Contents
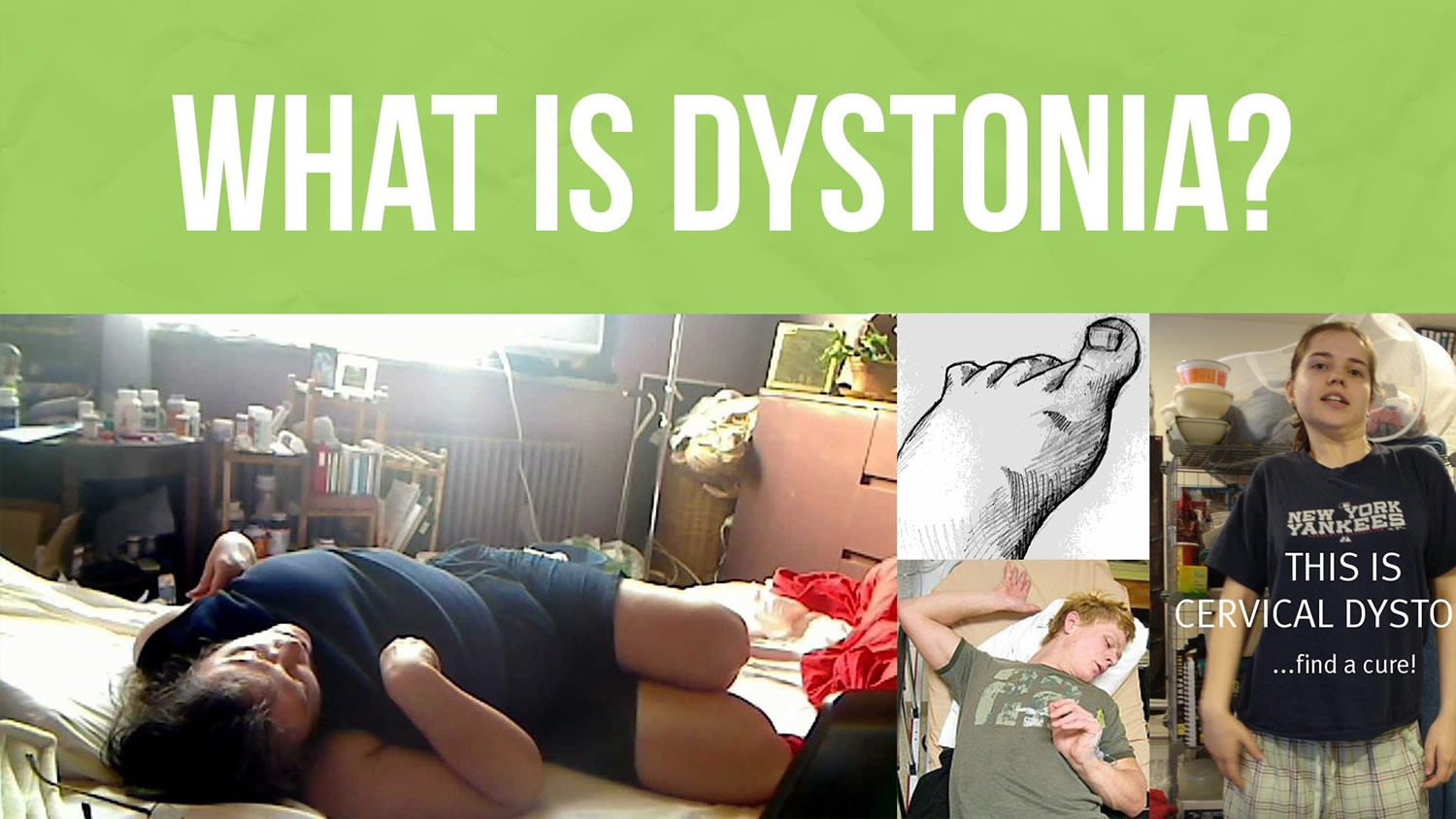
What is dystonia
The dystonias are movement disorders in which sustained muscle contractions and muscle spasms cause twisting and repetitive movements or abnormal postures. The muscle spasms and contractions may either be sustained or may come and go. The movements, which are involuntary and sometimes painful, may affect a single muscle; a group of muscles such as those in the arms, legs, or neck; or the entire body. Early symptoms may include deterioration in handwriting, foot cramps, or a dragging foot after running or walking some distance. Other possible symptoms are tremor and voice or speech difficulties.
Movements are often repetitive and cause unusual, awkward and sometimes painful postures. Tremor (shaking) can also be a characteristic of some types of dystonia.
Dystonia is thought to be a neurological condition (caused by underlying problems with the brain and nervous system). However, in most cases, brain functions such as intelligence, memory and language remain unaffected. About half the cases of dystonia have no connection to disease or injury and are called primary or idiopathic dystonia. Of the primary dystonias, many cases appear to be inherited. Dystonias can also be symptoms of other diseases, some of which may be hereditary. Dystonia can occur at any age, but is often described as either early, or childhood, onset versus adult onset.
Although there are several forms of dystonia and the symptoms may outwardly appear quite different, the element that all forms share is the repetitive, patterned, and often twisting involuntary muscle contractions. Dystonia is a chronic disorder, but the vast majority of dystonias do not impact cognition, intelligence, or shorten a person’s life span.
Dystonia is generally uncommon, although it’s one of the more common neurological conditions. Estimates suggest that no fewer than 300,000 people are affected in the United States and Canada alone.
Dystonia can affect men, women and children of all ages and backgrounds. It can be difficult to diagnose, and there may be many people with the condition who remain undiagnosed.
Dystonia causes varying degrees of disability and pain, from mild to severe. There is not yet a cure, but multiple treatment options exist and scientists around the world are actively pursuing research toward new therapies.
Dystonia types
Dystonia can affect only one muscle or a group of muscles. There are five main types of dystonia:
- Focal dystonia – where a single region, such as the hand or eyes, is affected. Cervical dystonia, blepharospasm (abnormal twitch of the eyelid), laryngeal dystonia and writer’s cramp are all examples of focal dystonia. If it only affects someone during specific activities, such as writing, it’s described as task-specific dystonia.
- Segmental dystonia – where two or more connected regions of the body are affected. Cranial dystonia (blepharospasm affecting the lower face and jaw or tongue) is an example.
- Multifocal dystonia – where two or more regions of the body that aren’t connected to each other, such as the left arm and left leg, are affected.
- Generalized dystonia – where the trunk and at least two other parts of the body are affected. The legs may or may not be affected.
- Hemidystonia – where one entire side of the body is affected.
About 90% of all cases are either cervical dystonia (which affects the neck muscles) or blepharospasm (which affects the eyelids). These are both focal dystonias that tend to develop later in life. They don’t usually get any worse and no other muscles are affected.
Dystonia prognosis
Dystonia is an unpredictable condition. It tends to progress slowly and the severity of a person’s symptoms can vary from one day to another. Focal dystonia usually progresses gradually over a period of about five years and then doesn’t get any worse.
The initial symptoms can be very mild and may be noticeable only after prolonged exertion, stress, or fatigue. Dystonias often progress through various stages. Initially, dystonic movements are intermittent and appear only during voluntary movements or stress. Later, individuals may show dystonic postures and movements while walking and ultimately even while they are relaxed. Dystonic motions may lead to permanent physical deformities by causing tendons to shorten.
Sometimes, a person’s symptoms improve or disappear completely. This is known as total remission and it’s thought to occur in around 5-10% of people.
Total remission is more likely in cases of secondary dystonia, such as dystonia that occurs after a stroke. If someone has another underlying condition, such as Parkinson’s disease, the symptoms of dystonia are more likely to last for the rest of their lives.
Is dystonia fatal?
In the overwhelming majority of people with dystonia, it does not shorten life expectancy or result in death. In very severe generalized dystonia that affects many body areas, there can be problems that arise secondary to the dystonia that may cause life-threatening conditions. However, these instances are quite rare and usually treatable. Dystonia does occur as a symptom of many degenerative disease, some of which do impact mortality, but the dystonia itself does not shorten life span.
My dystonia symptoms have been stable for five years. Should I expect them to remain the same, or will they progress?
After a period of about three to five years after symptoms begin, dystonia will often stabilize and not progress to other body areas. However, dystonia symptoms are somewhat notorious for changing subtly over time and varying in intensity depending on a number of factors (for example, fatigue, stress level, menstruation).
As a general rule, the older a person is when dystonia develops, the less likely it will progress to multiple body areas. The younger a person is when dystonia develops, the more likely that it will progress to multiple body parts over time, particularly if the dystonia begins in a leg. In those patients, the disorder will typically stabilize within a few years and not progress any further. Children who first develop dystonia in the neck or arm may experience little, if any, progression beyond those areas, and kids who develop paroxysmal dystonia or dyskinesias may have symptoms that plateau in mid-childhood, worsen during puberty, and improve significantly in adulthood.
In some dystonia patients, especially those with cervical dystonia, there may be a temporary remission that lasts months or years.
The bottom line, unfortunately, is that dystonia is unpredictable. There is no guarantee that the disease will not progress even after a period of stabilization, and no way to predict how symptoms may change over time. However, experienced physicians will be aware that symptoms may change subtly over time, and there are a variety of treatment options that can be used to adjust the treatment plan.
Can dystonia go into remission and reappear?
Yes, but remission happens only rarely. It was once believed that 10% of people with dystonia might have such a spontaneous remission. It is probably much less than that. More frequently, instead of a true remission, the severity of dystonic postures may be reduced for months or years in a small minority of patients. Nearly everyone has some degree of day-to-day fluctuation in the severity of his or her symptoms For a few, the fluctuation may be so much better and for such a long time that it seems like a remission. However, a careful exam will still reveal some involuntary postures. Those who do seem to have a true remission are likely to again have symptomatic dystonia sometime later.
What are the chances of a child with generalized dystonia affecting mainly the feet and legs developing other types of dystonia, like cervical dystonia?
When dystonia begins in childhood involving the legs and the feet, it is quite common for it to progress to involve the trunk, the arms, and even the neck. This is particularly true for early-onset generalized dystonia. Children who first develop symptoms in the arm or neck typically do not experience widespread progression to other areas. Early identification of symptoms and prompt treatment can often minimize the impact of dystonia on a child’s mobility and quality of life.
After years of having dystonia, is the skeletal system affected in any way?
Dystonia does not have a primary effect on bones, but because of the abnormal postures that result from dystonic spasms, unusual mechanical stress may be placed on bones. For instance, if someone has a severe dystonia that involves a very sustained posture in one position, he/she may get a shortening of the ligaments and tendons so that the joint becomes “contracted” and can no longer move freely through a full range of motion. With time, this might be expected to cause excessive wear on the affected bones. Even short of a contracture, some bones may experience excessive wear because of such abnormal mechanical stresses. Bone changes, however, are not usually symptomatically important to people with dystonia. It is more often the case that we are concerned about dystonia’s effect on muscles and related supportive tissues as they influence posture.
Can dystonia affect muscles such as the heart or diaphragm, or other organs?
Dystonia affects muscles that can be controlled voluntarily mostly the skeletal muscles. Dystonia does not affect smooth muscles, such as the heart. However, dystonia can affect breathing in several ways. Severe neck dystonia can cause difficulty breathing when the upper airway is impacted. Dystonia involving the vocal cords can potentially cause shortness of breath when the vocal cords close tight, but in general the tightness is present primarily when speaking. The act of breathing involves muscles between the ribs and a large muscle called the diaphragm. Dystonia can cause stiffness in the muscles between the ribs and can cause a sensation or shortness of breath. Occasionally, the diaphragm can also be affected. Finally, when a person with dystonia has involvement of the spine, twisting of the torso can limit how much the lungs can expand when breathing, and this can potentially cause shortness of breath.
The bladder is made up of smooth muscle, and therefore not affected by dystonia. However, the muscles around the opening of the bladder (the external sphincter) can very rarely become involved, resulting in difficulty of passing urine. This seems to occur most often dystonia that is a symptom of another neurological disease such as Parkinson’s disease.
How does dystonia affect the nervous system?
Dystonia disrupts the nervous system s ability to allow the brain and the muscles to communicate. The body s ability to control muscle movements is very complicated and involves many areas in the brain. The area of the brain that is believed to be most affected by dystonia is called the basal ganglia. The basal ganglia are a deep region of the brain that monitors the speed of movement and controls unwanted movements. The basal ganglia are responsible for sending signals to the muscles instructing them when to move and when to stop moving. For reasons scientists don t yet understand, the basal ganglia instructions to the muscles become irregular and chaotic, resulting in the unwanted muscle movements and contractions.
In addition, as researchers began learning more about task-specific dystonias such as the various forms that affect musicians, it became clear that there is a sensory component to dystonia symptoms. Not only does the brain send irregular messages to the brain, but the affected muscles send chaotic messages back to the brain the nervous system is overtaken by a self-perpetuating cycle of abnormal communication. This revelation led to a new perspective that suggested that the brain and muscles could be retrained to communicate through physical therapy. Rehabilitation is an active area of research that is likely to continue to provide direction for new therapies and may be particularly relevant to the treatment of secondary dystonias.
What causes dystonia
Exactly how dystonia develops remains uncertain, but it’s thought to be caused by a problem with the part of the brain that controls muscle movement (the basal ganglia).
Dystonia with no identifiable cause or if the cause is genetic mutation, it’s described as primary dystonia.
Secondary dystonia is where dystonia occurs as a symptom of an underlying condition or injury. Common causes include stroke, brain injury, encephalitis and Parkinson’s disease.
Primary dystonia
Most people with primary dystonia don’t have an identified cause. A minority of cases are associated with genetic mutations, which usually begin in childhood.
There are currently over 12 types (or sub-types) of dystonia linked to genetic mutations, including generalized dystonia, dopa-responsive dystonia and paroxysmal dystonia.
The genes responsible for these types of dystonia are passed down through families in a pattern that’s known as autosomal dominant. This means if you have one of these abnormal genes, there’s a one in two chance your children will inherit that gene and develop dystonia.
Secondary dystonia
Secondary dystonia, also known as acquired dystonia, can have a wide range of causes, including:
- Parkinson’s disease – a neurological condition caused by the lack of a neurotransmitter called dopamine
- Huntington’s disease – a genetic condition that can lead to psychiatric problems and difficulties with behaviour, feeding, communication and abnormal movements
- Wilson’s disease – a genetic condition that leads to a build-up of copper in the body’s tissues
- Multiple sclerosis (MS) – a condition caused by damage to the nervous system
- Cerebral palsy – a condition caused by brain damage that occurs before or soon after birth
- Certain medications – such as antipsychotics (used to treat certain mental health conditions) or anticonvulsants (used to treat epilepsy) which can cause dystonia in a small number of people
- Infections – such as HIV or encephalitis
- Injury – to the skull or spine
- Brain tumors
- Stroke– a serious medical condition, where the blood supply to part of the brain is cut off
- Poisoning – such as carbon monoxide poisoning
Can childhood illnesses such as measles cause dystonia?
Rarely is dystonia linked to the occurrence of a childhood illness. Dystonia can arise from birth injury, which can be associated with rare childhood metabolic disorders or following a brain infection such as encephalitis. Subacute sclerosing panencephalities is a rare complication of measles that has been associated with dystonia. In most instances, however, uncomplicated measles does not cause dystonia. The disorders mentioned above usually have other associated features, including cognitive problems, seizures, or other neurologic abnormalities, and do not typically cause only dystonic symptoms.
Sometimes trauma to the head or neck area may cause slippage of the bony spine, particularly in a child. This is called atlantoaxial dislocation and may result in symptoms that resemble spasmodic torticollis but is, in fact, not dystonia but an orthopedic problem. This condition may be called infant torticollis.
If a person is diagnosed with primary dystonia but there is no family history, does that mean it’s not genetic?
The absence of a clear family history of dystonia does not rule out a hereditary or genetic basis for childhood-onset or adult-onset dystonias that are diagnosed as primary (meaning that they cannot be attributed to trauma, medications, or another disease or condition) this applies to generalized and focal primary dystonias. Most primary forms of dystonia, including those for which no genes have yet been discovered, are believed to be caused by a combination of genes and other unknown factors. Those genes and factors have simply not been identified at this time.
It’s possible that breakthroughs in genetics may soon allow the diagnosis of hereditary dystonia even in families without a clear family history.
Can dystonia come about overnight? Are there any warning signs?
Dystonia generally develops gradually. Exceptions include rapid-onset dystonia-parkinsonism (which may develop over days or hours) and the acute dystonic reactions associated with certain antipsychotic drugs.
Symptoms of dystonia may begin very mildly. Subtle facial or jaw spasms, or difficulty chewing may suggest early face or jaw dystonia. Changes in the cadence or pitch of speech may be early signs of laryngeal dystonia/spasmodic dysphonia. Mild jerky head movements, stiff neck, or local neck discomfort may occur in the early stages of cervical dystonia. Cramping or fatiguing of the hands during writing, other manual activities, or walking may suggest limb dystonia. Similarly, children who develop generalized dystonia may first complain of cramps in a leg or a foot turning in. Sometimes a focal dystonia may arise directly following injury to that body region.
Sensory symptoms may precede focal dystonia in some people. Common examples would be a gritty sensation in the eye preceding blepharospasm and irritation of the throat preceding laryngeal dystonia/spasmodic dysphonia.
Dystonia complications
Depending on the type of dystonia, complications can include:
- Physical disabilities that affect your performance of daily activities or specific tasks
- Functional blindness from dystonia that affects your eyelids
- Difficulty with jaw movement, swallowing or speech
- Pain and fatigue, due to constant contraction of your muscles
- Depression, anxiety and social withdrawal
Dystonia symptoms
The symptoms of dystonia can vary, depending on the type of dystonia and when it develops.
In early-onset dystonia, the symptoms begin during childhood or early adulthood. Symptoms usually start in the legs or arms, before spreading to other limbs and sometimes the upper part of the body.
Dystonia that starts as an adult (late-onset) usually begins in the head, neck or one of the arms, and doesn’t progress to affect other parts of the body.
Early-onset dystonia
Generalized dystonia
Generalized dystonia refers to dystonia that is not limited to a single part of the body but affects multiple muscle groups throughout the body. Generalized dystonia typically affects muscles in the torso and limbs, and sometimes the neck and face. Patients have difficulty moving their bodies freely and controlling their body movements. It is important to note that dystonia does not target vital organs such as the heart.
Generalized dystonia often begins around the time a child reaches puberty. Generalized dystonia often begins in an arm or foot and progresses over months or years to affect additional areas of the body. If untreated, dystonia symptoms can cause orthopedic issues in the muscles and joints. Dystonia can cause pain, but not always. Early treatment can often slow or suppress symptom progression.
Generalized dystonia is frequently misdiagnosed, sometimes mistaken for Parkinson’s disease, tremor, cerebral palsy, orthopedic and structural conditions, and behavioral disorders or mental illness.
Symptoms of generalized dystonia can include:
- muscle spasms, for example in the torso or limbs
- having an abnormal, twisted posture, , with or without pain
- a foot, leg or arm turning inwards
- body parts jerking rapidly
- unusual walking with bending and twisting of the torso
- progression of symptoms leading to areas of the body remaining in sustained or fixed postures
In extreme cases, the development of increasingly frequent or continuous episodes of severe generalized dystonia causes a medical emergency called status dystonicus. If untreated, this rare condition can cause life-threatening complications. Status dystonicus is a treatable condition and, with prompt medical attention, symptoms typically can be brought under control.
Generalized dystonia cause
There are multiple causes for generalized dystonia. Dystonia may result from changes in certain genes, birth injury, exposure to certain drugs, head injury, infection, and other secondary causes. Dystonia symptoms that occur only on one side of the body strongly suggest a secondary cause. Dystonia resulting from secondary causes often occurs with additional movement and neurological symptoms, depending on the nature and severity of injury to the nervous system.
For many people who develop generalized dystonia, there is no identifiable cause.
Genetics
There are several genetic subtypes of generalized dystonia. For example:
- Early Onset Generalized Dystonia (DYT1/TOR1): DYT1 dystonia typically begins around age 10 years with the twisting of a foot or arm. Symptoms tend to begin in one body part and progress to involve additional limbs and the torso, but usually not the face or neck. In rare cases, the vocal cord muscles are affected. The symptoms tend to be less severe the later in life they start and if they start in a hand or arm. About 30% of individuals who have the DYT1 genetic mutation will develop dystonia. If a person does not manifest symptoms before the age of 28 years, they will usually remain symptom free for life—even if they have the DYT1 mutation. The DYT1 mutation is responsible for about 90% of early onset generalized dystonia in individuals of Ashkenazi Jewish ancestry and up to about 50% of early onset generalized dystonia in other ethnicities.
- Adolescent Onset Generalized Dystonia (DYT6/THAP): DYT6 may occur as generalized dystonia or remain focal to a specific part of the body. Although the symptoms may resemble DYT1 dystonia, onset of DYT6 is usually in the late teens and symptoms are more likely to occur above the neck. Symptoms typically affect the muscles of the tongue, vocal cords, and face. Patients often have difficulty speaking. About 40% of individuals who have the mutation will develop dystonia.
Testing for DYT1, DYT6, and other known dystonia genes is available. There are also inherited dystonias for which the gene has not yet been found and therefore cannot be detected with existing genetic tests. A genetic counselor can help families understand what genetic testing may be appropriate.
Generalized dystonia treatment
Individuals with dystonia are encouraged to seek treatment from a neurologist or child neurologist with special training in movement disorders. A multidisciplinary team of expert medical professionals may be appropriate to tailor treatment to the needs of the patient.
A movement disorder specialist will develop a treatment plan that is customized to each patient. Most individuals require a combination of therapies. Treatment to lessen dystonia symptoms may include oral medications such as anticholinergics, baclofen, and benzodiazepines combined with botulinum neurotoxin injections, and/or surgical procedures such as deep brain stimulation (DBS). Research suggests that individuals who have generalized dystonia without additional neurological or movement symptoms (with the exception of tremor) tend to have the best outcomes from DBS as well those who are younger, test positive for the DYT1 dystonia gene mutation, and are treated relatively early in the dystonia progression.
Specific treatment may be needed to prevent loss of motion in the joints and/or curvature of the spine due to the dystonic postures. Complementary therapies to support overall functioning and wellness may include occupational therapy, physical therapy, speech/voice therapy, and other interventions depending on a person’s symptoms. Individuals with childhood onset generalized dystonia may have increased risk for depression so monitoring and addressing emotional and mental health is often an important part of the treatment strategy.
Dopa responsive dystonia
Dopa responsive dystonia is a type of generalized dystonia. Dopa-responsive dystonia is a broad term used to describe forms of dystonia that respond to a medication called levodopa, which is a synthetic form of a brain chemical called dopamine.
The symptoms of this type of dystonia usually begin during childhood, between the ages of 6 and 16 years. The most common symptom is an abnormal, stiff way of walking. The sole of the foot can bend upwards or the foot may turn outwards at the ankle.
Symptoms of dopa responsive dystonia are often worse later in the day and may increase with exertion.
Some people with dopa-responsive dystonia may also have muscle stiffness and spasms in their arms and torso.
Dopa responsive dystonia can usually be treated effectively with a drug called levodopa, and most often a combination of levodopa and carbidopa.
Causes of dopa responsive dystonia
The most commonly identified form of dopa-responsive dystonia is sometimes referred to as DYT5 dystonia. DYT5 dystonia is a dominantly inherited condition caused by mutations in the GTP cyclohydrolase 1 gene (GTP-CH1). (A dominantly inherited disorder means that only one parent need have the gene mutation in order for a child to inherit the disorder.) This gene plays a role in the production of dopamine. When this gene is impaired and cannot fully accomplish the task of producing dopamine, the levels of dopamine in the body are compromised and a person will begin to have problems with movement.
About 40% of dopa responsive dystonia patients do not carry the mutation in the GTP-CH1 gene associated with DYT5 dystonia. Other known inherited metabolic conditions may cause dopa responsive dystonia (including a mutation in the recessively inherited tyrosine hydroxylase gene (hTH), autosomal recessive deficiencies of GTP-CH1 and aromatic L-amino acid decarboxylase, and other defects of tetrahydrobiopterin metabolism). These recessively inherited conditions often affect cognitive function, which is not associated with the dominantly inherited dopa responsive dystonia. However, if the symptoms of dominantly inherited dopa responsive dystonia affect a patient’s speech, a cognitive problem may be presumed even though, in reality, the individual’s cognitive function is normal.
Myoclonus dystonia
Myoclonus dystonia is a rare type of segmental dystonia that affects the muscles in the arms, neck and torso. Rarely the face and legs are affected. Segmental dystonia affects two or more connected parts of the body. It causes sudden “jerk-like” spasms (myoclonus) that are similar to the spasms someone has when they get an electric shock. The symptom distribution of myoclonus dystonia is different from typical early onset generalized dystonia as it more often affects the upper body whereas typical early-onset dystonia usually affects the legs. Symptoms may be impacted by the consumption of alcohol. Non-movement related features may be present including depression, anxiety, obsessive-compulsive disorder, personality disorders, and panic attacks. The age of onset is in the first or second decade of life, although some cases of adult-onset have been reported. Most frequently, the disorder appears to be slowly progressive for a few years after onset, stabilizes, and then fluctuates slightly over the years or shows a mild spontaneous improvement.
Myoclonus dystonia causes
Myoclonus dystonia is often a familial disorder seen in successive generations. Scientists have uncovered that multiple mutations in the epsilon-sarcoglycan gene associated with this form. The function of this gene is still unknown. This disorder is inherited dominantly but only a percentage of individuals who inherit the mutation develop symptoms.
Sporadic cases may arise, but it is unclear at this time if these cases are actually genetic in which the family history is “masked” by reduced penetrance.
Myoclonus dystonia diagnosis
Diagnosis of myoclonus dystonia is based on family history from the affected individual and the physical and neurological examination.
If the condition presents with both myoclonus and dystonia, it may be classified as myoclonus dystonia or “hereditary dystonia with lightning jerks responsive to alcohol.” If dystonia is not present or is only a minor component, it may be classified as “hereditary essential myoclonus.” Experts in the movement disorder field are aware of the different diagnoses, and debate continues as to whether all classifications may be an expression of a single genetic disorder.
Myoclonus dystonia treatment
Medications that may be helpful for the treatment of myoclonus dystonia include benztropine, clonazepam, neuroleptics, dopamine agonists, and perhaps gamma-hydroxybutyrate (GHB). A striking feature in some people with myoclonus dystonia is the alleviation of symptoms upon ingestion of alcohol, but response varies greatly even within individual families. Deep brain stimulation surgery is emerging as a promising option.Complementary therapies may be explored, especially physical therapy, aquatic physical therapy, and regular relaxation practices.
Paroxysmal dystonia
Paroxysmal dystonia is a rare type of dystonia, where muscle spasms and unusual body movements only occur at certain times. The sudden onset of symptoms is known as an attack.
The symptoms of paroxysmal dystonia can be similar to the symptoms of an epileptic fit. However, during an attack, only your muscles will be affected. Unlike epilepsy, you won’t lose consciousness and you’ll remain fully aware of your surroundings. Attacks can last from a few minutes to several hours.
Between attacks most people are generally neurologically normal, and there is no loss of consciousness during the attacks.
Certain situations or substances can trigger an attack of paroxysmal dystonia, including:
- stress
- fatigue
- alcohol
- coffee
- sudden movement
Identifying the types of movements associated with Paroxysmal dystonia is complicated. These movements may be dystonic, choreic, ballistic, or a combination.
An individual may show one specific type of movement or a combination of movements.
Dystonic movements are typically patterned and repetitive, causing twisting movements and abnormal postures. Dystonia occurs when opposing muscles are contracting simultaneously. The activation of these muscles may “overflow” to other muscle groups unintentionally.
Ballistic movements are more severe limb movements that involve portions of the limb such as the shoulder and elbow, and hip and knee.
Choreic movements may be described as brief, rapid, involuntary movements that serve no purpose. When mild, choreic movements may resemble fidgeting.
Athetoid movements are slower and more continuous than chorea with a writhing quality. They especially involve the hands and may also affect the torso and other parts of the body.
When chorea and athetosis occur simultaneously, the term choreoathetosis has been used. Choreoathetosis may coexist with dystonia or occur independently.
Terms used to describe paroxysmal dystonia include: paroxysmal dyskinesias. Forms of paroxysmal dyskinesias may be referred to as paroxysmal kinesigenic dyskinesia, DYT10 dystonia; paroxysmal nonkinesigenic dyskinesia, paroxysmal choreoathetosis paroxysmal dystonic choreoathetosis, DYT8 dystonia; paroxysmal hypnogenic dyskinesia, paroxysmal exertion-induced dyskinesia
Note: Paroxysmal dyskinesias are sometimes classified under the dystonia umbrella, and sometimes considered a separate category of movement disorders. Paroxysmal hypnogenic dyskinesias may be classified as a form of epilepsy, not dystonia.
Paroxysmal dystonia symptoms
History and (ideally) video documentation of the attacks are important tools toward diagnosing Paroxysmal dystonia. The work-up for diagnosing paroxysmal dyskinesias may also include an electroencephalogram (a test to measure brain waves), brain imaging (such as MRI or CT scan), blood chemistries, and calcium tests.
The paroxysmal dyskinesias are currently classified into four types:
- Paroxysmal kinesigenic (action-induced) dyskinesia (Paroxysmal Kinesigenic Dyskinesia)
- Paroxysmal non kinesigenic dyskinesia (PNKD)
- Paroxysmal exertion-induced dyskinesia (PED)
- Paroxysmal hypnogenic (nocturnal) dyskinesia (PHD). *Most cases of paroxysmal hypnogenic dyskinesia are currently classified as a form of frontal lobe epilepsy.
Paroxysmal Kinesigenic Dyskinesia may be inherited, meaning that it is passed genetically from a parent or ancestor. Inherited Paroxysmal Kinesigenic Dyskinesia is an autosomal dominant disorder. (The term “autosomal dominant” indicates that only one parent need have the Paroxysmal Kinesigenic Dyskinesia gene in order for a child to inherit the disorder.) The age of onset in inherited cases of Paroxysmal Kinesigenic Dyskinesia is from five to fifteen years. Paroxysmal Kinesigenic Dyskinesia may also occur sporadically, meaning that symptoms manifest without a family history. The age of onset in sporadic cases is variable. In both cases the attacks, which may occur up to 100 times per day, are often precipitated by a startle, a sudden movement, a particular movement, or other factors. The attacks are usually short, lasting seconds or minutes. The symptoms may be preceded by an unusual sensation in the limbs and may be limited to one side of the body or a single limb. Most people with Paroxysmal Kinesigenic Dyskinesia have dystonia, and some have a combination of chorea and dystonia or ballism.
Paroxysmal Nonkinesigenic Dyskinesia (PNKD) is also inherited in an autosomal dominant fashion. The age of onset is usually between early childhood and early adulthood. The frequency of attacks is less than that of Paroxysmal Kinesigenic Dyskinesia, averaging between three per day to two per year. Fatigue, alcohol, caffeine, excitement, and other factors may trigger symptoms. The attacks generally last between a few seconds and four hours or longer. The attacks may begin in one limb and spread throughout the body, including the face. A person affected by PNKD may not be able to communicate during an attack but remains conscious and continues to breathe normally.
Paroxysmal Exertion-induced Dyskinesia (PED). Both inherited and sporadic cases of PED have been reported. The attacks are triggered by prolonged exercise and may last between five to thirty minutes. The attacks may occur once a day or twice a month.
Paroxysmal Hypnogenic Dyskinesia (PHD) is characterized by attacks of dystonia, chorea, or ballism during non-REM sleep. These attacks may occur between five times a night to five times a year and usually last between thirty to forty-five seconds. The attacks may also sometimes occur during the day. PHD is probably a broad condition consisting of a several different types of episodes and symptoms. Most cases of PHD are currently classified as a form of frontal lobe epilepsy.
A miscellaneous episodic dystonic condition is benign paroxysmal torticollis of infancy, which typically begins in the few months after birth. These attacks may occur once every two or three weeks and last from hours to days. Typically, the head and/or trunk tilt to one or the other side. These symptoms are often treated with specific physical therapy and disappear when the child is between one and five years old.
Paroxysmal dystonia cause
As is the case with most dystonias, paroxysmal dyskinesias are generally attributed to dysfunction in the area of the brain called the basal ganglia. However, much has yet to be learned about how and why Paroxysmal dystonia occurs. Some regard Paroxysmal Kinesigenic Dyskinesia as a form of epilepsy involving specific parts of the brain (i.e., the basal ganglia and thalamus). There is a growing resource of evidence that suggests that Paroxysmal Kinesigenic Dyskinesia may in fact belong to a group of disorders similar to the inherited episodic ataxias, which are known to be associated with disorders of ion-channels. (Ion channel genes are responsible for the proteins that regulate the passage of salt atoms into and out of cells.)
Although the exact origin may not be known, most cases of Paroxysmal dystonia are inherited or sporadic. A gene for PNKD has been located on chromosome 2q, and a gene for Paroxysmal Kinesigenic Dyskinesia on chromosome 16.
Cases of Paroxysmal dystonia that are not considered inherited or sporadic and are associated with specific factors and conditions are classified as “secondary.”
Secondary causes of Paroxysmal Kinesigenic Dyskinesia include multiple sclerosis, cerebral palsy, metabolic disorders, physical trauma, cerebrovascular disease, and miscellaneous conditions including supranuclear palsy and AIDS. Most conditions associated with Paroxysmal Kinesigenic Dyskinesia may also be associated with PNKD. A few cases of secondary PED and PHD have been reported.
Paroxysmal dyskinesias have also been associated with encephalitis and injury to the brain due to stroke and tumors. Drugs such as cocaine and dopamine blocking agents may also induce dyskinesias.
In extremely rare cases, paroxysmal dyskinesias may be a manifestation of a psychiatric disorder. Only a qualified movement disorder and/or conversion disorder expert (preferably a team of multiple specialists that includes both) should make such a diagnosis. Unfortunately, authentic cases of Paroxysmal dystonia have often been inappropriately dismissed as “psychogenic.” An inaccurate psychiatric diagnosis not only causes unnecessary suffering to the person affected by Paroxysmal dystonia, but it may also preclude appropriate treatment options.
Paroxysmal dystonia treatment
There is no cure for dystonia or Paroxysmal dystonia at this time, but treatments are available. These treatments aim to reduce muscle spasms, pain, and disturbed posture and function.
The current poor understanding of the pathophysiology and biochemistry of Paroxysmal dystonia often makes establishing a satisfactory treatment plan difficult. Treatment needs to be tailored to the individual, and it may be necessary to try several options before symptoms are diminished or alleviated. Patience on the part of both physician and patient is important.
Medications
People with Paroxysmal Kinesigenic Dyskinesia generally respond well to anticonvulsant agents such as phenytoin, primidone, valporate, carbamazepine, phenobarbital, and diazepam. Other drugs that may be helpful include anticholinergics, levodopa, flunarizine, and tetrabenazine. Haloperidol has given inconsistent results.
Paroxysmal Nonkinesigenic Dyskinesia (PNKD) may respond to clonazepam, haloperidol, alternate day oxazepam, and anticholinergics. Anticonvulsants are ineffective in most cases. Trying to avoid triggering factors such as alcohol and caffeine is important.
There are a few cases of Paroxysmal Exertion-induced Dyskinesia (PED) that improve with levodopa and acetazolamide, but drug treatment is ineffective for the most part. Avoidance of prolonged exercise may reduce frequency of attacks.
People who experience short attacks of Paroxysmal Hypnogenic Dyskinesia (PHD) may respond to anticonvulsant drugs, including carbamazepine and phenytoin. Those who experience longer attacks may respond to haloperidol or acetazolamide.
Secondary Paroxysmal dystonia associated with multiple sclerosis responds well to anticonvulsants. Acetazolamide may be a helpful alternative or adjunct agent to anticonvulsants. Paroxysmal dystonia due to head injury may improve with anticonvulsant medications or a combination of anticonvulsants and trihexyphenidyl. Underlying conditions need to be addressed in other cases of secondary Paroxysmal dystonia.
The intermittent and transient nature of paroxysmal dyskinesia generally precludes the use of therapies such as botulinum toxin injections and surgery.
Rapid-onset Dystonia Parkinsonism
Rapid-onset dystonia Parkinsonism, a hereditary form of dystonia, is characterized by the abrupt onset of slowness of movement (parkinsonism) and dystonic symptoms.
Rapid-onset dystonia Parkinsonism Symptoms
The classic features of Rapid-onset dystonia Parkinsonism include involuntary dystonic spasms in the limbs, prominent involvement of the speech and swallowing muscles, slowness of movement, and poor balance. Onset of the combined dystonic and parkinsonian symptoms can be sudden, occurring over hours to days. Some people experience seizures. Rapid-onset dystonia Parkinsonism often follows a fever, prolonged exposure to heat or exercise, childbirth, or emotional stress. Symptoms usually stabilize in less than four weeks, after which, it is reported, there is little progression and symptoms may improve slightly. Rapid-onset dystonia Parkinsonism usually occurs in adolescence or young adulthood (age range 15 to 45), but onset of mild dystonia-parkinsonism has been reported in individuals up to the age of 58.
Rapid-onset dystonia Parkinsonism cause
Several mutations in the ATP1A3 gene (also called the DYT5 gene) are associated with Rapid-onset dystonia Parkinsonism and inherited autosomal dominantly with reduced penetrance. This means that only one parents needs to have the gene mutation for a child to inherit the disease, but not everyone who inherits the gene mutation will develop symptoms.
Rapid-onset dystonia Parkinsonism diagnosis
Diagnosis is based on neurological examination. A family history is required to distinguish the mild limb dystonia of Rapid-onset dystonia Parkinsonism from early-onset dystonia.
Rapid-onset dystonia Parkinsonism treatment
Treatment options for Rapid-onset dystonia Parkinsonism at this time is limited and must be customized to the individual’s unique needs. Levodopa/carbidopa or dopamine agonists may provide some mild improvement in some affected individuals. Individuals may benefit from non-drug approaches such as physical therapy and complementary therapies such as regular relaxation practices.
X-linked Dystonia-Parkinsonism
X-linked dystonia-parkinsonism is a genetic form of dystonia found almost entirely among males of Filipino descent.
X-linked dystonia-parkinsonism symptoms
X-linked dystonia-parkinsonism is a recessive disorder affecting males almost exclusively. It is characterized by both dystonia and parkinsonism including signs and symptoms such as slow movement (bradykinesia), tremor, rigidity, and a loss of postural reflexes. With disease progression, the dystonia usually becomes generalized. In some patients, signs of parkinsonism may accompany, precede, or “replace” symptoms of dystonia. The disease is transmitted through unaffected females, so-called carriers. A few cases have been described in which females who carry a copy of the disease gene may manifest mild symptoms of the disorder, such as relatively mild dystonia or chorea.
X-linked dystonia-parkinsonism is a primarily adult-onset disease starting at age 35 on average with a wide span of onset ranging from late adolescence to the early sixties.
X-linked dystonia-parkinsonism cause
X-linked dystonia-parkinsonism occurs throughout the Philippines but is also diagnosed in the US and Canada in people of Filipino descent. All known cases of X-linked dystonia-parkinsonism originate from one common ancestor. The gene associated with X-linked dystonia-parkinsonism , called the DYT3 gene, was discovered in 2003.
X-linked dystonia-parkinsonism diagnosis
Diagnosis of X-linked dystonia-parkinsonism is based on patient history and neurological examination. Positron emission tomography (PET scans) and olfactory testing may be prescribed.
X-linked dystonia-parkinsonism treatment
Treatment for X-linked dystonia-parkinsonism involves using medications to address dystonia, parkinsonism, or both. Parkinsonism symptoms may slightly improve with levodopa or dopamine agonist therapy, and dystonic features may respond to anticholinergics or benzodiazepines such as clonazepam (Klonopin®). Zolpidem and tetrabenazine may be used if dystonia symptoms become multifocal or generalized. Botulinum toxin injections may improve focal dystonias.
Late-onset dystonia
Cervical dystonia (spasmodic torticollis)
Cervical dystonia, also known as spasmodic torticollis, is the most common form of dystonia. It’s a type of focal dystonia (where only one body part is affected) that affects the neck muscles and sometimes the shoulders.
Involuntary contractions and spasms in the neck muscles can range from mild to severe and cause your head and neck to twist or be pulled forwards, backwards or from side to side.
Muscle spasms and contractions often cause neck pain and stiffness.
The symptoms of cervical dystonia can sometimes be relieved by touching your chin, neck or the back of your head. The reasons for this are unclear.
Blepharospasm
Blepharospasm is a type of focal dystonia that causes the muscles around your eyes (eyelids and brow) to spasm involuntarily.
Uncontrollable eye closure is a common characteristic of blepharospasm. In the most severe cases, a person may be unable to open their eyes for several minutes, effectively making them blind for short periods of time.
Frequent blinking, eye irritation and sensitivity to light (photophobia) are also possible characteristics of blepharospasm.
If you have blepharospasm, the pattern of your symptoms can change throughout the day. For example, you may have few or no symptoms when you wake up in the morning, but they may start to appear or get worse when you’re tired or stressed.
Blepharospasm can occur with dystonia affecting the mouth and/or jaw (oromandibular dystonia). When blepharospasm and oromandibular dystonia occur together, the condition may be referred to as Meige’s syndrome. In such cases, spasms of the eyelids are accompanied by jaw clenching or mouth opening, grimacing, and tongue protrusion.
Blepharospasm cause
Blepharospasm may develop spontaneously with no known precipitating factor or be inherited. Some people with blepharospasm have family members with dystonia affecting different body areas.
Blepharospasm may be secondary due to drug exposure or occur in association with disorders such as Parkinsonian syndromes and Wilson’s disease.
Blepharospasm diagnosis
Diagnosis of blepharospasm is based on information from the affected individual and the physical and neurological examination. At this time, there is no test to confirm diagnosis of blepharospasm, and, in most cases, assorted laboratory tests are normal.
Blepharospasm should not be confused with:
- Ptosis- drooping of the eyelids caused by weakness or paralysis of a levator muscle of the upper eyelid.
- Blepharitis- an inflammatory condition of the lids due to infection or allergies.
- Hemifacial spasm- a non-dystonic condition involving various muscles on one side of the face, often including the eyelid, and caused by irritation of the facial nerve. The muscle contractions are more rapid and transient than those of blepharospasm, and the condition is always confined to one side.
Blepharospasm treatment
One of the most effective treatments for blepharospasm is regular botulinum toxin injections to the affected muscles. Medications including clonazepam, lorazepam, and trihexyphenidyl are helpful in some cases. If botulinum toxin injections and medications are not effective, myectomy surgery in which portions of muscle are removed may also alleviate symptoms. Botulinum toxin injections may or may not be required following myectomy surgery.
Hemifacial spasm
Although it isn’t considered to be a dystonia, hemifacial spasm can cause similar symptoms, with repetitive twitching of the muscles on one side of the face, usually around the eyes and mouth. It can respond well to botulinum toxin injections.
Laryngeal dystonia (spasmodic dysphonia)
Laryngeal dystonia is a type of focal dystonia that causes the muscles of the voice box (larynx) to spasm. Your voice can either sound “strangled” or very quiet and “breathy”, depending on whether the muscles of your larynx spasm outwards or inwards.
Writer’s cramp (hand dystonia)
Writer’s cramp, also known as task-specific dystonia, is a type of focal dystonia that causes cramps and involuntary movements in the muscles of the fingers, wrist, hand and/or forearm. This makes handwriting difficult and uncomfortable.
As the name suggests, writer’s cramp usually affects people who do a lot of writing. Other less well-known types of task-specific dystonia include:
- musician’s cramp
- golfer’s cramp
- typist’s cramp
Symptoms usually appear when a person is trying to do a task that requires fine motor movements such as writing or playing a musical instrument. The symptoms may be isolated to only those tasks or affect the muscles in a more general way and spread to affect many tasks. Common symptoms include, for example, excessive gripping of a pen or utensil, flexing of the wrist, elevation of the elbow, and occasional extension of a finger or fingers causing the utensil to fall from the hand. As in other types of late-onset dystonias, tremor (shaking) may also be a prominent feature.
Oromandibular dystonia (cranial dystonia)
Oromandibular dystonia is a type of segmental dystonia that affects the lower facial muscles, tongue and/or jaw.
It can cause a number of different facial distortions, including grimacing and lip pursing. The jaw can repeatedly open and close or pull outwards and upwards. Tongue movements can be continuous or occur intermittently.
In some cases, the symptoms of oromandibular dystonia only occur when your mouth is being used, such as while eating or talking. In other cases, the symptoms may be improved by talking or chewing.
If you have oromandibular dystonia, you may also have difficulty swallowing (dysphagia).
Tardive dystonia
Tardive dystonia is a type of drug-induced dystonia. Tardive dystonia is a form of tardive dyskinesia, which includes involuntary movements that resemble multiple movement disorders. The term tardive means “late” to indicate that the condition occurs some time after drug exposure, and the terms dyskinesia and dystonia describe the types of movements involved. Tardive dyskinesias are neurologic syndromes caused by exposure to certain drugs, namely a class of medications called neuroleptics which are used to treat psychiatric disorders, some gastric conditions, and certain movement disorders. The amount of exposure to such drugs varies greatly among patients. Tardive dystonia and dyskinesias may also develop as a symptom of prolonged treatment with levodopa in some Parkinson’s disease patients.
Drugs belonging to this class of neuroleptics include (trade name listed in parenthesis):
- Acetohenazine (Tindal),
- Amoxapine (Asendin),
- Chlorpromazine (Thorazine),
- Fluphenazine (Permitil, Prolixin),
- Haloperidol (Haldol),
- Loxapine (Loxitane, Daxolin),
- Mesoridazine (Serentil), metaclopramide (Reglan),
- Molinndone (Lindone, Moban),
- Perphanzine (Trilafrom, Triavil),
- Piperacetazine (Quide),
- Prochlorperzine (Compazine, Combid),
- Promazine (Sparine), promethazine (Phenergan),
- Thiethylperazine (Torecan),
- Thioridazine (Mellaril),
- Thiothixene (Navane),
- Trifluoperazine (Stelazine),
- Triflupromazine (Vesprin), and
- Trimeprazine (Temaril).
Symptoms may develop after weeks or years of drug exposure. Both tardive dystonia and other tardive dyskinesias typically involve (but are not necessarily limited to) the muscles of the face. Symptoms may also include muscle spasms of the neck, trunk, and/or arms.
The movements typical of tardive dystonia are generally slower and more sustained than other dyskinesias, though the presence of a dystonic tremor in opposition to the main dystonia movement may cause a more rapid appearance of movement. Dyskinesias are usually characterized by quick, jerking movements that may include grimacing, tongue protrusion, lip smacking, puckering, and eye blinking. The arms, legs, and trunk may also be involved. Movements of the fingers may appear as though the individual is playing an invisible guitar or piano.
The frequency and pattern of movements may fluctuate. The predominant condition (for example if symptoms are mostly dystonic) will usually dictate the course of treatment.
Tardive dystonia treatment
The treatment of tardive dyskinesias will usually include a gradual withdrawal from the offending medication. If neuroleptics remain a crucial element of an individual’s health, a class of newer, “atypical” neuroleptics (such as clozapine, olanzapine, and quetiapine) may be a suitable substitute. Anticholinergics (such as trihexyphenidyl and benztropine) and muscle relaxers used to treat other forms of dystonia may also be helpful. Baclofen and clonazepam are also sometimes used to treat tardive dystonia. Botulinum toxin injections to a particular muscle group are an additional option for treatment.
Like the treatment of tardive dystonia, the treatment of other tardive dyskinesias is very specific to the individual patient. The first step may be to gradually minimize or discontinue the use of the offending medication. In many cases, discontinuing or lowering the dose of the causative drug will ease symptoms. Substitute drugs may be recommended to replace neuroleptics. In some cases, the symptoms will persist after use of the drug has been terminated but with careful management, symptoms may improve and/or disappear with time. Other drugs such as benzodiazepines, adrenergic antagonists, and dopamine agonists may also be beneficial.
Dystonia diagnosis
Diagnosing dystonia isn’t straightforward. It involves using a stepwise approach that starts by identifying the precise nature and specific features of your movement disorders.
The specialist will try to identify which type of dystonia classification your movement disorders fall into, taking into consideration a number of factors, including:
- how old you were when your symptoms started
- the order in which your symptoms developed
- the speed at which the condition is progressing
- the results of initial tests and investigations
It’s important to confirm whether you have primary or secondary dystonia to help determine the type of treatment you need.
In primary dystonia, muscle spasms are the only symptom and there’s no other associated condition. Secondary dystonia is caused by an underlying health condition, injury or some other type of damage.
Further tests
If you have the typical signs of late-onset focal dystonia, you may not need to have specific investigations. However, you may need to have a series of tests and examinations to confirm whether you have primary or secondary dystonia. These tests are described below:
- Your recent medical and family history will be discussed – for example, whether you’ve recently had a head injury, or whether you have a relative with dystonia.
- Urine and blood tests – to check how well your organs, such as your liver, are functioning and whether you have an infection or high levels of toxins in your body.
- Genetic testing – a DNA sample can be taken from your blood and checked for the abnormal genes associated with some types of dystonia; genetic testing can also confirm whether your dystonia is caused by a genetic condition, such as Huntington’s disease.
- A magnetic resonance imaging (MRI) scan – can check whether there’s any damage to your brain, or whether you have a condition that’s affecting your brain, such as a tumor.
If you have early-onset dystonia, you may also be given a course of medication called levodopa. If your symptoms improve significantly after taking levodopa, a diagnosis of dopa-responsive dystonia can be made.
What is a dystonic storm?
Rarely, patients with dystonic symptoms develop increasingly frequent and intense episodes of severe generalized dystonia called status dystonicus. A single episode of this severe dystonia may be referred to as a dystonic storm or dystonic attack.
Although the exact numbers are not known, anecdotal accounts suggest that relatively mild to moderate dystonic storms are a fairly regular experience for some individuals with generalized dystonia, especially secondary dystonias. Most cases of severe status dystonicus occur in persons who have generalized dystonia that is complicated by other conditions such as metabolic disease, secondary effects of a traumatic injury, or additional neurological conditions.
If a person s swallowing or breathing is affected by a dystonic storm, he/she may require emergency medical attention. In very severe cases, individuals may be admitted to an intensive care unit setting where they may be sedated with medication or need temporary mechanical ventilation to support breathing.
Although the exact origins of status dystonicus are not known, some documented cases appear to be triggered by an abrupt change in medication or severe infections. Medications and botulinum toxin may be used to reduce or alleviate symptoms of a severe dystonic storm. Individuals experiencing a relatively mild or moderate dystonic storm may have a specific medication prescribed by a physician to take at the onset of the attack, may get some relief from a sensory trick, or may simply wait for the symptoms to subside.
Is there a correlation between dystonia and fatigue?
The constant movement and muscle contractions of dystonia can be compared to working out approximately 18 hours a day and for people whose symptoms don’t stop during sleep, 24 hours a day. This can definitely result in fatigue and diminished stamina. Fatigue may be confused with lack of energy or motivation which may be a sign of depression or other medical conditions. Adequate rest and supplementing sleep with restorative practices such as meditation or relaxation techniques are a mainstay of coping with fatigue for many people.
Can dystonia cause difficulty swallowing or breathing?
Yes, sometimes. This depends primarily on the part(s) of the body affected. For instance, some people with dystonia involving the jaw or tongue may have chewing or swallowing difficulty. Occasionally, people with very severe cervical dystonia also may have some swallowing difficulty. Treatments, whether medications or botulinum toxin injections, can also potentially have swallowing side effects. Dystonia rarely affects breathing. Severe generalized dystonia may involve the diaphragm muscles (the primary breathing muscles) or cause enough truncal twisting to cause some problems with regular breathing.
Dystonia treatment
There’s no cure for dystonia, but the condition can usually be effectively managed. No one treatment has been found to be universally effective. Instead, doctors use a variety of therapies (medications, surgery, and other treatments such as physical therapy, splinting, stress management, and biofeedback) aimed at reducing or eliminating muscle spasms and pain. Since response to drugs varies among individuals and even in the same person over time, the most effective therapy is often individualized.
There are a number of treatment techniques that can control the involuntary movements and spasms of dystonia, including medication, physiotherapy, and in some cases, surgery.
The aim is to provide relief from the abnormal movements and postures of dystonia, plus any associated pain and discomfort.
In some cases, other conditions that arise as a result of dystonia, such as stress, anxiety or depression, may also need to be treated.
Treatment for dystonia should be based on the individual and their specific needs. As different people respond differently to different treatments, it may be necessary to try several options to find out which one works best.
There are four main types of treatment for dystonia. They are:
- Botulinum toxin
- Medication
- Physiotherapy
- Surgery, including deep brain stimulation (DBS)
Wherever possible, physiotherapy, medication or botulinum medication will be used to treat dystonia rather than surgery, particularly in the case of children and young people.
Botulinum toxin
Since being introduced into clinical practice in the late 1980s, botulinum toxin has become an effective and widely used form of treatment for a number of different neurological conditions that involve abnormal muscle contractions, such as dystonia.
It’s given by injection directly into the affected muscles and works by blocking the neurotransmitters responsible for muscle spasms reaching the affected muscles.
The effects of the injection usually last two to three months, after which time you’ll need another injection. The site of the injection may feel painful for a few days, but this should soon pass.
Other side effects of botulinum toxin will depend on which part of your body is injected. For example, injections:
- in the neck area may cause swallowing difficulties (dysphagia)
- around the eyes may lead to drooping of the eyes and double vision
- in the vocal cord may cause your voice to become soft and “breathy”
These types of side effects should pass after about a week.
Medication
There are a number of different medications that can be used to treat dystonia.
Anticholinergics
Anticholinergics are a type of medication that can be used to effectively treat all types of dystonia.
However, they’re mainly used to treat generalized dystonia, because botulinum toxin now tends to be used to treat focal dystonia and segmental dystonia (see below).
Anticholinergics work by blocking the release of a neurotransmitter called acetylcholine, known to cause muscle spasms in some cases of dystonia. Trihexyphenidyl and procyclidine are two examples of anticholinergics.
Side effects of anticholinergics include:
- dry mouth
- constipation
- difficulties urinating
- blurred vision
- memory problems
- confusion
Baclofen
Baclofen is a medication that’s sometimes used to treat spasticity (excessive muscular tension) caused by stroke or multiple sclerosis. However, it’s also helps in treating people with dystonia.
In particular, daily doses of baclofen are effective in treating people with segmental and generalized dystonia, as well as those with oromandibular dystonia.
Common side effects of Baclofen include:
- kidney problems – seek medical advice if you develop symptoms such as sleepiness or lethargy (lack of energy)
- nausea – this may be reduced by taking Baclofen with food or milk
- drowsinesss
- balance and co-ordination problems
- confusion
Muscle relaxants
Muscle relaxants are sometimes used to treat cases of dystonia that fail to respond to other types of medication. They work by increasing the levels of a neurotransmitter called gamma-aminobutyric acid (GABA), which helps to relax affected muscles.
Diazepam, lorazepam and clonazepam are all types of muscle relaxants that may be used to treat dystonia.
Depending on the pattern of your symptoms, muscle relaxants can be given by injection (intravenously) or in tablet form (orally). Side effects of muscle relaxants include:
- drowsiness
- tiredness
- muscle weakness
- dizziness
- impaired co-ordination
These side effects should be temporary and disappear once your body gets used to the medication. If you have symptoms of dizziness, avoid driving and operating heavy machinery.
Don’t suddenly stop taking muscle relaxants. If you do, you’ll experience withdrawal symptoms such as anxiety, sweating or tremors (shaking).
If your care team decides you should stop taking muscle relaxants, your dose will gradually be reduced.
Is there anything helpful that can be done to ease my dystonia in a stressful situation?
Although clearly stress does not cause dystonia, many people with dystonia have reported that their symptoms worsen in stressful situations. This worsening is temporary and resolves when the stressful situation has passed. Unfortunately, getting rid of all stress in life is not possible. Therefore, techniques which result in a lessening of the stressful feelings may be beneficial. Relaxation techniques can be of considerable help. Although there are medications which can decrease anxiety, the effects of stress are best managed without additional medications. Health-care professionals familiar with the techniques of stress reduction may be very helpful.
Physiotherapy
Physiotherapy uses specific exercises to help you maintain a full range of motion, improve your posture and prevent the shortening or weakening of affected muscles.
Some people with dystonia find their symptoms improve by simply touching the affected body part or a nearby area. This is known as a “sensory trick” or “geste antagoniste”.
For example, people with cervical dystonia (where the neck muscles spasm and tighten) often find their symptoms improve by touching the back of their head or the side of their face.
Pain management
Many people with certain types of dystonia experience pain, caused by spasms or repeated twisting of joints. You may be referred to a pain management programme to help with managing chronic pain.
Speech and language therapy
You may be referred to a speech and language therapist for certain types of dystonia, such as laryngeal dystonia, which causes difficulty speaking.
Surgery
Surgery may be recommended if your dystonia symptoms don’t respond to botulinum toxin, medication or physiotherapy.
Deep brain stimulation (DBS)
Deep brain stimulation (DBS) is a type of brain surgery used to treat dystonia. During surgery, two small holes will be drilled into your skull.
The surgeon will pass electrodes through each hole and position them in a part of the basal ganglia called the globus pallidus. The basal ganglia is part of the brain that affects muscle movement.
The electrodes will be connected to a small pulse generator that’s similar to a pacemaker. It will be implanted under your skin, usually on your chest or lower abdomen.
The pulse generator sends signals to the globus pallidus. This alters nerve impulses produced by the basal ganglia and improves the symptoms of dystonia.
The most common complication of deep brain stimulation is that either the pulse generator stops working or the electrodes become displaced, which may require further surgery to correct.
Deep brain stimulation is a relatively new technique, so there’s little information regarding its long-term safety or effectiveness. Therefore, before deciding to have deep brain stimulation, you should discuss the risks and benefits of the treatment with your surgical team.
If you have deep brain stimulation, you’re likely to need a series of follow-up appointments. This is because in most cases the signals produced by the pulse generator need to be adjusted to ensure your symptoms are being properly controlled.
It may be several weeks or months before you begin to feel the benefit of Deep brain stimulation. The benefit should continue to increase for a few years following surgery.
Selective peripheral denervation
Selective peripheral denervation is a type of surgery used to treat cervical dystonia. However, these days it only tends to be used in a few, select cases.
During the procedure, the surgeon will make an incision in your neck, before cutting some of the nerves connected to muscles prone to spams.
The surgery will be carried out under general anesthetic, which means you’ll be unconscious throughout the procedure and unable to feel pain or discomfort.
After the procedure, you’ll lose some feeling in your neck because the nerves have been disconnected.
Selective peripheral denervation is generally a safe type of surgery and complications are rare. However, possible complications include:
- infection in the neck
- short-term swelling of the neck
- a feeling of pins and needles in the neck
- occasional short episodes of neck pain
Lifestyle and home remedies
Dystonia has no cure, but you can do a number of things to minimize its effects:
- Sensory tricks to reduce spasms. Touching certain parts of your body may cause spasms to stop temporarily.
- Stress reduction. Try to avoid stressful situations because stress tends to make your symptoms worse.
- Heat or cold. Applying heat or cold can help ease muscle pain.
Alternative medicine
Alternative treatments for dystonia haven’t been well-studied. Ask your doctor about complementary treatments before you start. Consider:
- Meditation and deep breathing. Both might ease stress that can worsen spasms.
- Biofeedback. Electronic devices monitor your body’s functions, such as muscle tension, heart rate and blood pressure. You then learn how to control your
- body responses, which might help reduce muscle tension and stress.
- Yoga. Yoga combines physical postures, breathing techniques, and meditation or relaxation.
Stretching or massage. These can ease muscle pain.
Coping and support
Living with dystonia can be difficult and frustrating. Your body might not always move as you would like, and you may be uncomfortable in social situations. You and your family might find it helpful to talk to a therapist or join a support group.