Contents
- What is ischemic stroke
- Hemorrhagic stroke
- Hemorrhagic stroke causes
- Stroke recovery
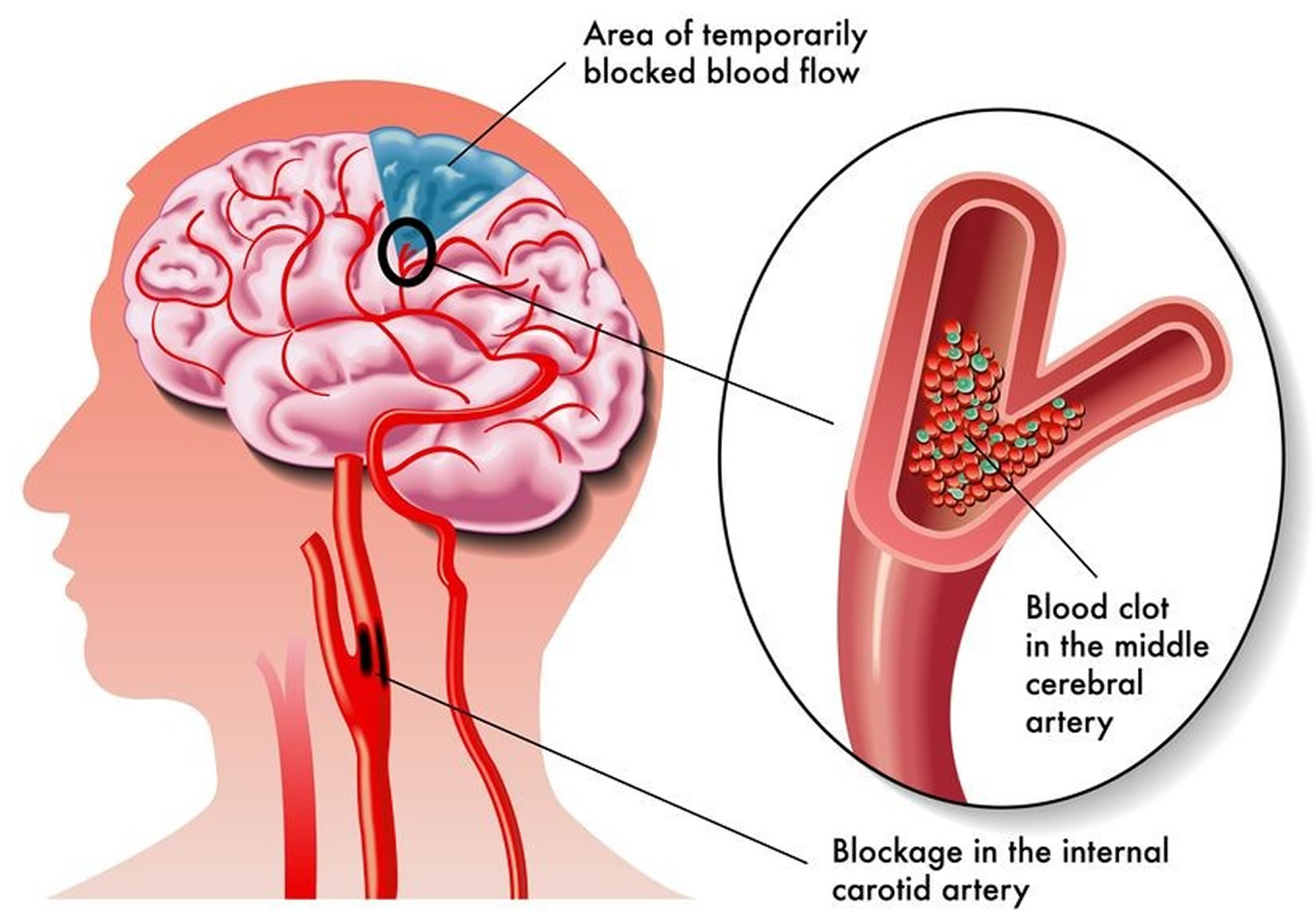
What is ischemic stroke
Ischemic stroke occurs when a clot or a mass clogs a blood vessel, cutting off the blood flow to brain cells, causing severely reduced blood flow (ischemia). The underlying condition for this type of obstruction is the development of fatty deposits lining the vessel walls. This condition is called atherosclerosis. Within minutes, brain cells begin to die. If brain cells die or are damaged because of a stroke, symptoms occur in the parts of the body that these brain cells control. Examples of stroke symptoms include sudden weakness; paralysis or numbness of the face, arms, or legs (paralysis is an inability to move); trouble speaking or understanding speech; and trouble seeing.
About 85 percent of strokes are ischemic strokes. The most common ischemic strokes include:
- Thrombotic stroke. A thrombotic stroke occurs when a blood clot (thrombus) forms in one of the arteries that supply blood to your brain. A clot may be caused by fatty deposits (plaque) that build up in arteries and cause reduced blood flow (atherosclerosis) or other artery conditions.
- Embolic stroke. An embolic stroke occurs when a blood clot or other debris forms away from your brain — commonly in your heart and large arteries of the upper chest and neck — and is swept through your bloodstream to lodge in narrower brain arteries. This type of blood clot is called an embolus. A second important cause of embolism is an irregular heartbeat, known as atrial fibrillation. It creates conditions where clots can form in the heart, dislodge and travel to the brain.
Figure 1. Ischemic stroke
- Strokes are a medical emergency and urgent treatment is essential.
- A stroke can cause lasting brain damage, long-term disability, or even death.
- Stroke is the no. 5 cause of death and a leading cause of disability in the United States.
The sooner a person receives treatment for a stroke, the less damage is likely to happen.
If you suspect that you or someone else is having a stroke, call your local emergency number immediately and ask for an ambulance.
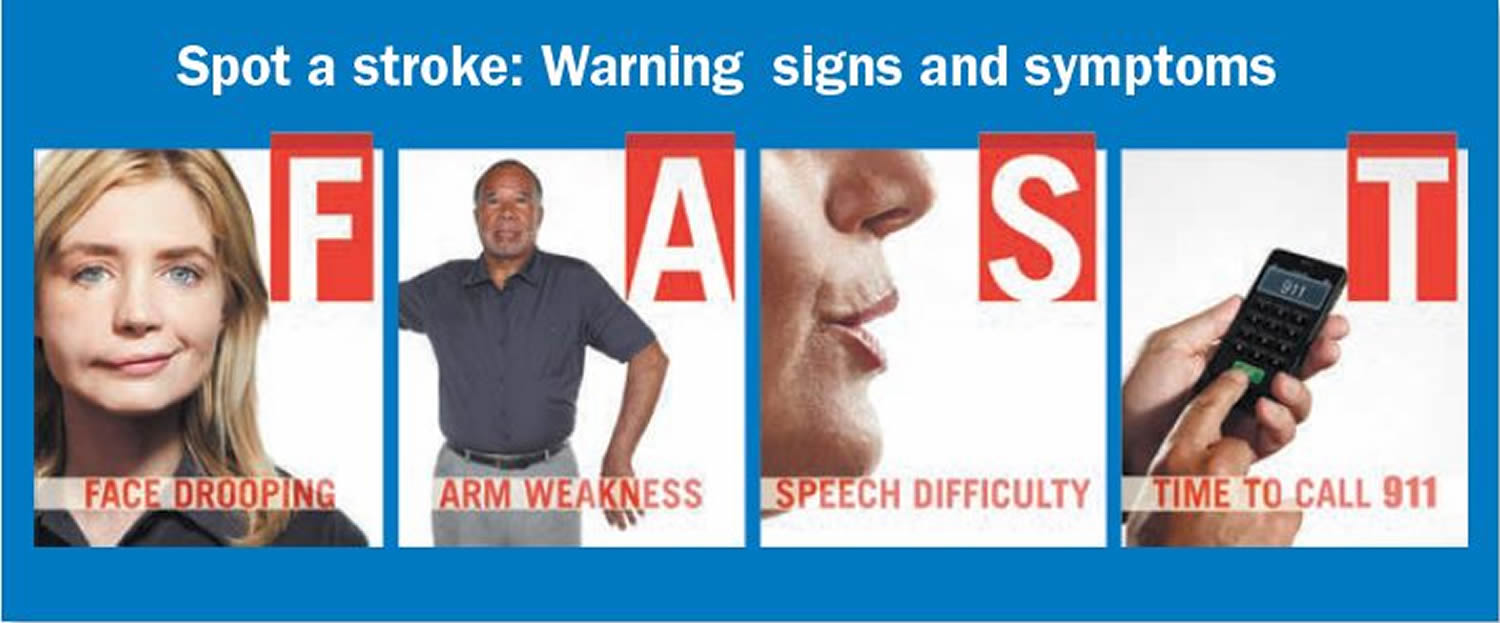
The main symptoms of stroke can be remembered with the word F.A.S.T.:
- Face – the face may have dropped on one side, the person may not be able to smile, or their mouth or eye may have dropped.
- Arms – the person with suspected stroke may not be able to lift both arms and keep them there because of weakness or numbness in one arm.
- Speech – their speech may be slurred or garbled, or the person may not be able to talk at all despite appearing to be awake.
- Time – it’s time to dial your local emergency number immediately if you see any of these signs or symptoms.
If you have any of these symptoms or if you suspect someone else is having a stroke, you must get to a hospital quickly to begin treatment. Acute stroke therapies try to stop a stroke while it is happening by quickly dissolving the blood clot or by stopping the bleeding.
Post-stroke rehabilitation helps individuals overcome disabilities that result from stroke damage. Drug therapy with blood thinners is the most common treatment for stroke.
Ischemic stroke causes
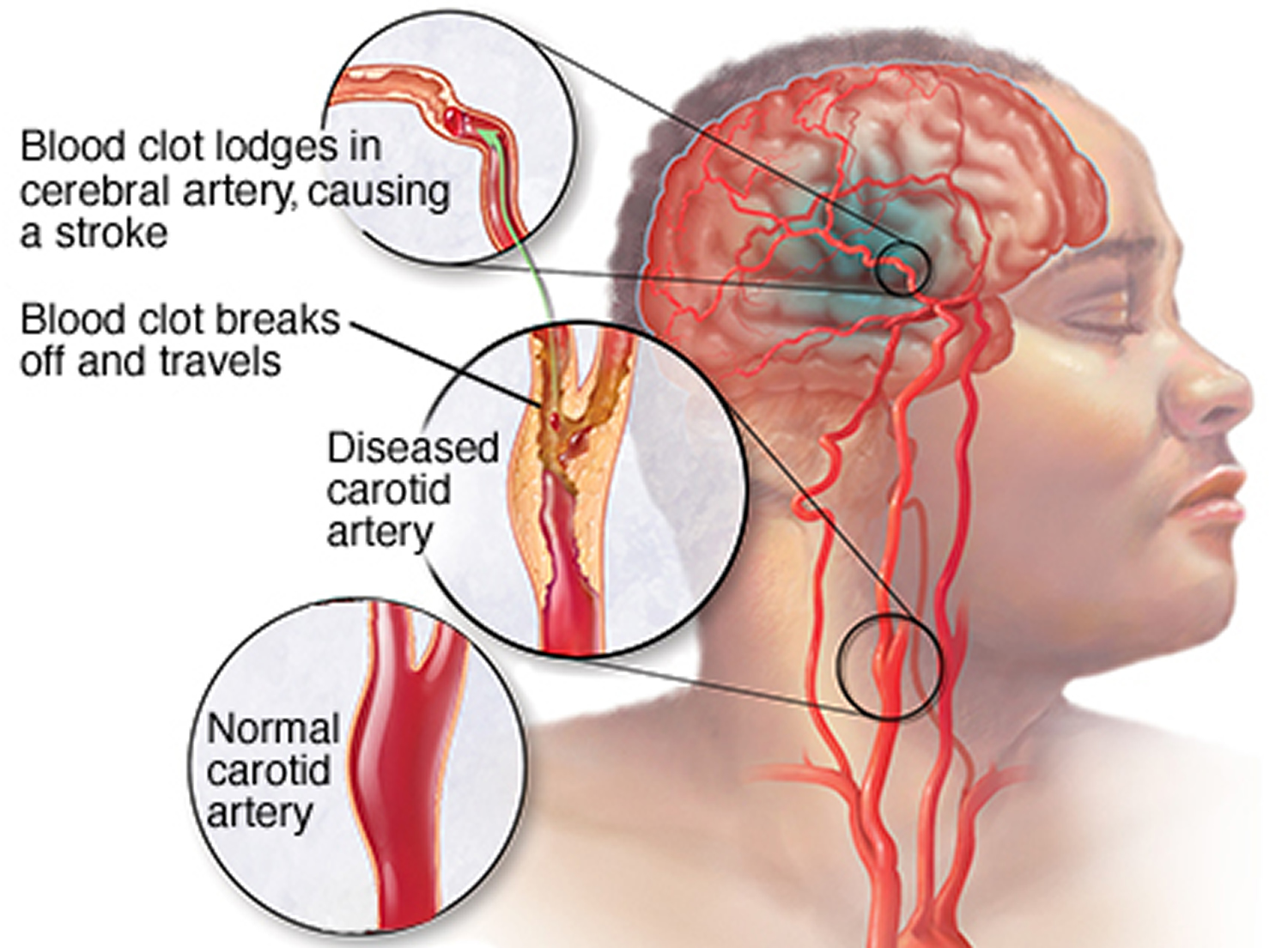
About 85 percent of strokes are ischemic strokes. Ischemic strokes occur when the arteries to your brain become narrowed or blocked, causing severely reduced blood flow (ischemia). The most common ischemic strokes include:
- Thrombotic stroke. A thrombotic stroke occurs when a blood clot (thrombus) forms in one of the arteries that supply blood to your brain. A clot may be caused by fatty deposits (plaque) that build up in arteries and cause reduced blood flow (atherosclerosis) or other artery conditions.
- Embolic stroke. An embolic stroke occurs when a blood clot or other debris forms away from your brain — commonly in your heart and large arteries of the upper chest and neck — and is swept through your bloodstream to lodge in narrower brain arteries. This type of blood clot is called an embolus. A second important cause of embolism is an irregular heartbeat, known as atrial fibrillation. It creates conditions where clots can form in the heart, dislodge and travel to the brain.
Transient ischemic attack (TIA)
A transient ischemic attack (TIA) — also known as a mini stroke — is a brief period of symptoms similar to those you’d have in a stroke. A temporary decrease in blood supply to part of your brain causes TIAs, which often last less than five minutes.
Like an ischemic stroke, a TIA occurs when a clot or debris blocks blood flow to part of your brain. A TIA doesn’t leave lasting symptoms because the blockage is temporary.
Seek emergency care even if your symptoms seem to clear up. Having a TIA puts you at greater risk of having a full-blown stroke, causing permanent damage later. If you’ve had a TIA, it means there’s likely a partially blocked or narrowed artery leading to your brain or a clot source in the heart.
It’s not possible to tell if you’re having a stroke or a TIA based only on your symptoms. Up to half of people whose symptoms appear to go away actually have had a stroke causing brain damage.
Figure 2. Transient ischemic attack (TIA) or mini stroke
 Risk factors for ischemic stroke
Risk factors for ischemic stroke
Many factors can increase your risk of a stroke. Some factors can also increase your chances of having a heart attack. Potentially treatable stroke risk factors include:
Lifestyle risk factors
- Being overweight or obese
- Physical inactivity
- Heavy or binge drinking
- Use of illicit drugs such as cocaine and methamphetamines
Medical risk factors
- High blood pressure (hypertension) — the risk of stroke begins to increase at blood pressure readings higher than 120/80 millimeters of mercury (mm Hg). Your doctor will help you decide on a target blood pressure based on your age, whether you have diabetes and other factors.
- Cigarette smoking or exposure to secondhand smoke. The risk of ischemic stroke in current smokers is about double that of nonsmokers after adjustment for other risk factors.
- High cholesterol.
- Diabetes.
- Obstructive sleep apnea — a sleep disorder in which the oxygen level intermittently drops during the night.
- Cardiovascular disease, including heart failure, heart defects, heart infection or abnormal heart rhythm (atrial fibrillation).
Other factors associated with a higher risk of stroke include:
- Personal or family history of stroke, heart attack or transient ischemic attack.
- Being age 55 or older.
- Race — African-Americans have a higher risk of stroke than do people of other races.
- Gender — Men have a higher risk of stroke than women. Women are usually older when they have strokes, and they’re more likely to die of strokes than are men. Also, they may have some risk from some birth control pills or hormone therapies that include estrogen, as well as from pregnancy and childbirth.
How to prevent ischemic stroke
Knowing your stroke risk factors, following your doctor’s recommendations and adopting a healthy lifestyle are the best steps you can take to prevent a stroke. If you’ve had a stroke or a transient ischemic attack (TIA), these measures may help you avoid having another stroke. The follow-up care you receive in the hospital and afterward may play a role as well.
Many stroke prevention strategies are the same as strategies to prevent heart disease. In general, healthy lifestyle recommendations include:
- Controlling high blood pressure (hypertension). One of the most important things you can do to reduce your stroke risk is to keep your blood pressure under control. If you’ve had a stroke, lowering your blood pressure can help prevent a subsequent transient ischemic attack or stroke.
Exercising, managing stress, maintaining a healthy weight, and limiting the amount of sodium and alcohol you eat and drink are all ways to keep high blood pressure in check.. In addition to recommending lifestyle changes, your doctor may prescribe medications to treat high blood pressure.
- Lowering the amount of cholesterol and saturated fat in your diet. Eating less cholesterol and fat, especially saturated fat and trans fats, may reduce the fatty deposits (plaques) in your arteries. If you can’t control your cholesterol through dietary changes alone, your doctor may prescribe a cholesterol-lowering medication.
- Quitting smoking. Smoking raises the risk of stroke for smokers and nonsmokers exposed to secondhand smoke. Quitting tobacco use reduces your risk of stroke.
- Controlling diabetes. You can manage diabetes with diet, exercise, weight control and medication.
- Maintaining a healthy weight. Being overweight contributes to other stroke risk factors, such as high blood pressure, cardiovascular disease and diabetes. Weight loss of as little as 10 pounds may lower your blood pressure and improve your cholesterol levels.
- Eating a diet rich in fruits and vegetables. A diet containing five or more daily servings of fruits or vegetables may reduce your risk of stroke. Following the Mediterranean diet, which emphasizes olive oil, fruit, nuts, vegetables and whole grains, may be helpful.
- Exercising regularly. Aerobic or “cardio” exercise reduces your risk of stroke in many ways. Exercise can lower your blood pressure, increase your level of high-density lipoprotein cholesterol, and improve the overall health of your blood vessels and heart. It also helps you lose weight, control diabetes and reduce stress. Gradually work up to 30 minutes of activity — such as walking, jogging, swimming or bicycling — on most, if not all, days of the week.
- Drinking alcohol in moderation, if at all. Alcohol can be both a risk factor and a protective measure for stroke. Heavy alcohol consumption increases your risk of high blood pressure, ischemic strokes and hemorrhagic strokes. However, drinking small to moderate amounts of alcohol, such as one drink a day, may help prevent ischemic stroke and decrease your blood’s clotting tendency. Alcohol may also interact with other drugs you’re taking. Talk to your doctor about what’s appropriate for you.
- Treating obstructive sleep apnea, if present. Your doctor may recommend an overnight oxygen assessment to screen for obstructive sleep apnea (OSA). If obstructive sleep apnea is detected, it may be treated by giving you oxygen at night or having you wear a small device in your mouth.
- Avoiding illicit drugs. Certain street drugs, such as cocaine and methamphetamines, are established risk factors for a TIA or a stroke. Cocaine reduces blood flow and can cause narrowing of arteries.
Preventive medications
If you’ve had an ischemic stroke or TIA, your doctor may recommend medications to help reduce your risk of having another stroke. These include:
- Anti-platelet drugs. Platelets are cells in your blood that initiate clots. Anti-platelet drugs make these cells less sticky and less likely to clot. The most commonly used anti-platelet medication is aspirin. Your doctor can help you determine the right dose of aspirin for you. Your doctor may also consider prescribing Aggrenox, a combination of low-dose aspirin and the anti-platelet drug dipyridamole, to reduce the risk of blood clotting. If aspirin doesn’t prevent your TIA or stroke, or if you can’t take aspirin, your doctor may instead prescribe an anti-platelet drug such as clopidogrel (Plavix).
- Anticoagulants. These drugs, which include heparin and warfarin (Coumadin), reduce blood clotting. Heparin is fast-acting and may be used over a short period of time in the hospital. Slower acting warfarin may be used over a longer term. Warfarin is a powerful blood-thinning drug, so you’ll need to take it exactly as directed and watch for side effects. Your doctor may prescribe these drugs if you have certain blood-clotting disorders, certain arterial abnormalities, an abnormal heart rhythm or other heart problems. Other newer blood thinners may be used if your TIA or stroke was caused by an abnormal heart rhythm.
Ischemic stroke symptoms
The signs and symptoms of a stroke vary from person to person, but usually begin suddenly.
As different parts of your brain control different parts of your body, your symptoms will depend on the part of your brain affected and the extent of the damage.
The main stroke symptoms can be remembered with the word F.A.S.T.:
- Face – the face may have dropped on one side, the person may not be able to smile, or their mouth or eye may have drooped.
- Arms – the person with suspected stroke may not be able to lift both arms and keep them there because of weakness or numbness in one arm.
- Speech – their speech may be slurred or garbled, or the person may not be able to talk at all despite appearing to be awake.
- Time – it’s time to dial your local emergency immediately if you notice any of these signs or symptoms.
It’s important for everyone to be aware of these signs and symptoms, particularly if you live with or care for somebody in a high-risk group, such as someone who is elderly or has diabetes or high blood pressure.
Other possible symptoms
Symptoms in the F.A.S.T. test identify most strokes, but occasionally a stroke can cause different symptoms.
Other symptoms and signs may include:
- Sudden numbness, paralysis or weakness of the face, arm or leg (especially on one side of the body)
- Sudden loss or blurring of vision in one or both eyes
- Dizziness
- Sudden trouble walking, dizziness, loss of balance or coordination
- Sudden confusion, trouble speaking or understanding speech
- Difficulty understanding what others are saying
- Problems with balance and co-ordination
- Difficulty swallowing (dysphagia)
- Sudden and very severe headache resulting in a blinding pain unlike anything experienced before
- Loss of consciousness
However, there may be other causes for these symptoms.
Transient ischemic attack (TIA)
The symptoms of a TIA, also known as a mini-stroke, are the same as a stroke, but tend to only last between a few minutes and a few hours before disappearing completely.
Although the symptoms do improve, a TIA should never be ignored as it’s a serious warning sign of a problem with the blood supply to your brain. It means you’re at an increased risk of having a stroke in the near future.
Complications of ischemic stroke
A stroke can sometimes cause temporary or permanent disabilities, depending on how long the brain lacks blood flow and which part was affected. Complications may include:
- Paralysis or loss of muscle movement. You may become paralyzed on one side of your body, or lose control of certain muscles, such as those on one side of your face or one arm. Physical therapy may help you return to activities hampered by paralysis, such as walking, eating and dressing.
- Difficulty talking or swallowing. A stroke may cause you to have less control over the way the muscles in your mouth and throat move, making it difficult for you to talk clearly (dysarthria), swallow or eat (dysphagia). You also may have difficulty with language (aphasia), including speaking or understanding speech, reading or writing. Therapy with a speech and language pathologist may help.
- Memory loss or thinking difficulties. Many people who have had strokes experience some memory loss. Others may have difficulty thinking, making judgments, reasoning and understanding concepts.
- Emotional problems. People who have had strokes may have more difficulty controlling their emotions, or they may develop depression.
- Pain. People who have had strokes may have pain, numbness or other strange sensations in parts of their bodies affected by stroke. For example, if a stroke causes you to lose feeling in your left arm, you may develop an uncomfortable tingling sensation in that arm. People also may be sensitive to temperature changes, especially extreme cold after a stroke. This complication is known as central stroke pain or central pain syndrome. This condition generally develops several weeks after a stroke, and it may improve over time. But because the pain is caused by a problem in your brain, rather than a physical injury, there are few treatments.
- Changes in behavior and self-care ability. People who have had strokes may become more withdrawn and less social or more impulsive. They may need help with grooming and daily chores.
As with any brain injury, the success of treating these complications will vary from person to person.
Ischemic stroke treatment
Emergency treatment for stroke depends on whether you’re having an ischemic stroke blocking an artery — the most common kind — or a hemorrhagic stroke that involves bleeding into the brain.
Ischemic stroke
To treat an ischemic stroke, doctors must quickly restore blood flow to your brain.
Emergency treatment with medications
Therapy with clot-busting drugs must start within 3 hours if they are given into the vein — and the sooner, the better. Quick treatment not only improves your chances of survival but also may reduce complications. You may be given:
- Aspirin. Aspirin is an immediate treatment given in the emergency room to reduce the likelihood of having another stroke. Aspirin prevents blood clots from forming.
- Intravenous injection of tissue plasminogen activator (TPA). Some people can benefit from an injection of a recombinant tissue plasminogen activator (TPA), also called alteplase. An injection of TPA is usually given through a vein in the arm. This potent clot-busting drug needs to be given within 4.5 hours after stroke symptoms begin if it’s given in the vein. TPA restores blood flow by dissolving the blood clot causing your stroke, and it may help people who have had strokes recover more fully. Your doctor will consider certain risks, such as potential bleeding in the brain, to determine if TPA is appropriate for you.
Emergency procedures
Doctors sometimes treat ischemic strokes with procedures that must be performed as soon as possible, depending on features of the blood clot:
- Medications delivered directly to the brain. Doctors may insert a long, thin tube (catheter) through an artery in your groin and thread it to your brain to deliver TPA directly into the area where the stroke is occurring. The time window for this treatment is somewhat longer than for intravenous TPA but is still limited.
- Mechanical clot removal. Doctors may use a catheter to maneuver a tiny device into your brain to physically break up or grab and remove the clot.
However, recent studies suggest that for most people, delivering medication directly to the brain (intra-arterial thrombolysis) or using a device to break up or remove clots (mechanical thrombectomy) may not be beneficial. Researchers are working to determine who might benefit from this procedure.
Other procedures to decrease your risk of having another stroke
To decrease your risk of having another stroke or transient ischemic attack, your doctor may recommend a procedure to open up an artery that’s narrowed by fatty deposits (plaques). Doctors sometimes recommend the following procedures to prevent a stroke.
Options will vary depending on your situation:
- Carotid endarterectomy. In a carotid endarterectomy, a surgeon removes plaques from arteries that run along each side of your neck to your brain (carotid arteries). In this procedure, your surgeon makes an incision along the front of your neck, opens your carotid artery and removes plaques that block the carotid artery. Your surgeon then repairs the artery with stitches or a patch made from a vein or artificial material (graft). The procedure may reduce your risk of ischemic stroke. However, a carotid endarterectomy also involves risks, especially for people with heart disease or other medical conditions.
- Angioplasty and stents. In an angioplasty, a surgeon gains access to your carotid arteries most often through an artery in your groin. Here, he or she can gently and safely navigate to the carotid arteries in your neck. A balloon is then used to expand the narrowed artery. Then a stent can be inserted to support the opened artery.
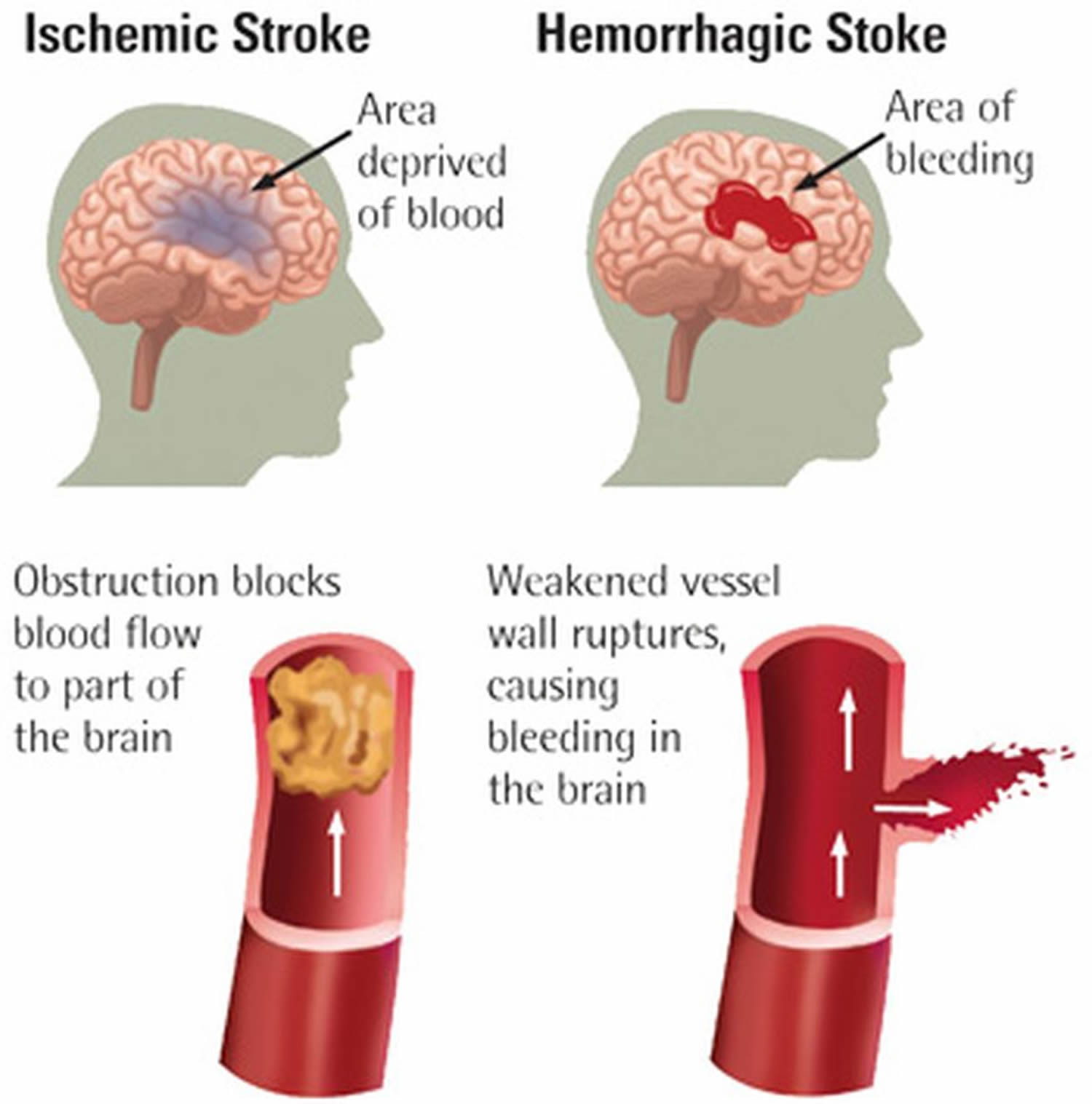
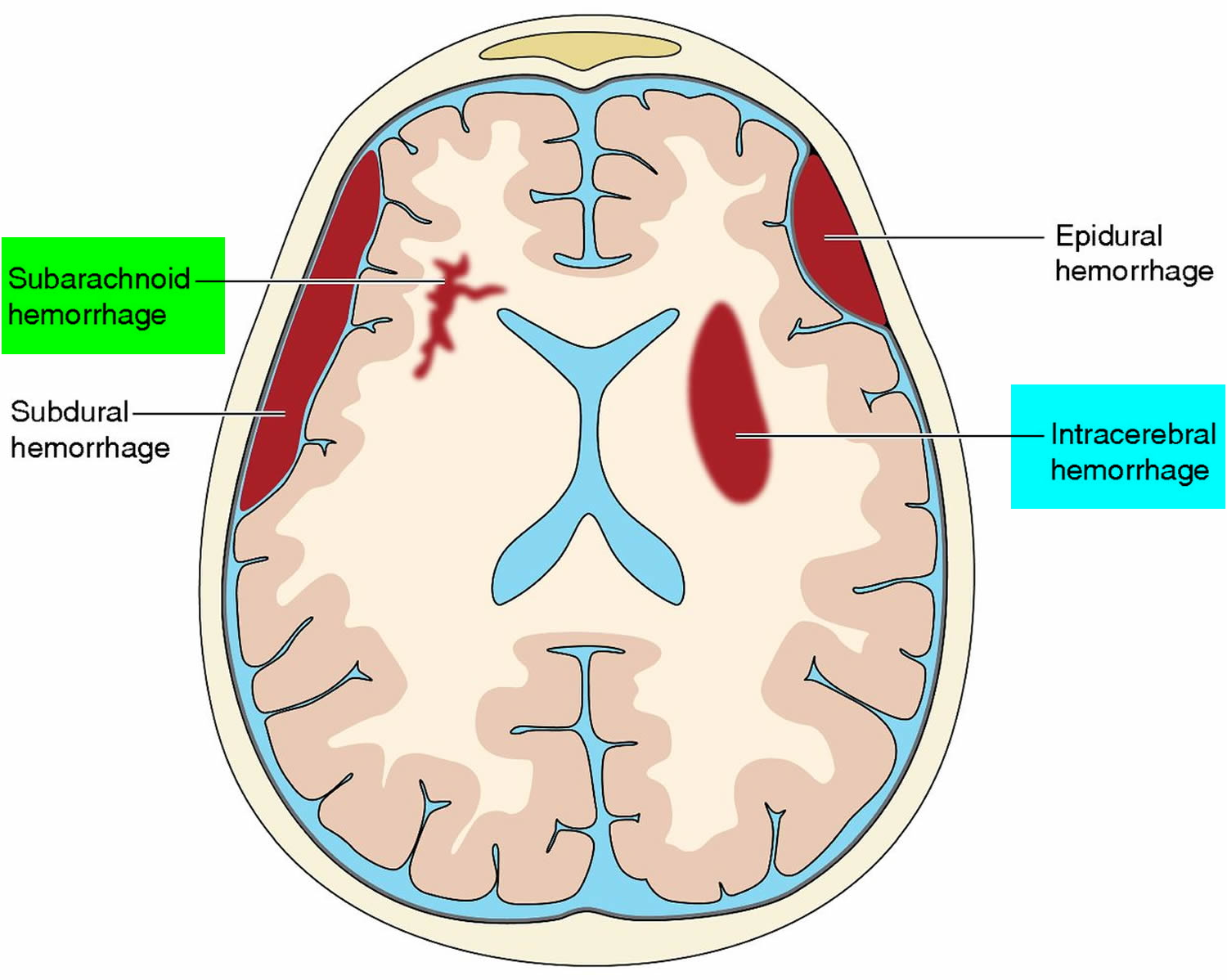
Ischemic stroke vs Hemorrhagic stroke
Ischemic stroke is the more common kind of stroke caused by a blood clot that blocks or plugs a blood vessel in the brain.
Hemorrhagic stroke occurs if an artery in the brain leaks blood or ruptures (breaks open) and bleeds into the surrounding brain. The blood accumulates and compresses the surrounding brain tissue. The pressure from the leaked blood damages brain cells.
The two types of hemorrhagic stroke are intracerebral and subarachnoid. In an intracerebral hemorrhage, a blood vessel inside the brain leaks blood or ruptures deep within the brain.
In a subarachnoid hemorrhage, a blood vessel on the surface of the brain leaks blood or ruptures. When this happens, bleeding occurs between the inner and middle layers of the membranes that cover the brain.
In both types of hemorrhagic stroke, the leaked blood causes swelling of the brain and increased pressure in the skull. The swelling and pressure damage cells and tissues in the brain.
Figure 3. Ischemic stroke vs Hemorrhagic stroke
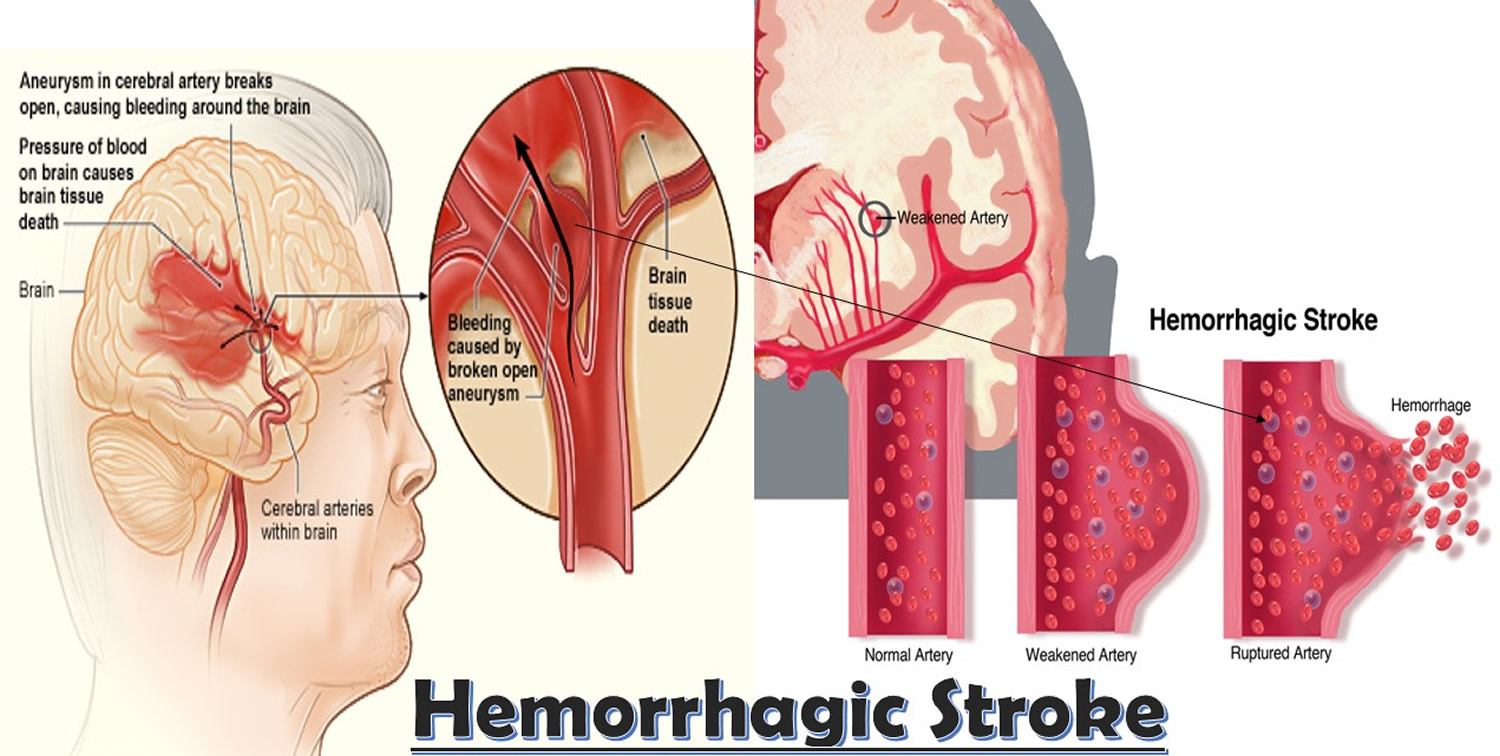
Hemorrhagic stroke
Hemorrhagic stroke occurs when a blood vessel in your brain leaks or ruptures. Brain hemorrhages can result from many conditions that affect your blood vessels, including uncontrolled high blood pressure (hypertension), overtreatment with anticoagulants and weak spots in your blood vessel walls (aneurysms).
A less common cause of hemorrhage is the rupture of an abnormal tangle of thin-walled blood vessels (arteriovenous malformation) present at birth. Types of hemorrhagic stroke include:
- Intracerebral hemorrhage. In an intracerebral hemorrhage, a blood vessel in the brain bursts and spills into the surrounding brain tissue, damaging brain cells. Brain cells beyond the leak are deprived of blood and also damaged.
High blood pressure, trauma, vascular malformations, use of blood-thinning medications and other conditions may cause an intracerebral hemorrhage.
- Subarachnoid hemorrhage. In a subarachnoid hemorrhage, an artery on or near the surface of your brain bursts and spills into the space between the surface of your brain and your skull. This bleeding is often signaled by a sudden, severe headache.
A subarachnoid hemorrhage is commonly caused by the bursting of a small sack-shaped or berry-shaped outpouching on an artery known as an aneurysm. After the hemorrhage, the blood vessels in your brain may widen and narrow erratically (vasospasm), causing brain cell damage by further limiting blood flow.
Figure 4. Hemorrhagic stroke
Hemorrhagic stroke causes
Subarachnoid hemorrhage (SAH)
Subarachnoid hemorrhage is bleeding in the area between the brain and the thin tissues that cover the brain. This area is called the subarachnoid space.
Causes of subarachnoid hemorrhage
Subarachnoid hemorrhage can be caused by:
- Bleeding from a tangle of blood vessels called an arteriovenous malformation (AVM)
- Bleeding disorder
- Bleeding from a cerebral aneurysm
- Head injury
- Unknown cause (idiopathic)
- Use of blood thinners
Subarachnoid hemorrhage caused by injury is often seen in the older people who have fallen and hit their head. Among the young, the most common injury leading to subarachnoid hemorrhage is motor vehicle crashes.
Risks factor for subarachnoid hemorrhage include:
- Aneurysm in other blood vessels
- Fibromuscular dysplasia (FMD) and other connective tissue disorders
- High blood pressure
- History of polycystic kidney disease
- Smoking
A strong family history of aneurysms may also increase your risk.
Who gets it?
The cause of cerebral aneurysms is not known. They may develop from birth or in childhood and grow very slowly. Some people have multiple aneuryms. Subarachnoid hemorrhage can occur at any age, including in teenagers and young adults and is slightly more common in women than men.
Hemorrhagic stroke – subarachnoid hemorrhage symptoms
The main symptom is a severe headache that starts suddenly (often called thunderclap headache). It is often worse near the back of the head. Many people often describe it as the “worst headache ever” and unlike any other type of headache pain. The headache may start after a popping or snapping feeling in the head.
Other symptoms:
- Decreased consciousness and alertness
- Eye discomfort in bright light (photophobia)
- Mood and personality changes, including confusion and irritability
- Muscle aches (especially neck pain and shoulder pain)
- Nausea and vomiting
- Numbness in part of the body
- Seizure
- Stiff neck
- Vision problems, including double vision, blind spots, or temporary vision loss in one eye
Other symptoms that may occur with subarachnoid hemorrhage:
- Eyelid drooping
- Pupil size difference
- Sudden stiffening of back and neck, with arching of the back (opisthotonos; not very common)
Subarachnoid hemorrhage diagnosis
Signs include:
- A physical exam may show a stiff neck
- A brain and nervous system exam may show signs of decreased nerve and brain function (focal neurologic deficit)
- An eye exam may show decreased eye movements. A sign of damage to the cranial nerves (in milder cases, no problems may be seen on an eye exam)
If your doctor thinks you have a subarachnoid hemorrhage, a head CT scan (without contrast dye) will be done right away. In some cases, the scan is normal, especially if there has only been a small bleed. If the CT scan is normal, a lumbar puncture (spinal tap) may be done.
Other tests that may be done include:
- Cerebral angiography of blood vessels of the brain
- CT scan angiography (using contrast dye)
- Transcranial Doppler ultrasound, to look at blood flow in the arteries of the brain
- Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) (occasionally)
Hemorrhagic stroke treatment
The goals of treatment are to:
- Save your life
- Repair the cause of bleeding
- Relieve symptoms
- Prevent complications such as permanent brain damage (stroke)
Surgery
- Remove large collections of blood or relieve pressure on the brain if the hemorrhage is due to an injury
- Repair the aneurysm if the hemorrhage is due to an aneurysm rupture
If the person is critically ill, surgery may have to wait until the person is more stable.
Surgery may involve:
- Craniotomy (cutting a hole in the skull) and aneurysm clipping, to close the aneurysm
- Endovascular coiling: placing coils in the aneurysm and stents in the blood vessel to cage the coils reduces the risk of further bleeding
If no aneurysm is found, the person should be closely watched by a health care team and may need more imaging tests.
Treatment for coma or decreased alertness includes:
- Draining tube placed in the brain to relieve pressure
- Life support
- Methods to protect the airway
- Special positioning
A person who is conscious may need to be on strict bed rest. The person will be told to avoid activities that can increase pressure inside the head, including:
- Bending over
- Straining
- Suddenly changing position
Treatment may also include:
- Medicines given through an IV line to control blood pressure
- Medicine to prevent artery spasms
- Painkillers and anti-anxiety medicines to relieve headache and reduce pressure in the skull
- Medicines to prevent or treat seizures
- Stool softeners or laxatives to prevent straining during bowel movements
Outlook (Prognosis) of subarachnoid hemorrhage
How well a person with subarachnoid hemorrhage does depends on a number of different factors, including:
- Location and amount of bleeding
- Complications
Older age and more severe symptoms can lead to a poorer outcome.
People can recover completely after treatment. But some people die, even with treatment.
Complications of subarachnoid hemorrhage
Repeated bleeding is the most serious complication. If a cerebral aneurysm bleeds for a second time, the outlook is much worse.
Changes in consciousness and alertness due to a subarachnoid hemorrhage may become worse and lead to coma or death.
Other complications include:
- Complications of surgery
- Medicine side effects
- Seizures
- Stroke.
Intracerebral Hemorrhage
Intracerebral hemorrhage occurs when a diseased blood vessel within the brain bursts, allowing blood to leak inside the brain. (The name means within the cerebrum or brain). The sudden increase in pressure within the brain can cause damage to the brain cells surrounding the blood. If the amount of blood increases rapidly, the sudden buildup in pressure can lead to unconsciousness or death. Intracerebral hemorrhage usually occurs in selected parts of the brain, including the basal ganglia, cerebellum, brain stem, or cortex.
Intracerebral hemorrhage causes
The most common cause of intracerebral hemorrhage is high blood pressure (hypertension). Since high blood pressure by itself often causes no symptoms, many people with intracranial hemorrhage are not aware that they have high blood pressure, or that it needs to be treated. Less common causes of intracerebral hemorrhage include trauma, infections, tumors, blood clotting deficiencies, and abnormalities in blood vessels (such as arteriovenous malformations).
Who gets it?
Intracerebral hemorrhage occurs at all ages. The average age is lower than for ischemic stroke. Less common than ischemic strokes, hemorrhagic strokes make up about 12 percent of all strokes.
Intracerebral hemorrhage treatment
Emergency treatment of hemorrhagic stroke focuses on controlling your bleeding and reducing pressure in your brain. Surgery also may be performed to help reduce future risk.
Emergency measures
If you take warfarin (Coumadin) or anti-platelet drugs such as clopidogrel (Plavix) to prevent blood clots, you may be given drugs or transfusions of blood products to counteract the blood thinners’ effects. You may also be given drugs to lower pressure in your brain (intracranial pressure), lower your blood pressure, prevent vasospasm or prevent seizures.
Once the bleeding in your brain stops, treatment usually involves supportive medical care while your body absorbs the blood. Healing is similar to what happens while a bad bruise goes away. If the area of bleeding is large, your doctor may perform surgery to remove the blood and relieve pressure on your brain.
Surgical blood vessel repair
Surgery may be used to repair blood vessel abnormalities associated with hemorrhagic strokes. Your doctor may recommend one of these procedures after a stroke or if an aneurysm or arteriovenous malformation (AVM) or other type of vascular malformation caused your hemorrhagic stroke:
- Surgical clipping. A surgeon places a tiny clamp at the base of the aneurysm, to stop blood flow to it. This clamp can keep the aneurysm from bursting, or it can prevent re-bleeding of an aneurysm that has recently hemorrhaged.
- Coiling (endovascular embolization). In this procedure, a surgeon inserts a catheter into an artery in your groin and guides it to your brain using X-ray imaging. Your surgeon then guides tiny detachable coils into the aneurysm (aneurysm coiling). The coils fill the aneurysm, which blocks blood flow into the aneurysm and causes the blood to clot.
- Surgical arteriovenous malformation (AVM) removal. Surgeons may remove a smaller AVM if it’s located in an accessible area of your brain, to eliminate the risk of rupture and lower the risk of hemorrhagic stroke. However, it’s not always possible to remove an AVM if its removal would cause too large a reduction in brain function, or if it’s large or located deep within your brain.
- Intracranial bypass. In some unique circumstances, surgical bypass of intracranial blood vessels may be an option to treat poor blood flow to a region of the brain or complex vascular lesions, such as aneurysm repair.
- Stereotactic radiosurgery. Using multiple beams of highly focused radiation, stereotactic radiosurgery is an advanced minimally invasive treatment used to repair vascular malformations.
Stroke recovery
Following emergency treatment, stroke care focuses on helping you regain your strength, recover as much function as possible and return to independent living. The impact of your stroke depends on the area of the brain involved and the amount of tissue damaged.
If your stroke affected the right side of your brain, your movement and sensation on the left side of your body may be affected. If your stroke damaged the brain tissue on the left side of your brain, your movement and sensation on the right side of your body may be affected. Brain damage to the left side of your brain may cause speech and language disorders.
In addition, if you’ve had a stroke, you may have problems with breathing, swallowing, balancing and vision.
People who survive a stroke are often left with long-term problems caused by injury to their brain.
Some people need a long period of rehabilitation before they can recover their former independence, while many never fully recover and need support adjusting to living with the effects of their stroke.
Most stroke survivors receive treatment in a rehabilitation program. Your doctor will recommend the most rigorous therapy program you can handle based on your age, overall health and your degree of disability from your stroke. Your doctor will take into consideration your lifestyle, interests and priorities, and the availability of family members or other caregivers.
Your rehabilitation program may begin before you leave the hospital. It may continue in a rehabilitation unit of the same hospital, another rehabilitation unit or skilled nursing facility, an outpatient unit, or your home.
Every person’s stroke recovery is different. Depending on your condition, your treatment team may include:
- Doctor trained in brain conditions (neurologist)
- Rehabilitation doctor (physiatrist)
- Nurse
- Dietitian
- Physical therapist
- Occupational therapist
- Recreational therapist
- Speech therapist
- Social worker
- Case manager
- Psychologist or psychiatrist
- Chaplain
Psychological impact
Two of the most common psychological problems that can affect people after a stroke are:
- Depression – many people experience intense bouts of crying, and feel hopeless and withdrawn from social activities
- Anxiety – where people experience general feelings of fear and anxiety, sometimes punctuated by intense, uncontrolled feelings of anxiety (anxiety attacks)
Feelings of anger, frustration and bewilderment are also common.
You’ll receive a psychological assessment from a member of your healthcare team soon after your stroke to check if you’re experiencing any emotional problems.
Advice should be given to help deal with the psychological impact of stroke. This includes the impact on relationships with other family members and any sexual relationship.
There should also be a regular review of any problems of depression and anxiety, and psychological and emotional symptoms generally.
These problems may settle down over time, but if they are severe or last a long time, doctors can refer people for expert healthcare from a psychiatrist or clinical psychologist.
For some people, medicines and psychological therapies, such as counselling or cognitive behavioral therapy (CBT), can help. Cognitive behavioral therapy (CBT) is a therapy that aims to change the way you think about things to produce a more positive state of mind.
Cognitive impact
Cognitive is a term used by scientists to refer to the many processes and functions our brain uses to process information.
One or more cognitive functions can be disrupted by a stroke, including:
- Communication – both verbal and written
- Spatial awareness – having a natural awareness of where your body is in relation to your immediate environment
- Memory
- Concentration
- Executive function – the ability to plan, solve problems and reason about situations
- Praxis – the ability to carry out skilled physical activities, such as getting dressed or making a cup of tea
As part of your treatment, each one of your cognitive functions will be assessed and a treatment and rehabilitation plan will be created.
You can be taught a wide range of techniques that can help you relearn disrupted cognitive functions, such as recovering your communication skills through speech and language therapy.
There are many ways to compensate for any loss of cognitive function, such as using memory aids, diaries and routines to help plan daily tasks.
Most cognitive functions will return after time and rehabilitation, but you may find they don’t return to the way they were before.
The damage a stroke causes to your brain also increases the risk of developing vascular dementia. This may happen immediately after a stroke or may develop some time after the stroke occurred.
Movement problems
Strokes can cause weakness or paralysis on one side of the body, and can result in problems with co-ordination and balance.
Many people also experience extreme tiredness (fatigue) in the first few weeks after a stroke, and may also have difficulty sleeping, making them even more tired.
As part of your rehabilitation, you should be seen by a physiotherapist, who will assess the extent of any physical disability before drawing up a treatment plan.
Physiotherapy will often involve several sessions a week, focusing on areas such as exercises to improve your muscle strength and overcome any walking difficulties.
The physiotherapist will work with you by setting goals. At first, these may be simple goals, such as picking up an object. As your condition improves, more demanding long-term goals, such as standing or walking, will be set.
A careworker or carer, such as a member of your family, will be encouraged to become involved in your physiotherapy. The physiotherapist can teach you both simple exercises you can carry out at home.
If you have problems with movement and certain activities, such as getting washed and dressed, you may also receive help from an occupational therapist. They can find ways to manage any difficulties.
Occupational therapy may involve adapting your home or using equipment to make everyday activities easier, and finding alternative ways of carrying out tasks you have problems with.
Communication problems
After having a stroke, many people experience problems with speaking and understanding, as well as reading and writing.
If the parts of the brain responsible for language are damaged, this is called aphasia, or dysphasia. If there is weakness in the muscles involved in speech as a result of brain damage, this is known as dysarthria.
You should see a speech and language therapist as soon as possible for an assessment and to start therapy to help you with your communication.
This may involve:
- exercises to improve your control over your speech muscles
- using communication aids – such as letter charts and electronic aids
- using alternative methods of communication – such as gestures or writing
Swallowing problems
The damage caused by a stroke can interrupt your normal swallowing reflex, making it possible for small particles of food to enter your windpipe.
Problems with swallowing are known as dysphagia. Dysphagia can lead to damage to your lungs, which can trigger a lung infection (pneumonia).
You may need to be fed using a feeding tube during the initial phases of your recovery to prevent any complications from dysphagia.
The tube is usually put into your nose and passed into your stomach (nasogastric tube), or it may be directly connected to your stomach in a minor surgical procedure carried out using local anesthetic (percutaneous endoscopic gastrostomy, or PEG).
In the long term, you’ll usually see a speech and language therapist several times a week for treatment to manage your swallowing problems.
Treatment may involve tips to make swallowing easier, such as taking smaller bites of food and advice on posture, and exercises to improve control of the muscles involved in swallowing.
Visual problems
Stroke can sometimes damage the parts of the brain that receive, process and interpret information sent by the eyes.
This can result in losing half the field of vision – for example, only being able to see the left- or right hand side of what’s in front of you.
Strokes can also affect the control of the movement of the eye muscles. This can cause double vision.
If you have any problems with your vision after a stroke, you’ll be referred to an eye specialist called an orthoptist, who can assess your vision and suggest possible treatments.
For example, if you’ve lost part of your field of vision, you may be offered eye movement therapy. This involves exercises to help you look to the side with the reduced vision.
You may also be given advice about particular ways to perform tasks that can be difficult if your vision is reduced on one side, such as getting dressed.
Bladder and bowel control
Some strokes damage the part of the brain that controls bladder and bowel movements. This can result in urinary incontinence and difficulty with bowel control.
Some people may regain bladder and bowel control quite quickly, but if you still have problems after leaving hospital, help is available from the hospital, your GP, and specialist continence advisers.
Don’t be embarrassed – seek advice if you have a problem, as there are lots of treatments that can help.
These include:
- bladder retraining exercises
- medications
- pelvic floor exercises
- using incontinence products
Sex after a stroke
Having sex won’t put you at higher risk of having a stroke. There’s no guarantee you won’t have another stroke, but there’s no reason why it should happen while you’re having sex.
Even if you’ve been left with a severe disability, you can experiment with different positions and find new ways of being intimate with your partner.
Be aware that some medications can reduce your sex drive (libido), so make sure your doctor knows if you have a problem – there may be other medicines that can help.
Some men may experience erectile dysfunction after having a stroke. Speak to your GP or rehabilitation team if this is the case, as there are a number of treatments available that can help.
Driving after a stroke
If you’ve had a stroke or TIA, you can’t drive for one month. Whether you can return to driving depends on what long-term disabilities you may have and the type of vehicle you drive.
It’s often not physical problems that can make driving dangerous, but problems with concentration, vision, reaction time and awareness that can develop after a stroke.
Your doctor can advise you on whether you can start driving again a month after your stroke, or whether you need further assessment at a mobility center.
Preventing further strokes
If you’ve had a stroke, your chances of having another one are significantly increased.
You’ll usually require long-term treatment with medications aimed at improving the underlying risk factors for your stroke.
For example:
- medication – to help lower your blood pressure
- anticoagulants or antiplatelets – to reduce your risk of blood clots
- statins – to lower your cholesterol levels
You’ll also be encouraged to make lifestyle changes to improve your general health and lower your stroke risk, such as:
- eating a healthy diet
- exercising regularly
- stopping smoking if you smoke
- cutting down on the amount of alcohol you drink
Caring for someone who’s had a stroke
There are many ways you can provide support to a friend or relative who’s had a stroke to speed up their rehabilitation process.
These include:
- helping them practise physiotherapy exercises in between their sessions with the physiotherapist
- providing emotional support and reassurance their condition will improve with time
- helping motivate them to reach their long-term goals
- adapting to any needs they may have, such as speaking slowly if they have communication problems
Caring for somebody after a stroke can be a frustrating and lonely experience. The advice outlined below may help.
Be prepared for changed behavior
Someone who’s had a stroke can often seem as though they’ve had a change in personality and appear to act irrationally at times. This is the result of the psychological and cognitive impact of a stroke.
They may become angry or resentful towards you. Upsetting as it may be, try not to take it personally.
It’s important to remember they’ll often start to return to their old self as their rehabilitation and recovery progresses.
Try to remain patient and positive
Rehabilitation can be a slow and frustrating process, and there will be periods of time when it appears little progress has been made.
Encouraging and praising any progress, no matter how small it may appear, can help motivate someone who’s had a stroke to achieve their long-term goals.
Make time for yourself
If you’re caring for someone who’s had a stroke, it’s important not to neglect your own physical and psychological wellbeing. Socializing with friends or pursuing leisure interests will help you cope better with the situation.
Ask for help
There are a wide range of support services and resources available for people recovering from strokes, and their families and carers. This ranges from equipment that can help with mobility, to psychological support for carers and families.
The hospital staff involved with the rehabilitation process can provide advice and relevant contact information.