an extra chromosome 21 (also called trisomy 21) 12. Congenital heart defects are also thought to be caused by the combination of genes and other factors that might increase the risk of having a baby with a congenital heart defect, such as things the mother comes in contact with in her environment, what she eats or drinks, or certain medications she uses during pregnancy 12.
Diagnosis for Atrioventricular Septal Defects
Atrioventricular Septal Defect may be diagnosed during pregnancy or soon after the baby is born.
During Pregnancy
During pregnancy, there are screening tests (also called prenatal tests) to check for birth defects and other conditions. Atrioventricular Septal Defect may be diagnosed during pregnancy with an ultrasound test (which creates pictures of the baby using sound waves), but whether or not the defect can be seen with the ultrasound test depends on the size or type (partial or complete) of the Atrioventricular Septal Defect. The healthcare provider can request a fetal echocardiogram to confirm the diagnosis if Atrioventricular Septal Defect is suspected. A fetal echocardiogram is an ultrasound of the baby’s heart which shows more detail than the routine prenatal ultrasound test. The fetal echocardiogram can show problems with the structure of the heart and how well the heart is working.
After the Baby is Born
During a physical exam of an infant, a complete Atrioventricular Septal Defect may be suspected. Using a stethoscope, a doctor will often hear a heart murmur (an abnormal “whooshing” sound caused by blood flowing through the abnormal hole). However, not all heart murmurs are present at birth. Babies with a complete Atrioventricular Septal Defect usually do show signs of problems within the first few weeks after birth. When symptoms do occur, they may include
- Breathing problems
- Pounding heart
- Weak pulse
- Ashen or bluish skin color
- Poor feeding, slow weight gain
- Tiring easily
- Swelling of the legs or belly
For partial Atrioventricular Septal Defects, if the holes between the chambers of the heart are not large, the signs and symptoms may not occur in the newborn or infancy periods. In these cases, people with a partial Atrioventricular Septal Defect might not be diagnosed for years.
Symptoms which might indicate that a child’s complete Atrioventricular Septal Defect or partial Atrioventricular Septal Defect is getting worse include
- Arrhythmia, an abnormal heart rhythm. An arrhythmia can cause the heart to beat too fast, too slow, or erratically. When the heart does not beat properly, it can’t pump blood effectively.
- Congestive heart failure, when the heart cannot pump enough blood and oxygen to meet the needs of the body.
- Pulmonary hypertension, a type of high blood pressure that affects the arteries in the lungs and the right side of the heart.
The healthcare provider can request one or more tests to confirm the diagnosis of Atrioventricular Septal Defect. The most common test is an echocardiogram. This is an ultrasound of the heart that can show problems with the structure of the heart, like holes between the chambers of the right and left side of the heart, and any irregular blood flow. An electrocardiogram (EKG), which measures the electrical activity of the heart, chest x-rays, and other medical tests may also be used to make the diagnosis. Because many babies with Down syndrome have an Atrioventricular Septal Defect, all infants with Down syndrome should have an echocardiogram to look for an Atrioventricular Septal Defect or other heart defects.
Treatments for Atrioventricular Septal Defects
All Atrioventricular Septal Defects, both partial and complete types, usually require surgery. During surgery, any holes in the chambers are closed using patches. If the mitral valve does not close completely, it is repaired or replaced. For a complete Atrioventricular Septal Defect, the common valve is separated into two distinct valves – one on the right side and one on the left side.
The age at which surgery is done depends on the child’s health and the specific structure of the Atrioventricular Septal Defect. If possible, surgery should be done before there is permanent damage to the lungs from too much blood being pumped to the lungs. Medication may be used to treat congestive heart failure, but it is only a short term measure until the infant is strong enough for surgery.
Infants who have surgical repairs for Atrioventricular Septal Defect are not cured; they might have lifelong complications. The most common of these complications is a leaky mitral valve. This is when the mitral valve does not close all the way so that it allows blood to flow backwards through the valve. A leaky mitral valve can cause the heart to work harder to get enough blood to the rest of the body; a leaky mitral valve might have to be surgically repaired. A child or adult with an Atrioventricular Septal Defect will need regular follow-up visits with a cardiologist (a heart doctor) to monitor his or her progress, avoid complications, and check for other health conditions that might develop as the child gets older. With proper treatment, most babies with Atrioventricular Septal Defect grow up to lead healthy, productive lives.
Patent Ductus Arteriosus
Patent ductus arteriosus is a fairly common heart defect that can occur soon after birth 8. In patent ductus arteriosus, abnormal blood flow occurs between the aorta and the pulmonary artery.
Before birth, these arteries are connected by a blood vessel called the ductus arteriosus. This blood vessel is an essential part of fetal blood circulation. Within minutes or up to a few days after birth, the ductus arteriosus closes.
In some babies, however, the ductus arteriosus remains open (patent). The opening allows oxygen-rich blood from the aorta to mix with oxygen-poor blood from the pulmonary artery. This can strain the heart and increase blood pressure in the lung arteries.
A heart murmur might be the only sign of patent ductus arteriosus. A heart murmur is an extra or unusual sound heard during a heartbeat. Other signs and symptoms can include shortness of breath, poor feeding and growth, tiring easily, and sweating with exertion.
Patent ductus arteriosus is treated with medicines, catheter-based procedures, and surgery. Small patent ductus arteriosus often close without treatment 8.
Figure 8. Patent Ductus Arteriosus
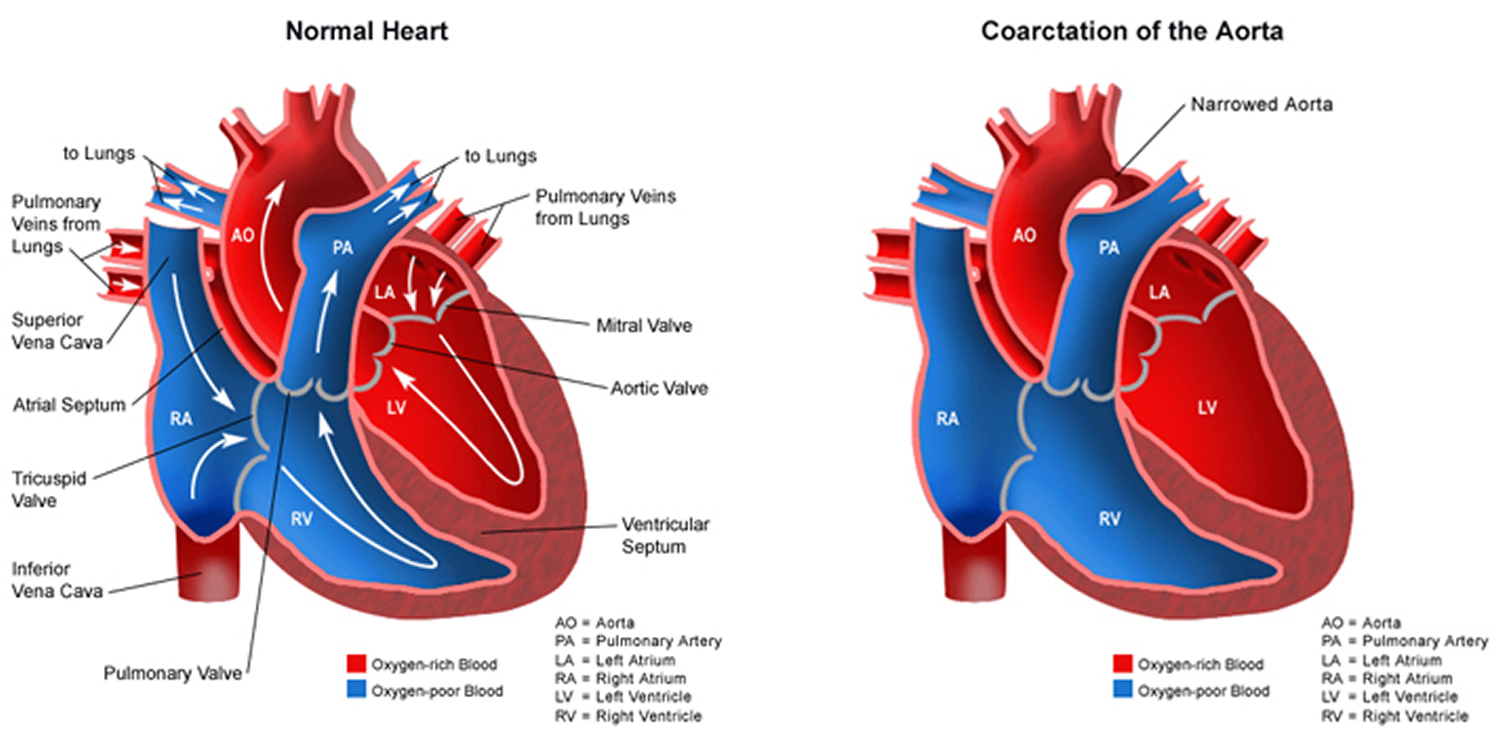
Coarctation of the Aorta
Coarctation of the aorta is a birth defect in which a part of the aorta is narrower than usual 14. If the narrowing is severe enough and if it is not diagnosed, the baby may have serious problems and may need surgery or other procedures soon after birth. For this reason, coarctation of the aorta is often considered a critical congenital heart defect. The defect occurs when a baby’s aorta does not form correctly as the baby grows and develops during pregnancy. The narrowing of the aorta usually happens in the part of the blood vessel just after the arteries branch off to take blood to the head and arms, near the patent ductus arteriosus, although sometimes the narrowing occurs before or after the ductus arteriosus. In some babies with coarctation, it is thought that some tissue from the wall of ductus arteriosus blends into the tissue of the aorta. When the tissue tightens and allows the ductus arteriosus to close normally after birth, this extra tissue may also tighten and narrow the aorta.
The narrowing, or coarctation, blocks normal blood flow to the body. This can back up flow into the left ventricle of the heart, making the muscles in this ventricle work harder to get blood out of the heart. Since the narrowing of the aorta is usually located after arteries branch to the upper body, coarctation in this region can lead to normal or high blood pressure and pulsing of blood in the head and arms and low blood pressure and weak pulses in the legs and lower body.
If the condition is very severe, enough blood may not be able to get through to the lower body. The extra work on the heart can cause the walls of the heart to become thicker in order to pump harder. This eventually weakens the heart muscle. If the aorta is not widened, the heart may weaken enough that it leads to heart failure. Coarctation of the aorta often occurs with other congenital heart defects.
Figure 9. Coarctation of the Aorta
Occurrence of Coarctation of the Aorta
The Centers for Disease Control and Prevention estimates that about 4 out of every 10,000 babies are born each year in the United States with coarctation of the aorta 15.
Causes and Risk Factors of Coarctation of the Aorta
The causes of heart defects, including coarctation of the aorta, among most babies are unknown 14. Some babies have heart defects because of changes in their genes or chromosomes. Heart defects, like coarctation of the aorta, are also thought to be caused by a combination of genes and other risk factors, such as things the mother comes in contact with in the environment, what the mother eats or drinks, or medicines the mother uses 14.
Diagnosis of Coarctation of the Aorta
Coarctation of the aorta is usually diagnosed after the baby is born. How early in life the defect is diagnosed usually depends on how mild or severe the symptoms are. Those with severe narrowing will have symptoms early in life, while babies with mild narrowing may never have problems, or signs may not be detected until later in life 14.
In babies with a more serious condition, early signs usually include:
- pale skin
- irritability
- heavy sweating
- difficulty breathing
Detection of the defect is often made during a physical exam. In infants and older individuals, the pulse will be noticeably weaker in the legs or groin than it is in the arms or neck, and a heart murmur—an abnormal whooshing sound caused by disrupted blood flow—may be heard through a doctor’s stethoscope 14. Older children and adults with coarctation of the aorta often have high blood pressure in the arms.
Once suspected, an echocardiogram is the most commonly used test to confirm the diagnosis. An echocardiogram is an ultrasound of the heart that can show problems with the structure of the heart and the blood flow through it, and how well the heart is working. It will show the location and severity of the coarctation and whether any other heart defects are present. Other tests to measure the function of the heart may be used including chest x-ray, electrocardiogram (EKG), magnetic resonance imaging (MRI), and cardiac catheterization.
Coarctation of the aorta is often considered a critical congenital heart defect because if the narrowing is severe enough and it is not diagnosed, the baby may have serious problems soon after birth 14. Critical congenital heart defects also can be detected with newborn pulse oximetry screening. Pulse oximetry is a simple bedside test to determine the amount of oxygen in a baby’s blood. Low levels of oxygen in the blood can be a sign of a critical congenital heart defect. Newborn screening using pulse oximetry can identify some infants with a critical congenital heart defect, like coarctation of the aorta, before they show any symptoms.
Treatments for Coarctation of the Aorta
No matter what age the defect is diagnosed, the narrow aorta will need to be widened once symptoms are present. This can be done with surgery or a procedure called balloon angioplasty. A balloon angioplasty is a procedure that uses a thin, flexible tube, called a catheter, which is inserted into a blood vessel and directed to the aorta. When the catheter reaches the narrow area of the aorta, a balloon at the tip is inflated to expand the blood vessel. Sometimes a mesh-covered tube (stent) is inserted to keep the vessel open. The stent is used more often to initially widen the aorta or re-widen it if the aorta narrows again after surgery has been performed. During surgery to correct a coarctation, the narrow portion is removed and the aorta is reconstructed or patched to allow blood to flow normally through the aorta.
Even after surgery, children with a coarctation of the aorta often have high blood pressure that is treated with medicine. It is important for children and adults with coarctation of the aorta to follow up regularly with a cardiologist (a heart doctor) to monitor their progress and check for other health conditions that might develop as they get older.
Dextro-Transposition of the Great Arteries
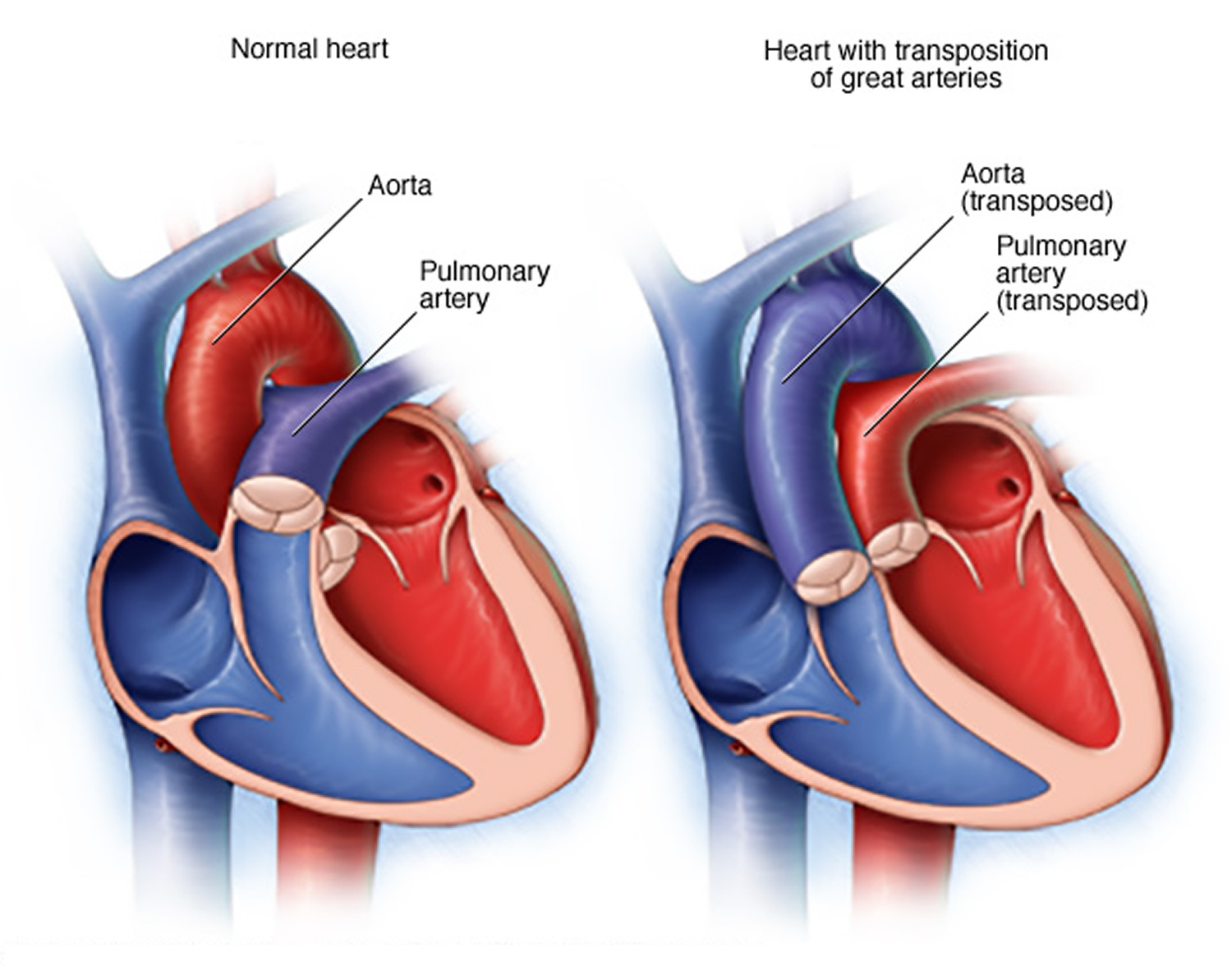
Dextro-Transposition of the Great Arteries is a birth defect of the heart in which the two main arteries carrying blood out of the heart – the main pulmonary artery and the aorta – are switched in position, or “transposed” 16. Because a baby with this defect may need surgery or other procedures soon after birth, Dextro-Transposition of the Great Arteries is considered a congenital heart defect.
In transposition of the great arteries, the aorta is in front of the pulmonary artery and is either primarily to the right (dextro) or to the left (levo) of the pulmonary artery. Dextro-Transposition of the Great Arteries is often simply called “TGA.” However, “TGA” is a broader term that includes both dextro-TGA (d-TGA) and a rarer heart defect called levo-TGA (l-TGA), or congenitally corrected TGA, which is not discussed here.
In a baby without a congenital heart defect, the right side of the heart pumps oxygen-poor blood from the heart to the lungs through the pulmonary artery. The left side of the heart pumps oxygen-rich blood to the rest of the body through the aorta. The aorta is usually behind the pulmonary artery.
In babies with Dextro-Transposition of the Great Arteries, oxygen-poor blood from the body enters the right side of the heart. But, instead of going to the lungs, the blood is pumped directly back out to the rest of the body through the aorta. Oxygen-rich blood from the lungs entering the heart is pumped straight back to the lungs through the main pulmonary artery.
Often, babies with Dextro-Transposition of the Great Arteries have other heart defects, such as a hole between the lower chambers of the heart (a ventricular septal defect) or the upper chambers of the heart (an atrial septal defect) that allow blood to mix so that some oxygen-rich blood can be pumped to the rest of the body. The patent ductus arteriosus also allows some oxygen-rich blood to be pumped to the rest of the body.
Figure 10. Transposition of the Great Arteries
Occurrence of Transposition of the Great Arteries
The Centers for Disease Control and Prevention estimates that about 1,250 babies are born with TGA each year in the United States 17. This means that every 1 in 3,300 babies born in the US is affected by this defect.
Causes and Risk Factors for Transposition of the Great Arteries
The causes of congenital heart defects, such as dextro-Transposition of the Great Arteries, among most babies are unknown. Some babies have congenital heart defects because of changes in their genes or chromosomes. Heart defects are also thought to be caused by the combination of genes and other risk factors such as things the mother comes in contact with in her environment, or what the mother eats or drinks, or certain medications she uses.
Diagnosis of Transposition of the Great Arteries
This defect may be diagnosed during pregnancy or soon after the baby is born.
During Pregnancy
During pregnancy, there are screening tests that the mother can have (also called prenatal tests) to check for birth defects and other conditions. Dextro-Transposition of the Great Arteries may be diagnosed during pregnancy with an ultrasound test (which creates pictures of the baby). Some findings from the ultrasound may make the health care provider suspect a baby could have dextro-Transposition of the Great Arteries. If so, the health care provider can request a fetal echocardiogram to confirm the diagnosis. A fetal echocardiogram is a more detailed ultrasound of the baby’s heart. This test can show problems with the structure of the heart and how the heart is working with this defect.
After the Baby is Born
Symptoms occur at birth or very soon afterwards. How severe the symptoms are will depend on whether there is a way for blood to mix and for oxygen-rich blood to get out to the rest of the body. For example, if an infant with dextro-Transposition of the Great Arteries has another defect, like an atrial septal defect (ASD), the atrial septal defect forms a passageway for some oxygen-rich blood to be pumped to the rest of the body. This infant with both dextro-Transposition of the Great Arteries and an atrial septal defect may not have as severe symptoms as infants whose hearts don’t have any mixing of blood. Infants with dextro-Transposition of the Great Arteries can have a bluish looking skin color—called cyanosis—because their blood doesn’t carry enough oxygen. Infants with dextro-Transposition of the Great Arteries or other conditions causing cyanosis can have symptoms such as:
- Problems breathing
- Pounding heart
- Weak pulse
- Ashen or bluish skin color
- Poor feeding
Because the infant might be bluish in color and have trouble breathing, d-TGA is usually diagnosed within the first week of life. The health care provider can request one or more tests to confirm the diagnosis. The most common test is an echocardiogram. An echocardiogram is an ultrasound of the heart that can show problems with the structure of the heart, like incorrect positioning of the two large arteries, and any irregular blood flow. An electrocardiogram (EKG), which measures the electrical activity of the heart, chest x-rays, and other medical tests may also be used to make the diagnosis.
D-TGA is a that also can be detected with newborn pulse oximetry screening. Pulse oximetry is a simple bedside test to determine the amount of oxygen in a baby’s blood. Low levels of oxygen in the blood can be a sign of a critical congenital heart defect. Newborn screening using pulse oximetry can identify some infants with a critical congenital heart defect, like d-TGA, before they show any symptoms.
Treatments for Transposition of the Great Arteries
Surgery is required for all babies born with d-TGA. Other procedures may be done before surgery in order to maintain, enlarge or create openings that will allow oxygen-rich blood to get out to the body.
There are two types of surgery to repair d-TGA:
- Arterial Switch Operation: This is the most common procedure and it is usually done in the first month of life. It restores usual blood flow through the heart and out to the rest of the body. During this surgery, the arteries are switched to their usual positions—the pulmonary artery arising from the right ventricle and the aorta from the left ventricle. The coronary arteries (small arteries that provide blood to the heart muscle) also must be moved and reattached to the aorta.
- Atrial Switch Operation: This procedure is less commonly performed. During this surgery, the arteries are left in place, but a tunnel (baffle) is created between the top chambers (atria) of the heart. This tunnel allows oxygen-poor blood to move from the right atrium to the left ventricle and out the pulmonary artery to the lungs. Returning oxygen-rich blood moves through the tunnel from the left atrium to the right ventricle and out the aorta to the body. Although this repair helps blood to go to the lungs and then out to the body, it also makes extra work for the right ventricle to pump blood to the entire body. Therefore, this repair can lead to difficulties later in life.
After surgery, medications may be needed to help the heart pump better, control blood pressure, help get rid of extra fluid in the body, and slow down the heart if it is beating too fast. If the heart is beating too slowly, a pacemaker can be used.
Infants who have these surgeries are not cured; they may have lifelong complications. A child or adult with d-TGA will need regular follow-up visits with a cardiologist (a heart doctor) to monitor their progress and avoid complications or other health problems. With proper treatment, most babies with d-TGA grow up to lead healthy, productive lives.
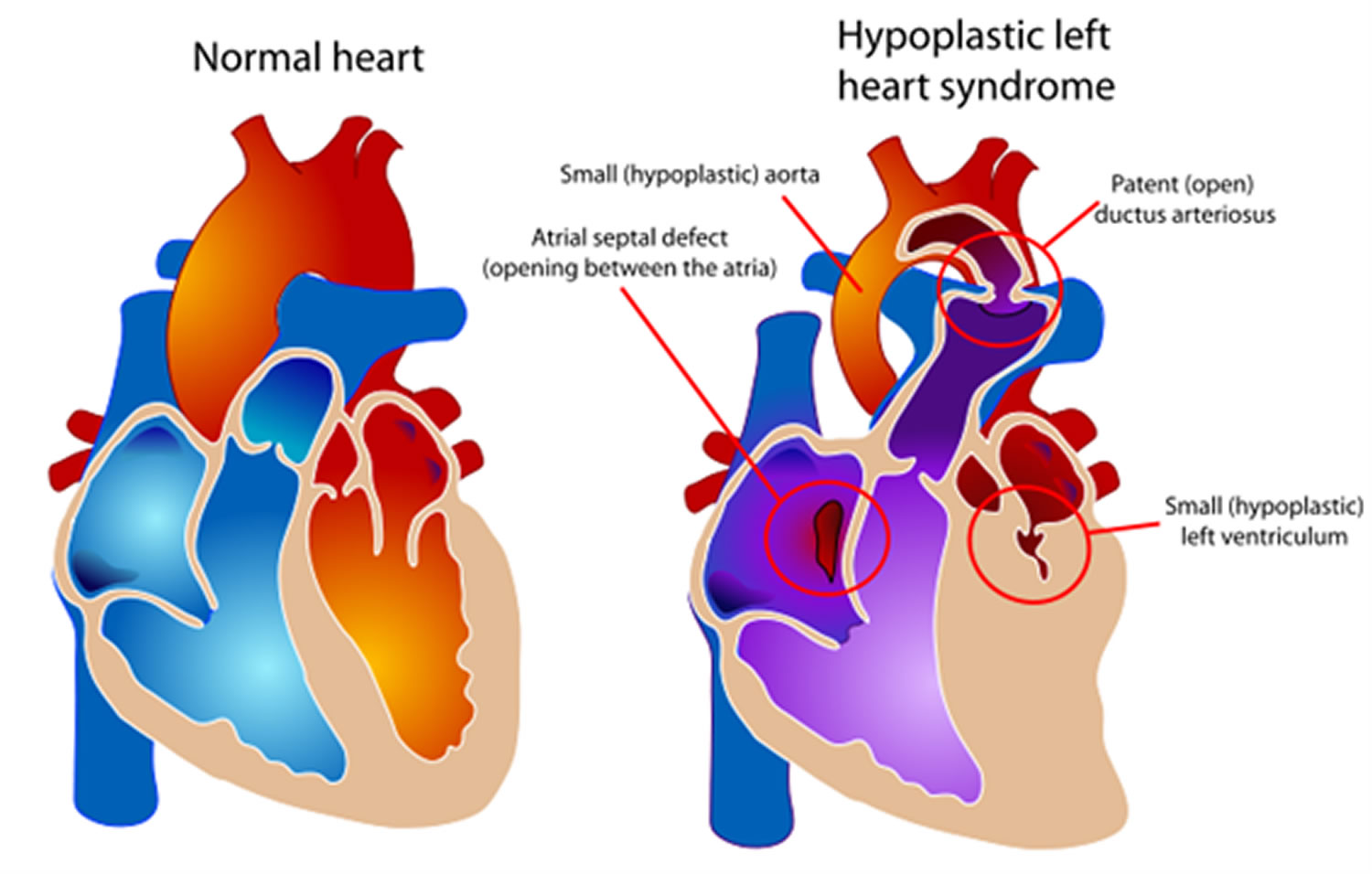
Hypoplastic Left Heart Syndrome
Hypoplastic left heart syndrome is a birth defect that affects normal blood flow through the heart. As the baby develops during pregnancy, the left side of the heart does not form correctly. Hypoplastic left heart syndrome is one type of congenital heart defect.
Hypoplastic left heart syndrome affects a number of structures on the left side of the heart that do not fully develop 18, for example:
- The left ventricle is underdeveloped and too small.
- The mitral valves is not formed or is very small.
- The aortic valve is not formed or is very small.
- The ascending portion of the aorta is underdeveloped or is too small.
- Often, babies with hypoplastic left heart syndrome also have an atrial septal defect, which is a hole between the left and right upper chambers (atria) of the heart.
In a baby without a congenital heart defect, the right side of the heart pumps oxygen-poor blood from the heart to the lungs. The left side of the heart pumps oxygen-rich blood to the rest of the body. When a baby is growing in a mother’s womb during pregnancy, there are two small openings between the left and right sides of the heart: the patent ductus arteriosus and the patent foramen ovale. Normally, these openings will close a few days after birth.
In babies with hypoplastic left heart syndrome, the left side of the heart cannot pump oxygen-rich blood to the body properly. During the first few days of life for a baby with hypoplastic left heart syndrome, the oxygen-rich blood bypasses the poorly functioning left side of the heart through the patent ductus arteriosus and the patent foramen ovale. The right side of the heart then pumps blood to both the lungs and the rest of the body. However, among babies with hypoplastic left heart syndrome, when these openings close, it becomes hard for oxygen-rich blood to get to the rest of the body.
Figure 11. Hypoplastic Left Heart Syndrome
Occurrence of Hypoplastic Left Heart Syndrome
The Centers for Disease Control and Prevention (CDC) estimates that each year about 960 babies in the United States are born with hypoplastic left heart syndrome 19. In other words, about 1 out of every 4,344 babies born in the United States each year is born with hypoplastic left heart syndrome.
Causes and Risk Factors of Hypoplastic Left Heart Syndrome
The causes of heart defects such as hypoplastic left heart syndrome among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. These types of heart defects also are thought to be caused by a combination of genes and other risk factors, such as things the mother comes in contact with in the environment or what the mother eats or drinks or the medicines the mother uses.
Diagnosis of Hypoplastic Left Heart Syndrome
Hypoplastic left heart syndrome may be diagnosed during pregnancy or soon after the baby is born.
During Pregnancy
During pregnancy, there are screening tests (also called prenatal tests,) to check for birth defects and other conditions. Hypoplastic left heart syndrome may be diagnosed during pregnancy with an ultrasound, (which creates pictures of the body). Some findings from the ultrasound may make the health care provider suspect a baby may have hypoplastic left heart syndrome. If so, the health care provider can request a fetal echocardiogram, an ultrasound of the baby’s heart, to confirm the diagnosis.This test can show problems with the structure of the heart and how the heart is working with this defect.
After the Baby Is Born
Babies with hypoplastic left heart syndrome might not have trouble for the first few days of life while the patent ductus arteriosus and the patent foramen ovale (the normal openings in the heart) are open, but quickly develop signs after these openings are closed, including:
- Problems breathing,
- Pounding heart,
- Weak pulse, or
- Ashen or bluish skin color.
During a physical examination, a doctor can see these signs or might hear a heart murmur (an abnormal whooshing sound caused by blood not flowing properly). If a murmur is heard or other signs are present, the health care provider might request one or more tests to make a diagnosis, the most common being an echocardiogram. Echocardiography also is useful for helping the health care provider follow the child’s health over time.
Treatments for Hypoplastic Left Heart Syndrome
Treatments for some health problems associated with hypoplastic left heart syndrome might include:
Medicines
Some babies and children will need medicines to help strengthen the heart muscle, lower their blood pressure, and help the body get rid of extra fluid.
Nutrition
Some babies with hypoplastic left heart syndrome become tired while feeding and do not eat enough to gain weight. To make sure babies have a healthy weight gain, a special high-calorie formula might be prescribed. Some babies become extremely tired while feeding and might need to be fed through a feeding tube.
Surgery
Soon after a baby with hypoplastic left heart syndrome is born, multiple surgeries done in a particular order are needed to increase blood flow to the body and bypass the poorly functioning left side of the heart. The right ventricle becomes the main pumping chamber to the body. These surgeries do not cure hypoplastic left heart syndrome, but help restore heart function. Sometimes medicines are given to help treat symptoms of the defect before or after surgery. Surgery for hypoplastic left heart syndrome usually is done in three separate stages:
- Norwood Procedure
This surgery usually is done within the first 2 weeks of a baby’s life. Surgeons create a “new” aorta and connect it to the right ventricle. They also place a tube from either the aorta or the right ventricle to the vessels supplying the lungs (pulmonary arteries). Thus, the right ventricle can pump blood to both the lungs and the rest of the body. This can be a very challenging surgery. After this procedure, an infant’s skin still might look bluish because oxygen-rich and oxygen-poor blood still mix in the heart.
- Bi-directional Glenn Shunt Procedure
This usually is performed when an infant is 4 to 6 months of age. This procedure creates a direct connection between the pulmonary artery and the vessel (the superior vena cava) returning oxygen-poor blood from the upper part of the body to the heart. This reduces the work the right ventricle has to do by allowing blood returning from the body to flow directly to the lungs.
- Fontan Procedure
This procedure usually is done sometime during the period when an infant is 18 months to 3 years of age. Doctors connect the pulmonary artery and the vessel (the inferior vena cava) returning oxygen-poor blood from the lower part of the body to the heart, allowing the rest of the blood coming back from the body to go to the lungs. Once this procedure is complete, oxygen-rich and oxygen-poor blood no longer mix in the heart and an infant’s skin will no longer look bluish.
Infants who have these surgeries are not cured; they may have lifelong complications.
Infants with hypoplastic left heart syndrome will need regular follow-up visits with a cardiologist (a heart doctor) to monitor their progress. If the hypoplastic left heart syndrome defect is very complex, or the heart becomes weak after the surgeries, a heart transplant may be needed. Infants who receive a heart transplant will need to take medicines for the rest of their lives to prevent their body from rejecting the new heart.
Narrowed Valves
Simple congenital heart defects also can involve the heart’s valves. These valves control the flow of blood from the atria to the ventricles and from the ventricles into the two large arteries connected to the heart (the aorta and the pulmonary artery).
Valves can have the following types of defects 8:
- Stenosis. This defect occurs if the flaps of a valve thicken, stiffen, or fuse together. As a result, the valve cannot fully open. Thus, the heart has to work harder to pump blood through the valve.
- Atresia. This defect occurs if a valve doesn’t form correctly and lacks a hole for blood to pass through. Atresia of a valve generally results in more complex congenital heart disease.
- Regurgitation. This defect occurs if a valve doesn’t close tightly. As a result, blood leaks back through the valve.
The most common valve defect is pulmonary valve stenosis, which is a narrowing of the pulmonary valve. This valve allows blood to flow from the right ventricle into the pulmonary artery. The blood then travels to the lungs to pick up oxygen.
Pulmonary valve stenosis can range from mild to severe. Most children who have this defect have no signs or symptoms other than a heart murmur. Treatment isn’t needed if the stenosis is mild.
In babies who have severe pulmonary valve stenosis, the right ventricle can get very overworked trying to pump blood to the pulmonary artery. These infants may have signs and symptoms such as rapid or heavy breathing, fatigue (tiredness), and poor feeding. Older children who have severe pulmonary valve stenosis may have symptoms such as fatigue while exercising.
Some babies may have pulmonary valve stenosis and Patent Ductus Arteriosus or Atrial Septal Defects. If this happens, oxygen-poor blood can flow from the right side of the heart to the left side. This can cause cyanosis. Cyanosis is a bluish tint to the skin, lips, and fingernails. It occurs because the oxygen level in the blood leaving the heart is below normal.
Severe pulmonary valve stenosis is treated with a catheter procedure.
Pulmonary Atresia
Pulmonary atresia is a birth defect of the pulmonary valve, which is the valve that controls blood flow from the right ventricle (lower right chamber of the heart) to the main pulmonary artery (the blood vessel that carries blood from the heart to the lungs). Pulmonary atresia is when this valve didn’t form at all, and no blood can go from the right ventricle of the heart out to the lungs 20. Because a baby with pulmonary atresia may need surgery or other procedures soon after birth, this birth defect is considered a critical congenital heart defect.
In a baby without a congenital heart defect, the right side of the heart pumps oxygen-poor blood from the heart to the lungs through the pulmonary artery. The blood that comes back from the lungs is oxygen-rich and can then be pumped to the rest of the body. In babies with pulmonary atresia, the pulmonary valve that usually controls the blood flowing through the pulmonary artery is not formed, so blood is unable to get directly from the right ventricle to the lungs.
In pulmonary atresia, since blood cannot directly flow from the right ventricle of the heart out to the pulmonary artery, blood must use other routes to bypass the unformed pulmonary valve. The foramen ovale, a natural opening between the right and left upper chambers of the heart during pregnancy that usually closes after the baby is born, often remains open to allow blood flow to the lungs. Additionally, doctors may give medicine to the baby to keep the baby’s patent ductus arteriosus open after the baby’s birth. The patent ductus arteriosus is the blood vessel that allows blood to move around the baby’s lungs before the baby is born and it also usually closes after birth.
Figure 12. Pulmonary Atresia
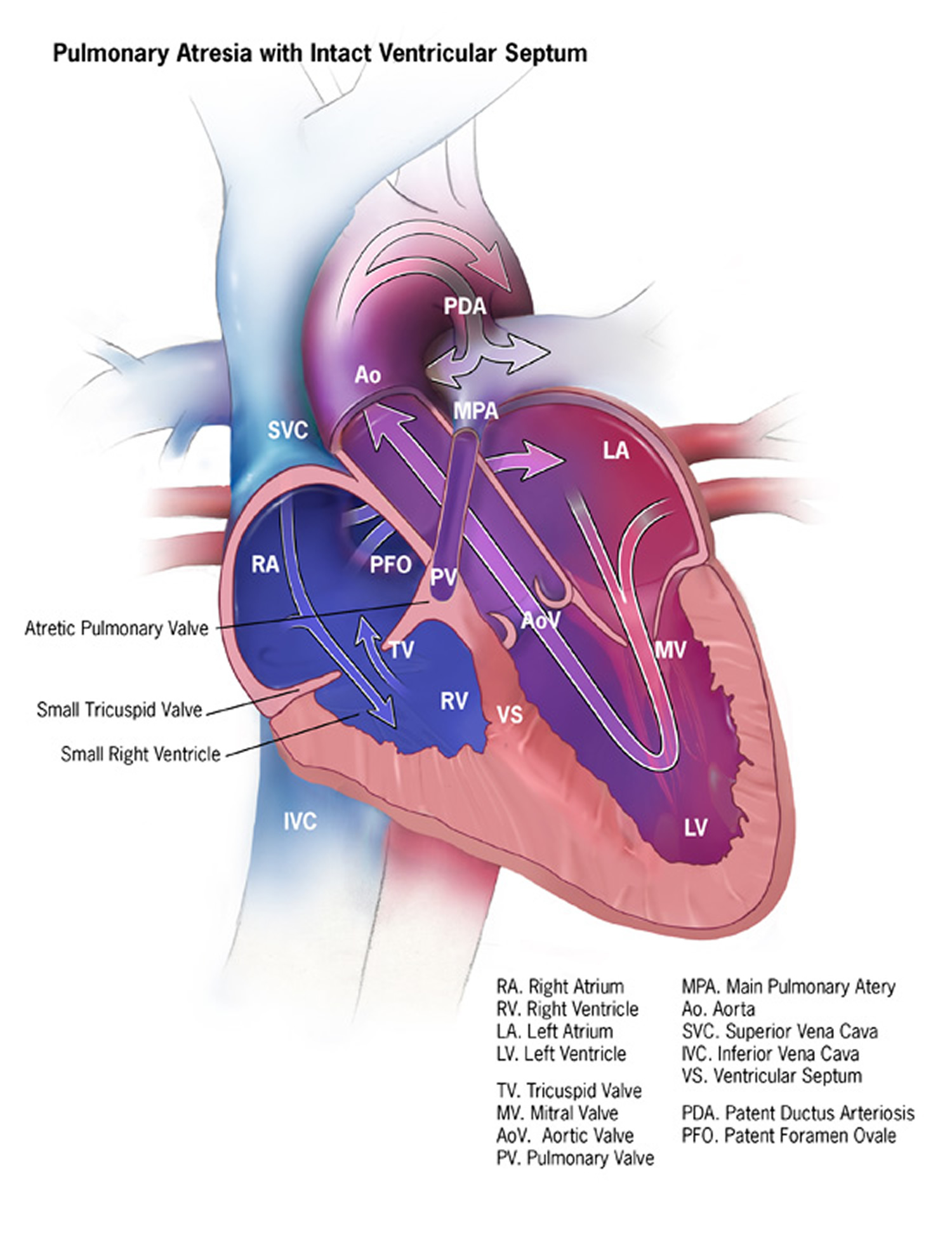
Types of Pulmonary Atresia
There are typically two types of pulmonary atresia, according to whether or not a baby also has a ventricular septal defect (a hole in the wall that separates the two lower chambers, or ventricles, of the heart):
- Pulmonary atresia with an intact ventricular septum: In this form of pulmonary atresia, the wall, or septum, between the ventricles remains complete and intact. During pregnancy when the heart is developing, very little blood flows into or out of the right ventricle (RV), and therefore the RV doesn’t fully develop and remains very small. If the RV is under-developed, the heart can have problems pumping blood to the lungs and the body. The artery which usually carries blood out of the right ventricle, the main pulmonary artery (MPA), remains very small, since the pulmonary valve (PV) doesn’t form.
- Pulmonary atresia with a ventricular septal defect: In this form of pulmonary atresia, a ventricular septal defect (VSD) allows blood to flow into and out of the right ventricle (RV). Therefore, blood flowing into the RV can help the ventricle develop during pregnancy, so it is typically not as small as in pulmonary atresia with an intact ventricular septum. Pulmonary atresia with a VSD is similar to another condition called tetralogy of Fallot. However, in tetralogy of Fallot, the pulmonary valve (PV) does form, although it is small and blood has trouble flowing through it – this is called pulmonary valve stenosis. Thus, pulmonary atresia with a VSD is like a very severe form of tetralogy of Fallot.
Occurrence of Pulmonary Atresia
In a 2012 study using data from birth defects tracking systems across the United States, researchers estimated that about 1 out of every 10,000 babies is born with pulmonary atresia 21.
Causes and Risk Factors of Pulmonary Atresia
The causes of heart defects, such as pulmonary atresia, among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. Heart defects also are thought to be caused by a combination of genes and other factors, such as the things the mother comes in contact with in the environment, or what the mother eats or drinks, or certain medicines she uses.
Diagnosis of Pulmonary Atresia
Pulmonary atresia may be diagnosed during pregnancy or soon after a baby is born.
During Pregnancy
During pregnancy, there are screening tests (also called prenatal tests) to check for birth defects and other conditions. Pulmonary atresia might be seen during an ultrasound (which creates pictures of the body). Some findings from the ultrasound may make the healthcare provider suspect a baby may have pulmonary atresia. If so, the healthcare provider can request a fetal echocardiogram to confirm the diagnosis. A fetal echocardiogram is an ultrasound specifically of the baby’s heart and major blood vessels that is performed during the pregnancy. This test can show problems with the structure of the heart and how well the heart is working.
After the Baby is Born
Babies born with pulmonary atresia will show symptoms at birth or very soon afterwards. They may have a bluish looking skin color, called cyanosis, because their blood doesn’t carry enough oxygen. Infants with pulmonary atresia can have additional symptoms such as:
- Problems breathing
- Ashen or bluish skin color
- Poor feeding
- Extreme sleepiness
During a physical examination, a doctor can see the symptoms, such as bluish skin or problems breathing. Using a stethoscope, a doctor will check for a heart murmur (an abnormal “whooshing” sound caused by blood not flowing properly). However, it is not uncommon for a heart murmur to be absent right at birth.
If a doctor suspects that there might be a problem, the doctor can request one or more tests to confirm the diagnosis of pulmonary atresia. The most common test is an echocardiogram. This test is an ultrasound of the baby’s heart that can show problems with the structure of the heart, like holes in the walls between the chambers, and any irregular blood flow. Cardiac catheterization (inserting a thin tube into a blood vessel and guiding it to the heart) also can confirm the diagnosis by looking at the inside of the heart and measuring the blood pressure and oxygen levels. An electrocardiogram (EKG), which measures the electrical activity of the heart, and other medical tests may also be used to make the diagnosis.
Pulmonary atresia is a critical congenital heart defect that may be detected with newborn screening using pulse oximetry (also known as pulse ox). Pulse oximetry is a simple bedside test to estimate the amount of oxygen in a baby’s blood. Low levels of oxygen in the blood can be a sign of a critical congenital heart defect. Newborn screening using pulse oximetry can identify some infants with a critical congenital heart defect, like pulmonary atresia, before they show any symptoms.
Treatments of Pulmonary Atresia
Most babies with pulmonary atresia will need medication to keep the ductus arteriosus open after birth. Keeping this blood vessel open will help with blood flow to the lungs until the pulmonary valve can be repaired.
Treatment for pulmonary atresia depends on its severity.
- In some cases, blood flow can be improved by using cardiac catheterization (inserting a thin tube into a blood vessel and guiding it to the heart). During this procedure, doctors can expand the valve using a balloon or they may need to place a stent (a small tube) to keep the ductus arteriosus open.
- In most cases of pulmonary atresia, a baby may need surgery soon after birth. During surgery, doctors widen or replace the pulmonary valve and enlarge the passage to the pulmonary artery. If a baby has a ventricular septal defect, the doctor also will place a patch over the ventricular septal defect to close the hole between the two lower chambers of the heart. These actions will improve blood flow to the lungs and the rest of the body. If a baby with pulmonary atresia has an underdeveloped right ventricle, he or she might need staged surgical procedures, similar to surgical repairs for hypoplastic left heart syndrome.
Most babies with pulmonary atresia will need regular follow-up visits with a cardiologist (a heart doctor) to monitor their progress and check for other health conditions that might develop as they get older. As adults, they may need more surgery or medical care for other possible problems.
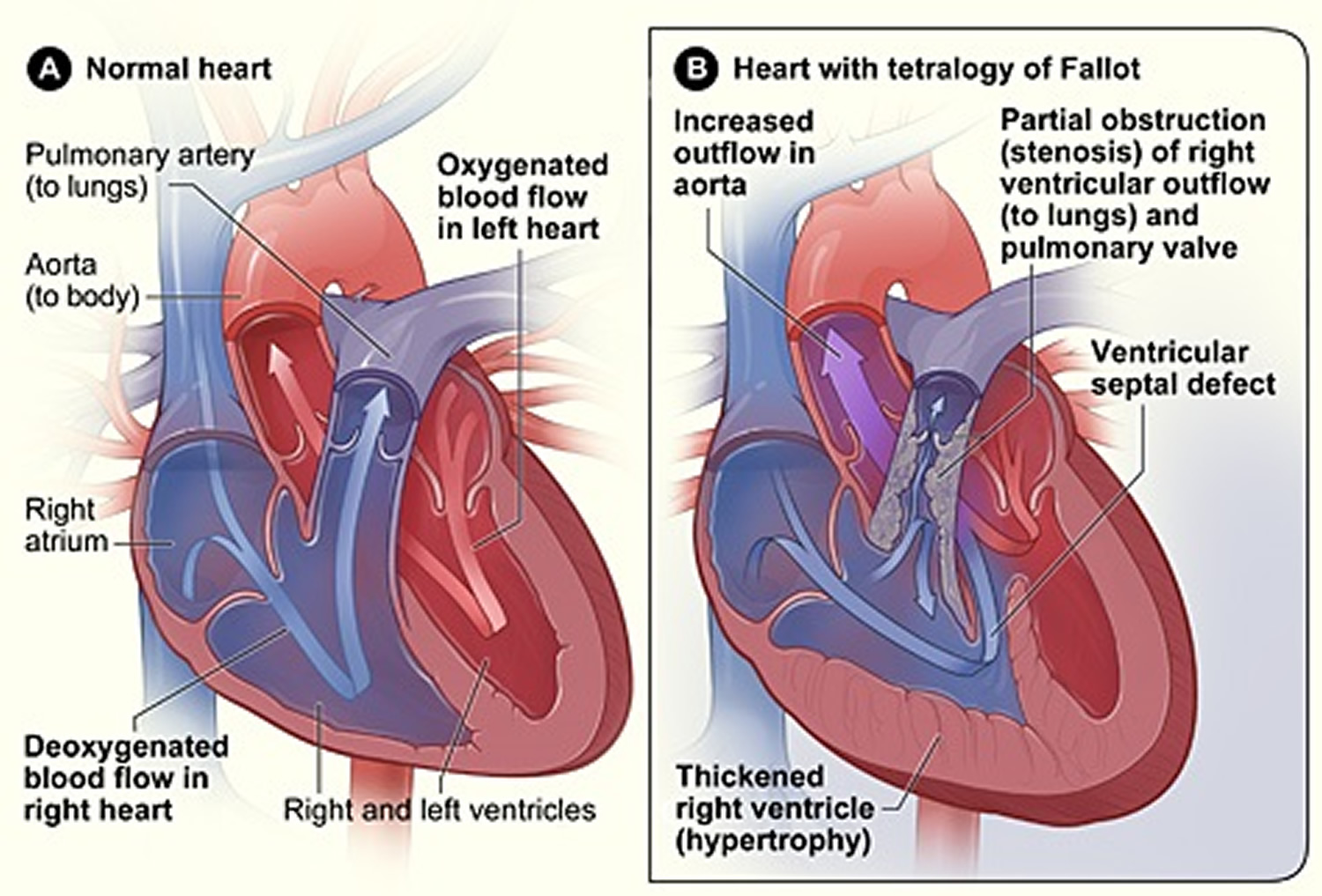
Tetralogy of Fallot
Tetralogy of Fallot is a complex congenital heart defect that affects normal blood flow through the heart. It happens when a baby’s heart does not form correctly as the baby grows and develops in the mother’s womb during pregnancy.
Tetralogy of Fallot is made up of the following four defects of the heart and its blood vessels 22:
- A hole in the wall between the two lower chambers―or ventricles―of the heart. This condition also is called a ventricular septal defect.
- A narrowing of the pulmonary valve and main pulmonary artery. This condition also is called pulmonary stenosis.
- The aortic valves, which opens to the aorta, is enlarged and seems to open from both ventricles, rather than from the left ventricle only, as in a normal heart. In this defect, the aortic valve sits directly on top of the ventricular septal defect.
- The muscular wall of the lower right chamber of the heart (right ventricle) is thicker than normal. This also is called ventricular hypertrophy.
Because a baby with tetralogy of Fallot may need surgery or other procedures soon after birth, this birth defect is considered a critical congenital heart defect.
This heart defect can cause oxygen in the blood that flows to the rest of the body to be reduced. Infants with tetralogy of Fallot can have a bluish-looking skin color―called cyanosis―because their blood doesn’t carry enough oxygen. At birth, infants might not have blue-looking skin, but later might develop sudden episodes of bluish skin during crying or feeding. These episodes are called tet spells.
Infants with tetralogy of Fallot or other conditions causing cyanosis can have problems including:
- A higher risk of getting an infection of the layers of the heart, called endocarditis.
- A higher risk of having irregular heart rhythms, called arrhythmia.
- Dizziness, fainting, or seizures, because of the low oxygen levels in their blood.
- Delayed growth and development.
Children who have had this heart defect repaired need lifelong medical care from a specialist to make sure they stay as healthy as possible.
Figure 13. Tetralogy of Fallot
Occurrence of Tetralogy of Fallot
The Centers for Disease Control and Prevention estimates that each year about 1,660 babies in the United States are born with tetralogy of Fallot 23. In other words, about 1 in every 2518 babies born in the United States each year are born with tetratology of Fallot.
Causes and Risk Factors of Tetralogy of Fallot
The causes of heart defects (such as tetralogy of Fallot) among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. Heart defects such as tetralogy of Fallot also are thought to be caused by a combination of genes and other risk factors, such as the things the mother or fetus come in contact with in the environment or what the mother eats or drinks or the medicines she uses.
Diagnosis of Tetralogy of Fallot
Tetralogy of Fallot may be diagnosed during pregnancy or soon after a baby is born.
During Pregnancy
During pregnancy, there are screening tests (also called prenatal tests) to check for birth defects and other conditions. Tetralogy of Fallot might be seen during an ultrasound (which creates pictures of the body). Some findings from the ultrasound may make the health care provider suspect a baby may have tetralogy of Fallot. If so, the health care provider can request a fetal echocardiogram to confirm the diagnosis. A fetal echocardiogram is an ultrasound of the heart of the fetus. This test can show problems with the structure of the heart and how the heart is working with this defect.
After a Baby Is Born
Tetralogy of Fallot usually is diagnosed after a baby is born, often after the infant has an episode of turning blue during crying or feeding (a tet spell). Some findings on a physical exam may make the health care provider think a baby may have tetralogy of Fallot, including bluish-looking skin or a heart murmur (a “whooshing” sound caused by blood not flowing properly through the heart). However, it is not uncommon for a heart murmur to be absent right at birth.
The health care provider can request one or more tests to confirm the diagnosis. The most common test is an echocardiogram. An echocardiogram is an ultrasound of the heart that can show problems with the structure of the heart and how the heart is working (or not) with this defect. Echocardiography also is useful for helping the doctor follow the child’s health over time.
Tetralogy of Fallot is a critical congenital heart defect that may be detected with newborn screening using pulse oximetry (also known as pulse ox). Pulse oximetry is a simple bedside test to estimate the amount of oxygen in a baby’s blood. Low levels of oxygen in the blood can be a sign of a critical congenital heart defect. Newborn screening using pulse oximetry can identify some infants with a critical congenital heart defect, like pulmonary atresia, before they show any symptoms.
Treatments of Tetralogy of Fallot
Tetralogy of Fallot can be treated by surgery soon after the baby is born. During surgery, doctors widen or replace the pulmonary valve and enlarge the passage to the pulmonary artery. They also will place a patch over the ventricular septal defect to close the hole between the two lower chambers of the heart. These actions will improve blood flow to the lungs and the rest of the body.
Most infants will live active, healthy lives after surgery. However, they will need regular follow-up visits with a cardiologist (a heart doctor) to monitor their progress and check for other health conditions that might develop as they get older. As adults, they may need more surgery or medical care for other possible problems.
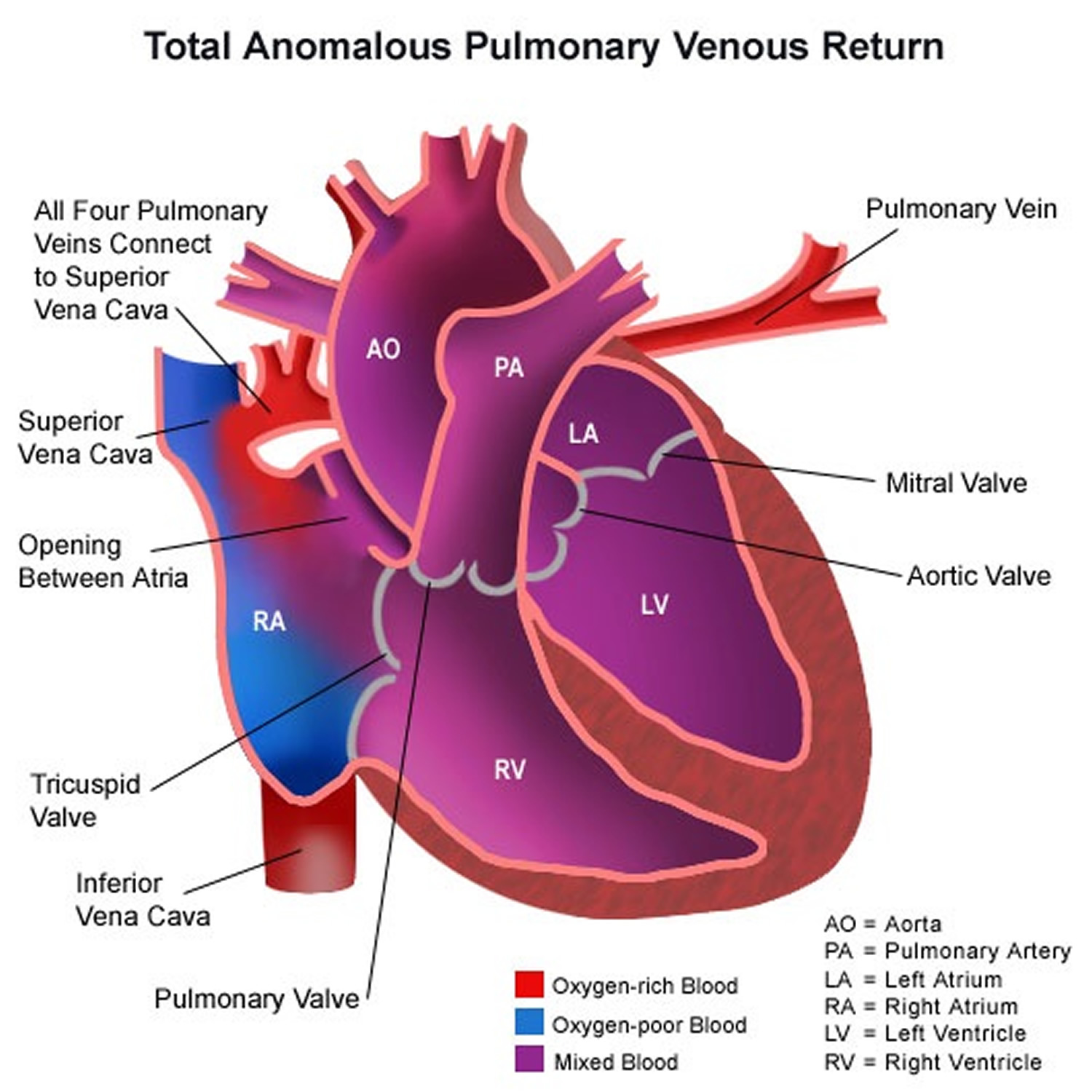
Total Anomalous Pulmonary Venous Return
Total anomalous pulmonary venous return is a birth defect of the heart. In a baby with total anomalous pulmonary venous return, oxygen-rich blood does not return from the lungs to the left atrium 24. Instead, the oxygen-rich blood returns to the right side of the heart. Here, oxygen-rich blood mixes with oxygen-poor blood. This causes the baby to get less oxygen than is needed to the body. To survive with this defect, babies with total anomalous pulmonary venous return usually have a hole between the right atrium and the left atrium (an atrial septal defect) that allows the mixed blood to get to the left side of the heart and pumped out to the rest of the body. Some children can have other heart defects along with total anomalous pulmonary venous return, aside from the atrial septal defect. Because a baby with this defect may need surgery or other procedures soon after birth, total anomalous pulmonary venous return is considered a critical congenital heart defect. Congenital means present at birth. In a related defect, partial anomalous pulmonary venous return, not all of the veins have an abnormal connection. There are some abnormal connections, but one or more of the veins return normally to the left atrium. Therefore, partial anomalous pulmonary venous return is not as critical as total anomalous pulmonary venous return.
In a baby without a congenital heart defect, the right side of the heart pumps oxygen-poor blood from the heart to the lungs through the pulmonary artery. The blood that comes back from the lungs is oxygen-rich, and it moves through the pulmonary veins to the left atrium. The left side of the heart pumps oxygen-rich blood to the rest of the body through the aorta.
Types of Total Anomalous Pulmonary Venous Return
There are different types of Total Anomalous Pulmonary Venous Return, based on where the pulmonary veins connect:
- Supracardiac– In supracardiac total anomalous pulmonary venous return, the pulmonary veins come together and form an abnormal connection above the heart to the superior vena cava, which is a main blood vessel that brings oxygen-poor blood from the upper part of the body to the heart. In this type of total anomalous pulmonary venous return, a mixture of oxygen-poor and oxygen-rich blood returns to the right atrium through the superior vena cava.
- Cardiac – In cardiac total anomalous pulmonary venous return, the pulmonary veins meet behind the heart and connect to the right atrium. The coronary sinus, which is a vein that helps bring oxygen-poor blood from the heart muscle back to the heart, helps connect the pulmonary veins to the right atrium in this type of total anomalous pulmonary venous return
- Infracardiac – In infracardiac total anomalous pulmonary venous return, the pulmonary veins come together and form abnormal connections below the heart. A mixture of oxygen-poor blood and oxygen-rich blood returns to the right atrium from the veins of the liver and the inferior vena cava, which is the main blood vessel that brings oxygen-poor blood from the lower part of the body to the heart.
Figure 14. Total Anomalous Pulmonary Venous Return
Occurrence of total anomalous pulmonary venous return
In a 2013 study, using data from the Metropolitan Atlanta Congenital Defects Program, researchers estimated that, together, total anomalous pulmonary venous return and partial anomalous pulmonary venous return occur in about one out of every 10,000 births 15.
Causes and Risk Factors of total anomalous pulmonary venous return
The causes of heart defects, such as total anomalous pulmonary venous return, among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. Heart defects also are thought to be caused by a combination of genes and other risk factors, such as the things the mother or fetus come in contact with in the environment or what the mother eats or drinks or the medicines she uses.
Diagnosis of total anomalous pulmonary venous return
Total anomalous pulmonary venous return and partial anomalous pulmonary venous return might be diagnosed during pregnancy, but more often these defects are diagnosed soon after a baby is born.
During Pregnancy
During pregnancy, there are screening tests (also called prenatal tests) to check for birth defects and other conditions. Total anomalous pulmonary venous return might be diagnosed during pregnancy with an ultrasound (which creates pictures of the body). Some findings from the ultrasound may make the health care provider suspect a baby could have total anomalous pulmonary venous return. If so, the health care provider can request a fetal echocardiogram to confirm the diagnosis. A fetal echocardiogram is an ultrasound specifically of the baby’s heart and major blood vessels that is performed during the pregnancy. This test can show problems with the structure of the heart and how well the heart is working. However, total anomalous pulmonary venous return defect is not commonly detected during pregnancy. It is hard for doctors to see the pulmonary veins on the prenatal screening tests since not much blood goes to the lungs before the baby is born. It is easier to detect this defect after birth when the blood is flowing to the lungs and returning to the heart.
After a Baby is Born
Symptoms usually occur at birth or very soon afterwards. Infants with total anomalous pulmonary venous return can have a bluish looking skin color, called cyanosis, because their blood doesn’t carry enough oxygen. Infants with total anomalous pulmonary venous return or other conditions causing cyanosis can have symptoms such as:
- Problems breathing
- Pounding heart
- Weak pulse
- Ashen or bluish skin color
- Poor feeding
- Extreme sleepiness
Using a stethoscope, a doctor will often hear a heart murmur (an abnormal “whooshing” sound caused by blood flowing through the atrial septal defect). However, it is not uncommon for a heart murmur to be absent right at birth.
If a doctor suspects that there might be a problem, the doctor can request one or more tests to confirm the diagnosis of total anomalous pulmonary venous return. The most common test is an echocardiogram. This is an ultrasound of the heart that can show problems with the structure of the heart, like holes in the walls between the chambers, and any irregular blood flow. Cardiac catheterization also can confirm the diagnosis by showing that the blood vessels are abnormally attached. An electrocardiogram (EKG), which measures the electrical activity of the heart, chest x-rays, and other medical tests may also be used to make the diagnosis.
Total anomalous pulmonary venous return is a critical congenital heart defect that also can be detected with newborn pulse oximetry screening. Pulse oximetry is a simple bedside test to determine the amount of oxygen in a baby’s blood. Low levels of oxygen in the blood can be a sign of a critical congenital heart defect. Newborn screening using pulse oximetry can identify some infants with a critical congenital heart defect, like total anomalous pulmonary venous return, before they show any symptoms.
Treatment of total anomalous pulmonary venous return
Babies with total anomalous pulmonary venous return will need surgery to repair the defect. The age at which the surgery is done depends on how sick the child is and the specific structure of the abnormal connections between the pulmonary veins and the right atrium. The goal of the surgical repair of total anomalous pulmonary venous return is to restore normal blood flow through the heart. To repair this defect, doctors usually connect the pulmonary veins to the left atrium, close off any abnormal connections between blood vessels, and close the atrial septal defect.
Infants whose defects are surgically repaired are not cured; they may have lifelong complications. A child or adult with total anomalous pulmonary venous return will need regular follow-up visits with a cardiologist (a heart doctor) to monitor their progress, avoid complications, and check for other health conditions that might develop as they get older.
Tricuspid Atresia
Tricuspid atresia is a birth defect of the tricuspid valve, which is the valve that controls blood flow from the right atrium (upper right chamber of the heart) to the right ventricle (lower right chamber of the heart). Tricuspid atresia occurs when this valve doesn’t form at all, and no blood can go from the right atrium through the right ventricle to the lungs for oxygen 25. Because a baby with tricuspid atresia may need surgery or other procedures soon after birth, this birth defect is considered a critical congenital heart defect. Congenital means present at birth.
In a baby without a congenital heart defect, the right side of the heart pumps oxygen-poor blood from the heart to the lungs through the main pulmonary artery. The blood that comes back from the lungs is oxygen-rich and can then be pumped to the rest of the body through the aorta. In babies with tricuspid atresia, the tricuspid valve that controls blood flow from the right atrium to the right ventricle is not formed, so blood is unable to get to the right ventricle and out to the lungs. For this reason, the right ventricle can be underdeveloped. The main pulmonary artery may also be small with very little blood going through it to the lungs.
In tricuspid atresia, since blood cannot directly flow from the right atrium to the right ventricle, blood must use other routes to bypass the unformed tricuspid valve. Babies born with tricuspid atresia often also have an atrial septal defect, which is a hole between the right and left atria, or a ventricular septal defect, which is a hole between the right and left ventricles. These defects allow oxygen-rich blood to mix with oxygen-poor blood, so that oxygen-rich blood has a way to get pumped to the rest of the body.
Doctors may give the baby medicine to keep the baby’s patent ductus arteriosus open after the baby’s birth. The patent ductus arteriosus is the blood vessel that allows blood to move around the baby’s lungs before the baby is born, and it usually closes after birth. Keeping this connection open allows blood to get to the lungs for oxygen and bypass the small right side of the heart.
Some babies with tricuspid atresia can also have other heart defects, including transposition of the great arteries. In transposition of the great arteries, the main connections (arteries) from the heart are reversed. The main pulmonary artery, which normally carries oxygen-poor blood from the right side of the heart to the lungs, now arises from the left side and carries oxygen-rich blood returning from the lungs back to the lungs. The aorta, which normally carries blood from the left side of the heart to the body, now arises from the right side and carries oxygen-poor blood back out to the body. When a baby has both tricuspid atresia and transposition of the great arteries, blood is able to get to the lungs because the main pulmonary artery arises from the developed left ventricle. However, blood cannot get out to the body because the aorta arises from the poorly formed right ventricle and is small.
Figure 15. Tricuspid Atresia
Occurrence of Tricuspid Atresia
In a 2012 study using data from birth defects surveillance systems across the United States, researchers estimated that about 1 out of every 10,000 babies is born with tricuspid atresia 26.
Causes and Risk Factors of Tricuspid Atresia
The causes of heart defects, such as tricuspid atresia, among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. Heart defects also are thought to be caused by a combination of genes and other factors, such as the things the mother comes in contact with in the environment, or what the mother eats or drinks, or certain medicines she uses.
Diagnosis of Tricuspid Atresia
Tricuspid atresia may be diagnosed during pregnancy or soon after a baby is born.
During Pregnancy
During pregnancy, there are screening tests (also called prenatal tests) to check for birth defects and other conditions. Tricuspid atresia might be seen during an ultrasound (which creates pictures of the body). Some findings from the ultrasound may make the health care provider suspect that a baby might have tricuspid atresia. If so, the health care provider can request a fetal echocardiogram to confirm the diagnosis. A fetal echocardiogram is an ultrasound specifically of the baby’s heart and major blood vessels that is performed during the pregnancy. This test can show problems with the structure of the heart and how the heart is working with this defect.
After a Baby is Born
Babies born with tricuspid atresia will show symptoms at birth or very soon afterwards. They may have a bluish looking skin color, called cyanosis, because their blood doesn’t carry enough oxygen. Infants with tricuspid atresia can have additional symptoms such as:
- Problems breathing
- Ashen or bluish skin color
- Poor feeding
- Extreme sleepiness
During a physical examination, a doctor can see the symptoms, such as bluish skin or problems breathing. Using a stethoscope, a doctor will check for a heart murmur (an abnormal “whooshing” sound caused by blood not flowing properly), or other sounds that may indicate a heart problem. However, it is not uncommon for a heart murmur to be absent right at birth.
If a doctor suspects that there might be a problem, the doctor can request one or more tests to confirm the diagnosis of tricuspid atresia. The most common test is an echocardiogram. This is an ultrasound of the heart that can show problems with the structure of the heart, like holes in the walls between the chambers, and any irregular blood flow. Cardiac catheterization (inserting a thin tube into a blood vessel and guiding it to the heart) also can confirm the diagnosis by looking at the inside of the heart and measuring the blood pressure and oxygen. An electrocardiogram (EKG), which measures the electrical activity of the heart, and other medical tests may also be used to make the diagnosis.
Tricuspid atresia is a critical congenital heart defect (critical CHD) that also can be detected with newborn screening using pulse oximetry (also known as pulse ox). Pulse oximetry is a simple, painless bedside test to estimate the amount of oxygen in a baby’s blood. The test is done using a machine called a pulse oximeter, with sensors placed on the baby’s skin. Low levels of oxygen in the blood can be a sign of a critical CHD. Newborn screening using pulse oximetry can identify some infants with a critical CHD, like tricuspid atresia, before they show any symptoms.
Treatment for Tricuspid Atresia
Medicines
Some babies and children will need medicines to help strengthen the heart muscle, lower their blood pressure, and help the body get rid of extra fluid.
Nutrition
Some babies with tricuspid atresia become tired while feeding and do not eat enough to gain weight. To make sure babies have a healthy weight gain, a special high-calorie formula might be prescribed. Some babies become extremely tired while feeding and might need to be fed through a feeding tube.
Surgery
Surgical treatment for tricuspid atresia depends on its severity and presence of other heart defects. Soon after a baby with tricuspid atresia is born, one or more surgeries may be needed to increase blood flow to the lungs and bypass the poorly functioning right side of the heart. Other surgeries or procedures may be needed later. These surgeries, described below, do not cure tricuspid atresia, but they help restore heart function. Sometimes medicines are given to help treat symptoms of the defect before or after surgery.
- Septostomy
A septostomy may be done within the first few days or weeks of a baby’s life, and creates or enlarges the atrial septal defect, the hole between the right and left upper chambers (atria). This is done so that more oxygen-poor blood can mix with oxygen-rich blood, so that more oxygen-rich blood can get to the body.
- Banding
If the baby has other heart defects along with tricuspid atresia, sometimes there is too much blood flowing to the lungs and not enough going out to the rest of the body. Too much blood in the lungs can damage them. If this is the problem, surgery may be done within the first few weeks of a baby’s life to place a band around the artery going to the lungs (main pulmonary artery) to control the blood flow to the lungs. This banding is a temporary procedure and will likely be removed.
- Shunt Procedure
This surgery usually is done within the first 2 weeks of a baby’s life. Surgeons create a bypass (shunt) from the aorta to the main pulmonary artery, allowing blood to get to the lungs. If the aorta is small, as occurs when the baby also has transposition of the great arteries, the surgeon will also enlarge the aorta at this time. After this procedure, an infant’s skin still might look bluish because oxygen-rich and oxygen-poor blood still mix in the heart.
- Bi-directional Glenn Procedure
This usually is performed when an infant is 4 to 6 months of age. This procedure creates a direct connection between the main pulmonary artery and the superior vena cava, the vessel returning oxygen-poor blood from the upper part of the body to the heart. This allows blood returning from the body to flow directly to the lungs and bypass the heart.
- Fontan Procedure
This procedure usually is done sometime around 2 years of age. Doctors connect the main pulmonary artery and the inferior vena cava, the vessel returning oxygen-poor blood from the lower part of the body to the heart, allowing the rest of the blood coming back from the body to go to the lungs. Once this procedure is complete, oxygen-rich and oxygen-poor blood no longer mix in the heart and an infant’s skin will no longer look bluish.
Infants who have these surgeries are not cured; they might have lifelong complications. If the tricuspid atresia is very complex, or the heart becomes weak after the surgeries, a heart transplant might be needed. An infant or child who receives a heart transplant will need to take medicines for the rest of his or her life to prevent the body from rejecting the new heart.
Babies born with tricuspid atresia will need regular follow-up visits with a cardiologist (a heart doctor) to monitor their progress and check for other health conditions that might develop as they get older. As adults, they may need more surgery or medical care for other possible problems.
Truncus Arteriosus
Truncus arteriosus is a birth defect of the heart. It occurs when the blood vessel coming out of the heart in the developing baby fails to separate completely during development, leaving a connection between the aorta and pulmonary artery 27. There are several different types of truncus, depending on how the arteries remain connected. There is also usually a hole between the bottom two chambers of the heart (ventricles) called a ventricular septal defect. Because a baby with this defect may need surgery or other procedures soon after birth, truncus arteriosus is considered a congenital heart defect.
In a baby without a congenital heart defect, the right side of the heart pumps oxygen-poor blood through the pulmonary artery to the lungs. The left side of the heart pumps oxygen-rich blood through the aorta to the rest of the body.
In babies with a truncus arteriosus, oxygen-poor blood and oxygen-rich blood are mixed together as blood flows to the lungs and the rest of the body. As a result, too much blood goes to the lungs and the heart works harder to pump blood to the rest of the body. Also, instead of having both an aortic valve and a pulmonary valve, babies with truncus arteriosus have a single common valve (truncal valve) controlling blood flow out of the heart. The truncal valve is often abnormal. The valve can be thickened and narrowed, which can block the blood as it leaves the heart. It can also leak, causing blood that leaves the heart to leak back into the heart across the valve.
Figure 16. Truncus Arteriosus
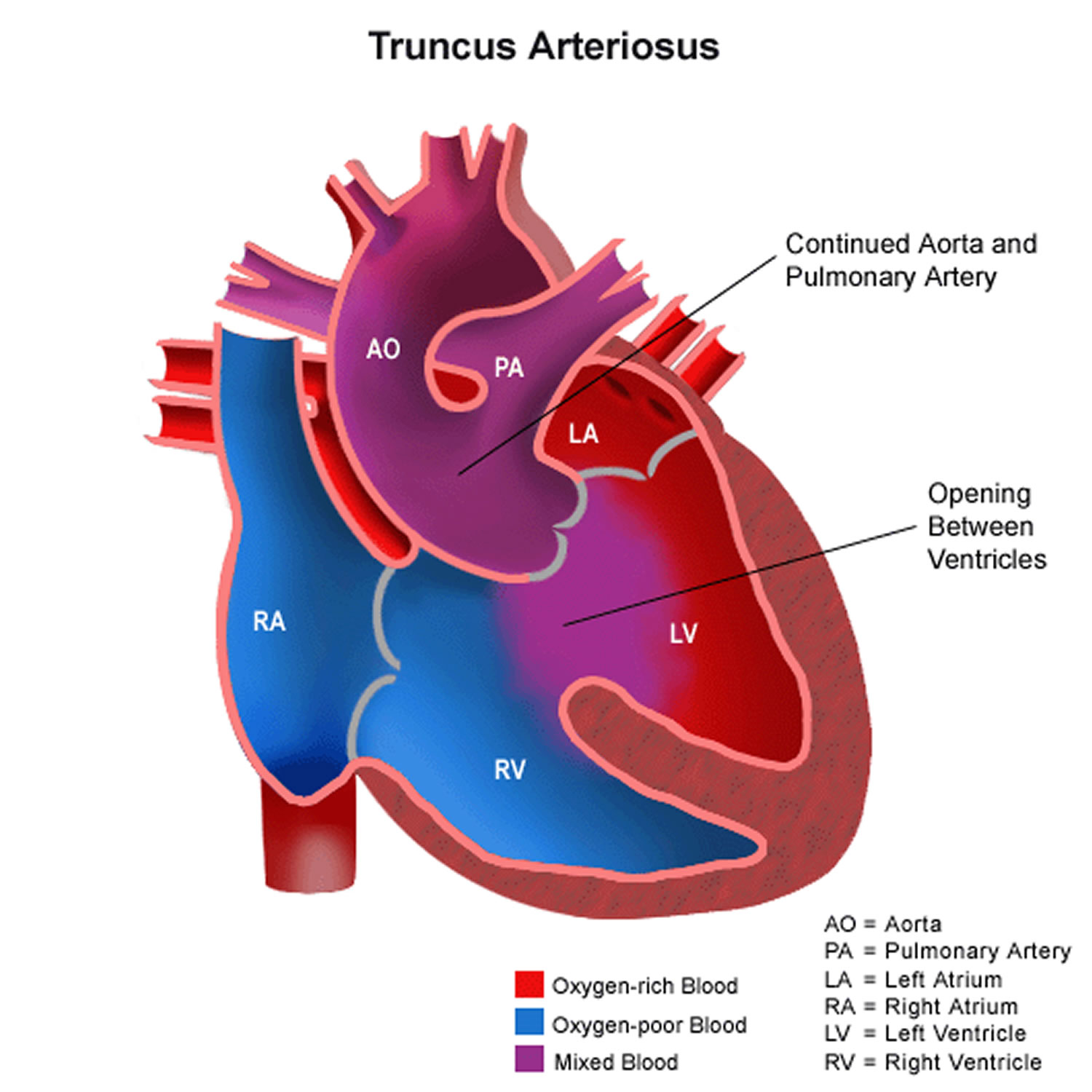
Occurrence of Truncus Arteriosus
Truncus arteriosus occurs in less than one out of every 10,000 live births. It can occur by itself or as part of certain genetic disorders. There are about 300 cases of truncus arteriosus per year in the United States 23.
Causes and Risk Factors of Truncus Arteriosus
The causes of heart defects, such as truncus arteriosus, among most babies are unknown. Some babies have congenital heart defects because of changes in their genes or chromosomes. Congenital heart defects are also thought to be caused by the combination of genes and other risk factors such as things the mother comes in contact with in her environment, or what the mother eats or drinks, or certain medications she uses.
Diagnosis of Truncus Arteriosus
Truncus arteriosus may be diagnosed during pregnancy or soon after the baby is born.
During Pregnancy
During pregnancy, there are screening tests (also called prenatal tests) to check for birth defects and other conditions. Some heart defects might be seen during an ultrasound (which creates pictures of the body). If a health care provider suspect a baby might have truncus arteriosus, the health care provider can request a fetal echocardiogram to confirm the diagnosis. A fetal echocardiogram is a more detailed ultrasound of the baby’s heart. This test can show problems with the structure of the heart, like a single large vessel coming from the heart, and how the heart is working with this defect.
After a Baby is Born
Infants with truncus arteriosus usually are in distress in the first few days of life because of the high amount of blood going to the lungs which makes the heart work harder. Infants with truncus arteriosus can have a bluish looking skin color, called cyanosis, because their blood doesn’t carry enough oxygen. Infants with truncus arteriosus or other conditions causing cyanosis can have symptoms such as:
- Problems breathing
- Pounding heart
- Weak pulse
- Ashen or bluish skin color
- Poor feeding
- Extreme sleepiness
If a health care provider suspects a baby might have truncus arteriosus, the health care provider can request an echocardiogram to confirm the diagnosis. An echocardiogram is an ultrasound of the heart that can show problems with the structure of the heart, like the single large vessel coming from the heart or misshapen truncal valve. It can also show how the heart is working (or not) with this defect, like if the blood is leaking back into the heart or if it is moving through a hole between the ventricles. Echocardiograms are also useful for helping the doctor follow the child’s health over time.
Truncus arteriosus is a that also can be detected with newborn pulse oximetry screening. Pulse oximetry is a simple bedside test to determine the amount of oxygen in a baby’s blood. Low levels of oxygen in the blood can be a sign of a critical congenital heart disease. Newborn screening using pulse oximetry can identify some infants with a critical congenital heart disease, like truncus arteriosus, before they show any symptoms.
Treatment of Truncus Arteriosus
Medications
Some babies with truncus arteriosus also will need medicines to help strengthen the heart muscle, lower their blood pressure, and help their body get rid of extra fluid.
Nutrition
Some babies with truncus arteriosus might become tired while feeding and might not eat enough to gain weight. To make sure babies have a healthy weight gain, a special high-calorie formula might be prescribed. Some babies become extremely tired while feeding and might need to be fed through a feeding tube.
Surgery
Surgery is needed to repair the heart and blood vessels. This is usually done in the first few months of life. Options for repair depend on how sick the child is and the specific structure of the defect. The goal of the surgery to repair truncus arteriosus is to create a separate flow of oxygen-poor blood to the lungs and oxygen-rich blood to the body. Usually, surgery to repair this defect involves the following steps:
- Close the hole between the bottom chambers of the heart (ventricular septal defect) usually with a patch.
- Use the original single blood vessel to create a new aorta to carry oxygen-rich blood from the left ventricle out to the body.
- Use an artificial tube (conduit) with an artificial valve to connect the right ventricle to the arteries going to the lungs in order to carry oxygen-poor blood to the lungs.
Most babies with truncus arteriosus survive the surgical repair, but may need more surgery or other procedures as they get older. For example, the artificial tube doesn’t grow, so it will need to be replaced as the child grows. There also may be blockages to blood flow which may need to be relieved, or problems with the truncal valve. Thus, a person born with truncus arteriosus will need regular follow-up visits with a cardiologist (a heart doctor) to monitor their progress and avoid complications or other health problems.
Cyanotic congenital heart disease
Cyanotic heart disease refers to a group of many different heart defects that are present at birth (congenital). They result in a low blood oxygen level 28. Cyanosis refers to a bluish color of the skin and mucous membranes.
Normally, blood returns from the body and flows through the heart and lungs.
- Blood that is low in oxygen (blue blood) returns from the body to the right side of the heart.
- The right side of the heart then pumps the blood to the lungs, where it picks up more oxygen and becomes red.
- The oxygen-rich blood returns from the lungs to the left side of the heart. From there, it is pumped to the rest of the body.
Heart defects that children are born with can change the way blood flows through the heart and lungs. This causes non-oxygenated blood to be pumped out to the body without going through the lungs to pick up oxygen. As a result:
- The blood that is pumped out to the body is lower in oxygen.
- Less oxygen delivered to the body can make the skin look blue (cyanosis).
Many of these heart defects involve the heart valves. Heart valves are found between the heart and the large blood vessels that bring blood to and from the heart. These valves open up enough for blood to flow through. Then they close, keeping blood from flowing backward.
Heart valve defects that can cause cyanosis include:
- Tricuspid valve (the valve between the 2 chambers on the right side of the heart) may be absent or unable to open wide enough.
- Pulmonary valve (the valve between the heart and the lungs) may be absent or unable to open wide enough.
- Aortic valve (the valve between the heart and the blood vessel to the rest of the body) is unable to open wide enough.
Other heart defects that may cause cyanosis include:
- Coarctation of the aorta
- Double outlet right ventricle
- Ebstein anomaly
- Hypoplastic left heart syndrome
- Interrupted aortic arch
- Pulmonary atresia
- Single ventricle
- Tetralogy of Fallot
- Total anomalous pulmonary venous return
- d-Transposition of the great arteries
- Tricuspid artresia
- Truncus ateriosus
- Other critical congenital heart defects requiring treatment in the first year of life.
About 1 in every 4 babies born with a heart defect has a critical congenital heart defect (also known as critical congenital heart disease) 3. Babies with a critical congenital heart defect need surgery or other procedures in the first year of life 29.
In the United States, about 7,200 babies born every year have critical congenital heart defects 30. Typically, these types of heart defects lead to low levels of oxygen in a newborn and may be identified using pulse oximetry screening at least 24 hours after birth. Some babies with a critical congenital heart defect need surgery or other procedures in the first year of life. Other heart defects can be just as severe as critical congenital heart defects and may also require treatment soon after birth.
Double outlet right ventricle
This anomaly is associated with a very wide spectrum of anatomy and physiology depending on the size and location of the ventricular septal defect (VSD), as well as the presence and degree of pulmonic stenosis 31. In the most common variety with a subaortic VSD, a complete repair is possible with closure of the VSD in such a way as to direct left ventricular outflow to the aorta.
Ebstein anomaly
Ebstein’s anomaly is a rare heart defect where the valve on the right side of the heart (the tricuspid valve), which separates the right atrium from the right ventricle, doesn’t develop properly 32. The abnormality causes the tricuspid valve to leak blood backwards into the right atrium. This means blood can flow the wrong way within the heart, and the right ventricle may be smaller and less effective than normal. The backup of blood flow can lead to heart swelling and fluid buildup in the lungs or liver. Sometimes, not enough blood gets out of the heart into the lungs and the person may appear blue. The condition is congenital, which means it is present at birth. Symptoms range from mild to very severe. Treatment depends on the severity of the defect and may include medications, oxygen therapy, or surgery.
Ebstein’s anomaly can occur on its own, but it often occurs with an atrial septal defect, pulmonic stenosis, and Wolff-Parkinson-White syndrome. It’s estimated that Ebstein’s anomaly accounts for less than 1% of congenital heart disease cases.
The tricuspid valve is normally made of three parts, called leaflets or flaps. The leaflets open to allow blood to move from the right atrium (top chamber) to the right ventricle (bottom chamber) while the heart relaxes. They close to prevent blood from moving from the right ventricle to the right atrium while the heart pumps.
In persons with Ebstein anomaly, the leaflets are placed deep in the right ventricle instead of the normal position. The leaflets are often larger than normal. The defect most often causes the valve to work poorly, and blood may go the wrong way. Instead of flowing out to the lungs, the blood flows back into the right atrium. The backup of blood flow can lead to heart enlargement and fluid buildup in the body. There may be narrowing of the valve that leads to the lungs (pulmonary valve).
In many cases, patients also have a hole in the wall separating the heart’s two upper chambers (atrial septal defect) and blood flow across this hole may cause oxygen-poor blood to go to the body. This can cause cyanosis, a blue tint to the skin caused by oxygen-poor blood.
Ebstein anomaly occurs as a baby develops in the womb. The exact cause is unknown. The use of certain drugs (such as lithium or benzodiazepines) during pregnancy may play a role. The condition is rare. It is more common in white people.
There is a remarkably wide spectrum of presentation, ranging from severely cyanotic newborns to cardiomegaly with mild cyanosis in childhood to a previously asymptomatic adult presenting with atrial arrhythmias or reentry supraventricular tachycardia. The onset of symptoms depends on the degree of tricuspid valve anatomic and functional derangement and presence of accessory pathways (e.g, Wolff-Parkinson-White syndrome). When symptoms result from a severely dysfunctional tricuspid valve, surgical repair should be considered.
Single ventricle spectrum
These anomalies include any complex lesion with only one functional ventricle and include hypoplastic right ventricle (RV) and left ventricle (LV) and, less commonly, a true undifferentiated single ventricular chamber 31. Surgical management involves ensuring adequate pulmonary blood flow via a systemic-to-pulmonary artery anastomosis (eg, modified Blalock-Taussig shunt [see Tetralogy of Fallot : Definitive management]) for patients with decreased pulmonary blood flow or protecting the pulmonary vascular bed via pulmonary artery banding if pulmonary overcirculation exists. Later, the Fontan procedure (see Tricuspid Atresia : Treatment) can be used as definitive treatment to make the functioning single ventricle solely a systemic ventricle.
Symptoms of cyanotic congenital heart disease
Some heart defects cause major problems right after birth.
The main symptom is cyanosis. This is a bluish color of the lips, fingers, and toes that is caused by the low oxygen content in the blood. It may occur while the child is resting or only when the child is active.
Some children have breathing problems (dyspnea). They may get into a squatting position after physical activity to relieve breathlessness.
Others have spells, in which their bodies are suddenly starved of oxygen. During these spells, symptoms may include:
- Anxiety
- Breathing too quickly (hyperventilation)
- Sudden increase in bluish color to the skin
Infants may get tired or sweat while feeding and may not gain as much weight as they should.
Fainting (syncope) and chest pain may occur.
Other symptoms depend on the type of cyanotic heart disease, and may include:
- Feeding problems or reduced appetite, leading to poor growth
- Grayish skin
- Puffy eyes or face
- Tiredness all the time
Exams and Tests for cyanotic congenital heart disease
Physical examination confirms cyanosis. Older children may have clubbed fingers.
The doctor will listen to the heart and lungs with a stethoscope. Abnormal heart sounds, a heart murmur, and lung crackles may be heard.
Tests will vary depending on the cause, but may include:
- Chest x-ray
- Checking oxygen level in the blood using an arterial blood gas test or by checking it through the skin with a pulse oximeter
- Complete blood count (CBC)
- ECG (electrocardiogram)
- Looking at the heart structure and blood vessels using echocardiogram or MRI of the heart
- Passing a thin flexible tube (catheter) into the right or left side of the heart, usually from the groin (cardiac catheterization)
- Transcutaneous oxygen monitor (pulse oximeter)
- Echo-Doppler
- Testing the heart’s electrical system
Treatment for cyanotic congenital heart disease
Some infants may need to stay in the hospital after birth so they can receive oxygen or be put on a breathing machine. They may receive medicines to:
- Get rid of extra fluids
- Help the heart pump harder
- Keep certain blood vessels open
- Treat abnormal heartbeats or rhythms
The treatment of choice for most congenital heart diseases is surgery to repair the defect. There are many types of surgery, depending on the kind of birth defect. Surgery may be needed soon after birth, or it may be delayed for months or even years.
Your child may need to take water pills (diuretics) and other heart medicines before or after surgery. Be sure to follow the correct dosage. Regular follow-up with the doctor is important.
Many children who have had heart surgery must take antibiotics before, and sometimes after having any dental work or other medical procedures. Make sure you have clear instructions from your child’s heart doctor.
Ask your child’s doctor before getting any immunizations. Most children can follow the recommended guidelines for childhood vaccinations.
Outlook (Prognosis) for cyanotic congenital heart disease
The outlook depends on the specific disorder.
Possible Complications for cyanotic heart disease
Complications of cyanotic heart disease include:
- Abnormal heart rhythms and sudden death
- Chronic high blood pressure in the blood vessels of the lung
- Heart failure
- Infection in the heart
- Stroke
Prevention of cyanotic congenital heart disease
Women who are pregnant should get good prenatal care.
- Avoid using alcohol and drugs during pregnancy.
- Tell your doctor that you are pregnant before taking any prescribed medicines.
- Get a blood test early in the pregnancy to see if you are immune to rubella. If you are not immune, you must avoid any exposure to rubella and should get immunized right after delivery.
- Pregnant women with diabetes should try to get good control over their blood sugar level.
Some inherited factors may play a role in congenital heart disease. Many family members may be affected. If you are planning to get pregnant, talk to your doctor about screening for genetic diseases.
- National Institutes of Health. National Heart, Lung and Blood Institute. Congenital Heart Defects. https://www.nhlbi.nih.gov/health/health-topics/topics/chd/[↩][↩][↩][↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Congenital Heart Defects (CHDs). https://www.cdc.gov/ncbddd/heartdefects/index.html[↩][↩][↩][↩][↩]
- Oster M, Lee K, Honein M, Colarusso T, Shin M, Correa A. Temporal trends in survival for infants with critical congenital heart defects. Pediatrics. 2013;131(5):e1502-8.[↩][↩][↩]
- American Heart Association. About Arrhythmia. http://www.heart.org/HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/About-Arrhythmia_UCM_002010_Article.jsp[↩]
- Jenkins KJ, Correa A, Feinstein JA, Botto L, Britt AE, Daniels SR, Elixson M, Warnes CA, Webb CL. Noninherited risk factors and congenital cardiovascular defects: current knowledge: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young: endorsed by the American Academy of Pediatrics. Circulation. 2007;115(23):2995-3014.[↩][↩]
- Patel SS, Burns TL. Nongenetic risk factors and congenital heart defects. Pediatr Cardiol. 2013;34(7):1535-55.[↩][↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Facts about Atrial Septal Defect. https://www.cdc.gov/ncbddd/heartdefects/atrialseptaldefect.html[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Types of Congenital Heart Defects. https://www.nhlbi.nih.gov/health/health-topics/topics/chd/types[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, et al; for the National Birth Defects Prevention Network. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol. 2010;88(12):1008-16.[↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Facts about Ventricular Septal Defect. https://www.cdc.gov/ncbddd/heartdefects/ventricularseptaldefect.html[↩][↩][↩]
- Reller MD, Strickland MJ, Riehle-Colarusso T, Mahle WT, Correa A. Prevalence of Congenital Heart Defects in Metropolitan Atlanta, 1998-2005. J Pediatr. 2008;153:807-13.[↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Facts about Atrioventricular Septal Defect (AVSD). https://www.cdc.gov/ncbddd/heartdefects/avsd.html[↩][↩][↩][↩][↩]
- Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, Anderson P, Mason CA, Collins JS, Kirby RS, & Correa A, for the National Birth Defects Prevention Network. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol 2010;88:1008-1016.[↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Facts about Coarctation of the Aorta. https://www.cdc.gov/ncbddd/heartdefects/coarctationofaorta.html[↩][↩][↩][↩][↩][↩]
- Bjornard, K., Riehle-Colarusso, T., Gilboa, S. M. and Correa, A. Patterns in the prevalence of congenital heart defects, metropolitan Atlanta, 1978 to 2005. Birth Defects Res Part A: Clin Mol Teratol. 2013;97:87–94.[↩][↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Facts about dextro-Transposition of the Great Arteries (d-TGA). https://www.cdc.gov/ncbddd/heartdefects/d-tga.html[↩]
- Parker SE, Mai CT, Canfield MA, et al. for the National Birth Defects Prevention Network. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol 2010;88:1008-1016.[↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Facts about Hypoplastic Left Heart Syndrome. https://www.cdc.gov/ncbddd/heartdefects/hlhs.html[↩]
- Parker SE, Mai CT, Canfield MA, et al; for the National Birth Defects Prevention Network. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol. 2010;88:1008-16. [↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Facts about Pulmonary Atresia. https://www.cdc.gov/ncbddd/heartdefects/pulmonaryatresia.html[↩]
- Mai CT, Riehle-Colarusso T, O’Halloran A, Cragan JD, Olney RS, Lin A, Feldkamp M, Botto LD, Rickard R, Anderka M, Ethen M, Stanton C, Ehrhardt J, Canfield M; National Birth Defects Prevention Network. Selected Birth Defects Data from Population-based Birth Defects Surveillance Programs in the United States, 2005-2009: Featuring Critical Congenital Heart Defects Targeted for Pulse Oximetry Screening. Birth Defects Research Part A: Clinical and Molecular Teratology. 2012;94: 970-983.[↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Facts about Tetralogy of Fallot. https://www.cdc.gov/ncbddd/heartdefects/tetralogyoffallot.html[↩]
- Parker SE, Mai CT, Canfield MA, et al; for the National Birth Defects Prevention Network. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol. 2010;88:1008-16.[↩][↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Facts about Total Anomalous Pulmonary Venous Return or TAPVR. https://www.cdc.gov/ncbddd/heartdefects/tapvr.html[↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Facts about Tricuspid Atresia. https://www.cdc.gov/ncbddd/heartdefects/tricuspid-atresia.html[↩]
- Mai CT, Riehle-Colarusso T, O’Halloran A, Cragan JD, et al. Selected Birth Defects Data from Population-based Birth Defects Surveillance Programs in the United States, 2005-2009: Featuring Critical Congenital Heart Defects Targeted for Pulse Oximetry Screening. Birth Defects Research Part A: Clinical and Molecular Teratology. 2012;94: 970-983.[↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Facts about Truncus Arteriosus. https://www.cdc.gov/ncbddd/heartdefects/truncusarteriosus.html[↩]
- U.S. National Library of Medicine. Cyanotic heart disease. https://medlineplus.gov/ency/article/001104.htm[↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Facts about Critical Congenital Heart Defects. https://www.cdc.gov/ncbddd/heartdefects/cchd-facts.html[↩]
- Adapted from Reller, MD, Strickland, MJ, Riehle-Colarusso, TJ, Mahle, WT, Correa, A. Prevalence of congenital heart defects in metropolitan Atlanta, 1998-2005. J Pediatr. 2008;153:807-13.[↩]
- Merck Sharp & Dohme Corp. Merck Manual. Congenital Cardiovascular Anomalies. https://www.merckmanuals.com/professional/pediatrics/congenital-cardiovascular-anomalies/other-congenital-cardiac-anomalies[↩][↩]
- Kaneshiro NK, Chen MA. Ebstein’s anomaly. MedlinePlus. https://medlineplus.gov/ency/article/007321.htm[↩]