Contents
What is optic neuritis
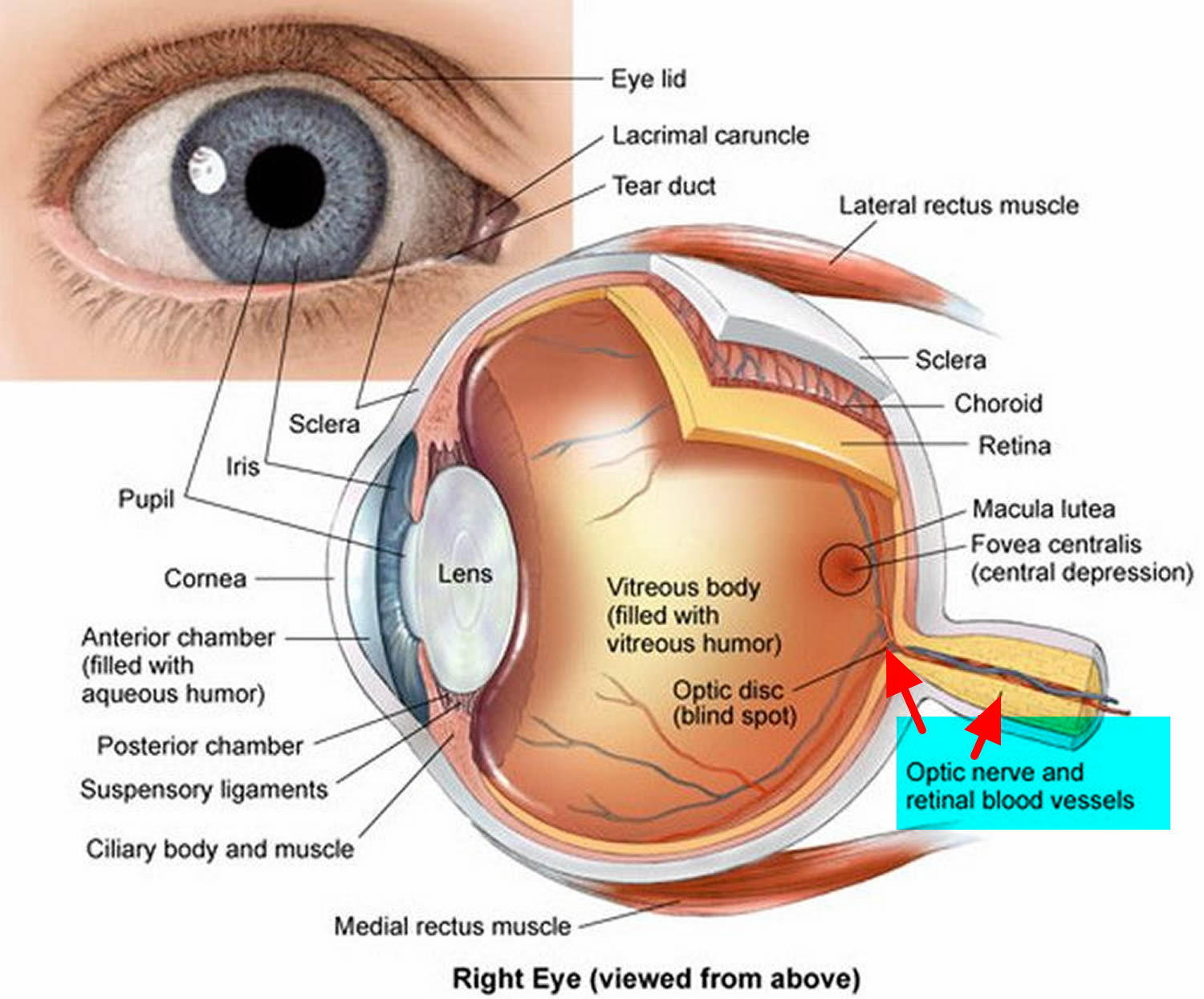
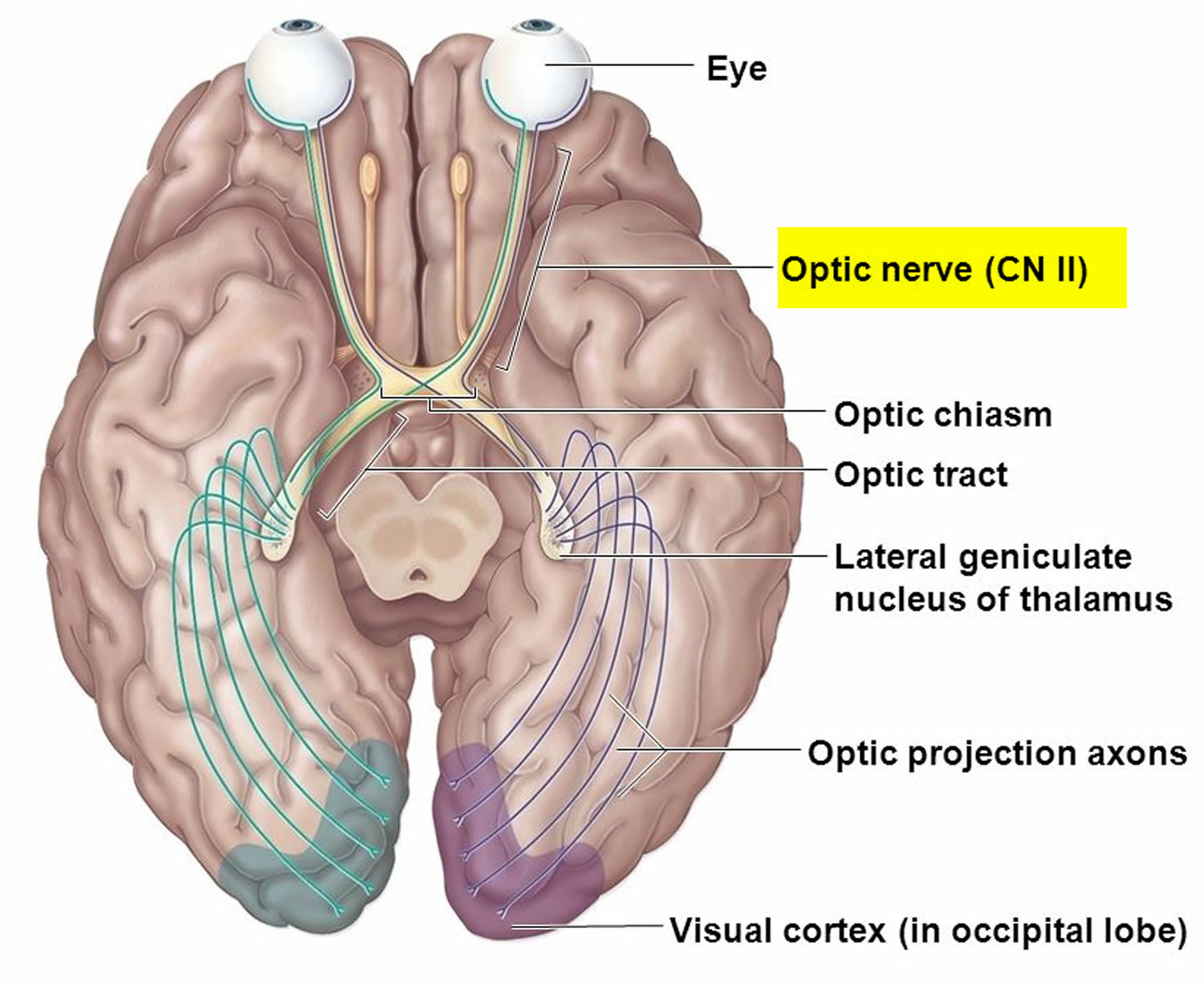
Optic neuritis is a potentially blinding inflammation of the optic nerve, which can be caused by infection and immune-related illnesses (see Figure 4). In many cases, doctors are unable to determine a cause for the optic neuritis. This inflammation can cause loss of vision because the optic nerve is crucial for vision. Optic nerve is the structure that carries visual information from the eye to the brain to produce visual images.
Many aliments affect the optic nerve including viral diseases (mumps, rubella, and cytomegalovirus), bacterial infections (cat-scratch fever and tuberculosis), sinus infections, and inflammation in the eye or other parts of the body.
Optic neuritis can also be associated with other diseases that affect the brain and nervous system, particularly multiple sclerosis (MS). Multiple sclerosis is a disease that causes inflammation and damage to nerves in your brain and spinal cord. Signs and symptoms of optic neuritis can be the first indication of multiple sclerosis, or they can occur later in the course of MS. Magnetic resonance imaging (MRI) studies of the brain in patients with optic neuritis have been shown to be useful for predicting risk of developing multiple sclerosis. For example, the presence of brain lesions on MRI is associated with a higher risk of development of multiple sclerosis in the future compared to an absence of MRI brain lesions. Besides multiple sclerosis (MS), optic neuritis can occur with other infections or immune diseases, such as lupus.
The diagnosis of multiple sclerosis (MS) is based on both of the following criteria: (1) remissions and exacerbations—attacks of the disease come and go—and (2) multiple areas of the nervous system are involved in separate attacks. In other words multiple sclerosis (MS), the disease is multiple both in time and site.
The percentage of optic neuritis patients who later develop multiple sclerosis (MS) or neurologic symptoms other than visual loss varies with length of follow-up in large studies. When patients are followed up for more than 15 years after an attack of optic neuritis, more than 60% develop other neurologic symptoms. One possibility is that all patients with optic neuritis have a limited form of MS, in which many are not destined to have any other attacks. Another possibility is that optic neuritis is a syndrome— a collection of signs and symptoms with various underlying causes and mechanisms—in which only a fraction of patients have MS.
Optic neuritis is the most common optic nerve disease to affect young people. The average age at the first attack is 31 years, but teenagers and persons over 40 may develop this disease for the first time. Optic neuritis affects more women than men. Symptoms of optic neuritis include sudden visual loss that progressively worsens over days up to 2 weeks, associated with pain on eye movements. Typically people with optic neuritis have blurred central vision (the vision used to read and see fine detail), reduced sensation of light brightness, and reduced color vision. Commonly there is aching pain in the eye made worse by eye movement.
The pain often goes away within a week or so but the blurred vision lasts for weeks to several months. Three fourths of the patients have nearly complete return of central vision, as measured by reading the eye chart. However, there is usually some permanent residual haziness, which patients describe as “looking through smoke” even though outlines of objects are sharp. Fifteen percent of patients remain blind in the affected eye. Recurrences in the same or the other eye are uncommon, and residual foggy vision following these is more prominent than after a first attack. Thus, optic neuritis can be a serious problem that leads to significant visual disability.
In children the first symptom of optic neuritis is most commonly a rapid, often profound decrease in vision (visual acuity less than 20/400). Optic neuritis can occur in both eyes and it may be worse in one eye than another. Patients may also have headaches and pain with eye movement. Many children with optic neuritis have a history of a fever, flu-like illness, or immunizations 1-2 weeks prior to the onset of the decreased vision.
Most people who have a single episode of optic neuritis eventually recover their vision. Most cases (92%) of optic neuritis will experience improvement with or without treatment. Treatment with steroid medications may speed up vision recovery after optic neuritis.
What are the differences between optic neuritis in children and adults?
Both eyes are usually affected in children, while adults usually have only one eye affected. Children with optic neuritis usually have a history of recent illness or immunization and adults do not. Both adults and children have an increased risk of multiple sclerosis if they develop optic neuritis, but children have much less risk.
Figure 1. Optic nerve
Figure 2. Optic nerve and visual pathway
Figure 3. Normal optic nerve
Figure 4. Optic neuritis – the photo demonstrates, the optic nerve becomes swollen and the blood vessels become larger.
Optic neuritis prognosis
Most people regain close to normal vision within 12 months after an optic neuritis episode. Over 90% of patients experience improvement in their vision. Vision may not always return totally to normal, for example, patients may be aware of a ‘grey patch’ in their vision that persists, or colors may not appear as bright as before the attack of optic neuritis.
People with recurrent optic neuritis have a greater risk of developing MS. Optic neuritis can recur in people without underlying conditions. But those people generally have a better long-term prognosis for their vision than do people with multiple sclerosis or neuromyelitis optica.
Optic neuritis complications
Complications arising from optic neuritis may include:
- Optic nerve damage. Most people have some permanent optic nerve damage after an episode of optic neuritis, but the damage might not cause symptoms.
- Decreased visual acuity. Most people regain normal or near normal vision within several months, but a partial loss of color discrimination might persist. For some people, vision loss persists after the optic neuritis has improved.
- Side effects of treatment. Steroid medications used to treat optic neuritis subdue your immune system, which causes your body to become more susceptible to infections. Other side effects include mood changes and weight gain.
Optic neuritis causes
The exact cause of optic neuritis is unknown. It’s believed to develop when the immune system mistakenly targets the substance covering your optic nerve (myelin), resulting in inflammation and damage to the myelin. Occasionally, the inflammation may affect both optic nerves, or various sites within the brain substance.
Normally, the myelin helps electrical impulses travel quickly from the eye to the brain, where they’re converted into visual information. Optic neuritis disrupts this process, affecting vision.
The following autoimmune conditions often are associated with optic neuritis:
- Multiple sclerosis. Multiple sclerosis is a disease in which your autoimmune system attacks the myelin sheath covering nerve fibers in your brain and spinal cord. In people with optic neuritis, the risk of developing multiple sclerosis following one episode of optic neuritis is about 50 percent over a lifetime. Your risk of developing multiple sclerosis after optic neuritis increases further if an MRI scan shows lesions on your brain.
- Neuromyelitis optica. In this condition, inflammation recurs in the optic nerve and spinal cord. Neuromyelitis optica has similarities to multiple sclerosis, but neuromyelitis optica doesn’t cause damage to the nerves in the brain as often as multiple sclerosis does.
Other factors that have been linked to the development of optic neuritis include:
- Infections. Bacterial infections, including Lyme disease, tuberculosis, cat-scratch fever, syphilis; fungal infection cryptococcosis or viruses, such as measles, mumps and herpes, can cause optic neuritis.
- Respiratory infections, including mycoplasma pneumonia and other common upper respiratory tract infections
- Autoimmune diseases such as lupus, sarcoidosis, and Behçet disease can cause recurrent optic neuritis.
- Drugs. Some drugs have been associated with the development of optic neuritis. They include quinine and some antibiotics.
Risk factors for developing optic neuritis
Risk factors for developing optic neuritis include:
- Age. Optic neuritis most often affects adults ages 20 to 40.
- Sex. Women are much more likely to develop optic neuritis than men are.
- Race. In the United States, optic neuritis occurs more frequently in whites than it does in blacks.
- Genetic mutations. Certain genetic mutations might increase your risk of developing optic neuritis or multiple sclerosis.
Preventing multiple sclerosis
If you have optic neuritis, and you have two or more brain lesions evident on MRI scans, you might benefit from drugs, called beta interferons that may delay or help prevent multiple sclerosis. For patients with a first episode of optic neuritis and MRI evidence of inflammation in the brain, treatment with beta interferons initiated at the time of the optic neuritis has been shown to reduce the rate of conversion to multiple sclerosis. These injectable medications are used for people at high risk for developing MS. Possible side effects include depression, injection site irritation and flu-like symptoms.
All patients who are found to have MRI evidence of brain inflammation are referred to a neurologist specializing in multiple sclerosis for full neurologic assessment.
Optic neuritis symptoms
Optic neuritis usually affects one eye. Symptoms might include:
- Pain. Most people who develop optic neuritis have eye pain that’s worsened by eye movement. Sometimes the pain feels like a dull ache behind the eye.
- Vision loss in one eye. Most people have at least some temporary reduction in vision, but the extent of loss varies. Noticeable vision loss usually develops over hours or days and improves over several weeks to months. Vision loss is permanent in some cases.
- Visual field loss. Side vision loss can occur in any pattern.
- Loss of color vision. Optic neuritis often affects color perception. You might notice that colors appear less vivid than normal.
- Flashing lights. Some people with optic neuritis report seeing flashing or flickering lights with eye movements.
Optic neuritis diagnosis
You’re likely to see an ophthalmologist for a diagnosis, which is generally based on your medical history and an exam. The ophthalmologist likely will perform the following eye tests:
- A routine eye exam. Your eye doctor will check your vision and your ability to perceive colors and measure your side (peripheral) vision.
- Ophthalmoscopy. During this examination, your doctor shines a bright light into your eye and examines the structures at the back of your eye. This eye test evaluates the optic disk, where the optic nerve enters the retina in your eye. The optic disk becomes swollen in about one-third of people with optic neuritis.
- Pupillary light reaction test. Your doctor may move a flashlight in front of your eyes to see how your pupils respond when they’re exposed to bright light. Pupils in eyes affected by optic neuritis don’t constrict as much as those in healthy eyes do when stimulated by light.
Other tests to diagnose optic neuritis might include:
- Magnetic resonance imaging (MRI) scan. An MRI scan uses a magnetic field and pulses of radio wave energy to make pictures of your body. During an MRI to check for optic neuritis, you might receive an injection of a contrast solution to make the optic nerve and other parts of your brain more visible on the images. An MRI is important to determine whether there are damaged areas (lesions) in your brain. Such lesions indicate a high risk of developing multiple sclerosis. An MRI can also rule out other causes of visual loss, such as a tumor.
- Blood tests. A blood test is available to check for antibodies for neuromyelitis optica. People with severe optic neuritis may undergo this test to determine whether they’re likely to develop neuromyelitis optica.
- Optical coherence tomography. This measures the thickness of the retinal nerve fiber layer, which is often thinner from optic neuritis.
- Visual evoked response. During this test, you sit before a screen on which an alternating checkerboard pattern is displayed. Attached to your head are wires with small patches to record your brain’s responses to the visual stimuli. This type of test detects the slowing of electrical conduction resulting from damage to the optic nerve.
Your doctor is likely to ask you to return for follow-up exams two to four weeks after your symptoms begin to confirm the diagnosis of optic neuritis.
Optic neuritis treatment
Optic neuritis usually improves on its own. In some cases, steroid medications are used to reduce inflammation in the optic nerve. Possible side effects from steroid treatment include weight gain, mood changes, facial flushing, stomach upset and insomnia.
Steroid treatment is usually given by vein (intravenously). Intravenous steroid therapy might speed vision recovery, but it doesn’t appear to affect the amount of vision you’ll recover. It has never been proved that treatment with any form of steroid regimen improves the long-range outcome of optic neuritis. Steroid treatment is also used to reduce the risk of developing multiple sclerosis (MS) or slow its development.
When steroid therapy fails and severe vision loss persists, a treatment called plasma exchange therapy might help some people recover their vision. Studies haven’t confirmed that plasma exchange therapy is effective for optic neuritis.