Contents
- What is non-alcoholic fatty liver disease
- Liver anatomy
- What is non-alcoholic steatohepatitis?
- What is alcoholic fatty liver disease?
- Non-alcoholic fatty liver disease causes
- Non-alcoholic fatty liver disease prevention
- Non-alcoholic fatty liver disease stages
- Non-alcoholic fatty liver disease symptoms
- Non-alcoholic fatty liver disease complications
- Non-alcoholic fatty liver disease diagnosis
- Non-alcoholic fatty liver disease treatments
- Non-alcoholic fatty liver disease prognosis
What is non-alcoholic fatty liver disease
Nonalcoholic fatty liver disease (NAFLD) now called metabolic dysfunction-associated steatotic liver disease (MASLD) is a liver disease in which too much fat builds up in your liver and this buildup of fat is not caused by heavy alcohol use 1, 2. It is normal for your liver to contain some fat. However, if more than 5% to 10% percent of your liver’s weight is fat, then it is called a fatty liver (steatosis). Non-alcoholic fatty liver disease (NAFLD) is the most common form of liver disease in the world, with the highest rates being reported in South America and the Middle East, followed by Asia, the USA, and Europe; NAFLD is less common in Africa 3, 4, 5, 6. This study found that approximately 900 million people suffered from NAFLD in 2017 4. When heavy alcohol use causes fat to build up in your liver, this condition is called alcoholic fatty liver disease (AFLD). NAFLD is a growing cause of end-stage liver disease and has been recognized as a cause of liver cancer (hepatocellular cancer [HCC]), even in the absence of underlying cirrhosis 7.
Non-alcoholic fatty liver disease (NAFLD) is seen most often in people who are overweight or obese. NAFLD is becoming more common, especially in North African and Middle Eastern countries (including Qatar, Libya and Kuwait) and Western nations as the number of people with obesity and type 2 diabetes rises 8, 9. Global reports relating to the epidemiology of NAFLD have estimated a global prevalence of NAFLD between 25% and 35%, with Europe as high as 30%, 35% in South American countries and 35% in North America 10, 11, 12, 13, 10, 14.
Well-established risk factors for NAFLD include obesity, type 2 diabetes, an unhealthy diet (eg, high intake of red meat and processed meat) and physical inactivity 15, 16, 17, 18, 19. Of these, an unhealthy lifestyle is deemed to be the most important contributor to NAFLD 20. Key lifestyle factors include an increased intake of glucose, fructose, and saturated fat, induced hepatic de novo lipogenesis, subclinical inflammation in the adipose tissue and liver, and insulin resistance in adipose tissue, the liver, and skeletal muscle 21. These lifestyle factors are also accompanied by an increased risk of type 2 diabetes 21.
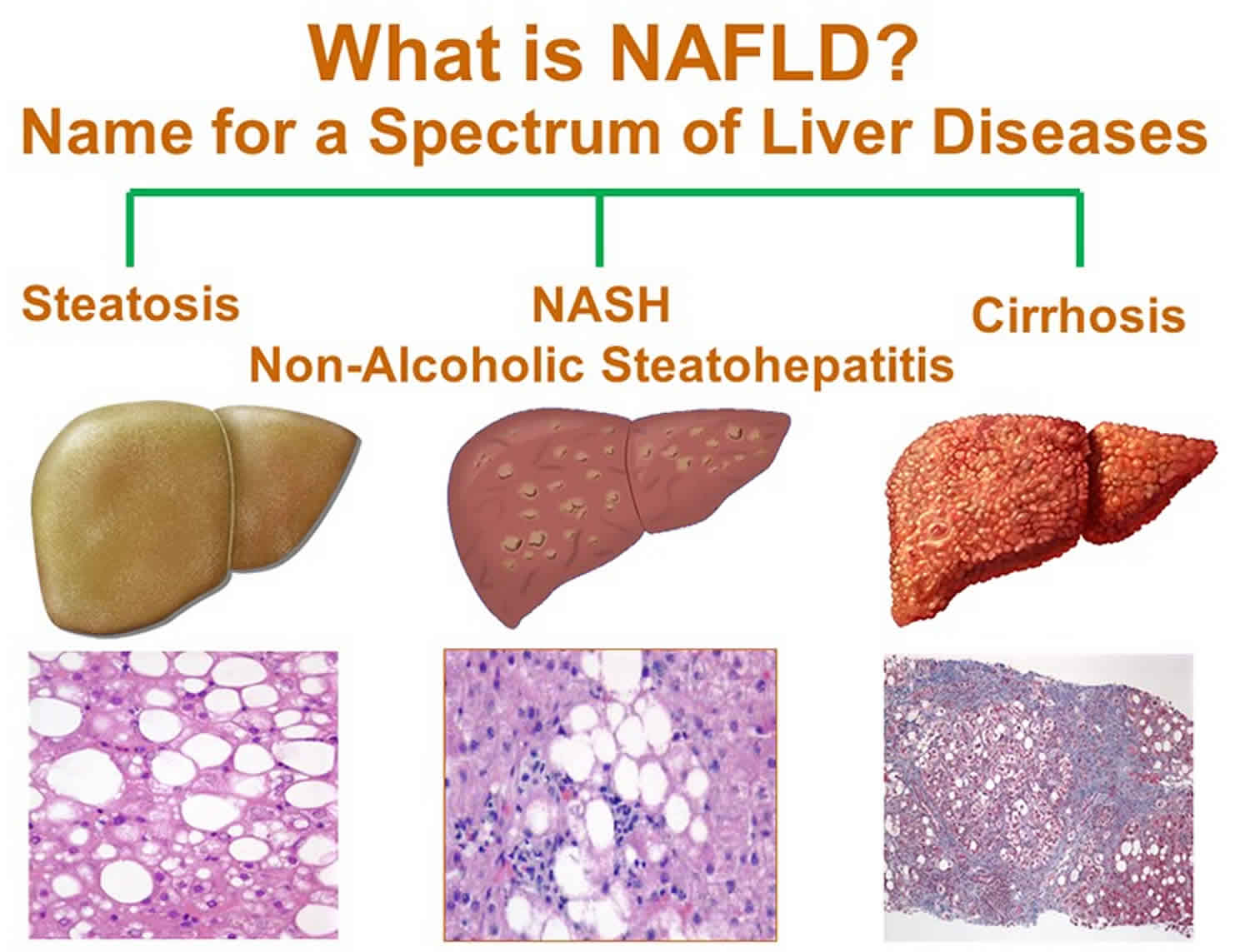
Non-alcoholic fatty liver disease (NAFLD) ranges in severity from nonalcoholic fatty liver (NAFL) to a more severe form of the disease called nonalcoholic steatohepatitis (NASH) 2.
- Nonalcoholic fatty liver (NAFL). Nonalcoholic fatty liver (NAFL) is a form of NAFLD in which you have fat in your liver but little or no inflammation or liver damage. Nonalcoholic fatty liver (NAFL) typically does not progress to cause liver damage or complications. However, nonalcoholic fatty liver (NAFL) can cause pain from enlargement of the liver and have a higher risk for other health problems 22.
- Nonalcoholic steatohepatitis (NASH). Nonalcoholic steatohepatitis (NASH) is the form of NAFLD in which you have inflammation of the liver and liver damage, in addition to fat in your liver. The inflammation and liver damage of NASH can cause fibrosis, or scarring, of the liver. NASH may lead to cirrhosis, in which the liver is scarred and permanently damaged. Cirrhosis can lead to liver cancer. Furthermore, people with NASH have an increased chance of dying from liver-related causes 23. It is hard to tell apart NAFLD from NASH without a clinical evaluation and testing.
Scientists are not sure why some people with NAFLD have NASH while others have nonalcoholic fatty liver (NAFL) 24. People typically develop one type of NAFLD or the other, although sometimes people with one form are later diagnosed with the other form of NAFLD. The majority of people with NAFLD have nonalcoholic fatty liver (NAFL). Only a small number of people with NAFLD have NASH. Experts guess that about 10% to 24% of Americans have nonalcoholic fatty liver disease (NAFLD) and about 1.5% to 6.5% have nonalcoholic steatohepatitis (NASH) 22, 25.
Non-alcoholic fatty liver disease (NAFLD) is more common in people who have certain diseases and conditions, including obesity, and conditions that may be related to obesity, such as type 2 diabetes 24. Studies suggest that one-third to two-thirds of people with type 2 diabetes have NAFLD 22. Research also suggests that NAFLD is present in up to 75% of people who are overweight and in more than 90% of people who have severe obesity 26, 27.
NAFLD can affect people of any age, including children. Research suggests that close to 10% of U.S. children ages 2 to 19 have NAFLD 28. However, people are more likely to develop NAFLD as they age.
While NAFLD occurs in people of all races and ethnicities, it is most common among Hispanic individuals, followed by non-Hispanic whites and Asian Americans, including those of East Asian and South Asian descent 23, 29. NAFLD is less common among non-Hispanic Blacks 23. On average, Asian Americans with NAFLD have a lower body mass index (BMI) than non-Hispanic whites with NAFLD 29. Experts think that genes may help explain some of the racial and ethnic differences in NAFLD 24.
Non-alcoholic fatty liver disease (NAFLD) usually is a silent disease with few or no symptoms 30. When it does, they may include:
- Fatigue.
- Not feeling well, or malaise.
- Pain or discomfort in the upper right belly area.
People with non-alcoholic fatty liver disease (NAFLD) have a higher risk for certain health problems, including:
- Cardiovascular disease, which is the most common cause of death in people who have NAFLD 23
- Type 2 diabetes
- Metabolic syndrome
- Conditions that may be part of metabolic syndrome, such as high blood pressure and abnormal levels of fats—cholesterol and triglycerides—in the blood.
Early-stage NAFLD does not usually cause any harm, but it can lead to serious liver damage, including cirrhosis, if it gets worse.
Having high levels of fat in your liver is also associated with an increased risk of serious health problems, such as type 2 diabetes, high blood pressure and kidney disease.
If you already have diabetes, NAFLD increases your chance of developing heart problems.
If detected and managed at an early stage, it’s possible to stop NAFLD getting worse and reduce the amount of fat in your liver.
Doctors recommend weight loss, done through a combination of calorie reduction, exercise, and healthy eating, to treat nonalcoholic fatty liver disease (NAFLD) 31, 32, 33. Weight loss can reduce fat, inflammation, and fibrosis or scarring in your liver 34.
If you are overweight or have obesity, losing weight by making healthy food choices, limiting portion sizes, and being physically active can improve nonalcoholic fatty liver disease (NAFLD). Losing at least 3% to 5% of your body weight can reduce fat in the liver 35, 23. You may need to lose up to 7% to 10% of your body weight to reduce liver inflammation and fibrosis 36, 33, 37, 23. Physical activity alone, even without weight loss, is also beneficial.
The best way to lose weight is done by:
- Reducing the number of calories you eat. Keeping track of the calories you consume every day and employing portion control can help.
- Eating a healthy diet that’s rich in fruits and vegetables, whole grains and low in saturated fats. Limit animal-based foods, like red meat which is high in saturated fats, and eat more plant-based foods like beans, legumes, and nuts. Use good fats like olive oil. This is the basis for the Mediterranean diet – which isn’t a diet in the traditional sense, but a healthy way of eating inspired by the eating habits of people living in the Mediterranean area and is often recommended by doctors as a way to reduce some of the risk factors associated with fatty liver disease.
- Limiting the amount of salt and sugar in your diet, particularly sugar-sweetened beverages, like soda, juices, sports drinks, and sweetened tea. High consumption of fructose, one of the main sweeteners in these beverages, increases your odds of developing obesity, type 2 diabetes, metabolic syndrome, and NAFLD.
- Limit your intake of saturated fats, which are found in meat, poultry skin, butter, shortening, milk and dairy products (except fat-free versions). Replace them with monounsaturated fats (olive, canola, and peanut oils) and polyunsaturated fats (corn, safflower, soybean oils, and many types of nuts). Particularly helpful in reducing heart disease are omega-3 fatty acids, a type of polyunsaturated fat found in oily fish such as salmon, flaxseed oil, and walnuts. Healthy eating combined with exercise – and taking cholesterol-lowering medications if prescribed by your doctor – will help keep your cholesterol and triglyceride levels where they need to be.
- Exercise and be more active – exercise is important for many reasons; it can help with weight control, boost your immune system, and alleviate stress and depression. Aim for at least 150 minutes of exercise a week. Depending on how much weight you’re trying to lose, you may need to up that amount. Getting exercise doesn’t mean you have to go to a gym – walking, gardening, and even housework counts. However, if you don’t already exercise, get your doctor’s okay first and build slowly. The goal is to participate in exercise of a moderate intensity (examples include light jogging, biking, swimming or playing a sport that boosts your heart rate and results in sweating).
Doctors recommend gradually losing weight to improve NAFLD. Rapid weight loss and malnutrition can make liver disease worse.
If you’ve tried to lose weight in the past without success, talk to your dietitian about getting help. You may also be a candidate for a medically-supervised weight loss program that employs medication along with diet and exercise. Alternatively, there are weight-loss (bariatric) surgical procedures and endoscopic therapies that work by either physically limiting the amount of food your stomach can hold, or reducing the amount of nutrients and calories your body absorbs. Talk to your doctor about which option may be best for you.
Figure 1. Nonalcoholic fatty liver disease (NAFLD)
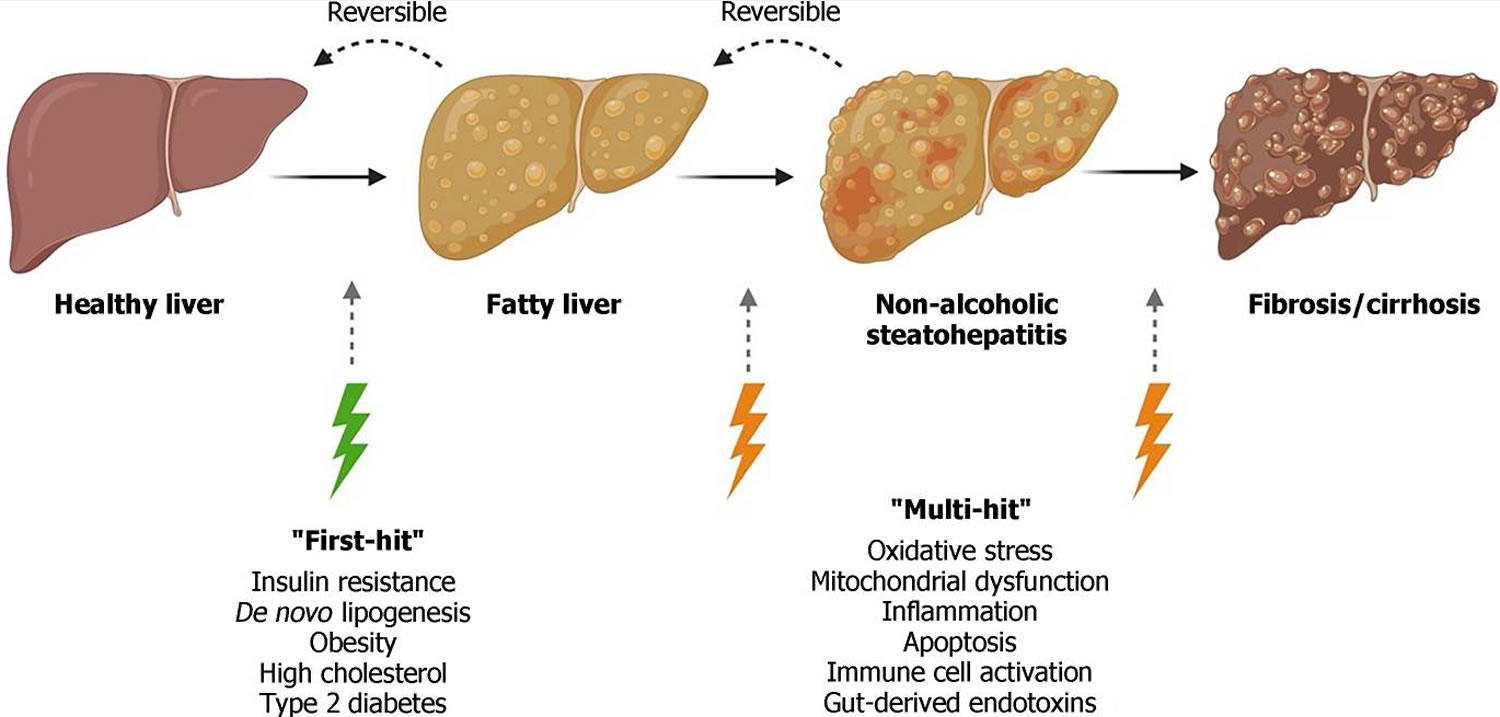
Figure 2. Non-alcoholic fatty liver disease progression
Footnotes: Non-alcoholic fatty liver disease (NAFLD) encompasses a range of liver damage, from simple accumulation of fat in liver cells, named steatosis, to more severe forms of the diseases such as nonalcoholic steatohepatitis (NASH), involving inflammation which can lead to fibrosis and cirrhosis. In the “multiple-hit” theory of progression, the first cause or “first-hit” in NAFLD is insulin resistance, obesity, type 2 diabetes, and metabolic syndrome. As the first hit occurs, free fatty acids are stored in the liver as triglycerides, resulting in simple steatosis. Disease progresses when multiple factors, or “multi-hits”, such as oxidative stress, inflammatory mediators, apoptosis, and mitochondrial dysfunction cause liver damage.
[Source 31 ]Liver anatomy
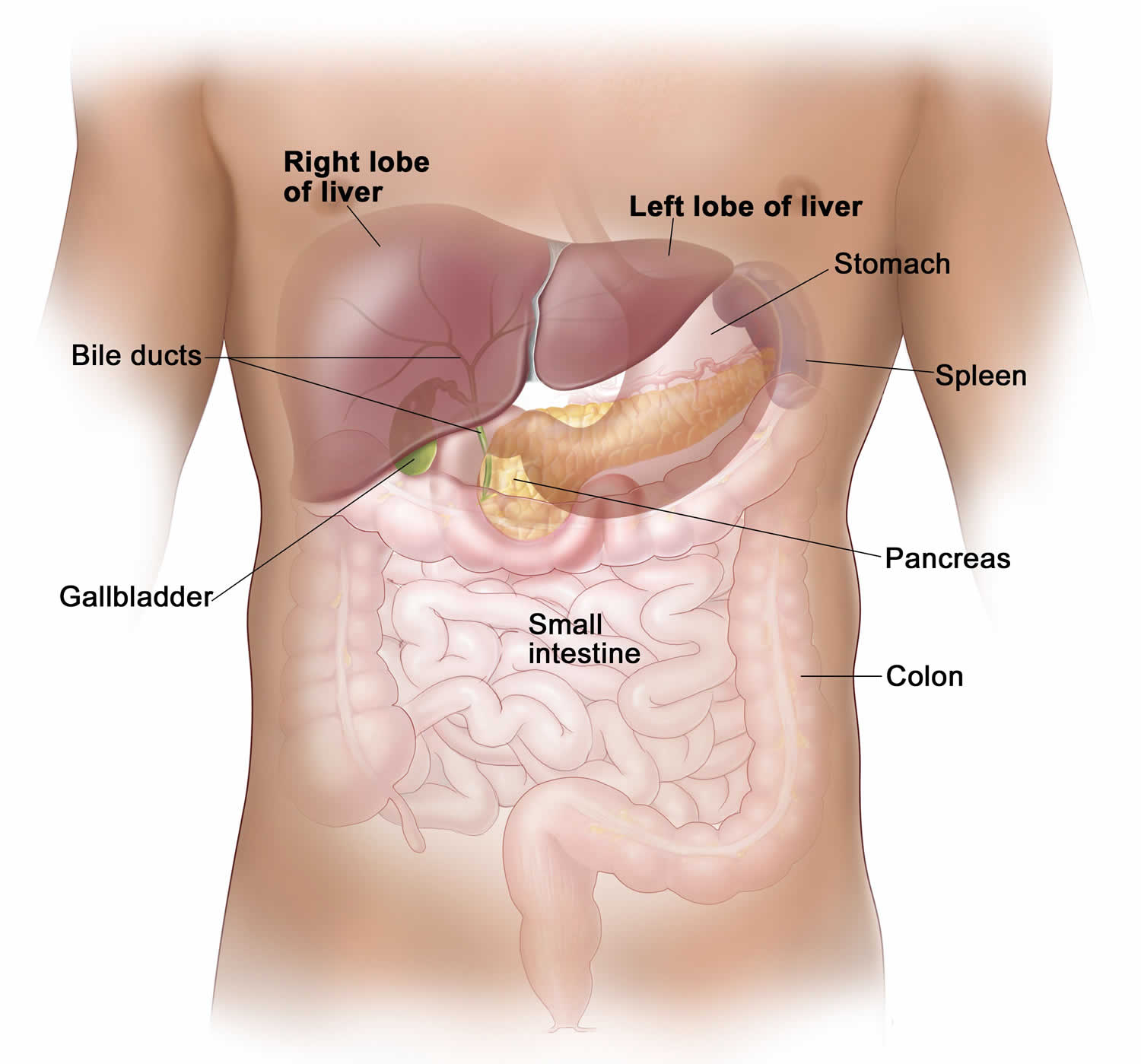
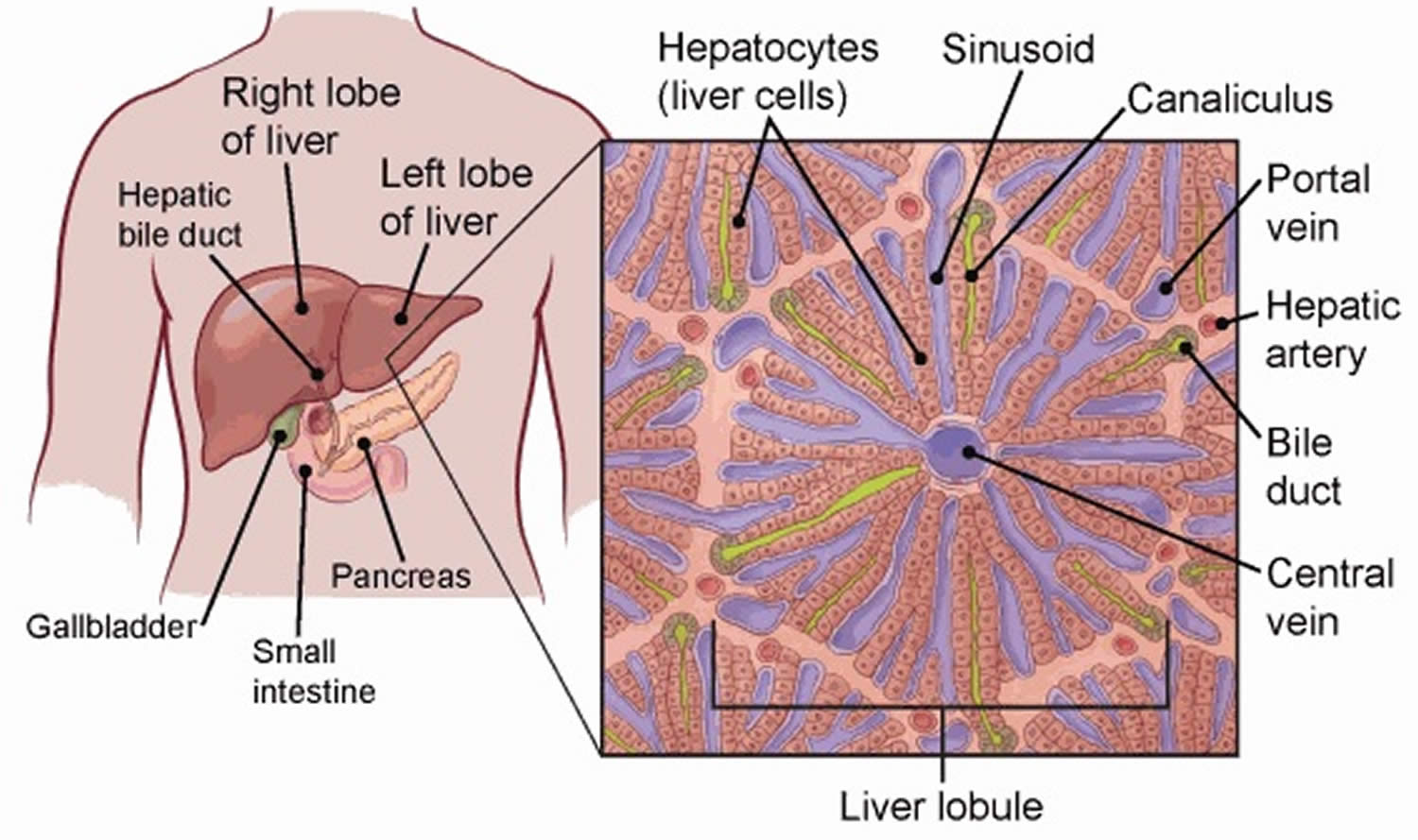
Your liver is essential to your life. You cannot live without your liver. Your liver is the largest internal organ in your body. Your liver is about the size of a football and weighs about 3 to 3.5 pounds (1.36–1.59kg). Your liver lies under your right ribs just beneath your right lung. Your liver has two lobes (sections). Your liver is made up mainly of liver cells called hepatocytes. It also has other types of cells, including cells that line its blood vessels and cells that line small tubes in the liver called bile ducts. The bile ducts carry bile from the liver to the gallbladder or directly to the intestines.
Your liver has many important functions:
- It breaks down and stores many of the nutrients absorbed from the intestine that your body needs to function. Some nutrients must be changed (metabolized) in the liver before they can be used for energy or to build and repair body tissues.
- It makes most of the clotting factors that keep you from bleeding too much when you are cut or injured.
- It delivers bile into the intestines to help absorb nutrients (especially fats).
- It breaks down alcohol, drugs, and toxic wastes in the blood, which then pass from the body through urine and stool.
Figure 3. Liver anatomy
What is non-alcoholic steatohepatitis?
Nonalcoholic steatohepatitis also called NASH or metabolic dysfunction associated steatohepatitis (MASH) is a fatty liver disease characterized by fatty changes with lobular hepatitis in people who drink little or no history of excessive alcohol consumption 38, 39, 40, 41, 42, 43. Jurgen Ludwig and colleagues in July 1980, at Mayo Clinic in Rochester, Minnesota, published the first article to identify non-alcoholic steatohepatitis (NASH) 38. At the time, steatohepatitis, which is a term to describe an inflammation of the liver that is accompanied by the abnormal accumulation of fat, was thought to be caused by excessive alcohol consumption. But the Mayo study described 20 people with fatty and inflamed livers — none of whom was a heavy alcohol drinker 38. Most had some liver scarring, also known as fibrosis 38. Three of the patients had cirrhosis, liver damage that results from such scarring. The study also noted that “most patients were moderately obese, and many had obesity-associated diseases” 38. Obesity and type 2 diabetes, two conditions associated with insulin resistance, are major risk factors for the development of NASH. Accumulating evidence suggests that the hyperinsulinemia associated with insulin resistance may be important in the pathogenesis of NASH.
Nonalcoholic steatohepatitis (NASH) is a severe form of nonalcoholic fatty liver disease (NAFLD) now called metabolic dysfunction-associated steatotic liver disease (MASLD) a term applied to a liver disease involving the presence of too much fat in the liver cells with or without inflammation and cellular injury that is not caused by alcohol 44, 45. Nonalcoholic steatohepatitis (NASH) is the form of NAFLD in which you have inflammation of the liver and liver damage, in addition to fat in your liver. The inflammation and liver damage of NASH may lead to serious liver scarring, called cirrhosis. NASH may progress to cirrhosis, in which the liver is scarred and permanently damaged. Cirrhosis can lead to liver cancer.
Experts guess that about 10% to 24% of Americans have nonalcoholic fatty liver disease (NAFLD) and about 1.5% to 6.5% have nonalcoholic steatohepatitis (NASH) 22, 25.
A diagnosis of nonalcoholic steatohepatitis (NASH) is established by the presence of morphologic changes on liver biopsy similar to those seen in alcoholic hepatitis, including hepatocellular fat accumulation, evidence of lobular inflammation and cell injury, and in some cases, progressive fibrosis, but are found in the absence of alcohol abuse. Nonalcoholic steatohepatitis (NASH) is typically identified during the evaluation of elevated ALT (alanine aminotransferase) or AST (aspartate aminotransferase) levels after exclusion of viral, metabolic, and other causes of liver disease.
Nonalcoholic steatohepatitis (NASH) is increasingly recognized as a relatively common disorder occurring in 3% of adults that may progress to hepatic fibrosis, a precursor to cirrhosis in 15% to 40% of nonalcoholic steatohepatitis (NASH) patients 42. Cirrhosis is a condition in which your liver is scarred and permanently damaged. Scar tissue replaces healthy liver tissue and prevents your liver from working normally. Scar tissue also partly blocks the flow of blood through your liver. As cirrhosis gets worse, your liver begins to fail. Exactly how many patients with nonalcoholic steatohepatitis (NASH) progress to cirrhosis is unknown, but 1% to 2% of liver transplants are now performed because of a pretransplant diagnosis of nonalcoholic steatohepatitis (NASH).
If you have nonalcoholic steatohepatitis (NASH), you may have symptoms that could take years for them to develop. If liver damage from nonalcoholic steatohepatitis (NASH) leads to permanent scarring and hardening of your liver, this is called cirrhosis.
Symptoms from nonalcoholic steatohepatitis (NASH) may include:
- Severe tiredness
- Weakness
- Weight loss
- Yellowing of the skin or eyes (jaundice)
- Spiderlike blood vessels on your skin
- Long-lasting itchy skin.
Nonalcoholic steatohepatitis (NASH) that turns into cirrhosis could cause symptoms like fluid retention, abdominal swelling (ascites), shortness of breath, swelling of the legs, enlarged spleen, red palms, internal bleeding, muscle wasting, and confusion. People with cirrhosis over time may develop liver failure and need a liver transplant.
If you have nonalcoholic steatohepatitis (NASH), no medication is available to reverse the fat buildup in your liver. In some cases, the liver damage stops or even reverses itself. But in others, nonalcoholic steatohepatitis (NASH) continues to progress. If you have nonalcoholic steatohepatitis (NASH), it’s important to control any conditions that may contribute to fatty liver disease.
Nonalcoholic steatohepatitis (NASH) treatments and lifestyle changes may include:
- Losing weight
- Medication to reduce cholesterol or triglycerides
- Medication to reduce blood pressure
- Medication to control diabetes
- Limiting over-the-counter (OTC) drugs
- Avoiding alcohol
- Seeing a liver specialist
Some medications are being studied as possible treatments for nonalcoholic steatohepatitis (NASH). These include antioxidants like vitamin E. Scientists are also studying some new diabetes medications for nonalcoholic steatohepatitis (NASH) that may be given even if you don’t have diabetes. However, you should only take these medicines after consulting with a liver specialist.
What is alcoholic fatty liver disease?
Alcoholic fatty liver disease (AFLD) is a fatty liver disease caused to heavy alcohol (ethanol) consumption 46. Alcoholic fatty liver disease (AFLD) is characterized by the excessive accumulation of triglycerides and cholesterol in liver cells 47. If you have a history of heavy alcohol use and fat in your liver, your doctor may determine you have alcohol-associated liver disease instead of nonalcoholic fatty liver disease (NAFLD). If you have risks for nonalcoholic fatty liver disease (NAFLD) and also drink alcohol (ethanol) excessively, you could have both nonalcoholic fatty liver disease (NAFLD) and alcohol-associated liver disease at the same time. No tests can easily tell how much each plays a role.
Your liver breaks down most of the alcohol (ethanol) you drink using liver enzymes – alcohol dehydrogenase (ADH), aldehyde dehydrogenase (ALDH), and Cytochrome P450 2E1 (CYP2E1), so it can be removed from your body 47, 48, 49. But the process of breaking alcohol down can generate harmful substances: (1) acetaldehyde accumulation; (2) an alteration in the nicotinamide adenine dinucleotide (NAD)H/NAD+ ratio; and/or (3) generation of reactive oxygen species (ROS) 46. These substances can damage liver cells, promote liver inflammation (hepatitis), and weaken your body’s natural defenses 47, 49, 50, 51, 52. The more alcohol that you drink, the more you damage your liver. Alcoholic fatty liver disease is the earliest stage of alcohol-related liver disease. The next stages are alcoholic hepatitis and cirrhosis. Alcohol is a toxin and a psychoactive and dependence-producing substance and has been classified as a Group 1 carcinogen by the International Agency for Research on Cancer (IARC) decades ago – this is the highest risk group, which also includes asbestos, radiation and tobacco 53, 54, 53, 55. According to the latest 2023 report from the World Health Organization (WHO), alcohol (ethanol) is a major factor in the development of around 200 diseases, and no amount of alcohol consumption is considered safe 56. Alcohol consumption is the third major cancer risk factor after tobacco use and excess body weight and alcohol consumption is an established cause of at least 7 types of cancer, such as oral cavity cancer, pharyngeal cancer, laryngeal cancer, esophageal cancer, liver cancer, colorectal cancer, and female breast cancer 57, 58, 59, 60, 61, 62, 63. The risk of developing cancer increases substantially the more alcohol you consumed 56, 64.
Non-alcoholic fatty liver disease causes
Scientists don’t know exactly why fat builds up in some livers and not others. They also don’t fully understand why some fatty livers turn into non-alcoholic fatty liver disease (NAFLD).
Non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) are both linked to the following 65, 66, 67, 68, 69:
- Genetics. Researchers have found that certain genes may make you more likely to develop NAFLD. These genes may help explain why NAFLD is more common in certain racial and ethnic groups. Studies have identified many genetic changes that may be associated with the development of NAFLD and NASH. Among these is a particular variation in the PNPLA3 gene 70. The PNPLA3 gene provides instructions for making a protein called adiponutrin, which is found in fat cells (adipocytes) and liver cells (hepatocytes). The function of this protein is not well understood, but it is thought to help regulate the production and breakdown of fats (lipogenesis and lipolysis) and the development of adipocytes. Studies indicate that the activity (expression) of the PNPLA3 gene decreases during periods without food (fasting) and increases after eating, suggesting that the amount of adiponutrin protein produced is regulated as needed to help process and store fats in the diet. The PNPLA3 gene variation associated with NAFLD is thought to lead to increased production and decreased breakdown of fats in the liver. Research is ongoing to determine how this and other genetic changes contribute to the development of NAFLD and its complications.
- Overweight or obesity.
- Insulin resistance, which happens when your cells don’t take up sugar in response to the hormone insulin.
- Type 2 diabetes, sometimes called high blood sugar or hyperglycemia.
- High levels of fats (abnormal levels of cholesterol—high total cholesterol, high LDL cholesterol, or low HDL cholesterol), especially triglycerides, in the blood.
These combined health problems may contribute to a fatty liver. However, some people get NAFLD even if they do not have any risk factors.
Risk factors for developing non-alcoholic fatty liver disease
Many diseases and health problems can increase your risk of non-alcoholic fatty liver disease (NAFLD), including:
- Family history of fatty liver disease or obesity.
- Growth hormone deficiency, which means the body doesn’t make enough hormones to grow.
- High cholesterol.
- High levels of triglycerides in the blood.
- Insulin resistance.
- Metabolic syndrome. Metabolic syndrome is a group of traits and medical conditions linked to overweight and obesity. Doctors define metabolic syndrome as the presence of any three of the following:
- large waist size
- high levels of triglycerides in your blood
- low levels of HDL cholesterol in your blood
- high blood pressure
- higher than normal blood glucose levels or a diagnosis of type 2 diabetes
- Obesity, especially when fat is centered in the waist.
- Polycystic ovary syndrome (PCOS).
- Obstructive sleep apnea.
- Type 2 diabetes.
- Underactive thyroid, also called hypothyroidism.
- Underactive pituitary gland, or hypopituitarism.
If you have risks for NAFLD and also drink alcohol excessively, you could have both NAFLD and alcohol-associated liver disease at the same time. No tests can easily tell how much each plays a role.
Nonalcoholic steatohepatitis (NASH) is more likely in these groups:
- People older than 50.
- People with certain genetic risk factors.
- People with obesity.
- People with diabetes or high blood sugar.
- People with symptoms of metabolic syndrome, such as high blood pressure, high triglycerides and a large waist size.
Having more of these health conditions increases your chances of developing NASH. Losing weight may cause nonalcoholic steatohepatitis (NASH) to switch to nonalcoholic fatty liver (NAFL) and regaining weight may cause nonalcoholic fatty liver (NAFL) to switch to nonalcoholic steatohepatitis (NASH).
Non-alcoholic fatty liver disease prevention
You may be able to prevent non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) by being physically active regularly, eating a healthy diet, limiting your portion sizes, and maintaining a healthy weight.
To reduce your risk of non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH):
- Eat a healthy diet. Eat a healthy diet that’s rich in fruits, vegetables, whole grains and healthy fats.
- Limit alcohol, simple sugars and portion sizes. Avoid sugary drinks like soda, sports drinks, juices and sweet tea. Drinking alcohol can damage your liver and should be avoided or minimized.
- Keep a healthy weight. If you are overweight or obese, work with your health care team to gradually lose weight. If you are a healthy weight, work to keep it by eating a healthy diet and exercising.
- Exercise. Be active most days of the week. Get an OK from your health care team first if you haven’t been exercising regularly.
Non-alcoholic fatty liver disease stages
Staging and grading systems have been developed to characterize the histological changes in non-alcoholic fatty liver disease (NAFLD), mainly as a tool for clinical research.
Non-alcoholic fatty liver disease (NAFLD) Grades 71, 72, 73, 74, 75:
- Grade 0 (Normal) is defined as a normal liver containing fat in less than 5% of liver cells (hepatocytes)
- Grade 1 (Mild): Fatty liver (steatosis) up to 66%, occasional ballooning in zone 3, scattered polymorphs with or without lymphocytes, mild or no portal inflammation
- Grade 2 (Moderate): Any degree of steatosis, obvious ballooning predominantly in zone 3, intralobular inflammation with polymorphs and chronic inflammation, and mild to moderate portal inflammation
- Grade 3 (Severe): Panacinar steatosis, ballooning, and obvious disarray predominantly in zone 3, intralobular inflammation with scattered polymorphs with or without mild chronic and mild to moderate portal inflammation
Non-alcoholic fatty liver disease (NAFLD) Stages 71, 72, 73, 74, 75, 76, 77, 78:
- Stage 0: No fibrosis
- Stage 1: Zone 3 perisinusoidal fibrosis only
- Stage 2: Zone 3 perisinusoidal and periportal fibrosis
- Stage 3: Bridging fibrosis
- Stage 4: Cirrhosis
Progression of the fibrosis stage to a cirrhotic scarred liver can vary between individuals, with cirrhosis occurring up to 15 to 20 years after initial diagnosis 77, 79. The median survival rate for patients with compensated cirrhosis is approximately 9 to 12 years, however, patients with decompensated cirrhosis have a significantly lower median survival rate of approximately 2 years 80. Patients in the compensated stage are frequently asymptomatic, and often remain undiagnosed 80. Therefore, early detection of cirrhotic patients who are still in the compensated stage is crucial, as early diagnosis could prevent or slow down disease progression 31.
Non-alcoholic fatty liver disease symptoms
Often, there are no symptoms of non-alcoholic fatty liver disease (NAFLD) in its early stages. It is more common for symptoms to develop once significant damage to the liver has occurred. Some symptoms of non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) may include:
- Discomfort or pain in the abdomen (belly area)
- Fatigue (feeling very tired)
- Irritability
- Headaches
- Difficulty concentrating
- Depression and anxiety
- Changes in skin color near joints and the back of the neck/upper back
If cirrhosis develops, the following symptoms may be present:
- Jaundice (yellowing of the skin and whites of the eyes)
- Itchy skin
- Swelling of the lower stomach
- Bruising easily
- Dark urine
Non-alcoholic fatty liver disease complications
Severe liver scarring, or cirrhosis, is the main complication of non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH). Cirrhosis happens because of liver injury, such as the damage caused by inflammation in NASH. As the liver tries to stop inflammation, it creates areas of scarring, also called fibrosis. With ongoing inflammation, fibrosis spreads and takes up more liver tissue.
If nothing is done to stop the scarring, cirrhosis can lead to:
- Fluid buildup in the stomach area, called ascites.
- Swollen veins in your esophagus, or esophageal varices, which can rupture and bleed.
- Confusion, sleepiness and slurred speech, also called hepatic encephalopathy.
- Overactive spleen, or hypersplenism, which can cause too few blood platelets.
- Liver cancer.
- End-stage liver failure, which means the liver has stopped working.
Non-alcoholic fatty liver disease diagnosis
Doctors use your medical history, a physical exam, and tests to diagnose nonalcoholic fatty liver disease (NAFLD) including nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH). Because nonalcoholic fatty liver disease (NAFLD) typically causes no symptoms, it is often found when tests done for other reasons point to a liver problem. For example, your blood work may show high levels of liver enzymes, or an ultrasound of your abdomen might reveal that your liver looks enlarged, which can lead to more testing. Doctors use blood tests, imaging tests, and sometimes liver biopsy to diagnose NAFLD and to tell the difference between nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH).
Medical history
Your doctor will ask if you have a history of health conditions or diseases that make you more likely to develop NAFLD, such as:
- overweight or obesity
- insulin resistance or type 2 diabetes
- high levels of triglycerides or abnormal levels of cholesterol in your blood
- metabolic syndrome
Your doctor will ask about your diet and lifestyle factors that may make you more likely to develop liver disease or fat in your liver.
- What medicines you take to determine whether a medicine might be causing your fatty liver.
- Your doctor will ask about your alcohol intake to find out whether fat in your liver is a sign of alcohol-associated liver disease or NAFLD. Medical tests cannot show whether alcohol is the cause of fat in the liver, so it’s important to be honest with your doctor.
- What your diet is like (eating a diet high in sugar, or drinking sugary beverages), your level of physical activity, and other lifestyle factors that can contribute to the likelihood of developing NAFLD.
Physical exam
During a physical exam, a doctor usually examines your body and checks your weight and height to calculate your body mass index (BMI). Your BMI estimates how much you should weigh based on your height. Most experts say that a BMI greater than 30 (obesity) is unhealthy. If you want to figure out your BMI on your own, there are many websites that calculate it for you when you enter your height and weight. If you have more or less muscle than is normal, your BMI may not be a perfect measure of how much body fat you have. Your doctor may also take your waist circumference and waist-to-hip ratio into consideration.
Your doctor will look for signs of nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH), such as:
- an enlarged liver
- signs of insulin resistance, such as darkened skin patches over your knuckles, elbows, and knees
- signs of cirrhosis, such as an enlarged spleen, ascites, spiderlike blood vessels on your skin, yellowing of your skin and whites of your eyes (jaundice) and muscle loss
Blood tests
Your doctor may take a blood sample from you and send the sample to a lab.
Your blood tests may include:
- Complete blood count.
- Iron studies, which show how much iron is in your blood and other cells.
- Liver enzyme and liver function tests.
- Tests for chronic viral hepatitis (hepatitis A, hepatitis C and others).
- Celiac disease screening test.
- Fasting blood sugar.
- Hemoglobin A1C, which shows how stable your blood sugar is.
- Lipid profile, which measures blood fats, such as cholesterol and triglycerides.
Your doctor may suspect you have NAFLD if your blood test shows increased levels of the liver enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST). The cells in your liver contain proteins called enzymes, which are chemicals that help the liver do its work. When liver cells are damaged or destroyed, the enzymes in the cells leak out into the blood where they can be measured by blood tests. Liver enzyme testing usually checks the blood for two main enzymes 36, 81:
- ALT (alanine aminotransferase)
- AST (aspartate aminotransferase)
If your liver is damaged due to inflammation, the level of these enzymes may be higher than normal. However, ALT and AST levels do not tell you how much scarring (fibrosis) may be present in your liver or predict how much liver damage will develop. In some people with NAFLD these liver enzymes may be normal as well.
Fibrosis assessment tests
These blood tests result in a score that estimates your level of liver scarring or fibrosis. They include:
- AST-to-Platelet Ratio Index (APRI) score
- Fibrosis-4 (Fib-4) score. The fibrosis-4 scoring system uses a patients age, platelet count, AST (aspartate aminotransferase) and ALT (alanine aminotransferase) to determine a liver fibrosis score and can help to predict advanced fibrosis.
These scores can help doctors identify or rule out advanced liver fibrosis, or scarring.
Your doctor may perform additional blood tests to find out if you have other health conditions that may increase your liver enzyme levels.
Imaging tests
Your doctor may order tests that take images, or pictures, of your liver to help make the diagnosis of liver disease. Different types of images can be obtained by using various types of equipment. However, these tests can’t show inflammation or fibrosis, so your doctor can’t use these tests to find out whether you have nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH). If you have cirrhosis, routine imaging tests may show nodules, or lumps, in your liver.
Your doctor may use the following imaging tests to help diagnose NAFLD:
- Abdominal ultrasound, which uses a device called a transducer that bounces safe, painless sound waves off your organs to create an image of their structure. Abdominal ultrasoundis often the first test used when liver disease is suspected.
- Computed tomography (CT) scan, which uses a combination of x-rays and computer technology to create images of your liver.
- Magnetic resonance imaging (MRI), which uses radio waves and magnets to produce detailed images of organs and soft tissues without using x-rays.
- Transient elastography, a newer type of ultrasound that measures the stiffness of your liver to determine if you have advanced liver fibrosis. Liver stiffness is a sign of fibrosis or scarring. Commonly used types of elastography are:
- Vibration-controlled transient elastography, a special type of ultrasound
- Sheer wave elastography, another type of ultrasound to detect increased liver stiffness
- Magnetic resonance elastography (MRE), is a newer, noninvasive test that combines features of ultrasound and MRI imaging to create a visual map showing gradients of stiffness throughout the liver. MRE has been shown to be a more reliable measure of liver stiffness in severely obese patients.
Liver biopsy
If other tests show signs of more-advanced liver disease or nonalcoholic steatohepatitis (NASH), or if your test results are unclear, your doctor may suggest a liver biopsy. Liver biopsy is a procedure to remove a small piece of tissue from your liver. It is usually done using a needle through the abdominal wall. The tissue sample is looked at in a lab for signs of inflammation and scarring. Liver biopsy is the only test that can prove a diagnosis of NASH and clearly shows the amount of liver damage.
Liver biopsy can show fibrosis at earlier stages than elastography can. However, doctors don’t recommend liver biopsy for everyone with suspected NAFLD. Your doctor may recommend a liver biopsy if you are more likely to have nonalcoholic steatohepatitis (NASH) with advanced fibrosis or if your other tests show signs of advanced liver disease or cirrhosis. In some cases, doctors may recommend a liver biopsy to rule out other liver diseases.
During a liver biopsy, a doctor using a needle that is passed through the abdominal wall and into the liver will take small pieces of tissue from your liver. A pathologist will examine the tissue under a microscope to look for signs of damage or disease.
A liver biopsy can be uncomfortable, and it does have risks that your doctor will go over with you in detail.
Non-alcoholic fatty liver disease treatments
Doctors recommend weight loss, done through a combination of calorie reduction, exercise, and healthy eating, to treat nonalcoholic fatty liver disease (NAFLD) 31, 32, 33, 34. Weight loss can reduce fat, inflammation, and fibrosis or scarring in your liver 34.
If you are overweight or have obesity, losing weight by making healthy food choices, limiting portion sizes, and being physically active can improve nonalcoholic fatty liver disease (NAFLD). Losing at least 3% to 5% of your body weight can reduce fat in the liver 35, 23. You may need to lose up to 7% to 10% of your body weight to reduce liver inflammation and fibrosis 36, 33, 37, 23. Physical activity alone, even without weight loss, is also beneficial.
The best way to lose weight is done by:
- Reducing the number of calories you eat. Keeping track of the calories you consume every day and employing portion control can help.
- Eating a healthy diet that’s rich in fruits and vegetables, whole grains and low in saturated fats. Limit animal-based foods, like red meat which is high in saturated fats, and eat more plant-based foods like beans, legumes, and nuts. Use good fats like olive oil. This is the basis for the Mediterranean diet – which isn’t a diet in the traditional sense, but a healthy way of eating inspired by the eating habits of people living in the Mediterranean area and is often recommended by doctors as a way to reduce some of the risk factors associated with fatty liver disease.
- Limiting the amount of salt and sugar in your diet, particularly sugar-sweetened beverages, like soda, juices, sports drinks, and sweetened tea. High consumption of fructose, one of the main sweeteners in these beverages, increases your odds of developing obesity, type 2 diabetes, metabolic syndrome, and NAFLD.
- Limit your intake of saturated fats, which are found in meat, poultry skin, butter, shortening, milk and dairy products (except fat-free versions). Replace them with monounsaturated fats (olive, canola, and peanut oils) and polyunsaturated fats (corn, safflower, soybean oils, and many types of nuts). Particularly helpful in reducing heart disease are omega-3 fatty acids, a type of polyunsaturated fat found in oily fish such as salmon, flaxseed oil, and walnuts. Healthy eating combined with exercise – and taking cholesterol-lowering medications if prescribed by your doctor – will help keep your cholesterol and triglyceride levels where they need to be.
- Exercise and be more active – exercise is important for many reasons; it can help with weight control, boost your immune system, and alleviate stress and depression. Aim for at least 150 minutes of exercise a week. Depending on how much weight you’re trying to lose, you may need to up that amount. Getting exercise doesn’t mean you have to go to a gym – walking, gardening, and even housework counts. However, if you don’t already exercise, get your doctor’s okay first and build slowly. The goal is to participate in exercise of a moderate intensity (examples include light jogging, biking, swimming or playing a sport that boosts your heart rate and results in sweating).
Doctors recommend gradually losing weight to improve NAFLD. Rapid weight loss and malnutrition can make liver disease worse.
If you’ve tried to lose weight in the past without success, talk to your dietitian about getting help. You may also be a candidate for a medically-supervised weight loss program that employs medication along with diet and exercise. Alternatively, there are weight-loss (bariatric) surgical procedures and endoscopic therapies that work by either physically limiting the amount of food your stomach can hold, or reducing the amount of nutrients and calories your body absorbs. Talk to your doctor about which option may be best for you.
Patients with NASH are to be followed by liver specialists or gastroenterologists. NASH with cirrhosis requires hepatocellular carcinoma (HCC) surveillance with an ultrasound every six months 65.
Non-alcoholic fatty liver disease diet
If you have NAFLD, your doctor may suggest changes to your diet such as:
- Limiting your intake of fats, which are high in calories and increase your chance of developing obesity.
- Replacing saturated fats and trans fats in your diet with unsaturated fats, especially omega-3 fatty acids, which may reduce your chance of heart disease if you have NAFLD.
- Eating more low-glycemic (low GI) index foods such as most fruits, vegetables, and whole grains. These foods affect your blood glucose less than high-glycemic index foods, such as white bread, white rice, and potatoes.
- Avoiding foods and drinks that contain large amounts of simple sugars, especially fructose. Fructose is found in sweetened soft drinks, sports drinks, sweetened tea, and juices. Table sugar, called sucrose, is rapidly changed to glucose and fructose during digestion and is therefore a major source of fructose.
If you have NAFLD, you should minimize alcohol use, which can further damage your liver.
Evidence has suggested that the ketogenic diet (diet with very low in carbohydrate and very high in fat = 75-80% fat, 10-15% protein and ≤ 5% carbohydrate) is an effective treatment for NAFLD 83, 34, 84, 31. Ketogenesis is a metabolic process resulting in the production of ketone bodies, namely acetoacetate, beta-hydroxybutyrate and acetone, which act as alternative energy sources 85, 83. The ketogenic diet has been shown to change hepatic mitochondrial fluxes and redox state as well as significantly reducing liver fat content and liver insulin resistance 86. These changes were found to be accompanied by an increase in the net hydrolysis of liver triglycerides, a decrease in endogenous glucose production, and lower serum insulin levels 86. Beta-hydroxybutyrate has also been shown to interact with inflammasomes 87, 88 and neutralize reactive oxygen species (ROS) 89, leading to a reduction in inflammatory cytokines and oxidative damage via its antioxidant capacity. These findings suggest a ketogenic diet can contribute to the reversal of NAFLD through improvement of insulin resistance and cellular redox function 31.
Non-alcoholic fatty liver disease medication
No medicines have been approved to treat nonalcoholic fatty liver disease (NAFLD) 90, 65, 31. However, a new medicine called Resmetirom (Rezdiffra) can help reduce the amount of fat that collects in the liver is available to treat people who have nonalcoholic steatohepatitis (NASH) with moderate to severe liver scarring. In March 2024, the US Food and Drug Administration (FDA) approved the use of resmetirom (Rezdiffra) for people with NASH and stage 2 or 3 fibrosis (but not cirrhosis) along with eating a healthy diet and participating in regular exercise. This is the first drug approved for nonalcoholic steatohepatitis (NASH) in the United States and the approval was based on resolution of NASH and improvement in fibrosis in about a quarter of the patients treated in a large international trial 91. Resmetirom (Rezdiffra) is not recommended for people with cirrhosis. For those who have cirrhosis due to NASH, a liver transplant may be needed.
Resmetirom (Rezdiffra) drug works by revving up the thyroid hormone pathway in the liver to increase the metabolism of liver fat. The most common side effects of treatment are nausea and diarrhea. Gallstones and gallbladder inflammation also developed in some patients in the trials. It can also interact with other medications such as statins, gemfibrozil (Lopid) and clopidogrel (Plavix), so be sure that your doctor has a full list of your medications before prescribing resmetirom (Rezdiffra). A liver biopsy is not essential to start resmetirom (Rezdiffra) because other tests that can show the accumulation of liver fibrosis such as Fibroscan or other measures of liver stiffness can provide the necessary information. Resmetirom (Rezdiffra) is not for people who do not have evidence of significant liver fibrosis.
Weight loss surgery
Weight loss surgery also called bariatric surgery been shown to be an effective treatment for nonalcoholic fatty liver disease (NAFLD) by improving overall liver health via facilitating weight loss, improving insulin sensitivity, and subsiding inflammation 92, 93. Roux-en-Y gastric bypass (RYGB) and laparoscopic sleeve gastrectomy are the most prevalent weight loss surgical procedures, which lead to significant weight loss and metabolic health improvements 94.
Several research studies have investigated the impact of weight loss surgery in NAFLD and have shown positive results. Studies have indicated that weight loss surgery resulted in significant improvements in liver enzymes and histology, with a decrease in liver fat and fibrosis. Results from two meta-analyses have shown that treatment of NAFLD using weight loss surgery resulted in a biopsy-confirmed resolution of steatosis (56%-66%), inflammation (45%-50%), ballooning degeneration (49%-76%), and fibrosis (25%-40%), as well as showing a decrease in NAS scoring 94, 95, 96. Weight loss surgery has therefore proven to be effective in ameliorating NAFLD, however, it is important to clarify which type of weight loss surgery is most effective. A study by Baldwin et al 97 compared Roux-en-Y gastric bypass (RYGB) and laparoscopic sleeve gastrectomy against its effectiveness at improving AST and ALT concentration, NAS and NAFLD fibrosis score. Overall, both procedures reduce AST and ALT levels, however, laparoscopic sleeve gastrectomy showed slightly more favourable results 93. Another study has shown NAS scoring reduced significantly in patients who underwent both surgery types 12-mo after the surgery 93. Roux-en-Y gastric bypass patients had a more significantly decreased steatosis and superior improvement in plasma lipid profile 98. Furthermore, weight loss surgery has been demonstrated to lower the risk of liver-related complications and death in individuals with NAFLD. Weight loss surgery can therefore be considered as a promising treatment option for those with NAFLD who are overweight or obese.
Protect your liver
Don’t do things that put extra stress on your liver:
- Avoid drinking alcohol.
- Take medications and over-the-counter drugs only as instructed by your doctor.
- Be cautious about taking dietary supplements. Certain vitamins and minerals – like vitamins A, iron, and niacin – can be harmful to your liver in higher doses than necessary or prescribed.
Check with your doctor before trying any herbal remedies. Just because a product is called “natural,” does not mean it’s safe. - Get vaccinated for hepatitis A and hepatitis B. If you get hepatitis A or B, along with fatty liver, it’s more likely to lead to liver failure.
- Manage your diabetes. Follow your doctor’s advice to manage your diabetes. Take your medicines as told by your care team and watch your blood sugar closely.
- Lower your cholesterol and blood pressure. Improve your cholesterol levels and blood pressure if they are high. A healthy diet, exercise and medicines can help keep your cholesterol, triglycerides and blood pressure at healthy levels.
Vitamin E, which is an antioxidant, in theory could help protect the liver by reducing or canceling out the damage caused by inflammation. But more research is needed. Some evidence suggests vitamin E supplements may be helpful for people with liver damage due to NAFLD and NASH who don’t have type 2 diabetes. Researchers in one study found that a daily dose of the natural form of vitamin E – the kind that comes from food sources and isn’t made in a laboratory – improved NASH in study participants overall by reducing fat and inflammation although not scarring. This medication is not for everyone and may have potential side effects as well. Vitamin E has been linked with a slightly increased risk of heart disease and prostate cancer. Discuss the potential benefits and side effects of vitamin E with your doctor.
Some studies suggest that coffee may benefit the liver by reducing the risk of liver diseases like NAFLD and lowering the chance of scarring. It’s not yet clear how coffee may prevent liver damage. But certain compounds in coffee are thought to lower inflammation and slow scar tissue growth. If you already drink coffee, these results may make you feel better about your morning cup. But if you don’t already drink coffee, this probably isn’t a good reason to start. Discuss the possible benefits of coffee with your health care team.
Non-alcoholic fatty liver disease prognosis
Patients with nonalcoholic fatty liver disease (NAFLD) have a decreased survival as compared to the general population 99. Individuals with non-alcoholic fatty liver disease (NAFLD) exhibit increased mortality rates when compared to the general population 100, 101, 65. People with non-alcoholic fatty liver disease (NAFLD) have a high risk of mortality from cardiovascular causes as these patients have metabolic derangements, followed by cancers and only then liver disease 99, 102, 100, 65. Cardiovascular causes of mortality are higher in non-alcoholic fatty liver disease (NAFLD) patients than liver causes 103, 104. NAFLD patients die 9 times more often from liver disease than the general population 102.
NAFLD is a slowly progressive disease 105, 106; simple faty liver (steatosis) is reversible and non-progressive, whereas nonalcoholic steatohepatitis (NASH) can progress to cirrhosis 104. The main risk factors for having advanced liver fibrosis are older age 107, 108, presence of obesity and central obesity 109, as well as type 2 diabetes 110 and hypertension 111. In a 13 year follow-up study by Ekstedt et al 106 the progression of cirrhosis were seen in 41% subjects. These subjects more often had a weight gain exceeding 5 kg, they were more insulin resistant and they exhibited more pronounced hepatic fatty infiltration at follow-up 106. Most NAFLD patients will develop diabetes or impaired glucose tolerance in the long term 106. A meta-analysis on 17 studies done by White et al. 112 showed that in cohorts of NAFLD or NASH with few or no cases of cirrhosis, the risk of developing liver cancer (hepatocellular carcinoma [HCC]) was minimal at 0 to 3% over a 20 year follow up, and in cohorts with NASH with cirrhosis, the risk was high at 2.4 to 12.8% after 3 to 12 years of follow up. In fact, NAFLD-associated cirrhosis accounts for 15%-30% of cases of hepatocellular carcinoma (HCC) 113. Patients with NAFLD can also progress to hepatocellular carcinoma (HCC), even without cirrhosis 114. Some cases of hepatocellular carcinoma (HCC) were reported in patients with simple steatosis, without NASH or fibrosis 115, 116.
- Francque SM, Marchesini G, Kautz A, Walmsley M, Dorner R, Lazarus JV, Zelber-Sagi S, Hallsworth K, Busetto L, Frühbeck G, Dicker D, Woodward E, Korenjak M, Willemse J, Koek GH, Vinker S, Ungan M, Mendive JM, Lionis C. Non-alcoholic fatty liver disease: A patient guideline. JHEP Rep. 2021 Sep 17;3(5):100322. doi: 10.1016/j.jhepr.2021.100322[↩]
- Sayiner M, Koenig A, Henry L, Younossi ZM. Epidemiology of Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis in the United States and the Rest of the World. Clin Liver Dis. 2016 May;20(2):205-14. doi: 10.1016/j.cld.2015.10.001[↩][↩]
- Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016 Jul;64(1):73-84. doi: 10.1002/hep.28431[↩]
- Ge X, Zheng L, Wang M, Du Y, Jiang J. Prevalence trends in non-alcoholic fatty liver disease at the global, regional and national levels, 1990-2017: a population-based observational study. BMJ Open. 2020 Aug 3;10(8):e036663. doi: 10.1136/bmjopen-2019-036663[↩][↩]
- Younossi Z, Tacke F, Arrese M, Chander Sharma B, Mostafa I, Bugianesi E, Wai-Sun Wong V, Yilmaz Y, George J, Fan J, Vos MB. Global Perspectives on Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis. Hepatology. 2019 Jun;69(6):2672-2682. doi: 10.1002/hep.30251[↩]
- Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, George J, Bugianesi E. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018 Jan;15(1):11-20. doi: 10.1038/nrgastro.2017.109[↩]
- Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018 Jan;67(1):123-133. doi: 10.1002/hep.29466[↩]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016 Apr 9;387(10027):1513-1530. doi: 10.1016/S0140-6736(16)00618-8. Epub 2016 Apr 6. Erratum in: Lancet. 2017 Feb 4;389(10068):e2. doi: 10.1016/S0140-6736(16)32060-8[↩]
- Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014 Aug 30;384(9945):766-81. doi: 10.1016/S0140-6736(14)60460-8. Epub 2014 May 29. Erratum in: Lancet. 2014 Aug 30;384(9945):746.[↩]
- Le MH, Yeo YH, Li X, Li J, et al. 2019 Global NAFLD Prevalence: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2022 Dec;20(12):2809-2817.e28. doi: 10.1016/j.cgh.2021.12.002[↩][↩]
- Huang DQ, El-Serag HB, Loomba R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2021 Apr;18(4):223-238. doi: 10.1038/s41575-020-00381-6[↩]
- Alexander M, Loomis AK, Fairburn-Beech J, van der Lei J, Duarte-Salles T, Prieto-Alhambra D, Ansell D, Pasqua A, Lapi F, Rijnbeek P, Mosseveld M, Avillach P, Egger P, Kendrick S, Waterworth DM, Sattar N, Alazawi W. Real-world data reveal a diagnostic gap in non-alcoholic fatty liver disease. BMC Med. 2018 Aug 13;16(1):130. doi: 10.1186/s12916-018-1103-x[↩]
- Teng ML, Ng CH, Huang DQ, Chan KE, Tan DJ, Lim WH, Yang JD, Tan E, Muthiah MD. Global incidence and prevalence of nonalcoholic fatty liver disease. Clin Mol Hepatol. 2023 Feb;29(Suppl):S32-S42. doi: 10.3350/cmh.2022.0365[↩]
- Mitra S, De A, Chowdhury A. Epidemiology of non-alcoholic and alcoholic fatty liver diseases. Transl Gastroenterol Hepatol. 2020 Apr 5;5:16. doi: 10.21037/tgh.2019.09.08[↩]
- Lu FB, Hu ED, Xu LM, Chen L, Wu JL, Li H, Chen DZ, Chen YP. The relationship between obesity and the severity of non-alcoholic fatty liver disease: systematic review and meta-analysis. Expert Rev Gastroenterol Hepatol. 2018 May;12(5):491-502. doi: 10.1080/17474124.2018.1460202[↩]
- Ayonrinde OT, Oddy WH, Adams LA, Mori TA, Beilin LJ, de Klerk N, Olynyk JK. Infant nutrition and maternal obesity influence the risk of non-alcoholic fatty liver disease in adolescents. J Hepatol. 2017 Sep;67(3):568-576. doi: 10.1016/j.jhep.2017.03.029[↩]
- Cusi K, Sanyal AJ, Zhang S, Hartman ML, Bue-Valleskey JM, Hoogwerf BJ, Haupt A. Non-alcoholic fatty liver disease (NAFLD) prevalence and its metabolic associations in patients with type 1 diabetes and type 2 diabetes. Diabetes Obes Metab. 2017 Nov;19(11):1630-1634. doi: 10.1111/dom.12973[↩]
- Zelber-Sagi S, Ivancovsky-Wajcman D, Fliss Isakov N, Webb M, Orenstein D, Shibolet O, Kariv R. High red and processed meat consumption is associated with non-alcoholic fatty liver disease and insulin resistance. J Hepatol. 2018 Jun;68(6):1239-1246. doi: 10.1016/j.jhep.2018.01.015[↩]
- Mitchell T, McKinnon E, Ayonrinde O, Adams LA, Trinder D, Chua ACG, Newton RU, Straker L, Olynyk JK. Decreased Physical Working Capacity in Adolescents With Nonalcoholic Fatty Liver Disease Associates With Reduced Iron Availability. Clin Gastroenterol Hepatol. 2020 Jun;18(7):1584-1591. doi: 10.1016/j.cgh.2019.10.017[↩]
- Stefan N, Häring HU, Cusi K. Non-alcoholic fatty liver disease: causes, diagnosis, cardiometabolic consequences, and treatment strategies. Lancet Diabetes Endocrinol. 2019 Apr;7(4):313-324. doi: 10.1016/S2213-8587(18)30154-2[↩]
- Stefan N, Kantartzis K, Häring HU. Causes and metabolic consequences of Fatty liver. Endocr Rev. 2008 Dec;29(7):939-60. doi: 10.1210/er.2008-0009[↩][↩]
- Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi:10.1002/hep.28431[↩][↩][↩][↩]
- Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–357. doi:10.1002/hep.29367[↩][↩][↩][↩][↩][↩][↩][↩]
- Nonalcoholic Fatty Liver Disease (NAFLD) & NASH. https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash[↩][↩][↩]
- Nonalcoholic fatty liver disease. https://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/symptoms-causes/syc-20354567[↩][↩]
- Cotter TG, Rinella M. Nonalcoholic fatty liver disease 2020: the state of the disease. Gastroenterology. 2020;158(7):1851–1864. doi:10.1053/j.gastro.2020.01.052[↩]
- Machado M, Marques-Vidal P, Cortez-Pinto H. Hepatic histology in obese patients undergoing bariatric surgery. Journal of Hepatology. 2006;45(4):600–606. doi: 10.1016/j.jhep.2006.06.013[↩]
- Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118(4):1388–1393. doi: 10.1542/peds.2006-1212[↩]
- Golabi P, Paik J, Hwang JP, Wang S, Lee HM, Younossi ZM. Prevalence and outcomes of non-alcoholic fatty liver disease (NAFLD) among Asian American adults in the United States. Liver International. 2019;39(4):748–757. doi:10.1111/liv.14038[↩][↩]
- Khoonsari M, Mohammad Hosseini Azar M, Ghavam R, Hatami K, Asobar M, Gholami A, Rajabi A, Safarnezhad Tameshkel F, Amirkalali B, Sohrabi M. Clinical Manifestations and Diagnosis of Nonalcoholic Fatty Liver Disease. Iran J Pathol. 2017 Spring;12(2):99-105. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5831064[↩]
- Petagine L, Zariwala MG, Patel VB. Non-alcoholic fatty liver disease: Immunological mechanisms and current treatments. World J Gastroenterol. 2023 Aug 28;29(32):4831-4850. doi: 10.3748/wjg.v29.i32.4831[↩][↩][↩][↩][↩][↩][↩]
- Mantovani A, Dalbeni A. Treatments for NAFLD: State of Art. Int J Mol Sci. 2021 Feb 26;22(5):2350. doi: 10.3390/ijms22052350[↩][↩]
- Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, Torres-Gonzalez A, Gra-Oramas B, Gonzalez-Fabian L, Friedman SL, Diago M, Romero-Gomez M. Weight Loss Through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology. 2015 Aug;149(2):367-78.e5; quiz e14-5. doi: 10.1053/j.gastro.2015.04.005[↩][↩][↩][↩]
- Moore MP, Cunningham RP, Dashek RJ, Mucinski JM, Rector RS. A Fad too Far? Dietary Strategies for the Prevention and Treatment of NAFLD. Obesity (Silver Spring). 2020 Oct;28(10):1843-1852. doi: 10.1002/oby.22964[↩][↩][↩][↩]
- Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ; American Gastroenterological Association; American Association for the Study of Liver Diseases; American College of Gastroenterologyh. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012 Jun;142(7):1592-609. doi: 10.1053/j.gastro.2012.04.001 Erratum in: Gastroenterology. 2012 Aug;143(2):503.[↩][↩]
- Pouwels S, Sakran N, Graham Y, Leal A, Pintar T, Yang W, Kassir R, Singhal R, Mahawar K, Ramnarain D. Non-alcoholic fatty liver disease (NAFLD): a review of pathophysiology, clinical management and effects of weight loss. BMC Endocr Disord. 2022 Mar 14;22(1):63. doi: 10.1186/s12902-022-00980-1[↩][↩][↩]
- Wong VW, Chan RS, Wong GL, Cheung BH, Chu WC, Yeung DK, Chim AM, Lai JW, Li LS, Sea MM, Chan FK, Sung JJ, Woo J, Chan HL. Community-based lifestyle modification programme for non-alcoholic fatty liver disease: a randomized controlled trial. J Hepatol. 2013 Sep;59(3):536-42. doi: 10.1016/j.jhep.2013.04.013[↩][↩]
- Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980 Jul;55(7):434-8.[↩][↩][↩][↩][↩]
- Anderson, M.L. (2006), Treating NASH. Journal of Gastroenterology and Hepatology, 21: 14-14. https://doi.org/10.1111/j.1440-1746.2005.04216.x[↩]
- CINAR, K., COBAN, S., IDILMAN, R., TUZUN, A., SARIOGLU, M., BEKTAS, M., ERDEN, E., BOZKAYA, H. and OZDEN, A. (2006), Long-term prognosis of nonalcoholic fatty liver disease: Is pharmacological therapy actually necessary?. Journal of Gastroenterology and Hepatology, 21: 169-173. https://doi.org/10.1111/j.1440-1746.2005.04221.x[↩]
- Neuschwander-Tetri BA. Fatty liver and nonalcoholic steatohepatitis. Clin Cornerstone. 2001;3(6):47-57. doi: 10.1016/s1098-3597(01)90078-x[↩]
- Neuschwander-Tetri BA. Evolving pathophysiologic concepts in nonalcoholic steatohepatitis. Curr Gastroenterol Rep. 2002 Feb;4(1):31-6. doi: 10.1007/s11894-002-0035-x[↩][↩]
- Drew L. Fatty liver disease: turning the tide. Nature. 2017 Oct 11;550(7675):S101. https://doi.org/10.1038/550S101a[↩]
- Nonalcoholic Fatty Liver Disease (NAFLD). https://liverfoundation.org/liver-diseases/fatty-liver-disease/nonalcoholic-fatty-liver-disease-nafld[↩]
- Nonalcoholic Steatohepatitis (NASH). https://liverfoundation.org/liver-diseases/fatty-liver-disease/nonalcoholic-steatohepatitis-nash[↩]
- Rabelo ACS, Andrade AKL, Costa DC. The Role of Oxidative Stress in Alcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis of Preclinical Studies. Nutrients. 2024 Apr 15;16(8):1174. doi: 10.3390/nu16081174[↩][↩]
- Salete-Granado D., Carbonell C., Puertas-Miranda D., Vega-Rodríguez V.J., García-Macia M., Herrero A.B., Marcos M. Autophagy, Oxidative Stress, and Alcoholic Liver Disease: A Systematic Review and Potential Clinical Applications. Antioxidants. 2023;12:1425. doi: 10.3390/antiox12071425[↩][↩][↩]
- Zima T., Fialová L., Mestek O., Janebová M., Crkovská J., Malbohan I., Stípek S., Mikulíková L., Popov P. Oxidative stress, metabolism of ethanol and alcohol-related diseases. J. Biomed. Sci. 2001;8:59–70. doi: 10.1007/BF02255972[↩]
- You M., Fischer M., Deeg M.A., Crabb D.W. Ethanol Induces Fatty Acid Synthesis Pathways by Activation of Sterol Regulatory Element-Binding Protein (SREBP) J. Biol. Chem. 2002;277:29342–29347. doi: 10.1074/jbc.M202411200[↩][↩]
- Tan H.K., Yates E., Lilly K., Dhanda A.D. Oxidative Stress in Alcohol-Related Liver Disease. World J. Hepatol. 2020;12:332–349. doi: 10.4254/wjh.v12.i7.332[↩]
- Diesinger T., Buko V., Lautwein A., Dvorsky R., Belonovskaya E., Lukivskaya O., Naruta E., Kirko S., Andreev V., Buckert D. Drug Targeting CYP2E1 for the Treatment of Early-Stage Alcoholic Steatohepatitis. PLoS ONE. 2020;15:e0235990. doi: 10.1371/journal.pone.0235990[↩]
- Lívero F.A.R., Acco A. Molecular Basis of Alcoholic Fatty Liver Disease: From Incidence to Treatment. Hepatol. Res. 2016;46:111–123. doi: 10.1111/hepr.12594[↩]
- Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, Bouvard V, Altieri A, Cogliano V; WHO International Agency for Research on Cancer Monograph Working Group. Carcinogenicity of alcoholic beverages. Lancet Oncol. 2007 Apr;8(4):292-3. doi: 10.1016/s1470-2045(07)70099-2[↩][↩]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Alcohol Drinking. Lyon (FR): International Agency for Research on Cancer; 1988. (IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 44.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK531657[↩]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Personal Habits and Indoor Combustions. Lyon (FR): International Agency for Research on Cancer; 2012. (IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 100E.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK304391[↩]
- No level of alcohol consumption is safe for our health. https://www.who.int/europe/news/item/04-01-2023-no-level-of-alcohol-consumption-is-safe-for-our-health[↩][↩]
- Gapstur SM, Bouvard V, Nethan ST, Freudenheim JL, Abnet CC, English DR, Rehm J, Balbo S, Buykx P, Crabb D, Conway DI, Islami F, Lachenmeier DW, McGlynn KA, Salaspuro M, Sawada N, Terry MB, Toporcov T, Lauby-Secretan B. The IARC Perspective on Alcohol Reduction or Cessation and Cancer Risk. N Engl J Med. 2023 Dec 28;389(26):2486-2494. doi: 10.1056/NEJMsr2306723[↩]
- Yoo JE, Han K, Shin DW, Kim D, Kim BS, Chun S, Jeon KH, Jung W, Park J, Park JH, Choi KS, Kim JS. Association Between Changes in Alcohol Consumption and Cancer Risk. JAMA Netw Open. 2022 Aug 1;5(8):e2228544. doi: 10.1001/jamanetworkopen.2022.28544[↩]
- Islami F, Goding Sauer A, Miller KD, et al.. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68(1):31-54. doi: 10.3322/caac.21440[↩]
- Connor J. Alcohol consumption as a cause of cancer. Addiction. 2017;112(2):222-228. doi: 10.1111/add.13477[↩]
- Ahmad Kiadaliri A, Jarl J, Gavriilidis G, Gerdtham UG. Alcohol drinking cessation and the risk of laryngeal and pharyngeal cancers: a systematic review and meta-analysis. PLoS One. 2013;8(3):e58158. doi: 10.1371/journal.pone.0058158[↩]
- Jarl J, Gerdtham UG. Time pattern of reduction in risk of oesophageal cancer following alcohol cessation: a meta-analysis. Addiction. 2012;107(7):1234-1243. doi: 10.1111/j.1360-0443.2011.03772.x[↩]
- Heckley GA, Jarl J, Asamoah BO, G-Gerdtham U. How the risk of liver cancer changes after alcohol cessation: a review and meta-analysis of the current literature. BMC Cancer. 2011;11:446. doi: 10.1186/1471-2407-11-446[↩]
- GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020 Oct 17;396(10258):1223-1249. doi: 10.1016/S0140-6736(20)30752-2[↩]
- Kudaravalli P, John S. Nonalcoholic Fatty Liver. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541033[↩][↩][↩][↩][↩]
- Kim CH, Younossi ZM. Nonalcoholic fatty liver disease: a manifestation of the metabolic syndrome. Cleve Clin J Med. 2008 Oct;75(10):721-8. doi: 10.3949/ccjm.75.10.721[↩]
- Rector RS, Thyfault JP, Wei Y, Ibdah JA. Non-alcoholic fatty liver disease and the metabolic syndrome: an update. World J Gastroenterol. 2008 Jan 14;14(2):185-92. doi: 10.3748/wjg.14.185[↩]
- Brennan PN, Elsharkawy AM, Kendall TJ, Loomba R, Mann DA, Fallowfield JA. Antifibrotic therapy in nonalcoholic steatohepatitis: time for a human-centric approach. Nat Rev Gastroenterol Hepatol. 2023 Oct;20(10):679-688. doi: 10.1038/s41575-023-00796-x[↩]
- Kim K, Kim KH. Targeting of Secretory Proteins as a Therapeutic Strategy for Treatment of Nonalcoholic Steatohepatitis (NASH). Int J Mol Sci. 2020 Mar 26;21(7):2296. doi: 10.3390/ijms21072296[↩]
- PNPLA3 gene. https://medlineplus.gov/genetics/gene/pnpla3[↩]
- Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999 Sep;94(9):2467-74. doi: 10.1111/j.1572-0241.1999.01377.x[↩][↩]
- Brown GT, Kleiner DE. Histopathology of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Metabolism. 2016 Aug;65(8):1080-6. doi: 10.1016/j.metabol.2015.11.008[↩][↩]
- Takahashi Y, Fukusato T. Histopathology of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J Gastroenterol. 2014 Nov 14;20(42):15539-48. doi: 10.3748/wjg.v20.i42.15539[↩][↩]
- Nassir F, Rector RS, Hammoud GM, Ibdah JA. Pathogenesis and Prevention of Hepatic Steatosis. Gastroenterol Hepatol (N Y). 2015 Mar;11(3):167-75. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4836586[↩][↩]
- Qayyum A, Nystrom M, Noworolski SM, Chu P, Mohanty A, Merriman R. MRI steatosis grading: development and initial validation of a color mapping system. AJR Am J Roentgenol. 2012 Mar;198(3):582-8. doi: 10.2214/AJR.11.6729[↩][↩]
- Hardy T, Oakley F, Anstee QM, Day CP. Nonalcoholic Fatty Liver Disease: Pathogenesis and Disease Spectrum. Annu Rev Pathol. 2016 May 23;11:451-96. doi: 10.1146/annurev-pathol-012615-044224[↩]
- Heyens LJM, Busschots D, Koek GH, Robaeys G, Francque S. Liver Fibrosis in Non-alcoholic Fatty Liver Disease: From Liver Biopsy to Non-invasive Biomarkers in Diagnosis and Treatment. Front Med (Lausanne). 2021 Apr 14;8:615978. doi: 10.3389/fmed.2021.615978[↩][↩]
- El-Kamary SS, Mohamed MM, El-Raziky M, Shardell MD, Shaker OG, ElAkel WA, Esmat G. Liver fibrosis staging through a stepwise analysis of non-invasive markers (FibroSteps) in patients with chronic hepatitis C infection. Liver Int. 2013 Aug;33(7):982-90. doi: 10.1111/liv.12139[↩]
- Bataller R, Brenner DA. Liver fibrosis. J Clin Invest. 2005 Feb;115(2):209-18. doi: 10.1172/JCI24282. Erratum in: J Clin Invest. 2005 Apr;115(4):1100. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC546435[↩]
- Shetty A, Jun Yum J, Saab S. The Gastroenterologist’s Guide to Preventive Management of Compensated Cirrhosis. Gastroenterol Hepatol (N Y). 2019 Aug;15(8):423-430. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6771034[↩][↩]
- Piazzolla VA, Mangia A. Noninvasive Diagnosis of NAFLD and NASH. Cells. 2020 Apr 17;9(4):1005. doi: 10.3390/cells9041005[↩]
- Kumar R, Teo EK, How CH, Wong TY, Ang TL. A practical clinical approach to liver fibrosis. Singapore Med J. 2018 Dec;59(12):628-633. doi: 10.11622/smedj.2018145[↩][↩]
- Watanabe M, Tozzi R, Risi R, Tuccinardi D, Mariani S, Basciani S, Spera G, Lubrano C, Gnessi L. Beneficial effects of the ketogenic diet on nonalcoholic fatty liver disease: A comprehensive review of the literature. Obes Rev. 2020 Aug;21(8):e13024. doi: 10.1111/obr.13024[↩][↩]
- Schugar RC, Crawford PA. Low-carbohydrate ketogenic diets, glucose homeostasis, and nonalcoholic fatty liver disease. Curr Opin Clin Nutr Metab Care. 2012 Jul;15(4):374-80. doi: 10.1097/MCO.0b013e3283547157[↩]
- Cooper ID, Brookler KH, Kyriakidou Y, Elliott BT, Crofts CAP. Metabolic Phenotypes and Step by Step Evolution of Type 2 Diabetes: A New Paradigm. Biomedicines. 2021 Jul 9;9(7):800. doi: 10.3390/biomedicines9070800[↩]
- Luukkonen PK, Dufour S, Lyu K, Zhang XM, Hakkarainen A, Lehtimäki TE, Cline GW, Petersen KF, Shulman GI, Yki-Järvinen H. Effect of a ketogenic diet on hepatic steatosis and hepatic mitochondrial metabolism in nonalcoholic fatty liver disease. Proc Natl Acad Sci U S A. 2020 Mar 31;117(13):7347-7354. doi: 10.1073/pnas.1922344117[↩][↩]
- Achanta LB, Rae CD. β-Hydroxybutyrate in the Brain: One Molecule, Multiple Mechanisms. Neurochem Res. 2017 Jan;42(1):35-49. doi: 10.1007/s11064-016-2099-2[↩]
- Wu Y, Teng Y, Zhang C, Pan Y, Zhang Q, Zhu X, Liu N, Su X, Lin J. The ketone body β-hydroxybutyrate alleviates CoCrMo alloy particles induced osteolysis by regulating NLRP3 inflammasome and osteoclast differentiation. J Nanobiotechnology. 2022 Mar 9;20(1):120. doi: 10.1186/s12951-022-01320-0[↩]
- Miller VJ, Villamena FA, Volek JS. Nutritional Ketosis and Mitohormesis: Potential Implications for Mitochondrial Function and Human Health. J Nutr Metab. 2018 Feb 11;2018:5157645. doi: 10.1155/2018/5157645[↩]
- National Guideline Centre (UK). Non-Alcoholic Fatty Liver Disease: Assessment and Management. London: National Institute for Health and Care Excellence (NICE); 2016 Jul. (NICE Guideline, No. 49.) 17, Pharmacological interventions. Available from: https://www.ncbi.nlm.nih.gov/books/NBK384725[↩]
- Harrison SA, Bedossa P, Guy CD, et al. MAESTRO-NASH Investigators. A Phase 3, Randomized, Controlled Trial of Resmetirom in NASH with Liver Fibrosis. N Engl J Med. 2024 Feb 8;390(6):497-509. doi: 10.1056/NEJMoa2309000[↩]
- O’Brien PE, Hindle A, Brennan L, Skinner S, Burton P, Smith A, Crosthwaite G, Brown W. Long-Term Outcomes After Bariatric Surgery: a Systematic Review and Meta-analysis of Weight Loss at 10 or More Years for All Bariatric Procedures and a Single-Centre Review of 20-Year Outcomes After Adjustable Gastric Banding. Obes Surg. 2019 Jan;29(1):3-14. doi: 10.1007/s11695-018-3525-0[↩]
- Głuszyńska P, Lemancewicz D, Dzięcioł JB, Razak Hady H. Non-Alcoholic Fatty Liver Disease (NAFLD) and Bariatric/Metabolic Surgery as Its Treatment Option: A Review. J Clin Med. 2021 Dec 7;10(24):5721. doi: 10.3390/jcm10245721[↩][↩][↩]
- Lee KC, Wu PS, Lin HC. Pathogenesis and treatment of non-alcoholic steatohepatitis and its fibrosis. Clin Mol Hepatol. 2023 Jan;29(1):77-98. doi: 10.3350/cmh.2022.0237[↩][↩]
- Lee Y, Doumouras AG, Yu J, Brar K, Banfield L, Gmora S, Anvari M, Hong D. Complete Resolution of Nonalcoholic Fatty Liver Disease After Bariatric Surgery: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2019 May;17(6):1040-1060.e11. doi: 10.1016/j.cgh.2018.10.017[↩]
- Fakhry TK, Mhaskar R, Schwitalla T, Muradova E, Gonzalvo JP, Murr MM. Bariatric surgery improves nonalcoholic fatty liver disease: a contemporary systematic review and meta-analysis. Surg Obes Relat Dis. 2019 Mar;15(3):502-511. doi: 10.1016/j.soard.2018.12.002[↩]
- Baldwin D, Chennakesavalu M, Gangemi A. Systematic review and meta-analysis of Roux-en-Y gastric bypass against laparoscopic sleeve gastrectomy for amelioration of NAFLD using four criteria. Surg Obes Relat Dis. 2019 Dec;15(12):2123-2130. doi: 10.1016/j.soard.2019.09.060[↩]
- Pedersen JS, Rygg MO, Serizawa RR, Kristiansen VB, Albrechtsen NJW, Gluud LL, Madsbad S, Bendtsen F. Effects of Roux-en-Y Gastric Bypass and Sleeve Gastrectomy on Non-Alcoholic Fatty Liver Disease: A 12-Month Follow-Up Study with Paired Liver Biopsies. J Clin Med. 2021 Aug 24;10(17):3783. doi: 10.3390/jcm10173783[↩]
- Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005 Jul;129(1):113-21. doi: 10.1053/j.gastro.2005.04.014[↩][↩]
- Rafiq N, Bai C, Fang Y, Srishord M, McCullough A, Gramlich T, Younossi ZM. Long-term follow-up of patients with nonalcoholic fatty liver. Clin Gastroenterol Hepatol. 2009 Feb;7(2):234-8. doi: 10.1016/j.cgh.2008.11.005[↩][↩]
- Söderberg C, Stål P, Askling J, Glaumann H, Lindberg G, Marmur J, Hultcrantz R. Decreased survival of subjects with elevated liver function tests during a 28-year follow-up. Hepatology. 2010 Feb;51(2):595-602. doi: 10.1002/hep.23314[↩]
- Ong JP, Pitts A, Younossi ZM. Increased overall mortality and liver-related mortality in non-alcoholic fatty liver disease. J Hepatol. 2008 Oct;49(4):608-12. doi: 10.1016/j.jhep.2008.06.018[↩][↩]
- Machado MV, Cortez-Pinto H. Non-alcoholic fatty liver disease: what the clinician needs to know. World J Gastroenterol. 2014 Sep 28;20(36):12956-80. doi: 10.3748/wjg.v20.i36.12956[↩]
- Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med. 2011 Dec;43(8):617-49. doi: 10.3109/07853890.2010.518623[↩][↩]
- Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999 Jun;116(6):1413-9. doi: 10.1016/s0016-5085(99)70506-8[↩]
- Ekstedt M, Franzén LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, Kechagias S. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006 Oct;44(4):865-73. doi: 10.1002/hep.21327[↩][↩][↩][↩]
- Angulo P, Keach JC, Batts KP, Lindor KD. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology. 1999 Dec;30(6):1356-62. doi: 10.1002/hep.510300604[↩]
- Noureddin M, Yates KP, Vaughn IA, Neuschwander-Tetri BA, Sanyal AJ, McCullough A, Merriman R, Hameed B, Doo E, Kleiner DE, Behling C, Loomba R; NASH CRN. Clinical and histological determinants of nonalcoholic steatohepatitis and advanced fibrosis in elderly patients. Hepatology. 2013 Nov;58(5):1644-54. doi: 10.1002/hep.26465[↩]
- Wong VW, Wong GL, Choi PC, Chan AW, Li MK, Chan HY, Chim AM, Yu J, Sung JJ, Chan HL. Disease progression of non-alcoholic fatty liver disease: a prospective study with paired liver biopsies at 3 years. Gut. 2010 Jul;59(7):969-74. doi: 10.1136/gut.2009.205088[↩]
- Nakahara T, Hyogo H, Yoneda M, Sumida Y, Eguchi Y, Fujii H, Ono M, Kawaguchi T, Imajo K, Aikata H, Tanaka S, Kanemasa K, Fujimoto K, Anzai K, Saibara T, Sata M, Nakajima A, Itoh Y, Chayama K, Okanoue T; Japan Study Group of Nonalcoholic Fatty Liver Disease. Type 2 diabetes mellitus is associated with the fibrosis severity in patients with nonalcoholic fatty liver disease in a large retrospective cohort of Japanese patients. J Gastroenterol. 2014 Nov;49(11):1477-84. doi: 10.1007/s00535-013-0911-1[↩]
- Dixon JB, Bhathal PS, O’Brien PE. Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology. 2001 Jul;121(1):91-100. doi: 10.1053/gast.2001.25540[↩]
- White DL, Kanwal F, El-Serag HB. Association between nonalcoholic fatty liver disease and risk for hepatocellular cancer, based on systematic review. Clin Gastroenterol Hepatol. 2012 Dec;10(12):1342-1359.e2. doi: 10.1016/j.cgh.2012.10.001[↩]
- Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol. 2013 Nov;10(11):656-65. doi: 10.1038/nrgastro.2013.183[↩]
- Yasui K, Hashimoto E, Tokushige K, Koike K, Shima T, Kanbara Y, Saibara T, Uto H, Takami S, Kawanaka M, Komorizono Y, Okanoue T; Japan NASH Study Group. Clinical and pathological progression of non-alcoholic steatohepatitis to hepatocellular carcinoma. Hepatol Res. 2012 Aug;42(8):767-73. doi: 10.1111/j.1872-034X.2012.00986.x[↩]
- Guzman G, Brunt EM, Petrovic LM, Chejfec G, Layden TJ, Cotler SJ. Does nonalcoholic fatty liver disease predispose patients to hepatocellular carcinoma in the absence of cirrhosis? Arch Pathol Lab Med. 2008 Nov;132(11):1761-6. doi: 10.5858/132.11.1761[↩]
- Paradis V, Zalinski S, Chelbi E, Guedj N, Degos F, Vilgrain V, Bedossa P, Belghiti J. Hepatocellular carcinomas in patients with metabolic syndrome often develop without significant liver fibrosis: a pathological analysis. Hepatology. 2009 Mar;49(3):851-9. doi: 10.1002/hep.22734[↩]