Contents
What is claudication
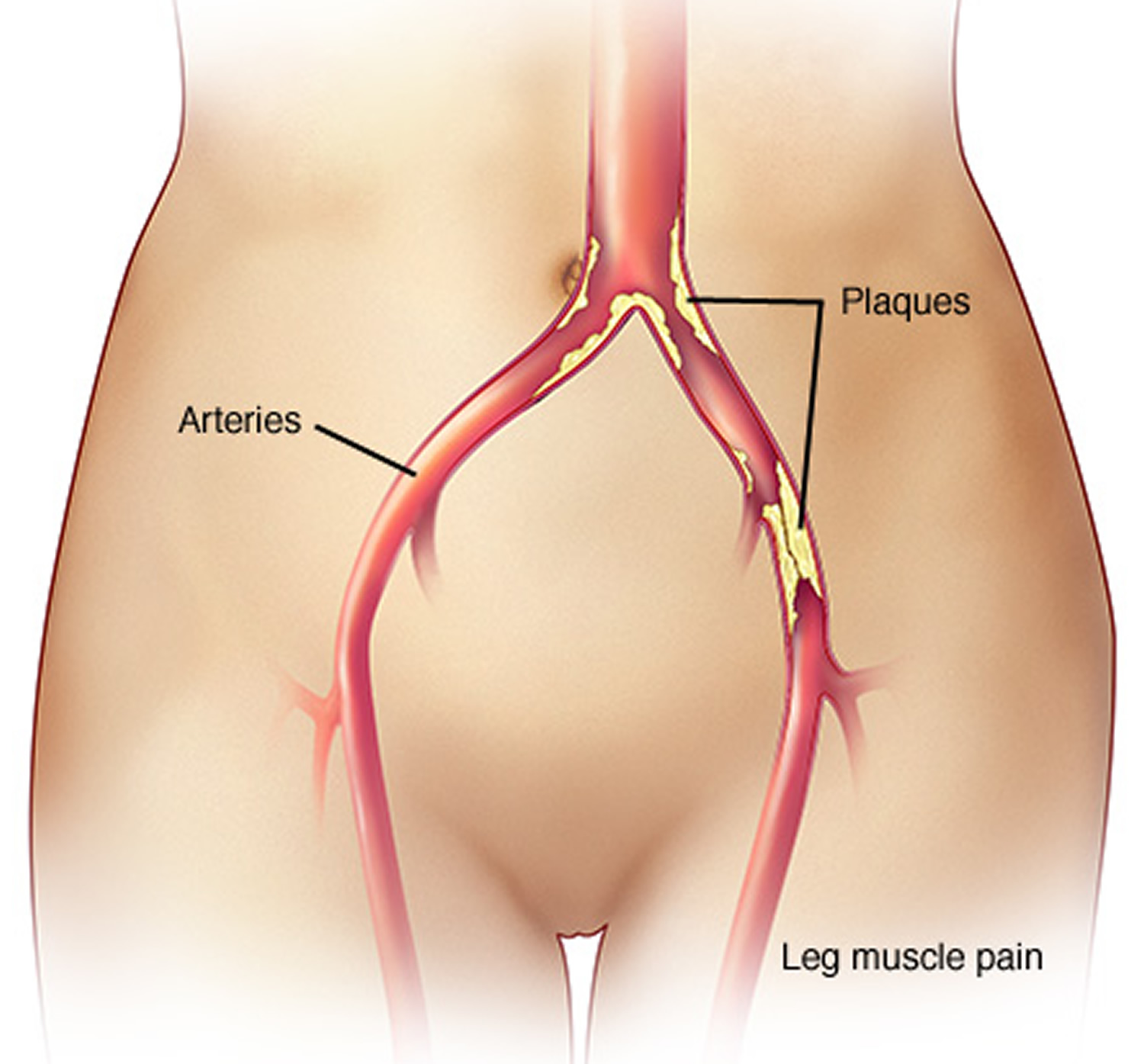
Claudication is a pain, cramp, aching or sense of fatigue in muscles of the buttocks, thigh or calf that occurs with exertion and relieved promptly by a few minutes of rest while standing evenly on both feet 1. Claudication occurs elsewhere in the body, but it is the symptom arising in the legs that has major clinical significance. Claudication is caused by atherosclerosis (poor circulation) of the blood to the lower extremities, a condition commonly known as peripheral artery disease.
Atherosclerosis is the hardening and narrowing of the arteries over time thorough a build-up of plaque. Plaque is made up of fat, cholesterol, calcium, and other substances found in the blood. Over time, plaque hardens and narrows the arteries blocking the flow of blood through them. This limits the flow of oxygen-rich blood to organs and other parts of of the body.
Although it’s sometimes considered a disease, claudication is technically a symptom of a disease. Most often, claudication is a symptom of peripheral artery disease, a potentially serious but treatable circulation problem in which the vessels that supply blood flow to your legs or arms are narrowed.
Twelve percent of the U.S. population or nine million people experience occasional claudication, twenty percent In people over 70. Individuals with intermittent claudication may also have diabetes—often undiagnosed.
In the early stages of peripheral artery disease, patients may experience cramping or fatigue in the legs or buttocks while walking or exercising. This is referred to as “intermittent claudication.” Claudication may occur in one or both legs, depending on where the blockage is. The pain or other symptoms subside when the activity is stopped. Claudication pain can range from mild to disabling. At first, you’ll probably notice claudication pain only when you’re exercising, but as claudication worsens, the pain may affect you even when you’re at rest.
Claudication, if left untreated, can progress to critical limb ischemia, a severe obstruction of blood flow to the extremities, often accompanied by severe pain and/or skin ulcers or sores with the risk of amputation.
Fortunately, with treatment, you may be able to maintain an active lifestyle without pain.
What is atherosclerosis
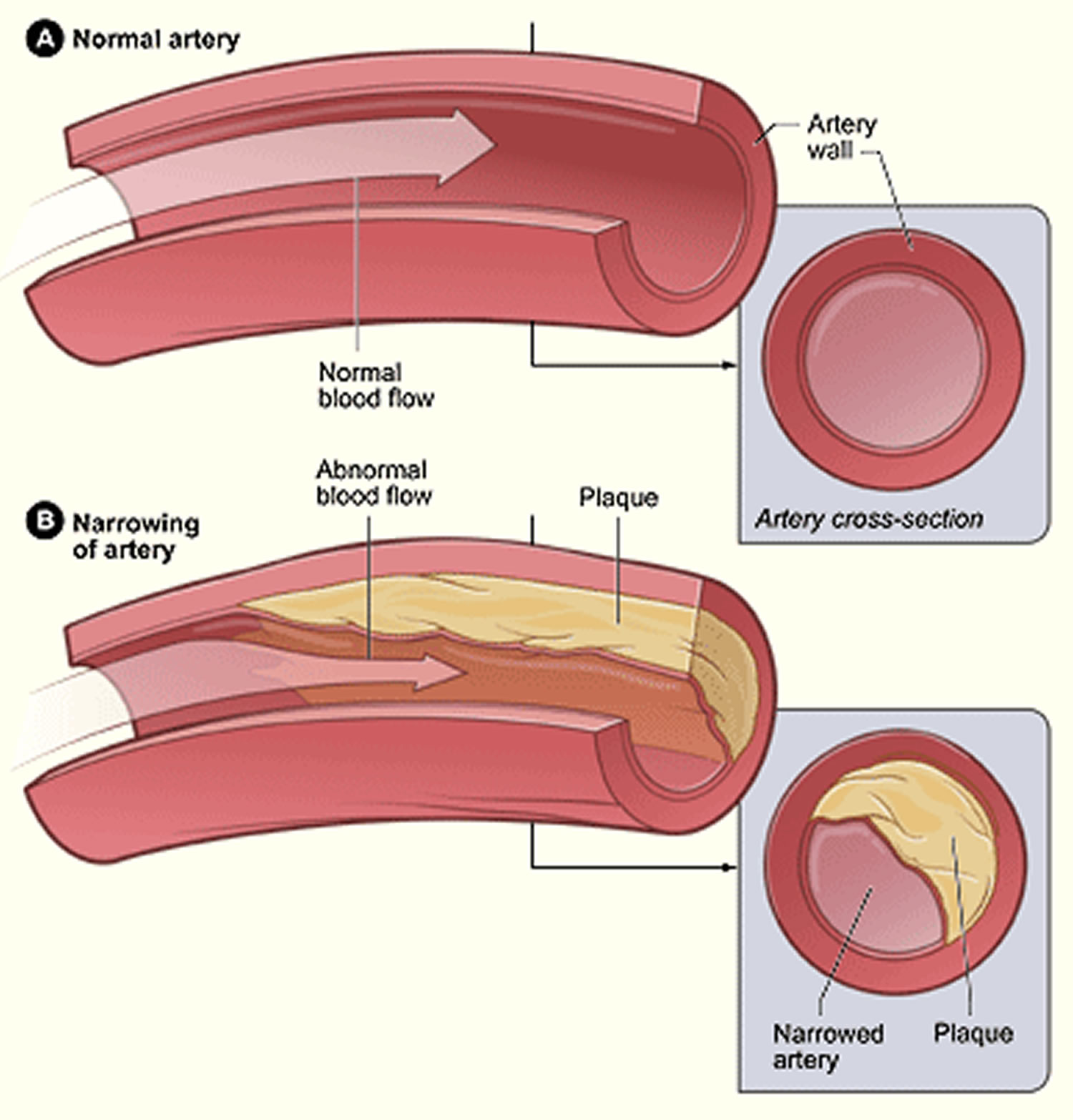
Atherosclerosis (also known as hardening of the arteries or stiffening of the arteries or arteriosclerosis) is a disease in which plaque builds up inside your arteries. Atherosclerosis can lead to serious problems, including heart attack, stroke, or even death. Arteries are blood vessels that carry oxygen-rich blood to your heart and other parts of your body. Atherosclerosis is a disease of the blood vessels (the arteries) that carry blood and oxygen from the heart to the rest of the body. The arteries are normally quite flexible, but over many years, the artery walls gradually lose their elasticity. The walls become hardened and stiff due to the build-up of a substance called plaque that is rich in cholesterol.
Cholesterol is a fatty substance that is made by the body but which is also found in some foods. High levels in the blood of a type of cholesterol (called ‘bad’ cholesterol, or LDL-cholesterol) increases the risk of developing heart disease, including atherosclerosis. Estimates suggest that around a third of the adult Australian population has high levels of cholesterol.
Plaque is made up of fat, bad cholesterol, calcium, white blood cells and other substances found in the blood that slowly and silently builds up inside the walls of the arteries. As the plaque grows over many years, it can begin to interfere with the flow of blood through the artery. This limits the flow of oxygen-rich blood to your organs and other parts of your body. Atherosclerosis can affect arteries anywhere in the body, and these plaques can burst, triggering a blood clot which may lead to a serious medical emergency, such as a heart attack, stroke or even death. In severe cases, the flow of blood can be completely blocked.
The cause of atherosclerosis isn’t known. However, certain traits, conditions, or habits may raise your risk for the disease. These conditions are known as risk factors. For example, the development of plaque is affected by what you eat, your weight, how much physical activity you do, and whether you’re a smoker. It is also affected by your age and gender, and whether you have a history of high cholesterol in your family.
You can control some risk factors, such as lack of physical activity, smoking, and an unhealthy diet. Others you can’t control, such as age and a family history of heart disease.
Some people who have atherosclerosis have no signs or symptoms. They may not be diagnosed until after a heart attack or stroke.
The main treatment for atherosclerosis is lifestyle changes. You also may need medicines and medical procedures. These treatments, along with ongoing medical care, can help you live a healthier life.
Figure 1. Atherosclerosis
There are 3 main stages in the development of atherosclerosis:
Stage 1 – Plaque builds up in an artery (Figure 2)
The inside lining of a healthy artery is normally smooth to make it easy for blood to flow. However, if the inner lining of the artery becomes damaged – for example, due to high cholesterol, high blood pressure or smoking – it allows plaque to start accumulating within the artery wall.
Over time, a tough, fibrous cap or scar forms over the top of the plaque, so that the mixture of ‘bad’ cholesterol, fats (lipids), calcium and white blood cells is kept separate from the blood.
The growth of the plaque can narrow the artery, which reduces the flow of blood through the artery.
Figure 2. Atherosclerosis development stage 1
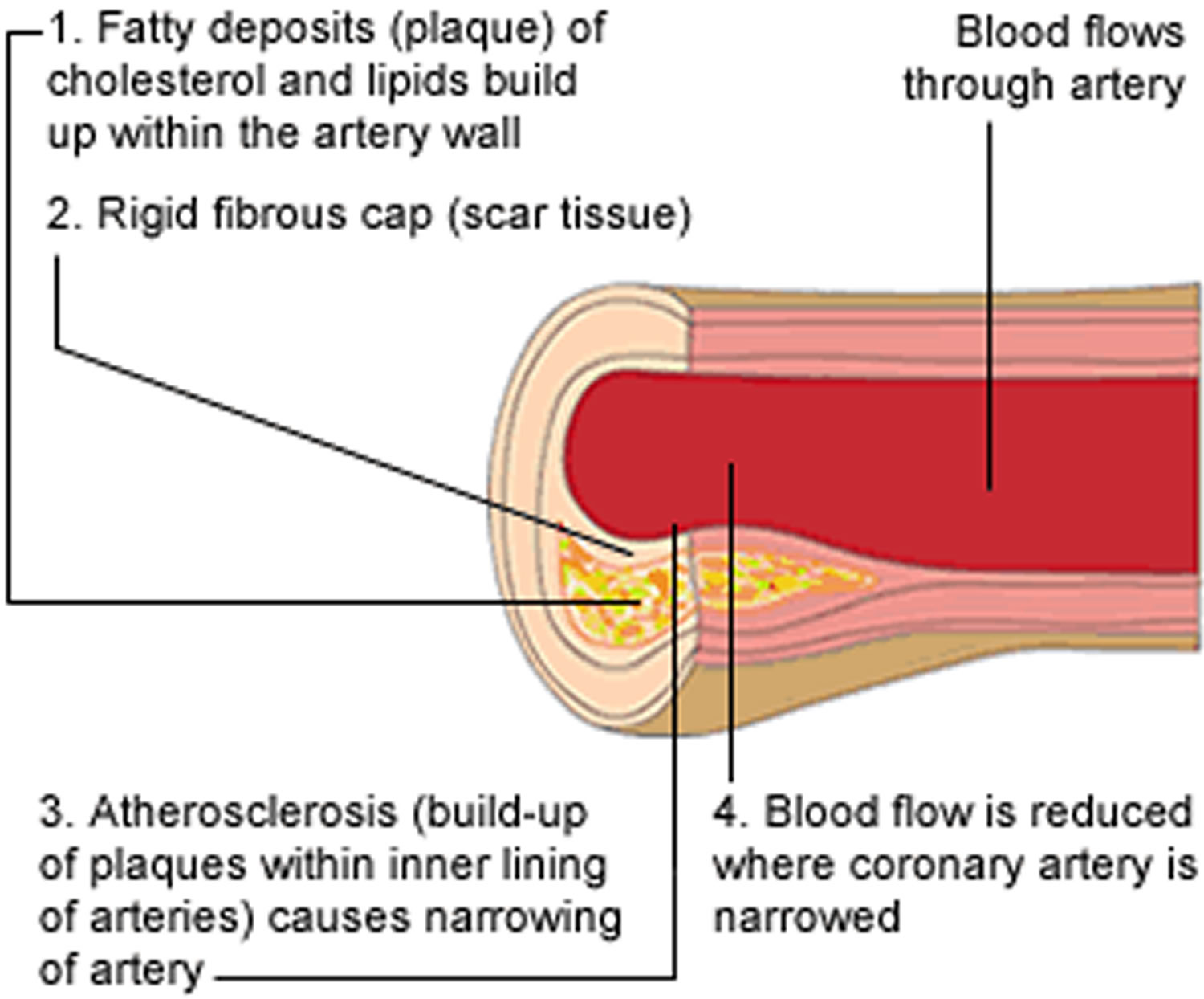
Stage 2 – The plaque gets bigger and becomes unstable (Figure 3)
There are different types of plaque. Some plaques grow slowly and may never cause any symptoms, even if the plaque is large enough to severely restrict blood flow through the artery.
The most dangerous type of plaque is called unstable plaque. In these plaques, the tough fibrous cap on top of the cholesterol-rich plaque becomes thin and weak, which makes it more likely to burst.
Figure 3. Atherosclerosis development stage 2
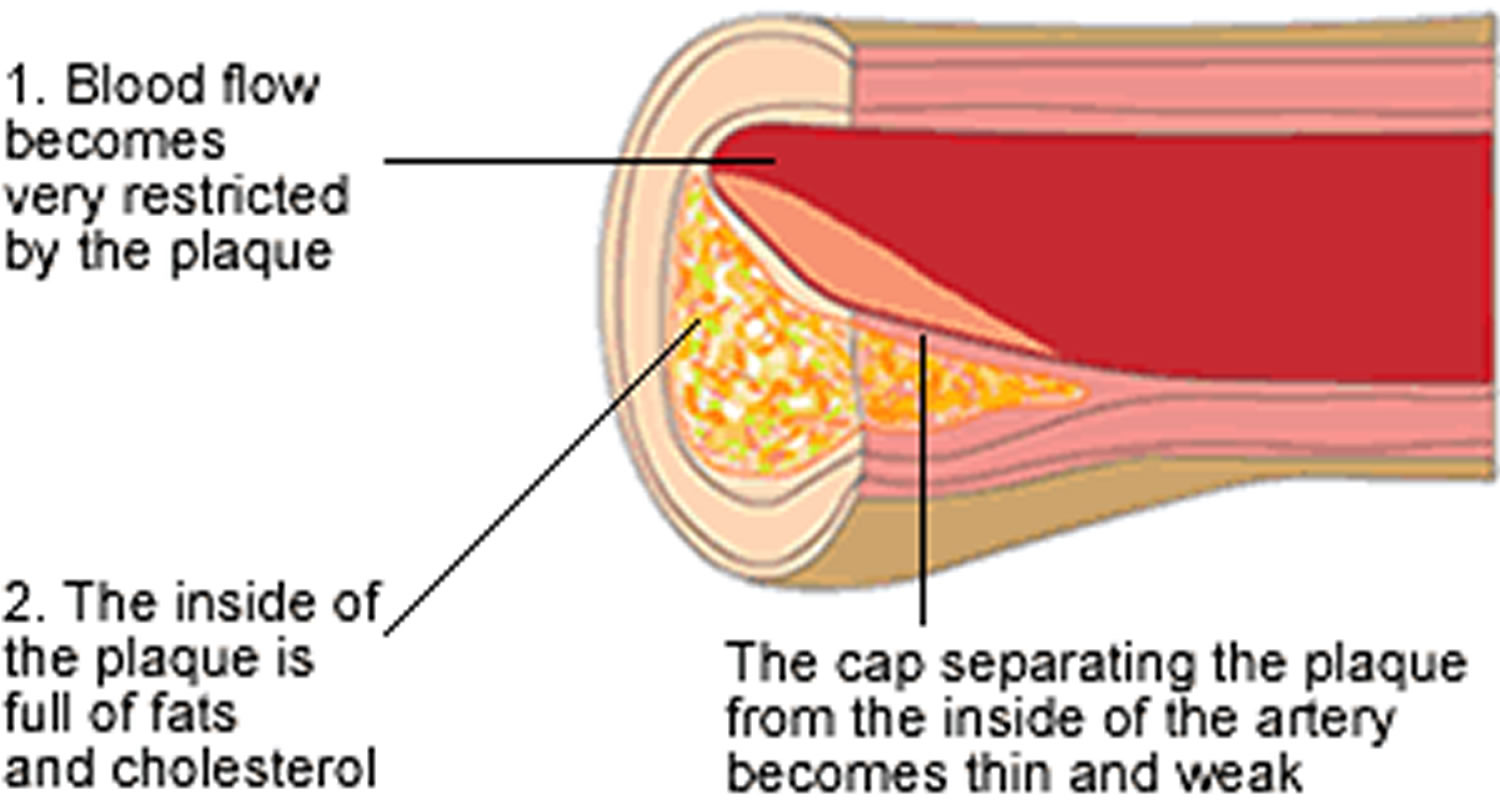
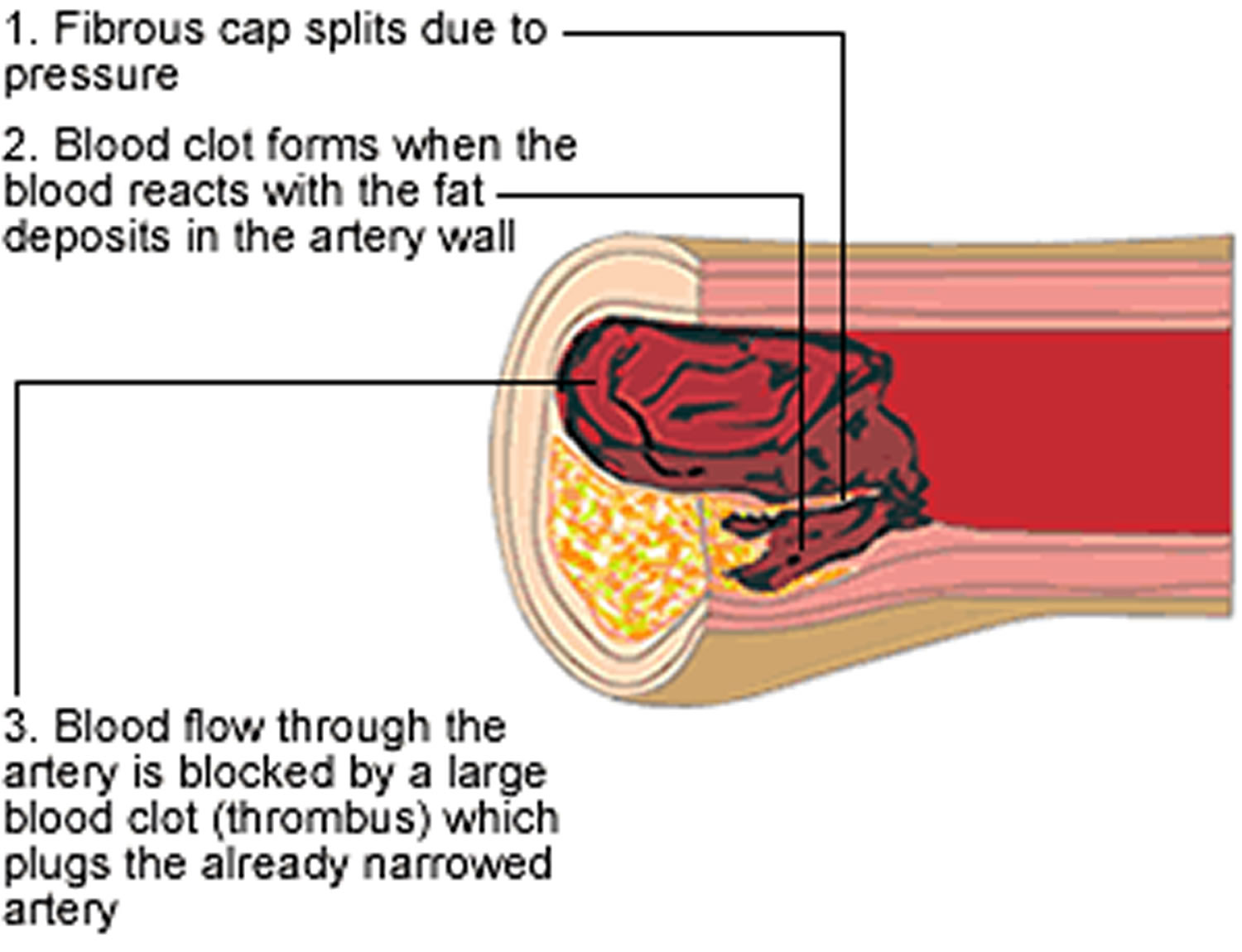
Stage 3 – The plaque bursts and a blood clot blocks the artery (Figure 4)
Narrowing of the artery due to the build-up of plaque makes it harder for blood to flow through the artery. Forcing the blood through a narrower space increases blood pressure in the artery, which can tear open the fibrous cap of the unstable plaque.
As the cap bursts, the contents of the plaque – including cholesterol, fats, and white blood cells – are released into the blood. This can trigger the development of a large blood clot (or thrombus) which can completely block the already narrowed artery.
Depending on where the blockage occurs, the blood clot can cause a medical emergency, such as a heart attack (if an artery supplying the heart becomes blocked) or a stroke (if the blockage affects an artery supplying the brain).
Figure 4. Atherosclerosis development stage 3
 Neurogenic claudication
Neurogenic claudication
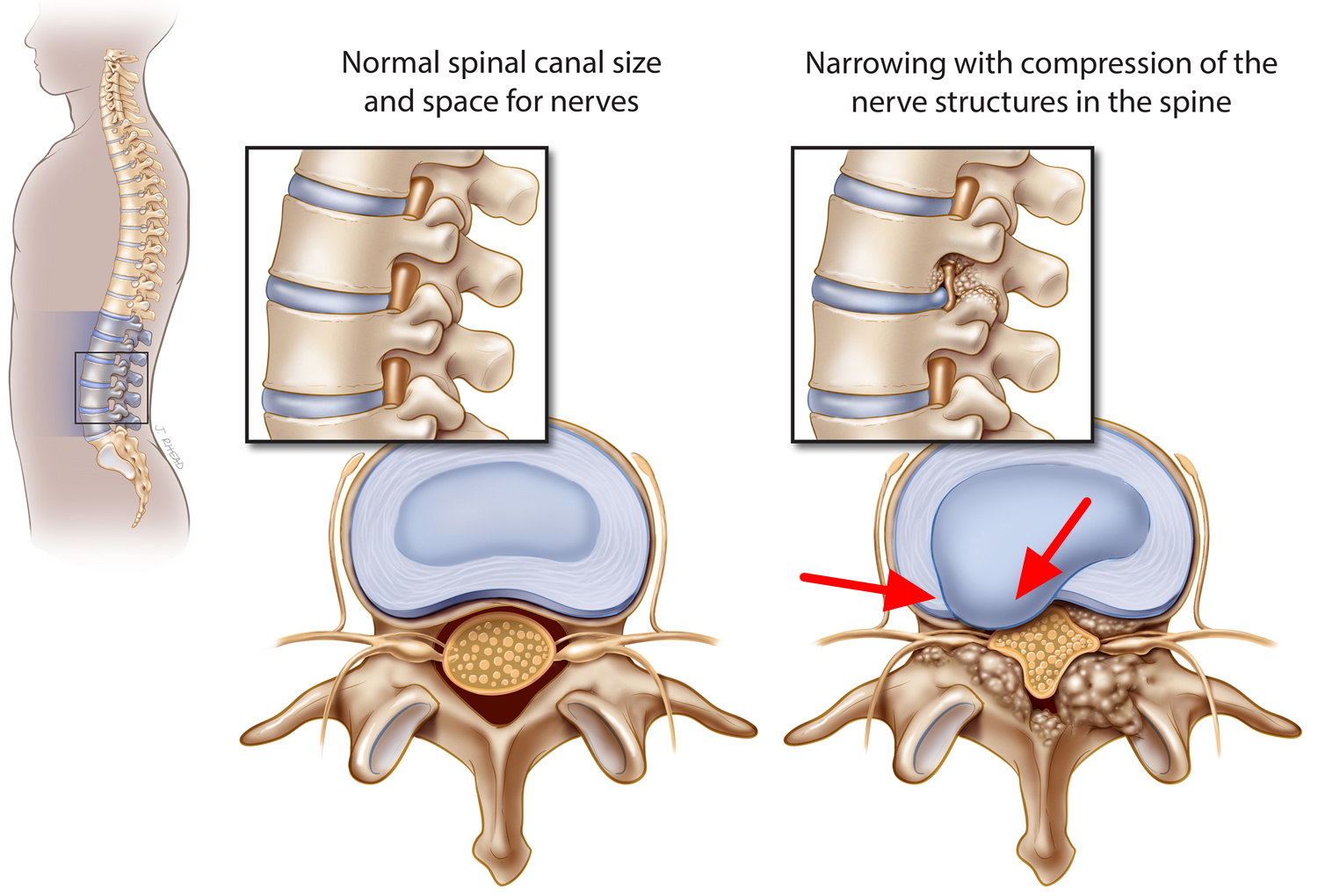
Spinal stenosis is a condition that occurs when spaces within your spine begin to narrow, putting pressure on your spinal cord and nerves. The word “stenosis” means narrowing. Spinal stenosis occurs most often in the lower back and the neck. As spinal stenosis becomes more severe, there can be painful compression or squeezing of the spinal cord and its nerves. Spinal stenosis is often caused by the natural aging process or arthritis, and commonly occurs in the neck (cervical stenosis) and lower back (lumbar stenosis).
The spinal cord is a bundle of nerves that runs through your vertebrae. Some people with spinal stenosis may not have symptoms. When stenosis (narrowing) occurs, you may experience persistent pain, tingling in your arms and legs, numbness, and muscle weakness. In severe forms, you may experience problems with loss of balance, coordination, bladder control, or bowel function.
Spinal stenosis is most commonly caused by wear-and-tear changes in the spine related to osteoarthritis. In severe cases of spinal stenosis, doctors may recommend surgery to create additional space for the spinal cord or nerves.
Types of spinal stenosis
The types of spinal stenosis are classified according to where on the spine the condition occurs. It’s possible to have more than one type. The two main types of spinal stenosis are:
- Cervical stenosis. In this condition, the narrowing occurs in the part of the spine in your neck.
- Lumbar stenosis. In this condition, the narrowing occurs in the part of the spine in your lower back. It’s the most common form of spinal stenosis.
Lumbar spinal stenosis is a common degenerative condition of the spine, leading to significant pain, disability and functional limitations 2. The prevalence of lumbar spinal stenosis is estimated to be 9% in the general population, and up to 47% in people over age 60 3. Lumbar spinal stenosis is the most common reason for spine surgery in patients over 65 4, with a current estimated 2-year cost of $4 billion in the US 5. Given the aging population, both the prevalence and economic burden of lumbar spinal stenosis are expected to increase dramatically 6.
Figure 5. Lumbar stenosis (spinal stenosis occurs when the space within the spinal canal or around the nerve roots becomes narrowed)
Spinal stenosis causes
The backbone (spine) runs from your neck to your lower back. The bones of your spine form a spinal canal, which protects your spinal cord (nerves).
Some people are born with a small spinal canal. But most spinal stenosis occurs when something happens to narrow the open space within the spine.
For many patients, spinal osteoarthritis (called spondylosis) may be the primary cause of spinal stenosis. Arthritis is a condition caused by the breakdown of joints of the spine. Wear and tear damage from osteoarthritis on your spinal bones can prompt the formation of bone spurs, which can grow into the spinal canal. Paget’s disease, a bone disease that usually affects adults, also can cause bone overgrowth in the spine.
Other causes of spinal stenosis may include:
- Disc herniation: The soft cushions that act as shock absorbers between your vertebrae tend to dry out with age. Cracks in a disk’s exterior may allow some of the soft inner material to escape and press on the spinal cord or nerves.
- Past injuries to your spine: Car accidents and other trauma can cause dislocations or fractures of one or more vertebrae. Displaced bone from a spinal fracture may damage the contents of the spinal canal. Swelling of nearby tissue immediately after back surgery also can put pressure on the spinal cord or nerves.
- Tumors: Abnormal growths can form inside the spinal cord, within the membranes that cover the spinal cord or in the space between the spinal cord and vertebrae. These are uncommon and identifiable on spine imaging with an MRI or CT.
- Family history of spine problems.
- Thickened ligaments. The tough cords that help hold the bones of your spine together can become stiff and thickened over time. These thickened ligaments can bulge into the spinal canal.
Some people are born with spinal stenosis. For them, symptoms can begin to surface between the ages of 30 and 50.
Risk factors for spinal stenosis
Most people with spinal stenosis are over the age of 50. Though degenerative changes can cause spinal stenosis in younger people, other causes need to be considered. These include trauma, congenital spinal deformity such as scoliosis, and a genetic disease affecting bone and muscle development throughout the body. Spinal imaging can differentiate these causes.
Spinal stenosis symptoms
Many people have evidence of spinal stenosis on an MRI or CT scan but may not have symptoms. When they do occur, they often start gradually and worsen over time. Symptoms vary depending on the location of the stenosis and which nerves are affected.
Spinal stenosis may cause no signs or symptoms in some people. Others may experience the following:
- Back or neck pain that can range from mild to severe.
- Back pain. People with spinal stenosis may or may not have back pain, depending on the degree of arthritis that has developed.
- Less pain with leaning forward or sitting. Studies of the lumbar spine show that leaning forward can actually increase the space available for the nerves. Many patients may note relief when leaning forward and especially with sitting. Pain is usually made worse by standing up straight and walking. Some patients note that they can ride a stationary bike or walk leaning on a shopping cart. Walking more than 1 or 2 blocks, however, may bring on severe sciatica or weakness.
- Tingling in arms and legs
- Burning pain in buttocks or legs (sciatica). Pressure on spinal nerves can result in pain in the areas that the nerves supply. The pain may be described as an ache or a burning feeling. It typically starts in the area of the buttocks and radiates down the leg. As it progresses, it can result in pain in the foot.
- Numbness, cramping, or weakness in the arms or legs
- Numbness or tingling in buttocks or legs. As pressure on the nerve increases, numbness and tingling often accompany the burning pain. Although not all patients will have both burning pain and numbness and tingling.
- Difficulty standing or walking
- Weakness in the legs or “foot drop.” Once the pressure reaches a critical level, weakness can occur in one or both legs. Some patients will have a foot-drop, or the feeling that their foot slaps on the ground while walking.
- Difficulty with hand coordination (with tasks like buttoning or zipping)
- Unexpected or unexplained trouble with balance and coordination
- Problems with bladder control or bowel function
- Loss of sexual ability
In the neck (cervical spine)
- Numbness or tingling in a hand, arm, foot or leg
- Weakness in a hand, arm, foot or leg
- Problems with walking and balance
- Neck pain
- In severe cases, bowel or bladder dysfunction (urinary urgency and incontinence)
In the lower back (lumbar spine)
- Numbness or tingling in a foot or leg
- Weakness in a foot or leg
- Pain or cramping in one or both legs when you stand for long periods of time or when you walk, which usually eases when you bend forward or sit
- Back pain
If you are experiencing any of the symptoms listed above, you should consult with your physician. Some of the symptoms of spinal stenosis could also indicate a more serious underlying medical condition.
Spinal stenosis complications
Rarely, untreated severe spinal stenosis may progress and cause permanent:
- Numbness
- Weakness
- Balance problems
- Incontinence
- Paralysis
Spinal stenosis diagnosis
To diagnose spinal stenosis, your physician will ask you about your symptoms. The physician will do a medical history and inquire about the degree and duration of pain. Imaging tests will often be ordered to identify the cause of the symptoms.
Tests to Diagnose Spinal Stenosis X-rays
Traditional x-rays can visually depict the alignment of the vertebrae. If previous x-rays have been performed, a radiologist can compare the x-rays to see if there are any changes over time.
Magnetic Resonance Imaging (MRI)
An MRI allows excellent visualization of the soft tissues of the spine, including the nerves and spinal cord. The images can show tumors, growths, inflammation, and even damage to discs, ligaments, and cartilage.
Computerized tomography (CT) myelogram
A CT scan shows the bony detail of the spine and when combined with a myelogram can demonstrate any stenosis or narrowing and pressure on the nerves or spinal cord.
Spinal stenosis treatment
There is currently no cure for spinal stenosis. Treatment for spinal stenosis depends on the location of the stenosis and the severity of your signs and symptoms. With proper treatments and exercise, most people with spinal stenosis will live normal lives.
Talk to your doctor about the treatment that’s best for your situation. If your symptoms are mild or you aren’t experiencing any, your doctor may monitor your condition with regular follow-up appointments. He or she may offer some self-care tips that you can do at home. If these don’t help, he or she may recommend medications or physical therapy. Surgery may be an option if other treatments haven’t helped.
Treatments for Spinal Stenosis
- Pain relievers. Pain medications such as ibuprofen (Advil, Motrin IB, others), naproxen (Aleve, others) and acetaminophen (Tylenol, others) may be used temporarily to ease the discomfort of spinal stenosis. They are typically recommended for a short time only, as there’s little evidence of benefit from long-term use.
- Antidepressants. Nightly doses of tricyclic antidepressants, such as amitriptyline, can help ease chronic pain.
- Anti-seizure drugs. Some anti-seizure drugs, such as gabapentin (Neurontin) and pregabalin (Lyrica), are used to reduce pain caused by damaged nerves.
- Opioids. Drugs that contain codeine-related drugs such as oxycodone (Oxycontin, Roxicodone) and hydrocodone (Norco, Vicodin) may be useful for short-term pain relief. Opioids may also be considered cautiously for long-term treatment. But they carry the risk of serious side effects, including becoming habit forming.
- Activity modifications
- Physical therapy and exercises
- Weight loss
- Corticosteroid Injections. Cortisone is a powerful anti-inflammatory drug. Cortisone injections around the nerves or in the “epidural space” can decrease swelling, as well as pain. They also reduce numbness, but not weakness, in the legs. Patients should receive no more than three injections a year.
Physical therapy
It’s common for people who have spinal stenosis to become less active, in an effort to reduce pain. But that can lead to muscle weakness, which can result in more pain. A physical therapist can teach you exercises that may help:
- Build up your strength and endurance
- Maintain the flexibility and stability of your spine
- Improve your balance
Steroid injections
Your nerve roots may become irritated and swollen at the spots where they are being pinched. While injecting a steroid medication (corticosteroid) into the space around impingement won’t fix the stenosis, it can help reduce the inflammation and relieve some of the pain.
Steroid injections don’t work for everyone. And repeated steroid injections can weaken nearby bones and connective tissue, so you can only get these injections a few times a year.
In severe cases of spinal stenosis, surgery may be recommended.
Lifestyle and home remedies
General healthy lifestyle habits can often help prevent spinal stenosis. Anything that you can do to prevent any amount of degeneration to your spine can help prevent the occurrence of spinal stenosis. Since the condition is often caused by the natural aging process, there are several steps you can take to prevent spinal stenosis.
- Maintaining a healthy weight. Aim to keep a healthy weight. If you’re overweight or obese, your doctor may recommend that you lose weight. Losing excess weight can reduce pain by taking some stress off the back, particularly the lumbar portion of the spine.
- Exercise regularly. Flexing, stretching and strengthening exercises may help open up the spine. Talk with a physical therapist or your doctor about what exercises are safe to do at home.
- Stretch daily
- Avoid smoking
- Practice good posture
- When lifting, use good posture and proper lifting techniques
- Trying pain relievers. Over-the-counter medications such as aspirin, ibuprofen (Advil, Motrin IB, others), naproxen (Aleve, others) and acetaminophen (Tylenol, others) can help reduce pain and inflammation.
- Applying hot or cold packs.Some symptoms of cervical spinal stenosis may be relieved by applying heat or ice to your neck.
- Using a cane or walker. In addition to providing stability, these assistive devices can help relieve pain by allowing you to bend forward while walking.
Alternative medicine
Integrative medicine and alternative therapies may be used with conventional treatments to help you cope with spinal stenosis pain. Examples include:
- Massage therapy
- Chiropractic manipulation. Chiropractic manipulation is generally safe and can help with some of the pain from lumbar stenosis. Care should be taken if a patient has osteoporosis or disk herniation. Manipulation of the spine in these cases can worsen symptoms or cause other injuries.
- Acupuncture. Acupuncture can be helpful in treating some of the pain for less severe cases of lumbar stenosis. Although it can be very safe, long-term success with this treatment has not been proven scientifically.
Talk with your doctor if you’re interested in these treatment options.
Decompression procedure
With this procedure, needle-like instruments are used to remove a portion of a thickened ligament in the back of the spinal column to increase spinal canal space and remove nerve root impingement. Only patients with lumbar spinal stenosis and a thickened ligament are eligible for this type of decompression.
The procedure is called percutaneous image-guided lumbar decompression. It has also been called minimally invasive lumbar decompression, but to avoid confusion with minimally invasive surgical procedures, doctors have adopted the term percutaneous image-guided lumbar decompression.
Because percutaneous image-guided lumbar decompression is performed without general anesthesia, it may be an option for some people with high surgical risks from other medical problems.
Surgery
Surgery may be considered if other treatments haven’t helped or if you’re disabled by your symptoms. The goals of surgery include relieving the pressure on your spinal cord or nerve roots by creating more space within the spinal canal. Surgery to decompress the area of stenosis is the most definitive way to try to resolve symptoms of spinal stenosis.
Research shows that spine surgeries result in fewer complications when done by highly experienced surgeons. Don’t hesitate to ask about your surgeon’s experience with spinal stenosis surgery. If you have any doubts, get a second opinion.
Examples of surgical procedures to treat spinal stenosis include:
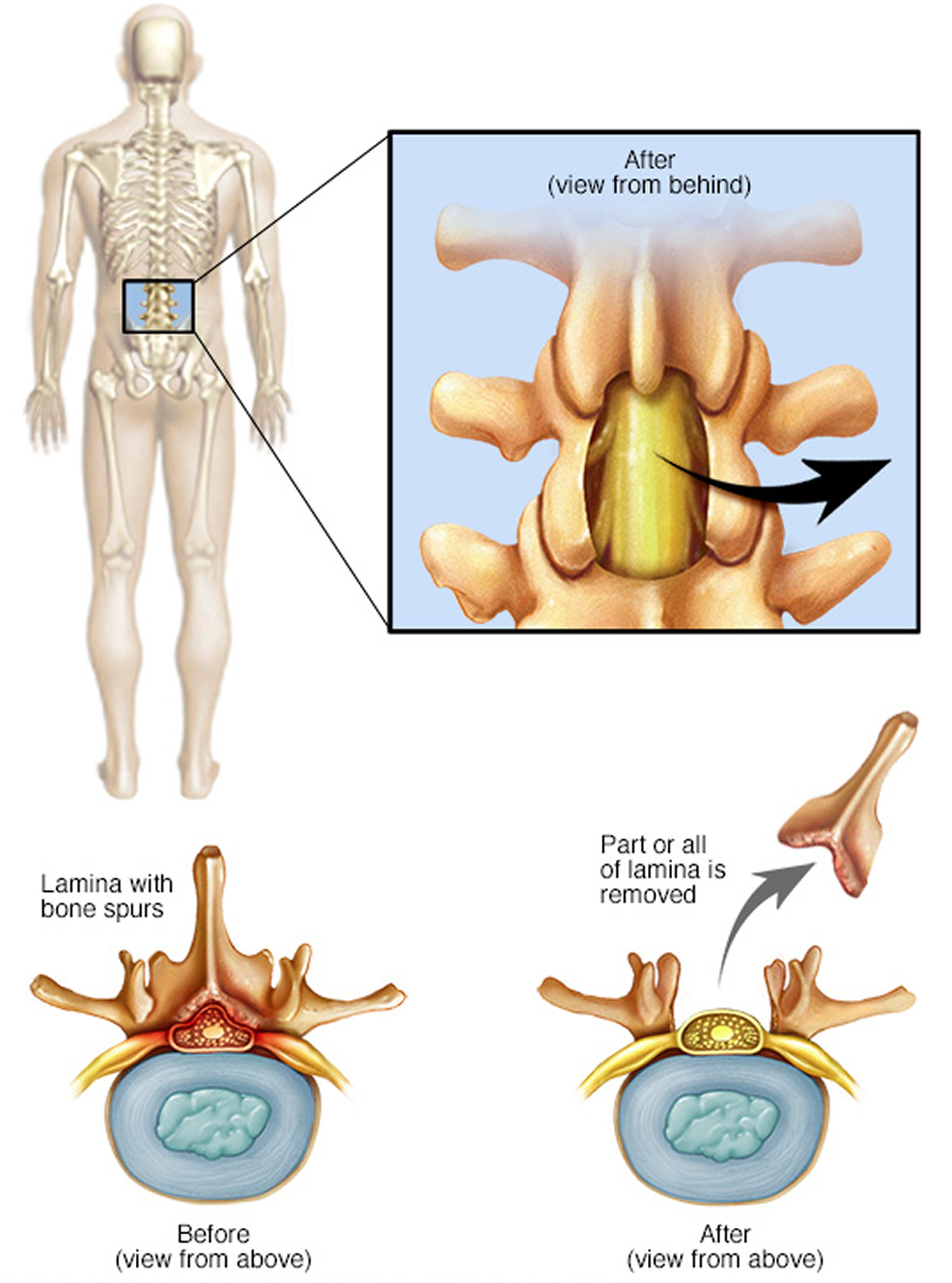
- Laminectomy. This procedure removes the back part (lamina) of the affected vertebra. A laminectomy is sometimes called decompression surgery because it eases the pressure on the nerves by creating more space around them. In some cases, that vertebra may need to be linked to adjoining vertebrae with metal hardware and a bone graft (spinal fusion) to maintain the spine’s strength.
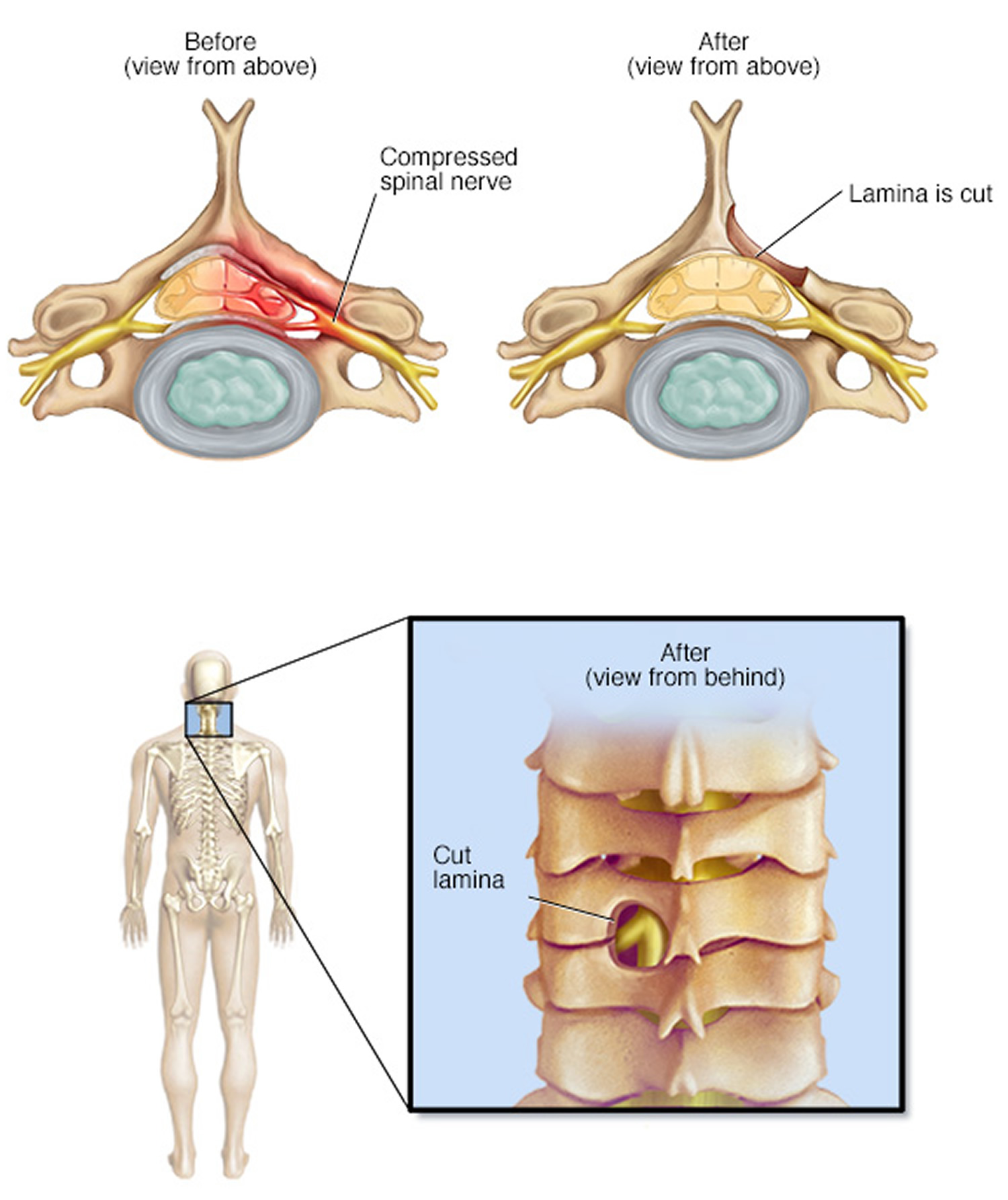
- Laminotomy. This procedure removes only a portion of the lamina, typically carving a hole just big enough to relieve the pressure in a particular spot.
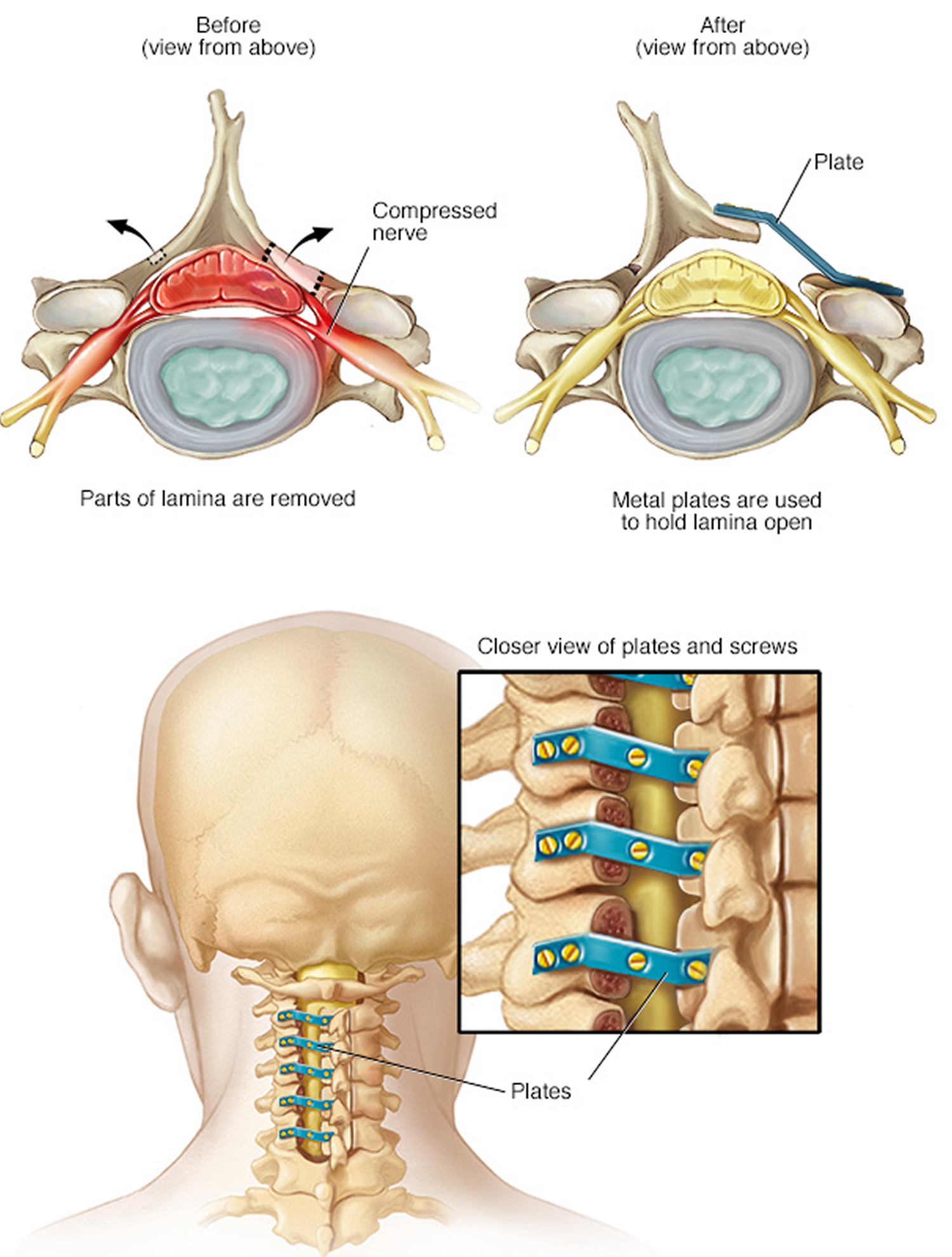
- Laminoplasty. This procedure is performed only on the vertebrae in the neck (cervical spine). It opens up the space within the spinal canal by creating a hinge on the lamina. Metal hardware bridges the gap in the opened section of the spine.
- Minimally invasive surgery. This approach to surgery removes bone or lamina in a way that reduces the damage to nearby healthy tissue. Decompression can be performed using smaller incisions. When using such minimally invasive techniques, there is less injury to the surrounding soft tissues, and recovery may be quicker. With these minimally invasive techniques, surgeons rely more on microscopes to see the area for surgery. They may also take X-rays during the operation. A traditional open procedure requires more direct visualization of the patient’s anatomy, and therefore requires a larger incision. This can be more painful for the patient. The limitation of minimally invasive surgery is the degree of visualization available. If the spinal stenosis extends over a large area of the spine, an open technique is the only method that can address the problem. The advantages of minimally invasive procedures include reduced hospital stays and shorter recovery time. However, both open and minimally invasive techniques relieve stenosis symptoms equally. Your doctor will be able to discuss with you the options that best meet your healthcare needs.
- Minimally invasive surgical technique results in less need to do fusions. While fusions are a useful way to stabilize the spine and reduce pain, by avoiding them you can reduce potential risks, such as post-surgical pain and inflammation and disease in nearby sections of the spine. In addition to reducing the need for spinal fusion, a minimally invasive approach to surgery has been shown to result in a shorter recovery time.
- Spinal fusion. If arthritis has progressed to spinal instability, a combination of decompression and stabilization or spinal fusion may be recommended.
In most cases, these space-creating operations help reduce spinal stenosis symptoms. But some people’s symptoms stay the same or get worse after surgery. Other surgical risks include infection, a tear in the membrane that covers the spinal cord, a blood clot in a leg vein and neurological deterioration.
Figure 6. Lumbar laminectomy
Figure 7. Cervical laminectomy (a cervical laminectomy involves the removal of the back portion of a vertebra in your neck, to create more room within the spinal canal)
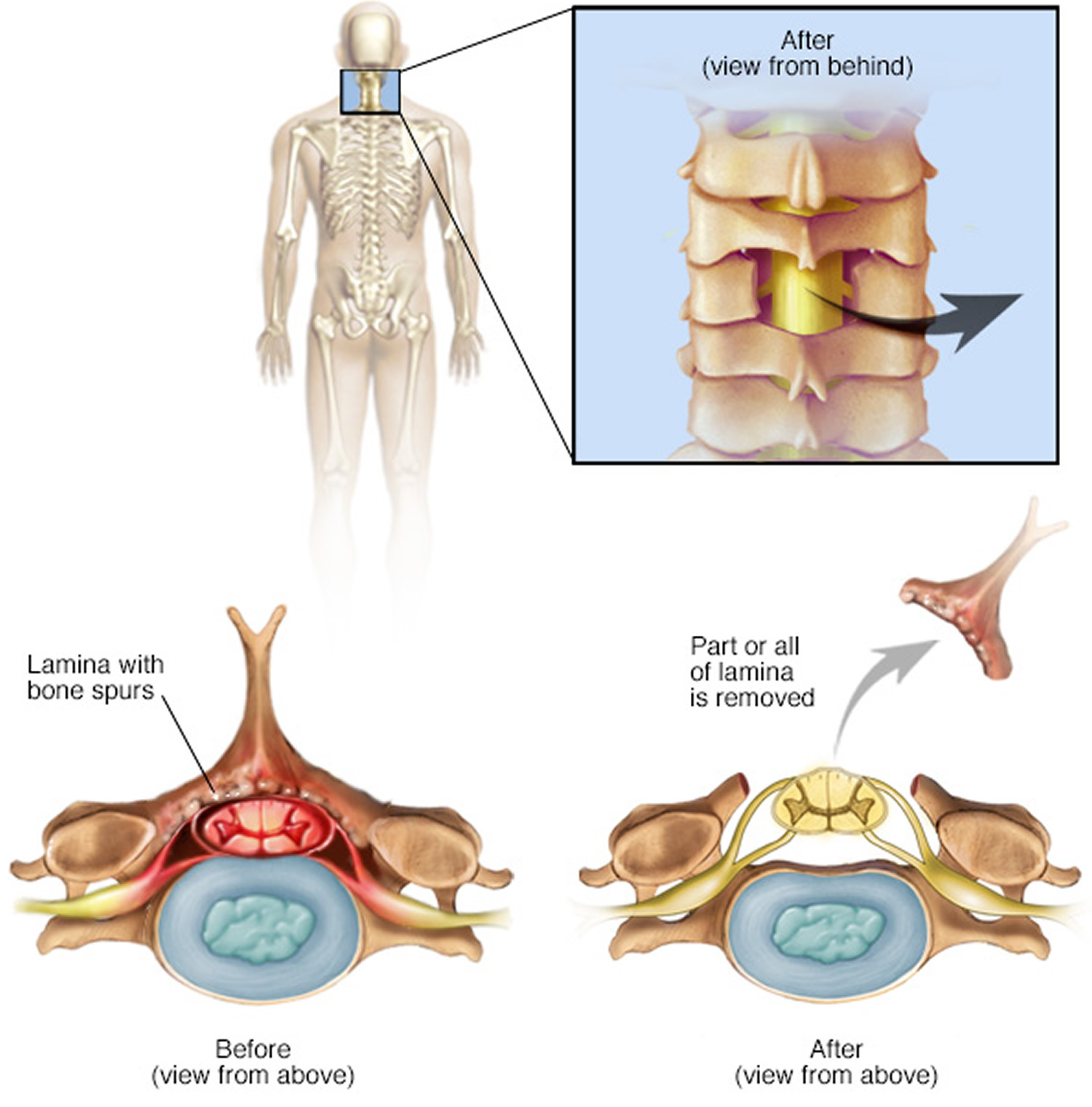 Figure 8. Laminotomy (a laminotomy removes only a portion of the lamina, typically carving a hole just big enough to relieve the pressure in a particular spot. While shown here on the neck, it can also be performed in the lumbar spine)
Figure 8. Laminotomy (a laminotomy removes only a portion of the lamina, typically carving a hole just big enough to relieve the pressure in a particular spot. While shown here on the neck, it can also be performed in the lumbar spine)Note: Laminoplasty is performed only on the vertebrae in the neck (cervical spine). It opens up the space within the spinal canal by creating a hinge on the lamina. Metal hardware bridges the gap in the opened section of the spine.
Surgical risks
There are minor risks associated with every surgical procedure. These include bleeding, infection, blood clots, and reaction to anesthesia. These risks are usually very low.
Elderly patients have higher rates of complications from surgery. So do overweight patients, diabetics, smokers, and patients with multiple medical problems.
Specific complications from surgery for spinal stenosis include:
- Tear of the sac covering the nerves (dural tear)
- Failure of the bone fusion to heal
- Failure of screws or rods
- Nerve injury
- Need for further surgery
- Failure to relieve symptoms
- Return of symptoms
Surgical outcomes
Overall, the results of laminectomy with or without spinal fusion for lumbar stenosis are good to excellent in the majority of patients. Patients tend to see more improvement of leg pain than back pain. Most patients are able to resume a normal lifestyle after a period of recovery from surgery.
Potential future treatments
Clinical trials are underway to test the use of stem cells to treat degenerative spinal disease, an approach sometimes called regenerative medicine. Genomic medicine trials are also being done, which could result in new gene therapies for spinal stenosis.
Interspinous Process Devices
Interspinous process devices, or spacers, are inserted between the spinous processes in the back of the spine. These devices spread the vertebrae apart and keep the space for the nerves open and functioning. This procedure is a minimally invasive surgical option for lumbar spinal stenosis.
Interspinous process spacers were approved in 2005. Many procedures have been performed since then. In some studies, success rates are greater than 80 percent.
Numerous spacer devices are currently being evaluated. They may be a safe alternative to an open laminectomy for some patients. Limited bone (lamina) is removed with this procedure, and it may be performed under local anesthesia.
The key to success with this procedure is appropriate selection of the patients. The appropriate candidate must have relief of buttock and leg pain when sitting or bending forward. The pain returns upon standing.
Rehabilitation
After surgery, you may stay in the hospital for a short time, depending on your health and the procedure performed. Healthy patients who undergo just decompression may go home the same or next day, and may return to normal activities after only a few weeks. Fusion generally adds 2 to 3 days to the hospital stay.
Your surgeon may give you a brace or corset to wear for comfort. He or she will likely encourage you to begin walking as soon as possible. Most patients only need physical therapy to strengthen their backs.
Your physical therapist may show you exercises to help you build and maintain strength, endurance, and flexibility for spinal stability. Some of these exercises will help strengthen your abdominal muscles, which help support your back. Your physical therapist will create an individualized program, taking into consideration your health and history.
Most people can go back to a desk job within a few days to a few weeks after surgery. They may return to normal activities after 2 to 3 months. Older patients who need more care and assistance may be transferred from the hospital to a rehabilitation facility prior to going home.
Claudication complications
In extreme cases, the circulation in your legs or arms can be so limited that you feel pain even when you aren’t exercising, and your legs or arms might feel cool to the touch. Severe peripheral artery disease can lead to poor healing of skin injuries and ulcers. These cuts and ulcers can develop gangrene and require limb amputation.
Spinal stenosis complications
Rarely, untreated severe spinal stenosis may progress and cause permanent:
- Numbness
- Weakness
- Balance problems
- Incontinence
- Paralysis
Claudication causes
Claudication is most often a symptom of peripheral artery disease. In peripheral artery disease, the arteries that supply blood to your limbs are damaged, usually as a result of atherosclerosis. Atherosclerosis can develop in any of your arteries, especially those in your heart. When atherosclerosis affects your arms and legs, it’s called peripheral artery disease.
Atherosclerosis narrows the arteries and makes them stiffer and harder. That’s because the arteries get clogged with clumps of fat, cholesterol and other material, called atherosclerotic plaques. These plaques can make arteries so narrow that less blood can flow through them. You feel pain because your leg muscles are not getting enough oxygenated blood. Oxygen is the fuel that muscles need to contract.
Atherosclerosis isn’t the only possible cause of your symptoms of claudication. Other conditions associated with similar symptoms that need to be considered include spinal stenosis, peripheral neuropathy, certain musculoskeletal conditions and deep venous thrombosis.
Risk Factors for claudication
The exact cause of atherosclerosis isn’t known. However, certain traits, conditions, or habits may raise your risk for the disease. These conditions are known as risk factors. The more risk factors you have, the more likely it is that you’ll develop atherosclerosis.
You can control most risk factors and help prevent or delay atherosclerosis. Other risk factors can’t be controlled.
- Unhealthy blood cholesterol levels. This includes high LDL cholesterol (sometimes called “bad” cholesterol) and low HDL cholesterol (sometimes called “good” cholesterol).
- High blood pressure (hypertension). Blood pressure is considered high if it stays at or above 140/90 mmHg over time. If you have diabetes or chronic kidney disease, high blood pressure is defined as 130/80 mmHg or higher. (The mmHg is millimeters of mercury—the units used to measure blood pressure.)
- Smoking. Smoking can damage and tighten blood vessels, raise cholesterol levels, and raise blood pressure. Smoking also doesn’t allow enough oxygen to reach the body’s tissues.
- Insulin resistance. This condition occurs if the body can’t use its insulin properly. Insulin is a hormone that helps move blood sugar into cells where it’s used as an energy source. Insulin resistance may lead to diabetes.
- Diabetes. With this disease, the body’s blood sugar level is too high because the body doesn’t make enough insulin or doesn’t use its insulin properly.
- Overweight or obesity. The terms “overweight” and “obesity” refer to body weight that’s greater than what is considered healthy for a certain height.
- Lack of physical activity. A lack of physical activity can worsen other risk factors for atherosclerosis, such as unhealthy blood cholesterol levels, high blood pressure, diabetes, and overweight and obesity.
- Unhealthy diet. An unhealthy diet can raise your risk for atherosclerosis. Foods that are high in saturated and trans fats, cholesterol, sodium (salt), and sugar can worsen other atherosclerosis risk factors.
- Older age. As you get older, your risk for atherosclerosis increases. Genetic or lifestyle factors cause plaque to build up in your arteries as you age. By the time you’re middle-aged or older, enough plaque has built up to cause signs or symptoms. In men, the risk increases after age 45. In women, the risk increases after age 55.
- Family history of early heart disease. Your risk for atherosclerosis increases if your father or a brother was diagnosed with heart disease before 55 years of age, or if your mother or a sister was diagnosed with heart disease before 65 years of age.
Although age and a family history of early heart disease are risk factors, it doesn’t mean that you’ll develop atherosclerosis if you have one or both. Controlling other risk factors often can lessen genetic influences and prevent atherosclerosis, even in older adults.
Studies show that an increasing number of children and youth are at risk for atherosclerosis. This is due to a number of causes, including rising childhood obesity rates.
Emerging risk factors for atherosclerosis
Scientists continue to study other possible risk factors for atherosclerosis.
- High levels of a protein called C-reactive protein (CRP) in the blood may raise the risk for atherosclerosis and heart attack. High levels of CRP are a sign of inflammation in the body. Inflammation is the body’s response to injury or infection. Damage to the arteries’ inner walls seems to trigger inflammation and help plaque grow. People who have low CRP levels may develop atherosclerosis at a slower rate than people who have high CRP levels. Research is under way to find out whether reducing inflammation and lowering CRP levels also can reduce the risk for atherosclerosis.
- High levels of triglyceride in the blood also may raise the risk for atherosclerosis, especially in women. Triglycerides are a type of fat.
Studies are under way to find out whether genetics may play a role in atherosclerosis risk.
Other factors that affect atherosclerosis
Other factors also may raise your risk for atherosclerosis, such as:
- Sleep apnea. Sleep apnea is a disorder that causes one or more pauses in breathing or shallow breaths while you sleep. Untreated sleep apnea can raise your risk for high blood pressure, diabetes, and even a heart attack or stroke.
- Stress. Research shows that the most commonly reported “trigger” for a heart attack is an emotionally upsetting event, especially one involving anger.
- Alcohol. Heavy drinking can damage the heart muscle and worsen other risk factors for atherosclerosis. Men should have no more than two drinks containing alcohol a day. Women should have no more than one drink containing alcohol a day.
Claudication prevention
The best way to prevent claudication is to maintain a healthy lifestyle. That means:
- Quit smoking if you’re a smoker.
- If you have diabetes, keep your blood sugar in good control.
- Exercise regularly.
- Lower your cholesterol and blood pressure levels, if necessary.
- Eat foods that are low in saturated fat.
- Maintain a healthy weight.
Claudication symptoms
Claudication symptoms include:
- Pain in the buttocks, thigh, or calf while exercising that resolves at rest. You may feel pain or discomfort in your feet, calves, thighs, hips or buttocks, depending on where you might have artery narrowing or damage. Claudication can also occur in your arms, although this is less common.
- Intermittent pain. Your pain may come and go as you do less-strenuous activities.
- Pain when at rest. As your condition progresses, you may feel pain in your legs even when you’re sitting or lying down.
- Discolored skin or ulcerations. If blood flow is severely reduced, your toes or fingers may look bluish or feel cold to the touch. You may also develop sores on your lower legs, feet, toes, arms or fingers.
Other possible symptoms include:
- An aching or burning sensation in the buttocks, thigh or calf while walking or exercising
- Weakness
Claudication diagnosis
Claudication may go undiagnosed because many people consider the pain an unwelcome but inevitable consequence of aging, and some people just reduce their activity level to avoid the pain. But the tests your doctor may use to diagnose your condition are often noninvasive and can get you back on your way to resuming an active life.
Tests to diagnose claudication include:
- Auscultation – The presence of a bruit (“whooshing” sound), in the arteries of the legs, confirmed using a stethoscope.
- Ankle-brachial index (ABI) – Systolic blood pressure in the ankle divided by the systolic pressure at the arm.
- Doppler Ultrasound – A type of ultrasound that can measure the direction and velocity of blood flow through the vessels.
- CT Angiography – An advanced X-ray procedure using a computer to generate three-dimensional images of blood vessels.
- Magnetic Resonance Angiography (MR angiography) – Patient is exposured to radiofrequency waves in a strong magnetic field. The energy released is measured and utlized to create two- and three-dimensional images of the blood vessels.
- Angiogram – An X-ray study of the blood vessels using contrast dyes.
The pain in your legs could be due to another condition, such as spine, joint or muscle problems. Your doctor can make a diagnosis based on your symptoms and a medical history, physical exam and appropriate tests.
Claudication treatment
Lifestyle Changes and Medical Therapy
Treatment of claudication and peripheral artery disease can help prevent your disease from getting worse and reduce your symptoms. Lifestyle changes, such as quitting smoking and participating in a regular exercise regimen, are often the first steps in treating claudication.
This includes smoking cessation, exercise and weight loss, and medication and include:
- Smoking cessation
- Walking, usually 30 minutes a day
- Medication and lifestyle changes aimed at reducing cholesterol, blood pressure and blood-sugar levels
- Medication, such as aspirin, to prevent heart attack and stroke
- Medication to improve walking distance, such as cilostazol (Pletal)
- Diet low in saturated fats.
Home remedies
The plaques that have damaged your arteries are often the result of unhealthy lifestyle habits. So a key part of treatment is stopping any unhealthy habits and adopting healthy ones.
If you have claudication or peripheral artery disease, make sure you:
- Don’t smoke. Smoking is the most significant risk factor for the development and worsening of peripheral artery disease. Smoking increases the chance that you’ll eventually require an amputation or even die of the disease. Avoid secondhand smoke, too.
- Exercise. You may wonder how exercise can be helpful if that’s what brings on the claudication pain. Actually, exercise helps condition your muscles so that they use oxygen more efficiently. So even if your muscles are getting less oxygen, they can use what they do get more effectively. That can eventually mean less pain during exertion. Your health care team can help develop a supervised exercise program that will enable you to gradually increase the distance you’re able to walk without pain and increase your overall mobility.
- Know and control your cholesterol levels. If your cholesterol levels aren’t what they need to be, your doctor may recommend medication to get them to the proper levels. A meal plan that includes a variety of low-fat foods, emphasizing fruits, vegetables, grains and legumes, can help, too. Combined with exercise, a healthy diet can help control your blood pressure and cholesterol levels, both of which can contribute to atherosclerosis.
- Avoid certain medications. Don’t use drugs that cause your blood vessels to constrict. Many sinus and cold medications sold over-the-counter contain pseudoephedrine, which is known to constrict blood vessels. Ask your doctor if there are any other medications you need to avoid.
- Avoid injury to your feet and legs. Reduced blood flow increases your risk of complications from injuries. Choose well-fitting shoes that will protect your feet if you are participating in activities or work that might lead to injury.
- Keep your legs below your heart. Doing so can help improve the circulation to your feet. To keep the blood flowing well to your legs and feet at night, it helps to raise the head of your bed by 4 to 6 inches.
Alternative medicine
There aren’t any alternative medicine treatments that have been proved effective for claudication.
Several treatments have had mixed results, proving beneficial in some studies, but then showing no benefit in others. These include:
- Ginkgo
- Propionyl-L-carnitine
Another treatment, L-arginine, appeared to help relieve symptoms of claudication.
Vitamin E and omega-3 fatty acids have also been suggested as treatments for claudication, but when studied in clinical trials, these treatments didn’t help relieve symptoms.
Coping and support
It can be frightening to learn that the reason you’re having pain is that your blood vessels are narrowing. Learning all you can about what’s causing your claudication can put you in control, and you’ll know exactly what steps to take to ease your pain.
Some people also find it helpful to talk with other people who are going through the same thing that they are. In a support group, you may find encouragement, advice and maybe even an exercise partner or two. Ask your doctor if there are any support groups in your area.
If your claudication symptoms don’t improve after adopting a healthier lifestyle and home remedies, your doctor may suggest other treatment options, including:
Endovascular Procedures
For most people with peripheral artery disease, symptoms may be mild or absent, and no treatment of the artery blockages is required. However as these blockages become more extensive, patients may experience pain and disability that limits their walking, and in the most advanced cases, individuals may be at risk for loss of the limb unless circulation is improved. Both minimally invasive treatments such as angioplasty or stenting and traditional procedures such as bypass surgery have important roles. Minimally invasive endovascular treatments may be recommended if the claudication becomes severe enough to interfere with the patient’s lifestyle and improvement seems likely.
Determining the best procedure for an individual patient is a complex decision based on:
- The overall health of the patient
- History of their vascular problem and prior treatments
- Location and severity of the arterial blockages in the leg
Catheter-based procedures such as angioplasty are less invasive, but also generally less durable, and have technical limitations when blockages are most extensive.
For patients with severe peripheral artery disease, attempts to improve blood flow in the leg are usually indicated. The goals of improving blood flow to the limb are to reduce pain, improve functional ability and quality of life, and to prevent amputation.
- Angioplasty – A tiny balloon is inserted through a puncture in the groin. The balloon is inflated using a saline solution to expand the narrowed (occluded) artery.
- Stenting – Metal mesh tubes are expanded and left in place to provide scaffolding for an artery that has been opened using a balloon angioplasty.
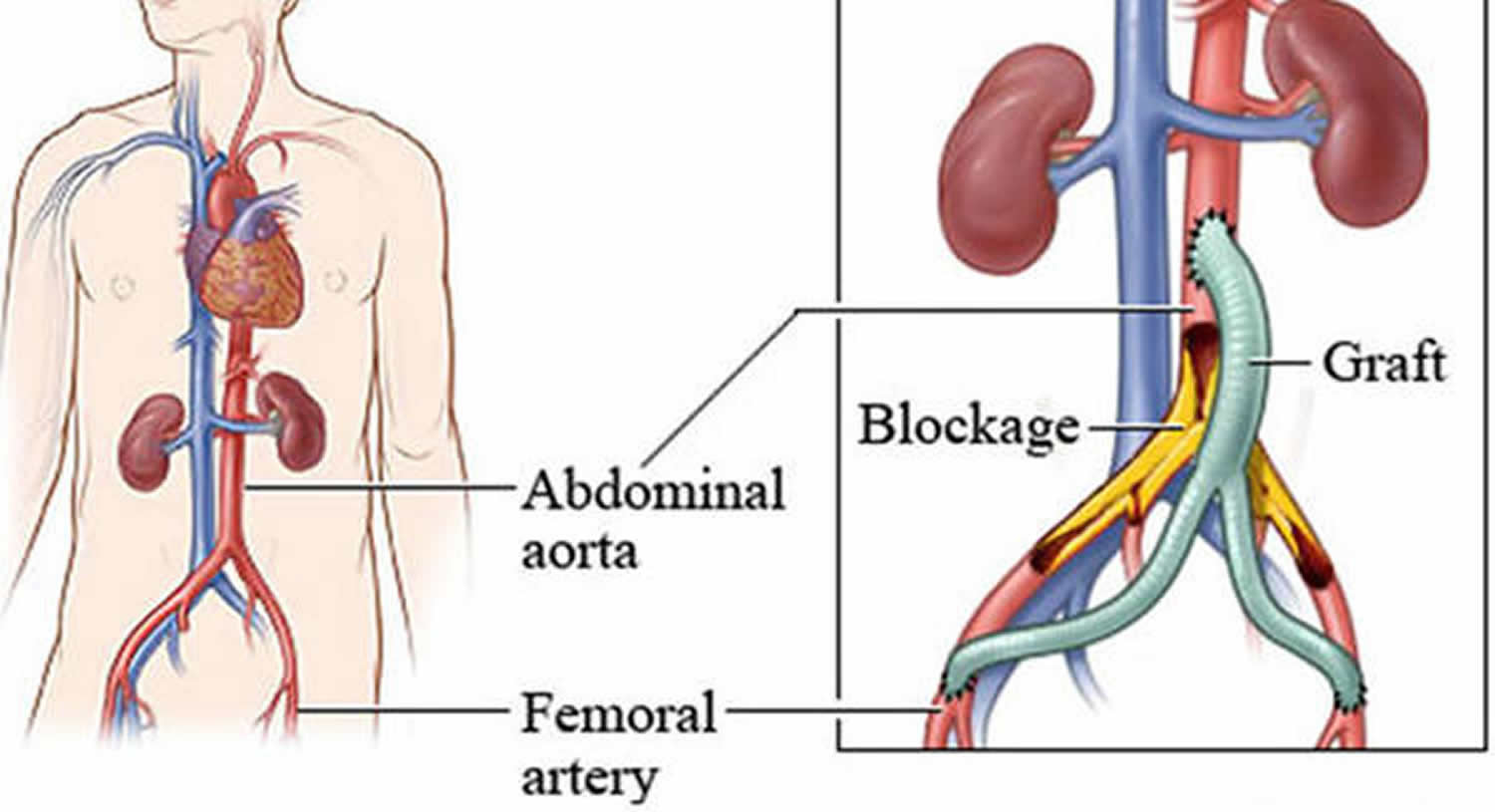
Lower Extremity Bypass Surgery
For patients who are not good candidates for angioplasty, or who have already failed a prior angioplasty attempt, lower extremity bypass surgery is a well-established and highly effective procedure.
In these procedures, surgeons create an alternative conduit for blood flow to circumvent the area of blockage and restore direct flow to the lower leg and foot. This is a major surgical procedure performed under anesthesia via incisions in the leg.
Careful assessment of the risks and benefits prior to surgery, as well as diligent medical, anesthetic, and surgical care, insures the best outcomes following leg bypass operations.
The best results are obtained by using a patient’s own vein, the saphenous vein from the inside of the leg, to perform these grafts. When a good saphenous vein of sufficient length is not available, surgeons may choose to use other veins from the arm or leg, or to use an artificial (prosthetic) graft-however there is a fall-off in results for these alternatives. Therefore, an important consideration in selecting this procedure for a given patient is whether a good vein is likely to be available to perform the bypass.
Figure 10. Lower Extremity Bypass Surgery
Risks of leg bypass surgery
Like all surgical procedures, leg bypass surgery carries significant risks including heart attacks, blood clots, infections and even death in 2 to 3 percent of patients. Patients with advanced peripheral artery disease have a high frequency of significant heart disease, so a thorough evaluation for cardiac problems and a careful review of medical therapies is required prior to surgery.
The use of medications such as aspirin, blood pressure, and cholesterol-lowering drugs is critical before and after the operation. The other major complications are related to the leg itself, and include the risk of failure of the bypass and wound healing problems. Overall, bypass surgery is immediately successful in 90 to 95 percent of cases. The short and long-term success of the procedure is most closely linked to two factors:
- The material employed for the bypass graft itself and
- The quality of the arteries in the lower leg to which the graft is attached.
Post-Operative Period and Follow-up
Because blockages in the leg arteries extend over a considerable length, long incisions are often required, and various problems related to the healing of these wounds can occur in up to 20 percent of patients. These are often minor complications that may require dressings or antibiotics at home, but some can be more serious and lead to prolonged hospitalization or additional procedures.
Careful surgical technique and postoperative care are required to minimize these problems.In general, a vein bypass in the leg can be expected to last five years or longer in 60 to 70 percent of patients; though about one-quarter to one-third will require additional procedures to maintain the function of these grafts. Long-term follow-up, with regularly scheduled vascular examinations and ultrasound studies of the graft, is absolutely essential to achieve maximal benefit.
Abstinence from smoking and continued medical management including aspirin and cholesterol-lowering drugs is critical after surgery. Once recuperation is complete, patients who have had successful bypass surgery should expect to achieve relief of pain, improved healing of wounds on the foot, improved walking ability and long-term freedom from amputation as long as the graft continues to function. For many patients with advanced peripheral artery disease, lower extremity bypass surgery provides the most effective and most durable solution currently available.
- Smith RB III. Claudication. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 13. Available from: https://www.ncbi.nlm.nih.gov/books/NBK235/[↩]
- Tomkins-Lane C, Melloh M, Lurie J, et al. Consensus on the clinical diagnosis of lumbar spinal stenosis: Results of an International Delphi Study. Spine. 2016;41(15):1239-1246. doi:10.1097/BRS.0000000000001476. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4966995/[↩]
- Kalichman L, et al. Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J. 2009;9:545–550. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3775665/[↩]
- Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine. 2005;30:1441–1445. discussion 1446-1447. https://www.ncbi.nlm.nih.gov/pubmed/15959375[↩]
- Parker SL, et al. Two-year comprehensive medical management of degenerative lumbar spine disease (lumbar spondylolisthesis, stenosis, or disc herniation): a value analysis of cost, pain, disability, and quality of life: clinical article. J. Neurosurg. Spine. 2014;21:143–149. https://www.ncbi.nlm.nih.gov/pubmed/24785973[↩]
- Harrop JS, Hilibrand A, Mihalovich KE, Dettori JR, Chapman J. Cost-effectiveness of surgical treatment for degenerative spondylolisthesis and spinal stenosis. Spine. 2014;39:S75–S85. https://www.ncbi.nlm.nih.gov/pubmed/25299263[↩]