Contents
- What are causes of falls in the elderly
- Risk factors for falls in the elderly
- Most common causes of falls in the elderly
- Falls in the elderly statistics
- Consequences of falls in the elderly
- How to prevent falls in the elderly
What are causes of falls in the elderly
Falls are the leading cause of fatal and nonfatal injuries among adults 65 and older and 10,000 people in the United States turn 65 every day. Some patients think that falls just happen when you get older or are the result of bad luck, but falls are not an inevitable part of aging. There are specific things that you can do to reduce your patients’ chances of falling.
Falls are preventable. People are living longer and falls will increase unless we make a serious commitment to providing effective fall prevention programs. Fortunately, the opportunity to help reduce falls among older adults has never been better, because research has demonstrated that falls can be prevented. Today, there are effective fall prevention programs that can be used in community settings to reduce falls and help older adults maintain their health and independence.
Each year, millions of older people—those 65 and older—fall. In fact, more than one out of four older people falls each year, but less than half tell their doctor 1. Falling once doubles your chances of falling again 2.
Falls can be devastating. Falls are the leading cause of nonfatal injuries among older adults. One out of ten falls causes a serious injury, such as a hip fracture or head injury, which requires hospitalization. In addition to the physical and emotional pain, many people need to spend at least a year recovering in a long-term care facility. Some are never able to live independently again.
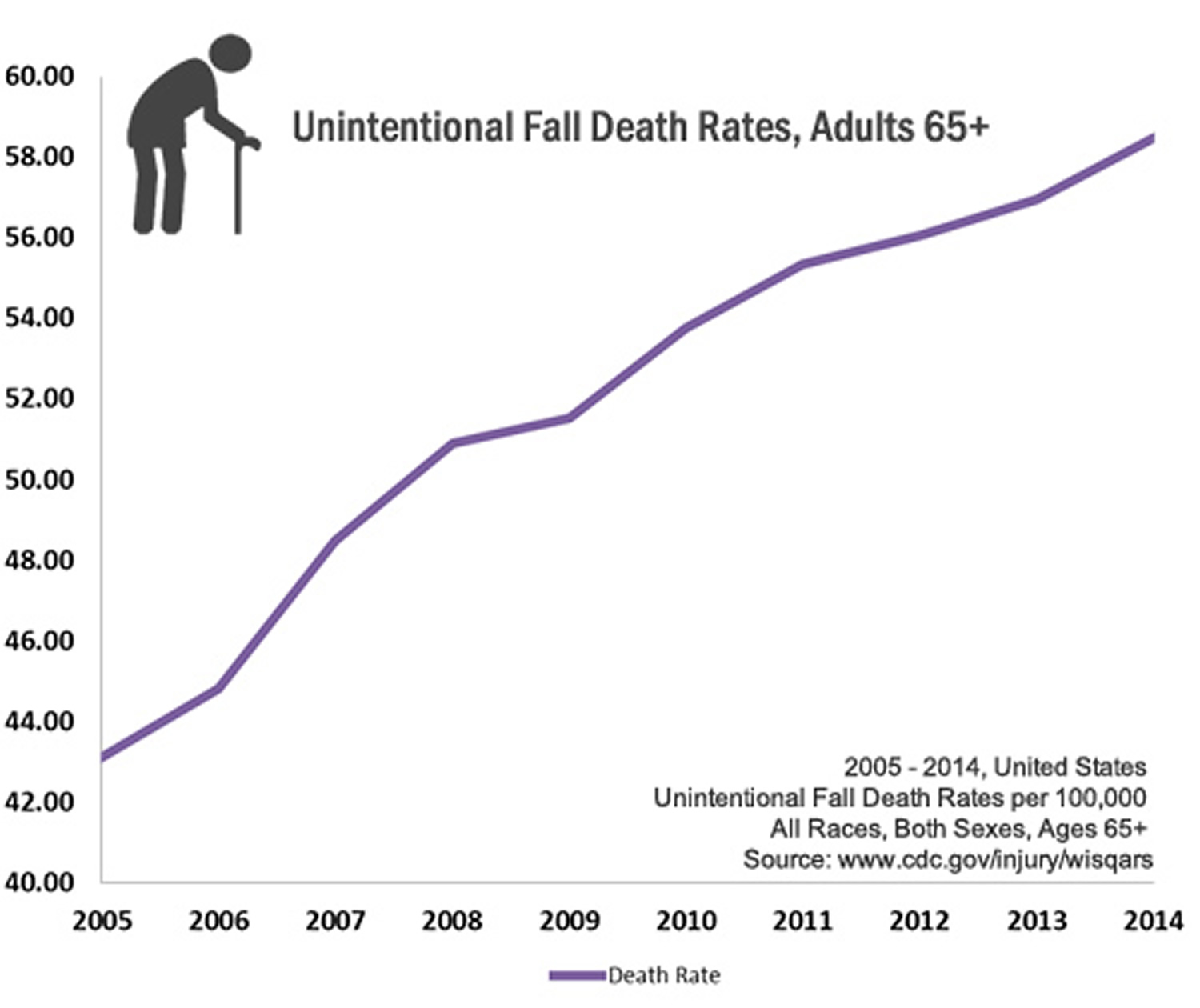
Falls can be deadly. Among older adults, falls are the leading cause of fatal injuries. Each year, at least 25,000 older adults die as a result of falls. And the rate of fall related deaths among older adults in the United States has been rising steadily over the past decade.
- Consider carrying a mobile or portable phone with you as you move about your house could make it easier to call someone if you need assistance. An emergency response system, which lets you push a button on a special necklace or bracelet to call for help, is another option.
Risk factors for falls in the elderly
A fall risk factor is something that increases a person’s chances of falling. This may be a biological characteristic, a behavior, or an aspect of the environment.
These risk factors include:
Biological risk factors
- Muscle weakness, reduced range of motions or balance problems
- Medication side effects and/or interactions
- Chronic health conditions such as arthritis and stroke
- Vision changes and vision loss. Sight Reduction of your ability to accommodate, visual acuity, tolerance to glare, discriminative capacity for colors.
- Loss of sensation in feet
- Hearing – Reduced discrimination capability between contemporary voices in conversation; reduced perception of pure tones, increased production of earwax with frequent development of caps.
Pathological conditions
Neurologic
| Musculoskeletal
|
Cardiovascular
| Genitourinary
|
Gastrointestinal
| Psychiatric
|
Endocrine and internal medicine
| Iatrogenic
|
Behavioral risk factors
- Inactivity
- Risky behaviors such as standing on a chair in place of a step stool
- Alcohol use
Environmental risk factors
Environmental risk factors are responsible for 30–50% of the falls, even though falls are often determined by interaction within the environment or dangerous activities and increased individual susceptibility 4.
- Clutter and tripping hazards
- Poor lighting
- Lack of stair railings
- Lack of grab bars inside and outside the tub or shower
- Poorly designed public spaces
Usually two or more risk factors interact to cause a fall (such as poor balance and low vision) 5. The more risk factors a person has, the greater their chances of falling 6.
Home or environmental risk factors play a role in about half of all falls 7. Understanding these risk factors is the first step to reducing older adult falls.
Most common causes of falls in the elderly
Research has identified many conditions that contribute to falling. These are called risk factors. Many risk factors can be changed or modified to help prevent falls. They include:
- Lower body weakness
- Vitamin D deficiency (that is, not enough vitamin D in your system)
- Difficulties with walking and balance
- Use of medicines, such as tranquilizers, sedatives, or antidepressants. Even some over-the-counter medicines can affect balance and how steady you are on your feet.
- Vision problems
- Foot pain or poor footwear
- Home hazards or dangers such as
- broken or uneven steps, and
- throw rugs or clutter that can be tripped over.
Most falls are caused by a combination of risk factors. The more risk factors a person has, the greater their chances of falling.
Healthcare providers can help cut down a person’s risk by reducing the fall risk factors listed above.
Falls in the elderly statistics
- One out of five falls causes a serious injury such as broken bones or a head injury 8, 9.
- Each year, 2.8 million older people are treated in emergency departments for fall injuries 10.
- Over 800,000 patients a year are hospitalized because of a fall injury, most often because of a head injury or hip fracture 10.
- Each year at least 300,000 older people are hospitalized for hip fractures 11.
- More than 95% of hip fractures are caused by falling 12, usually by falling sideways 13.
- Falls are the most common cause of traumatic brain injuries (TBI) 14.
- Adjusted for inflation, the direct medical costs for fall injuries are $31 billion annually 15. Hospital costs account for two-thirds of the total.
Figure 1. Unintentional Fall and Death Rates
Consequences of falls in the elderly
Many falls do not cause injuries. But one out of five falls does cause a serious injury such as a broken bone or a head injury 17, 8. These injuries can make it hard for a person to get around, do everyday activities, or live on their own.
- Falls can cause broken bones, like wrist, arm, ankle, and hip fractures.
- Falls can cause head injuries. These can be very serious, especially if the person is taking certain medicines (like blood thinners). An older person who falls and hits their head should see their doctor right away to make sure they don’t have a brain injury.
- Many people who fall, even if they’re not injured, become afraid of falling. This fear may cause a person to cut down on their everyday activities. When a person is less active, they become weaker and this increases their chances of falling 18.
Hip Fractures Among Older Adults
One of the most serious fall injuries is a broken hip. It is hard to recover from a hip fracture and afterward many people are not able to live on their own. As the U.S. population gets older, the number of hip fractures is likely to go up.
- Each year over 300,000 older people—those 65 and older—are hospitalized for hip fractures 19.
- More than 95% of hip fractures are caused by falling 13, usually by falling sideways 12.
- Women experience three-quarters of all hip fractures 19.
- Women fall more often than men.
- Women more often have osteoporosis, a disease that weakens bones and makes them more likely to break.
- The chances of breaking your hip go up as you get older.
What You Can Do to Prevent Hip Fractures
You can prevent hip fractures by taking steps to strengthen your bones and prevent falls:
Talk to Your Doctor
- Ask your doctor or healthcare provider to evaluate your risk for falling and talk with them about specific things you can do.
- Ask your doctor or pharmacist to review your medicines to see if any might make you dizzy or sleepy. This should include prescription medicines and over-the counter medicines.
- Ask your doctor or healthcare provider about taking vitamin D supplements.
Get Screened for Osteoporosis
- Get screened for osteoporosis and treated if needed.
Do Strength and Balance Exercises
- Do exercises that make your legs stronger and improve your balance. Tai Chi is a good example of this kind of exercise.
Have Your Eyes Checked
Have your eyes checked by an eye doctor at least once a year, and be sure to update your eyeglasses if needed.
It you have bifocal or progressive lenses, you may want to get a pair of glasses with only your distance prescription for outdoor activities, such as walking. Sometimes these types of lenses can make things seem closer or farther away than they really are.
Make Your Home Safer
- Get rid of things you could trip over.
- Add grab bars inside and outside your tub or shower and next to the toilet.
- Put railings on both sides of stairs.
- Make sure your home has lots of light by adding more or brighter light bulbs.
See more tips of falls prevention.
How to prevent falls in the elderly
Fall prevention may not seem like a lively topic, but it’s important. As you get older, physical changes and health conditions — and sometimes the medications used to treat those conditions — make falls more likely. In fact, falls are a leading cause of injury among older adults. Still, fear of falling doesn’t need to rule your life.
- You can also grab a copy of Falls Prevention Guide produced by the Centers for Disease Control and Prevention here: https://www.cdc.gov/steadi/pdf/What_You_Can_Do_brochure-a.pdf
In the rapidly aging population, older adult fall prevention demands immediate attention. The good news is that you can make a big difference in your own or loved ones lives. You can help them stay healthy and independent longer by reducing their chances of falling.
When you see loved ones over aged 65 years and older or if you are over 65, make sure these 3 questions become a routine part of your conversation:
- Have you fallen in the past year ?
- Do you feel unsteady when standing or walking ?
- Do you worry about falling ?
People who answer “yes” to any of these key screening questions are considered at increased risk of falling and further assessment by their doctor is recommended.
Consider these six simple fall-prevention strategies 20:
1)Make an appointment with your doctor
Begin your fall-prevention plan by making an appointment with your doctor. Always tell your doctor if you have fallen since your last checkup, even if you aren’t hurt when you fall. A fall can alert your doctor to a new medical problem or problems with your medications or eyesight that can be corrected. Your doctor may suggest physical therapy, a walking aid, or other steps to help prevent future falls.
Be prepared to answer questions such as:
- Ask your doctor or healthcare provider to evaluate your risk for falling and talk with them about specific things you can do.
- Ask your doctor or pharmacist to review your medicines to see if any might make you dizzy or sleepy. This should include prescription medicines and over-the counter medicines.
- Ask your doctor or healthcare provider about taking vitamin D supplements.
- What medications are you taking ? Make a list of your prescription and over-the-counter medications and supplements, or bring them with you to the appointment. Your doctor can review your medications for side effects and interactions that may increase your risk of falling. To help with fall prevention, your doctor may consider weaning you off medications that make you tired or affect your thinking, such as sedatives and some types of antidepressants.
- Have you fallen before ? Write down the details, including when, where and how you fell. Be prepared to discuss instances when you almost fell but were caught by someone or managed to grab hold of something just in time. Details such as these may help your doctor identify specific fall-prevention strategies.
- Could your health conditions cause a fall ? Certain eye and ear disorders may increase your risk of falls. Be prepared to discuss your health conditions and how comfortable you are when you walk — for example, do you feel any dizziness, joint pain, shortness of breath, or numbness in your feet and legs when you walk? Your doctor may evaluate your muscle strength, balance and walking style (gait) as well.
Vitamin D supplementation has been shown to reduce the risk of falling in older adults who are vitamin D deficient and is a simple thing that your patients can add to their daily routines.
Furthermore, medication management works by reducing interactions and side effects that may lead to falls.
Effectively managing medications includes:
- Eliminating medications if there is no active indication;
- Reducing doses of necessary medications to the lowest effective dose; and
- Avoiding medications for an older person in whom the risk from side effects outweighs the benefits of the drug.
Many medications have been linked to falls. However, three types of medications that you should immediately consider reducing or eliminating:
- Psychoactive medications (especially benzodiazepines);
- Medications with anticholinergic side effects; and
- Sedatives that can be purchased over-the-counter, such as Tylenol® PM and Benadryl®.
2) Stay Physically Active and Keep moving
Physical activity is an important part of healthy aging. To help you fit exercise and physical activity into your daily life. Physical activity can go a long way toward fall prevention.
How Exercise Can Help You
Exercise and physical activity are good for just about everyone, including older adults. No matter your health and physical abilities, you can gain a lot by staying active. In fact, in most cases you have more to lose by not being active.
Here are just a few of the benefits. Exercise and physical activity:
- Can help maintain and improve your physical strength and fitness.
- Can help improve your ability to do the everyday things you want to do.
- Can help improve your balance.
- Can help manage and improve diseases like diabetes, heart disease, and osteoporosis.
- Can help reduce feelings of depression and may improve mood and overall well-being.
- May improve your ability to shift quickly between tasks, plan an activity, and ignore irrelevant information.
The key word in all these benefits is YOU — how fit and active you are now and how much effort you put into being active. To gain the most benefits, enjoy all 4 types of exercise, stay safe while you exercise, and be sure to eat a healthy diet, too!
With your doctor’s OK, consider activities such as walking, water workouts or tai chi — a gentle exercise that involves slow and graceful dance-like movements. Such activities reduce the risk of falls by improving strength, balance, coordination and flexibility.
If you avoid physical activity because you’re afraid it will make a fall more likely, tell your doctor. He or she may recommend carefully monitored exercise programs or refer you to a physical therapist. The physical therapist can create a custom exercise program aimed at improving your balance, flexibility, muscle strength and gait.
Exercise and Physical Activity
4 Types of Exercise
Exercise and physical activity fall into four basic categories—endurance, strength, balance, and flexibility 21. Most people tend to focus on one activity or type of exercise and think they’re doing enough. Each type is different, though. Doing them all will give you more benefits. Mixing it up also helps to reduce boredom and cut your risk of injury.
Though we’ve described each type separately, some activities fit into more than one category. For example, many endurance activities also build strength. Strength exercises also help improve balance.
1)Endurance exercise
Endurance, or aerobic, activities increase your breathing and heart rate. They keep your heart, lungs, and circulatory system healthy and improve your overall fitness. Building your endurance makes it easier to carry out many of your everyday activities.
- Brisk walking or jogging
- Yard work (mowing, raking, digging)
- Dancing
2) Strength exercise
Strength exercises make your muscles stronger. They may help you stay independent and carry out everyday activities, such as climbing stairs and carrying groceries. These exercises also are called “strength training” or “resistance training.”
- Lifting weights
- Using a resistance band
- Using your own body weight
3) Balance exercise
Balance exercises help prevent falls, a common problem in older adults. Many lower-body strength exercises also will improve your balance.
- Standing on one foot
- Heel-to-toe walk
- Tai Chi
Improve Your Balance
Balance exercises can help prevent falls and avoid the disability that may result from falling.
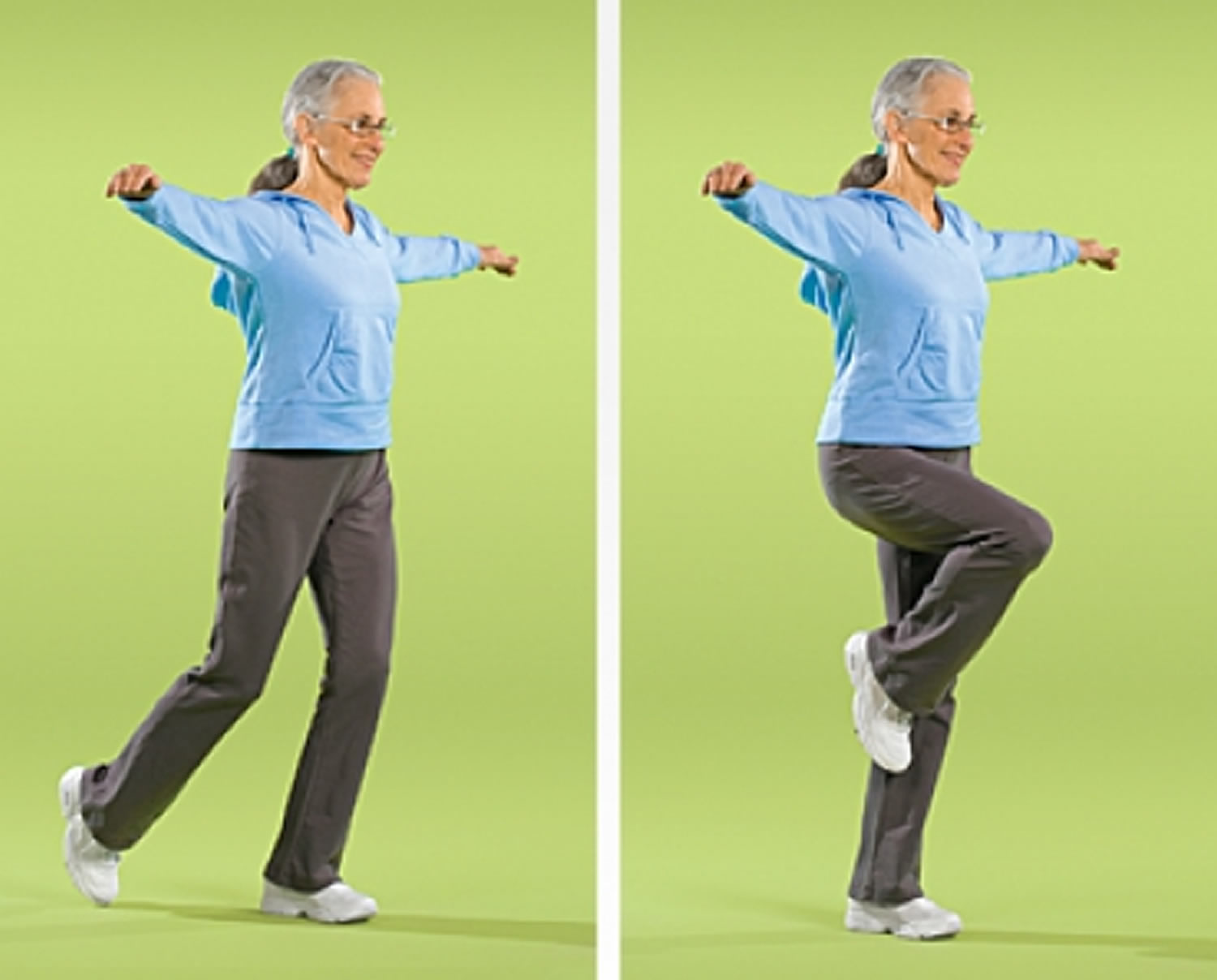
- Stand on One Foot
You can do this exercise while waiting for the bus or standing in line at the grocery. For an added challenge, you can modify the exercise to improve your balance.
- Stand on one foot behind a sturdy chair, holding on for balance.
- Hold position for up to 10 seconds.
- Repeat 10-15 times.
- Repeat 10-15 times with other leg.
- Repeat 10-15 more times with each leg.
Figure 2. Stand on One Foot

- Heel-to-Toe Walk
Having good balance is important for many everyday activities, such as going up and down stairs.
- Position the heel of one foot just in front of the toes of the other foot. Your heel and toes should touch or almost touch.
- Choose a spot ahead of you and focus on it to keep you steady as you walk.
- Take a step. Put your heel just in front of the toe of your other foot.
- Repeat for 20 steps.
Note: If you are unsteady on your feet, try doing this exercise near a wall so you can steady yourself if you need to.
Figure 3. Heel-to-Toe Walk

- Balance Walk
Good balance helps you walk safely and avoid tripping and falling over objects in your way.
- Raise arms to sides, shoulder height.
- Choose a spot ahead of you and focus on it to keep you steady as you walk.
- Walk in a straight line with one foot in front of the other.
- As you walk, lift your back leg. Pause for 1 second before stepping forward.
- Repeat for 20 steps, alternating legs.
Note: As you progress, try looking from side to side as you walk, but skip this step if you have inner ear problems.
Figure 4. Balance Walk
- Tai Chi
Balance is important to help you perform many of your daily activities and prevent falls. Research has shown that tai chi can significantly reduce the risk of falls among older people. In tai chi, which is sometimes called “moving meditation,” you work to improve your balance by moving your body slowly, gently, and precisely, while breathing deeply.
Other benefits from practicing tai chi include:
- improvements in bone and heart health
- easing of pain and stiffness from osteoarthritis
- better sleep
- improvements in overall wellness
Note: Try to put aside distracting thoughts and focus on being aware of your movements.
Figure 5. Tai Chi

4) Flexibility exercise
Flexibility exercises stretch your muscles and can help your body stay limber. Being flexible gives you more freedom of movement for other exercises as well as for your everyday activities.
- Shoulder and upper arm stretch
- Calf stretch
- Yoga
Improve Your Flexibility
Flexibility, or stretching, exercises give you more freedom of movement for your physical activities and for everyday activities such as getting dressed and reaching objects on a shelf. Stretching exercises can improve your flexibility, but they will not improve your strength or endurance.
- Getting Down on the Floor
To Get Down on the Floor:
- Stand facing the seat of a sturdy chair.
- Put your hands on the seat, and lower yourself down on one knee.
- Bring the other knee down.
- Put your left hand on the floor. Leaning on your hand, slowly bring your left hip to the floor. Put your right hand on the floor next to your left hand to steady yourself, if needed.
- You should now be sitting with your weight on your left hip.
- Straighten your legs.
- Bend your left elbow until your weight is resting on it. Using your right hand as needed for support, straighten your left arm. You should now be lying on your left side.
- Roll onto your back.
Note: You don’t have to use your left side. You can use your right side, if you prefer.
Figure 6. Getting Down on the Floor

- Getting Up from the Floor
To Get Up from the Floor: Stand facing the seat of a sturdy chair.
- Roll onto your left side.
- Place your right hand on the floor at about the level of your ribs and use it to push your shoulders off the floor. Use your left hand to help lift you up, as needed.
- You should now be sitting with your weight on your left hip.
- Roll forward, onto your knees, leaning on your hands for support.
- Reach up and lean your hands on the seat of a sturdy chair.
- Lift one of your knees so that one leg is bent, foot flat on the floor.
- Leaning your hands on the seat of the chair for support, rise from this position.
Note: You don’t have to use your left side. You can use your right side, if you prefer.
Figure 7. Getting Up from the Floor

- Shoulder and Upper Arm
This exercise to increase flexibility in your shoulders and upper arms will help make it easier to reach for your seatbelt. If you have shoulder problems, talk with your doctor before trying this stretch.
- Stand with feet shoulder-width apart.
- Hold one end of a towel in your right hand.
- Raise and bend your right arm to drape the towel down your back. Keep your right arm in this position and continue holding on to the towel.
- Reach behind your lower back and grasp the towel with your left hand.
- To stretch your right shoulder, pull the towel down with your left hand. Stop when you feel a stretch or slight discomfort in your right shoulder.
- Repeat at least 3-5 times.
- Reverse positions, and repeat at least 3-5 times.
Figure 8. Shoulder and Upper Arm

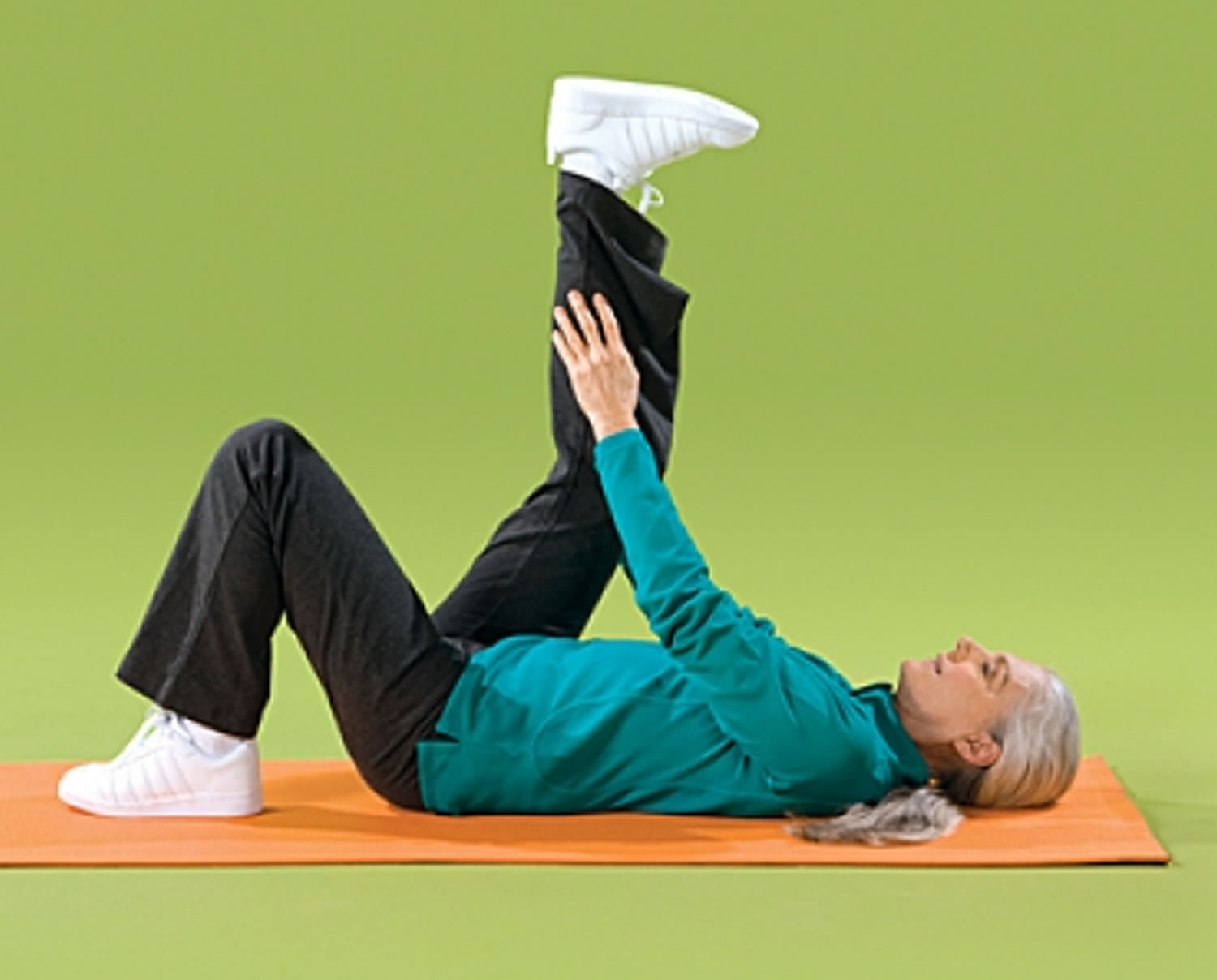
- Back of Leg (Floor)
This exercise stretches the muscles in the back of your legs. If you’ve had hip or back surgery, talk with your doctor before trying this stretch.
- Lie on your back with left knee bent and left foot flat on the floor.
- Raise right leg, keeping knee slightly bent.
- Reach up and grasp right leg with both hands. Keep head and shoulders flat on the floor.
- Gently pull right leg toward your body until you feel a stretch in the back of your leg.
- Hold position for 10-30 seconds.
- Repeat at least 3-5 times.
- Repeat at least 3-5 times with left leg.
Figure 9. Back of Leg (Floor)
- Back of Leg (sitting)
Here’s another exercise that stretches the muscles in the back of your legs. If you’ve had hip or back surgery, talk with your doctor before trying this stretch.
- Sit sideways on a bench or other hard surface, such as two chairs placed together.
- Keeping back straight, stretch one leg out on the bench, toes pointing up.
- Keep other foot flat on the floor.
- If you feel a stretch at this point, hold position for 10-30 seconds.
- If you don’t feel a stretch, lean forward from hips (not waist) until you feel stretching in the leg on the bench.
- Hold position for 10-30 seconds.
- Repeat at least 3-5 times.
- Repeat at least 3-5 times with your other leg.
Figure 10. Back of Leg

- Lower Back
This exercise stretches the muscles of your lower back. If you’ve had hip or back surgery, talk with your doctor before trying this stretch.
- Lie on your back with your legs together, knees bent, and feet flat on the floor. Try to keep both arms and shoulders flat on the floor throughout the stretch.
- Keeping knees bent and together, slowly lower both legs to one side as far as you comfortably can.
- Hold position for 10-30 seconds.
- Bring legs back up slowly and repeat toward other side.
- Continue alternating sides for at least 3-5 times on each side.
Figure 11. Lower Back

- Thigh Stretching (Standing)
Here’s another exercise that stretches your thigh muscles. If you’ve had hip or back surgery, talk with your doctor before trying this stretch.
- Stand behind a sturdy chair with your feet shoulder-width apart and your knees straight, but not locked.
- Hold on to the chair for balance with your right hand.
- Bend your left leg back and grab your foot in your left hand. Keep your knee pointed to the floor. If you can’t grab your ankle, loop a resistance band, belt, or towel around your foot and hold both ends.
- Gently pull your leg until you feel a stretch in your thigh.
- Hold position for 10-30 seconds.
- Repeat at least 3-5 times.
- Repeat at least 3-5 times with your right leg.
Figure 12. Thigh Stretching (Standing)

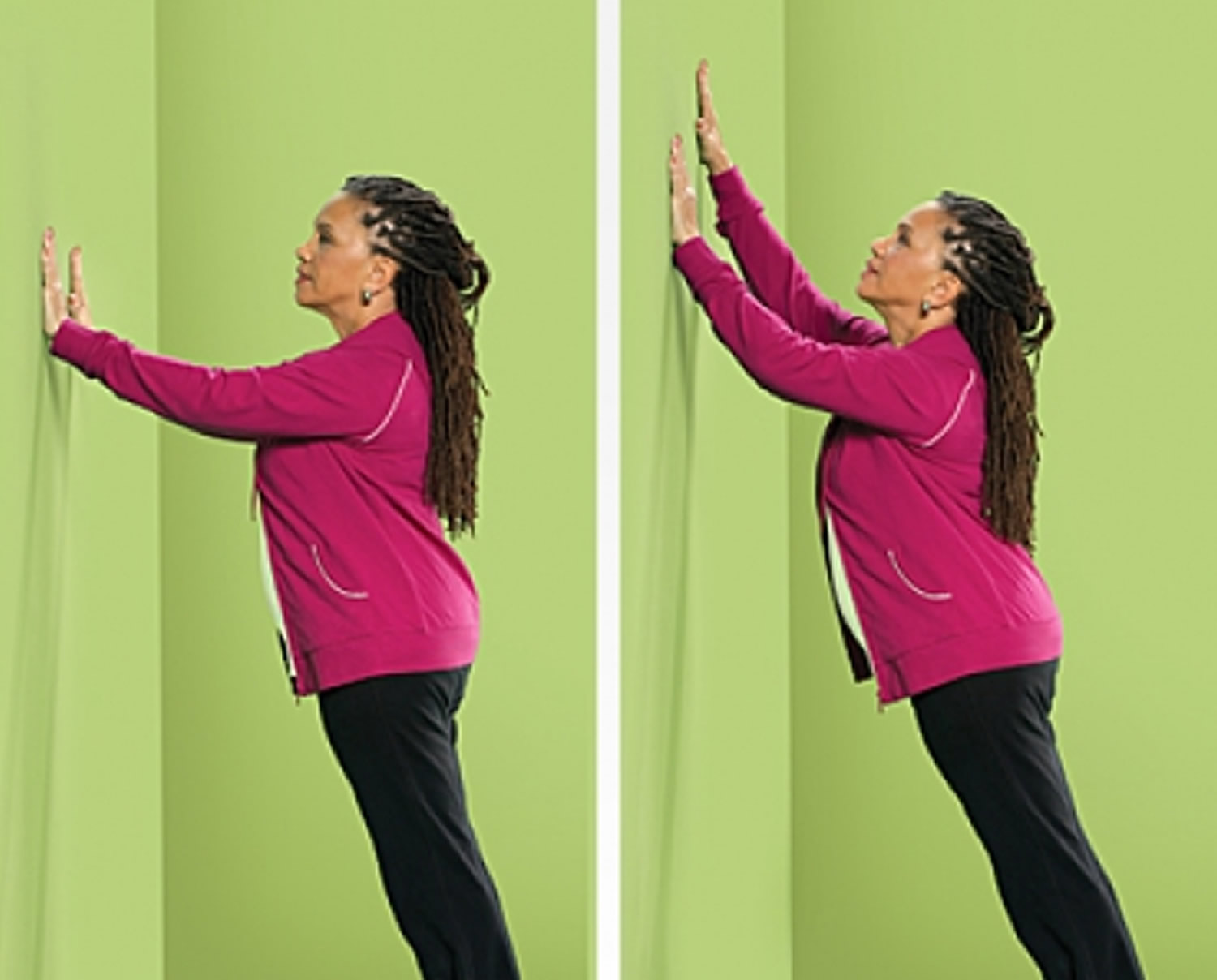
- Upper Body Stretching
This exercise increases the flexibility of your arms, chest, and shoulders, and will help you reach items on the upper shelves of your closet or kitchen cabinet.
- Stand facing a wall slightly farther than arm’s length from the wall, feet shoulder-width apart.
- Lean your body forward and put your palms flat against the wall at shoulder height and shoulder-width apart.
- Keeping your back straight, slowly walk your hands up the wall until your arms are above your head.
- Hold your arms overhead for about 10-30 seconds.
- Slowly walk your hands back down.
- Repeat at least 3-5 times.
Note: As you progress, the goal is to reach higher.
Figure 13. Upper Body Stretching
3) Wear sensible shoes
Consider changing your footwear as part of your fall-prevention plan. High heels, floppy slippers and shoes with slick soles can make you slip, stumble and fall. So can walking in your stocking feet. Instead, wear properly fitting, sturdy shoes with nonskid soles. Sensible shoes may also reduce joint pain.
- Wear non-skid, rubber-soled, low-heeled shoes, or lace-up shoes with non-skid soles that fully support your feet. It is important that the soles are not too thin or too thick. Don’t walk on stairs or floors in socks or in shoes and slippers with smooth soles.
4) Make Your Home Safer by removing home hazards
Six out of every 10 falls happen at home, where you spend much of your time and tend to move around without thinking about your safety. There are many changes you can make to your home that will help you avoid falls and ensure your safety.
Take a look around your home. Your living room, kitchen, bedroom, bathroom, hallways and stairways may be filled with hazards. To make your home safer:
- Get rid of things you could trip over.
- Add grab bars inside and outside your tub or shower and next to the toilet.
- Put railings on both sides of stairs.
- Make sure your home has lots of light by adding more or brighter light bulbs.
- Remove boxes, newspapers, electrical cords and phone cords from walkways.
- Move coffee tables, magazine racks and plant stands from high-traffic areas.
- Secure loose rugs with double-faced tape, tacks or a slip-resistant backing — or remove loose rugs from your home.
- Repair loose, wooden floorboards and carpeting right away.
- Store clothing, dishes, food and other necessities within easy reach.
- Immediately clean spilled liquids, grease or food.
- Use nonslip mats in your bathtub or shower. Use a bath seat, which allows you to sit while showering.
- Be very careful when walking on wet or icy surfaces. They can be very slippery ! Try to have sand or salt spread on icy areas by your front or back door.
In Stairways, Hallways, and Pathways
- Have handrails on both sides of the stairs, and make sure they are tightly fastened. Hold the handrails when you use the stairs, going up or down. If you must carry something while you’re on the stairs, hold it in one hand and use the handrail with the other. Don’t let what you’re carrying block your view of the steps.
- Make sure there is good lighting with light switches at the top and bottom of stairs and on each end of a long hall. Remember to use the lights!
- Keep areas where you walk tidy. Don’t leave books, papers, clothes, and shoes on the floor or stairs.
- Check that all carpets are fixed firmly to the floor so they won’t slip. Put no-slip strips on tile and wooden floors. You can buy these strips at the hardware store.
- Don’t use throw rugs or small area rugs.
In Bathrooms and Powder Rooms
- Mount grab bars near toilets and on both the inside and outside of your tub and shower.
- Place non-skid mats, strips, or carpet on all surfaces that may get wet.
- Remember to turn on night lights.
In Your Bedroom
- Put night lights and light switches close to your bed.
- Keep a flashlight by your bed in case the power is out and you need to get up.
- Keep your telephone near your bed.
In Other Living Areas
- Keep electric cords and telephone wires near walls and away from walking paths.
- Secure all carpets and large area rugs firmly to the floor.
- Arrange your furniture (especially low coffee tables) and other objects so they are not in your way when you walk.
- Make sure your sofas and chairs are the right height for you to get in and out of them easily.
- Don’t walk on newly washed floors—they are slippery.
- Keep items you use often within easy reach.
- Don’t stand on a chair or table to reach something that’s too high—use a “reach stick” instead or ask for help. Reach sticks are special grabbing tools that you can buy at many hardware or medical-supply stores. If you use a step stool, make sure it is steady and has a handrail on top. Have someone stand next to you.
- Don’t let your cat or dog trip you. Know where your pet is whenever you’re standing or walking.
- Keep emergency numbers in large print near each telephone.
If you have fallen, your doctor might suggest that an occupational therapist, physical therapist, or nurse visit your home. These healthcare providers can assess your home’s safety and advise you about making changes to prevent falls.
Your Own Medical Alarm
If you’re concerned about falling, think about getting an emergency response system. If you fall or need emergency help, you push a button on a special necklace or bracelet to alert your local emergency service provider. There is a fee for this service, and it is not usually covered by insurance.
5) Have your eyes checked
Have your eyes checked by an eye doctor at least once a year, and be sure to update your eyeglasses if needed.
If you have bifocal or progressive lenses, you may want to get a pair of glasses with only your distance prescription for outdoor activities, such as walking. Sometimes these types of lenses can make things seem closer or farther away than they really are.
6) Light up your living space
Keep your home brightly lit to avoid tripping on objects that are hard to see. Also:
- Place night lights in your bedroom, bathroom and hallways.
- Place a lamp within reach of your bed for middle-of-the-night needs.
- Make clear paths to light switches that aren’t near room entrances. Consider trading traditional switches for glow-in-the-dark or illuminated switches.
- Turn on the lights before going up or down stairs.
- Store flashlights in easy-to-find places in case of power outages.
7) Use assistive devices
Your doctor might recommend using a cane or walker to keep you steady. Other assistive devices can help, too. For example:
- Hand rails for both sides of stairways
- Nonslip treads for bare-wood steps
- A raised toilet seat or one with armrests
- Grab bars for the shower or tub
- A sturdy plastic seat for the shower or tub — plus a hand-held shower nozzle for bathing while sitting down
If necessary, ask your doctor for a referral to an occupational therapist. He or she can help you brainstorm other fall-prevention strategies. Some solutions are easily installed and relatively inexpensive. Others may require professional help or a larger investment. If you’re concerned about the cost, remember that an investment in fall prevention is an investment in your independence.
8) Other Falls Preventive Measures
- Limit the amount of alcohol you drink. Even a small amount of alcohol can affect your balance and reflexes. Studies show that the rate of hip fractures in older adults increases with alcohol use.
- Get enough sleep. If you are sleepy, you are more likely to fall.
- Stand up slowly. Getting up too quickly can cause your blood pressure to drop. That can make you feel wobbly. Get your blood pressure checked when lying and standing.
- Use an assistive device if you need help feeling steady when you walk. Appropriate use of canes and walkers can prevent falls. If your doctor tells you to use a cane or walker, make sure it is the right size for you and the wheels roll smoothly. This is important when you’re walking in areas you don’t know well or where the walkways are uneven. A physical or occupational therapist can help you decide which devices might be helpful and teach you how to use them safely.
- Keep Your Bones Strong to Prevent Falls. Falls are a common reason for trips to the emergency room and for hospital stays among older adults. You can help prevent fractures by keeping your bones strong. Having healthy bones won’t prevent a fall, but if you fall, it might prevent breaking a hip or other bone, which may lead to a hospital or nursing home stay, disability, or even death. Getting enough calcium and vitamin D can help keep your bones strong. So can physical activity. Try to get at least 150 minutes per week of physical activity.
- Other ways to maintain bone health include quitting smoking and limiting alcohol use, which can decrease bone mass and increase the chance of fractures. Also, try to maintain a healthy weight. Being underweight increases the risk of bone loss and broken bones.
- Osteoporosis is a disease that makes bones weak and more likely to break. For people with osteoporosis, even a minor fall may be dangerous. Talk to your doctor about osteoporosis.
- Stevens JA, Ballesteros MF, Mack KA, Rudd RA, DeCaro E, Adler G. Gender differences in seeking care for falls in the aged Medicare Population. Am J Prev Med 2012;43:59–62.[↩]
- O’Loughlin J et al. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. American journal of epidemiology, 1993, 137:342-54.[↩]
- Mayor S. NICE issues guideline to prevent falls in elderly people. BMJ : British Medical Journal. 2004;329(7477):1258. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC534478/[↩]
- Risk factors for recurrent nonsyncopal falls. A prospective study. Nevitt MC, Cummings SR, Kidd S, Black D. JAMA. 1989 May 12; 261(18):2663-8. https://www.ncbi.nlm.nih.gov/pubmed/2709546/[↩]
- Rubenstein, L.Z. & Josephson, K.R. (2006). Falls and their prevention in elderly people: what does the evidence show? Med Clin North Am, 90(5), 807–824.[↩]
- Tinetti, M.E., Williams, T.F. & Mayewski, R. (1986). Fall risk index for elderly patients based on number of chronic disabilities. Am J Med, 80, 429–434.[↩]
- Bergen G, Chen LH, Warner M, Fingerhut LA. Injury in the United States: 2007 Chartbook. Hyattsville: National Center for Health Statistics, 2008.[↩]
- Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall–related injuries in older adults. American Journal of Public Health 1992;82(7):1020–3.[↩][↩]
- Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. Journal of Trauma–Injury, Infection and Critical Care 2001;50(1):116–9[↩]
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web–based Injury Statistics Query and Reporting System (WISQARS). https://www.cdc.gov/injury/wisqars/[↩][↩]
- HCUPnet. Healthcare Cost and Utilization Project (HCUP). 2012. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/[↩]
- Hayes WC, Myers ER, Morris JN, Gerhart TN, Yett HS, Lipsitz LA. Impact near the hip dominates fracture risk in elderly nursing home residents who fall. Calcif Tissue Int 1993;52:192-198.[↩][↩]
- Parkkari J, Kannus P, Palvanen M, Natri A, Vainio J, Aho H, Vuori I, Järvinen M. Majority of hip fractures occur as a result of a fall and impact on the greater trochanter of the femur: a prospective controlled hip fracture study with 206 consecutive patients. Calcif Tissue Int, 1999;65:183–7.[↩][↩]
- Jager TE, Weiss HB, Coben JH, Pepe PE. Traumatic brain injuries evaluated in U.S. emergency departments, 1992–1994. Academic Emergency Medicine 2000&359;7(2):134–40.[↩]
- Burns EB, Stevens JA, Lee RL. The direct costs of fatal and non-fatal falls among older adults—United States. J Safety Res 2016:58.[↩]
- Older Adult Falls. Centers for Disease Control and Prevention. https://www.cdc.gov/HomeandRecreationalSafety/Falls/adultfalls.html[↩]
- Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. Journal of Trauma–Injury, Infection and Critical Care 2001;50(1):116–9.[↩]
- Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ. Fear of falling and restriction of mobility in elderly fallers. Age and Ageing 1997;26:189–193.[↩]
- HCUPnet. Healthcare Cost and Utilization Project (HCUP). 2012. Agency for Healthcare Research and Quality, Rockville, MD. http://hcupnet.ahrq.gov.[↩][↩]
- Healthy aging. Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/healthy-aging/in-depth/fall-prevention/art-20047358[↩]
- 4 Types of Exercise. https://go4life.nia.nih.gov/4-types-exercise[↩]





