Contents
- What is lymphedema
- As a breast cancer survivor, what is my risk of getting lymphedema?
- How does surgery affect my risk of lymphedema?
- Does radiation increase the risk of lymphedema?
- If I have had lymph nodes removed under one arm, do I have to worry about the lymph nodes in other areas of my body?
- Do I have to worry about this for my whole life?
- Should I be using my arm (or leg) for everyday activities?
- The Lymphatic System
- Lymphedema causes
- Risk factors for lymphedema
- Lymphedema prevention
- Lymphedema signs and symptoms
- Lymphedema grade
- Lymphedema diagnosis
- Lymphedema treatment
What is lymphedema
Lymphedema is a long-term (chronic) lymphatic disease that causes disfiguring swelling in one or more parts of the body. Lymphedema happens when lymph builds up in your body’s soft and fatty tissues just under your skin. This build-up causes swelling (or edema) in any part of the body, most often in the arms or legs. Lymphedema can also affect the face, neck, abdomen (belly), and genitals – depending on the part of the body that was treated. Lymph is the protein-rich body fluid that contains white blood cells that defend against germs. Lymph can build up when the lymphatic system for fluid transport is damaged or blocked. The lymphatic system is part of the immune system made up of a network of channels and lymph glands throughout your body that helps fight infection and remove excess fluid. The lymphatic system fulfills the function of ‘immune trafficking,’ the process whereby infection-fighting cells can be mobilized to the tissues that require assistance. When the lymphatic system is compromised by surgery, trauma, or improper development, the affected part of the body is prone to recurrent infection because of the faulty surveillance mechanism.
Lymphedema can be hereditary (Primary Lymphedema) or it can occur after a surgical procedure, infection, radiation or other physical trauma (Secondary Lymphedema). In breast cancer, for example, lymphedema can appear in the arm on the same side as the cancer, after lymph nodes are removed from the armpit region for cancer staging. Primary Lymphedema often occurs in the lower extremities.
Up to 10 million Americans, and hundreds of millions worldwide, suffer from lymphedema and lymphatic diseases. More people suffer from these diseases in the United States than suffer from Multiple Sclerosis (MS), Muscular Dystrophy, amyotrophic lateral sclerosis (ALS), Parkinson’s disease, and AIDS – combined.
Causes of lymphedema include:
- Infection
- Cancer
- Scar tissue from radiation therapy or surgical removal of lymph nodes
- Inherited conditions in which lymph nodes or vessels are absent or abnormal
Lymphedema can result from surgery or radiation therapy to treat certain cancers. If you are being or have been treated for cancer, talk to someone on your cancer care team about your risk of lymphedema and what you can do to help lower it. Once chronic lymphedema has started, it cannot be cured. But early and careful management can reduce symptoms and help keep it from getting worse.
All cancer treatment survivors, including those of melanoma, prostate and ovarian cancer, are susceptible to developing lymphedema. Breast cancer survivors can be at a high risk for developing lymphedema and 100% of those treated for neck and head cancer will develop the disease. Physical trauma can also result in lymphedema, a major cause of lymphatic disease among our wounded veterans.
Children can be affected with debilitating lymphatic diseases, such as lymphatic malformation and lymphangiectasia, and over 100 million people worldwide suffer from the lymphatic disease filariasis (elephantiasis). The lymphatic system plays a role in AIDS, diabetes, heart disease, rheumatoid arthritis, lupus, and cancer metastasis.
It’s important that lymphedema is identified and treated as soon as possible. If it isn’t treated, it can get worse.
Treatment can help control symptoms. It includes exercise, compression devices, skin care, and massage.
Call your doctor, nurse, physical therapist, or lymphedema therapist if you notice any of the signs of lymphedema listed below or any of these changes:
- If any part of the affected area, such as an arm or a leg, feels hot, looks red, or swells suddenly. These could be a sign of infection or a blood clot, and you might need treatment right away.
- If you have a temperature of 100.5°F (38 °C) or higher (taken by mouth) that’s not related to a cold or flu
- If you have any new pain in the affected area with no known cause
If you’ve had lymph nodes removed or radiation treatment, look closely at your body in front of a mirror. Compare both sides of your body and look for changes in size, shape, or skin color. Get to know your body and what’s normal for you. This way you can spot changes and get treatment right away. Let your doctor or nurse know if you notice any of the signs listed above.
Some doctors measure the affected body part (like a leg or arm) before surgery, then re-measure afterward so that swelling can be detected and treated before it becomes obvious. You can ask your doctor to take these measurements or refer you to a physical therapist to have this done. If possible, ask to be referred to a certified lymphedema therapist.
To find a certified lymphedema therapist contact:
- Lymphology Association of North America (https://www.clt-lana.org/)
- National Lymphedema Network (https://www.lymphnet.org/)
As a breast cancer survivor, what is my risk of getting lymphedema?
Estimates vary and, fortunately, the risk has been progressively declining. In the beginning, breast cancer surgery carried a 50% risk of lymphedema development. Today, patients who have axillary lymph node dissection have a lifetime risk of 15-25%. For individuals whose surgery is limited to sentinel node techniques, without adjuvant radiation, the risk is about 6%.
It is important to strive to keep life as normal as possible in the face of the fixed demands related to the presence of lymphedema. Seeking support from your fellow patients is also often a wonderful way to collectively share the experience and help to mitigate the anger. The ability to talk about the problem is an important step toward acceptance.
How does surgery affect my risk of lymphedema?
The risk is chiefly aligned with lymph node removal. Individuals that have just lumpectomy, or other surgical interventions, are at such low risk that it is impossible to estimate. Sentinel node techniques, alone, are used in about 40% of current breast cancer patients. The sentinel node technique is defined as the removal of no more than four lymph nodes, where the risk is about 6%. If you have more than four lymph nodes removed, the risk rises to 15% to 25%.
Does radiation increase the risk of lymphedema?
Yes, radiation can traumatize the lymphatic system equivalently to surgery, even if surgery is not done. However, just as all surgery is not alike, not all radiation therapy is the same. In general, radiation therapy confers risk that is roughly equivalent to axillary lymph node dissection and increases the risk associated with surgery if both treatments are performed.
If I have had lymph nodes removed under one arm, do I have to worry about the lymph nodes in other areas of my body?
No. The lymphatic system is present throughout the body, but lymphedema is a regional disease that affects only the part of the body that is subjected to surgery or radiation.
Do I have to worry about this for my whole life?
The proper term to use is ‘vigilance.’ Stated positively, the primary risk for lymphedema development is in the first year following surgery and radiation therapy, when 90% of the cases occur. By the end of 3 years, 95% of the cases will have appeared. If you don’t have lymphedema after 3 years of vigilance, the risk remains, but it is quite small. If you take the proper precautions and use the proper surveillance, the risk can be maintained as small as possible.
Should I be using my arm (or leg) for everyday activities?
Yes, absolutely. Bear in mind, however, that physical activity increases blood flow, which increases the formation of lymph in the arm or leg at risk. You don’t want to push the lymphatic system ‘over the edge’. Once you recognize your threshold for activity, you can gently extend your limits over time, perhaps, in addition, by using a Class I compression garment during activity that is perceived to be physically stressful.
It is very important, to weigh the risk-to-benefit ratio of your activity. There is some finite risk of lymphedema with activities like surfing, rock climbing, to choose two random examples. But you have to weigh the importance to your life of those continuing experiences. With or without ‘risky’ activities appropriate treatment for lymphedema is essential when the lymphedema appears. It is very important to faithfully use the Class I compression garment that is provided to you, particularly during the activity that poses theoretical risk. It is very important to maintain surveillance for changes in the limb-at-risk. Take precautions against infection when there are breaks in the skin and seek medical attention early if any changes are observed. When you go outside, put on a sunscreen (SPF 30+), because sunburn can aggravate lymphedema. When you are working in the kitchen, be careful. When you’re in the garden, be careful, and wear gloves if there is the possibility of skin trauma. But what you want to lift, lift. What you want to do, do. And where you want to go, go. Just be careful. Once you are a cancer survivor, you must enjoy the gift of life!
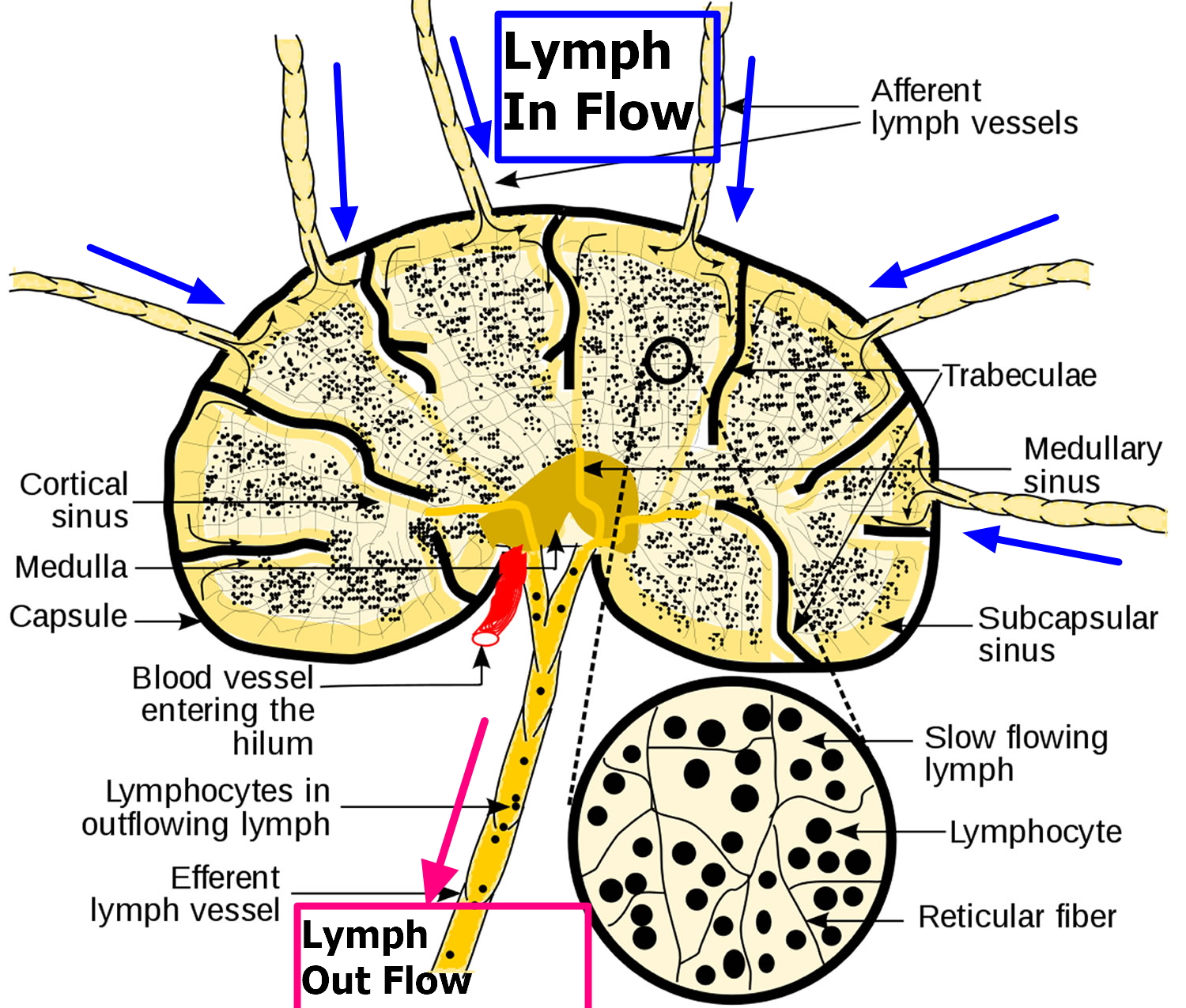
The Lymphatic System
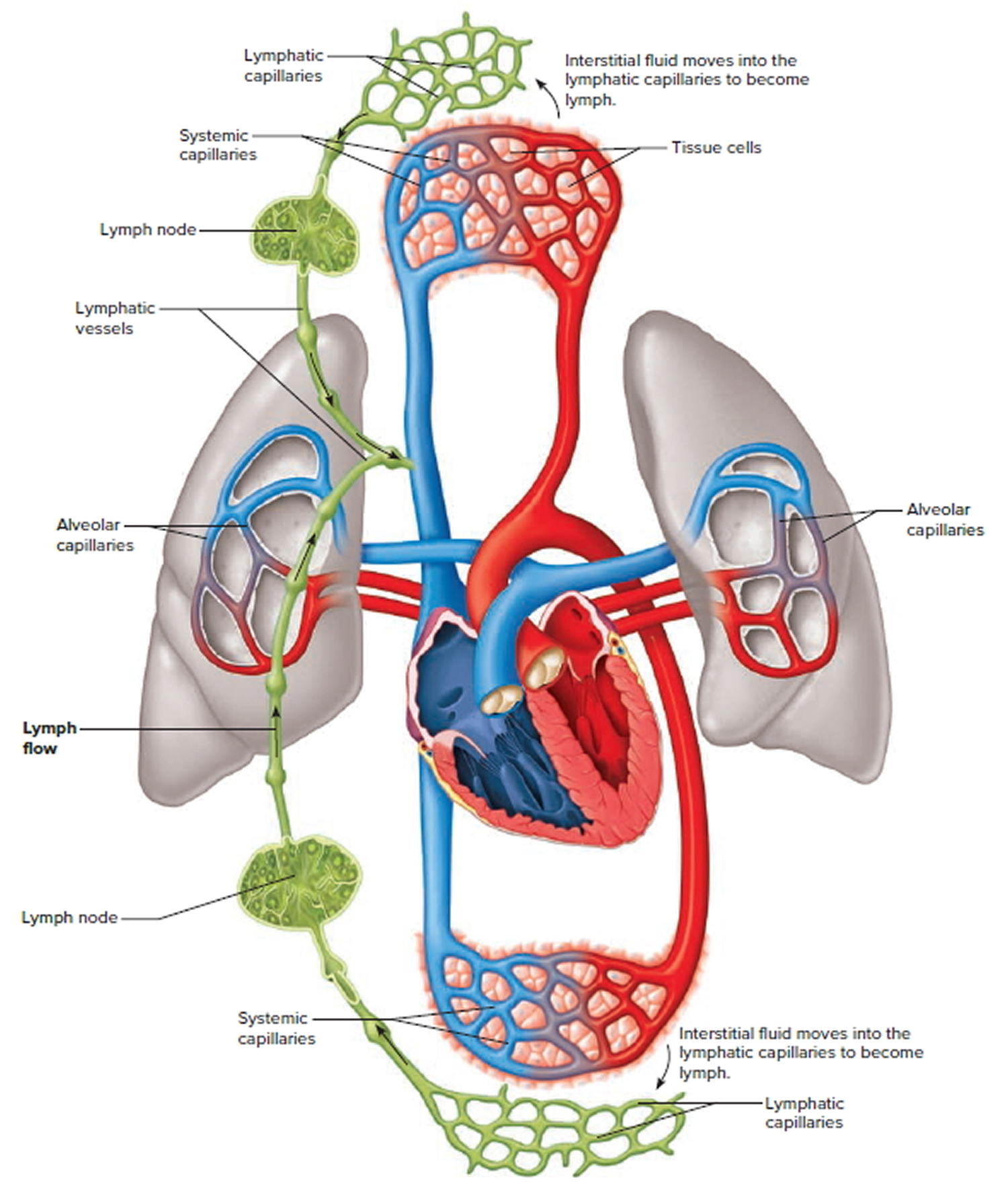
The lymphatic system is a vast collection of cells and biochemicals that travel in lymphatic vessels, and the organs and glands that produce them. The lymphatic system includes a network of vessels that assist in circulating body fluids, so it is closely associated with the cardiovascular system. Lymphatic vessels transport excess fluid away from interstitial spaces in most tissues and return it to the bloodstream (Figure 4). Without the lymphatic system, this fluid would accumulate in tissue spaces. Special lymphatic capillaries, called lacteals, are located in the lining of the small intestine. They absorb digested fats and transport them to the venous circulation.
The lymphatic system has a second major function— it enables you to live in a world with different types of organisms. Some of them live in or on the human body and in some circumstances may cause infectious diseases. Cells and biochemicals of the lymphatic system launch both generalized and targeted attacks against “foreign” particles, enabling the body to destroy infectious agents. This immunity against disease also protects against toxins and cancer cells. When the immune response is abnormal, persistent infection, cancer, allergies, and autoimmune disorders may result.
The larger lymphatic vessels lead to specialized organs called lymph nodes. After leaving the lymph nodes, the vessels merge to form still larger lymphatic trunks.
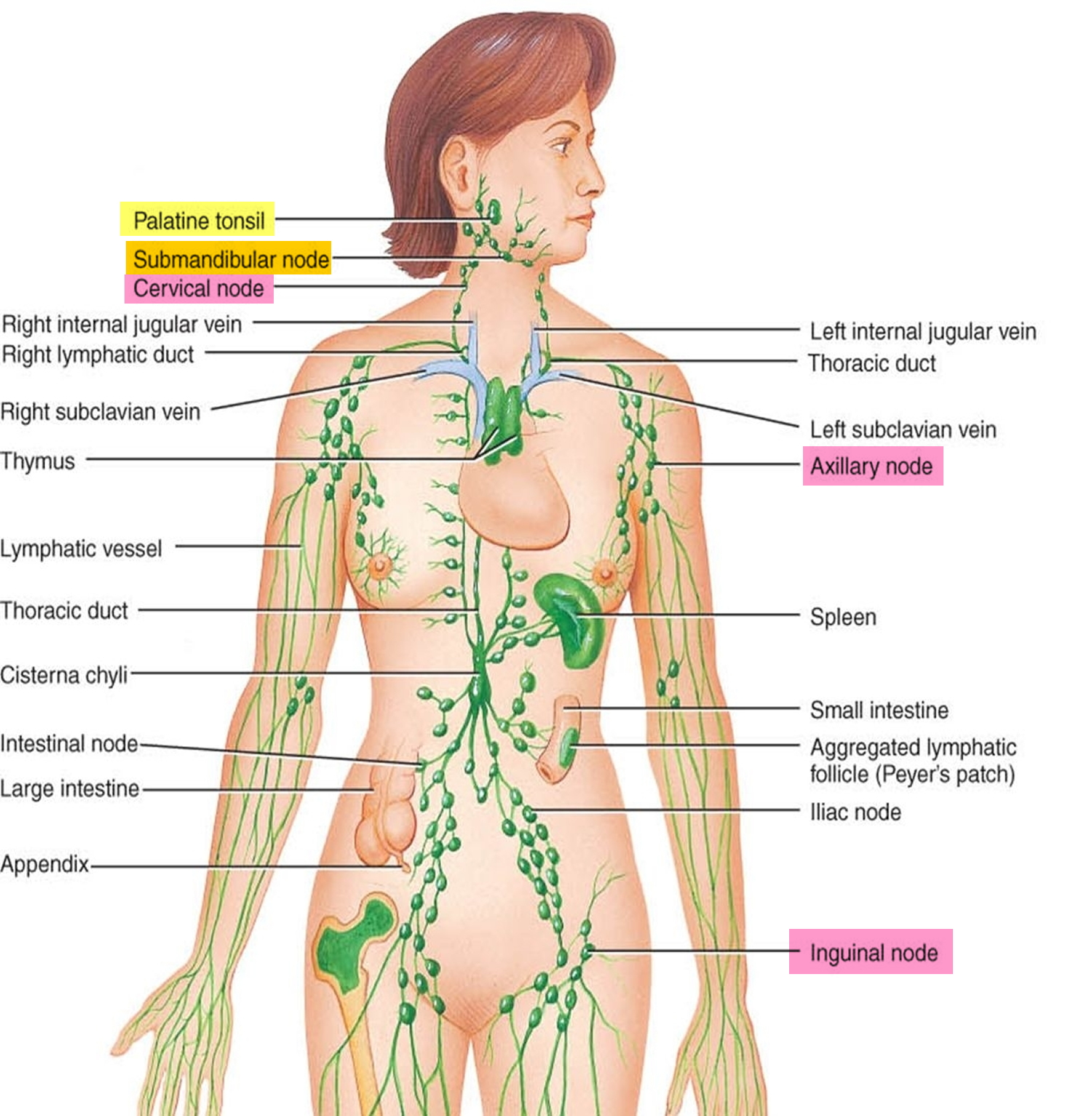
Figure 1. Locations of major lymph nodes
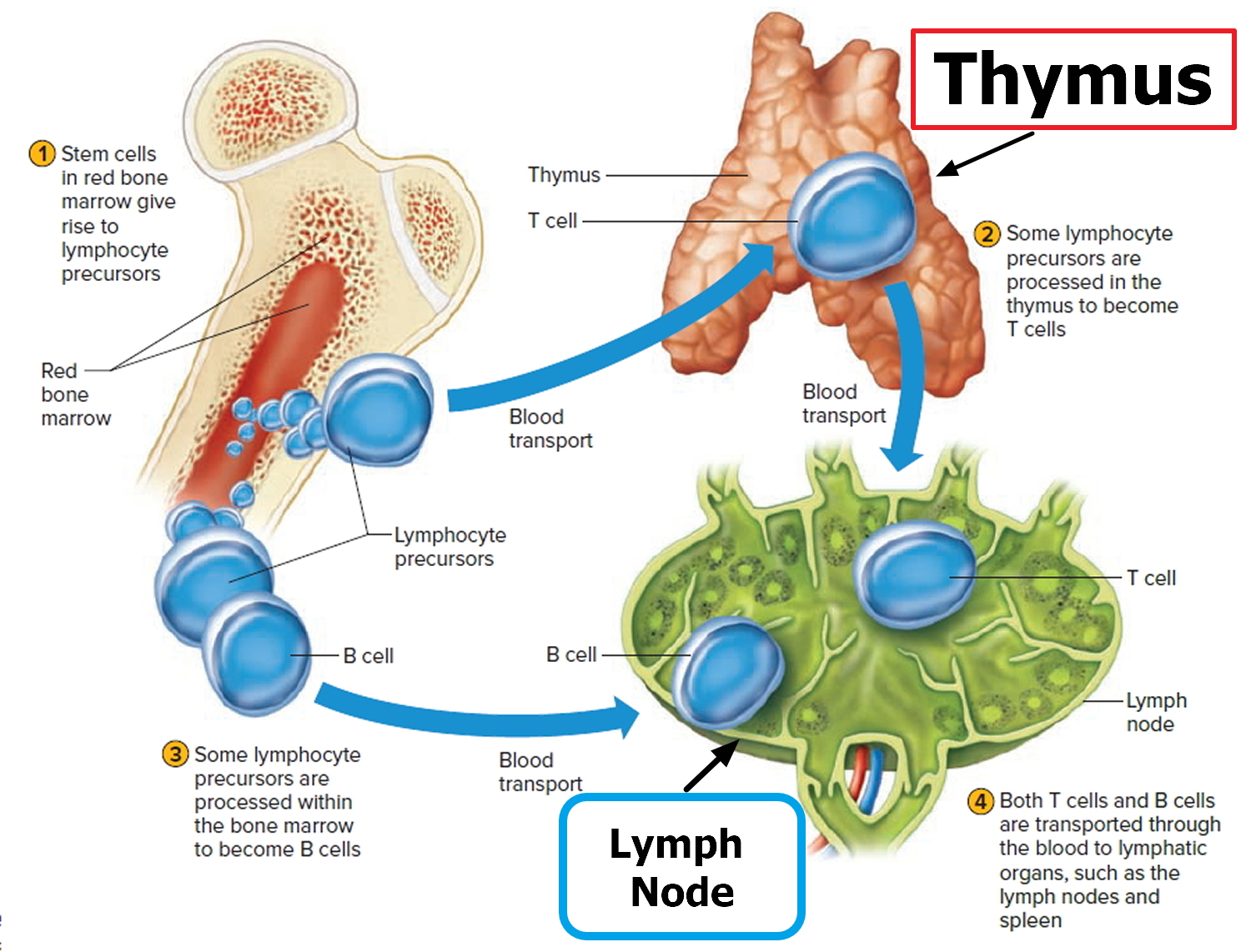
Figure 2. Functions of lymph nodes in the lymphatic system
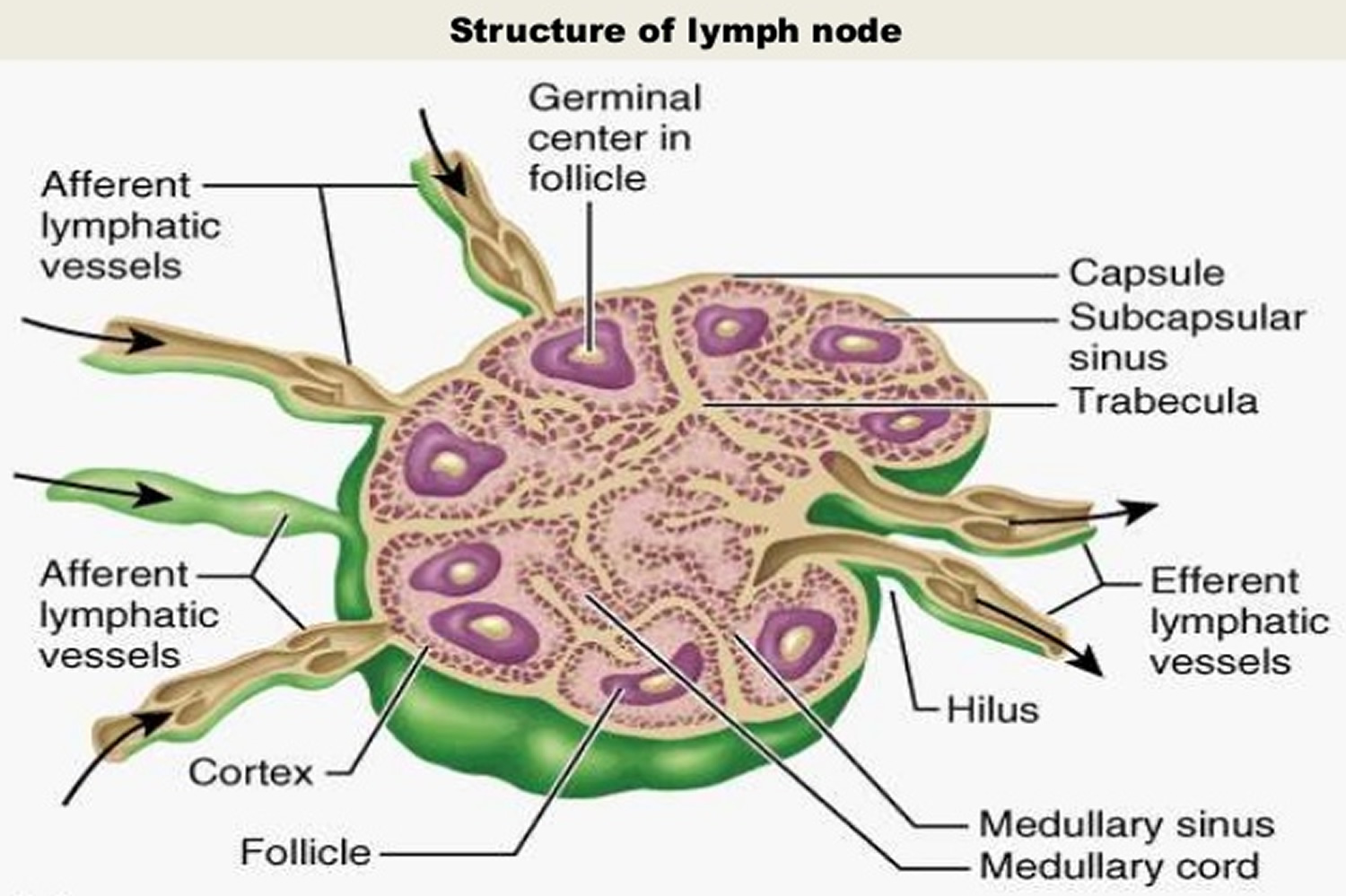
Figure 3. Lymph node anatomy
Figure 4. Schematic representation of lymphatic vessels transporting fluid from interstitial spaces to the bloodstream. Depending on its origin, lymph enters the right or left subclavian vein.
Lymph Movement
Lymph is essentially tissue fluid (interstitial fluid) that has entered a lymphatic capillary. Lymphatic capillaries are microscopic, closed-ended tubes that originate in the interstitial spaces of most tissues. Thus, lymph formation depends upon tissue fluid formation.
The walls of lymphatic vessels are similar to those of veins, but are thinner. Like some peripheral veins, lymphatic vessels have valves that help prevent backflow of lymph.
Filtration from the blood plasma normally exceeds reabsorption, leading to the net formation of tissue fluid. This accumulation of tissue fluid increases the tissue fluid hydrostatic pressure, which moves tissue fluid into lymphatic capillaries, forming lymph. Lymph returns to the bloodstream most of the small proteins that passed through the blood capillary walls. At the same time, lymph transports foreign particles, such as bacteria and viruses, to lymph nodes.
The hydrostatic pressure of tissue fluid drives lymph into lymphatic capillaries. However, muscular activity largely influences the movement of lymph through the lymphatic vessels. Lymph within lymphatic vessels, like venous blood, is under relatively low hydrostatic pressure and may not flow readily through the lymphatic vessels without help from contraction of skeletal muscles in the limbs, contraction of the smooth muscle in the walls of the larger lymphatic trunks, and pressure changes associated with breathing.
Contracting skeletal muscles compress lymphatic vessels. This squeezing action moves the lymph inside lymphatic vessels. Valves in these vessels prevent backflow, so lymph can only move toward a collecting duct. Additionally, smooth muscle in the walls of larger lymphatic trunks contracts rhythmically and compresses the lymph inside, forcing the fluid onward.
Breathing aids lymph circulation by creating a relatively low pressure in the thoracic cavity during inhalation. At the same time, the contracting diaphragm increases the pressure in the abdominal cavity. Consequently, lymph is squeezed out of the abdominal vessels and forced into the thoracic vessels. Once again, valves in lymphatic vessels prevent lymph backflow.
The continuous movement of fluid from interstitial spaces into blood and lymphatic capillaries stabilizes the volume of fluid in these interstitial spaces. Conditions that interfere with lymph movement cause tissue fluid to accumulate within the interstitial spaces, producing edema or swelling. Edema may develop when surgery removes lymphatic tissue, preventing lymph flow. For example, a surgeon removing a cancerous breast tumor may also remove nearby axillary lymph nodes to prevent associated lymphatic vessels from transporting cancer cells to other sites. Removing this lymphatic tissue can obstruct drainage from the upper limb, causing edema.
Figure 5. Lymph Movement
Lymphedema occurs when lymph is not able to flow through the body the way that it should.
When the lymph system is working as it should, lymph flows through the body and is returned to the bloodstream.
- Fluid and plasma leak out of the capillaries (smallest blood vessels) and flow around body tissues so the cells can take up nutrients and oxygen.
- Some of this fluid goes back into the bloodstream. The rest of the fluid enters the lymph system through tiny lymph vessels. These lymph vessels pick up the lymph and move it toward the heart. The lymph is slowly moved through larger and larger lymph vessels and passes through lymph nodes where waste is filtered from the lymph.
- The lymph keeps moving through the lymph system and collects near the neck, then flows into one of two large ducts:
- The right lymph duct collects lymph from the right arm and the right side of the head and chest.
- The left lymph duct collects lymph from both legs, the left arm, and the left side of the head and chest.
- These large ducts empty into veins under the collarbones, which carry the lymph to the heart, where it is returned to the bloodstream.
When part of the lymph system is damaged or blocked, fluid cannot drain from nearby body tissues. Fluid builds up in the tissues and causes swelling.
Figure 6. Lymphedema arm
Figure 7. Lymphedema leg
Lymphedema causes
There are two types of lymphedema
Lymphedema may be either primary or secondary:
- Primary lymphedema is caused by the abnormal development of the lymph system. Symptoms may occur at birth or later in life.
- Secondary lymphedema is caused by damage to the lymph system. The lymph system may be damaged or blocked by infection, injury, cancer, removal of lymph nodes, radiation to the affected area, or scar tissue from radiation therapy or surgery.
What causes lymphedema
Your lymphatic system is crucial to keeping your body healthy. It circulates protein-rich lymph fluid throughout your body, collecting bacteria, viruses and waste products. Your lymphatic system carries this fluid and harmful substances through your lymph vessels, which lead to lymph nodes. The wastes are then filtered out by lymphocytes — infection-fighting cells that live in your lymph nodes — and ultimately flushed from your body.
Lymphedema occurs when your lymph vessels are unable to adequately drain lymph fluid, usually from an arm or leg. Lymphedema can be either primary or secondary. This means it can occur on its own (primary lymphedema), or it can be caused by another disease or condition (secondary lymphedema). Secondary lymphedema is far more common than primary lymphedema.
Primary lymphedema
Primary lymphedema is a rare, inherited condition caused by alterations (mutations) in genes responsible for the development of the lymphatic system in your body. The “faulty” genes cause the parts of the lymphatic system responsible for draining fluid to not develop properly or not work as they should. Primary lymphoedema often runs in families, although not every child born to someone with the condition will develop it themselves.
Specific causes of primary lymphedema include:
- Milroy’s disease (congenital lymphedema). This disorder begins in infancy and causes lymph nodes to form abnormally.
- Meige’s disease (lymphedema praecox). This disorder often causes lymphedema around puberty or during pregnancy, though it can occur later, until age 35.
- Late-onset lymphedema (lymphedema tarda). This occurs rarely and usually begins after age 35.
Secondary lymphedema
Any condition or procedure that damages your lymph nodes or lymph vessels can cause lymphedema. Causes include:
- Surgery. Removal of or injury to lymph nodes and lymph vessels may result in lymphedema. For example, lymph nodes may be removed to check for spread of breast cancer, and lymph nodes may be injured in surgery that involves blood vessels in your limbs.
- Radiation treatment for cancer. Radiation can cause scarring and inflammation of your lymph nodes or lymph vessels.
- Cancer. If cancer cells block lymphatic vessels, lymphedema may result. For instance, a tumor growing near a lymph node or lymph vessel could enlarge enough to block the flow of the lymph fluid.
- Infection. An infection of the lymph nodes or parasites can restrict the flow of lymph fluid. Infection-related lymphedema is most common in tropical and subtropical regions and is more likely to occur in developing countries.
- Inflammation. Medical conditions that cause tissue to become red and swollen can also permanently damage the lymphatic system.Conditions that can cause lymphoedema include:
- rheumatoid arthritis – causes pain and swelling in the joints
- eczema – causes the skin to become itchy, reddened, dry and cracked
- Venous diseases. Diseases that affect the flow of blood through the veins can cause lymphoedema in some people. The abnormal or damaged veins can cause fluid to overflow from the veins into the tissue spaces. This overwhelms and eventually exhausts the parts of the lymphatic system responsible for draining this fluid. Some venous diseases that can lead to lymphoedema include:
- deep vein thrombosis (DVT) – a blood clot in one of the deep veins in the body
- swollen and enlarged veins (varicose veins) – where poor drainage of blood in the veins causes higher vein pressure and more fluid overflowing into the surrounding tissues
- Obesity. Obesity is another possible cause of secondary lymphoedema. People who are obese, particularly those who are severely obese, have an increased risk of developing swollen body parts. It’s not clear exactly why this is, but it’s been suggested that the extra fatty tissue affects the lymphatic channels in some way, reducing the flow of fluid through them. In these cases, weight loss is an important part of treatment and even just starting to lose weight can make a big difference to the swelling.
- Trauma and injury. In a small number of cases, lymphoedema can be caused by an accidental injury to the lymphatic system. For example, it can sometimes occur after a road traffic accident where there’s extensive bruising or soft tissue loss.
- Immobility. Movement and exercise help lymph drainage because muscle activity surrounding the lymphatic vessels massages fluid into and along them. Reduced movement can therefore lead to lymphoedema because the fluid in the lymphatic system doesn’t get moved along. For example, people who have limited mobility for a long period of time as a result of an illness, nerve damage or arthritis may be at risk of lymphoedema.
Surgery for cancer
Treatment for cancer can involve surgery to remove sections of the lymphatic system.
The surgeon will try to limit damage to your lymphatic system, although this isn’t always possible. There’s a particular risk of lymphoedema occurring after treatment for any cancer where lymph glands are removed.
Some of the more common cancers where this happens are:
- breast cancer
- melanoma skin cancer
- gynecological cancers – such as cervical cancer and vulval cancer
- genitourinary cancers – such as prostate cancer or penile cancer
Radiotherapy
Radiotherapy uses controlled doses of high-energy radiation to destroy cancerous tissue, but it can also damage healthy tissue.
If radiotherapy is needed to destroy cancerous cells in your lymphatic system, there’s a risk that the lymphatic system could become permanently damaged and unable to drain fluid properly.
Infections
An infection, such as cellulitis, can sometimes cause lymphoedema. Severe cellulitis can damage the tissue around the lymphatic system, causing it to become scarred.
Filariasis is another infectious cause of lymphoedema. Lymphatic filariasis is a parasitic disease caused by microscopic, thread-like worms.
The adult worms only live in the human lymphatic system and block lymph drainage. It’s a common cause of lymphoedema worldwide, but it isn’t generally a risk in the US.
Any change in the structure of the lymph system puts a person at risk for lymphedema.
Lymphedema can occur after any cancer or treatment that affects the flow of lymph through the lymph nodes, such as removal of lymph nodes. It may develop within days or many years after treatment. Most lymphedema develops within three years of surgery.
Lymphedema often occurs in breast cancer patients who had all or part of their breast removed and axillary (underarm) lymph nodes removed. Lymphedema in the legs may occur after surgery for uterine cancer, prostate cancer, lymphoma, or melanoma. It may also occur with vulvar cancer or ovarian cancer.
Surgery
During surgery for cancer the doctor may take out lymph nodes near the tumor to see if the cancer has spread. When lymph nodes are removed, lymph vessels that carry fluid from that area to the rest of the body are taken out, too, because they go through and are wrapped around the nodes.
Taking out lymph nodes and vessels makes it harder for the lymph fluid in the arms, legs, or other body parts to flow to the chest where it can get back into the bloodstream. If the remaining lymph vessels cannot remove enough of the fluid in the area, the fluid builds up and causes swelling, or lymphedema.
Radiation
Radiation treatment can affect the flow of lymph fluid by scarring and damaging the lymph nodes and vessels. This increases the risk for lymphedema.
Cancer
Sometimes, a tumor itself can block part of the lymph system and cause lymphedema.
Infection
Infections that restrict lymph flow can cause lymphedema.
Risk factors for lymphedema include the following:
- Removal and/or radiation of lymph nodes in the underarm, groin, pelvis, or neck. The risk of lymphedema increases with the number of lymph nodes affected. There is less risk with the removal of only the sentinel lymph node (the first lymph node to receive lymphatic drainage from a tumor).
- Being overweight or obese.
- Slow healing of the skin after surgery.
- A tumor that affects or blocks the left lymph duct or lymph nodes or vessels in the neck, chest, underarm, pelvis, or abdomen.
- Scar tissue in the lymph ducts under the collarbones, caused by surgery or radiation therapy.
When does lymphedema develop?
Just after surgery: Temporary lymphedema
Lymphedema can start right after surgery. This is called temporary (or short-term) lymphedema. It’s usually mild and goes away in the next month or so. It can also start later, about 6 to 8 weeks after surgery or radiation.
Even though this type of lymphedema usually goes away on its own over time, you should tell your doctor about it right away. The swollen area may look red and feel hot, which could also be a sign of blood clot, infection, or other problem that needs to be checked.
If there are no other problems causing the swelling, temporary lymphedema might be treated by raising the arm or leg and taking medicines to help reduce inflammation.
Months or years after cancer treatment: Chronic lymphedema
This form of lymphedema develops slowly over time. It may show up many months or even years after cancer treatment. The swelling can range from mild to severe. The lymph fluid that collects in the skin and underlying tissues can be very uncomfortable. It can keep nutrients from reaching the cells, interfere with wound healing, and lead to infections.
Lymphedema can be a long-term problem, but there are ways to manage it. The key is to get help right away. Lymphedema is easier to treat and more likely to respond to treatment if it’s treated early.
Risk factors for lymphedema
Factors that may increase your risk of developing lymphedema after cancer, from cancer treatment or from other secondary causes include:
- Older age
- Excess weight or obesity
- Rheumatoid arthritis or psoriatic arthritis
Lymphedema prevention
If you have had or you are going to have cancer surgery, ask your doctor whether your procedure will involve your lymph nodes or lymph vessels. Ask if your radiation treatment will be aimed at lymph nodes, so you’ll be aware of the possible risks.
To reduce your risk of lymphedema, try to:
- Protect your arm or leg. Avoid injury to your affected limb. Cuts, scrapes and burns can invite infection. Protect yourself from sharp objects. For example, shave with an electric razor, wear gloves when you garden or cook, and use a thimble when you sew. If possible, avoid medical procedures, such as blood draws and vaccinations, in your affected limb.
- Treat any cuts, burns, bites or scrapes immediately.
- Wear long oven mitts when cooking and gloves when gardening or doing yard work.
- Wear high-factor sun block or long-sleeved clothing to avoid sunburn.
- Use insect repellant when outside.
- Use an electric shaver or cream for hair removal; do not use a razor.
- Whenever possible use the arm without lymphedema when checking blood pressure or for blood tests.
- Rest your arm or leg while recovering. After cancer treatment, exercise and stretching are encouraged. But avoid strenuous activity until you’ve recovered from surgery or radiation.
- Avoid heat on your arm or leg. Don’t apply ice or heat, such as with a heating pad, to your affected limb. Also, protect your affected limb from extreme cold.
- Elevate your arm or leg. Whenever possible, elevate your affected limb above the level of your heart.
- Avoid tight clothing. Avoid anything that could constrict your arm or leg, such as tightfitting clothing and, in the case of your arm, blood pressure cuffs. Ask that your blood pressure be taken in your other arm.
- Keep your arm or leg clean. Make skin and nail care high priorities. Inspect the skin on your arm or leg daily, watching for changes or breaks in your skin that could lead to infection. Don’t go barefoot.
- Maintain an active lifestyle and healthy weight.
- Begin a weight-loss program if you are overweight.
- Call your doctor right away if you have fever, redness, tenderness, or warmth of the arm or leg. These can be the first signs of lymphedema.
- Do not move or carry very heavy objects.
- Do not use saunas.
- Check your hand and arm daily for signs of lymphedema or small injuries that could lead to the condition.
- When cleared by your doctor, do the recommended exercises to regain a full range of motion of the arm or leg.
There is no sure way to prevent all cases of lymphedema, but there are ways to lower the risk of it developing. For example, when lymph nodes need to be removed, some modern surgery techniques might be helpful:
- Sentinel lymph node biopsy is a major advance in cancer surgery. It’s used to find the lymph nodes the tumor drains into so they can be checked for cancer. If cancer is not found in these nodes, it allows the surgeon to remove fewer lymph nodes. Sentinel lymph node biopsy has shown to help reduce the risk of lymphedema.
- Axillary reverse mapping is a technique that uses a blue dye put in the upper arm to help find the lymph nodes that drain the arm. The surgeon can then try to not alter these lymph nodes. Results are not clear that axillary reverse mapping helps reduce lymphedema.
There might be things you can do to lower your risk as well. Talk to your health care team about your risk of lymphedema. If you are at risk, it’s important to know what to watch for (see below), and to take the steps to help reduce your risk part of your daily routine for the rest of your life.
Keep skin and nails clean and cared for, to prevent infection.
Bacteria can enter the body through a cut, scratch, insect bite, or other skin injury. Fluid that is trapped in body tissues by lymphedema makes it easy for bacteria to grow and cause infection. Look for signs of infection, such as redness, pain, swelling, heat, fever, or red streaks below the surface of the skin. Call your doctor right away if any of these signs appear. Careful skin and nail care helps prevent infection:
- Use cream or lotion to keep the skin moist.
- Treat small cuts or breaks in the skin with an antibacterial ointment.
- Avoid needle sticks of any type into the limb (arm or leg) with lymphedema. This includes shots or blood tests.
- Use a thimble for sewing.
- Avoid testing bath or cooking water using the limb with lymphedema. There may be less feeling (touch, temperature, pain) in the affected arm or leg, and skin might burn in water that is too hot.
- Wear gloves when gardening and cooking.
- Wear sunscreen and shoes when outdoors.
- Cut toenails straight across. See a podiatrist (foot doctor) as needed to prevent ingrown nails and infections.
- Keep feet clean and dry and wear cotton socks.
Avoid blocking the flow of fluids through the body.
It is important to keep body fluids moving, especially through an affected limb or in areas where lymphedema may develop.
- Do not cross legs while sitting.
- Change sitting position at least every 30 minutes.
- Wear only loose jewelry and clothes without tight bands or elastic.
- Do not carry handbags on the arm with lymphedema.
- Do not use a blood pressure cuff on the arm with lymphedema.
- Do not use elastic bandages or stockings with tight bands.
Keep blood from pooling in the affected limb.
- Keep the limb with lymphedema raised higher than the heart when possible.
- Do not swing the limb quickly in circles or let the limb hang down. This makes blood and fluid collect in the lower part of the arm or leg.
- Do not apply heat to the limb.
Lymphedema signs and symptoms
Signs of lymphedema
If lymphedema does develop, it’s important to recognize it early so you can start treatment right away.
Common signs and symptoms you should watch for include:
- Swelling
- Part of your body (like your arm, leg, belly, or genitals) feeling full or heavy
- Skin changing texture, feeling tight or hard, or looking red
- New aching, tingling, numbness, or other discomfort in the area
- Less movement or flexibility in nearby joints (like your hand, wrist, or ankle) or your eyelid(s), throat, or lips
- Trouble fitting into clothes in one area, such as a sleeve, pant leg, or shoe being tight
- Collars, rings, watches, and/or bracelets feeling tight even though you haven’t gained weight
At first, the skin usually stays soft, and raising the affected body part might relieve the swelling. But over time, the swollen area may become hot and red and the skin hard and stiff. If untreated, movement and use of the affected part may become limited.
Lymphedema signs and symptoms, which occur in your affected arm or leg, include:
- Swelling of part or all of your arm or leg, including fingers or toes
- A feeling of heaviness, fullness or tightness in an arm or leg.
- Restricted range of motion
- Trouble moving a joint in the arm or leg.
- A tight feeling in the skin.
- A feeling of tightness when wearing clothing, shoes, bracelets, watches, or rings.
- Aching or discomfort
- Recurring infections
- Hardening and thickening of the skin (fibrosis), with or without skin changes such as blisters or warts.
- Swelling of an arm or leg, which may include fingers and toes.
- Itching of the legs or toes.
- A burning feeling in the legs.
- Trouble sleeping.
- Loss of hair.
The swelling caused by lymphedema ranges from mild, hardly noticeable changes in the size of your arm or leg to extreme changes that make the limb hard to use. Daily activities and the ability to work or enjoy hobbies may be affected by lymphedema.
These symptoms may occur very slowly over time or more quickly if there is an infection or injury to the arm or leg.
Lymphedema caused by cancer treatment may not occur until months or years after treatment.
Lymphedema grade
A grading system is also used to diagnose and describe lymphedema. Grades 1, 2, 3, and 4 are based on size of the affected limb and how severe the signs and symptoms are.
Stages may be used to describe lymphedema.
- Stage I: The limb (arm or leg) is swollen and feels heavy. Pressing on the swollen area leaves a pit (dent). This stage of lymphedema may go away without treatment.
- Stage II: The limb is swollen and feels spongy. A condition called tissue fibrosis may develop and cause the limb to feel hard. Pressing on the swollen area does not leave a pit.
- Stage III: This is the most advanced stage. The swollen limb may be very large. Stage III lymphedema rarely occurs in breast cancer patients. Stage III is also called lymphostatic elephantiasis.
Lymphedema diagnosis
If you’re at risk of lymphedema — for instance, if you’ve recently had cancer surgery involving your lymph nodes — your doctor may diagnose lymphedema based on your signs and symptoms.
It is important to make sure there are no other causes of swelling, such as infection or blood clots. The following tests and procedures may be used to diagnose lymphedema:
- Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
- Lymphoscintigraphy: A method used to check the lymph system for disease. A very small amount of a radioactive substance that flows through the lymph ducts and can be taken up by lymph nodes is injected into the body. A scanner or probe is used to follow the movement of this substance. Lymphoscintigraphy is used to find the sentinel lymph node (the first node to receive lymph from a tumor) or to diagnose certain diseases or conditions, such as lymphedema.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI) produces 3-D, high-resolution images.
- CT scan. This X-ray technique produces detailed, cross-sectional images of your body’s structures. CT scans can reveal blockages in the lymphatic system.
- Doppler ultrasound. This variation of the conventional ultrasound looks at blood flow and pressure by bouncing high-frequency sound waves (ultrasound) off red blood cells. Ultrasound can help find obstructions.
- Radionuclide imaging of your lymphatic system (lymphoscintigraphy). During this test you’re injected with a radioactive dye and then scanned by a machine. The resulting images show the dye moving through your lymph vessels, highlighting blockages.
The swollen arm or leg is usually measured and compared to the other arm or leg. Measurements are taken over time to see how well treatment is working.
Measuring limb volume
In some cases, tests to calculate the volume of an affected limb may be carried out.
These may include:
- using a tape measure – to measure the circumference of the limb at certain intervals to calculate its volume
- water displacement – where the affected limb is placed in a tank of water and the amount of water that’s displaced is measured to calculate the volume of the limb
- perometry – where infrared light is used to measure the outline of an affected limb and calculate its volume
Bioimpedance testing
During a bioimpedance test, small metallic discs called electrodes are placed on different parts of your body.
The electrodes release a small, painless electric charge that’s measured using a handheld device. Changes in the strength of the current can indicate the presence of fluid in your tissue.
Lymphedema treatment
There’s no cure for lymphedema. The goal of treatment is to control the swelling, the pain and other problems caused by lymphedema. Damage to the lymph system cannot be repaired. Treatment is given to control the swelling caused by lymphedema and keep other problems from developing or getting worse. Physical (non-drug) therapies are the standard treatment. Treatment may be a combination of several of the physical methods. The goal of these treatments is to help patients continue with activities of daily living, to decrease pain, and to improve the ability to move and use the limb (arm or leg) with lymphedema. Drugs are not usually used for long-term treatment of lymphedema.
In cases of severe lymphedema, your doctor may consider surgery to remove excess tissue in your arm or leg to reduce swelling. There are also newer techniques for surgery that might be appropriate, such as lymphatic to venous anastomosis or lymph node transplants.
Lymphedema treatments include:
Lymphedema therapy
Lymphedema exercises
Studies have shown that carefully controlled exercise is safe for patients with lymphedema.
Light exercises in which you move your affected limb may encourage lymph fluid drainage and help prepare you for everyday tasks, such as carrying groceries. Exercises shouldn’t be strenuous or tire you but should focus on gentle contraction of the muscles in your arm or leg. A certified lymphedema therapist can teach you exercises that may help.
To find a certified lymphedema therapist contact:
- Lymphology Association of North America (https://www.clt-lana.org/)
- National Lymphedema Network (https://www.lymphnet.org/)
Exercise does not increase the chance that lymphedema will develop in patients who are at risk for lymphedema. In the past, these patients were advised to avoid exercising the affected limb. Studies have now shown that slow, carefully controlled exercise is safe and may even help keep lymphedema from developing. Studies have also shown that, in breast-cancer survivors, upper-body exercise does not increase the risk that lymphedema will develop.
Both light exercise and aerobic exercise (physical activity that causes the heart and lungs to work harder) help the lymph vessels move lymph out of the affected limb and decrease swelling.
- Talk with a certified lymphedema therapist before beginning exercise.
Patients who have lymphedema or who are at risk for lymphedema should talk with a certified lymphedema therapist before beginning an exercise routine.
Wear a pressure garment if lymphedema has developed.
Patients who have lymphedema should wear a well-fitting pressure garment during all exercise that uses the affected limb or body part.
When it is not known for sure if a woman has lymphedema, upper-body exercise without a garment may be more helpful than no exercise at all. Patients who do not have lymphedema do not need to wear a pressure garment during exercise.
Figure 8. Lymphedema compression garment
Breast cancer survivors should begin with light upper-body exercise and increase it slowly.
Some studies with breast cancer survivors show that upper-body exercise is safe in women who have lymphedema or who are at risk for lymphedema. Weight-lifting that is slowly increased may keep lymphedema from getting worse. Exercise should start at a very low level, increase slowly over time, and be overseen by the lymphedema therapist. If exercise is stopped for a week or longer, it should be started again at a low level and increased slowly.
If symptoms (such as swelling or heaviness in the limb) change or increase for a week or longer, talk with the lymphedema therapist. It is likely that exercising at a low level and slowly increasing it again over time is better for the affected limb than stopping the exercise completely.
More studies are needed to find out if weight-lifting is safe for cancer survivors with lymphedema in the legs.
Wrapping your arm or leg
Once the lymph fluid is moved out of a swollen limb, bandaging (wrapping) can help prevent the area from refilling with fluid. Bandages also increase the ability of the lymph vessels to move lymph fluid to flow back toward the trunk of your body. Lymphedema that has not improved with other treatments is sometimes helped with bandaging.
The bandage should be tightest around your fingers or toes and loosen as it moves up your arm or leg. A lymphedema therapist can show you how to wrap your limb.
Compression garments
Pressure garments are made of fabric that puts a controlled amount of pressure on different parts of the arm or leg to help move fluid and keep it from building up. Some patients may need to have these garments custom-made for a correct fit. Wearing a pressure garment during exercise may help prevent more swelling in an affected limb. It is important to use pressure garments during air travel, because lymphedema can become worse at high altitudes. Pressure garments are also called compression sleeves and lymphedema sleeves or stockings.
Long sleeves or stockings made to compress your arm or leg encourage the flow of the lymph fluid out of your affected limb. Wear a compression garment when exercising the affected limb.
Obtain a correct fit for your compression garment by getting professional help. Ask your doctor where you can buy compression garments in your community. Some people will require custom-made compression garments.
If you have difficulties putting on or taking off the compression garment, there are special techniques and aids to help with this; your lymphedema therapist can review options with you. In addition, if compression garments or compression wraps or both are not an option, sometimes a compression device with fabric fasteners can work for you.
About Compression Garments
In recent years, compression has become popular in athletics, especially in endurance sports. As you shop for garments, make sure you’re looking for those created specifically for lymphedema. Sports garments are designed differently and, if used improperly, could cause harm. If you’re unsure what kind of garment you need, talk with your healthcare team or a lymphedema specialist.
Finding the right garment for you may seem daunting but your providers will be able to help.
Here is more information to help you make an informed decision.
Custom and ready made garments
- Depending on your body and needs, you may be able to buy a pre-made garment online or in a store. Pre-made garments are for people of average proportions, and they are designed much like clothes you buy off-the-rack at department stores. These garments are available in different levels of
pressure, based on the size of the body part they are worn on. - If your limb doesn’t have average proportions — for example, if your wrist is small compared to the rest of your arm — you may have a hard time finding a garment that applies the right amount of pressure to your whole body part. In this case, you may want to consider a garment specially designed to fit you.
Fabric knit
- Compression sleeves come in one of two knits: circular and flat. In circular-knit, the sleeve was continuously knit in a circle pattern so that there is no seam. Flat-knit sleeves are knitted as a sheet that was then sewn into a tube, leaving a seam.
- Flat- and circular-knit sleeves offer you the same benefit, so it is up to you to choose which you prefer. Flat-knit fabric tends to be stiffer
and thicker than circular-knit, but no research has shown one knit is better than the other.
Lymphedema massage
Massage: Two basic types of massage are used to treat lymphedema.
- Manual lymphatic drainage is a precise and gentle form of massage that helps mobilize the fluid out of your arm or leg and direct it to other pathways. In this type of massage, the soft tissues of the body are lightly rubbed, tapped, and stroked. It is a very light touch, almost like a brushing.
- Soft tissue mobilization is a type of massage used to release scar tissue and other tightness that might be contributing to the swelling. Sometimes massage is taught to patients or family members to carry out at home.
Various massage treatments may benefit people with active cancer. Be sure to work with someone specially trained in these techniques. When done correctly, massage therapy does not cause medical problems.
Your lymphoedema therapist will also teach you a range of simpler massage techniques that you or your carer can use during the maintenance phase of treatment to help keep the swelling down. These self-massage techniques are known as simple lymphatic drainage.
Massage isn’t for everyone.
Massage should NOT be done on any of the following:
- Open wounds, bruises, or areas of broken skin.
- Tumors that can be seen on the skin surface.
- Active disease in the involved lymph drainage areas
- Areas with deep vein thrombosis (blood clot in a vein).
- Sensitive soft tissue where the skin was treated with radiation therapy.
Complete decongestive therapy
Complete decongestive therapy also called combined physical therapy, is a program of lifestyle changes, massage, bandaging, exercises, and skin care managed by a trained therapist. Complete decongestive therapy is an intensive phase of therapy, during which you may receive daily treatment for several weeks to help reduce the volume of the affected body part. This is followed by a second phase called the maintenance phase. You’ll be encouraged to take over your care using simple self-massage techniques, wearing compression garments, and continuing to exercise.
Four components to complete decongestive therapy:
- compression bandages – to complement exercise by moving fluid out of the affected limb and minimise further build-up
- skin care – to keep the skin in good condition and reduce the chances of infection
- exercises – to use muscles in the affected limb to improve lymph drainage
- specialised massage techniques – known as manual lymphatic drainage; this stimulates the flow of fluid in the lymphatic system and reduces swelling
At the beginning of the program, the therapist gives many treatments over a short time to decrease most of the swelling in the limb with lymphedema. Then the patient continues the program at home to keep the swelling down.
Generally, complete decongestive therapy isn’t recommended for people who have high blood pressure, diabetes, paralysis, heart failure, blood clots or acute infections.
Pneumatic compression
A sleeve worn over your affected arm or leg connects to a pump that intermittently inflates the sleeve, putting pressure on your limb and moving lymph fluid away from your fingers or toes. Compression devices may be helpful when added to complete decongestive therapy. The use of these devices should be supervised by a trained professional because too much pressure can damage lymph vessels near the surface of the skin.
Weight loss
In patients who are overweight, lymphedema related to breast cancer may improve with weight loss.
Laser therapy
Laser therapy may help decrease lymphedema swelling and skin hardness after a mastectomy. A hand-held, battery-powered device is used to aim low-level laser beams at the area with lymphedema.
Drug therapy
Lymphedema is not usually treated with drugs. Antibiotics may be used to treat and prevent infections. Other types of drugs, such as diuretics or anticoagulants (blood thinners), are usually not helpful and may make the lymphedema worse.
Coping and support
It can be frustrating to know there’s no cure for lymphedema. However, you can control some aspects of lymphedema. To help you cope, try to:
- Find out all you can about lymphedema. Knowing what lymphedema is and what causes it can help you communicate with your doctor or physical therapist.
- Take care of your affected limb. Do your best to prevent complications in your arm or leg. Clean your skin daily, looking over every inch of your affected limb for signs of trouble, such as cracks and cuts. Apply lotion to prevent dry skin.
- Take care of your whole body. Exercise daily, if you can. Reduce stress. Try to get enough sleep. Taking care of your body gives you more energy and encourages healing.
- Get support from others with lymphedema. Whether you attend support group meetings in your community or participate in online message boards and chat rooms, it helps to talk to people who understand what you’re going through. Contact the National Lymphedema Network (https://www.lymphnet.org/) to find support groups in your area. The organization can also put you in touch with other people with lymphedema.
Lymphedema diet
Eat a diet rich in fruits and vegetables.
- Vegetables and fruits are an important part of a healthy diet, and variety is as important as quantity.
- No single fruit or vegetable provides all of the nutrients you need to be healthy. Eat plenty everyday.
A diet rich in vegetables and fruits can lower blood pressure, reduce risk of heart disease and stroke, prevent some types of cancer, lower risk of eye and digestive problems, and have a positive effect upon blood sugar which can help keep appetite in check.
Eat a variety of types and colors of produce in order to give your body the mix of nutrients it needs. Try dark leafy greens; brightly colored red, yellow and orange vegetables and fruits; and cooked tomatoes.
Eat more vegetables and fruits each day
- Keep fruit where you can see it. That way you’ll be more likely to eat it.
- Explore the produce aisle and choose something new. Variety is the key to a healthy diet.
- Skip the potatoes. Choose other vegetables that are packed with more nutrients and more slowly digested carbohydrates.
- Make it a meal. Try cooking new recipes that include more vegetables. Salads and stir fries are two ideas for getting tasty vegetables on your plate.
The main message of the healthy eating is to focus on diet quality.
- The type of carbohydrate in the diet is more important than the amount of carbohydrate in the diet, because some sources of carbohydrate—like vegetables (other than potatoes), fruits, whole grains, and beans—are healthier than others.
- Healthy Eating also advises you to avoid sugary beverages, a major source of calories—usually with little nutritional value—in the American diet.
- Healthy Eating encourages you to use healthy oils, and it does not set a maximum on the percentage of calories people should get each day from healthy sources of fat.
Make most of your meal vegetables and fruits – ½ of your plate:
Aim for color and variety, and remember that potatoes don’t count as vegetables on the Healthy Eating Plate because of their negative impact on blood sugar.
Go for whole grains – ¼ of your plate:
Whole and intact grains—whole wheat, barley, wheat berries, quinoa, oats, brown rice, and foods made with them, such as whole wheat pasta—have a milder effect on blood sugar and insulin than white bread, white rice, and other refined grains.
Protein power – ¼ of your plate:
Fish, chicken, beans, and nuts are all healthy, versatile protein sources—they can be mixed into salads, and pair well with vegetables on a plate. Limit red meat, and avoid processed meats such as bacon and sausage.
Healthy plant oils – in moderation:
Choose healthy vegetable oils like olive, canola, soy, corn, sunflower, peanut, and others, and avoid partially hydrogenated oils, which contain unhealthy trans fats. Remember that low-fat does not mean “healthy.”
Drink water, coffee, or tea:
Skip sugary drinks, limit milk and dairy products to one to two servings per day, and limit juice to a small glass per day.
Stay active:
A reminder that staying active is also important in healthy.
Lymphedema surgery
If these therapies aren’t effective, surgery may help reduce the symptoms and swelling of lymphedema.
These procedures improve drainage of the lymph fluid, lessening the effects of lymphedema and keeping it from getting worse.
Patients who have less severe lymphedema for a shorter time tend to have better results from surgery. In some cases, patients may be able to stop using compression garments completely. All lymphedema surgeries are effective in reducing the number of infections you may have.
While these surgeries may result in significant improvement of lymphedema, you should continue all therapies and treatments unless your doctor or rehabilitation specialist tells you otherwise. This includes compression, massage, skin care and exercise.
Your surgeon will review your medical history, physical examination findings, and test results to determine the best procedure for you. Lymphedema surgical procedures include:
- Lymphovenous bypass: This is a minimally invasive procedure using a high-powered microscope, specialized instruments and sutures. Blocked lymphatic vessels less than half a millimeter in size are redirected to small veins. This improves the flow of lymphatic fluid out of the arm or leg and reduces the discomfort and swelling.
- Vascularized lymph node transfer: The doctor removes lymph nodes from your trunk, neck, groin area, or from within the abdomen, preserving their delicate blood supply. These are reattached to blood vessels in the affected arm or leg using microsurgery. The lymph nodes continue to function normally and drain fluid from the arm or leg. If you have undergone a mastectomy, it may be possible to combine this procedure with breast reconstruction to treat your lymphedema. Tests are performed to reduce the risk of lymphedema if the lymph nodes are taken from near an extremity.
- Liposuction debulking procedure: In chronic lymphedema, surgery to improve the fluid drainage may not be possible. Excess tissue that has grown due to the fluid can be removed with surgery. This is done using liposuction with minimal scarring. The appearance and function of the arm or leg are improved. The risk of future infections is reduced. The swelling will not return if compression garments are worn lifelong.
Liposuction
The accumulation of fat is a significant feature of lymphoedema swelling. Liposuction is where a thin tube is inserted through small cuts (incisions) in the skin to suck fat out of tissue.
It can be used to remove excess fat from an affected limb to help reduce its size.
After surgery, you’ll have to wear a compression garment on the affected limb day and night for at least a year to help keep the swelling down.
When lymphedema is severe and does not get better with treatment, other problems may be the cause.
Sometimes severe lymphedema does not get better with treatment or it develops several years after surgery. If there is no known reason, doctors will try to find out if the problem is something other than the original cancer or cancer treatment, such as another tumor.
Lymphangiosarcoma is a rare, fast-growing cancer of the lymph vessels. It is a problem that occurs in some breast cancer patients and appears an average of 10 years after a mastectomy. Lymphangiosarcoma begins as purple lesions on the skin, which may be flat or raised. A CT scan or MRI is used to check for lymphangiosarcoma. Lymphangiosarcoma usually cannot be cured.
Lymphedema Self-care
After intensive treatment reduces swelling, you must continue complete decongestive therapy at home. The therapist will make sure you get a garment that fits you properly. Your therapist will also teach you or a caregiver how to:
- do lymphatic decongestion or massage wrap bandages
- wear and care for compression garments
- exercise
- take care of your skin and use risk-reduction tips
Self-care may feel like a burden, but you must do it to keep lymphedema in check.
Depending on the severity of your condition, you may not need to bandage regularly at home. You may find a small amount of swelling acceptable if you do not have to bandage daily. Some bandage or wear a compression garment only at night.
Your therapist may advise you to wear a garment all day. There are different garment types, with varying amounts of pressure. With help from your therapist, make sure yours is not tight and does not irritate your skin. A too-snug garment can make lymphedema worse. As treatment reduces swelling, you will need to change size. If you have arthritis, zippered garments can help with taking the sleeve on and off.
Self-care includes the lymphatic exercises from intensive treatment, but now you may also be able to add aerobic, resistance and stretching activities. Wear a compression garment or bandages for all exercise. Swimming is great for lymphedema. The water supports your body and helps prevent injury, while the water pressure provides a gentle decongestion. Walking and bike riding are other good choices.
Some women find yoga helpful. You also might enjoy therapeutic movement programs in a class or at home on a DVD.
Begin exercise in small doses, at a slow pace. Pushing too hard can trigger or worsen lymphedema. Lifting weights is fine if you start with light loads and increase
weight gradually. Do not overuse your arms or rush to get to a higher exercise level. If your arm begins to feel tired, stop exercising. If, during or after exercise, you notice pain or odd feelings in the arm on your treated side, you may want to exercise less intensely.
Weight loss can be part of self-care. If you are overweight and drop pounds after developing lymphedema, it can lessen the swelling. Eating a balanced, low-salt
diet may help. Always talk with your healthcare team before starting any exercise or weight loss program.