Contents
What is idiopathic hypersomnia
Idiopathic hypersomnia is sleeping too much (hypersomnia) with daily periods of an irrepressible need to sleep without an obvious cause. People with idiopathic hypersomnia have a hard time staying awake during the day (chronic excessive daytime sleepiness) even though they seem to sleep well at night with a total sleep time of 12 to 14 hours is typical in a 24-hour period. People with idiopathic hypersomnia need to take frequent long naps, but usually do not feel refreshed upon waking and have difficulty waking up. Compared to patients who are long sleepers, patients with idiopathic hypersomnia never feel fully refreshed and awake. Simply increasing the total time spent in bed does not resolve the excessive daytime sleepiness. An increased amount of time spent asleep is not a feature of idiopathic hypersomnia 1.
The immediate need for sleep may come at anytime during the day, including while working, in class, or driving a car. People with idiopathic hypersomnia should avoid activities that may be dangerous, and should avoid driving or operating dangerous machinery unless sleepiness is well controlled by medication 2. Many people with idiopathic hypersomnia may feel very drowsy and confused when waking up (also known as “sleep drunkenness”). Other symptoms may include anxiety, feeling irritated, low energy, restlessness, slow thinking or speech, loss of appetite, and memory difficulties. Symptoms of idiopathic hypersomnia often develop during the teen or young adult years.
The prevalence of idiopathic hypersomnia among the general population is estimated at around 50 per 1 million individuals. Among patients seen in sleep centers, patients with idiopathic hypersomnia are five to ten percent less common than patients with narcolepsy. A large study of 6,000 sleep patients at a respiratory sleep center found that 1 percent of the patients seen had idiopathic hypersomnia 1.
The cause of idiopathic hypersomnia is unknown (note idiopathic means unknown). Currently there is no treatment approved by the Food and Drug Administration (FDA) specifically for idiopathic hypersomnia, but some people may be helped by medications used to treat other disorders.
Idiopathic hypersomnia is different from narcolepsy, because idiopathic hypersomnia does not involve suddenly falling asleep or losing muscle control due to strong emotions (cataplexy).
Idiopathic hypersomnia is diagnosed when a patient has experienced constantly severe excessive daytime sleepiness for at least three months without other defining features, such as REM sleep abnormalities or cataplexy.
Individuals with idiopathic hypersomnia often experience depression; depressive symptoms have been noted in 15 to 25 percent of these patients 1. They also are prone to headaches, with migraines and tension-type headaches reported by about 30 percent of patients with idiopathic hypersomnia 1.
The overall psychosocial handicap of patients with idiopathic hypersomnia is similar to that of patients with narcolepsy 3.
Idiopathic hypersomnia vs Narcolepsy
Narcolepsy is a rare long-term brain disorder that causes a person to suddenly fall asleep at inappropriate times. Narcolepsy is a lifelong sleep disorder that makes you feel overwhelmingly tired, and in severe cases, have sudden uncontrollable sleep attacks.
Narcolepsy can result in:
- excessive daytime sleepiness – feeling very drowsy throughout the day, and having difficulty concentrating and staying awake
- sleep attacks – falling asleep suddenly and without warning
- cataplexy – temporary loss of muscle control resulting in weakness and possible collapse, often in response to emotions such as laughter and anger
- sleep paralysis – a temporary inability to move or speak when waking up or falling asleep
- excessive dreaming and waking in the night – dreams often come as you fall asleep (hypnogogic hallucinations) or just before or during waking (hypnopompic hallucinations)
Narcolepsy doesn’t cause serious or long-term physical health problems, but it can have a significant impact on daily life and be difficult to cope with emotionally.
Excessive daytime sleepiness
In most cases, excessive daytime sleepiness is the first sign of narcolepsy. This can have a significant impact on everyday life.
Feeling drowsy throughout the day and struggling to stay awake makes it difficult to concentrate at work or school. People with narcolepsy may be misjudged as being lazy or rude.
Sleep attacks
Sleep attacks – falling asleep suddenly and without warning – are also common in people with narcolepsy. They may occur at any time.
The length of time a sleep attack lasts will vary from person to person. Some people will only have “microsleeps” lasting a few seconds, whereas others may fall asleep for several minutes.
If narcolepsy isn’t well controlled, sleep attacks may happen several times a day.
Cataplexy
Most people who have narcolepsy also experience cataplexy – sudden, temporary muscle weakness or loss of muscular control.
Typical symptoms are:
- the jaw dropping
- the head slumping down
- legs collapsing uncontrollably
- slurred speech
- double vision or finding it difficult to focus
Cataplexy attacks are usually triggered by an emotion, such as excitement, laughter, anger or surprise. Attacks can last from a few seconds to several minutes.
Some people with narcolepsy have cataplexy attacks once or twice a year, while others experience them several times a day. In an attempt to avoid attacks, some people may become emotionally withdrawn and socially isolated.
Sleep paralysis
Some people with narcolepsy experience episodes of sleep paralysis. This is a temporary inability to move or speak that occurs when waking up or falling asleep.
The episodes can last from a few seconds to several minutes. Although sleep paralysis doesn’t cause any harm, being unable to move can be frightening.
Other symptoms of narcolepsy
As well as the symptoms described above, narcolepsy can cause a number of other symptoms, including:
- hallucinations – seeing or hearing things that aren’t real, particularly when going to sleep or waking up; a presence in the bedroom is the most commonly
- reported hallucination
- memory problems
- headaches
- restless sleep – for example, having hot flushes, waking up frequently, having vivid nightmares, or physically acting out dreams
- automatic behavior – continuing with an activity without having any recollection of it afterwards
- depression
Narcolepsy can impact nearly every aspect of your life. It is dangerous because you can have excessive sleepiness or a sleep attack at any time of the day, in the middle of any activity including eating, walking or driving. Operating a vehicle with untreated narcolepsy can be very dangerous and some states even have laws against it.
Idiopathic hypersomnia causes
Idiopathic hypersomnia appears to have a genetic component, as 50% to 60% of cases are familial. Women may be at greater risk; a preponderance among female patients has been found in some, but not all, series. Metabolic data suggest the possibility of a dysfunction of aminergic arousal systems in idiopathic hypersomnia 4.
Because both idiopathic hypersomnia and narcolepsy share overlapping features, there is some interest in exploring the role of human leukocyte antigen (HLA) markers for idiopathic hypersomnia. Despite reports of an increase in HLA DQ1,8 DR5 and Cw2, and DQ3 and of a decrease of Cw3, no consistent findings have emerged. HLA typing currently does not play a role in the diagnosis of idiopathic hypersomnia 1.
Idiopathic hypersomnia symptoms
Individuals who have idiopathic hypersomnia take frequent naps that are un-refreshing, have difficulty waking up, and experience post-awakening confusion (also known as “sleep drunkenness”). Compared to patients who are long sleepers, patients with idiopathic hypersomnia never feel fully refreshed and awake. Simply increasing the total time spent in bed does not resolve the excessive daytime sleepiness.
Idiopathic hypersomnia is defined by the presence or absence of long sleep time (i.e., more than 10 hours).
Idiopathic hypersomnia diagnosis
To diagnose your condition, your doctor will review your symptoms, go over your family and medical history, including your medications, and conduct a physical examination. Your doctor might order several tests to diagnose your condition, determine the cause of your condition and rule out other conditions.
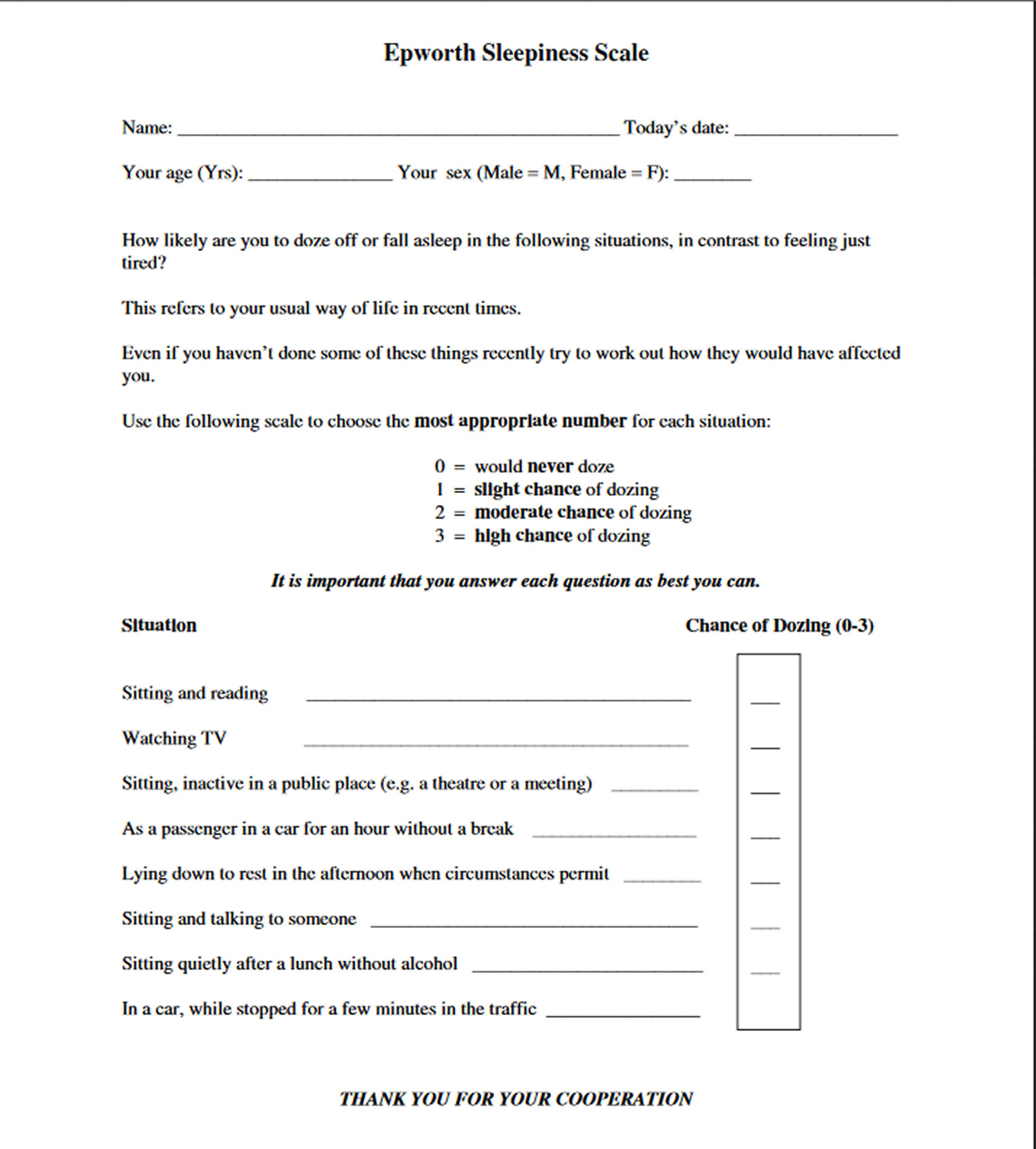
- Epworth Sleepiness Scale. Your doctor may ask you to rate your sleepiness with this tool to help determine how sleep affects your daily life.
- Sleep diary. Your doctor may ask you to keep a sleep diary in which you log your daily sleep and wake times to help show your sleep amounts and pattern.
- Polysomnogram. In this test, you stay in a sleep center overnight. A polysomnogram monitors your brain activity, eye movements, leg movements, heart rate, breathing functions and oxygen levels as you sleep.
- Multiple sleep latency test. This measures your sleepiness and the types and stages of sleep you go through during daytime naps. This test is generally conducted the day after a polysomnogram.
Idiopathic hypersomnia is diagnosed only after ruling out other possible causes, including: Behaviorally-induced insufficient sleep syndrome, delayed sleep phase syndrome, periodic limb movement disorder, sleep-related disordered breathing, narcolepsy, and secondary hypersomnia 1. In addition, the hypersomnia symptoms may not be caused by a different sleep disorder, medical disorder, psychiatric disorder, or by medication or substance abuse 5.
Among those with idiopathic hypersomnia, polysomnography shows “short sleep latency, a major sleep period of more than 10 hours, with laborious wakening in the morning or from naps, in the polysymptomatic form, or a major sleep period of 6 to 10 hours in the oligosymptomatic form.”5 The Multiple Sleep Latency Test shows a mean latency of less than eight minutes and no sleep-onset REM periods 5.
Epworth sleepiness scale
The Epworth sleepiness scale) is a questionnaire used to assess how likely you are to fall asleep while undertaking different activities. Your GP will use the results of your completed questionnaire to decide whether to refer you to a sleep specialist.
When you fill out the questionnaire, you will be asked to rank the likelihood that you will fall asleep in situations such as sitting and reading, watching television, and travelling as a passenger in a car.
A score of 10 or below indicates you have a level of daytime sleepiness equal to the general population. A score of 11 or above indicates you have an increased level of daytime sleepiness. If this is the case, your doctor will probably refer you to a sleep specialist for further investigation.
Figure 1. Epworth Sleepiness Scale Questionnaire
How to score the Epworth Sleepiness Scale
All Epworth Sleepiness Scale item-scores are intended to be integers (0-3). However, some people cannot decide on one number and report half-values. It is recommended that these scores be taken at face value. If, after adding them up, the total Epworth Sleepiness Scale score includes a half, it should be rounded up to the next whole number. If one or more item-scores are missing, that Epworth Sleepiness Scale is invalid because it is not feasible to interpolate missing item-scores. The Epworth Sleepiness Scale score (the sum of 8 item-scores) is the only number required under most circumstances.
- If total score less than 8 – indicates reported normal daytime alertness
- 8 to 11 – indicates mild sleepiness
- 12 to 15 – indicates moderate sleepiness
- 16 to 24 – indicates severe sleepiness
Polysomnography
Polysomnography is an investigation of your sleep carried out at a specialist sleep center. The study usually involves staying overnight at the sleep centre so your sleeping patterns can be analysed.
During the night, several different parts of your body will be carefully monitored using electrodes and bands that are placed on the surface of your body while you sleep. Sensors will also be placed on your legs and an oxygen sensor is attached to your finger.
A number of different tests will be carried out during polysomnography, including:
- electroencephalography (EEG) – which monitors brain waves
- electrooculography – which monitors eye movements
- electromyography (EMG) – which monitors muscle tone
- recordings of movements in your chest and abdomen
- recordings of airflow through your mouth and nose
- pulse oximetry – which measures your heart rate and blood oxygen levels
- electrocardiography (ECG) – which monitors your heart
Sound recording and video equipment may also be used to record sound and images.
After you have slept, a specialist will analyze your test results to determine whether you have normal brain wave activity, breathing patterns, and muscle and eye movement.
Multiple sleep latency test
A multiple sleep latency test measures how long it takes for you to fall asleep during the day. You may have this test after polysomnography.
You will be asked to take several naps throughout the day, and a specialist will analyse how quickly and easily you fall asleep.
If you have narcolepsy, you will usually fall asleep easily and enter rapid eye movement (REM) sleep very quickly.
Idiopathic hypersomnia treatment
Because the cause of idiopathic hypersomnia isn’t known, the treatment is aimed at easing symptoms. Treatments for hypersomnia (excessive daytime sleepiness) are generally aimed at excessive daytime sleepiness, rather than at sleep duration or sleep drunkenness (confusion upon waking up). Although there are multiple treatments approved by the Food and Drug Administration (FDA) for narcolepsy, there are no FDA-approved treatments idiopathic hypersomnia. Therefore, treatment generally involves off-label use of medications approved for narcolepsy. Unfortunately, the use of these medications is inadequate to improve symptoms in many people with idiopathic hypersomnia. These medication options may include 6:
- Wakefulness-promoting agents (modafinil and armodafinil)
- Traditional psychostimulants (amphetamines, methylphenidate, and their derivatives)
There are also several emerging therapies for cases that do not respond to the above types of medications. These include sodium oxybate, clarithromycin, and flumazenil 6.
Non-medical approaches such as behavior modification are not generally effective for people with idiopathic hypersomnia. Unlike in narcolepsy, where scheduled naps can help, daytime naps in people with idiopathic hypersomnia are typically long and nonrestorative 2.
Following up with physicians at least annually (preferably more frequently) is recommended to assess for side effects of medication, sleep or mood disturbances, adequate control of symptoms, and any work-related or social issues 2.
- Bassetti C, and Y Dauvilliers, “Idiopathic Hypersomnia,” In: Kryger MH, Roth T III, Dement WC, eds. Principles and Practice of Sleep Medicine (5th edition), Philadelphia, Pa: Elsevier Saunders; 2011:969-979.[↩][↩][↩][↩][↩][↩]
- Chervin R. Idiopathic Hypersomnia. UpToDate. Waltham, MA. https://www.uptodate.com/contents/idiopathic-hypersomnia[↩][↩][↩]
- Bassetti C, and Y Dauvilliers, “Idiopathic Hypersomnia,” In: Kryger MH, Roth T III, Dement WC, eds. Principles and Practice of Sleep Medicine (5th edition), Philadelphia, Pa: Elsevier Saunders; 2011, pages 969-979.[↩]
- Bassetti C, and Y Dauvilliers, “Idiopathic Hypersomnia,” In: Kryger MH, Roth T III, Dement WC, eds. Principles and Practice of Sleep Medicine (5th edition), Philadelphia, Pa: Elsevier Saunders; 2011: 970.[↩]
- Billiard M, Dauvilliers Y. Idiopathic hypersomnia. Sleep Med Rev. 2001;5:349-358.[↩][↩][↩]
- Saini P, Rye DB. Hypersomnia: Evaluation, Treatment, and Social and Economic Aspects. Sleep Med Clin. March, 2017; 12(1):47-60. https://www.ncbi.nlm.nih.gov/pubmed/28159097[↩][↩]