Contents
What is dyshidrosis
Dyshidrosis also called pompholyx is a form of hand dermatitis where vesicles or bullae (blisters) are prominent. Dyshidrosis is a form of vesicular dermatitis of hands and feet, also called vesicular endogenous eczema and may be the same condition as dyshidrotic eczema. It is sometimes subclassified as cheiropompholyx (hands) and pedopompholyx (feet). Dyshidrosis causes itchy, dry skin. People also develop small, deep-seated blisters, usually on their hands. It’s also possible to develop blisters on your feet. Whether on your hands, feet, of both, the blisters are often very itchy and painful.
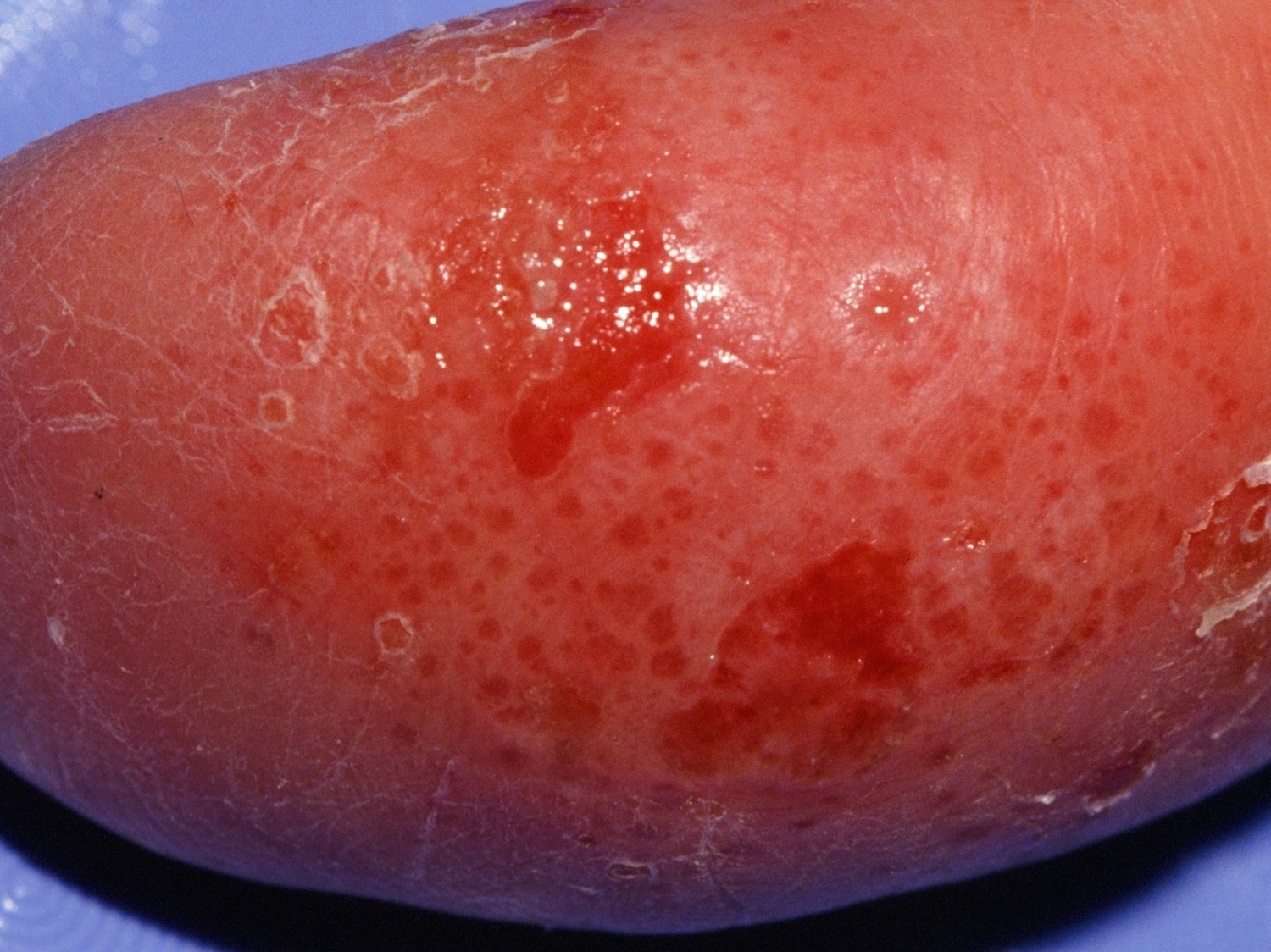
Tapioca-like vesicles on the hands and/or feet are typical (see Figures 1 to 3). Flares with lesions coming in crops are common. Coalescence into large blisters may rarely occur. Itching may be intense and may precede the vesicles. Scratching may alter the appearance and expose the skin to secondary infection. Sometimes, the red, scaly, eczematous areas of irritant hand dermatitis are present as well. Both conditions may occur and overlap.
When the blisters clear (usually in 2 or 3 weeks), the skin tends to be red, dry, and cracked. The blisters typically recur, sometimes before your skin heals completely from the previous blisters.
In severe cases, the blisters may be quite large and may spread to the backs of the hands, feet and limbs.
The skin can sometimes become infected. Signs of an infection can include the blisters becoming very painful and oozing pus or becoming covered in a golden crust.
The cause is thought to be allergic in nature and a variety of things can trigger it including contact with allergens, e.g. soluble oils, perfumes, balsum.
The people most likely to get dyshidrosis (pompholyx) are adults aged 20 to 40, who often have one or more of the following.
Treatment for dyshidrosis most often includes creams or ointments that you rub on the affected skin. In severe cases, your doctor may suggest corticosteroid pills, such as prednisone, or injections.
Certain medical condition: You have a higher risk of developing Dyshidrosis (pompholyx) if you have any of the following:
- Atopic dermatitis (eczema) or blood relatives who have eczema
- Contact dermatitis, especially an allergy to nickel
- Dyshidrotic eczema in your family
- Hay fever
Sweaty or moist hands: Some people have flares every spring or summer when the temperature rises.
Wet hands throughout the day or work with certain substances: Dyshidrosis (pompholyx) is more common in people who:
- Immerse their hands in water frequently during the day, such as healthcare workers, hair stylists, and florists
- Work with cement
- Work with chromium, cobalt, or nickel
Patients receiving immunoglobulin therapy may get Dyshidrosis (pompholyx)
If you are receiving intravenous (IV) immunoglobulin and develop blisters on your hands or feet after an infusion, be sure to tell your doctor. This is likely Dyshidrosis (pompholyx). A few patients develop this eczema after receiving immunoglobulin therapy.
The eczema can worsen with each infusion, so early diagnosis is important. With treatment, most cases of Dyshidrosis (pompholyx) due to this therapy are treated successfully. This will allow you to continue receiving immunoglobulin therapy.
Common triggers
Some people find that their Dyshidrosis (pompholyx) flares at certain times, such as periods of:
- Intense stress or worrying
- Warm weather, when heat and humidity rise
- Wet work (having wet hands frequently throughout the day)
There is no cure for dyshidrosis (pompholyx), so people can have flares. For many people, dyshidrosis (pompholyx) flares when they’re under a lot of stress, temperatures rise (such as in spring or summer), or their hands stay wet for long periods of time.
Dyshidrosis (pompholyx) flares range from mild to debilitating. A severe flare on your feet can make walking difficult. Having many blisters on your hands can make it difficult to work and perform everyday tasks like shampooing your hair and washing dishes.
Dyshidrosis (pompholyx) most often affects young adults.
- It is more common in females than males.
- Many of them report palmoplantar hyperhidrosis.
- There is a personal or family history of atopic eczema in 50%.
Finger 1. Dyshidrosis fingers
Finger 2. Dyshidrosis hands (cheiropompholyx)
Finger 3. Dyshidrosis feet (pedopompholyx)
Dyshidrosis causes
While researchers have discovered that some people are more likely to get dyshidrosis (pompholyx), the cause is still unknown and most likely multifactorial.
The cause may be a complex reaction that happens in your immune system. It can be associated with a similar skin disorder called atopic dermatitis, as well as with allergic conditions, such as hay fever. Eruptions may be seasonal in people with nasal allergies.
In many cases it appears to be related to sweating, as flares often occur during hot weather, humid conditions, or following emotional upset. Other contributing factors include:
- Genetics
- Contact with irritants such as water, detergents, solvents and friction
- Association with contact allergy to nickel and other allergens
- Inflammatory dermatophyte (tinea) infections (when it is known as a dermatophytid)
- Adverse reaction to drugs, most often immunoglobulin therapy.
If you think that you might have dyshidrosis (pompholyx), an accurate diagnosis and proper treatment are important.
Aggravating factors
As in other forms of hand dermatitis, dyshidrosis is aggravated by contact with irritants such as water, detergents and solvents. Contact with them must be avoided as much as possible and protective gloves worn to prevent additional irritant contact dermatitis.
People with dyshidrosis that are found to be allergic to nickel must try to avoid touching nickel items.
Aggravating factors for dyshidrosis include:
- Stress. Dyshidrosis appears to be more common during times of emotional or physical stress.
- Exposure to certain metals. These include cobalt and nickel — usually in an industrial setting.
- Sensitive skin. People who develop a rash after contact with certain irritants are more likely to experience dyshidrosis.
- Atopic eczema. Some people with atopic eczema may develop dyshidrotic eczema.
Dyshidrosis prevention
Because the cause of dyshidrosis is generally unknown, there’s no proven way to prevent this condition. You may help prevent the condition by managing stress and avoiding exposure to metal salts, such as cobalt and nickel.
Good skin care practices may help protect the skin as well. These include:
- Using mild cleansers and lukewarm water to wash your hands and drying your hands well
- Moisturizing regularly
- Wearing gloves
Dyshidrosis outlook (prognosis)
Some people have one mild outbreak that clears without treatment. It may recur in hot weather or after a period of stress, and in some patients is recalcitrant. Treatment can help control dyshidrosis (pompholyx), which cannot be cured.
Dyshidrosis complications
Secondary bacterial infection with Staphylococcus aureus and/or Streptococcus pyogenes is common in pompholyx, and results in pain, swelling and pustules on the hands and feet.
Dyshidrosis signs and symptoms
Dyshidrosis skin disease appears suddenly. For most people, the first sign is deep-seated blisters on their hands. Some people feel an itchy or burning sensation before the blisters appear.
When involving the distal finger adjacent or proximal to the nail fold, it can result in paronychia (nail fold swelling) and nail dystrophy with irregular pitting and ridges.
If you have dyshidrosis (pompholyx), you’ll likely notice:
- Small blisters that vary in size on your palms and sides of your fingers (and/or soles)
- A rash and scaly skin where blisters appear
- Excessive sweating where you have blisters
- An tching or burning feeling on blistered skin (and sometimes before the blisters appear)
- Pain where you have blisters
The blisters usually clear in 2 to 3 weeks — or sooner with treatment. As the blisters clear, the skin is often dry and cracked. It may peel.
If you have frequent dyshidrosis (pompholyx) flares, the skin can start to thicken, feel scaly, and develop deep, painful cracks.
Signs of infection
An infection can develop where you have dyshidrosis (pompholyx). A staph infection is most common. Signs of a staph infection include:
- Pain
- Swelling
- Crusting
- Pus-filled blisters
Dyshidrosis diagnosis
When dyshidrosis (pompholyx) flares, your doctor can diagnose it by looking at your skin.
Your doctor will also ask about your medical history, work, hobbies, and recent stress level.
If your doctor thinks that the dyshidrosis (pompholyx) could be due to an allergy, an allergy test called patch testing may be recommended. During patch testing, small amounts of substances that you may be allergic to are placed on your skin — often the skin on your back.
- If suspicious of a fungal infection (tinea pedis), skin scrapings should be taken for mycology.
- Patch testing is indicated in chronic or atypical cases.
- Skin biopsy is rarely necessary. It shows spongiotic eczema.
Dyshidrosis treatment
Dyshidrosis is challenging to treat. Topical therapy is relatively ineffective because of the thick horny layer of skin of palms and soles.
Your treatment plan will be designed to treat your signs and symptoms. You may be responsible for doing much of the treatment at home.
It is important to carefully follow your treatment plan, which may include several of the following:
- Soaks and cool compresses: Soaks or cool compresses using dilute potassium permanganate, aluminium acetate or acetic acid that you apply 2 to 4 times a day can be very effective for drying blisters. You apply these for 15 minutes at a time. After each soak or cool compress, you’ll likely need to apply a medicated cream or ointment, such as a corticosteroid.
- Cold packs
- Corticosteroid that you apply to your skin: This can reduce the inflammation and clear the blisters.
- Soothing emollient lotions and creams
- Potent antiperspirants applied to palms and soles at night
- Protective gloves should be worn when doing wet or dirty work
- Well-fitting footwear, with 2 pairs of socks to absorb sweat and reduce friction
- Anti-itch medicine: An antihistamine pill or other anti-itch medicine can reduce scratching. Anything you can do to reduce scratching is helpful because scratching tends to worsen dyshidrosis (pompholyx).
- Pramoxine: A cream or lotion containing this can relieve itch and pain.
- Moisturizer or a barrier repair cream: Your doctor will recommend a moisturizer or barrier repair cream. These can reduce dryness and flares of dyshidrosis (pompholyx).It’s important to apply the product after each shower, bath, and hand washing.
- Medicine to treat an infection: The skin with dyshidrosis (pompholyx) can get infected. Before prescribing this medicine, your doctor will first determine what type of infection you have. Infection may cause dyshidrotic eczema to linger. Having an infection can stop dyshidrosis (pompholyx) from clearing.
In one study, researchers found that about 33% of patients who had dyshidrosis (pompholyx) on their hands got rid of the dyshidrosis (pompholyx) only after treating an infection on their feet.
When treatment fails to clear dyshidrosis (pompholyx) or you have severe dyshidrosis (pompholyx)
If the above treatments fail to work or you have severe Dyshidrosis (pompholyx), your dermatologist may recommend one of the following:
Prescription medicines
- Ultrapotent topical corticosteroid creams applied to new blisters under occlusion, and ointments applied during the inflamed dry phase.
- Immune-suppressing ointments. Medications such as tacrolimus (Protopic) and pimecrolimus (Elidel) may be helpful for people who want to limit their exposure to steroids. A side effect of these drugs is an increased risk of skin infections.
- Oral antistaphylococcal antibiotics for secondary infection
- Topical and oral antifungal agents for confirmed dermatophyte infection
- In patients with hyperhidrosis, probanthine or oxybutynin is worth trying.
- In severe cases, immune modulating medicines are indicated. These include: methotrexate, mycophenolate mofetil, azathioprine and ciclosporin.
- Where available, alitretinoin is used for resistant chronic disease affecting the hands when other treatments haven’t worked.
- Botulinum toxin: These injections, which are given in a dermatologist’s office, bring some patients relief because botulinum toxin temporarily relaxes the muscles and stops excessive sweating. Botulinum toxin is FDA approved to treat wrinkles and excessive sweating in the underarms — but not Dyshidrosis (pompholyx). It’s legal to prescribe a medicine for a condition other than its FDA-approved use. This is called “off-label” use, which can be very helpful for some patients.
- Draining large blisters in the office. Draining blisters is safe and effective when performed in a dermatologist’s office, but you should not drain your own blisters. Attempting this at home can lead to an infection, which can worsen dyshidrosis (pompholyx) and prevent clearing.
- Corticosteroid that works throughout the body: For a severe case, a corticosteroid pill or injection may be prescribed. Short courses of systemic corticosteroids, eg prednisone or prednisolone, for flare-ups
- Light treatments: This treatment exposes the skin with dyshidrosis (pompholyx) to ultraviolet (UV) light for a prescribed amount of time. Under a dermatologist’s care, light treatment can be a safe and effective treatment for dyshidrosis (pompholyx). In one study, more than 90% of patients report good to excellent results after 6 to 8 weeks of treatment. It’s extremely important to get these treatments at a hospital, clinic, or your dermatologist’s office. Trying to treat your skin by using a tanning bed is not recommended.
- Changing your diet: Sometimes, dyshidrosis (pompholyx) continues to flare despite all you do to treat it. If this happens, your dermatologist may recommend a change to your diet. Eliminating foods that contain nickel or cobalt helps some people. Many foods contain nickel or cobalt. If you are allergic to either, your dermatologist can tell you how to change your diet.
Dyshidrosis home remedies
Wash skin with dyshidrosis (pompholyx) gently: When washing, you’ll want to:
- Remove rings: Always remove these before washing your hands. If the skin beneath your ring gets wet and stays damp, the dyshidrosis (pompholyx) can flare.
- Use lukewarm water: Using lukewarm water every time can help prevent flares.
- Wash with mild, fragrance-free cleansers: Skip the antibacterial soaps, waterless hand sanitizers, and deodorant soaps, which can cause Dyshidrosis (pompholyx) to flare.
Even when the eczema clears, you’ll want to continue gently washing the skin that had eczema. This will help prevent flares.
Apply moisturizer frequently: You’ll want to apply moisturizer:
- After washing
- Throughout the day when your skin feels dry. Dermatologists often recommend using a product called a barrier repair cream that contains dimethicone. This product allows skin to breathe. It also helps relieve itch and creates a barrier to protect you from things that can irritate your skin.
If you opt to use another moisturizer, make sure it is:
- Thick and creamy
- Fragrance free (“Fragrance free” and “unscented” are different.)
- Something you like enough to use frequently
Avoid moisturizer that is thin and runny as are many lotions. Lotions contain a lot of water, which can worsen Dyshidrosis (pompholyx).
Learn to manage stress really well:
Some patients find that they can clear their skin by practicing a stress-reduction technique and treating their skin as directed.
It can be helpful to continue finding ways to relieve your stress. Many people say that the dyshidrosis (pompholyx) returns when they feel stressed.
Try to avoid scratching:
Anything you can do to reduce scratching is helpful because scratching tends to worsen dyshidrosis (pompholyx).
Avoid dry environments and hot conditions that cause you to sweat a lot: Both heat and dryness can trigger flares.
Ask your doctor if something could be triggering your dyshidrosis (pompholyx). If the dyshidrosis (pompholyx) won’t clear, you may:
- Have an allergy
- Be irritating your skin
Your doctor can ask questions to find out if something is irritating your skin. Allergy testing can find out whether you have allergies.
Avoid what causes an allergic reaction and what irritates your skin. If either allergens or irritants are the problem, avoiding them may be necessary to clear your skin — and keep it clear.
Wear gloves to protect your hands:
Many things that touch your skin can cause Dyshidrosis (pompholyx) to flare. Water, detergents, and household cleaners are a few.
To protect your hands, you’ll want to put gloves on before you get your hands wet and before touching something that irritates your skin. Doctors recommend the following:
- Wear 100% cotton gloves (hands won’t get wet)
- Wear 100% cotton gloves under waterproof gloves (wet work)
Remove your rings:
Rings can irritate your sensitive skin. To reduce irritation, dermatologists recommend that you remove your rings BEFORE:
- Washing your hands
- Applying moisturizer
- Going to sleep
Wear moisture-wicking socks:
If you have dyshidrotic eczema on your feet, this will help keep your feet dry.