Contents
What is diverticulitis
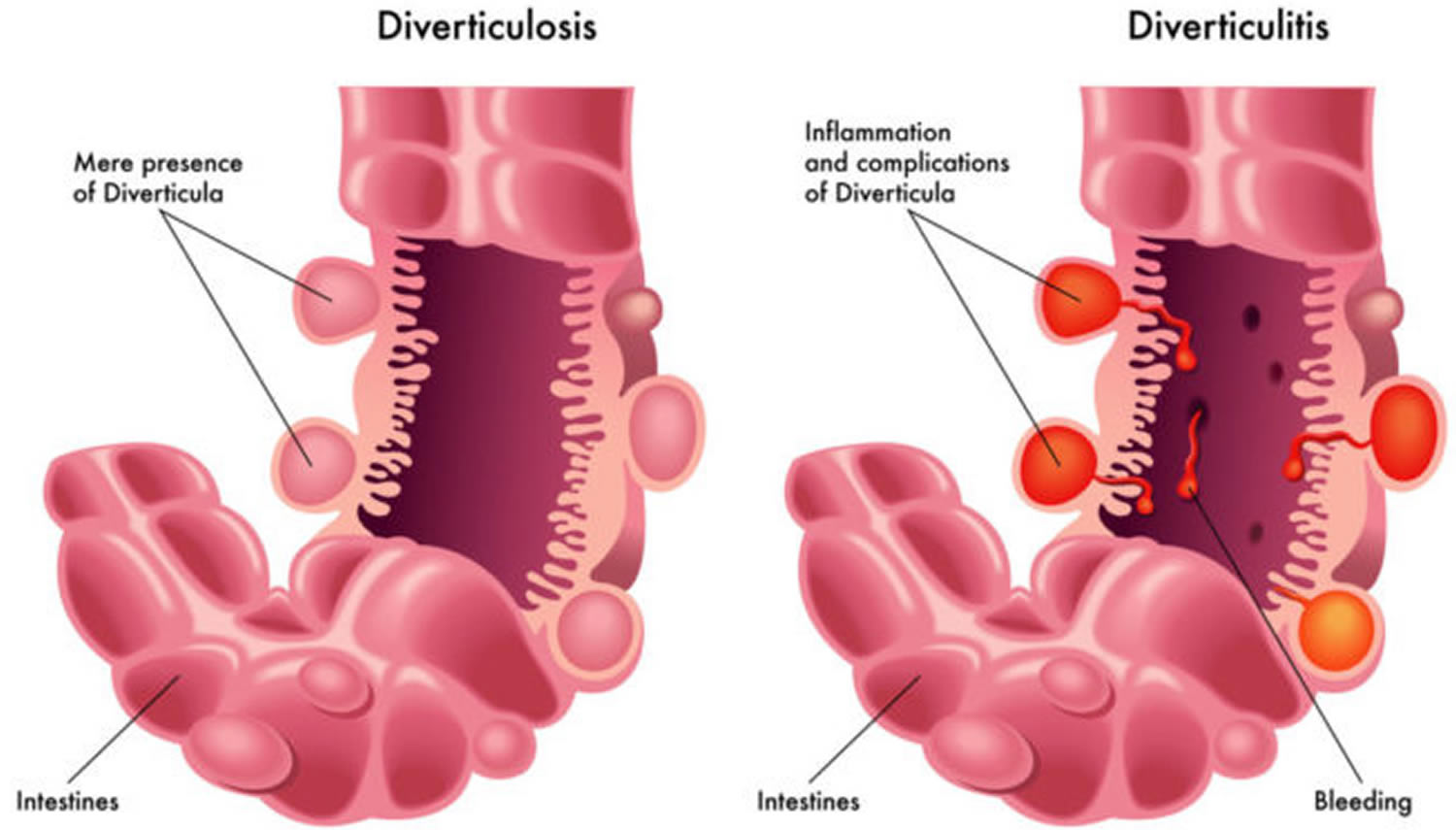
Diverticular disease is a group of conditions that affect your large intestine (colon) 1. Diverticula are small pouches or sacs that bulge outward through the colon or large intestine. If you have these pouches, you have a condition called diverticulosis.
These pouches can form in your large intestine wall and cause problems. The most common conditions of diverticular disease are:
- Diverticulosis. This is the base condition where the pouches form. It becomes more common as you age. Most people with diverticulosis don’t know they have it.
- Diverticulitis. This occurs when the pouches become inflamed or infected. It can cause pain and other symptoms. Serious cases could require staying in the hospital.
- Diverticular bleeding. Diverticular bleeding occurs when a blood vessel next to the pouches bursts. It is not as common as diverticulitis.
Diverticular disease becomes more common as people age. About 60 percent of all people over age 60 have it 2. Doctors believe the main cause is a low-fiber diet. The best way to prevent diverticular disease is with a healthy lifestyle and a high-fiber diet. You can increase the amount of fiber in your diet by eating more fruits, vegetables, and whole-grain foods. Also, be sure to drink plenty of fluids and exercise regularly.
Most people with diverticulosis don’t have symptoms. Sometimes it causes mild cramps, bloating or constipation. Diverticulosis is often found through tests ordered for something else. For example, it is often found during a colonoscopy to screen for cancer. A high-fiber diet and mild pain reliever will often relieve symptoms.
If the diverticular pouches become inflamed or infected, you have a condition called diverticulitis 3. Approximately 4-5% of patients with diverticulosis will develop acute diverticulitis, defined as clinically evident macroscopic inflammation of a diverticulum or diverticula. The most common symptom is abdominal pain, usually on the left side. You may also have fever, nausea, vomiting, chills, cramping, and constipation.
- If you start feeling symptoms of diverticulitis, call your doctor right away. Untreated diverticulitis can lead to dangerous complications. These include intestinal blockages and openings in the bowel wall.
About 25 percent of people with acute diverticulitis develop complications, which may include:
- An abscess, which occurs when pus collects in the pouch.
- A blockage in your colon or small intestine caused by scarring.
- An abnormal passageway (fistula) between sections of bowel or the bowel and bladder.
- Peritonitis, which can occur if the infected or inflamed pouch ruptures, spilling intestinal contents into your abdominal cavity. Peritonitis is a medical emergency and requires immediate care.
In serious cases, diverticulitis can lead to bleeding, tears, or blockages. Your doctor will do a physical exam and imaging tests to diagnose it. Treatment may include antibiotics, pain relievers, and a liquid diet. A serious case may require a hospital stay or surgery. About eighty-five percent of episodes of acute diverticulitis are uncomplicated (defined by absence of abscess, bowel obstruction, perforation, or fistula formation), although 15% to 30% of patients who develop acute diverticulitis experience a recurrence. Diverticulitis remains the leading indication for elective colon resection.
How do doctors treat diverticulosis ?
The goal of treating diverticulosis is to prevent the pouches from causing symptoms or problems. Your doctor may recommend the following treatments.
High-fiber diet
Although a high-fiber diet may not prevent diverticulosis, it may help prevent symptoms or problems in people who already have diverticulosis. A doctor may suggest that you increase fiber in your diet slowly to reduce your chances of having gas and pain in your abdomen.
Fiber supplements
Your doctor may suggest you take a fiber product such as methylcellulose (Citrucel) or psyllium (Metamucil) one to three times a day. These products are available as powders, pills, or wafers and provide 0.5 to 3.5 grams of fiber per dose. You should take fiber products with at least 8 ounces of water.
Medicines
Some studies suggest that mesalazine (Asacol) taken every day or in cycles may help reduce symptoms that may occur with diverticulosis, such as pain in your abdomen or bloating. Studies suggest that the antibiotic rifaximin (Xifaxan) may also help with diverticulosis symptoms.
Probiotics
Some studies show that probiotics may help with diverticulosis symptoms and may help prevent diverticulitis 4. However, researchers are still studying this subject. Probiotics are live bacteria like those that occur normally in your stomach and intestines. You can find probiotics in dietary supplements—in capsule, tablet, and powder form—and in some foods, such as yogurt.
For safety reasons, talk with your doctor before using probiotics or any complementary or alternative medicines or medical practices.
What are the complications of Diverticulitis ?
Diverticulitis is inflammation of one or a few diverticula in the same area of the colon (usually the sigmoid or descending colon). Diverticulitis occurs in less than 5% of people who have diverticulosis. People with diverticulitis characteristically present with the fairly sudden onset of pain in the abdomen, usually on the lower left side. Other common symptoms include fever, diarrhea and/or constipation, decreased appetite, nausea and fatigue.
People with diverticulitis can develop related complications including:
- Abscess – a collection of infected fluid outside of the intestinal/colon wall.
- Stricture – a narrowing of the colon in the area of diverticulitis
- Fistula – a connection between the bowel and nearby organs including the bladder or the vagina.
- Perforation – a hole in the colon that allows bowel contents to leak into the abdomen. This is the most serious complication of diverticulitis.
Bleeding can occur from a rupture in one of the vessels that lines a diverticulum. Bleeding from diverticulosis is a less common complication of diverticulosis than diverticulitis. Patients with this condition typically pass a large amount of red or maroon blood from the rectum. The bleeding tends to occur without warning and there is no associated abdominal pain. Most bleeding will stop on its own. However, endoscopic examination of the colon may be necessary to diagnose and treat the bleeding. Nuclear medicine bleeding scans (a type of radiology test) can also be used to identify the site of the diverticular bleeding if endoscopy does not or if bleeding is very severe. Occasionally, angiography (injection of dye into the abdominal blood vessels by a radiologist) is needed to identify and treat diverticular bleeding. In rare cases in which endoscopic or radiologic management fails to control the bleeding, surgery may be necessary to remove the part of the colon that is bleeding.
Figure 1. Diverticulitis
What causes diverticulitis
Doctors have not determined exactly what causes diverticular disease. They think it may be caused by not eating enough fiber. When you don’t eat enough fiber, your stools may not be as soft. You could get constipated. Constipation and hard stools increase the pressure in the bowel walls. This pressure may cause the diverticular pouches to form.
If you have diverticulosis, you may get flare-ups of diverticulitis from time to time. To prevent these, your doctor may suggest that you eat more fiber, drink plenty of fluids, and exercise regularly. This should help prevent the pouches from becoming infected or inflamed.
In the past, doctors thought people with diverticulosis should avoid certain foods. These included nuts, seeds, and popcorn. Research now suggests that these foods are not harmful, and will not cause diverticulitis flare-ups. Everyone is different, though. If you think certain foods are making your symptoms worse, you should stop eating them and see your doctor.
However, current literature data about the role of dietary pattern on the occurrence of colonic diverticulosis, diverticular disease and acute diverticulitis are still too conflicting. Recent findings showed that high-fiber diet does not prevent diverticulosis occurrence and nor was there an association between nut, corn or popcorn consumption and occurrence of diverticulosis, diverticular disease and acute diverticulitis 5. There seems to be a mild association between high alcohol intake and diverticulosis occurrence 5.
Higher red-meat consumption shows mild increased risk of acute diverticulitis, especially when consumed as unprocessed red meat (defined as consumption of ‘beef or lamb as main dish’, ‘pork as main dish’, ‘hamburger’ and ‘beef, pork or lamb as a sandwich or mixed dish’); higher consumption of poultry (viz. white meat) was not associated with risk of acute diverticulitis 5. Higher fish intake was associated with reduced risk of diverticulitis in age-adjusted model, but not after further adjustment for other potential confounders.
Other factors that could contribute to diverticular disease include 6:
- genetics
- lack of exercise
- obesity
- smoking
- decrease in healthy gut bacteria
- increase in disease-causing bacteria in your colon
- certain medicines, including steroids and nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen.
Individuals who are overweight or obese are more likely to have diverticulosis. Smoking may also increase the possibility of developing diverticulosis. Therefore, maintaining a healthy weight and abstaining from smoking may decrease the possibility of developing diverticulosis. Once diverticula have formed, they do not go away. And diverticular disease becomes more common as you age. Your risk starts increasing after you turn 40. Most people have it by the time they are 80 years old.
Can diverticulitis be prevented ?
People who eat a diet high in fiber are less likely to develop diverticulitis than those who eat little fiber (although, as noted above, a high-fiber diet does not appear to decrease the chances of developing diverticulosis) 7. Reducing the amount of red meat in the diet may also decrease the possibility of diverticulitis.
Table 1. Fiber-Rich Foods
| Grains | |
|---|---|
| Food and Portion Size | Amount of Fiber |
| 1⁄3–3⁄4 cup high-fiber bran ready-to-eat cereal | 9.1–14.3 grams |
| 1-11⁄4 cup of shredded wheat ready-to-eat cereal | 5.0–9.0 grams |
| 11⁄2 cup whole wheat spaghetti, cooked | 3.2 grams |
| 1 small oat bran muffin | 3.0 grams |
| Fruits | |
|---|---|
| Food and Portion Size | Amount of Fiber |
| 1 medium pear, with skin | 5.5 grams |
| 1 medium apple, with skin | 4.4 grams |
| 1⁄2 cup of raspberries | 4.0 grams |
| 1⁄2 cup of stewed prunes | 3.8 grams |
| Vegetables | |
|---|---|
| Food and Portion Size | Amount of Fiber |
| 1⁄2 cup of green peas, cooked | 3.5–4.4 grams |
| 1⁄2 cup of mixed vegetables, cooked from frozen | 4.0 grams |
| 1⁄2 cup of collards, cooked | 3.8 grams |
| 1 medium sweet potato, baked in skin | 3.8 grams |
| 1 medium potato, baked, with skin | 3.6 grams |
| 1⁄2 cup of winter squash, cooked | 2.9 grams |
| Beans | |
|---|---|
| Food and Portion Size | Amount of Fiber |
| 1⁄2 cup navy beans, cooked | 9.6 grams |
| 1⁄2 cup pinto beans, cooked | 7.7 grams |
| 1⁄2 kidney beans, cooked | 5.7 grams |
Studies show that people who maintain a healthy weight and/or exercise regularly are less likely to develop diverticulitis and diverticular bleeding than those who are overweight or who do not exercise 7. Avoiding smoking is also likely to help prevent diverticulitis, especially perforated diverticulitis 7.
Minimizing the use of non-steroidal anti-inflammatory drugs, such as ibuprofen and aspirin, may decrease the chances of developing diverticulitis. However, if you take aspirin for your heart or blood vessels, you should not stop aspirin without talking to your doctor. Opiate narcotics and corticosteroids also appear to predispose to diverticulitis.
Several different medications have been studied in hopes of preventing recurrent diverticulitis in patients who have had one or more attacks. Unfortunately, the best studied drug, mesalamine, has not reduced the likelihood of recurrent diverticulitis. There are only a few small studies on the use of probiotics (healthy bacteria) or rifaximin (a kind of antibiotic), so it isn’t clear if these medications might help reduce recurrent diverticulitis.
Foods to avoid with diverticulitis
Experts now believe you do not need to avoid certain foods if you have diverticulosis or diverticulitis.
In the past, doctors might have asked you to avoid nuts; popcorn; and seeds such as sunflower, pumpkin, caraway, and sesame. Recent research suggests that these foods are not harmful to people with diverticulosis or diverticulitis. The seeds in tomatoes, zucchini, cucumbers, strawberries, and raspberries, as well as poppy seeds, are also fine to eat.
Even so, each person is different. You may find that certain types or amounts of foods worsen your symptoms.
Diverticulitis symptoms
Diverticulosis normally does not have symptoms. It could cause mild cramps or pain in your lower abdomen, bloating, or constipation/diarrhea. Many other conditions can cause these symptoms, too.
The most common symptom of diverticulitis is severe abdominal pain. It is usually felt in the lower left side of your abdomen. It often comes on suddenly. It can start out mild and increase over several days.
Diverticulitis may also cause 9:
- Pain, which may be constant and persist for several days. Pain is usually felt in the lower left side of the abdomen, but may occur on the right, especially in people of Asian descent.
- constipation or less commonly diarrhea
- fevers and chills
- nausea or vomiting
- abdominal tenderness
You could find a large amount of blood in your stool or in the toilet. This could be a sign of diverticular bleeding. If you notice blood coming from your rectum, you should see your doctor right away.
How is diverticular disease diagnosed ?
If you are having symptoms, your doctor may check your abdomen for tenderness. He or she may ask you about your bowel habits, diet, and any medicines you take. They may want to do some tests to screen for diverticular disease:
- CT Scan. This type of X-ray allows your doctor to see if you have pouches in your colon. It can show if any are inflamed or infected. It is the most common test for diagnosing diverticular disease.
- Barium enema (also called a lower GI series). This test injects liquid barium into your rectum and colon. Then X-rays are taken. The barium makes your colon more visible on the X-rays.
- Flexible sigmoidoscopy. In this test, your doctor puts a thin, flexible tube with a light on the end into your rectum. The tube is connected to a tiny video camera. This allows your doctor to look at your rectum and the last part of your colon.
- Colonoscopy. In this procedure, the video camera and light go through your rectum and your whole colon. This allows your doctor to see the inside of your entire large intestine. Before the test, you are given medicine to make you relaxed and sleepy. A colonoscopy may be uncomfortable, but it is usually not painful.
Sometimes, diverticular disease is found when you are being tested for a different reason. This could include a routine screening to check for colorectal cancer or other digestive problems.
Diverticulitis treatment
Diverticulitis is typically treated with oral antibiotics and a liquid or low-residue diet until symptoms improve (similar to a low-fiber diet). However, some studies suggest that patients with mild diverticulitis who do not have an abscess or perforation and are otherwise healthy can be managed without antibiotics. People with severe diverticulitis (high fever, signs of severe infection) or with complications (abscess, perforation) require antibiotics and are usually treated in the hospital. There you can get intravenous (IV) antibiotics and the rest you need. Radiologic guided drainage (via a tube placed in the abdomen) may be needed to drain large abscesses. Surgery may be needed for cases that do not respond to medical management or for patients with perforation. A temporary colostomy (drainage of stool from the intestine into a bag on the outside of the abdomen) may be required during surgery for complicated diverticulitis. The colostomy is usually temporary.
How do doctors treat complications of diverticulitis ?
There are two main types of surgery:
- Primary bowel resection. The surgeon removes diseased segments of your intestine and then reconnects the healthy segments (anastomosis). This allows you to have normal bowel movements. Depending on the amount of inflammation, you may have open surgery or a minimally invasive (laparoscopic) procedure.
- Bowel resection with colostomy. If you have so much inflammation that it’s not possible to rejoin your colon and rectum, the surgeon will perform a colostomy. An opening (stoma) in your abdominal wall is connected to the healthy part of your colon. Waste passes through the opening into a bag. Once the inflammation has eased, the colostomy may be reversed and the bowel reconnected.
Your doctor may recommend the following to treat complications of diverticulitis:
Abscess
Your doctor may need to drain an abscess if it is large or does not clear up with antibiotics.
Perforation
If you have a perforation, you will likely need surgery to repair the tear or hole. Additional surgery may be needed to remove a small part of your colon if the surgeon cannot repair the perforation.
Peritonitis
Peritonitis requires immediate surgery to clean your abdominal cavity. You may need a colon resection at a later date after a course of antibiotics. You may also need a blood transfusion if you have lost a lot of blood. Without prompt treatment, peritonitis can be fatal.
Fistula
Surgeons can correct a fistula by performing a colon resection and removing the fistula.
Intestinal obstruction
If your large intestine is completely blocked, you will need emergency surgery, with possible colon resection. Partial blockage is not an emergency, so you can schedule the surgery or other corrective procedures.
How do doctors treat diverticular bleeding ?
Diverticular bleeding is rare. If you have bleeding, it can be severe. In some people, the bleeding may stop by itself and may not require treatment. However, if you have bleeding from your rectum—even a small amount—you should see a doctor right away.
To find the site of the bleeding and stop it, a doctor may perform a colonoscopy. Your doctor may also use a computerized tomography (CT) scan or an angiogram to find the bleeding site. An angiogram is a special kind of x-ray in which your doctor threads a thin, flexible tube through a large artery, often from your groin, to the bleeding area.
Colon resection
If your bleeding does not stop, a surgeon may perform abdominal surgery with a colon resection. In a colon resection, the surgeon removes the affected part of your colon and joins the remaining ends of your colon together. You will receive general anesthesia for this procedure.
In some cases, during a colon resection, it may not be safe for the surgeon to rejoin the ends of your colon right away. In this case, the surgeon performs a temporary colostomy. Several months later, in a second surgery, the surgeon rejoins the ends of your colon and closes the opening in your abdomen.
Diverticulitis diet
Mild cases of diverticulitis are usually treated with antibiotics and a diverticulitis diet, which includes clear liquids and low-fiber foods. More-severe cases typically require hospitalization.
A diverticulitis diet is a temporary measure to give your digestive system a chance to rest. Oral intake is usually reduced until bleeding and diarrhea subside.
A diverticulitis diet starts with only clear liquids for a few days. Examples of items allowed on a clear liquid diet include:
- Broth
- Fruit juices without pulp, such as apple juice
- Ice chips
- Ice pops without bits of fruit or fruit pulp
- Gelatin
- Water
- Tea or coffee without cream
As you start feeling better, your doctor will recommend that you slowly add low-fiber foods. Examples of low-fiber foods include:
- Canned or cooked fruits without skin or seeds
- Canned or cooked vegetables such as green beans, carrots and potatoes (without the skin)
- Eggs, fish and poultry
- Refined white bread
- Fruit and vegetable juice with no pulp
- Low-fiber cereals
- Milk, yogurt and cheese
- White rice, pasta and noodles
You should feel better within two or three days of starting the diet and antibiotics. If you haven’t started feeling better by then, call your doctor. Also contact your doctor if:
- You develop a fever
- Your abdominal pain is worsening
- You’re unable to keep clear liquids down
These may indicate a complication that requires hospitalization.
The diverticulitis diet has few risks. However, continuing a clear liquid diet for more than a few days can lead to weakness and other complications, since it doesn’t provide enough of the nutrients your body needs. For this reason, your doctor will want you to transition back to a normal diet as soon as you can tolerate it.
- Bhuket TP, Stollman NH. Diverticular disease of the colon. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger & Fordtran’s Gastrointestinal and Liver Disease. 10th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 121.[↩]
- Shah SD, Cifu AS. Management of Acute Diverticulitis. JAMA. 2017;318(3):291–292. doi:10.1001/jama.2017.6373 https://jamanetwork.com/journals/jama/article-abstract/2643748[↩]
- Stocci L. Diverticulitis. In: McNalley PR, ed. GI/Liver Secrets Plus. 5th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 47.[↩]
- Tursi A, Papa A, Danese S. Review article: the pathophysiology and medical management of diverticulosis and diverticular disease of the colon. Alimentary Pharmacology and Therapeutics. 2015;42(6):664–684.[↩]
- Dietary pattern and colonic diverticulosis. Current Opinion in Clinical Nutrition & Metabolic Care: September 2017 – Volume 20, Issue 5; p 409–413. http://journals.lww.com/co-clinicalnutrition/Abstract/2017/09000/Dietary_pattern_and_colonic_diverticulosis.17.aspx[↩][↩][↩]
- Diverticular Disease. American Academy of Family Physicians. https://familydoctor.org/condition/diverticular-disease[↩]
- Diverticulosis and Diverticulitis. American College of Gastroenterology. http://patients.gi.org/topics/diverticulosis-and-diverticulitis/[↩][↩][↩]
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. 2015–2020 Dietary Guidelines for Americans. 8th Edition. December 2015. https://health.gov/dietaryguidelines/2015/guidelines/[↩]
- Symptoms & Causes of Diverticular Disease. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/diverticulosis-diverticulitis/symptoms-causes[↩]




