Contents
What is Filariasis
Filariasis refers to parasitic infection caused by filarial parasites or nematodes (roundworms) of the family Filariidae transmitted to humans by blood-sucking insects, such as mosquitoes, blackflies, or midges, acting as biological vectors 1, 2, 3, 4, 5. Filarial infection is transmitted through the bite of an infected insect as it feeds upon human blood 6. Thereafter, parasite larvae mature into adult forms within the host. These adult parasites then multiply, producing microfilariae, which are subsequently ingested by blood-sucking insects along with human blood. These microfilariae undergo subsequent stages of development within the insect’s bodies (see Lymphatic Filariasis Life Cycle below) 7, 8, 9. Of the hundreds of described filarial parasites, only 8 species cause natural infections in humans 10:
- Onchocerca volvulus causing Onchocerciasis 11, 12
- Wuchereria bancrofti causing Bancroftian filariasis (lymphatic filariasis)
- Brugia malayi causing Malayan filariasis (lymphatic filariasis) 13, 14
- Brugia timori causing Malayan filariasis (lymphatic filariasis) 13, 14
- Loa loa causing Loiasis 15, 16
- Mansonella species (Dipetalonema spp), Mansonella perstans (Dipetalonema perstans), and Mansonella streptocerca (Dipetalonema streptocerca) causing Mansonelliasis 17, 18, 19, 20
- Dirofilaria species causing Dirofilariasis 21, 22
The location of these parasites within the human body varies from species to species. Filariasis affects a range of human tissues and often display little or no observable host response throughout their development 23, 24. An exception occurs when the parasite enters extremely sensitive tissues, such as the conjunctiva 25.
Filariasis can be classified based on the location of the parasite within the human host’s body 5, 25, 26, 27:
- Lymphatic filariasis: Wuchereria bancrofti, Brugia malayi, Brugia timori;
- Subcutaneous filariasis: Loa loa, Onchocerca volvulus;
- Serous cavity filariasis: Mansonella spp.
Filariasis signs and symptoms and treatment of filariasis depends on the type of filarial parasitic worm (nematode) infection you have.
Lymphatic filariasis commonly known as elephantiasis is caused by at least three species of nematodes (roundworms) that include Wuchereria bancrofti, Brugia malayi, and Brugia timori, which are transmitted between definitive human hosts by multiple mosquito vectors that include Aedes, Anopheles, Culex, Mansonia, and Ochlerotatus mosquitoes that have varying geographical distributions 28, 29. An estimated 90% of lymphatic filariasis cases are caused by Wuchereria bancrofti also known as Bancroftian filariasis, which are mostly acquired in childhood 30, 31, 32, 33. Brugia malayi and Brugia timori cause about 10% of lymphatic filariasis. Aedes, Anopheles, Culex, Mansonia, and Ochlerotatus mosquitoes are the main vectors responsible for filarial parasites transmission to humans. Mosquitoes serve as biological hosts that both develop and transmit the parasite during blood-feeding and establish the infection in humans 34. People get lymphatic filariasis when bitten by an infectious mosquito carrying the parasite. For the mosquito to become infectious, they must bite, or take a blood meal, from a person already infected with the parasite. About a week or so later, that same mosquito will bite the next person and the parasite may enter through the body through the person’s skin. And the cycle of infection continues (see Lymphatic Filariasis Life Cycle below). Once inside your body, the immature worms make their home in the person’s lymphatic system. They can live for 5 – 7 years there, eventually damaging the lymphatic vessels. In lymphatic filariasis, repeated episodes of inflammation and lymphedema (a chronic swelling of body tissues caused by a problem with the lymphatic system) lead to lymphatic damage, chronic swelling, and elephantiasis of the legs, arms, scrotum, vulva, and breasts 35, 36, 37, 38, 39, 40.
All filarial infections cause some type of skin problems in addition to systemic (affecting the whole body) signs and symptoms. In filariasis or filarial parasite infection, often acquired in childhood, can lead to damage to the lymphatic system, causing lymphedema (a chronic swelling of body tissues caused by a problem with the lymphatic system), fever, pain, and disfigurement, especially in the limbs (elephantiasis) and scrotal swelling or hydrocele (a fluid-filled sac that causes swelling in the scrotum, the pouch that holds the testicles) 30. The legs are involved in most cases, but the lymphedema can also involve the genitals, arms, and breasts. While some filarial parasite infections are asymptomatic, they still cause internal damage and can lead to permanent disability. People affected by lymphatic filariasis are not only physically disabled, but suffer mental, social and financial losses contributing to stigma and poverty.
No form of human filariasis is currently endemic to the United States 41. Wuchereria bancrofti once was prevalent in Charleston, South Carolina, because of the presence of suitable mosquito vectors. Immigrant populations and persons who have traveled long-term to the tropics are potential reservoirs of Wuchereria bancrofti infection. Returning missionaries and overseas workers/volunteers are at particular risk for lymphatic filariasis and onchocerciasis, because of the long pre-patent period and relatively high intensity of exposure required between exposure to infective insect bites and the development of sexually mature adult worms.
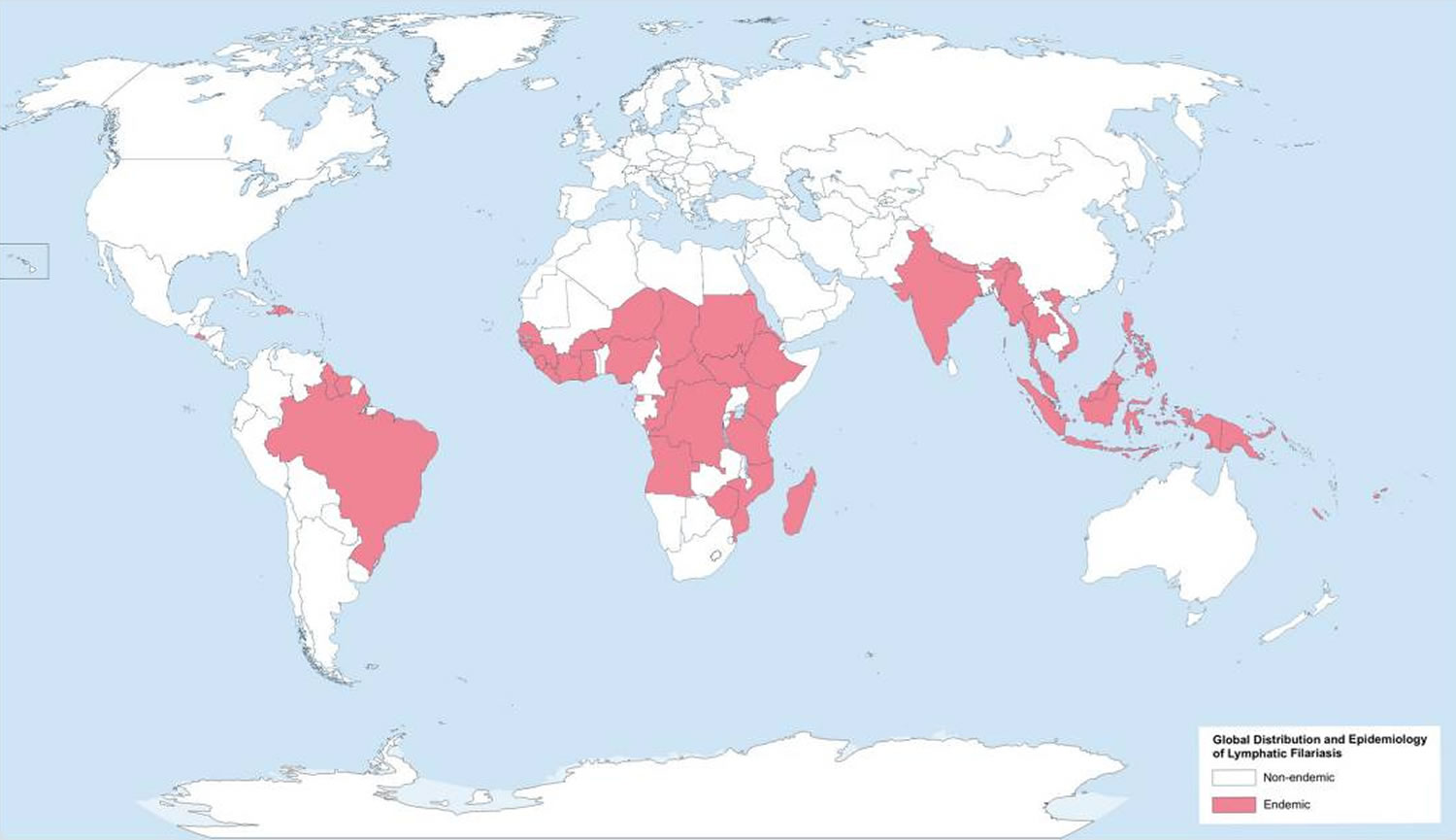
Lymphatic filariasis is common in tropical and subtropical regions with an estimated 120 million people in 81 countries being infected and a third of whom have overt clinical disease 42, 43, 44. About one-third of those with filariasis reside in India, a third in Africa, and the remainder in the Americas, South-East Asia and the Pacific 45. It is difficult to estimate prevalence accurately, but according to antigenic studies, prevalence of lymphatic filariasis infection in India (the country with the greatest disease burden) is 5.66% 42.
Filariasis signs and symptoms vary depending on the type of filarial infection, body location and can be acute or chronic in nature. Up to 70% of infected individuals remain asymptomatic. Symptoms usually do not manifest until adolescence or adulthood, when worm burden usually is the highest. Several symptomatic variations have been observed 46. Because cases of filariasis in North America and high-income countries are uncommon, physicians initially may miss the diagnosis in these areas. To avoid this pitfall, physicians should obtain and document a thorough travel history from patients with suspicious lesions.
The clinical course of lymphatic filariasis is broadly divided into the following:
- Asymptomatic microfilaremia – Patients with microfilaremia are generally asymptomatic, although those with heavy microfilarial loads may develop acute and chronic inflammatory granulomas secondary to splenic destruction. Passage of cloudy milklike urine may denote chyluria
- Acute phases of adenolymphangitis (ADL) – This refers to the sudden onset of febrile, painful lymphadenopathy. Pathologically, the lymph node is characterized by a retrograde lymphangitis, distinguishing it from bacterial lymphadenitis. Symptoms usually abate within 1 week, but recurrences are possible 47. Signs and symptoms of adenolymphangitis (ADL) include episodic attacks of fever associated with inflammation of the inguinal lymph nodes, testis, and spermatic cord, as well as with lymphedema. Skin exfoliation of the affected body part usually occurs with resolution of an episode.
- Chronic, irreversible lymphedema and hydrocele
- Lymphedema – the most common presentation that develops over a long period due to chronic lymphatic damage. It characteristically presents with swelling of the limbs either upper or lower depending on the involvement of inguinal or axillary lymphatic vessels. Pitting edema develops in the early stages of the disease, which later progresses into brawny non-pitting type. Elephantiasis is the most severe type of lymphedema characterized by severe swelling of the limbs, genitalia, and breasts. The skin becomes thick and hard, owing to hyperpigmentation and hyperkeratosis.
- Hydrocele (a fluid-filled sac around a testicle that causes painless swelling of the scrotum) – this is one of the debilitating morbidities associated with chronic lymphatic filariasis. It can be unilateral or bilateral, leading to enlargement of the scrotum. It can be very large, reaching up to 40 cm.
The majority of filarial infections are asymptomatic, showing no external signs of infection while contributing to the transmission of the parasite. These asymptomatic infections still cause damage to the lymphatic system and the kidneys and alter your body’s immune system.
Lymphatic filariasis symptoms predominantly result from the presence of adult worms residing in the lymphatics. They include the following 48:
- Fever
- Groin (inguinal) or armpit (axillary) swollen or enlarged lymph nodes (lymphadenopathy)
- Testicular and/or inguinal pain
- Skin exfoliation
- Limb or genital swelling. Repeated episodes of inflammation and lymphedema lead to lymphatic damage, chronic swelling, and elephantiasis of the legs, arms, scrotum (hydrocele), vulva, and breasts.
In general, the diagnostic approach varies by group of filariasis. Traditionally, the diagnosis of filariasis requires demonstrating microfilariae in the peripheral blood or skin. However, circulating filarial antigens (CFA) are now routinely used to diagnose Wuchereria bancrofti infection 49. The microfilariae of all species that cause lymphatic filariasis and the microfilariae of Loa loa, Mansonella ozzardi, and Mansonella perstans can be detected on a blood smear 50.
Microfilariae are detectable via examination of the following:
- Blood – The microfilariae of all species that cause lymphatic filariasis and the microfilariae of Loa loa, Mansonella ozzardi, and Mansonella perstans are detected in blood. Wuchereria bancrofti can be detected via circulating filarial antigen (CFA) assays. However, assays for circulating parasite antigen of Wuchereria bancrofti are not presently approved by the U.S. Food and Drug Administration (FDA). There are no antigen test for Brugia spp. Serologic enzyme immunoassay tests, including antifilarial IgG1 and IgG4, provide an alternative to microscopic detection of microfilariae for the diagnosis of lymphatic filariasis. Patients with active filarial infection typically have elevated levels of antifilarial IgG4 in the blood and these can be detected using routine assays.
- Urine – If lymphatic filariasis is suspected, urine should be examined macroscopically for chyluria and then concentrated to examine for microfilariae.
- Skin – Onchocerca volvulus and Mansonella streptocerca infections are diagnosed when microfilariae are detected in multiple skin-snip specimens taken from different sites.
- Eye – Microfilariae of Onchocerca volvulus may be detected in the cornea or anterior chamber of the eye using slit-lamp examination.
Useful imaging studies in the evaluation of filariasis include the following:
- Chest X-ray – Diffuse pulmonary infiltrates are visible in patients with tropical pulmonary eosinophilia (TPE)
- Ultrasound – Can be used to demonstrate and monitor lymphatic obstruction of the inguinal and scrotal lymphatics; has been used to demonstrate the presence of viable worms. Careful ultrasound may identify the random movement of adult worms in dilated lymphatics, known as the “filarial dance sign” (FDS). This is particularly useful in a patient with scrotal symptoms and is considered the gold standard investigation for detecting viable adult worms 51.
- Lymphoscintigraphy – A nuclear medicine imaging test that maps the lymphatic system by tracking a radioactive tracer injected under the skin, helping to identify the sentinel lymph node in cancer patients or assess lymphatic drainage in conditions like lymphedema 52
Histologic findings include the following:
- Lymphatic filariasis – Affected lymph nodes demonstrate fibrosis and lymphatic obstruction with the creation of collateral channels
- Elephantiasis – The skin is characterized by hyperkeratosis, acanthosis, lymph and fatty tissue, loss of elastin fibers, and fibrosis
- Onchocerciasis – Onchocercomas have a central stromal and granulomatous, inflammatory region where the adult worms are found and a peripheral, fibrous section; microfilariae in the skin incite a low-grade inflammatory reaction with loss of elasticity and fibrotic scarring.
Key clinical features that may assist in making a diagnosis of lymphatic filariasis include:
- History of residence in an endemic country for several years;
- Self-limiting nature of attacks, in contrast to bacterial cellulitis, incarcerated hernias or testicular torsion;
- Bilateral symptoms and signs;
- Recurrent episodes;
- Palpable regional masses or lymphadenopathy.
The diagnosis of symptomatic lymphatic filariasis requires strong clinical suspicion. Interestingly, many infected people remain asymptomatic. Risk factors for symptomatic disease include duration and intensity of exposure to vectors, adult worm burden, frequency of secondary infections and the host immune response 53.
A blood film and serological evaluation are alternative diagnostic options. In most endemic areas, circulating microfilariae (filarial larvae) exhibit nocturnal periodicity (coinciding with peak feeding of local mosquitos) and are best seen on blood films taken between 10 pm and 4 am. If nocturnal samples are not feasible, then provocation with diethylcarbamazine may enhance microfilarial detection 1–2 hours later. Pacific Island infections (except Papua New Guinea) are subperiodic, with maximal microfilaraemia in the late afternoon, and show unresponsiveness to provocation. Importantly, patients with the chronic manifestations of lymphatic filariasis often have low levels of circulating microfilariae, resulting in lower blood-film sensitivity 54.
Diethylcarbamazine citrate (DEC) remains the mainstay of filariasis treatment worldwide, which kills both immature and adult parasitic worms 30. The United States Centers for Disease Control and Prevention (CDC) recommends a single-day or 12-day course of diethylcarbamazine (DEC) at 6 mg/kg/day 55, 30.
The most common side effects of diethylcarbamazine (DEC) include 55:
- Dizziness
- Nausea
- Fever
- Headache
- Pain in muscles or joints
Diethylcarbamazine (DEC) has been used globally for more than 50 years. A single combined dose of ivermectin, albendazole, and diethylcarbamazine (DEC) resulted in clearance of microfilaria in 96% of affected patients for up to 3 years and is currently recommended by the World Health Organization (WHO) as triple therapy in areas not endemic with loaisis (Loa loa) 56. However, because lymphatic filariasis is rare in the United States, diethylcarbamazine (DEC) is no longer approved by the U.S. Food and Drug Administration (FDA) 55. Doctors can get diethylcarbamazine (DEC) from CDC, after a confirmed positive lab test.
Diethylcarbamazine (DEC) may not help people who have lymphedema, hydrocele or elephantiasis, as most people with these symptoms no longer have live parasites in their bodies 55. Your doctor might refer you to a lymphedema therapist to help manage your lymphedema. This includes learning how to keep the affected area clean, exercise, elevation, treatment of wounds and infections, and wearing appropriate footwear. There is limited evidence for the role of doxycycline as some studies advocate the use of doxycycline (200mg/day for 4 to 6 weeks) in adult worm killing and preventing the progression of lymphedema 30. If you have hydrocele (a fluid-filled sac that develops around one or both testicles, causing painless swelling in the scrotum), your doctor might recommend surgery to remove the fluid-filled swelling.
If you also have onchocerciasis or loaisis (Loa loa), also caused by filarial parasitic worms, taking diethylcarbamazine (DEC) might cause life-threatening side effects. Filaricidal action of diethylcarbamazine (DEC) induces an immunological reaction similar to the Mazzotti reaction (a potentially dangerous immune reaction that can occur after treatment for parasitic worm infections, particularly onchocerciasis caused by the rapid death and breakdown of microfilariae or larval worms in the body) seen in onchocerciasis, characterized by headache, joint pain, dizziness, anorexia, malaise, and urticaria 57, 58. Doxycycline and ivermectin or albendazole is the recommended combination in individuals with onchocerciasis or loaisis (Loa loa). Doxycycline is preferred in areas co-endemic with Loa loa (loaisis) and has also shown the ability to slow the inflammation and fibrosis that leads to worsening lymphedema. Doxycycline also treats Wolbachia, a genus of symbiotic bacteria that inhabit nematodes 28, 53. Filarial nematodes depend on Wolbachia for normal development and fertility 59. Doxycycline has been shown to clear filaria of Wolbachia symbionts, leading to microfilarial and macrofilarial death, and thus provides an attractive treatment option 60, 61, 62. Suramin is widely used in onchocerciasis, yet its role remains uncertain in lymphatic filariasis.
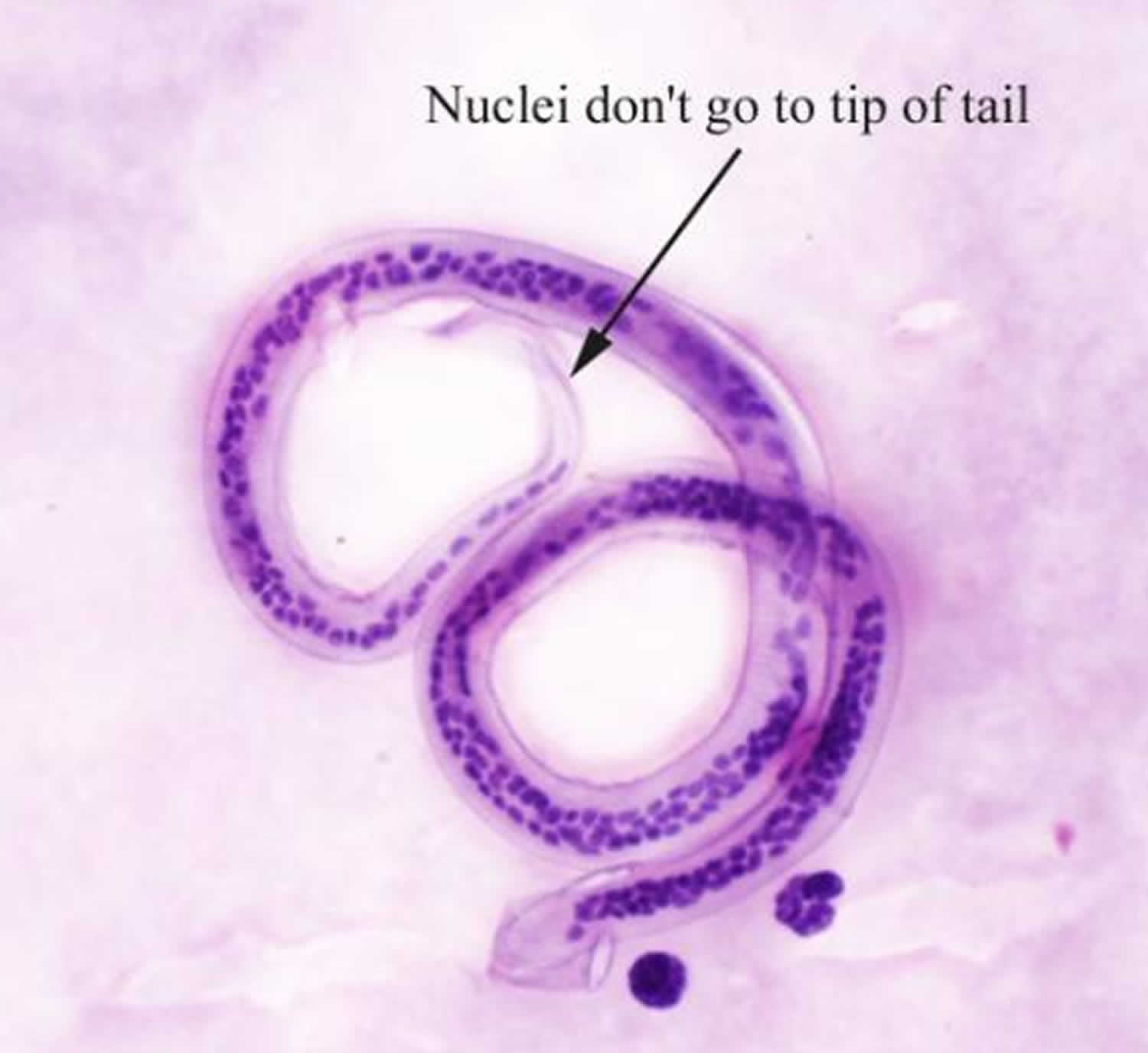
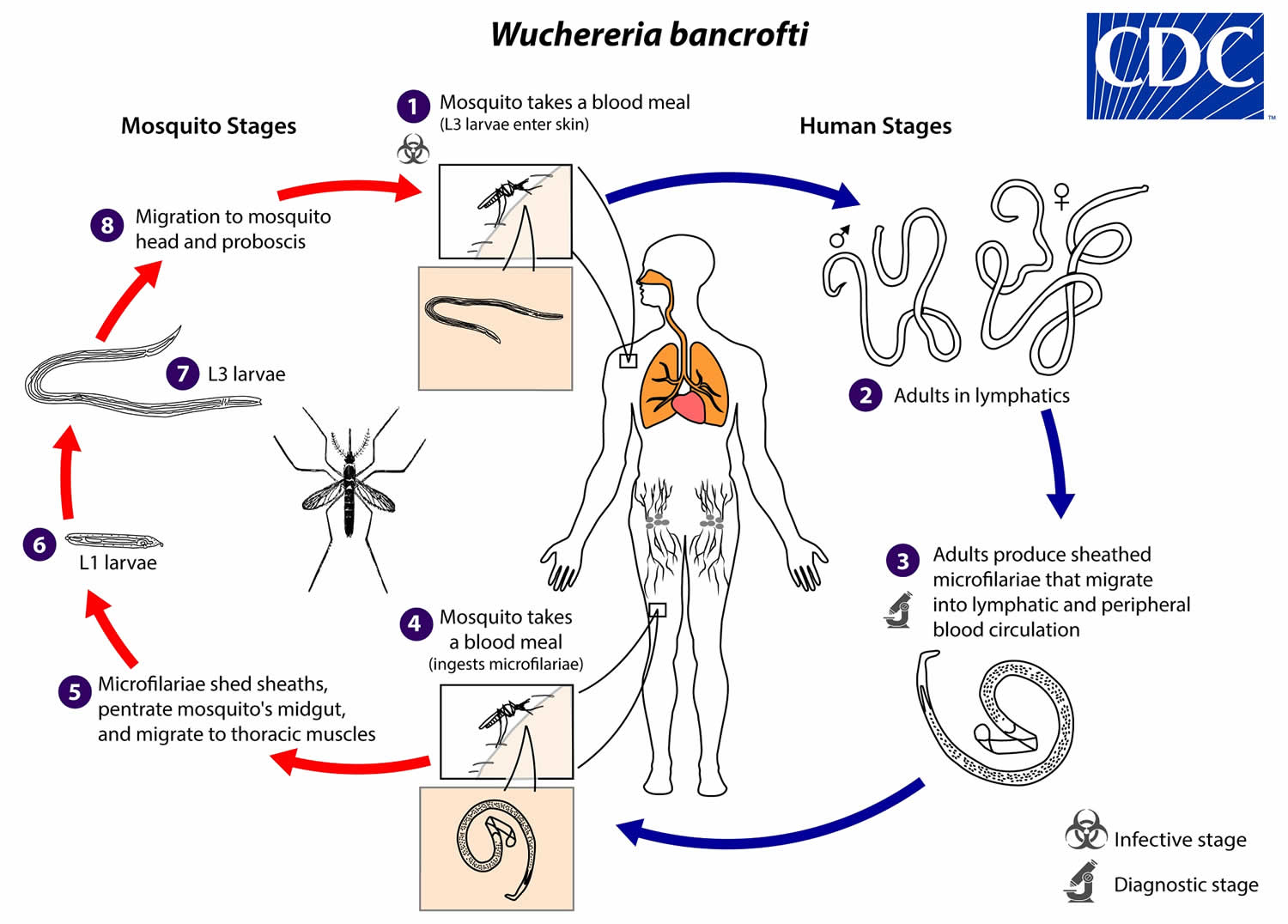
Figure 1. Wuchereria bancrofti
Footnote: Microfilaria of Wuchereria bancrofti in thick blood smear stained with Giemsa. Adults of Wuchereria bancrofti are long and threadlike. The males measure up to 40 mm long and females are 80—100 mm long. Adults are found primarily in lymphatic vessels, less commonly in blood vessels.
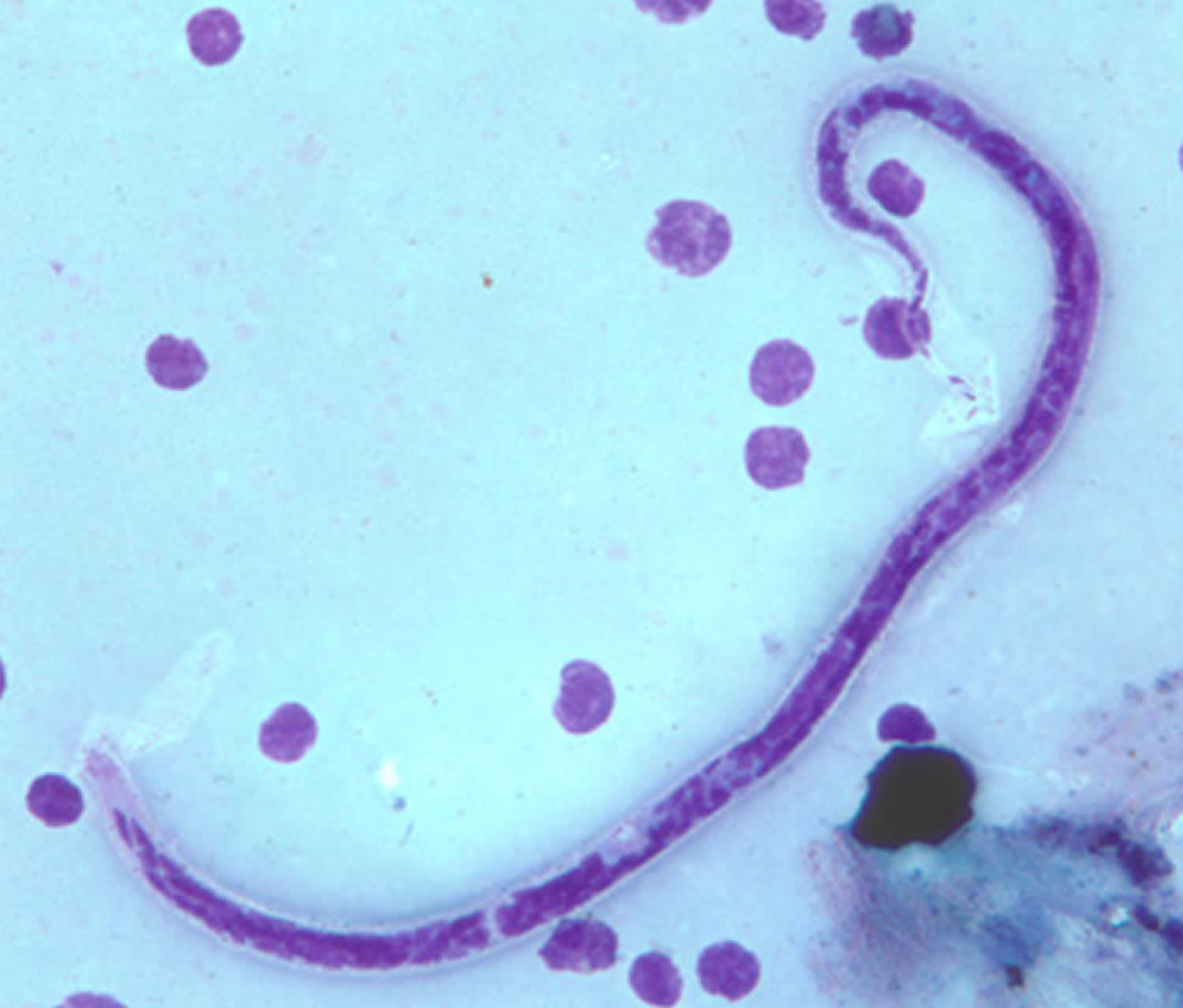
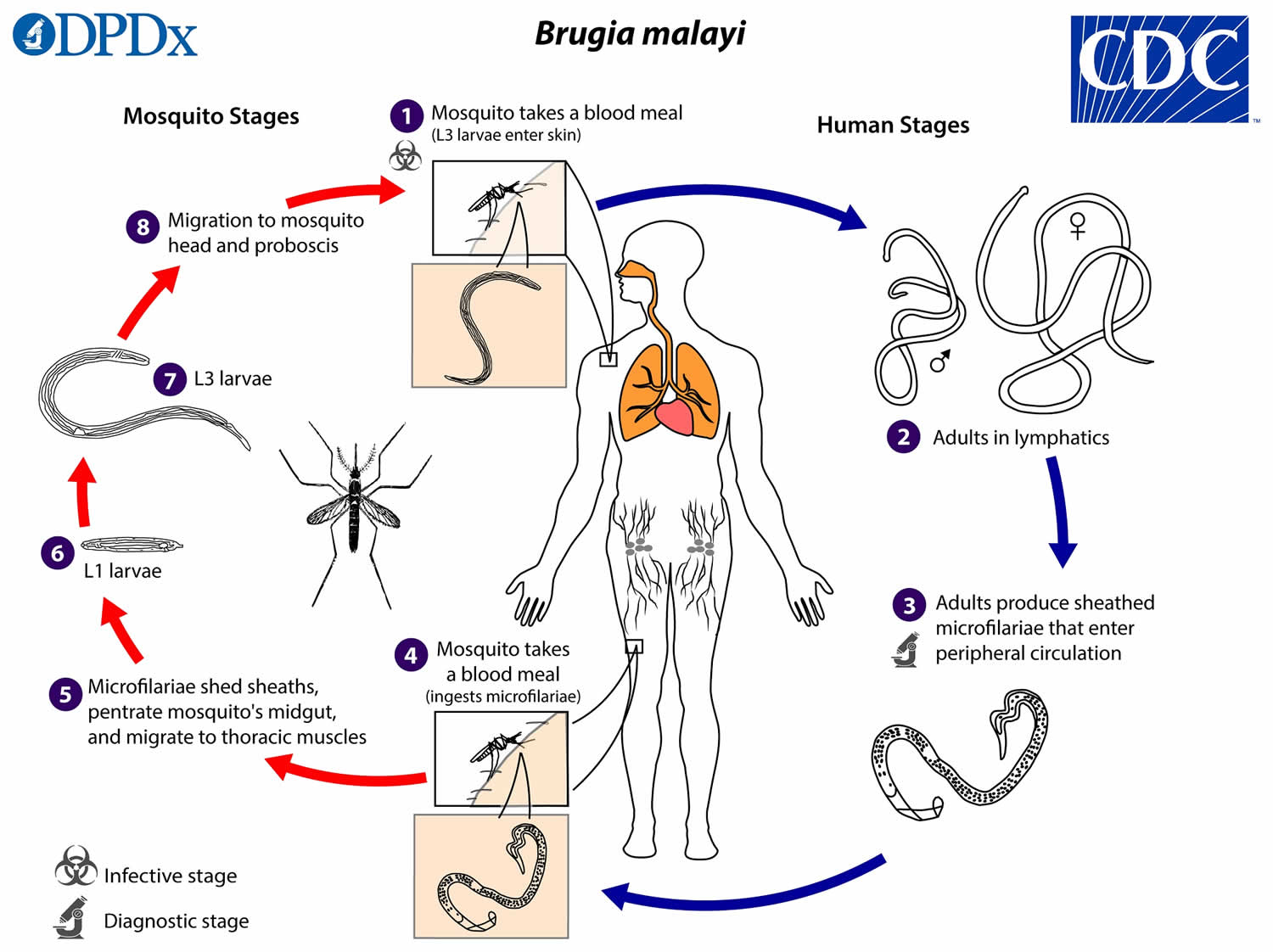
[Source 63 ]Figure 2. Brugia malayi
Footnote: Microfilaria of Brugia malayi in a thick blood smear, stained with Giemsa. The tail is tapered, with a significant gap between the terminal and subterminal nuclei. Microfilariae of Brugia malayi are sheathed and in stained blood smears measure 175—230 micrometer (μm). In 2% formalin they are longer, measuring 240—300 micrometer (μm).
[Source 64 ]Figure 3. Brugia timori
Footnote: Microfilaria of Brugia timori in a thick blood smear, stained with Giemsa and captured at 500x oil magnification. Microfilaria of Brugia timori are sheathed and measure on average 310 micrometer (μm) in stained blood smears and 340 micrometer (μm) in 2% formalin. Microfilaria of Brugia timori differ from Brugia malayi by a having a longer cephalic space, a sheath that does not stain with Giemsa, and a larger number of single-file nuclei towards the tail.
[Source 31 ]Figure 4. Lymphatic filariasis mosquito
Footnote: Aedes polynesiensis mosquito, one of the mosquitoes that transmit lymphatic filariasis. There are 9 species of Anopheles mosquitoes that can transmit lymphatic filariasis in tropical Africa alone. Other mosquitoes include Anopheles, Culex, Mansonia, and Ochlerotatus mosquitoes. Mosquitoes spread lymphatic filariasis from one person to another. Mosquitoes act as intermediate host that transmit microfilariae parasites from an infected human to a susceptible human through blood-feeding 65. When a mosquito bites a person who has lymphatic filariasis, microscopic worms in the person’s blood enter and infect the mosquito (the intermediate host), microfilariae develop into infective larvae (L3 larvae) inside the mosquito which can be transmitted to human. When the infectious mosquito bites another person, that person may be infected and the cycle of spreading lymphatic filariasis continues 66.
Figure 5. Culex quinquefasciatus
Footnotes: Culex quinquefasciatus mosquito is the most important mosquito for transmitting Wuchereria bancrofti. Other mosquitoes that can transmit Wuchereria bancrofti include Anopheles gambiae, Anopheles funestus, Aedes polynesiensis, Aedes scapularis and Aedes pseudoscutellaris. Brugia malayi is spread by Anopheles barbirostris, Anopheles sinensis, Anopheles donaldi and several species of Aedes and Mansonia mosquitoes. Finally, Brugiatimori is transmitted by Anopheles barbirostris.
[Source 67 ]Figure 6. Lymphatic filariasis global distribution
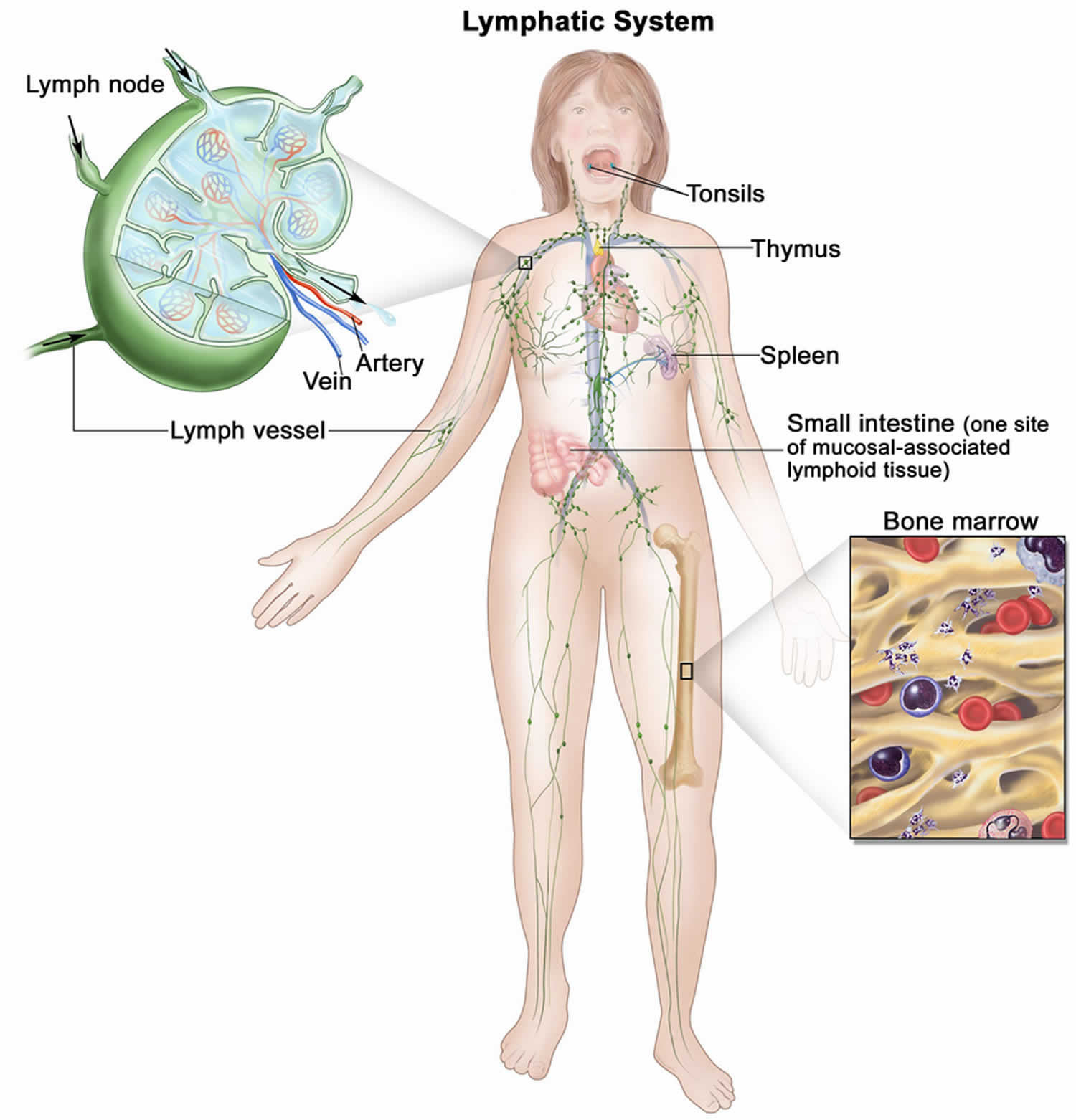
[Source 5 ]Figure 7. Lymphatic System
Footnotes: The human lymphatic system generally includes superficial or primary lymphatic vessels that form a complex dermal network of capillary-like channels. Primary lymphatic vessels lack muscular walls and do not have valves. They drain into larger, secondary lymphatic vessels located in the subdermal space. Secondary lymphatic vessels run parallel to the superficial veins and drain into deeper lymphatic vessels located in the subcutaneous fat adjacent to the fascia. Unlike the primary vessels, the secondary and deeper lymphatic vessels have muscular walls and numerous valves to accomplish active and unidirectional lymphatic flow. An intramuscular system of lymphatic vessels that parallels the deep arteries and drains the muscular compartment, joints, and synovium also exists. The superficial and deep lymphatic systems probably function independently, except in abnormal states, although there is evidence that they communicate near lymph nodes 68. Lymph drains from the lower limbs into the lumbar lymphatic trunk. The lumbar lymphatic trunk joins the intestinal lymphatic trunk and cisterna chyli to form the thoracic duct, which empties into the left subclavian vein. The lymphatic vessels of the left arm drain into the left subclavian lymphatic trunk and then into the left subclavian vein. The lymphatic vessels of the right arm drain into the right subclavian lymphatic trunk and then into the right subclavian vein.
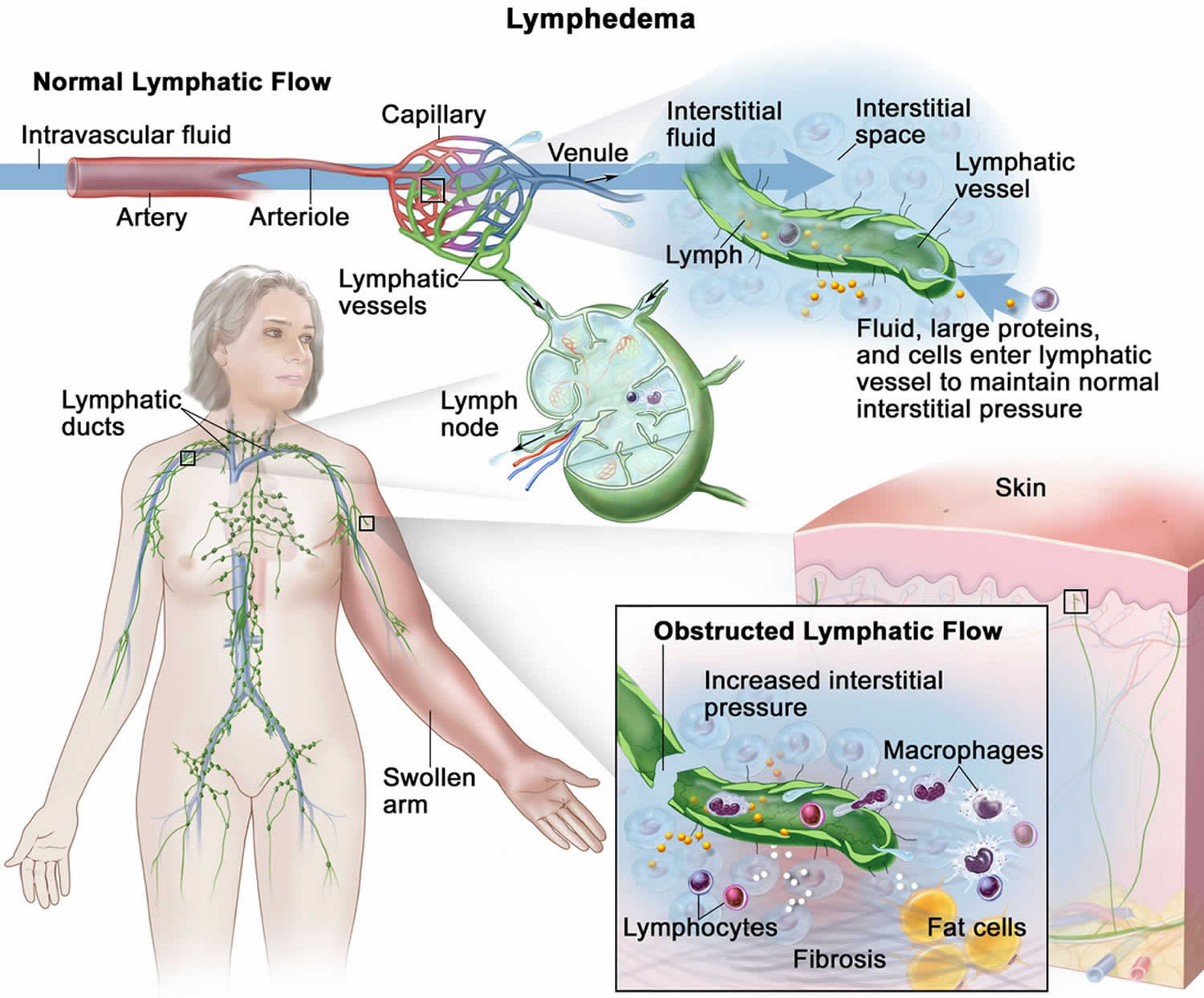
[Source 69 ]Figure 8. Lymphedema
Footnotes: The lymphatic vessels normally maintain normal interstitial pressures by removing the excess interstitial fluid that results from the imbalance between the intravascular fluid that enters from the arterioles and exits into the venules. Large proteins and cells that cannot exit the interstitial space through the venules leave the interstitial fluid through the lymphatic vessels. As the lymph moves through the lymphatic vessels, it passes through lymph nodes and eventually into one of two lymphatic ducts that empty into a large vein near the heart. In lymphedema, the flow of lymph through the lymphatic vessels is disrupted or blocked. This leads to increased interstitial pressure and an accumulation of interstitial fluid, large proteins, and cellular debris in the interstitial space, which induces inflammation. The inflammation may cause further damage to the lymphatic vessels. The macrophages and lymphocytes release inflammatory markers, which causes fibrosis, fat cell hypertrophy, and the classical sign of swelling. Lymphedema may be caused by cancer or cancer treatment.
[Source 69 ]Figure 9. Lymphatic filariasis
Footnotes: (A) A patient with elephantiasis of the left leg. (B) A Haitian Woman suffering from lymphatic filariasis presenting with bilateral lymphedema.
[Source 70 ]What is elephantiasis?
Elephantiasis also known as lymphatic filariasis, is a filarial parasitic infection (filarial worms) transmitted by mosquitoes that blocks your lymphatic system, causing severe swelling and thickening of the skin, often in the limbs, breasts, or genitals 71, 72, 30. People with elephantiasis may also develop inflammation, swelling and fever. Symptoms can take years to appear, even if the infection was acquired in childhood. The condition is a major cause of disability and poverty in tropical and subtropical regions of Africa, Asia, and South America. Diagnosis involves a blood test, and treatment includes antiparasitic medication to kill the worms and supportive care like compression to manage lymphedema. Without treatment, elephantiasis can cause health complications.
Is there a cure for lymphatic filariasis?
All people with filariasis who have microfilaremia (filarial larvae in the blood) or a positive antigen test should receive antifilarial drug treatment to eliminate the microfilariae. Unfortunately, the medicines available have limited effect on adult worms 66, 73.
What is the difference between lymphatic filariasis and podoconiosis?
Podoconiosis also called “mossy foot” or “dust in the feet” is a non-filarial environmentally-induced lymphedema caused by prolonged barefoot exposure to specific, irritant, silica-rich clay soils (silicates, quartz, iron oxides, zirconium) of volcanic origins found in tropical highland regions 74, 75). Podoconiosis results in chronic swelling, skin thickening, and “moss-like” growths on the feet and legs, significantly impacting individuals’ health, social well-being, and economic productivity. Prevention is straightforward and inexpensive, requiring only wearing shoes, covering floors, and practicing good foot hygiene
Podoconiosis is mostly found in highland areas of tropical and sub-tropical areas in Africa, Central and South America and South and South-East Asia 76.
Podoconiosis is a type of tropical lymphedema sharing some clinical characteristics with lymphatic filariasis, podoconiosis is caused by an abnormal inflammatory reaction to the passage of microparticles of silica and aluminum silicates through the skin 77. These particles are taken up by macrophages into the lymphatic system and result in an inflammatory process leading to fibrosis and obstruction of the vessels resulting in lymphedema 74.
Podoconiosis disease process has 3 phases: prodromal, early, and advanced. Prodromal symptoms include itching of the skin of the forefoot and a burning sensation in the foot and lower leg, with variable chills or generalized joint pains 74. These symptoms may progress to the early phase of swelling and splaying of the forefoot and leakage of clear lymph fluid 74. The skin develops hyperkeratotic papillomata that resemble moss or velvet, giving rise to the African term “mossy foot” 74. Acute episodes may cause fever, rigors, and a rapid increase in pain and swelling of the leg. In the advanced phase, hard, fibrotic swelling develops in both legs and feet, though one is usually more severely affected than the other 78.
Treatment of podoconiosis is currently based on lymphedema management (foot hygiene, compression, exercises and elevation), psychosocial and mental health support, and use of shoes to reduce exposure to irritant soil 75). Surgical removal of large nodules can be achieved with satisfactory healing rates, allowing patients to use custom designed shoes.
What causes filariasis?
Filariasis refers to parasitic infection caused by filarial parasites or nematodes (roundworms) of the family Filariidae transmitted to humans by blood-sucking insects, such as mosquitoes, blackflies, or midges, acting as biological vectors 1, 2, 3. Filarial infection is transmitted through the bite of an infected insect as it feeds upon human blood 6. Thereafter, parasite larvae mature into adult forms within the host. These adult parasites then multiply, producing microfilariae, which are subsequently ingested by blood-sucking insects along with human blood. These microfilariae undergo subsequent stages of development within the insect’s bodies (see Lymphatic Filariasis Life Cycle below) 7, 8, 9.
Of the hundreds of described filarial parasites, only 8 species cause natural infections in humans 10:
- Onchocerca volvulus causing Onchocerciasis 11, 12
- Wuchereria bancrofti causing Bancroftian filariasis (lymphatic filariasis)
- Brugia malayi causing Malayan filariasis (lymphatic filariasis) 13, 14
- Brugia timori causing Malayan filariasis (lymphatic filariasis) 13, 14
- Loa loa causing Loiasis 15, 16
- Mansonella species (Dipetalonema spp), Mansonella perstans (Dipetalonema perstans), and Mansonella streptocerca (Dipetalonema streptocerca) causing Mansonelliasis 17, 18, 19, 20
- Dirofilaria species causing Dirofilariasis 21, 22
The location of these parasites within the human body varies from species to species. Filariasis affects a range of human tissues and often display little or no observable host response throughout their development 23, 24. An exception occurs when the parasite enters extremely sensitive tissues, such as the conjunctiva 25.
Filariasis can be classified based on the location of the parasite within the human host’s body 5, 25, 26, 27:
- Lymphatic filariasis: Wuchereria bancrofti, Brugia malayi, Brugia timori;
- Subcutaneous filariasis: Loa loa, Onchocerca volvulus;
- Serous cavity filariasis: Mansonella spp.
Filariasis signs and symptoms and treatment of filariasis depends on the type of filarial parasitic worm (nematode) infection you have.
Filariasis is predominantly a disease of tropical countries and affects the lives of millions of people. Filariasis is spread from host-to-host via the bites of certain flies and mosquitoes that act as vectors for the parasites. For example the filarial nematode Onchocerca volvulus enters the skin from the bite of an infected blackfly (Simulium species). The nematode is in its third larval stage before it moults to its fourth larval stage in 4-6 weeks. Then after some months it moults again to become a juvenile adult that matures and mates after about a year to produce microfilariae. These adult worms live and mate encased in fibrous nodules just below the skin surface and can live there for up to 10-15 years.
It has been discovered that a type of Rickettsia (Wolbachia spp.) has a symbiotic relationship with filarial nematodes. The bacteria initiates the filarial disease process with a severe adverse inflammatory reaction.
Table 1. Filariasis
| Filarial parasite | Filarial disease |
|---|---|
| Onchocerca volvulus | Onchocerciasis |
| Wuchereria bancrofti | Bancroftian filariasis (lymphatic filariasis) |
| Brugia malayi and Brugia timori | Malayan filariasis (lymphatic filariasis) |
| Loa loa | Loiasis |
| Mansonella species | Mansonelliasis |
| Dirofilaria species | Dirofilariasis |
What causes lymphatic filariasis?
Lymphatic filariasis is caused by infection with parasites classified as nematodes (roundworms) of the family Filariodidea. There are 3 types of these thread-like filarial worms:
- Wuchereria bancrofti, which is responsible for 90% of lymphatic filariasis cases.
- Brugia malayi, which causes most of the remainder of lymphatic filariasis cases.
- Brugia timori, which also causes the lymphatic filariasis.
The majority of Wuchereria bancrofti infections occur in South and Southeast Asia, as well as sub-Saharan Africa. Central and South America and the Pacific islands are endemic regions. Brugia malayi has been reported in South and Southeast Asia, India, Indonesia, Thailand, Vietnam, Malaysia, and the Philippines. In contrast, Brugia timori is restricted to eastern Indonesia and East Timor 80.
Male adult filarial worms are about 3 to 4 centimeters in length, and female adult filarial worms 8 to 10 centimeters in length 81. The male and female adult filarial worms together form “nests” in the human lymphatic system and disrupt the normal function of the lymphatic system. The adult filarial worms can live for approximately 6–8 years and, during their life time, produce millions of microfilariae (immature larvae) that circulate in the blood (see Lymphatic Filariasis Life Cycle below). Mosquitoes are infected with microfilariae by ingesting blood when biting an infected host. Microfilariae must mature in the mosquito (the vector) before becoming infective. Microfilariae mature into infective larvae (L3 larvae) within the mosquito. When infected mosquitoes bite people, mature parasite larvae are deposited on the skin, from where they can enter the body. The larvae then migrate to the lymphatic vessels where they develop into adult worms, thus continuing a cycle of transmission.
Lymphatic filariasis is transmitted by 5 different types of mosquitoes including Aedes, Anopheles, Culex, Mansonia, and Ochlerotatus 28. For example by the Culex mosquito, widespread across urban and semi-urban areas, Anopheles, mainly found in rural areas, and Aedes, mainly in endemic islands in the Pacific 82. The typical vector for Brugia malayi and Brugia timori filariasis are mosquito species in the genera Mansonia and Aedes 31. Wuchereria bancrofti is transmitted by many different mosquito genera/species, depending on geographical distribution. Among them are Aedes spp., Anopheles spp., Culex spp., Mansonia spp., and Coquillettida juxtamansonia 31.
Acute lymphatic filariasis is related to larval molting and adult maturation to fifth-stage larvae. Adult worms are found in lymph nodes and lymphatic vessels distal to the nodes. Females measure 80-100 mm in length and males are 30 mm to 40 mm.
The most commonly affected lymph nodes are in the femoral and epitrochlear regions. Abscess formation may occur at the nodes or anywhere along the distal vessel. Infection with Brugia timori appears to result in more abscesses than infection with Brugia malayi or Wuchereria bancrofti 83.
Cellular invasion with plasma cells, eosinophils, and macrophages, together with hyperplasia of the lymphatic endothelium, occurs with repeated inflammatory episodes 83. The consequence is lymphatic damage and chronic leakage of protein-rich lymph in the tissues, thickening and verrucous changes of the skin, and chronic streptococcal and fungal infections, all of which contribute to the appearance of elephantiasis. The skin of individuals with elephantiasis is characterized by hyperkeratosis, acanthosis, lymph and fatty tissue, loss of elastin fibers, and fibrosis.
Brugia malayi elephantiasis is more likely to affect the upper and lower limbs, with genital pathology and chyluria being rare. Secondary bacterial infection in elephantiasis can result in blindness.
The exact mechanism behind the lymphatic damage involves a complex interplay of lymphangiectasia and inflammatory reactions triggered by the dying worms. Adult filarial worms usually reside in the afferent, efferent, and hilar lymphatics, causing blockage and subclinical lymphangiectasia. Moreover, lymphatic damage also results from the host’s immune response to the parasite’s endosymbiont Wolbachia. Antigens released by the dying worms trigger inflammatory reactions causing lymphatic damage.
Clinical progression of the disease varies in individuals depending on the host’s immune response. Chronicity of the infection has been attributed to the suppression of Th1 and Th2 immune responses. The asymptomatic carrier state has links to the synergistic interplay between poly-specific natural IgG4 and anti-filarial IgG4 in blocking the pathogenesis 84, 85, 86. Genetic predisposition to lymphedema and prenatal exposure in endemic areas also play a vital role.
What causes lymphedema?
The lymph or lymphatic system is part of your body’s immune system. The lymphatic system helps maintain the right balance of fluids in your body, transports immune cells and nutrients, and filters out germs and waste.
- Lymph fluid is the clear fluid inside lymph vessels that travels throughout the body. It contains proteins, salts, water, and white blood cells (infection-fighting cells).
- Lymph vessels carry the lymph fluid throughout the body. One-way valves inside lymph vessels help move the fluid and control the flow.
- Lymph nodes are small, bean-sized glands along the lymph vessels that help filter germs, dead cells, and other waste. Lymph nodes are in many parts of the body, including the neck, armpit, chest, abdomen (belly), and groin.
In some ways, the lymphatic system works like the cardiovascular system (heart and blood vessel system). Both systems transport fluid (blood or lymph) through vessels throughout your body. But your cardiovascular system (heart and blood vessel system) has a powerful pump (the heart) to move blood through the body. The lymph system doesn’t have a pump. Instead, it relies on lymph nodes and the movement of muscles to keep fluid moving. This is why the lymph system is more likely to have poor drainage in some places, especially if lymph nodes are damaged or removed.
Lymphedema occurs when disruption of normal lymphatic drainage leads to accumulation of protein-rich lymph fluid in the interstitial space (the space between cells in tissues). Cancer survivors who experience lymphedema report poor physical functioning, impaired ability to engage in normal activities of daily living, and increased psychological distress 87, 88, 89, 90, 91.
Lymphedema is most common in your arms and legs. But since you have lymph nodes throughout your body, it can develop anywhere.
It’s important to identify and treat lymphedema as early as possible when it’s most likely to be reversible. Lymphedema that isn’t treated can get worse and even become permanent. The goals of lymphedema treatment are to reduce swelling, prevent infection (cellulitis), improve ability to move and function, and relieve discomfort.
Common signs and symptoms of lymphedema can include:
- Swelling, fullness, or heaviness in the breast, chest, shoulder, arm, hand, leg, or foot
- Skin changes such as dryness, discoloration, thickening, or dimpling
- New aching, tingling, numbness, pain, or discomfort
- Less movement or flexibility in your joints
- Trouble putting clothes on, feeling clothes are tighter, or leaving indents on your skin
- Your shirt collar, ring, watch, or bracelet feels tight, even though you haven’t gained weight.
Stages of lymphedema
- Stage 0: No visible swelling, but slight symptoms such as feeling the area is heavy, full, or tight. Reversible.
- Stage 1 (mild): Visible swelling. Area might also feel heavy, full, or tight. If arms or legs are involved, the swelling improves when the arm or leg is raised. Usually reversible.
- Stage 2 (moderate): More swelling than stage 1. If arms or legs involved, swelling doesn’t get better when the arm or leg is raised. Worse symptoms than stage 1. May be reversible if treated early.
- Stage 3 (severe): Extreme swelling that often limits self-care or everyday activities. Skin can be very dry, thickened, or discolored. May have fluid leaking or blisters. Usually not reversible.
Lymphedema – graded based on the extent of the condition 92:
- Grade 1: Extremity pitting edema, reversible
- Grade 2: Extremity pitting or nonpitting edema, nonreversible
- Grade 3: Nonpitting, nonreversible edema, with skin thickening
- Grade 4: Nonpitting, nonreversible, thickened, and nodular appearance of the skin, classified as elephantiasis.
Lymphatic Filariasis Life Cycle
Brugia and Wuchereria species are similar in morphology and are the main cause of filariasis. The life cycle of lymphatic filariasis involves humans as the primary reservoir for this parasitic disease (definitive host), and mosquitoes are the vector (intermediate host). Mosquitoes of the genera Aedes, Anopheles, Culex, and Mansonia ingest microfilariae when they bite humans 93. The ingested microfilaria travel through the mosquitoes stomach wall into the flight muscles, where they mature into infective larval stages. These infectious form eventually migrate to the proboscis from where they get injected into the human skin during the bite. They then travel through the dermis into the regional lymph nodes and further mature into male and female larval worms. The larvae have a predilection to deposit in femoral lymph nodes. They undergo sexual reproduction, and females give birth to countless microfilariae, which are dumped into the bloodstream in a diurnal pattern reaching their highest concentration in the blood at night 94. Female larvae can give off eggs for approximately 5 years, and adults can live up to 9 years 48. With the proliferation of adult worms, the lymphatics become blocked, which disrupts the lymphatic drainage and increases the susceptibility to repeated infections – most notably streptococcal and fungal infections. This acute-on-chronic inflammation leads to fibrosis and remodeling of the lymphatics, further perpetuating contractile dysfunction and leading to the dermal skin changes seen with elephantiasis 95, 48.
Brugia and Wuchereria worms can be identified to the genus level using size, body wall composition, thickness, and morphology of the cuticle. The presence of small filarial worms in lymph nodes is pathognomonic for either Wuchereria or Brugia. Adult worms are typically found in lymph nodes in the groin or neck, whereas microfilariae are typically found in the peripheral blood 25.
The adult worms typically range in size from 45 to 100 micrometers in diameter and are typically found in lymph node cross-sections. Their descriptions include “thin, smooth cuticle which is thickened over lateral chords, three or four well-developed, low, broad muscle cells per quadrant, and relatively broad, flat lateral chords” 25.
Microfilariae can be seen with a blood smear or other peripheral blood sample that is stained with either Giemsa or hematoxylin and eosin (H&E) stain. The blood samples should be taken after 8 pm. The microfilariae vary in size from 200 to 300 micrometers in length and 2 to 8 micrometers in diameter and are identified by the terminal and subterminal nuclei in the tail region 25.
Wuchereria bancrofti life cycle
During a blood meal, an infected mosquito introduces third-stage filarial larvae onto the skin of the human host, where they penetrate into the bite wound (number 1). They develop in adults that commonly reside in the lymphatics (number 2). The female worms measure 80 to 100 mm in length and 0.24 to 0.30 mm in diameter, while the males measure about 40 mm by 1 mm. Adults produce microfilariae measuring 244 to 296 μm by 7.5 to 10 μm, which are sheathed and have nocturnal periodicity, except the South Pacific microfilariae which have the absence of marked periodicity. The microfilariae migrate into lymph and blood channels moving actively through lymph and blood (number 3). A mosquito ingests the microfilariae during a blood meal (number 4). After ingestion, the microfilariae lose their sheaths and some of them work their way through the wall of the proventriculus and cardiac portion of the mosquito’s midgut and reach the thoracic muscles (number 5). There the microfilariae develop into first-stage larvae (number 6) and subsequently into third-stage infective larvae (number 7). The third-stage infective larvae migrate through the hemocoel to the mosquito’s prosbocis (number 8) and can infect another human when the mosquito takes a blood meal (number 1).
Figure 10. Wuchereria bancrofti life cycle
Brugia malayi life cycle
During a blood meal, an infected mosquito typically Mansonia species and Aedes species introduces third-stage filarial larvae onto the skin of the human host, where they penetrate into the bite wound (number 1). They develop into adults that commonly reside in the lymphatics (number 2). The adult worms outwardly resemble those of Wuchereria bancrofti but are smaller. Female worms measure 43 to 55 mm in length by 130 to 170 μm in width, and males measure 13 to 23 mm in length by 70 to 80 μm in width. Adults produce microfilariae, measuring 177 to 230 μm in length and 5 to 7 μm in width, which are sheathed and have nocturnal periodicity (in some regions Brugia malayi may be sub-periodic, and note that microfilariae are usually not produced in Brugia pahangi infections). The microfilariae migrate into lymph and enter the blood stream reaching the peripheral blood (number 3). A mosquito ingests the microfilariae during a blood meal (number 4). After ingestion, the microfilariae lose their sheaths and work their way through the wall of the proventriculus and cardiac portion of the midgut to reach the thoracic muscles (number 5). There the microfilariae develop into first-stage larvae (number 6) and subsequently into third-stage larvae (number 7). The third-stage larvae migrate through the hemocoel to the mosquito’s proboscis (number 8) and can infect another human when the mosquito takes a blood meal (number 1).
Figure 11. Brugia malayi life cycle
[Source 97 ]Filariasis Prevention
The best way to prevent filariasis is by preventing spread of the parasites by vector control. This means eliminating or controlling infected flies and mosquitoes. Research is underway to find a biological agent that will eliminate the vector and is inexpensive, non-toxic to humans and deployable on a large scale. It is important to take steps to avoid mosquito bites even if you are taking medications as an added layer to prevent filariasis.
Elimination of lymphatic filariasis is possible by stopping the spread of the infection through preventive drug therapy. The World Health Organization (WHO) recommended preventive drug strategy for lymphatic filariasis elimination using mass drug administration (MDA) 98. Mass drug administration (MDA) involves administering an annual dose of medicines to the entire at-risk population. The medicines used have a limited effect on adult parasites but effectively reduce the density of larval worms in the body (microfilariae in the bloodstream) and prevent the spread of parasites to mosquitoes 98. It is worth noting that mass drug administration (MDA) does not cure filarial infections, but it can reduce or interrupt transmission of new infections by clearing larval parasites from human blood so that they are not available for mosquitoes, which are the vectors (intermediate hosts) 99 .
The mass drug administration (MDA) regimen recommended depends on the co-endemicity of lymphatic filariasis with other filarial diseases. WHO recommends the following mass drug administration (MDA) regimens 98:
- Albendazole (400 mg) alone twice per year for areas co-endemic with loiasis;
- Ivermectin (200 mcg/kg) and albendazole (400 mg) in countries with onchocerciasis;
- Diethylcarbamazine citrate (DEC) (6 mg/kg) and albendazole (400 mg) in countries without onchocerciasis; and
- Ivermectin (200 mcg/kg) together with diethylcarbamazine citrate (DEC) (6 mg/kg) and albendazole (400 mg) in countries without onchocerciasis and where other programmatic conditions are met.
The impact of mass drug administration (MDA) depends on the efficacy of the regimen and the coverage (proportion of total population ingesting the medicines). Mass drug administration (MDA) with the 2-medicine regimens have interrupted the transmission cycle when conducted annually for at least 4–6 years with effective coverage of the total population at risk. Salt fortified with diethylcarbamazine citrate (DEC) has also been used in a few unique settings to interrupt the transmission cycle.
Mosquito control
Mosquito control is used to reduce transmission of lymphatic filariasis and other mosquito-borne infections. Depending on the parasite-vector species, measures such as insecticide-treated nets, indoor residual spraying or personal protection measures may help protect people from infection. The use of insecticide-treated nets in areas where Anopheles is the primary vector for filariasis enhances the impact on transmission during and after mass drug administration (MDA). Historically, mosquito control has in select settings contributed to the elimination of lymphatic filariasis in the absence of large-scale preventive drug therapy.
Preventing Mosquito Bites
Mosquitoes bite day and night. They spread parasites through bites that can make you sick. Take steps to protect yourself and your family from mosquito bites that can make you sick.
- Use Environmental Protection Agency (EPA)-registered insect repellents.
- Tips for babies and children:
- Dress your child in clothing that covers arms and legs.
- Cover strollers and baby carriers with mosquito netting.
- When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) [a plant-derived ingredient] or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
- Adults: Apply repellent onto your hands and then apply to a child’s face.
- Tips for everyone:
- Always follow the product label instructions.
- Reapply repellent as directed.
- Do not apply repellent on the skin under clothing.
- If you are using sunscreen, apply sunscreen first and insect repellent second.
- Tips for babies and children:
- Wear loose-fitting, long-sleeved shirts and pants.
- Wear clothing and gear treated with permethrin. Permethrin is an insecticide that kills or repels mosquitoes.
- Permethrin-treated clothing provides protection after multiple washings.
- Do not use permethrin products directly on skin.
- Control mosquitoes indoors and outdoors. Stop mosquitoes from laying eggs in or near water.
- Check for water-holding containers both indoors and outdoors.
- Once a week, empty and scrub, turn over, cover, or throw out items that hold water, such as tires, buckets, toys, pools, birdbaths, flowerpot saucers, or trash containers.
Filariasis signs and symptoms
Filariasis signs and symptoms vary depending on the type of filarial infection, body location and can be acute or chronic in nature. Up to 70% of infected individuals remain asymptomatic. Symptoms usually do not manifest until adolescence or adulthood, when worm burden usually is the highest. Several symptomatic variations have been observed 46. Because cases of filariasis in North America and high-income countries are uncommon, physicians initially may miss the diagnosis in these areas. To avoid this pitfall, physicians should obtain and document a thorough travel history from patients with suspicious lesions.
Lymphatic filariasis signs and symptoms
Lymphatic filariasis can be caused by either Wuchereria bancrofti (Bancroftian filariasis), Brugia malayi (Malayan filariasis) or Brugia timori (Malayan filariasis).
The clinical course of lymphatic filariasis is broadly divided into the following:
- Asymptomatic microfilaremia – Patients with microfilaremia are generally asymptomatic, although those with heavy microfilarial loads may develop acute and chronic inflammatory granulomas secondary to splenic destruction. Passage of cloudy milklike urine may denote chyluria
- Acute phases of adenolymphangitis (ADL) – This refers to the sudden onset of febrile, painful lymphadenopathy. Pathologically, the lymph node is characterized by a retrograde lymphangitis, distinguishing it from bacterial lymphadenitis. Symptoms usually abate within 1 week, but recurrences are possible 47. Signs and symptoms of adenolymphangitis (ADL) include episodic attacks of fever associated with inflammation of the inguinal lymph nodes, testis, and spermatic cord, as well as with lymphedema. Skin exfoliation of the affected body part usually occurs with resolution of an episode.
- Chronic, irreversible lymphedema and hydrocele
- Lymphedema – the most common presentation that develops over a long period due to chronic lymphatic damage. It characteristically presents with swelling of the limbs either upper or lower depending on the involvement of inguinal or axillary lymphatic vessels. Pitting edema develops in the early stages of the disease, which later progresses into brawny non-pitting type. Elephantiasis is the most severe type of lymphedema characterized by severe swelling of the limbs, genitalia, and breasts. The skin becomes thick and hard, owing to hyperpigmentation and hyperkeratosis.
- Hydrocele (a fluid-filled sac around a testicle that causes painless swelling of the scrotum) – this is one of the debilitating morbidities associated with chronic lymphatic filariasis. It can be unilateral or bilateral, leading to enlargement of the scrotum. It can be very large, reaching up to 40 cm.
Lymphatic filariasis is a long-lasting, chronic, and persistent disease, with the majority of infected individuals remaining asymptomatic, showing no external signs of infection while contributing to the transmission of the parasite. These asymptomatic infections still cause damage to the lymphatic system and the kidneys and alter your body’s immune system.
Lymphatic filariasis can manifest in a wide range of clinical signs, including lymphedema of the legs, lymphangitis, elephantiasis, and, uniquely in Wuchereria bancrofti (Bancroftian filariasis)-infected individuals, hydrocele (a fluid-filled sac around a testicle that causes painless swelling of the scrotum) 100. Asymptomatic infections are characterized by the presence of several regulatory immune processes driven by living parasites that promote their long-term survival 101, 102, 103, 104. The precise mechanisms by which lymphatic filariasis clinical disease manifests remain uncertain, although it is likely to be associated with the host’s inflammatory response to dead or dying adult parasites. The parasites’ death results in inflammation of lymphatic vessels and lymph nodes, which may cause pain and swelling in the affected area 100, 105. The susceptibility to infection, host response, and the risk of developing pathological features are familial and probably related to host genetic predisposition 106, 107, 108.
Lymphatic filariasis symptoms predominantly result from the presence of adult worms residing in the lymphatics. They include the following 48:
- Fever
- Groin (inguinal) or armpit (axillary) swollen or enlarged lymph nodes (lymphadenopathy)
- Testicular and/or inguinal pain
- Skin exfoliation
- Limb or genital swelling. Repeated episodes of inflammation and lymphedema lead to lymphatic damage, chronic swelling, and elephantiasis of the legs, arms, scrotum (hydrocele), vulva, and breasts
The following acute syndromes have been described in lymphatic filariasis 2:
- Acute adenolymphangitis (ADL) – repeated bouts of lymphangitis causing lymphedema.
- Filariatic fever – manifests with lymphangitis and lymphadenitis with nonspecific symptoms, including headache, fever, chills, and general malaise.
- Filarial abscess – may form, causing localized swelling and pain until rupture, which results in the discharge of dead adult worms. Granulomatous reactions can lead to lumps in subcutaneous tissues 48.
- Tropical pulmonary eosinophilia (TPE). Tropical pulmonary eosinophilia (TPE) is an immune response or hypersensitivity lung reaction to filarial parasites, primarily from Wuchereria bancrofti and Brugia malayi, and is marked by peripheral hypereosinophilia (high eosinophil count) and eosinophilic pulmonary infiltrate causing pulmonary restrictive lung disease, wheezing, shortness of breath, dry paroxysmal nocturnal cough, chest pain, anorexia, malaise, weight loss, splenomegaly, and bloody sputum 109. The syndrome, often seen in tropical regions most frequently in South and Southeast Asia, but increasingly in travelers, is typically misdiagnosed as asthma and is effectively treated with diethylcarbamazine (DEC) 48. Without treatment, tropical pulmonary eosinophilia (TPE) can lead to interstitial lung disease and other complications.
Acute episodes of local inflammation involving skin, lymph nodes and lymphatic vessels often accompany chronic lymphoedema or elephantiasis. Some of these episodes are caused by the body’s immune response to the parasite. Most are the result of secondary bacterial skin infection where normal defenses have been partially lost due to underlying lymphatic damage. These acute attacks are debilitating, may last for weeks and are the primary cause of lost wages among people suffering with lymphatic filariasis.
When lymphatic filariasis develops into chronic conditions due to dysfunction of lymphatic vessels it leads to lymphoedema (tissue swelling) or elephantiasis (skin/tissue thickening) of limbs and hydrocele (scrotal swelling).
The most obvious symptom of lymphatic filariasis is elephantiasis. This is a condition where the limbs swell to the point that they resemble an elephant’s foreleg in size, texture and color and the skin may become thick and pitted and secondary infection are frequent due to lymphatic dysfunction. The thickening of the skin and swelling of underlying tissues (edema) is caused by parasites lodged in the lymphatic system, a network of channels, nodes and organs that maintain proper fluid levels in the body. Elephantiasis appears to be due an immune response to the dead and dying worms in the lymphatic system. Mainly limbs, breasts and genital organs are affected. Without treatment continued lymphatic damage will lead to irreversible elephantiasis. Such body deformities often lead to social stigma and sub-optimal mental health, loss of income-earning opportunities and increased medical expenses for patients and their caretakers. The socioeconomic burdens of isolation and poverty are immense.
Occult filariasis
Occult filariasis denotes filarial infection in which microfilariae are not observed in the blood but may be found in other body fluids and/or tissues.
The occult lymphatic filariasis syndromes are as follows:
- Tropical pulmonary eosinophilia (TPE) – Symptoms result from allergic and inflammatory reactions elicited by the microfilariae and parasite antigens of Wuchereria bancrofti and Brugia malayi that the lungs clear from the bloodstream
- Dirofilaria immitis or Dirofilaria repens infection (Dirofilariasis) – Human infection with Dirofilaria immitis may result in pulmonary lesions of immature Dirofilaria worms in the lung periphery; if Dirofilaria immitis larvae lodge in branches of the pulmonary arteries, they can cause pulmonary infarcts
- Filarial arthritis
- Filarial breast abscess
- Filarial-associated immune-complex glomerulonephritis
Subcutaneous Filariasis
Subcutaneous filariasis is primarily characterised by cutaneous (skin) and subcutaneous symptoms resulting from nematode infections, including those caused by Onchocerca volvulus, Loa loa, and Mansonella ozzardi 110.
Onchocerca volvulus (onchocerciasis) is predominantly impacting sub-Saharan Africa, Yemen, and regions of Central and South America 111, 112. Loa loa (Loiasis) primarily affects rural populations in Central and West Africa, with over 20 million patients chronically infected in regions with medium to high transmission rates 113, while Mansonella ozzardi, one of three species in the genus Mansonella (the others being Mansonella perstans and Mansonella streptocerca) causing mansonellosis 114, is common across the neotropical region from southern Mexico to northwestern Argentina 20.
Subcutaneous filariasis symptoms include the appearance of papules, nodules, and scratches on the skin surface, which becomes dry and thickened, often accompanied by changes in skin pigmentation and intense itch 115.
Onchocerciasis
Onchocerca volvulus microfilariae from the skin are ingested by the Simulium species of blackflies. Onchocercal dermatitis is the most common sign and symptom of onchocerciasis. The skin becomes very itchy and a red spotty rash is often present. Scratching often leads to bleeding, ulcers and secondary infections. The lower trunk, pelvis, buttocks, thighs and legs appear to be the most affected. Microfilariae are the main cause of Onchocercal dermatitis.
In addition to onchodermatitis, nodules containing adult worms called onchoceromas develop just below the skin surface. These nodules can be up to several centimetres in diameter and are usually firm, flattened or bean-shaped, movable and non-tender. They most often occur over bony parts of the body such as the skull, ribs, scapulae, elbows, and knees.
If left untreated, onchoceriasis can lead to chronic skin changes. Skin loses its elasticity and layers of the skin start to die and form scar tissue. This very thin wrinkled skin results in an elephant-skin appearance that later turns into something like lizard skin.
Chronic onchocerciasis cases are hyper-responsive to parasite antigen, have increased eosinophilia, and result in the presence of high levels of serum IgE. Patterns of onchocercal eye disease also are associated with parasite strain differences at the DNA level 116.
Eye lesions are usually related to the duration and severity of infection and are caused by an abnormal host immune response to microfilariae; loss of visual acuity may occur.
Common eye findings in onchocerciasis include the following 117:
- Punctate keratitis
- Pannus formation
- Corneal fibrosis
- Iridocyclitis
- Glaucoma
- Choroiditis
- Optic atrophy
Loiasis
Mango flies or deerflies of Chrysops genus transmit Loa loa infection also known as African eye worm or Loiasis. Response to Loa loa infection appears to differ between residents and nonresidents in endemic areas. Nonresidents with Loa loa infection (Loiasis) appear to be more prone to symptoms than residents despite lower levels of microfilaremia. Eosinophil, serum IgE, and antibody levels are also higher in nonresidents with infection 118. Loa loa infection or Loiasis, is currently not recognized by the World Health Organisation (WHO) as one of the key neglected tropical diseases. The typical clinical manifestation of loiasis, occurring in approximately 80% of individuals, is the migration of the adult parasite under the sclera or subconjunctival eyelid tissue 119.
The initial bite from a redfly infected with the Loa loa parasite causes redness, swelling and itching. As the parasite moults to larval stage 4 it causes red urticarial papules (itchy red spots) in the skin of the affected area. Then over the next 3 months or more as it develops into the adult form, patients may experience pain and numbness of the affected area, temporary swelling of a limb, itchiness and occasionally hives.
The diagnostic feature of loiasis is the Calabar swelling, a large transient area of localized, nonerythematous subcutaneous edema. This is most common observed around joints.
Peripheral nerve involvement in loiasis also has been described 120. Microfilaremia tends to be asymptomatic. Occasionally, the worm is observed migrating through subconjunctival or other tissues.
Meningoencephalopathy is a severe and often fatal complication of Loa loa infection. This syndrome is usually related to diethylcarbamazine (DEC) administration in individuals with high-density microfilaremia but it may occur without drug therapy 121. Diethylcarbamazine (DEC) causes a large influx of microfilariae into the cerebrospinal fluid, leading to capillary obstruction, cerebral edema, hypoxia, and coma. Localized necrotizing granulomas are also present, in response to microfilariae. Endomyocardial fibrosis, nephritic syndrome, and venous thrombosis also may be observed.
Mansonelliasis
Mansonella ozzardi infection can manifest as a skin rash, headache, fever, itching, lymphoedema (e.g., swelling of the arms or legs), and joint pain 122. Most patients infected with Mansonella perstans (Mansonellosis) do not experience any symptoms. Newcomers to an endemic area who become infected appear to experience more symptoms than local inhabitants. Symptoms include swelling of the arms, shoulders, and face; abdominal pain; itchiness; fatigue; and joint pain.
The most common symptom of a patient infected with Mansonella streptocerca (streptocerciasis) is chronic itching dermatitis that is often confined to one part of the torso. Constant scratching may thicken the skin.
Dirofilariasis
Humans are poor hosts for this filarial parasite (Dirofilaria immitis, Dirofilaria repens, and Dirofilaria tenuis) as the worm usually dies before reaching sexual maturity. However in recent years there has been a reported increase in the number of human dirofilariasis cases. The head, neck, breasts, arms, legs and scrotum are most commonly affected. A flesh-colored to red inflamed tender nodule develops. This can be painful and cause burning and itching.
Human infections with Dirofilaria immitis can result in areas of inflammation induced by dying adult worms in pulmonary arteries that appear as coin lesions on chest x-rays. Coin lesions can also be caused by cancer and other serious diseases, and a coin lesion discovered accidentally on chest x-ray usually leads to an invasive procedure to learn the cause. Most human cases of pulmonary dirofilariasis are diagnosed from samples taken during these procedures. Most reported cases of Dirofilaria immitis infection in humans have been in persons with no symptoms. People with symptoms can have cough (including coughing up blood), chest pain, fever, and pleural effusion (excess fluid between the tissues that line the lungs and the chest cavity). Rarely, Dirofilaria immitis worms have been found in humans at outside the lungs, including the brain, eye, and testicle. When Dirofilaria repens and Dirofilaria tenuis infection is reported in humans, it is generally as the cause of nodules under the skin, but on occasion, worms are found in the conjunctiva.
Filariasis Complications
The chronic manifestations of lymphedema and/or hydrocele will develop in approximately 30% of people infected 123. Lymphedema mostly affects the legs, but can also occur in the arms, breasts, and genitalia. Most people develop these symptoms years after the initial infection has cleared.
Filarial hydrocele is thought to be the consequence of lymphatic damage caused by adult worms. Chyluria, which results from rupture of dilated lymphatics into the renal pelvis, can occur as a manifestation of bancroftian filariasis. Microscopic hematuria and proteinuria are also found in lymphatic filariasis patients.
Recurrent secondary bacterial infections of the affected extremity, characterized by severe pain, fever and chills, hasten the progression of lymphedema to its advanced stage, known as elephantiasis.
Another complication of lymphatic filariasis is tropical pulmonary eosinophilia (TPE) syndrome, a potentially serious, progressive lung disease characterized by fever and non-productive, nocturnal cough, wheezing, or both. Symptoms result from immune hyper-responsiveness to microfilariae in the pulmonary capillaries. Signs include marked eosinophilia, high serum immunoglobulin E (IgE) concentrations, and positive antifilarial antibodies. Peripheral microfilaremia is absent in patients with tropical pulmonary eosinophilia (TPE). Most cases of tropical pulmonary eosinophilia (TPE) have been reported in long-term residents from Asia, with men ages 20 – 40 most commonly affected.
Filariasis diagnosis
In general, the diagnostic approach varies by group of filariasis. Traditionally, the diagnosis of filariasis requires demonstrating microfilariae in the peripheral blood or skin. However, circulating filarial antigens (CFA) are now routinely used to diagnose Wuchereria bancrofti infection 49. The microfilariae of all species that cause lymphatic filariasis and the microfilariae of Loa loa, Mansonella ozzardi, and Mansonella perstans can be detected on a blood smear 50.
Microfilariae are detectable via examination of the following:
- Blood – The microfilariae of all species that cause lymphatic filariasis and the microfilariae of Loa loa, Mansonella ozzardi, and Mansonella perstans are detected in blood. Wuchereria bancrofti can be detected via circulating filarial antigen (CFA) assays. However, assays for circulating parasite antigen of Wuchereria bancrofti are not presently approved by the U.S. Food and Drug Administration (FDA). There are no antigen test for Brugia spp. Serologic enzyme immunoassay tests, including antifilarial IgG1 and IgG4, provide an alternative to microscopic detection of microfilariae for the diagnosis of lymphatic filariasis. Patients with active filarial infection typically have elevated levels of antifilarial IgG4 in the blood and these can be detected using routine assays.
- Urine – If lymphatic filariasis is suspected, urine should be examined macroscopically for chyluria and then concentrated to examine for microfilariae.
- Skin – Onchocerca volvulus and Mansonella streptocerca infections are diagnosed when microfilariae are detected in multiple skin-snip specimens taken from different sites.
- Eye – Microfilariae of Onchocerca volvulus may be detected in the cornea or anterior chamber of the eye using slit-lamp examination.
Useful imaging studies in the evaluation of filariasis include the following:
- Chest X-ray – Diffuse pulmonary infiltrates are visible in patients with tropical pulmonary eosinophilia (TPE)
- Ultrasound – Can be used to demonstrate and monitor lymphatic obstruction of the inguinal and scrotal lymphatics; has been used to demonstrate the presence of viable worms. Careful ultrasound may identify the random movement of adult worms in dilated lymphatics, known as the “filarial dance sign” (FDS). This is particularly useful in a patient with scrotal symptoms and is considered the gold standard investigation for detecting viable adult worms 51.
- Lymphoscintigraphy – A nuclear medicine imaging test that maps the lymphatic system by tracking a radioactive tracer injected under the skin, helping to identify the sentinel lymph node in cancer patients or assess lymphatic drainage in conditions like lymphedema 52
Histologic findings include the following:
- Lymphatic filariasis – Affected lymph nodes demonstrate fibrosis and lymphatic obstruction with the creation of collateral channels
- Elephantiasis – The skin is characterized by hyperkeratosis, acanthosis, lymph and fatty tissue, loss of elastin fibers, and fibrosis
- Onchocerciasis – Onchocercomas have a central stromal and granulomatous, inflammatory region where the adult worms are found and a peripheral, fibrous section; microfilariae in the skin incite a low-grade inflammatory reaction with loss of elasticity and fibrotic scarring.
Key clinical features that may assist in making a diagnosis of lymphatic filariasis include:
- History of residence in an endemic country for several years;
- Self-limiting nature of attacks, in contrast to bacterial cellulitis, incarcerated hernias or testicular torsion;
- Bilateral symptoms and signs;
- Recurrent episodes;
- Palpable regional masses or lymphadenopathy.
The diagnosis of symptomatic lymphatic filariasis requires strong clinical suspicion. Interestingly, many infected people remain asymptomatic. Risk factors for symptomatic disease include duration and intensity of exposure to vectors, adult worm burden, frequency of secondary infections and the host immune response 53.
A blood film and serological evaluation are alternative diagnostic options. In most endemic areas, circulating microfilariae (filarial larvae) exhibit nocturnal periodicity (coinciding with peak feeding of local mosquitos) and are best seen on blood films taken between 10 pm and 4 am. If nocturnal samples are not feasible, then provocation with diethylcarbamazine may enhance microfilarial detection 1–2 hours later. Pacific Island infections (except Papua New Guinea) are subperiodic, with maximal microfilaraemia in the late afternoon, and show unresponsiveness to provocation. Importantly, patients with the chronic manifestations of lymphatic filariasis often have low levels of circulating microfilariae, resulting in lower blood-film sensitivity 54.
Lymphatic filariasis diagnosis
Microfilariae on blood smear examination: Draw blood at night, when levels of parasitemia are generally highest (most often at night between 10 PM – 2 AM). The three lymphatic filarial species can also be distinguished based on their morphologic characteristics on light microscopy.
Microscopy: Lymphatic filariasis is usually identified by the finding of microfilaria in peripheral blood smears (thick or thin) stained with Giemsa or hematoxylin-and-eosin and subsequent morphologic species identification. For increased sensitivity, concentration techniques can be used. These include centrifugation of the blood sample lysed in 2% formalin (Knott’s technique), or filtration through a polycarbonate membrane. Microfilariae of Wuchereria bancrofti and Brugia malayi or Brugia timori species exhibit a nocturnal periodicity and an accurate diagnosis is best achieved on blood collected at night. Wuchereria bancrofti that are sub-periodic may be encountered in some regions of the Pacific Islands, eastern Malaysia, and Vietnam. Sub-periodic Brugia malayi also occurs in parts of Malaysia. Adult worms can be seen in the lymphatics. Adults of both species may be identified in biopsy specimens of lymphatic tissue.
Circulating filarial antigen (CFA) detection: Antigen detection using an immunoassay for circulating filarial antigens are available for only Wuchereria bancrofti detection in lymphatic filariasis. Unlike microfilariae with nocturnal periodicity, filarial antigens can be detected in blood samples collected at any time of day. A rapid format immunochromatographic test has been shown to be a useful and sensitive tool for the detection of Wuchereria bancrofti antigen and is being used widely by lymphatic filariasis elimination programs. Currently, this test is not licensed for use in the United States and cannot be used for patient diagnosis.
Additional testing in lymphatic filariasis includes polymerase chain reaction (PCR) and antibody detection. Polymerase Chain Reaction (PCR) is not widely available and is mostly used in a research setting. Serologic enzyme immunoassay tests, including antifilarial IgG1 and IgG4, provide an alternative to microscopic detection of microfilariae for the diagnosis of lymphatic filariasis. Patients with active filarial infection typically have elevated levels of antifilarial IgG4 in the blood and these can be detected using routine assays. However, antibody detection for filarial antibodies cannot distinguish between past and present infection and are not typically specific for filarial infections. Specificity can be improved via IgG4 assays based on certain recombinant antigens, such as Wb123 in Wuchereria bancrofti 124.
The Brugia Rapid (Reszon Diagnostics International Sdn. Bhd., Selangor, Malaysia) is a rapid strip test operating on the principle of immunochromatographic technology 125. The Brugia Rapid test is based on the specific reaction of a recombinant BmR1 protein produced in Escherichia coli with antiparasitic antibodies found in the patient’s serum. The antibodies react with the BmR1 antigen, which then binds to monoclonal anti-human IgG4 antibodies linked to colloidal gold 126. The IgG4 enzyme-linked immunosorbent assay (ELISA), utilizing the BmR1 antigen, demonstrated a specificity rate of 95.6% and a sensitivity rate of 96% 127. For the Brugia Rapid test, the results indicated 97% sensitivity and 99% specificity 125. Furthermore, a second validation study was conducted. The sensitivity of the strip test was found to be 93%. In the field study, compared to microscopic examination of thick blood smears, the sensitivity of the test was 87% and the specificity was 100%. The rapid strip test was therefore a useful diagnostic tool for filariasis in Brugia malayi endemic areas 128. Other studies have also demonstrated the high sensitivity and specificity of the test in detecting infection with the parasite 129, 130, 131, 132. Based on the detection of specific IgG4 antibodies against recombinant BmR1 antigens, a Brugia Rapid test is commercially available from Reszon Diagnostics International Sdn. Bhd., Selangor, Malaysia. The WHO, in its Global Programme to Eliminate Lymphatic Filariasis, recommends the Brugia Rapid test for the detection of Brugia malayi invasion 133. However, it should be noted that Brugia Rapid tests, which detect IgG4 antibodies specific to filaria, may generate false-positive results in patients who have been previously infected and have undergone treatment. This is because individuals affected by lymphatic filariasis may retain B-cell memory, leading to the detection of antibodies for some time after the elimination of the parasite. Currently, there is a lack of a commercial test for the detection of Brugia malayi antigens, which highlights the need for further research to improve the diagnosis of lymphatic filariasis 134.
Cutaneous filariasis diagnosis
Definitive diagnosis of Onchocerca volvulus (onchocerciasis) and Mansonella streptocerca (streptocerciasis) infections occurs when microfilariae are detected in multiple skin snip specimens taken from different body sites. In addition, microfilariae of Onchocerca volvulus may be detected in the cornea or anterior chamber of the eye, using slit-lamp examination. Onchocerca volvulus may also be detected with antigen testing, although this is not regularly available 135. Additional testing with serology and PCR have similar application in these cases, as noted above. Of note, the Mazzoti test (detailed below) should not be routinely used in the diagnosis of onchocerciasis owing to its risk for severe adverse reactions.
Loa loa infection can be definitively diagnosed by observing microfilariae on blood smear examination or by detecting migrating adult worms in the subcutaneous tissue or conjunctiva. For travelers to endemic areas, serology can be useful to detect exposure to Loa loa. Sensitivity and specificity of such testing varies depending on the assay used.
Body cavity filariasis diagnosis
Mansonella ozzardi and Mansonella perstans infections can be definitively diagnosed by observing microfilariae on blood smear examination. Additional testing with serology and polymerase chain reaction (PCR) have similar application in these cases, as described above.
Filariasis Differential Diagnosis
Filariasis differential diagnosis includes 25, 92:
- Several zoonotic filariasis, including Onchocerca, Dirofilaria, Brugia, Dipetalonema, Loaina, Meningonema
- Lymphoma
- Allergic bronchopulmonary aspergillosis
- Systemic vasculitis
- Chronic eosinophilic pneumonia
- Idiopathic hypereosinophilic syndrome
- Acute poststreptococcal glomerulonephritis
- Testicular neoplasms
- Congenital abnormalities of lymphatics
- Pelvic cancer
- Damage to the lymph system secondary to surgery or radiation.
Differential diagnoses of lymphatic filariasis include the following 136:
- Bacterial or fungal lymphadenitis – Sporotrichosis resulting from Sporothrix schenckii infection
- Recurrent streptococcal lymphadenitis
- Congenital or hereditary lymphedema – Milroy syndrome
- Nonfilarial elephantiasis
- Congenital hydrocele
- Epididymal cysts
- Carcinoma of the testis and/or scrotum
- Lymphosarcoma
Differential diagnoses of occult filariasis include the following:
- Asthma
- Septic arthritis
- Bacterial breast abscess
- Idiopathic or poststreptococcal glomerulonephritis
Other differential diagnoses of filariasis include the following:
- Onchocerciasis – Vitiligo, trachoma, lepromatous leprosy
- Loiasis – Hereditary and/or localized idiopathic angioedema
Filariasis treatment
Diethylcarbamazine citrate (DEC) remains the mainstay of filariasis treatment worldwide, which kills both immature and adult parasitic worms 30. The United States Centers for Disease Control and Prevention (CDC) recommends a single-day or 12-day course of diethylcarbamazine (DEC) at 6 mg/kg/day 55, 30.
The most common side effects of diethylcarbamazine (DEC) include 55:
- Dizziness
- Nausea
- Fever
- Headache
- Pain in muscles or joints
Diethylcarbamazine (DEC) has been used globally for more than 50 years. A single combined dose of ivermectin, albendazole, and diethylcarbamazine (DEC) resulted in clearance of microfilaria in 96% of affected patients for up to 3 years and is currently recommended by the World Health Organization (WHO) as triple therapy in areas not endemic with loaisis (Loa loa) 56. However, because lymphatic filariasis is rare in the United States, diethylcarbamazine (DEC) is no longer approved by the U.S. Food and Drug Administration (FDA) 55. Doctors can get diethylcarbamazine (DEC) from CDC, after a confirmed positive lab test.
Diethylcarbamazine (DEC) may not help people who have lymphedema, hydrocele or elephantiasis, as most people with these symptoms no longer have live parasites in their bodies 55. Your doctor might refer you to a lymphedema therapist to help manage your lymphedema. This includes learning how to keep the affected area clean, exercise, elevation, treatment of wounds and infections, and wearing appropriate footwear. There is limited evidence for the role of doxycycline as some studies advocate the use of doxycycline (200mg/day for 4 to 6 weeks) in adult worm killing and preventing the progression of lymphedema 30. If you have hydrocele (a fluid-filled sac that develops around one or both testicles, causing painless swelling in the scrotum), your doctor might recommend surgery to remove the fluid-filled swelling.
If you also have onchocerciasis or loaisis (Loa loa), also caused by filarial parasitic worms, taking diethylcarbamazine (DEC) might cause life-threatening side effects. Filaricidal action of diethylcarbamazine (DEC) induces an immunological reaction similar to the Mazzotti reaction (a potentially dangerous immune reaction that can occur after treatment for parasitic worm infections, particularly onchocerciasis caused by the rapid death and breakdown of microfilariae or larval worms in the body) seen in onchocerciasis, characterized by headache, joint pain, dizziness, anorexia, malaise, and urticaria 57, 58. Doxycycline and ivermectin or albendazole is the recommended combination in individuals with onchocerciasis or loaisis (Loa loa). Doxycycline is preferred in areas co-endemic with Loa loa (loaisis) and has also shown the ability to slow the inflammation and fibrosis that leads to worsening lymphedema. Doxycycline also treats Wolbachia, a genus of symbiotic bacteria that inhabit nematodes 28, 53. Filarial nematodes depend on Wolbachia for normal development and fertility 59. Doxycycline has been shown to clear filaria of Wolbachia symbionts, leading to microfilarial and macrofilarial death, and thus provides an attractive treatment option 60, 61, 62. Suramin is widely used in onchocerciasis, yet its role remains uncertain in lymphatic filariasis.
Multiple clinical trials have demonstrated doxycycline’s efficacy in reducing adult worm viability (as measured by scrotal ultrasound), circulating antigenemia (a marker of adult worm burden) and microfilaremia 60, 61, 62. The degree of reduction of adult worm viability with doxycycline (75%–92%) appears to be far greater than that with any of the commonly used antifilarial agents. Furthermore, doxycycline has significant effects on disease progression, bringing about improvement in lymphatic function, hydrocoele size, lymphoedema, circulating levels of lymphangiogenic factors and rates of lymphangitis 60. The extent to which doxycycline’s effects are mediated through activity against secondary bacterial pathogens has not been evaluated.
The optimal dose and duration for doxycycline therapy is unclear, but studies using 200 mg daily for at least 6 weeks have shown the best results 60, 62. Whether doxycycline should be used in conjunction with ivermectin, albendazole or diethylcarbamazine remains unknown. These additional drugs increase adverse events; however, few trials have compared combination regimens to doxycycline alone 61. Overall, the evidence suggests that in non-endemic settings doxycycline is the treatment of choice for symptomatic lymphatic filariasis. All patients in this series demonstrated a good clinical response to doxycycline.
Table 2. Filariasis treatment options
| Filarial disease | Treatment options |
|---|---|
| Onchocerciasis |
|
| Lymphatic filariasis |
|
| Loiasis |
|
| Mansonelliasis |
|
| Dirofilariasis |
|
Lymphatic filariasis treatment
The usual treatment for lymphatic filariasis is a drug called diethylcarbamazine (DEC), which kills both immature and adult parasitic worms. Your doctor may recommend either a single-day treatment or taking the drug for 12 days.
The most common side effects of diethylcarbamazine (DEC) include 55:
- Dizziness
- Nausea
- Fever
- Headache
- Pain in muscles or joints
Diethylcarbamazine (DEC) has been used globally for more than 50 years. However, because lymphatic filariasis is rare in the United States, the drug is no longer approved by the U.S. Food and Drug Administration (FDA). Your doctor can get this drug from CDC, after a confirmed positive lab test.
Diethylcarbamazine (DEC) may not help people who have lymphedema or elephantiasis, as most people with these symptoms no longer have live parasites in their bodies. Your healthcare provider might refer you to a lymphedema therapist to help manage your condition. This includes learning how to keep the affected area clean, exercise, elevation, treatment of wounds and infections, and using appropriate footwear. If you have hydrocele, your doctor might recommend surgery to remove the fluid-filled swelling.
Wolbachia is an endosymbiont bacteria (microbes that live inside the cells of another organism, forming an intimate symbiotic relationship that can be beneficial, parasitic, or a combination of both) found in 50 per cent of insect species, including some mosquitoes, fruit flies, moths, dragonflies and butterflies, first identified by Hertig and Wolbach in 1924 in the mosquito Culex pipiens 137. Wolbachia is a Gram-negative alpha-proteobacteria, a member of the Rickettsiales order 138. Many filarial nematodes (roundworms) are recognized as host to Wolbachia 139, except a few species such as Loa loa, Acanthocheilonema viteae, Onchocerca flexuosa and Setaria equina 140, 141.
The main species for lymphatic filariasis and onchocerciasis such as Wuchereria bancrofti, Brugia malayi and Onchocerca volvulus were also found to contain an intracellular bacterium which showed similarities with Wolbachia according to DNA sequencing data 142. Moreover, filarial roundworms are found to be infected with Wolbachia at all stages of their life cycles 143. An important mutualistic symbiosis exists between Wolbachia and their nematode hosts. This interaction has contributed to their survival. Wolbachia is necessary for growth, fertility and viability of the nematode host, while the host supplies amino acids needed for Wolbachia’s development 144. Furthermore, Wolbachia is transmitted vertically via oocytes in the filarial worms 143. Therefore, sterilization of the worms will decrease the presence of the intracellular endosymbiont. Without Wolbachia, the viability of the filarial worms will be affected 145. All these features make Wolbachia an interesting target for filarial drug treatment 146.
The knowledge on the role of Wolbachia in the pathogenesis of human filarial infections is mostly derived from studies of the molecular pathogenesis of inflammation triggered by filarial nematodes 147. Since the first human clinical trial showing the effectiveness of doxycycline in eradicating Wolbachia and leading to the death of adult worms 148, doxycycline has been established as an effective anti-Wolbachia treatment with good macrofilaricidal activity 149, 150.
The first human trial of anti-Wolbachia drugs was done by Hoerauf et al 148 in Ghana. In this prospective trial to investigate the effectiveness of targeting Wolbachia in human onchocerciasis, doxycycline was administered at 100 mg daily dose for six weeks 148. One of the outcomes was the depletion of more than 80 per cent Wolbachia four months after the treatment 148. Furthermore, the embryogenesis of the treated worms was interrupted and viability affected compared to the non-treated worms. In the subsequent extension of the study 151, the patients who received doxycycline and ivermectin were compared with patients who had received ivermectin alone. When examined after 19 months, amicrofilaridermia was observed in the doxycycline and ivermectin group, suggesting that doxycycline significantly enhances the microfilaricidal effect of ivermectin. This study established that the worm sterilization was long term, up to 1.5 years after treatment and was probably irreversible 151.
Besides the synergistic microfilaricidal effect with ivermectin, macrofilaricidal effect as well as sterilization of the female Onchocerca worms after a course of doxycycline treatment was also discovered. Hoerauf et al 152, in their double-blind randomized placebo-controlled trial in Ghana, showed that a six-week course of doxycycline had a higher macrofilaricidal effect of up to 60 per cent, as compared to 50 per cent for the shorter four-week course. Furthermore, the residual live female worms analyzed from the onchocercomata nodules were sterile. A similar randomized controlled study in Cameroon 153 and another open study by Hoerauf et al 154 using doxycycline at 100 mg/day for five weeks confirmed that both macrofilaricidal and embryotoxic activities were attributable to the monotherapy with doxycycline without administration of ivermectin. A good safety profile was observed as no serious adverse events were reported from the doxycycline-treated group. Besides, the utilization of antibiotics in areas of co-endemicity with loiasis is shown to be safe and effective for onchocerciasis 153.
Doxycycline antibiotic can be used as an adjunct (add-on) in managing lymphatic filariasis 155. According to a randomized controlled trial conducted with 356 participants in Ghana found that, while the main approach to managing lymphatic filariasis was preventive chemotherapy, combining doxycycline with strict hygiene protocol could successfully prevent acute attacks 156. Another randomized controlled trial conducted in Ghana revealed that patients treated with doxycycline experienced a significant reduction in lymphedema severity after 12–24 months, with 43.9% showing major improvement 157. Similarly, a randomized controlled trial conducted in Thailand, where a single dose of doxycycline was given, reported a significant reduction in the severity of adverse reactions compared to the placebo 158. Furthermore, a double blind, randomized placebo-controlled trial in Tanzania reported that after the first 6 months of the treatment, the doxycycline group experienced significantly fewer acute adenolymphangitis attacks—which is a chronically disabling part of lymphatic filariasis—compared to the placebo group. Hence, doxycycline plays a key role in halting the progression of lymphatic filariasis 155.
One of the main benefits of using doxycycline is its widely available and cost-effective property, making it a viable choice for widespread use in endemic areas. Due to doxycycline’s high safety profile and mild side effects, especially in non-pregnant patients, doxycycline can be used more frequently. Moreover, there is no appreciable risk of resistance emerging, making doxycycline a dependable and long-lasting choice in the continuous battle against lymphatic filariasis 159. There is a growing need to integrate doxycycline therapy into the management of lymphatic filariasis. When combined with hygiene interventions, such as proper care of affected limbs to prevent infections, doxycycline can help maintain cleaner conditions, reducing the risk of secondary infections, and improving patient outcomes.
A Cochrane systematic review analyzed three randomized controlled trials comparing the treatment of doxycycline added to ivermectin versus ivermectin only on 466 onchocerciasis patients in West Africa 160. In the two previous studies 152, 153, microfilarial loads in skin snips were quantified. The results showed sustained effects of six-week doxycycline treatment of Wolbachia depletion, microfilaricidal and macrofilaricidal as well as sterilization effect for up to two years 152, 153. In the study that measured visual outcomes at six-month follow up, they found that although the onchocerciasis clinical symptoms improved, no significant visual improvement was found among the patients treated with doxycycline plus ivermectin when compared to those who received ivermectin alone 161. Better designed trials of doxycycline with standardized clinical outcomes such as the efficacy of the interventions in preventing visual acuity and visual field loss would provide more condusive evidence.
Doxycycline has also demonstrated its efficacy as anti-Wolbachia therapy to reduce the burden of lymphatic filariasis. In a randomized clinical study, doxycycline therapy for three weeks significantly reduced the microfilarial load and was more effective in inducing a microfilaremia for up to two years when compared to monotherapy with either albendazole or ivermectin 162. The severity of lymphedema also improved after treatment with doxycycline 163. These results were translated into the use of doxycycline to improve clinical symptoms. In another randomized controlled trial which compared doxycycline with amoxicillin on patients with and without active lymphatic filariasis infection, though significant improvement of the severity of lymphedema was noted for both drugs at one and two years of follow up, higher progression of disease was observed in 29 per cent of patients in the amoxicillin group and 56 per cent of patients in the placebo group, compared to a lower five per cent in the doxycycline arm 164. The treatment time of lymphatic filariasis with doxycycline is also shorter compared to that in onchocerciasis 165, possibly due to the presence of the filarial nematodes in the lymphatic vessels rather than the skin where drug penetration is more difficult. Taking into account the benefits shown even in patients without active infection and the fact that the efficacy of albendazole or ivermectin as microfilaricides is still undetermined for lymphatic filariasis 166, the addition of doxycycline as part of the standard treatment for lymphatic filariasis should be considered.
Regarding the treatment duration, intermittent short multiple courses over a longer period are found to be better than a continuous intensive once-off shorter duration course 167, 168, 169. For example, an in vivo study using Onchocerca ochengi in cattle discovered a significant post-treatment macrofilaricidal activity in the group receiving intermittent antibiotics (20 mg/kg monthly for 6 months) compared to a continuous course (10 mg/kg daily for 2 week) 167. This superiority of the prolonged intermittent regimen was explained by the findings from an in vitro study using the Wolbachia-infected Aedes albopictus mosquito, which showed that significant Wolbachia depletion occurred after antibiotics withdrawal 168. A later animal study also proved that a six-month regimen of oxytetracycline with once a month administration was more efficacious than a shorter but continuous course, either at three or six weeks duration 169.
If you also have onchocerciasis or loaisis (Loa loa), also caused by filarial parasitic worms, taking diethylcarbamazine (DEC) might cause life-threatening side effects. Filaricidal action of diethylcarbamazine (DEC) induces an immunological reaction similar to the Mazzotti reaction (a potentially dangerous immune reaction that can occur after treatment for parasitic worm infections, particularly onchocerciasis caused by the rapid death and breakdown of microfilariae or larval worms in the body) seen in onchocerciasis, characterized by headache, joint pain, dizziness, anorexia, malaise, and urticaria 57, 58. Doxycycline and ivermectin or albendazole is the recommended combination in individuals with onchocerciasis or loaisis (Loa loa). Suramin is widely used in onchocerciasis, yet its role remains uncertain in lymphatic filariasis.
Lymphedema treatment
Lymphedema can progress due to repeated attacks of adenolymphangitis (ADL), even in the absence of lymphatic filariasis. Adenolymphangitis (ADL) refers to acute, recurrent, painful, and inflammatory episodes of lymphatic filariasis characterized by fever, limb swelling, and lymph node or lymph vessel inflammation, which are often the first signs of lymphatic filariasis and lead to lymphedema. Though the precise cause remains unclear, adenolymphangitis (ADL) episodes are thought to be triggered by secondary bacterial or fungal infections accessing the lymphatic system, which is already compromised by the underlying parasitic worms. Basic hygiene interventions are shown to reduce adenolymphangitis (ADL) episodes, which contribute to the progression of lymphedema and the loss of the patient’s ability to perform daily tasks
Common treatments for early-stage or mild lymphedema include 92, 170, 48:
- Elevation of affected area to allow gravity to help drain extra fluid.
- Exercises and movements that promote fluid drainage and improve range of motion.
- Skin and nail care to prevent cuts or injuries to the skin around the affected area, which can make lymphedema worse or lead to cellulitis.
- Antibiotic and antifungal creams to prevent flares of lymphangitis
- Manual lymphatic drainage (MLD) is a type of gentle massage that helps move lymph fluid out of the swollen area. A trained therapist does this and might teach you how to do self manual lymphatic drainage (MLD) at home.
- Compression garments are special sleeves or stockings to prevent fluid build-up. A prescription from your doctor is needed. They are fitted to you by a professional and apply different amounts of pressure in different areas. Never wear a compression garment that hasn’t been fitted for you. This can trigger lymphedema or make it worse.
- Promote fluid circulation. Body areas that have damaged or missing lymph nodes can’t move and drain lymph fluid through the area as well. But there are things you can do to promote drainage of lymph fluid:
- Don’t wear tight clothing, jewelry, or other items that constrict or squeeze the affected area.
- Wearing comfortable shoes
- If you wear a compression garment, wear it as directed. These garments apply measured and specific amounts of pressure to different areas and are not the same as tight clothing.
- Don’t wear a compression garment that doesn’t fit or that you’ve grown out of. Get re-fitted for a garment every few months.
- Avoid having blood pressure measurements taken on the affected arm, when possible.
- Ask your doctor or therapist what exercises are good for your type and area of lymphedema.
- Raising the affected arm or leg (above the level of your heart if possible) can improve swelling.
- If you have lymphedema in your lower body, avoid crossing your legs.
- Ask how to do manual lymph drainage (MLD) on yourself.
- Note any changes in size, shape, or color of the affected area. Compare to the non-affected side if possible. Tell your doctor right away if you notice any changes.
- Drinking plenty of fluids each day is important for everyone at every age. Drinking enough water helps the body filter and get rid of excess fluid and waste products. Researchers recently studied how people cope with lymphedema. One part of the study looked at their eating and drinking habits. The researchers found:
- About 1 in 3 study participants reported that increasing their daily water intake was helpful for their symptoms.
- About 1 in 4 study participants rated decreased alcohol intake as very helpful in controlling symptoms.
- Water is usually the best choice for daily hydration. In addition to water, choosing unsweetened, low-fat beverages can support fluid intake. Water is also found in many foods, such as vegetables, fruits, broths and soups.
Treating moderate lymphedema
Complete decongestive therapy (CDT) is the combination of manual lymphatic drainage (MLD), compression therapy, skin care, exercises, and elevation. Complete decongestive therapy (CDT) is often used to manage mild to moderate lymphedema.
Treating severe lymphedema
For severe lymphedema, intermittent pneumatic compression (IPC) might be added to the treatment plan. Intermittent pneumatic compression (IPC) is a type of compression therapy where a sleeve or stocking is applied to the affected areas and inflated like a blood pressure cuff. It applies specific amounts of pressure to move fluid out of the area. Intermittent pneumatic compression (IPC) might also be used for less severe cases of lymphedema if a person can’t wear compression garments or can’t do manual self-lymphatic drainage.
Surgery might be an option if lymphedema is severe and hasn’t improved with other treatments.
- Liposuction removes extra fat that can develop in areas of lymphedema.
- Lympho-venous or lymphatic bypass takes lymph vessels and attaches them to small veins to improve drainage.
- Vascularized lymph node transfer (VLNT) takes healthy lymph nodes from another part of the body and places them in the area with lymphedema.
Surgical treatments
Surgical treatments exist for the debulking of skin and creating lymphovenous anastomosis to improve drainage. Topical coumarin and flavonoids were shown to be effective in reducing lymphedema. It is thought that increased macrophage activity leads to the reuptake of proteinaceous material 92.
A case report documented the success of ablative carbon dioxide laser treatment of skin lesions and lymphocutaneous fistulas, which resulted in significant improvement of skin lesions. It works by causing thermal damage to the dermis, resulting in the remodeling of superficial tissue and dermal tightening. This was done in a patient with non-filarial elephantiasis but could have an application in filarial disease 171.
Filariasis prognosis
Filariasis prognosis is good if filariasis is recognized early and treated in a timely fashion to prevent deformity 30, 2, 172. Filariasis responds to 5 annual doses of diethylcarbamazine (DEC) with or without ivermectin or albendazole. However, those having chronic lymphatic damage in the form of lymphedema or elephantiasis will respond poorly. Elephantiasis is the most severe form and is due to many years of acute on chronic superimposed infections. There is some ability to treat lymphedema, but it is difficult to manage once reaching advanced stages of the disease. These chronic forms have a poor prognosis. Patients with hydrocele might respond to surgery, but recurrence is common. Long-term disability may result from chronic lymphatic damage or blindness, depending on the infectious filarial organism. Lymphedema or elephantiasis is debilitating rendering the person incapable of performing daily activities.
- Anderson R.C. Nematode Parasites of Vertebrates: Their Development and Transmission. Cabi; Wallingford, UK: 2000.[↩][↩]
- Newman TE, Juergens AL. Filariasis. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556012[↩][↩][↩][↩]
- Knopp S, Steinmann P, Hatz C, Keiser J, Utzinger J. Nematode infections: filariases. Infect Dis Clin North Am. 2012 Jun;26(2):359-81. doi: 10.1016/j.idc.2012.02.005[↩][↩]
- Mackenzie CD, Kapa DR, Krishnasastry S, Douglass J, Hoerauf A, Ottesen EA. Managing Lymphedema Induced by Lymphatic Filariasis: Implementing and Improving Care at the Individual and Programmatic Levels. Am J Trop Med Hyg. 2024 Jul 30;111(4_Suppl):3-21. doi: 10.4269/ajtmh.23-0905[↩]
- Pietrzak D, Łuczak JW, Wiśniewski M. Beyond Tradition: Exploring Cutting-Edge Approaches for Accurate Diagnosis of Human Filariasis. Pathogens. 2024 May 24;13(6):447. doi: 10.3390/pathogens13060447[↩][↩][↩][↩]
- Paily K.P., Hoti S.L., Das P.K. A Review of the Complexity of Biology of Lymphatic Filarial Parasites. J. Parasites Dis. 2009;33:3–12. doi: 10.1007/s12639-009-0005-4[↩][↩]
- Maizels R.M., Kurniawan A., Selkirk M.E., Yazdanbakhsh M. Immune Responses to Filarial Parasites. Immunol. Lett. 1991;30:249–254. doi: 10.1016/0165-2478(91)90033-7[↩][↩]
- Korzeniewski K. Choroby Skóry w Gorącej Strefie Klimatycznej. Forum Med. Rodz. 2013;7:185–197.[↩][↩]
- Simón F., González-Miguel J., Diosdado A., Gómez P.J., Morchón R., Kartashev V. The Complexity of Zoonotic Filariasis Episystem and Its Consequences: A Multidisciplinary View. BioMed Res. Int. 2017;2017:6436130. doi: 10.1155/2017/6436130[↩][↩]
- Filariasis. https://emedicine.medscape.com/article/217776-overview[↩][↩]
- Lefoulon E., Giannelli A., Makepeace B.L., Mutafchiev Y., Townson S., Uni S., Verocai G.G., Otranto D., Martin C. Whence River Blindness? The Domestication of Mammals and Host-Parasite Co-Evolution in the Nematode Genus Onchocerca. Int. J. Parasitol. 2017;47:457–470. doi: 10.1016/j.ijpara.2016.12.009[↩][↩]
- Hotterbeekx A., Namale Ssonko V., Oyet W., Lakwo T., Idro R. Neurological Manifestations in Onchocerca Volvulus Infection: A Review. Brain Res. Bull. 2019;145:39–44. doi: 10.1016/j.brainresbull.2018.08.024[↩][↩]
- Orihel T.C., Beaver P.C. Zoonotic Brugia Infections in North and South America. Am. J. Trop. Med. Hyg. 1989;40:638–647. doi: 10.4269/ajtmh.1989.40.638[↩][↩][↩][↩]
- Eberhard M.L., DeMeester L.J., Martin B.W., Lammie P.J. Zoonotic Brugia Infection in Western Michigan. Am. J. Surg. Pathol. 1993;17:1058–1061. doi: 10.1097/00000478-199310000-00012[↩][↩][↩][↩]
- Antinori S., Schifanella L., Million M., Galimberti L., Ferraris L., Mandia L., Trabucchi G., Cacioppo V., Monaco G., Tosoni A., et al. Imported Loa Loa Filariasis: Three Cases and a Review of Cases Reported in Non-Endemic Countries in the Past 25 Years. Int. J. Infect. Dis. 2012;16:e649–e662. doi: 10.1016/j.ijid.2012.05.1023[↩][↩]
- Dieki R., Nsi-Emvo E., Akue J.P. The Human Filaria Loa Loa: Update on Diagnostics and Immune Response. Res. Rep. Trop. Med. 2022;13:41–54. doi: 10.2147/RRTM.S355104[↩][↩]
- Huynh T. Dipetalonema Reconditum in the Human Eye. Br. J. Ophthalmol. 2001;85:1384. doi: 10.1136/bjo.85.11.1384i[↩][↩]
- John M., Mathew S., Sebastian V., Biswas J., Raman M. Multiple Live Subconjunctival Dipetalonema: Report of a Case. Indian J. Ophthalmol. 2012;60:228. doi: 10.4103/0301-4738.95881[↩][↩]
- Kabego L., Kasengi J.B., Mirindi P., Ruhanya V., Lupande D., Bulabula A., Ngoma P. Pulmonary Localization of Mansonella Perstans in a 16 Months-Old Male Patient in a Tertiary Care Hospital in Bukavu, Democratic Republic of Congo. Germs. 2016;6:151–154. doi: 10.11599/germs.2016.1101[↩][↩]
- Ferreira M.U., Crainey J.L., Luz S.L.B. Mansonella Ozzardi. Trends Parasitol. 2021;37:90–91. doi: 10.1016/j.pt.2020.03.005[↩][↩][↩]
- Perles L., Dantas-Torres F., Krücken J., Morchón R., Walochnik J., Otranto D. Zoonotic Dirofilariases: One, No One, or More than One Parasite. Trends Parasitol. 2024;40:257–270. doi: 10.1016/j.pt.2023.12.007[↩][↩]
- Simón F., Siles-Lucas M., Morchón R., González-Miguel J., Mellado I., Carretón E., Montoya-Alonso J.A. Human and Animal Dirofilariasis: The Emergence of a Zoonotic Mosaic. Clin. Microbiol. Rev. 2012;25:507–544. doi: 10.1128/CMR.00012-12[↩][↩]
- Hübner M.P., Layland L.E., Hoerauf A. Helminth Infections and Their Impact on Global Public Health. Springer; Vienna, Austria: 2014. Lymphatic and Tissue Filariasis; pp. 367–409.[↩][↩]
- Mackenzie C.D. Human and Animal Filariases. Wiley; Hoboken, NY, USA: 2022. Human Filarial Infections: Reflections on the Current Understanding of Their Importance, Pathobiology, and Management; pp. 33–73.[↩][↩]
- Orihel TC, Eberhard ML. Zoonotic filariasis. Clin Microbiol Rev. 1998 Apr;11(2):366-81. doi: 10.1128/CMR.11.2.366[↩][↩][↩][↩][↩][↩][↩][↩]
- Nanduri J., Kazura J.W. Clinical and Laboratory Aspects of Filariasis. Clin. Microbiol. Rev. 1989;2:39–50. doi: 10.1128/CMR.2.1.39[↩][↩]
- Shaukat A., Aleem M.T., Kanwal A., Kalim A., Kalim F., Memoon A., Siddique M.H., Samad M.A., Shaukat R., Shaukat I. Recent Advances in Diagnosis of Filariasis. Int. J. Agric. Biosci. 2023;2:45–57. doi: 10.47278/book.zoon/2023.xx[↩][↩]
- Rebollo MP, Bockarie MJ. Can Lymphatic Filariasis Be Eliminated by 2020? Trends Parasitol. 2017 Feb;33(2):83-92. doi: 10.1016/j.pt.2016.09.009[↩][↩][↩][↩]
- Kubkomawa Hayatu Ibrahim, Kenneth-Chukwu Oluchi Margret, Iyiola Vivian Ogechi, Anyanwu Vivian Chinenye. A Critical and Systematic Review of Lymphatic filariasis Elephantiasis): A Neglected Tropical Disease (NTD) That Affects Negatively Agricultural Activities Across the World. International Journal of Biomedical Materials Research. Vol. 9, No. 2, 2021, pp. 13-17. doi: 10.11648/j.ijbmr.20210902.11[↩]
- Zulfiqar H, Malik A. Bancroftian Filariasis. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547682[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Lymphatic Filariasis. https://www.cdc.gov/dpdx/lymphaticfilariasis/index.html[↩][↩][↩][↩]
- Summary of global update on preventive chemotherapy implementation in 2016: crossing the billion. Wkly Epidemiol Rec. 2017 Oct 6;92(40):589-93. English, French. https://iris.who.int/bitstream/handle/10665/259184/WER9240.pdf[↩]
- Small ST, Ramesh A, Bun K, Reimer L, Thomsen E, Baea M, Bockarie MJ, Siba P, Kazura JW, Tisch DJ, Zimmerman PA. Population genetics of the filarial worm wuchereria bancrofti in a post-treatment region of Papua New Guinea: insights into diversity and life history. PLoS Negl Trop Dis. 2013 Jul 11;7(7):e2308. doi: 10.1371/journal.pntd.0002308[↩]
- Guideline: Alternative Mass Drug Administration Regimens to Eliminate Lymphatic Filariasis. Geneva: World Health Organization; 2017. 1, Background. Available from: https://www.ncbi.nlm.nih.gov/books/NBK487832[↩]
- Okon OE, Iboh CI, Opara KN. Bancroftian filariasis among the Mbembe people of Cross River state, Nigeria. J Vector Borne Dis. 2010 Jun;47(2):91-6. http://www.mrcindia.org/journal/issues/472091.pdf[↩]
- Addiss DG, Louis-Charles J, Roberts J, Leconte F, Wendt JM, Milord MD, Lammie PJ, Dreyer G. Feasibility and effectiveness of basic lymphedema management in Leogane, Haiti, an area endemic for bancroftian filariasis. PLoS Negl Trop Dis. 2010 Apr 20;4(4):e668. doi: 10.1371/journal.pntd.0000668[↩]
- Mathieu E, Dorkenoo A, Otogbe FK, Budge PJ, Sodahlon YK. A laboratory-based surveillance system for Wuchereria bancrofti in Togo: a practical model for resource-poor settings. Am J Trop Med Hyg. 2011 Jun;84(6):988-93. doi: 10.4269/ajtmh.2011.10-0610[↩]
- Uttah EC. Prevalence of endemic Bancroftian filariasis in the high altitude region of south-eastern Nigeria. J Vector Borne Dis. 2011 Jun;48(2):78-84. http://www.mrcindia.org/journal/issues/482078.pdf[↩]
- Molyneux DH. Tropical lymphedemas–control and prevention. N Engl J Med. 2012 Mar 29;366(13):1169-71. doi: 10.1056/NEJMp1202011[↩]
- Meyrowitsch DW, Simonsen PE, Garred P, Dalgaard M, Magesa SM, Alifrangis M. Association between mannose-binding lectin polymorphisms and Wuchereria bancrofti infection in two communities in North-Eastern Tanzania. Am J Trop Med Hyg. 2010 Jan;82(1):115-20. doi: 10.4269/ajtmh.2010.09-0342[↩]
- Filariasis Epidemiology. https://emedicine.medscape.com/article/217776-overview#a6[↩]
- Michael E, Bundy DA, Grenfell BT. Re-assessing the global prevalence and distribution of lymphatic filariasis. Parasitology. 1996 Apr;112 ( Pt 4):409-28. doi: 10.1017/s0031182000066646[↩][↩]
- Maldjian C, Khanna V, Tandon B, Then M, Yassin M, Adam R, Klein MJ. Lymphatic filariasis disseminating to the upper extremity. Case Rep Radiol. 2014;2014:985680. doi: 10.1155/2014/985680[↩]
- Pryce J, Mableson HE, Choudhary R, Pandey BD, Aley D, Betts H, Mackenzie CD, Kelly-Hope LA, Cross H. Assessing the feasibility of integration of self-care for filarial lymphoedema into existing community leprosy self-help groups in Nepal. BMC Public Health. 2018 Jan 30;18(1):201. doi: 10.1186/s12889-018-5099-0[↩]
- Jeremiah CJ, Aboltins CA, Stanley PA. Lymphatic filariasis in Australia: an update on presentation, diagnosis and treatment. Med J Aust. 2011 Jun 20;194(12):655-7. doi: 10.5694/j.1326-5377.2011.tb03154.x[↩]
- Kazura J. Guerrant R, Walker DH, Weller PF, eds. Tropical Infectious Diseases: Principles, Pathogens and Practice. Philadelphia, PA: Churchill Livingstone; 1999. Vol 2: 852.[↩][↩]
- Pani SP, Yuvaraj J, Vanamail P, Dhanda V, Michael E, Grenfell BT, Bundy DA. Episodic adenolymphangitis and lymphoedema in patients with bancroftian filariasis. Trans R Soc Trop Med Hyg. 1995 Jan-Feb;89(1):72-4. doi: 10.1016/0035-9203(95)90666-5[↩][↩]
- Chandy A, Thakur AS, Singh MP, Manigauha A. A review of neglected tropical diseases: filariasis. Asian Pac J Trop Med. 2011 Jul;4(7):581-6. https://doi.org/10.1016/S1995-7645(11)60150-8[↩][↩][↩][↩][↩][↩][↩]
- Filariasis Workup. https://emedicine.medscape.com/article/217776-workup[↩][↩]
- Rosenblatt JE. Laboratory diagnosis of infections due to blood and tissue parasites. Clin Infect Dis. 2009 Oct 1;49(7):1103-8. doi: 10.1086/605574[↩][↩]
- Amaral F, Dreyer G, Figueredo-Silva J, Noroes J, Cavalcanti A, Samico SC, Santos A, Coutinho A. Live adult worms detected by ultrasonography in human Bancroftian filariasis. Am J Trop Med Hyg. 1994 Jun;50(6):753-7. doi: 10.4269/ajtmh.1994.50.753[↩][↩]
- Subramanyam P, Palaniswamy SS. Lymphoscintigraphy in unilateral lower limb and scrotal lymphedema caused by filariasis. Am J Trop Med Hyg. 2012 Dec;87(6):963-964. doi: 10.4269/ajtmh.2012.12-0422[↩][↩]
- Taylor MJ, Hoerauf A, Bockarie M. Lymphatic filariasis and onchocerciasis. Lancet. 2010 Oct 2;376(9747):1175-85. doi: 10.1016/S0140-6736(10)60586-7[↩][↩][↩][↩]
- Chanteau S, Moulia-Pelat JP, Glaziou P, Nguyen NL, Luquiaud P, Plichart C, Martin PM, Cartel JL. Og4C3 circulating antigen: a marker of infection and adult worm burden in Wuchereria bancrofti filariasis. J Infect Dis. 1994 Jul;170(1):247-50. doi: 10.1093/infdis/170.1.247[↩][↩]
- Treatment of Lymphatic Filariasis. https://www.cdc.gov/filarial-worms/treatment/index.html[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Bjerum CM, Ouattara AF, Aboulaye M, Kouadio O, Marius VK, Andersen BJ, Weil GJ, Koudou BG, King CL. Efficacy and Safety of a Single Dose of Ivermectin, Diethylcarbamazine, and Albendazole for Treatment of Lymphatic Filariasis in Côte d’Ivoire: An Open-label Randomized Controlled Trial. Clin Infect Dis. 2020 Oct 23;71(7):e68-e75. doi: 10.1093/cid/ciz1050[↩][↩]
- Ottesen EA. Description, mechanisms and control of reactions to treatment in the human filariases. Ciba Found Symp. 1987;127:265-83. doi: 10.1002/9780470513446.ch18[↩][↩][↩]
- Olson, Bradley G. MD; Domachowske, Joseph B. MD. MAZZOTTI REACTION AFTER PRESUMPTIVE TREATMENT FOR SCHISTOSOMIASIS AND STRONGYLOIDIASIS IN A LIBERIAN REFUGEE. The Pediatric Infectious Disease Journal 25(5):p 466-468, May 2006. DOI: 10.1097/01.inf.0000217415.68892.0c[↩][↩][↩]
- Taylor MJ, Bandi C, Hoerauf A. Wolbachia bacterial endosymbionts of filarial nematodes. Adv Parasitol. 2005;60:245-84. doi: 10.1016/S0065-308X(05)60004-8[↩][↩]
- Debrah AY, Mand S, Specht S, Marfo-Debrekyei Y, Batsa L, Pfarr K, Larbi J, Lawson B, Taylor M, Adjei O, Hoerauf A. Doxycycline reduces plasma VEGF-C/sVEGFR-3 and improves pathology in lymphatic filariasis. PLoS Pathog. 2006 Sep;2(9):e92. doi: 10.1371/journal.ppat.0020092[↩][↩][↩][↩][↩]
- Supali T, Djuardi Y, Pfarr KM, Wibowo H, Taylor MJ, Hoerauf A, Houwing-Duistermaat JJ, Yazdanbakhsh M, Sartono E. Doxycycline treatment of Brugia malayi-infected persons reduces microfilaremia and adverse reactions after diethylcarbamazine and albendazole treatment. Clin Infect Dis. 2008 May 1;46(9):1385-93. doi: 10.1086/586753[↩][↩][↩][↩]
- Taylor MJ, Makunde WH, McGarry HF, Turner JD, Mand S, Hoerauf A. Macrofilaricidal activity after doxycycline treatment of Wuchereria bancrofti: a double-blind, randomised placebo-controlled trial. Lancet. 2005 Jun 18-24;365(9477):2116-21. doi: 10.1016/S0140-6736(05)66591-9[↩][↩][↩][↩]
- Singh, Gurjeet & Raksha, & Urhekar, A. (2013). Advanced Techniques for Detection of Filariasis -A Review. International Journal of Research Studies in Biosciences. 1. 17-22. [↩]
- Newman TE, Juergens AL. Filariasis. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. [Figure, Brugia malayi. Lee Moore, MD,…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK556012/figure/article-21756.image.f1[↩]
- Fischer P, Erickson SM, Fischer K, Fuchs JF, Rao RU, Christensen BM, Weil GJ. Persistence of Brugia malayi DNA in vector and non-vector mosquitoes: implications for xenomonitoring and transmission monitoring of lymphatic filariasis. Am J Trop Med Hyg. 2007 Mar;76(3):502-7. https://pmc.ncbi.nlm.nih.gov/articles/PMC2196403[↩]
- Lymphatic filariasis. https://www.who.int/news-room/fact-sheets/detail/lymphatic-filariasis[↩][↩]
- About Culex Mosquitoes. https://www.cdc.gov/mosquitoes/about/culex-mosquitoes.html[↩]
- Horsley JS, Styblo T: Lymphedema in the postmastectomy patient. In: Bland KI, Copeland EM, eds.: The Breast: Comprehensive Management of Benign and Malignant Diseases. Saunders, 1991, pp 701-6.[↩]
- Lymphedema (PDQ®)–Health Professional Version. https://www.cancer.gov/about-cancer/treatment/side-effects/lymphedema/lymphedema-hp-pdq[↩][↩][↩]
- Institute of Medicine (US) Forum on Microbial Threats. The Causes and Impacts of Neglected Tropical and Zoonotic Diseases: Opportunities for Integrated Intervention Strategies. Washington (DC): National Academies Press (US); 2011. FIGURE WO-6-14, Lymphatic filariasis. Available from: https://www.ncbi.nlm.nih.gov/books/NBK62526/figure/workshopoverview.box1.f14[↩]
- Lamula SQ, Aladejana EB, Aladejana EA, Buwa-Komoreng LV. Prevalence of elephantiasis, an overlooked disease in Southern Africa: a comprehensive review. J Venom Anim Toxins Incl Trop Dis. 2024 Oct 14;30:e20240007. doi: 10.1590/1678-9199-JVATITD-2024-0007[↩]
- Matapo BB, Mpabalwani EM, Kaonga P, et al. Lymphatic Filariasis Elimination Status: Wuchereria bancrofti Infections in Human Populations after Five Effective Rounds of Mass Drug Administration in Zambia. Trop Med Infect Dis. 2023 Jun 22;8(7):333. doi: 10.3390/tropicalmed8070333[↩]
- Lymphatic filariasis. https://www.who.int/westernpacific/health-topics/lymphatic-filariasis#tab=tab_1[↩]
- Gahlinger PM. Podoconiosis: A Possible Cause of Lymphedema in Micronesia. Hawaii J Health Soc Welf. 2021 Sep;80(9):218-221. https://pmc.ncbi.nlm.nih.gov/articles/PMC8433576[↩][↩][↩][↩][↩]
- Podoconiosis (non-filarial lymphoedema). https://www.who.int/news-room/fact-sheets/detail/podoconiosis-(non-filarial-lymphoedema[↩][↩]
- Deribe K, Cano J, Newport MJ, Pullan RL, Noor AM, Enquselassie F, Murray CJL, Hay SI, Brooker SJ, Davey G. The global atlas of podoconiosis. Lancet Glob Health. 2017 May;5(5):e477-e479. doi: 10.1016/S2214-109X(17)30140-7[↩]
- Molla YB, Wardrop NA, Le Blond JS, Baxter P, Newport MJ, Atkinson PM, Davey G. Modelling environmental factors correlated with podoconiosis: a geospatial study of non-filarial elephantiasis. Int J Health Geogr. 2014 Jun 20;13:24. doi: 10.1186/1476-072X-13-24[↩]
- Price EW. The association of endemic elephantiasis of the lower legs in East Africa with soil derived from volcanic rocks. Trans R Soc Trop Med Hyg. 1976;70(4):288-95. doi: 10.1016/0035-9203(76)90078-x[↩]
- Filariasis. https://dermnetnz.org/topics/filariasis[↩][↩]
- Ajendra J., Hoerauf A.P., Hübner M. Parasitic Helminths and Zoonoses—From Basic to Applied Research. IntechOpen; London, UK: 2022. Biology of the Human Filariases.[↩]
- Lymphatic filariasis. https://www.who.int/news-room/questions-and-answers/item/lymphatic-filariasis[↩]
- Murugan K, Nataraj D, Madhiyazhagan P, et al. Carbon and silver nanoparticles in the fight against the filariasis vector Culex quinquefasciatus: genotoxicity and impact on behavioral traits of non-target aquatic organisms. Parasitol Res. 2016 Mar;115(3):1071-83. doi: 10.1007/s00436-015-4837-9[↩]
- Filariasis. https://emedicine.medscape.com/article/217776-overview#a5[↩][↩]
- Nutman TB. Insights into the pathogenesis of disease in human lymphatic filariasis. Lymphat Res Biol. 2013 Sep;11(3):144-8. doi: 10.1089/lrb.2013.0021[↩]
- Babu S, Nutman TB. Immunopathogenesis of lymphatic filarial disease. Semin Immunopathol. 2012 Nov;34(6):847-61. doi: 10.1007/s00281-012-0346-4[↩]
- Mishra R, Panda SK, Sahoo PK, Mishra S, Satapathy AK. Self-reactive IgG4 antibodies are associated with blocking of pathology in human lymphatic filariasis. Cell Immunol. 2019 Jul;341:103927. doi: 10.1016/j.cellimm.2019.103927[↩]
- Ridner SH. Quality of life and a symptom cluster associated with breast cancer treatment-related lymphedema. Support Care Cancer. 2005 Nov;13(11):904-11. doi: 10.1007/s00520-005-0810-y[↩]
- Dunberger G, Lindquist H, Waldenström AC, Nyberg T, Steineck G, Åvall-Lundqvist E. Lower limb lymphedema in gynecological cancer survivors–effect on daily life functioning. Support Care Cancer. 2013 Nov;21(11):3063-70. doi: 10.1007/s00520-013-1879-3[↩]
- Zhang X, McLaughlin EM, Krok-Schoen JL, Naughton M, Bernardo BM, Cheville A, Allison M, Stefanick M, Bea JW, Paskett ED. Association of Lower Extremity Lymphedema With Physical Functioning and Activities of Daily Living Among Older Survivors of Colorectal, Endometrial, and Ovarian Cancer. JAMA Netw Open. 2022 Mar 1;5(3):e221671. doi: 10.1001/jamanetworkopen.2022.1671[↩]
- Pyszel A, Malyszczak K, Pyszel K, Andrzejak R, Szuba A. Disability, psychological distress and quality of life in breast cancer survivors with arm lymphedema. Lymphology. 2006 Dec;39(4):185-92.[↩]
- Gjorup CA, Groenvold M, Hendel HW, Dahlstroem K, Drzewiecki KT, Klausen TW, Hölmich LR. Health-related quality of life in melanoma patients: Impact of melanoma-related limb lymphoedema. Eur J Cancer. 2017 Nov;85:122-132. doi: 10.1016/j.ejca.2017.07.052[↩]
- Shenoy RK. Clinical and pathological aspects of filarial lymphedema and its management. Korean J Parasitol. 2008 Sep;46(3):119-25. doi: 10.3347/kjp.2008.46.3.119[↩][↩][↩][↩]
- Erickson SM, Thomsen EK, Keven JB, Vincent N, Koimbu G, Siba PM, Christensen BM, Reimer LJ. Mosquito-parasite interactions can shape filariasis transmission dynamics and impact elimination programs. PLoS Negl Trop Dis. 2013 Sep 12;7(9):e2433. doi: 10.1371/journal.pntd.0002433[↩]
- Paily KP, Hoti SL, Das PK. A review of the complexity of biology of lymphatic filarial parasites. J Parasit Dis. 2009 Dec;33(1-2):3-12. doi: 10.1007/s12639-009-0005-4[↩]
- Chakraborty S, Gurusamy M, Zawieja DC, Muthuchamy M. Lymphatic filariasis: perspectives on lymphatic remodeling and contractile dysfunction in filarial disease pathogenesis. Microcirculation. 2013 Jul;20(5):349-64. doi: 10.1111/micc.12031[↩]
- https://www.cdc.gov/dpdx/lymphaticfilariasis/modules/W_bancrofti_LifeCycle_lg.jpg[↩]
- https://www.cdc.gov/dpdx/lymphaticfilariasis/modules/B_malayi_LifeCycle_lg.jpg[↩]
- Lymphatic filariasis. https://www.cdc.gov/filarial-worms/testing/index.html[↩][↩][↩]
- Ramaiah K.D., Ottesen E.A. Progress and impact of 13 years of the global programme to eliminate lymphatic filariasis on reducing the burden of filarial disease. PLoS Negl. Trop. Dis. 2014;8:e3319. doi: 10.1371/journal.pntd.0003319[↩]
- Dreyer G., Norões J., Figueredo-Silva J., Piessens W.F. Pathogenesis of Lymphatic Disease in Bancroftian Filariasis: A Clinical Perspective. Parasitol. Today. 2000;16:544–548. doi: 10.1016/S0169-4758(00)01778-6[↩][↩]
- Hoerauf A., Satoguina J., Saeftel M., Specht S. Immunomodulation by Filarial Nematodes. Parasite Immunol. 2005;27:417–429. doi: 10.1111/j.1365-3024.2005.00792.x[↩]
- Babu S., Blauvelt C.P., Kumaraswami V., Nutman T.B. Cutting Edge: Diminished T Cell TLR Expression and Function Modulates the Immune Response in Human Filarial Infection. J. Immunol. 2006;176:3885–3889. doi: 10.4049/jimmunol.176.7.3885[↩]
- Babu S., Blauvelt C.P., Kumaraswami V., Nutman T.B. Regulatory Networks Induced by Live Parasites Impair Both Th1 and Th2 Pathways in Patent Lymphatic Filariasis: Implications for Parasite Persistence. J. Immunol. 2006;176:3248–3256. doi: 10.4049/jimmunol.176.5.3248[↩]
- Babu S., Kumaraswami V., Nutman T.B. Alternatively Activated and Immunoregulatory Monocytes in Human Filarial Infections. J. Infect. Dis. 2009;199:1827–1837. doi: 10.1086/599090[↩]
- Pfarr K.M., Debrah A.Y., Specht S., Hoerauf A. Filariasis and Lymphoedema. Parasite Immunol. 2009;31:664–672. doi: 10.1111/j.1365-3024.2009.01133.x[↩]
- Cuenco K.T., Halloran M.E., Lammie P.J. Assessment of Families for Excess Risk of Lymphedema of the Leg in a Lymphatic Filariasis-Endemic Area. Am. J. Trop. Med. Hyg. 2004;70:185–190. doi: 10.4269/ajtmh.2004.70.185[↩]
- Cuenco K.T., Halloran M.E., Louis-Charles J., Lammie P.J. A Family Study of Lymphedema of the Leg in a Lymphatic Filariasis-Endemic Area. Am. J. Trop. Med. Hyg. 2004;70:180–184. doi: 10.4269/ajtmh.2004.70.180[↩]
- Cuenco K.T., Ottesen E.A., Williams S.A., Nutman T.B., Steel C. Heritable Factors Play a Major Role in Determining Host Responses to Wuchereria Bancrofti Infection in an Isolated South Pacific Island Population. J. Infect. Dis. 2009;200:1271–1278. doi: 10.1086/605844[↩]
- Jha SK, Killeen RB, Mahajan K. Tropical Pulmonary Eosinophilia. [Updated 2025 Jan 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557524[↩]
- Mendoza N., Li A., Gill A., Tyring S. Filariasis: Diagnosis and Treatment. Dermatol. Ther. 2009;22:475–490. doi: 10.1111/j.1529-8019.2009.01271.x[↩]
- Kapoor U., Sharma V., Chittoria R.S. Onchocercoma in a United Nations Peacekeeper. Med. J. Armed Forces India. 2015;71:S104–S106. doi: 10.1016/j.mjafi.2013.05.005[↩]
- Nicholls R.S., Duque S., Olaya L.A., López M.C., Sánchez S.B., Morales A.L., Palma G.I. Elimination of Onchocerciasis from Colombia: First Proof of Concept of River Blindness Elimination in the World. Parasites Vectors. 2018;11:237. doi: 10.1186/s13071-018-2821-9[↩]
- Ramharter M., Butler J., Mombo-Ngoma G., Nordmann T., Davi S.D., Zoleko Manego R. The African Eye Worm: Current Understanding of the Epidemiology, Clinical Disease, and Treatment of Loiasis. Lancet Infect. Dis. 2024;24:e165–e178. doi: 10.1016/S1473-3099(23)00438-3[↩]
- Ta-Tang T.-H., Crainey J., Post R.J., Luz S.L.B., Rubio J. Mansonellosis: Current Perspectives. Res. Rep. Trop. Med. 2018;9:9–24. doi: 10.2147/RRTM.S125750[↩]
- Tyring S., Lupi O., Hengge U., editors. Tropical Dermatology. Elsevier; Amsterdam, The Netherlands: 2006.[↩]
- Tamarozzi F, Halliday A, Gentil K, Hoerauf A, Pearlman E, Taylor MJ. Onchocerciasis: the role of Wolbachia bacterial endosymbionts in parasite biology, disease pathogenesis, and treatment. Clin Microbiol Rev. 2011 Jul;24(3):459-68. doi: 10.1128/CMR.00057-10[↩]
- Filariasis Clinical Presentation. https://emedicine.medscape.com/article/217776-clinical#b3[↩]
- Zouré HG, Wanji S, Noma M, Amazigo UV, Diggle PJ, Tekle AH, Remme JH. The geographic distribution of Loa loa in Africa: results of large-scale implementation of the Rapid Assessment Procedure for Loiasis (RAPLOA). PLoS Negl Trop Dis. 2011 Jun;5(6):e1210. doi: 10.1371/journal.pntd.0001210[↩]
- Veletzky L., Hergeth J., Stelzl D.R., Mischlinger J., Manego R.Z., Mombo-Ngoma G., McCall M.B.B., Adegnika A.A., Agnandji S.T., Metzger W.G., et al. Burden of Disease in Gabon Caused by Loiasis: A Cross-Sectional Survey. Lancet Infect. Dis. 2020;20:1339–1346. doi: 10.1016/S1473-3099(20)30256-5[↩]
- Gobbi F, Boussinesq M, Mascarello M, Angheben A, Gobbo M, Rossanese A, Corachán M, Bisoffi Z. Case report: Loiasis with peripheral nerve involvement and spleen lesions. Am J Trop Med Hyg. 2011 May;84(5):733-7. doi: 10.4269/ajtmh.2011.10-0458[↩]
- Carme B, Boulesteix J, Boutes H, Puruehnce MF. Five cases of encephalitis during treatment of loiasis with diethylcarbamazine. Am J Trop Med Hyg. 1991 Jun;44(6):684-90. doi: 10.4269/ajtmh.1991.44.684[↩]
- Fischer P., Bamuhiiga J., Büttner D.W. Occurrence and Diagnosis of Mansonella Streptocerca in Uganda. Acta Trop. 1997;63:43–55. doi: 10.1016/S0001-706X(96)00607-9[↩]
- Clinical Overview of Lymphatic Filariasis. https://www.cdc.gov/filarial-worms/hcp/clinical-overview[↩]
- Kubofcik J, Fink DL, Nutman TB. Identification of Wb123 as an early and specific marker of Wuchereria bancrofti infection. PLoS Negl Trop Dis. 2012;6(12):e1930. doi: 10.1371/journal.pntd.0001930[↩]
- Rahmah N., Taniawati S., Shenoy R.K., Lim B.H., Kumaraswami V., Anuar A.K., Hakim S.L., Hayati M.I.N., Chan B.T., Suharni M., et al. Specificity and Sensitivity of a Rapid Dipstick Test (Brugia Rapid) in the Detection of Brugia Malayi Infection. Trans. R Soc. Trop. Med. Hyg. 2001;95:601–604. doi: 10.1016/S0035-9203(01)90091-4[↩][↩]
- Rahmah N., Shenoy R.K., Nutman T.B., Weiss N., Gilmour K., Maizels R.M., Yazdanbakhsh M., Sartono E. Multicentre Laboratory Evaluation of Brugia Rapid Dipstick Test for Detection of Brugian Filariasis. Trop. Med. Int. Health. 2003;8:895–900. doi: 10.1046/j.1365-3156.2003.01102.x[↩]
- Rahmah N., Lim B.H., Anuar A.K., Shenoy R.K., Kumaraswami V., Hakim S.L., Chotechuang P., Kanjanopas K., Ramachandran C.P. A Recombinant Antigen-Based IgG4 ELISA for the Specific and Sensitive Detection of Brugia Malayi Infection. Trans. R Soc. Trop. Med. Hyg. 2001;95:280–284. doi: 10.1016/S0035-9203(01)90234-2[↩]
- Jamail M., Andrew K., Junaidi D., Krishnan A.K., Faizal M., Rahmah N. Field Validation of Sensitivity and Specificity of Rapid Test for Detection of Brugia Malayi Infection. Trop. Med. Int. Health. 2005;10:99–104. doi: 10.1111/j.1365-3156.2004.01334.x[↩]
- Lammie P.J., Weil G., Noordin R., Kaliraj P., Steel C., Goodman D., Lakshmikanthan V.B., Ottesen E. Recombinant Antigen-Based Antibody Assays for the Diagnosis and Surveillance of Lymphatic Filariasis—A Multicenter Trial. Filaria J. 2004;3:9. doi: 10.1186/1475-2883-3-9[↩]
- Fischer P., Bonow I., Supali T., Rückert P., Rahmah N. Detection of Filaria-Specific IgG4 Antibodies and Filarial DNA, for the Screening of Blood Spots for Brugia Timori. Ann. Trop. Med. Parasitol. 2005;99:53–60. doi: 10.1179/136485905X13339[↩]
- Rahmah N., Lim B.H., Mehdi R., Nazmi M.N. Treatment Follow-up of Brugia Malayi Microfilaraemic and Amicrofilaraemic Individ-Uals with Serological Evidence of Active Infection. Malays. J. Microbiol. 2005;1:42–47.[↩]
- Melrose W, Rahmah N. Use of Brugia Rapid dipstick and ICT test to map distribution of lymphatic filariasis in the Democratic Republic of Timor-Leste. Southeast Asian J Trop Med Public Health. 2006 Jan;37(1):22-5.[↩]
- World Health Organization . Monitoring and Epidemiological Assessment of Mass Drug Administration in the Global Programme to Eliminate Lymphatic Filariasis: A Manual for National Elimination Programmes. World Health Organization; Geneva, Switzerland: 2011.[↩]
- Abdo A.I.K., Ngoh Y.Y., Lew M.H., Dass S.A., Rahumatullah A., Noordin R., Tye G.J. Generation of Human ScFv–IgG1Fc Antibodies for Detection of Lymphatic Filarial Recombinant Antigens, BmR1 and BmSXP. Biotechnol. Appl. Biochem. 2022;69:70–76. doi: 10.1002/bab.2082[↩]
- Ayong LS, Tume CB, Wembe FE, Simo G, Asonganyi T, Lando G, Ngu JL. Development and evaluation of an antigen detection dipstick assay for the diagnosis of human onchocerciasis. Trop Med Int Health. 2005 Mar;10(3):228-33. doi: 10.1111/j.1365-3156.2004.01384.x[↩]
- Garg PK, Bhatt S, Kashyap B, George A, Jain BK. Genital filariasis masquerading as testicular torsio. J Vector Borne Dis. 2011 Jun;48(2):119-21. http://www.mrcindia.org/journal/issues/482119.pdf[↩]
- Hertig M, Wolbach SB. Studies on Rickettsia-Like Micro-Organisms in Insects. J Med Res. 1924 Mar;44(3):329-374.7. https://pmc.ncbi.nlm.nih.gov/articles/instance/2041761/pdf/jmedres00003-0073.pdf[↩]
- Williams KP, Sobral BW, Dickerman AW. A robust species tree for the alphaproteobacteria. J Bacteriol. 2007 Jul;189(13):4578-86. doi: 10.1128/JB.00269-07[↩]
- Casiraghi M, Bain O, Guerrero R, Martin C, Pocacqua V, Gardner SL, Franceschi A, Bandi C. Mapping the presence of Wolbachia pipientis on the phylogeny of filarial nematodes: evidence for symbiont loss during evolution. Int J Parasitol. 2004 Feb;34(2):191-203. doi: 10.1016/j.ijpara.2003.10.004[↩]
- McGarry HF, Pfarr K, Egerton G, Hoerauf A, Akue JP, Enyong P, et al. Evidence against Wolbachia symbiosis in Loa loa. Filaria J. 2003;2:9. doi: 10.1186/1475-2883-2-9[↩]
- Chirgwin SR, Porthouse KH, Nowling JM, Klei TR. The filarial endosymbiont Wolbachia sp. is absent from Setariaequina. J Parasitol. 2002;88:1248–50. doi:10.1645/0022-3395(2002)088[1248:TFEWSI]2.0.CO;2[↩]
- Sironi M, Bandi C, Sacchi L, Di Sacco B, Damiani G, Genchi C, et al. Molecular evidence for a close relative of the arthropod endosymbiont Wolbachia in a filarial worm. Mol Biochem Parasitol. 1995;74:223–7. doi: 10.1016/0166-6851(95)02494-8[↩]
- Taylor MJ, Bilo K, Cross HF, Archer JP, Underwood AP. 16S rDNA phylogeny and ultrastructural characterization of Wolbachia intracellular bacteria of the filarial nematodes Brugia malayi, B.pahangi, and Wuchereria bancrofti. Exp Parasitol. 1999;91:356–61. doi: 10.1006/expr.1998.4383[↩][↩]
- Foster J, Ganatra M, Kamal I, Ware J, Makarova K, Ivanova N, et al. The Wolbachia genome of Brugia malayi: Endosymbiont evolution within a human pathogenic nematode. PLoS Biol. 2005;3:E121. doi: 10.1371/journal.pbio.0030121[↩]
- Landmann F, Voronin D, Sullivan W, Taylor MJ. Anti-filarial activity of antibiotic therapy is due to extensive apoptosis after Wolbachia depletion from filarial nematodes. PLoS Pathog. 2011;7:E1002351. doi: 10.1371/journal.ppat.1002351[↩]
- Taylor MJ, Hoerauf A, Bockarie M. Lymphatic filariasis and onchocerciasis. Lancet. 2010;376:1175–85. doi: 10.1016/S0140-6736(10)60586-7[↩]
- Brattig NW, Rathjens U, Ernst M, Geisinger F, Renz A, Tischendorf FW, et al. Lipopolysaccharide-like molecules derived from Wolbachia endobacteria of the filarial Onchocerca volvulus are candidate mediators in the sequence of inflammatory and antiinflammatory responses of human monocytes. Microbes Infect. 2000;2:1147–57. doi: 10.1016/s1286-4579(00)01269-7[↩]
- Hoerauf A, Volkmann L, Hamelmann C, Adjei O, Autenrieth IB, Fleischer B, et al. Endosymbiotic bacteria in worms as targets for a novel chemotherapy in filariasis. Lancet. 2000;355:1242–3. doi: 10.1016/S0140-6736(00)02095-X[↩][↩][↩][↩]
- Mand S, Debrah AY, Klarmann U, Batsa L, Marfo-Debrekyei Y, Kwarteng A, et al. Doxycycline improves filarial lymphedema independent of active filarial infection: A randomized controlled trial. Clin Infect Dis. 2012;55:621–30. doi: 10.1093/cid/cis486[↩]
- Taylor MJ, Makunde WH, McGarry HF, Turner JD, Mand S, Hoerauf A, et al. Macrofilaricidal activity after doxycycline treatment of Wuchereria bancrofti: A double-blind, randomised placebo-controlled trial. Lancet. 2005;365:2116–21. doi: 10.1016/S0140-6736(05)66591-9[↩]
- Hoerauf A, Mand S, Adjei O, Fleischer B, Büttner DW. Depletion of Wolbachia endobacteria in Onchocerca volvulus by doxycycline and microfilaridermia after ivermectin treatment. Lancet. 2001;357:1415–6. doi: 10.1016/S0140-6736(00)04581-5[↩][↩]
- Hoerauf A, Specht S, Büttner M, Pfarr K, Mand S, Fimmers R, et al. Wolbachia endobacteria depletion by doxycycline as antifilarial therapy has macrofilaricidal activity in onchocerciasis: A randomized placebo-controlled study. Med Microbiol Immunol. 2008;197:295–311. doi: 10.1007/s00430-007-0062-1[↩][↩][↩]
- Turner JD, Tendongfor N, Esum M, Johnston KL, Langley RS, Ford L, et al. Macrofilaricidal activity after doxycycline only treatment of Onchocerca volvulus in an area of Loa loa co-endemicity: A randomized controlled trial. PLoS Negl Trop Dis. 2010;4:e660. doi: 10.1371/journal.pntd.0000660[↩][↩][↩][↩]
- Hoerauf A, Specht S, Marfo-Debrekyei Y, Büttner M, Debrah AY, Mand S, et al. Efficacy of 5-week doxycycline treatment on adult Onchocerca volvulus. Parasitol Res. 2009;104:437–47. doi: 10.1007/s00436-008-1217-8[↩]
- Ngenya A, Klarmann-Schulz U, John W, et al. Efficacy of Intensified Hygiene Measures with or without the Addition of Doxycycline in the Management of Filarial Lymphedema: A Randomized Double-Blind, Placebo-Controlled Clinical Trial in Tanzania. Am J Trop Med Hyg. 2024 Aug 27;111(4_Suppl):33-51. doi: 10.4269/ajtmh.24-0049[↩][↩]
- Debrah LB, Klarmann-Schulz U, Osei-Mensah J, et al. Adherence to Hygiene Protocols and Doxycycline Therapy in Ameliorating Lymphatic Filariasis Morbidity in an Endemic Area Post-Interruption of Disease Transmission in Ghana. Am J Trop Med Hyg. 2024 Oct 1;111(4_Suppl):66-82. doi: 10.4269/ajtmh.24-0313[↩]
- Mand S, Debrah AY, Klarmann U, Batsa L, Marfo-Debrekyei Y, Kwarteng A, Specht S, Belda-Domene A, Fimmers R, Taylor M, Adjei O, Hoerauf A. Doxycycline improves filarial lymphedema independent of active filarial infection: a randomized controlled trial. Clin Infect Dis. 2012 Sep;55(5):621-30. doi: 10.1093/cid/cis486[↩]
- Sanprasert V, Sujariyakul A, Nuchprayoon S. A single dose of doxycycline in combination with diethylcarbamazine for treatment of bancroftian filariasis. Southeast Asian J Trop Med Public Health. 2010 Jul;41(4):800-12.[↩]
- Wan Sulaiman WA, Kamtchum-Tatuene J, Mohamed MH, Ramachandran V, Ching SM, Sazlly Lim SM, Hashim HZ, Inche Mat LN, Hoo FK, Basri H. Anti-Wolbachia therapy for onchocerciasis & lymphatic filariasis: Current perspectives. Indian J Med Res. 2019 Jun;149(6):706-714. doi: 10.4103/ijmr.IJMR_454_17[↩]
- Abegunde AT, Ahuja RM, Okafor NJ. Doxycycline plus ivermectin versus ivermectin alone for treatment of patients with onchocerciasis. Cochrane Database Syst Rev. 2016:CD011146. doi: 10.1002/14651858.CD011146.pub2[↩]
- Masud H, Qureshi TQ, Dukley M. Effects of Ivermectin with and without doxycycline on clinical symptoms of onchocerciasis. J Coll Physicians Surg Pak. 2009 Jan;19(1):34-8.[↩]
- Turner JD, Mand S, Debrah AY, Muehlfeld J, Pfarr K, McGarry HF, et al. A randomized, double-blind clinical trial of a 3-week course of doxycycline plus albendazole and ivermectin for the treatment of Wuchereria bancrofti infection. Clin Infect Dis. 2006;42:1081–9. doi: 10.1086/501351[↩]
- Debrah AY, Mand S, Specht S, Marfo-Debrekyei Y, Batsa L, Pfarr K, et al. Doxycycline reduces plasma VEGF-C/sVEGFR-3 and improves pathology in lymphatic filariasis. PLoS Pathog. 2006;2:e92. doi: 10.1371/journal.ppat.0020092[↩]
- Hoerauf A, Mand S, Fischer K, Kruppa T, Marfo-Debrekyei Y, Debrah AY, et al. Doxycycline as a novel strategy against bancroftian filariasis-depletion of Wolbachia endosymbionts from Wuchereria bancrofti and stop of microfilaria production. Med Microbiol Immunol. 2003;192:211–6. doi: 10.1007/s00430-002-0174-6[↩]
- Taylor MJ, Hoerauf A, Townson S, Slatko BE, Ward SA. Anti-Wolbachia drug discovery and development: Safe macrofilaricides for onchocerciasis and lymphatic filariasis. Parasitology. 2014;141:119–27. doi: 10.1017/S0031182013001108[↩]
- Critchley J, Addiss D, Gamble C, Garner P, Gelband H, Ejere H, et al. Albendazole for lymphatic filariasis. Cochrane Database Syst Rev. 2005:CD003753. doi: 10.1002/14651858.CD003753.pub3[↩]
- Gilbert J, Nfon CK, Makepeace BL, Njongmeta LM, Hastings IM, Pfarr KM, et al. Antibiotic chemotherapy of onchocerciasis: In a bovine model, killing of adult parasites requires a sustained depletion of endosymbiotic bacteria (Wolbachia species) J Infect Dis. 2005;192:1483–93. doi: 10.1086/462426[↩][↩]
- Makepeace BL, Rodgers L, Trees AJ. Rate of elimination of Wolbachia pipientis by doxycycline in vitro increases following drug withdrawal. Antimicrob Agents Chemother. 2006;50:922–7. doi: 10.1128/AAC.50.3.922-927.2006[↩][↩]
- Bah GS, Ward EL, Srivastava A, Trees AJ, Tanya VN, Makepeace BL, et al. Efficacy of three-week oxytetracycline or rifampin monotherapy compared with a combination regimen against the filarial nematode Onchocerca ochengi. Antimicrob Agents Chemother. 2014;58:801–10. doi: 10.1128/AAC.01995-13[↩][↩]
- Stocks ME, Freeman MC, Addiss DG. The Effect of Hygiene-Based Lymphedema Management in Lymphatic Filariasis-Endemic Areas: A Systematic Review and Meta-analysis. PLoS Negl Trop Dis. 2015 Oct 23;9(10):e0004171. doi: 10.1371/journal.pntd.0004171[↩]
- Robinson CG, Lee KR, Thomas VD. The Successful Treatment of Elephantiasis Nostras Verrucosa With Ablative Carbon Dioxide Laser. J Cutan Med Surg. 2018 Nov/Dec;22(6):611-613. doi: 10.1177/1203475418763548[↩]
- Filariasis. https://emedicine.medscape.com/article/217776-overview#a7[↩]