Contents
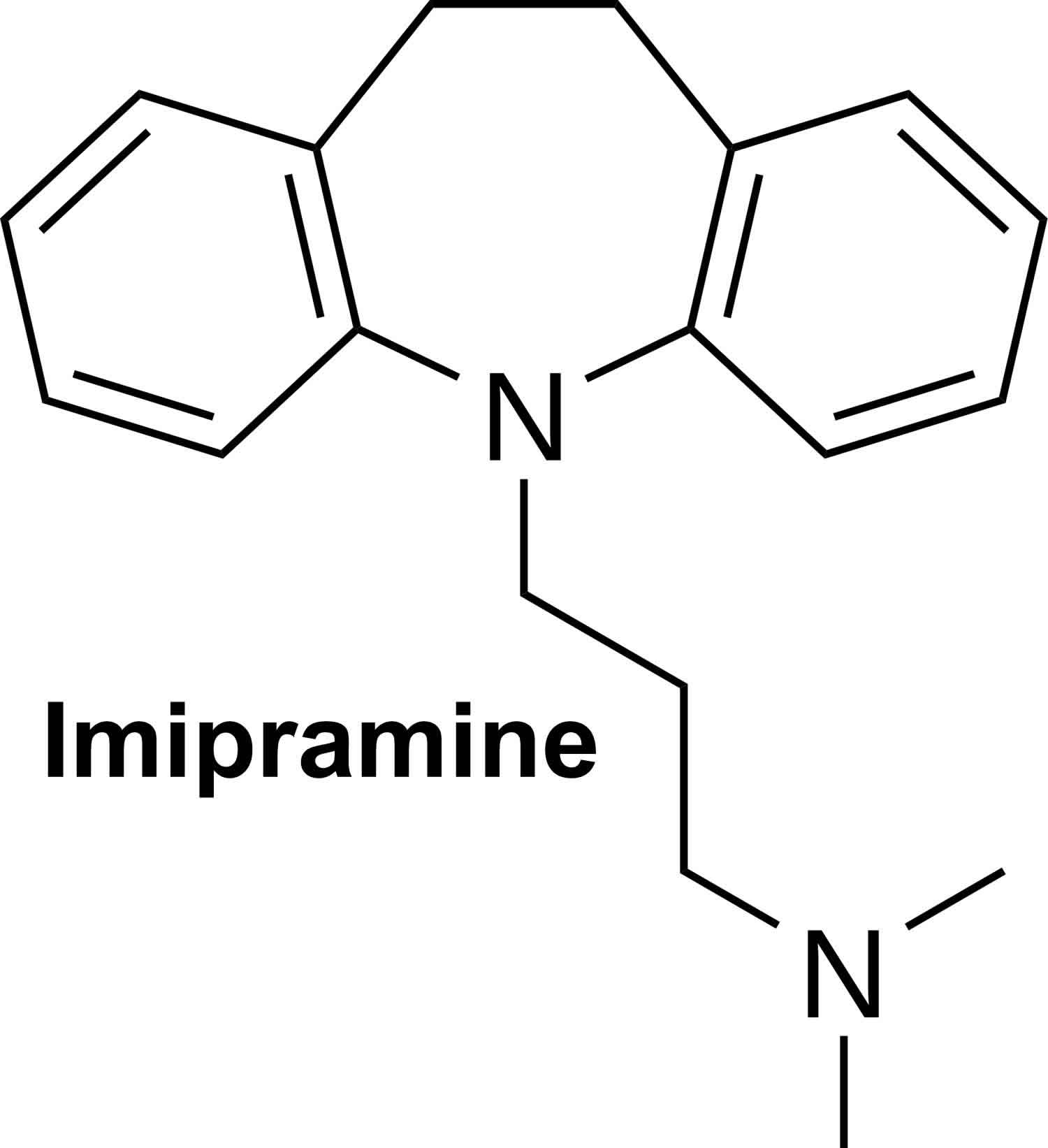
What is imipramine
Imipramine is a tricyclic antidepressant that continues to be widely used in the therapy of depression. Imipramine is also used for childhood bedwetting (enuresis) in children ages 6 and older. Imipramine is available in generic forms and under the brand names of Tofranil in 10, 25, and 50 mg tablets and as capsules of 75, 100, 125 and 150 mg for nighttime dosing. The typical recommended dose for depression in adults is 75 to 100 mg daily in divided doses, increasing gradually to a maximum of 200 mg daily. Imipramine can also be given as a single nighttime dose. The recommended dose in children (ages 6 years or above) is 25 to 75 mg daily 1 hour before bedtime. Common side effects include dizziness, headache, drowsiness, restlessness, confusion, gastrointestinal upset, increased appetite, weight gain, blurred vision, dry mouth and urinary retention. Imipramine can cause mild and transient serum enzyme elevations and is rare cause of clinically apparent acute cholestatic liver injury.
Imipramine is a dibenzazepine derived tricyclic antidepressant that acts by inhibition of serotonin and norepinephrine reuptake within synaptic clefts in the central nervous system, thus increasing brain levels of these neurotransmitters. Imipramine is indicated for therapy of depression and was approved for this indication in the United States in 1959; it is still widely used, with more than 1 million prescriptions being filled yearly.
Imipramine comes as a tablet and a capsule to take by mouth. When imipramine tablets or capsules are used to treat depression, they are usually taken one or more times a day and may be taken with or without food. When imipramine tablets are used to prevent bedwetting in children, they are usually taken one hour before bedtime. Children who wet the bed early in the evening may be given one dose in the mid-afternoon and another dose at bedtime. Try to take imipramine at around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take imipramine exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Your doctor may start you on a low dose of imipramine and gradually increase your dose.
It may take 1-3 weeks or longer for you to feel the full benefit of imipramine. Continue to take imipramine even if you feel well. Do not stop taking imipramine without talking to your doctor. Your doctor will probably want to decrease your dose gradually.
A small number of children, teenagers, and young adults (up to 24 years of age) who took antidepressants (‘mood elevators’) such as imipramine during clinical studies became suicidal (thinking about harming or killing oneself or planning or trying to do so). Children, teenagers, and young adults who take antidepressants to treat depression or other mental illnesses may be more likely to become suicidal than children, teenagers, and young adults who do not take antidepressants to treat these conditions. However, experts are not sure about how great this risk is and how much it should be considered in deciding whether a child or teenager should take an antidepressant. Children younger than 18 years of age should not normally take imipramine except to prevent bedwetting, but in some cases, a doctor may decide that imipramine is the best medication to treat a child’s condition.
You should know that your mental health may change in unexpected ways when you take imipramine or other antidepressants even if you are an adult over 24 years of age. You may become suicidal, especially at the beginning of your treatment and any time that your dose is increased or decreased. You, your family, or your caregiver should call your doctor right away if you experience any of the following symptoms: new or worsening depression; thinking about harming or killing yourself, or planning or trying to do so; extreme worry; agitation; panic attacks; difficulty falling asleep or staying asleep; aggressive behavior; irritability; acting without thinking; severe restlessness; and frenzied abnormal excitement. Be sure that your family or caregiver knows which symptoms may be serious so they can call the doctor if you are unable to seek treatment on your own.
Your healthcare provider will want to see you often while you are taking imipramine, especially at the beginning of your treatment. Be sure to keep all appointments for office visits with your doctor.
The doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with imipramine. Read the information carefully and ask your doctor or pharmacist if you have any questions. You also can obtain the Medication Guide from the FDA website: https://www.fda.gov/Drugs/default.htm
No matter your age, before you take an antidepressant, you, your parent, or your caregiver should talk to your doctor about the risks and benefits of treating your condition with an antidepressant or with other treatments. You should also talk about the risks and benefits of not treating your condition. You should know that having depression or another mental illness greatly increases the risk that you will become suicidal. This risk is higher if you or anyone in your family has or has ever had bipolar disorder (mood that changes from depressed to abnormally excited) or mania (frenzied, abnormally excited mood) or has thought about or attempted suicide. Talk to your doctor about your condition, symptoms, and personal and family medical history. You and your doctor will decide what type of treatment is right for you.
Imipramine special precautions
Before taking imipramine,
- tell your doctor and pharmacist if you are allergic to imipramine, any other medications, or any of the ingredients in imipramine tablets or capsules. Ask your doctor or pharmacist for a list of the ingredients.
- tell your doctor if you are taking a monoamine oxidase (MAO) inhibitor such as isocarboxazid (Marplan), linezolid (Zyvox), methylene blue, phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate), or if you have stopped taking an MAO inhibitor within the past 14 days. Your doctor will probably tell you not to take imipramine. If you stop taking imipramine, you should wait at least 14 days before you start to take an MAO inhibitor.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: anticoagulants (blood thinners) such as warfarin (Coumadin, Jantoven); antihistamines; cimetidine (Tagamet); flecainide (Tambocor); levodopa (Sinemet, Larodopa); lithium (Eskalith, Lithobid); medication for high blood pressure, mental illness, nausea, seizures, Parkinson’s disease, asthma, colds, or allergies; methylphenidate (Ritalin); muscle relaxants; propafenone (Rhythmol); quinidine; sedatives; selective serotonin reuptake inhibitors (SSRIs) such as citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac, Sarafem), fluvoxamine (Luvox), paroxetine (Paxil), and sertraline (Zoloft); sleeping pills; thyroid medications; and tranquilizers. Your doctor may need to change the doses of your medications or monitor you carefully for side effects. Your doctor may tell you not to take imipramine if you have taken fluoxetine in the past 5 weeks.
- tell your doctor if you have recently had a heart attack. Your doctor may tell you not to take imipramine.
- tell your doctor if you are being treated with electroshock therapy (procedure in which small electric shocks are administered to the brain to treat certain mental illnesses), and if you have or have ever had an enlarged prostate (a male reproductive gland), difficulty urinating, seizures, an overactive thyroid gland, or liver, kidney, or heart disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking imipramine, call your doctor.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking imipramine.
- you should know that this medication may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- remember that alcohol can add to the drowsiness caused by this medication.
- tell your doctor if you use tobacco products. Cigarette smoking may decrease the effectiveness of this medication.
- plan to avoid unnecessary or prolonged exposure to sunlight and to wear protective clothing, sunglasses, and sunscreen. Imipramine may make your skin sensitive to sunlight.
- talk to your doctor about the risks and benefits of taking imipramine if you are 65 years of age or older. Older adults should not usually take imipramine because it is not as safe and effective as other medications that can be used to treat the same condition.
- you should know that imipramine may cause angle-closure glaucoma (a condition where the fluid is suddenly blocked and unable to flow out of the eye causing a quick, severe increase in eye pressure which may lead to a loss of vision). Talk to your doctor about having an eye examination before you start taking this medication. If you have nausea, eye pain, changes in vision, such as seeing colored rings around lights, and swelling or redness in or around the eye, call your doctor or get emergency medical treatment right away.
Breastfeeding
There are no adequate studies in women for determining infant risk when using imipramine during breastfeeding. Weigh the potential benefits against the potential risks before taking imipramine while breastfeeding.
Drug Interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking imipramine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using imipramine with any of the following medicines is not recommended. Your doctor may decide not to treat you with imipramine or change some of the other medicines you take.
- Amifampridine
- Bepridil
- Bromopride
- Cisapride
- Dronedarone
- Furazolidone
- Grepafloxacin
- Iproniazid
- Isocarboxazid
- Levomethadyl
- Linezolid
- Mesoridazine
- Methylene Blue
- Metoclopramide
- Moclobemide
- Pargyline
- Phenelzine
- Pimozide
- Piperaquine
- Procarbazine
- Ranolazine
- Rasagiline
- Safinamide
- Saquinavir
- Selegiline
- Sparfloxacin
- Terfenadine
- Thioridazine
- Tranylcypromine
- Ziprasidone
Using imipramine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Acecainide
- Aceclofenac
- Acemetacin
- Albuterol
- Alfentanil
- Alfuzosin
- Almotriptan
- Amiodarone
- Amisulpride
- Amitriptyline
- Amoxapine
- Amphetamine
- Amtolmetin Guacil
- Anagrelide
- Apomorphine
- Aprindine
- Aripiprazole
- Aripiprazole Lauroxil
- Arsenic Trioxide
- Artemether
- Asenapine
- Aspirin
- Astemizole
- Atazanavir
- Azimilide
- Azithromycin
- Benzhydrocodone
- Benzphetamine
- Bretylium
- Bromfenac
- Bufexamac
- Buprenorphine
- Bupropion
- Buserelin
- Celecoxib
- Chloral Hydrate
- Chloroquine
- Chlorpromazine
- Choline Salicylate
- Ciprofloxacin
- Clarithromycin
- Clomipramine
- Clonidine
- Clonixin
- Clozapine
- Codeine
- Crizotinib
- Cyclobenzaprine
- Dabrafenib
- Darifenacin
- Darunavir
- Dasatinib
- Degarelix
- Delamanid
- Desipramine
- Deslorelin
- Desmopressin
- Desvenlafaxine
- Deutetrabenazine
- Dexibuprofen
- Dexketoprofen
- Dextroamphetamine
- Dextromethorphan
- Diclofenac
- Diflunisal
- Dihydrocodeine
- Dipyrone
- Disopyramide
- Dofetilide
- Dolasetron
- Domperidone
- Donepezil
- Droperidol
- Droxicam
- Efavirenz
- Encorafenib
- Enflurane
- Epinephrine
- Erythromycin
- Escitalopram
- Etilefrine
- Etodolac
- Etofenamate
- Etoricoxib
- Felbinac
- Fenoprofen
- Fentanyl
- Fepradinol
- Feprazone
- Fingolimod
- Flecainide
- Floctafenine
- Fluconazole
- Flufenamic Acid
- Fluoxetine
- Flurbiprofen
- Foscarnet
- Frovatriptan
- Gatifloxacin
- Gemifloxacin
- Glycopyrrolate
- Glycopyrronium Tosylate
- Gonadorelin
- Goserelin
- Granisetron
- Halofantrine
- Haloperidol
- Halothane
- Histrelin
- Hydrocodone
- Hydromorphone
- Hydroxychloroquine
- Hydroxyzine
- Ibuprofen
- Ibutilide
- Iloperidone
- Indomethacin
- Inotuzumab Ozogamicin
- Iobenguane I 123
- Iobenguane I 131
- Isoflurane
- Isradipine
- Ivabradine
- Ivosidenib
- Ketoprofen
- Ketorolac
- Lapatinib
- Leuprolide
- Levalbuterol
- Levofloxacin
- Levomilnacipran
- Levorphanol
- Levothyroxine
- Lidoflazine
- Lisdexamfetamine
- Lithium
- Lofexidine
- Lorcainide
- Lorcaserin
- Lornoxicam
- Loxapine
- Loxoprofen
- Lumefantrine
- Lumiracoxib
- Macimorelin
- Meclofenamate
- Mefenamic Acid
- Mefloquine
- Meloxicam
- Meperidine
- Metaxalone
- Methadone
- Methamphetamine
- Methoxamine
- Metronidazole
- Midodrine
- Mifepristone
- Mirtazapine
- Moricizine
- Morniflumate
- Morphine
- Morphine Sulfate Liposome
- Moxifloxacin
- Nabumetone
- Nafarelin
- Nalbuphine
- Naproxen
- Naratriptan
- Nefopam
- Nepafenac
- Niflumic Acid
- Nilotinib
- Nimesulide
- Nimesulide Beta Cyclodextrin
- Norepinephrine
- Norfloxacin
- Nortriptyline
- Octreotide
- Ofloxacin
- Ondansetron
- Osimertinib
- Oxaprozin
- Oxilofrine
- Oxycodone
- Oxymetazoline
- Oxymorphone
- Oxyphenbutazone
- Paliperidone
- Palonosetron
- Panobinostat
- Parecoxib
- Paroxetine
- Pasireotide
- Pazopanib
- Peginterferon Alfa-2b
- Pentamidine
- Pentazocine
- Phenylbutazone
- Phenylephrine
- Piketoprofen
- Pimavanserin
- Piroxicam
- Pitolisant
- Pixantrone
- Posaconazole
- Pranoprofen
- Procainamide
- Prochlorperazine
- Proglumetacin
- Promethazine
- Propafenone
- Propyphenazone
- Proquazone
- Protriptyline
- Quetiapine
- Quinidine
- Quinine
- Remifentanil
- Ribociclib
- Risperidone
- Rofecoxib
- Salicylic Acid
- Salsalate
- Secretin Human
- Sematilide
- Sertindole
- Sertraline
- Sevoflurane
- Sodium Phosphate
- Sodium Phosphate, Dibasic
- Sodium Phosphate, Monobasic
- Sodium Salicylate
- Solifenacin
- Sorafenib
- Sotalol
- Spiramycin
- Sufentanil
- Sulfamethoxazole
- Sulindac
- Sulpiride
- Sultopride
- Sumatriptan
- Sunitinib
- Tacrolimus
- Tapentadol
- Tedisamil
- Telavancin
- Telithromycin
- Tenoxicam
- Tetrabenazine
- Tiaprofenic Acid
- Tiotropium
- Tolfenamic Acid
- Tolmetin
- Toremifene
- Tramadol
- Trazodone
- Trifluoperazine
- Trimethoprim
- Triptorelin
- Tryptophan
- Valdecoxib
- Vandetanib
- Vardenafil
- Vasopressin
- Vemurafenib
- Venlafaxine
- Vilanterol
- Vilazodone
- Vinflunine
- Voriconazole
- Vortioxetine
- Zolmitriptan
- Zotepine
- Zuclopenthixol
Using imipramine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Acenocoumarol
- Alprazolam
- Arbutamine
- Atomoxetine
- Cannabis
- Carbamazepine
- Cimetidine
- Citalopram
- Dicumarol
- Fluvoxamine
- Fosphenytoin
- Mibefradil
- Phenindione
- Phenprocoumon
- Phenytoin
- Ritonavir
- S-Adenosylmethionine
Other Interactions
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using imipramine with any of the following is usually not recommended, but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use this medicine, or give you special instructions about the use of food, alcohol, or tobacco.
- Tobacco
Using imipramine with any of the following may cause an increased risk of certain side effects but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use this medicine, or give you special instructions about the use of food, alcohol, or tobacco.
- Ethanol
What should I avoid while taking imipramine?
Do not drink alcohol. Dangerous side effects or death can occur when alcohol is combined with imipramine. Check your food and medicine labels to be sure these products do not contain alcohol.
Imipramine can cause side effects that may impair your thinking or reactions. Be careful if you drive or do anything that requires you to be awake and alert.
Avoid exposure to sunlight or tanning beds. Imipramine can make you sunburn more easily. Wear protective clothing and use sunscreen (SPF 30 or higher) when you are outdoors.
Imipramine mechanism of action
Imipramine hydrochloride is a synthetic tricyclic antidepressant. Imipramine treats depression by increasing the amounts or activity of a chemical called serotonin and norepinephrine in certain areas of the brain that are needed to maintain mental balance. There is not enough information to explain how imipramine prevents bedwetting.
In childhood bedwetting, imipramine is thought to work one of several ways:
- by changing the child’s sleep and wakening pattern
- by affecting the time a child can hold urine in the bladder or
- by reducing the amount of urine produced.
Imipramine also induces sedation through histamine-1 receptor blockage; hypotension through beta-adrenergic blockage; and diverse parasympatholytic effects. Imipramine has less sedative effect than other members of its therapeutic family. Imipramine is used in major depression, dysthymia, bipolar depression, attention-deficit disorders, agoraphobia, and panic disorders.
Imipramine uses
Imipramine tablets and capsules are used to treat depression. Imipramine tablets are also used to prevent bedwetting (enuresis) in children ages 6 and older. Imipramine generally is not used to treat bed-wetting in children younger than 6 to 7 years of age. Success rates have been found to be higher in older children. As with all drugs used to treat bed-wetting if imipramine is stopped, bed-wetting is likely to reoccur. The usual dose of imipramine is taken 1 to 2 hours before bedtime for children 6 to 8 years old. A higher dose is needed for older children and adolescents. A child should be seen by a doctor after three to six months on the drug. If the child starts wetting again, then a repeat course of treatment may be restarted.
Imipramine is also used occasionally to treat eating disorders and panic disorders. Talk to your doctor about the possible risks of using this medication for your condition.
Imipramine may be prescribed for other uses. Ask your doctor or pharmacist for more information.
Imipramine dosage
Follow all directions on your prescription label. Your doctor may occasionally change your dose to make sure you get the best results. Do not use imipramine in larger or smaller amounts or for longer than recommended.
If you need surgery, tell the surgeon ahead of time that you are using imipramine. You may need to stop using the medicine for a short time.
It may take up to 3 weeks before your symptoms improve. Keep using the medication as directed and tell your doctor if your symptoms do not improve.
Call your doctor if your symptoms do not improve, or if they get worse.
You should not stop using imipramine suddenly. Follow your doctor’s instructions about tapering your dose.
The following information includes only the average doses of imipramine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of imipramine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take imipramine depend on the medical problem for which you are using imipramine.
Adult Dose for Depression
Use: Relief of symptoms of depression
TABLETS:
Hospitalized Patients:
- Initial dose: 100 mg orally once a day, increasing to 200 mg/day if necessary
- Titration dose: After increasing the dose to 200 mg/day, if there is no response after 2 weeks, increase the dose to 250 to 300 mg/day.
- Maintenance dose: 100 to 200 mg orally once a day
- Maximum dose: 300 mg/day
Outpatients:
- Initial dose: 75 mg orally once a day
- Maintenance dose: 50 to 150 mg orally once a day
- Maximum dose: 200 mg/day
CAPSULES:
Hospitalized Patients:
- Initial dose: 100 to 150 mg orally once a day, increasing to 200 mg/day if necessary
- Titration dose: After increasing the dose to 200 mg/day, if there is no response after 2 weeks, increase the dose to 250 to 300 mg/day.
- Maintenance dose: 75 to 150 mg orally once a day
- Maximum dose: 300 mg/day
Outpatients:
- Initial dose: 75 mg orally once a day
- Maintenance dose: 75 to 150 mg orally once a day
- Maximum dose: 200 mg/day
Comments:
- Approximately 1 to 3 weeks of treatment may be needed before effects are observed.
- Treatment may be more effective in patients with endogenous depression compared to patients with other depressive states.
- The daily dosage may be given at bedtime or in divided doses.
- In cases of relapse due to premature withdrawal of the drug, the effective dosage should be reinstituted.
Geriatric Dose for Depression
Use: Relief of symptoms of depression
TABLETS:
- Initial dose: 30 to 40 mg orally once a day
- Maximum dose: 100 mg/day
CAPSULES:
- Initial dose: 25 to 50 mg orally once a day
- Maximum dose: 100 mg/day
Comments:
- Approximately 1 to 3 weeks of treatment may be needed before effects are observed.
- Treatment may be more effective in patients with endogenous depression compared to patients with other depressive states.
- Capsules may be used when total daily dosage is established at 75 mg or higher.
- The daily dosage may be given at bedtime or in divided doses.
- In cases of relapse due to premature withdrawal of the drug, the effective dosage should be reinstituted.
Pediatric Dose for Bedwetting
Use: Temporary adjunctive therapy in reducing bedwetting (enuresis) in children after possible organic causes have been excluded by appropriate tests
TABLETS:
6 years to 12 years:
- Initial dose: 25 mg orally once a day
- Maintenance dose: 50 mg orally once a day
- Maximum dose: 2.5 mg/kg/day
12 years to 18 years:
- Initial dose: 25 mg orally once a day
- Maintenance dose: 75 mg orally once a day
- Maximum dose: 2.5 mg/kg/day
Comments:
- Examination may include voiding cystourethrography and cystoscopy in patients with daytime symptoms of frequency and urgency.
- Effectiveness may decrease with continued treatment.
- This dose should be given one hour before bedtime.
- In early night bedwetters, the drug is more effective when given earlier and in divided amounts, i.e., 25 mg in midafternoon, repeated at bedtime.
- Dosage should be tapered off gradually.
Renal Dose Adjustments
- Mild to moderate renal dysfunction: Data not available
- Severe renal dysfunction: Use with caution
Liver Dose Adjustments
- Mild to moderate liver dysfunction: Data not available
- Severe liver dysfunction: Use with caution
What should I do if I forget a dose?
Take the missed dose as soon as you remember it. However, if it is almost time for your next dose, skip the missed dose and continue your regular dosing schedule.
Imipramine side effects
Imipramine may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- nausea
- drowsiness
- weakness or tiredness
- excitement or anxiety
- nightmares
- dry mouth
- skin more sensitive to sunlight than usual
- changes in appetite or weight
- constipation
- difficulty urinating
- frequent urination
- changes in sex drive or ability
- excessive sweating
Some side effects can be serious. If you experience any of the following symptoms or those listed in the IMPORTANT WARNING or SPECIAL PRECAUTIONS sections, call your doctor immediately or get emergency medical treatment:
- jaw, neck, and back muscle spasms
- slow or difficult speech
- shuffling walk
- uncontrollable shaking of a part of the body
- fever, sore throat, or other signs of infection
- difficulty breathing or swallowing
- severe rash
- yellowing of the skin or eyes
- irregular heartbeat
Imipramine may cause other side effects. Tell your doctor if you have any unusual problems while you are taking this medication.
Imipramine overdose
In case of overdose, call the poison control helpline at 1-800-222-1222. Information is also available online at https://www.poisonhelp.org/help. If the victim has collapsed, had a seizure, has trouble breathing, or can’t be awakened, immediately call your local emergency services number.
Imipramine overdose symptoms
Below are symptoms of an imipramine overdose in different parts of the body.
AIRWAYS AND LUNGS
- Slow, labored breathing
BLADDER AND KIDNEYS
- Cannot urinate
- Hard to start urinating, or weak urine stream
EYES, EARS, MOUTH, NOSE, AND THROAT
- Blurred vision
- Dry mouth
- Enlarged pupils
- Very dry eyes
- Ringing in the ears
HEART AND BLOOD VESSELS
- Low blood pressure
- Irregular heartbeat
- Pounding heartbeat (palpitations)
- Rapid heartbeat
NERVOUS SYSTEM
- Agitation
- Coma (lack of responsiveness)
- Confusion
- Seizures
- Delirium (confusion and agitation)
- Depression
- Drowsiness
- Hallucinations
- Inability to concentrate
- Nervousness
- Tremor
- Unsteadiness
SKIN
- Dry, red skin
STOMACH AND INTESTINES
- Constipation
- Increased appetite
- Weight gain
- Vomiting
What to expect at the emergency room
Take the container to the hospital with you, if possible.
The health care provider will measure and monitor the person’s vital signs, including temperature, pulse, breathing rate, and blood pressure.
Tests that may done include:
- Blood and urine tests
- Chest x-ray
- CT scan (computerized tomography or advanced imaging)
- ECG (electrocardiogram, or heart tracing)
Treatment may include:
- Fluids through a vein (by IV)
- Medicines to treat symptoms
- Activated charcoal
- Laxative
- Breathing support, including a tube through the mouth into the lungs and connected to a breathing machine (ventilator)
Imipramine overdose prognosis
An imipramine overdose can be very serious. Heart rhythm disturbances can be fatal.
People who overdose on this drug are almost always admitted to the hospital. The faster they get medical help, the better the chance of recovery. Complications such as pneumonia, muscle damage from lying on a hard surface for a prolonged period of time, or brain damage from lack of oxygen may result in permanent disability. Death can occur.