Contents
- What is Lazy Eye?
- Table 1. Risk Factors for Amblyopia
- How can I tell if my child has amblyopia?
- Can amblyopia be prevented or avoided?
- Why is early treatment for amblyopia important?
- Can my child grow out of amblyopia?
- When should amblyopia be treated?
- How old is TOO old for amblyopia treatment?
- Can amblyopia be treated in adults?
- What happens if amblyopia is not treated?
- How can you get early treatment for amblyopia?
- What happens if amblyopia treatment does not work?
- Can surgery be performed to treat amblyopia?
- Amblyopia types
- Table 2. Major Types of Lazy Eye (Amblyopia) and Identifying Characteristics
- Lazy eye causes
- Risk factors for developing lazy eye
- Lazy Eye Pathophysiology
- Lazy eye signs and symptoms
- Lazy eye Complications
- Lazy eye diagnosis
- Lazy eye treatment
- How is lazy eye treated in children?
- Eye Patching
- How to choose and use an eye patch
- What kind of eye patch should be used?
- Should glasses be worn during eye patching?
- What if the eye patch adhesive causes skin irritations?
- During which activities should patching be performed?
- Should patching be performed during school hours?
- What if my child refuses to wear the patch?
- What can be done to encourage better eye patching?
- How long does amblyopia eye patching therapy take to work?
- Atropine eye drops
- Bangerter filter
- Glasses or contact lenses
- Newer treatments
- Lazy eye surgery
- Lazy eye exercises
- Living with lazy eye
- Lazy eye prognosis
What is Lazy Eye?
Lazy eye also known as amblyopia is the medical term used when the vision in one eye (common) or both eyes (less common) is reduced because the eye fails to work properly with the brain 1, 2, 3, 4, 5, 6, 7, 8, 9. Amblyopia is when vision in one or both eyes does not develop properly during childhood. The eye itself looks normal, but for various reasons the brain favors the other eye. If a child has amblyopia, one of their eyes has blurry vision and the other has clear vision. Their brain starts ignoring their blurry eye and only uses the eye with clear vision to see. As their brain relies more on their stronger eye, their weaker eye’s vision becomes even worse over time. Amblyopia is a neurodevelopmental disorder that arises from abnormal processing of visual images that leads to a functional reduction of visual acuity and its associated risk factors 10, 9. Over time, the brain relies more and more on the other, stronger eye — while vision in the weaker eye gets worse. It’s called “lazy eye” because the stronger eye works better. But people with amblyopia are not lazy, and they can’t control the way their eyes work.
Historically, various forms of amblyopia have been reported to affect 1% to 5% of the population, with a 1.2% lifetime risk of vision loss attributed to amblyopia 11, 12, 13. Amblyopia is a common problem in babies and young children, accounting for over three-quarters of attendance in children’s eye clinics 14. Unless it is successfully treated in early childhood amblyopia usually persists into adulthood, and is the most common cause of permanent one-eye vision impairment among children and young and middle-aged adults 15, 3, 16. However, more recent data suggest that the global prevalence of amblyopia falls within the range of 1.1% to 1.8% of the population 17, 18, 19. Population-based studies have reported varying prevalence rates, with estimates ranging from 0.7% to 2.6% among children aged 30 to 70 months and 1.0% to 5.5% in older children 20.
A number of eye diseases can contribute to the development of amblyopia. Amblyopia can result from any condition that prevents the eye from focusing clearly. Sometimes this causes the weaker (“lazy”) eye to wander outward, inward, upward or downward. When an eye wanders causing misalignment of the two eyes, that condition is called strabismus. With strabismus, the eyes can cross in (esotropia) or turn out (exotropia). Amblyopia and strabismus are commonly confused. When most people think of “lazy eye” they are actually thinking of wandering or misaligned eyes, which is strabismus. “Lazy eye” is amblyopia — poor vision in one or both eyes. This poor vision (amblyopia) can lead to eye misalignment (strabismus). Strabismus is more commonly referred to as crossed eyes, wandering eyes, or drifting eyes. If for some reason one eye of a child has decreased vision, the brain will not use that eye and it becomes lazy (reduced vision) from lack of use. That is amblyopia — the eye is lazy from lack of use. If one eye happens to be looking somewhere other than the other eye, that is strabismus. Lazy eyes with amblyopia just do not see well, it DOES NOT mean they wander or drift 21.
Occasionally, amblyopia can be caused by a clouding of the front part of the eye stopping your child from seeing, a condition called cataract.
The 3 most common eye conditions that can lead to amblyopia are:
- Refractive errors. These include common vision problems like nearsightedness (having trouble seeing far away), farsightedness (having trouble seeing things up close), and astigmatism. Normally, these problems are easy to fix with glasses or contacts. But if they’re not treated, the brain may start to rely more on the eye with stronger vision.
- Farsightedness (having trouble seeing things up close), or hyperopia, occurs when the distance from the front to the back of the eye is too short. Eyes that are farsighted tend to focus better at a distance but have more difficulty focusing on near objects.
- Nearsightedness (having trouble seeing far away), or myopia, occurs when the eye is too long from front to back. Eyes with nearsightedness tend to focus better on near objects.
- Eyes with astigmatism have difficulty focusing on far and near objects because of their irregular shape. Astigmatism is a common eye condition where the cornea or sometimes the lens doesn’t have a perfectly round, spherical shape, leading to blurry or distorted vision at all distances. This irregular shape causes light rays to focus at multiple points on the retina instead of a single point, resulting in a fuzzy or wavy image.
- Strabismus. Usually, the eyes move together as a pair. But in kids with strabismus, the eyes don’t line up. One eye might drift in, out, up, or down.
- Cataract. This causes cloudiness in the lens of the eye, making things look blurry. While most cataracts happen in older people, babies and children can also develop cataracts.
Symptoms of amblyopia can be hard to notice. Most kids aren’t diagnosed with amblyopia until a doctor or eye care specialist gives them an eye exam. Children with amblyopia may have poor depth perception — they have trouble telling how near or far something is.
A child with amblyopia may:
- Bump into objects (especially on one side of their body).
- Favor one side of their body.
- Shut one eye.
- Squint a lot.
- Frequently tilt their head to one side.
- Rubbing one eye (not just when tired)
- Have crossed eyes (strabismus).
- Holding items close to the eyes to see them.
- Have a droopy eyelid.
In many cases, parents don’t know their child has amblyopia until a doctor diagnoses it during an eye exam. That’s why it’s important for all children to get a vision screening at least once between ages 3 and 5. Early vision screening by a pediatrician, family doctor or an ophthalmologist is important in detecting children with amblyopia as young as possible. Children who grow up without treatment may have lifelong vision problems. Amblyopia treatment is usually less effective in adults than in children.
In 2016, the American Academy of Pediatrics, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Certified Orthoptists, and American Academy of Ophthalmology released a joint clinical report recommending routine preschool vision screening 22. The joint report recommends vision assessment in children aged 6 months to 3 years with physical examination (e.g., external inspection, the fixation and follow test, the red reflex test, and pupil examination). Instrument-based vision screening with autorefractors or photoscreeners may be used, when available, in children aged 1 to 3 years. Visual acuity screening may be attempted at age 3 years using HOTV or Lea Symbols charts; children aged 4 to 5 years should have visual acuity assessed using HOTV or Lea Symbols charts, the cover-uncover test, and the red reflex test 23, 22.
The American Academy of Family Physicians recommends vision screening in all children at least once between the ages of 3 and 5 years to detect amblyopia or its risk factors; it concluded that the current evidence is insufficient to assess the balance of benefits and harms of vision screening in children younger than 3 years 24.
The American Optometric Association recommends initial vision screening in infants at birth. Regular comprehensive eye examinations should occur at age 6 months, age 3 years, and prior to entry into first grade; eye examinations should then occur at 2-year intervals unless children are considered at high risk for vision abnormalities 25.
The U.S. Preventive Services Task Force 26 makes recommendations about the effectiveness of specific preventive care services for patients without obvious related signs or symptoms. It bases its recommendations on the evidence of both the benefits and harms of the service and an assessment of the balance. The U.S. Preventive Services Task Force recommended vision screening for amblyopia and its risk factors in all children aged 3 to 5 years. The U.S. Preventive Services Task Force concluded that the evidence was insufficient to assess the balance of benefits and harms of vision screening in children younger than 3 years 27.
Early recognition and treatment are important to prevent vision loss. Amblyopia treatment should be started as early as possible because 21:
- over time the amblyopic “lazy” eye could become permanently blind;
- depth perception (3-D vision) could be lost; and
- if the other, better-seeing, eye becomes diseased or injured, the amblyopic “lazy” eye cannot replace the loss in vision.
Amblyopia is treated by wearing a patch over the good eye for a while or using atropine eye drops in the good eye each day 28, 29, 30. In children with moderate amblyopia, patching for two hours per day is as effective as six hours, and daily atropine is as effective as daily patching. The patch and drops force your child to use the weak eye to see. Some children may need surgery. Your child’s eye doctor will help you decide what is best for your child. It is important to see the eye doctor regularly to check on your child’s vision, even after treatment, because amblyopia recurs in 25% of children, so continued surveillance is important.
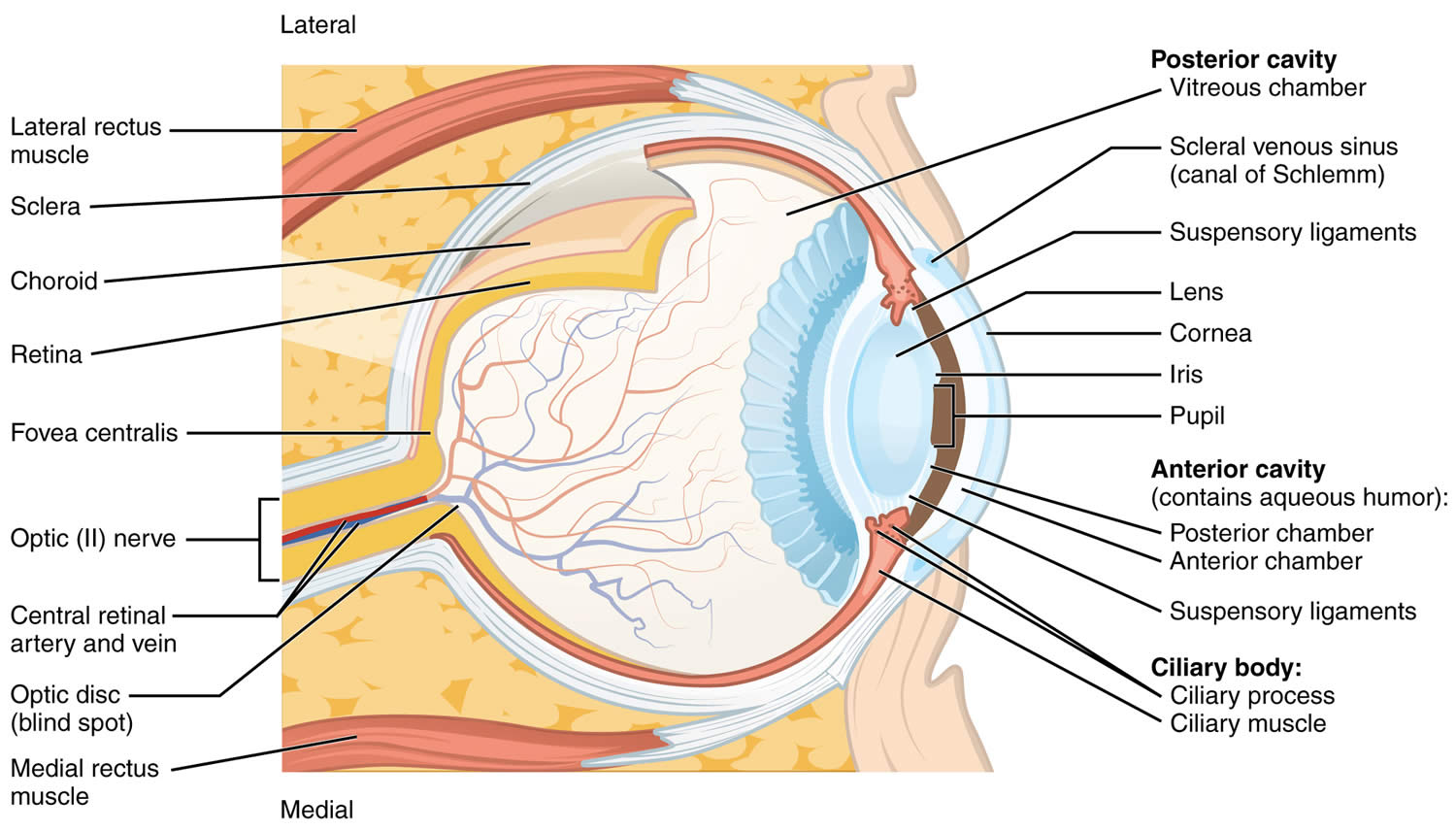
Figure 1. Eye anatomy
Figure 2. Amblyopia (Lazy Eye)
[Source 31 ]Table 1. Risk Factors for Amblyopia
| Risk Factor c | Age | ||
|---|---|---|---|
| 12 to 30 months | 31 to 48 months | >48 months | |
| Astigmatism, diopters | >2.0 D | >2.0 D | >1.5 D |
| Hyperopia, diopters | >4.5 D | >4.0 D | >3.5 D |
| Anisometropia, diopters | >2.5 D | >2.0 D | >1.5 D |
| Myopia, diopters | >-3.5 D | >-3.0 D | >-1.5 D |
| Manifest strabismus in primary position, prism diopters | >8 D | >8 D | >8 D |
| Media opacity, mm | >1 mm | >1 mm | >1 mm |
Footnotes:
a Adapted from Donahue et al.32
b Amblyopia is a neurodevelopmental disorder that arises from abnormal processing of visual images that leads to a functional reduction of visual acuity. It results from conditions that interfere with normal binocular vision. Specific conditions associated with amblyopia are anisometropia (a difference in refractive power between the eyes, in which one foveal image is more blurred than the other), strabismus (ocular misalignment, in which each eye does not have the same image on the fovea), and deprivation (caused by the blockage of the visual pathway, often attributable to cataracts, ptosis, or refractive error due tomyopia, hyperopia, and/or astigmatism) 33, 34, 35, 36, 37. Strabismic and anisometropic amblyopia can coexist. Strabismus can also inhibit development of normal binocular vision in the absence of amblyopia 38.
c Ptosis has been removed from the list because nearly all amblyopia-related ptosis occurs in the setting of superimposed anisometropia.32
How can I tell if my child has amblyopia?
Amblyopia can be tricky for parents or caregivers to spot because children don’t usually complain about blurry vision. Children will use the stronger eye that sees better and won’t notice that anything is wrong. Also, the weaker eye may look normal.
If you think your child has a problem with his or her eyes, see your doctor right away. Starting treatment early can help stop your child from losing his or her sight. You should tell your doctor if your child:
- Holds things close to his or her face to see them
- Squints or tilts his or her head to see things
- Has an eye that crosses or moves from one side to the other (drifts)
- Is unable to watch you as you walk across a room
If your child can’t see a close object or has trouble seeing the eye chart, your doctor must send your child to an eye doctor (ophthalmologist) for testing.
Can amblyopia be prevented or avoided?
Amblyopia cannot be prevented. But vision loss resulting from it can be avoided. Watch your child’s vision habits. If you have any concerns, bring your child to see an eye doctor (ophthalmologist). When amblyopia is caught and treated early, children should be able to keep most of their vision. If it is left untreated past the age of 10, they will probably have vision problems for the rest of their life. Early detection is the key to preventing vision loss. A vision check is especially important if there’s a family history of crossed eyes, childhood cataracts or other eye conditions.
For all children, a complete eye exam is recommended between ages 3 and 5.
Why is early treatment for amblyopia important?
The first years of life are the most important for eyesight development. During a child’s first 7 to 10 years, connections between the eye and brain are created. It is much more effective to treat amblyopia while those connections are still maturing. After your child’s vision system is fully developed, it is hard to change. If the amblyopia hasn’t been treated, they will most likely have poor vision for life. It won’t be possible to fix it with glasses, patching, or any other treatment.
One clinical trial showed that there could be benefits for treating children up to age 17. More research is needed on how treatment could help teenagers or adults.
Can my child grow out of amblyopia?
NO, amblyopia doesn’t go away on its own and children can’t grow out of it. If it’s not treated, amblyopia can cause permanent vision issues, including blindness in the affected eye. The best way to catch amblyopia early is with regular vision tests.
When should amblyopia be treated?
Amblyopia should be treated as early as possible because treatment works better in younger children 39. If necessary, children with refractive errors (nearsightedness, farsightedness or astigmatism) can wear glasses or contact lenses when they are as young as one week old. Children with cataracts or other “amblyogenic” conditions are usually treated promptly in order to minimize the development of amblyopia.
Recent studies by the National Institutes of Health found that starting treatment in younger teenagers up to age 14 years can still help vision, but not as much as starting treatment at younger ages. The key is to start treatment early for the best results.
How old is TOO old for amblyopia treatment?
A recent National Institutes of Health study confirmed that SOME improvement in vision can be attained with amblyopia therapy initiated in younger teenagers through age 14 years 39. The precise age at which amblyopia treatment becomes ineffective is not uniformly established 40. Nevertheless, The Pediatric Eye Disease Investigator Group has indicated that children aged 7 to 12 showed some degree of benefit from amblyopia treatment. In contrast, children 13 and older typically exhibit minimal improvement with treatment 41.
Can amblyopia be treated in adults?
Studies are very limited at this time, and scientists don’t know the success rate for treating amblyopia in adults. During the first seven to ten years of life, the visual system develops rapidly. Important connections between the eye and the brain are created during this period of growth and development. Scientists are exploring whether treatment for amblyopia in adults can improve vision.
Most textbooks do not recommend trying amblyopia therapy in the second decade of life but some improvement can be obtained in few cases. A study of amblyopia therapy in children aged 7-17 years found that amblyopia improves to some degree with optical correction alone in about one fourth of patients. However most required additional treatment for amblyopia 41. For patients aged 7 to 12 years, 2 to 6 hours per day of eye patching with near visual activities and atropine eye drops improved visual acuity even if the amblyopia had been previously treated. For patients 13 to 17 years, improvement was only noted in those children who had not been previously treated. The degree of improvement in these older children was much more modest than results from other studies of younger children, so the importance of early detection and treatment remains.
What happens if amblyopia is not treated?
If amblyopia is not treated the vision in the affected eye(s) will be permanently decreased causing deficits in depth perception and peripheral vision. Moreover if the good eye becomes injured or affected by a disease, significant lifetime disability may result.
The ophthalmologist will give the instructions and monitor the progress but the patient and the family will do the hard work of actually performing the treatment. Children do not like to have their good eye patched, especially if the vision in the amblyopic eye is very low, but parents must stand by them and help them do what’s best. Parents play probably the most important role in a successful treatment.
How can you get early treatment for amblyopia?
Some forms of amblyopia, such as that associated with large-deviation strabismus, may be easily detected by parents. Other types of amblyopia (from high refractive error) might cause a child to move very close to objects or squint his or her eyes. Still other forms of amblyopia may NOT be obvious to parents and therefore must be detected by Vision Screening.
What happens if amblyopia treatment does not work?
In some cases, treatment for amblyopia may not succeed in substantially improving vision. It is hard to decide to stop treatment, but sometimes it is best for both the child and the family. Children who have amblyopia in one eye and good vision only in their other eye can wear safety glasses and sports goggles to protect the normal eye from injury. As long as the good eye stays healthy, these children function normally in most aspects of society
In most cases loss of vision from amblyopia can be prevented or successfully treated if started early enough and if the degree of amblyopia is not extreme.
Can surgery be performed to treat amblyopia?
There is no surgery to improve the vision for amblyopia. Surgery can be performed to straighten misaligned eyes such as crossing. Surgery to make the eyes straight can only help enable the eyes to work together as a team. Children with strabismic amblyopia still need close monitoring and treatment for the amblyopia, and this treatment is usually performed before strabismus surgery is considered.
Children who are born with cataracts may need surgery to take out the cataracts. After surgery, the child will usually need vision correction with glasses or contact lenses and patching.
Amblyopia types
There are 3 main types of amblyopia classified by cause 42, 43:
- Refractive amblyopia – This is the most common type. It happens when a child needs glasses but doesn’t wear them early in life. The eyes that need glasses do not develop good vision even though they look normal.
- Strabismic amblyopia– This is caused by eye movement problems. One eye may turn in, out, up or down. When this happens, the brain begins to ignore, or “turns off” the wandering eye and does not learn to see well.
- Deprivational amblyopia – Rarely, problems like ptosis (a droopy eyelid), cataract (cloudy spot in the lens/focusing part of the eye) or cornea scar (cloudy spot in the clear front part of the eye) can stop a child from seeing. If not treated very early, these children never learn to see very well and can have very poor vision.
Table 2. Major Types of Lazy Eye (Amblyopia) and Identifying Characteristics
| Amblyopia type | Characteristics |
|---|---|
| Common | |
| Strabismic | Eye misalignment leads to visual cortex suppression |
| Anisometropic (refractive) | Difference in refraction (from prescription lenses) between eyes leads to the vision in the eye with a higher prescription being chronically blurred |
| Combined strabismic and refractive | Eye misalignment with refractive error leads to visual cortex suppression and chronic image blur |
| Less common | |
| Ametropic | Bilateral high, symmetric refractive error leads to chronic image blur in both eyes, and subsequent subnormal visual cortex development |
| Deprivation (rare) | Obstruction of visual axis leads to visual cortex suppression |
Refractive amblyopia
Refractive amblyopia also called anisometric amblyopia happens when there is a large or unequal amount of refractive error (glasses strength) between a child’s eyes 45. The brain learns how to see well from the eye that has less need for glasses and does NOT learn to see well from the eye that has a greater need for glasses. The vision problem may be invisible because the child does not complain of blurry vision. The child sees well with the better seeing eye. Additionally, the amblyopic eye may not look any different from the normal seeing eye. Therefore, parents and pediatricians may not think there is a problem because the child’s eyes look normal. For these reasons, this kind of amblyopia in children may not be found until the child has a vision test. Refractive amblyopia can affect one or both eyes and can be best helped if the problem is found early.
Refractive amblyopia results from blurred visual input caused by farsightedness (hyperopia), nearsightenedness (myopia) or astigmatism (a common eye condition where the cornea or sometimes the lens doesn’t have a perfectly round, spherical shape, leading to blurry or distorted vision at all distances, resulting in a fuzzy or wavy image), typically with a difference of refractive error exceeding 1 diopter (D) between the eyes 46. When the difference in refraction error between the eyes falls within the range of 1 diopter (1D) to 2 diopters (2D) of spherical equivalence, the odds of developing amblyopia are 4.5 times higher. This risk can escalate to a 40-fold increase when the difference in refraction error exceeds 2 diopters (2D) 47.
Generally, eyes with farsightedness (hyperopia) or astigmatism are more prone to developing amblyopia than nearsightenedness (myopia), as myopic eyes can still maintain a clear focus on nearby objects.
Anisometric amblyopia is a type of vision impairment occurring in 1 eye due to uncorrected and unequal refractive errors between the eyes, which results in a poorly focused image primarily affecting the weaker eye and can manifest with or without strabismus (“crossed eyes”) 48. Research has shown that the risk and severity of amblyopia are correlated with the degree of anisometropia (a condition where there’s a significant difference in the refractive error between the two eyes), refractive error magnitude, and astigmatism 49.
While bilateral refractive amblyopia is less common, it can occur when both eyes consistently receive blurred images on their retinas due to severe uncorrected refractive errors during development. The first-line treatment for individuals with bilateral refractive amblyopia involves a thorough assessment of best-corrected visual acuity (BCVA) and the prescription of corrected lenses to fully correct the underlying refractive errors 40.
Strabismic amblyopia
Strabismic amblyopia develops when both eyes are not straight. One eye may turn in, out, up or down. When this happens, the brain begins to ignore or “turns off” the eye that is not straight to prevent diplopia (double vision) and the vision subsequently drops in that eye 50. In these individuals, both retinas receive stimulation in noncorresponding areas, hindering the establishment of proper binocular vision and the fusion of images from both eyes. Consequently, the suppression of visual input primarily affects the amblyopic eye 51. Amblyopia risk has been reported to be between 3 and 18 times greater compared to individuals without strabismus 52.
In cases of amblyopia associated with strabismus, the tropia, or deviation of the eye from its normal position concerning the central line of vision, tends to be unequal and not alternating. Such conditions are usually observed in patients with esotropia (a type of strabismus where one or both eyes turn inward toward the nose).
Mixed and strabismic amblyopia is typically diagnosed at an earlier age, with an average age of 7.4 years, compared to refractive amblyopia (anisometropic amblyopia), which is usually diagnosed at an average age of 12.7 12. The prevalence of amblyopia appears to be similar between right and left eyes, and there is no observed gender preference.
While strabismus can be treated through methods like surgery or the use of prism glasses to realign the eyes, amblyopia can persist despite treating the underlying strabismus. This highlights the necessity of addressing amblyopia directly through appropriate therapies to restore visual function in the affected eye 40.
Deprivation Amblyopia
Deprivation amblyopia develops when cataracts or similar conditions obstructing the visual pathway, leading to partial or complete blockage and consequently causing blurred or degraded images to be projected onto the retina, “depriving” young children’s eyes of visual experience 46. Various factors, including early-onset or congenital cataracts, corneal opacity, intraocular inflammation of either noninfectious or infectious origin, vitreous hemorrhage, retina damage, optic nerve pathologies, or droopy eyelid (congenital ptosis) can contribute to this obstruction 53. Visual deprivation amblyopia can even result from the absence of visual stimuli, such as covering one eye or living in complete darkness.
If not treated very early, these children never learn to see very well and can have very poor vision. Sometimes deprivation amblyopia can affect both eyes.
Although deprivation amblyopia is the least common form of amblyopia, it tends to be the most severe and challenging form to treat 40. The prognosis for patients with deprivation amblyopia is usually more favorable when early intervention within the first 2 months of age is undertaken, particularly in cases involving the removal of cataracts or the cause of the optical opacity 54.
Occlusion or Reverse Amblyopia
Occlusion amblyopia is uncommon, resulting from prolonged visual deprivation in the healthy eye, often induced by pharmaceutical cycloplegia or therapeutic patching 55. Research has indicated that best-corrected visual acuity (BCVA) may decline by more than 2 lines following 6 months of daily eye patching for 6 hours daily or topical atropine in the non-amblyopic eye 56. This form of iatrogenic-induced amblyopia is quite rare 40.
Visual acuity typically returns to normal once atropine or patching is discontinued, and optimal refractive correction spectacles are used for the healthy eye 40. This underscores the importance of promptly monitoring and managing occlusion amblyopia to ensure the best visual outcomes 40.
The severity of resulting amblyopia tends to be more pronounced when the degree of visual deprivation is greater 40. The critical period for visual development is primarily concentrated within the first 7 years of life, with the initial few years and even months being particularly critical 57. Delaying the start of amblyopia treatment makes it increasingly challenging to achieve clinical reversal of the condition. Early-onset visual deprivation can lead to permanent anatomic alterations in the magnocellular (M) and parvocellular (P) visual pathways 40.
For this reason, surgical intervention may be necessary very early, often within a week of discovery, when dealing with dense congenital monocular cataracts 40. Even a few months of having a congenital cataract could potentially cause irreversible amblyopia 40. There is typically a bit more flexibility in cases of binocular cataracts with equal density, allowing for intervention within a few weeks 58, 59.
Lazy eye causes
Normal vision develops during the first few years of life. At birth all babies have very poor vision, however as they use their eyes the vision improves because the vision centers in the brain are developing. For good eyesight, both eyes need to provide the same clear, focused image. If infants are not able to use their eyes from various reasons the vision centers do not develop properly and the vision is decreased despite normal appearance of the structures of the eyes.
Amblyopia can result from any condition that prevents the eye from focusing clearly. The 3 most common conditions are:
- Strabismus also called “crossed eyes”. Amblyopia can be caused by the misalignment of the two eyes where the eyes don’t line up in the same direction—a condition called strabismus. With strabismus, the eyes can cross in (esotropia) or turn out (exotropia). Strabismus also called “crossed eyes” is the most common cause of amblyopia.
- Refractive error: This term refers to the inability of the eye to focus light on the retina. It is more likely to cause amblyopia if the error is greater in one eye. Amblyopia can occur when one eye is more nearsighted, more farsighted, or has more astigmatism.
- Farsightedness (having trouble seeing things up close), or hyperopia, occurs when the distance from the front to the back of the eye is too short. Eyes that are farsighted tend to focus better at a distance but have more difficulty focusing on near objects.
- Nearsightedness (having trouble seeing far away), or myopia, occurs when the eye is too long from front to back. Eyes with nearsightedness tend to focus better on near objects.
- Eyes with astigmatism have difficulty focusing on far and near objects because of their irregular shape. Astigmatism is a common eye condition where the cornea or sometimes the lens doesn’t have a perfectly round, spherical shape, leading to blurry or distorted vision at all distances. This irregular shape causes light rays to focus at multiple points on the retina instead of a single point, resulting in a fuzzy or wavy image.
- Cataracts – These cause clouding in the lens of the eye. Cataracts in children are uncommon. Cataracts may be unilateral or bilateral, may or may not have related signs (e.g., musculoskeletal or neurologic symptoms), may be progressive or nonprogressive, and can occur congenitally or develop during infancy. Most are idiopathic 60. Estimates of cataracts in children incidence are one to six per 10,000 live births. Up to one-third of cataracts are inherited, and they may be autosomal dominant, autosomal recessive, or X-linked 60. A family history of childhood cataracts necessitates an ophthalmologist’s evaluation 61. Examination may show dull, irregular, or absent red reflex, or white pupil (leukokoria).
Any condition that prevents the eye from focusing clearly can cause amblyopia.
The most common cause is refractive error in one or both eyes that is not corrected early in childhood resulting in poor development of the visual function in the affected eye(s). This is called refractive amblyopia 6.
Another common cause is strabismus or eye misalignment. This is called strabismic. Rarely there is a structural anomaly that impairs the visual function like a droopy eyelid or opacity in the visual axis like cataract or corneal scar. This is called deprivation amblyopia. However, multiple causative factors can coexist. These problems can cause your child to get a different picture from each eye. Your child’s brain naturally tries to fix this problem by blocking out the weaker picture. If the problem is not fixed when your child is young, your child’s brain will always ignore pictures from the weak eye. This causes amblyopia.
Some children have a higher risk of having amblyopia. These include children who:
- Were born prematurely.
- Were small at birth.
- Have a family history of amblyopia.
- Have developmental disabilities.
Strabismus
This is when the eyes point in two different directions. One eye may be focused straight ahead while the other turns in, out, up, or down. To avoid seeing double, the child’s brain may ignore the image from the eye that is not focused straight ahead. But this can keep that eye from developing properly.
Refractive errors
Having a refractive error means being nearsighted, farsighted, or having astigmatism (distorted or blurry vision). A child may have a refractive error that is worse in one eye. That eye can “turn off,” and vision will not develop properly. This can be difficult to tell since the child’s vision seems fine when using both eyes.
Cloudiness in the normally clear parts of the eye
Some children are born with a cataract, where the eye’s normally clear lens is cloudy. This can keep vision from developing properly in that eye.
Droopy eyelid (ptosis)
Ptosis or a droopy eyelid, can block vision in a child’s developing eye and lead to amblyopia.
Risk factors for developing lazy eye
Some children are born with amblyopia and others develop it later in childhood.
Several risk factors contribute to the development of amblyopia and these include 48, 62:
- Premature birth (gestational age less than 30 weeks)
- Low birth weight (less than 1500 g)
- Children born small for gestational age
- Have a family history of amblyopia, childhood cataracts, or other eye conditions
- Maternal smoking
- Alcohol or drug use during pregnancy
- Developmental delay
- Ptosis (droopy eyelid)
- Strabismus
- Childhood glaucoma
- Early-onset cataracts
- Uveitis: Uveitis is inflammation inside the eye specifically affecting the uvea, the middle layer of the eye wall, often caused by an autoimmune response or infection
- Craniofacial disorders
- Certain genetic conditions, such as Down syndrome (trisomy 21), 22q deletion syndrome, Williams syndrome and Noonan syndrome
- Systemic conditions with eye complication.
Lazy Eye Pathophysiology
Amblyopia is a neurodevelopmental condition that results in impaired best-corrected vision in one or both eyes 63. The development of visual acuity in the postnatal period relies on continuous exposure to high-quality visual stimuli by both eyes and the proper functioning of the visual pathways 40. Research has pinpointed a sensitive or critical period during which amblyopia can develop due to incomplete visual pathway development, with a susceptibility window extending to approximately 7 to 10 years of age 64. Any deviations from normal vision during the first decade of life caused by unilateral or bilateral blurred retinal images can lead to permanent vision loss if not promptly diagnosed and treated 65.
Disruptions along the normal visual pathways can arise from various factors, including anisometropia (a condition where there’s a significant difference in the refractive error between the two eyes), uncorrected refractive errors, strabismus, and ocular media opacities 66. Early recognition and intervention are crucial in addressing these underlying causes to prevent the potentially irreversible consequences of amblyopia.
In cases of monocular visual deprivation during the critical period of visual development, a competitive process unfolds between the neural networks of both eyes that are vying for influence over cortical neurons in the primary visual cortex. Various aspects of neuronal selectivity, such as synaptic plasticity, activity dependence, and neuronal network learning, exhibit distinct sensitive periods and are consequently affected in diverse ways by the types of vision deprivation experienced 40.
Research conducted using functional magnetic resonance imaging (fMRI) and optical coherence tomography (OCT) in individuals with amblyopia have revealed neuroanatomical structural and functional alterations in the gray matter volume of the corresponding visual cortex hemispheres 67, alteration in cortical thickness within several white matter volumes 68, variations in ciliary muscle thickness 69, changes in choroidal thickness 70, differences in retinal nerve fiber thickness 71, variations in central macular thickness 72, and modifications in other structures along the visual pathway 73. These findings highlight the extensive impact of amblyopia on both the structural and functional aspects of the visual system 40.
Amblyopia is influenced by the anatomical relationships between photoreceptors and ganglion cell receptor fields, the relationships between ganglion cell receptor fields and the layers within the lateral geniculate, and the connections between the lateral geniculate and the layers of the visual cortex 40. These intricate neural connections play a pivotal role in developing and manifesting amblyopia.
The depth and severity of amblyopia are closely tied to the age at which it begins and its untreated duration 40. In general, the earlier the onset of amblyopia and the longer it persists without intervention, the more challenging it becomes to correct and reduce its effects on your vision 74.
Lazy eye signs and symptoms
Amblyopia can be tricky for parents or caregivers to spot because children don’t usually complain about blurry vision. Children will use the stronger eye that sees better and won’t notice that anything is wrong. Also, the weaker eye may look normal. Many times, a problem will only be found with a vision test.
Amblyopia usually starts between birth and age 7. Symptoms in your child could include:
- Eyes that don’t work together
- One eye that wanders inward or outward
- Squinting, shutting one eye, or tilting the head to look at something
- Problems with depth perception
- An upper eyelid that droops
Sometimes symptoms are not noticeable except in an eye exam.
If you notice any of the above symptoms in your child, even when they are an infant, bring your child to see an eye doctor (ophthalmologist). Your child’s eye doctor (ophthalmologist) will do an eye exam. Your child’s eye doctor will ask about your child’s symptoms, family history, and risk factors.
Otherwise, children should have an initial eye checkup between the ages of 3 and 5.
Lazy eye Complications
The primary complication of amblyopia is an irreversible, lifelong reduction in vision 40. These functional visual abnormalities include diminished best-corrected visual acuity (BCVA), reduced contrast sensitivity, impaired vernier acuity, spatial distortion, abnormal spatial interactions, and compromised contour detection 40. Individuals with amblyopia typically exhibit binocular abnormalities, including poor stereoscopic acuity and abnormal binocular summation 40. While the monocular vision deficits are usually specific to the amblyopic eye, there have been instances of subclinical deficits observed in the nonamblyopic eye 40.
Individuals with amblyopia often encounter challenges when perceiving 3-dimensional (3D) images hidden in stereoscopic displays such as autostereograms. However, their perception of depth derived from monocular cues, such as variations in size, perspective, and motion parallax in the nonamblyopic eye, typically remains normal 40.
Children with amblyopia may experience impaired learning abilities and are found to read and respond to multiple-choice questions at a slower pace than children without amblyopia 75, 76. Another potential complication associated with amblyopia is the worsening of strabismus, which can occur due to impaired binocular fusion.
Lazy eye diagnosis
Your child might not be aware of having better vision in one eye than the other. And you may not realize it either unless your child has strabismus or other eye problem you can see 77. Early diagnosis of amblyopia is key to optimize the likelihood of successful treatment 78. Children younger than 7 years are more likely than older children to have a good response to treatment 79. Recommendations from the U.S. Preventive Services Task Force (USPSTF), supported by the American Academy of Family Physicians, suggest screening all children three to five years of age for amblyopia or its risk factors at least once 80. Children with an increased risk of amblyopia should be referred for an ophthalmologic examination as soon as a risk factor is identified. These include ptosis, gestational age less than 30 weeks, birth weight less than 1,500 g (3 lb, 5 oz), cerebral palsy, syndromes with ocular involvement (e.g., Down syndrome), and a family history of amblyopia or strabismus.
The American Academy of Pediatrics and the American Association for Pediatric Ophthalmology and Strabismus recommend starting vision screening in newborns 81, 82, 83. Because treatment is more likely to succeed if initiated at a younger age 84, it is crucial to make the diagnosis of amblyopia as early as possible. A meta-analysis of four randomized clinical trials evaluating the effect of age on response to amblyopia treatment concluded that children seven years and older were less responsive to treatment than children three to six years of age 85. There was also a trend of greater responsiveness in children three to younger than five years, compared with children five to younger than seven years with severe amblyopia. Although the U.S. Preventive Services Task Force recommends vision screening for all children at least once between three and five years of age, it found insufficient evidence that vision screening for children younger than three years leads to improved visual outcomes 86.
Screening for Lazy Eye
Amblyopia holds significant global prevalence and is the leading cause of unilateral visual loss in children 87. Early detection and timely treatment of this condition can prevent or decrease the severity of permanent visual impairments. Consequently, screening programs for amblyopia are frequently integrated into the public healthcare systems of many nations worldwide.
Guidelines and methods of screening children for amblyopia vary worldwide and even within countries due to social, political, and economic influences 88. Multiple national guidelines for amblyopia screening have been established, including the following:
- In the United States, most states do not have official screening programs for children, despite recommendations by various American Medical Associations 89. However, in some states, vision screening tests are mandatory for school-age children, typically from kindergarten to grade 12 90.
- In Canada, certain provinces have implemented amblyopia screening programs for children aged 3 to 5 years, while others, like Ontario and Quebec, do not endorse these national programs 91.
- Recent guidelines in France recommend ophthalmologic assessments in the first year of life for children with risk factors for amblyopia. A systematic orthoptic examination, which includes nonmydriatic refraction, best-corrected visual acuity (BCVA), and oculomotor testing, is recommended at 3 years of age with referral to an ophthalmologist in cases of suspected amblyopia 92.
- The National Screening Committee in the United Kingdom recommends orthoptist screening assessments for children aged 4 to 5 years 93.
- In Singapore, children aged 4 to 5 years attending kindergarten undergo their initial vision screening, which continues annually until age 14 94. Children with suspected amblyopia or those requiring spectacle correction are referred to ophthalmologists.
- South Korea has integrated nationwide toddler and infant aged 3-6 years screening programs into its national healthcare programs since 2008 95.
Table 3. Techniques for Pediatric Vision Screening
| Age | Tests | Referral Criteria Comments |
|---|---|---|
| Newborn to 12 months |
|
|
| 12 to 36 months |
|
|
| 36 months to 5 years |
|
|
| 5 years and older* *Repeat screening every 1-2 years after age 5. |
|
|
Clinical History
Children with a family history of strabismus or amblyopia have an increased risk of amblyopia. If a child has amblyopia, siblings should be observed for risk factors and undergo vision screening. If the child with amblyopia required glasses before two-and-a-half years of age, and did not have strabismus as a detectable risk factor, it is reasonable to refer a younger sibling for a comprehensive dilated eye examination.
Physicians should ask parents about torticollis (abnormal head posture), nystagmus, squinting of one eye, or strabismus. Torticollis, nystagmus, and squinting of one eye can all indicate strabismus. Torticollis with visual tasks may be a sign of strabismus, because the child may adopt a head position to better align his or her eyes. Torticollis is commonly associated with vertical strabismus, such as in congenital superior oblique palsy.
Children with nystagmus may adopt a head turn to find a visual area in which their nystagmus decreases (null zone), thus improving their vision. They may also demonstrate eye crossing while fixing on a near target as a result of converging their eyes to dampen the nystagmus. Any patient with strabismus is at risk of amblyopia, so a child with torticollis requires a comprehensive eye examination to rule out eye misalignment. Squinting of one eye, especially in bright light conditions, can be a sign of intermittent exotropia, or eye wandering.
The diagnosis of amblyopia is made when a child has decreased vision usually associated with an amblyogenic risk factor and without ocular structural abnormalities. It can also be diagnosed in a child after removal of a visual axis obstruction (i.e., cataract) with persistent reduced vision. The diagnosis of amblyopia is always determined with best-corrected vision.
Clinical Examination
Ophthalmologists diagnose amblyopia by checking to see if vision differs between the two eyes. To check a baby’s or young child’s vision, the ophthalmologist may cover one of the child’s eyes and watch how well they can follow a moving object. The doctor may also watch how the child reacts when one eye is covered. If one eye has amblyopia and the other is covered, the child may try to look above or below the patch, pull it off or cry.
The ophthalmologist will do a complete medical eye exam, looking for other eye problems that could be affecting vision.
Red reflex testing (Corneal Light Reflex)
In a corneal light reflex test, the child’s attention is attracted to a target (a light or a brightly colored object), while a light in front of the child is directed at the child’s eyes. The light’s reflection will be symmetric in each pupil by four to six months of age in patients with normally aligned eyes. A wide nasal bridge or epicanthal folds may give the appearance of eye deviation; however, on closer examination, the light reflection will be found to be symmetric. This is pseudostrabismus, a normal variant.
In infants and children, red reflex testing (in which a direct ophthalmoscope is used to compare the reflex in both eyes for asymmetry) is valuable in detecting risk factors for amblyopia, such as a cataract, refractive error, and retinal pathology. Any abnormal finding (e.g., asymmetry of color or occurrence of dark or white spots) is a reason for referral to an ophthalmologist 96, 97.
A common cause of an asymmetric red reflex is a refractive error in one or both eyes. This condition could lead to a serious outcome of amblyopia if left untreated 98.
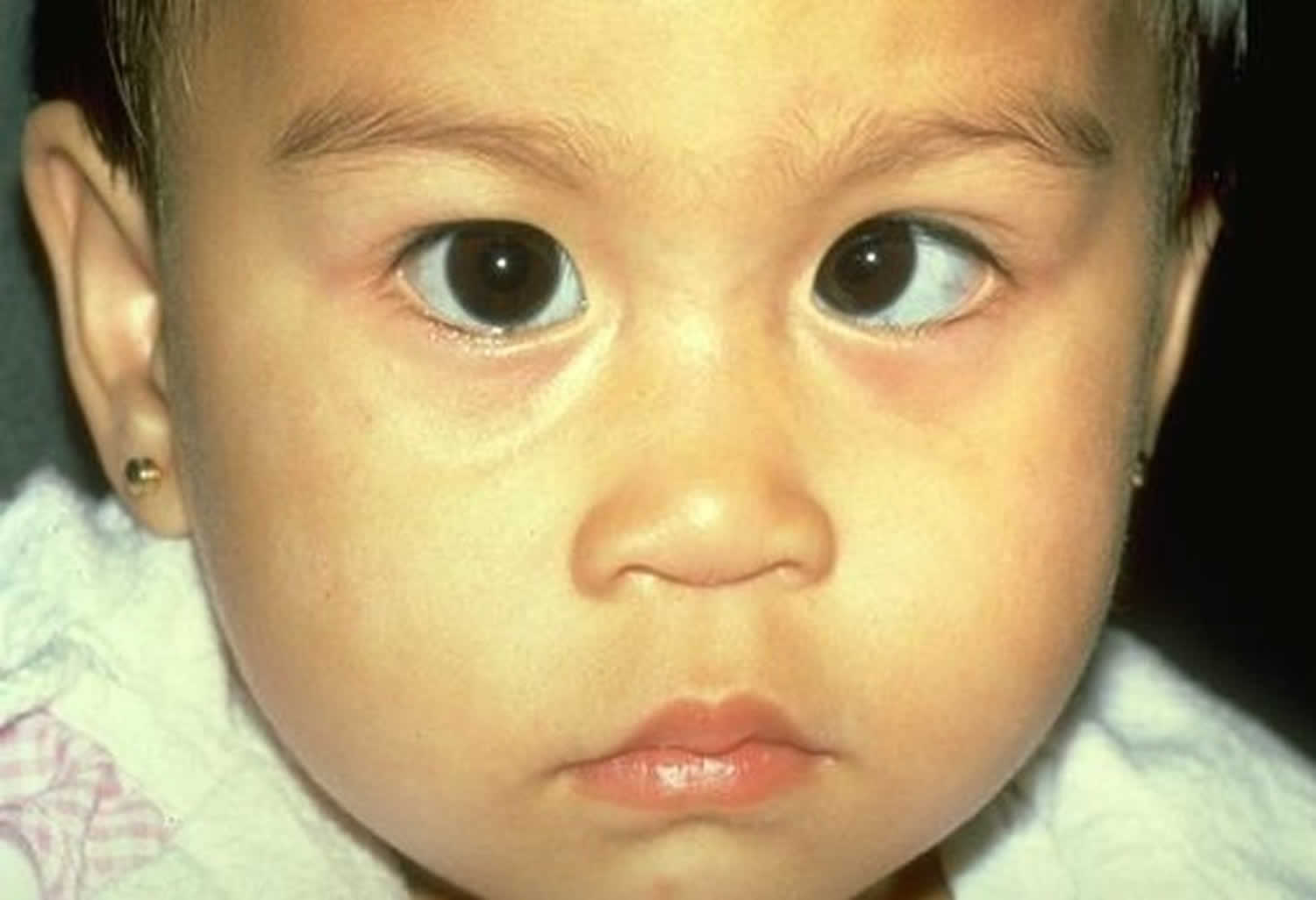
One of the concerning outcomes of an abnormal red reflex examination is the identification of a retinoblastoma. This neuroblastic tumor is the most common primary intraocular malignancy and the seventh most common malignancy of childhood, occurring in about one in 20,000 children 99, 100. Leukokoria or white pupil is the most common finding and is often discovered by a family member who does not realize its serious cause 99, 100. There are a multitude of alternate presenting signs for retinoblastoma, including strabismus, tearing, red eye, iris discoloration, corneal clouding, hyphema, and glaucoma. Retinoblastoma is fatal without treatment, although there is potential for a more than 90% cure rate with prompt recognition and management. Because preserving the eye and functional vision is related to the magnitude of the disease, any abnormal finding should lead to a prompt referral. Although less than 25% of patients with retinoblastoma have a family history of the disease, the presence of a family history necessitates a referral regardless of the physical examination findings 99, 100, 101.
Another potentially serious cause of an abnormal red reflex examination is a cataract. Cataracts may be unilateral or bilateral, may or may not have related signs (e.g., musculoskeletal or neurologic symptoms), may be progressive or nonprogressive, and can occur congenitally or develop during infancy. Most are idiopathic 60. Urgent referral for treatment is recommended because prognosis is improved with earlier intervention, although treatment varies depending on the density and location of the opacity 99, 100, 101.
Figure 3. Red Reflex
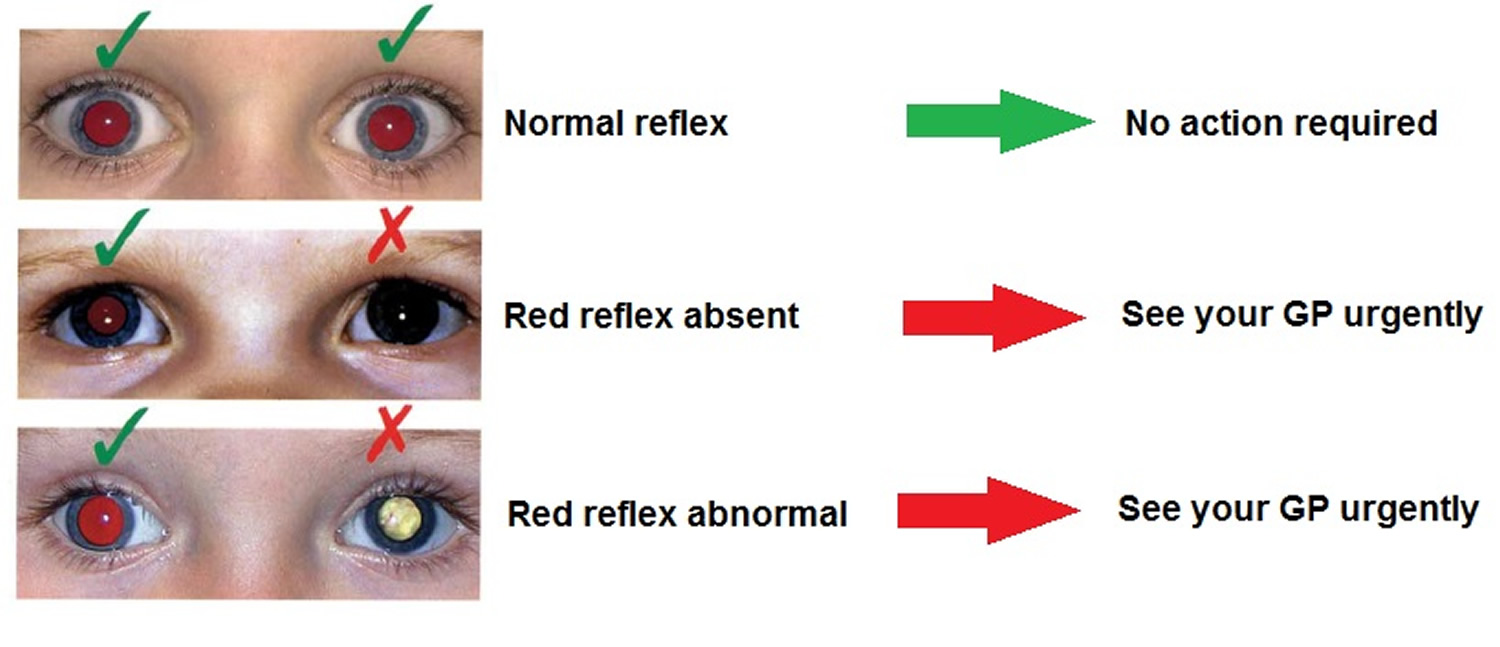 Footnotes: Red reflex examination. (A) Normal, symmetric red reflex. (B) Normal red reflex in the patient’s right eye, and abnormal, diminished red reflex in the patient’s left eye, which is most commonly caused by refractive error between the eyes but can also be caused by a more serious pathology (e.g., retinoblastoma). (C) Normal red reflex in the patient’s right eye and no reflex in the patient’s left eye, which occurs when the reflection is blocked by an opacity, such as a cataract.
Footnotes: Red reflex examination. (A) Normal, symmetric red reflex. (B) Normal red reflex in the patient’s right eye, and abnormal, diminished red reflex in the patient’s left eye, which is most commonly caused by refractive error between the eyes but can also be caused by a more serious pathology (e.g., retinoblastoma). (C) Normal red reflex in the patient’s right eye and no reflex in the patient’s left eye, which occurs when the reflection is blocked by an opacity, such as a cataract.Figure 4. Asymmetry in the red reflexes
Footnotes: Red reflex should be equal in both eyes when the red reflexes are viewed simultaneously. An abnormality is exposed if one reflex appears more prominent than the other, or if one reflex is of a different color or intensity, as in this patient.
[Source 102 ]Figure 5. Child with right esotropia (in-turning of right eye) resulting in right eye amblyopia

Note: Child with right esotropia demonstrated with asymmetric corneal light reflex. The patient has a left eye fixation preference and amblyopia of the right eye.
Figure 6. Child with vertical deviation strabismus

Note: This child has a dissociated vertical deviation strabismus in which one eye will periodically drift upward, while the other eye stays put. Surgery can be curative.
Cover and Cover-Uncover Test
Alignment is further screened with several tests using a cover over one eye. In the cover test, the child’s attention is attracted to a target. The vision of one eye is then occluded. The tested (uncovered) eye is observed for movement from a deviated position to one that fixes on the target (a sign of tropia, also called manifest strabismus). The untested eye is then uncovered and the tested eye is observed again for any drift out of alignment.
Fixation preference of one eye can signify amblyopia. In infants and children up to two-and-a-half years of age, using a toy or other near fixation target to hold the child’s attention, one eye is occluded with an occluder or adhesive patch, and fixation behavior is observed. When the other eye is then occluded, a similar fixation behavior is expected. If a child consistently appears uncooperative when patching one eye, amblyopia is suspected. In children with straight eyes, fixation preference can be determined by using a prism over one eye to induce separate visual images (induced tropia test). In a child with strabismus, fixation preference is often easily determined in the nondeviating eye.
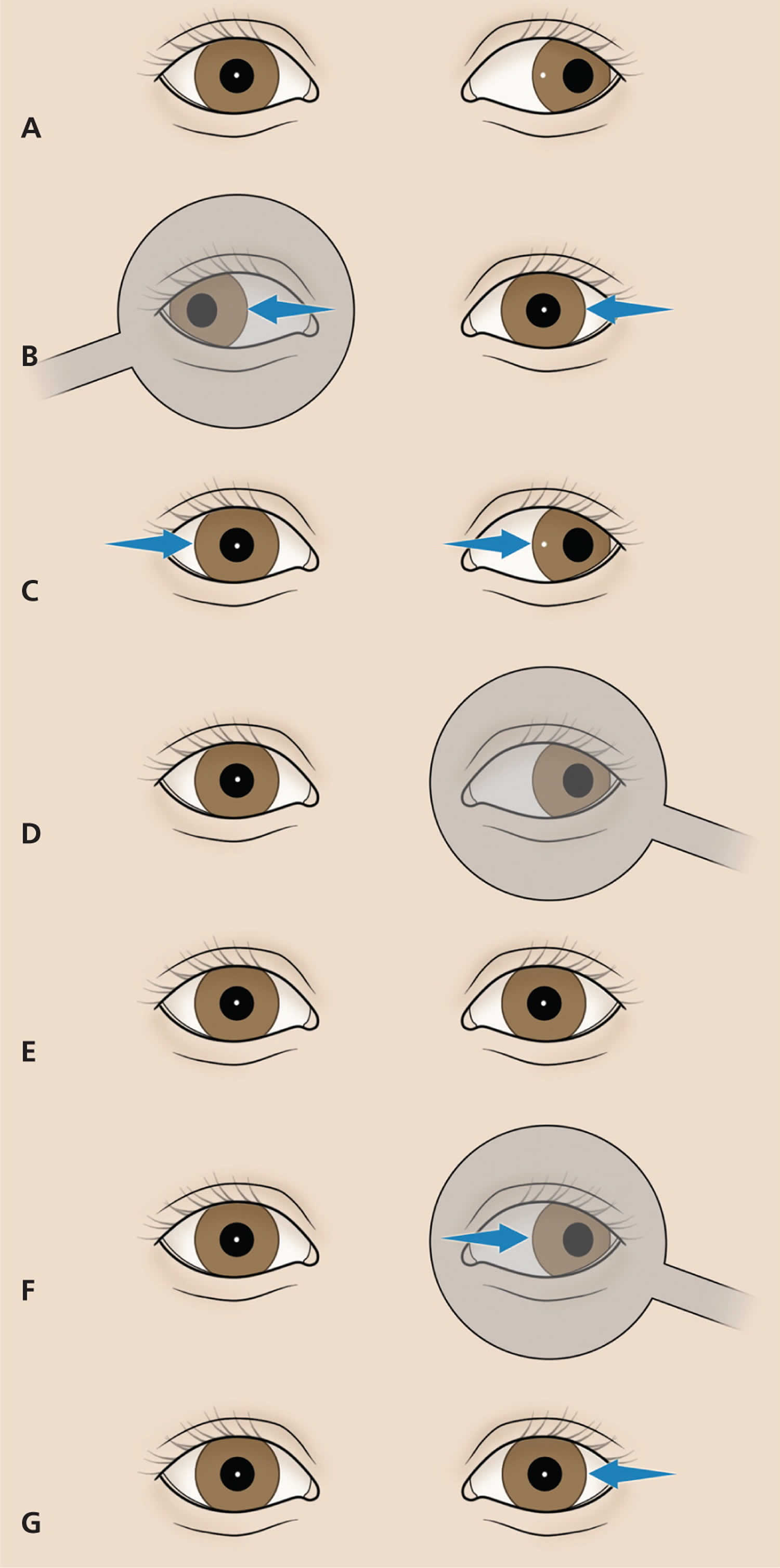
Figure 7. Cover and Cover-Uncover Eye Test
Footnotes: Screening tests for abnormal eye alignment. (A through D) The cover test. (A) On simple observation, one eye (the tested eye, which is the patient’s left eye in this illustration) appears to deviate. (B) The uncovered (tested) eye is observed for movement into alignment as the other eye is covered (in this illustration, an exotropia is exposed). This movement into alignment can come from any direction and is generally reproducible on repeat examinations. (C) When the opposite eye is uncovered, the tested eye is observed to return to its original location. (D) When the test eye is the normal eye (which is the patient’s right eye in this illustration), it does not move when the opposite eye is covered or uncovered. (E through G) The cover-uncover test. (E) The tested eye (which is the patient’s left eye in this illustration) is covered. On simple observation, before it is covered, the eye appears to be in alignment. (F) The tested eye is covered for a few seconds. (G) As the cover is rapidly removed, the tested eye is observed for movement back into alignment (in this illustration, an exophoria is exposed).
[Source 102 ]Photoscreening
Photoscreening provides another approach to vision screening. Photoscreening is a useful add-on to detect amblyopia risk in younger children, those who are uncooperative with chart-based vision testing, or those who are nonverbal. The equipment is designed for use with minimal personnel training and has been associated with successful amblyopia treatment in children identified with risk factors 103. In photoscreening, the red reflex of both eyes is taken simultaneously with digital or flash photography and evaluated for signs of uncorrected refractive error, ocular opacities, or misalignment. The images are analyzed by software or human interpreters, and if an abnormality is detected, referral to an ophthalmologist is recommended 104, 105, 106. Previously, a physician would have had to buy a photoscreener to perform this screening, which was usually cost prohibitive. However, there is now a photoscreening app for mobile devices that is affordable and easily accessible 107. A photograph of the eyes is taken with the phone, and the app analyzes it for amblyopia risk factors. It has a sensitivity of 65% and a specificity of 83% 107. However, photoscreeners have high false-positive rates, leading to higher rates of referral of children with normal vision 108, 109. Although photoscreening should not replace traditional vision chart testing, it may be a useful adjunct in children who cannot cooperate for vision chart testing.
Vision Testing
In children three years and older, vision testing is performed monocularly with standard eye charts. The charts are labeled with the proper testing distance of 10 or 20 feet (approximately 3 or 6 m) 102. The most advanced test that a child can perform is recommended, because picture testing may mildly overestimate vision compared with letter testing. The American Association for Pediatric Ophthalmology and Strabismus vision screening guidelines are provided in Table 3 82. Any child three-and-a-half to five years of age with best-corrected vision less than 20/40 in either eye, or five years and older with best-corrected vision less than 20/32 in either eye, or with a two-line difference between eyes, should be referred to a pediatric ophthalmologist 82. Children should be tested with lines of letters, and not a single letter, because the latter can overestimate vision. An adhesive patch to cover the eye is preferred for testing over a handheld occluder, because children may peek around the occluder unnoticed, and amblyopia can be missed. Patients with nystagmus (rapid involuntary movements of the eyes) should have their vision tested with both eyes first, which gives their true functioning visual acuity. When a patch or occluder is placed over one eye, increased nystagmus may occur, further decreasing the patient’s vision. This results in falsely lowered monocular visual acuity.
Ophthalmologists diagnose amblyopia by checking to see if vision differs between the two eyes. To check a baby’s or young child’s vision, the ophthalmologist may cover one of the child’s eyes and watch how well they can follow a moving object. The doctor may also watch how the child reacts when one eye is covered. If one eye has amblyopia and the other is covered, the child may try to look above or below the patch, pull it off or cry 77.
The ophthalmologist will do a complete medical eye exam, looking for other eye problems that could be affecting vision 77.
Poor vision in one eye does not always mean a child has amblyopia 77. In some cases, wearing glasses to correct a refractive error in one eye can improve vision.
When should a child’s vision be tested?
All children should have their vision checked by their pediatrician, family physician or ophthalmologist at or before their 4th birthday 77. If there is a family history of misaligned eyes, childhood cataracts or serious eye disease, an ophthalmologist should check their eyes when they are an infant.
Most doctors test vision as part of a child’s medical exam. If they see any sign of eye problems, they may send a child to an ophthalmologist for further tests.
Lazy eye treatment
Treatment for amblyopia involves your child using the weaker eye more and helping the weaker eye get stronger. Amblyopia is usually corrected by making your child use their weaker eye 110. This can be done by putting a patch over the child’s stronger eye 110. Most children wear their eye patches 2 to 6 hours a day. Another way is to make vision blurry in the stronger eye using eye drops 110. Or the child may wear eyeglasses with a lens that blurs vision in the good eye 110. This also makes the weaker eye work harder and strengthens it. Glasses or contact lenses can fix problems with nearsightedness (myopia) or farsightedness (hyperopia). Treatment usually lasts until vision is normal, or until vision stops getting better. For most children, this takes several weeks to several months. A few children need to use eye patches until they are 8 to 10 years old. There’s a small chance that using an eye patch for too long can hurt the strong eye. Children who are wearing eye patches should see their doctor often during the treatment.
It can take several weeks to several months for vision to get stronger in the weaker eye. Once the child has better vision in that eye, he or she may need to wear an eye patch part-time for a few years. This helps keep their vision strong.
In some cases, the ophthalmologist will recommend surgery to correct certain eye problems causing amblyopia. Surgery may be needed for cataracts, droopy eyelids (congenital ptosis), or crossed eyes (strabismus). After surgery, the child may need to keep wearing a patch or otherwise cover the strong eye until his or her vision improves.
It is possible to prevent vision loss from amblyopia. But treatment only works if your child only uses the weaker eye to see 110. Children do not like to have their stronger eye patched or blurred. However, you need to help your child do what is best for them.
- When a child has amblyopia, it is important to make vision stronger in the weak eye 110. Even if eye problems causing amblyopia are corrected with glasses or surgery, the amblyopia itself must be treated. If not, the child may have lifelong vision problems 110.
How is lazy eye treated in children?
Individual treatment plans depend on the age of the patient, the severity of amblyopia, and compliance with patching or atropine regimen and follow-up. For example, a seven-year-old patient with anisometropia who is initially diagnosed with dense amblyopia would likely benefit from a combination of glasses with patching instead of observation with glasses alone. A similar three-year-old patient may be treated with glasses alone, followed by patching after any improvement in vision stabilizes. Surveillance for occlusion amblyopia (decreased vision in the patched eye due to deprivation) and amblyopia recurrence after successful treatment are critical. Amblyopia recurs in 25 percent of children after patching is discontinued 111. Tapering the amount of time a patch is worn each day at the end of treatment reduces the risk of recurrence.
Treating amblyopia involves forcing the child to use the eye with weaker vision. There are two common ways to treat amblyopia 6:
Eye Patching
An adhesive patch is worn over the stronger eye for weeks to months. This therapy forces the child to use the eye with amblyopia. Patching stimulates vision in the weaker eye and helps parts of the brain involved in vision develop more completely. A less utilized therapy option is the Bangerter filter, in which a graded adhesive is applied to the child’s glasses over the lens of the nonamblyopic eye, producing a blurred image. This is mostly used in older children who prefer a less noticeable option than patching.
An National Eye Institute study 112 showed that patching the unaffected eye of children with moderate amblyopia for two hours daily works as well as patching for six hours daily 6. Shorter patching time can lead to better compliance with treatment and improved quality of life for children with amblyopia. However, a recent study 113 showed that children whose amblyopia persists despite two hours of daily patching may improve if daily patching is extended to 6 hours.
Previously, eye care professionals thought that treating amblyopia would be of little benefit to older children. However, results from a nationwide clinical trial 114 showed that many children from ages seven to 17 years old benefited from treatment for amblyopia. This study shows that age alone should not be used as a factor to decide whether or not to treat a child for amblyopia.
Things to consider with eye patching treatment:
- In very rare instances it is possible to overuse the patch or blurring eye drops. This can affect vision in the stronger eye. Be sure to keep the child’s appointments with the ophthalmologist so that vision in both eyes can be closely monitored.
- The skin near your child’s eye patch can get irritated. To help, try a different size or type of patch, and angle the patch differently each day.
- Your child may initially be clumsy when wearing a patch. Try to keep an eye on your child when they are climbing stairs or being active.
Figure 8. Amblyopia eye patch
Footnotes: Patching Right Eye. Treatment for amblyopia in this child’s Left lazy eye is obtained by patching the fellow right normal eye.
[Source 40 ]How to choose and use an eye patch
An eye patch should be comfortable, yet remain firmly in place. It should also not allow the child to peek around its edges. Most drug stores have a variety of sizes and types of eye patches. Decorated fun patches are available online. Do not use the black eye patches with elastic bands or ties such as a pirate-type patches. These are too easy for a child to remove or peek around. To wear the patch, simply attach it to the skin around your child’s eye.
If your child wears glasses, there are patches designed to attach to the lens. These may be good for children who are used to wearing a patch, but they are not as good for a child new to treatment. This is because the patch can slip or the child may learn to peek around it. If your child wears glasses and is not used to patching, it is best to attach the patch directly around the stronger eye underneath the glasses.
What kind of eye patch should be used?
The best type of eye patch is one with adhesive on the back, like a Band-Aid. It should be big enough to completely cover your child’s eye. Sometimes it helps to fold the eye patch a little before peeling off the backing to make it more curved. This gives more room for your child’s eyelashes to blink. Some eye patches come with fun designs to encourage kids to wear them.
There are also cloth eye patches that fit over glasses. For the eye patches that fit over glasses to work, the glasses must fit well on your child’s face, and the patch should cover the whole lens and the space around the eye, so your child can’t peek around the patch. Pirate eye patches with straps don’t work well because they don’t fit tightly enough, and kids often move them to peak around them. If you notice your child turning their head or lifting their chin to peek while wearing the eye patch, make sure to watch them closely and check how well the eye patch is fitting.
Should glasses be worn during eye patching?
Yes. The glasses should be worn over the sticky eye patch. Do not stick the eye patch on the glasses lens. It will not work well as the child will be able to peek around the lens and the patch.
What if the eye patch adhesive causes skin irritations?
After removing the eye patch, using lotion or moisturizer can help soothe the skin. Different eye patches have different adhesives, so switching to another brand might help reduce irritation. Another idea is to rub Milk of Magnesia on the skin where the eye patch will go. Let it dry on the skin before applying the patch. This helps keep the adhesive from sticking too much to the skin. If the eye patch feels too sticky, you can stick it to a clean cloth, like a shirt, a few times before putting it on the child’s face.
During which activities should patching be performed?
There is no particular activity that will improve the vision more than another activity. The most important part of treatment is keeping the patch on for the prescribed treatment time. As long as the child is conscious and has his or her eyes open, visual input will be processed by the amblyopic eye. On the other hand, the child may be more cooperative or more open to bargaining if patching is performed during certain, favorite activities (such as watching a preferred television program or video). Some eye doctors believe that the performance of near activities (reading, coloring, hand-held computer games) during treatment may be more stimulating to the brain and produce better or more rapid recovery of vision.
Should patching be performed during school hours?
In many instances, school is an excellent time to patch, taking advantage of a nonparental authority figure. Patching during school hours gives the class an opportunity to learn valuable lessons about accepting differences between children. While in most instances, children may not need to modify their school activities while patching, sometimes adjustments such as sitting in the front row of the classroom will be necessary. If the patient, teacher, and classmates are educated appropriately, school patching need not be a socially stigmatizing experience. On the other hand, frequently a parental or other family figure may be more vigilant in monitoring patching than is possible in the school setting. Parents should be flexible in choosing when to schedule patching.
What if my child refuses to wear the patch?
Many children will resist wearing a patch at first. Children do not like to have their stronger eye patched or blurred. Successful patching may require persistence and plenty of encouragement from family members, neighbors, teachers, etc. Otherwise, treatment will not work. Children will often throw a temper-tantrum, but then they eventually learn not to remove the patch. Another way to help is to provide a reward to the child for keeping the patch on for the prescribed time period.
It can take a while for your child to get used to wearing a patch. Over time, this should get easier for them and you. Remember that strengthening the weaker eye is the only way to develop healthy, normal vision.
If your child still takes off the patch, as a last resort, you might cover his or her hands with gloves, mittens, or socks.
What can be done to encourage better eye patching?
To help younger children keep the eye patch on, make it part of their daily routine. Spending one-on-one time with an infant or toddler can help keep them distracted and stop them from taking off the eye patch. Giving your child a fun activity, like watching a favorite TV show or playing video games, can also help. For infants and toddlers, sometimes using Velcro wraps around the arms can prevent them from taking the eye patch off. These wraps usually only need to be used a few times. Talk to your child’s pediatric ophthalmologist before using this method.
Older children might need rewards to help them stick to their eye patching. You can use fun posters where the child fills in a box each time they wear the eye patch. They can get a prize when they complete the poster.
How long does amblyopia eye patching therapy take to work?
Although vision improvement frequently occurs within weeks of beginning patching treatment, optimal results often take many months. Once vision has been improved, less (maintenance) patching or periodic use of atropine eyedrops may be required to keep the vision from slipping or deteriorating. This maintenance treatment may be advisable for several months to years.
Atropine eye drops
A drop of a drug called atropine is placed in the stronger eye to temporarily blur vision so that the child will use the eye with amblyopia, especially when focusing on near objects. Atropine 1% eye drops block parasympathetic innervation to the ciliary muscle and pupil, causing temporary loss of accommodation (focusing at near) and pupillary dilation. Atropine is more effective in farsighted eyes, because removing the ability to accommodate in such eyes does not allow the child to focus at near. The goal of atropine use is to stimulate preferential near fixation of the amblyopic eye, leading to visual improvement.
National Eye Institute-supported research 115 has shown that atropine eye drops, when placed in the unaffected eye once a day, work as well as eye patching. Atropine eye drops are sometimes easier for parents and children to use.
However, not all children benefit from eye drop treatment for amblyopia. Eye drops (such as atropine) do not work as well when the stronger eye is nearsighted or when the degree of amblyopia is severe 39.
Bangerter filter
Bangerter filter (Ryser Optik AG) is a special filter that is placed on the eyeglass lens of the stronger eye. The filter blurs the stronger eye and, like an eye patch, works to stimulate the weaker eye. Filters are an appropriate choice for treatment for children with mild amblyopia who do not improve with refractive corrections alone 42. This filter has been used mostly as maintenance treatment after initial treatment with either eye patching or atropine eye drops. A randomized controlled trial assessed the effectiveness of Bangerter filters as primary treatment for amblyopia compared with 2 hours per day of eye patching 116. On average, the eye patching and Bangerter filter groups had similar improvement in visual acuity for moderate amblyopia 117, 118, 119, 120, 121, 122, 123, 124.
Glasses or contact lenses
Glasses or contact lenses can correct problems such as nearsightedness (myopia), farsightedness (hyperopia) or astigmatism that result in lazy eye. They can also be prescribed to blur sight in the eye that’s being used. This forces the brain to work with the eye it’s ignoring. As vision improves, your child’s eyeglass prescription may change.
Newer treatments
There are some newer treatments available in the U.S. and approved to treat amblyopia. These treatments use virtual reality (VR) with the child wearing a headset or special glasses while watching movies or videos. During treatment, the headset or glasses blurs the stronger eye to help the weaker eye. Children tend to like doing this treatment and seems to work just as well as eye patching. These newer treatments are still being studied to understand what types of amblyopia they work best for. Speak with your child’s ophthalmologist if you have questions about these new amblyopia treatments.
Lazy eye surgery
“Lazy eye surgery” does not exist 21. Lazy eye (amblyopia) cannot be treated with surgery. It can only be treated when the patient is a child. The younger it is detected and treated the better. In fact, after age 6 the success rate of treatment goes way down. Glasses and eye patches are the most common treatments for amblyopia, or lazy eye.
Strabismus, or eye misalignment, CAN be treated with surgery on the eye muscles. This surgery can be performed on both adults and children. Eye muscle surgery can improve not only the cosmetic appearance of the eyes but also visual function.
When most people ask about “lazy eye surgery”, they are really talking about strabismus surgery, or surgery to correct misalignment of the eyes.
If you are considering eye muscle surgery, here are the key facts to know:
- The surgery works by either loosening or tightening the eye muscles. This changes the alignment of the eyes relative to each other.
- Approximately 1.2 million eye alignment surgeries are performed each year, making it the third most common eye surgery in the United States.
- Eye muscle surgery has a high success rate and serious complications are extremely rare.
- It is a one-day procedure that usually does not require staying overnight in the hospital.
- Children can return to school after a few days of rest. Most adults can return to work within a week.
- Pain, soreness, redness, and double vision are the most common side effects of eye muscle surgery. These are usually temporary.
The are two main types of surgery:
- Recession is when an eye muscle is detached and then reattached further away from the front of the eye to weaken the muscle.
- Resection is when a portion of an eye muscle is removed to make the muscle stronger.
Whether you are looking into this “lazy eye surgery” for yourself or your child, a vital first step is to discuss your goals and expectations for the surgery with your ophthalmologist.
Lazy eye exercises
Currently there is no human studies on eye exercises for lazy eye (amblyopia). The only research we could find was on mice. That research 125 has demonstrated that voluntary physical exercise and visual perceptual learning, two totally non invasive procedures, share the remarkable capability to potentiate plasticity in the adult visual cortex, favoring recovering of visual functions in adult amblyopic rodents. Running and locomotion is associated not only with activation of cortical Vasoactive Intestinal Peptide neurons, but also with increases in multiple neuromodulators, including serotonin, which has been shown to be enhanced by environmental enrichment 126 and to promote adult primary visual plasticity 127. The impact of physical exercise on amblyopic adults remains to be elucidated, with preliminary results in this laboratory study showing a strong enhancement of visual cortical plasticity in healthy subjects after a period of voluntary physical activity 128.
There’s no evidence that eye exercises can treat or fix amblyopia 129, 130, 131. Your child’s eye specialist might suggest that your child do specific tasks like playing games or solving puzzles while they’re wearing an eye patch or using medicated eye drops. These activities will help strengthen the connection between their brain and weaker eye. There aren’t specific exercises or eye motions that can correct amblyopia.
Living with lazy eye
Depending on your child’s age, it could be difficult for them to wear an eye patch. If a patch bothers your child, ask your doctor if you have other options. Glasses or eye drops might be a better choice for your child.
Amblyopia can come back after treatment is finished — which can happen in up to 25 percent of children with amblyopia. It’s important to continue to watch your child for symptoms of lazy eye. If symptoms do come back, treatment will need to be repeated. Some children’s treatment lasts until they are 10 years old.
Lazy eye prognosis
Identifying and treating amblyopia early prevents children from having permanent visual loss. All children should have a complete eye exam at least once between ages 3 and 5.
The prognosis (outlook) of amblyopia depends on the age at which treatment is initiated and the severity of the condition. Children who get treated before age 5 almost always recover vision that is close to normal. However, they may continue to have problems with depth perception 132, 133.
When treated, over 70% of children experience significant vision improvement within 12 months 40. Even after successful treatment, there may be some gradual decline in vision in subsequent years with visual acuity may slightly decline over time in approximately 50% of children with amblyopia 40. Factors associated with a heightened risk of not achieving complete vision restoration include the age at which treatment commenced with later treatment typically yielding a less favorable outcome, deprivation amblyopia, and poor initial visual acuity 40.
Permanent vision problems may result if treatment is delayed. Children treated after age 10 can expect vision to recover only partially 134, 135, 136.
Studies have demonstrated that amblyopic children read significantly more slowly than controls, even when the vision in the amblyopic eye is only reduced to 20/30 vision 137, 75. Amblyopia can also impact academic related fine-motor outcomes, such as multiple-choice answer completion time 76.
- Birch EE, Kelly KR, Wang J. Recent Advances in Screening and Treatment for Amblyopia. Ophthalmol Ther. 2021 Dec;10(4):815-830. doi: 10.1007/s40123-021-00394-7[↩]
- Lam M, Suh D. Screening, Diagnosis, and Treatment of Pediatric Ocular Diseases. Children (Basel). 2022 Dec 10;9(12):1939. doi: 10.3390/children9121939[↩]
- Birch EE, Kelly KR. Amblyopia and the whole child. Prog Retin Eye Res. 2023 Mar;93:101168. doi: 10.1016/j.preteyeres.2023.101168[↩][↩]
- Proudlock FA, Hisaund M, Maconachie G, Papageorgiou E, Manouchehrinia A, Dahlmann-Noor A, Khandelwal P, Self J, Beisse C, Gottlob I; EUPatch study group. Extended optical treatment versus early patching with an intensive patching regimen in children with amblyopia in Europe (EuPatch): a multicentre, randomised controlled trial. Lancet. 2024 May 4;403(10438):1766-1778. doi: 10.1016/S0140-6736(23)02893-3. Erratum in: Lancet. 2024 Jun 22;403(10445):2694. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)02893-3/fulltext[↩]
- Lingham G, McGuinness MB, Safi S, Gordon I, Evans JR, Keel S. Clinical Practice Guidelines for the Detection and Treatment of Amblyopia: A Systematic Literature Review. J Binocul Vis Ocul Motil. 2022 Apr-Jun;72(2):77-85.[↩]
- The National Eye Institute, National Institutes of Health. Facts About Amblyopia. https://nei.nih.gov/health/amblyopia/amblyopia_guide[↩][↩][↩][↩]
- McConaghy JR, McGuirk R. Amblyopia: Detection and Treatment. Am Fam Physician. 2019 Dec 15;100(12):745-750. https://www.aafp.org/pubs/afp/issues/2019/1215/p745.html[↩]
- Bradfield YS. Identification and treatment of amblyopia [published correction appears in Am Fam Physician. 2013;88(3):159]. Am Fam Physician. 2013;87(5):348-352. https://www.aafp.org/pubs/afp/issues/2013/0301/p348.html[↩]
- Doshi NR, Rodriguez ML. Amblyopia. Am Fam Physician. 2007;75(3):361-367. https://www.aafp.org/pubs/afp/issues/2007/0201/p361.html[↩][↩]
- Seignette K, Levelt CN. Amblyopia: The Thalamus Is a No-Go Area for Visual Acuity. Curr Biol. 2018 Jun 18;28(12):R709-R712. doi: 10.1016/j.cub.2018.04.081[↩]
- Webber AL, Wood J. Amblyopia: prevalence, natural history, functional effects and treatment. Clin Exp Optom. 2005 Nov;88(6):365-75. doi: 10.1111/j.1444-0938.2005.tb05102.x[↩]
- Attebo K, Mitchell P, Cumming R, Smith W, Jolly N, Sparkes R. Prevalence and causes of amblyopia in an adult population. Ophthalmology. 1998 Jan;105(1):154-9. doi: 10.1016/s0161-6420(98)91862-0[↩][↩]
- Centers for Disease Control and Prevention. Common Eye Disorders. https://www.cdc.gov/visionhealth/basics/ced/index.html[↩]
- Stewart CE, Shah S, Wren S, Roberts CJ. Paediatric Eye Services: How Much of the Workload Is Amblyopia-Related? Strabismus. 2016 Sep;24(3):109-12. doi: 10.1080/09273972.2016.1205102[↩]
- Rahi J, Logan S, Timms C, Russell-Eggitt I, Taylor D. Risk, causes, and outcomes of visual impairment after loss of vision in the non-amblyopic eye: a population-based study. Lancet. 2002 Aug 24;360(9333):597-602. doi: 10.1016/s0140-6736(02)09782-9[↩]
- Koklanis K, Abel LA, Aroni R. Psychosocial impact of amblyopia and its treatment: a multidisciplinary study. Clin Exp Ophthalmol. 2006 Nov;34(8):743-50. doi: 10.1111/j.1442-9071.2006.01317.x[↩]
- Hu B, Liu Z, Zhao J, Zeng L, Hao G, Shui D, Mao K. The Global Prevalence of Amblyopia in Children: A Systematic Review and Meta-Analysis. Front Pediatr. 2022 May 4;10:819998. doi: 10.3389/fped.2022.819998[↩]
- Hashemi H, Pakzad R MSc, Yekta A, Bostamzad P, Aghamirsalim M, Sardari S MSc, Valadkhan M MSc, Pakbin M MSc, Heydarian S, Khabazkhoob M. Global and regional estimates of prevalence of amblyopia: A systematic review and meta-analysis. Strabismus. 2018 Dec;26(4):168-183. doi: 10.1080/09273972.2018.1500618[↩]
- Nitzan I, Bez M, Megreli J, Bez D, Barak A, Yahalom C, Levine H. Socio-demographic disparities in amblyopia prevalence among 1.5 million adolescents. Eur J Public Health. 2021 Dec 1;31(6):1211-1217. doi: 10.1093/eurpub/ckab111[↩]
- Xiao O, Morgan IG, Ellwein LB, He M; Refractive Error Study in Children Study Group. Prevalence of Amblyopia in School-Aged Children and Variations by Age, Gender, and Ethnicity in a Multi-Country Refractive Error Study. Ophthalmology. 2015 Sep;122(9):1924-31. doi: 10.1016/j.ophtha.2015.05.034[↩]
- American Academy of Ophthalmology. Lazy Eye Surgery Facts. https://www.aao.org/eye-health/tips-prevention/lazy-eye-surgery-facts[↩][↩][↩]
- Donahue SP, Baker CN; Committee on Practice and Ambulatory Medicine, American Academy of Pediatrics; Section on Ophthalmology, American Academy of Pediatrics; American Association of Certified Orthoptists; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology. Procedures for the evaluation of the visual system by pediatricians. Pediatrics. 2016;137(1).[↩][↩]
- Jonas DE, Amick HR, Wallace IF, et al. Vision Screening in Children Ages 6 Months to 5 Years: A Systematic Review for the US Preventive Services Task Force. Evidence Synthesis No. 153. AHRQ Publication No. 17-05228-EF-1. Rockville, MD: Agency for Healthcare Research and Quality; 2017.[↩]
- American Academy of Family Physicians. Clinical preventive service recommendation: visual difficulties and impairment. http://www.aafp.org/patient-care/clinical-recommendations/all/visual.html[↩]
- American Optometric Association. Optometric clinical practice guideline: pediatric eye and vision examination. https://www.aoa.org/documents/optometrists/CPG-2.pdf[↩]
- US Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Document/evidence-summary/vision-in-children-ages-6-months-to-5-years-screening[↩]
- Final Recommendation Statement. Vision in Children Ages 6 Months to 5 Years: Screening. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/vision-in-children-ages-6-months-to-5-years-screening[↩]
- Repka M.X., Beck R.W., Holmes J.M., Birch E.E., Chandler D.L., Cotter S.A., Hertle R.W., Kraker R.T., Moke P.S., Quinn G.E., et al. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch. Ophthalmol. 2003;121:603–611. doi: 10.1001/archopht.121.5.603[↩]
- Cotter S.A., Pediatric Eye Disease Investigator G., Edwards A.R., Wallace D.K., Beck R.W., Arnold R.W., Astle W.F., Barnhardt C.N., Birch E.E., Donahue S.P., et al. Treatment of anisometropic amblyopia in children with refractive correction. Ophthalmology. 2006;113:895–903. doi: 10.1016/j.ophtha.2006.01.068[↩]
- Pediatric Eye Disease Investigator G. A randomized trial of atropine vs. patching for treatment of moderate amblyopia in children. Arch. Ophthalmol. 2002;120:268–278. doi: 10.1001/archopht.120.3.268[↩]
- Amblyopia. https://eyewiki.org/Amblyopia[↩]
- Donahue SP, Arthur B, Neely DE, Arnold RW, Silbert D, Ruben JB; POS Vision Screening Committee. Guidelines for automated preschool vision screening: a 10-year, evidence-based update. J AAPOS. 2013 Feb;17(1):4-8. doi: 10.1016/j.jaapos.2012.09.012[↩][↩]
- Pascual M, Huang J, Maguire MG, et al; Vision In Preschoolers (VIP) Study Group. Risk factors for amblyopia in the vision in preschoolers study. Ophthalmology. 2014;121(3):622-629.[↩]
- Ying GS, Huang J, Maguire MG, et al; Vision in Preschoolers Study Group. Associations of anisometropia with unilateral amblyopia, interocular acuity difference, and stereoacuity in preschoolers. Ophthalmology. 2013;120(3):495-503.[↩]
- Arnold RW. Amblyopia risk factor prevalence. J Pediatr Ophthalmol Strabismus. 2013;50(4):213-217.[↩]
- Pai AS, Rose KA, Leone JF, et al. Amblyopia prevalence and risk factors in Australian preschool children. Ophthalmology. 2012;119(1):138-144.[↩]
- Pai AS, Wang JJ, Samarawickrama C, et al. Prevalence and risk factors for visual impairment in preschool children: the Sydney Paediatric Eye Disease Study. Ophthalmology. 2011;118(8):1495-1500.[↩]
- Ciner EB, Schmidt PP, Orel-Bixler D, et al. Vision screening of preschool children: evaluating the past, looking toward the future. Optom Vis Sci. 1998;75(8):571-584.[↩]
- American Association for Pediatric Ophthalmology and Strabismus. Amblyopia. https://aapos.org/terms/conditions/21[↩][↩][↩]
- Blair K, Cibis G, Zeppieri M, et al. Amblyopia. [Updated 2024 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430890[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Randomized Trial of Treatment of Amblyopia in Children Aged 7 to 17 Years. Arch Ophthalmol. 2005;123(4):437–447. doi:10.1001/archopht.123.4.437[↩][↩]
- Cruz OA, Repka MX, Hercinovic A, Cotter SA, Lambert SR, Hutchinson AK, Sprunger DT, Morse CL, Wallace DK; American Academy of Ophthalmology Preferred Practice Pattern Pediatric Ophthalmology/Strabismus Panel. Amblyopia Preferred Practice Pattern. Ophthalmology. 2023 Mar;130(3):P136-P178. doi: 10.1016/j.ophtha.2022.11.003[↩][↩]
- American Academy of Ophthalmology Basic and Clinical Science Course Subcommittee. Basic andclinical science course. Pediatric ophthalmology and strabismus: Section 6, 2022–2023. San Francisco, CA: American Academy of Ophthalmology; 2022.[↩]
- Identification and Treatment of Amblyopia. Am Fam Physician. 2013 Mar 1;87(5):348-352. http://www.aafp.org/afp/2013/0301/p348.html[↩]
- Repka MX. Amblyopia Outcomes Through Clinical Trials and Practice Measurement: Room for Improvement: The LXXVII Edward Jackson Memorial Lecture. Am J Ophthalmol. 2020 Nov;219:A1-A26. doi: 10.1016/j.ajo.2020.07.053[↩]
- Hamm L, Chen Z, Li J, Black J, Dai S, Yuan J, Yu M, Thompson B. Interocular suppression in children with deprivation amblyopia. Vision Res. 2017 Apr;133:112-120. doi: 10.1016/j.visres.2017.01.004[↩][↩]
- Tarczy-Hornoch K, Varma R, Cotter SA, McKean-Cowdin R, Lin JH, Borchert MS, Torres M, Wen G, Azen SP, Tielsch JM, Friedman DS, Repka MX, Katz J, Ibironke J, Giordano L; Joint Writing Committee for the Multi-Ethnic Pediatric Eye Disease Study and the Baltimore Pediatric Eye Disease Study Groups. Risk factors for decreased visual acuity in preschool children: the multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology. 2011 Nov;118(11):2262-73. doi: 10.1016/j.ophtha.2011.06.033[↩]
- Sen S, Singh P, Saxena R. Management of amblyopia in pediatric patients: Current insights. Eye (Lond). 2022 Jan;36(1):44-56. doi: 10.1038/s41433-021-01669-w[↩][↩]
- Pascual M, Huang J, Maguire MG, Kulp MT, Quinn GE, Ciner E, Cyert LA, Orel-Bixler D, Moore B, Ying GS; Vision In Preschoolers (VIP) Study Group. Risk factors for amblyopia in the vision in preschoolers study. Ophthalmology. 2014 Mar;121(3):622-9.e1. doi: 10.1016/j.ophtha.2013.08.040[↩]
- Najem K, Asuncion RMD, Margolin E. Diplopia. [Updated 2024 Feb 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441905[↩]
- Şahin Karamert S, Atalay HT, Özdek Ş. Strabismus in Retinopathy of Prematurity: Risk Factors and the Effect of Macular Ectopia. Turk J Ophthalmol. 2023 Aug 19;53(4):241-246. doi: 10.4274/tjo.galenos.2023.48310[↩]
- Afsari S, Rose KA, Gole GA, Philip K, Leone JF, French A, Mitchell P. Prevalence of anisometropia and its association with refractive error and amblyopia in preschool children. Br J Ophthalmol. 2013 Sep;97(9):1095-9. doi: 10.1136/bjophthalmol-2012-302637[↩]
- Hamm LM, Chen Z, Li J, Dai S, Black J, Yuan J, Yu M, Thompson B. Contrast-balanced binocular treatment in children with deprivation amblyopia. Clin Exp Optom. 2018 Jul;101(4):541-552. doi: 10.1111/cxo.12630[↩]
- Cheng KP, Hiles DA, Biglan AW, Pettapiece MC. Visual results after early surgical treatment of unilateral congenital cataracts. Ophthalmology. 1991 Jun;98(6):903-10. doi: 10.1016/s0161-6420(91)32203-6[↩]
- Elhusseiny AM, Wu C, MacKinnon S, Hunter DG. Severe reverse amblyopia with atropine penalization. J AAPOS. 2020 Apr;24(2):106-108. doi: 10.1016/j.jaapos.2019.12.001[↩]
- The Pediatric Eye Disease Investigator Group. A Randomized Trial of Atropine vs Patching for Treatment of Moderate Amblyopia in Children. Arch Ophthalmol. 2002;120(3):268–278. doi:10.1001/archopht.120.3.268[↩]
- de Zárate BR, Tejedor J. Current concepts in the management of amblyopia. Clin Ophthalmol. 2007 Dec;1(4):403-14. https://pmc.ncbi.nlm.nih.gov/articles/PMC2704537/[↩]
- Holmes JM, Levi DM. Treatment of amblyopia as a function of age. Vis Neurosci. 2018 Jan;35:E015. doi: 10.1017/S0952523817000220[↩]
- Kiorpes L, Daw N. Cortical correlates of amblyopia. Vis Neurosci. 2018 Jan;35:E016. doi: 10.1017/S0952523817000232[↩]
- Zetterström C, Lundvall A, Kugelberg M. Cataracts in children. J Cataract Refract Surg. 2005 Apr;31(4):824-40. doi: 10.1016/j.jcrs.2005.01.012[↩][↩][↩]
- American Academy of Pediatrics, Section on Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology; American Association of Certified Orthoptists. Red reflex examination in neonates, infants, and children. Pediatrics. 2008;122(6):1401-1404.[↩]
- Pathai S, Cumberland PM, Rahi JS. Prevalence of and early-life influences on childhood strabismus: findings from the Millennium Cohort Study. Arch Pediatr Adolesc Med. 2010 Mar;164(3):250-7. doi: 10.1001/archpediatrics.2009.297[↩]
- Levi DM. Rethinking amblyopia 2020. Vision Res. 2020 Nov;176:118-129. doi: 10.1016/j.visres.2020.07.014[↩]
- Duan Y, Norcia AM, Yeatman JD, Mezer A. The Structural Properties of Major White Matter Tracts in Strabismic Amblyopia. Invest Ophthalmol Vis Sci. 2015 Aug;56(9):5152-60. doi: 10.1167/iovs.15-17097[↩]
- Varma R, Tarczy-Hornoch K, Jiang X. Visual Impairment in Preschool Children in the United States: Demographic and Geographic Variations From 2015 to 2060. JAMA Ophthalmol. 2017 Jun 1;135(6):610-616. doi: 10.1001/jamaophthalmol.2017.1021[↩]
- Lin HW, Young ML, Pu C, Huang CY, Lin KK, Lee JS, Hou CH. Changes in anisometropia by age in children with hyperopia, myopia, and antimetropia. Sci Rep. 2023 Aug 22;13(1):13643. doi: 10.1038/s41598-023-40831-0[↩]
- Mendola JD, Lam J, Rosenstein M, Lewis LB, Shmuel A. Partial correlation analysis reveals abnormal retinotopically organized functional connectivity of visual areas in amblyopia. Neuroimage Clin. 2018 Jan 31;18:192-201. doi: 10.1016/j.nicl.2018.01.022[↩]
- Kantarci FA, Tatar MG, Uslu H, Colak HN, Yildirim A, Goker H, Gurler B. Choroidal and peripapillary retinal nerve fiber layer thickness in adults with anisometropic amblyopia. Eur J Ophthalmol. 2015 Sep-Oct;25(5):437-42. doi: 10.5301/ejo.5000594. Epub 2015 Mar 21. Erratum in: Eur J Ophthalmol. 2016 Dec 29;27(1):113. doi: 10.5301/EJO.2016.16527[↩]
- Cevher S, Şahin T. Does anisometropia affect the ciliary muscle thickness? An ultrasound biomicroscopy study. Int Ophthalmol. 2020 Dec;40(12):3393-3402. doi: 10.1007/s10792-020-01625-9[↩]
- Nishi T, Ueda T, Hasegawa T, Miyata K, Ogata N. Choroidal thickness in children with hyperopic anisometropic amblyopia. Br J Ophthalmol. 2014 Feb;98(2):228-32. doi: 10.1136/bjophthalmol-2013-303938. Epub 2013 Nov 1. Erratum in: Br J Ophthalmol. 2016 Jul;100(7):1016. doi: 10.1136/bjophthalmol-2013-303938corr1[↩]
- Tekin K, Cankurtaran V, Inanc M, Sekeroglu MA, Yilmazbas P. Effect of myopic anisometropia on anterior and posterior ocular segment parameters. Int Ophthalmol. 2017 Apr;37(2):377-384. doi: 10.1007/s10792-016-0272-x[↩]
- Bruce A, Pacey IE, Bradbury JA, Scally AJ, Barrett BT. Bilateral changes in foveal structure in individuals with amblyopia. Ophthalmology. 2013 Feb;120(2):395-403. doi: 10.1016/j.ophtha.2012.07.08[↩]
- Meng C, Zhang Y, Wang S. Anisometropic amblyopia: A review of functional and structural changes and treatment. Eur J Ophthalmol. 2023 Jul;33(4):1529-1535. doi: 10.1177/11206721221143164[↩]
- Jang J, Kyung SE. Assessing amblyopia treatment using multifocal visual evoked potentials. BMC Ophthalmol. 2018 Aug 13;18(1):196. doi: 10.1186/s12886-018-0877-0[↩]
- Kelly KR, Jost RM, De La Cruz A, Dao L, Beauchamp CL, Stager D Jr, Birch EE. Slow reading in children with anisometropic amblyopia is associated with fixation instability and increased saccades. J AAPOS. 2017 Dec;21(6):447-451.e1. doi: 10.1016/j.jaapos.2017.10.001[↩][↩]
- Kelly KR, Jost RM, De La Cruz A, Birch EE. Multiple-Choice Answer Form Completion Time in Children With Amblyopia and Strabismus. JAMA Ophthalmol. 2018 Aug 1;136(8):938-941. doi: 10.1001/jamaophthalmol.2018.2295[↩][↩]
- American Academy of Ophthalmology. Amblyopia: Lazy Eye Diagnosis. https://www.aao.org/eye-health/diseases/amblyopia-lazy-eye-diagnosis[↩][↩][↩][↩][↩]
- Kirk VG, Clausen MM, Armitage MD, Arnold RW. Preverbal Photoscreening for Amblyogenic Factors and Outcomes in Amblyopia Treatment: Early Objective Screening and Visual Acuities. Arch Ophthalmol. 2008;126(4):489–492. doi:10.1001/archopht.126.4.489[↩]
- Holmes JM, Lazar EL, Melia BM, Astle WF, Dagi LR, Donahue SP, Frazier MG, Hertle RW, Repka MX, Quinn GE, Weise KK; Pediatric Eye Disease Investigator Group. Effect of age on response to amblyopia treatment in children. Arch Ophthalmol. 2011 Nov;129(11):1451-7. doi: 10.1001/archophthalmol.2011.179[↩]
- US Preventive Services Task Force; Grossman DC, Curry SJ, Owens DK, Barry MJ, Davidson KW, Doubeni CA, Epling JW Jr, Kemper AR, Krist AH, Kurth AE, Landefeld CS, Mangione CM, Phipps MG, Silverstein M, Simon MA, Tseng CW. Vision Screening in Children Aged 6 Months to 5 Years: US Preventive Services Task Force Recommendation Statement. JAMA. 2017 Sep 5;318(9):836-844. doi: 10.1001/jama.2017.11260[↩]
- COMMITTEE ON PRACTICE AND AMBULATORY MEDICINE, SECTION ON OPHTHALMOLOGY, AMERICAN ASSOCIATION OF CERTIFIED ORTHOPTISTS, AMERICAN ASSOCIATION FOR PEDIATRIC OPHTHALMOLOGY AND STRABISMUS, AMERICAN ACADEMY OF OPHTHALMOLOGY, Geoffrey R. Simon, Alexy Darlyn Arauz Boudreau, Cynthia N. Baker, Graham Arthur Barden, Jesse M. Hackell, Amy Peykoff Hardin, Kelley E. Meade, Scot B. Moore, Julia Richerson, Sharon S. Lehman, David B. Granet, Geoffrey E. Bradford, Steven E. Rubin, R. Michael Siatkowski, Donny Won Suh, David B. Granet; Visual System Assessment in Infants, Children, and Young Adults by Pediatricians. Pediatrics January 2016; 137 (1): e20153596. 10.1542/peds.2015-3596[↩]
- American Association for Pediatric Ophthalmology and Strabismus. Vision Screening Recommendations – Techniques for Pediatric Vision Screening. https://aapos.org/terms/conditions/131[↩][↩][↩][↩]
- American Academy of Pediatrics Section on Ophthalmology and Committee on Practice and Ambulatory Medicine, American Academy of Ophthalmology, American Association for Pediatric Ophthalmology and Strabismus. American Association of Certified Orthoptists. Instrument-based pediatric vision screening policy statement. Pediatrics. 2012;130(5):983–986.[↩]
- Kirk VG, Clausen MM, Armitage MD, Arnold RW. Preverbal photoscreening for amblyogenic factors and outcomes in amblyopia treatment: early objective screening and visual acuities. Arch Ophthalmol. 2008;126(4):489–492.[↩]
- Holmes JM, Lazar EL, Melia BM, et al.; Pediatric Eye Disease Investigator Group. Effect of age on response to amblyopia treatment in children. Arch Ophthalmol. 2011;129(11):1451–1457.[↩]
- U.S. Preventive Services Task Force. Screening for visual impairment in children ages 1 to 5 years. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/visual-impairment-in-children-ages-1-5-screening[↩]
- Bui Quoc E, Kulp MT, Burns JG, Thompson B. Amblyopia: A review of unmet needs, current treatment options, and emerging therapies. Surv Ophthalmol. 2023 May-Jun;68(3):507-525. doi: 10.1016/j.survophthal.2023.01.001[↩]
- Powell C, Hatt SR. Vision screening for amblyopia in childhood. Cochrane Database Syst Rev. 2009 Jul 8;(3):CD005020. doi: 10.1002/14651858.CD005020.pub3[↩]
- Hambidge SJ, Emsermann CB, Federico S, Steiner JF. Disparities in pediatric preventive care in the United States, 1993-2002. Arch Pediatr Adolesc Med. 2007 Jan;161(1):30-6. doi: 10.1001/archpedi.161.1.30[↩]
- Wahl MD, Fishman D, Block SS, Baldonado KN, Friedman DS, Repka MX, Collins ME. A Comprehensive Review of State Vision Screening Mandates for Schoolchildren in the United States. Optom Vis Sci. 2021 May 1;98(5):490-499. doi: 10.1097/OPX.0000000000001686[↩]
- Mema SC, McIntyre L, Musto R. Childhood vision screening in Canada: public health evidence and practice. Can J Public Health. 2012 Jan-Feb;103(1):40-5. doi: 10.1007/BF03404067[↩]
- Lequeux L, Thouvenin D, Couret C, Audren F, Costet C, Dureau P, Leruez S, Defoordt-Dhellemmes S, Daien V, Espinasse Berrod MA, Arsene S, Lebranchu P, Denis D, Bui-Quoc E, Speeg-Schatz C. Le dépistage visuel chez l’enfant : les recommandations de l’Association Francophone de Strabologie et d’Ophtalmologie Pédiatrique (AFSOP) [Vision screening for children: Recommended practices from AFSOP]. J Fr Ophtalmol. 2021 Feb;44(2):244-251. French. doi: 10.1016/j.jfo.2020.07.005[↩]
- Tailor V, Bossi M, Greenwood JA, Dahlmann-Noor A. Childhood amblyopia: current management and new trends. Br Med Bull. 2016 Sep;119(1):75-86. doi: 10.1093/bmb/ldw030[↩]
- Handa S, Chia A. Amblyopia therapy in Asian children: factors affecting visual outcome and parents’ perception of children’s attitudes towards amblyopia treatment. Singapore Med J. 2019 Jun;60(6):291-297. doi: 10.11622/smedj.2018151[↩]
- Jeong SH, Kim US. Ten-Year Results of Home Vision-Screening Test in Children Aged 3-6 Years in Seoul, Korea. Semin Ophthalmol. 2015;30(5-6):383-8. doi: 10.3109/08820538.2014.912335[↩]
- Committee on Practice and Ambulatory Medicine, Section on Ophthalmology. American Association of Certified Orthoptists; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology. Eye examination in infants, children, and young adults by pediatricians. Pediatrics. 2003 Apr;111(4 Pt 1):902-7.[↩]
- American Academy of Pediatrics; Section on Ophthalmology; American Association for Pediatric Ophthalmology And Strabismus; American Academy of Ophthalmology; American Association of Certified Orthoptists. Red reflex examination in neonates, infants, and children. Pediatrics. 2008 Dec;122(6):1401-4. doi: 10.1542/peds.2008-2624. Erratum in: Pediatrics. 2009 Apr;123(4):1254.[↩]
- Tingley DH. Vision screening essentials: screening today for eye disorders in the pediatric patient. Pediatr Rev. 2007 Feb;28(2):54-61. doi: 10.1542/pir.28-2-54[↩]
- Hered RW. Effective vision screening of young children in the pediatric office. Pediatr Ann. 2011 Feb;40(2):76-82. doi: 10.3928/00904481-20110117-06[↩][↩][↩][↩]
- Melamud A, Palekar R, Singh A. Retinoblastoma. Am Fam Physician. 2006 Mar 15;73(6):1039-44. Erratum in: Am Fam Physician. 2007 Apr 1;75(7):980. https://www.aafp.org/pubs/afp/issues/2006/0315/p1039.html[↩][↩][↩][↩]
- Reedy-Cooper A, Scartozzi C, Yurkonis T. Childhood Eye Examination in Primary Care. Am Fam Physician. 2023 Jul;108(1):40-50. https://www.aafp.org/pubs/afp/issues/2023/0700/childhood-eye-examination.html[↩][↩]
- Bell AL, Rodes ME, Collier Kellar L. Childhood eye examination [published correction appears in Am Fam Physician. 2014;89(2):76]. Am Fam Physician. 2013;88(4):241-248. https://www.aafp.org/pubs/afp/issues/2013/0815/p241.html[↩][↩][↩]
- Teed RG, Bui CM, Morrison DG, Estes RL, Donahue SP. Amblyopia therapy in children identified by photoscreening. Ophthalmology. 2010;117(1):159–162.[↩]
- Modest JR, Majzoub KM, Moore B, Bhambhani V, McLaughlin SR, Vernacchio L. Implementation of Instrument-Based Vision Screening for Preschool-Age Children in Primary Care. Pediatrics. 2017 Jul;140(1):e20163745. doi: 10.1542/peds.2016-3745[↩]
- Peterseim MMW, Rhodes RS, Patel RN, Wilson ME, Edmondson LE, Logan SA, Cheeseman EW, Shortridge E, Trivedi RH. Effectiveness of the GoCheck Kids Vision Screener in Detecting Amblyopia Risk Factors. Am J Ophthalmol. 2018 Mar;187:87-91. doi: 10.1016/j.ajo.2017.12.020[↩]
- Forcina BD, Peterseim MM, Wilson ME, Cheeseman EW, Feldman S, Marzolf AL, Wolf BJ, Trivedi RH. Performance of the Spot Vision Screener in Children Younger Than 3 Years of Age. Am J Ophthalmol. 2017 Jun;178:79-83. doi: 10.1016/j.ajo.2017.03.014.[↩]
- Arnold RW, O’Neil JW, Cooper KL, Silbert DI, Donahue SP. Evaluation of a smartphone photoscreening app to detect refractive amblyopia risk factors in children aged 1-6 years. Clin Ophthalmol. 2018 Aug 23;12:1533-1537. doi: 10.2147/OPTH.S171935[↩][↩]
- Matta NS, Arnold RW, Singman EL, Silbert DI. Comparison between the plusoptiX and MTI photoscreeners. Arch Ophthalmol. 2009;127(12):1591–1595.[↩]
- Donahue SP, Baker JD, Scott WE, et al. Lions Clubs International Foundation Core Four Photoscreening: results from 17 programs and 400,000 preschool children. J AAPOS. 2006;10(1):44–48.[↩]
- American Academy of Ophthalmology. Amblyopia: Lazy Eye Treatment. https://www.aao.org/eye-health/diseases/amblyopia-lazy-eye-treatment[↩][↩][↩][↩][↩][↩][↩]
- Holmes JM, Melia M, Bradfield YS, Cruz OA, Forbes B; Pediatric Eye Disease Investigator Group. Factors associated with recurrence of amblyopia on cessation of patching. Ophthalmology. 2007;114(8):1427–1432.[↩]
- Repka MX, Beck RW, Holmes JM, Birch EE, Chandler DL, Cotter SA, Hertle RW, Kraker RT, Moke PS, Quinn GE, Scheiman MM, Pediatric Eye Disease Investigator Group. A Randomized Trial of Patching Regimens for Treatment of Moderate Amblyopia in Children. Arch Ophthalmol. 2003 May. https://www.ncbi.nlm.nih.gov/pubmed/12742836[↩]
- Pediatric Eye Disease Investigator Group, Wallace DK, Lazar EL, et al. A Randomized Trial of Increasing Patching for Amblyopia. Ophthalmology. 2013;120(11):10.1016/j.ophtha.2013.04.008. doi:10.1016/j.ophtha.2013.04.008. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3833469/[↩]
- Scheiman MM, Hertle RW, Beck RW, Edwards AR, Birch E, Cotter SA, Crouch ER Jr, Cruz OA, Davitt BV, Donahue S, Holmes JM, Lyon DW, Repka MX, Sala NA, Silbert DI, Suh DW, Tamkins SM, Pediatric Eye Disease Investigator Group. Randomized Trial of Treatment of Amblyopia in Children Aged 7 to 17 Years. Arch Ophthalmol. 2005 Apr. https://www.ncbi.nlm.nih.gov/pubmed/15824215[↩]
- Pediatric Eye Disease Investigator Group. A Randomized Trial of Atropine Vs. Patching for Treatment of Moderate Amblyopia in Children. Arch Ophthalmol. 2002 Mar. https://www.ncbi.nlm.nih.gov/pubmed/11879129[↩]
- Pediatric Eye Disease Investigator Group Writing Committee; Rutstein RP, Quinn GE, Lazar EL, Beck RW, Bonsall DJ, Cotter SA, Crouch ER, Holmes JM, Hoover DL, Leske DA, Lorenzana IJ, Repka MX, Suh DW. A randomized trial comparing Bangerter filters and patching for the treatment of moderate amblyopia in children. Ophthalmology. 2010 May;117(5):998-1004.e6. doi: 10.1016/j.ophtha.2009.10.014[↩]
- Birch EE, Jost RM, De La Cruz A, Kelly KR, Beauchamp CL, Dao L, Stager D Jr, Leffler JN. Binocular amblyopia treatment with contrast-rebalanced movies. J AAPOS. 2019 Jun;23(3):160.e1-160.e5. doi: 10.1016/j.jaapos.2019.02.007[↩]
- Holmes JM, Manh VM, Lazar EL, Beck RW, Birch EE, Kraker RT, Crouch ER, Erzurum SA, Khuddus N, Summers AI, Wallace DK; Pediatric Eye Disease Investigator Group. Effect of a Binocular iPad Game vs Part-time Patching in Children Aged 5 to 12 Years With Amblyopia: A Randomized Clinical Trial. JAMA Ophthalmol. 2016 Dec 1;134(12):1391-1400. doi: 10.1001/jamaophthalmol.2016.4262[↩]
- Pineles SL, Aakalu VK, Hutchinson AK, Galvin JA, Heidary G, Binenbaum G, VanderVeen DK, Lambert SR. Binocular Treatment of Amblyopia: A Report by the American Academy of Ophthalmology. Ophthalmology. 2020 Feb;127(2):261-272. doi: 10.1016/j.ophtha.2019.08.024[↩]
- Li SL, Jost RM, Morale SE, De La Cruz A, Dao L, Stager D Jr, Birch EE. Binocular iPad treatment of amblyopia for lasting improvement of visual acuity. JAMA Ophthalmol. 2015 Apr;133(4):479-80. doi: 10.1001/jamaophthalmol.2014.5515[↩]
- Birch EE, Li SL, Jost RM, Morale SE, De La Cruz A, Stager D Jr, Dao L, Stager DR Sr. Binocular iPad treatment for amblyopia in preschool children. J AAPOS. 2015 Feb;19(1):6-11. doi: 10.1016/j.jaapos.2014.09.009[↩]
- Hess RF, Mansouri B, Thompson B. A new binocular approach to the treatment of amblyopia in adults well beyond the critical period of visual development. Restor Neurol Neurosci. 2010;28(6):793-802. doi: 10.3233/RNN-2010-0550[↩]
- Knox PJ, Simmers AJ, Gray LS, Cleary M. An exploratory study: prolonged periods of binocular stimulation can provide an effective treatment for childhood amblyopia. Invest Ophthalmol Vis Sci. 2012 Feb 21;53(2):817-24. doi: 10.1167/iovs.11-8219. Erratum in: Invest Ophthalmol Vis Sci. 2012;53(10):6196.[↩]
- Gao TY, Guo CX, Babu RJ, Black JM, Bobier WR, Chakraborty A, Dai S, Hess RF, Jenkins M, Jiang Y, Kearns LS, Kowal L, Lam CSY, Pang PCK, Parag V, Pieri R, Raveendren RN, South J, Staffieri SE, Wadham A, Walker N, Thompson B; BRAVO Study Team. Effectiveness of a Binocular Video Game vs Placebo Video Game for Improving Visual Functions in Older Children, Teenagers, and Adults With Amblyopia: A Randomized Clinical Trial. JAMA Ophthalmol. 2018 Feb 1;136(2):172-181. doi: 10.1001/jamaophthalmol.2017.6090[↩]
- Sale A, Berardi N. Active training for amblyopia in adult rodents. Frontiers in Behavioral Neuroscience. 2015;9:281. doi:10.3389/fnbeh.2015.00281. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4621305/[↩]
- Baroncelli L., Sale A., Viegi A., Maya Vetencourt J. F., De Pasquale R., Baldini S., et al. . (2010). Experience-dependent reactivation of ocular dominance plasticity in the adult visual cortex. Exp. Neurol. 226, 100–109. 10.1016/j.expneurol.2010.08.009. https://www.ncbi.nlm.nih.gov/pubmed/20713044[↩]
- Maya Vetencourt J. F., Sale A., Viegi A., Baroncelli L., De Pasquale R., O’Leary O. F., et al. . (2008). The antidepressant fluoxetine restores plasticity in the adult visual cortex. Science 320, 385–388. 10.1126/science.1150516. https://www.ncbi.nlm.nih.gov/pubmed/18420937[↩]
- A cycling lane for brain rewiring. Lunghi C, Sale A. Curr Biol. 2015 Dec 7; 25(23):R1122-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5040496/[↩]
- Scheiman M, Wick B. Clinical management of binocular vision : Heterophoric, accommodative, and eye movement disorders, Fourth ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2014; 732 p.[↩]
- Suttle CM. Active treatments for amblyopia: a review of the methods and evidence base. Clin Exp Optom. 2010 Sep;93(5):287-99. doi: 10.1111/j.1444-0938.2010.00486.x[↩]
- Li RW, Young KG, Hoenig P, Levi DM. Perceptual learning improves visual performance in juvenile amblyopia. Invest Ophthalmol Vis Sci. 2005 Sep;46(9):3161-8. doi: 10.1167/iovs.05-0286[↩]
- Kraus CL, Culican SM. New advances in amblyopia therapy II: refractive therapies. Br J Ophthalmol. 2018 Dec;102(12):1611-1614. doi: 10.1136/bjophthalmol-2018-312173[↩]
- Kelly KR, Jost RM, Wang YZ, Dao L, Beauchamp CL, Leffler JN, Birch EE. Improved Binocular Outcomes Following Binocular Treatment for Childhood Amblyopia. Invest Ophthalmol Vis Sci. 2018 Mar 1;59(3):1221-1228. doi: 10.1167/iovs.17-23235[↩]
- Levi DM. Amblyopia. Handb Clin Neurol. 2021;178:13-30. doi: 10.1016/B978-0-12-821377-3.00002-7[↩]
- Birch EE, Subramanian V, Weakley DR. Fixation instability in anisometropic children with reduced stereopsis. J AAPOS. 2013 Jun;17(3):287-90. doi: 10.1016/j.jaapos.2013.03.011[↩]
- Webber AL. The functional impact of amblyopia. Clin Exp Optom. 2018 Jul;101(4):443-450. doi: 10.1111/cxo.12663[↩]
- Kelly KR, Jost RM, De La Cruz A, Birch EE. Amblyopic children read more slowly than controls under natural, binocular reading conditions. J AAPOS. 2015 Dec;19(6):515-20. doi: 10.1016/j.jaapos.2015.09.002[↩]