Contents
- Pancreas problems and diseases
Pancreas problems and diseases
The pancreas is both an endocrine and exocrine gland. The endocrine part of the pancreas consists of groups of cells that are closely associated with blood vessels. These groups form “islands” of cells called pancreatic islets (islets of Langerhans). The pancreatic islets include two distinct types of cells—alpha cells, which secrete the hormone glucagon, and beta cells, which secrete the hormone insulin.
About 99% of the pancreas is exocrine tissue, which secretes 1,200 to 1,500 mL of pancreatic juice per day. Pancreatic islets are relatively concentrated in the tail of the pancreas, whereas the head is more exocrine. Over 90% of pancreatic cancers arise from the ducts of the exocrine portion (ductal carcinomas), so cancer is most common in the head of the gland.
Problems with the pancreas can lead to many health problems. There are a variety of disorders of the pancreas including:
- Pancreatitis – acute pancreatitis and chronic pancreatitis, hereditary pancreatitis or inflammation of the pancreas: This happens when digestive enzymes start digesting the pancreas itself.
- Pancreatic cancer
- Cystic fibrosis, a genetic disorder in which thick, sticky mucus can also block tubes in your pancreas
The pancreas also plays a role in diabetes. In type 1 diabetes, the beta cells of the pancreas no longer make insulin because the body’s immune system has attacked them. In type 2 diabetes, the pancreas loses the ability to secrete enough insulin in response to meals.
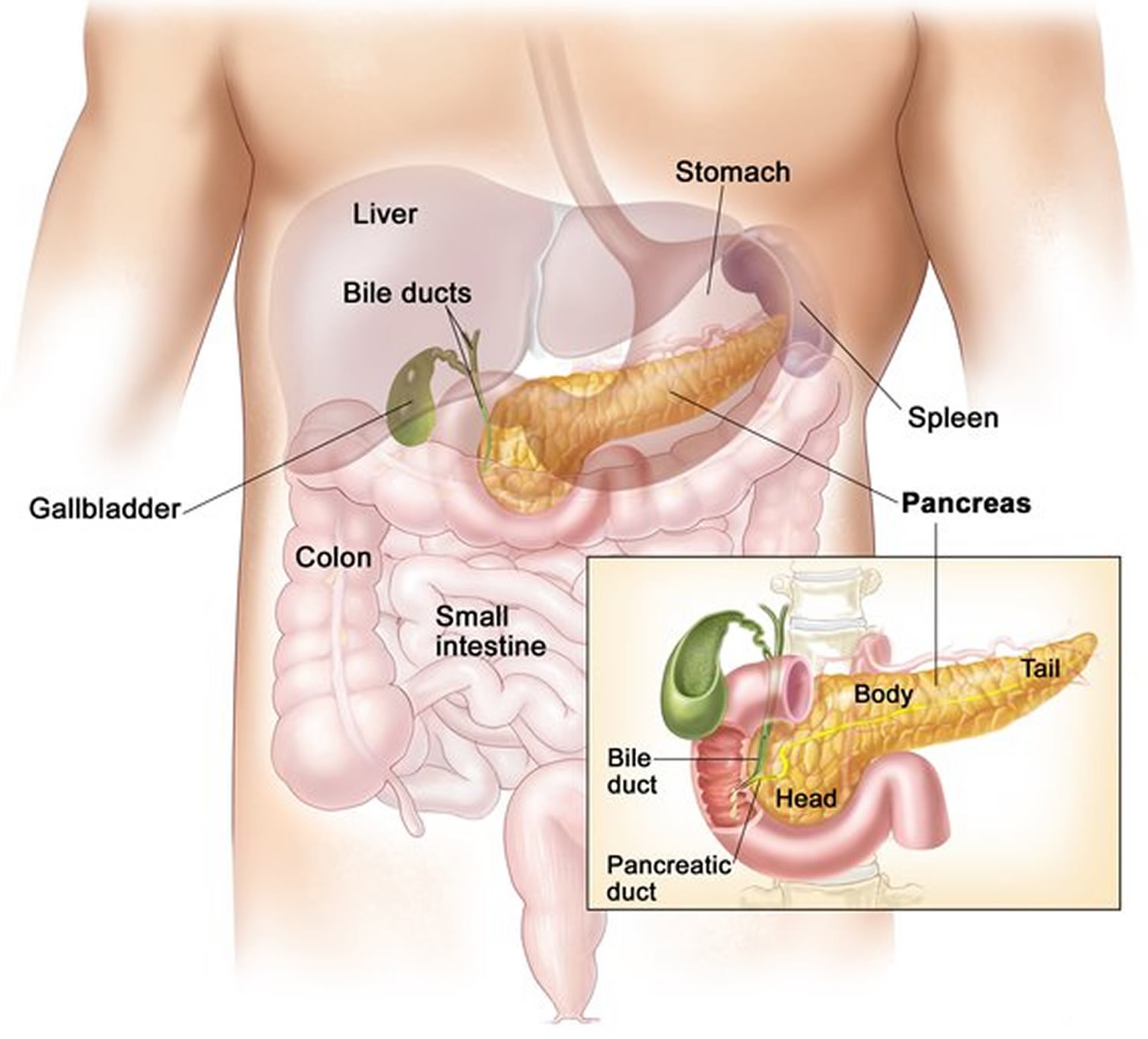
Figure 1. Pancreas location
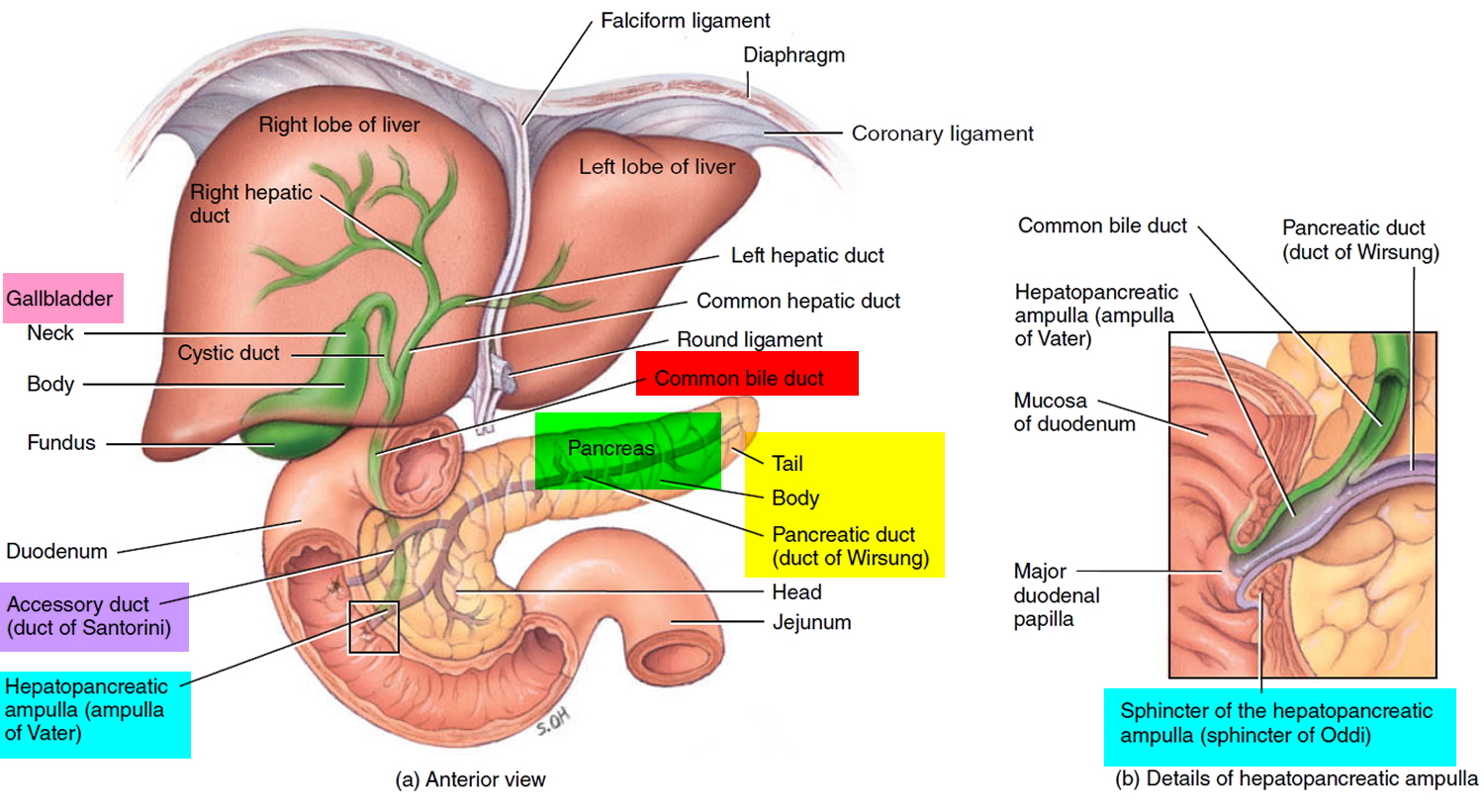
Figure 2. Relationship of the pancreas to the liver, gallbladder, and duodenum
What is pancreatitis ?
Pancreatitis is inflammation of the pancreas 1. The pancreas is a large gland behind the stomach and close to the duodenum—the first part of the small intestine. The pancreas secretes digestive juices, or enzymes, into the duodenum through a tube called the pancreatic duct. Pancreatic enzymes join with bile—a liquid produced in the liver and stored in the gallbladder—to digest food. The pancreas also releases the hormones insulin and glucagon into the bloodstream. These hormones help the body regulate the glucose it takes from food for energy.
Normally, digestive enzymes secreted by the pancreas do not become active until they reach the small intestine. But when the pancreas is inflamed, the enzymes inside it attack and damage the tissues that produce them.
Pancreatitis can be acute or chronic. Either form is serious and can lead to complications. In severe cases, bleeding, infection, and permanent tissue damage may occur.
Both forms of pancreatitis occur more often in men than women.
How common is pancreatitis in children ?
Chronic pancreatitis in children is rare. Trauma to the pancreas and hereditary pancreatitis are two known causes of childhood pancreatitis. Children with cystic fibrosis—a progressive and incurable lung disease—may be at risk of developing pancreatitis. But more often the cause of pancreatitis in children is unknown.
What is acute pancreatitis ?
Acute pancreatitis is inflammation of the pancreas that occurs suddenly and usually resolves in a few days with treatment. Acute pancreatitis can be a life-threatening illness with severe complications 1. Each year, about 210,000 people in the United States are admitted to the hospital with acute pancreatitis 2. The most common cause of acute pancreatitis is the presence of gallstones—small, pebble-like substances made of hardened bile—that cause inflammation in the pancreas as they pass through the common bile duct. Chronic, heavy alcohol use is also a common cause. Acute pancreatitis can occur within hours or as long as 2 days after consuming alcohol. Other causes of acute pancreatitis include abdominal trauma, medications, infections, tumors, and genetic abnormalities of the pancreas.
Symptoms of Acute pancreatitis
Acute pancreatitis usually begins with gradual or sudden pain in the upper abdomen that sometimes extends through the back. The pain may be mild at first and feel worse after eating. But the pain is often severe and may become constant and last for several days. A person with acute pancreatitis usually looks and feels very ill and needs immediate medical attention. Other symptoms may include:
- a swollen and tender abdomen
- nausea and vomiting
- fever
- a rapid pulse
Severe acute pancreatitis may cause dehydration and low blood pressure. The heart, lungs, or kidneys can fail. If bleeding occurs in the pancreas, shock and even death may follow 1.
Diagnosis of Acute pancreatitis
While asking about a person’s medical history and conducting a thorough physical examination, the doctor will order a blood test to assist in the diagnosis. During acute pancreatitis, the blood contains at least three times the normal amount of amylase and lipase, digestive enzymes formed in the pancreas. Changes may also occur in other body chemicals such as glucose, calcium, magnesium, sodium, potassium, and bicarbonate. After the person’s condition improves, the levels usually return to normal.
Diagnosing acute pancreatitis is often difficult because of the deep location of the pancreas. The doctor will likely order one or more of the following tests:
- Abdominal ultrasound. Sound waves are sent toward the pancreas through a handheld device that a technician glides over the abdomen. The sound waves bounce off the pancreas, gallbladder, liver, and other organs, and their echoes make electrical impulses that create a picture—called a sonogram—on a video monitor. If gallstones are causing inflammation, the sound waves will also bounce off them, showing their location.
- Computerized tomography (CT) scan. The CT scan is a noninvasive x ray that produces three-dimensional pictures of parts of the body. The person lies on a table that slides into a donut-shaped machine. The test may show gallstones and the extent of damage to the pancreas.
- Endoscopic ultrasound (EUS). After spraying a solution to numb the patient’s throat, the doctor inserts an endoscope—a thin, flexible, lighted tube—down the throat, through the stomach, and into the small intestine. The doctor turns on an ultrasound attachment to the scope that produces sound waves to create visual images of the pancreas and bile ducts.
- Magnetic resonance cholangiopancreatography (MRCP). MRCP uses magnetic resonance imaging, a noninvasive test that produces cross-section images of parts of the body. After being lightly sedated, the patient lies in a cylinder-like tube for the test. The technician injects dye into the patient’s veins that helps show the pancreas, gallbladder, and pancreatic and bile ducts.
Treatment of Acute pancreatitis
Treatment for acute pancreatitis requires a few days’ stay in the hospital for intravenous (IV) fluids, antibiotics, and medication to relieve pain. The person cannot eat or drink so the pancreas can rest. If vomiting occurs, a tube may be placed through the nose and into the stomach to remove fluid and air.
Unless complications arise, acute pancreatitis usually resolves in a few days. In severe cases, the person may require nasogastric feeding—a special liquid given in a long, thin tube inserted through the nose and throat and into the stomach—for several weeks while the pancreas heals.
Before leaving the hospital, the person will be advised not to smoke, drink alcoholic beverages, or eat fatty meals. In some cases, the cause of the pancreatitis is clear, but in others, more tests are needed after the person is discharged and the pancreas is healed.
Therapeutic Endoscopic Retrograde Cholangiopancreatography (ERCP) for Acute and Chronic Pancreatitis
ERCP is a specialized technique used to view the pancreas, gallbladder, and bile ducts and treat complications of acute and chronic pancreatitis—gallstones, narrowing or blockage of the pancreatic duct or bile ducts, leaks in the bile ducts, and pseudocysts—accumulations of fluid and tissue debris.
Soon after a person is admitted to the hospital with suspected narrowing of the pancreatic duct or bile ducts, a physician with specialized training performs ERCP.
After lightly sedating the patient and giving medication to numb the throat, the doctor inserts an endoscope—a long, flexible, lighted tube with a camera—through the mouth, throat, and stomach into the small intestine. The endoscope is connected to a computer and screen. The doctor guides the endoscope and injects a special dye into the pancreatic or bile ducts that helps the pancreas, gallbladder, and bile ducts appear on the screen while x rays are taken.
The following procedures can be performed using ERCP:
- Sphincterotomy. Using a small wire on the endoscope, the doctor finds the muscle that surrounds the pancreatic duct or bile ducts and makes a tiny cut to enlarge the duct opening. When a pseudocyst is present, the duct is drained.
- Gallstone removal. The endoscope is used to remove pancreatic or bile duct stones with a tiny basket. Gallstone removal is sometimes performed along with a sphincterotomy.
- Stent placement. Using the endoscope, the doctor places a tiny piece of plastic or metal that looks like a straw in a narrowed pancreatic or bile duct to keep it open.
- Balloon dilatation. Some endoscopes have a small balloon that the doctor uses to dilate, or stretch, a narrowed pancreatic or bile duct. A temporary stent may be placed for a few months to keep the duct open.
People who undergo therapeutic ERCP are at slight risk for complications, including severe pancreatitis, infection, bowel perforation, or bleeding. Complications of ERCP are more common in people with acute or recurrent pancreatitis. A patient who experiences fever, trouble swallowing, or increased throat, chest, or abdominal pain after the procedure should notify a doctor immediately.
Complications of Acute pancreatitis
Gallstones that cause acute pancreatitis require surgical removal of the stones and the gallbladder. If the pancreatitis is mild, gallbladder removal—called cholecystectomy—may proceed while the person is in the hospital. If the pancreatitis is severe, gallstones may be removed using therapeutic endoscopic retrograde cholangiopancreatography (ERCP)—a specialized technique used to view the pancreas, gallbladder, and bile ducts and treat complications of acute and chronic pancreatitis. Cholecystectomy is delayed for a month or more to allow for full recovery.
If an infection develops, ERCP or surgery may be needed to drain the infected area, also called an abscess. Exploratory surgery may also be necessary to find the source of any bleeding, to rule out conditions that resemble pancreatitis, or to remove severely damaged pancreatic tissue.
Pseudocysts—accumulations of fluid and tissue debris—that may develop in the pancreas can be drained using ERCP or EUS. If pseudocysts are left untreated, enzymes and toxins can enter the bloodstream and affect the heart, lungs, kidneys, or other organs.
Acute pancreatitis sometimes causes kidney failure. People with kidney failure need blood-cleansing treatments called dialysis or a kidney transplant.
In rare cases, acute pancreatitis can cause breathing problems. Hypoxia, a condition that occurs when body cells and tissues do not get enough oxygen, can develop. Doctors treat hypoxia by giving oxygen to the patient. Some people still experience lung failure—even with oxygen—and require a respirator for a while to help them breathe.
What is chronic pancreatitis ?
Chronic pancreatitis is inflammation of the pancreas that does not heal or improve—it gets worse over time and leads to permanent damage. Chronic pancreatitis, like acute pancreatitis, occurs when digestive enzymes attack the pancreas and nearby tissues, causing episodes of pain. Chronic pancreatitis often develops in people who are between the ages of 30 and 40.
The most common cause of chronic pancreatitis is many years of heavy alcohol use. The chronic form of pancreatitis can be triggered by one acute attack that damages the pancreatic duct. The damaged duct causes the pancreas to become inflamed. Scar tissue develops and the pancreas is slowly destroyed.
Other causes of chronic pancreatitis are
- hereditary disorders of the pancreas
- cystic fibrosis—the most common inherited disorder leading to chronic pancreatitis
- hypercalcemia—high levels of calcium in the blood
- hyperlipidemia or hypertriglyceridemia—high levels of blood fats
- some medicines
- certain autoimmune conditions
- unknown causes
Hereditary pancreatitis can present in a person younger than age 30, but it might not be diagnosed for several years. Episodes of abdominal pain and diarrhea lasting several days come and go over time and can progress to chronic pancreatitis. A diagnosis of hereditary pancreatitis is likely if the person has two or more family members with pancreatitis in more than one generation.
Symptoms of chronic pancreatitis
Most people with chronic pancreatitis experience upper abdominal pain, although some people have no pain at all. The pain may spread to the back, feel worse when eating or drinking, and become constant and disabling. In some cases, abdominal pain goes away as the condition worsens, most likely because the pancreas is no longer making digestive enzymes. Other symptoms include:
- nausea
- vomiting
- weight loss
- diarrhea
- oily stools
People with chronic pancreatitis often lose weight, even when their appetite and eating habits are normal. The weight loss occurs because the body does not secrete enough pancreatic enzymes to digest food, so nutrients are not absorbed normally. Poor digestion leads to malnutrition due to excretion of fat in the stool.
Diagnosis of chronic pancreatitis
Chronic pancreatitis is often confused with acute pancreatitis because the symptoms are similar. As with acute pancreatitis, the doctor will conduct a thorough medical history and physical examination. Blood tests may help the doctor know if the pancreas is still making enough digestive enzymes, but sometimes these enzymes appear normal even though the person has chronic pancreatitis.
In more advanced stages of pancreatitis, when malabsorption and diabetes can occur, the doctor may order blood, urine, and stool tests to help diagnose chronic pancreatitis and monitor its progression.
After ordering x rays of the abdomen, the doctor will conduct one or more of the tests used to diagnose acute pancreatitis—abdominal ultrasound, CT scan, EUS, and MRCP.
Treatment of chronic pancreatitis
Treatment for chronic pancreatitis may require hospitalization for pain management, IV hydration, and nutritional support. Nasogastric feedings may be necessary for several weeks if the person continues to lose weight.
When a normal diet is resumed, the doctor may prescribe synthetic pancreatic enzymes if the pancreas does not secrete enough of its own. The enzymes should be taken with every meal to help the person digest food and regain some weight. The next step is to plan a nutritious diet that is low in fat and includes small, frequent meals. A dietitian can assist in developing a meal plan. Drinking plenty of fluids and limiting caffeinated beverages is also important.
People with chronic pancreatitis are strongly advised not to smoke or consume alcoholic beverages, even if the pancreatitis is mild or in the early stages.
Complications of chronic pancreatitis
People with chronic pancreatitis who continue to consume large amounts of alcohol may develop sudden bouts of severe abdominal pain.
As with acute pancreatitis, ERCP is used to identify and treat complications associated with chronic pancreatitis such as gallstones, pseudocysts, and narrowing or obstruction of the ducts. Chronic pancreatitis also can lead to calcification of the pancreas, which means the pancreatic tissue hardens from deposits of insoluble calcium salts. Surgery may be necessary to remove part of the pancreas.
In cases involving persistent pain, surgery or other procedures are sometimes recommended to block the nerves in the abdominal area that cause pain.
When pancreatic tissue is destroyed in chronic pancreatitis and the insulin-producing cells of the pancreas, called beta cells, have been damaged, diabetes may develop. People with a family history of diabetes are more likely to develop the disease. If diabetes occurs, insulin or other medicines are needed to keep blood glucose at normal levels. A health care provider works with the patient to develop a regimen of medication, diet, and frequent blood glucose monitoring.
What is Exocrine Pancreatic Insufficiency
Exocrine pancreatic insufficiency is a condition characterized by deficiency of the exocrine pancreatic enzymes, resulting in the inability to digest food properly, or maldigestion 3.
Who gets exocrine pancreatic insufficiency ?
Exocrine pancreatic insufficiency is associated with certain diseases and conditions that affect the pancreas. Some of these diseases you are born with, like cystic fibrosis, while others may occur later in life, as is the case with chronic pancreatitis.
Exocrine pancreatic insufficiency may be associated with chronic pancreatitis and cystic fibrosis. If you have one of these conditions and symptoms of exocrine pancreatic insufficiency, we recommend that you talk to your doctor.
Chronic Pancreatitis
Chronic pancreatitis is the most common cause of exocrine pancreatic insufficiency in adults. Over the course of years the inflammation can lead to irreversible damage to the pancreas, including the cells that secrete pancreatic digestive enzymes and the cells that produce insulin leading to diabetes.
Cystic fibrosis
Cystic fibrosis is an inherited genetic condition that leads to chronic disease that mainly affects the lungs and digestive and reproductive systems. In patients with cstic fibrosis, a thick, sticky mucus is produced in certain organs throughout the body, most commonly in the lungs and digestive system, including the pancreas. Many people living with cystic fibrosis are unable to properly digest food because they may also have exocrine pancreatic insufficiency.
Diagnosing exocrine pancreatic insufficiency
If you have exocrine pancreatic insufficiency, your body cannot properly digest fats, proteins, and carbohydrates in the food you eat. In addition to preventing adequate digestion, exocrine pancreatic insufficiency produces uncomfortable gastrointestinal (GI) symptoms.
Only your doctor can tell if your GI symptoms are due to exocrine pancreatic insufficiency or another digestive condition. That is why it is so important to see to your doctor about your medical history and all of your medications including all vitamins and supplements you take. And make sure to open up and share all of your symptoms at your next visit.
Living with exocrine pancreatic insufficiency
Getting nutrition from food
The food you eat contains 3 main nutrients—fat, protein, and carbohydrates. Your body uses these nutrients to help give you energy to function.
- FAT is found in foods like nuts and cheese.
- PROTEIN comes from foods like meat, poultry and fish.
- CARBOHYDRATES can be found in bread and pasta. Carbohydrates are broken down into sugars.
If you have exocrine pancreatic insufficiency, your pancreas cannot properly break down foods, resulting in poor digestion of nutrients—especially fats. Eating healthy is important for all of us. But it’s especially important that people with exocrine pancreatic insufficiency eat a nutrient-rich diet—along with taking pancreatic enzyme replacement therapy with every meal and snack—since exocrine pancreatic insufficiency interferes with nutrient absorption.
If you have been diagnosed with exocrine pancreatic insufficiency, you should work with your doctor or nutritionist to make sure that all your dietary needs are being met.
Pancreatic enzyme replacement therapies
Your doctor may start you on a prescription treatment called pancreatic enzyme replacement therapy, or PERT. Pancreatic enzyme replacement therapies are the main treatment for exocrine pancreatic insufficiency—they replace the digestive enzymes that your pancreas isn’t producing anymore. When taken with food, pancreatic enzyme replacement therapies help break down the nutrients in food.
Vitamins and supplements
If you have exocrine pancreatic insufficiency, your body may not absorb the nutrients from the food you eat. Your doctor may prescribe vitamin and mineral supplements to help you maintain proper levels of the fat-soluble vitamins A, D, E, and K.
Eating healthy with exocrine pancreatic insufficiency and cystic fibrosis
A high-calorie diet with adequate amounts of fat is especially important to help patients with cystic fibrosis grow, develop, and thrive. Patients with cystic fibrosis should work with their dietitian or nutritionist to make sure their proper nutrition needs are met.
What is Pancreas Divisum
Pancreas divisum is a common congenital anomaly (an anomaly that is present at birth) of the pancreatic duct(s) in which parts of the pancreas do not join together 4.
Causes of Pancreas divisum
The human embryo begins life with two ducts in the pancreas, the ventral duct and the dorsal duct. Normally, the two ducts will fuse together to form one main pancreatic duct; this occurs in more than 90% of embryos. In approximately 10% of embryos the ventral and dorsal ducts fail to fuse together, resulting in pancreas divisum. In utero, the majority of the pancreas is drained by the dorsal duct which opens up into the minor papilla. The ventral duct drains the minority of the pancreas and opens into the major papilla. In adults however, this situation is reversed whereby 70% of the pancreas is drained by the ventral duct. Therefore in pancreas divisum, where fusion of the ducts does not occur, the major drainage of the pancreas is done by the dorsal duct which opens up into the minor papilla.
Symptoms of Pancreas divisum
A majority of individuals born with pancreas divisum will not have symptoms. In some cases, pancreas divisum is only detected during autopsy. A small group of individuals will develop symptoms which commonly include abdominal pain, nausea, vomiting, and acute and chronic pancreatitis.
Diagnosis of Pancreas divisum
The most common and accurate way of diagnosing an individual with this anomaly is by MRCP (Magnetic Resonance Cholangiopancreatography) or ERCP (Endoscopic Retrograde Cholangiopancreatography). This test can demonstrate the presence of two separately draining ducts within the pancreas. Other tests can assist doctors with diagnosis, such as a CT scan and an MRI.
Treatment for Pancreas divisum
Pancreas divisum in individuals with no symptoms does not require treatment. Treatment of those with symptoms varies and has not been well established. A surgeon may attempt a Puestow procedure or sphincterotomy by cutting the minor papilla to enlarge the opening and allow pancreatic enzymes to flow normally. During surgery, a stent may be inserted into the duct to ensure that the duct will not close causing a blockage. This surgery can cause pancreatitis in patients, or in rare cases, kidney failure and death.
Pancreatic Cancer
Pancreatic cancer is the fourth most common cause of cancer death in men and the fifth in women 5. The National Cancer Institute estimated that in 2013, there were 45,220 new cases of pancreatic cancer, and 38,460 deaths because of it. The incidence of pancreatic cancer has been increasing since 2004; however, the National Cancer Institute recently reported that for the first time since 2004, the number of deaths per year has gradually started to decline. One of the major challenges associated with pancreatic cancer is that the condition often goes undetected for a long period of time because signs and symptoms seldom occur until advanced stages. By the time symptoms occur, cancer cells are likely to have spread (metastasized) to other parts of the body, often preventing surgical removal of tumors.
Cancer of the pancreas is resistant to many standard treatments including chemotherapy and radiation therapy. This cancer grows insidiously and initially does not cause symptoms. The classic presentation of pancreatic cancer is referred to as painless jaundice, a yellowish skin discoloration with no other symptoms. The diagnosis is usually made using different radiographic imaging techniques.
If detected in the early stages, pancreatic cancer can be cured by surgical resection. Unfortunately, early detection is more the exception than the rule. At later stages, treatment can improve the quality of life by controlling symptoms and complications.
Causes of Pancreatic Cancer
The exact cause of pancreatic cancer is yet to be determined 6. However, genetics appear to play a large role, as they do with other cancers. People with family members who have been diagnosed with pancreatic cancer are at a greater risk of developing it themselves.
In addition, a number of diseases have been associated with an increased risk of pancreatic cancer, including:
- Familial adenomatous polyposis
- Hereditary nonpolyposis colon cancer (Lynch syndrome)
- Familial breast cancer associated with the BRAC2 gene
- Hereditary pancreatitis
- Familial atypical multiple mole melanoma syndrome (a form of skin cancer)
Hereditary risk for any of the above diseases can lead to an increased risk of pancreatic cancer. However, this predisposition accounts for only approximately 10% of all pancreatic cancers. A far greater number of cases develop as a result of environmental and lifestyle factors such as smoking, diet, and chemical exposure. A personal history of chronic pancreatitis is associated with an increased risk of developing pancreatic cancer.
Risk Factors for pancreatic cancer
Risks for pancreatic cancer include the following:
- Age. The vast majority of cases of pancreatic cancer occur in individuals aged 65 years and older.
- Race. Black men and women have a greater likelihood of developing pancreatic cancer.
- Sex. Men are more likely to develop pancreatic cancer.
- Excess alcohol. People who drink 9 or more alcoholic drinks every day are at increased risk for developing pancreatic cancer.
- Cigarette smoking. Smokers are 2 to 3 times more likely to develop pancreatic cancer than nonsmokers. Smoking is the single greatest risk factor, associated with almost one-third of all cases of pancreatic cancer.
- Diabetes. Multiple large studies have shown that people diagnosed with diabetes (abnormal glucose metabolism) are at significantly increased risk of developing pancreatic cancer.
- Weight. Multiple large studies have shown that people who are obese, with a body mass index (BMI) 30 or greater, are at increased risk for developing pancreatic cancer (a large study showed that the risk was 47% greater compared to people who were not obese).
- Diet. Diets high in animal fats and low in fruits and vegetables are more likely to develop pancreatic cancer. A large study has also shown that consumption of processed meat and red meat is associated with an increased risk of developing pancreatic cancer.
- Chemical exposure. Individuals working with petroleum agents such as gasoline and fuel oils are at increased risk of developing pancreatic cancer.
- Bacteria. Helicobacter pylori (H. pylori) is a bacterium that can infect the gut, and it is one of the most common gut infections in humans, affecting approximately one-third of the US population. H. pylori is well known to cause ulcers, but many studies are now linking it to the development of pancreatic cancer.
- ABO blood type has also been shown to be associated with a risk of developing pancreatic cancer.
Signs and Symptoms of Pancreatic Cancer
In many cases, there are no symptoms in pancreatic cancer until its late stages. The following is a list of symptoms that could indicate pancreatic cancer, but many other conditions can present with similar symptoms. If you exhibit any of the below symptoms, contact your physician as soon as possible:
- Upper abdominal pain that may extend to the middle or upper back
- Weight loss
- Jaundice—yellowing of the skin and whites of the eyes. This condition is fairly common among patients with pancreatic cancer and develops when blood cells become worn out and break down into bilirubin. Normally, bilirubin is eliminated in the bile, which is a fluid produced by the liver. However, if a pancreatic tumor blocks the flow of bile, jaundice may occur.
- Sever itching may occur, owing to a build-up of bile acids.
- Nausea and vomiting can occur during later stages if a pancreatic tumor has grown sufficiently large to block a portion of the digestive tract (usually the duodenum).
- Digestive problems can occur because the pancreas is an integral part of the digestive system.
Staging of Pancreatic Cancer
In the Tumor, Node, Metastasis (TNM) model, tumor size, lymph node status, and metastasis are measured separately, each with its own number scale.
For tumor (T) size:
- T1 denotes a tumor size less than 2 cm across in any direction
- T2 denotes a tumor larger than 2 cm across
- T3 denotes a tumor that has started to grow into the duodenum and bile ducts that surround the pancreas
- T4 denotes that the tumor has invaded the spleen, large intestine, and major blood vessels
For lymph node (N) status:
- N0 indicates that there are no lymph nodes containing cancer
- N1 indicates that there are lymph nodes containing cancer, and therefore, the tumor has likely metastasized beyond the pancreas.
For metastasis (M) status:
- M0 indicates that the tumor has not spread
- M1 indicates that it has spread.
The second model of pancreatic cancer has 4 numbered stages, as follows:
Stage I. The tumor has not progressed outside of the pancreas. The TNM equivalent would be T1 or 2, N0, M0, meaning that there has been no spread, and that the tumor is relatively small.
Stage II. The tumor has grown into nearby tissues and perhaps the duodenum. Lymph nodes are not affected. The TNM equivalent would be T3, N0, M0.
Stage III. The tumor may be quite large and has spread to the lymph node system, and thus is capable of spread to other organs. The TNM equivalent would be T1–3, N1, M0.
Stage IV. This stage is often divided into 2 sub-stages:
- Stage IVA describes a situation in which cancer has grown into nearby organs, including the spleen and/or stomach, as well as large blood vessels. The TNM equivalent would be T4, N1 or 2, M0.
- Stage IVB describes a situation in which cancer has spread to other organs, such as the liver or lungs, with a TNM equivalent of T1–4, N0 or 1, M1.
Treatment of Pancreatic Cancer
Treatment options for pancreatic cancer depend on the type and stage of cancer. Medical research is ongoing to determine the best methods for relieving pain and eliminating cancer.
Palliative treatment options include stenting of the obstructed biliary tree (to relieve jaundice), surgical biliary bypass (especially in younger patients), and complex pain-relief options. In addition, enzyme supplements may be useful because the main pancreatic duct is usually blocked. Chemotherapy is an option and has been shown to increase the chance of survival, especially over longer periods of time. Curative treatment options include partial or total removal of the pancreas to prevent metastasis. Postoperative morbidity is high (30%–40%), and patients generally require intensive care for at least 24 hours after surgery.
Localized Pancreatic Tumor:
If a tumor of the pancreas is localized and blood vessels are not impacted by the tumor, surgery is often recommended to remove the tumor. In many cases after surgery, the physician will recommend additional therapy to prevent the cancer from growing back, such as chemotherapy, radiation therapy, or both.
Pancreatic Surgeries: There are several different types of surgeries used to remove a localized pancreatic tumor. As technology has advanced, options for surgical intervention have advanced, but the type of surgery recommended depends on the stage of cancer and location of the tumor.
- Whipple Procedure is often used to remove tumors in the head of the pancreas.
- Distal pancreatectomy is often used to remove tumors in the tail of the pancreas.
- Total pancreatectomy is removal of the entire pancreas, and often removal of gallbladder, spleen, and other areas as deemed necessary by the surgeon.
- Central pancreatectomy is removal of the middle of the pancreas
Locally Advanced Tumor:
If a tumor impacts blood vessels, surgery is not usually recommended because of potential complications. For many locally advanced tumors, physicians will recommend chemotherapy and radiation therapy to try to shrink the tumor and prevent spread. If the locally advanced tumor shrinks enough and blood vessels are no longer involved, surgery may be recommended.
Symptomatic Treatment: Patents who undergo treatment for pancreatic cancer can experience different symptoms, such as significant pain, jaundice and itching, digestion problems, and depression. Your physician will treat these symptoms if they occur on a case-by-case basis, and may bring in other team members, such as pain management specialists, nutritional counseling, occupational therapy, and psychological counseling/therapy.
Prognosis and Survival of pancreatic cancer
The primary factors that influence prognosis are:
- Whether the tumor is localized and can be completely resected.
- Whether the tumor has spread to lymph nodes or elsewhere.
Exocrine pancreatic cancer is rarely curable and has an overall survival rate of less than 6% 7.
The highest cure rate occurs if the tumor is truly localized to the pancreas; however, this stage of disease accounts for less than 20% of cases. For patients with localized disease and small cancers (<2 cm) with no lymph node metastases and no extension beyond the capsule of the pancreas, complete surgical resection is associated with an actuarial 5-year survival rate of 18% to 24% 8.
Surgical resection is the mainstay of curative treatment and provides a survival benefit in patients with small, localized pancreatic tumors. Patients with unresectable, metastatic, or recurrent disease are unlikely to benefit from surgical resection.
Pancreatic tumors are resistant to treatment with chemotherapy and radiation.
Patients with any stage of pancreatic cancer can appropriately be considered candidates for clinical trials because of the poor response to chemotherapy, radiation therapy, and surgery as conventionally used.
What are Pancreatic Cysts
With increasing use of imaging tests such as computed tomography (CT) or magnetic resonance imaging (MRI), pancreatic cysts are now being detected with increasing frequency 9. If you or someone you care about has been recently diagnosed with a cyst of the pancreas, you are not alone.
In many cases, these cysts are detected on a CT or MRI scan obtained for an entirely different reason. After being informed of this new finding, you may have already searched the internet to learn more about the nature of these cysts. Unfortunately, much of the scientific literature is filled with a dizzying array of terms like serous cystadenoma, intraductal papillary mucinous neoplasia or mucinous cystic neoplasm. The sheer complexity of the nomenclature can be discouraging when trying to figure out 1) Do I have cancer? and 2) If not, what are the chances that this cyst may some day develop into a cancer?
Where to begin ?
Because of the wide variety of cysts than can arise in the pancreas, it’s a good idea to schedule a visit with someone that has experience in managing these lesions. Several centers around the country including now offer comprehensive consultation services for the evaluation of pancreatic cysts. There are several additional steps you can take to be as informed as possible: 1) keep a copy of both the original report and actual digital images from your imaging test: you are entitled to copies of these as part of your medical record. The actual images on a compact disc or other digital media will enable you to quickly obtain a second opinion if necessary. 2) Be proactive. Ask your local provider what type of cyst they think you have and why. Are there additional tests that they recommend? Do they think a second opinion would be worthwhile? 3) Know your history. Have you ever had acute pancreatitis? This is important information for your physician to know, as fluid collections that arise as a result of acute pancreatitis are very different from other types of cysts in the pancreas.
A bit of background
In general, there are two main varieties of pancreatic cysts based on the type of fluid they contain. The most common cysts are either serous (containing a thin type of fluid) or mucinous (containing a thicker, more viscous fluid). For the most part, serous cysts tend to be benign (non-cancerous). Most of the mucinous cysts are benign as well although there are a few subtypes that can be more concerning. These include the mucinous cystic neoplasm (MCN) that contain ovarian tissue and are almost exclusively found in women as well as main-duct intrapapillary mucinous neoplasm (IPMN), a type of mucinous cyst that contains many tiny fingerlike projections that involves the main pancreatic duct.
What’s next ?
In many cases, your doctor may be able to get a sense of what type of cyst you have based on the already available imaging tests. Otherwise, MRI can be especially useful for further characterization. If potentially concerning features are detected on imaging studies or if there remains significant uncertainty related to the nature of the cyst, additional information can be gained by an endoscopic ultrasound. This test is similar to a regular ultrasound (as in pregnancy) except that we use a probe connected to an endoscope. Once the endoscope is passed into the stomach, we can obtain up-close images of the pancreas. If you have never had upper endoscopy, the procedure is relatively brief and uses sedation similar to that used for colonoscopy. Using endoscopic ultrasound, we can also obtain a sample of the fluid from the cyst, which can provide further diagnostic information.
What treatment is available ?
At present, the only curative treatment is surgery. As any surgery on the pancreas is a major undertaking. Therefore, it is best to reserve resection for cases in which there is a significant concern for cancer. This represents a minority of cases. In the vast majority of cases, surveillance with periodic imaging tests is all that is needed.
What approach is going to work best for you ?
You should be aware that the management of these cysts continues to evolve. Researchers in the field are working diligently to identify more accurate early markers of malignancy. Further research is being conducted to determine the best surveillance interval to monitor these cysts. In the meantime, it is important that you work together with your healthcare provider to arrive at the best management plan to suit your individual needs.
What are Pancreatic Fluid Collections
Pancreatic fluid collections result from many causes, including damage to the pancreas or premalignant or malignant conditions 10. Fluid collections can be large and cause symptoms such as pain and fevers, although most are smaller and asymptomatic.
Classification of Pancreatic Fluid Collections
There are many types of pancreatic fluid collections. The most common is called a pancreatic pseudocyst. These collections are called “pseudocysts” because they lack what is called an epithelial layer, which is typically present in “true” cysts. However, pseudocysts always develop as a result of injury to the pancreas and are defined by the fact that that are fluid filled. Most pseudocysts are asymptomatic and will resolve on their own. However, occasionally, these need to be drained if pain, fever or infection develop. Another type of fluid collection that results from pancreatic injury is called Walled Off Pancreatic Necrosis or “WOPN.” In the past, WOPN has been called other terms such as pancreatic abscess. These collections are similar to pseudocysts in that they result from injury to the pancreas. However, in contrast, these are filled with solid debris, and usually do not resolve on their own without operative intervention. There are many types of fluid collections that are termed cystic neoplasms. However, the vast majority of these fluid collections will not develop into cancer because they are so slow growing 10. These cysts have names such as intraductal papillary neoplasms (IMPN), mucinous neoplasms (MCN) and serous cystadenoma (SCA). Occasionally, these cysts will need to be removed operatively when they are first diagnosed. However, most do not need to be removed 10. It is important, however, that if you are found to have one of these types of fluid collections, that it be followed carefully by your physician to make sure it does not transform into a malignancy. Other types of fluid collections, such as inclusion cysts, are benign and do not need to be removed.
Diagnosis of Pancreatic Fluid Collections
The most important diagnostic consideration for fluid collections is a good clinical history to be taken by your physician. For example, in patients who have had acute pancreatitis and developed a fluid collection, the most likely type of fluid collection is a pseudocyst or WOPN. Your physician usually will want to take a picture of the fluid collection either with a computed tomography (CT) or Magnetic Resonance Imaging (MRI) scan. Both are painless and non-invasive, and will generally be a good indicator of the type of collection present. Occasionally, your physician may want to evaluate the collection with a procedure called an endoscopic ultrasound (EUS). This procedure, in which an endoscope is passed via the mouth while the patient is sedated, allows a specialist to evaluate the cyst with very good accuracy by using an internal ultrasound device. The device also allows for sampling of the fluid collection, which is often helpful to determine its cause. There are also a collection of blood and fluid tests that can be helpful in determining the cause of the fluid collection.
Treatment of Pancreatic Fluid Collections
The type of treatment recommended will depend on the type of fluid collection. For benign fluid collections like psudocysts or WOPN, the treatment is usually observation unless symptoms develop. If symptoms develop, endoscopic or operative drainage is generally recommended. For fluid collections that have the opportunity to transform into cancer, most of these collections can be watched closely without intervention. Occasionally, however, depending on the type of collection, its size, the underlying characteristics of the patient, and the rate at which the collection is growing, operative intervention may be recommended. It is important to discuss all management options with your physician prior to proceeding with any operative resection.
Conclusions
Pancreatic fluid collections are very common and the vast majority will never develop into any serious medical issue 10. However, it is important that they be accurately diagnosed and if any worrisome features are noted, they be removed 10. Specialists such as gastroenterologists, pancreatic surgeons, or medical oncologists should be consulted in virtually all instances when a pancreatic fluid collection is discovered.
What Are Pancreatic Neuroendocrine Tumors
Pancreatic neuroendocrine tumors are less common than the more familiar pancreatic adenocarcinoma, comprising about 5% of pancreas tumors 11. Pancreatic neuroendocrine tumors arise from cells in the pancreas called islet cells. Islet cells are that part of the pancreas which makes chemicals called hormones that are released into the bloodstream and regulate certain body functions.
Pancreatic adenocarcinoma, which causes over 90% of pancreatic cancers, arise from the cells which line the cells of the drainage tubes of the pancreas – the ductal cells. As a result, pancreatic neuroendocrine tumors and pancreatic adenocarcinoma behave in very different ways.
In general, pancreatic neuroendocrine tumors grow at a much, much slower rate than pancreatic adenocarcinoma. While each type of tumor can spread (metastasize) from the pancreas to other organs, pancreatic neuroendocrine tumors usually spread over a period of years. Pancreatic adenocarcinoma, on the other hand, typically spreads over a period of months.
Treatment of pancreatic neuroendocrine tumors
The cure for both types of tumors is surgery. If the tumor cannot be removed, chemotherapy is often given to try and prevent the tumor from growing further. The type of chemotherapy is different for each type of tumor.
In very rare situations, liver transplants are performed in patients who have neuroendocrine tumors which have spread to the liver. The rationale behind this is that because neuroendrocine tumors are so slow growing, removing the entire tumor in the liver with a transplant allows for several more years of life. Again, because pancreatic adenocaricnoma is faster moving, liver transplants are not offered in this disease when it has spread to the liver.
Summary
While both pancreatic neuroendocrine tumors and adenocarcinoma arise from the pancreas, they are vastly different in terms of prognosis. Adenocarcinomas are unfortunately much more common than neuroendocrine tumors, and typically have a worse overall prognosis.
What is Zollinger-Ellison syndrome
Zollinger-Ellison syndrome is a rare disorder characterized by the development of a tumor called a gastrinoma found in the pancreas and/or duodenum 12. Gastronoma’s secrete excessive levels of gastrin, a hormone that stimulates production of acid by the stomach. Normally, the body releases small amounts of gastrin after eating, which triggers the stomach to make gastric acid that helps break down food and liquid in the stomach. The extra acid causes peptic ulcers to form in the duodenum and elsewhere in the upper intestine.
Although anyone can get Zollinger-Ellison syndrome, the disease is more common among men 30 to 50 years old. The prevalence of the disease occur in approximately 10 per million of the population.1 Also a child who has a parent with MEN1 is also at increased risk for Zollinger-Ellison syndrome 13.
Medical researchers are still studying the exact cause of Zollinger-Ellison syndrome. About 25 to 30 percent of Gastrinoma’s are caused by an inherited genetic disorder called multiple endocrine neoplasia type 1 (MEN1) 14. Multiple endocrine neoplasia type 1 (MEN1) causes hormone-releasing tumors in the endocrine glands and the duodenum. Symptoms of MEN1 include increased hormone levels in the blood, kidney stones, diabetes, muscle weakness, weakened bones, and fractures.
Symptoms of Zollinger-Ellison syndrome
Zollinger-Ellison syndrome signs and symptoms are similar to those of peptic ulcers. A dull or burning pain felt anywhere between the navel and midchest is the most common symptom of a peptic ulcer.
Other symptoms Zollinger-Ellison syndrome include:
- diarrhea
- mild to severe abdominal pain
- steatorrhea (increased amounts of fat in the stools)
- bloating
- burping
- nausea
- vomiting
- weight loss
- poor appetite
Some people with Zollinger-Ellison syndrome have only diarrhea, with no other symptoms. Others develop gastroesophageal reflux (GER), which occurs when stomach contents flow back up into the esophagus.
How are Gastrinoma’s diagnosed ?
A diagnosis of a Gastrinoma should be considered in a patient with peptic ulcers that recur frequently and are resistant to treatment. A medical professional may suggest a biochemical study called the Secretin Stimulated blood test to check for an elevated gastrin level after an infusion of secretin.
Secretin is a hormone that causes Gastrinoma’s to release more gastrin. A technician or nurse places an intravenous (IV) needle in a vein in the arm to give an infusion of secretin. A medical professional may suspect Zollinger-Ellison syndrome if blood drawn after the infusion shows an elevated gastrin level. Once a diagnosis is made, localizing the tumor is important. Most Gastrinoma are small lesions and therefore, localizing the tumor may be difficult. Some of the tests that are performed to localize the tumor include a CT scan, octreotide scan and MRI and an endoscopic ultrasound.
An experienced surgeon will detect these tumors at surgery even when they are not visible on preoperative imaging tests.
How are Gastrinoma’s treated ?
Treatment of choice for Gastrinoma is to remove the surgically where possible. Peptic ulcers must be aggressively treated and controlled prior to surgery. The type of surgery for Gastrinoma’s depends on the location of the tumor. Since these tumors may frequently occur at more than one spot in the pancreas and the surrounding tissues more than one procedure may be required. The following operative procedures may be utilized to treat Gastrinoma’s.
- Enucleation: Many small Gastrinoma’s in the pancreas may be treated by enucleation alone. This is a procedure of choice for patients that have small tumors (less than 1cm) where the tumor is located on the surface of the pancreas.
- Resection of the pancreas: in patients with large tumors a distal pancreatectomy or a Whipple operation may be indicated depending on where the tumor is located in the pancreas.
- Duodenal exploration: Gastrinomas often occur in the wall of the duodenum (first part of the intestine) and therefore opening duodenum and carefully feeling it to remove any tumors in this area is important.
- Lymph nodes: In some patients the tumor may be located in the lymph glands outside the pancreas therefore careful palpation and removal of these glands is important at the time of surgery
In some affected individuals with aggressively invasive Gastrinoma, recommended treatment may include the use of certain anticancer drugs (chemotherapy) to help reduce tumor mass and blood gastrin levels.
Genetic counseling may be of benefit for affected individuals and their families. Other treatment for this disease is symptomatic and supportive.
- Pancreatitis. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis[↩][↩][↩]
- Russo MW, Wei JT, Thiny MT, et al. Digestive and liver disease statistics, 2004. Gastroenterology. 2004;126:1448–1453.[↩]
- EXOCRINE PANCREATIC INSUFFICIENCY (EPI). The National Pancreas Foundation. https://pancreasfoundation.org/patient-information/ailments-pancreas/exocrine-pancreatic-insufficiency-epi/[↩]
- Pancreas Divisum. The National Pancreas Foundation. https://pancreasfoundation.org/patient-information/ailments-pancreas/pancreas-divisum/[↩]
- About Pancreatic Cancer. The National Pancreas Foundation. https://pancreasfoundation.org/patient-information/pancreatic-cancer/[↩]
- Pancreatic Cancer Risks and Symptoms. The National Pancreas Foundation. https://pancreasfoundation.org/patient-information/pancreatic-cancer/pancreatic-cancer-risks-and-symptoms/[↩]
- Siegel R, Naishadham D, Jemal A: Cancer statistics, 2013. CA Cancer J Clin 63 (1): 11-30, 2013. http://onlinelibrary.wiley.com/doi/10.3322/caac.21166/full[↩]
- Yeo CJ, Abrams RA, Grochow LB, et al.: Pancreaticoduodenectomy for pancreatic adenocarcinoma: postoperative adjuvant chemoradiation improves survival. A prospective, single-institution experience. Ann Surg 225 (5): 621-33; discussion 633-6, 1997. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1190807/[↩]
- Pancreatic Cysts. The National Pancreas Foundation. https://pancreasfoundation.org/patient-information/ailments-pancreas/pancreatic-cysts/[↩]
- Pancreatic Fluid Collections. The National Pancreas Foundation. https://pancreasfoundation.org/patient-information/ailments-pancreas/pancreatic-fluid-collections/[↩][↩][↩][↩][↩]
- Pancreatic Neuroendocrine Tumors. The National Pancreas Foundation. https://pancreasfoundation.org/patient-information/pancreatic-cancer/pancreatic-neuroendocrine-tumors/[↩]
- Zollinger-Ellison Syndrome/Gastrinoma. The National Pancreas Foundation. https://pancreasfoundation.org/zollinger-ellison-syndromegastrinoma/[↩]
- Del Valle J. Zollinger-Ellison syndrome. In: Yamada T, ed. Textbook of Gastroenterology. 5th ed. Hoboken, NJ: Blackwell Publishing; 2009: 982–1002.[↩]
- Metz DC. Diagnosis of the Zollinger-Ellison syndrome. Clinical Gastroenterology and Hepatology. 2012;10(2):126–130.[↩]