Contents
What is kidney infection
Kidney infection also known as pyelonephritis, is a type of urinary tract infection (UTI) that affects one or both kidneys 1.
Kidney infections cause most of the 100,000 hospital visits for urinary tract infections (UTIs) in the United States each year 2.
Most kidney infections are caused by bacteria or viruses that first infect your lower urinary tract, usually your bladder or urethra 3. Then, the infection moves upstream to one or both of your kidneys, which are part of the upper urinary tract.
In some cases, you can get a kidney infection after surgery if bacteria enter your body during the procedure and travel through your blood to the kidneys.
Your body has ways to defend against infections in the urinary tract. For example, urine normally flows one way from your kidneys to your bladder. Viruses or bacteria that enter are flushed out by urinating. This one-way flow of urine usually prevents an infection in your urinary tract. Learn more about your urinary tract and how it works.
Sometimes your body’s defenses fail and bacteria or viruses cause a urinary tract infection in the bladder. If you have symptoms of a bladder infection, see a health care professional. You may need treatment to prevent the infection from spreading to your kidneys. Kidney infections are often very painful and can cause serious health problems.
A kidney infection requires prompt medical attention. If not treated properly, a kidney infection can permanently damage your kidneys or the bacteria can spread to your bloodstream and cause a life-threatening infection.
Kidney infection treatment, which usually includes antibiotics, might require hospitalization.
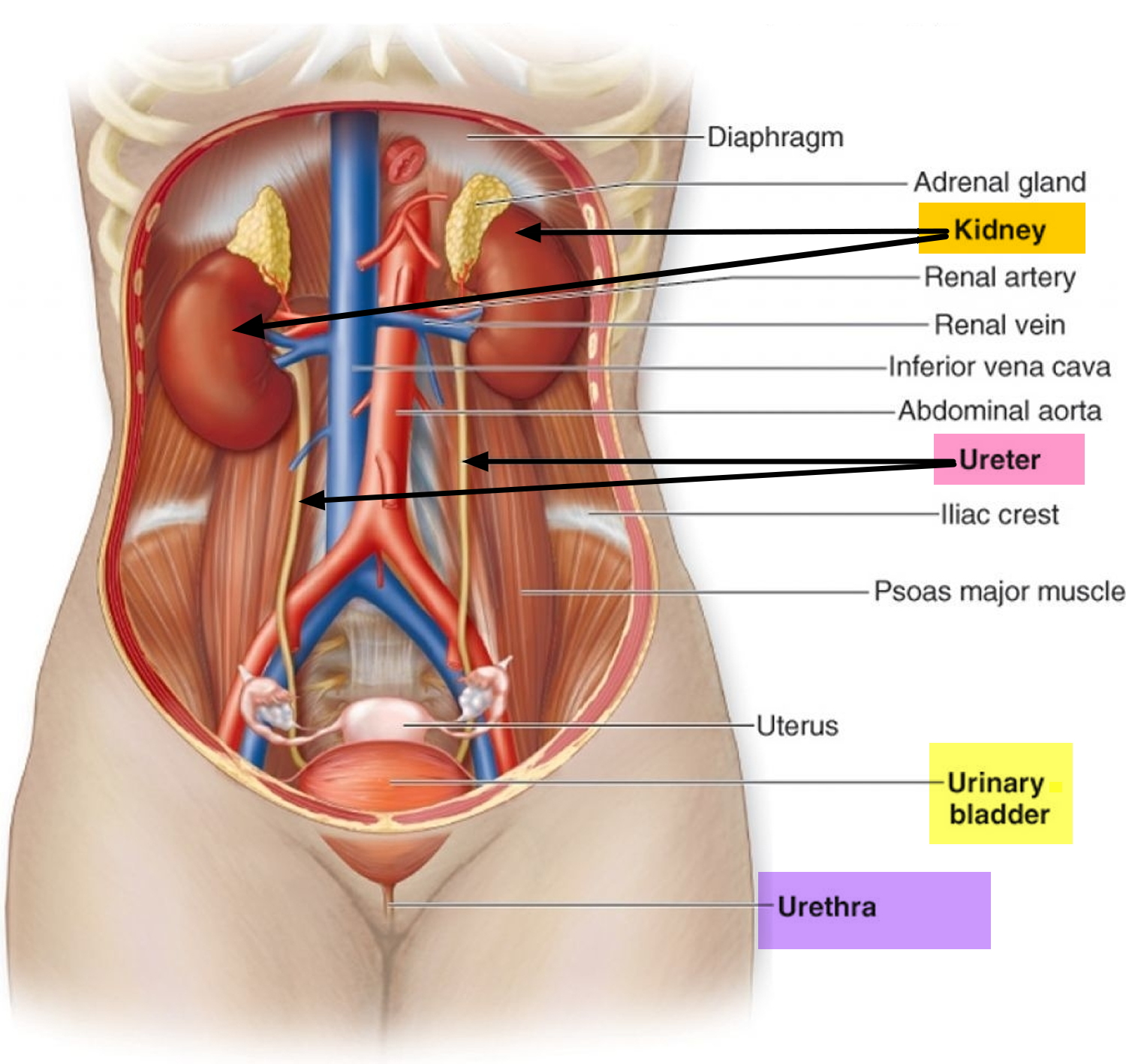
Figure 1. The Urinary Tract
Who is more likely to develop a kidney infection ?
You are more likely to develop a kidney infection if you 4:
- Are a woman
- have a urinary tract infection in the bladder.
- had a urinary tract infection during the past 12 months.
- are pregnant. Scientists think that hormonal changes and shifts in the position of the urinary tract during pregnancy make it easier for bacteria to travel to the kidneys and cause infection.
- have a problem in your urinary tract that blocks or changes the normal flow of urine. The flow of urine may be blocked if you have a defect in the structure of your urinary tract, such as a narrowed urethra, an enlarged prostate, or a kidney stone.
- have vesicoureteral reflux, which is when urine can back up, or reflux, into one or both kidneys. Health care professionals most commonly diagnose vesicoureteral reflux in children 5.
- have diabetes or problems with your body’s immune, or natural defense, system.
- have a spinal cord injury or nerve damage around the bladder.
- have trouble emptying your bladder completely, called urinary retention.
- using a urinary catheter for a time. Urinary catheters are tubes used to drain urine from the bladder. You might have a catheter placed during and after some surgical procedures and diagnostic tests. You might use one continuously if you’re confined to a bed.
What are the complications of kidney infections ?
In rare cases, kidney infections may cause:
- high blood pressure
- kidney failure
- permanent kidney scars, called renal scarring, which can lead to chronic kidney disease
- Blood poisoning (septicemia). Your kidneys filter waste from your blood and return your filtered blood to the rest of your body. Having a kidney infection can cause the bacteria to spread through your bloodstream.
- Pregnancy complications. Women who develop a kidney infection during pregnancy may have an increased risk of delivering low birth weight babies.
Your chance of a complication is slightly greater if you have:
- kidney disease from other causes
- a problem with the structure of your urinary tract
- repeated episodes of kidney infection
Complications from a kidney infection are rare if a health care professional prescribes antibiotics to treat your infection.
How do you get a kidney infection
Kidney infections are caused by bacteria or viruses.
Scientists believe that most kidney infections start as a bladder infection or in the urethra that moves upstream to infect one or both of your kidneys. This is the most common cause of kidney infections. Most often, the infection is caused by bacteria that normally live in your bowel. The urinary tract has several ways to prevent infection from moving up the urinary tract. For example, urination most often flushes out bacteria before it reaches the bladder. Sometimes your body can’t fight the bacteria and the bacteria cause a UTI. If you don’t get medical treatment to stop the infection, the bacteria may infect your kidneys.
In some cases, your blood can carry bacteria or viruses from another part of your body to your kidneys. Although it’s unusual to develop a kidney infection, it can happen — for instance, if you have an artificial joint or heart valve that becomes infected.
Rarely, kidney infection results after kidney surgery.
How do you prevent getting a kidney infection
Reduce your risk of kidney infection by taking steps to prevent urinary tract infections. Women, in particular, may reduce their risk of urinary tract infections if they:
- Drink fluids, especially water. Fluids can help remove bacteria from your body when you urinate.
- Urinate as soon as you need to. Avoid delaying urination when you feel the urge to urinate.
- Empty the bladder after intercourse. Urinating as soon as possible after intercourse helps clear bacteria from the urethra, reducing your risk of infection.
- Wipe carefully. Wiping from front to back after urinating and after a bowel movement helps prevent bacteria from spreading to the urethra.
- Avoid using feminine products in the genital area. Using products such as deodorant sprays in your genital area or douches can be irritating.
Kidney infection symptoms and signs
Symptoms of kidney infections vary by age. Symptoms may include
- Chills
- Fever
- Pain in your back, side, or groin
- Nausea and vomiting
- Burning sensation or pain when urinating
- Cloudy, dark, bloody, or foul-smelling urine
- Pus or blood in your urine (hematuria)
- Frequent urination
- Strong, persistent urge to urinate
- Abdominal pain
A child younger than 2 years old with a kidney infection may only have a high fever.
An adult older than age 65 with a kidney infection may have none of the typical symptoms. An older person may only have problems with thinking, such as
- confusion
- hallucinations
- jumbled speech
When to see a doctor
Seek medical attention right away if you have kidney infection symptoms. A kidney infection can sometimes lead to a dangerous condition called sepsis, which can be life threatening. Symptoms of sepsis include fever, chills, rapid breathing and heart rate, rash, and confusion.
A kidney infection that becomes chronic, or long lasting, can cause permanent damage to your kidneys.
How is kidney infection diagnosed
Health care professionals use your medical history, a physical exam, and tests to diagnose a kidney infection.
A health care professional will ask if you have a history of health conditions that make you more likely to develop a kidney infection. During a physical exam, the health care professional will ask you about your symptoms.
If you are a man and the health care professional suspects you have a kidney infection, he or she may perform a digital rectal examination (DRE). During a DRE, the health care professional has you bend over a table or lie on your side while holding your knees close to your chest. After putting on a glove, the health care professional slides a lubricated finger into your anus to check for a swollen or enlarged prostate blocking the neck of your bladder.
What tests do doctors use to diagnose a kidney infection ?
Doctors may use lab or imaging tests to diagnose a kidney infection.
Lab tests
Urinalysis. For a urinalysis, you will collect a urine sample in a special container at a doctor’s office or at a lab. A health care professional will look at the sample under a microscope for bacteria and white blood cells, which the body produces to fight infection. Bacteria also can be found in the urine of healthy people, so a kidney infection is diagnosed based both on your symptoms and a lab test.
Urine culture. A health care professional may culture your urine to find out what type of bacteria is causing the infection. A health care professional can see how the bacteria have multiplied, usually in 1 to 3 days, and can then determine the best treatment.
Imaging tests
A health care professional may use imaging tests, such as a computed tomography (CT) scan, magnetic resonance imaging (MRI), or ultrasound, to help diagnose a kidney infection. Other tests might include an ultrasound, CT scan or a type of X-ray called a voiding cystourethrogram. A voiding cystourethrogram involves injecting a contrast dye to take X-rays of the bladder when full and while urinating.
A technician performs these tests in an outpatient center or a hospital. A technician may perform an ultrasound in a doctor’s office as well. A radiologist reads and reports on the images. You don’t need anesthesia for these tests.
How to treat a kidney infection
Antibiotics for kidney infections
Antibiotics are the first line of treatment for kidney infections. Which drugs you use and for how long depend on your health and the bacteria found in your urine tests.
Ciprofloxacin 500 mg po bid for 7 days and levofloxacin 750 mg po once/day for 5 days are 1st-line antibiotics if < 10% of the uropathogens in the community are resistant 6. A 2nd option is usually trimethoprim/sulfamethoxazole 160/800 mg po bid for 14 days. However, local sensitivity patterns should be considered because in some parts of the US, > 20% of E. coli are resistant to sulfa.
Patients not eligible for outpatient treatment should be hospitalized and given parenteral therapy selected on the basis of local sensitivity patterns. First-line antibiotics are usually renally excreted fluoroquinolones, such as ciprofloxacin and levofloxacin. Other choices, such as ampicillin plus gentamicin, broad-spectrum cephalosporins (eg, ceftriaxone, cefotaxime, cefepime), aztreonam, beta-lactam/beta-lactam inhibitor combinations (ampicillin/sulbactam, ticarcillin/clavulanate, piperacillin/tazobactam), and imipenem/cilastatin, are usually reserved for patients with more complicated pyelonephritis (eg, with obstruction, calculi, resistant bacteria, or a hospital-acquired infection) or recent urinary tract instrumentation.
Parenteral therapy is continued until defervescence (abatement of a fever) and other signs of clinical improvement occur. In > 80% of patients, improvement occurs within 72 h. Oral therapy can then begin, and the patient can be discharged for the remainder of a 7- to14-day treatment course. Complicated cases require longer courses of IV antibiotics with total duration of 2 to 3 wk and urologic correction of anatomic defects.
Outpatient management can be considered in pregnant women with pyelonephritis, but only if symptoms are mild, close follow-up is available, and (preferably) pregnancy is < 24 wk gestation. Outpatient treatment is with cephalosporins (eg, ceftriaxone 1 to 2 g IV or IM, then cephalexin 500 mg po qid for 10 days). Otherwise, 1st-line IV antibiotics include cephalosporins, aztreonam, or ampicillin plus gentamicin. If pyelonephritis is severe, possibilities include piperacillin/tazobactam or meropenem. Fluoroquinolones and TMP/SMX should be avoided. Because recurrence is common, some authorities recommend prophylaxis after the acute infection resolves with nitrofurantoin 100 mg po or cephalexin 250 mg po every night during the remainder of the pregnancy and for 4 to 6 wk after pregnancy.
Usually, the signs and symptoms of a kidney infection begin to clear up within a few days of treatment. But you might need to continue antibiotics for a week or longer. Take the entire course of antibiotics recommended by your doctor even after you feel better.
Your doctor might recommend a repeat urine culture to ensure the infection has cleared. If the infection is still present, you’ll need to take another course of antibiotics.
Hospitalization for severe kidney infections
If your kidney infection is severe, your doctor might admit you to the hospital. Treatment might include antibiotics and fluids that you receive through a vein in your arm (intravenously). How long you’ll stay in the hospital depends on the severity of your condition.
Treatment for recurrent kidney infections
An underlying medical problem such as a misshapen urinary tract can cause you to get repeated kidney infections. In that case, you might be referred to a kidney specialist (nephrologist) or urinary surgeon (urologist) for an evaluation. You might need surgery to repair a structural abnormality.
How can you make sure your kidney infection is completely gone ?
If you recently had a kidney infection, the health care professional will often repeat urine cultures after your treatment ends to make sure your infection has completely gone away and has not come back. If a repeat test shows infection, you may take another round of antibiotics. If your infection comes back again, he or she may prescribe antibiotics for a longer time period.
If your health care professional prescribes antibiotics, take all of the antibiotics as prescribed and follow the advice of the health care professional. Even if you start to feel better, you should finish all of your medicine.
How can you prevent a kidney infection ?
Many kidney infections start as a bladder infection, so preventing bladder infections may help prevent kidney infections. Scientists are still trying to understand the best ways to prevent bladder infections, but these small changes in your daily habits may help:
Drink lots of liquid, especially water
Liquids can help flush bacteria from the urinary system. Water is best. Most healthy people should try to drink six to eight, 8-ounce glasses of liquid each day. If you need to drink less water because of other health conditions, such as bladder control problems, kidney failure or heart disease , ask your health care provider how much liquid is healthy for you.
Wipe from front to back after using the toilet
Women should wipe from front to back to keep bacteria from getting into the urethra. This step is most important after a bowel movement.
Urinate often and when the urge arises
Try to urinate at least every 3 to 4 hours. Bacteria are more likely to grow in the bladder when urine stays in the bladder too long.
Urinate after sex
Both women and men should urinate shortly after sex to flush away bacteria that may have entered the urethra during sex.
If these techniques are unsuccessful, antibiotic prophylaxis should be considered.
Common options are continuous and postcoital prophylaxis.
Continuous prophylaxis commonly begins with a 6 month trial. If urinary tract infection recurs after 6 mo of prophylactic therapy, prophylaxis may be reinstituted for 2 or 3 yr. Choice of antibiotic depends on susceptibility patterns of prior infections. Common options are trimethoprim/sulfamethoxazole 40/200 mg po once/day or 3 times/wk, nitrofurantoin 50 or 100 mg orally once/day, cephalexin 125 to 250 mg orally once/day, and fosfomycin 3 g orally every 10 days. Fluoroquinolones are effective but are not usually recommended because resistance is increasing. Also, fluoroquinolones are contraindicated in pregnant women and children. Nitrofurantoin is contraindicated if creatinine clearance is < 60 mL/min. Long-term use can rarely cause damage to the lungs, liver, and nervous system.
Postcoital prophylaxis in women may be more effective if urinary tract infections are temporally related to sexual intercourse. Usually, a single dose of one of the drugs used for continuous prophylaxis (other than fosfomycin) is effective.
Contraception is recommended for women using a fluoroquinolone because these drugs can potentially injure a fetus. Although concern exists that antibiotics may decrease the effectiveness of oral contraceptives, pharmacokinetic studies have not shown a significant or consistent effect. Nonetheless, some experts still recommend that women who use oral contraceptives use barrier contraceptives while they are taking antibiotics.
In pregnant women, effective prophylaxis of urinary tract infection is similar to that in nonpregnant women, including use of postcoital prophylaxis. Appropriate patients include those with acute pyelonephritis during a pregnancy, patients with > 1 episode (despite treatment) of urinary tract infection or bacteriuria during pregnancy, and patients who required prophylaxis for recurrent urinary tract infection before pregnancy.
In postmenopausal women, antibiotic prophylaxis is similar to that described previously. Additionally, topical estrogen therapy markedly reduces the incidence of recurrent urinary tract infection in women with atrophic vaginitis or atrophic urethritis.
- Pyelonephritis. National Center for Biotechnology Information, U.S. National Library of Medicine. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0027334/[↩]
- Grabe M, Bartoletti R, Bjerklund Johansn T.E., Cai T. Guidelines on Urological Infections. European Association of Urology; The Netherlands: 2015[↩]
- What is a kidney infection? National Institute of Diabetes and Digestive and Kidney Diseases https://www.niddk.nih.gov/health-information/urologic-diseases/kidney-infection-pyelonephritis/definition-facts[↩]
- Czaja CA, Scholes D, Hooton TM, Stamm WE. Population-based epidemiologic analysis of acute pyelonephritis. Clinical Infectious Diseases. 2007;45(3):273–280.[↩]
- Guarino N, Casamassima MG, Tadini B, Marras E, Lace R, Bianchi M. Natural history of vesicoureteral reflux associated with kidney anomalies. Urology. 2005;65(6):1208–1211.[↩]
- Bacterial Urinary Tract Infections (UTIs). Merck Manual. https://www.merckmanuals.com/professional/genitourinary-disorders/urinary-tract-infections-utis/bacterial-urinary-tract-infections-utis[↩]