Contents
- What is giardiasis
- Chronic giardiasis
- Giardia and Pets
- Can I get Giardia infection from my pet?
- How does my dog or cat get infected with Giardia?
- How do I treat my pet for Giardia infection?
- How do I protect myself if my dog or cat has a Giardia infection?
- If my pet has a Giardia infection, how do I clean and disinfect my house?
- How do I reduce the amount of Giardia in my yard or outdoor environment?
- Giardiasis lifecycle
- Giardiasis causes
- Giardiasis prevention
- Giardiasis complications
- Giardiasis signs and symptoms
- Giardiasis diagnosis
- Giardiasis treatment
What is giardiasis
Giardiasis is a diarrheal illness caused by giardia infection with the tummy protozoan parasite Giardia intestinalis (also known as Giardia lamblia or Giardia duodenalis) that causes symptoms like diarrhea, farting, bloating, nausea, weight loss and abdominal pain 1. Giardiasis usually goes away in about a week if it’s treated, but can sometimes last much longer. In addition to its acute symptoms, giardiasis may also cause anorexia and failure to thrive. Indeed, Giardia infections may have detrimental effects on nutritional status, growth status and cognitive function in humans 2. Giardia infections may also have detrimental effects on body weight in food-producing animals making this a serious concern for the agricultural industry 3.
Giardia is found on surfaces or in soil, food, or water that has been contaminated with feces (poop) from infected humans or animals. Giardia is protected by an outer shell that allows it to survive outside the body for long periods of time and makes it tolerant to chlorine disinfection. While the parasite can be spread in different ways, water (drinking water and recreational water) is the most common mode of transmission.
Giardiasis is a global disease. The prevalence of giardiasis (Giardia lamblia infection) varies in different parts of the world, but it is generally higher in developing countries where reported prevalences range from 3% to 38% 4. Seroprevalence studies suggest that in some settings between 23% and 40% of children are infected before six months of age 5. In developed countries, Giardia lamblia (also known as Giardia intestinalis or Giardia duodenalis) infects about 2% of adults and between 6% to 8% of children, and is responsible for frequent waterborne outbreaks of diarrhea 6. Hörman 2004 7 estimated the prevalence of giardiasis, determined by stool examination, in the Nordic countries (Denmark, Finland, Norway, and Sweden) by combining data from 13 studies; the estimated prevalence in asymptomatic populations was 2.97% and 5.81% in symptomatic populations.
Giardiasis infects nearly 2% of adults and 6% to 8% of children in developed countries worldwide. In the United States, Giardia infection is the most common intestinal parasitic disease affecting humans 8.
People become infected with Giardia by swallowing Giardia cysts (hard shells containing Giardia) found in contaminated food or water. Cysts are instantly infectious once they leave the host through feces (poop) 9. An infected person might shed 1-10 billion cysts daily in their feces (poop) and this might last for several months 9. However, swallowing as few as 10 cysts might cause someone to become ill 9. Giardia may be passed from person-to-person or even from animal-to-person 9, 10. Also, oral-anal contact during sex has been known to cause infection 11. Symptoms of giardiasis normally begin 1 to 3 weeks after a person has been infected 12.
Risk factors for Giardia infection include consuming untreated or inadequately treated water 13, traveling to disease-endemic areas 14, age between one and nine years (particularly in childcare settings), close or intimate contact with infected people 6, poor hygienic conditions (eg living in a household without a latrine or with a mud floor in the sleeping rooms) 15, contact with infected animals 6, and oral-anal sexual contact 6. Giardia cysts can survive for several months in cold water, but once they are ingested and reach the small intestine, they develop into the disease-causing form (trophozoite). A prospective study suggested that the time between infection and the appearance of Giardia lamblia cysts in the stool is 12 to 19 days 16. However, symptoms may appear between one and 75 days after infection and usually at six to 15 days from the date of infection. Symptoms are usually gastrointestinal disturbances 17.
Giardia infection rates have been known to go up in late summer 18. Between 2006-2008 in the United States, known cases of giardiasis were twice as high between June-October as they were between January-March 9.
Giardia trophozoites (disease-causing forms) damage the epithelial absorptive surface and upper intestine. This results in the malabsorption of glucose, sodium, and water, and reduces disaccharidase activity, which can lead to diarrhea and malnutrition. The trophozoites do not invade the surrounding tissues or enter the blood stream, but the immune response results in an increased inflammation of the intestine 19. Generally, giardiasis is a self-limiting clinical illness. The spectrum of giardiasis disease varies from asymptomatic carriage to severe diarrhoea, weight loss, malabsorption, and failure of children to thrive. Acute giardiasis is typically characterized by the sudden onset of acute, watery diarrhoea usually containing neither blood nor pus. Other symptoms may include abdominal cramps, malaise, nausea, vomiting, epigastric pain, bloating, weight loss, and weakness. Acute giardiasis generally resolves in one to four weeks, but may become chronic and persist for months, leading to malabsorption and malnutrition particularly in children 6. Chronic giardiasis may or may not have been preceded by an acute episode, and is typically characterized by intermittent or periodic episodes of diarrhoea, increased flatulence, epigastric pain, and weight loss 20. The infection can be prolonged in people who are immunocompromised 21. Malnutrition and intestinal parasitic infections are common among children in developing countries and have been associated with poor physical development and impaired resistance to infections 22.
Anyone may become infected with Giardia. However, those at greatest risk are 9:
- Travelers to countries where giardiasis is common
- People in childcare settings
- Those who are in close contact with someone who has the disease
- People who swallow contaminated drinking water
- Backpackers or campers who drink untreated water from lakes or rivers
- People who have contact with animals who have the disease
- Men who have sex with men
The risk of humans acquiring Giardia infection from dogs or cats is small 23. The exact type of Giardia that infects humans is usually not the same type that infects dogs and cats 23, 24.
Giardiasis is diagnosed by the identification of cysts or trophozoites in stool specimens, duodenal fluid, or small bowel biopsy. Repeated samplings may be necessary to find the parasite in symptomatic people. Different staining techniques of three separate stool specimens are frequently used to identify cysts; trophozoites are rarely identified in stools and are usually detected in duodenal biopsies 25. Alternate methods used for detection of parasites include antigen detection tests by enzyme-linked immunosorbent assay (ELISA) and immunofluorescence. These tests have a sensitivity of 88% to 98% and a specificity of 87% to 100% 26. About 85% to 90% of cases are detected when three separate stool samples are examined 27. Stool microscopy is relatively inexpensive and commonly used. However if a single stool exam is performed, Giardia lamblia cysts may be missed resulting in under-diagnosis of cases. Duodenal aspirate biopsy (needle aspiration) is more invasive and requires an endoscopy. In direct comparison studies to stool microscopy, this method may have a lower diagnostic yield 28. Notably, the copro-antigen assays are less time-consuming, easier to perform, and more sensitive and specific (over 90%) than stool specimen examination 29.
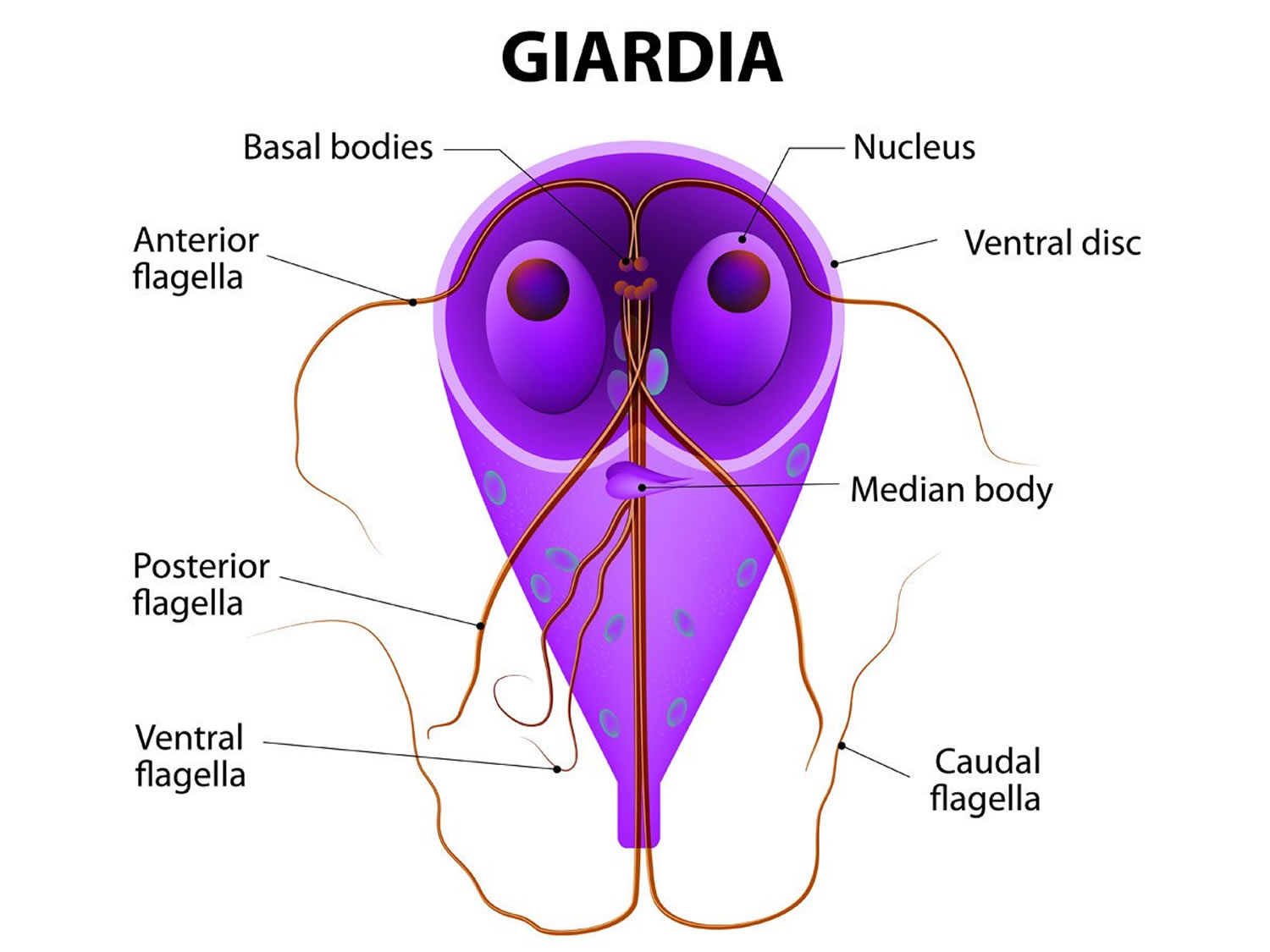
Figure 1. Giardia duodenalis trophozoite (also called Giardia intestinalis or Giardia lamblia)
Note: Giardia duodenalis trophozoites are pear-shaped and measure 10-20 micrometers in length. In permanent, stained specimens, 2 large nuclei are usually visible. The sucking disks (used for attaching to the host’s mucosal epithelium), median bodies, and flagella may also be seen.
How is Giardia spread?
Anything that comes into contact with feces (poop) from infected humans or animals can become contaminated with the Giardia parasite. People and animals become infected when they swallow the parasite. It is not possible to become infected through contact with blood.
How long does Giardia survive in the environment?
- In the soil 30
- In cold temperatures (around 4°C/39.2°F), Giardia can survive for approximately 7 weeks (49 days).
- At room temperature (around 25°C/77°F), Giardia can survive for approximately 1 week (7 days).
- Dry vs. moist surface or environment
- In a dry, warm environment that experiences direct sunlight, Giardia can survive for only a few days 31.
- In a moist, cool environment, Giardia can survive for up to several weeks.
- Water 32
- In water temperatures below 10°C/50°F (for example, lake water or puddle water during the winter, refrigerated water), Giardia can survive for 1–3 months.
- In water temperatures above 10°C/50°F (for example, river water during the fall, tap water, and puddles during the summer), Giardia can survive for less time than in colder temperatures. For example, in water above 37°C/98.6°F, Giardia can survive less than 4 days.
Chronic giardiasis
Until recently, the scientific literature rarely reported extra-intestinal manifestations in giardiasis. However, a recent study estimated that 1/3 of the patients infected with Giardia parasite will express long-term extra-intestinal symptoms, suggesting that this phenomenon is not as uncommon as previously thought 33.
Ocular pathologies
The first description of ocular complications in patients with giardiasis was made by Barraquer 34, who reported cases of iridocyclitis, choroiditis, and retinal hemorrhages in patients that presented diarrhea linked to the presence of Giardia. More recent observations described a “salt and pepper” degeneration (punctuate areas of normal hyperpigmentation on a light yellow pink-retina) involving the retinal pigmented epithelium in children suffering from giardiasis 35. The same complication was described in children with past giardiasis, indicating that the ocular changes observed did not require the concurrent presence of the parasite in the gut 36. Small children appear to be more susceptible to ocular lesions during giardiasis, and the lesions are thought to be caused by damage to the cells of the retina, accompanied by the release of pigment granules in retinal layers, where they can be seen as blackish dots 36. The mechanisms linking ocular lesions with giardiasis remain obscure, but they exclude the possibility of direct invasion by the parasite. It has been speculated that the pigmented degeneration may result from toxic metabolites produced by the parasites, which has yet to be proven 35. The role of increased intestinal permeability in the ocular complications seen in giardiasis needs to be elucidated.
Arthritis
Reactive arthritis is classically seen following infection with enteric pathogens such as Yersinia sp., Salmonella sp., Campylobacter jejuni and Shigella sp., but inflammatory arthritis has also been described following enteric infections with other organisms such as Clostridium difficile, Brucella sp. and Giardia sp. 37. The interval between the preceding infection and the manifestation of arthritis is 2 to 4 week 37. Post-infectious arthritis has a predilection for joints of the lower limbs particularly the knee and ankle 38. Post-infectious reactive arthritis has been classified as a classical spondyloarthropathy associated with human leukocyte antigen (HLA)-B27, an allele of the major histocompatibility complex class I present in 50% of the cases of patients with enteric-infection-related arthritis 39. However, inflammatory arthritis following infection with Clostridium sp. or G. duodenalis does not fit classical spondyloarthropathy, as it fails to show association with HLA-B27 37. Therefore, these are referred to enteric-infection-related-arthritides. Although G. duodenalis infections account for a significant proportion of enteric infections worldwide, reports of an association with post-infectious arthritis are relatively few. Little is known of the pathogenesis of arthritis in these conditions. Unlike post-enteric reactive arthritis, these arthritides are characteristically responsive to antibiotic therapies 39. The variable degrees of host immune responses, and the lack of a robust systemic inflammatory response, may account for the infrequency of post-giardiasis arthritis despite the high prevalence rate of the infection 37. Antigens from enteric bacteria have been isolated from the synovial fluid of affected joints 39. In a case of Yersinia pseudotuberculosis reactive arthritis, evidence of viable bacteria within the joint was demonstrated over a year later 40. Here again, a possible role for increased intestinal permeability in enteric-infection-related-arthritis warrants further investigation.
Allergies
Concomitant presence of G. duodenalis, cutaneous allergic manifestations, and gastrointestinal symptoms have been described, which may explain why complete symptom resolution can be achieved with metronidazole and corticosteroids 41. Significant anecdotal evidence suggests a causative link between giardiasis and the development of urticaria. In a recent study in children, giardiasis was associated with an increase in total serum immunoglobulin E (IgE) levels, and an enhanced IgE antibody response to common allergens 42. These patients also demonstrated IgE reactivity to cow’s milk and Giardia antigens. These observations suggests that alteration in antigen uptake from the small intestine during giardiasis, perhaps in association with connective tissue mast cell proliferation, may contribute to the development of allergic disease 43. Dysfunction of the intestinal barrier during giardiasis may facilitate the translocation of food macromolecules and in turn prime the host for sensitization 42.
Muscular complications
Hypokalemic myopathy has been associated with celiac disease, radiation enteropathy, immunosuppressive drugs, and various infectious diseases. In the patient, this presents as marked proximal muscular weakness in all four limbs and the neck 44. Analyses of muscular biopsies reveal an abnormal size of the muscular fiber due to the presence of numerous rounded atrophic and hypertrophic fibers, proliferation of myonuclei, and necrotic fibers 45. The findings are consistent with impairment of muscle excitability and denervation due to muscle necrosis. Analysis of these fiber components showed that glycogen and lipid levels, as well as the inter-myofibrillar network pattern, are normal 45. Several cases of myopathy following hypokalemia induced by giardiasis have been reported in both immunocompetent and immunocompromised patients 45. This suggests that G. duodenalis infections can trigger muscular manifestations independently of the immune status of the host. During giardiasis, potassium loss is closely related to the number of bouts of diarrhea per day 46. Loss of potassium result in hypokalemia which can trigger a severe and transient myopathy 45. In fact, muscular symptoms can improve with increased levels of potassium and recovery from diarrhea 44. However, G. duodenalis diarrhea as a cause of myopathy due to hypokalemia is rare. It seems that the duration of symptoms is crucial for development of hypokalemic myopathy 45. Giardiasis-associated hypokalemia occurs more often in elderly people, particularly women, who are hospitalized for giardiasis 47. The causes, and the clinical consequences, of Giardia-associated hypokalemia remain unclear. It has been suggested that giardiasis-induced impairment of nutrient and electrolyte absorption may contribute at least in part to hypokalemia and hyponatremia 48.
Nutritional consequences
In developing countries of the world, because of infectious diseases and lack of food, 206 million children under 5 years of age suffer from stunting, 50 million from chronic wasting disease, and 167 million are grossly underweight 49. Growth failure, reflected in stunting, wasting and underweight conditions, is assessed by anthropometric indices of height-for-age, weight-for-age, and weight-for-height 50. Optimum health for children has long been linked to physical, socio-cultural, economic and environmental factors. In developing countries, the incidence of giardiasis is often over four times higher than the incidence reported in industrialized countries 51. Children between 6 mo and 5 years of age are the most susceptible 52. In combination with diarrhea, G. duodenalis infection can cause iron deficiency anemia, micronutrient deficiencies, protein-energy malnutrition, growth and cognitive retardation, and malabsorption 53. Studies conducted on children from Brazil and Peru found that diarrheal disease occurring in the first 2 years of life negatively correlates with cognitive function, verbal fluency, and physical fitness, and may lead to long-term growth faltering 54. These studies demonstrate that the effects of early childhood diarrhea are more far-reaching than merely causing dehydration. Diarrhea caused by Giardia sp. or Cryptosporidium sp. has frequently been associated with stunting and lower cognitive function 54 (see Table 1). Intriguingly, a recent study observed that in a cohort of Tanzanian children infected with Giardia, infection had a protective role against diarrhea, and that this protection was lost with multi-nutrient supplementation 55. Research needs to determine whether these interesting findings reflect a negative regulation by Giardia sp. of other enteric pathogenic processes that may occur in these children.
Table 1. International reports of post-giardiasis metabolic consequences
| Post-giardiasis effects | Country | Selected references |
| Lower cognitive function | India, Peru, Turkey | 56 |
| Lower intellectual quotient | ||
| Lower social quotient | ||
| Lower weight | Brazil, Columbia, Ecuadora, Guatemala, Iran, Israel, Mexico, Rwanda, Turkey, United States | 2 |
| Lower height | ||
| Stunting | ||
| Failure to Thrive | Columbia, Ecuadora, United States | 57 |
| Nutrient deficiencies | Iran, Mexico, Tanzania | 58 |
Functional gastrointestinal disorders
Functional gastrointestinal disorders represent a group of disorders characterized by recurring or chronic gastrointestinal symptoms without an identifiable disease process. Irritable bowel syndrome (IBS) and functional dyspepsia are the best described functional gastrointestinal disorders. Post-infectious-IBS has been reported following acute gastroenteritis due to bacteria such as Salmonella sp., Shigella sp. and Campylobacter jejuni. Recent evidence now indicates that a proportion of patients diagnosed with Giardia duodenalis will also develop post-infectious-IBS symptoms in the absence of detectable parasitic loads 60, 61.
Early reports indicated that Giardia may cause prolonged symptoms, including secondary lactose intolerance, for several weeks after successful treatment 62. Chronic giardiasis resembles irritable bowel syndrome (IBS), and symptomatic infection may exacerbate existing IBS 63. Giardia infection has been diagnosed in 5%-10% of patients with IBS[101,102], and it was recently demonstrated that G. duodenalis may indeed cause irritable bowel syndrome (IBS) and functional dyspepsia 61. High frequency of microscopic duodenal inflammation was found in patients post-giardiasis when the infection lasted 2-4 month, further supporting the hypothesis that longer duration of infection is a risk factor for post-infectious-IBS 64. Early diagnosis of Giardia infection and treatment may shorten the duration of the infection and hence may help reduce the risk for such complications 65.
Giardia and Pets
Giardia intestinalis (aka: Giardia duodenalis, Giardia lamblia) is a common, microscopic (intestinal) parasite that commonly affects humans, dogs, and cats 66.
Common signs and symptoms of Giardia infection (in both humans and pets) are diarrhea, gas, abdominal discomfort, nausea, and vomiting. However, it is possible to be infected and have no signs or symptoms of illness 67.
Can I get Giardia infection from my pet?
The risk of humans acquiring Giardia infection from dogs or cats is small 68. The exact type of Giardia that infects humans is usually not the same type that infects dogs and cats 24, 23, 69.
Note: If you own other household or exotic pets, please contact your veterinarian. Seek further information, as some rodents and other species can harbor human strains of Giardia.
How does my dog or cat get infected with Giardia?
Your dog or cat might get infected by:
- Being in contact with infected feces (poop) from another dog or cat
- Rolling and playing in contaminated soil
- Licking its body after contact with a contaminated surface (for example, a dirty litter box or dog cage or crate)
- Drinking water from a contaminated creek, pond, or other body of water
Young pets, like puppies and kittens, have a higher risk of illness than adult dogs and cats.
How do I treat my pet for Giardia infection?
- If your pet has persistent diarrhea, seek veterinary care. Diarrhea has different causes and could result in dehydration or other serious complications.
- Diagnosis and treatment of Giardia infection must be done by a licensed veterinarian.
- No approved over-the-counter treatment is available for Giardia infection.
- Giardia can be passed in stool intermittently, and an animal may appear healthy or without signs of disease before it stops passing Giardia. Repeated fecal tests may be necessary 68.
- Follow your veterinarian’s recommendations, and take your pet to all follow-up appointments.
How do I protect myself if my dog or cat has a Giardia infection?
The risk of acquiring Giardia infection from your dog or cat is small. However, there are some steps you can take to minimize your exposure to Giardia if you have dogs or cats:
- Wear gloves when gardening to reduce the risk of coming into contact with infected feces (poop) or soil.
- Clean household surfaces regularly.
- Clean and disinfect areas that your pet has access to—as well as items like toys, bedding, and water and food bowls—regularly.
- Wash hands frequently and properly:
- Wet your hands with clean, running water (warm or cold) and apply soap.
- Rub your hands together to make a lather and scrub them well; be sure to scrub the backs of your hands, between your fingers, and under your nails.
- Continue rubbing your hands for at least 20 seconds.
- Rinse your hands well under running water.
- Dry your hands using a clean towel or air dry them.
If my pet has a Giardia infection, how do I clean and disinfect my house?
Giardia is hard to completely eliminate from the environment, but there are things you can do to decrease the risk of your pets’ reinfection and of human infection.
Hard surfaces (for example: cement and tile floors, crates, tables, trash cans, etc.)
- Cleaning
- Wear gloves.
- Remove feces and discard in a plastic bag.
- Clean and scrub surfaces using soap. Rinse surface thoroughly until no obvious visible contamination is present.
- Disinfection
- Wear gloves.
- Disinfect according to manufacturer guidelines using one of the following:
- Follow product instructions, ensuring the product stays in contact with the surface for the recommended amount of time.
- Rinse with clean water.
- Carpet / Upholstered Furniture
- Cleaning
- Wear gloves.
- If feces are on a carpet or upholstered furniture, remove them with absorbent material (for example, double layered paper towels).
- Place and discard the feces in a plastic bag.
- Clean the contaminated area with regular detergent or carpet cleaning agent.
- Allow carpet or upholstered furniture to fully dry.
- Disinfection
- Wear gloves.
- Steam clean the area at 158°F (70 °C) for 5 minutes or 212°F (100 °C) for 1 minute.
- Quaternary ammonium compound products (QATS) are found in some carpet cleaning products and can also be used after cleaning to disinfect. Read the product labels for specifications, and follow all instructions.
- Cleaning
- Other items (toys, clothing, pet bed, etc.)
- Household items should be cleaned and disinfected daily while a dog or cat is being treated for Giardia infection.
- Dishwasher
- Dishwasher-safe toys and water and food bowls can be disinfected in a dishwasher that has a dry cycle or a final rinse that exceeds one of the following:
- 113°F (45 °C) for 20 minutes
- 122°F (50 °C) for 5 minutes
- 162°F (72.2 °C) for 1 minute
- If a dishwasher is not available, submerge dishwasher-safe items in boiling water for at least 1 minute (at elevations above 6,500 feet, boil for 3 minutes).
- Dishwasher-safe toys and water and food bowls can be disinfected in a dishwasher that has a dry cycle or a final rinse that exceeds one of the following:
- Washer and Dryer
- Clothing, some pet items (for example, bedding and cloth toys) and linens (sheets and towels) can be washed in the washing machine and then heat-dried on the highest heat setting for 30 minutes.
- If a clothes dryer is not available, allow clothes to thoroughly air dry under direct sunlight.
How often and for how long should I clean and disinfect my home after my dog or cat is diagnosed with Giardia infection?
- Clean and disinfect potentially contaminated items (toys, water bowls and food bowls, pet bedding, floors, dog crates, linens, towels, litter box, etc.) regularly for as long as your pet is sick.
- If your pet is taking medication, clean and disinfect frequently (daily if possible) until a few days after the last dose of medication is given.
- Giardia survival depends on many factors, so we recommend that you consult your veterinarian for further advice.
How do I reduce the amount of Giardia in my yard or outdoor environment?
Giardia is hard to completely eliminate from the environment, but there are things you can do to help decrease the risk of pet reinfection and of human infection. Please remember that despite your best efforts to clean the environment, Giardia can persist in outdoor spaces and pet reinfection is possible 68.
- Wear gloves when handling feces.
- Remove feces promptly and put them in a plastic bag.
- Limit access to common outdoor spaces, where possible, if pets have diarrhea or are being treated for Giardia.
- Eliminate any source of standing water (for example, puddles, containers with water, and fountains that are not in use).
- Do NOT attempt to use bleach or quaternary ammonium compound products (the active ingredient may be listed as alkyl dimethyl ammonium chloride) in your soil or grass area, as they will be ineffective.
- Do NOT allow any new animals, especially young ones, to enter the yard or other outdoor space until advised by your veterinarian.
How do I prevent my dog or cat from getting re-infected, or sickening my other pets, during treatment?
- If you have other dogs or cats, make sure you tell your veterinarian even if they are not showing signs of diarrhea. Other pets may also be put on medicine depending on the situation. Even animals showing no signs of Giardia infection could be infected and shedding Giardia into the environment 68.
- Bathe all household pets with pet shampoo following medical treatment to ensure no fecal residue is in the pet’s coat 70.
- Clean dogs’ and cats’ environment, as described above (holding areas, floors, crate, etc.) and wash water bowls daily with soap and water.
- Limit your dog’s access to untreated surface water (creeks, ponds, lakes) to avoid re-infecting your animal and contaminating the water which could make other animals sick.
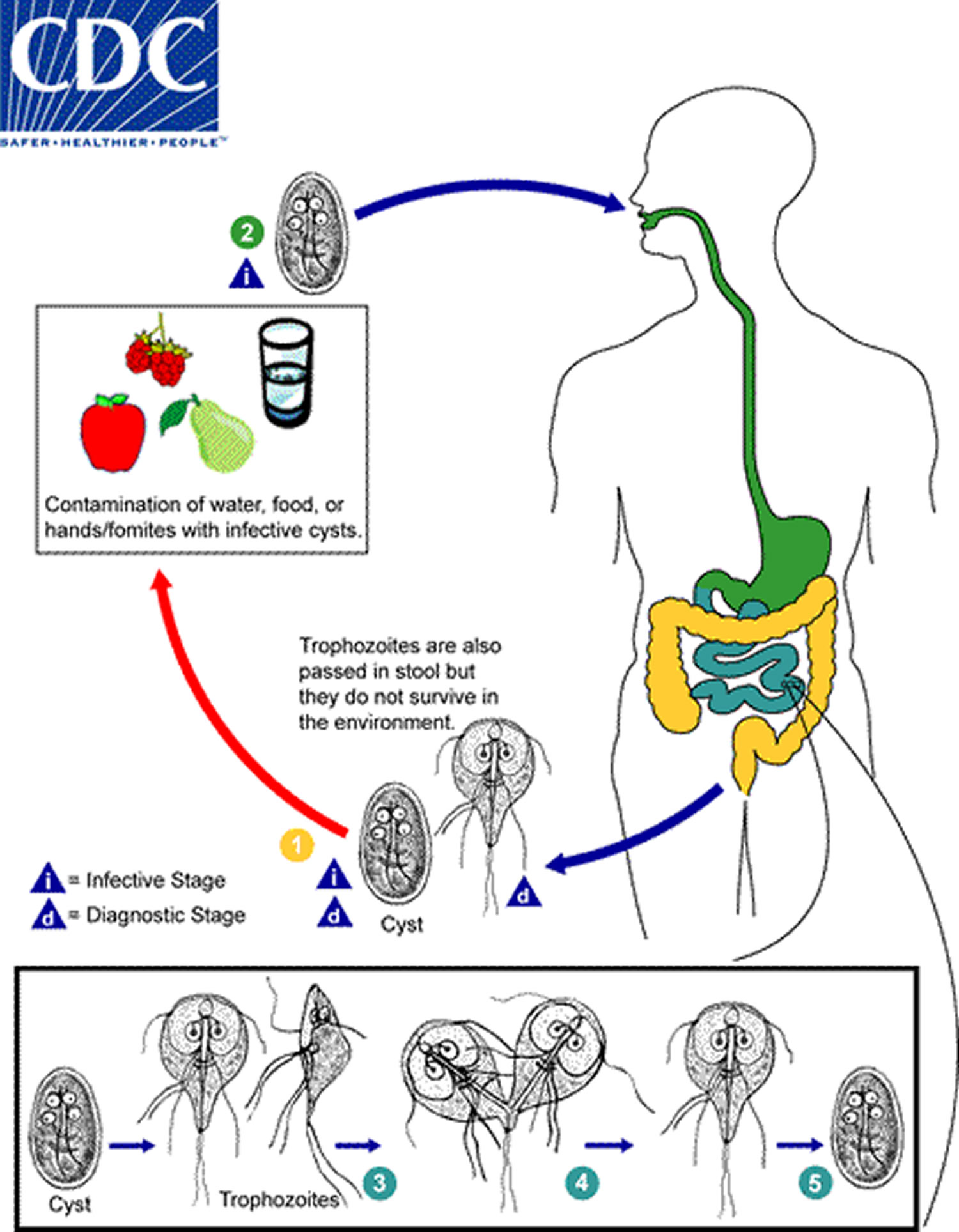
Giardiasis lifecycle
Giardia duodenalis is a protozoan flagellate (Diplomonadida). This protozoan was initially named Cercomonas intestinalis by Lambl in 1859. It was renamed Giardia lamblia by Stiles in 1915 in honor of Professor A. Giard of Paris and Dr. F. Lambl of Prague. However, many consider the name, Giardia duodenalis, (Davaine 1875) to be the correct taxonomic name for this protozoan.
- Cysts are resistant forms and are responsible for transmission of giardiasis. Both cysts and trophozoites can be found in the feces (diagnostic stages). The cysts are hardy and can survive several months in cold water.
- Infection occurs by the ingestion of cysts in contaminated water, food, or by the fecal-oral route (hands or fomites).
- In the small intestine, excystation releases trophozoites (each cyst produces two trophozoites).
- Trophozoites multiply by longitudinal binary fission, remaining in the lumen of the proximal small bowel where they can be free or attached to the mucosa by a ventral sucking disk. Encystation occurs as the parasites transit toward the colon.
- The cyst is the stage found most commonly in nondiarrheal feces. Because the cysts are infectious when passed in the stool or shortly afterward, person-to-person transmission is possible. While animals are infected with Giardia, their importance as a reservoir is unclear.
Clinical Presentation
The spectrum varies from asymptomatic carriage to severe diarrhea and malabsorption. Acute giardiasis develops after an incubation period of 1 to 14 days (average of 7 days) and usually lasts 1 to 3 weeks. Symptoms include diarrhea, abdominal pain, bloating, nausea, and vomiting. In chronic giardiasis the symptoms are recurrent and malabsorption and debilitation may occur.
Figure 2. Giardiasis lifecycle
Giardiasis causes
Giardia parasites live in the intestines of people and animals. Before the microscopic parasites are passed in stool, they become encased within hard shells called cysts, which allows them to survive outside the intestines for months. Once inside a host, the cysts dissolve and the parasites are released.
Infection occurs when you accidentally ingest the parasite cysts. This can occur by swallowing contaminated water, by eating contaminated food or through person-to-person contact.
Swallowing contaminated water
The most common way to become infected with giardia is after swallowing contaminated water. Giardia parasites are found in lakes, ponds, rivers and streams worldwide, as well as in municipal water supplies, wells, cisterns, swimming pools, water parks and spas. Ground and surface water can become contaminated from agricultural runoff, wastewater discharge or animal feces. Children in diapers and people with diarrhea may accidentally contaminate pools and spas.
Eating contaminated food
Giardia parasites can be transmitted through food — either because food handlers with giardiasis don’t wash their hands thoroughly or because raw produce is irrigated or washed with contaminated water. Because cooking food kills giardia, food is a less common source of infection than water is, especially in industrialized countries.
Person-to-person contact
You can contract giardiasis if your hands become contaminated with fecal matter — parents changing a child’s diapers are especially at risk. So are child care workers and children in child care centers, where outbreaks are increasingly common. The giardia parasite can also spread through anal sex.
Risk factors for giardiasis
The giardia parasite is a very common intestinal parasite. Although anyone can pick up giardia parasites, some people are especially at risk:
- Children. Giardia infection is far more common in children than it is in adults. Children are more likely to come in contact with feces, especially if they wear diapers, are toilet training or spend time in a child care center. People who live or work with small children also are at higher risk of developing giardia infection.
- People without access to safe drinking water. Giardiasis is rampant wherever sanitation is inadequate or water isn’t safe to drink. You’re at risk if you travel to places where giardiasis is common, especially if you aren’t careful about what you eat and drink. The risk is greatest in rural or wilderness areas.
- People who have anal sex. Having anal sex without using a condom puts you at increased risk of giardia infection, as well as sexually transmitted infections.
Giardiasis prevention
No drug or vaccine can prevent giardia infection. But common-sense precautions can go a long way toward reducing the chances that you’ll become infected or spread the infection to others.
- Wash your hands. This is the simplest and best way to prevent most kinds of infection. Wash your hands after using the toilet or changing diapers and before eating or preparing food. When soap and water aren’t available, alcohol-based sanitizers are an excellent alternative.
- Purify wilderness water. Avoid drinking untreated water from shallow wells, lakes, rivers, springs, ponds and streams unless you filter it or boil it for at least 10 minutes at 158 °F (70 °C) first.
- Keep your mouth closed. Try not to swallow water when swimming in pools, lakes or streams.
- Use bottled water. When traveling to parts of the world where the water supply is likely to be unsafe, drink and brush your teeth with bottled water that you open yourself. Don’t use ice, and avoid raw fruits and vegetables, even those you peel yourself.
- Practice safer sex. If you engage in anal sex, use a condom every time. Avoid oral-anal sex unless you’re fully protected.
Giardiasis complications
Giardia infection is almost never fatal in industrialized countries, but it can cause lingering symptoms and serious complications, especially in infants and children. The most common complications include:
- Dehydration. Often a result of severe diarrhea, dehydration occurs when the body doesn’t have enough water to carry out its normal functions.
- Failure to thrive. Chronic diarrhea from giardia infection can lead to malnutrition and harm children’s physical and mental development.
- Lactose intolerance. Many people with giardia infection develop lactose intolerance — the inability to properly digest milk sugar. The problem may persist long after the infection has cleared.
Giardiasis signs and symptoms
Giardiasis is the most frequently diagnosed intestinal parasitic disease in the United States and among travelers with chronic diarrhea 71. Signs and symptoms may vary and can last for 1 to 2 weeks or longer. In some cases, people infected with Giardia have no symptoms, but still carry the parasite and can spread it to others through their stool.
Acute symptoms include 10:
- Watery, sometimes foul-smelling diarrhea that may alternate with soft, greasy stools
- Gas
- Greasy stools that tend to float
- Stomach or abdominal cramps
- Upset stomach or nausea/vomiting
- Dehydration (loss of fluids)
- Fatigue or malaise
- Bloating
- Gas or flatulence
- Nausea
- Weight loss
Other, less common symptoms include itchy skin, hives, and swelling of the eye and joints 72. Sometimes, the symptoms of giardiasis might seem to resolve, only to come back again after several days or weeks. Giardiasis can cause weight loss and failure to absorb fat, lactose, vitamin A and vitamin B12 73.
In children, severe giardiasis might delay physical and mental growth, slow development, and cause malnutrition 74.
Giardiasis diagnosis
Giardiasis is diagnosed by the identification of cysts or trophozoites in the feces, using direct mounts as well as concentration procedures. Cysts are typically seen in wet mount preparations, while trophozoites are seen in permanent mounts (i.e. trichrome). Repeated samplings may be necessary. In addition, samples of duodenal fluid (e.g., Enterotest) or duodenal biopsy may demonstrate trophozoites. Alternate methods for detection include antigen detection tests by enzyme immunoassays, and detection of parasites by immunofluorescence. Both methods are available in commercial kits.
Basic guidelines
- A. Multiple stool samples (at least 3) should be tested before a negative result is reported.
- B. To maximize recovery of cysts, stool samples in formalin, or other fixatives, should be concentrated prior to microscopic examination (e.g., 10 min at 500 × g when using the formalin-ethyl acetate concentration procedure).
- Exception:
- Specimens to be used for EIA or rapid cartridge assays should NOT be concentrated because antigens are lost during the procedure!
- Exception:
- C. Choice of diagnostic techniques depends on available equipment and reagents, experience, and considerations of time and cost.
Because Giardia cysts can be excreted intermittently, multiple stool collections (i.e., three stool specimens collected on separate days) increase test sensitivity 75. The use of concentration methods and trichrome staining might not be sufficient to identify Giardia because variability in the concentration of organisms in the stool can make this infection difficult to diagnose. For this reason, fecal immunoassays that are more sensitive and specific should be used 76.
Rapid immune-chromatographic cartridge assays also are available but should not take the place of routine ova and parasite examination 76. Only molecular testing (e.g., polymerase chain reaction or PCR) can be used to identify the subtypes of Giardia.
Direct Immunofluorescence Assay (DFA)
A direct immunofluorescence assay (DFA) is available for diagnosing Giardia duodenalis infections. Antibodies tagged with fluorescent markers are added to stool and incubated. This test includes antibodies for Cryptosporidium and both diseases can be tested for simultaneously. Visualization under a fluorescent microscope shows the Giardia cysts as green, glowing ovoid objects.
This technique offers the highest combination of sensitivity and specificity and is considered the gold standard by many laboratories. For commercial direct immunofluorescence assay (DFA) kits, it is recommended that a concentrated stool specimen be used to increase the probability of detection of low numbers of cysts. However, special equipment (fluorescence microscope) and commercially available test kits are required and it does not provide a permanently stained slide that can be archived.
Enzyme immunoassay (EIA)
The enzyme immunoassay (EIA) does not rely on microscopy and is useful for screening large numbers of specimens. Borderline positives and questionable negatives obtained with this technique should be further confirmed by direct immunofluorescence assay (DFA). Antigens of Giardia are detected in the feces using this method; therefore, specimens should not be concentrated prior to testing. However, special equipment (microplate reader) and commercially available test kits are required.
Rapid immunochromatographic cartridge assays
The rapid cartridge assays may be used with preserved specimens and are quick and easy to perform. Antigens of Giardia are detected in the feces using this method; therefore, specimens should not be concentrated prior to testing. Borderline positives and questionable negatives obtained with this technique should be further confirmed by direct immunofluorescence assay (DFA). No special equipment is needed.
Giardiasis treatment
Several drugs can be used to treat giardiasis. Effective treatments include metronidazole, albendazole, tinidazole, and nitazoxanide 77, 78. Alternatives to these medications include paromomycin, quinacrine, and furazolidone 79. Some of these drugs may not be routinely available in the United States.
- Metronidazole (Flagyl). Metronidazole is the most commonly used antibiotic for giardia infection. Side effects may include nausea and a metallic taste in the mouth. Don’t drink alcohol while taking this medication.
- Tinidazole (Tindamax). Tinidazole works as well as metronidazole and has many of the same side effects, but it can be given in a single dose.
- Nitazoxanide (Alinia). Because it comes in a liquid form, nitazoxanide may be easier for children to swallow. Side effects may include nausea, flatulence, yellow eyes and brightly colored yellow urine.
Different factors may shape how effective a drug regimen will be, including medical history, nutritional status, and condition of the immune system 78. Therefore, it is important to discuss treatment options with a healthcare provider.
There are no consistently recommended medications for giardiasis in pregnancy because of the potential for adverse drug effects to the baby. If your symptoms are mild, your doctor may recommend delaying treatment until after the first trimester. If treatment is necessary, discuss the best available treatment option with your doctor.
- Roxström-Lindquist K, Palm D, Reiner D, Ringqvist E, Svärd SG. Giardia immunity–an update. Trends Parasitol. 2006;22:26–31. http://www.cell.com/trends/parasitology/fulltext/S1471-4922(05)00311-9[↩]
- Farthing MJ, Mata L, Urrutia JJ, Kronmal RA. Natural history of Giardia infection of infants and children in rural Guatemala and its impact on physical growth. Am J Clin Nutr. 1986;43:395–405. https://www.ncbi.nlm.nih.gov/pubmed/3953479[↩][↩]
- Geurden T, Vercruysse J, Claerebout E. Field testing of a fenbendazole treatment combined with hygienic and management measures against a natural Giardia infection in calves. Vet Parasitol. 2006;142:367–371 https://www.ncbi.nlm.nih.gov/pubmed/16959430[↩]
- de Souza EA, da Silva-Nunes M, Malafronte Rdos S, Muniz PT, Cardoso MA, Ferreira MU. Prevalence and spatial distribution of intestinal parasitic infections in a rural Amazonian settlement, Acre State, Brazil. Cadernos de Saúde Pública 2007;23(2):427-34. https://www.ncbi.nlm.nih.gov/pubmed/17221092[↩]
- Abdel Fattah SM, Maklad KA, Gadallah MA. Age-related rate of seropositivity of antibody to Giardia lamblia in different age groups in Cairo. Journal of the Egyptian Society of Parasitology 1991;21(3):707-13. https://www.ncbi.nlm.nih.gov/pubmed/1765682[↩]
- Yoder JS, Beach MJ, Centers for Disease Control and Prevention (CDC). Giardiasis surveillance – United States, 2003-2005. MMWR Surveillance summaries 2007;56(7):11-8. https://www.cdc.gov/mmwr/preview/mmwrhtml/ss5607a2.htm[↩][↩][↩][↩][↩]
- Hörman A, Korpela H, Sutinen J, Wedel H, Hänninen ML. Meta-analysis in assessment of the prevalence and annual incidence of Giardia spp. and Cryptosporidium spp. infections in humans in the Nordic countries. International Journal for Parasitology 2004;34(12):1337-46. https://www.ncbi.nlm.nih.gov/pubmed/15542094[↩]
- Kappus KD, Lundgren RG, Jr., Juranek DD, Roberts JM, Spencer HC. Intestinal parasitism in the United States: update on a continuing problem. Am J Trop Med Hyg. 1994;50(6):705-13. http://www.ajtmh.org/content/journals/10.4269/ajtmh.1994.50.705[↩]
- CDC. Giardiasis surveillance – United States, 2006-2008. MMWR Morb Mortal Wkly Rep. 2010;59(SS06):15-25. https://www.cdc.gov/mmwr/preview/mmwrhtml/ss5906a2.htm[↩][↩][↩][↩][↩][↩]
- Robertson LJ, Hanevik K, Escobedo AA, Morch K, Langeland N. Giardiasis–why do the symptoms sometimes never stop? Trends Parasitol. 2010;26(2):75-82. http://www.cell.com/trends/parasitology/fulltext/S1471-4922(09)00261-X[↩][↩]
- Escobedo AA, Cimerman S. Giardiasis: a pharmacotherapy review. Expert Opin Pharmacother. 2007;8(12):1885-1902.[↩]
- Rendtorff RC. The experimental transmission of human intestinal protozoan parasites. II. Giardia lamblia cysts given in capsules.Am J Hyg. 1954;59(2):209-20. https://academic.oup.com/aje/article-abstract/59/2/209/89320[↩]
- Pinheiro Ide O, de Castro MF, Mitterofhe A, Pires FA, Abramo C, Ribeiro LC, et al. Prevalence and risk factors for giardiasis and soil-transmitted helminthiasis in three municipalities of Southeastern Minas Gerais State, Brazil: risk factors for giardiasis and soil-transmitted helminthiasis. Parasitology Research 2011;108(5):1123-30. https://www.ncbi.nlm.nih.gov/pubmed/21243507[↩]
- Freedman DO, Weld LH, Kozarsky PE, Fisk T, Robins R, von Sonnenburg F, et al. Spectrum of disease and relation to place of exposure among ill returned travelers. New England Journal of Medicine 2006;354(2):119-30. http://www.nejm.org/doi/full/10.1056/NEJMoa051331[↩]
- Mahmud MA, Chappell C, Hossain MM, Habib M, Dupont HL. Risk factors for development of first symptomatic Giardia infection among infants of a birth cohort in rural Egypt. American Journal of Tropical Medicine and Hygiene 1995;53(1):84-8. https://www.ncbi.nlm.nih.gov/pubmed/7625540[↩]
- Jokipii AM, Hemila M, Jokipii L. Prospective study of acquisition of Cryptosporidium, Giardia lamblia, and gastrointestinal illness. Lancet 1985;2(8453):487-9. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(85)90412-X/abstract[↩]
- Fricker CR, Medema GD, Smith HV. Protozoan parasites (Cryptosporidium, Giardia, Cyclospora). Guidelines for drinking-water quality. Second Edition. Geneva: World Health Organization, 1993:70-118.[↩]
- Naumova EN, Jagai JS, Matyas B, DeMaria A, Jr., MacNeill IB, Griffiths JK. Seasonality in six enterically transmitted diseases and ambient temperature. Epidemiol Infect. 2007;135(2):281-92. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2870561/[↩]
- Buret A. Mechanisms of epithelial dysfunction in giardiasis. Gut 2007;56(3):316-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1856818/[↩]
- American Academy of Pediatrics. Red book: Report of the Committee on Infectious Diseases. 27th Edition. Illinois: Academy of Pediatrics, 2006.[↩]
- Newman RD, Moore SR, Lima AA, Nataro JP, Guerrant RL, Sears CL. A longitudinal study of Giardia lamblia infection in north-east Brazilian children. Tropical Medicine and International Health 2001;6(8):624-34. https://www.ncbi.nlm.nih.gov/pubmed/11555428[↩]
- Mukhopadhyay C, Wilson G, Pradhan D, Shivananda PG. Intestinal protozoal infestation profile in persistent diarrhea in children below age 5 years in western Nepal. Southeast Asian Journal of Tropical Medicine and Public Health 2007;38(1):13-9. https://www.ncbi.nlm.nih.gov/pubmed/17539240[↩]
- Feng Y, Xiao L. Zoonotic potential and molecular epidemiology of Giardia species and giardiasis. Clin Microbiol Rev. 2011;24(1):110-40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3021202/[↩][↩][↩]
- Berrilli F, Di Cave D, De Liberato C, Franco A, Scaramozzino P, Orecchia P. Genotype characterisation of Giardia duodenalis isolates from domestic and farm animals by SSU-rRNA gene sequencing. Vet Parasitol. 2004;122:193-9. https://www.ncbi.nlm.nih.gov/pubmed/15219360[↩][↩]
- Mank TG, Zaat JO. Diagnostic advantages and therapeutic options for giardiasis. Expert Opinion on Investigational Drugs 2001;10(8):1513-9. https://www.tandfonline.com/doi/abs/10.1517/13543784.10.8.1513[↩]
- Weitzel T, Dittrich S, Möhl I, Adusu E, Jelinek T. Evaluation of seven commercial antigen detection tests for Giardia and Cryptosporidium in stool samples. Clinical Microbiology and Infection 2006;12(7):656-9. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1469-0691.2006.01457.x[↩]
- Hiatt RA, Markell EK, Ng E. How many stool examinations are necessary to detect pathogenic intestinal protozoa?. American Journal of Tropical Medicine and Hygiene 1995;53(1):36-9. https://www.ncbi.nlm.nih.gov/pubmed/7625530[↩]
- Hanevik K, Hausken T, Morken MH, Strand EA, Mørch K, Coll P, et al. Persisting symptoms and duodenal inflammation related to Giardia duodenalis infection. Journal of Infection 2007;55(6):524-30. https://www.ncbi.nlm.nih.gov/pubmed/17964658[↩]
- Garcia LS, Garcia JP. Detection of Giardia lamblia antigens in human fecal specimens by a solid-phase qualitative immunochromatographic assay. Journal of Clinical Microbiology 2006;44(12):4587-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1698425/[↩]
- Erickson MC, Ortega YR. Inactivation of protozoan parasites in food, water, and environmental systems. J Food Protect. 2006;69:2786–808. https://www.ncbi.nlm.nih.gov/pubmed/17133829[↩]
- Erickson MC, Ortega YR. Inactivation of protozoan parasites in food, water, and environmental systems. J Food Protect. 2006;69:2786–808. https://www.ncbi.nlm.nih.gov/pubmed/17133829[↩][↩]
- DeRegnier DP, Cole L, Schupp DG, Erlandsen SL. Viability of Giardia cysts suspended in lake, river, and tap water. Appl Environ Microbiol. 1989;55(5):1223. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3067073/[↩]
- Cantey PT, Roy S, Lee B, Cronquist A, Smith K, Liang J, Beach MJ. Study of nonoutbreak giardiasis: novel findings and implications for research. Am J Med. 2011;124:1175.e1–1175.e8. https://www.ncbi.nlm.nih.gov/pubmed/22014792[↩]
- Barraquer I. Sur la coïncidence de la lambliase et de certaineslésions du fond de l’oeil. Bulletin de la Sociétéde Pathologie Exotique. 1938;31:55–58.[↩]
- Pettoello Mantovani M, Giardino I, Magli A, di Martino L, Guandalini S. Intestinal giardiasis associated with ophthalmologic changes. J Pediatr Gastroenterol Nutr. 1990;11:196–200. https://www.ncbi.nlm.nih.gov/pubmed/2395058[↩][↩]
- Corsi A, Nucci C, Knafelz D, Bulgarini D, Di Iorio L, Polito A, De Risi F, Ardenti Morini F, Paone FM. Ocular changes associated with Giardia lamblia infection in children. Br J Ophthalmol. 1998;82:59–62. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1722351/[↩][↩]
- Carlson DW, Finger DR. Beaver fever arthritis. J Clin Rheumatol. 2004;10:86–88. https://www.ncbi.nlm.nih.gov/pubmed/17043473[↩][↩][↩][↩]
- Borman P, Seçkin U, Ozoran K. Beaver fever–a rare cause of reactive arthritis. J Rheumatol. 2001;28:683. http://www.jrheum.org/content/28/3/683.long[↩]
- Hill Gaston JS, Lillicrap MS. Arthritis associated with enteric infection. Best Pract Res Clin Rheumatol. 2003;17:219–239. https://www.ncbi.nlm.nih.gov/pubmed/12787523[↩][↩][↩]
- Gaston JS, Cox C, Granfors K. Clinical and experimental evidence for persistent Yersinia infection in reactive arthritis. Arthritis Rheum. 1999;42:2239–2242. https://www.ncbi.nlm.nih.gov/pubmed/10524699[↩]
- Giacometti A, Cirioni O, Antonicelli L, D’Amato G, Silvestri C, Del Prete MS, Scalise G. Prevalence of intestinal parasites among individuals with allergic skin diseases. J Parasitol. 2003;89:490–492. https://www.ncbi.nlm.nih.gov/pubmed/12880246[↩]
- Di Prisco MC, Hagel I, Lynch NR, Jiménez JC, Rojas R, Gil M, Mata E. Association between giardiasis and allergy. Ann Allergy Asthma Immunol. 1998;81:261–265. https://www.ncbi.nlm.nih.gov/pubmed/9759805[↩][↩]
- Hardin JA, Buret AG, Olson ME, Kimm MH, Gall DG. Mast cell hyperplasia and increased macromolecular uptake in an animal model of giardiasis. J Parasitol. 1997;83:908–912. https://www.ncbi.nlm.nih.gov/pubmed/9379297[↩]
- Cervelló A, Alfaro A, Chumillas MJ. Hypokalemic myopathy induced by Giardia lamblia. N Engl J Med. 1993;329:210–211. http://www.nejm.org/doi/full/10.1056/NEJM199307153290318[↩][↩]
- Genovese A, Spadaro G, Santoro L, Gasparo Rippa P, Onorati AM, Marone G. Giardiasis as a cause of hypokalemic myopathy in congenital immunodeficiency. Int J Clin Lab Res. 1996;26:132–135. https://www.ncbi.nlm.nih.gov/pubmed/8856367[↩][↩][↩][↩][↩]
- [↩]
- Addiss DG, Lengerich EJ. Hypokalemic myopathy induced by Giardia lamblia. N Engl J Med. 1994;330:66–67. http://www.nejm.org/doi/full/10.1056/NEJM199401063300115[↩]
- Araújo NS, Mundim MJ, Gomes MA, Amorim RM, Viana JC, Queiroz RP, Rossi MA, Cury MC. Giardia duodenalis: pathological alterations in gerbils, Meriones unguiculatus, infected with different dosages of trophozoites. Exp Parasitol. 2008;118:449–457. https://www.ncbi.nlm.nih.gov/pubmed/18083166[↩]
- Simsek Z, Zeyrek FY, Kurcer MA. Effect of Giardia infection on growth and psychomotor development of children aged 0-5 years. J Trop Pediatr. 2004;50:90–93. https://www.ncbi.nlm.nih.gov/pubmed/15088797[↩]
- Botero-Garcés JH, García-Montoya GM, Grisales-Patiño D, Aguirre-Acevedo DC, Alvarez-Uribe MC. Giardia intestinalis and nutritional status in children participating in the complementary nutrition program, Antioquia, Colombia, May to October 2006. Rev Inst Med Trop Sao Paulo. 2009;51:155–162.[↩]
- Thompson RC, Reynoldson JA, Mendis AH. Giardia and giardiasis. Adv Parasitol. 1993;32:71–160.[↩]
- Lengerich EJ, Addiss DG, Juranek DD. Severe giardiasis in the United States. Clin Infect Dis. 1994;18:760–763.[↩]
- Koruk I, Simsek Z, Tekin Koruk S, Doni N, Gürses G. Intestinal parasites, nutritional status and physchomotor development delay in migratory farm worker’s children. Child Care Health Dev. 2010;36:888–894.[↩]
- Guerrant DI, Moore SR, Lima AA, Patrick PD, Schorling JB, Guerrant RL. Association of early childhood diarrhea and cryptosporidiosis with impaired physical fitness and cognitive function four-seven years later in a poor urban community in northeast Brazil. Am J Trop Med Hyg. 1999;61:707–713.[↩][↩]
- Veenemans J, Mank T, Ottenhof M, Baidjoe A, Mbugi EV, Demir AY, Wielders JP, Savelkoul HF, Verhoef H. Protection against diarrhea associated with Giardia intestinalis Is lost with multi-nutrient supplementation: a study in Tanzanian children. PLoS Negl Trop Dis. 2011;5:e1158. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3110167/[↩]
- Berkman DS, Lescano AG, Gilman RH, Lopez SL, Black MM. Effects of stunting, diarrhoeal disease, and parasitic infection during infancy on cognition in late childhood: a follow-up study. Lancet. 2002;359:564–571. https://www.ncbi.nlm.nih.gov/pubmed/11867110[↩]
- Botero-Garcés JH, García-Montoya GM, Grisales-Patiño D, Aguirre-Acevedo DC, Alvarez-Uribe MC. Giardia intestinalis and nutritional status in children participating in the complementary nutrition program, Antioquia, Colombia, May to October 2006. Rev Inst Med Trop Sao Paulo. 2009;51:155–162. https://www.ncbi.nlm.nih.gov/pubmed/19551290[↩]
- Ettehad GH, Daryani A, Nemati A. Effect of Giardia infection on nutritional status in primary schoolchildren, in northwest Iran. Pak J Biol Sci. 2010;13:229–234. https://www.ncbi.nlm.nih.gov/pubmed/20464945[↩]
- Halliez MC, Buret AG. Extra-intestinal and long term consequences of Giardia duodenalis infections. World Journal of Gastroenterology : WJG. 2013;19(47):8974-8985. doi:10.3748/wjg.v19.i47.8974. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3870550/[↩]
- Dizdar V, Gilja OH, Hausken T. Increased visceral sensitivity in Giardia-induced postinfectious irritable bowel syndrome and functional dyspepsia. Effect of the 5HT3-antagonist ondansetron. Neurogastroenterol Motil. 2007;19:977–982. https://www.ncbi.nlm.nih.gov/pubmed/17973637[↩]
- Hanevik K, Dizdar V, Langeland N, Hausken T. Development of functional gastrointestinal disorders after Giardia lamblia infection. BMC Gastroenterol. 2009;9:27. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2676300/[↩][↩]
- Farthing MJ. Giardiasis. Gastroenterol Clin North Am. 1996;25:493–515. https://www.ncbi.nlm.nih.gov/pubmed/8863037[↩]
- D’Anchino M, Orlando D, De Feudis L. Giardia lamblia infections become clinically evident by eliciting symptoms of irritable bowel syndrome. J Infect. 2002;45:169–172. https://www.ncbi.nlm.nih.gov/pubmed/12387773[↩]
- Hanevik K, Hausken T, Morken MH, Strand EA, Mørch K, Coll P, Helgeland L, Langeland N. Persisting symptoms and duodenal inflammation related to Giardia duodenalis infection. J Infect. 2007;55:524–530. https://www.ncbi.nlm.nih.gov/pubmed/17964658[↩]
- Mørch K, Hanevik K, Rortveit G, Wensaas KA, Eide GE, Hausken T, Langeland N. Severity of Giardia infection associated with post-infectious fatigue and abdominal symptoms two years after. BMC Infect Dis. 2009;9:206. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2808308/[↩]
- The Merck Veterinary Manual. Overview of giardiasis. United States: Merck; 2016. www.merckvetmanual.com/digestive-system/giardiasis/overview-of-giardiasis[↩]
- Ballweber LR, Xiao L, Bowman D, Kahn G, Cama VA. Giardiasis in dogs and cats: update on epidemiology and public health significance. Trends Parasitol. 2010;26(4):180-9. https://www.ncbi.nlm.nih.gov/pubmed/20202906[↩]
- Tangtrongsup S, Scorza V. Update on the diagnosis and management of Giardia spp infections in dogs and cats. Top Companion Anim Med. 2010;25(3):155-62. https://actualidadveterinaria.files.wordpress.com/2011/08/update-on-the-diagnosis-and-management-of-giardia-spp-infections-in-dogs-and-cats.pdf[↩][↩][↩][↩][↩]
- Xiao L, Fayer R. Molecular characterisation of species and genotypes of Cryptosporidium and Giardia and assessment of zoonotic transmission. Int J Parasitol. 2008;38:1239–55. https://www.ncbi.nlm.nih.gov/pubmed/18479685[↩]
- Fletcher R, Deplazes P, Schnyder M. Control of Giardia infections with ronidazole and intensive hygiene management in a dog kennel. Vet Parasitol. 2011;187(1-2):93-8. http://www.zora.uzh.ch/id/eprint/61694/4/Fiechter_et_al_Control_of_Giarda_infections.pdf[↩]
- Huang DB, White AC. An updated review on Cryptosporidium and Giardia. Gastroenterol Clin North Am. 2006;35(2):291-314, viii. https://www.ncbi.nlm.nih.gov/pubmed/16880067[↩]
- Borman P, Seckin U, Ozoran K. Beaver fever–a rare cause of reactive arthritis. J Rheumatol. 2001;28(3):683. https://www.ncbi.nlm.nih.gov/pubmed/10606388[↩]
- Hill DR. Giardia lamblia. In: Gillespie SH, Pearson RD, eds. Principles and practice of clinical parasitology. Chisester, England: Joan Wiley & Sons; 2001.[↩]
- Rev Inst Med Trop Sao Paulo. 2009;51(3):155-62. http://www.scielo.br/pdf/rimtsp/v51n3/v51n3a06.pdf[↩]
- Clinical and Laboratory Standards Institute. Procedures for the recovery and identification of parasites from the intestinal tract; approved guideline. CLSI document M28-A2. 2nd ed. Wayne, PA: Clinical Laboratory Standards Institute; 2005.[↩]
- Johnston SP, Ballard MM, Beach MJ, Causer L, Wilkins PP. Evaluation of three commercial assays for detection of Giardia and Cryptosporidium organisms in fecal specimens. J Clin Microbiol. 2003;41(2):623-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC149727/[↩][↩]
- Drugs for Parasitic Infections: The Medical Letter; 2010.[↩]
- Solaymani-Mohammadi S, Genkinger JM, Loffredo CA, Singer SM. A meta-analysis of the effectiveness of albendazole compared with metronidazole as treatments for infections with Giardia duodenalis. PLoS Negl Trop Dis. 2010;4(5):e682. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2867942/[↩][↩]
- Escobedo AA, Cimerman S. Giardiasis: a pharmacotherapy review. Expert Opin Pharmacother. 2007;8(12):1885-1902. https://www.tandfonline.com/doi/full/10.1517/14656566.8.12.1885[↩]