Contents
- What are hemorrhoids
- Types of hemorrhoids
- What do hemorrhoids look like?
- What causes hemorrhoids?
- Hemorrhoids prevention
- Hemorrhoids symptoms
- Hemorrhoids complications
- Hemorrhoids diagnosis
- Hemorrhoids treatment
What are hemorrhoids
Hemorrhoids also called piles, are swollen, inflamed veins around the anus and lower rectum 1. Hemorrhoids are either inside the anus or under the skin around the anus. Hemorrhoids have a number of causes, although often the cause is unknown. They often result from straining to have a bowel movement or from the increased pressure on these veins during pregnancy. Other factors include aging and chronic constipation or diarrhea. Hemorrhoids may be located inside the rectum (internal hemorrhoids), or they may develop under the skin around the anus (external hemorrhoids).
If you have a hemorrhoid, you may feel a tender lump on the edge of your anus. You may also see blood on the toilet paper or in the toilet after a bowel movement.
Hemorrhoids are very common in both men and women. Nearly half of Americans have hemorrhoids by age 50 2. Nearly 5% of the US population (15,000,000 people) has sought medical care for symptomatic hemorrhoids. Many more have problems with hemorrhoids, but never seek formal medical attention.
The most common symptom of hemorrhoids inside the anus is bright red blood covering the stool, on toilet paper or in the toilet bowl. Symptoms usually go away within a few days.
- If you have rectal bleeding you should see a doctor.
- You need to make sure bleeding is not from a more serious condition such as colorectal or anal cancer.
Sometimes hemorrhoids don’t cause symptoms but at other times hemorrhoids cause itching, discomfort and bleeding.
Occasionally, a clot may form in a hemorrhoid (thrombosed hemorrhoid). These are not dangerous but can be extremely painful and sometimes need to be lanced and drained.
Treatment may include warm baths and a cream or other medicine.
If you have large hemorrhoids, you may need surgery and other treatments.
The anus
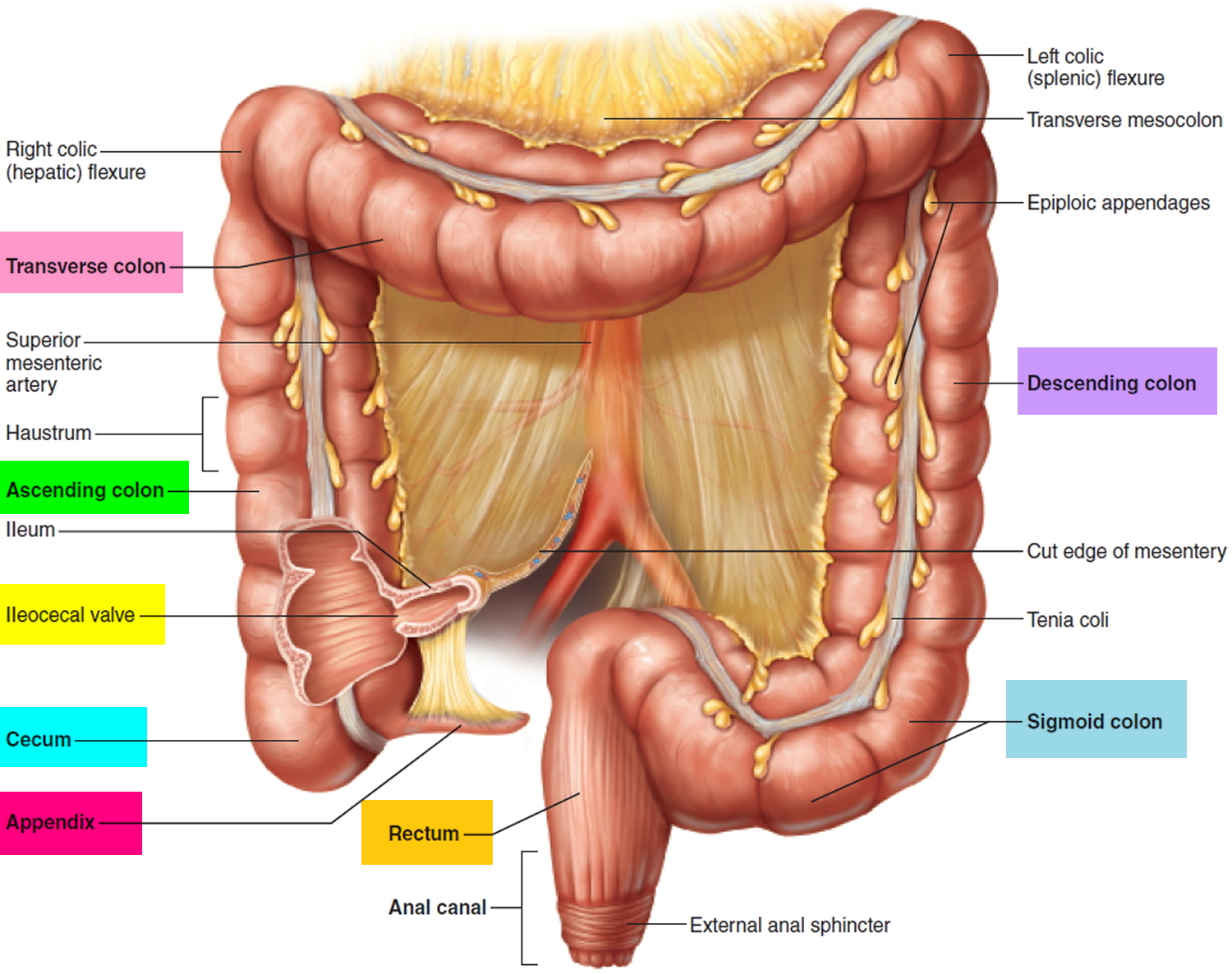
The anus is connected to the rectum by the anal canal. The anus is the continuation of the large intestine (the colon or large bowel) inferior to the rectum. It’s where the end of the intestines connect to the outside of the body.
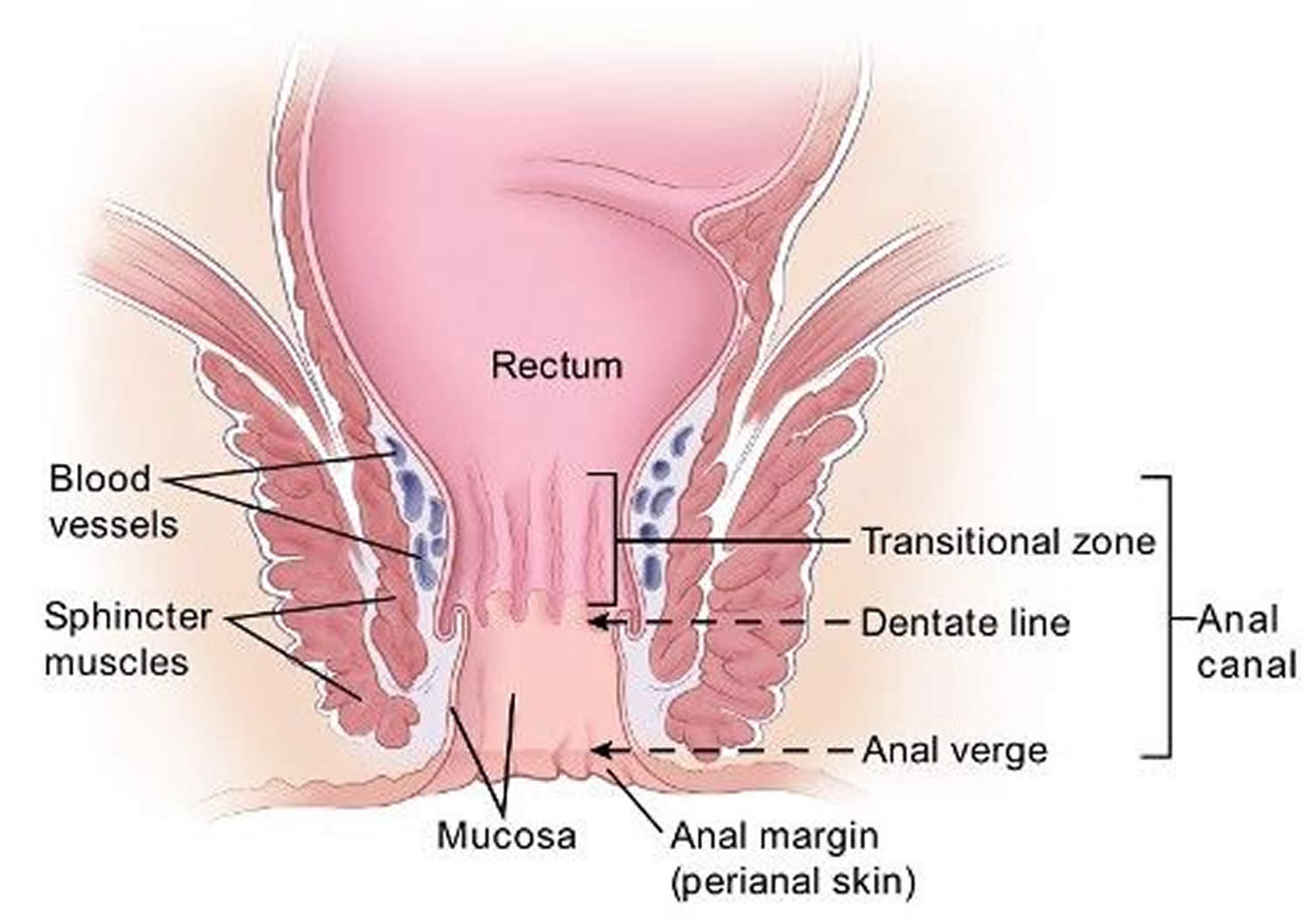
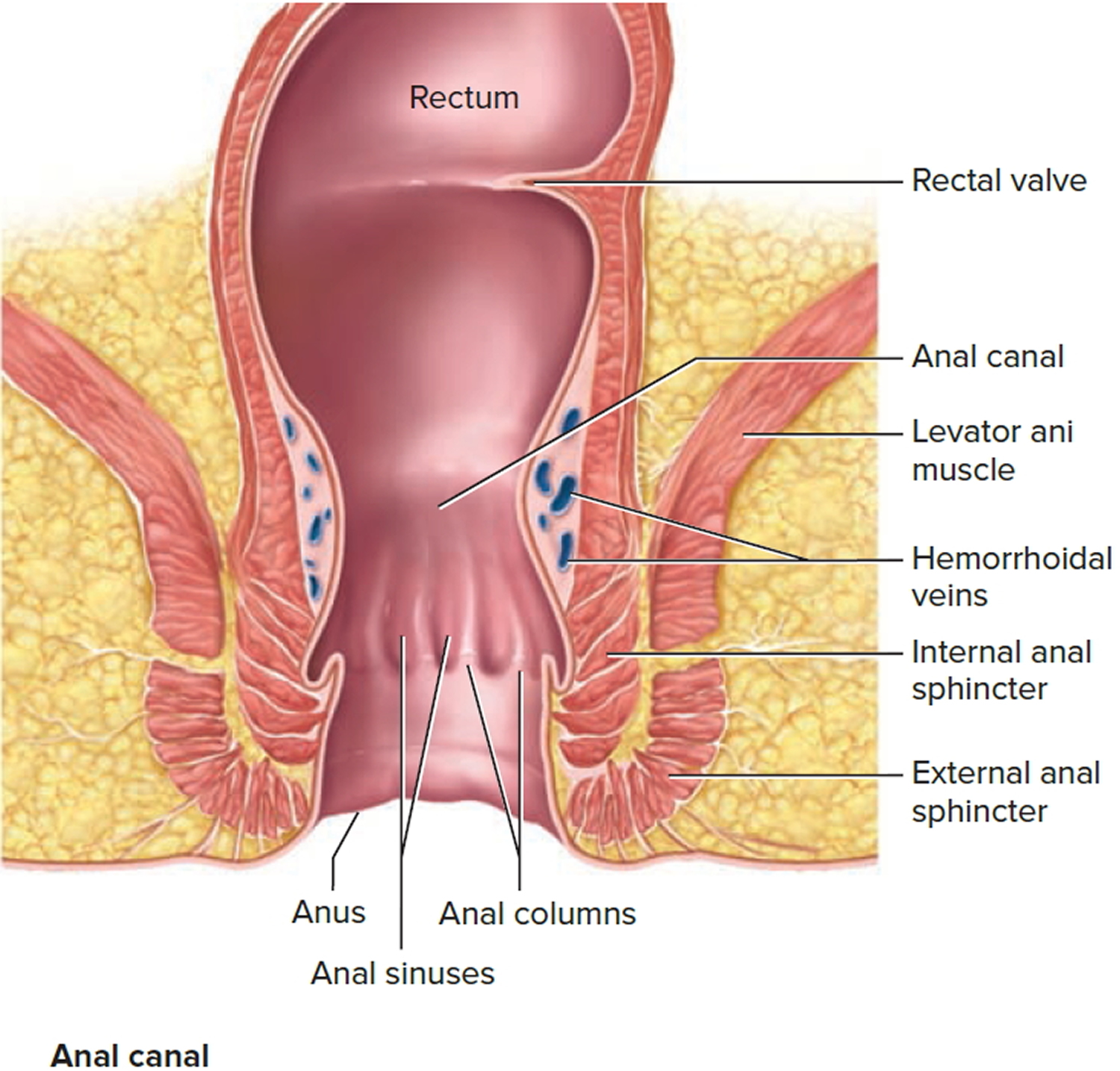
The anal canal is about 1-1/2 inches (about 3 to 5 cm) long, it begins where the rectum passes through the levator ani (the muscle that forms the pelvic floor) and goes to the anal verge. The anal verge is where the anal canal connects to the outside skin at the anus. This skin around the anal verge is called the perianal skin (previously called the anal margin). The anal canal has two ring-shaped muscles (called sphincter muscles – an internal and external anal sphincter) that keep the anus closed and prevent stool from leaking out.
As food is digested, it passes from the stomach to the small intestine. It then moves from the small intestine into the main part of the large intestine (called the colon). The colon absorbs water and salt from the digested food. The waste matter that’s left after going through the colon is known as feces or stool. Stool is stored in the last part of the large intestine, called the rectum. From there, stool is passed out of the body through the anus as a bowel movement.
The inner lining of the anal canal is the mucosa. Most anal cancers start from cells in the mucosa. Glands and ducts (tubes leading from the glands) are found under the mucosa. The glands make mucus, which acts as a lubricating fluid. Anal cancers that start from cells in the glands are called adenocarcinomas.
The anal canal changes as it goes from the rectum to the anal verge. The parts of the anus include the:
- Cells above the anal canal (in the rectum) and in the part of the anal canal close to the rectum are shaped like tiny columns.
- Most cells near the middle of the anal canal are shaped like cubes and are called transitional cells. This area is called the transitional zone – this is where the rectum meets the anal canal.
- About midway down the anal canal is the dentate line, which is where most of the anal glands empty into the anus.
- Below the dentate line are flat (squamous) cells.
- At the anal verge, the squamous cells of the lower anal canal merge with the skin just outside the anus. This skin around the anal verge called the perianal skin or the anal margin, is also made up of squamous cells, but it also contains sweat glands and hair follicles, which are not found in the lining of the lower anal canal. The anal margin is the lower part of the anal canal and it contains muscles called the anal sphincters. You have an internal and external anal sphincter. They are the muscles that control your bowel movements.
Figure 1. Rectum
Figure 2. Rectum anatomy and Anus (anal canal)
Types of hemorrhoids
The type of hemorrhoid you have depends on where it occurs.
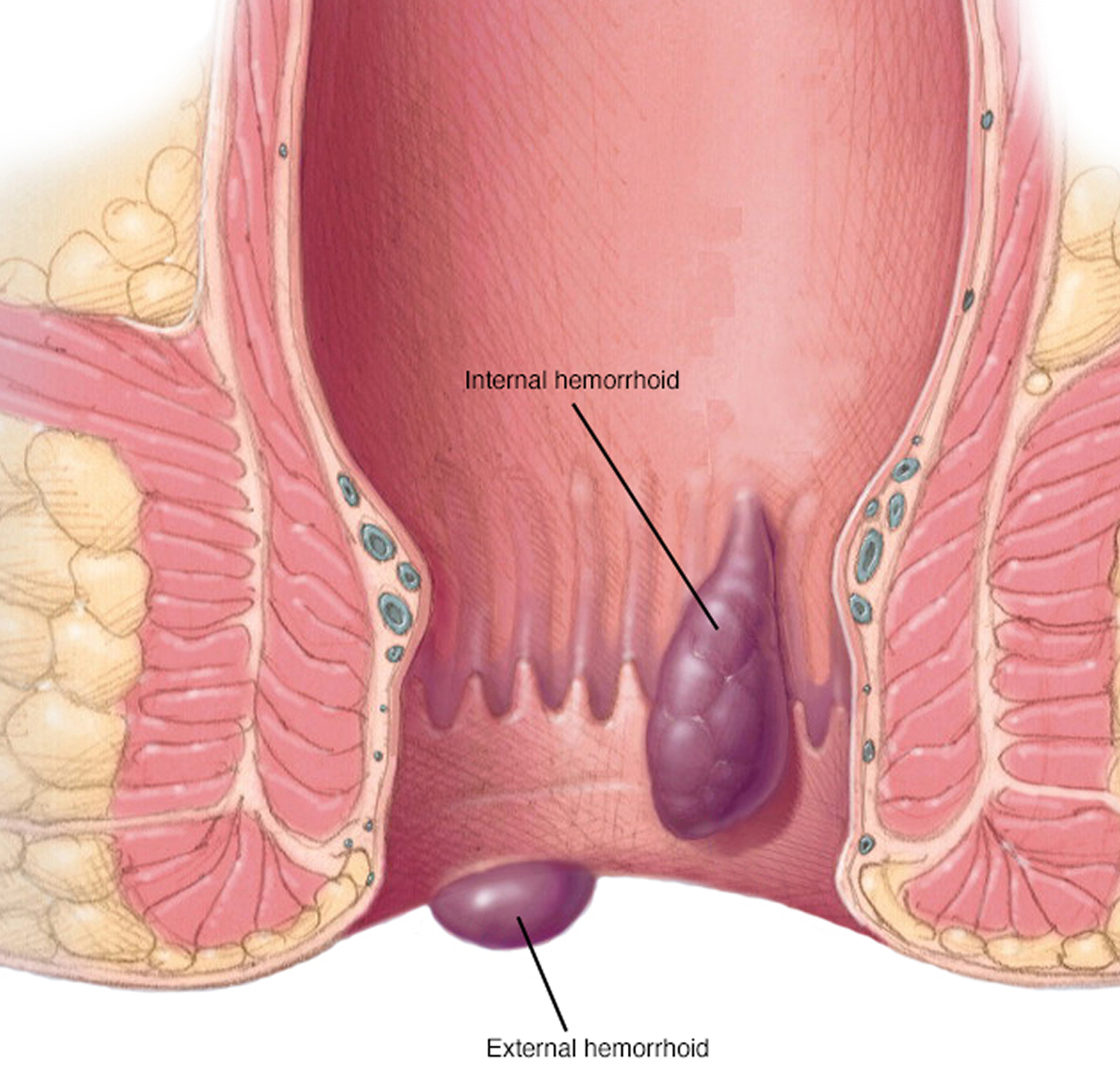
- Internal hemorrhoids involve the veins inside your rectum. Internal hemorrhoids usually don’t hurt but they may bleed painlessly.
- Prolapsed hemorrhoids may stretch down until they bulge outside your anus. A prolapsed hemorrhoid may go back inside your rectum on its own, or you can gently push it back inside.
- External hemorrhoids involve the veins outside the anus. They can be itchy or painful and can sometimes crack and bleed.
Classification of a hemorrhoid corresponds to its position relative to the dentate line. External hemorrhoids are located below the dentate line and develop from ectoderm embryonically 3. External hemorrhoids are covered with anoderm, composed of squamous epithelium, and are innervated by somatic nerves supplying the perianal skin and thus producing pain. Vascular outflows of external hemorrhoids are via the inferior rectal veins into the pudendal vessels and then into the internal iliac veins. In contrast, internal hemorrhoids lie above the dentate line and are derived from endoderm 3. They are covered by columnar epithelium, innervated by visceral nerve fibers and thus cannot cause pain. Vascular outflows of internal hemorrhoids include the middle and superior rectal veins, which subsequently drain into the internal iliac vessels.
Internal hemorrhoids
Painless rectal bleeding or prolapse of anal tissue is often associated with symptomatic internal hemorrhoids. Prolapse is hemorrhoidal tissue coming from the inside that can often be felt on the outside of the anus when wiping or having a bowel movement. This tissue often goes back inside spontaneously or can be pushed back internally by the patient. The symptoms tend to progress slowly over a long time and are often intermittent.
Internal hemorrhoids are classified by their degree of prolapse, which helps determine management 4, 5:
- Grade One: No prolapse out of the canal but are characterized by prominent vascularity.
- Grade Two: Prolapse outside of the canal during bowel movements or straining, but reduce spontaneously.
- Grade Three: Prolapse out of the canal and require manual reduction (pushed back in) by the patient
- Grade Four: Prolapse that cannot be pushed back in by the patient (often very painful)
Bleeding attributed to internal hemorrhoids is usually bright red and can be quite brisk. It may be found on the wipe, dripping into the toilet bowl, or streaked on the bowel movement itself. Not all people with symptomatic internal hemorrhoids will have significant bleeding. Instead, prolapse may be the main or only symptom. Prolapsing tissue may result in significant irritation and itching around the anus. People with internal hemorrhoids may also complain of mucus discharge, difficulty with cleaning themselves after a bowel movement or a sense that their stool is “stuck” at the anus with bowel movements. People without significant symptoms from internal hemorrhoids do not require treatment based on their appearance alone.
Most patients with grade 1 or 2 hemorrhoids, and many with grade 3 hemorrhoids, can be treated in primary care offices. Patients in whom office-based treatment is ineffective (see below under Treatment) and those with mixed hemorrhoids may require treatment in surgical suites with facilities for anesthesia. The most common surgical treatments are ligation or tissue destruction, fixation techniques (i.e., hemorrhoidopexy – hemorrhoid stapling), and excision (i.e., hemorrhoidectomy).
External hemorrhoids
Symptomatic external hemorrhoids often present as a bluish-colored painful lump just outside the anus and they tend to occur spontaneously and may have been preceded by an unusual amount of straining. The skin overlying the outside of the anus is usually firmly attached to the underlying tissues. If a blood clot or thrombosis develops in this tightly held area, the pressure goes up rapidly in these tissues often causing pain. The pain is usually constant and can be severe. Occasionally the elevated pressure in the thrombosed external hemorrhoid results in breakdown of the overlying skin and the clotted blood begins leaking out. Patients may also complain of intermittent swelling, pressure and discomfort, related to external hemorrhoids which are not thrombosed.
Thrombosed external hemorrhoids
Thrombosed external hemorrhoids cause acute, severe pain. Without intervention, the pain typically improves over two to three days, with continued improvement as the thrombus gradually absorbs over several weeks. Analgesics and stool softeners may be beneficial. Topical therapy with nifedipine and lidocaine cream is more effective for pain relief than lidocaine (Xylocaine) alone 6.
In patients with severe pain from thrombosed hemorrhoids, excision or incision and evacuation of the thrombus within 72 hours of symptom onset provide more rapid pain relief than conservative treatment 7. Both procedures can be performed under local anesthesia, and the resulting wound can be left open or sutured 8.
Hemorrhoids in Pregnancy
Pregnancy predisposes women to symptomatic hemorrhoids that usually resolve after delivery. Surgical intervention is contraindicated because of the risk of inducing labor 9. Conservative treatment is recommended, with excision of thrombosed external hemorrhoids if necessary.
Patients often complain of painless, soft tissue felt on the outside of the anus. These can be the residual effect of a previous problem with an external hemorrhoid. The blood clot stretches out the overlying skin and remains stretched out after the blood clot is absorbed by the body, thereby leaving a skin tag. Other times, patients will have skin tags without an obvious preceding event. Skin tags will occasionally bother patients by interfering with their ability to clean the anus following a bowel movement, while others just don’t like the way they look. Usually, nothing is done to treat them beyond reassurance. However, surgical removal is occasionally considered.
What do hemorrhoids look like?
Hemorrhoids are swollen veins in your lower rectum. Internal hemorrhoids are usually painless, but tend to bleed. External hemorrhoids may cause pain.
Figure 3. Hemorrhoids
What causes hemorrhoids?
Hemorrhoids are caused by increased pressure in the veins of your anus or rectum. One of the main causes is straining when you’re trying to have a bowel movement. This may happen if you’re constipated or if you have diarrhea. It may also happen if you sit on the toilet too long. Hemorrhoids can also be caused by obesity, heavy lifting or any other activity that caused you to strain.
The veins around your anus tend to stretch under pressure and may bulge or swell. Swollen veins (hemorrhoids) can develop from increased pressure in the lower rectum due to:
- Straining during bowel movements
- Sitting for long periods of time on the toilet
- Chronic diarrhea or constipation
- Obesity
- Pregnancy
- Anal intercourse
- Low-fiber diet
Hemorrhoids are more likely with aging because the tissues that support the veins in your rectum and anus can weaken and stretch.
The exact pathophysiology of symptomatic hemorrhoid disease is poorly understood. Previous theories of hemorrhoids as anorectal varices are now obsolete—as shown by Goenka et al, patients with portal hypertension and varices do not have an increased incidence of hemorrhoids 10. Currently, the theory of sliding anal canal lining, which proposes that hemorrhoids occur when the supporting tissues of the anal cushions deteriorate, is more widely accepted. Advancing age and activities such as strenuous lifting, straining with defecation, and prolonged sitting are thought to contribute to this process. Hemorrhoids are therefore the pathological term to describe the abnormal downward displacement of the anal cushions causing venous dilatation 11. On histopathological examination, changes seen in the anal cushions include abnormal venous dilatation, vascular thrombosis, degenerative process in the collagen fibers and fibroelastic tissues, and distortion and rupture of the anal subepithelial muscle. In severe cases, a prominent inflammatory reaction involving the vascular wall and surrounding connective tissue has been associated with mucosal ulceration, ischemia, and thrombosis 12.
Who gets hemorrhoids?
Just about everyone has hemorrhoids at some time. But some things may make you more likely to get them. People whose parents had hemorrhoids may be more likely to get them. Pregnant women often get hemorrhoids because of the strain from carrying the baby and from giving birth. Being very overweight or standing or lifting too much can make hemorrhoids worse.
Hemorrhoids prevention
The best way to prevent hemorrhoids is to keep your stools soft, so they pass easily. To prevent hemorrhoids and reduce symptoms of hemorrhoids, follow these tips:
- Eat high-fiber foods. Eat more fruits, vegetables and whole grains. Doing so softens the stool and increases its bulk, which will help you avoid the straining that can cause hemorrhoids. Add fiber to your diet slowly to avoid problems with gas.
- Drink plenty of fluids. Drink six to eight glasses of water and other liquids (not alcohol) each day to help keep stools soft.
- Consider fiber supplements. Most people don’t get enough of the recommended amount of fiber — 25 grams a day for women and 38 grams a day for men — in their diet. Studies have shown that over-the-counter fiber supplements, such as Metamucil and Citrucel, improve overall symptoms and bleeding from hemorrhoids. These products help keep stools soft and regular. If you use fiber supplements, be sure to drink at least eight glasses of water or other fluids every day. Otherwise, the supplements can cause constipation or make constipation worse.
- Don’t strain. Straining and holding your breath when trying to pass a stool creates greater pressure in the veins in the lower rectum.
- Go as soon as you feel the urge. If you wait to pass a bowel movement and the urge goes away, your stool could become dry and be harder to pass.
- Exercise. Stay active to help prevent constipation and to reduce pressure on veins, which can occur with long periods of standing or sitting. Exercise can also help you lose excess weight that may be contributing to your hemorrhoids.
- Avoid long periods of sitting. Sitting too long, particularly on the toilet, can increase the pressure on the veins in the anus.
Hemorrhoids symptoms
Signs and symptoms of hemorrhoids may include:
- Painless bleeding during bowel movements — you might notice small amounts of bright red blood on your toilet tissue or in the toilet
- Itching or irritation in your anal region
- Pain or discomfort
- Swelling around your anus
- A lump near your anus, which may be sensitive or painful (may be a thrombosed hemorrhoid)
Hemorrhoid symptoms usually depend on the location.
Internal hemorrhoids. These lie inside the rectum. You usually can’t see or feel these hemorrhoids, and they rarely cause discomfort. But straining or irritation when passing stool can damage a hemorrhoid’s surface and cause it to bleed. When they cause symptoms, the most common are painless rectal bleeding, which usually is seen as bright red blood on the toilet paper or in the toilet bowl. It is important to know that just a few drops of blood in toilet water can change the color of the water dramatically.
Occasionally, straining can push an internal hemorrhoid through the anal opening. This is known as a protruding or prolapsed hemorrhoid and can cause pain and irritation.
External hemorrhoids. These are under the skin around your anus and cause no symptoms. When they cause symptoms, the most common are pain, itching, pressure and bleeding; they can often be felt as a bulge in the skin near the anal opening.
Thrombosed hemorrhoids. Sometimes blood may pool in an external hemorrhoid and form a clot (thrombus) that can result in severe pain, swelling, inflammation and a hard lump near your anus.
When to see a doctor
Bleeding during bowel movements is the most common sign of hemorrhoids. Your doctor can do a physical examination and perform other tests to confirm hemorrhoids and rule out more-serious conditions or diseases.
Also talk to your doctor if you know you have hemorrhoids and they cause pain, bleed frequently or excessively, or don’t improve with home remedies.
- Don’t assume rectal bleeding is due to hemorrhoids, especially if you are over 40 years old.
- Rectal bleeding can occur with other diseases, including colorectal cancer and anal cancer.
- If you have bleeding along with a marked change in bowel habits or if your stools change in color or consistency, consult your doctor.
- These types of stools can signal more extensive bleeding elsewhere in your digestive tract.
Seek emergency care if you experience large amounts of rectal bleeding, lightheadedness, dizziness or faintness.
Hemorrhoids complications
Complications of hemorrhoids are very rare but include:
- Anemia. Rarely, chronic blood loss from hemorrhoids may cause anemia, in which you don’t have enough healthy red blood cells to carry oxygen to your cells.
- Strangulated hemorrhoid. If the blood supply to an internal hemorrhoid is cut off, the hemorrhoid may be “strangulated,” another cause of extreme pain.
Hemorrhoids diagnosis
Your doctor may be able to see if you have external hemorrhoids simply by looking. Tests and procedures to diagnose internal hemorrhoids may include examination of your anal canal and rectum:
- Digital examination. During a digital rectal exam, your doctor inserts a gloved, lubricated finger into your rectum. He or she feels for anything unusual, such as growths. The exam can suggest to your doctor whether further testing is needed.
- Visual inspection. Because internal hemorrhoids are often too soft to be felt during a rectal exam, your doctor may also examine the lower portion of your colon and rectum with an anoscope, proctoscope or sigmoidoscope.
Your doctor may want to examine your entire colon using colonoscopy if:
- Your signs and symptoms suggest you might have another digestive system disease
- You have risk factors for colorectal cancer
- You’re middle-aged and haven’t had a recent colonoscopy.
The American Society of Colon and Rectal Surgeons recommends taking the patient history and performing a physical examination with anoscopy and further endoscopic evaluation if there is concern for inflammatory bowel disease or cancer 13. A complete evaluation of the colon is warranted in the following groups 13:
- Patients who are 50 years or older and have not had a complete examination of the colon within the past 10 years
- Patients who are 40 years or older and have not had a complete examination of the colon within the past 10 years, and who have one first-degree relative in whom colorectal cancer or adenoma was diagnosed at age 60 years or younger
- Patients who are 40 years or older and have not had a complete examination of the colon within the past five years, and who have more than one first-degree relative in whom colorectal cancer or adenoma was diagnosed at age 60 years or younger
- Patients with iron deficiency anemia
- Patients who have a positive fecal occult blood test.
Hemorrhoids treatment
Home remedies
You can often relieve the mild pain, swelling and inflammation of hemorrhoids with home treatments. Often these are the only treatments needed.
Treatments for hemorrhoids include:
- Eat high-fiber foods. Eat more fruits, vegetables and whole grains – it is usually recommended you eat 20-35 grams of fiber per day. Doing so softens the stool and increases its bulk, which will help you avoid the straining that can worsen symptoms from existing hemorrhoids. Add fiber to your diet slowly to avoid problems with gas.
- Stool softeners to help reduce straining and constipation
- Use topical treatments. Apply an over-the-counter hemorrhoid cream or suppository containing hydrocortisone, or use pads containing witch hazel or a numbing agent to help reduce pain and swelling. Hemorrhoid creams with lidocaine to help reduce pain
- Soak regularly in a warm bath or sitz bath. Soak your anal area in plain warm water 10 to 15 minutes two to three times a day. A sitz bath fits over the toilet.
- Keep the anal area clean. Bathe (preferably) or shower daily to cleanse the skin around your anus gently with warm water. Avoid alcohol-based or perfumed wipes. Gently pat the area dry or use a hair dryer.
- Wear cotton underwear.
- Don’t use dry toilet paper. To help keep the anal area clean after a bowel movement, use moist towelettes or wet toilet paper that doesn’t contain perfume or alcohol.
- Apply cold. Apply ice packs or cold compresses on your anus to relieve swelling.
- Take oral pain relievers. You can use acetaminophen (Tylenol, others), aspirin or ibuprofen (Advil, Motrin IB, others) temporarily to help relieve your discomfort.
With these treatments, hemorrhoid symptoms often go away within a week. See your doctor if you don’t get relief in a week, or sooner if you have severe pain or bleeding.
Dietary Fiber
Dietary fiber is a type of carbohydrate made up of many sugar molecules linked together. But unlike other carbohydrates, dietary fiber is bound together in such a way that it cannot be easily digested in the small intestine.
There are two types of dietary fiber:
- Soluble dietary fiber dissolves in water to form a thick gel-like substance in the stomach. It is broken down by bacteria in the large intestine and provides some calories. Soluble dietary fiber can interfere with the absorption of dietary fat and cholesterol. This, in turn, can help lower low-density lipoprotein (LDL or “bad”) cholesterol levels in the blood. Soluble fiber can also slow digestion and the rate at which carbohydrates and other nutrients are absorbed into the bloodstream. This can help control the level of blood glucose (often referred to as blood sugar) by preventing rapid rises in blood glucose following a meal.
- Insoluble dietary fiber does not dissolve in water and may pass through the gastrointestinal tract relatively intact and, therefore, is not a source of calories. Insoluble dietary fiber can speed up the movement of food and waste through the digestive system.
Both soluble and insoluble dietary fiber can make you feel full, which may lower your calorie intake by helping you eat less and yet stay satisfied longer.
Diets higher in dietary fiber can increase the frequency of bowel movements and can reduce the risk of developing cardiovascular disease.
The US Department of Agriculture and US Department of Health and Human Services recommend that you eat 25 g to 40 g of fiber daily, but most people get less than half this recommendation 14. Adequate fiber intake is important for many reasons:
- Fiber helps regulate bowel movements by softening hard stool to reduce constipation and adding bulk to loose stool to reduce diarrhea
- Common anal problems such as anal fissures and hemorrhoids are caused by inadequate fiber and water intake
- Adequate fiber will reduce the risk of developing colorectal cancer, diverticulosis, and complications of diverticulitis
- Adequate fiber will reduce cholesterol.
Table 1. Food Sources of Dietary Fiber
| FOOD ab | STANDARD PORTION c | CALORIES | FIBER (g) | |
|---|---|---|---|---|
| Grains | ||||
| Ready-to-eat cereal, high fiber, unsweetened | 1/2 cup | 62 | 14 | |
| Ready-to-eat cereal, whole grain kernels | 1/2 cup | 209 | 7.5 | |
| Ready-to-eat cereal, wheat, shredded | 1 cup | 172 | 6.2 | |
| Popcorn | 3 cups | 169 | 5.8 | |
| Ready-to-eat cereal, bran flakes | 3/4 cup | 98 | 5.5 | |
| Bulgur, cooked | 1/2 cup | 76 | 4.1 | |
| Spelt, cooked | 1/2 cup | 123 | 3.8 | |
| Teff, cooked | 1/2 cup | 128 | 3.6 | |
| Barley, pearled, cooked | 1/2 cup | 97 | 3 | |
| Ready-to-eat cereal, toasted oat | 1 cup | 111 | 3 | |
| Oat bran | 1/2 cup | 44 | 2.9 | |
| Crackers, whole wheat | 1 ounce | 122 | 2.9 | |
| Chapati or roti, whole wheat | 1 ounce | 85 | 2.8 | |
| Tortillas, whole wheat | 1 ounce | 88 | 2.8 | |
| Vegetables | ||||
| Artichoke, cooked | 1 cup | 89 | 9.6 | |
| Navy beans, cooked | 1/2 cup | 128 | 9.6 | |
| Small white beans, cooked | 1/2 cup | 127 | 9.3 | |
| Yellow beans, cooked | 1/2 cup | 128 | 9.2 | |
| Lima beans, cooked | 1 cup | 209 | 9.2 | |
| Green peas, cooked | 1 cup | 134 | 8.8 | |
| Adzuki beans, cooked | 1/2 cup | 147 | 8.4 | |
| French beans, cooked | 1/2 cup | 114 | 8.3 | |
| Split peas, cooked | 1/2 cup | 116 | 8.2 | |
| Breadfruit, cooked | 1 cup | 170 | 8 | |
| Lentils, cooked | 1/2 cup | 115 | 7.8 | |
| Lupini beans, cooked | 1/2 cup | 115 | 7.8 | |
| Mung beans, cooked | 1/2 cup | 106 | 7.7 | |
| Black turtle beans, cooked | 1/2 cup | 120 | 7.7 | |
| Pinto beans, cooked | 1/2 cup | 123 | 7.7 | |
| Cranberry (roman) beans, cooked | 1/2 cup | 121 | 7.6 | |
| Black beans, cooked | 1/2 cup | 114 | 7.5 | |
| Fufu, cooked | 1 cup | 398 | 7.4 | |
| Pumpkin, canned | 1 cup | 83 | 7.1 | |
| Taro root (dasheen or yautia), cooked | 1 cup | 187 | 6.7 | |
| Brussels sprouts, cooked | 1 cup | 65 | 6.4 | |
| Chickpeas (garbanzo beans), cooked | 1/2 cup | 135 | 6.3 | |
| Sweet potato, cooked | 1 cup | 190 | 6.3 | |
| Great northern beans, cooked | 1/2 cup | 105 | 6.2 | |
| Parsnips, cooked | 1 cup | 110 | 6.2 | |
| Nettles, cooked | 1 cup | 37 | 6.1 | |
| Jicama, raw | 1 cup | 46 | 5.9 | |
| Winter squash, cooked | 1 cup | 76 | 5.7 | |
| Pigeon peas, cooked | 1/2 cup | 102 | 5.7 | |
| Kidney beans, cooked | 1/2 cup | 113 | 5.7 | |
| White beans, cooked | 1/2 cup | 125 | 5.7 | |
| Black-eyed peas, dried and cooked | 1/2 cup | 99 | 5.6 | |
| Cowpeas, dried and cooked | 1/2 cup | 99 | 5.6 | |
| Yam, cooked | 1 cup | 158 | 5.3 | |
| Broccoli, cooked | 1 cup | 54 | 5.2 | |
| Tree fern, cooked | 1 cup | 56 | 5.2 | |
| Luffa gourd, cooked | 1 cup | 100 | 5.2 | |
| Soybeans, cooked | 1/2 cup | 148 | 5.2 | |
| Turnip greens, cooked | 1 cup | 29 | 5 | |
| Drumstick pods (moringa), cooked | 1 cup | 42 | 5 | |
| Avocado | 1/2 cup | 120 | 5 | |
| Cauliflower, cooked | 1 cup | 34 | 4.9 | |
| Kohlrabi, raw | 1 cup | 36 | 4.9 | |
| Carrots, cooked | 1 cup | 54 | 4.8 | |
| Collard greens, cooked | 1 cup | 63 | 4.8 | |
| Kale, cooked | 1 cup | 43 | 4.7 | |
| Fava beans, cooked | 1/2 cup | 94 | 4.6 | |
| Chayote (mirliton), cooked | 1 cup | 38 | 4.5 | |
| Snow peas, cooked | 1 cup | 67 | 4.5 | |
| Pink beans, cooked | 1/2 cup | 126 | 4.5 | |
| Spinach, cooked | 1 cup | 41 | 4.3 | |
| Escarole, cooked | 1 cup | 22 | 4.2 | |
| Beet greens, cooked | 1 cup | 39 | 4.2 | |
| Salsify, cooked | 1 cup | 92 | 4.2 | |
| Cabbage, savoy, cooked | 1 cup | 35 | 4.1 | |
| Cabbage, red, cooked | 1 cup | 41 | 4.1 | |
| Wax beans, snap, cooked | 1 cup | 44 | 4.1 | |
| Edamame, cooked | 1/2 cup | 94 | 4.1 | |
| Okra, cooked | 1 cup | 36 | 4 | |
| Green beans, snap, cooked | 1 cup | 44 | 4 | |
| Hominy, canned | 1 cup | 115 | 4 | |
| Corn, cooked | 1 cup | 134 | 4 | |
| Potato, baked, with skin | 1 medium | 161 | 3.9 | |
| Lambsquarters, cooked | 1 cup | 58 | 3.8 | |
| Lotus root, cooked | 1 cup | 108 | 3.8 | |
| Swiss chard, cooked | 1 cup | 35 | 3.7 | |
| Mustard spinach, cooked | 1 cup | 29 | 3.6 | |
| Carrots, raw | 1 cup | 52 | 3.6 | |
| Hearts of palm, canned | 1 cup | 41 | 3.5 | |
| Mushrooms, cooked | 1 cup | 44 | 3.4 | |
| Bamboo shoots, raw | 1 cup | 41 | 3.3 | |
| Yardlong beans, cooked | 1/2 cup | 101 | 3.3 | |
| Turnip, cooked | 1 cup | 34 | 3.1 | |
| Red bell pepper, raw | 1 cup | 39 | 3.1 | |
| Rutabaga, cooked | 1 cup | 51 | 3.1 | |
| Plantains, cooked | 1 cup | 215 | 3.1 | |
| Nopales, cooked | 1 cup | 22 | 3 | |
| Dandelion greens, cooked | 1 cup | 35 | 3 | |
| Cassava (yuca), cooked | 1 cup | 267 | 3 | |
| Asparagus, cooked | 1 cup | 32 | 2.9 | |
| Taro leaves, cooked | 1 cup | 35 | 2.9 | |
| Onions, cooked | 1 cup | 92 | 2.9 | |
| Cabbage, cooked | 1 cup | 34 | 2.8 | |
| Mustard greens, cooked | 1 cup | 36 | 2.8 | |
| Beets, cooked | 1 cup | 49 | 2.8 | |
| Celeriac, raw | 1 cup | 66 | 2.8 | |
| Fruits | ||||
| Sapote or Sapodilla | 1 cup | 217 | 9.5 | |
| Durian | 1 cup | 357 | 9.2 | |
| Guava | 1 cup | 112 | 8.9 | |
| Nance | 1 cup | 82 | 8.4 | |
| Raspberries | 1 cup | 64 | 8 | |
| Loganberries | 1 cup | 81 | 7.8 | |
| Blackberries | 1 cup | 62 | 7.6 | |
| Soursop | 1 cup | 148 | 7.4 | |
| Boysenberries | 1 cup | 66 | 7 | |
| Gooseberries | 1 cup | 66 | 6.5 | |
| Pear, Asian | 1 medium | 75 | 6.5 | |
| Blueberries, wild | 1 cup | 80 | 6.2 | |
| Passion fruit | 1/4 cup | 57 | 6.1 | |
| Persimmon | 1 fruit | 118 | 6 | |
| Pear | 1 medium | 103 | 5.5 | |
| Kiwifruit | 1 cup | 110 | 5.4 | |
| Grapefruit | 1 fruit | 130 | 5 | |
| Apple, with skin | 1 medium | 104 | 4.8 | |
| Cherimoya | 1 cup | 120 | 4.8 | |
| Durian | 1/2 cup | 179 | 4.6 | |
| Starfruit | 1 cup | 41 | 3.7 | |
| Orange | 1 medium | 73 | 3.7 | |
| Figs, dried | 1/4 cup | 93 | 3.7 | |
| Blueberries | 1 cup | 84 | 3.6 | |
| Pomegranate seeds | 1/2 cup | 72 | 3.5 | |
| Mandarin orange | 1 cup | 103 | 3.5 | |
| Tangerine (tangelo) | 1 cup | 103 | 3.5 | |
| Pears, dried | 1/4 cup | 118 | 3.4 | |
| Peaches, dried | 1/4 cup | 96 | 3.3 | |
| Banana | 1 medium | 112 | 3.2 | |
| Apricots | 1 cup | 74 | 3.1 | |
| Prunes or dried plum | 1/4 cup | 105 | 3.1 | |
| Strawberries | 1 cup | 49 | 3 | |
| Dates | 1/4 cup | 104 | 3 | |
| Blueberries, dried | 1/4 cup | 127 | 3 | |
| Cherries | 1 cup | 87 | 2.9 | |
| Protein Foods | ||||
| Wocas, yellow pond lily seeds | 1 ounce | 102 | 5.4 | |
| Pumpkin seeds, whole | 1 ounce | 126 | 5.2 | |
| Coconut | 1 ounce | 187 | 4.6 | |
| Chia seeds | 1 Tbsp | 58 | 4.1 | |
| Almonds | 1 ounce | 164 | 3.5 | |
| Chestnuts | 1 ounce | 106 | 3.3 | |
| Sunflower seeds | 1 ounce | 165 | 3.1 | |
| Pine nuts | 1 ounce | 178 | 3 | |
| Pistachio nuts | 1 ounce | 162 | 2.9 | |
| Flax seeds | 1 Tbsp | 55 | 2.8 | |
| Hazelnuts (filberts) | 1 ounce | 178 | 2.8 | |
Footnotes:
a Some fortified foods and beverages are included. Other fortified options may exist on the market, but not all fortified foods are nutrient-dense. For example, some foods with added sugars may be fortified and would not be examples in the lists provided here.
b Some foods or beverages are not appropriate for all ages, (e.g., nuts, popcorn), particularly young children for whom some foods could be a choking hazard.
c Portions listed are not recommended serving sizes. Two lists—in ‘standard’ and ‘smaller’ portions–are provided for each dietary component. Standard portions provide at least 2.8 g of dietary fiber. Smaller portions are generally one half of a standard portion.
[Source 15 ]Table 2. Fiber supplementation instructions
| My daily fiber intake goal | 25–40 g daily |
|---|---|
| The US Department of Agriculture and US Department of Health and Human Services recommend that I eat 25 g to 40 g of fiber DAILY | Adequate fiber will regulate my bowel movements by softening hard stool and reducing the frequency of constipation adding bulk to loose stool and reducing the frequency of diarrhea. Adequate fiber will improve my anal problems and bleeding by softening hard stool and making bowel movements less traumatic thickening loose stool and making bowel movements less traumatic. Adequate fiber will reduce my risk of developing colon and rectal cancer diverticulosis complications of diverticulitis: Perforation, infection, emergency surgery. Adequate fiber will reduce my cholesterol |
| How much fiber is in the food I eat? | The fiber content in foods that you eat can be found on the “Nutrition Facts” label for processed foods. For fresh foods, fruits, and vegetables, there are a variety of Web sites that can give you the amount of fiber per serving. |
| Go slow and keep it up | Gradually work your way up to taking 20 g of fiber daily in the form of a fiber supplement AND increase fiber in your diet so that you are eating at least 10 g to 20 g of dietary fiber daily. Fiber supplementa: 20 g daily Dietary fiber: + 10–20 g daily Total fiber intake: 25–40 g daily |
| Slow and steady fiber supplement ramp-up plan | Week 1: Start counting the amount of fiber you consume in your diet on a daily basis. Purchase a fiber product that you will be able to take every day for the rest of your life. Read the label to check the fiber content. Many fiber products, especially fiber pills, have very small amounts of fiber. Choose a fiber product with 5 g or more of fiber per serving. Start drinking 8 to 10 glasses of water daily. |
| Week 2: Supplement your diet with 5 g of additional fiber daily. Drink 8 to 10 eight-oz. glasses of water daily. | |
| Week 3: Supplement your diet with 10 g of additional fiber daily. Drink 8 to 10 glasses of water daily. | |
| Week 4 and beyond: Continue to increase the amount of additional fiber daily by 5 g per week until you reach your goal of 25 g to 40 g of fiber daily for life. TIP: If you feel bloated or develop excessive gas, you are increasing your daily fiber too quickly. You may need to increase your daily fiber over a longer period of time. |
Footnotes: a Common fiber supplements: Metamucil, Konsyl, Citrucel, Fiber One. Choose the fiber supplement that works best for you. Be sure to calculate the fiber amount per serving size. Choose a fiber supplement that you would be willing to take every day as a 20-g dose (goal at the end of the ramp-up period). If you experience diarrhea with a natural fiber supplement or fiber supplement that claims “easy to take/dissolves in water,” consider changing to one of the above brand names because some natural fiber supplements contain natural laxatives as well.
Warning: If you take Coumadin (warfarin), please be sure to speak with your primary care physician or cardiologist before starting a fiber supplement because fiber may interfere with your Coumadin international normalized ratio levels.
[Source 16 ]Medications
Your hemorrhoids might only produce mild discomfort. In this case, your health care provider may suggest creams, ointments, suppositories or pads that you can buy without a prescription. These products contain ingredients such as witch hazel, or hydrocortisone and lidocaine, which can temporarily relieve pain and itching.
Hydrocortisone is a steroid that can thin your skin when used for more than a week. Ask your health care provider how long you should use it.
External hemorrhoid thrombectomy
If a painful blood clot has formed within an external hemorrhoid, your health care provider can remove the hemorrhoid. Removal can provide relief right away. This procedure, done with a medicine that numbs a part of the body, also called a local anesthetic, works best when done within 72 hours of getting a clot.
Minimally invasive procedures
For persistent bleeding or painful hemorrhoids, your doctor may recommend one of the other minimally invasive procedures available. These treatments can be done in your doctor’s office or other outpatient setting and do not usually require anesthesia.
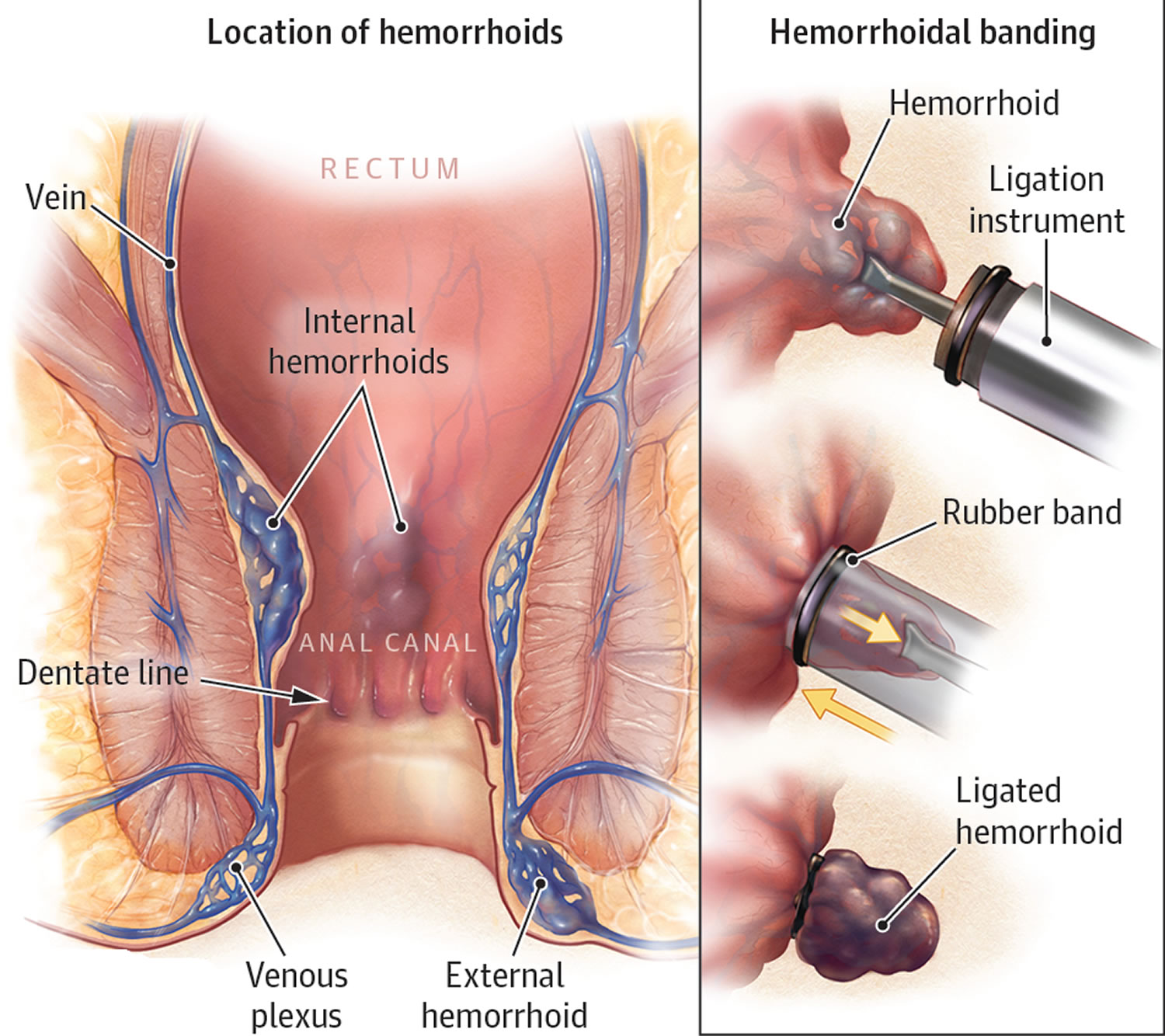
Rubber band ligation
Rubber band ligation is the most commonly performed procedure in the office and is indicated for grade 2 and 3 internal hemorrhoids 17. Your doctor places one or two tiny rubber bands around the base of an internal hemorrhoid to cut off its circulation. Performing rubber band ligation does not require any local anesthetic. The hemorrhoid withers and falls off within a week, at which time you may notice a small amount of bleeding. This procedure is effective for many people. Rubber band ligation contraindications include symptomatic external disease and patients with bleeding disorders (coagulopathies) or on chronic blood thinners (anticoagulation) due to risk of delayed hemorrhage 3. There is also an increased risk of sepsis in immunocompromised patients 18.
Your doctor may place anywhere from one to three rubber bands per visit and this may require several short visits to achieve relief of your symptoms, but is not associated with any significant recovery time for most people. Rubber band can be associated with a dull ache or feeling of pressure lasting 1 to 3 days that is usually well-treated with Ibuprofen or Tylenol. Upon completion of your banding session(s), you likely will not need further treatment, provided you continue the previously described dietary and lifestyle changes. If your symptoms return, repeat banding certainly can be considered. Hemorrhoidectomy is always an option if significant progress is not made with banding. Complications are very uncommon, but may include delayed bleeding, pain, urinary retention, and perineal infection, among others. Overall, banding is a safe, quick, and effective procedure for internal hemorrhoids.
Figure 4. Hemorrhoids rubber band ligation
Injection (sclerotherapy)
Sclerotherapy is indicated for patients with grade 1 and 2 internal hemorrhoids. In this procedure, your doctor injects a chemical solution into the hemorrhoid tissue to shrink it. Like rubber band ligation, sclerotherapy does not require local anesthesia. Performed through an anoscope, internal hemorrhoids are located and injected with a sclerosant material—typically a solution including phenol in vegetable oil—into the submucosa. The sclerosant subsequently causes fibrosis, fixation to the anal canal, and eventual obliteration of the redundant hemorrhoidal tissue. Sclerotherapy is similarly quick, often painless, has few complications, and may take several short sessions to achieve relief of symptoms. Sclerotherapy has the potential to be used in patients taking blood thinners such as Coumadin, Heparin, or Plavix, but would need to be discussed with your physician. Complications of sclerotherapy include minor discomfort or bleeding. However, rectal fistulas or perforation can very rarely occur due to misplaced injections 19.
Coagulation (infrared, laser or bipolar)
Coagulation techniques use laser or infrared light or heat direct application to the hemorrhoidal tissues and can be used for grade 1 and 2 internal hemorrhoids. To perform this procedure, the tip of the infrared coagulation applicator is usually applied to the base of the internal hemorrhoid for 2 seconds, with three to five treatments per hemorrhoid. By converting infrared light waves to heat, the applicator causes necrosis of the hemorrhoid, visualized as a white, blanched mucosa. Over time, the affected mucosa scars and shrivel, leading to retraction of the prolapsed hemorrhoid mucosa. Coagulation techniques are very safe with only minor pain and bleeding reported 20. This procedure is usually quick, painless, has few complications, but may take several short sessions to achieve relief of symptoms.
While coagulation has few side effects and may cause little immediate discomfort, it’s associated with a higher rate of hemorrhoids coming back (recurrence) than is the rubber band treatment. MacRae and McLeod 20 conducted a meta-analysis of 18 trials and concluded that rubber band ligation was better than sclerotherapy in response to treatment for grade 1 and 3 hemorrhoids, with no differences in the complication rate. The authors also noted that patients treated with sclerotherapy or infrared coagulation were more likely to require additional subsequent procedure or therapies in comparison to those treated with rubber band ligation. Finally, although pain was greater after rubber band ligation, recurrent symptoms were less common.
Doppler-guided hemorrhoidal artery ligation
First described by Morinaga et al in 1995, this technique involves use of Doppler ultrasound to identify and tie up (ligate) the hemorrhoidal arteries 21. This is also referred to as transanal hemorrhoidal dearterialization (THD). Different platforms with different associated nomenclatures exist for this technique, but the principles include the use of a Doppler probe to identify the six main feeding arteries within the anal canal, ligation of these arteries with absorbable suture and a specialized anoscope, and then plication of redundant hemorrhoidal mucosa 3. The plication is often referred to as recto-anal-repair, mucopexy, or hemorrhoidopexy. Proposed benefits of this procedure are similar to stapled hemorrhoidopexy, with less associated pain due to the suturing being above the dentate line.
Early results of Doppler-guided hemorrhoidal artery ligation or transanal hemorrhoidal dearterialization (THD) were promising, with lower pain scores than hemorrhoidectomy, and relief of bleeding and tissue prolapse in over 90% of patients 22. Since then, several randomized clinical trials have been performed with mixed results 23, 24, 25. Currently, Doppler-guided hemorrhoidal artery ligation or transanal hemorrhoidal dearterialization (THD) remains a viable approach to multicolumn internal hemorrhoids. However, the short-term benefits regarding postoperative pain have recently not been as remarkable as in the earlier studies 3.
Surgical procedures
If other procedures haven’t been successful or you have large hemorrhoids, your doctor may recommend a surgical procedure. Your surgery may be done as an outpatient or may require an overnight hospital stay.
For patients who present with thrombosed external hemorrhoids, surgical evaluation and intervention within 72 hours of thrombosis may result in significant relief, as pain and edema peak at 48 hours 26. However, after 48 to 72 hours, organization of the thrombus and reduction of symptoms generally obviates the need for surgical evacuation, which is consistent with the natural history of hemorrhoidal thrombosis. After the initial 72-hour window, the pain typically plateaus and slowly improves, at which point the pain from hemorrhoid excision would exceed the pain from the thrombosis itself 3.
Table 3. Surgical Treatment by Hemorrhoid Type
| Hemorrhoid type/grade | Office-based procedures | Hospital-based procedures |
|---|---|---|
| External (not graded) | In patients with severe symptoms, excision or incision under local anesthesia within 72 hours of onset; after 72 hours use medical treatment | — |
| Combined external and internal | — | Excisional hemorrhoidectomy |
| Internal grade 1 | Rubber band ligation, infrared coagulation | Rubber band ligation; excisional hemorrhoidectomy if primary treatment is ineffective |
| Internal grade 2 | Rubber band ligation, infrared coagulation | Rubber band ligation; stapled hemorrhoidopexy; excisional hemorrhoidectomy if primary treatment is ineffective |
| Internal grade 3 | Rubber band ligation | Rubber band ligation; excisional hemorrhoidectomy; stapled hemorrhoidopexy |
| Internal grade 4 | — | Excisional hemorrhoidectomy; stapled hemorrhoidopexy |
Hemorrhoidectomy
Hemorrhoidectomy also called hemorrhoid removal, your surgeon removes excessive tissue that causes bleeding. Various techniques may be used (Ferguson, or closed hemorrhoidectomy and the Milligan–Morgan, or open hemorrhoidectomy). The surgery may be done with a local anesthetic combined with sedation, a spinal anesthetic or a general anesthetic. Patients with grade 3 and 4 internal hemorrhoids benefit the most from surgical hemorrhoidectomy. Most people experience some pain after the procedure. Medications can relieve your pain. Soaking in a warm bath also may help.
Hemorrhoidectomy is the most effective and complete way to treat severe or recurring hemorrhoids. Complications may include temporary difficulty emptying your bladder and resulting urinary tract infections. Bleeding may occur in 1 to 2% of patients after 1 week from surgery as a result of scar tissue separation and is usually self-limited.22 Infection is uncommon after hemorrhoid surgery with submucosal abscesses occurring in less than 1% of cases and severe fasciitis or necrotizing infections are rare 27. Urinary retention has been reported to be as high as 34% after hemorrhoidectomy, which is attributed to pelvic floor spasm, narcotic use, and excess intravenous fluids 28. Treatment for urinary retention after hemorrhoidectomy is temporary Foley catheter insertion with self-resolution in majority of cases. Injury to the sphincter resulting in fecal incontinence occurs in 2 to 10% of cases and can have significant impact on quality of life 29. Lastly, anal stenosis is a late complication that can result from excessive tissue resection or aggressive suturing. Anal stenosis is more common with multiple excised quadrants; it is often difficult to treat and should be diligently avoided by assuring adequate mucosal bridges between the excised hemorrhoids.
Despite its relative higher morbidity, surgical hemorrhoidectomy is more effective than band ligation for preventing recurrent symptoms 20. In a randomized trial among elective cases, there were no differences in open versus closed hemorrhoidectomy 30.
Stapled Hemorrhoidopexy
Stapled hemorrhoidectomy also called stapled hemorrhoidopexy or hemorrhoid stapling, is a procedure where a stapling device is used to cut blood flow to hemorrhoidal tissue and fixate the internal hemorrhoid tissues to the rectal wall. Stapled hemorrhoidectomy is typically used only for internal hemorrhoids.
Since the staple line is above the dentate line, patients typically experience less pain than those who undergo hemorrhoidectomy and allows for earlier return to regular activities. To perform this procedure, a circular stapler is introduced into the anus and prolapsing tissue is brought into the stapler. The most critical component of stapled hemorrhoidopexy is the placement of a circumferential, purse-string, nonabsorbable suture in the submucosa far enough away to avoid any sphincter muscle involvement—usually at ∼4 cm from the dentate line. Additionally, before engaging the stapler, an examination of the posterior vaginal wall should be conducted. Finally, the staple line should be evaluated for any bleeding that would require additional suture ligation.
Compared with hemorrhoidectomy, stapling has been associated with a greater risk of recurrence and rectal prolapse, in which part of the rectum protrudes from the anus. Complications from stapled hemorrhoidopexy can also include bleeding from the staple line, incontinence for injury of the sphincter muscles, anal stenosis from incorporation of excess rectal tissue, urinary retention and pain, as well as, rarely, a life-threatening blood infection (sepsis). Moreover, there is a risk of recto-vaginal fistula in women due to incorporation of vaginal tissue into the purse-string. Talk with your doctor about the best option for you.
Moving your bowels after hemorrhoid surgery is always a concern for patients. Most colon and rectal surgeons recommend having a bowel movement within the first 48 hours after surgery. You should already be taking a diet high in fiber, a fiber supplement, and increased liquid intake. If this does not produce a bowel movement, you may need to take laxatives to achieve this. Your doctor should make recommendations as to the best medications to use in this situation, given your particular medical issues. Expect to have some bleeding with bowel movements for several weeks after surgery. Call your surgeon if you are experiencing bleeding that doesn’t seem to stop after the bowel movement.
Three systematic reviews concluded that stapled hemorrhoidopexy was less effective than conventional hemorrhoidectomy 31, 32, 33. Stapled hemorrhoidopexy was associated with a higher long-term risk of hemorrhoid recurrence. Due to need for additional operations, the incidence of prolapse and tenesmus was also higher after stapled hemorrhoidopexy as compared with hemorrhoidectomy. Conversely, the stapled approach was associated with significantly less pain, shorter operative time, and shorter time to resumption of normal activity. In a 2010 European multicenter randomized trial of stapled hemorrhoidopexy versus hemorrhoidectomy, both options were shown to be equally effective in preventing recurrence after 1 year 34. Patients undergoing hemorrhoidectomy were more likely to have symptomatic relief from the hemorrhoids (69 vs. 44%), but had significantly greater postoperative pain 34.
Overall, stapled hemorrhoidopexy remains a viable alternative to hemorrhoidectomy, and is especially attractive for patients without much external disease. However, while the published complication rates are low, they can be quite severe, and the surgeon must have appropriate training and proceed with great caution, when performing this procedure 3.
- Hemorrhoids. Medline Plus. https://medlineplus.gov/hemorrhoids.html[↩]
- Hemorrhoids and Other Anal Disorders. American College of Gastroenterology. http://patients.gi.org/topics/hemorrhoids-and-other-anal-disorders/[↩]
- Sun Z, Migaly J. Review of Hemorrhoid Disease: Presentation and Management. Clin Colon Rectal Surg. 2016 Mar;29(1):22-9. doi: 10.1055/s-0035-1568144[↩][↩][↩][↩][↩][↩][↩]
- Hemorrhoids. American Society of Colon and Rectal Surgeons. https://www.fascrs.org/patients/disease-condition/hemorrhoids-expanded-version[↩]
- Banov L Jr, Knoepp LF Jr, Erdman LH, Alia RT. Management of hemorrhoidal disease. J S C Med Assoc. 1985 Jul;81(7):398-401.[↩]
- Perrotti P, Antropoli C, Molino D, De Stefano G, Antropoli M. Conservative treatment of acute thrombosed external hemorrhoids with topical nifedipine. Dis Colon Rectum. 2001;44(3):405–409.[↩]
- Greenspon J, Williams SB, Young HA, Orkin BA. Thrombosed external hemorrhoids: outcome after conservative or surgical management. Dis Colon Rectum. 2004;47(9):1493–1498.[↩]
- Zuber TJ. Hemorrhoidectomy for thrombosed external hemorrhoids. Am Fam Physician. 2002;65(8):1629–1632.[↩]
- Hemorrhoids. Am Fam Physician. 2011 Jul 15;84(2):204-210. http://www.aafp.org/afp/2011/0715/p204.html[↩][↩]
- Goenka MK, Kochhar R, Nagi B, Mehta SK. Rectosigmoid varices and other mucosal changes in patients with portal hypertension. Am J Gastroenterol. 1991 Sep;86(9):1185-9.[↩]
- Thomson WH. The nature of haemorrhoids. Br J Surg. 1975 Jul;62(7):542-52. doi: 10.1002/bjs.1800620710[↩]
- Morgado PJ, Suárez JA, Gómez LG, Morgado PJ Jr. Histoclinical basis for a new classification of hemorrhoidal disease. Dis Colon Rectum. 1988 Jun;31(6):474-80. doi: 10.1007/BF02552621[↩]
- Cataldo P, Ellis CN, Gregorcyk S, et al.; Standards Practice Task Force, The American Society of Colon and Rectal Surgeons, USA. Practice parameters for the management of hemorrhoids (revised). Dis Colon Rectum. 2005;48(2):189–194.[↩][↩]
- Dietary Guidelines for Americans. https://www.dietaryguidelines.gov[↩]
- Food Sources of Dietary Fiber. https://www.dietaryguidelines.gov/resources/2020-2025-dietary-guidelines-online-materials/food-sources-select-nutrients/food-0[↩]
- Chang J, Mclemore E, Tejirian T. Anal Health Care Basics. Perm J. 2016 Fall;20(4):15-222. doi: 10.7812/TPP/15-222[↩]
- Iyer VS, Shrier I, Gordon PH. Long-term outcome of rubber band ligation for symptomatic primary and recurrent internal hemorrhoids. Dis Colon Rectum. 2004 Aug;47(8):1364-70. doi: 10.1007/s10350-004-0591-2[↩]
- Buchmann P, Seefeld U. Rubber band ligation for piles can be disastrous in HIV-positive patients. Int J Colorectal Dis. 1989;4(1):57-8. doi: 10.1007/BF01648552[↩]
- Barwell J, Watkins RM, Lloyd-Davies E, Wilkins DC. Life-threatening retroperitoneal sepsis after hemorrhoid injection sclerotherapy: report of a case. Dis Colon Rectum. 1999 Mar;42(3):421-3. doi: 10.1007/BF02236364[↩]
- MacRae HM, McLeod RS. Comparison of hemorrhoidal treatment modalities. A meta-analysis. Dis Colon Rectum. 1995 Jul;38(7):687-94. doi: 10.1007/BF02048023[↩][↩][↩]
- Morinaga K, Hasuda K, Ikeda T. A novel therapy for internal hemorrhoids: ligation of the hemorrhoidal artery with a newly devised instrument (Moricorn) in conjunction with a Doppler flowmeter. Am J Gastroenterol. 1995 Apr;90(4):610-3.[↩]
- Giordano P, Overton J, Madeddu F, Zaman S, Gravante G. Transanal hemorrhoidal dearterialization: a systematic review. Dis Colon Rectum. 2009 Sep;52(9):1665-71. doi: 10.1007/DCR.0b013e3181af50f4[↩]
- De Nardi P, Capretti G, Corsaro A, Staudacher C. A prospective, randomized trial comparing the short- and long-term results of doppler-guided transanal hemorrhoid dearterialization with mucopexy versus excision hemorrhoidectomy for grade III hemorrhoids. Dis Colon Rectum. 2014 Mar;57(3):348-53. doi: 10.1097/DCR.0000000000000085[↩]
- Denoya PI, Fakhoury M, Chang K, Fakhoury J, Bergamaschi R. Dearterialization with mucopexy versus haemorrhoidectomy for grade III or IV haemorrhoids: short-term results of a double-blind randomized controlled trial. Colorectal Dis. 2013;15(10):1281-8. doi: 10.1111/codi.12303[↩]
- Elmér SE, Nygren JO, Lenander CE. A randomized trial of transanal hemorrhoidal dearterialization with anopexy compared with open hemorrhoidectomy in the treatment of hemorrhoids. Dis Colon Rectum. 2013 Apr;56(4):484-90. doi: 10.1097/DCR.0b013e31827a8567[↩]
- Aigner F, Gruber H, Conrad F, Eder J, Wedel T, Zelger B, Engelhardt V, Lametschwandtner A, Wienert V, Böhler U, Margreiter R, Fritsch H. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease. Int J Colorectal Dis. 2009 Jan;24(1):105-13. doi: 10.1007/s00384-008-0572-3[↩]
- Bleday R, Pena JP, Rothenberger DA, Goldberg SM, Buls JG. Symptomatic hemorrhoids: current incidence and complications of operative therapy. Dis Colon Rectum. 1992 May;35(5):477-81. doi: 10.1007/BF02049406[↩]
- Hoff SD, Bailey HR, Butts DR, Max E, Smith KW, Zamora LF, Skakun GB. Ambulatory surgical hemorrhoidectomy–a solution to postoperative urinary retention? Dis Colon Rectum. 1994 Dec;37(12):1242-4. doi: 10.1007/BF02257789[↩]
- Gravié JF, Lehur PA, Huten N, Papillon M, Fantoli M, Descottes B, Pessaux P, Arnaud JP. Stapled hemorrhoidopexy versus milligan-morgan hemorrhoidectomy: a prospective, randomized, multicenter trial with 2-year postoperative follow up. Ann Surg. 2005 Jul;242(1):29-35. doi: 10.1097/01.sla.0000169570.64579.31[↩]
- Reis Neto JA, Quilici FA, Cordeiro F, Reis Júnior JA. Open versus semi-open hemorrhoidectomy: a random trial. Int Surg. 1992 Apr-Jun;77(2):84-90.[↩]
- Giordano P, Gravante G, Sorge R, Ovens L, Nastro P. Long-term outcomes of stapled hemorrhoidopexy vs conventional hemorrhoidectomy: a meta-analysis of randomized controlled trials. Arch Surg. 2009 Mar;144(3):266-72. doi: 10.1001/archsurg.2008.591[↩]
- Lumb KJ, Colquhoun PH, Malthaner RA, Jayaraman S. Stapled versus conventional surgery for hemorrhoids. Cochrane Database Syst Rev. 2006 Oct 18;2006(4):CD005393. doi: 10.1002/14651858.CD005393.pub2[↩]
- Nisar PJ, Acheson AG, Neal KR, Scholefield JH. Stapled hemorrhoidopexy compared with conventional hemorrhoidectomy: systematic review of randomized, controlled trials. Dis Colon Rectum. 2004 Nov;47(11):1837-45. doi: 10.1007/s10350-004-0679-8[↩]
- Nyström PO, Qvist N, Raahave D, Lindsey I, Mortensen N; Stapled or Open Pile Procedure (STOPP) trial study group. Randomized clinical trial of symptom control after stapled anopexy or diathermy excision for haemorrhoid prolapse. Br J Surg. 2010 Feb;97(2):167-76. doi: 10.1002/bjs.6804[↩][↩]