Contents
What is De Quervain’s tenosynovitis
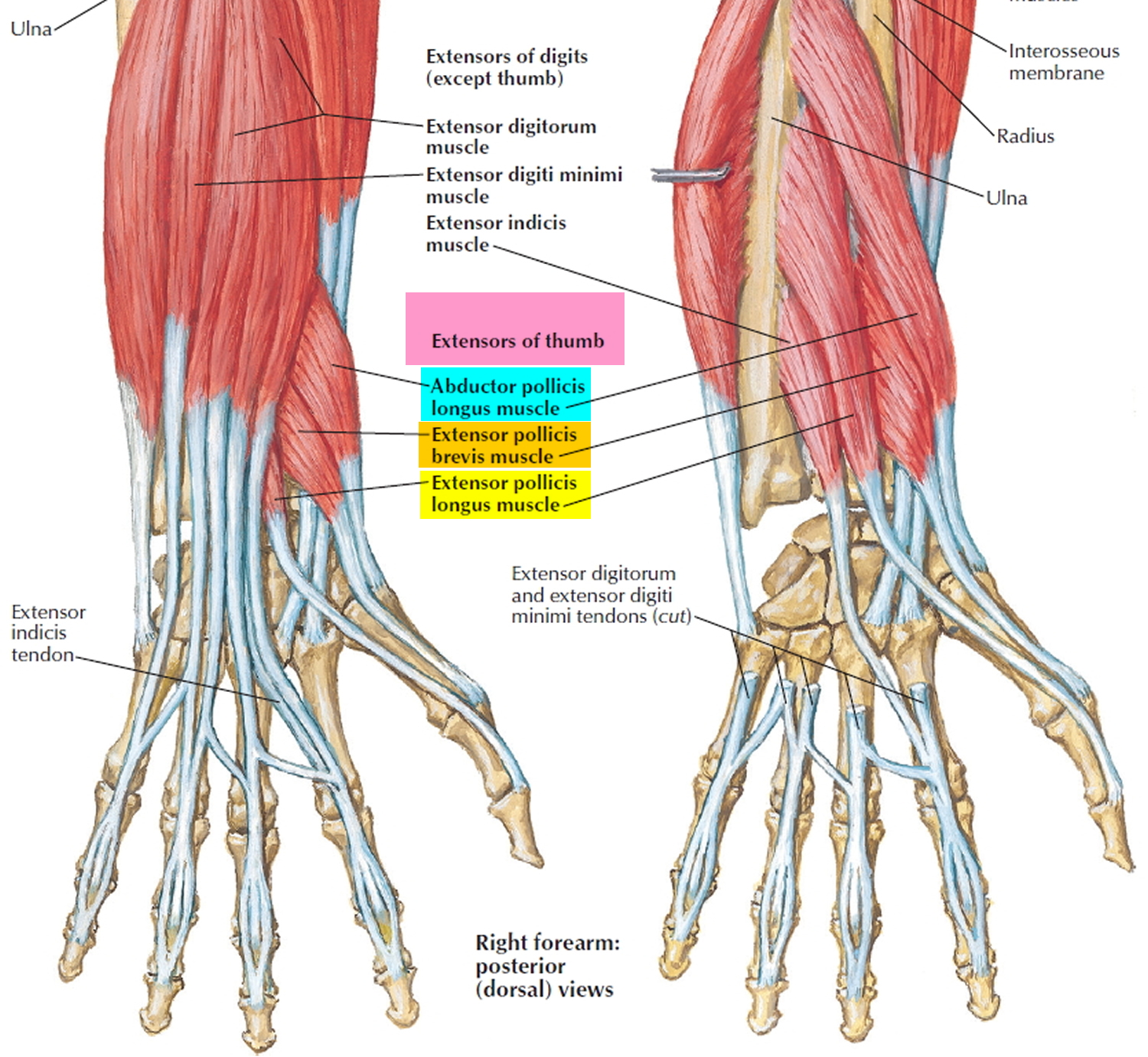
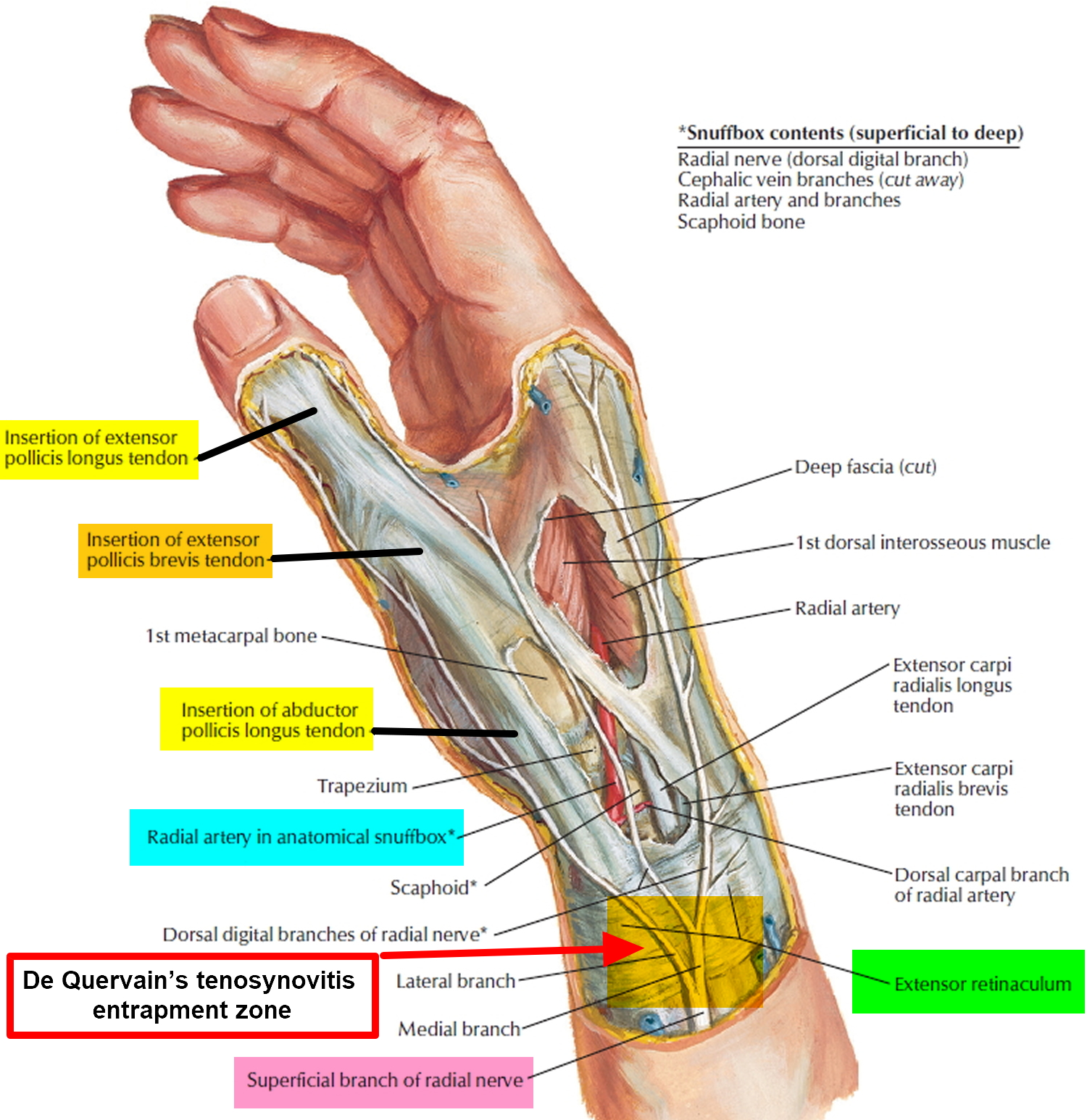
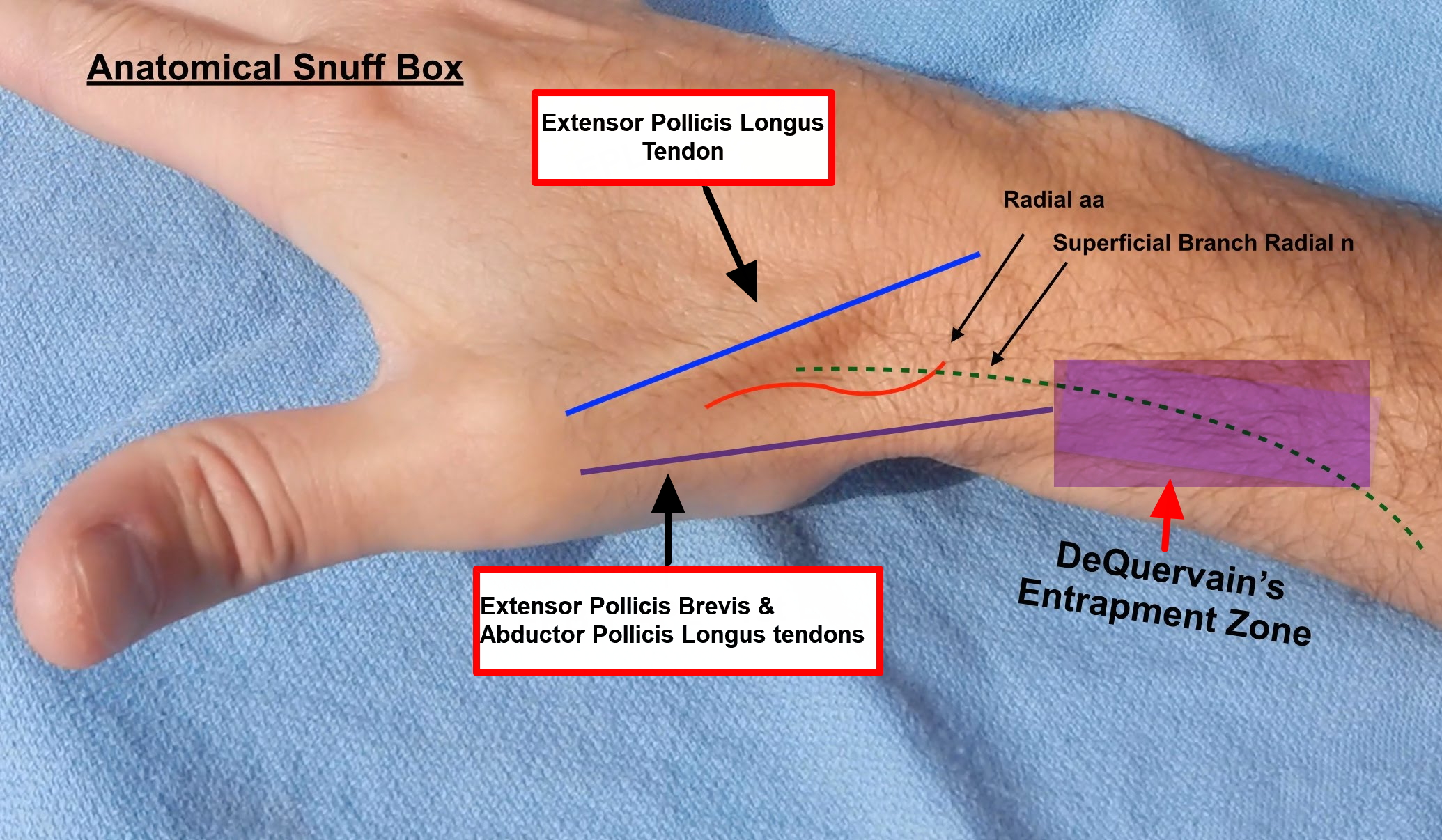
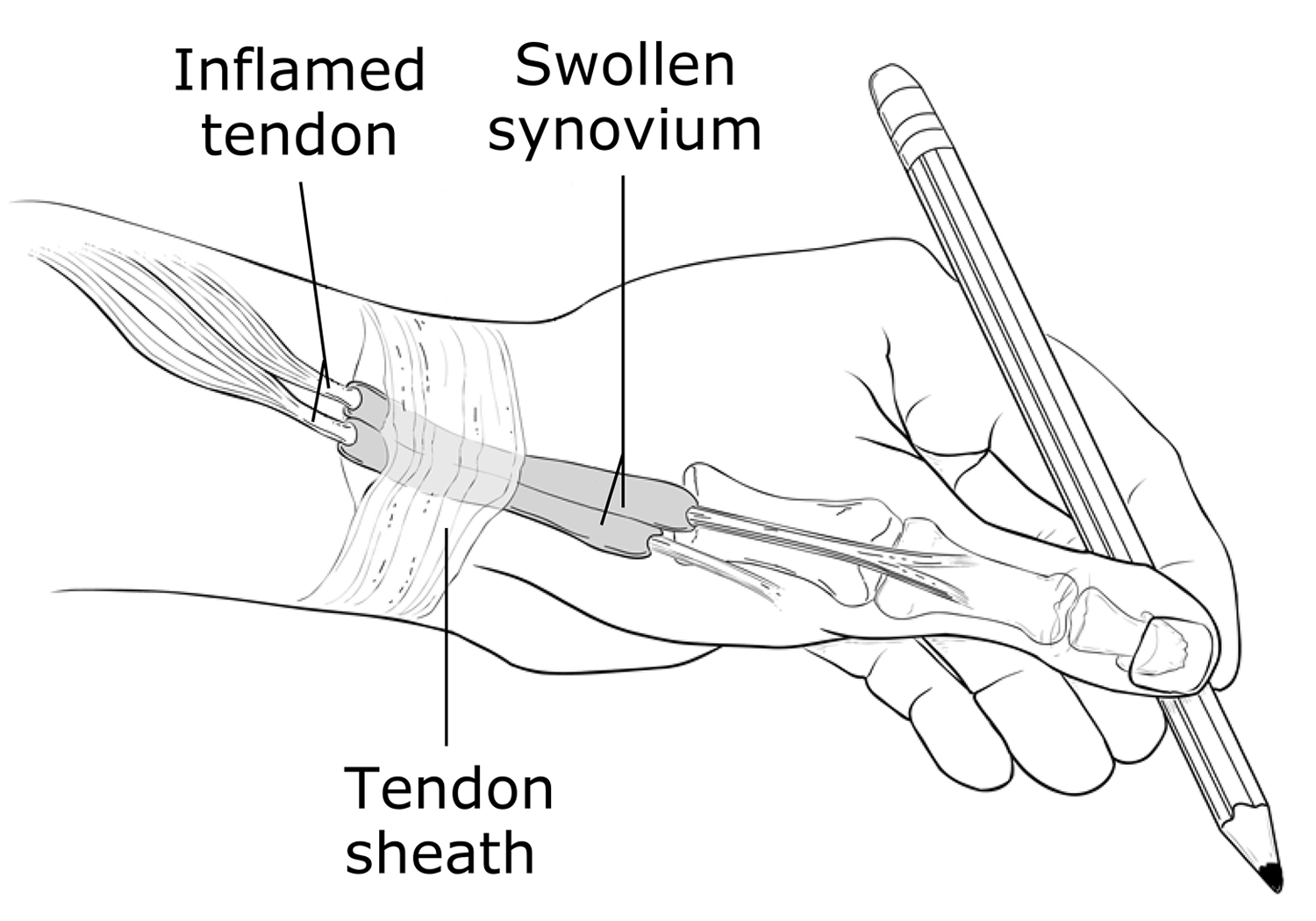
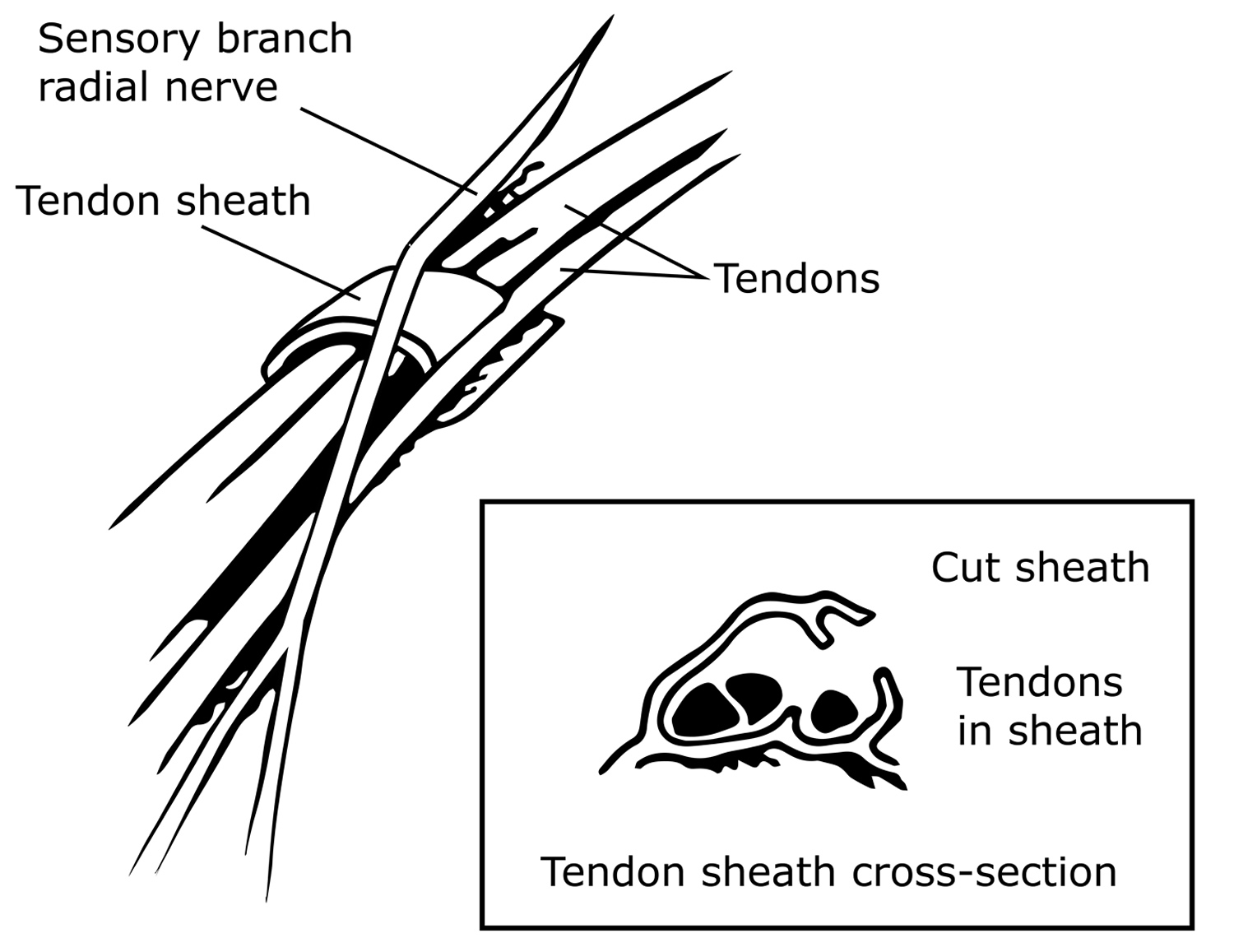
De Quervain’s tenosynovitis sometimes called washerwoman’s sprain, is a painful wrist condition involving two of the tendons on the thumb side of your wrist tendons, which pass through the first dorsal compartment of the wrist – the thumb extensors called extensor pollicis brevis (EPB) and abductor pollicis longus (APL) at the base of the thumb 1. Two of the main tendons to the thumb pass through a tunnel (or series of pulleys) located on the thumb side of the wrist (see Figures 1 and 2). Tendons are rope-like structures that attach muscle to bone. Tendons are covered by a slippery thin soft-tissue layer, called synovium. This layer allows the tendons to slide easily through a fibrous tunnel called a sheath.
Any swelling of the tendons and/or thickening of the sheath, results in increased friction and pain with certain thumb and wrist movements.
If you have de Quervain’s tenosynovitis, it will probably hurt when you turn your wrist, grasp anything or make a fist.
Although the exact cause of de Quervain’s tenosynovitis isn’t known, any activity that relies on repetitive hand or wrist movement — such as working in the garden, playing golf or racket sports, or lifting your baby — can make it worse. Swelling of the tendons, and the tendon sheath, can cause pain and tenderness along the thumb side of the wrist. This is particularly noticeable when forming a fist, grasping or gripping something, or when turning the wrist.
Although conservative treatment like resting the thumb in a splint in combination with NSAIDs and corticosteroid injections has shown relief of symptoms in de Quervain’s tenosynovitis, surgery involving a first dorsal compartment release may be necessary if continued symptoms persist.
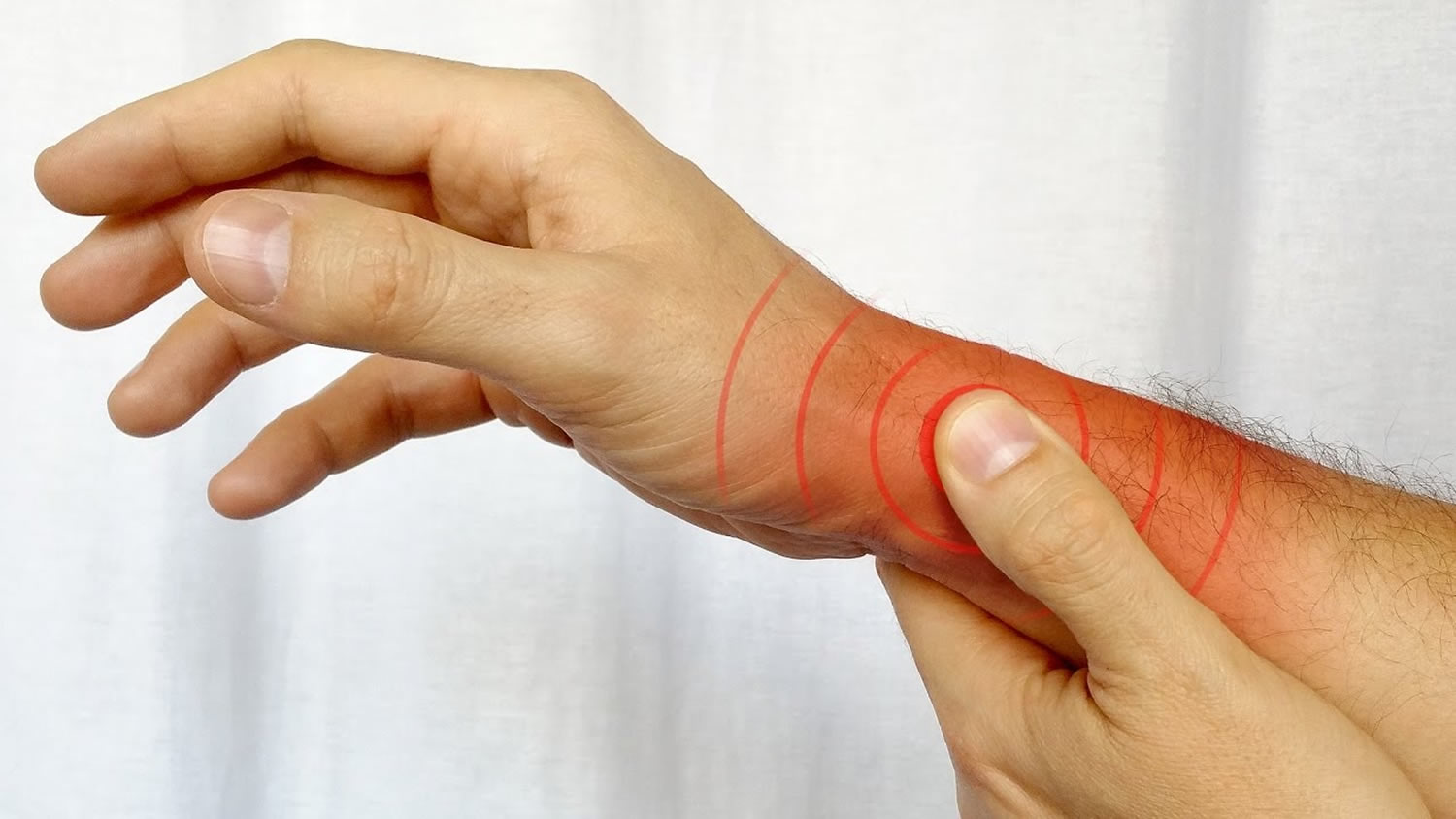
Figure 1. De Quervain’s tenosynovitis anatomy
Figure 2. De Quervain’s tenosynovitis entrapment zone
De Quervain’s tenosynovitis causes
Chronic overuse of your wrist extensor pollicis brevis and abductor pollicis longus tendons as they pass under a thickened and swollen extensor retinaculum is commonly associated with de Quervain’s tenosynovitis 2.
Tendons are rope-like structures that attach muscle to bone. When you grip, grasp, clench, pinch or wring anything in your hand, two tendons in your wrist and lower thumb normally glide smoothly through the small tunnel that connects them to the base of the thumb. Repeating a particular motion day after day may irritate the sheath around the two tendons, causing thickening and swelling that restricts their movement.
Other causes of de Quervain’s tenosynovitis include:
- Direct injury to your wrist or tendon; scar tissue can restrict movement of the tendons
- Inflammatory arthritis, such as rheumatoid arthritis
Risk factors for de Quervain’s tenosynovitis
Risk factors for de Quervain’s tenosynovitis include:
- Age. If you’re between the ages of 30 and 50, you have a higher risk of developing de Quervain’s tenosynovitis than do other age groups, including children.
- Sex. The condition is more common in women.
- Being pregnant. The condition may be associated with pregnancy.
- Baby care. Lifting your child repeatedly involves using your thumbs as leverage and may also be associated with the condition.
- Jobs or hobbies that involve repetitive hand and wrist motions. These may contribute to de Quervain’s tenosynovitis.
Parents or caretakers of infants are at increased risk of developing de Quervain’s tenosynovitis due to repetitive lifting and carrying actions forcing the wrist into ulnar deviation 3. Therefore, new parents and those involved in childcare are encouraged to limit lifting and carrying children as much as possible. Furthermore, soft tissue edema, fluid retention, and ligamentous laxity are common effects of pregnancy, which can impact the inflammatory response and pressure upon the first dorsal compartment 3.
De Quervain’s tenosynovitis symptoms
Symptoms of de Quervain’s tenosynovitis include:
- Pain near the base of your thumb. This is the main symptom. The pain may appear either gradually or suddenly. Pain is felt in the wrist and can travel up the forearm. The pain is usually worse when the hand and thumb are in use. This is especially true when forcefully grasping objects or twisting the wrist.
- Swelling may be seen over the thumb side of the wrist. This swelling may accompany a fluid-filled cyst in this region.
- Difficulty moving your thumb and wrist when you’re doing something that involves grasping or pinching
- A “sticking”, “catching” or “stop-and-go” sensation may be felt when moving your thumb.
- Pain and swelling may make it difficult to move the thumb and wrist.
If the condition goes too long without treatment, the pain may spread further into your thumb, back into your forearm or both. Pinching, grasping and other movements of your thumb and wrist aggravate the pain.
De Quervain’s tenosynovitis complications
Untreated de Quervain’s tenosynovitis might make it hard to use your hand and wrist properly and limit your wrist’s range of motion.
De Quervain’s tenosynovitis diagnosis
To diagnose de Quervain’s tenosynovitis, your doctor will examine your hand to see if you feel pain when pressure is applied on the thumb side of the wrist.
De Quervain’s tenosynovitis test
Your doctor will also perform a Finkelstein test, in which you bend your thumb across the palm of your hand and bend your fingers down over your thumb. Then you bend your wrist toward your little finger. If this causes pain on the thumb side of your wrist, you likely have de Quervain’s tenosynovitis.
Imaging tests, such as X-rays, generally aren’t needed to diagnose de Quervain’s tenosynovitis.
Figure 3. De Quervain’s tenosynovitis test – Finkelstein test
De Quervain’s tenosynovitis treatment
Treatment for de Quervain’s tenosynovitis is aimed at reducing inflammation, preserving movement in the thumb and preventing recurrence.
If you start treatment early, your symptoms should improve within four to six weeks. If your de Quervain’s tenosynovitis starts during pregnancy, symptoms are likely to end around the end of either pregnancy or breast-feeding.
Initial treatment of de Quervain’s tenosynovitis may include:
- Immobilizing your thumb and wrist, keeping them straight with a splint or brace to help rest your tendons
- Avoiding repetitive thumb movements as much as possible
- Avoiding pinching with your thumb when moving your wrist from side to side
- Applying ice to the affected area
The use of a thumb spica splint has been shown to assist with pain management by immobilizing the thumb and wrist joints, thereby preventing thumb metacarpophalangeal joint flexion and wrist ulnar deviation 4. Ilyas et al. 2 state that splinting is effective with a corticosteroid injection in immobilizing and resting the extensor pollicis brevis and abductor pollicis longus tendons in a position to decrease the friction in the joint that can lead to increased pain and inflammation. However, studies have not shown splinting as a treatment tool to provide long-lasting relief beyond allowing the joints to rest in an immobilized position 5. In a study by Harvey et al. 6, immobilization with corticosteroid injection was not found necessary; instead, mobilization was encouraged resulting in extended relief of pain symptoms in 80 % of cases. Others have recommended splint use for comfort only in patients with increased pain 5. If a splint is prescribed, a forearm-based thumb spica splint that immobilizes the joints with the wrist in neutral, 30° of carpometacarpal joint flexion and 30° of thumb abduction with the thumb interphalangeal joint free is recommended 2 (Figure. 4).
Figure 4. De Quervain’s tenosynovitis splint that immobilizes the joints with the wrist in neutral, 30° of carpometacarpal joint flexion and 30° of thumb abduction with the thumb interphalangeal joint free
Medications
To reduce pain and swelling, your doctor may recommend using over-the-counter pain relievers, such as ibuprofen (Advil, Motrin IB, others) and naproxen (Aleve).
Your doctor may also recommend injections of corticosteroid medications into the tendon sheath to reduce swelling. If treatment begins within the first six months of symptoms, most people recover completely after receiving corticosteroid injections, often after just one injection. The corticosteroid injection is delivered into the first dorsal compartment 6. Harvey et al. 6 found corticosteroid injection provided prolonged relief in 80 % of cases in a study involving 71 patients. Poor response to a corticosteroid injection has been correlated with poor technique and a likelihood of the extensor pollicis brevis tendon lying in a separate compartment 6.
Hand therapy
You may also see a physical or occupational therapist. These therapists may review how you use your wrist and give suggestions on how to make adjustments to relieve stress on your wrists. Your therapist can also teach you exercises for your wrist, hand and arm to strengthen your muscles, reduce pain and limit tendon irritation.
De Quervain’s tenosynovitis exercises
The goal of therapeutic exercises is to enhance gliding of the extensor pollicis brevis and abductor pollicis longus tendons in the first dorsal compartment 7. Pain-free active range of motion (AROM) exercise is initiated to the patient’s tolerance, focusing on the wrist and thumb joints. Tendon gliding of the extensor pollicis brevis and abductor pollicis longus tendons is gently incorporated into thumb metacarpophalangeal flexion combined with wrist ulnar deviation 7. Strengthening exercises are then initiated to assist in return to functional activity 7.
Patient is initially prescribed exercises consisting of static stretching for the thenar muscle group (Figure 5) and forearm extensors/flexors. In addition, eccentric unweighted hammer curl exercises with no concentric component were prescribed (Figure 6 A–C). The patient was instructed to assist with the other hand during the concentric (radial deviation) movement phase. In week 3, eccentric thumb extension and abduction exercises with an elastic band (Figure 7 and and 8), were introduced. At the beginning of week 5, eccentric wrist extension and flexion exercises with a dumbbell (Figure 9 and and 10), along with eccentric forearm pronation and supination exercises with theraband® (Figure 11 and and 12) were introduced. All eccentric exercises were performed without the concentric component permitted. A summary of the full rehabilitative exercise treatment protocol is included in Table 1.
Table 1. Overview of the rehabilitative exercises prescribed in de Quervain’s tenosynovitis
| EXERCISE | INSTRUCTIONS |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
Figure 5. Stretching for the thenar muscle group
Figure 6. The eccentric training protocol – (A) The patient starts with the unweighted hand in the hammer curl position. (B) The wrist is then eccentrically loaded by slowly lowering the hand into a position of ulnar deviation. (C) The patient returns to the starting position using the contralateral unaffected hand to avoid concentric loading (radial deviation)
Figure 7. Eccentric thumb extension exercise
Figure 8. Eccentric thumb abduction exercise
Figure 9. Eccentric wrist extension
Figure 10. Eccentric wrist flexion
Figure 11. Eccentric forearm pronation
Figure 12. Eccentric forearm supination
De Quervain’s tenosynovitis surgery
If your case is more serious, your doctor may recommend outpatient surgery. Surgery involves a procedure in which your doctor inspects the sheath surrounding the involved tendon or tendons, and then opens the sheath to release the pressure so your tendons can glide freely.
Your orthopaedic surgeon will talk to you about how to rest, strengthen and rehabilitate your body after surgery. A physical or occupational therapist may meet with you after surgery to teach you new strengthening exercises and help you adjust your daily routine to prevent future problems.
Figure 13. De Quervain’s tenosynovitis surgery – your doctor will cut open the tendon sheath over the inflamed tendons.
Home remedies
If you don’t need surgery, caring for your condition is much the same as preventing it:
- Avoid moving your wrists the same way repeatedly.
- Wear a brace or splint if suggested by your doctor.
- Follow through with recommended exercises.
- Note activity that causes pain, swelling or numbness in your thumb and wrist, try to avoid it, and share that information with your doctor.
- A patient with de Quervain’s tenosynovitis: a case report using an Australian approach to manual therapy. Anderson M, Tichenor CJ. Phys Ther. 1994 Apr; 74(4):314-26. https://www.ncbi.nlm.nih.gov/pubmed/8140144/[↩]
- Ilyas AM, Ast M, Schaffer AA, Thoder J. De Quervain tenosynovitis of the wrist. J Am Acad Orthop Surg. 2007;15(12):757–764. https://www.ncbi.nlm.nih.gov/pubmed/18063716[↩][↩][↩]
- Borg-Stein J, Dugan SA. Musculoskeletal disorders of pregnancy, delivery and postpartum. Phys Med Rehabil Clin N Am. 2007;18:459–476. doi: 10.1016/j.pmr.2007.05.005. https://www.ncbi.nlm.nih.gov/pubmed/17678762[↩][↩]
- Fedorczyk JM. Tendinopathies of the elbow, wrist, and hand: histopathology and clinical considerations. J Hand Ther. 2012;25(2):191–200. doi: 10.1016/j.jht.2011.12.001. https://www.ncbi.nlm.nih.gov/pubmed/22507213[↩]
- Ilyas A. Nonsurgical treatment of de Quervain’s tenosynovitis. J Hand Surg. 2009;34A:928–929. doi: 10.1016/j.jhsa.2008.12.030. https://www.ncbi.nlm.nih.gov/pubmed/19410999[↩][↩]
- Harvey FJ, Harvey PM, Horsley MW. De Quervain’s disease: surgical or nonsurgical treatment. J Hand Surg. 1990;15A:83–87. doi: 10.1016/S0363-5023(09)91110-8 https://www.ncbi.nlm.nih.gov/pubmed/2299173[↩][↩][↩][↩]
- Jaworski CA, Krause M, Brown J. Rehabilitation of the wrist and hand following sports injury. Clin Sports Med. 2010;29(1):61–80. doi: 10.1016/j.csm.2009.09.007 https://www.ncbi.nlm.nih.gov/pubmed/19945587[↩][↩][↩]
- Papa JA. Conservative management of De Quervain’s stenosing tenosynovitis: a case report. The Journal of the Canadian Chiropractic Association. 2012;56(2):112-120. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3364060/[↩]