Contents
What is ocular rosacea
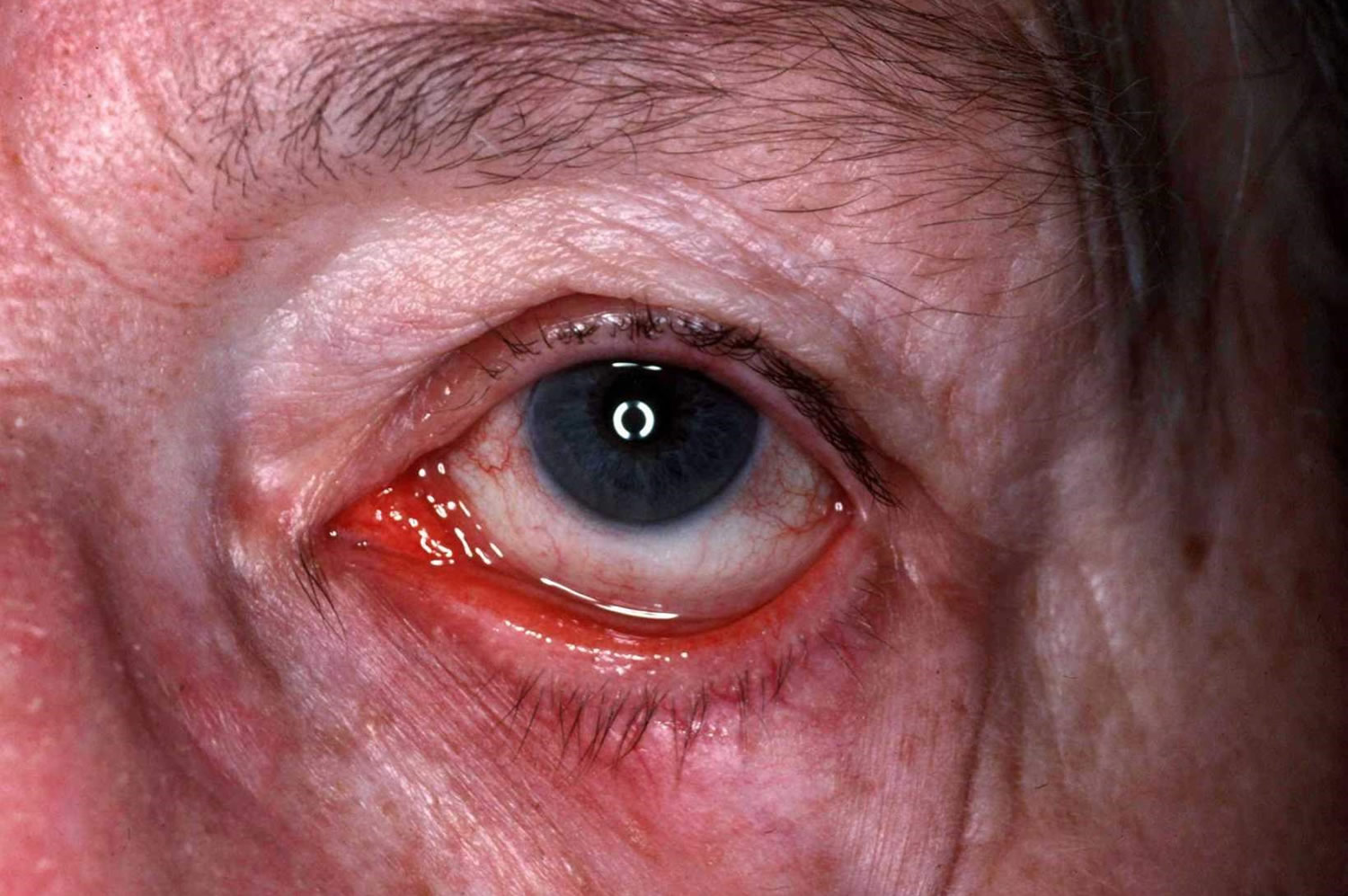
Ocular rosacea is a form of rosacea that involves the eyelids and the front of the eye. Rosacea is a common chronic inflammation of the face skin of unknown cause and without a permanent cure. Rosacea is characterized by mid-facial flushing, redness, prominent vasculature, swelling, papules and/or pustules. Ocular rosacea, which may occur before skin changes with a burning or gritty feeling that may be present as well as reddening of the eyes and lids. Moreover, more than one third of the ocular rosace patients have decreased tear production 1. Sometimes ocular, or eye, rosacea is the first sign that you may later develop the facial type. Both the quality and quantity abnormalities of the tear film can lead to dry eye complaints. The instability of the tear film results in hyperosmolarity of the ocular surface, stimulation of inflammatory cell cytokine release and activation of matrix metalloproteinase leading to damage of the ocular surface 2. Conjunctival hyperemia is common in ocular rosacea, usually found in the interpalpebral zone and worsened by tear film abnormalities. Punctate keratopathy and superficial vascularization of peripheral cornea are also common findings 3.
Ocular rosacea includes:
- Blepharitis
- Conjunctival hyperemia
- Rosacea-associated keratitis
The primary defect in ocular rosacea is the meibomian gland inflammation with dilation and plugging of the gland orifices leading to dysfunction of the glands. Chronic inflammation can lead to hyperkeratinization of the ductal epithelium and loss of secretion 3. These result in blepharitis, meibomitis, chalazia, telangiectasias (dilated small blood vessels on the white part of the eye) and eyelid irregularities. The abnormal lipid secretions from the meibomian glands can lead to qualitative abnormalities of the tear film and rapid evaporation 4.
Ocular rosacea affects adult males and females equally, with one study reporting an average age at presentation of 56 years. It is uncommon in children and generally starts after the age of 30 years.
It usually occurs in patients with existing rosacea but it can be the first sign of the disease. Ocular rosacea tends to occur in patients with facial flushing 5.
There is currently no standard and satisfactory treatment for ocular manifestations of rosacea. Traditional treatments include lid hygiene, oral tetracyclines, steroids and artificial tears. Measures to protect the ocular surface from irritation such as lid hygiene and artificial tears are seldom sufficient. Oral doxycycline has been the mainstay of treatment for ocular rosacea but it seems to provide moderate benefit and to have many side effects limiting its usage 6.
Figure 1. Ocular rosacea
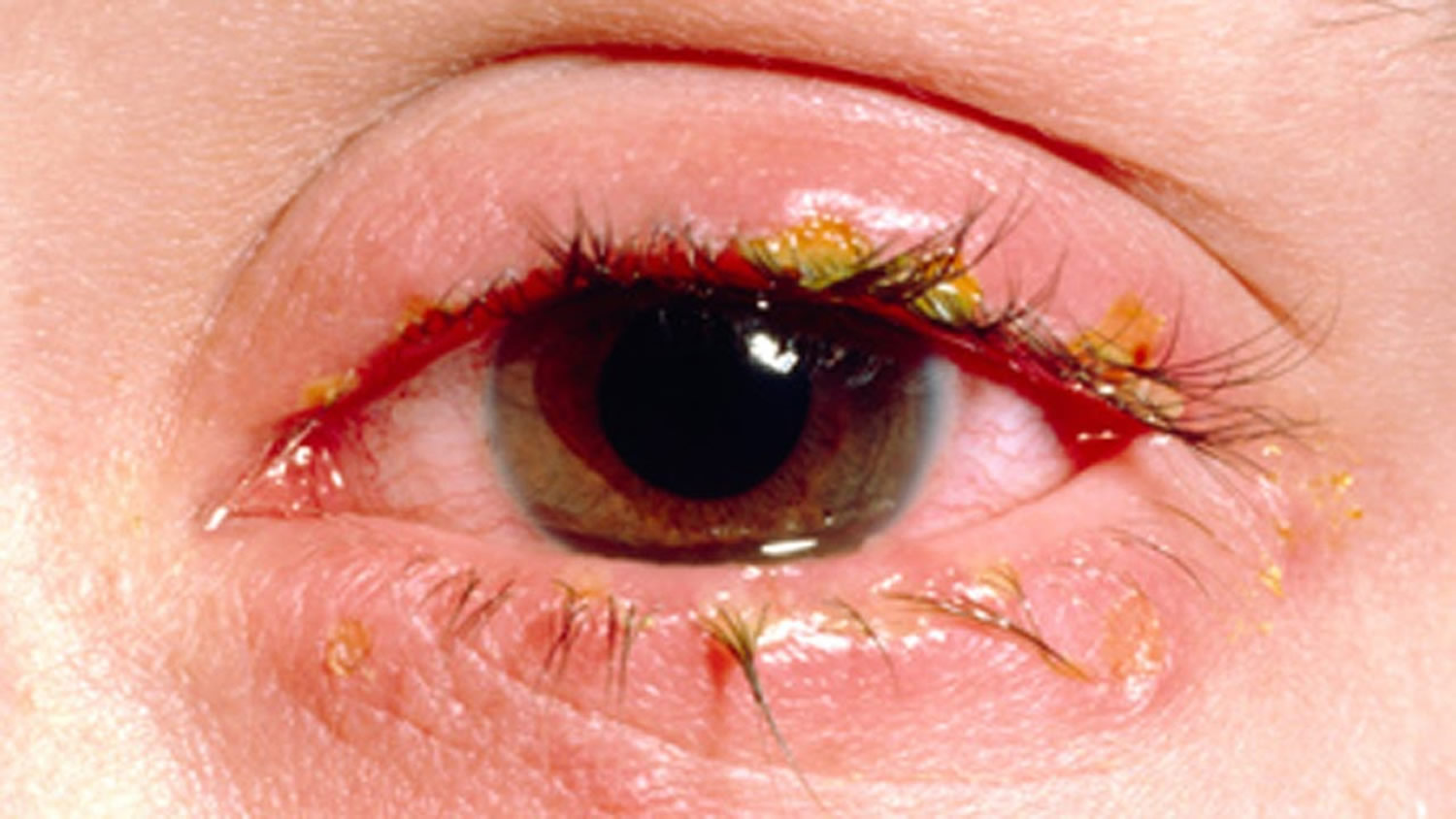
Figure 2. Ocular rosacea note conjunctival hyperaemia
Figure 3. Ocular rosacea
Figure 4. Ocular rosacea blepharitis
What cause ocular rosacea
Ocular rosacea is common in people with rosacea, although you can also have eye rosacea without the skin being involved. Skin rosacea affects more women than men, and ocular rosacea affects men and women equally. Some studies suggest that among people with rosacea, those who blush easily may be more likely to also develop eye symptoms.
The exact cause of ocular rosacea is unknown. However, immunological factors, micro-organisms on the skin surface, and reactive blood vessels are involved.
- Demodex mites, normal inhabitants of eyelash follicles, may stimulate inflammation in ocular rosacea and anterior blepharitis.
- Bacteria may play a role, as ocular rosacea improves with antibiotics. One theory is that bacterial lipases release toxic free fatty acids and glycerides from lipids secreted by meibominan glands.
- The pro-inflammatory cytokine interleukin 1-alpha (IL-1α) increases metallomatrix protein-9 (MMP-9) in the tear fluid. Upregulation of metallomatrix protein-9 damages ocular tissues.
- Heredity
- Environmental factors
- Blocked glands in the eyelids
Obstruction of meibomian glands changes tear film composition leading to:
- Reduced tear film lipid layer
- Tear film instability
- Tear hyperosmolarity
Ocular rosacea triggers
A number of factors can aggravate rosacea, so they can aggravate ocular rosacea, as well. Some of these factors include:
- Hot or spicy foods or beverages
- Alcohol
- Sunlight, wind or temperature extremes
- Certain emotions, such as stress, anger or embarrassment
- Strenuous exercise
- Hot baths or saunas
- Some medications, such as cortisone creams and drugs that dilate blood vessels.
Ocular rosacea complications
Ocular rosacea may affect the surface of your eye (cornea), particularly when you have dry eyes from a deficiency of tears. Corneal complications can lead to visual symptoms. Inflammation of your eyelids (blepharitis) can cause secondary irritation of the cornea from misdirected eyelashes or other complications. Ultimately, corneal complications can lead to vision loss.
Ocular rosacea symptoms
Signs and symptoms of ocular rosacea can precede the skin symptoms of rosacea, develop at the same time, develop later or occur on their own. Ocular rosacea mostly affect the eyelids, conjunctiva and cornea. Rarely, it can involve the iris and sclera.
Symptoms can include:
- Itchy eyes
- Burning or stinging in the eyes
- Red, swollen eyelids
- Increased tears
- Photophobia (light sensitivity)
- Blurred vision
- Redness
- Grittiness or feeling of having a foreign body in the eye or eyes
- Dry eyes
- Inflamed papules
- Dilated small blood vessels on the white part of the eye that are visible when you look in a mirror
- Corneal ulcers
- Red eye
The severity of ocular rosacea symptoms don’t always match the severity of skin symptoms.
Eyelid and conjunctiva
Anterior blepharitis involves the lid margin and lash line. Signs include:
- Swelling and thickening of lid margin
- Redness and dilated blood vessels
- Scaly debris at the base of the eyelashes
- Loss of eyelashes (madarosis) or misdirected eyelashes.
Posterior blepharitis involves obstruction of the ducts and loss of the Meibomian glands. This leads to:
- Conjunctival hyperaemia (dilated conjunctival vessels)
- Cloudy secretions
- Papillary and follicular reactions in the tarsal plate
- Conjunctival scarring
- Chalazions (granulomatous inflammatory lesions around meibomian glands)
- Hordeolum externum (stye, ie eyelash infection with Staphyloccocus aureus)
Cornea
An inflamed cornea (keratitis) is a rare but serious ocular complication of rosacea and can threaten vision.
- Keratitis may affect one or both eyes.
- The thinned cornea becomes inflamed with superficial punctate erosions, increased blood vessels and opacities.
- Keratitis due to ocular rosacea tends to begin at one edge or the bottom of the eye and then spread to affect lower half to two-thirds of the cornea.
- Recurrent attacks lead to corneal thinning, increased corneal opacity and vessel invasion.
- Severe ocular disease rarely can result in descemetocoele (deep ulcer) and corneal perforation.
- Corneal disease can include pannus formation (a layer of vascular fibrous tissue) and phlyctenules (allergic corneal nodules).
Iris and sclera
- Iritis: inflamed iris
- Episcleritis: inflammation of the layer between conjunctiva and cornea
- Scleritis: inflammation of the white of the eye
Iritis, episcleritis and scleritis are rare in ocular rosacea. They cause a painful, watery red eye and may affect vision.
Ocular rosacea diagnosis
Ocular rosacea may be suspected in a patient with cutaneous rosacea that has eyelid or eye disease. The symptoms and signs are nonspecific, so the diagnosis is more difficult in the absence of cutaneous rosacea.
Blepharitis can also be due to seborrheic dermatitis, a scaly skin condition, and inflammatory papules on and around the eyelids may be due to periorificial dermatitis.
Ocular rosacea treatment
Ocular rosacea can usually be controlled with medication and home eye care. But these steps don’t cure the condition, which often remains chronic or recurs after an apparent remission.
Home remedies
You can help manage your ocular rosacea by following a good eye-care routine. Keep up this routine even when your condition clears up to help prevent flare-ups. These tips may help.
- Lid hygiene: dilute baby shampoo, dilute bicarbonate solution or proprietary preparation can be applied with a cotton bud to clean eyelid margins and remove scale along the lash line.
- Warm compresses to closed eyelids for five to ten minutes daily can improve flow of meibomian gland secretions, chalazion and hordeolum.
- Artificial tears (ocular lubricants) reduce symptoms due to dry eye.
- Avoid wearing contact lenses if they irritate the inflamed eye.
- Avoid makeup if your eyes are inflamed. When you’re able to wear makeup, choose types that are nonoily (noncomedogenic) and free of fragrance.
- Prevent flare-ups by avoiding things that trigger or worsen your rosacea or ocular rosacea, if possible. Items that tend to dilate blood vessels in the face include hot, spicy foods and alcoholic beverages.
Eye drops for ocular rosacea
Topical antimicrobials
Anterior blepharitis can be successfully treated with various topical antiseptics and antibiotics including:
- Erythromycin
- Metronidazole
- Azithromycin
- Bacitracin
- Polymyxin B
- Fusidic acid
Topical anti-inflammatory agents
- Topical nonsteroidal anti-inflammatory agents such as ibuprofen may be helpful.
- Topical steroids are used short-term to treat marked lid inflammation or rosacea keratitis. Long-term use of topical steroids should be avoided, as they can lead to glaucoma and cataracts.
- Topical ciclosporin is typically used in ocular rosacea that has not responded to topical steroids.
Systemic antibiotics
The following oral antibiotics are used for ocular rosacea:
- Tetracyclines such as doxycycline
- Macrolides such as erythromycin
They reduce bacteria, improve tear film stability and normalise meibonian gland secretions.
Oral antibiotics are generally continued for 6–12 weeks, and then slowly tapered over the course of one to two months. Further courses of oral antibiotics can be used for disease flare-ups.
Styes failing to clear with topical antibiotic are treated with oral anti-staphylococcal antibiotics such as flucloxacillin.
Oral retinoids
Oral isoretinoin can be used in low dose to treat ocular rosacea but with caution because its adverse effects include increased infections, dry eye, and other ocular effects.
Ocular rosacea natural treatment
Oral omega-3 fatty acid supplementation has been reported to be beneficial for some patients with dry eyes.
Surgical intervention
Surgery may be required to repair corneal opacification or perforation due to rosacea keratitis. The procedure is called keratoplasty.
Hordeola that fail to improve with warm compresses and antibiotic therapy may be excised.
- Arman A, Demirseren DD, Takmaz T. Treatment of ocular rosacea: comparative study of topical cyclosporine and oral doxycycline. International Journal of Ophthalmology. 2015;8(3):544-549. doi:10.3980/j.issn.2222-3959.2015.03.19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4458660/[↩]
- Vieira AC, Mannis MJ. Ocular rosacea: common and commonly missed. J Am Acad Dermatol. 2013;69(6 Suppl 1):S36–41. https://www.ncbi.nlm.nih.gov/pubmed/24229635[↩]
- Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology:a review of recent findings. J Am Acad Dermatol. 2013;69:15–26. https://www.ncbi.nlm.nih.gov/pubmed/24229632[↩][↩]
- Suzuki T. Meibomitis-related keratoconjunctivitis: implications and clinicalsignificance of meibomian gland inflammation. Cornea. 2012;31(Suppl 1):S41–44. https://www.ncbi.nlm.nih.gov/pubmed/23038034[↩]
- https://www.uptodate.com/contents/rosacea-pathogenesis-clinical-features-and-diagnosis#H394012175[↩]
- Eiseman AS. The ocular manifestations of atopic dermatitis and rosacea. Curr Allergy Asthma Rep. 2006;6(4):292–298. https://www.ncbi.nlm.nih.gov/pubmed/16822381[↩]